Abstract
Arterial aneurysms are very rare in children, with iliac aneurysms being even more uncommon. We report the case of a 61-day-old girl with a right common iliac artery aneurysm that was an incidental finding on the third day of life. The aneurysm was treated by direct aneurysm puncture and endovascular coil embolization. The patient was discharged with no complications, and complete exclusion of the aneurysm was confirmed on the 3-month follow-up examination.
Keywords: Iliac aneurysm, Neonate, Children, Coil
Arterial aneurysms are very rare in children, with iliac aneurysms being even more uncommon. Most of these aneurysms have been reported in only a few cases or small series. We report the case of an incidentally found right common iliac artery (RCIA) aneurysm in a 61-day-old girl and describe diagnostic workup and treatment by direct aneurysm puncture and endovascular coil embolization. A written consent for publication was obtained from the patient's parents.
Case report
A 42-day-old female neonate presented to our university hospital with an RCIA aneurysm. The patient, weighing 3.1 kg, was born by cesarean section at 35 weeks' gestation because of shoulder presentation. Apart from that, the pregnancy was uncomplicated. Apgar scores of 8 and 8 were assigned at 1 minute and 5 minutes. She was started on mechanical ventilation and received surfactant therapy at 13 hours of life. The mechanical support was maintained until the third day of life. Blood culture was negative. Because of progression of changes depicted on chest radiography, she was started on empirical antibiotics. On her third day of life, an abdominal ultrasound examination routinely performed in premature newborns revealed RCIA aneurysm. No central lines or other vascular interventions were done in the hospital where the aneurysm was diagnosed.
Before admission to our hospital, computed tomography angiography (CTA) and magnetic resonance (MR) examinations were performed. However, both examinations were of unsatisfactory diagnostic value to delineate details because of improper phase or motion artifacts.
On physical examination, there were no features to suggest a connective tissue disorder or genetically triggered disease. There was no family history of aneurysms, connective tissue disorders, or genetic defects. Echocardiography and MR of the head and neck, the findings of which were normal, were performed to exclude other vascular anomalies. We thought that additional CTA was justified because of the different therapeutic approaches considered. Ultrasound revealed the yin-yang sign, indicating bidirectional flow due to swirling of blood within the aneurysm (Fig 1). CTA showed an irregular aneurysm located in the RCIA (Fig 2). Only the proximal part of the RCIA was depicted, which was 9 mm in length and 4.5 mm in diameter. The contralateral common iliac artery was 3 mm in diameter; the aorta above the bifurcation was 4.5 mm. The right external iliac artery was not seen, and blood supply to the right common femoral artery was from collateral circulation.
Fig 1.

Doppler ultrasound revealing yin-yang sign, indicating bidirectional flow within the aneurysm.
Fig 2.
Computed tomography angiography (CTA). A, Three-dimensional volume rendered image showing a right common iliac artery (RCIA) aneurysm. The right common femoral artery is supplied by collateral circulation. B, Axial image.
On the basis of change in size (from 33 × 26 × 25 mm to 45 × 37 × 32 mm in 34 days), involving greater risk of rupture and sufficient collateral blood supply to the lower extremity, we decided to treat the aneurysm. On the day of treatment, the patient was 61 days old. In the first step, under ultrasound guidance, the aneurysm was directly punctured through the abdominal wall. Before thrombin injection, we performed direct aneurysmography to exclude communication with the external iliac artery. In addition, before the procedure, the aorta was compressed under ultrasound guidance to assess flow change in the aneurysm. With the use of 350 units of thrombin, approximately three-fourths of the volume of the aneurysm was excluded. Unfortunately, thrombin injection was ineffective, presumably because of high flow in the aneurysm. In case of thrombin embolized distally, thrombolytic therapy should be applied.
Through the other direct puncture, six coils (total coil length of 170 cm) were inserted in the remaining part of the aneurysm. However, the first loop of the last coil had been replaced to the contralateral left common iliac artery. Because of high risk of damaging the artery while retrieving the coil, it was decided to stop the procedure.
The next day, radiography showed spontaneous retrieval of the coil to the aneurysm. Two days later, the second step of treatment was performed through the left femoral approach. With the use of three coils (total coil length of 120 cm), the remaining part of the aneurysm and its neck were completely excluded (Fig 3). Before the intervention, the collateral flow to the right lower extremity was through lumbar, iliolumbar, epigastric, median sacral, and obturator arteries. After the intervention, collateral flow through the median sacral artery was more prominent.
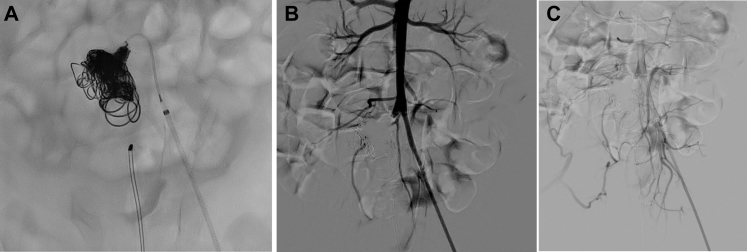
Fig 3.
A, Deployment of the last coil. B and C, Final digital subtraction angiography showing complete exclusion of the aneurysm (B) with prevention of the blood supply to the lower right extremity (C).
There were no complications related to the last procedure. On the 3-month follow-up Doppler ultrasound examination, there was no flow in the aneurysm. Both lower extremities were equally warm, with no relative growth arrest.
Discussion
Aneurysms in the pediatric population are very rare. Moreover, there are just a few case reports regarding iliac aneurysms.1, 2, 3, 4, 5, 6, 7, 8 Based on autopsy series in adults, the incidence of isolated iliac artery aneurysms is approximately 0.03%.9 The idiopathic etiology is the rarest, with most of these aneurysms being multiple.10 Aneurysms in multiple locations are uncommon; however, complete examination of the vascular system should be performed.11 In our patient, the complete vascular system was assessed with different modalities. Apart from the RCIA aneurysm, no other aneurysms were depicted.
In our patient, there was no history of trauma (including umbilical artery catheterization); there were no signs of vascular malformation or connective tissue disorders. Shortly after delivery, our patient presented with clinical and radiographic signs of pneumonia. However, blood culture was negative, making diagnosis of mycotic aneurysm less likely. With no specific cause, the aneurysm was classified as congenital-idiopathic.
Aneurysms, if left untreated, may lead to death as a result of rupture or limb loss due to thrombosis or distal embolization.12 The patient's age, future vessel growth, and equipment size are also an issue. Khandanpour et al5 reported successful treatment of an internal iliac aneurysm by coil embolization. Our case also supports this approach, being effective in the neonate.
In our patient, the external iliac artery was not completely visualized on pretreatment imaging. However, before thrombin injection, direct aneurysmography was performed to exclude communication with the external or internal iliac artery. In case of visualization of iliac artery patency, open surgery should be considered. Reconstruction materials include prosthetic grafts, reversed saphenous veins, and cryopreserved veins.13 In pediatric patients, autologous grafts should be the first choice. Zimmermann et al2 reported the case of an 11-year-old child with common iliac artery aneurysm. They resected the aneurysm and replaced it by a reversed femoral vein with additional bypass with a reversed great saphenous vein because of external iliac artery atrophy.
Because of the issue of radiation exposure, ultrasound is the modality of choice for follow-up in children. We plan to perform ultrasound every 3 months for the first year and then once a year in an uncomplicated scenario. MR is superior for whole body imaging, but it requires anesthesia for stillness in small children. Once the child is mature enough (eg, 6-8 years old), we plan to perform whole body MR imaging. In addition, limb length measurements are obtained. Inadequate perfusion would result in growth arrest, and limb growth measurement combined with ultrasound follow-up should be optimal. If the limb is not growing appropriately, open surgery with the use of reconstruction materials should be considered.
To the best of our knowledge, this is the youngest patient to be diagnosed with iliac artery aneurysm. Arterial aneurysms in pediatric patients are very rare. In spite of being an incidental finding in many cases, prompt surgical treatment is required because of the risk of rupture or distal embolization complications. Surgical treatment requires an individualized approach because of the small vessels and future growth.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Lucas A., Kerdiles Y., Guias B., Cordon A., Calon E. Iliac aneurysm in a child complicating umbilical artery catheterization. Ann Vasc Surg. 1994;8:500–505. doi: 10.1007/BF02133072. [DOI] [PubMed] [Google Scholar]
- 2.Zimmermann A., Kuehnl A., Seidl S., Eckstein H.H. Idiopathic aneurysm of the common iliac artery in an 11-year-old child. J Vasc Surg. 2009;50:663–666. doi: 10.1016/j.jvs.2009.04.056. [DOI] [PubMed] [Google Scholar]
- 3.Chithra R., Ajai Sundar R., Velladuraichi B., Sritharan N., Amalorpavanathan J., Vidyasagaran T. Pediatric isolated bilateral iliac aneurysm. J Vasc Surg. 2013;58:215–216. doi: 10.1016/j.jvs.2012.11.036. [DOI] [PubMed] [Google Scholar]
- 4.Taketani S., Imagawa H., Kadoba K., Sawa Y., Sirakura R., Matsuda H. Idiopathic iliac arterial aneurysms in a child. J Pediatr Surg. 1997;32:1519–1521. doi: 10.1016/s0022-3468(97)90582-0. [DOI] [PubMed] [Google Scholar]
- 5.Khandanpour N., Chaudhuri A., Roebuck D.J., Armon M.P. Neonatal mycotic internal iliac aneurysm due to methicillin-resistant Staphylococcus aureus (MRSA) septicaemia successfully treated by coil embolisation. Eur J Vasc Endovasc Surg. 2007;33:687–689. doi: 10.1016/j.ejvs.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 6.Lee J., Oh C., Youn J.K., Han J., Kim H., Jung S. Right iliac arterial aneurysm in a 4-year-old girl who does not have a right external iliac artery. Ann Surg Treat Res. 2016;91:265–268. doi: 10.4174/astr.2016.91.5.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoshiko F.M., Zampieri E.H., Dalio M.B., Dezotti N.R., Joviliano E.E. Repair of ruptured iliac artery aneurysm in a child. J Vasc Bras. 2017;16:48–51. doi: 10.1590/1677-5449.008616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis F.M., Eliason J.L., Ganesh S.K., Blatt N.B., Stanley J.C., Coleman D.M. Pediatric nonaortic arterial aneurysms. J Vasc Surg. 2016;63:466–476. doi: 10.1016/j.jvs.2015.08.099. [DOI] [PubMed] [Google Scholar]
- 9.Brunkwall J., Hauksson H., Bengtsson H., Bergqvist D., Takolander R., Bergentz S.E. Solitary aneurysms of the iliac arterial system: an estimate of their frequency of occurrence. J Vasc Surg. 1989;10:381–384. doi: 10.1067/mva.1989.13733. [DOI] [PubMed] [Google Scholar]
- 10.Callicutt C.S., Rush B., Eubanks T., Abul-Khoudoud O.R. Idiopathic renal artery and infrarenal aortic aneurysms in a 6-year-old child: case report and literature review. J Vasc Surg. 2005;41:893–896. doi: 10.1016/j.jvs.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 11.English W.P., Edwards M.S., Pearce J.D., Mondi M.M., Hundley J.C., Hansen K.J. Multiple aneurysms in childhood. J Vasc Surg. 2004;39:254–259. doi: 10.1016/j.jvs.2003.07.019. [DOI] [PubMed] [Google Scholar]
- 12.Halpern V., O’Connor J., Murello M., Siegel D., Cohen J.R. Multiple idiopathic arterial aneurysms in children: a case report and review of the literature. J Vasc Surg. 1997;25:949–956. doi: 10.1016/s0741-5214(97)70229-5. [DOI] [PubMed] [Google Scholar]
- 13.Kaye A.J., Slemp A.E., Chang B., Mattei P., Fairman R., Velazquez O.C. Complex vascular reconstruction of abdominal aorta and its branches in the pediatric population. J Pediatr Surg. 2008;43:1082–1088. doi: 10.1016/j.jpedsurg.2008.02.035. [DOI] [PubMed] [Google Scholar]