Abstract
Approximately 700,000 people die of Hepatocellular Carcinoma (HCC) each year worldwide, making it the third leading cause of cancer related deaths. Rupture is a potentially life-threatening complication of HCC. The incidence of HCC rupture is higher in Asia and Africa than in Europe. In Asia approximately 10% of patients with a diagnosis of HCC die due to rupture each year. Spontaneous rupture is the third most common cause of death due to HCC after tumor progression and liver failure. The diagnosis of rupture in patients without history of cirrhosis or HCC may be difficult. The most common symptom of ruptured HCC is abdominal pain (66–100%). Shock at presentation can be seen in 33–90% of cases; abdominal distension is reported in 33%. Abdominal paracentesis documenting hemoperitoneum is a reliable test to provisionally diagnose rupture of HCC, it can be seen in up to 86% of clinically suspected cases. The diagnoses can be confirmed by computed tomography scan or ultrasonography, or both in 75% of cases. Careful pre-treatment evaluation is essential to decide the best treatment option. Management of ruptured HCC involves multi-disciplinary care where hemostasis remains a primary concern. Earlier studies have reported a mortality rate of 25–75% in the acute phase of ruptured HCC. However, recent studies have reported a significant decrease in the incidence of mortality. There is also a decrease in the incidence of ruptured HCC due to improved surveillance and early detection of HCC. Transarterial Embolization is the least invasive method to effectively induce hemostasis in the acute stage with a success rate of 53–100%. Hepatic resection in the other hand has the advantage of achieving hemostasis and in the same go offers a potentially curative resection in selected patients.
Abbreviations: CTP, Child Turcotte Pugh; HBV, Hepatitis B Virus; HCC, Hepatocellular Carcinoma; HCV, Hepatitis C Virus; TACE, Trans-arterial Chemo-embolization; TAE, Transarterial Embolization; VEGF, Vascular Endothelial Growth Factor
Keywords: hepatocellular carcinoma, spontaneous rupture, hemoperitoneum, transarterial embolization
Approximately 700,000 people die of Hepatocellular Carcinoma (HCC) each year worldwide, making it the third leading cause of cancer related deaths.1 HCC develops in the background of cirrhotic liver in 85–95% of cases.2 Spontaneous rupture is a potentially life-threatening complication of HCC. The mortality due to rupture of HCC in the acute phase is reported to be high at 25–75%, however, with earlier detection of HCC the incidence of rupture is decreasing.3, 4 In Asia, approximately 10% of patients with a diagnosis of HCC die due to rupture each year.5 Spontaneous rupture is the third most common cause of death due to HCC after tumor progression and liver failure.6 In ruptured HCC the best treatment approach is still debated. Primary goals remain correction of hypovolemic shock and stabilization of the patient.4, 6 The outcome of conservative treatment alone is generally poor, with a hospital mortality rate of 85–100%.7, 8 Hence, after initial resuscitation and stabilization therapeutic options should be decided and individualized according to underlying liver function, tumor stage and feasibility for resection. Management of ruptured HCC involves multidisciplinary care where hemostasis remains a primary concern. Transarterial Embolization (TAE) effectively induces hemostasis in the acute stage with a success rate of 53–100%.4, 9, 10, 11 Hepatic resection in the other hand has the advantage of achieving hemostasis and in the same go, potentially curative resection of the tumor offers a hope for cure in selected patients.4
Incidence
The reported incidence of HCC rupture shows a distinct global variation. In the West, the incidence of HCC is increasing but HCC ruptures are relatively uncommon, with an incidence of less than 3%.12, 13, 14 However, in Asia and Africa, the incidence is considerably higher, ranging between 3% and 26%.14, 15 The incidences of ruptured HCC reported from around the globe are 10% from Japan, 12.4% from Thailand, 12.7% from southern Africa, 14.5% from Hong Kong, 26% from Taiwan and 3% from United Kingdom.7, 8, 13, 16, 17, 18, 19, 20 There is a recent decrease in the incidence of mortality due to ruptured HCC; earlier in Japan spontaneous rupture of HCC was responsible for 10% of deaths among HCC patients, which has decreased to 6.4% according to recent report.21 There are few case reports and case series of HCC rupture from India, however there is no data on the exact incidence of HCC rupture from India.22, 23, 24, 25, 26
Pathophysiology
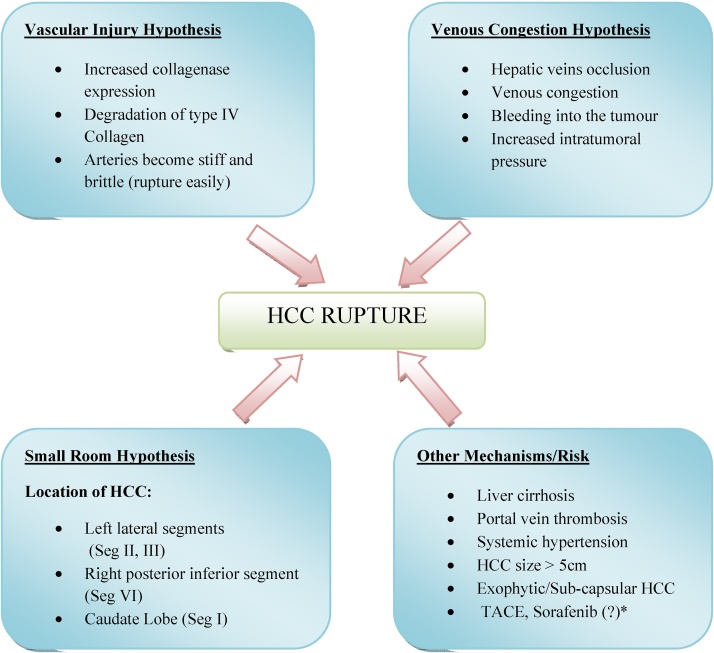
The mechanism of spontaneous HCC rupture has not been fully understood. In order to precisely explain the mechanism of rupture, several hypotheses have been proposed. Normal hepatic parenchyma surrounding the HCC can protect the tumor from rupture.27 A centrally located HCC must grow large enough to reach up to the liver surface before it ruptures. A thin hepatic parenchyma surrounding the HCC makes the tumor prone for rupture. Caudate lobe HCC or HCC which is subcapsular in location tend to rupture earlier and at a relatively smaller size compared to a centrally located HCC.27 Tumor in the left lobe of liver are at high risk of rupture due to relatively small room for a space occupying lesion, compared to that in the right lobe.20 The following hypotheses have been proposed to explain the pathophysiology of HCC rupture (Figure 1).
Figure 1.
Pathogenesis of rupture of hepatocellular carcinoma (proposed hypotheses & risk factors). Liver segments are classified according to the Couinaud (French) classification. HCC: Hepatocellular Carcinoma; TACE: Trans-arterial Chemoembolization. *Treatment with Sorafenib (a multi-kinase inhibitor) contributing to the risk of HCC rupture is doubtful in view of lack of enough data.
The Small Room Hypothesis
Li et al. in a series of 89 cases of ruptured HCC reported that most tumors were localized to the left lateral segments (seg II and III) and right posterior-inferior segment (seg VI). Compared to other parts of the liver, these segments have relatively small room restricted outside by the tough liver capsule.27 Therefore when the tumor grows beyond its capacity the inner pressure splits open the surrounding parenchyma and tear the capsule leading to rupture.27 Many studies have reported that HCC size more than 5 cm are associated with high risk of rupture.15, 20 However, size is not an absolute criterion for rupture, as HCC as small as 2 cm have been found to have ruptured.3
The Vascular Injury Hypothesis
Zhu et al. proposed that, specific changes in the arterial wall supplying the tumor are the main cause of HCC rupture.28, 29 This explains why some of the small tumors may also present with rupture.30 Vascular injuries included increased collagenase expression, elastin proliferation, and degradation of type IV collagen fibrils. These changes more selectively were seen in the small arteries and in the biopsy specimen from ruptured HCC than that from non-ruptured HCC. These pathological changes make the small arteries supplying the tumor stiff and brittle, which rupture easily when subjected to increase in vascular load secondary to portal hypertension or minor trauma.28, 29, 30
The Venous Congestion Hypothesis
Invasion and occlusion of hepatic veins results in increased pressure within the tumor which lead to the rupture of HCC.31, 32 The consequent venous congestion in combination with various factors like tumor necrosis and coagulopathy lead to intratumoral hemorrhage and subsequent increase in intratumoral pressure leading to rupture.4, 8 Necrosis within the tumor or a rapid growth of the tumor can also lead to increased intratumoral pressure and consequent rupture.4
Rupture Related to Previous Treatment
Rupture of HCC has also been reported in patients previously treated with Trans-arterial Chemo-embolization (TACE) with an incidence of 0.4–0.9%.33, 34, 35 Exact pathogenesis is not clear but it may be related to acute ischemic necrosis of the liver capsule surrounding superficial tumors or due to vascular injuries related to TACE.34 In 2 series from Asia involving 3 (n = 351) and 6 (n = 391) patients respectively who had rupture following TACE, large tumor size or extra capsular extension of the tumor appeared to be predisposing risk factors for rupture.34, 36 In a retrospective study, Zhu et al. showed that inflammatory mediators released secondary to vascular injury during TACE digest the elastin and collagen fibrils which predispose to the splitting and rupture of weakened blood vessels.37 Sakamoto et al. reported five cases of multiple intrahepatic aneurysms which developed within 25–45 days after 1300 TACEs and attributed the changes to an acute inflammatory response, leading to weakening of the arterial wall predisposing to aneurysm formation and rupture.36 Rupture of HCC after TACE has been found to have occurred as early as 6 h after the procedure.37 Jia et al.38 in a series of 6 patients, reported that the interval between the procedure and HCC rupture was 2–17 days (Mean [SD] 10.33 days). Another study by Sun et al.39 reported 5 cases of ruptured HCC which developed within 16 h to 7 months after 1005 TACEs. However, there is no such study on the time interval from the diagnosis of HCC and its spontaneous rupture.
Rombola et al. reported a case of HCC rupture and attributed the risk to Sorafenib use.40 Sorafenib, a multikinase inhibitor of the Vascular Endothelial Growth Factor (VEGF) pathway is known to increase the risk of bleeding however, it is unclear whether it could also lead to the risk of rupture of HCC in susceptible individuals.40
Other Risk Factors
In a study by Zhu et al. hypertension, liver cirrhosis, portal vein thrombus and extrahepatic invasion were also found to be independent predictors of spontaneous rupture of HCC.15 In a nationwide study from Japan by Aoki et al.,41 Child Turcotte Pugh (CTP) Score has been shown to be an independent predictor of rupture of HCC, however, other studies have failed to show any relation between CTP score and risk of rupture.15, 27, 42 In most of the reported series of ruptured HCC, chronic viral hepatitis especially due to Hepatitis B Virus (HBV) infection was the predominant underlying etiology of liver disease.10, 11, 15, 27, 43, 44, 45, 46, 47, 48 However, the etiology of liver cirrhosis has not been reported by any study as an independent risk factor for rupture of HCC. The largest series of ruptured HCC by Aoki et al. from Japan also reported chronic viral hepatitis due to Hepatitis C Virus (HCV) followed by HBV infections to be the predominant etiology of cirrhosis and a risk factor of rupture on univariate analysis but failed to show a role as an independent predictor on multivariate logistic regression analysis.41
Some authors have also proposed the role of trauma causing rupture either from outside due to abdominal blunt trauma to a tumor lying close to liver surface or from within as a result of repeated respiratory movements especially for HCC lying close to the diaphragm.8, 32, 49
Clinical Features and Diagnosis
Clinical Presentations
Ruptured HCC is a potentially life threatening situation, its diagnosis in patients without history of cirrhosis or HCC may be difficult. The most common symptom of ruptured HCC is acute abdominal pain which occurs in 66–100% of cases.5, 50, 51 Shock at presentation can be seen in 33–90% of patients.5, 14, 50, 51, 52, 53 Abdominal distension has been reported in 33% of cases.13 In the acute phase liver failure has been reported to occur in 12–42% of patients.4 Abdominal paracentesis documenting hemoperitoneum has been found to be a reliable test to establish the diagnosis of ruptured HCC in up to 86% of clinically suspected cases.5 HCC rupture can also rarely present as hemothorax, more commonly due to rupture of a metastatic HCC in the lungs, than to rupture of a primary tumor in the liver.54
Diagnosis
With active surveillance of HCC in cirrhosis and improvement in the imaging modalities the rate of diagnosis of HCC rupture has gradually improved. On Ultrasound the rupture site appears as a hyperechoic area around the tumor in 66% of cases.55 The diagnoses of rupture of HCC can be confirmed by computed tomography scan or ultrasonography or both in 75% cases.18, 56, 57 According to previous studies, in 20–33% of cases the diagnoses were made only during emergency exploratory laparotomies.14, 18 As per Zhu et al. a correct diagnosis of rupture of HCC was possible in 86% by paracentesis, 66% by ultrasonography, 100% by computed tomography and only in 20% by conventional angiography.32
Computed Tomography Scan
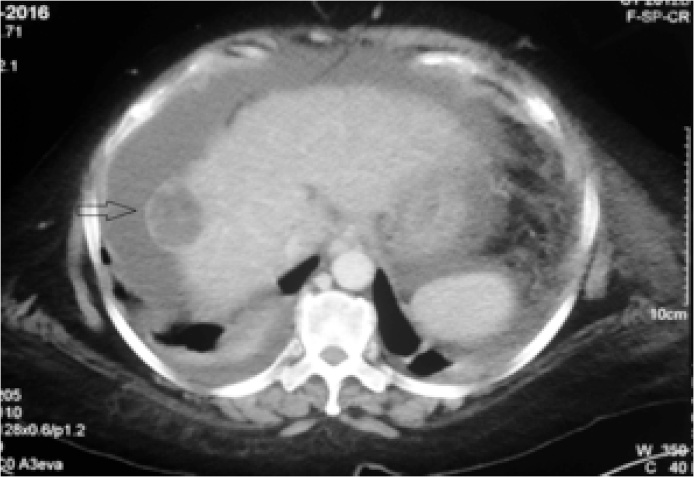
Triple Phase Computed Tomography (TPCT) is the modality of choice in the diagnosis of HCC rupture. There are many findings on TPCT which suggest rupture of HCC, such as peripherally located tumor with a contour bulge, discontinuity of the liver capsule, hemoperitoneum, subcapsular hematoma, active extravasation of contrast, and “enucleation sign”.58, 59, 60, 61, 62, 63 The “enucleation sign” (Figure 2) is defined as separation of tumor content with intraperitoneal rupture into the perihepatic space which is seen as a non enhancing low attenuating lesion with peripheral rim enhancement.61, 62, 63 Low attenuation is due to extensive loss of blood from the tumor and arterial vasoconstriction and ischemic changes secondary to hypovolemic shock. Rim enhancement is due to compressed normal liver parenchyma and does not represent the tumor. The enucleation sign, if associated with surrounding hematoma and/or active contrast extravasation on dynamic contrast enhance CT is highly specific for rupture of HCC.56, 61, 63 The triad of a peripherally located large tumor, a small localized or intraperitoneal collection and apparent retraction of liver capsule underneath the collection have 100% sensitivity for early stage of a confined rupture.59 The indentation on the tumor surface leading to apparent capsular retraction represents compression by the hematoma and not a true capsular retraction (“pseudo retraction sign”).59
Figure 2.
A sub-capsular and exophytic lesion in segment VII of liver with the “enucleation sign (black open arrow) due to rupture of hepatocellular carcinoma, seen as separation of tumor content into the perihepatic space with hypodense center and peripheral rim enhancement on arterial phase of Triple Phase Computed Tomography (TPCT).
Hepatic Artery Angiography
Active extravasations of contrast from the tumor, which is the most important diagnostic feature of rupture of HCC on angiography, can be demonstrated only in 13.2–35.7% of cases (19. 25, 58). Moreover, for active extravasation to be visible on angiography the bleeding from the rupture site should be more than 1 ml/min.60 These facts limit the diagnostic sensitivity of angiography in ruptured HCC. In one study CT scan was found to be more reliable than angiography in detecting the site of active contrast leakage.10 A recent study has described three new angiographic findings called “sentinel signs” (sentinel vessels, hypovascular areas and delayed dots) and showed that they are superior to active contrast extravasation for the diagnosis of a ruptured HCC.64 Sentinel vessels are abnormally dilated and tortuous blood vessels in the tumor vicinity; hypovascular areas are areas within the HCC that lack contrast and delayed dots are dot like residual contrast within the tumor which persists after hepatic angiography.64 A delayed image acquisition of more than 12 s is required to look for the sentinel signs, especially the delayed dots.64 The study also highlights that sentinel signs may not be an appropriate tool to identify rupture of caudate lobe HCC and small HCC, which can only be diagnosed by a hepatic angiogram which is highly selective. In the current era, the diagnosis of an HCC with signs of impending rupture is as important as the diagnosis of already ruptured HCC. A well validated study to prove the diagnostic accuracy of sentinel signs in future could help identify HCC with impending rupture and provide scope for early intervention and improved survival.
Contrast Enhance Ultrasonography (CEUS)
There are only few studies of Contrast Enhanced Ultrasound (CEUS) in the diagnosis of ruptured HCC.65, 66, 67 In a small series of 10 patients with ruptured HCC, CEUS has sensitivity, specificity and diagnostic accuracy of 75%, 50% and 60% respectively, compared to conventional angiography.65 It can reliably differentiate between active leaks from non-active bleeding by demonstrating contrast extravasation into the ascites.65 Jet like extravasation and bubble leakage were two patterns of active bleeding described by Sugihara et al. in rupture of HCC.66 Several contrast agents have been used for CEUS, however, Sonazoid (Daiichi Sankyo, Japan) has been considered a better agent which allows continuous scanning without destruction of the microbubbles.66 Moreover, Sonazoid is cleared through gas exchange via the pulmonary circulation; therefore it is a preferred agent in patients with renal failure.68
Management
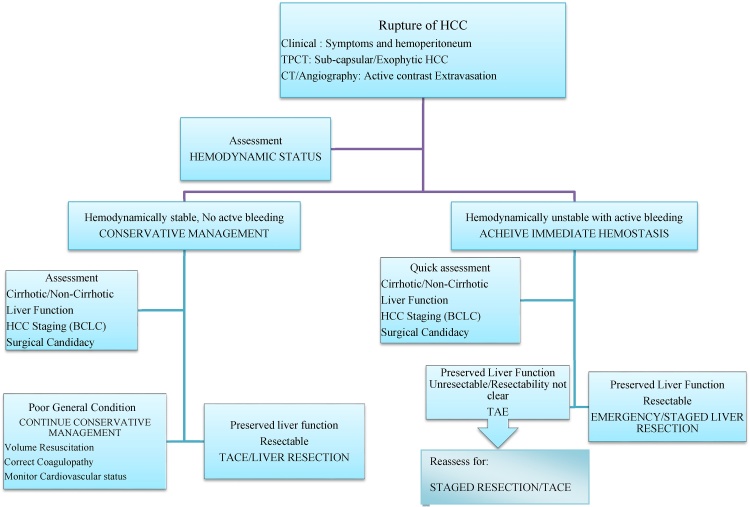
Correction of hypovolemic shock which occurs due to massive intraperitoneal hemorrhage and preservation of liver parenchymal functions are the primary aims of management in ruptured HCC.4, 6, 34 In ruptured HCC the best treatment approach is still debated, a careful pre-treatment evaluation is essential to decide the best treatment option. Treatment should be individualized taking into account various factors like hemodynamic status, underlying liver function, tumor characteristics and stage of HCC.6 Hemodynamically stable patients with no active bleeding should be managed conservatively, followed by a definitive treatment like liver resection or TACE.69 Patients who are hemodynamically unstable, hemostasis should be achieved immediately. A management algorithm has been proposed here to guide the best treatment approach for patients presenting with HCC rupture to the emergency room (Figure 3).
Figure 3.
The proposed management algorithm for rupture of hepatocellular carcinoma. HCC: Hepatocellular Carcinoma; TPCT: Triple Phase Computed Tomography Scan; BCLC: Barcelona Clinic Liver Cancer staging; TAE: Trans-arterial Embolization; TACE: Trans-arterial Chemoembolization.
Conservative Management
Conservative treatment consists of volume resuscitation, blood transfusion, correction of coagulopathy and cardiovascular monitoring. While conservative management being initiated, a thorough assessment of liver function and tumor stage should be performed to determine the eligibility for TAE or hepatic resection. The outcomes of conservative treatment alone however are generally poor with a hospital mortality rate of 85–100% and a median survival as low as 13 days.8 In a large multicentre study from China involving 162 patients with ruptured HCC presenting as hemorrhagic shock, out of the 35 patients who received only conservative treatment, 32 (91%) patients died and the causes of 30 day mortality in them were re-bleeding in 21 (65.6%) patients and liver failure in 9 (28.1%) patients.48 Most HCC has a rich blood supply derived largely from the hepatic artery, thus the risk of continuous and recurrent bleeding is higher with conservative management alone.48 Hence, conservative management should only be offered to moribund patients with poor liver function and advanced tumor stage where both TAE and surgery are not feasible.
Methods to Achieve Hemostasis
Trans-arterial Embolization (TAE)
Patients who are hemodynamically unstable with signs of active bleeding should be managed to achieve immediate hemostasis. TAE is the least invasive approach to stop bleeding from rupture HCC in the acute phase with a high success rate of 53–100%.4, 9, 10, 11, 18 Compared to open surgical methods, TAE also has a lower (0–37% vs. 28–75%), 30-day mortality rate.4 Surgery may be initially difficult due to hemodynamic instability; TAE followed by staged liver resection can solve this problem. TAE can be complicated by the development of liver failure in 12–34% of patients.4, 18, 25 Selective embolization of the bleeding artery identified by CT scan or angiography is associated with less risk of liver failure especially in those with multifocal HCC. Mean survival time after TAE in patients with ruptured HCC varies according to the baseline liver function. Lau et al. in his study reported a mean survival of 218.3 days, 83.4 days and 11.0 days in Child–Pugh A, B and C patients undergoing TAE for ruptured HCC respectively.70 Serum bilirubin has been considered as a reliable indicator of liver function in patients with HCC rupture.10, 25, 47, 71 In a study by Nagan et al. patients undergoing TAE for ruptured HCC with a bilirubin level higher than 2.9 mg/dl (50 μmol/L), the median survival was only 1 week and none survived for more than 9 weeks, however with levels less than 2.9 mg/dl (50 μmol/L) the survival was 15 weeks, on average.25 Leung et al. similarly reported a mean survival of 165 days with bilirubin levels less than 2.9 mg/dl (50 μmol/L) compared to only 34 days in patients where the bilirubin levels were more than 2.9 mg/dl (50 μmol/L).72 Thus, a serum bilirubin value of less than 3 mg/dl (51 μmol/L) can be taken as a cut-off for successful TAE outcomes in ruptured HCC.47, 71 Other potential complications of TAE are post-embolization syndrome, abscess formation and re-rupture.4, 57 HCC re-rupture rate after TAE has been reported to be between 7% and 25%, and patients who suffer re-rupture generally have a poor prognosis.56, 57, 71, 72
Surgical Hemostasis
Hepatic Resection
The feasibility of performing hepatic resection is dependent on the hepatic reserve and the underlying liver cirrhosis. Selected patients can achieve prolonged survival with definitive treatment.4, 73 The resectability rates of ruptured HCC according to previous studies ranged from 12.5% to 59.3%.18, 74, 75 Emergency liver resection is primarily intended for hemostasis but has also been shown to have a potential curative role in rupture of HCC.4, 48 In the study by Zhu et al. out of 200 cases of HCC rupture, 105 (52%) undergone resection where R0 resection was possible in 92 patients (88%), in which 166 (83%) had tumor size more than 5 cm.15 In another series by Yang et al. where 409 patients presented with rupture of HCC, partial-hepatectomy was performed in 143 patients (emergency hepatectomy in 28 and staged hepatectomy in 115) in them R0 resection was achieved in 116 (81%) patients.76 R0 resection is defined as complete resection of all microscopic and macroscopic tumors.76
Unlike the case in un-ruptured HCC, there is no guideline which provides objective criteria for selection of patients for resection after rupture of HCC. Child A and Child B cirrhosis were also included for resection in ruptured HCC by several studies.44, 48, 76 The results of these studies showed that emergency liver resection is still a good treatment modality in selected patients with relatively preserved liver function. However, in a systematic review, Lai EC et al. have suggested that resection should be reserved for small, superficial and easily accessible HCC in a non-cirrhotic liver for better outcomes.4
Emergency liver resection has a higher in hospital mortality rate (17–100% vs. 0–9%) and a lower success rate (13–31% vs. 21–56%) than staged liver resection.4 Miyamoto et al. found that liver failure was responsible for half of the hospital mortality after emergency liver resection for ruptured HCC.5 The Indian National Association for Study of the Liver (INASL) recommends staged liver resection after achieving initial hemostasis to be better than emergency liver resection.73 However, emergency liver resection has the advantage of achieving hemostasis and potentially curative resection of the tumor in the same go.4, 14 Cumulative data from previous studies also have shown a mean hospital mortality rate as low as 27% (range 0–100%) with emergency liver resection.77 Moreover, early resection and clearing of intraperitoneal hematoma reduce the occurrence of peritoneal dissemination.17, 46 On the other hand, staged hepatic resection has been shown to increase the incidence of peritoneal dissemination compared to emergency resection.77 Other disadvantages of staged hepatic resection are potential for tumor stage progression, prolong hospital stay and cost.44 Outcomes of emergency liver resection can be facilitated by appropriate patient selection and improved surgical techniques. Laparoscopic surgery with improvised techniques like LigaSure and newer devices like the Harmonic scalpel and linear staplers with good hemostatic effects can largely cut short the surgical time especially in peripherally located small HCC.78, 79
Few recent studies have failed to show any statistically significant difference in survival benefit between TAE and surgical resection, though there is a tendency for better cumulative Overall Survival (OS) rate in the surgical group.11, 80 However, in a nationwide database of 1160 patients in Japan with ruptured HCC, Aoki et al. showed that liver resection was associated with better survival than other modalities of treatment.41 Study has also documented curative liver resection to be the only independent prognostic factor for OS.81
Other Rare Techniques of Hemostasis
Rare surgical techniques of hemostasis like perihepatic packing and Hepatic Artery Ligation (HAL) are rarely used now days. In ruptured HCC, HAL has a hemostatic success rate of 68–100%.8, 32, 82 Selective HAL is associated with less chance of liver failure and is preferred to common HAL.8 Preservation of contra-lateral arterial supply allows future definitive liver resection and TACE possible. However, HAL is associated with a high in hospital mortality rate of 50–77%.8, 32, 82 Perihepatic packing is limited by rate of infections up to 23–32%, if the packs are retained for 72 h; pack removal also is associated with the risk of re-bleeding.49, 83, 84 Packing is feasible if the ruptured tumor lies below the diaphragm as the later acts as a tamponade, it is less useful for tumors located on the inferior surface of the liver and in the presence of active bleeding rather than simple ooze.49, 85
For patients who have liver dysfunction or who are in poor general condition, Radio Frequency Ablation (RFA) can be an alternative treatment option. RFA is minimally invasive and can be performed during open surgery, laparoscopically or percutaneously. There are only limited literatures which describe the use of RFA to treat ruptured HCC.86, 87, 88, 89 Sun et al. used RFA both as salvage therapy and curative treatment for spontaneous rupture of a giant HCC.88 Percutaneous RFA has also been used to achieve successful hemostasis in two cases of ruptured HCC reported by Manikam et al.89 Cheung et al. reported that, compared to conventional HAL, RFA used for hemostasis during laparotomy greatly reduced the hospital mortality rate.90 There is also case report of Cynoacrylate glue being injected intraoperatively to achieve successful hemostasis in ruptured HCC.80
Liver Transplantation (LT) in Ruptured HCC
The BCLC (Barcelona Clinic Liver Cancer) staging system for HCC which is the most commonly used staging system to guide therapy and for assessing prognosis does not include ruptured HCC as a separate entity.91 However the current (Seventh) AJCC/UICC (American Joint Committee on Cancer/Union for International Cancer Control) TNM staging system classifies ruptured HCC as T4 even if the tumor is small, solitary and without extra-hepatic spread and vascular invasion.42, 92 Moreover, intraperitoneal seeding of HCC is not uncommon following rupture of HCC and has been reported to be as high as 9.4–20%.93, 94, 95 Peritoneal lavage with distilled water or instillation of 5-Fluoro-uracil after liver resection has been shown to reduce the chances of tumor recurrences. Peritoneal lavage with distilled water during surgery was also found to be associated with significantly better Disease Free Survival (DFS) and OS in patients after HCC rupture.93, 94, 95 Due to the above reasons and the potential risk of disease recurrence, LT in ruptured HCC seems an unreasonable option. The Current United Kingdom listing criteria for LT for HCC also consider ruptured HCC as an absolute contraindication.96 There are only few isolated case reports of successful outcomes of LT in ruptured HCC.97, 98
Survival after HCC Rupture
Ruptured HCC is the third most common cause of death due to HCC after tumor progression and liver failure.6 The incidence of ruptured HCC is decreasing due to improved surveillance and early detection of HCC. Earlier studies have reported a mortality rate of 25–75% in the acute phase of ruptured HCC.3, 4 However recent study has reported a significant decrease in the incidence of mortality, with an overall mortality of 23.5% and mortality as low as 0.95% among patients in whom hepatectomy was successfully conducted.15 Thus prolonged survival can be achieved with hepatic resection in selected patients with ruptured HCC.
Survival Related to the Eligibility for Different Treatments
If left untreated the median survival in ruptured HCC is as low as 1.2–4 months.99 Survival after rupture of HCC with different modalities of treatment has been variably reported in different series (Table 1). Conservative management generally is associated with poor outcomes compared to either TAE or liver resection. According to a study by Zhong et al. including 162 patients with ruptured HCC the survival rates at 30 days and 1 year were 8.6% and 0%, respectively in patients who were treated conservatively.48 In a series of 48 cirrhotic patients with spontaneous rupture of HCC, the median survival time in patients undergoing conservative treatment was 13.1 days compared to 244.8 days in patients managed with TAE.100 Study has shown conservative treatment compared to TAE or hepatic resection as the only risk factor (Odd Ratio 61.67) associated with 30 days mortality after rupture of HCC.43 The study has also found conservative treatment to be an independent predictor of poor long term survival after rupture of HCC.43 The average 1 month mortality rates in patients who were treated with TAE, emergency hepatic resection and conservative treatment were 48%, 50% and 71% respectively.101 The survival at 30 days and 1 year were found to be significantly better with either hepatectomy (92.5% and 59.4% respectively) or TAE (66.7% and 28.6% respectively).48 Ruptured HCC treated by hepatic resection, the 1-, 3- and 5-year OS rates were 76.0%, 48.6% and 33.9%, respectively.4 However, in patients with staged hepatectomy the OS rates were 90.0%, 67.5% and 67.5% at 1, 3 and 5 year respectively.4 According to a systematic review, staged liver resection has a much lower in-hospital mortality rate (0–9%) and higher 1 year (54.2–100%), 3 years (21.2–67.5%) and 5 years (15–67.5%) OS rates compared to emergency liver resection.4
Table 1.
Clinical Presentation, Management and Survival Outcome in Patients With Rupture of Hepatocellular Carcinoma (HCC).
| HCC rupture series | Center and year of study | Clinical presentation | Management | Survival outcome |
|---|---|---|---|---|
| Zhu et al.15 (n = 200) |
China 2002–2006 |
Abdominal pain 134 (67%) Shock 102 (51%) Abdominal distension 66 (33%) |
Conservative 62 (31%) TAE 33 (16.5%) Resection 105 (52.5%) |
MST Conservative group: 1 month (range 1–19) TAE group: 4 months (range 1–30) Resection group: 12 months (range 1–72) OS at 1, 3 and 5 Yrs (32.5%, 10% and 4% respectively) |
| Leu et al.44 (n = 135) |
China 1994–2003 |
Epigastric or right hypochondrial pain 135 (100%) Abdominal distension/peritonitis 27 (20%) Shock 5 (3%) |
Conservative 16 (11.8%) TAE 83 (61.5%) Resection/enucleation 33 (24.4%) |
OS at 1, 3, and 5 years Conservative group: NR TAE group: NR Resection group: 88%, 54%, and 51% respectively |
| Yang et al. 15 (n = 143) |
China 2000–2009 |
Epigastric or right hypochondrial pain 137 (95.8%) Hemoperitoneum 138 (96.5%) Abdominal distension/peritonitis 27 (18.8%) Shock 32 (22.4%) |
Emergency TAE 13 (9.1%) Emergency hepatectomy 28 (19.6%) Staged hepatectomy 115 (80.4%) |
OS at 1, 3 and 5 years (66.2%, 25.1% and 16.8% respectively) RFS at 1, 3 and 5 years (40.5%, 25.8% and 14.8% respectively) |
| Zhang et al. 46 (n = 49) |
China 1990–2006 |
Epigastric or right hypochondrial pain 47 (95.9%) Signs of peritonitis 42 (85.7%) Shock 40 (81.6%) |
Emergency resection 21 (35.6%) HAL 4 (0.82%) Suture placation 5 (1.02%) Perihepatic packing 2 (0.4%) Microwave ablation 5 (1.02%) Combined 12 (24.5%) |
MST 8.8 months In hospital mortality 10.2% |
| Jin et al.11 (n = 54) |
South Korea 2003–2012 |
NR | Conservative 23 (42.6%) TAE 25 (46.3%) Surgery 6 (11.1%) |
Cumulative survival rates at 2, 4 and 6 months Conservative group: 8.7%, 0% and 0% TAE group: 36%, 20% and 20% respectively Surgery group: 60%, 60% and 60% respectively |
| Aoki et al.41 (n = 1106) |
Japan 2000–2005 |
NR | Conservative 275 (24.9%) TAE/TACE 489 (44.2%) Local ablative therapy 32 (0.3%) Resection 298 (26.9%) Chemotherapy 65 (0.6%) |
OS at 1, 3 and 5 years Conservative: NR TAE/TACE group: 39.7%, 14.1% and 6.0% respectively Resection group: 76%, 48.6% and 33.9% respectively |
| Sada et al.80 (n = 64) |
Japan 1986–2013 |
NR | Best supportive care 21 (32.8%) TAE alone 27 (42.2%) Emergency hepatectomy 4 (0.6%) Staged hepatectomy 12 (18.7%) |
MST in years Best supportive care: 0.10 (range 0–2.44) TAE group: 0.53 (range 0–11.60) Surgery group: 1.06 (range 0.24–12.13) (a) 0.35 (range 0.28–1.06) for one-stage resection (b) 1.72 (range 0.24–12.13) for staged resection |
| Hsueh et al.43 (n = 54) |
Taiwan 2004–2010 |
Hemodynamic instability 48 (88.9%) Hemoperitoneum on ascitic tap 8 (14.8%) |
Conservative 6 (11.1%) TAE alone 29 (53.7%) Emergency hepatectomy 19 (41.3%) Staged hepatectomy 18 (33.3%) |
Survival rate at 30 days and 1 year Conservative group: NR TAE alone group: 81.8% and 18% respectively Hepatectomy group: 97.3% and 62.2% respectively |
| Sahu et al.104 (n = 20) |
India 2014–2017 |
Epigastric or right hypochondrial pain 17 (85%) Distension of abdomen 16 (80%) Hemoperitoneum on diagnostic paracentesis 15 (75%) Hypovolemic shock 8 (40%) |
Conservative 5 (25%) TAE 14 (70%) Hepatic resection 1 (5%) |
Mortality at 30 days Conservative group: 100% TAE group: 29% Hepatic resection group: 0% OS at 3 months 35% |
Data are presented as frequency (percentages), MST: median survival time, OS: overall survival, TAE/TACE: Trans-arterial (chemo) Embolization, HAL: Hepatic Artery Ligation, RFS: Recurrence Free Survival, DFS: Disease Free Survival, NR: Not Reported.
Survival Related to Tumor Stage
A study involving 79 patients with ruptured HCC, has reported that, the BCLC stage was an important predictor of survival even in ruptured HCC. The mean survival time for ruptured HCC with BCLC stages A, B and C were 251, 175 and 40 days respectively.45
Survival in Ruptured vs. Non-ruptured HCC
Ruptured HCC is associated with poor survival compared to non-ruptured HCC with a median OS of 8.9 weeks and 28 weeks respectively.18 Aoki et al. also have shown that survival was significantly worse in patients with ruptured HCC as compared to HCC without rupture.41 However two recent studies have challenged this concept and showed similar OS between the groups especially with similar baseline factors like tumor stage and liver function.102, 103 Hence rupture of HCC should not be labeled universally as a terminal event, even though, it potentially alters the natural history of HCC.
Other Predictors of Survival
Many studies have described shock at presentation to be an important factor influencing the survival after HCC ruptures.18, 51, 80, 100 Other factors that are associated with poor survival are higher blood transfusion requirement, tumors which involve both lobes of the liver and presence of portal vein thrombosis.47
Summary
Rupture of HCC is a potentially life threatening complication of HCC and is not uncommon. Although the prognosis is generally poor with conservative treatment alone, long term survival could be achieved in patients with resectable disease and good functional liver reserve. There is no consensus on the best treatment approach for this entity; treatment should be individualized taking into account the hemodynamic status, underlying liver function and tumor stage. TAE is the least invasive method to achieve hemostasis with a high success rate. Hepatic resection is associated with improved survival and offers a hope for cure in selected patients.
Conflicts of Interest
The authors have none to declare.
Acknowledgement
The authors did not receive any grant or financial support to prepare this manuscript.
References
- 1.Ferlay J., Shin H.R., Bray F., Forman D., Mathers C., Parkin D.M. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Fattovich G., Stroffolini T., Zagni I., Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 2004;127(5 suppl 1):S35–S50. doi: 10.1053/j.gastro.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 3.Tanaka A., Takeda R., Mukaihara S. Treatment of ruptured hepatocellular carcinoma. Int J Clin Oncol. 2001;6:291–295. doi: 10.1007/s10147-001-8030-z. [DOI] [PubMed] [Google Scholar]
- 4.Lai E.C., Lau W.Y. Spontaneous rupture of hepatocellular carcinoma: a systematic review. Arch Surg. 2006;141:191–198. doi: 10.1001/archsurg.141.2.191. [DOI] [PubMed] [Google Scholar]
- 5.Miyamoto M., Sudo T., Kuyama T. Spontaneous rupture of hepatocellular carcinoma: a review of 172 Japanese cases. Am J Gastroenterol. 1991;86:67–71. [PubMed] [Google Scholar]
- 6.Bassi N., Caratozzolo E., Bonariol L. Management of ruptured hepatocellular carcinoma: implications of therapy. World J Gastroenterol. 2010;16:1221–1225. doi: 10.3748/wjg.v16.i10.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chearanai O., Plengvanit U., Asavanich C. Spontaneous rupture of primary hepatoma: report of 63 cases with particular reference to the pathogenesis and rationale of treatment by hepatic artery ligation. Cancer. 1983;51:1532–1536. doi: 10.1002/1097-0142(19830415)51:8<1532::aid-cncr2820510829>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 8.Hirai K., Kawazoe Y., Yamashita K. Transcatheter arterial embolization for spontaneous rupture of hepatocellular carcinoma. Am J Gastroenterol. 1986;81:275–279. [PubMed] [Google Scholar]
- 9.Yoshida H., Mamada Y., Taniai N., Uchida E. Spontaneous ruptured hepatocellular carcinoma. Hepatol Res. 2016;46:13–21. doi: 10.1111/hepr.12498. [DOI] [PubMed] [Google Scholar]
- 10.Kung C.T., Liu B.M., Ng S.H. Transcatheter arterial embolization in the emergency department for hemodynamic instability due to ruptured hepatocellular carcinoma: analysis of 167 cases. Am J Roentgenol. 2008;191:W231–W239. doi: 10.2214/AJR.07.3983. [DOI] [PubMed] [Google Scholar]
- 11.Jin Y.J., Lee J.W., Park S.W. Survival outcome of patients with spontaneously ruptured hepatocellular carcinoma treated surgically or by transarterial embolization. World J Gastroenterol. 2013;19:4537–4544. doi: 10.3748/wjg.v19.i28.4537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamagata M., Maeda T., Ikeda Y., Shirabe K., Nishizaki T., Koyanagi N. Surgical results of spontaneously ruptured hepatocellular carcinoma. Hepatogastroenterology. 1995;42:461–464. [PubMed] [Google Scholar]
- 13.Clarkston W., Inciardi M., Kirkpatrick S., Mc Ewen G., Ediger S., Schubert T. Acute hemoperitoneum from rupture of a hepatocellular carcinoma. J Clin Gastroenterol. 1988;10:221–225. doi: 10.1097/00004836-198804000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Vergara V., Muratore A., Bouzari H. Spontaneous rupture of hepatocelluar carcinoma: surgical resection and long-term survival. Eur J Surg Oncol. 2000;26:770–772. doi: 10.1053/ejso.2000.1001. [DOI] [PubMed] [Google Scholar]
- 15.Zhu Q., Li J., Yan J.J., Huang L., Wu M.C., Yan Y.Q. Predictors and clinical outcomes for spontaneous rupture of hepatocellular carcinoma. World J Gastroenterol. 2012;18(48):7302–7307. doi: 10.3748/wjg.v18.i48.7302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kew M.C., Paterson A.C. Unusual clinical presentations of hepatocellular carcinoma. Trop Gastroenterol. 1985;6:10–22. [PubMed] [Google Scholar]
- 17.Ong G.B., Taw J.L. Spontaneous rupture of hepatocellular carcinoma. Br Med J. 1972;4:146–149. doi: 10.1136/bmj.4.5833.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu C.L., Fan S.T., Lo C.M. Management of spontaneous rupture of hepatocellular carcinoma: single centre experience. J Clin Oncol. 2001;19:3725–3732. doi: 10.1200/JCO.2001.19.17.3725. [DOI] [PubMed] [Google Scholar]
- 19.Marini P., Vilgrain V., Belghiti J. Management of spontaneous rupture of liver tumours. Dig Surg. 2002;19:109–113. doi: 10.1159/000052022. [DOI] [PubMed] [Google Scholar]
- 20.Chen C.Y., Lin X.Z., Shin J.S. Spontaneous rupture of hepatocellular carcinoma: a review of 141 Taiwanese cases and comparison with non-rupture cases. J Clin Gastroenterol. 1995;21:238–242. [PubMed] [Google Scholar]
- 21.Ikai I., Arii S., Okazaki M. Report of the 17th nationwide follow-up survey of primary liver cancer in Japan. Hepatol Res. 2007;37:676–691. doi: 10.1111/j.1872-034X.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- 22.Islam M., Deka P., Kapur R., Ansari M.M. Non-bleeding spontaneous rupture of hepatocellular carcinoma. Niger J Surg. 2013;19:82–84. doi: 10.4103/1117-6806.119241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rathod K., Sheth R., Shah P., Rege S. Active contrast extravasation in spontaneous rupture of hepatocellular carcinoma: a rare CT finding. J Postgrad Med. 2000;46:35–36. [PubMed] [Google Scholar]
- 24.Somu A. Angio-embolization in HCC rupture—a tertiary care experience. J Clin Exp Hepatol. 2015;5(S2):S57–S65. [Google Scholar]
- 25.Ngan H., Tso W.K., Lai C.L., Fan S.T. The role of hepatic arterial embolization in the treatment of spontaneous rupture of hepatocellular carcinoma. Clin Radiol. 1998;53:338–341. doi: 10.1016/s0009-9260(98)80004-4. [DOI] [PubMed] [Google Scholar]
- 26.Rathor M., Lal A., Dhiman R. Spontaneous rupture of hepatocellular carcinoma. J Clin Exp Hepatol. 2014;4(2):188–189. doi: 10.1016/j.jceh.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li J., Huang L., Liu C.F. Risk factors and surgical outcomes for spontaneous rupture of BCLC stages A and B hepatocellular carcinoma: a case–control study. World J Gastroenterol. 2014;20(27):9121–9127. doi: 10.3748/wjg.v20.i27.9121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhu L., Geng X., Fan S. Relationship between vascular elasticity and spontaneous rupture of hepatocellular carcinoma. Chin-German J Clin Oncol. 2003;2(1):18–22. [Google Scholar]
- 29.Zhu L.X., Geng X.P., Fan S.T. Spontaneous rupture of hepatocellular carcinoma and vascular injury. Arch Surg. 2001;136:682–687. doi: 10.1001/archsurg.136.6.682. [DOI] [PubMed] [Google Scholar]
- 30.Zhu L.X., Liu Y., Fan S.T. Ultra-structural study of the vascular endothelium of patients with spontaneous rupture of hepatocellular carcinoma. Asian J Surg. 2002;25:157–162. doi: 10.1016/S1015-9584(09)60166-4. [DOI] [PubMed] [Google Scholar]
- 31.Ong G.B., Chu E.P.H., Yu F.Y.K., Lee T.C. Spontaneous rupture of hepatocellular carcinoma. Br J Surg. 1965;52:123–129. doi: 10.1002/bjs.1800520210. [DOI] [PubMed] [Google Scholar]
- 32.Zhu L.X., Wang G.S., Fan S.T. Spontaneous rupture of hepatocellular carcinoma. Br J Surg. 1996;83:602–607. doi: 10.1002/bjs.1800830507. [DOI] [PubMed] [Google Scholar]
- 33.Liu C.L., Ngan H., Lo C.M., Fan S.T. Ruptured hepatocellular carcinoma as a complication of transarterial oily chemoembolization. Br J Surg. 1998;85:512–514. doi: 10.1046/j.1365-2168.1998.00664.x. [DOI] [PubMed] [Google Scholar]
- 34.Battula N., Srinivasan P., Madanur M. Ruptured hepatocellular carcinoma following chemoembolization: a western experience. Hepatobiliary Pancreat Dis Int. 2007;6:49–51. [PubMed] [Google Scholar]
- 35.Chung J.W., Park J.H., Han J.K. Hepatic tumors: predisposing factors for complications of transcatheter oily chemoembolization. Radiology. 1996;198:33–40. doi: 10.1148/radiology.198.1.8539401. [DOI] [PubMed] [Google Scholar]
- 36.Sakamoto I., Aso N., Nagaoki K. Complications associated with transcatheter arterial embolization for hepatic tumours. Radiographics. 1998;18:605–619. doi: 10.1148/radiographics.18.3.9599386. [DOI] [PubMed] [Google Scholar]
- 37.Kang H.J., Lee B.H., Han Y.H., Hwang Y.J., Kim S.Y., Lee J.Y. Rupture of hepatocellular carcinoma following transcatheter arterial chemoembolization: a case report. J Korean Soc Radiol. 2012;67(2):109–112. [Google Scholar]
- 38.Jia Z., Feng M.M.S., BMed T., Jiang G. Ruptured hepatic carcinoma after transcatheter arterial chemoembolization. Curr Therap Res. 2013;74:41–43. doi: 10.1016/j.curtheres.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sun J.H., Wang L.G., Bao H.W. Emergency embolization in the treatment of ruptured hepatocellular carcinoma following transcatheter arterial chemoembolization. Hepatogastroenterology. 2010;57:616–619. [PubMed] [Google Scholar]
- 40.Rombolà F., Caravetta A., Mollo F., Spinoso A., Peluso L., Guarino R. Sorafenib, risk of bleeding and spontaneous rupture of hepatocellular carcinoma: a clinical case. Acta Med. 2011;54(4):177–179. doi: 10.14712/18059694.2016.46. [DOI] [PubMed] [Google Scholar]
- 41.Aoki T., Kokudo N., Matsuyama Y., Izumi N., Ichida T., Kudo M. Prognostic impact of spontaneous tumor rupture in patients with hepatocellular carcinoma an analysis of 1160 cases from a nationwide survey. Ann Surg. 2013:1–11. doi: 10.1097/SLA.0b013e31828846de. [DOI] [PubMed] [Google Scholar]
- 42.Wen H.C., Chien F.H., Kuang T.P. Impact of spontaneous tumor rupture on prognosis of patients with T4 hepatocellular carcinoma. J Surg Oncol. 2016;113:789–795. doi: 10.1002/jso.24245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hsueh K.C., Fan H.L., Chen T.W. Management of spontaneously ruptured hepatocellular carcinoma and hemoperitoneum manifested as acute abdomen in the emergency room. World J Surg. 2012;36:2670–2676. doi: 10.1007/s00268-012-1734-6. [DOI] [PubMed] [Google Scholar]
- 44.Liu H., Pen Y.H., Yong F., Li R.F. One-stage liver resection for spontaneous rupture of hepatocellular carcinoma. World J Surg. 2005;29:1316–1318. doi: 10.1007/s00268-005-7626-2. [DOI] [PubMed] [Google Scholar]
- 45.Han X.J., Su H.Y., Shao H.B., Xu K. Prognostic factors of spontaneously ruptured hepatocellular carcinoma. World J Gastroenterol. 2015;21(24):7488–7494. doi: 10.3748/wjg.v21.i24.7488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang H., Cong J., Chen C. Spontaneous rupture of primary hepatocellular carcinoma: experience of emergency laparotomy over a 16-year period. Chin J Clin Oncol. 2007;4(5):322–326. [Google Scholar]
- 47.Shin B.S., Park M.H., Jeon G.S. Outcome and prognostic factors of spontaneous ruptured hepatocellular carcinoma treated with transarterial embolization. Acta Radiol. 2011;52:331–335. doi: 10.1258/ar.2010.100369. [DOI] [PubMed] [Google Scholar]
- 48.Zhong F., Cheng X.S., He K., Sun S.B., Zhou J., Chen H.M. Treatment outcomes of spontaneous rupture of hepatocellular carcinoma with hemorrhagic shock: a multicenter study. Springer Plus. 2016;5:1101–1120. doi: 10.1186/s40064-016-2762-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kew M.C., Hodkinson J. Rupture of hepatocellular carcinoma as a result of blunt abdominal trauma. Am J Gastroenterol. 1991;86:1083–1085. [PubMed] [Google Scholar]
- 50.Dewar G.A., Griffin S.M., Ku K.W., Lau W.Y., Li A.K.C. Management of bleeding liver tumours in Hong Kong. Br J Surg. 1991;78:463–466. doi: 10.1002/bjs.1800780424. [DOI] [PubMed] [Google Scholar]
- 51.Xu H.S., Yan J.B. Conservative management of spontaneous ruptured hepatocellular carcinoma. Am Surg. 1994;60:629–633. [PubMed] [Google Scholar]
- 52.Muhammad I., Mabogunje O. Spontaneous rupture of primary hepatocellular carcinoma in Zaria, Nigeria. J R Coll Surg Edinb. 1991;36:117–120. [PubMed] [Google Scholar]
- 53.Lau W.Y. Management of hepatocellular carcinoma. J R Coll Surg Edinb. 2002;47:389–399. [PubMed] [Google Scholar]
- 54.Fuminori O., Masaki H., Noriyuki O. Hemothorax caused by spontaneous rupture of hepatocellular carcinoma: a case report and review of the literature. World J Surg Oncol. 2012;10:215. doi: 10.1186/1477-7819-10-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Corr P., Chan M., Lau W.Y., Metreweli C. The role of hepatic arterial embolization in the management of ruptured hepatocellular carcinoma. Clin Radiol. 1993;48:163–165. doi: 10.1016/s0009-9260(05)80129-1. [DOI] [PubMed] [Google Scholar]
- 56.Castells L., Moreiras M., Quiroga S. Hemoperitoneum as a first manifestation of hepatocellular carcinoma in western patients with liver cirrhosis: effectiveness of emergency treatment with transcatheter arterial embolization. Dig Dis Sci. 2001;46:555–562. doi: 10.1023/a:1005699132142. [DOI] [PubMed] [Google Scholar]
- 57.Kanematsu M., Imaeda T., Yamawaki Y. Rupture of hepatocellular carcinoma: predictive value of CT findings. Am J Roentgenol. 1992;158:1247–1250. doi: 10.2214/ajr.158.6.1317090. [DOI] [PubMed] [Google Scholar]
- 58.Kim H.C., Yang D.M., Jin W., Park S.J. The various manifestations of ruptured hepatocellular carcinoma: CT imaging findings. Abdom Imaging. 2008;33:633–642. doi: 10.1007/s00261-007-9353-7. [DOI] [PubMed] [Google Scholar]
- 59.Tsitouridis I., Michaelides M., Christopoulou A. Early stage of intraperitoneal rupture of hepatocellular carcinoma: CT and MRI evaluation. Ann Gastroenterol. 2007;20(4):282–285. [Google Scholar]
- 60.Kim P.T., Su J.C., Buczkowski A.K. Computed tomography and angiographic interventional features of ruptured hepatocellular carcinoma: pictorial essay. Can Assoc Radiol J. 2006;57:159–168. [PubMed] [Google Scholar]
- 61.Choi B.G., Park S.H., Byun J.Y. The findings of ruptured hepatocellular carcinoma on helical CT. Br J Radiol. 2001;74(858):142–146. doi: 10.1259/bjr.74.878.740142. [DOI] [PubMed] [Google Scholar]
- 62.Singhal M., Sinha U., Kalra N., Duseja A., Khandelwal N. Enucleation sign: a computed tomographic appearance of ruptured hepatocellular carcinoma. J Clin Exp Hepatol. 2016;6(4):335–336. doi: 10.1016/j.jceh.2016.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mayuree K., Jaturon T., Laddawan V. Findings of ruptured hepatocellular carcinoma on computed tomography in Thailand. Asian Biomed. 2007;1:289–294. [Google Scholar]
- 64.Yun S.J., Nam D.H. Hepatic angiographic findings of ruptured hepatocellular carcinoma: “sentinel signs” versus extravasation. J Korean Soc Radiol. 2014;70(5):335–342. [Google Scholar]
- 65.Matsumoto N., Ogawa M., Nakagawara H. Clinical efficacy of contrast-enhanced ultrasonography (CEUS) in the diagnosis of ruptured hepatocellular carcinoma. J Med Ultrason. 2007;34:101–105. doi: 10.1007/s10396-007-0136-0. [DOI] [PubMed] [Google Scholar]
- 66.Sugihara T., Koda M., Okamoto T., Miyoshi K., Matono T., Isomoto H. Two patterns of contrast-enhanced ultrasonography with Sonazoid in spontaneous rupture of hepatocellular carcinoma: a report of four cases. J Med Ultrason. 2017 doi: 10.1007/s10396-017-0812-7. [DOI] [PubMed] [Google Scholar]
- 67.Shiozawa K., Watanabe M., Ikehara T. Usefulness of contrast enhanced ultrasonography in the diagnosis of ruptured hepatocellular carcinoma. Clin J Gastroenterol. 2013;6:334–337. doi: 10.1007/s12328-013-0398-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Landmark K.E., Johansen P.W., Johnson J.A., Johansen B., Uran S., Skotland T. Pharmacokinetics of perfluorobutane following intravenous bolus injection and continuous infusion of sonazoid in healthy volunteers and in patients with reduced pulmonary diffusing capacity. Ultrasound Med Biol. 2008;34:494–501. doi: 10.1016/j.ultrasmedbio.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 69.Wang B., Lu Y., Zhang X.F., Yu L., Pan C.E., Wu Z. Management of spontaneous rupture of hepatocellular carcinoma. ANZ J Surg. 2008;78:501–503. doi: 10.1111/j.1445-2197.2008.04543.x. [DOI] [PubMed] [Google Scholar]
- 70.Lau K.Y., Wong T.P., Wong W.W., Tan L.T., Chan J.K., Lee A.S. Emergency embolization of spontaneous ruptured hepatocellular carcinoma: correlation between survival and Child–Pugh classification. Australas Radiol. 2003;47:231–235. doi: 10.1046/j.1440-1673.2003.01168.x. [DOI] [PubMed] [Google Scholar]
- 71.Okazaki M., Higashihara H., Koganemaru F. Intraperitoneal hemorrhage from hepatocellular carcinoma: emergency chemoembolization or embolization. Radiology. 1991;180(3):647–651. doi: 10.1148/radiology.180.3.1651524. [DOI] [PubMed] [Google Scholar]
- 72.Leung C.S., Tang C.N., Fung K.H., Li M.K.W. A retrospective review of transcatheter hepatic arterial embolization for ruptured hepatocellular carcinoma. J R Coll Surg Edinb. 2002;47:685–688. [PubMed] [Google Scholar]
- 73.Kumar A., Acharya S.K., Singh S.P. The Indian National Association for Study of the Liver (INASL) consensus on prevention, diagnosis and management of hepatocellular carcinoma in India: the Puri recommendations. J Clin Exp Hepatol. 2014;4:S3–S26. doi: 10.1016/j.jceh.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nakanishi Y., Sano H., Kimura J., Konno T., Kasai Y. Clinical evaluation of palliative therapy for unresectable primary liver cancer. Cancer. 1986;58:329–331. doi: 10.1002/1097-0142(19860715)58:2<329::aid-cncr2820580220>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 75.Cherqui D., Panis Y., Rotman N., Fagniez P.L. Emergency liver resection for spontaneous rupture of hepatocellular carcinoma complicating cirrhosis. Br J Surg. 1993;80:747–749. doi: 10.1002/bjs.1800800631. [DOI] [PubMed] [Google Scholar]
- 76.Yang T., Sun Y.F., Zhang J. Partial hepatectomy for ruptured hepatocellular carcinoma. Br J Surg. 2013;100:1071–1079. doi: 10.1002/bjs.9167. [DOI] [PubMed] [Google Scholar]
- 77.Anon C. Delayed versus emergency hepatectomy for ruptured hepatocellular carcinoma. Indian J Surg. 2006;68(4):209–215. [Google Scholar]
- 78.Chiappa A., Bertani E., Biffi R. Effectiveness of LigaSure diathermy coagulation in liver surgery. Surg Technol Int. 2008;17:1733–1738. [PubMed] [Google Scholar]
- 79.Cherqui D., Husson E., Hammoud R. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg. 2000;232:753–762. doi: 10.1097/00000658-200012000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tan F.L., Tan Y.M., Chung A.Y. Factors affecting early mortality in spontaneous rupture of hepatocellular carcinoma. ANZ J Surg. 2006;76:448–452. doi: 10.1111/j.1445-2197.2006.03750.x. [DOI] [PubMed] [Google Scholar]
- 81.Sada H., Ohira M., Kobayashi T., Tashiro H., Chayama K., Ohdan H. An analysis of surgical treatment for the spontaneous rupture of hepatocellular carcinoma. Dig Surg. 2016;33:43–50. doi: 10.1159/000441531. [DOI] [PubMed] [Google Scholar]
- 82.Lai E.C.S., Wu K.M., Choi T.K., Fan S.T., Wong J. Spontaneous ruptured hepatocellular carcinoma: an appraisal of surgical treatment. Ann Surg. 1989;210:24–28. doi: 10.1097/00000658-198907000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sharp K.W., Locicero R.J. Abdominal packing for surgically uncontrollable hemorrhage. Ann Surg. 1992;215:467–474. doi: 10.1097/00000658-199205000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Caruso D.M., Battistella F.D., Owings J.T., Lee S.L., Samaco R.C. Perihepatic packing of major liver injuries: complications and mortality. Arch Surg. 1999;134:958–962. doi: 10.1001/archsurg.134.9.958. [DOI] [PubMed] [Google Scholar]
- 85.Hsieh J.S., Huang C.J., Huang Y.S., Sheen P.C., Huang T.J. Intraperitoneal hemorrhage due to spontaneous rupture of hepatocellular carcinoma: treatment by hepatic arterial embolization. Am J Roentgen. 1987;149:715–717. doi: 10.2214/ajr.149.4.715. [DOI] [PubMed] [Google Scholar]
- 86.Ng K.K., Lam C.M., Poon R.T., Law W.L., Seto C.L., Fan S.T. Radiofrequency ablation as a salvage procedure for ruptured hepatocellular carcinoma. Hepatogastroenterology. 2003;50:1641–1643. [PubMed] [Google Scholar]
- 87.Fuchizaki U., Miyamori H., Kitagawa S., Kaneko S. Radiofrequency ablation for life-threatening ruptured hepatocellular carcinoma. J Hepatol. 2004;40:354–355. doi: 10.1016/j.jhep.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 88.Sun W.B., Ding X.M., Ke S., Gao J., Zhang Y.F. Repeated radiofrequency ablation as both salvage solution and curative treatment for spontaneous rupture of giant medial lobe hepatocellular carcinoma. Chin Med J (Engl) 2009;122:2067–2070. [PubMed] [Google Scholar]
- 89.Manikam J., Mahadeva S., Goh K.L., Abdullah B.J. Percutaneous, non-operative radio frequency ablation for haemostasis of ruptured hepatocellular carcinoma. Hepatogastroenterology. 2009;56:227–230. [PubMed] [Google Scholar]
- 90.Cheung T.T., Poon R.T., Chok K.S. Management of spontaneously ruptured hepatocellular carcinomas in the radiofrequency ablation era. PLOS ONE. 2014;9:944–953. doi: 10.1371/journal.pone.0094453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Llovet J.M., Brú C., Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19:329–338. doi: 10.1055/s-2007-1007122. [DOI] [PubMed] [Google Scholar]
- 92.Collaborative Staging Task Force of the American Committee on Cancer . NIH Publication; Bethesda: 2004. Collaborative Staging Manual and Coding Instructions, Version 1.0. Published jointly by the American Joint Committee on Cancer (Chicago, IL) and the U.S. Department of Health and Human Services (Bethesda, Maryland) No. 04-5496. [Google Scholar]
- 93.Lin C.H., Hsieh H.F., Yu J.C., Chen T.W., Yu C.Y., Hsieh C.B. Peritoneal lavage with distilled water during liver resection in patients with spontaneously ruptured hepatocellular carcinomas. J Surg Oncol. 2006;94:255–256. doi: 10.1002/jso.20596. [DOI] [PubMed] [Google Scholar]
- 94.Sonoda T., Kanematsu T., Takenaka K., Sugimachi K. Ruptured hepatocellular carcinoma evokes risk of implanted metastases. J Surg Oncol. 1989;41:183–186. doi: 10.1002/jso.2930410310. [DOI] [PubMed] [Google Scholar]
- 95.Zhou S.J., Zhang E.L., Liang B.Y., Zhang Z.Y., Chen X.P., Huang Z.Y. Distilled water lavage during surgery improves long-term outcomes of patients with ruptured hepatocellular carcinoma. J Gastrointest Surg. 2015;19:1737–1738. doi: 10.1007/s11605-015-2797-0. [DOI] [PubMed] [Google Scholar]
- 96.Blood N.H.S. 2009. Transplant Liver Advisory Group. Protocols and Guidelines for adults Undergoing Deceased Donor Liver Transplantation in the UK. Accessed 29.10.17. [Google Scholar]
- 97.Prieto-Puga A.T., Romacho L.L., Suarez M.A., Sanchez P.B., Santoyo S.J. Spontaneous rupture of a hepatocellular carcinoma: is a liver transplant indicated? Cir Esp. 2015;93(7):478–479. doi: 10.1016/j.ciresp.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 98.Chen C.L., Chen Y.S., Goto S., Jawan B., Cheng Y.F., Eng H.L. Successful transplantation in a patient with ruptured large hepatocellular carcinoma with diaphragmatic invasion. Surgery. 2000;127:228–229. doi: 10.1067/msy.2000.100719. [DOI] [PubMed] [Google Scholar]
- 99.Al-Mashat F.M., Sibiany A.M., Kashgari R.H. Spontaneous rupture of hepatocellular carcinoma. Saudi Med J. 2002;23:866–870. [PubMed] [Google Scholar]
- 100.Kirikoshi H., Saito S., Yoneda M. Outcomes and factors influencing survival in cirrhotic cases with spontaneous rupture of hepatocellular carcinoma: a multicenter study. BMC Gastroenterology. 2009;9:29. doi: 10.1186/1471-230X-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen W.K., Chang Y.T., Chung Y.T., Yang H.R. Outcomes of emergency treatment in ruptured hepatocellular carcinoma in the ED. Am J Emerg Med. 2005;23:730–736. doi: 10.1016/j.ajem.2005.02.052. [DOI] [PubMed] [Google Scholar]
- 102.Yeh C.N., Lee W.C., Jeng L.B., Chen M.F., Yu M.C. Spontaneous tumour rupture and prognosis in patients with hepatocellular carcinoma. Br J Surg. 2002;89:1125–1129. doi: 10.1046/j.1365-2168.2002.02188.x. [DOI] [PubMed] [Google Scholar]
- 103.Mizuno S., Yamagiwa K., Ogawa T. Are the results of surgical treatment of hepatocellular carcinoma poor if the tumor has spontaneously ruptured? Scand J Gastroenterol. 2004;39:567–570. doi: 10.1080/00365520410005135. [DOI] [PubMed] [Google Scholar]
- 104.Sahu S.K., Taneja S., Kalra N. Rupture of hepatocellular carcinoma: a tale of 20 cases from a tertiary care center from Northern India. J Gastrointest Canc. 2018 doi: 10.1007/s12029-018-0063-x. https://doi.org/10.1007/s12029-018-0063-x. [DOI] [PubMed] [Google Scholar]