Abstract
Being one of the most widely prevalent diseases throughout the world, hypertension has emerged as one of the leading causes of global premature morbidity and mortality. Hence, blood pressure (BP) measurements are essential for physicians in the diagnosis and management of hypertension. Current American College of Cardiology/American Heart Association (ACC/AHA) guidelines recommend initiating antihypertensive medications on the basis of office BP readings. However, office BP readings provide a snapshot evaluation of the patient's BP, which might not reflect patient's true BP, with the possibility of being falsely elevated or falsely low. Recently, there is ample evidence to show that ambulatory blood pressure monitoring (ABPM) is a better predictor of major cardiovascular events than BP measurements at clinic settings. ABPM helps in reducing the number of possible false readings, along with the added benefit of understanding the dynamic variability of BP. This article will focus on the significance of ambulatory BP, its advantages and limitations compared with the standard office BP measurement and a brief outlook on its use and interpretation to diagnose and treat hypertension.
Keywords: Ambulatory blood pressure, White coat hypertension, Masked hypertension, Nocturnal hypertension, Dipping
1. Introduction
Being one of the most widely prevalent diseases throughout the world, hypertension has emerged as one of the leading causes of global premature morbidity and mortality.1 The prevalence is on the rise not only worldwide but in India as well, with crude prevalence of 25.3%, based on data collected from 2012 to 2014.2 This figure is only expected to increase, as the recent updated American College of Cardiology/American Heart Association (ACC/AHA) 2017 guidelines have been modified to call any patient with a systolic blood pressure more than 130 mm Hg as hypertensive,3 in place of earlier guidelines which had a cut-off value of 140 mm Hg to classify a person as hypertensive. ACC/AHA 2017 guidelines categorize blood pressure (BP) as normal, elevated, and hypertension (stage 1 and stage 2), based on ≥2 measurements on ≥ 2 separate occasions, as shown in Table 1. Hypertension is defined as office BP reading of at least 130 mm Hg systolic and 80 mm Hg diastolic, with the corresponding 24 h ambulatory BP readings being 125 mm Hg systolic and 75 mm Hg diastolic.3 Hypertension is one of the major risk factors for coronary artery disease (CAD), stroke, myocardial infarction, heart failure and chronic kidney disease (CKD); however, it is a modifiable risk factor, with nonpharmacological and pharmacological measures providing substantial risk reduction of these conditions.4, 5 Hence, BP measurements are essential for physicians in the diagnosis and management of hypertension.6 Current ACC/AHA guidelines recommend initiating antihypertensive medications on the basis of office BP readings.3 However, office BP readings provide a snapshot evaluation of the patient's BP, which might not reflect patient's true BP, with the possibility of being falsely elevated or falsely low.7 Second, office BP measurement does not give any idea about the variation of BP throughout the day or the effect of the antihypertensive on the variation. Ambulatory BP measurement (ABPM) helps in reducing the number of possible false readings, along with the added benefit of understanding the dynamic variability of BP. This article will focus on the significance of ABPM and its advantages and limitations compared with the standard office BP measurement and a brief outlook on its use and interpretation to diagnose and treat hypertension.
Table 1.
Classification of blood pressure measurements based on the ACC/AHA 2017 guidelines.3
| Blood pressure | Normal | Elevated | Stage 1 hypertension | Stage 2 hypertension |
|---|---|---|---|---|
| SBP | <120 mm Hg | 120–129 mm Hg | 130-139 Hg | ≥140 mm Hg |
| & | & | Or | Or | |
| DBP | <80 mm Hg | <80 mm Hg | 80–89 mm Hg | ≥90 mm Hg |
ACC/AHA, American College of Cardiology/American Heart Association; SBP: systolic blood pressure; DBP: diastolic blood pressure.
2. Ambulatory blood pressure monitoring
ABPM refers to BP recording, usually over 24 h, to assess the pressure variability patterns. It provides a superior and more precise assessment of true BP than standard one-time measurement. ABPM can detect circadian changes (diurnal rhythmic changes, including nocturnal dipping and morning surge) and BP variation with different environmental and emotional changes.7 In addition, it is a better tool than one-time BP for assessing the effect of antihypertensive therapy and prediction of cardiovascular outcomes.4 BP is recorded every 15–30 min over the entire span of 24 h. As per the ACC/AHA 2017 guidelines, a normotensive patient should have a daytime ABPM <120/80 mm Hg and a night time ABPM < 100/65 mm Hg.3 Even though ABPM can detect very fine changes in the BP variation in the circadian rhythm, the clinical significance of BP variability other than diurnal variation (such as beat-to-beat variation) remains uncertain.8
3. Technique
Whereas standard office BP readings often make use of manual labour with a sphygmomanometer, ambulatory BP is measured by automatic BP monitors and use oscillometric technique.8 The cuff is wrapped around on the upper arm, which should be kept still while recording. The American Society of Hypertension and International Society of Hypertension guidelines 2014 state that wrist and finger cuffs are often inaccurate, and arm cuffs should be preferred.9 The cuff is inflated, and then while gradually deflating it, the oscillations start appearing when the pressure is gradually decreased and disappear at a level lower than the diastolic blood pressure, with the point of maximal oscillations denoting the mean arterial BP10 and the entire area known as the oscillation envelope.
The point of maximal oscillations, denoting the mean arterial pressure, divides the oscillations into a rising phase (from the start of the oscillations to the point of maximal oscillations) and a falling phase (from the point of maximal oscillations to the disappearance of the oscillations). One can use characteristic empiric oscillation ratios to identify a systolic pressure point on the rising phase of the pressure tracing and a diastolic pressure point on the falling phase. However, calculation of systolic and diastolic blood pressures is usually not defined using this method for multiple reasons, including that these ratios are highly sensitive to changes in physiological conditions, including change in pulse pressure and variability in the degree of arterial stiffness.11 Hence, every 15–30 min, the BP is recorded, and readings are then analysed using a computer, with the simultaneous calculation of systolic and diastolic BP using complicated algorithms.10, 8
The 2017 ACC/AHA guidelines have defined corresponding values of BP based on the site where BP is recorded, mode of measurement (office BP vs ambulatory BP) and the time of recording BP (day vs night time).3 For example, a BP of 120/80 mm Hg in a clinic setting is corresponding to an equal value of 120/80 mmHg in a daytime ABPM reading, 100/65 mm Hg in a nighttime ABPM reading and 115/75 mm Hg in a 24-h ABPM reading. Similarly, BP of 130/80 mm Hg (stage 1 hypertension) based on office readings corresponds to an equal value of 130/80 mm Hg in a daytime ABPM record, 110/65 mm Hg in nighttime ABPM record and 125/75 in 24-h ABPM record.
Ambulatory BP can be monitored with a tonometric watch-like device, which captures the radial pulse wave reflection and thereby calculates ambulatory brachial BP. Such wrist devices have been previously validated and have met the European society of Hypertension (ESH) and Advancing safety in Medical Technology standards.
There are important indices in ABPM report, which help in its interpretation, which are listed as follows:
-
1.
Hyperbaric index (HBI) is one of the indices which might indicate the BP load on various organs. Its interpretation can be correlated with underlying organ damage, including kidney damage, diabetes mellitus and other diseases. It is calculated as the area between the ABPM graph the boundary line of hypertension. A recently published article showed HBI to be a sensitive indicator for reduction in renal function.12
-
2.
The diurnal/dipping index is another index which can be indicative of underlying target organ damage or inappropriate antihypertensive treatment. It is calculated by dividing the difference between day and nighttime mean BP, respectively, by mean daytime BP and multiplying the resultant value by 100.13 There is not much literature available on its utility, and further studies need to be carried out to understand its absolute significance.
-
3.
BP load refers to the percentage of ABPM readings above the 95th percentile during the entire 24-h period, both for systolic and diastolic pressures.13
-
4.
Nocturnal dipping is one of the most important indices on the ABPM report. The presence and absence, and also the degree of dipping, have been used in the prognosis of underlying organ damage, diabetes mellitus and other diseases. Morning surge is also one the indices which can be interpreted. Dipping and morning surge have been explained further in this article.
-
5.
Other indices may include hypertensive time index and hypotensive index. Hypertensive time index refers to the proportion of time duration that the BP has remained above reference normal limits. On the other hand, hypotensive time index refers to the proportion of time that the BP has remained lower than the reference normal range. They have not been studied into much extent, and more data are required to understand their utility.
4. Advantages and limitations
Advantages include the possibility of removal of the cuff during shower, the fact that a brachial artery transducer is not required and an error margin within 5 mm Hg of the standard mercury sphygmomanometer.10, 14 Automated oscillometric BP monitors are of much use in critical care patients to detect significant changes in the pattern of BP variability.
However, role of oscillatory method in out-of-office screening of elevated BP and hypertension can be doubtful, as the accuracy of detection of systolic and diastolic blood pressure readings is questionable.11 Another limitation of this technique includes the inability to accurately record BP during physical activity.10 The reproducibility of ABPM data is also questionable, and there often occurs inability to detect artefacts in the measurement.15 Patients often report discomfort while sleeping, and may choose not to get it repeated, in case required. Other limitations may include limited availability, high cost, lack of knowledge, awareness and approach of different practitioners towards ambulatory monitoring and scarcity of research over the potential benefits of ABPM.
Home BP monitoring (HBPM) and ABPM are the two modalities which can be used to monitor BP variability. HBPM refers to obtaining serial BP readings at home or at work but not in a continuous fashion, unlike ABPM. Even though there is no evidence strong enough to support the superiority of ABPM over HMPM in the management of hypertension, there are some concepts which can be used to understand it. ABPM is continuous and can elucidate the diurnal variation (especially nocturnal changes) better than HBPM,15 which is discontinuous monitoring at specific periods of time during the day. There is more evidence highlighting the significance of ABPM with cardiovascular events and/or mortality than HBPM.16
Validity of the readings on ABPM requires certain criteria, none of which is said to be the best. These include obtaining around 70% of the planned readings or recording of at least 14 daytime readings or obtaining at least 10 daytime and 5 nighttime readings.17
5. Ambulatory BP dipping
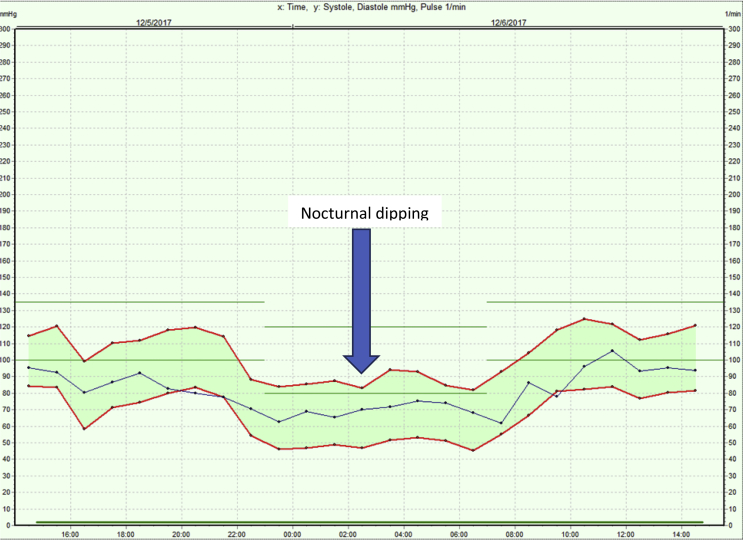
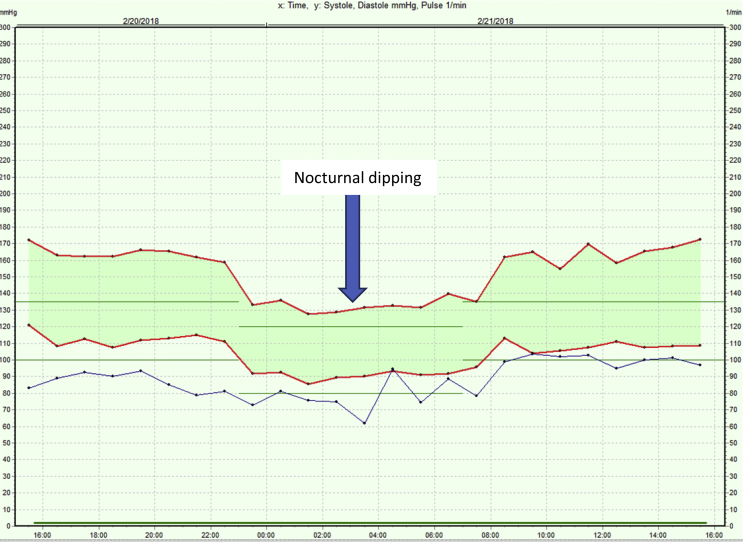
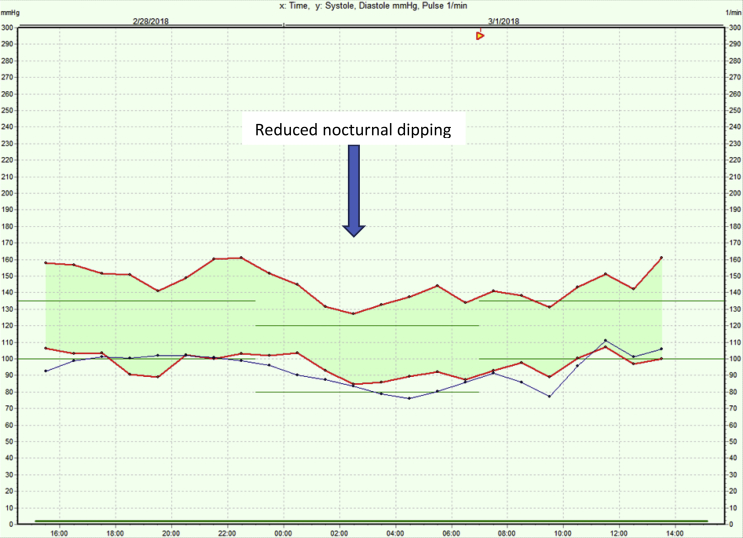
Dipping of BP during night (nocturnal dipping) is a common normal phenomenon (Fig. 1, Fig. 2), occurring in more than 50% of the population, which leads to the nocturnal BP being 10%–20% lower than awake BP.4 It can be observed only in ABPM, not in HBPM or office BP. When the dip is less than 10% of daytime BP, the person is said to be a nondipper (Fig. 3). Other alterations include reverse dipping (rise in nighttime BP) and extreme dipping (nocturnal BP falls more than 20% of the daytime BP).18 Nondipping is different from nocturnal hypertension, which is an elevation of nighttime BP, whereas nondipping arises because of improper control and regulation mechanism of BP.18 Nondipping and reverse dipping have been shown to be associated with more organ damage, including cardiovascular (left ventricular [LV] hypertrophy), cerebrovascular (stroke) and renal (proteinuria) disorders, with the rate being more in reverse dippers than in nondippers. Extreme dippers have been known to have increased stroke rates.18 Another aspect to be understood is the morning surge, which is a physiological neural and humoral response composing of activation of sympathetic system. Excess surge is known to be associated with stroke, myocardial infarction and sudden death.19
Fig. 1.
Normotension with preserved nocturnal dipping. Average daytime and nighttime systolic and diastolic blood pressure values within normal limits.
Fig. 2.
Systo-diastolic hypertension with reduced nocturnal dipping. Average daytime and nighttime systolic and diastolic blood pressure values more than normal limits.
Fig. 3.
Systo-diastolic hypertension with reduced nocturnal dipping. Average daytime and nighttime systolic and diastolic blood pressure values more than normal limits.
6. Ambulatory BP in clinical practice
In clinical practice, ABPM has diagnostic, prognostic and therapeutic utility. ABPM remains the gold standard test to diagnose hypertension, including white coat, masked and nocturnal hypertension.20 Ambulatory BP has been known to help start treatment of hypertension in patients with differential cardiovascular risks,4 which may include low-risk patients with white coat hypertension, or with high risk, including sustained hypertensive patients. Other indications might include screening for obstructive sleep apnoea, and in patients with postprandial heart rate variability and hypotensive symptoms, to rule out autonomic malfunction.21 Genetic syndromes such as neurofibromatosis type 1, Turner syndrome and Williams syndrome, which may have underlying renal artery stenosis and/or aortic coarctation.13 For patients on treatment for hypertension, it can be useful in monitoring antihypertensive therapy, development of hypotensive symptoms on treatment, drug resistance and correlation with office BP readings. However, office BP readings are still used in the monitoring of antihypertensive therapy.
6.1. White coat hypertension
White coat hypertension is an entity of falsely elevated BP in the office setting, whereas the BP readings at home (with ABPM) are normal. It should be suspected in cases with BP more than 130/80 mm Hg but less than 160/100 mm Hg and daytime ambulatory BP readings less than 130/80 mm Hg.3 Its incidence is more common in older adults, women, smokers and people without end organ damage.22 In a recent database analysis study of 2209 patients by Tocci et al23, 351 patients (15.9%) had white coat hypertension, which was associated with increased risk of hospitalization due to hypertension, myocardial infarction and heart failure. Even though white coat hypertension is a false elevation of BP in the office, such patients do not need treatment apart from lifestyle modification and annual ambulatory BP or home BP monitoring to assess progression to sustained hypertension.3 Hence, not only does the misdiagnosis and mistreatment of these patients as true hypertensives put them at unnecessary chronic medication use but it is also not cost efficient, and this is avoidable with the use of ABPM.22, 24
6.2. Resistant hypertension
White coat hypertension is also known to occur in patients on drug therapy. Many patients of suspected resistant hypertension turn out to be white coat hypertensives, i.e., they have well-controlled BP on ambulatory BP readings but falsely elevated office readings. In a study of 8295 patients with resistant hypertension, de la Sierra et al25 found out that 37.5% of patients had white coat resistance. The latest ACC/AHA guidelines recommend screening of white coat hypertension in hypertensive patients on three or more medications, with the office BP 5–10 mm Hg more than the goal, which is confirmed with normal home or ambulatory BP reading.3 Hence, ambulatory readings should be considered before dose escalation of a medication or starting a new medicine.4
6.3. Masked hypertension
When a patient has a nonelevated BP reading in the office but elevated out-of-office BP reading, he/she is known to have masked hypertension (MH). More than 30% of the population with normal BP is diagnosed with MH, based on ambulatory BP readings.26 With the introduction of latest ACC/AHA criteria of BP elevation in 2017, the prevalence of MH and masked uncontrolled hypertension has doubled compared with ESH proposed criteria in 201327 (See Table 2). As stated previously, it is suspected in patients with elevated office BP at any time, people with left ventricular hypertrophy and normal or high normal BP, people with positive family history of hypertension in both parents and diabetic and obese individuals,28 and it should be screened if office BP is elevated (120–129/<80 mm Hg) for 3 months after lifestyle modification. It is confirmed with daytime ambulatory BP or home BP reading of ≥130/80 mm Hg.3 However, using only daytime ambulatory BP readings can result in underestimation of actual burden of the problem, and it is suggested that all daytime, nighttime, and 24-h ambulatory BP readings be taken.29 For example, in the Jackson Heart study, prevalence of MH on the basis of individual daytime, nighttime and 24-h readings was 22%, 41% and 26%, respectively, whereas overall prevalence using all three combined was 44.1%.30 Hence, all of them should be taken into consideration, but no single time period reading has been known to accurately calculate the prevalence.29 These patients are at increased risk of organ damage, including renal dysfunction (proteinuria, decreased GFR), increased left ventricular index and hypertrophy, carotid atherosclerosis, stroke, myocardial infarction and increased level of urine albumin-to-creatinine ratio and serum cystatin C.28, 29 These patients should continue lifestyle modification and be started on antihypertensive drugs. However, if the daytime ambulatory BP is not ≥130/80 mm Hg, it is treated as elevated BP with lifestyle modification and annual ambulatory BP and/or home BP reading.3
Table 2.
Comparison between the ESH 2013 criteria and the ACC/AHA 2017 criteria cut-off value of ABPM to diagnose masked hypertension (MH) and masked uncontrolled hypertension (MUCH) in patients with office BP <130/80 mm Hg on antihypertensive treatment.
| Criteria | ESH, 2013 | ACC/AHA, 2017 |
|---|---|---|
| Mean daytime ABPM | ≥135 or 85 mm Hg | ≥130/80 mm Hg |
| Mean 24-h ABPM | ≥130 or 80 mm Hg | ≥125/75 mm Hg |
| Mean night-time ABPM | ≥120 or 70 mm Hg | ≥110/65 mm Hg |
ACC/AHA, American College of Cardiology/American Heart Association; ESH, European Society of Hypertension; ABPM: ambulatory blood pressure monitoring.
6.4. Nocturnal hypertension
According to the latest ACC/AHA 2017 guidelines, nocturnal hypertension is defined as a BP more than 110/65 mm Hg (lowered from the earlier value of ≥120/70 mm Hg at night).3 According to a study of more than 30,000 untreated patients and more than 60,000 patients on antihypertensive therapy (from Spanish Ambulatory Blood Pressure monitoring registry), it's prevalence was found to be more than 40% in the untreated and nearly 50% in the treated group.31 As stated previously, nocturnal hypertension and nocturnal dipping are separate entities; however, both of them are associated with poor cardiovascular outcomes, either separately or together. Independently, nocturnal hypertension, even when not associated with nocturnal dip, has also been shown to have association with subclinical end organ damage, especially microalbuminuria.32 Cerebrovascular bleeding, smoking and diabetes also correlate with nocturnal hypertension. Although female sex is more commonly associated with nocturnal dipping, the prevalence of nocturnal hypertension is found to be greater in the male population.31 Control of nighttime BP carries more significance in patients with once daily morning dosage of antihypertensive medication, as the BP is usually well controlled during the day.33 In a large cohort study, night time BP elevation in patients on antihypertensive medication had a poor prognostic outcome in regards to cardiovascular complications (fatal and nonfatal), as the BP was controlled during the day but remained elevated at night.34
6.5. Pregnancy
Ambulatory BP has been shown to be useful in monitoring BP in pregnant women, especially during the last trimester of pregnancy. It has been shown to predict the outcome of pregnancy, with hypertensive patients being at an increased risk of lower segment cesarean section.35 Normal values of ambulatory BP in various trimesters of pregnancy are available, and they are usually higher than conventional BP.36 ABPM in pregnant women can also help predict the development of preeclampsia and/or IUGR (intrauterine growth retardation); however, there are no guidelines which take into account its role in the management of these conditions, either antepartum or intrapartum.36 The most significant use of ABPM in pregnancy is to rule out white coat hypertension, the prevalence of which was found to be about 30% in a study by Bellomo et al. These women can avoid the use of antihypertensive medication without any impact on the outcome of the pregnancy.35, 37
6.6. Monitoring drug therapy
ABPM is indicated in all patients before starting pharmacological therapy. In addition to the potential initiation of antihypertensive therapy, ABPM can also be used to monitor therapy in patients already on antihypertensive drug(s). For example, after initiation of therapy, ABPM should be repeated within every 15–20 days to monitor for adequate effect until the desired BP is achieved. Once adequate control has been achieved, it can be repeated annually or biannually.38 The overall frequency of monitoring with ABPM depends on the degree of hypertension and treatment response with dose and/or medication alteration15. However, there are no standardized recommendations on the use of ABPM in monitoring the efficacy of antihypertensive treatment.38
6.7. Ambulatory hypotension and autonomic dysfunction
ABPM can be used to assess the BP variability over the entire course of 24 h, including the fall in BP. In a cohort study of more than 5000 elderly patients (≥80 years), more than 50% of them had hypotension on daytime ABPM, whereas no such BP changes were recorded on office BP readings.39 It can also be used to identify hypotensive events in young patients and in patients on antihypertensive medications.40
ABPM may also be used to monitor BP changes in patients with orthostatic hypotension, which is considered as an indicator of underlying autonomic disease. Such patients often report postprandial hypotension, inability of the heart rate to compensate for the fall in BP and reversal of normal circadian rhythm.41
6.8. Underlying systemic abnormalities
ABPM has been used in untreated hypertensive patients who present with snoring, to screen them for underlying obstructive sleep apnoea, with the changes including nocturnal hypertension and mild to moderate hypertension.42 It is also used in Parkinson’s disease, which can present with cardiovascular complications including supine hypertension, and postural hypotension being the most common findings. Other findings might include nondipping, postprandial and exercise-dependent hypotension, and drug (l-DOPA) induced hypotension.43 It can also be used in the assessment of stroke and in causes of endocrine hypertension, including adrenal disorders, pituitary disorders, thyroid disorders and diabetes.
6.9. ABPM in infants and children
ABPM has also been successfully used in infants, toddlers and children. The indications are similar as listed previously. Older children tolerate ABPM better. Careful precautions should be used in paediatric ABPM. Cuff size should be used appropriately. Pulse wave amplitude and elastic properties of arteries of children differ from adults; hence, the monitor and algorithm need validation using a standardized protocol.44 Parents should be trained to keep the arm of the child still while recording the reading. In addition, it is better to perform it on a school day (without significant exertion) to capture the BP variability with appropriate activity level. Despite numerous limitations including lack of normative data, technical difficulties and expense of the procedure, use of ABPM to diagnose hypertension and other indications is on the rise.
7. Follow up
When to consider repeating ABPM is largely at the discretion of the physician, based on underlying patient factors including high variability in BP, unexpected response to treatment, the presence of adverse risk factors and the need for straight night BP control in patient with heart disease, renal disease or diabetes.40 Owing to patient inconvenience, the chances of repeating are further limited. The most common reasons for repeating ABPM include equivocal results with initial measurement, to confirm the presence of white coat and MH, patients who have had poor results with antihypertensive therapy or who have had their treatment changed. It is also indicated to diagnose nocturnal hypertension as ABPM is the only noninvasive method to diagnose it.15
8. Contraindications
Even though ABPM has been shown to be superior to the office BP measurement, it has some contraindications, which need to be ruled out while taking the history. These include severe clotting disorders, severe cardiac rhythm abnormalities such as severe atrial fibrillation, and latex allergy, which can be found while using particular equipment brands. Use of the nondominant arm to apply the monitor, in case it has an arterio-venous fistula, is also contraindicated, as in patients on permanent dialysis.13
9. Conclusion
ABPM has become an indispensable tool in the diagnosis and management of hypertension and its therapy. Recent guidelines from ESC recommend that diagnosis of hypertension should be based on repeated office BP measurements or ABPM if economically feasible.45 Analysis of various indices on the ABPM graph, such as hyperbaric index, diurnal index, dipping and other indices can provide useful information about the prognosis of diseases such as hypertension, diabetes mellitus, CKD and so on. It can also be used to monitor the therapeutic efficacy of the antihypertensive treatment. In addition, ABPM is the single most effective tool to diagnose white coat, masked and nocturnal hypertension, it and can help direct the treatment in such patients when required. Overall, ABPM readings can guide towards the prognosis of underlying organ damage and can be a useful predictor of cardiovascular risk.
Conflicts of interest
All authors have none to declare.
Contributor Information
Apaar Dadlani, Email: apaar27@gmail.com.
Kushal Madan, Email: kushalmadan@gmail.com.
J.P.S. Sawhney, Email: jpssawhney@yahoo.com.
References
- 1.Mills K.T., Bundy J.D., Kelly T.N. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016 Aug 9;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geldsetzer P., Manne-Goehler J., Theilmann M. Diabetes and hypertension in India: a nationally representative study of 1.3 million adults. JAMA Intern Med. 2018 Mar 1;178(3):363–372. doi: 10.1001/jamainternmed.2017.8094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whelton P.K., Carey R.M., Aronow W.S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of cardiology/American heart association task force on clinical practice guidelines. Hypertension. 2018 Jun 1;71(6):1269–1324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 4.Turner J.R., Viera A.J., Shimbo D. Ambulatory blood pressure monitoring in clinical practice: a review. Am J Med. 2015 Jan;128(1):14–20. doi: 10.1016/j.amjmed.2014.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devi P., Rao M., Sigamani A. Prevalence, risk factors and awareness of hypertension in India: a systematic review. J Hum Hypertens. 2013 May;27(5):281–287. doi: 10.1038/jhh.2012.33. [DOI] [PubMed] [Google Scholar]
- 6.Turner J.R., Hoofwijk T.J. Clinical trials in new drug development. J Clin Hypertens Greenwich Conn. 2013 May;15(5):306–309. doi: 10.1111/jch.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grossman E. Ambulatory blood pressure monitoring in the diagnosis and management of hypertension. Diabetes Care. 2013 Aug;36(Suppl 2):S307–S311. doi: 10.2337/dcS13-2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pickering T.G., Shimbo D., Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006 Jun 1;354(22):2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 9.Weber M.A., Schiffrin E.L., White W.B. Clinical practice guidelines for the management of hypertension in the community a statement by the American society of hypertension and the international society of hypertension. J Hypertens. 2014 Jan;32(1):3–15. doi: 10.1097/HJH.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 10.Ogedegbe G., Pickering T. Principles and techniques of blood pressure measurement. Cardiol Clin. 2010 Nov;28(4):571–586. doi: 10.1016/j.ccl.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Babbs C.F. Oscillometric measurement of systolic and diastolic blood pressures validated in a physiologic mathematical model. Biomed Eng Online. 2012 Aug 22;11:56. doi: 10.1186/1475-925X-11-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iimuro S., Imai E., Watanabe T. Hyperbaric area index calculated from ABPM elucidates the condition of CKD patients: the CKD-JAC study. Clin Exp Nephrol. 2015;19(1):114–124. doi: 10.1007/s10157-014-0965-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Flynn J.T., Daniels S.R., Hayman L.L. Update: ambulatory blood pressure monitoring in children and Adolescents: a scientific statement from the American heart association. Hypertension. 2014 May 1;63(5):1116–1135. doi: 10.1161/HYP.0000000000000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Brien E., Pickering T., Asmar R. Working group on blood pressure monitoring of the european society of hypertension international protocol for validation of blood pressure measuring devices in adults. Blood Press Monit. 2002 Feb;7(1):3–17. doi: 10.1097/00126097-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 15.O'Brien E., Parati G., Stergiou G. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013 Sep;31(9):1731–1768. doi: 10.1097/HJH.0b013e328363e964. [DOI] [PubMed] [Google Scholar]
- 16.Verdecchia P., Angeli F., Mazzotta G., Gentile G., Reboldi G. Home blood pressure measurements will not replace 24-hour ambulatory blood pressure monitoring. Hypertens Dallas Tex 1979. 2009 Aug;54(2):188–195. doi: 10.1161/HYPERTENSIONAHA.108.122861. [DOI] [PubMed] [Google Scholar]
- 17.Shimbo D., Abdalla M., Falzon L., Townsend R.R., Muntner P. Role of ambulatory and home blood pressure monitoring in clinical practice: a narrative review. Ann Intern Med. 2015 Nov 3;163(9):691–700. doi: 10.7326/M15-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vij R., Peixoto A.J. Management of nocturnal hypertension. Expert Rev Cardiovasc Ther. 2009 Jun 1;7(6):607–618. doi: 10.1586/erc.09.42. [DOI] [PubMed] [Google Scholar]
- 19.Bilo G., Grillo A., Guida V., Parati G. Morning blood pressure surge: pathophysiology, clinical relevance and therapeutic aspects. Integrated Blood Pres Contr. 2018 May 24;11:47–56. doi: 10.2147/IBPC.S130277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parati G., Stergiou G., O'Brien E. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014 Jul;32(7):1359–1366. doi: 10.1097/HJH.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 21.Kinsara A.J. Ambulatory blood pressure monitoring in daily practice. Indian Heart J. 2017 Dec;69(6):788–789. doi: 10.1016/j.ihj.2017.09.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Franklin S.S., Thijs L., Hansen T.W., O'Brien E., Staessen J.A. White-coat hypertension: new insights from recent studies. Hypertens Dallas Tex 1979. 2013 Dec;62(6):982–987. doi: 10.1161/HYPERTENSIONAHA.113.01275. [DOI] [PubMed] [Google Scholar]
- 23.Tocci G., Presta V., Figliuzzi I. Prevalence and clinical outcomes of white-coat and masked hypertension: analysis of a large ambulatory blood pressure database. J Clin Hypertens Greenwich Conn. 2018 Feb;20(2):297–305. doi: 10.1111/jch.13181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lovibond K., Jowett S., Barton P. Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study. Lancet Lond Engl. 2011 Oct 1;378(9798):1219–1230. doi: 10.1016/S0140-6736(11)61184-7. [DOI] [PubMed] [Google Scholar]
- 25.de la Sierra A., Segura J., Banegas J.R. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertens Dallas Tex 1979. 2011 May;57(5):898–902. doi: 10.1161/HYPERTENSIONAHA.110.168948. [DOI] [PubMed] [Google Scholar]
- 26.Palla M., Saber H., Konda S., Briasoulis A. Masked hypertension and cardiovascular outcomes: an updated systematic review and meta-analysis. Integrated Blood Pres Contr. 2018;11:11. doi: 10.2147/IBPC.S128947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sierra A de la, Banegas J.R., Vinyoles E. Prevalence of masked hypertension in untreated and treated patients with office blood pressure below 130/80 mm Hg. Circulation. 2018 Apr 30;118:034619. doi: 10.1161/CIRCULATIONAHA.118.034619. CIRCULATIONAHA. [DOI] [PubMed] [Google Scholar]
- 28.Aronow W.S. vol. 5. 2017 Dec. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5733331/ (Masked Hypertension. Ann Transl Med [Internet]). [cited 2018 Jun 8]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anstey D.E., Pugliese D., Abdalla M., Bello N.A., Givens R., Shimbo D. An update on masked hypertension. Curr Hypertens Rep. 2017 Oct 25;19(12):94. doi: 10.1007/s11906-017-0792-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Omboni S., Aristizabal D., De la Sierra A. Hypertension types defined by clinic and ambulatory blood pressure in 14 143 patients referred to hypertension clinics worldwide. Data from the ARTEMIS study. J Hypertens. 2016;34(11):2187–2198. doi: 10.1097/HJH.0000000000001074. [DOI] [PubMed] [Google Scholar]
- 31.de la Sierra A., Gorostidi M., Banegas J.R., Segura J., de la Cruz J.J., Ruilope L.M. Nocturnal hypertension or nondipping: which is better associated with the cardiovascular risk profile? Am J Hypertens. 2014 May;27(5):680–687. doi: 10.1093/ajh/hpt175. [DOI] [PubMed] [Google Scholar]
- 32.Oliveras A., Armario P., Martell-Clarós N., Ruilope L.M., de la Sierra A. Spanish Society of Hypertension-Resistant Hypertension Registry. Urinary albumin excretion is associated with nocturnal systolic blood pressure in resistant hypertensives. Hypertens Dallas Tex 1979. 2011 Mar;57(3):556–560. doi: 10.1161/HYPERTENSIONAHA.110.165563. [DOI] [PubMed] [Google Scholar]
- 33.Kario K. Nocturnal hypertension: new Technology and evidence. Hypertension. 2018 Jun 1;71(6):997–1009. doi: 10.1161/HYPERTENSIONAHA.118.10971. [DOI] [PubMed] [Google Scholar]
- 34.Boggia J., Li Y., Thijs L. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet Lond Engl. 2007 Oct 6;370(9594):1219–1229. doi: 10.1016/S0140-6736(07)61538-4. [DOI] [PubMed] [Google Scholar]
- 35.Bellomo G., Narducci P.L., Rondoni F. Prognostic value of 24-hour blood pressure in pregnancy. JAMA. 1999 Oct 20;282(15):1447–1452. doi: 10.1001/jama.282.15.1447. [DOI] [PubMed] [Google Scholar]
- 36.Brown M.A. Is there a role for ambulatory blood pressure monitoring in pregnancy? Clin Exp Pharmacol Physiol. 2014 Jan;41(1):16–21. doi: 10.1111/1440-1681.12106. [DOI] [PubMed] [Google Scholar]
- 37.Shahbazian N., Shahbazian H., Mohammadjafari R., Mousavi M. Ambulatory monitoring of blood pressure and pregnancy outcome in pregnant women with white coat hypertension in the third trimester of pregnancy. J Nephropharmacol. 2013 Jan 1;2(1):5–9. [PMC free article] [PubMed] [Google Scholar]
- 38.O'Brien E., Dolan E. Ambulatory blood pressure monitoring for the effective management of antihypertensive drug treatment. Clin Ther. 2016 Oct;38(10):2142–2151. doi: 10.1016/j.clinthera.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 39.Divisón-Garrote J.A., Ruilope L.M., de la Sierra A. Magnitude of hypotension based on office and ambulatory blood pressure monitoring: results from a cohort of 5066 treated hypertensive patients Aged 80 Years and older. J Am Med Dir Assoc. 2017 May 1;18(5):452.e1–452.e6. doi: 10.1016/j.jamda.2017.01.015. [DOI] [PubMed] [Google Scholar]
- 40.O'Brien E., Coats A., Owens P. Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British Hypertension Society. BMJ. 2000 Apr 22;320(7242):1128–1134. doi: 10.1136/bmj.320.7242.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Alquadan K.F., Singhania G., Koratala A., Ejaz A.A. vol. 23. 2017 Mar 15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5351249/ (Office Orthostatic Blood Pressure Measurements and Ambulatory Blood Pressure Monitoring in the Prediction of Autonomic Dysfunction. Clin Hypertens [Internet]). [cited 2018 Jul 17]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Torres G., Sánchez-de-la-Torre M., Martínez-Alonso M. Use of ambulatory blood pressure monitoring for the screening of obstructive sleep apnea. J Clin Hypertens Greenwich Conn. 2015 Oct;17(10):802–809. doi: 10.1111/jch.12619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stuebner E., Vichayanrat E., Low D.A., Mathias C.J., Isenmann S., Haensch C.-A. vol. 4. 2013 May 15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3654335/ (Twenty-four Hour Non-invasive Ambulatory Blood Pressure and Heart Rate Monitoring in Parkinson's Disease. Front Neurol [Internet]). [cited 2018 Jul 17]. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stergiou G.S., Boubouchairopoulou N., Kollias A. Accuracy of automated blood pressure measurement in children: evidence, issues, and perspectives. Hypertens Dallas Tex 1979. 2017;69(6):1000–1006. doi: 10.1161/HYPERTENSIONAHA.116.08553. [DOI] [PubMed] [Google Scholar]
- 45.Williams B., Mancia G., Spiering W. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep 1;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]