Pheochromocytomas (PHEOs) are rare neuroendocrine tumors that arise from the chromaffin cells of the adrenal medulla, while their extra-adrenal chromaffin counterparts of the sympathetic ganglia are known as paraganglioma’s (PGLs). PHEO/PGLs oversecrete catecholamines, which can surge to enormous levels and result in paroxysmal hypertenstion, diaphoresis, pallor, and tachycardia (1, 2). Surgery remains the only curative, therapeutic option for PHEO/PGLs; however, resection bears high perioperative risks and complications (3, 4).
Numerous observational, retrospective studies have reviewed perioperative morbidity, mortality, and risks associated with surgical resection of a PHEO/PGL (4–11). Recently, Groeben et al have published a consecutive case series of 276 patients who underwent surgical exision of a PHEO/PGL. Of their 276 patients, 110 were prescribed a preoperative alpha adrenoceptor blockade, while 166 were not. Results revealed no difference in maximal intraoperative systolic pressure, excessive hypertensive episodes, or major complications between the two populations (5). In accordance with their findings, Groeben et al proposed altering the current standard practice of preoperative care – an alpha adrenoceptor blocker to prevent perioperative cardiovascular complications (1). Additionally, the report warned of the significant side effects associated with alpha adrenoceptor blockade administration, including vertigo, malaise, headache, gastrointestinal distress, and postoperative hypotension and tachycardia (5). However, Isaacs and Lee hypothesized that medicinal side effects are significantly easier to control than the potentially devastating intraoperative complications to an unblocked surgical candidate from excess catecholamine release (11), and postoperative hypotension secondary to an alpha adrenoceptor blockade has long been recognized, but is adequently controlled with hydration and if necessary, the administration of vasporessors. Furthermore, in a multicenter, retrospective analysis, Conzo et al discovered that when treated with preoperative doxazosin, only seven of their 48 patients experienced a perioperative hypertensive crisis, and just four patients experienced postoperative hypotension. While Conzo et al acknowledged that doxazosin did not prevent all intraoperative hypertensive crises; they credited the medication with limiting the duration of operative blood pressures greater than 180/90 mm Hg, and preventing major cardiovascular complications, which in turn allowed for low morbidity (6). Similarly, Livingston et al reported that preoperative phenoxybenzamine was a significant factor in achieving hemodynamic stability (8), and after Weingarten et al studied the relationship between preoperative hormonal levels and postoperative volume overload resulting in hypotension following surgical excision, they also recommended a preoperative alpha adrenoceptor blockade be given to all patients undergoing a PHEO/PGL resection (7).
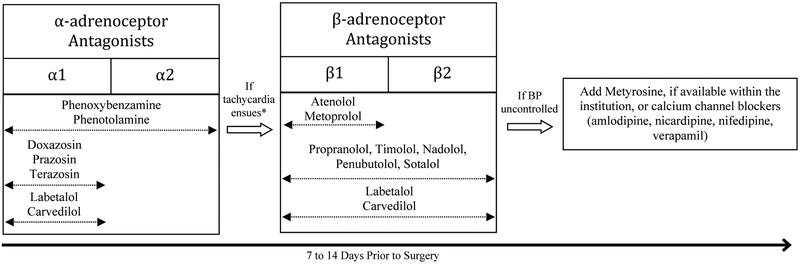
While an alpha adrenoceptor blocade is instrumental in achieving adequate blood pressure control in the operating room, its foremost goal is avoidance of a sudden release of catecholamines during daily psychological and physical stressors, as well as from various medications and minor procedures like dental work (12, 13). Inappropriately blocked PHEO/PGL patients present to surgery with at least one sign or symptom associated with excess catecholamine release, which can escalate aforementioned cardiovascular and other organ-specific complications (14). While it is imperative adrenoceptor blockade be administred, it is just as crucial that the correct medication be prescribed. Beta adrenoceptor blockers can be added to the patients regimen following catecholamine or alpha adrenoceptor-induced tachycardia (2); however, they must only be given after the inititation of an alpha adrenoceptor blocker. In a multi-institutional retrospective cohort study, Luiz et al discovered that over a third of patients were not treated according to US Endocrine Society practice guidelines (14). Of those patients, greater than 50% were not given any pharmacological blockade, and 11% of the patients were given a beta adrenoceptor blockade as initial therapy, which can precipitate a catecholamine-induced hypertensive crisis instead of protect the patient from one (14). During anesthesia and intraoperative tumor manipulation, a physician is at the ready to counteract the detrimental effects of a hypertensive crisis; however, an alpha and beta adrenoceptor blockade can act as a safeguard when the patient is not in the operating room under the care of an experienced surgical staff.
We also recognize the presence of extenuating circusmtances, which may prevent an idealistic plan for tumor removal. The rule of surgical divergence describes PHEO/PGL patients undergoing emergency procedures without a proper blockade or prior to PHEO/PGL excision (15). During these critical scenarios, physicians must remain vigilant and attempt to protect the patient from the potentially catastrophic consequences of circulating catecholamines with administration of an alpha adrenoceptor blockade throughout surgery, and with persistent blood pressure monitoring and correction when necessary. We also awknowledge that while the evidence used in the US Endocrine Society guideline is based purely on observational studies, their recommendations are founded on robust evidence favoring a preoperative alpha adrenoceptor blockade (1). Prospective studies identifying an appropriate population to forego adrenoceptor blockade administration do not exist. Therefore, to ensure the safety, protection, and well-being of patients, prolonged circulating catecholamines must be carefully, adequately, and appropriately managed with the current first line of medical care – an alpha adrenoceptor blockade. It is our experience and opinion that this current approach will ensure the Hippocratic oath “primum non noere” to its best standards and values.
Figure 1.
Preferred Blockade Administration for Preoperative PHEO/PGL Patients
BP, Blood Pressure; *Cannot be administered until after 2–3 days of alpha adrenoreceptor blockade
Acknowledgements:
This work was supported by the Eunice Kennedy Shriver National Institutue of Child Health and Human Development at the National Institutes of Health, Bethesda, Maryland, USA
Footnotes
Conflicts of Interest: All Authors declare there are no conflicts of interest
References
- 1.Lenders JW, Duh QY, Eisenhofer G, et al. Pheochromocytoma and Parangalgioma: An Endocrine Society Clinical Practice Guidline. J Clin Endocrinol Metab. 2014;99:1915–1942. [DOI] [PubMed] [Google Scholar]
- 2.Pacak. Approach to the Patient. Preoperative Management of the Pheochromocytoma Patient. J Clin Endocrinol Metab. 2007;92:4069–4079. [DOI] [PubMed] [Google Scholar]
- 3.Kazic MR, Zivaljevic VR, Milan ZB, et al. Perioperative Risk Factors, Morbidity, and Outcome of 145 Patients during Pheochromocytoma Resection. Acta Chir Belg. 2011;111:223–227. [PubMed] [Google Scholar]
- 4.Plouin PF, Duclos JM, Soppelsa F, et al. Factors Associated with Perioperative Morbidty and Mortality in Patients with Pheochromocytoma: Analysis of 165 Operations at a Single Center. J Clin Endocrinol Metab. 2011;86:1480–1486. [DOI] [PubMed] [Google Scholar]
- 5.Groeben H, Nottebaum BJ, Alesina PF, et al. Perioperative α-Receptor Blockade in Phaechromocytoma Surgery: An Observational Case Series. Br J Anaesth. 2017;118:182–189. [DOI] [PubMed] [Google Scholar]
- 6.Conzo G, Musella M, Corcioner F, et al. Role of Preoperative Adrenergic Blockade with Doxazosin on Hemodynamic Control during the Surgical Treatment of Pheochromocytoma: A Restrospective Study of 48 cases. Am Surg. 2013;79:1196–1202. [PubMed] [Google Scholar]
- 7.Weingarten TN, Welch TL, Moore TL, et al. Preoperative Levels of Catecholamines and Metanephrines and Intraoperative Hemodynamics of Patients Undergoing Pheochromocytoma and Paraganglioma Resection. Urology. 2017;100:131–138. [DOI] [PubMed] [Google Scholar]
- 8.Livingston M, Duttchen K, Thompson J, et al. Hemodynamic Stability During Pheochromocytoma Resection: Lessons Learned Over the Last Two Decades. Ann Surg Oncol. 2015;22:4175–4180. [DOI] [PubMed] [Google Scholar]
- 9.Brunaud L, Boutami M, Nbuyen-Thi PL, et al. Both Preoperative Alpha and Calcium Channel Blockade Impact Intraoperative Hemodynamic Stability Similarly in the Management of Pheochromocytoma. Surgery. 2014;156:1410–1418. [DOI] [PubMed] [Google Scholar]
- 10.Newell KA, Prinz RA, Brooks MH, et al. Plasma Catecholamine Changes During Excision of Pheochromocytoma. Surgery. 1988;104:1064–1073. [PubMed] [Google Scholar]
- 11.Isaacs M, Lee P. Preoperative Alpha-Blockade in Phaechromocytoma and Paragangliomas: Is it Always Necessary? Clin Endocrinol. 2017;86:309–314. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed A Perioperative Management of Pheochromocytoma: Anaesthetic Implications. J Pak Med Assoc. 2007;57:140–146. [PubMed] [Google Scholar]
- 13.Horton WB, Frey LM, Hawkins UA, et al. Pheochromocytoma Presenting as Acute Non-ST Elevation Myocardial Infarction Following Elective Hysterectomy. J Miss State Med Assoc. 2015;56:4–6. [PubMed] [Google Scholar]
- 14.Luiz HV, Tanchee MJ, Pavaltou MG, et al. Are Patients with Hormonally Functional Phaechromocytoma and Paraganglioma Initially Receiving a Proper Adrenoceptor Blockade? A Retrospective Cohort Study. Clin Endocrinol. 2016;85:62–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pacak. Pheochromocytoma Resection: The Rule of Surgical Divergence. AACE Clin Case Rep. 2016; 2:e78–e79. [Google Scholar]