Abstract
Background
Antimicrobial resistance (AMR) is a major public health problem. Elderly residents in long-term-care facilities (LTCFs) are frequently prescribed antibiotics, particularly for urinary tract infections. Optimizing appropriate antibiotic use in this vulnerable population requires close collaboration between NHS healthcare providers and LTCF providers.
Objectives
Our aim was to identify and quantify antibiotic prescribing in elderly residents in UK LTCFs. This is part of a wider programme of work to understand opportunities for pharmacy teams in the community to support residents and carers.
Methods
This was a retrospective longitudinal cohort study. Data were extracted from a national pharmacy chain database of prescriptions dispensed for elderly residents in UK LTCFs over 12 months (November 2016–October 2017).
Results
Data were analysed for 341536 residents in LTCFs across the four UK nations, from which a total of 544796 antibiotic prescriptions were dispensed for 167002 residents. The proportion of residents prescribed at least one antibiotic over the 12 month period varied by LTCF, by month and by country.
Conclusions
Whilst national data sets on antibiotic prescribing are available for hospitals and primary care, this is the first report on antibiotic prescribing for LTCF residents across all four UK nations, and the largest reported data set in this setting. Half of LTCF residents were prescribed at least one antibiotic over the 12 months, suggesting that there is an opportunity to optimize antibiotic use in this vulnerable population to minimize the risk of AMR and treatment failure. Pharmacy teams are well placed to support prudent antibiotic prescribing and improved antimicrobial stewardship in this population.
Introduction
Antimicrobial resistance (AMR) is a major global public health problem which could ultimately prevent the treatment of common bacterial infections.1 International as well as national efforts exist to try to deal with the issues.2 The UK Government is committed to improving the appropriate use of antibiotics in all four nations across England, Northern Ireland, Scotland and Wales, and in 2016 set a target to reduce inappropriate prescribing by 50% by the year 2020.3 Inappropriate use of antibiotics includes prescribing an antibiotic in the absence of evidence or clear rationale of a bacterial infection, and continuation of the course beyond recommended guidelines.4 National guidance for the management of common infections in primary care is published by PHE,5 and more recently by NICE.6 Research published by PHE has quantified the level of inappropriate prescribing in primary care in England as 20%,7 suggesting that levels of prescribing should be reduced by 10% to meet the Government target. This has been integrated into national targets in England.
There are 459000 residential places in long-term-care facilities (LTCFs) across England,8 16000 across Northern Ireland,9 41000 across Scotland10 and 26000 across Wales.11 The majority of residents in LTCFs are elderly and have complex healthcare needs that are exacerbated by multiple comorbidities and medication-related issues from polypharmacy.12 Nurses and carers provide the majority of long-term care for older people in UK LTCFs; they help residents to live in an environment they can call home, where quality of life matters.13 Across the UK, pharmacists (particularly those working in the community setting) support residents within LTCFs by dispensing and supplying medicines, as well as providing advice and support to carers on medicine use, storage and waste. Providing high-quality care for LTCF residents requires close collaboration between healthcare providers and LTCF managers to support both residents and carers.14 Residents in these settings are known to be prescribed higher rates of antibiotics, particularly for urinary tract infections (UTIs),15 which are frequently associated with antibiotic-resistant organisms that can lead to treatment failure and bloodstream infections. Issues can exist with diagnosis of infections, as up to half of adults over the age of 65 years old and most people with a urinary catheter will have bacteria present in the bladder without signs of an infection.16
The 2016–17 point prevalence survey (PPS) coordinated by the ECDC17 found that 6.2% of residents in LTCFs in Scotland were taking at least one antimicrobial, 10.1% in Wales and 10.3% in Northern Ireland. England did not participate in this PPS, but results from an earlier 2013 European survey found that 9.0% of residents were taking at least one antimicrobial.18 Similarly, a 2016 PPS in Australia reported that 9.7% of residents were prescribed antibiotics, most frequently for pneumonia, UTIs and skin or soft tissue infections.19 A 2011 retrospective longitudinal cohort study in England (following 7481 residents over a period of 12 months) found that annual prescriptions for antibiotics in those aged 75 years and older increased from 142/100 to 199/100 among those living in an LTCF.15
Collecting data in LTCFs to understand healthcare needs of residents and carers can be complex and challenging as these environments are residents’ homes, and not NHS healthcare settings.13 The objective of this study was to identify the scale of antibiotic prescribing in LTCFs across all four UK nations, and is part of a programme of work to identify opportunities for community pharmacists to support both residents and carers.
Methods
This was a retrospective longitudinal cohort study. Anonymized data were extracted using SQL query analyser from a national pharmacy chain database on NHS antibiotic prescriptions dispensed for residents in LTCFs across the UK for 12 months from November 2016 to October 2017. Antibiotics were defined as those listed within British National Formulary20 Chapter 5.1 (antibacterial drugs). Data fields extracted were: anonymized patient identifier, dispensed date, drug name, code, form (e.g. capsules, tablets, injection or suspension), strength, pack size, dosage directions and dispensed quantity. Days of therapy were calculated using fields of quantity dispensed and dosage instructions, and were calculable for 75.6% of antibiotics. Although data on age were not collected, the information extracted was based on dispensing services provided mainly to residential and nursing homes and will therefore primarily be aimed at elderly residents. All analysis was conducted in Microsoft Excel 2013. The study was approved by the Research Governance Board within the pharmacy chain who confirmed that ethics approval was not required as the study was based on an internal audit of anonymized data to help inform service development to the LTCF resident population serviced by the national pharmacy chain.
Results
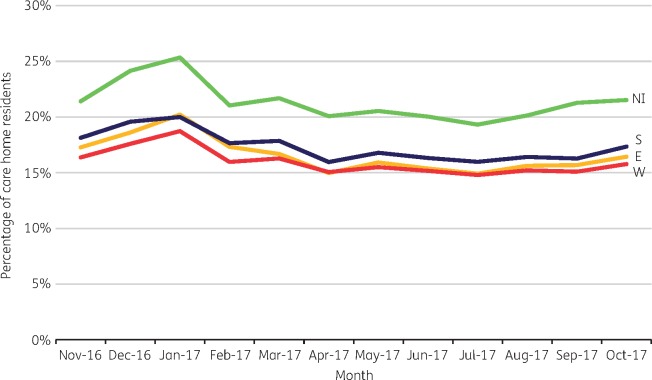
Data were analysed for 341536 residents in LTCFs across the UK (287912 in England, 28076 in Scotland, 16409 in Wales and 9139 in Northern Ireland). The percentage of residents receiving at least one antibiotic prescription during the 12 month period November 2016–October 2017 was: 56.6% in Northern Ireland, 53.2% in Scotland, 48.5% in England and 45.0% in Wales. The mean percentage of residents prescribed antibiotics each month by country (Figure 1) was 21.4% in Northern Ireland, 17.4% in Scotland, 16.6% in England and 16.0% in Wales.
Figure 1.
Mean percentage of LTCF residents prescribed antibiotics by month and country. NI, Northern Ireland; S, Scotland; E, England; W, Wales. This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
Half of the residents (52.1%) were dispensed one antibiotic drug over the 12 month period, a quarter (27.5%) were dispensed two different antibiotics, 12.9% were dispensed three and 5.1% were dispensed four (the remaining 2.4% were dispensed between 5 and 10 different antibiotics). If a resident only had amoxicillin over the 12 months then this would be classed as one drug, even if they had several prescriptions for it. The distribution of the number of antibiotic prescriptions per resident over the 12 month period is positively skewed, with a median of 2 (IQR 1–4). Of those residents taking antibiotics over the 12 month period, 38.4% had one antibiotic prescription, 21.3% had two, 12.5% had three, 7.9% had four and 19.9% had five or more antibiotic prescriptions. In total, 10561 residents (6.3%) had ≥10 antibiotic prescriptions during the 12 month period. Here, the definition of prescription would include the same antibiotic being dispensed more than once over the 12 month period (e.g. a resident having three prescriptions for amoxicillin and a further two for trimethoprim over the 12 months would be classed as having five prescriptions).
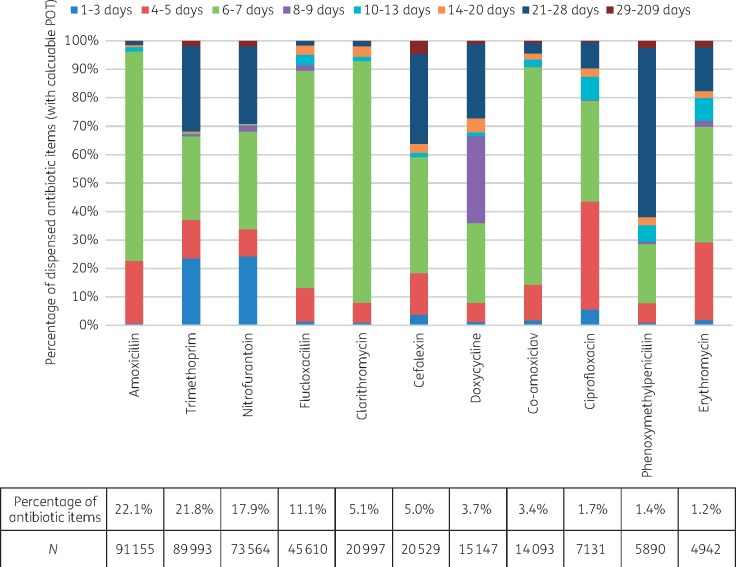
Four antibiotics (amoxicillin, trimethoprim, nitrofurantoin and flucloxacillin) accounted for 66.4% of all antibiotic prescribing. The 11 antibiotics shown in Figure 2 accounted for 92.8% of all antibiotic prescribing, of which it was possible to calculate days of therapy for 77.0% of them. Figure 2 shows the days of therapy variation for each of these antibiotics; for example, amoxicillin accounted for 22.1% of antibiotics dispensed with a calculable value for days of therapy, of which 73.6% were for 6–7 days and 22.0% for 4–5 days. Trimethoprim accounted for 21.8% of antibiotics, of which 30.0% were for 21–28 days, 29.5% for 6–7 days, 23.6% for 1–3 days and 13.4% for 4–5 days.
Figure 2.
Days of therapy by antibiotic. POT, period of treatment. Figure 2 is reproduced for England, Northern Ireland, Scotland and Wales in Figures S1–S4 (available as Supplementary data at JAC Online). This figure appears in colour in the online version of JAC and in black and white in the print version of JAC.
Discussion
Whilst the results presented herein are focused on antibiotic use, they highlight that some residents in LTCFs take multiple courses of antibiotics over a 12 month period, and that there is wide variability in days of therapy. Rates of antibiotic consumption are higher than seen in previous studies,15,17–19 although these were based on a single point in time rather than a 12 month period as seen here. Although no information was available on the reason for the antibiotic prescription from the data set used, some indication can be assumed for certain antibiotics (particularly where not broad spectrum) and, therefore, comparison can be made on appropriateness of prescription duration and variation against clinical indication and national guidelines.5,6 For antibiotics used routinely for treatment of respiratory infections, amoxicillin had a consistent dosage length of 5 or 7 days (93.6% of prescriptions), phenoxymethylpenicillin for 5–10 days was 33.5% and doxycycline for 5–10 days was 62.1%. For UTI antibiotics, trimethoprim and nitrofurantoin had wide variability, with <60% of each being for the recommended 3 or 7 days duration. For skin infections, flucloxacillin duration of 7 days accounted for 76.1% of prescriptions and a further 3.1% for 14 days. Most of the penicillin prescriptions appeared to be for prophylaxis, with 59.0% of items dispensed as 28 day courses.
Antibiotics can be given in response to unscheduled care (unplanned health or social care) which can include prescribing out of hours by healthcare professionals not normally involved in the care of those residents. Pharmacists have a role in supporting the safe and effective use of medicines in LTCFs, including promoting self-care (through homely remedy policies), helping carers to identify and deal with early signs of deterioration and, when antibiotics are prescribed, providing advice on whether they are appropriate (in line with local guidelines) and to support them being used effectively.21 In 2014 the Five Year Forward View22 was published, which aimed to promote integrated working across healthcare disciplines and sectors, in order to promote more efficient and effective care within the NHS. To support this, and enable pharmacists and their teams to spend more time delivering clinical care to patients across NHS settings (including LTCFs), the Pharmacy Integration Fund was created.23 The fund is part of a national scheme to help facilitate using pharmacists’ clinical skills further, embedding them into practice and supporting integrated care alongside other healthcare professionals. Given the acute nature of many antibiotic prescriptions, pharmacists working with LTCFs need to work alongside pharmacists within the community, providing dispensing services to these residents (although with increasing portfolio careers these can often be the same individuals, or within the same teams). Community pharmacy teams dispense acute prescriptions for antibiotics for residents, and can identify potential interactions with current medications and any known allergies. Extending the use of the summary care record by all pharmacists to provide additional information and advice to residents and carers can support the antibiotic being used effectively as part of local guidelines (including days of therapy and associated advice on use). Given the role of carers within LTCFs, there is an opportunity for pharmacy teams to work more closely with them as partners to deliver healthcare to residents, in supporting appropriate and effective use of antibiotics, including infection prevention measures such as flu vaccinations and encouraging adequate hydration to prevent UTIs.21
Limitations
Although the data reported are only from one national pharmacy chain, they are likely to be representative of the situation across the UK owing to the large sample size and inclusion of homes that are classed as independent (sole providers) as well as large national care organizations (multisite). The data are limited by being dependent on what is captured as part of the prescription dispensing process, and therefore miss further opportunities to explore the data further on appropriateness compared with diagnosis and clinical outcome. This could be an opportunity for exploration in future research, alongside looking at concurrent and sequential use of antibiotics.
Conclusions
This study provides baseline data that highlight the levels of antibiotic use across LTCFs in the UK, including multiple courses and variability in duration of treatment, identifying potential areas in which pharmacists and their teams can support both residents and carers in the appropriate and effective use of antibiotics. Following the recent focus on increasing the clinical role of pharmacists within LTCFs, there is an opportunity to consider actions to support prudent antibiotic prescribing and improved antimicrobial stewardship across the UK, and to revisit the audit at a later date to understand evidence of their impact.
Funding
Data were generated as part of the routine work of Boots UK. T. T. and A. N. are employees of Boots UK, but no additional funding was received for the writing of this paper. D. A.-O., P. H. and E. B. received no funding from Boots UK.
Transparency declarations
T. T. and A. N. are employees of Boots UK, but do not own any stocks or shares. T. T., P. H., D. A.-O. and E. B. are members of the Royal Pharmaceutical Society Antimicrobial Expert Advisory Group.
Supplementary Material
References
- 1.Public Health England. UK Five Year Antimicrobial Resistance Strategy2013 to 2018.https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/244058/20130902_UK_5_year_AMR_strategy.pdf.
- 2.Review on Antimicrobial Resistance. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations Wellcome Trust. https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf.
- 3.HM Government. Government Response to the Review on Antimicrobial Resistance2016 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/553471/Gov_response_AMR_Review.pdf.
- 4. Advisory Committee on Antimicrobial Prescribing, Resistance and Healthcare Associated Infection (APRHAI), 8th Annual Report, April 2016–March 2017 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/714000/APRHAI_Annual_Report_2016-2017_.pdf.
- 5. Managing Common Infections: Guidance for Primary Care https://www.gov.uk/government/publications/managing-common-infections-guidance-for-primary-care.
- 6.NICE. Managing Common Infections – Antimicrobial Prescribing Guidelines.https://www.nice.org.uk/guidance/indevelopment/gid-ng10050.
- 7. Davies S. Reducing inappropriate prescribing of antibiotics in English primary care: evidence and outlook. J Antimicrob Chemother 2018; 73: 833–4. [DOI] [PubMed] [Google Scholar]
- 8.Care Quality Commission. The State of Health Care and Adult Social Care in England 2017/18.https://www.cqc.org.uk/publications/major-report/state-care.
- 9.Regulation and Quality Improvement Authority, Northern Ireland. Annual Quality Report 2017–18 https://www.rqia.org.uk/RQIA/files/d9/d9ede6b4-90d5-4465-b7be-5ba4ad4f39ba.pdf.
- 10.UK Statistics Authority. Care Home Census for Adults in Scotland. Figures for 2007–2017 http://www.isdscotland.org/Health-Topics/Health-and-Social-Community-Care/Publications/2018-09-11/2018-09-11-CHCensus-Report.pdf.
- 11.StatsWales. CIW Services and Places by Setting Type and Year.https://statswales.gov.wales/Catalogue/Health-and-Social-Care/Services-for-Social-Care-and-Childrens-Day-Care/cssiwservicesandplaces-by-setting-year.
- 12. Falconer M, O’Neill D.. Profiling disability within nursing homes: a census based approach. Age Ageing 2007; 36: 209–13. [DOI] [PubMed] [Google Scholar]
- 13.National Institute for Health Research (NIHR). Enabling Research in Care Homes (ENRICH). The Care Home Sector: Home Not Hospital.http://enrich.nihr.ac.uk/page/understanding-care-homes.
- 14. Goodman C, Davies SL, Gordon AL. et al. Optimal NHS service delivery to care homes: a realist evaluation of the features and mechanisms that support effective working for the continuing care of older people in residential settings. Health Serv Deliv Res 2017; 5: 1–242. [PubMed] [Google Scholar]
- 15. Sundvall PD, Stuart B, Davis M. et al. Antibiotic use in the care home setting: a retrospective cohort study analysing routine data. BMC Geriatrics 2015; 15: 71.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NICE. NICE Guideline NG109. Urinary Tract Infection (Lower): Antimicrobial Prescribing(2018) https://www.nice.org.uk/guidance/ng109.
- 17. Ricchizzi E, Latour K, Karki T. et al. Antimicrobial use in European long-term care facilities: results from the third point prevalence survey of healthcare-associated infections and antimicrobial use, 2016 to 2017. Euro Surveill 2018; 23: pii=1800394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.European Centre for Disease Prevention and Control. Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Long-Term Care Facilities2013 https://ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/healthcare-associated-infections-point-prevalence-survey-long-term-care-facilities-2013.pdf.
- 19.Australian Commission on Safety and Quality in Healthcare. Aged Care National Antimicrobial Prescribing Survey2016 https://www.safetyandquality.gov.au/publications/aged-care-national-antimicrobial-prescribing-survey-2016/.
- 20.British Medical Association and Royal Pharmaceutical Society. British National Formulary 66 (September 2013–March 2014). London: BMJ Group, 2013.
- 21.Royal Pharmaceutical Society. The Pharmacy Contribution to Antimicrobial Stewardship 2017 https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Policy/AMS%20policy.pdf.
- 22.NHS England. NHS Five Year Forward View 2014.https://www.england.nhs.uk/publication/nhs-five-year-forward-view/.
- 23.NHS England. Pharmacy Integration Fund.https://www.england.nhs.uk/commissioning/primary-care/pharmacy/integration-fund/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.