Abstract
We present the case of a 50-year-old patient with folliculotropic mycosis fungoides (FMF) unresponsive to retinoids and the chemotherapeutic regimens CHOP, gemcitabine, and brentuximab-vedotin. During immunosuppressive therapy, the patient developed extensive progressive molluscum contagiosum. The mollusca did not respond to topical imiquimod but showed a swift complete response to interferon-alpha 2a (IFNa). Recently, the patient started with alemtuzumab as induction therapy for an allogenic stem cell transplantation and simultaneously continued IFNa therapy.
Key Words: Molluscum contagiosum, Interferon alpha, Folliculotropic, Mycosis fungoides
Introduction
Molluscum contagiosum is an infectious auto-inoculable cutaneous disease, caused by a double-stranded DNA poxvirus. The course of the disease is most often self-limiting and occurs regularly during childhood. Due to the benign self-limiting disease course and the possible side effects of therapies (i.e., scarring, hyperpigmentation), treatment is not recommended in immunocompetent patients [1]. The management of the disease performed by dermatologists and primary care physicians is primarily focused on relieving symptoms (like pruritus and pain) and preventing comorbidities (like secondary infections and Gianotti-Crosti syndrome). However, in immunocompromised patients, molluscum contagiosum is notoriously persistent and difficult to treat. Small case series describe an effect of topical imiquimod in those patients, but results are disappointing [2]. Few case series suggest interferon-alpha 2a (IFNa) as an effective treatment option [3, 4, 5].
Folliculotropic mycosis fungoides (FMF) is a primary cutaneous T-cell lymphoma. In general, the prognosis is favorable; however, it deteriorates in more advanced stages [6]. Due to immunosuppressive therapies, patients are more prone to opportunistic infections, including molluscum contagiosum [7]. Nevertheless, FMF without extracutaneous involvement can also be treated with IFNa, a biological response modifier which inhibits tumor proliferation [8]. In this report, we describe a patient with advanced-stage FMF, who developed multiple large molluscum contagiosum lesions in the head and neck area.
Case Report
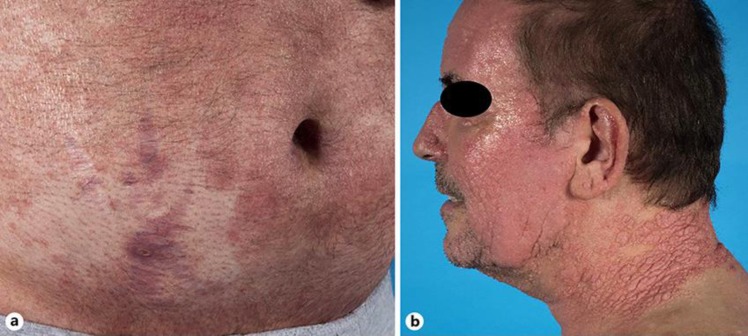
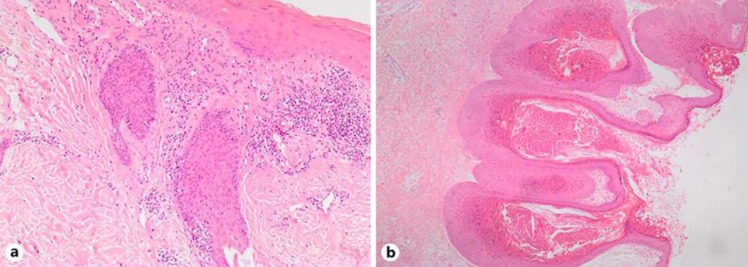
A 50-year-old man with a history of FMF resistant to CHOP treatment (cyclophosphamide, doxorubicin, vincristine, and prednisolone) was seen at the outpatient clinic of the dermatology department. He presented with extensive patches and plaques on the trunk and extremities (Fig. 1a) and itchy, more infiltrated plaques in the head and neck area (Fig. 1b). Histologic examination of a patch on the abdomen showed FMF (Fig. 2a), while skin biopsies of the infiltrated plaques in the head and neck area showed a histology compatible with molluscum contagiosum (Fig. 2b). Staging procedures, including complete blood count, biochemical analysis, PET-CT scan, and bone marrow examination, showed lymphadenopathy and blood involvement (leukocytes: 7.78 × 109/L, atypical lymphocytes: 2.64 × 109/L, CD3+CD4+: 2.45 × 109/L, CD4/CD8 ratio: 20.56). At the time he was treated with retinoids 150 mg/day without effect on skin lesions or blood involvement. In cooperation with the hematology department, mono-chemotherapy with gemcitabine was initiated as induction treatment before the intended consolidation with an allogeneic stem cell transplantation. Due to an insufficient response, therapy was switched to brentuximab-vedotin as next induction therapy. During these treatment regimens, the molluscum contagiosum lesions progressed and expanded. Topical imiquimod therapy showed no effect on the mollusca and the patient responded insufficiently to brentuximab. Subsequently, the allogenic stem cell transplantation course was postponed until further notice and IFNa was administered (3 million units 3 times a week). Within 1 month, all molluscum contagiosum lesions had disappeared completely (Fig. 3). The molluscum remained in complete remission for 2 months. However, the patient reported progressive FMF with pruritus, erythroderma, and increasing blood involvement (leukocytes: 18.69 × 109/L, atypical lymphocytes: 13.59 × 109/L, CD3+CD4+: 12.92 × 109/L, CD4/CD8 ratio: 323.11). As next line of induction therapy, alemtuzumab was started simultaneously to IFNa, demonstrating a significant drop in lymphocyte counts and decrease of pruritus and erythroderma. Subsequent response evaluation will guide whether to proceed with an allogeneic stem cell transplantation or not.
Fig. 1.
Clinical images of the patient. a Alopecia and generalized erythematosquamous patches on the trunk. b Tumorous lesions on the neck and face.
Fig. 2.
Histopathologic images. a HE stain 100×, folliculotropic mycosis fungoides: atypical lymphocytes infiltrating the epithelial layer of the hair follicle. b HE stain 100×, molluscum contagiosum: central umbilication and epidermal hyperplasia. The keratinocytes contain a large intracytoplasmic inclusion compressing the nucleus.
Fig. 3.
Clinical images. a Before therapy with IFNa. b During therapy. c After 2 months of therapy.
Discussion/Conclusion
The current case demonstrates that IFNa is an effective treatment option in molluscum contagiosum. Molluscum contagiosum is notoriously persistent and difficult to treat in immunocompromised patients. Only few case series evaluated treatment options in molluscum contagiosum [1, 2, 3, 4, 5, 9]. Conventional treatments such as salicylic acid, retinoids, cryotherapy, imiquimod, and curettage often show insufficient effect, especially in case of generalized lesions. Few case reports evaluated the effect of IFNa in molluscum contagiosum. IFNa acts in an immunomodulatory manner and induces production of effector proteins in cells, which inhibit viral replication. Böhm et al. [3] described a 31-year-old immunocompromised female patient with skin lesions on her arms and trunk. After 16 months of treatment with IFNa (50 μg/week subcutaneously) a complete response was achieved [3]. Hourihane et al. [4] reported a sister (6 years) and brother (8 years) with a combined immunodeficiency who developed extensive molluscum contagiosum. They were both treated with IFNa (3 million units 3 times a week subcutaneously) and achieved approximately 95% clearance of the skin lesions [4]. Kilic and Kilicbay [5] reported a case of widely disseminated molluscum contagiosum in an immunocompromised 9-year-old boy. The patient was treated successfully with IFNa (3 million units 3 times a week subcutaneously for 6 months) [5]. In the current case, treatment with IFNa was started to achieve a combined effect on FMF and molluscum contagiosum. Although the FMF responded insufficiently, the patient was free from molluscum contagiosum. The current case showed that IFNa (3 million units 3 times a week subcutaneously) can be an effective treatment, is safe together with alemtuzumab, and should be considered in refractory molluscum contagiosum.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to declare.
Author Contributions
All authors were closely involved in the diagnostic and therapeutic phase of the disease of the patient and contributed equally to the formation of this article.
References
- 1.Forbat E, Al-Niaimi F, Ali FR. Molluscum Contagiosum: Review and Update on Management. Pediatr Dermatol. 2017 Sep;34((5)):504–15. doi: 10.1111/pde.13228. [DOI] [PubMed] [Google Scholar]
- 2.DiBiagio JR, Pyle T, Green JJ. Reviewing the use of imiquimod for molluscum contagiosum. Dermatol Online J. 2018 Aug;24((6)):13030/qt3b4606qt. [PubMed] [Google Scholar]
- 3.Böhm M, Luger TA, Bonsmann G. Disseminated giant molluscum contagiosum in a patient with idiopathic CD4+ lymphocytopenia. Successful eradication with systemic interferon. Dermatology. 2008;217((3)):196–8. doi: 10.1159/000141649. [DOI] [PubMed] [Google Scholar]
- 4.Hourihane J, Hodges E, Smith J, Keefe M, Jones A, Connett G. Interferon alpha treatment of molluscum contagiosum in immunodeficiency. Arch Dis Child. 1999 Jan;80((1)):77–9. doi: 10.1136/adc.80.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kilic SS, Kilicbay F. Interferon-alpha treatment of molluscum contagiosum in a patient with hyperimmunoglobulin E syndrome. Pediatrics. 2006 Jun;117((6)):e1253–5. doi: 10.1542/peds.2005-2706. [DOI] [PubMed] [Google Scholar]
- 6.van Santen S, Roach RE, van Doorn R, Horváth B, Bruijn MS, Sanders CJ, et al. Clinical Staging and Prognostic Factors in Folliculotropic Mycosis Fungoides. JAMA Dermatol. 2016 Sep;152((9)):992–1000. doi: 10.1001/jamadermatol.2016.1597. [DOI] [PubMed] [Google Scholar]
- 7.Lebas E, Arrese JE, Nikkels AF. Risk Factors for Skin Infections in Mycosis Fungoides. Dermatology. 2016;232((6)):731–7. doi: 10.1159/000455944. [DOI] [PubMed] [Google Scholar]
- 8.Olsen EA, Bunn PA. Interferon in the treatment of cutaneous T-cell lymphoma. Hematol Oncol Clin North Am. 1995 Oct;9((5)):1089–107. [PubMed] [Google Scholar]
- 9.Nguyen HP, Franz E, Stiegel KR, Hsu S, Tyring SK. Treatment of molluscum contagiosum in adult, pediatric, and immunodeficient populations. J Cutan Med Surg. 2014 Oct;18((5)):299–306. doi: 10.2310/7750.2013.13133. [DOI] [PubMed] [Google Scholar]