Abstract
Objective
Fractional flow reserve (FFR) using adenosine has been the gold standard in the functional assessment of intermediate coronary stenoses in the catheterization laboratory. We aim to study the correlation of adenosine-free indices such as whole cycle Pd/Pa [the ratio of mean distal coronary pressure (Pd) to the mean pressure observed in the aorta (Pa)], instantaneous wave-free ratio (iFR), and contrast-induced submaximal hyperemia (cFFR) with FFR.
Methods
This multicenter, prospective, observational study included patients with stable angina or acute coronary syndrome (>48 h since onset) with discrete intermediate coronary lesions (40–70% diameter stenosis). All patients underwent assessment of whole cycle Pd/Pa, iFR, cFFR, and FFR. We then evaluated the correlation of these indices with FFR and assessed the diagnostic efficiencies of them against FFR ≤0.80.
Results
Of the 103 patients from three different centers, 83 lesions were included for analysis. The correlation coefficient (r value) of whole cycle Pd/Pa, iFR, and cFFR in relation to FFR were +0.84, +0.77, and +0.70 (all p values < 0.001), respectively, and the c-statistic against FFR ≤0.80 were 0.92 (0.86–0.98), 0.89(0.81–0.97), and 0.91 (0.85–0.97) (all p values < 0.001), respectively. The best cut-off values identified by receiver–operator characteristic curve for whole cycle Pd/Pa, iFR, and cFFR were 0.94, 0.90, and 0.88, respectively, for an FFR ≤0.80. By the concept of “adenosine-free zone” (iFR = 0.86–0.93), 59% lesions in this study would not require adenosine.
Conclusion
All the three adenosine-free indices had good correlation with FFR. There is no difference in the diagnostic accuracies among the indices in functional evaluation of discrete intermediate coronary stenoses. However, further validation is needed before adoption of adenosine-free pressure parameters into clinical practice.
Keywords: Intermediate coronary stenosis, Fractional flow reserve, Instantaneous wave-free ratio, Whole cycle Pd/Pa, Contrast FFR
1. Introduction
Coronary angiography has limited role in the evaluation of hemodynamic significance of coronary stenosis which needs additional noninvasive or invasive diagnostic modalities. Functional assessment of stenosis in the coronary vasculature in catheterization laboratory is performed by measuring either intracoronary flow velocity (coronary flow velocity reserve CFR) or pressure [fractional flow reserve FFR)] or both [hyperemic stenotic resistance HSR)].1 Of these parameters, the use of FFR has been supported by adequate evidence demonstrating its value in clinical decision-making and has also been shown to improve clinical outcomes.2
In spite of its proven diagnostic value, FFR has not been widely adapted because of the need for adenosine for hyperemia and its associated side-effects. Recent research is directed toward identification of adenosine-free indices to determine the functional significance of intermediate coronary lesions with comparable diagnostic accuracies to FFR.3 In this regard, various parameters such as whole cycle Pd/Pa [the ratio of mean distal coronary pressure (Pd) to the mean pressure observed in the aorta (Pa)], instantaneous wave-free ratio (iFR), and contrast-FFR are being evaluated.4, 5, 6 Our study aims to compare the diagnostic accuracies of whole cycle Pd/Pa, iFR, and contrast-FFR against the gold standard measurement, adenosine-FFR, in intermediate coronary lesions.
2. Materials and methodology
This is a multicenter, prospective observational study (CTRI/2017/08/009537) to assess the intermediate coronary lesions with specific pressure indices. The measured pressure indices included whole cycle Pd/Pa at rest, iFR at rest, contrast-FFR measured during submaximal hyperemia, and FFR measured during maximal hyperemia with adenosine. The definitions followed in the study have been enlisted in Supplementary Table 1. The study was approved by institutional ethics committee of each of the participating hospitals.
The study was conducted in three centers in South India. The patients included in the study were those with stable angina or acute coronary syndromes (ACSs) (nonculprit vessels and culprit vessels >48 h from symptoms onset in the case of myocardial infarction) with coronary lesions ranging from 40% to 70% diameter stenosis in one or more native major epicardial vessels or its branches, at least 2 mm in diameter, as estimated by visual assessment. The exclusion criteria have been enlisted in the Supplementary Table 2. These criteria were designed to exclude all possible confounders of measurement of pressure indices.
Cardiac catheterization was performed either by radial or femoral access. Clinical parameters such as pulse rate, systolic blood pressure, and diastolic blood pressure were recorded at the time of the study. The lesion was profiled in two orthogonal angiographic views. Intracoronary nitroglycerine (200 μg) was administered to minimize epicardial resistance. A dedicated 0.014-inch pressure sensor–tipped wire (VerrataR coronary pressure wire, Volcano Corporation) was introduced at least three vessel diameters beyond the lesion after equalization. The whole cycle Pd/Pa was obtained at rest. An iFR reading was obtained by switching on the iFR algorithm on the console. Then, adenosine was used intravenously in all the patients at a dose of 140μ/kg/min through the antecubital vein. The measurement of FFR was made at 1 min after confirmation of steady-state hyperemia. After pressures returned to baseline, submaximal hyperemia was achieved by injecting around 6–8 ml of radiocontrast material (iohexol/iodixanol) into the coronary artery, following which the measurement of contrast-FFR was made. The pressure wire was pulled back at the end of the procedure to assess pressure drift. A drift of ±0.02 was considered erroneous, and the whole procedure was repeated.
Baseline demographics and procedure details were recorded for all the patients. All the pressure data were captured from the console after procedure and were analyzed offline at the Indian Cardiology Research Foundation core laboratory in a blinded fashion, independently, by two certified technicians and verified by a physician using a custom software package designed with Matlab (Mathworks, Inc., Natick, Massachusetts) and CoreR integrated console, Volcano corporation). The algorithm used for calculation of “iFR” (HarvestR, Volcano corporation) considered five consecutive cardiac cycles and a wave-free period for mean Pd/Pa measurement which was calculated from mathematical equations. “Whole cycle Pd/Pa” was calculated in similar fashion to iFR except that Pd/Pa was time averaged over the entire cardiac cycle using the FFR function of the console, thus including both systole and diastole. “Contrast-FFR” value was measured as the lowest Pd/Pa value following injection of the contrast. “Adenosine-FFR” was calculated independently from the original readout as the lowest artifact-free Pd/Pa during maximal steady-state hyperemia. Quantitative coronary angiography was performed by experienced observers who were blinded to the FFR findings at the Cardio-vascular angiographic analysis systems work-station (version 7.5, Pie medical imaging, Netherlands).
The primary objective of the trial was to study the correlation of whole cycle Pd/Pa, iFR, and contrast Pd/Pa with the existing standard-FFR. The secondary objectives were (1) to study the correlation of iFR with FFR across various subgroups; (2) to derive at best cut-off values for whole cycle Pd/Pa, iFR, and contrast Pd/Pa in relation to FFR≤0.80, by a receiver–operator characteristic curve (ROC) analysis; (3) to study the diagnostic efficiencies of whole cycle Pd/Pa, iFR, and contrast Pd/Pa at prespecified cut-off values in relation to FFR≤0.80; (4) to study the discordancy rate of iFR at a cut-off of 0.90 in relation to FFR≤0.80; (5) to study the proportion of patients in the “adenosine-free zone” using a prespecified cut-off range of iFR (0.86–0.93); and (6) to study the various predictors of iFR<0.90. Values of FFR ≤0.80 and iFR <0.90 were considered positive for ischemia. The treatment of the coronary lesion was left to the discretion of the treating physician.
3. Statistics
Given the observational design of the study, the primary analysis has been descriptive in nature. Statistical tests assessing observed difference in proportions have been analyzed by chi-square test. Total sample size required to determine whether the correlation coefficient would differ from 0 was 29, based on assumptions of α = 0.05, β = 0.2, and r = 0.5. The relationship between the FFR and each of the pressure indices for the entire patient population, prespecified cohorts, and all subsequent subgroup analyses have been quantified with a Pearson's product–moment correlation coefficient. Receiver-operator characteristic curves have been used to estimate the diagnostic efficiency of all the pressure indices and to identify the most appropriate cut-off value for each compared with the FFR treatment threshold of 0.8. Optimal cut-off values have been derived from ROC curves. Continuous variables have been expressed as mean (±standard deviation) or median (25th−75th percentile), and comparison has been performed using the Student t test. Categorical variables have been presented as frequencies (percentage) and compared with the χ2 test. A 2-sided a-level of 0.05 has been considered statistically significant.
4. Results
A total of 106 coronary lesions of intermediate severity from 103 patients were enrolled during the study period. Eighty-three lesions were suitable for final analysis, and 23 were excluded as they involved in-stent restenosis, diffuse/tandem lesions, poor recordings, and significant renal derangements. A pressure drift was recorded in 21 lesions (19.8%) requiring reassessment. Of them, 14 lesions were excluded because of erroneous measurements during reassessment of pressure drift. The baseline demographic characteristics, distribution of coronary artery disease (CAD), and values of biochemical investigations are enlisted in Table 1. The lesion characteristics are shown in Table 2. The mean values of all the studied pressure indices in total and with respective to each epicardial vessel are provided in Supplementary Table 3. Iodixanol was used for contrast FFR measurements in 78.3% patients, and iohexol was used in the remaining. Adverse events were recorded in three patients during adenosine infusion: bradycardia in one and dyspnea in two patients. However, these events did not necessitate stoppage of adenosine. No procedural complications were recorded.
Table 1.
Demographic characteristics (n = 80).
| Variables | Mean ± SD/N (%) | Variables | Mean ± SD/N (%) | Variables | Mean ± SD/N (%) |
|---|---|---|---|---|---|
| Age | 58.4 ± 10 | CSA | 45 (56.2) | SVD | 26 (32.5) |
| Male | 54 (67.5) | UA | 12 (15) | DVD | 42 (52.5) |
| Diabetes mellitus | 41 (51.2) | NSTEMI (>48 h) | 10 (12.5) | TVD | 12 (15) |
| Smokers | 8 (10) | STEMI (>48 h) | 13 (16.2) | LAD | 74 (92.5) |
| Hypertension | 41 (51.2) | Time of study since MI (Days) | 17 ± 35 | LCX | 39 (48.7) |
| LVEF (%) | 55.5 ± 8 | Recent MI | 16 (20) | RCA | 54 (67.5) |
| Impaired LV function (EF <50%) | 12 (15) | Hb (g/dl) | 12.8 ± 1.7 | Se. urea (mg/dl) | 26 ± 12 |
| SBP on admission (mmhg) | 133 ± 21 | TC (mg/dl) | 133 ± 35 | Se. creatine (mg/dl) | 0.98 ± 0.28 |
| DBP on admission (mmhg) | 77 ± 11 | LDL (mg/dl) | 74 ± 33 | ||
| Pulse rate on admission (bpm) | 70 ± 11 |
All continuous variables are expressed as mean ± SD with 95% CI, and all categorical variables are represented as frequency (percentages).
LVEF, left ventricular ejection fraction; SBP- systolic blood pressure; DBP, diastolic blood pressure; CSA, chronic stable angina; UA, unstable angina; NSTEMI, non-ST elevation myocardial infarction; STEMI, ST elevation myocardial infarction; Hb, hemoglobin; TC, total cholesterol; LDL, low-density lipoprotein; SVD, single vessel disease; DVD, double vessel disease; TVD, triple vessel disease; LAD, left anterior descending artery; LCX, left circumflex artery; RCA, right coronary artery; Se., serum; SD, standard deviation; CI, confidence interval.
Table 2.
Lesion characteristics of “Intermediate stenoses” (n = 83).
| Type of lesion+ | Range of stenosis (%) | ||
| Type A | 61 (73.5) | LAD | 45–70 |
| Type B1 | 18 (21.7) | LCX | 30–70 |
| Type B2 | 4 (4.8) | RCA | 40–70 |
| Vessel involved | Quantitative analysis (n=68) | ||
| LAD | 48 (57.8) | Lesion length (mm) | 17.7 ± 13.7 |
| LCX | 8 (9.6) | % Diameter stenosis | 50.4 ± 10 |
| RCA | 27 (32.5) | Plaque burden (cu.mm) | 32 ± 29 |
| Mean stenosis (Visual estimation, %) | RVD (mm) | 2.5 ± 0.6 | |
| LAD | 63 ± 17 | Range of % stenosis | 30–70 |
| LCX | 63 ± 23 | Range of lesion length (mm) | 3.82–57 |
| RCA | 64 ± 22 | Range of RVD (mm) | 1.5–4.6 |
All continuous variables are expressed as mean ± SD with 95% CI, and all categorical variables are represented as frequency (percentages).
+According to AHA classification of coronary lesions.
LAD, left anterior descending artery; LCX, left circumflex artery; RCA, right coronary artery; RVD-reference vessel diameter; SD, standard deviation; CI, confidence interval.
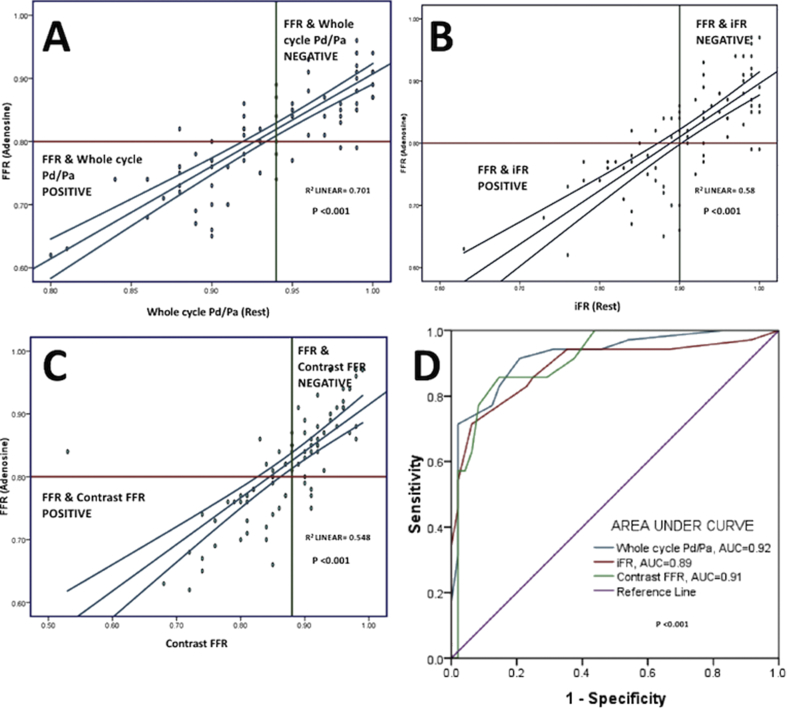
The correlation matrix of all the pressure indices in relation to FFR is shown in Table 3. All the three pressure indices–whole cycle Pd/Pa, iFR, and contrast-FFR had a significant correlation with FFR (Pearson's coefficient, r = +0.84, +0.77, +0.70, respectively). Table 3 also shows the c-statistic for whole cycle Pd/Pa, iFR, and contrast FFR in relation to a positive FFR (≤0.80) measurement: 0.92 (0.86–0.98), 0.89 (0.81–0.97), 0.91 (0.85–0.97), respectively (Fig. 1). In a post hoc analysis, iFR correlated with FFR in all the subgroups: males, diabetics, hypertensives, chronic stable angina, and ACS. The correlation of iFR with FFR was significant across all epicardial vessels: left anterior descending artery (+0.65), right coronary artery (+0.8), and left circumflex artery (+0.7). There was no significant influence of heart rate or blood pressure on the correlation of these pressure indices with FFR.
Table 3.
Correlation matrix for rest Pd/Pa, iFR, and contrast-Pd/Pa.
| Variables |
Whole cycle Pd/Pa |
iFR |
Contrast-FFR |
|||
|---|---|---|---|---|---|---|
| r value | p value | r value | p value | r value | p value | |
| FFR | +0.84 | <0.001 | +0.77 | <0.001 | +0.7 | <0.001 |
| Whole cycle Pd/Pa | – | +0.92 | +0.8 | |||
| Contrast-Pd/Pa | +0.81 | +0.79 | – | |||
| iFR | +0.92 | – | +0.79 | |||
| SBP (mmhg) | −0.12 | 0.3 | −0.08 | 0.49 | −0.12 | 0.3 |
| DBP (mmhg) | −0.2 | 0.06 | −0.19 | 0.1 | −0.2 | 0.05 |
| Pulse rate (per mt) | −0.05 | 0.6 | −0.12 | 0.3 | −0.8 | 0.5 |
| % stenosis | −0.3 | 0.006 | −0.31 | 0.01 | −0.2 | 0.7 |
| Lesion length (mm) |
−0.5 |
<0.001 |
−0.38 |
0.001 |
−0.4 |
<0.001 |
|
Whole cycle Pd/Pa |
iFR |
Contrast-FFR |
||||
|
AUC (95% CI) |
p value |
AUC (95% CI) |
p value |
AUC (95% CI) |
p value |
|
| FFR ≤0.80 | 0.92 (0.86–0.98) | <0.001 | 0.89 (0.81–0.97) | <0.001 | 0.91 (0.85–0.97) | <0.001 |
FFR, fractional flow reserve; iFR, instantaneous wave-free ratio; SBP-systolic blood pressure; DBP, diastolic blood pressure; AUC, area under curve; Pd/Pa, the ratio of mean distal coronary pressure (Pd) to the mean pressure observed in the aorta (Pa); CI, confidence interval; r value, correlation coefficient.
Fig. 1.
Panels A–C show scatter-plot of whole cycle Pd/Pa, iFR, and contrast-FFR values (x axis) and adenosine-FFR values (y axis) of all lesions and the correlation coefficient; Panel D shows the area under curve for whole cycle Pd/Pa, iFR, and contrast-FFR for diagnosing a positive FFR lesion (≤0.80). FFR, fractional flow reserve; iFR, instantaneous wave-free ratio; Pd/Pa, the ratio of mean distal coronary pressure (Pd) to the mean pressure observed in the aorta (Pa)
The best cut-off values for whole cycle Pd/Pa, iFR, and contrast-FFR revealed by ROC analysis to detect an FFR-positive lesion were 0.94, 0.90, and 0.88, respectively. The corresponding sensitivity and specificity were 83% and 85%, 74% and 90%, and 86% and 85%, respectively. Specificities of 100% were noted for rest Pd/Pa, iFR, and contrast Pd/Pa for an FFR-positive lesion at 0.88, 0.84, 0.83, respectively. The positive predictive values, negative predictive values, and diagnostic accuracies for an FFR-positive lesion were 80.6%, 87.2%, and 84.3%, respectively, for whole cycle Pd/Pa at a cut-off of 0.94; 84%, 83%, and 83.2%, respectively, for iFR at a cut-off of 0.90, and 81.1%, 89.1% and 85.5%, respectively for contrast FFR at a cut-off value of 0.88.
The agreement between iFR and FFR at cut-offs of 0.90 and 0.80, respectively, was 83.2% [74.3% for treatment and 89.6% for deferring percutaneous coronary intervention (PCI)]. Similarly, the agreement was 84.4% for whole cycle Pd/Pa at cut-off of 0.94 and 86.5% for contrast FFR at cut-off of 0.88. At prespecified cut-offs of iFR of ≤0.85 and ≥ 0.93, 59% lesions were outside the adenosine zone (Table 4).
Table 4.
Distribution of iFR and FFR at prespecified cut-offs.
| FFR treat | FFR “gray zone” | FFR defer | ||
|---|---|---|---|---|
| <0.75 | 0.75–0.80 | >0.80 | ||
| iFR treat | ≤0.85 | 9 | 6 | 1 |
| iFR “adenosine zone” | 0.86–0.93 | 7 | 11 | 16 |
| iFR defer | >0.93 | 0 | 2 | 31 |
FFR, fractional flow reserve; iFR, instantaneous wave-free ratio.
In a post hoc regression analysis to study the predictors of a positive iFR (<0.90), only FFR ≤0.80 had a significant association among other variables: age, males, diabetics, hypertensives, left ventricular ejection fraction (LVEF), chronic stable angina, ACS, and hemodynamic variables such as heart rate and blood pressure. A post hoc analysis was also performed to study the correlation, diagnostic performance, and area under curve (AUC) by ROC analysis of each of the pressure indices in comparison to FFR in the subset of patients with stable CAD and ACS. The results are highlighted in Table 5. Each of the pressure indices correlated well with FFR irrespective of the subclassification into stable CAD and ACS; however, the correlation, area under curve, and diagnostic accuracies were better in stable CAD than in patients with ACS.
Table 5.
Post hoc analysis of pressure indices in stable CAD and ACS patients.
| Studied pressure indices | Stable CAD patients (n = 45) | ACS patients (n = 35) |
|---|---|---|
| Correlation | ||
| Whole cycle Pd/Pa vs FFR | +0.88 | +0.78 |
| iFR vs FFR | +0.81 | +0.74 |
| Contrast-FFR vs FFR | +0.76 | +0.81 |
| Area under curve by ROC analysis (against FFR≤ 0.80) | ||
| Whole cycle Pd/Pa | 0.98 (0.94–1) | 0.88 (0.76–0.99) |
| iFR | 0.96 (0.92–1) | 0.79 (0.64–0.96) |
| Contrast-FFR | 0.94 (0.87–1) | 0.88 (0.76–0.98) |
| Diagnostic accuracy (against FFR≤ 0.80) | ||
| Whole cycle Pd/Pa (<0.94) | 87% | 80% |
| iFR (<0.90) | 89% | 77% |
| Contrast-FFR (<0.88) | 91% | 77% |
FFR, fractional flow reserve using adenosine; contrast-FFR, fractional flow reserve using contrast; iFR, instantaneous wave-free ratio; CAD, coronary artery disease; ACS, acute coronary syndrome; ROC, receiver–operating characteristic analysis; Pd/Pa, the ratio of mean distal coronary pressure (Pd) to the mean pressure observed in the aorta (Pa).
5. Discussion
Our study highlights the following findings: (1) iFR had a significant and positive correlation with FFR uniformly across all subgroups. The best diagnostic accuracies (83%) for iFR were observed at a cut-off of 0.90, wherein the study agreement was 83.2% between iFR and FFR at cut-offs of <0.90 and ≤ 0.80, respectively, and (2) rest Pd/Pa and contrast FFR also showed a positive correlation with FFR and the best diagnostic accuracies were observed at cut-offs of 0.94 and 0.88, respectively.
iFR performed using high-fidelity pressure wires isolates a specific period in diastole, called the wave-free period, and uses the ratio Pd/Pa over this period. Various studies have evaluated the correlation between iFR and FFR. In the ADVISE study, iFR correlated very closely with FFR (r = 0.9, p < 0.001), and a cut-off value of 0.83 showed the best diagnostic efficiency (AUC of 93%, at FFR <0.8, specificity, sensitivity, negative, and positive predictive values of 91%, 85%, 85%, and 91%, respectively).7 The RESOLVE study demonstrated an overall accuracy of 80% for both nonhyperemic indices-iFR and whole cycle Pd/Pa. The optimal iFR cut-off point for FFR ≤0.8 was 0.90 [C statistic: 0.81 (0.79–0.83); overall accuracy: 80.4%].8
Later, the ADVISE II study evaluated iFR at cut-off values of 0.85, 0.89, and 0.93 by analyzing 919 intermediate lesions.9 In this study, a cut-off value of 0.89 for iFR could correctly classify 82.5% of the stenoses with a sensitivity of 73.0% and specificity of 87.8% [c-statistic: 0.90 (0.88–0.92, p < 0.001)]. Similarly, in our study, at cut-off value of iFR<0.90, we could correctly classify 83.2% of the stenoses with a sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of 74%, 90%, 84%, 83%, and 83.2%, respectively [c-statistic: 0.89 (0.81–0.97, p < 0.001)]. The agreement between iFR and FFR was 89.6% for deferring PCI. The observed correlation coefficient of +0.77 between iFR and FFR was significant and uniform in all subgroups and was independent of heart rate or systemic blood pressure. Our study reports a correlation of +0.77 and AUC of 0.89 for iFR against FFR, which is comparable to the correlation of +0.8 and AUC of 0.89 observed in a recent meta-analysis.10
The “hybrid iFR–FFR” approach was introduced by the ADVISE II study. At prespecified values of iFR for treatment (≤0.85) and deferral (≥0.94), the hybrid iFR–FFR approach obviated vasodilators from 65.1% of patients and 69.1% of stenoses.9 Using the same cut-offs of iFR, our study also reveals 59% lesions in the adenosine-free zone. Also, a cut-off of <0.84 seems to be safe for deferring adenosine and treating patients as the specificities approached 100%. Similarly, a cut-off of ≥0.94 seems to be safe for deferring adenosine as well as PCI. Moreover, clinical studies of late, the iFR-SWEDEHEART and DEFINE-FLAIR, had validated the cut-off of 0.90 for iFR for clinical decision-making. These studies showed that coronary revascularization guided by iFR was noninferior to revascularization guided by FFR with respect to the risk of major adverse cardiac events at 1 year. The rate of adverse procedural signs and symptoms was lower, and the procedural time was shorter with iFR than with FFR.11, 12
Our study throws light on certain other pressure indices such as the whole cycle Pd/Pa and contrast-FFR. There have not been much studies with respect to these indices and their correlation with FFR. Also, clinical studies validating these variables in clinical decision-making are lacking. The current study showed a positive correlation between these pressure indices with FFR. We could also derive upon the cut-offs with the best diagnostic accuracies for these pressure indices. Whole cycle Pd/Pa, at rest, correlated with a positive FFR (≤0.80) at cut-off of <0.94 with sensitivity and specificity of 83% and 85%, respectively [c-statistic: 0.92 (0.86–0.98)]. A cut-off of 0.88 seems to be safe for deferring adenosine and treating patients as the specificity approached 100%. In the RESOLVE study, the optimal cut-off for whole cycle Pd/Pa was 0.92 [c-statistic: 0.82 (0.80–0.84); overall accuracy: 81.5%].8 In an earlier study, in an Asian cohort, the resting whole cycle Pd/Pa cut-off of 0.91 demonstrated a diagnostic accuracy of 82% (AUC: 0.9). However, iFR had higher discriminatory power than the resting whole cycle Pd/Pa.13
Several studies have demonstrated that contrast-FFR measured during submaximal hyperemia is a novel index and a feasible measurement method that accurately predicts the functional significance of intermediate coronary artery stenosis assessed by FFR.14, 15 The RINASCI study had shown a strong correlation between contrast FFR and adenosine FFR (r = 0.94, p < 0.001). In the study, ROC curve analysis showed an excellent accuracy of contrast FFR cut-off of ≤0.83 in predicting FFR value ≤ 0.80 [AUC: 0.97 (0.91–0.99, specificity 96.1%, sensitivity 85.7%)].16 In a recent analysis using contrast FFR, cut-off values of ≤0.83 in predicting an FFR value of ≤0.80 yielded a sensitivity of 100%, specificity of 96.1%, positive predictive value of 92.3%, negative predictive value of 100%, and diagnostic accuracy of 96%.17 In our study, the contrast FFR had a strong correlation with FFR (r = +0.7, p < 0.001) and had good diagnostic accuracies at cut-off of 0.88 [AUC: 0.91 (0.85–0.97) and sensitivities and specificity of 86%]. A cut-off of 0.83 seems to be safe for deferring adenosine and treating patients as the specificities approached 100%.
ACSs (unstable angina and myocardial infarction) constituted nearly half (43.8%) of the study group. In the ADVISE study, stable angina constituted 96% of the lesions. However, it must be emphasized that only those with intermediate lesions and time-lapse of at least 48 h since myocardial infarction and LVEF>40% were included in the study. Though the study involved a significant proportion of patients with ACS, a post hoc regression analysis did not reveal any significant influence of this variable on positive iFR. The correlation and AUC of each of the pressure indices were also significant compared with FFR in both stable CAD and ACS patients, however was better in patients with stable CAD. Similar conclusions of better diagnostic accuracies were observed for each of the pressure indices compared with FFR in patients of stable CAD than in patients of ACS. The results of our post hoc analysis are comparable to that of the FORECAST study, wherein iFR and FFR were studied in nonculprit vessels during the index procedure in 53 patients, the diagnostic accuracies iFR in ACS were not inferior, though numerically better in stable CAD (79.5% in ACS and 84.4% in CAD; p = 0.497), and correlation was also nonsignificant but slightly higher in stable CAD (r = 0.66 in ACS vs. r = 0.69 in CAD).18
Our study has certain limitations. The study followed strict exclusion criteria. Only discrete and intermediate type A and B lesions were included in the study, and hence the results would hold good only for similar lesions. We have studied newer pressure indices such as the whole cycle Pd/Pa and contrast-FFR which have not been validated in large studies. Pending validation of these indices in major clinical trials, the proposed cut-offs for rest Pd/Pa and contrast-FFR are not desirable for use in clinical practice. The sample size, though is small with only 83 intermediate lesions, was sufficient to prove a strong correlation of the measured pressure indices with FFR. Comparison of the study indices against a reference, such as a stress nuclear study, or an invasive flow-based parameter, such as coronary flow reserve or HSR index, would have added value to the study. A detailed analysis of the characteristics of classification disagreement would have added value to the study, however was not done considering the small numbers.
6. Conclusion
Our study, in a South-Asian cohort, reiterates the finding that iFR has good correlation with FFR and can be used in clinical practice at a cut-off of 0.90. Even with the hybrid iFR–FFR approach, a significant portion of patients can be spared from adenosine infusion. Whole cycle Pd/Pa and contrast-FFR correlated well with FFR, and best diagnostic efficiencies were observed at cut-offs of 0.94 and 0.88, respectively. All the correlations were significant in patients with ACS as well as in stable CAD.
Conflicts of interest
All authors have none to declare.
Source of funding
The research drew support and funding from the research council of the Madras Medical Mission.
What is already known?
FFR is the existing standard for assessment of intermediate coronary stenosis. FFR has been extensively validated in clinical studies and shown to improve clinical outcomes in evaluation of stenosis in stable CAD. However, measurement of FFR requires administration of adenosine for inducing maximal hyperemia. Search is on for adenosine-free indices such as iFR, whole cycle Pd/Pa, and contrast-FFR. iFR has been validated recently in clinical studies and found to be noninferior to FFR in clinical decision-making. However, there is not much insight into the other indices–whole cycle Pd/Pa and contrast-FFR.
What this study adds?
Our study shows that whole cycle Pd/Pa, iFR, and contrast-FFR correlate well with adenosine-FFR, and the best diagnostic efficiencies were observed at cut-offs of 0.94, 0.90, and 0.88, respectively, irrespective of the presentation with ACSs or stable CAD.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ihj.2018.11.016.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.van de Hoef T.P., Petraco R., van Lavieren M.A. Basal stenosis resistance index derived from simultaneous pressure and flow velocity measurements. Euro Interv. 2016;12(2):e199–e207. doi: 10.4244/EIJV12I2A33. [DOI] [PubMed] [Google Scholar]
- 2.De Bruyne B., Pijls N.H., Kalesan B., FAME 2 Trial Investigators Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367(11):991–1001. doi: 10.1056/NEJMoa1205361. [DOI] [PubMed] [Google Scholar]
- 3.Warisawa T., Cook C.M., Akashi Y.J., Davies J.E. Past, present and future of coronary physiology. Rev Esp Cardiol (Engl Ed). 2018 Mar 15 doi: 10.1016/j.rec.2018.02.003. pii: S1885-5857(18)30037-30039. [DOI] [PubMed] [Google Scholar]
- 4.Park J.J., Petraco R., Nam C.W. Clinical validation of the resting pressure parameters in the assessment of functionally significant coronary stenosis; results of an independent, blinded comparison with fractional flow reserve. Int J Cardiol. 2013;168(4):4070–4075. doi: 10.1016/j.ijcard.2013.07.030. [DOI] [PubMed] [Google Scholar]
- 5.Sen S., Asrress K.N., Nijjer S. Diagnostic classification of the instantaneous wave-free ratio is equivalent to fractional flow reserve and is not improved with adenosine administration. Results of CLARIFY (Classification Accuracy of Pressure-Only Ratios against Indices Using Flow Study) J Am Coll Cardiol. 2013;61(13):1409–1420. doi: 10.1016/j.jacc.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 6.Petraco R., van de Hoef T.P., Nijjer S. Baseline instantaneous wave-free ratio as a pressure-only estimation of underlying coronary flow reserve: results of the JUSTIFY-CFR study (joined coronary pressure and flow analysis to determine diagnostic characteristics of basal and hyperemic indices of functional lesion severity-coronary flow reserve) Circ Cardiovasc Interv. 2014;7(4):492–502. doi: 10.1161/CIRCINTERVENTIONS.113.000926. [DOI] [PubMed] [Google Scholar]
- 7.Sen S., Escaned J., Malik I.S. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol. 2012;59(15):1392–1402. doi: 10.1016/j.jacc.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Jeremias A., Maehara A., Généreux P. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: the RESOLVE Study. J Am Coll Cardiol. 2014;63:1253–1261. doi: 10.1016/j.jacc.2013.09.060. [DOI] [PubMed] [Google Scholar]
- 9.Escaned J., Echavarría-Pinto M., Garcia-Garcia H.M., ADVISE II Study Group Prospective assessment of the diagnostic accuracy of instantaneous wave-free ratio to assess coronary stenosis relevance: results of ADVISE II international, multicenter study (adenosine vasodilator independent stenosis evaluation II) JACC Cardiovasc Interv. 2015;8(6):824–833. doi: 10.1016/j.jcin.2015.01.029. [DOI] [PubMed] [Google Scholar]
- 10.De Rosa S.D., Polimeni A., Petraco R., Davies J.E., Indolfi C. Diagnostic performance of the instantaneous wave-free ratio comparison with fractional flow reserve. Circ Cardiovasc Interv. 2018;11:e004613. doi: 10.1161/CIRCINTERVENTIONS.116.004613. [DOI] [PubMed] [Google Scholar]
- 11.Götberg M., Christiansen E.H., Gudmundsdottir I.J., iFR-SWEDEHEART Investigators Instantaneous wave-free ratio versus fractional flow reserve to guide PCI. N Engl J Med. 2017;376:1813–1823. doi: 10.1056/NEJMoa1616540. [DOI] [PubMed] [Google Scholar]
- 12.Davies J.E., Sen S., Dehbi H.M. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N Engl J Med. 2017;376:1824–1834. doi: 10.1056/NEJMoa1700445. [DOI] [PubMed] [Google Scholar]
- 13.Mamas M.A., Horner S., Welch E. Resting Pd/Pa measured with intracoronary pressure wire strongly predicts fractional flow reserve. J Invasive Cardiol. 2010;22:260–265. [PubMed] [Google Scholar]
- 14.Johnson N.P., Jeremias A., Zimmermann F.M. Continuum of vasodilator stress from rest to contrast medium to adenosine hyperemia for fractional flow reserve assessment. JACC Cardiovasc Interv. 2016;9(8):757–767. doi: 10.1016/j.jcin.2015.12.273. [DOI] [PubMed] [Google Scholar]
- 15.Leone A.M., Pepe F.L., Arioti M., Crea F. Contrast Fractional Flow Reserve (cFFR): a pragmatic response to the call for simplification of invasive functional assessment. Int J Cardiol. 2018;268:45–50. doi: 10.1016/j.ijcard.2018.04.048. [DOI] [PubMed] [Google Scholar]
- 16.Leone A.M., Scalone G., De Maria G.L. Efficacy of contrast medium-induced Pd/Pa ratio in predicting functional significance of intermediate coronary artery stenosis assessed by fractional flow reserve: insights from the RINASCI study. Euro Intervent. 2015;11(4):421–427. doi: 10.4244/EIJY14M07_02. [DOI] [PubMed] [Google Scholar]
- 17.Van Wyk P., Puri A., Blake J. The utility of contrast medium fractional flow reserve in functional assessment of coronary disease in daily practice. Heart Lung Circ. 2018;27(2):212–218. doi: 10.1016/j.hlc.2017.03.158. [DOI] [PubMed] [Google Scholar]
- 18.Indolfi C., Mongiardo A., Spaccarotella C. The instantaneous wave-free ratio (iFR) for evaluation of non-culprit lesions in patients with acute coronary syndrome and multivessel disease. Int J Cardiol. 2015;178:46–54. doi: 10.1016/j.ijcard.2014.03.210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.