Abstract
Background:
Achieving a rapid onset and durable methods of treatment for major depressive disorders is an issue pursuing in psychiatry. This study was designed to assess the therapeutic efficacy of intravenous (IV) ketamine injection in controlling depressive symptoms in comparison with electroconvulsive therapy (ECT) in major depressed disordered patients.
Materials and Methods:
Thirty-two patients over 18 years of age who were candidates for ECT were enrolled in the study. They were allocated into two groups using block design randomization. Sixteen patients received IV infusion of 0.5-mg/kg ketamine and 16 patients underwent a bitemporal ECT. To evaluate the changes in depression severity, researchers administered Hamilton Depression Rating Scale (HDRS) at baseline, before each treatment session, and four time points posttreatment (week 1 and months 1, 2, and 3). The Wechsler Memory Scale was used to evaluate the cognitive state of patients in week 1, month 1, and month 3 of the treatment.
Results:
The HDRS showed improvement in depressive symptoms in both the groups with no statistically significant difference. Cognitive state was more favorable (but not significant) in the ketamine group (P > 0.5).
Conclusion:
Treatment with IV ketamine in depressed people has the same antidepressant effects as ECT treatment without any memory deficiency.
Keywords: Depression, electroconvulsive therapy, ketamine
Introduction
Major depressive disorder (MDD) was characterized by depressed mood, lack of interest and enjoyment, altered appetite and sleep pattern, anxiety, physical and mental sluggishness, low energy, feeling of worthlessness, and poor concentration. It constitutes one of the most prevalent (16%–20%) psychiatric disorders worldwide.[1] Conventionally, monoaminergic systems (norepinephrine, serotonin, and dopamine) were the focus of depression neurobiology, and all the current classes of antidepressants target these systems. Recent investigations show that glutamate plays a crucial role in pathophysiology of depression.[2,3,4]
Electroconvulsive therapy (ECT) is the fastest and most effective available therapy for MDD. It considered in patients who do not respond to antidepressant drugs or the presence of severe symptoms such as suicidal or homicidal thoughts, agitation, or stupor.[5] Although ECT is a relatively safe therapeutic strategy overall, it causes significant complications, including headache, cognitive impairment, delirium, and musculoskeletal pain, leading the psychiatrists to look for other safer antidepressant agents with rapid-onset response.[6]
Ketamine is a noncompetitive high-affinity N-methyl-D-aspartate receptor antagonist that using for general anesthesia, induction and clinical studies have shown its rapid-onset antidepressant effect.[7,8,9] The adverse effects of ketamine, such as psychotic or dissociative symptoms, are modest and transient in subanesthetic dose of 0.5 mg/kg and disappear within 1–2 h.[10,11] In addition, it reported that its antidepressant effect appears in a short time (about 2 h) and lasts for a week or longer.[12,13,14]
A study comparing the rapid antidepressant effects of ketamine and ECT found that the effects were comparable for 3 days. This suggests that ketamine may be a suitable alternative to ECT because of the rapid antidepressant effects.[15]
Data show that there is little documentation in comparing the antidepressant effects of ketamine and ECT. We designed this clinical trial to compare the speed of onset and duration of antidepressant effects of these two- antidepressant therapies and their side effects.
This study was conducted in 2010–2011 and published in 2012 in Persian language with an abstract in English.[16] It published in English to better serve English speaking researchers.
Materials and Methods
In a blinded randomized clinical trial in 2010–2011, by reviewing relatively similar studies and general patterns of clinical trials, 40 eligible patients with depression admitted to the ECT health center of Khorshid Hospital in Isfahan, Iran. Eight patients excluded because they were reluctant to participate in the study and did not match the inclusion criteria. Thirty-two patients were selected for the study. They were allocated randomly in two groups of intervention and control using block design randomization method. The objectives of the study were explained clearly to the participants, and they all signed written consent forms. The study was conducted in accordance with the ethical guidelines set by the Ethics Committee of the Isfahan University of Medical Sciences and registered in the Iranian Registry of Clinical Trials Center (IRCT201104092266N2).
Inclusion criteria were being 19–59 years old, having no history of psychosis, having no drug abuse in the past 3 months, not being pregnant or breastfeeding, having no serious physical conditions including liver, kidney, digestive, respiratory, cardiovascular, endocrine, neurologic, or hematologic diseases (based on medical counseling and paraclinical assessments), and not having untreated hypothyroidism.
Exclusion criteria were having delirium following ketamine injection or unwillingness to continue participating in the study.
Before the start of the intervention, a trained psychiatry resident evaluated the baseline depression severity and memory function in both the groups using a structured interview based on the Hamilton Depression Rating Scale (HDRS) and the Wechsler Memory Scale (WMS).
The ECT group received an intravenous (IV) injection of thiopental 3 mg/kg, for induction of general anesthesia, along with atropine 0.25 mg and succinylcholine 20 mg. Then, ECT was performed through the placement of bitemporal electrodes, and 20–100 joules of electric energy was applied (based on the patient response) using a Thymatron® DGx machine to induce generalized tonic–clonic seizures for at least 25 s. The participants’ vital signs were monitored throughout the procedure. The ketamine group received ketamine hydrochloride produced by Rotexmedica, 0.5 mg/kg in 50 cc of normal saline infused over 40 min through an IV pump or a microdrip set, while their electrocardiogram and blood pressure and oxygen saturation monitored constantly. Patients in both the groups were under the prescription of ECT or ketamine twice a week up to the complete remission of depressive symptoms.
To evaluate the changes in depression severity, researchers administered HDRS at baseline, before each treatment session, and four time points post treatment (week 1 and months 1, 2, and 3). The changes in memory functions of patients were evaluated using WMS at baseline, 1 week, and 1 month after the last treatment session. The ECT or ketamine complications evaluated before each treatment session using a checklist of ketamine and ECT side effects respectively extracted by the authors. The patients and evaluator were blinded to the method of treatment.
All patients referred back to the referring physicians for treatment follow-ups, and subsequent evaluations regarding the depressive sign and symptoms were done through telephone calls using HDRS.
The collected data were analyzed with SPSS version 18 software (Chicago: SPSS Inc. IBM Corp). The results of quantitative variables were reported as mean ± standard deviation and the qualitative variables were presented as frequency (percentage). The changes in depression severity and memory function scores were analyzed with the repeated measures ANOVA test. We used the Chi-square test to compare the frequency of complications between the study groups. The significance level for the tests was 0.05.
Results
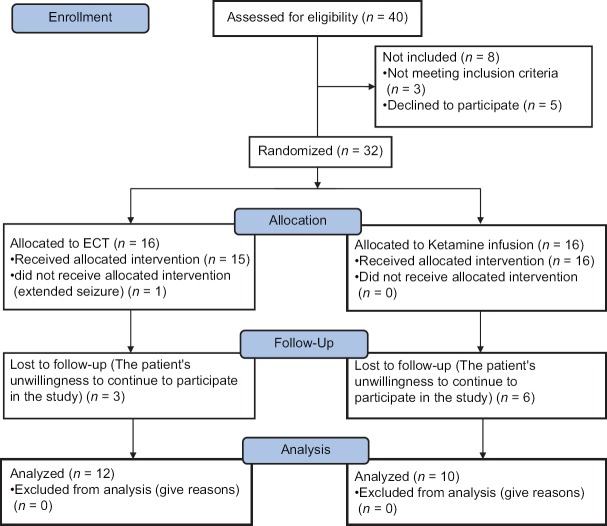
Thirty-two patients were enrolled in the study and assigned to two equal groups; however, only 12 in the ECT group and 10 in the ketamine group completed the trial [Figure 1].
Figure 1.
CONSORT 2010 flow diagram of selection, allocation, and follow-up of studied patients with depression treated with electroconvulsive therapy and intravenous ketamine
The mean age of the participants in the ECT group was 36.4 ± 14.1 years and that of the ketamine group was 41.7 ± 12.9. There was no significant difference between the two groups in age (P > 0.05). Females constituted 36% of all the participants, and there was no significant difference in terms of gender composition of the groups (ECT: n = 5, 33.3%; ketamine: n = 4, 40%; P > 0.5).
Table 1 presents the mean scores for HDRS and WMS at baseline, during the treatment, and follow-up. There was no significant difference between the two groups at different stages.
Table 1.
The results of Hamilton and Wechsler’ Memory Scales in 22 patients with depression by two methods of electroconvulsive therapy and intravenous ketamine in various stages of treatment and follow-up
| Follow-up time | Results | |||||
|---|---|---|---|---|---|---|
| Hamilton scale | Wechsler Memory Scale† | |||||
| ECT group | Ketamine group | P* | ECT group | Ketamine group | P* | |
| Before therapy | 26.1±3.8 | 24.6±2.4 | 0.3 | 50.3±8.8 | 42.9±8.2 | 0.8 |
| Session 1 therapy | 24.5±4.2 | 20.9±2.4 | 0.6 | - | - | |
| Session 2 therapy | 23.4±4.4 | 19.1±3.9 | 0.5 | - | - | |
| Session 3 therapy | 21.9±3.5 | 17.9±3.1 | 0.8 | - | - | |
| Session 4 therapy | 19±2.2 | 17.3±3.3 | 0.4 | - | - | |
| Session 5 therapy | 16.6±2.6 | 16.8±4.4 | 0.3 | - | - | |
| Session 6 therapy | 14.7±3.3 | 16.4±4.1 | 0.6 | - | - | |
| 1-week later | 13.6±3.1 | 16.9±3.3 | 0.5 | 47±8.9 | 50.4±8.4 | 0.5 |
| 1-month later | 12.9±2.6 | 19.4±1.5 | 0.3 | 47.8±9.5 | 49.8±9.9 | 0.3 |
| 2-months later | 12.5±2.9 | 21.1±1.6 | 0.1 | - | - | |
| 3-months later | 13.9±2.9 | 22.6±1.8 | 0.4 | - | - | |
The results reported as mean±1SD. *P-values computed by GLM repeated measures of ANOVA, †Wechsler Memory Scale evaluated in the patients before therapy, 1 week after and 1 month after therapy. ECT: Electroconvulsive therapy, SD: Standard deviation, GLM: General linear model
Table 2 shows the mean frequencies of the side effects reported by the patients during the treatment for depression with ECT or IV ketamine.
Table 2.
The comparison of the mean frequencies of side effects reported during the intervention in 22 patients with depression treated with electroconvulsive therapy and intravenous ketamine
| Reported side effects | Electroconvulsive group[12] | Ketamine group[10] | Chi-square test | ||
|---|---|---|---|---|---|
| n (%) | Mean±SD | n (%) | Mean±SD | ||
| Nausea | 9 (75) | 2.1±2.5 | 3 (30) | 1.9±0.8 | 0.08 |
| Headache | 12 (100) | 1.2±4.7 | 6 (60) | 1.8±1.3 | 0.029 |
| Dizziness | 11 (91.7) | 1.6±4.3 | 10 (100) | 1.7±2.7 | 1 |
| Muscle pain | 11 (91.7) | 1.3±2.8 | 0 | 0 | <0.0001 |
| Joint pain | 6 (50) | 0.9±0.75 | 0 | 0 | 0.015 |
| Orientation disorder | 4 (33.3) | 1.3±0.75± | 0 | 0 | 0.09 |
| Blurry vision | 0 | 0 | 6 (60) | 1.9±2.1 | 0.003 |
| Vertigo | 0 | 0 | 4 (40) | 1.5±1.1 | 0.029 |
| Diplopia | 0 | 0 | 4 (40) | 0.9±0.6 | 0.029 |
| Numbness of half body | 0 | 0 | 6 (60) | 1.2±1.2 | 0.003 |
| Depersonalization | 0 | 0 | 6 (60) | 1.4±1.4 | 0.003 |
SD: Standard deviation
One case of extended seizure occurred in the ECT group, and nystagmus and increased respiration and heart rate, 1 case each, occurred in the group receiving IV ketamine.
Discussion
The present study aimed to compare the efficacy of ECT versus IV ketamine infusion for controlling depressive symptoms in patients who were candidates for ECT. The comparison of HDRS score changes in the groups [Table 1] suggests that the reduction in depression scores was more rapid in the ketamine group than in the ECT group, although it gradually returned to baseline values within 3 months after cessation of the therapy. It shows that antidepressant effect of IV ketamine appears rapidly compared to ECT, but it had less durability. This means that the repeated dose of ketamine may be needed. Ghasemi et al. compared the antidepressant effects of IV ketamine and ECT; however, they followed the study participants only for 3 days, which do not seem to be enough for drawing a firm conclusion.[15]
A number of side effects occurred in the patients who received ketamine treatment. These included blurry vision, vertigo, diplopia, numbness on one side of the body, and depersonalization. It is also possible that other side effects, such as positive psychotic symptoms, might have appeared transiently or with modest severity; therefore, they were overlooked by the researchers.
Patients in the ECT group also experienced complications including headache and muscle and bone pain, which were significant and were unique to this mode of treatment.
The conclusion is that ketamine would be a suitable alternative to ECT for inducing rapid symptom relief in patients with severe depression symptoms who need urgent psychiatric care.
Memory function, as measured with the scores on WMS, displayed a decreasing pattern in the ECT group. The mean WMS scores in various time points were higher in the ketamine group compared with the ECT group. These differences, although not statistically significant, might bear clinical significance and show that ketamine infusion not only did not have adverse effects on memory (a major concern in ECT) but also had a protective effect on memory.
The results of the comparison of side effects of the two intervention methods in Table 2 showed that headache; muscle pain, and joint pain in ECT group were significantly more than ketamine group, while blurry vision, vertigo, double vision, half body numbness, and depersonalization were more common in ketamine group compared to ECT group.
Further research should aim to determine the long-term efficacy of ketamine, examine the effects of repeated doses, and evaluate the efficacy of other routs of drug administration in patients with various degrees of depression. Larger samples are needed to get results that are more reliable and draw definitive conclusions.
Conclusion
The treatment with IV ketamine in depressed people has the same antidepressant effects as the treatment with ECT, with the added benefit that it may also have a protective effect on memory.
Limitations
The main limitation of this study was the small number of patients; we are going to repeat the study with a larger number of participants.
Financial support and sponsorship
This research was financially supported by Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Hereby, we thank all the participants and the staff in ECT center in Khorshid Hospital of Isfahan University of Medical Science.
References
- 1.Sadock BJ, Sadock VA, Ruiz P. 11th ed. Vol. 1. Philaledphia: Lippincott Williams & Wilkins; 2015. Mood disorders. Synopsis of Psychiatry; p. 347. [Google Scholar]
- 2.Jaso BA, Niciu MJ, Iadarola ND, Lally N, Richards EM, Park M, et al. Therapeutic modulation of glutamate receptors in major depressive disorder. Curr Neuropharmacol. 2017;15:57–70. doi: 10.2174/1570159X14666160321123221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdallah CG, Jiang L, De Feyter HM, Fasula M, Krystal JH, Rothman DL, et al. Glutamate metabolism in major depressive disorder. Am J Psychiatry. 2014;171:1320–7. doi: 10.1176/appi.ajp.2014.14010067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdallah CG, Adams TG, Kelmendi B, Esterlis I, Sanacora G, Krystal JH, et al. Ketamine's mechanism of action: A path to rapid-acting antidepressants. Depress Anxiety. 2016;33:689–97. doi: 10.1002/da.22501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sadock BJ, Sadock VA, Ruiz P. Synopsis of Psychiatry. 11th ed. Vol. 2. Philaledphia: Lippincott Williams & Wilkins; 2015. Brain stimulation methods; p. 1067. [Google Scholar]
- 6.Sadock BJ, Sadock VA, Ruiz P. Synopsis of Psychiatry. 11th ed. Vol. 2. Philaledphia: Lippincott Williams & Wilkins; 2015. Brain stimulation methods; pp. 1071–2. [Google Scholar]
- 7.Zarate CA, Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63:856–64. doi: 10.1001/archpsyc.63.8.856. [DOI] [PubMed] [Google Scholar]
- 8.Fond G, Loundou A, Rabu C, Macgregor A, Lançon C, Brittner M, et al. Ketamine administration in depressive disorders: A systematic review and meta-analysis. Psychopharmacology (Berl) 2014;231:3663–76. doi: 10.1007/s00213-014-3664-5. [DOI] [PubMed] [Google Scholar]
- 9.Thase M. Mood disorders: Neurobiology. Kaplan and Sadock's Comprehensive Textbook of Psychiatry. In: Sadock BJ, Sadock VA, Ruiz P, editors. 9th ed. Vol. 1. Philadelphia: Lippincott Willams & Wilkins; 2009. p. 1670. [Google Scholar]
- 10.Aan Het Rot M, Collins KA, Murrough JW, Perez AM, Reich DL, Charney DS, et al. Safety and efficacy of repeated-dose intravenous ketamine for treatment-resistant depression. Biol Psychiatry. 2010;67:139–45. doi: 10.1016/j.biopsych.2009.08.038. [DOI] [PubMed] [Google Scholar]
- 11.Alberich S, Martínez-Cengotitabengoa M, López P, Zorrilla I, Núñez N, Vieta E, et al. Efficacy and safety of ketamine in bipolar depression: A systematic review. Rev Psiquiatr Salud Ment. 2017;10:104–12. doi: 10.1016/j.rpsm.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Chilukuri H, Reddy NP, Pathapati RM, Manu AN, Jollu S, Shaik AB, et al. Acute antidepressant effects of intramuscular versus intravenous ketamine. Indian J Psychol Med. 2014;36:71–6. doi: 10.4103/0253-7176.127258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Talbot JN, Geffert LM, Jorvig JE, Goldstein RI, Nielsen CL, Wolters NE, et al. Rapid and sustained antidepressant properties of an NMDA antagonist/monoamine reuptake inhibitor identified via transporter-based virtual screening. Pharmacol Biochem Behav. 2016;150-151:22–30. doi: 10.1016/j.pbb.2016.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maeng S, Zarate CA., Jr The role of glutamate in mood disorders: Results from the ketamine in major depression study and the presumed cellular mechanism underlying its antidepressant effects. Curr Psychiatry Rep. 2007;9:467–74. doi: 10.1007/s11920-007-0063-1. [DOI] [PubMed] [Google Scholar]
- 15.Ghasemi M, Kazemi MH, Yoosefi A, Ghasemi A, Paragomi P, Amini H, et al. Rapid antidepressant effects of repeated doses of ketamine compared with electroconvulsive therapy in hospitalized patients with major depressive disorder. Psychiatry Res. 2014;215:355–61. doi: 10.1016/j.psychres.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 16.Kheirabadi GR, Vafaie M, Attari A. Intravenous ketamine therapy vs. electroconvulsive therapy in depressive cases. J Isfahan Med Sch. 2012;29:1289–97. [Google Scholar]