Abstract
Purpose
Respiratory syncytial virus (RSV) infection can cause various neurological complications. This study aimed to investigate the RSV-associated neurologic manifestations that present with seizures.
Methods
We retrospectively reviewed the medical records of patients aged less than 15 years with laboratory-confirmed RSV infections and seizures between January 2011 and December 2016 in a regional hospital in South Korea.
Results
During this period, 1,193 patients with laboratory-confirmed RSV infection were identified. Of these, 35 (35 of 1,193, 2.93%; boys, 19; girls, 16; mean age: 20.8±16.6 months) presented with seizure. Febrile seizure was the most common diagnosis (27 of 35, 77.1%); simple febrile seizures in 13 patients (13 of 27, 48.1%) and complex febrile seizures in 14 (14 of 27, 51.9%). Afebrile seizures without meningitis or encephalopathy were observed in 5 patients (5 of 35, 14.3%), seizures with meningitis in 2 (2 of 35, 5.7%), and seizure with encephalopathy in 1 (1 of 35, 2.9%) patient. Lower respiratory symptoms were not observed in 8 patients. In a patient with encephalopathy, brain diffusion-weighted magnetic resonance imaging revealed transient changes in white matter, suggesting cytotoxic edema as the mechanism underlying encephalopathy. Most patients recovered with general management, and progression to epilepsy was noted in only 1 patient.
Conclusion
Although febrile seizures are the most common type of seizure associated with RSV infection, the proportion of patients with complex febrile seizures was higher than that of those with general febrile seizures. Transient cytotoxic edema may be a pathogenic mechanism in RSV-related encephalopathy with seizures.
Keywords: Respiratory syncytial virus, Child, Seizure, Magnetic resonance imaging
Introduction
The respiratory syncytial virus (RSV) is an important cause of acute respiratory tract infection in young children. The common respiratory manifestations are bronchiolitis, pneumonia, bronchitis, and croup. By the age of 2 years, approximately 90% children are infected by RSV, and approximately 45% of the RSV-related hospital admissions occur in children younger than 6 months [1,2].
As in other common viral infections, RSV may be associated with neurological manifestations, including seizures, encephalopathy, extraocular movement disorder, and central apnea [3-8]. Although the pathogenesis of the neurologic complications are not fully understood, the possible contributions of immune-related cytokine responses, less well-proven direct invasion of virus particles, and brain stem-related mechanisms for respiratory control have been recognized [3,5,9-11].
The incidence of RSV-associated neurologic complications varies across studies and study populations. Sweetman et al. [7] reported the incidence of RSV-associated neurologic complications to be 1.2%, which did not include cases with simple febrile seizure, and Ng et al. [12] reported the incidence of RSV-associated encephalopathy to be 1.8%. In a pediatric intensive care unit (PICU)-based study, Kho et al. [13] reviewed the cases of children between birth and 2 years of age with acute neurological symptoms and identified 39.1% of them as RSV-positive. In contrast, Millichap and Wainwright [5] reported that only 1% of the RSV-positive patients were admitted to the PICU with neurologic complications. In a study comparing the common viruses responsible for febrile seizure, Chung and Wong [14] revealed that the incidence of febrile seizure for RSV was 5.3%, and among them, complex febrile seizure was observed in 13.6% of cases, which was lower than the percentage of such cases for influenza and adenovirus.
In a previous study in Korea during November 2002 and June 2007, Yoon et al. [15] reported that the overall incidences of RSVassociated neurologic complications and seizures were 7.1% and 1.9%, respectively. Another study in Korea by Park et al. [16] reported that the incidence of RSV-associated encephalitis was 0.08%. The same study showed that RSV-associated brain magnetic resonance imaging (MRI) findings may resemble those of other viral and limbic encephalitis, and no abnormality on diffusion-weighted imaging (DWI) was found [16,17].
Although the study by Yoon et al. [15] was the first and the only study on the overall RSV-associated neurologic complications in Korea, further analysis of patients with seizure based on presumed causes was needed. In addition, most of the previous studies were regarding encephalopathy or relatively severe patients, and did not focus on overall features of RSV-associated seizures. It has not yet been fully determined whether the clinical characteristics of the RSV-associated febrile seizure are similar to those of the general febrile seizure, and whether RSV-associated afebrile seizures are benign situation-related seizures, as reported by Miyama and Goto [6]. Based on this background, we aimed to investigate the RSV-associated neurologic manifestations in children who presented with seizures. Furthermore, we report a transient DWI change in a young child with acute encephalopathy symptoms exhibiting seizures.
Materials and methods
1. Patients
The medical records of the patients admitted to Hanyang University Guri Hospital from January 2011 to December 2016 were reviewed retrospectively. The inclusion criteria were as follows: children younger than 15 years, laboratory-confirmed RSV infection, and presentation of neurologic symptoms with seizures during the infection. The patients whose neurological symptoms were caused by factors other than RSV infections, and those with epilepsy were excluded. In this study, a simple febrile seizure was defined as a seizure occurring during a febrile illness and not caused by an acute disease of the nervous system in children aged between 6 months and 5 years [18]. The seizure should be generalized and short (duration less than 15 minutes) and not recur within 24 hours. Complex febrile seizure was defined as a 1) focal, 2) generalized, and prolonged seizure lasting more than 15 minutes and recurring with 24 hours, or 3) postictal neurological abnormalities, such as Todd's palsy [18]. This study was performed in a regional hospital in Guri, a city located in the metropolitan area around Seoul. All research protocols were approved by the Institutional Review Board (IRB) at Hanyang University Guri Hospital (approval number: 2017-12-014). Informed consent was exempted by the IRB.
2. Data collection
Demographic information and clinical courses of the patients; information regarding combined diseases; results of blood tests; cerebrospinal fluid (CSF) examinations; electroencephalography (EEG); and brain imaging techniques such as MRI (including DWI) were analyzed. Detection of RSV was performed using real-time reverse transcription-polymerase chain reaction, with samples obtained by nasopharyngeal swabbing (AdvanSure, LG, Seoul, Korea).
3. Statistical analysis
Descriptive statistics were used to analyze demographic data. The continuous variables are presented as mean±standard deviation. The statistical analysis was performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA). The incidence reported by national RSV surveillance during the study period was used for comparison with the incidence pattern of this study.
Results
1. Demographic data
We identified a total of 1,193 children who were diagnosed with laboratory-confirmed RSV infection during the study period; 35 of them had neurological complications with seizures (35 of 1,193, 2.93%), (boys, 19; girls, 16). Their mean age was 20.8±16.6 months (range, 7 weeks-87 months) (Table 1). Most of them were younger than 36 months (32 of 35, 91.4%).The peak incidence month was November, and the seasonal distribution of incidence corresponded with the outbreak report of Korea Centers for Disease Control and Prevention (Fig. 1).
Table 1.
Clinical manifestations of children with respiratory syncytial virus-associated seizures
| Manifestation | No. (%) | Age (mo), mean±SD | Sex, boy:girl |
|---|---|---|---|
| Febrile seizure only | |||
| Simple | 13 (37.1) | 24.3±13.1 | 6:7 |
| Complex | 14 (40.0) | 22.6±20.1 | 9:5 |
| Afebrile seizure only | 5 (14.3) | 16.8±14.4 | 4:1 |
| Encephalopathy with seizure | 1 (2.9) | 1.6 | 0:1 |
| Meningitis with seizure | 2 (5.7) | 4.0±4.2 | 0:2 |
| Total | 35 (100) | 20.8±16.6 | 19:16 |
SD, standard deviation.
Fig. 1.
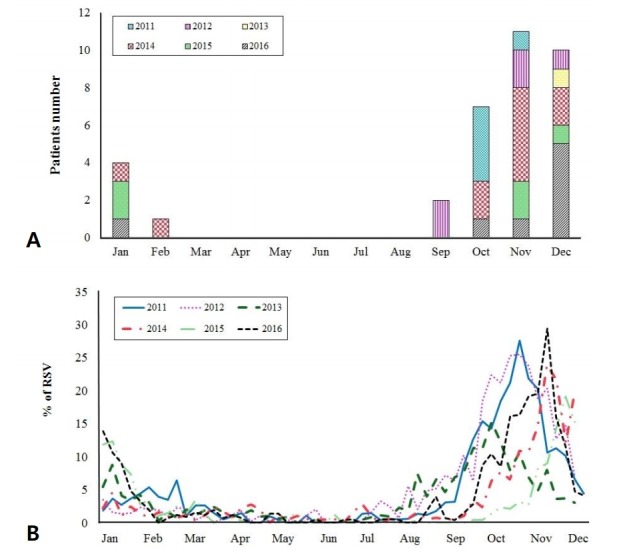
(A) Seasonal distribution of patients with respiratory syncytial virus (RSV)-associated seizures in 2011–2016, showing that the peak incidence month was November. (B) Seasonal distribution of national RSV report of the Korea Centers for Disease Control and Prevention (KCDC) in 2011–2016. The distribution of the incidence of RSV-associated seizures was consistent with the report of the RSV epidemic by KCDC consistent with the report of the RSV epidemic by KCDC.
2. Neurologic manifestations with seizures
The most common neurologic manifestation was febrile seizure, identified in 27 patients (27 of 35, 77.1%); afebrile seizures without meningitis or encephalopathy were observed in 5 (5 of 35, 14.3%); seizures with meningitis were found in 2 (2 of 35, 5.7%); and seizures with encephalopathy were reported in 1 (1 of 35, 2.9%). Eight of the 35 patients (22.9%) did not present with respiratory symptoms such as pneumonia or bronchiolitis. In 15 patients, coinfections were identified (15 of 35, 42.9%). The details of overall clinical characteristics are described in Table 1.
For 21 patients (21 of 35, 60.0%), EEG signals were recorded, and six of them (6 of 21, 28.6%) showed abnormal focal discharges. Neuroimages were acquired for 26 patients (26 of 35, 74.3%), and 4 of them (4 of 26, 15.4%) showed abnormal results. The CSF examinations were performed in 21 patients, and 5 of them (5 of 21, 23.8%) showed abnormal results: CSF leukocytosis in 2 patients (38.5 ±37.5/mm3; range, 12–65/mm3) and high opening pressure (>18 cmH2O; range, 20–26 cmH2O) in 3 patients.
Among the patients with febrile seizure (boys, 15; girls, 12; mean age, 23.4±16.8 months), simple febrile seizure was observed in 13 (48.1%) and complex febrile seizure in 14 (51.9%). The mean age of patients with simple febrile seizure (24.3±13.1 months) and those with complex febrile seizure (22.6±20.1 months) was similar. The characteristics of complex febrile seizures included multiple seizures in a day (10 of 14, 71.4%) and prolonged seizures, of over 20 minutes (4 of 14, 28.6%). Abnormal EEG signals were observed in 2 patients (both with complex febrile seizure): epileptiform discharges from the frontal (n=1) and fronto-central (n=1) areas. Brain MRI abnormalities were observed in 2 patients (both with complex febrile seizure): decreased perfusion in the left frontal lobe (n=1) and benign lipoma (n=1). Abnormal CSF pressure was observed in 3 of the patients: simple febrile seizure (n=1) and complex febrile seizure (n=2). Details of the clinical profiles of febrile seizure are described in Table 2. All the patients with febrile seizure recovered without complication.
Table 2.
Detailed characteristics of patients with respiratory syncytial virus infection and febrile seizure
| Patient | Sex/age (mo) | Seizure type | Features | Other conditions | CSF | Brain image | EEG | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | M//19 | S, GTC | - | Bronchiolitis | ND | ND | ND | Recovered |
| 2 | F/13 | S, GT | - | - | NL | CT (NL) | ND | Recovered |
| 3 | F/18 | S, GTC | - | Pneumonia (rhinovirus, mycoplasma) | ND | ND | ND | Recovered |
| 4 | F/21 | S, GT | - | Pneumonia | ND | ND | ND | Recovered |
| 5 | M/15 | S, GTC | - | Bronchiolitis | ND | ND | ND | Recovered |
| 6 | M/19 | S, GTC | - | Bronchiolitis | ND | ND | ND | Recovered |
| 7 | M/55 | S, GTC | - | Bronchitis | ND | ND | ND | Recovered |
| 8 | F/18 | S, GTC | - | Pneumonia | NL | CT (NL) | ND | Recovered |
| 9 | F/49 | S, GTC | - | Pneumonia (rhinovirus) | ND | ND | ND | Recovered |
| 10 | F/30 | S, GTC | - | - | ND | ND | ND | Recovered |
| 11 | M/23 | S, GTC | - | Pneumonia (mycoplasma) | ND | ND | ND | Recovered |
| 12 | F/14 | S, GTC | - | - | NL | MRI (NL) | ND | Recovered |
| 13 | M/21 | S, GTC | - | - | ND | CT (NL) | ND | Recovered |
| 14 | F/12 | C, GTC | 3 times/day | Bronchitis | NL | MRI (NL) | NL | Recovered |
| 15 | F/19 | C, GTC | 2 times/day | Bronchiolitis | NL | MRI (decreased focal perfusion) | Focal spikes (fronto-central) | Recovered |
| 16 | F/21 | C, GTC | 2 times/day | Pneumonia (mycoplasma) | NL | CT (NL) | NL | Recovered |
| 17 | M/17 | C, GTC | 3 times/day | Pneumonia | NL | CT (NL) | ND | Recovered |
| 18 | M/15 | C, GTC | 2 times/day | - | NL | MRI (NL) | ND | Recovered |
| 19 | M/31 | C, GTC | >20 min | Pneumonia (parainflu) | NL | MRI (NL) | NL | Recovered |
| 20 | M/4 | C, hypomotor | >20 min | Bronchiolitis (rhinovirus, coronavirus) | NL | MRI (NL) | NL | Recovered |
| 21 | M/40 | C, GTC | 2 times/day | Bronchitis | NL | CT (NL) | ND | Recovered |
| 22 | M/87 | C, GTC | >20 min | - | NL | MRI (Lipoma) | NL | Recovered |
| 23 | F/20 | C, GTC | 2 times/day | Bronchitis (adenovirus) | ND | MRI (NL) | ND | Recovered |
| 24 | M/12 | C, GC | 2 times/day | Pneumonia | ND | MRI (NL) | NL | Recovered |
| 25 | F/23 | C, GTC | 3 times/day | Pneumonia (rhinovirus) | NL | CT (NL) | Diffuse slowing | Recovered |
| 26 | M/18 | C, GTC | 2 times/day | - | NL | MRI (NL) | Focal spikes (frontal) | Recovered |
| 27 | M/30 | C, GT | >20 min | Pneumonia | ND | CT (NL) | NL | Recovered |
S, simple; C, complex; GTC, generalized tonic clonic; GT, generalized tonic; GC, generalized clonic; ND, not done; NL, normal; CT, computed tomography; MRI, magnetic resonance image; EEG, electroencephalography.
Five patients showed afebrile seizures without meningitis or encephalopathy (boy, 4; girl, 1; mean age, 16.8±14.4 months). The types of seizure were as follows: generalized tonic-clonic (n=2), generalized tonic (n=1), hypomotor (n=1), and myoclonic (n=1). The patients had no family history of epilepsy and showed respiratory symptoms. Abnormal EEG signals were observed in 2 of the patients: focal epileptiform discharges from the parietal (n=1) and occipital (n=1) areas. Brain MRI abnormalities were observed in one of the patients: benign cavernous angioma. CSF examinations were performed in 4 patients, and all of them showed normal results. One of the patients who presented with epileptiform discharges from the parietal area during the first seizure later evolved to epilepsy. Further details of the clinical profiles of afebrile seizures are described in Table 3.
Table 3.
Detailed characteristics of patients with respiratory syncytial virus infection and afebrile seizure
| Patient | Sex/age (mo) | Seizure type | Previous seizure | Other conditions | CSF | Brain image | EEG | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | M//2 | GTC | No | Bronchiolitis | NL | MRI (NL) | NL | Recovered |
| 2 | M/35 | Hypomotor | No | Bronchitis (adenovirus) | NL | MRI (NL) | Focal spikes (left parietal) | Epilepsy |
| 3 | M/22 | Myoclonic | No | Pneumonia (adenovirus, coronavirus) | ND | MRI (NL) | NL | Recovered |
| 4 | F/23 | GTC | Yes | Pneumonia (rhinovirus) | NL | CT (NL) | ND | Recovered |
| 5 | M/2 | GC | No | Bronchiolitis | NL | MRI (cavernous angioma) | Focal spikes (parieto-occipital) | Recovered |
GTC, generalized tonic clonic; GC, generalized clonic; ND, not done; NL, normal; CT, computed tomography; MRI, magnetic resonance image; EEG, electroencephalography.
Seizure with meningitis, confirmed by CSF examination, was observed in 2 patients (both girls; mean age, 4.0±4.2 months). One of the patients was a 7-month-old girl with urinary tract infection; she did not present with definite respiratory symptoms and showed abnormal EEG signals (continuous theta on left frontal electrode). In the patients with meningitis, CSF bacterial cultures and tests for enterovirus yielded negative results. Brain MRI results were normal in both patients. We did not perform the CSF examinations for the RSV. All the patients recovered without complication. Seizure with encephalopathy was observed in 1 patient. Detailed findings have been described below.
3. A case with encephalopathy and transient MRI changes
The patient was a 7-week-old female baby who visited our hospital due to respiratory difficulty, high fever (38.7ºC), and lethargy. Her 3-year-old elder brother had had a respiratory infection recently. Before admission, the patient was healthy and had no family history of seizure disorders. On the day of admission, she experienced three consecutive generalized tonic-clonic seizures with fever. Consciousness recovery between seizures was uncertain. After the administration of intravenous lorazepam and phenobarbital, the seizures stopped. A polymerase chain reaction-based virus test using nasopharyngeal swab revealed RSV infection; CSF cytological tests, biochemical tests, and bacterial cultures yielded no abnormalities. Brain MRI with DWI performed at first hospital day revealed high signal intensity (HSI) at the internal capsule and splenium of corpus callosum on DWI and subtle low signals on apparent diffusion coefficient (ADC) imaging at the same area. The HSI on DWI rapidly disappeared by the fourth hospital day, suggesting that the mechanism of encephalopathy was transient cytotoxic edema (Fig. 2). The EEG recordings showed sharp discharges from the frontotemporal area. The patient was admitted to the PICU, and gradually recovered over a week. In a follow-up visit at 12 months of age, neurological complication was not found and the abnormal discharges on EEG had disappeared.
Fig. 2.
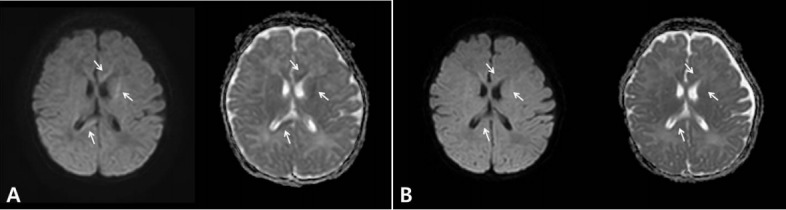
(A) Brain magnetic resonance imaging (MRI) with diffusion-weighted imaging (DWI) on the first hospital day shows high signal intensity (HSI) at the internal capsule (upper and middle arrow) and splenium of the corpus callosum (lower arrow) on DWI (left) and subtle low signals on apparent diffusion coefficient (ADC) imaging (right) in the same area. (B) Brain MRI with DWI (left) and ADC (right) on the fourth hospital day shows disappearance of HSI on DWI, suggesting that the mechanism of encephalopathy was transient cytotoxic edema.
Discussion
In the present study, we reported overall RSV-associated seizures in children. In summary, febrile seizure was the most common followed by afebrile seizure. Notably, the incidence of complex febrile seizure was higher, even more than that of simple febrile seizure. Although rare, RSV-associated meningitis and encephalopathy also accompanied seizures. Brain DWI of a patient with encephalopathy showed transient white matter change, which was presumed to be cytotoxic edema. The outcomes were mostly favorable, including that of the patient with encephalopathy, and one of the patients who presented with afebrile seizure evolved to epilepsy later.
An enveloped virus with negative-sense single-stranded RNA genome, RSV belongs to the Paramyxoviridae family [9,19]. According to a recent systematic review, 33.1 million children aged less than 5 years are estimated to exhibit RSV-associated acute lower respiratory infections globally. Among them, 3.2 million are hospitalized and 59,600 cases result in in-hospital deaths [1]. Beside the common respiratory manifestations, extrapulmonary symptoms can be caused by RSV infection of the heart, liver, kidney, endocrine, and central nervous system [3,9].
Although uncommon, central nervous system involvement is an important complication of RSV infection. The representative neurological manifestations are encephalopathy, seizures, and apnea. The rare complications are strabismus, acute axonal polyneuropathy, and diaphragmatic flutter [4,20,21]. However, most of the previous studies have focused on acute encephalopathy and PICU cases, and only a few have investigated the milder febrile seizure and afebrile seizures [11,12,22]. In the present study, we included overall seizures, which were reasonably presumed to be caused by RSV infection.
Febrile seizure may occur in any condition with acute elevation of body temperature in genetically predisposed children. The peak incidence age is approximately 18 months [23]. Most of the febrile seizures are generalized, with approximately one-third of the patients exhibiting complex febrile seizure and febrile status epilepticus occurring in 5% of the cases [24]. However, the RSVrelated febrile seizure have not been well-characterized. The well-known study of Sweetman et al. [7] reported the incidence of neurological complication associated with RSV to be 1.2% (12 of 964 patients). The authors included 1 patient with complex febrile seizure but excluded five patients with simple febrile seizure. In the present study, the incidence of RSV-associated seizures, including febrile seizure, was 2.9%, which is higher than the finding of Sweetman et al. [7] The global features of febrile seizure observed in this study were similar to those of the generally known febrile seizure, such as age and benign nature. However, the incidence of complex febrile seizure was higher than that of simple febrile seizure. Most of the patients showed multiple seizures in a day, which may be a distinguishing characteristic of RSV-associated febrile seizure. The reason of higher incidence of complex febrile seizure in RSV-associated febrile seizure is unclear. Previous studies reported the increased levels of CSF proinflammatory cytokines such as interleukin (IL)-6, IL-8, monocyte chemoattractant protein-1 and macrophage inflammatory protein-1β in patients with encephalopathy who had RSV infection. Although febrile seizure is not as severe as encephalopathy is, RSV-specific cytokine responses may be related with multiple or prolonged RSV-associated febrile seizures [11,25,26]. As RSV is one of the common infections in young children, there should be further studies of the characteristics of febrile seizure in RSV infection.
The incidence of RSV-associated afebrile seizure in Japanese children has been reported to be 0.59% (6 of 1,019 patients), which is similar to the incidence reported in our study (0.42%, 5 of 1,193) [6]. The authors suggested that the RSV-associated afebrile seizures were situation-related, and prognoses were quite favorable [6]. In our study population, the seizures were of various types, and in one of the cases, progressed to epilepsy. It is uncertain whether the RSV infection was merely incidental or might have influenced the occurrence of epilepsy. Further studies are needed to clarify the role of RSV in epilepsy.
Encephalopathy is a well-recognized RSV-associated complication, and its incidence has been reported to be 1.8% [12]. RSV-associated encephalopathies are often present with seizure [12]. Millichap and Wainwright [5] reported a greater severity of the neurological complications of RSV infection. They authors reported the cases of 9 patients, of which 4 (44%) were complicated by cardiac arrest, and 2 of the patients died [5]. Uda and Kitazawa [8] reported that the RSV-positive status epilepticus group required more ventilator care and antiepileptic drug treatment than did the RSV-negative status epilepticus group, and nearly one-third of them developed encephalopathy and profound neurological sequelae. In the present study, encephalopathy with seizure was rare and observed in only one patient. She recovered without complications, and DWI showed transient changes.
There are various RSV-associated neuroradiological findings. In most cases, brain MRI reveals no changes. However, the findings of brain edema on computed tomography and focal HSI on MRI (fluid attenuation inversion recovery and DWI) in CSF RSV-positive patients with seizures in another study suggest a pathogenic heterogeneity [11]. Furthermore, DWI abnormalities in the globus pallidus in the patient suggest ischemic changes [5]. In the study by Park et al. [16], the abnormal MRI findings for RSV-related encephalitis were rhombenmesencephalitis, limbic encephalitis, and acute disseminated encephalomyelitis, and diffusion abnormality on DWI was not found. In our encephalopathy case, the patient showed transient HSI on DWI on the first day of acute symptoms; this rapidly disappeared over 3 days. Our case suggests that cytotoxic edema is one of the pathogenic mechanisms underlying RSV-associated encephalopathy. Moreover, DWI can detect the early changes in encephalitis, and appropriate timing of MRI is important to reveal the dynamic changes [27]. In the very acute stage, restricted diffusion can be detected; in the subacute stage, diffusion restriction diminishes and the ADC value increases [27]. A good outcome is usually related with the absence of cytotoxic edema, because it implies cellular edema, which may result in cellular death [27]. However, the outcome of our patient was favorable; hence, cytotoxic edema of white matter in RSV-associated encephalopathy may not always be associated with poor outcome. Transient white matter cytotoxic edema is rare, and has been previously reported in a child with traumatic brain injury, whose DWI and ADC revealed restricted diffusion in the corpus callosum and peri-atrial white matter [28,29]. The abundant N-methyl-D-aspartate-receptors in the corpus callosum may lead to intracellular calcium entry [28]. Increased Ca2+ activates enzymes such as ATPase, phospholipase, protease, and endonucleases can lead to the cell injury and death [30].
The limitation of this study lies in not including the nonseizure RSV-associated neurological complications and the inability to test RSV from CSF. Considering the high incidence and morbidity of RSV infection in young children, more studies are needed in the future.
We investigated the RSV-associated neurologic complications which are presented with seizures. It should be kept in mind that during an RSV epidemic, febrile seizure is more likely to repeat within 24 hours than is generally expected. Furthermore, DWI can detect early brain changes and reflect the pathophysiology of RSVassociated encephalopathy.
Acknowledgments
This work was supported by the research fund of Hanyang University (HY-2016).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Shi T, McAllister DA, O'Brien KL, Simoes EAF, Madhi SA, Gessner BD, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet. 2017;390:946–58. doi: 10.1016/S0140-6736(17)30938-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins PL, Graham BS. Viral and host factors in human respiratory syncytial virus pathogenesis. J Virol. 2008;82:2040–55. doi: 10.1128/JVI.01625-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohmwald K, Espinoza JA, Becerra D, Rivera K, Lay MK, Bueno SM, et al. Inflammatory damage on respiratory and nervous systems due to hRSV infection. Curr Opin Immunol. 2015;36:14–21. doi: 10.1016/j.coi.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Eisenhut M. Extrapulmonary manifestations of severe respiratory syncytial virus infection--a systematic review. Crit Care. 2006;10:R107. doi: 10.1186/cc4984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Millichap JJ, Wainwright MS. Neurological complications of respiratory syncytial virus infection: case series and review of literature. J Child Neurol. 2009;24:1499–503. doi: 10.1177/0883073808331362. [DOI] [PubMed] [Google Scholar]
- 6.Miyama S, Goto T. Afebrile seizures associated with respiratory syncytial virus infection: a situation-related seizure disorder in early infancy. Pediatr Int. 2011;53:113–5. doi: 10.1111/j.1442-200X.2010.03188.x. [DOI] [PubMed] [Google Scholar]
- 7.Sweetman LL, Ng YT, Butler IJ, Bodensteiner JB. Neurologic complications associated with respiratory syncytial virus. Pediatr Neurol. 2005;32:307–10. doi: 10.1016/j.pediatrneurol.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 8.Uda K, Kitazawa K. Febrile status epilepticus due to respiratory syncytial virus infection. Pediatr Int. 2017;59:878–84. doi: 10.1111/ped.13300. [DOI] [PubMed] [Google Scholar]
- 9.Bohmwald K, Espinoza JA, Rey-Jurado E, Gómez RS, González PA, Bueno SM, et al. Human respiratory syncytial virus: infection and pathology. Semin Respir Crit Care Med. 2016;37:522–37. doi: 10.1055/s-0036-1584799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moon JH, Na JY, Kim JH, Yum MK, Oh JW, Kim CR, et al. Neurological and muscular manifestations associated with influenza B infection in children. Pediatr Neurol. 2013;49:97–101. doi: 10.1016/j.pediatrneurol.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Kawashima H, Ioi H, Ushio M, Yamanaka G, Matsumoto S, Nakayama T. Cerebrospinal fluid analysis in children with seizures from respiratory syncytial virus infection. Scand J Infect Dis. 2009;41:228–31. doi: 10.1080/00365540802669543. [DOI] [PubMed] [Google Scholar]
- 12.Ng YT, Cox C, Atkins J, Butler IJ. Encephalopathy associated with respiratory syncytial virus bronchiolitis. J Child Neurol. 2001;16:105–8. doi: 10.1177/088307380101600207. [DOI] [PubMed] [Google Scholar]
- 13.Kho N, Kerrigan JF, Tong T, Browne R, Knilans J. Respiratory syncytial virus infection and neurologic abnormalities: retrospective cohort study. J Child Neurol. 2004;19:859–64. doi: 10.1177/08830738040190110301. [DOI] [PubMed] [Google Scholar]
- 14.Chung B, Wong V. Relationship between five common viruses and febrile seizure in children. Arch Dis Child. 2007;92:589–93. doi: 10.1136/adc.2006.110221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoon SW, Kim HJ, Yum MK, Seol IJ. Neurologic complications associated with respiratory syncytial virus infection in childhood. J Korean Child Neurol Soc. 2008;16:206–12. [Google Scholar]
- 16.Park A, Suh SI, Son GR, Lee YH, Seo HS, Eun BL, et al. Respiratory syncytial virus-related encephalitis: magnetic resonance imaging findings with diffusion-weighted study. Neuroradiology. 2014;56:163–8. doi: 10.1007/s00234-013-1305-z. [DOI] [PubMed] [Google Scholar]
- 17.Park A, Suh S. Respiratory syncytial virus-related encephalitis: magnetic resonance imaging findings with diffusion-weighted study: response to a "letter to the editor". Neuroradiology. 2014;56:433. doi: 10.1007/s00234-014-1341-3. [DOI] [PubMed] [Google Scholar]
- 18.Capovilla G, Mastrangelo M, Romeo A, Vigevano F. Recommendations for the management of "febrile seizures": Ad Hoc Task Force of LICE Guidelines Commission. Epilepsia. 2009;50 Suppl 1:2–6. doi: 10.1111/j.1528-1167.2008.01963.x. [DOI] [PubMed] [Google Scholar]
- 19.Hacking D, Hull J. Respiratory syncytial virus--viral biology and the host response. J Infect. 2002;45:18–24. doi: 10.1053/jinf.2002.1015. [DOI] [PubMed] [Google Scholar]
- 20.Adams JA, Zabaleta IA, Sackner MA. Diaphragmatic flutter in three babies with bronchopulmonary dysplasia and respiratory syncytial virus bronchiolitis. Pediatr Pulmonol. 1995;19:312–6. doi: 10.1002/ppul.1950190511. [DOI] [PubMed] [Google Scholar]
- 21.Eisenhut M. Extrapulmonary manifestations of severe RSV bronchiolitis. Lancet. 2006;368:988. doi: 10.1016/S0140-6736(06)69409-9. [DOI] [PubMed] [Google Scholar]
- 22.Morichi S, Kawashima H, Ioi H, Yamanaka G, Kashiwagi Y, Hoshika A, et al. Classification of acute encephalopathy in respiratory syncytial virus infection. J Infect Chemother. 2011;17:776–81. doi: 10.1007/s10156-011-0259-5. [DOI] [PubMed] [Google Scholar]
- 23.Berg AT, Shinnar S. Complex febrile seizures. Epilepsia. 1996;37:126–33. doi: 10.1111/j.1528-1157.1996.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 24.Patel N, Ram D, Swiderska N, Mewasingh LD, Newton RW, Offringa M. Febrile seizures. BMJ. 2015;351:h4240. doi: 10.1136/bmj.h4240. [DOI] [PubMed] [Google Scholar]
- 25.Kawashima H, Kashiwagi Y, Ioi H, Morichi S, Oana S, Yamanaka G, et al. Production of chemokines in respiratory syncytial virus infection with central nervous system manifestations. J Infect Chemother. 2012;18:827–31. doi: 10.1007/s10156-012-0418-3. [DOI] [PubMed] [Google Scholar]
- 26.Zlateva KT, Van Ranst M. Detection of subgroup B respiratory syncytial virus in the cerebrospinal fluid of a patient with respiratory syncytial virus pneumonia. Pediatr Infect Dis J. 2004;23:1065–6. doi: 10.1097/01.inf.0000143654.12493.c9. [DOI] [PubMed] [Google Scholar]
- 27.Donmez FY. Respiratory syncytial virus-related encephalitis: magnetic resonance imaging findings with diffusion-weighted study. Neuroradiology. 2014;56:431–2. doi: 10.1007/s00234-014-1337-z. [DOI] [PubMed] [Google Scholar]
- 28.Al Brashdi YH, Albayram MS. Reversible restricted-diffusion lesion representing transient intramyelinic cytotoxic edema in a patient with traumatic brain injury. Neuroradiol J. 2015;28:409–12. doi: 10.1177/1971400915598071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takayama H, Kobayashi M, Sugishita M, Mihara B. Diffusion-weighted imaging demonstrates transient cytotoxic edema involving the corpus callosum in a patient with diffuse brain injury. Clin Neurol Neurosurg. 2000;102:135–9. doi: 10.1016/s0303-8467(00)00079-2. [DOI] [PubMed] [Google Scholar]
- 30.Kovac S, Domijan AM, Walker MC, Abramov AY. Seizure activity results in calcium- and mitochondria-independent ROS production via NADPH and xanthine oxidase activation. Cell Death Dis. 2014;5:e1442. doi: 10.1038/cddis.2014.390. [DOI] [PMC free article] [PubMed] [Google Scholar]


