Abstract
The Affordable Care Act (ACA) aims to expand health insurance coverage and minimize financial barriers to receiving health care services for individuals. However, little is known about how the ACA has impacted individuals with mental health conditions. This study finds that the implementation of the ACA is associated with an increase in rate of health insurance coverage among nonelderly adults with serious psychological distress (SPD) and a reduction in delaying and forgoing necessary care. The ACA also reduced the odds of an individual with SPD not being able to afford mental health care. Mental health care access among racial and ethnic minority populations and people with low income has improved during 2014–2016, but gaps remain.
Keywords: Access to care, Mental health, Serious psychological distress, Affordable Care Act
Introduction
Since the enactment of the Affordable Care Act (ACA) in 2010 and its implementation in 2014, an estimated net of 17 to 20 million individuals between the ages of 18–64 have gained health insurance coverage in the United States (Carman et al. 2015; Avery et al. 2015). This increase in insurance coverage is due to various provisions of the ACA, such as the expansions in coverage through Medicaid, the health insurance exchanges, and the young adult mandate that allowed individuals between the ages of 19–26 to stay on their parent’s employer-sponsored health insurance (Majerol et al. 2016). Recent studies have demonstrated that the implementation of the ACA is associated with significant improvement in access to primary care, medications, and health outcomes (Chen et al. 2016; Cutler 2015; Sommers et al. 2015).
In estimating the impact of this increased health insurance coverage, a population of interest is those with a mental health condition. Approximately 1 out of 5 uninsured individuals in the U.S. has a mental health condition (Ali et al. 2016a), and these individuals are at a higher risk for poor health outcomes and having reduced access to care (Cohen and Zammitti 2016). Recent research has shown that ACA’s Medicaid expansion provision might have led to an increase in treatment utilization among those with a mental health condition (Creedon and Le Cook 2016), however, limited research exists that has estimated the impact of the implementation of the ACA (i.e., the impact of both the Medicaid expansion, health insurance exchanges, and increased employer sponsored coverage) on this population.
As a population, people with mental health conditions are at greater risk than those without mental health conditions for inadequate care for several reasons. First, the prevalence of mental health conditions is higher among low-income individuals. So being uninsured or poorly insured for this population may mean not being able to access the necessary treatment because of cost (Han et al. 2015). Second, the medical infrastructure to care for mental health conditions is more fragmented than for other medical conditions because of lower reimbursement rates (Mark et al. 2017) and decades of falling state funding for mental health facilities (Croft and Parish 2013). The siloed health care system may place the burden of care coordination activities on the shoulders of those least able to perform self-management tasks. Therefore, it is important to examine how the implementation of the ACA may affect health insurance coverage and barriers to health care access among adults with mental health conditions.
In this study we examine the impact of the implementation (Medicaid expansion, implementation of the health insurance exchanges, and employer mandated coverage in 2015 for employers with ≥ 100 lives) of the ACA on rate of health insurance coverage and reported barriers to health care access among individuals with serious psychological distress (SPD), an indicator of mental health problems severe enough to cause moderate-to-serious impairment in social, occupational, or school functioning, and to require treatment (Cohen and Zammitti 2016). We also examine whether the ACA has had a more pronounced effect on minorities with SPD; and low-income people with SPD. Although studies of Massachusetts health care reform and the Oregon Medicaid lottery experiment showed significant increases in health insurance coverage and services utilization with insurance expansion (Long et al. 2012; Baicker and Finkelstein 2011), to our knowledge, no studies have investigated the impact of the full implementation of ACA among individuals with SPD.
Methods
Data
This study uses data from the 2011–2016 National Health Interview Survey (NHIS), which is a cross sectional nationally representative survey of the noninstitutionalized, civilian U.S. population collected by the National Center for Health Statistics (NCHS) of the Centers for Disease Control. Of the sample selected for participation, 80% of households successfully participate in the survey. This survey contains detailed information on participants’ health care utilization and access during each year of participation, and respondents provide demographic, socioeconomic, and health-related characteristics, including Kessler 6 (K6) scores (Kessler et al. 2002), which are standardized scores for psychological functioning (all Kessler 6 questions used are available at https://www.cdc.gov/nchs/nhis/). Race and ethnicity are collected for all respondents; the CDC/NCHS employs multiple imputation for income variables to increase usability of NHIS data. Details on the data imputation method are provided on their website (Centers for Disease Control/National Center for Health Statistics 2015).
This study focuses on individuals’ ages 18–64 years of age, who had SPD. Individuals were considered to have severe psychological distress (SPD) if they had a K6 composite score of 13 or greater. There were a total of 6,052 individuals ages 18–64 who met the definition of severe psychological distress, as indicated by a K6 score ≥ 13. The range of scores in the total survey population was from 0 to 24 (Prochaska et al. 2012). The Kessler 6 screener has been used extensively in the literature and has been demonstrated to be clinically valid, accurate and reliable (Prochaska et al. 2012). The Kessler-6 has 6 screening questions that use a Likert scale to query respondents on feelings such as hopelessness, depression, or anxiety in the previous 30 days, by asking questions such as “During the last 30 days, about how often did you feel so nervous that nothing could calm you down?”. If a respondent reports rarely or never having felt the negative emotions ascertained in the survey, s/he would have a score of 0.
Conceptual Model and Control Variables
Our outcome variables include four measures that have been used in the literature (Carman et al. 2015; Wherry and Miller 2016). These include being uninsured, having any delayed necessary medical care, having any forgone medical care, and whether the respondents stated they could not afford mental health care or counseling in the past 12 months. We use the Andersen behavioral model of health care utilization to guide the selection of covariates (Andersen and Newman 1973; Andersen 1995).The covariates we include can be categorized across predisposing, enabling, and need factors.
The predisposing factors include race and ethnicity (i.e., non-Latino White (White), non-Latino African American (African American), Latino, and “other”); immigration status (i.e., U.S. born citizens and naturalized U.S. citizens; and non-U.S. citizens). Citizenship is relevant because under current U.S. law, Lawful Permanent Residents cannot receive Medicaid coverage in their first 5 years of legal residency in the United States, whereas Lawful Permanent Residents who have permanently resided in the U.S. for 5 years and filed tax returns may qualify for Medicaid coverage; undocumented immigrants and non-permanent resident visa holders are not eligible for Medicaid. Additional predisposing factors in the Andersen model include sex, and marital status (i.e., married or not). The Andersen Model enabling factors encompass family income (i.e., less than 100% of the Federal Poverty Level (FPL), 100–200% FPL, and more than 200% FPL), education (i.e., less than high school degree, high school degree, college degree, and advanced degree), interview language (i.e., Spanish, English, and other), and U.S. Census region (i.e., Northeast, Midwest, South, and West). Within the Andersen model, race and ethnicity are considered “predisposing” factors because they are rough approximates for lived experiences, such as access to resources, discrimination, and cultural paradigms that influence the interpretation of physical symptoms. We limit our analysis to the mutually exclusive categories of White, African America, Latino, and “other” in order to ensure adequate sub-sets of the population for statistical inference. There were not adequate sample numbers to produce reliable estimates for the Asian-Amer-ican, Native-American, and mixed-non Latino respondents with SPD in individual sub-categories; for this reason, we have combined these respondents and include them in an “other” category. While NCHS oversamples African American, Latino, Asian-American, Native-American, and mixed race individuals, the prevalence of SPD in the general population was between 3 and 5% in any calendar year, resulting in small specific sub-categories for Asian-Americans, Native Americans, and mixed race individuals. Our research question focuses on the effects of the ACA on White, African American, Latino, and “other” populations with SPD; and so the omission of specific sub-populations is not a limitation in relation to our study aim.
Personal need factors within the Andersen model are selfreported physical health (i.e., excellent, very good, good, fair, and poor), and any self-reported functional limitations. These Andersen Model domains and variables have been widely used to guide the examination of health care access and utilization (Cook et al. 2016; Chen et al. 2015, 2016; Bustamante et al. 2009). Descriptive statistics on the study sample and the variables used in the analysis are provided in Table 1.
Table 1.
Population characteristics of adults with serious psychological distress by barriers to health care access
| Being uninsured | Delaying any necessary care |
Forgoing any care | Could not afford mental health care |
|||||
|---|---|---|---|---|---|---|---|---|
| 2014—2016 Mean |
2011–2013 Mean |
2014–2016 Mean |
2011–2013 Mean |
2014–2016 Mean |
2011–2013 Mean |
2014–2016 Mean |
2011–2013 Mean |
|
| Race and ethnicity | ||||||||
| White | 0.60 | 0.60 | 0.69 | 0.68 | 0.67 | 0.63 | 0.72 | 0.69 |
| African-American | 0.14 | 0.15 | 0.12 | 0.12 | 0.15 | 0.16 | 0.10 | 0.13 |
| Latino | 0.20 | 0.18 | 0.12 | 0.12 | 0.12 | 0.14 | 0.12 | 0.12 |
| Other | 0.06 | 0.07 | 0.07 | 0.07 | 0.06 | 0.07 | 0.06 | 0.05 |
| Age | ||||||||
| 18–24 | 0.08 | 0.09 | 0.09 | 0.06* | 0.08 | 0.07 | 0.10 | 0.08 |
| 25–34 | 0.26 | 0.21 | 0.15 | 0.16 | 0.14 | 0.17 | 0.19 | 0.20 |
| 35–44 | 0.22 | 0.24 | 0.19 | 0.19 | 0.20 | 0.20 | 0.22 | 0.21 |
| 45–54 | 0.28 | 0.27 | 0.31 | 0.31 | 0.31 | 0.30 | 0.28 | 0.30 |
| 55–64 | 0.16 | 0.19 | 0.25 | 0.29 | 0.27 | 0.27 | 0.21 | 0.21 |
| Gender | ||||||||
| Female | 0.59 | 0.58 | 0.61 | 0.60 | 0.62 | 0.59 | 0.65 | 0.63 |
| Marital status | ||||||||
| Married | 0.30 | 0.28 | 0.26 | 0.25 | 0.26 | 0.24 | 0.26 | 0.28 |
| US citizenship | ||||||||
| US citizen | 0.87 | 0.89 | 0.95 | 0.94 | 0.95 | 0.94 | 0.96 | 0.96 |
| Non-US citizen | 0.13 | 0.11 | 0.05 | 0.06 | 0.05 | 0.06 | 0.04 | 0.04 |
| Family income | ||||||||
| Below 100% federal poverty line (FPL) | 0.43 | 0.49 | 0.40 | 0.43 | 0.42 | 0.48* | 0.41 | 0.47 |
| 100–200% FPL | 0.32 | 0.31 | 0.31 | 0.32 | 0.31 | 0.31 | 0.28 | 0.28 |
| Above 200% FPL | 0.25 | 0.21 | 0.29 | 0.25 | 0.27 | 0.21* | 0.31 | 0.24* |
| Education | ||||||||
| Less than high school | 0.27 | 0.25 | 0.21 | 0.22 | 0.22 | 0.24 | 0.20 | 0.21 |
| High school | 0.34 | 0.32 | 0.27 | 0.30 | 0.27 | 0.30 | 0.25 | 0.32* |
| Some college education | 0.19 | 0.22 | 0.25 | 0.24 | 0.26 | 0.24 | 0.26 | 0.25 |
| College degree | 0.17 | 0.18 | 0.23 | 0.21 | 0.21 | 0.19 | 0.24 | 0.18 |
| College degree and higher | 0.02 | 0.03 | 0.04 | 0.04 | 0.04 | 0.03 | 0.05 | 0.04 |
| Interviewed language | ||||||||
| English | 0.91 | 0.93 | 0.97 | 0.97 | 0.97 | 0.96 | 0.98 | 0.97 |
| Self-reported health status | ||||||||
| Excellent | 0.10 | 0.06* | 0.04 | 0.04 | 0.04 | 0.04 | 0.06 | 0.04 |
| Very good | 0.16 | 0.15 | 0.13 | 0.12 | 0.11 | 0.11 | 0.15 | 0.13 |
| Good | 0.26 | 0.32 | 0.25 | 0.27 | 0.23 | 0.26 | 0.21 | 0.26 |
| Fair | 0.33 | 0.30 | 0.35 | 0.32 | 0.38 | 0.33 | 0.33 | 0.33 |
| Poor | 0.15 | 0.17 | 0.23 | 0.26 | 0.25 | 0.26 | 0.26 | 0.25 |
| US census region | ||||||||
| Northeast | 0.09 | 0.11 | 0.11 | 0.12 | 0.10 | 0.12 | 0.10 | 0.11 |
| Midwest | 0.19 | 0.21 | 0.25 | 0.22 | 0.24 | 0.22 | 0.28 | 0.25 |
| South | 0.55 | 0.47* | 0.43 | 0.44 | 0.45 | 0.45 | 0.34 | 0.43** |
| West | 0.18 | 0.21 | 0.21 | 0.22 | 0.21 | 0.20 | 0.28 | 0.21** |
| n | 553 | 923 | 992 | 1182 | 903 | 1082 | 591 | 767 |
| Population size | 242,789 | 395,156 | 455,377 | 541,569 | 408,738 | 489,292 | 268,886 | 353,020 |
p < 0.01,
p < 0.05 (2014–2016 vs. 2011–2013)
Analysis
We first summarize the trends of health care access and utilization among individuals with SPD from 2011 to 2016 (Fig. 1). We summarize the trends of health care access and utilization among individuals with SPD and low-income from 2011 to 2016 (Fig. 2). We then present population characteristics of individuals with or without reported health care barriers in 2011–2013 and compare them with characteristics in 2014–2016 in Table 1. Since we use the NHIS population survey weights, the results are nationally representative; however, we do not include state-level indicator variables due to data limitations. We next present multivariate logistic regression models used to estimate the trends of health care insurance and barriers to care under the ACA in Table 2. To explore whether the ACA differentially impacted racial and ethnic minorities among low-income individuals, we create a post-ACA indicator variable. This approach has been widely used to estimate the impact of the ACA, a natural experiment, on health care utilization and access (Akosa et al. 2015; Novak et al. 2016; Scott et al. (2015).
Fig. 1.
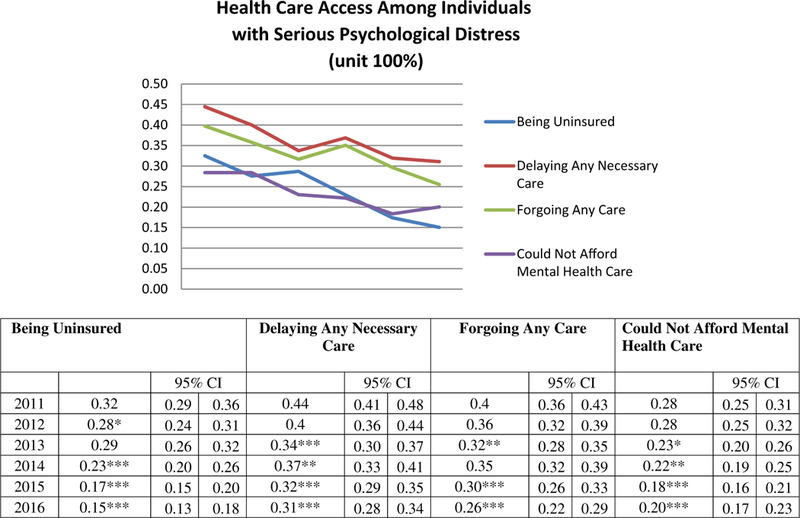
Health care access and coverage among adults (aged 18–64) with serious psychological distress (2011–2016). ***p < 0.001, **p < 0.01, *p < 0.05 (2011 is the reference year)
Fig. 2.
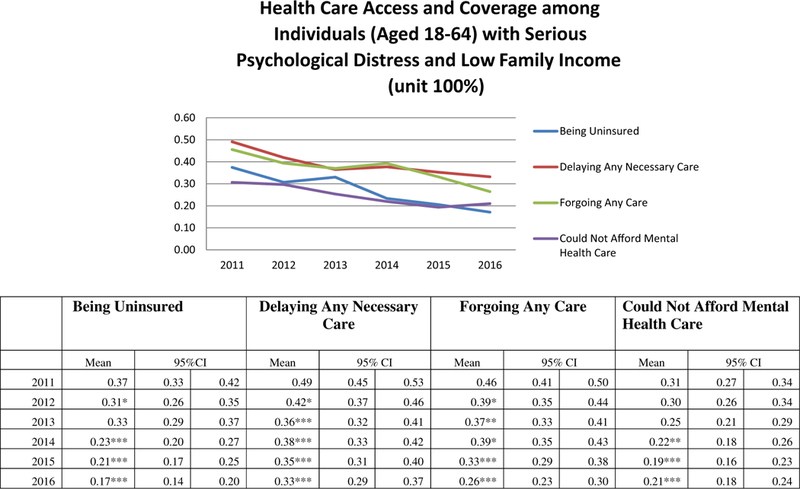
Health care access and coverage among individuals (aged 18–64) with serious psychological distress and low family income (< 200% federal poverty line) (2011–2016). ***p < 0.001, **p < 0.01, *p < 0.05 (2011 is the reference year)
Table 2.
Multivariable logistic regression for adults with serious psychological distress, average marginal effects reported
| Being uninsured | Delaying any necessary care | Forgoing any care | Could not afford mental health care |
|||||
|---|---|---|---|---|---|---|---|---|
| ME (standard error) |
p | ME (standard error) |
p | ME (standard error) |
p | ME (standard error) |
p | |
| Year indicator | ||||||||
| 2011 | Reference | Reference | Reference | Reference | ||||
| 2012 | − 0.04 (0.044) | 0.02 | − 0.04(0.023) | 0.11 | − 0.04(0.021) | 0.07 | − 0.01 (0.021) | 0.72 |
| 2013 | − 0.03 (0.018) | 0.15 | − 0.09 (0.023) | < 0.001 | − 0.07 (0.022) | < 0.001 | − 0.05 (0.019) | 0.02 |
| 2014 | − 0.08 (0.018) | < 0.001 | − 0.07 (0.024) | 0.01 | − 0.04 (0.022) | 0.002 | − 0.06 (0.019) | < 0.001 |
| 2015 | − 0.12(0.017) | < 0.001 | − 0.11 (0.022) | < 0.001 | − 0.08 (0.022) | < 0.001 | − 0.09 (0.018) | < 0.001 |
| 2016 | − 0.14(0.015) | < 0.001 | − 0.12(0.021) | < 0.001 | − 0.13 (0.020) | < 0.001 | − 0.08 (0.017) | < 0.001 |
| Race and ethnicity | ||||||||
| White | Reference | Reference | Reference | Reference | ||||
| African-American | − 0.01 (0.019) | 0.39 | − 0.08 (0.020) | < 0.001 | 0.01 (0.019) | 0.54 | − 0.06 (0.018) | < 0.001 |
| Latino | 0.00 (0.019) | 0.95 | − 0.07 (0.023) | 0.01 | − 0.02(0.021) | 0.30 | − 0.04 (0.020) | 0.07 |
| Other | 0.00 (0.025) | 0.93 | − 0.01 (0.029) | 0.73 | − 0.01 (0.029) | 0.82 | − 0.08 (0.027) | 0.01 |
| Family income | ||||||||
| Below 100% federal poverty line (FPL) | Reference | Reference | Reference | Reference | ||||
| 100–200% FPL | 0.02 (0.014) | 0.30 | 0.07 (0.017) | < 0.001 | 0.04 (0.017) | 0.03 | 0.00 (0.015) | 0.94 |
| Above 200% FPL | − 0.09 (0.018) | < 0.001 | − 0.05 (0.019) | 0.02 | − 0.09 (0.019) | < 0.001 | − 0.05 (0.018) | 0.01 |
| Other covariates | Controlled | Controlled | Controlled | Controlled | ||||
Average Marginal Effects (ME) were reported
Other covariates included in the regressions were sex, marital status, education, citizenship status, interview language, census region, physical health, and limitations in activities of daily living
We report average marginal effects (ME) for each specified group of interest. The Medicaid insurance expansion was needs based, therefore it is reasonable to expect that at lower income levels, people would have been more likely to benefit from public insurance expansion; the extent to which certain races or ethnicities might have benefitted is a matter of ongoing discussion, and therefore we address this in our empirical analysis. Stata 14 was used to conduct all analysis.
Results
Figure 1 presents the trends in health care coverage and indicators of health care access among individuals between the ages of 18 to 64 with SPD from 2011 to 2016. The uninsured rates for individuals with SPD have been reduced from 32% in 2011 to 15% after the implementation of the ACA (p < 0.001). Figure 1 also shows a reduction in the rates of having any delayed or forgone care. Rates of delaying any necessary care declined from 44% in 2011 to 31% in 2016 (p < 0.001). Similarly, the rate of forgoing any necessary care was 26% in 2016, down from 40% in 2011 (p < 0.001). Reductions can also be seen in the rates of not being able to afford any mental health care, which decreased from 28% in 2011 to 20% in 2016 (p < 0.001).
Figure 2 presents the trends in health insurance coverage, reporting delayed or forgone care, or reporting an inability to pay for needed mental health care among low-income individuals. Low-income individuals ages 18–64 were key targets of the Medicaid expansion and thus we sought to investigate if the implementation of the ACA had a differential impact on low-income people. Our findings suggest that people with SPD from low-income families were more likely to be uninsured, and to report delaying, foregoing or being unable to afford mental health care compared with their non-low-income peers who also had SPD. These rates of uninsurance were reduced for low-income individuals with SPD from 37% in 2011 to 17% in 2016; the rate of delaying care decreased from 49% in 2011 to 33% in 2016; forgone care decreased from 46% in 2011 to 26% in 2016; reports of not being able to afford mental healthcare decreased from 31% in 2011 to 21% in 2016.
Table 1 presents the population characteristics of adults reporting SPD regarding uninsured status, delaying necessary care, forgoing any care, and reporting that they were not able to afford mental health care or counseling. Among people with SPD, the highest reported negative outcome was delaying any care, followed by foregoing care, being uninsured, and not being able to afford mental health care or counseling. Thirteen percent of the uninsured population with SPD was non-US citizen in 2014–2016, compared with the 11% rate in 2011–2013 (p < 0.001). Among the uninsured, the rates of individuals with less than high school increased from 25% in 2011–2013 to 27% to 2014–2016 (p < 0.001). Between 2014 and 2016, geographic variation became significant, with 55% of the uninsured people with SPD living in the South, compared with 47% in the 2011–2013 period. Meanwhile, 9% of people who lived in the Northeast were uninsured in 2014–2016, compared to 11% in 2011–2013.
Table 2 shows the results of multivariable logistic regression models that control for an extensive array of predisposing, enabling, and need factors. After controlling for all the covariates, marginal effects of year indicators demonstrated that overall trends of health care access among SPD individuals have been significantly improved compared to 2011, especially after 2014. In particular, post-ACA implementation years, 2015 and 2016, were associated with significant reduction in the likelihoods of being uninsured (average marginal effects (ME) = − 0.12, p < 0.001 in 2015; ME = − 0.14, p < 0.001 in 2016), delaying any necessary care (MEs = − 0.11, and − 0.12, p < 0.001, 2015 and 2016 respectively), forgoing any necessary care (MEs = − 0.08, –0.13, p < 0.001, 2015 and 2016 respectively), and not being able to afford needed mental health care (MEs = − 0.09 to –0.08, p < 0.001, 2015 and 2016 respectively), compared with 2011.
Compared to Whites with SPD, African Americans and Latinos were less likely to report delaying care. African Americans (ME = − 0.06, p < 0.001) and those in the “other” racial category (ME = − 0.08, p < 0.001) had decreases in saying that they could not afford mental health care. Individuals with family income above 200% FPL were also 5–9% less likely to face access barriers, compared to those with income below the 100% FPL.
We report average marginal effects (ME) for each specified group of interest in Table 3. Marginal effects of “post-ACA” indicator were also calculated for African Americans, Latinos, “other” racial and ethnic groups, and people with low family income. MEs were all significant and the magnitudes of the MEs were similar across all groups. Results suggest that mental health care access among racial and ethnic minority populations and people with low income has been significantly improved during 2014–2016, however, gaps in insurance coverage, delaying care, forgoing care, and not being able to afford mental health care remained.
Table 3.
Estimated average differential effect of ACA implementation for racial and ethnic minorities, and people with family income under 200% FPL, among populations with SPD
| Being uninsured | Delaying any necessary care | Forgoing any care | Could not afford mental health care |
|||||
|---|---|---|---|---|---|---|---|---|
| Average marginal effects of post-ACA indicator |
Average marginal effects of post-ACA indicator |
Average marginal effects of post-ACA indicator |
Average marginal effects of post-ACA indicator |
|||||
| ME (standard error) |
P | ME (standard error) |
P | ME (standard error) |
P | ME (standard error) |
P | |
| All races/ethnicities | − 0.11 (0.013) | < 0.001 | − 0.06 (0.015) | < 0.001 | − 0.05 (0.014) | < 0.001 | − 0.06 (0.013) | < 0.001 |
| African American | − 0.10(0.014) | < 0.001 | − 0.05 (0.014) | < 0.001 | − 0.05 (0.014) | < 0.001 | − 0.05 (0.012) | < 0.001 |
| Latino | − 0.11 (0.014) | < 0.001 | − 0.05 (0.014) | < 0.001 | − 0.05 (0.014) | < 0.001 | − 0.06 (0.012) | < 0.001 |
| Other race/ ethnicity | − 0.11 (0.015) | < 0.001 | − 0.06 (0.014) | < 0.001 | − 0.05 (0.014) | < 0.001 | − 0.05 (0.011) | < 0.001 |
| Low Income | − 0.12(0.014) | < 0.001 | − 0.06 (0.015) | < 0.001 | − 0.06 (0.015) | < 0.001 | − 0.07 (0.014) | < 0.001 |
Marginal effects produced by varying the characteristic of interest, i.e., 2014–2016 time frame
Other covariates included in the regressions were sex, marital status, education, citizenship status, interview language, census region, physical health, and limitations in activities of daily living
Discussion
This study utilized a nationally representative data set to examine the impact of the implementation of the ACA on health insurance coverage and barriers to health care access among individuals with SPD. As has been previously suggested, large nationally representative data sets may not necessarily be the ideal data sets to document the unique needs of smaller ethnic groups such as Native Americans and Asians-Americans (Assistant Secretary for Planning and Evaluation 2013; Moffitt et al. 2015).
Notwithstanding, our results provide preliminary correlational evidence that previously uninsured individuals with SPD gained access to health insurance coverage and experienced reductions in the rates of delaying or forgoing necessary care and not being able to afford mental health care in 2014–2016.
This study finds that the implementation of the ACA is associated with an increase in rate of health insurance coverage among nonelderly adults with SPD and a reduction in delaying and forgoing necessary care. The ACA also reduced the odds of individuals with SPD not being able to afford mental health care. Mental health care access among racial and ethnic minority populations with SPD and people with low income and SPD has improved during the 2014–2016 time period, but gaps remain.
Our findings contribute to the emerging literature on the impact of the ACA (Gonzales et al. 2016; Saloner et al. 2017), whose findings suggest that access to health insurance and utilization of services has increased (Wherry and Miller 2016), health care related financial burdens have decreased (Ali et al. 2016b), and barriers to paying for health services have been reduced (Chen et al. 2016). Our findings are consistent with this, in that we found that adults with SPD were more likely to have health insurance coverage and experience lower barriers in accessing treatments after 2014. This study also complements Creedon and Le Cook (2016) who showed an increase in treatment utilization among those with a mental health condition. Taken together, this implies that the ACA not only increased treatment utilization, but also reduced barriers to treatment, including delaying, forgoing, or not being able to afford mental health care among African Americans, Latinos, and “other” races. The improvement in ability to pay for needed mental health care is especially salient in the light of recent work by Mark and colleagues examining psychiatrist reimbursement and psychiatrist participation in health insurance (Mark et al. 2017). This work suggests that psychiatrist may be less likely to participate in insurance networks than other medical specialties, allowing psychiatrists to charge out of network prices that cause the cost of mental healthcare to be higher, better aligning their remuneration with medical specialist rates.
Individuals with mental illness have historically had disproportionately lower rates of health insurance coverage and experienced significant barriers to accessing needed treatments (Han et al. 2015; Croft and Parish 2012; Mechanic 2012). These barriers are frequently related not only to the relatively high cost of mental health treatment in comparison with physical health, but also underscore the need for better integration of physical and mental health care as suggested by leading health Agencies such as the Health Resources and Services Administration and the Substance Abuse Mental Health Services Administration (SAMHSA 2017). The findings that more people were insured and fewer people reported delaying, foregoing, or being unable to afford health care after the implementation of the ACA is consistent with the literature examining the Oregon Health Insurance Experiment and Massachusetts health reform, which has shown evidence of reduced barriers to treatment among the newly insured (Long et al. 2012; Baicker and Finkelstein 2011). We have included 3 years of data after the expansion of Medicaid in 2014 in our analysis, and improvements in health care access appear across all years. If the ACA is not repealed, further reductions in barriers to treatment among individuals with a mental health condition may occur.
Our study has several limitations that are worth noting. First, we were unable to conduct an analysis to estimate whether there was an increase in mental health service utilization among the population of interest. It is unclear whether reduced barriers to health care actually translate into mental or physical health services utilization. Indeed, “delaying any necessary care” and “forgoing any care” do not necessarily apply to mental health services exclusively. Examining whether there was an increase in utilization of mental health services as a result of the implementation of the ACA could be an important avenue for future research. Secondly, prior to the implementation of the ACA, various provisions of the legislation, such as the young adult mandate and early expansion of Medicaid in certain states, were already enacted. The existence of these various provisions in the pre-period of our analysis (i.e., prior to 2011) imparts a conservative bias to our findings. Third, the income thresholds we used in this study (e.g., 200% FPL) are not those used to determine eligibility in the ACA, as states have some liberty in deciding who may receive Medicaid (up to 400% of the FPL). Fourthly, we do not use state identifiers to control for the difference between states that did and didn’t expand Medicaid eligibility. These data limitations (e.g., our inability to identify whether the respondent was from a Medicaid expansion state or not) preclude us from disentangling whether the impacts we observed were due to Medicaid expansion, the health insurance marketplaces, increased employer sponsored insurance, or other provisions of the ACA.
This initial study provides some immediate insights into the impact of ACA among those with SPD. There were changes in both insurance coverage and barriers to care. Since health insurance by itself may be insufficient to guarantee that people with mental illness receive the treatment they need, ongoing outreach initiatives to help patients navigate the health care system might be warranted (Ali et al. 2015). Efforts are needed to encourage the newly enrolled to seek appropriate treatment and to facilitate access to services. As additional years of data become available, future research will be able to better analyze the impact that ACA had on those with mental illness and gain a fuller understanding of the barriers they continue to face in getting care.
Acknowledgments
FundingFunding was provided by National Institute of Mental Health (Grant No. R01MD011523).
Footnotes
Compliance with Ethical Standards
Conflict of interest Ms. Novak was an employee of the Agency for Healthcare Research and Quality at the time this manuscript was prepared. The views expressed in this manuscript are those of the authors who are solely responsible for the content. The views in this manuscript do not represent those of the US Government, the Department of Health and Human Services, or the Agency for Healthcare Research and Quality. Mr. Anderson has nothing to disclose. Dr. Chen has nothing to disclose.
References
- Akosa Antwi Y., Moriya AS, & Simon KI (2015). Access to health insurance and the use of inpatient medical care: evidence from the Affordable Care Act young adult mandate. Journal of Health Economics, 39, 171–187. 10.1016/j.jhealeco.2014.11.007. [DOI] [PubMed] [Google Scholar]
- Ali MM, Chen J, Mutter R, Novak P, & Mortensen K (2016a). The ACA’s dependent coverage expansion and out-of-pocket spending by young adults with behavioral health conditions. Psychiatric Services. 10.1176/appi.ps.201500346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali MM, Teich J, Woodward A, & Han B (2016b). The implications of the affordable care act for behavioral health services utilization. Administration and Policy in Mental Health and Mental Health Services Research Adm Policy Ment Health, 43(1), 11–22. 10.1007/s10488-014-0615-8. [DOI] [PubMed] [Google Scholar]
- Ali MM, Teich JL, & Mutter R (2015). The role of perceived need and health insurance in substance use treatment: implications for the Affordable Care Act. Journal of Substance Abuse Treatment, 54, 14–20. https://doi.org/10.1016Zj.jsat.2015.02.002. [DOI] [PubMed] [Google Scholar]
- Andersen R, & Newman JF (1973). Societal and individual determinants of medical care utilization in the united states. The Milbank Memorial Fund Quarterly. Health and Society, 51(1), 95 10.2307/3349613. [DOI] [PubMed] [Google Scholar]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior, 36(1), 1 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- Assistant Secretary for Planning and Evaluation. (2013). The Feasibility Of Using Electronic Health Data for Research on Small Populations Coverage of Asian-American Subpopulations in Federal Data Collection. Retrieved December 3, 2017, from https://aspe.hhs.gov/report/feasibility-using-electronic-health-data-research- small-populations/coverage-asian-american-subpopulations-feder al-data-collection.
- Avery K, Gardner M, Gee E, Marchetti-Bowick E, McDowell A, Sen A Health plan choice and premiums in the 2016 Health Insurance Marketplace. (2015). Office of the Assistant Secretary for Planning and Evaluation, US Department of Health and Human Services. Retrieved 24 May, 2017 from https://aspe.hhs.gov/pdf-report/health-plan-choice-and-premiums-2016-health-insurance-marketplace.
- Baicker K, & Finkelstein A (2011). The effects of medicaid coverage—learning from the oregon experiment. New England Journal of Medicine N Engl J Med, 365(8), 683–685. 10.1056/nejmp1108222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bustamante AV, Fang H, Rizzo JA, & Ortega AN (2009). Understanding observed and unobserved health care access and utilization disparities among U.S. Latino adults. Medical Care Research and Review, 66(5), 561–577. 10.1177/1077558709338487. [DOI] [PubMed] [Google Scholar]
- Carman KG, Eibner C, & Paddock SM (2015). Trends in health insurance enrollment. 2013–15 Health Affairs, 34(6), 1044–1048. 10.1377/hlthaff.2015.0266. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control/National Center for Health Statistics. 2015. Data Release Imputed Income Files. Retrieved December 1, 2017, from https://www.cdc.gov/nchs/nhis/nhis_2015_data_release.htm.
- Chen J, Bustamante AV, & Tom SE (2015). Health care spending and utilization by race/ethnicity under the Affordable Care Act’s dependent coverage expansion. American Journal of Public Health, 10.2105/ajph.2014.302542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Vargas-Bustamante A, Mortensen K, & Ortega AN (2016). Racial and ethnic disparities in health care access and utilization under the Affordable Care Act. Medical Care, 54(2), 140–146. 10.1097/mlr.0000000000000467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen R, & Zammitti E (2016). Access to care among adults aged 18–64 with serious psychological distress: Early release of estimates from the National Health Interview Survey, 2012-Septem- ber 2015. National Center for Health Statistics, Available from: https://www.cdc.gov/nchs/data/nhis/earlyrelease/er_spd_access_2015_f_auer.pdf. [Google Scholar]
- Cook BL, Zuvekas SH, Chen J, Progovac A, & Lincoln AK (2016). Assessing the individual, neighborhood, and policy predictors of disparities in mental health care. Medical Care Research and Review. 10.1177/1077558716646898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creedon TB, & Cook BL (2016). Access to mental health care increased but not for substance use, while disparities remain. Health Affairs (Millwood), 35(6), 1017–1021. https://doi. org/10.1377/hlthaff.2016.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croft B, & Parish SL (2012). Care integration in the Patient Protection and Affordable Care Act: Implications for behavioral health. Administration and Policy in Mental Health and Mental Health Services Research, 40(4), 258–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler DM (2015). From the Affordable Care Act to affordable care. JAMA, 314(4), 337 10.1001/jama.2015.7683. [DOI] [PubMed] [Google Scholar]
- Gonzales G, Golberstein E, Hill SC, & Zuvekas SH (2016). Psychological distress and enrollment in medicaid. J Behav Health Serv Res. 10.1007/s11414-016-9532-9. [DOI] [PubMed] [Google Scholar]
- Han B, Gfroerer J, Kuramoto SJ, Ali M, Woodward AM, & Teich J (2015). Medicaid expansion under the Affordable Care Act: potential changes in receipt of mental health treatment among low-income nonelderly adults with serious mental illness. American Journal of Public Health, 105(10), 1982–1989. 10.2105/ajph.2014.302521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Andrews G, Colpe L, Hiripi E, Mroczek D, Normand S,…Zaslavsky A (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine 32(6), 959–976. 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Long SK, Stockley K, & Dahlen H (2012). Massachusetts health reforms: Uninsurance remains low, self-reported health status improves as state prepares to tackle costs. Health Affairs, 31(2), 444–451. 10.1377/hlthaff.2011.0653. [DOI] [PubMed] [Google Scholar]
- Majerol M, Newkirk V, & Garfield R (2015). The uninsured: A Primer. Retrieved from http://kff.org/uninsured/report/the-uninsured-a-primer-key-facts-about-health-insurance-and-the-unins ured-in-the-era-of-health-reform/.
- Mark TL, Olesiuk W, Ali MM, Sherman LJ, Mutter R, & Teich JL (2017). Differential reimbursement of psychiatric services by psychiatrists and other medical providers. Psychiatric Services. 10.1176/appi.ps.201700271. [DOI] [PubMed] [Google Scholar]
- Mechanic D (2012). seizing opportunities under the affordable care act for transforming the mental and behavioral health system. Health Affairs, 31(2), 376–382. 10.1377/hlthaff.2011.0623. [DOI] [PubMed] [Google Scholar]
- Moffitt R, Schoeni RF, Brown C, Chase-Lansdale PL, Couper MP, Diez-Roux AV,. Seltzer JA (2015). Assessing the need for a new nationally representative household panel survey in the United States Journal of Economic and Social Measurement, 40(1–4), 1–26. 10.3233/JEM-150411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak P, Williams-Parry KF, & Chen J (2016). Racial and ethnic disparities among the remaining uninsured young adults with behavioral health disorders after the aca expansion of dependent coverage. Journal of Racial and Ethnic Health Disparities. 10.1007/s40615-016-0264-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JJ, Sung H-Y, Max W, Shi Y, & Ong M (2012). Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. International Journal of Methods in Psychiatric Research, 21(2), 88–97. 10.1002/mpr.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloner B, Bandara S, Bachhuber M, & Barry CL Insurance coverage and treatment use under the Affordable Care Act among adults with mental and substance use disorders. Psychiatric Services. 2017; 10.1176/appi.ps.201600182. [DOI] [PubMed] [Google Scholar]
- Scott JW, Sommers BD, Tsai TC, Scott KW, Schwartz AL, & Song Z (2015). Dependent coverage provision led to uneven insurance gains and unchanged mortality rates in young adult trauma patients. Health Affairs (Millwood), 34(1), 125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommers BD, Gunja MZ, Finegold K, & Musco T (2015). Changes in self-reported insurance coverage, access to care, and health under the Affordable Care Act. JAMA, 314(4), 366 https ://doi.org/10.1001/jama.2015.8421. [DOI] [PubMed] [Google Scholar]
- Substance Abuse Mental Health Services Administration. (2017). Integrating Behavioral Health Into Primary Care. Retrieved 1 May, 2017 from http://www.integration.samhsa.gov/integrated-care- models/behavioral-health-in-primary-care.
- Wherry LR, & Miller S (2016). Early coverage, access, utilization, and health effects associated with the Affordable Care Act medicaid expansions. Annals of Internal Medicine, 164(12), 795 10.7326/m15-2234. [DOI] [PMC free article] [PubMed] [Google Scholar]


