Abstract
A Dieulafoy's lesion is defined as a dilated submucosal vessel that erodes the overlying epithelium without evidence of a primary ulcer or erosion. It is a rare cause of gastrointestinal bleeding that is difficult to identify and subsequently manage. Most commonly, they occur in the upper gastrointestinal tract, namely the stomach. A Dieulafoy's lesion of the rectum, however, is an exceedingly rare presentation that can lead to life-threatening gastrointestinal bleeding. Our case consists of an 84-year-old man, who presented with lower gastrointestinal bleeding secondary to a Dieulafoy's lesion of the rectum.
Key Words: Dieulafoy's lesion, Gastrointestinal hemorrhage, Endoscopy, Hemostasis
Introduction
First described by Gallard in 1884, Dieulafoy's lesions are a rare cause of gastrointestinal (GI) bleeding [1]. They are believed to account for an estimated 1–2% of all cases of acute GI bleeding and carry an estimated mortality rate of 80% [2]. Risk factors associated with their development include advanced age and male gender [3], both of which were present in our patient. With regards to location, Dieulafoy's lesions are most commonly encountered in the stomach (70%) and the esophagus (15%). Of these, many are found on the lesser curvature of the stomach within 6 cm of the gastroesophageal junction. Dieulafoy's lesions of the rectum, however, are a rare entity, observed in a mere 2% of reported cases in the literature [4, 5]. Dieulafoy's lesions of the gallbladder have also been reported, but are outside the scope of this discussion [6].
Case Presentation
The patient is an 84-year-old male with a medical history of hypertension, previous cerebrovascular accident, and end-stage renal disease (on hemodialysis) who presented to our institution's emergency department complaining of shortness of breath and fatigue after missing a session of hemodialysis 2 days prior. On presentation, the patient's respiratory status quickly deteriorated requiring endotracheal intubation. Vital signs were remarkable for a blood pressure of 130/60 mm Hg, a heart rate of 97 beats per minute, and a respiratory rate of 14 breaths per minute. Notable laboratory findings in the emergency department included a hemoglobin 12.1 g/dL, a white blood cell count of 8.3 × 103/μL, platelet count 394 × 103/μL, sodium 142 mEq/L, potassium 7.6 mEq/L, creatinine 33.7 mg/dL, blood urea nitrogen 206 mg/dL, Lactic acid 5 mmol/L, and an elevated troponin level of 1.2 ng/L. Following these findings, the patient was admitted to the intensive care unit under the impression of acute hypoxic respiratory failure and acute encephalopathy secondary to uremia. On arrival to the intensive care unit, an electrocardiogram showed atrial flutter at a rate of 162 beats per minute that resolved with the administration of intravenous diltiazem. Cardiology was consulted regarding the patient's elevated troponin level and the impression was demand ischemia. The patient's troponin then returned to normal levels and repeat electrocardiogram was unremarkable. Shortly after admission, the patient's hyperkalemia and lactic acidosis both resolved after hemodialysis. While this aspect improved, the patient's course was complicated by fevers and multiple episodes of hematochezia resulting in a swift drop in his hemoglobin to 6.6 g/dL. In addition, the patient was unable to be weaned off of the ventilator and required the creation of a tracheostomy. Resuscitation was begun with 1 packed red blood cell transfusion and antibiotics were started due to blood cultures yielding methicillin-sensitive Staphylococcus aureus. Repeat blood cultures were later negative, but the patient's hemoglobin failed to respond to multiple transfusions. The gastroenterology service was consulted for a possible colonoscopy, but the patient's health care proxy refused. Because no intervention took place, the patient's hemodynamic status continued to deteriorate requiring a total of 21 packed red blood cell transfusions. After further consideration, and 1 week of continued hematochezia, the health care proxy then agreed to a colonoscopy. Colonoscopy was swiftly done (online suppl. Video 1; see www.karger.com/doi/10.1159/000497139) and revealed an actively spurting Dieulafoy's lesion in the distal rectum just proximal to the pectinate line associated with underlying friable mucosa (Fig. 1). Hemostasis was achieved with 3 hemostatic clips and injection of 3 mL of 1: 1,000 epinephrine (Fig. 2). Subsequently, the patient remained stable, required no further transfusions, and was discharged to an assisted nursing facility.
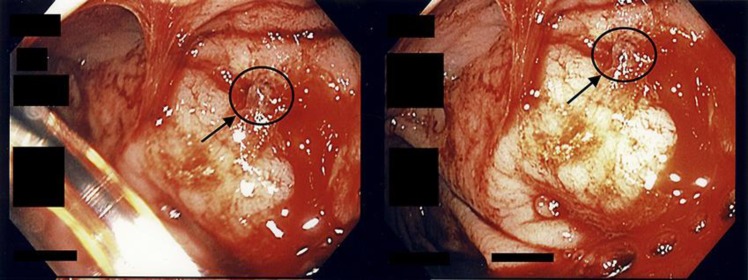
Fig. 1.
An actively bleeding Dieulafoy's lesion in the distal rectum, just proximal to the pectinate line.
Fig. 2.
Hemostasis achieved with 3 hemostatic clips.
Discussion
Dieulafoy's lesions are a rare but important cause of GI bleeding due to the severity of bleeding it induces if left untreated. The lesion is characterized by a dilated, large-calibered submucosal artery or arteriole typically scouring the overlying GI mucosa and submucosal tissue without any predisposing ulcer, aneurysm, or intrinsic mural abnormality [1]. Dieulafoy's lesions are usually reported in the stomach [2], especially in and around the lesser curvature, which can be attributed to the rich blood supply found in this area [7]. This makes our case exceedingly rare, where a Dieulafoy's lesion was identified in the rectum just proximal to the pectinate line. Dieulafoy's lesions can be asymptomatic; however, lesions with acute, profound bleeding require medical attention. Most patients with gastric lesions present with hematemesis or melena, whereas colonic and rectal lesions are characterized by bright red bleeding per rectum [8]. Transfusion-dependent severe anemia and hemodynamic instability can occur rapidly and are attributed to the arterial nature of the vessel. In a case series involving 20 patients with Dieulafoy's lesions, about 50% presented to the hospital with hemodynamic instability as the presenting symptom [8]. Occult GI bleeding and chronic anemia are very rarely associated with these lesions [9].
Esophagogastroduodenoscopy is the preferred test during any massive upper or lower GI bleed, not only as a diagnostic tool but also as a therapeutic intervention. Recent advances in endoscopy and the low threshold physicians carry to perform it have led to increased detection of Dieulafoy's lesions [2]. Dieulafoy's lesions should be distinguished from other lesions with similar endoscopic appearance and clinical presentation. These include arteriovenous malformations, telangiectasias, vascular polyps, and neoplasms [9]. Good history gathering and the rapid development of GI hemorrhage, manifested by hemodynamic instability, are clues that can help the clinician suspect Dieulafoy's lesions as the culprit.
Endoscopic therapies like hypertonic saline-epinephrine injection, sclerotherapy, band ligation, thermal cautery, and hemoclip application have been described in various studies and show a high success rate [10, 11, 12]. One study consisting of 44 patients with Dieulafoy's lesions showed a treatment success rate of 88.6% during the initial endoscopy [13]. Another study echoed these findings showing a success rate of 95% in 27 patients diagnosed with Dieulafoy's lesions [10]. Rebleeding, although rare, can be a major life-threatening bleeding episode and high vigilance is recommended. Concomitant NSAID or anticoagulant use and Forrest classification of bleeding are the predictors of rebleeding in patients that achieved primary hemostasis [13]. In patients who fail to achieve primary hemostasis with endoscopic interventions or those who experience rebleeding, other therapeutic modalities like transarterial embolization or surgery should be considered [13, 14]. Selective angiography is preferred in patients that failed endoscopic therapy, for lesions beyond the reach of therapeutic endoscopy, or in patients who are poor candidates for surgery [2]. In past years, surgical resection was the mainstay of treatment, particularly in cases of colonic Dieulafoy's lesions with massive GI hemorrhage [15]. In conclusion, Dieulafoy's lesions are an important cause of GI bleeding. They most commonly present in the stomach and esophagus, but can rarely present in the rectum resulting in life-threatening hemorrhage. Despite their rarity, Dieulafoy's lesions should be considered as part of the differential diagnosis in cases of lower GI bleeding given the mortality that is invariably associated with them. Once identified through endoscopy or colonoscopy, they can be successfully treated with epinephrine injection, sclerotherapy, band ligation, thermal cautery, or hemostatic clips.
Statement of Ethics
This case report was approved by the institute's Institutional Review Board as per its policy.
Disclosure Statement
None of the authors have any financial conflicts of interest.
Author Contributions
E.O.T., R.B., and A.O.: involved in conception and design; E.O.T., R.B., A.O., and P.R.: drafted the article; A.C. and V.G.: critically revised the article for important intellectual content; E.O.T., R.B., A.O., P.R., A.C., and V.G.: involved in final approval of the article.
Supplementary Material
Supplementary data
Acknowledgements
This case report was presented in the form of an abstract (poster) at the American College of Gastroenterology conference in Philadelphia, PA, USA (October 2018).
References
- 1.Lee YT, Walmsley RS, Leong RW, Sung JJ. Dieulafoy's lesion. Gastrointest Endosc. 2003 Aug;58((2)):236–43. doi: 10.1067/mge.2003.328. [DOI] [PubMed] [Google Scholar]
- 2.Baxter M, Aly EH. Dieulafoy's lesion: current trends in diagnosis and management. Ann R Coll Surg Engl. 2010 Oct;92((7)):548–54. doi: 10.1308/003588410X12699663905311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stark ME, Gostout CJ, Balm RK. Clinical features and endoscopic management of Dieulafoy's disease. Gastrointest Endosc. 1992 Sep-Oct;38((5)):545–50. doi: 10.1016/s0016-5107(92)70513-6. [DOI] [PubMed] [Google Scholar]
- 4.Dogan U, Gomceli I, Koc U, Habibi M, Bulbuller N. Rectal dieulafoy lesions: a rare etiology of chronic lower gastrointestinal bleeding. Case Rep Med. 2014;2014:180230. doi: 10.1155/2014/180230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gauci J, Galea S, Galea J, Schembri M. Extragastric Dieulafoy's lesion. BMJ Case Rep. 2014 Sep;2014(sep12 1):bcr2014204627. doi: 10.1136/bcr-2014-204627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu JM, Zaitoun AM. A galling disease? Dieulafoy's lesion of the gallbladder. Int J Surg Case Rep. 2018;44:62–5. doi: 10.1016/j.ijscr.2018.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barlow TE, Bentley FH, Walder DN. Arteries, veins, and arteriovenous anastomoses in the human stomach. Surg Gynecol Obstet. 1951 Dec;93((6)):657–71. [PubMed] [Google Scholar]
- 8.López-Arce G, Zepeda-Gómez S, Chávez-Tapia NC, García-Osogobio S, Franco-Guzmán AM, Ramírez-Luna MA, et al. Upper gastrointestinal dieulafoy's lesions and endoscopie treatment: first report from a mexican centre. Therap Adv Gastroenterol. 2008 Sep;1((2)):97–101. doi: 10.1177/1756283X08096285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nojkov B, Cappell MS. Gastrointestinal bleeding from Dieulafoy's lesion: clinical presentation, endoscopic findings, and endoscopic therapy. World J Gastrointest Endosc. 2015 Apr;7((4)):295–307. doi: 10.4253/wjge.v7.i4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baettig B, Haecki W, Lammer F, Jost R. Dieulafoy's disease: endoscopic treatment and follow up. Gut. 1993 Oct;34((10)):1418–21. doi: 10.1136/gut.34.10.1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skok P. Endoscopic hemostasis in exulceratio simplex-Dieulafoy's disease hemorrhage: a review of 25 cases. Endoscopy. 1998 Sep;30((7)):590–4. doi: 10.1055/s-2007-1001361. [DOI] [PubMed] [Google Scholar]
- 12.Laine L. Multipolar electrocoagulation in the treatment of active upper gastrointestinal tract hemorrhage. A prospective controlled trial. N Engl J Med. 1987 Jun;316((26)):1613–7. doi: 10.1056/NEJM198706253162601. [DOI] [PubMed] [Google Scholar]
- 13.Lim W, Kim TO, Park SB, Rhee HR, Park JH, Bae JH, et al. Endoscopic treatment of dieulafoy lesions and risk factors for rebleeding. Korean J Intern Med (Korean Assoc Intern Med) 2009 Dec;24((4)):318–22. doi: 10.3904/kjim.2009.24.4.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guy RJ, Ang ES, Tan KC, Tsang CB. Massive bleeding from a Dieulafoy-like lesion of the rectum in a burns patient. Burns. 2001 Nov;27((7)):767–9. doi: 10.1016/s0305-4179(01)00031-6. [DOI] [PubMed] [Google Scholar]
- 15.Ma C, Hundal R, Cheng EJ. Colonic Dieulafoy's Lesion: A Rare Cause of Lower Gastrointestinal Hemorrhage and Review of Endoscopic Management. Case Rep Gastrointest Med. 2014;2014:436293. doi: 10.1155/2014/436293. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data