Abstract
Background
Multiple‐micronutrient (MMN) deficiencies often coexist among women of reproductive age in low‐ to middle‐income countries. They are exacerbated in pregnancy due to the increased demands, leading to potentially adverse effects on the mother and developing fetus. Though supplementation with MMNs has been recommended earlier because of the evidence of impact on pregnancy outcomes, a consensus is yet to be reached regarding the replacement of iron and folic acid supplementation with MMNs. Since the last update of this Cochrane review, evidence from a few large trials has recently been made available, the inclusion of which is critical to inform policy.
Objectives
To evaluate the benefits of oral multiple‐micronutrient supplementation during pregnancy on maternal, fetal and infant health outcomes.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (11 March 2015) and reference lists of retrieved articles and key reviews. We also contacted experts in the field for additional and ongoing trials.
Selection criteria
All prospective randomised controlled trials evaluating MMN supplementation with iron and folic acid during pregnancy and its effects on the pregnancy outcome were eligible, irrespective of language or the publication status of the trials. We included cluster‐randomised trials, but quasi‐randomised trials were excluded.
Data collection and analysis
Two review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy. The quality of the evidence was assessed using the GRADE approach.
Main results
Nineteen trials (involving 138,538 women) were identified as eligible for inclusion in this review but only 17 trials (involving 137,791 women) contributed data to the review. Fifteen of these 17 trials were carried out in low and middle‐income countries and compared MMN supplements with iron and folic acid versus iron with or without folic acid. Two trials carried out in the UK compared MMN with a placebo.
MMN with iron and folic acid versus iron, with or without folic acid (15 trials): MMN resulted in a significant decrease in the number of newborn infants identified as low birthweight (LBW) (average risk ratio (RR) 0.88, 95% confidence interval (CI) 0.85 to 0.91; high‐quality evidence) or small‐for‐gestational age (SGA) (average RR 0.92, 95% CI 0.86 to 0.98; moderate‐quality evidence). No significant differences were shown for other maternal and pregnancy outcomes: preterm births (average RR 0.96, 95% CI 0.90 to 1.03; high‐quality evidence), stillbirth (average RR 0.97, 95% CI 0.87, 1.09; high‐quality evidence), maternal anaemia in the third trimester (average RR 1.03, 95% CI 0.85 to 1.24), miscarriage (average RR 0.91, 95% CI 0.80 to 1.03), maternal mortality (average RR 0.97, 95% CI 0.63 to 1.48), perinatal mortality (average RR 1.01, 95% CI 0.91 to 1.13; high‐quality evidence), neonatal mortality (average RR 1.06, 95% CI 0.92 to 1.22; high‐quality evidence), or risk of delivery via a caesarean section (average RR 1.04; 95% CI 0.74 to 1.46).
A number of prespecified, clinically important outcomes could not be assessed due to insufficient or non‐available data. Single trials reported results for: very preterm birth < 34 weeks, macrosomia, side‐effects of supplements, nutritional status of children, and congenital anomalies including neural tube defects and neurodevelopmental outcome: Bayley Scales of Infant Development (BSID) scores. None of these trials reported pre‐eclampsia, placental abruption, premature rupture of membranes, cost of supplementation, and maternal well‐being or satisfaction.
When assessed according to GRADE criteria, the quality of evidence for the review's primary outcomes overall was good. Pooled results for primary outcomes were based on multiple trials with large sample sizes and precise estimates. The following outcomes were graded to be as of high quality: preterm birth, LBW, perinatal mortality, stillbirth and neonatal mortality. The outcome of SGA was graded to be of moderate quality, with evidence downgraded by one for funnel plot asymmetry and potential publication bias.
We carried out sensitivity analysis excluding trials with high levels of sample attrition (> 20%); results were consistent with the main analysis except for the findings for SGA (average RR 0.91, 95% CI 0.84 to 1.00). We explored heterogeneity through subgroup analyses by maternal height and body mass index (BMI), timing of supplementation and dose of iron. Subgroup differences were observed for maternal BMI for the outcome preterm birth, with significant findings among women with low BMI. Subgroup differences were also observed for maternal BMI and maternal height for the outcome SGA, indicating a significant impact among women with higher maternal BMI and height. The overall analysis of perinatal mortality, although showed a non‐significant effect of MMN supplements versus iron with or without folic acid, was found to have substantial statistical heterogeneity. Subgroup differences were observed for timing of supplementation for this outcome, indicating a significantly higher impact with late initiation of supplementation. The findings between subgroups for other primary outcomes were inconclusive.
MMN versus placebo (two trials): A single trial in the UK found no clear differences between groups for preterm birth, SGA, LBW or maternal anaemia in the third trimester. A second trial reported the number of women with pre‐eclampsia; there was no evidence of a difference between groups. Other outcomes were not reported.
Authors' conclusions
Our findings support the effect of MMN supplements with iron and folic acid in improving some birth outcomes. Overall, pregnant women who received MMN supplementation had fewer low birthweight babies and small‐for‐gestational‐age babies. The findings, consistently observed in several systematic evaluations of evidence, provide a basis to guide the replacement of iron and folic acid with MMN supplements containing iron and folic acid for pregnant women in low and middle‐income countries where MMN deficiencies are common among women of reproductive age. Efforts could focus on the integration of this intervention in maternal nutrition and antenatal care programs in low and middle‐income countries.
Keywords: Female; Humans; Pregnancy; Dietary Supplements; Drug Interactions; Folic Acid; Folic Acid/administration & dosage; Iron, Dietary; Iron, Dietary/administration & dosage; Micronutrients; Micronutrients/administration & dosage; Micronutrients/adverse effects; Micronutrients/deficiency; Pregnancy Complications; Pregnancy Complications/therapy; Pregnancy Outcome; Randomized Controlled Trials as Topic
Multiple‐micronutrient supplementation for women during pregnancy
What is the issue?
In low‐ and middle‐income countries, many women have poor diets and are deficient in nutrients and micronutrients which are required for good health. Micronutrients are vitamins and minerals that are needed by the body in very small quantities but are important for normal functioning, growth and development. During pregnancy, these women often become more deficient, with the need to provide nutrition for the baby too, and this can impact on their health and that of their babies.
Why is this important?
Combining multiple micronutrients has been suggested as a cost‐effective way to achieve multiple benefits for women during pregnancy. Micronutrient deficiencies are known to interact and a greater effect may be achieved by multiple supplementation rather than single‐nutrient supplementation, although interactions may also lead to poor absorption of some of the nutrients. High doses of some nutrients may also cause harm to the mother or her baby.
What evidence did we find?
We searched Cochrane Pregnancy and Childbirth's Trials Register (11 March 2015). This systematic review included 19 trials involving 138,538 women, but only 17 trials involving 137,791 women contributed data. The included trials compared pregnant women who supplemented their diets with multiple micronutrients with iron and folic acid with pregnant women who received a placebo or supplementation with iron, with or without folic acid. Overall, pregnant women who received multiple‐micronutrient supplementation had fewer low birthweight babies and small‐for‐gestational‐age babies than pregnant women who received only iron, with or without folic acid. The evidence for the main outcomes was found to be of high quality.
What does this mean?
These findings, consistently observed in several other systematic reviews of evidence, provide a strong basis to guide the replacement of iron and folic acid with multiple‐micronutrient supplements for pregnant women in low‐ and middle‐income countries countries where multiple‐micronutrient deficiencies are prevalent among women.
Summary of findings
Summary of findings for the main comparison.
Multiple micronutrients compared with control (iron and/or folic acid) for women during pregnancy
| Multiple micronutrients compared with control (iron and/or folic acid) for women during pregnancy | ||||||
| Patient or population: Pregnant women Settings: Trials took place in Bangladesh (2), Burkina Faso, China (2), Guinea‐Bissau, India, Indonesia (3), Mexico, Nepal (2), Niger, Pakistan, Tanzania and Zimbabwe. Intervention: Multiple micronutrients Comparison: Control (iron with or without folic acid) | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Median control group risk (iron and/or folic acid) | Multiple micronutrients | |||||
| Preterm births | Moderate | average RR 0.96 (0.90 to 1.03) | 90892 (15 RCTs) | ⊕⊕⊕⊕ HIGH | Denominators have been taken from individual trial reports or from a series of articles published in the FNB supplement (Fall 2009). Where different denominators are stated in different reports, we have taken the larger. Both the participant totals and the median control group risk are for illustrative purposes only. In the majority of the trials in this review, the final risk ratio presented will not correspond with raw event and participant data due to adjustments made for the effects of cluster design. |
|
| 183 per 1000 | 176 per 1000 (163 to 187) | |||||
| Small‐for‐gestational age | Moderate | average RR 0.92 (0.86 to 0.98) | 67036 (14 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 118 per 1000 | 105 per 1000 (98 to 113) | |||||
| Low birthweight | Moderate | average RR 0.88 (0.85 to 0.91) | 70044 (15 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 136 per 1000 | 120 per 1000 (117 to 124) | |||||
| Perinatal mortality | Moderate | average RR 1.01 (0.91 to 1.13) | 94780 (12 RCTs) | ⊕⊕⊕⊕ HIGH 2 | ||
| 40 per 1000 | 37 per 1000 (34 to 40) | |||||
| Stillbirths | Moderate | average RR 0.97 (0.87 to 1.09) | 98808 (15 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 31 per 1000 | 28 per 1000 (26 to 30) | |||||
| Neonatal mortality | Moderate | average RR 1.06 (0.92 to 1.22) | 83103 (11 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 31 per 1000 | 30 per 1000 (28 to 33) | |||||
| *The basis for the assumed risk is the median control group risk. This rate has been calculated from event and participant raw data, where available. If we found no raw event and participant data in published reports, these trials were not included in the calculation of the median control group risk. We have labelled this risk moderate because it is the median of a range of control group rates. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the control group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Statistical heterogeneity I² = 43%. We have not downgraded evidence for heterogeneity. There is evidence of funnel plot asymmetry for this outcome (‐1).
2Statistical heterogeneity I² = 45%. We have not downgraded evidence for heterogeneity.
Background
Description of the condition
Micronutrient deficiencies are common among women of reproductive age (15 to 49 years of age) (Black 2013). Women in low‐ and middle‐income countries often have limited intake of animal products, fruits, vegetables and fortified foods resulting in multiple‐micronutrient (MMN) deficiencies (FAO/WHO 2004; Huffman 1998). Pregnant women are at an increased risk of multiple deficiencies. These deficiencies are exacerbated during pregnancy because of the increased requirements of the growing fetus, placenta and maternal tissues. An inability to fulfil the increased requirements/demands results in potentially adverse effects on the mother and the fetus (Berti 2011).
Anaemia due to iron deficiency is one of the most prevalent micronutrient deficiencies globally. According to 2011 estimates, the worldwide prevalence of anaemia in pregnant women was 38% (95% confidence interval 33% to 43%), translating into 32 (28 to 36) million pregnant women globally (Stevens 2013). More than 50% of these cases were due to iron deficiency in regions where fewer other causes were present. The majority of these women live in south Asia, and central and west Africa (Stevens 2013). Anaemia during pregnancy has been found to be associated with increased risk of infants with low birthweight (LBW) (Haider 2013). It is also associated with an increased risk of maternal mortality (Murray‐Kolb 2013). Vitamin A deficiency is another important nutritional deficiency that leads to night blindness. According to the global estimates for the time period between 1995 and 2005, vitamin A deficiency measured using night blindness and low serum retinol levels affected 9.8 million (95% CI 8.7 to 10.8 million) and 19.1 million pregnant women (95% CI 9.30 to 29.0 million), respectively. This corresponds to 7.8% and 15.3% of pregnant women in populations at risk of vitamin A deficiency globally (WHO 2009). Deficiency of vitamin A was indicated to be associated with poor birth and mortality outcomes; however, supplementation with vitamin A during pregnancy has demonstrated no beneficial effect on these outcomes (Edmond 2012; Tielsch 2008).
In the past decade, deficiency of vitamin D has also emerged as an important nutritional problem as women of reproductive age and those pregnant have been found to have low levels of vitamin D. High prevalence has not only been reported in studies conducted in low‐income countries but also from high‐income countries (Datta 2002; Ginde 2010; Sachan 2005). Iodine deficiency is also common among pregnant women. National surveys in several countries found lower than normal urinary iodine levels in pregnant women. The median urinary iodine level in a nationally representative sample of pregnant women in Nepal was reported to be 134 mcg/L (Benoist 2008), indicating insufficient iodine intake (Andersson 2007). Severe iodine deficiency during pregnancy results in pregnancy loss, mental retardation and cretinism (Dunn 1993). Although severe deficiency is now rare, mild to moderate deficiency continues to be a problem (Andersson 2007).
Deficiencies of other micronutrients are also common among pregnant women. According to the 2012 estimates, around 17% of the world’s population have reduced dietary intake of zinc (Wessells 2012). Zinc deficiency has been associated with complications of pregnancy and delivery such as pre‐eclampsia, premature rupture of membranes, congenital abnormalities in some studies (Black 2001; Caulfield 1998). However, a review of trials of zinc supplementation showed a reduction in the risk of preterm birth only (Hess 2009; Ota 2015). Folic acid deficiency can lead to haematological consequences and congenital malformations; however, association with other birth outcomes is equivocal (Black 2001; De‐Regil 2010). Concurrent deficiencies have also been reported in studies conducted among pregnant women (Jiang 2005; Pathak 2004). These include deficiencies of vitamins A, D, E, riboflavin, B6, B12, folic acid, iron and zinc. Deficiencies of other minerals such as magnesium, selenium, copper and calcium have also been associated with complications of pregnancy, childbirth or fetal development (Black 2001).
Description of the intervention
The World Health Organization (WHO) currently recommends iron and folic acid supplementation for women during pregnancy as part of the routine antenatal care (WHO 2012). The recommended dose of iron ranges from 30 mg to 60 mg. In areas where anaemia is a severe public health problem, defined as a prevalence of 40% or higher; a daily dose of 60 mg of iron is preferred. The standard dose of 60 mg of iron was first recommended in 1959 and was based on maternal requirements during pregnancy (WHO 1959). Despite its provision as part of national antenatal care programs for the last few decades in most low and middle‐income countries, the compliance with the supplement is low. The gastrointestinal side‐effects including constipation, nausea, vomiting, and diarrhoea are the most common complaints among women consuming high dose of iron (Oriji 2011; Seck 2008).
Supplementation with iron and folic acid during pregnancy has been found to be associated with reduction in the risk of maternal anaemia and infants with LBW (Haider 2013; Pena‐Rosas 2015). To overcome other possible maternal micronutrient deficiencies, the United Nations Children's Fund (UNICEF), United Nations University (UNU) and the WHO, in 1999, agreed on the composition of a proposed multiple‐micronutrient (MMN) tablet (UNICEF 1999). This UNIMMAP tablet provides one recommended daily allowance of vitamin A, vitamin B1, vitamin B2, niacin, vitamin B6, vitamin B12, folic acid, vitamin C, vitamin D, vitamin E, copper, selenium and iodine with 30 mg of iron and 15 mg of zinc for pregnant women. In contrast to the WHO recommendation, a lower dose of iron was recommended as the absorption of iron was expected to be enhanced due to vitamin C, vitamin A, and riboflavin, and given that the majority of pregnant women suffer from mild anaemia and the potential side‐effects associated with higher doses of iron.
How the intervention might work
Vitamins and minerals play critical roles in cellular metabolism, growth and maintenance of normal functioning of the human body. These are also important in many enzymatic processes, signal transduction and transcription pathways (McArdle 1999; WHO 2004). Deficiencies of these micronutrients rarely exist in isolation. Additionally, because of their role at various levels in the biological pathways, it is difficult to assign a clinical or pre‐clinical condition to the deficiency of a single micronutrient (McArdle 1999). Micronutrient deficiencies are also known to interact. Combining MMN in a single delivery mechanism has been suggested as a cost‐effective way to achieve multiple benefits.
Why it is important to do this review
The interest of the research community globally in eliminating these deficiencies is because of their significant impact on the health of the women and infants. The health effects during the fetal life may also have consequences later as an adult. Several trials have demonstrated that supplementation with MMN during pregnancy reduces the risk of micronutrient deficiencies (Haider 2012). The findings of the individual trials regarding the benefit on other maternal and pregnancy outcomes are inconsistent as the individual studies may not have statistical power to evaluate statistically significant effects on these outcomes. Several meta‐analyses have systematically reviewed and synthesised the evidence of the effect of supplementation with these micronutrients, with the first such synthesis of evidence being an earlier version of this Cochrane review (Bhutta 2012; Haider 2006; Haider 2011; Haider 2012; Kawai 2011; Ramakrishnan 2012a). On the basis of the evidence, supplementation with MMN during pregnancy has been recommended (Bhutta 2008; Bhutta 2013). However, a consensus is yet to be reached at regarding the replacement of iron and folic acid supplementation with MMN. Since the last update of this Cochrane review (Haider 2012), evidence from a few large trials has recently been made available, inclusion of which is critical to inform global policy.
This review updates a previously published Cochrane review on MMN supplementation during pregnancy that had demonstrated positive effect of supplementation on birth outcomes (Haider 2012). The effects of supplementation with individual micronutrients during pregnancy have been evaluated in other Cochrane reviews. The effect of MMN supplementation in HIV‐infected pregnant women has been evaluated in another Cochrane review (Siegfried 2012).
Objectives
To evaluate the benefits of oral multiple‐micronutrient (MMN) supplementation during pregnancy on maternal, fetal and infant outcomes.
Methods
Criteria for considering studies for this review
Types of studies
All prospective randomised controlled trials evaluating multiple micronutrient (MMN) supplementation during pregnancy and its effects on the pregnancy outcome were eligible, irrespective of language or publication status of the trials. We included cluster‐randomised trials, but quasi‐randomised trials were excluded.
Types of participants
Pregnant women. There was no limit on the length of gestation at the time of enrolment in the study. HIV‐infected pregnant women were excluded from the review as this population is at a greater risk of nutritional disorders compared to uninfected women. We also excluded studies recruiting women at high risk of nutritional disorders for other reasons. The effect of MMN supplementation in HIV‐infected pregnant women has been evaluated in another Cochrane review (Siegfried 2012).
Types of interventions
Since WHO recommends use of iron folic acid supplementation in women during pregnancy as a part of routine antenatal care, we evaluated the effect of MMN supplementation with iron and folic acid in pregnant women versus supplementation with iron, with or without folic acid. Studies comparing the outcomes of providing pregnant women with MMN supplements with iron and folic acid compared to placebo was also included
We evaluated the effects of micronutrients that were different in the two groups and not any co‐interventions. Trials that used fewer than three micronutrients in the intervention group were excluded regardless of their outcomes. There were no limits on the duration of supplementation.
The following specific comparisons were included in the review.
Multiple micronutrients with iron and folic acid versus control (iron with or without folic acid)
Multiple micronutrients versus control (placebo)
The review focuses on daily oral supplements; trials examining parenteral MMN or food fortification with MMN are not included.
Types of outcome measures
Primary outcomes
Preterm births (births before 37 weeks of gestation)
Small‐for‐gestational age (SGA) (as defined by the authors of the trials)
Low birthweight (LBW) (birthweight less than 2500 g)
Perinatal mortality
Stillbirths
Neonatal mortality
Secondary outcomes
Maternal anaemia (third trimester haemoglobin (Hb) < 110 g/L)
Maternal mortality
Miscarriage (loss of pregnancy before 28 weeks of gestation)
Premature rupture of membranes
Pre‐eclampsia
Mode of delivery: caesarean section (not prespecified)
Macrosomia (not prespecified)
Placental abruption
Very preterm births (births before 34 weeks of gestation)
Neurodevelopmental delay (assessed using Bayley Scale of Infant Development (BSID) at six and 12 months of age)
Nutritional status of children (stunting, wasting and underweight at six, 12 and 24 months of age)
Cost of supplementation
Side‐effects of MMN supplements
Congenital anomalies (including neural tube defects)
Maternal well‐being or satisfaction
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (11 March 2015).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE, Embase and CINAHL, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
Searching other resources
We searched reference lists of retrieved articles and key reviews. We contacted experts in the field for additional and ongoing trials.
We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous version of this review, seeHaider 2012.
For this update, the following methods were used for assessing the reports that were identified as a result of the updated search.
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we planned to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Assessment of the quality of the evidence using the GRADE approach
For this update, the quality of the evidence was assessed using the GRADE approach as outlined in the GRADE Handbook. We assessed the quality of the body of evidence relating to the following outcomes for the comparison of MMN versus iron and folic acid supplements:
Preterm births
Small‐for‐gestational age (SGA)
Low birthweight (LBW)
Perinatal mortality
Stillbirths
Neonatal mortality
We used the GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014) in order to create a 'Summary of findings' table. A summary of the intervention effect and a measure of quality for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence was downgraded from 'high quality' by one level for serious limitations (or by two levels for very serious), depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias. We did not downgrade evidence for heterogeneity with an I² value of less than 60%, though we have noted moderate heterogeneity in the footnotes of the 'Summary of findings' table.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
We used the mean difference if outcomes were measured in the same way between trials. In future updates as appropriate, we plan to use the standardised mean difference to combine trials that measure the same outcome, but use different methods.
Unit of analysis issues
Cluster‐randomised trials
We included cluster‐randomised trials in the analyses along with individually‐randomised trials. We extracted cluster‐adjusted effect estimates with their confidence intervals, which were analysed along with individually‐randomised trials using the generic inverse variance method.
Trials with multiple intervention groups
For trials with multiple intervention groups, we selected one pair of interventions and excluded the others. This is one approach recommended by the Cochrane Handbook [16.5.4].
Trials with more than two intervention groups were included in the analysis after selecting the comparison groups (intervention and control groups) that satisfied the "types of intervention" criterion and were relevant to the review. For Christian 2003, data for group 4 (MMN group with iron and folic acid) versus group 2 (control group iron with or without folic acid) were included. Groups 1 (folic acid with vitamin A) and 5 (vitamin A only) were not included since they did not satisfy the inclusion criterion of the review. Further, group 3 (iron, folic acid, vitamin A, and zinc) did not include the majority of micronutrients being considered for inclusion in a MMN supplement for pregnant women and was also not comparable to the UNIMMAP formulation proposed by UNICEF, UNU, and WHO. For Kaestel 2005, groups 1 (MMN with iron and folic acid) and group 3 (iron and folic acid) were included in the review. The group with one RDA was selected since the MMN supplement in group 1 was comparable to the UNIMMAP formulation. For Lui 2013, data for groups 3 (MMN with iron and folic acid) versus group 2 (iron and folic acid) fit the types of intervention criterion of the review and were included in the analyses. Similarly, data for the comparison of groups 3 (MMN with iron and folic acid) versus 2 (iron and folic acid) were included for Zeng 2008. Group 1 in both Lui 2013 and Zeng 2008 had received folic acid only and did not satisfy the control definition of the review.
If more than two intervention groups had met the eligibility criteria, we would have combined groups to create a single pair‐wise comparison [16.5.4] the Cochrane Handbook.
Dealing with missing data
For included studies, we noted levels of attrition. We assessed the impact of including studies with high levels of missing data (> 20%) in the overall assessment of treatment effect by using sensitivity analysis. For all outcomes, analyses were carried out, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if an I² was greater than 30% and either a Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. If we identified substantial heterogeneity (above 30%), we explored it by pre‐specified subgroup analysis.
Assessment of reporting biases
Where there are 10 or more studies in the meta‐analysis, we investigated reporting biases (such as publication bias) using funnel plots. We assessed funnel plot asymmetry visually.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar.
If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average range of possible treatment effects, and we discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we did not combine trials. If we used random‐effects analyses, the results were presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
If we identified substantial heterogeneity, we investigated it using subgroup analyses and sensitivity analyses. We considered whether an overall summary was meaningful, and if it was, we used random‐effects analysis to produce it.
We carried out the following subgroup analyses.
Timing of supplementation (categorised as either before or after 20 weeks of gestation)
Dose of iron in the MMN and control supplements (30 mg versus 60 mg of iron)
Baseline nutritional status of the mother (including body mass index (BMI) and height)
We assessed subgroup differences by interaction tests available within RevMan (RevMan 2014). We reported the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Sensitivity analysis
We carried out sensitivity analyses to explore the effect of trial quality assessed by high attrition rates, with poor quality studies being excluded from the analyses in order to assess whether this made any difference to the overall result.
Results
Description of studies
Results of the search
For the 2015 update, 81 new reports were assessed for inclusion. We included two new trials in this update (Lui 2013; West 2014).
Nineteen trials (involving 138,538 women) were identified as eligible for inclusion in this review but only 17 trials (involving 137,791 women) contributed data to the review. We excluded 97 trials. Two trials are in the Studies awaiting classification section (Ashorn 2015; Gathwala 2012). We have contacted authors to see if separate analyses for HIV‐ women are available in one trial (Ashorn 2015) and are seeking clarification on missing group denominators in the second trial (Gathwala 2012). There are seven ongoing trials (Biggs 2011; Dewey 2011; Hirschberg 2014; Moore 2011; Mridha 2014; Ramakrishnan 2012; Tu 2013). SeeCharacteristics of ongoing studies for more information.
Included studies
A total of 19 trials (involving 138,538 women) were identified as eligible for inclusion in this review. Of these, two studies (Hininger 2004; Sood 1975) either did not report outcomes that were of interest in this review or presented data in a format that precluded their inclusion. Hence, these studies did not contribute data to the analyses. A total of 137,791 women participated in the remaining 17 included trials (Bhutta 2009a; Brough 2010; Christian 2003; Fawzi 2007; Friis 2004; Kaestel 2005; Lui 2013; Osrin 2005; Ramakrishnan 2003; Roberfroid 2008; SUMMIT 2008; Sunawang 2009; Theobald 1937; Tofail 2008; West 2014; Zagre 2007; Zeng 2008), of which seven were cluster‐randomised (Bhutta 2009a; Christian 2003; SUMMIT 2008; Sunawang 2009; West 2014; Zagre 2007; Zeng 2008). Three trials were conducted in developed countries (Brough 2010; Hininger 2004; Theobald 1937). Most of the outcomes were defined in the same way across different trials except for anaemia for which different cut‐offs were used in two trials (Fawzi 2007; Zeng 2008). See the Characteristics of included studies table for further details of included studies.
Participants
The 17 included trials contributing data to the analysis included 137,791 pregnant women at varying gestational stages, ranging from early pregnancy to 36 weeks of gestation. Pregnant women with a haemoglobin (Hb) of less than 80 g/L, with a serious medical condition or a complication of pregnancy such as cardiac disease, pneumonia and threatened abortion were not eligible for inclusion in the trials. One trial (Friis 2004) included a subgroup of pregnant women who were HIV‐1 infected but the data for this subgroup were not included in the review. Baseline characteristics of the participants in the intervention and the control groups were comparable in the included trials except for minor differences in five trials (Christian 2003; Friis 2004; Ramakrishnan 2003; Roberfroid 2008; Zagre 2007); and these characteristics were not reported in one trial (Theobald 1937). In Friis 2004, a higher proportion of primigravidae were found in the placebo group. In Ramakrishnan 2003, there was a higher proportion of single mothers and a lower mean BMI in the intervention group. In Christian 2003, more participants in the control group belonged to a specific ethnic background and owned land. In Roberfroid 2008, the Hb level was lower in the intervention group and the BMI was lower in the control group. In Zagre 2007, the intervention group had more households and preventive measures against malaria, whereas the placebo group had less education and more poverty.
Intervention
Fourteen trials assessed MMN supplementation versus control (Bhutta 2009a; Christian 2003; Fawzi 2007; Kaestel 2005; Lui 2013; Osrin 2005; Ramakrishnan 2003; Roberfroid 2008; SUMMIT 2008; Sunawang 2009; Tofail 2008; West 2014; Zagre 2007; Zeng 2008). Two trials also had a component of nutritional education along with supplementation (Bhutta 2009a; Zagre 2007). Three supplementation trials assessed MMN against a placebo (Brough 2010; Fawzi 2007; Friis 2004); however, in Fawzi 2007 and Friis 2004, all participants received iron and folic acid supplements. In Brough 2010, participants not taking folic acid were asked to take it daily.
The composition of the MMN supplement was different in all included trials. Fourteen trials included iron and folic acid in the MMN supplement (Bhutta 2009a; Brough 2010; Christian 2003; Kaestel 2005; Lui 2013; Osrin 2005; Ramakrishnan 2003; Roberfroid 2008; SUMMIT 2008; Sunawang 2009; Tofail 2008; West 2014; Zagre 2007; Zeng 2008). All supplements were given orally to the pregnant women throughout pregnancy from the time of enrolment. However, the duration of supplementation varied because the time of enrolment differed across the trials. Seven trials enrolled participants in the first trimester of pregnancy (Brough 2010; Christian 2003; Ramakrishnan 2003; Roberfroid 2008; Tofail 2008; West 2014; Zagre 2007). One trial enrolled participants with a gestation of less than 20 weeks (Lui 2013), and another less than 28 weeks (Zeng 2008). Three trials enrolled participants in the second trimester (Bhutta 2009a; Osrin 2005; Sunawang 2009), one trial enrolled women in both second and third trimester (Friis 2004), while three trials enrolled pregnant women who were less than 37 weeks' gestation (Fawzi 2007; Kaestel 2005; SUMMIT 2008). Supplementation was given until delivery in 10 of the included trials (Bhutta 2009a; Brough 2010; Lui 2013; Friis 2004; Kaestel 2005; Osrin 2005; Ramakrishnan 2003; Tofail 2008; Zagre 2007; Zeng 2008). Supplementation continued until four weeks after delivery in one trial (Sunawang 2009), six weeks after delivery in the Fawzi 2007 trial, 12 weeks after delivery in four trials (Christian 2003; Roberfroid 2008; SUMMIT 2008; West 2014), and for five weeks after a stillbirth or miscarriage (Christian 2003).
Excluded studies
Ninety‐seven trials were excluded from the review. Briefly, 36 trials evaluated the effects of a single or two micronutrients or compounds (Beazley 2002; Bergmann 2006; Carrasco 1962; Caulfield 1999; Caulfield 1999a; Chames 2002; Goldenberg 1995; Gopalan 2004; Hillman 1963; Holly 1955; Hossain 2014; Hunt 1983; Hunt 1984; Hunt 1985; Iannotti 2008; Lucia 2007; Ma 2008; Malvasi 2014; Marya 1987; Mathan 1979; Merialdi 1999; Muslimatun 2001a; Muslimatun 2001b; Ochoa‐Brust 2007; Raqib 2013; Robertson 1991; Sachdeva 1993; Sagaonkar 2009; Salzano 2001; Schmidt 2001; Schmidt 2002; Semba 2000; Semba 2001; Suharno 1993; Suprapto 2002; Tanumihardjo 2002; Zavaleta 2000). Twelve trials did not satisfy the study design criteria (Aguayo 2005; Biswas 1984; Kubik 2004; Kynast 1986; Itam 2003; Menon 1962; Patimah 2013; Park 1999; People's League 1946; Sun 2010; Thauvin 1992; Wijaya‐Erhardt 2014), and five trials studied HIV‐positive women (Fawzi 1998; Khavari 2014; Merchant 2005; Olofin 2014; Webb 2009) and hence were excluded from the review. In four trials, MMN supplements were given to both groups of patients (Asemi 2014; Dawson 1987; Dawson 1998; Magon 2014). Czeizel 1996, ICMR 2000, Cooper 2012, and Khulan 2012 evaluated supplementation in the periconceptional period, and Nguyen 2012 evaluated the effect of pre‐conception supplementation. An 2001, Guldholt 1991, Graham 2007, Fleming 1986, and Wibowo 2012 assessed different doses of micronutrients; Agarwal 2012 evaluated different durations of the same micronutrients, while Feyi‐Waboso 2005 and Nwagha 2010 evaluated parenteral infusion or injection. Ramirez‐Velez 2011 compared nine versus three micronutrients, and Ling 1996 evaluated a herbal tonic. Li 2014 evaluated the effect of supplementation with folic acid and milk. Four excluded trials assessed the effect of fortification with MMN (Dieckmann 1944; Jarvenpaa 2007; Tatala 2002; Vadillo‐Ortega 2011). Two trials included high‐risk women (Gupta 2007; Rumiris 2006). Eight trials were excluded because they evaluated the acceptability of different forms of supplementation such as powder, tablet or spread (Choudhury 2012; Hambidge 2014; Lanou 2014; Young 2010); balanced energy protein supplementation (Huybregts 2009; Huybregts 2013); weekly food provision (Wijaya‐Erhardt 2011); or polyunsaturated fatty acids fortification in milk fortified with MMN (Mardones 2007). The cohort of an included study (Tofail 2008) was later randomised to breastfeeding counselling or standard care groups measuring the impact on postnatal growth in children (Kabir 2009) and hence was excluded. Leroy 2010 was excluded because it compared a traditional food assisted MCHN program versus a newly designed approach to prevent malnutrition in children. One abstract of a trial was excluded because it was a trial in women with alcohol consumption during pregnancy (Kable 2012).
Fall 2007 was moved from ongoing to excluded for the 2015 update because it is not a trial of supplementation.
See the Characteristics of excluded studies table for more details.
One abstract comparing MMN supplements versus iron folic acid remains in awaiting assessment due to missing group denominators (Gathwala 2012).
Risk of bias in included studies
The methodological quality of the included studies was generally good with at least 50% of the judgements at "low risk" for the various domains. It is unlikely that the evidence presented in this review is affected by the biases evaluated.
SeeFigure 1; Figure 2 and Characteristics of included studies table for further details on the methodological quality of the included studies.
Figure 1.
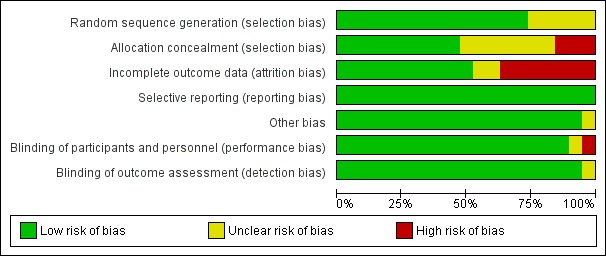
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Figure 2.
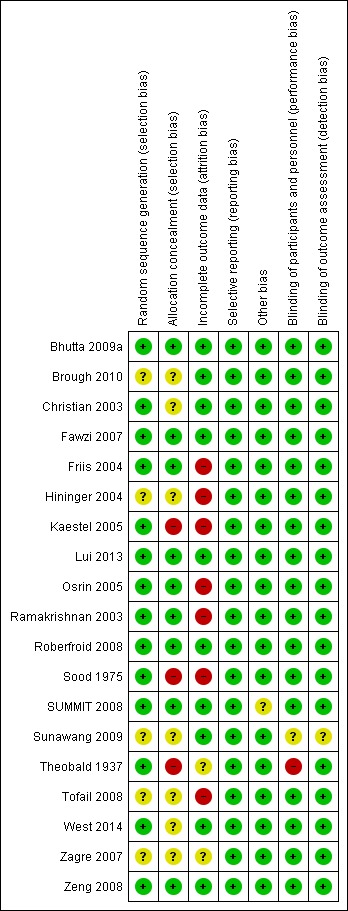
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
The included trials were of variable methodological quality. Participants were adequately randomised to the treatment groups in 14 trials (Bhutta 2009a; Christian 2003; Lui 2013;Fawzi 2007; Friis 2004; Kaestel 2005; Osrin 2005; Ramakrishnan 2003; Roberfroid 2008; Sood 1975; SUMMIT 2008; Theobald 1937; West 2014; Zeng 2008), whereas the method used for generating the randomisation sequence was not described in sufficient detail in the remaining studies to permit judgement.
Allocation of participants in to the intervention and control groups was concealed in nine trials (Bhutta 2009a; Fawzi 2007; Friis 2004; Lui 2013; Ramakrishnan 2003; Roberfroid 2008; SUMMIT 2008; Zeng 2008); it was unclear in seven trials (Brough 2010; Christian 2003; Hininger 2004; Sunawang 2009; Tofail 2008; West 2014; Zagre 2007); whereas allocation was not probably concealed in the remaining three trials (Kaestel 2005; Sood 1975; Theobald 1937).
Blinding
In two trials (Bhutta 2009a; Tofail 2008), the participants and the outcome assessors were blinded to the treatment allocation. Another 15 trials showed blinding of the participants, caregivers and the outcome assessors (Brough 2010; Christian 2003; Fawzi 2007; Friis 2004; Hininger 2004; Kaestel 2005; Lui 2013; Osrin 2005; Ramakrishnan 2003; Roberfroid 2008; SUMMIT 2008; Tofail 2008; West 2014; Zagre 2007; Zeng 2008). However, Sunawang 2009 showed blinding of participants only and Theobald 1937 indicated blinding only of outcome assessors.
Incomplete outcome data
Loss to follow‐up was less than 5% in two trials (West 2014; Zeng 2008); between 5% to 9.9% in six trials (Christian 2003; Fawzi 2007; Lui 2013; Osrin 2005; Roberfroid 2008; SUMMIT 2008); and between 10% to 19.9% in four trials (Bhutta 2009a; Brough 2010; Sunawang 2009; Zagre 2007). It was more than 20% in six trials (Friis 2004; Hininger 2004; Kaestel 2005; Ramakrishnan 2003; Sood 1975; Tofail 2008); and not reported in Theobald 1937. In Osrin 2005, although attrition was 5% and reasons for it were reported, exclusion was 39.5% and reasons were not reported and so it has been assessed as being at "high risk". Intention‐to‐treat analysis was used in all of the trials. In this review, an intention‐to‐treat analysis was conducted for all outcome measures.
Selective reporting
There was no indication of selective reporting in any of the included trials. All outcomes mentioned in the methods section or the protocol were presented in the various published papers of the trials.
Other potential sources of bias
No other potential sources of bias were identified in most of the included trials.
Effects of interventions
See: Table 1
Comparison 1: Multiple micronutrients (MMN) versus control (all trials)
Seventeen trials contributed data to this comparison, however, 15 of these 17 trials were carried out in low‐ and middle‐income countries and compared MMN supplements with iron and folic acid versus iron, with or without folic acid. Two trials carried out in the UK compared MMN with a placebo and contributed data to a very limited number of outcomes. In view of the differences in the settings where trials were conducted, and the in control group conditions, we have presented results separately in the forest plots and in the text below.
Multiple micronutrients (MMN) with iron and folic acid versus iron, with or without folic acid
In this comparison, we included 15 trials conducted in low and middle‐income countries and evaluating UNIMMAP or similar formulations (Bhutta 2009a; Christian 2003; Fawzi 2007; Friis 2004; Kaestel 2005; Lui 2013; Osrin 2005; Ramakrishnan 2003; Roberfroid 2008; SUMMIT 2008; Sunawang 2009; Tofail 2008; West 2014; Zagre 2007; Zeng 2008). In two trials (Fawzi 2007; Friis 2004), women received iron and folic acid as separate supplements, and in one trial (Ramakrishnan 2003), women in the control group received iron only.
Primary outcomes
When MMN supplementation was compared against iron with or without folic acid supplementation, there was a reduction in small‐for‐gestational age (SGA) (average risk ratio (RR) 0.92, 95% confidence interval (CI) 0.86 to 0.98; studies = 14; random‐effects, Tau² = 0.00, I² = 48%; moderate‐quality evidence;Analysis 1.2) and low birthweight (LBW) (average RR 0.88, 95% CI 0.85 to 0.91; studies = 15; high‐quality evidence;Analysis 1.3). No differences were observed between groups for the other primary outcomes: preterm births (average RR 0.96, 95% CI 0.90 to 1.03; studies = 15; random‐effects, Tau² = 0.01, I² = 52%; high‐quality evidence;Analysis 1.1), perinatal mortality (average RR 1.01, 95% CI 0.91 to 1.13; studies = 13; random‐effects, Tau² = 0.01, I² = 46%; high‐quality evidence;Analysis 1.4), stillbirth (average RR 0.97, 95% CI 0.87 to 1.09; studies = 15; random‐effects, Tau² = 0.01, I² = 26%; high‐quality evidence;Analysis 1.5), and neonatal mortality (average RR 1.06, 95% CI 0.92 to 1.22; studies = 11; random‐effects, Tau² = 0.01, I² = 31%; high‐quality evidence;Analysis 1.6).
Analysis 1.2.
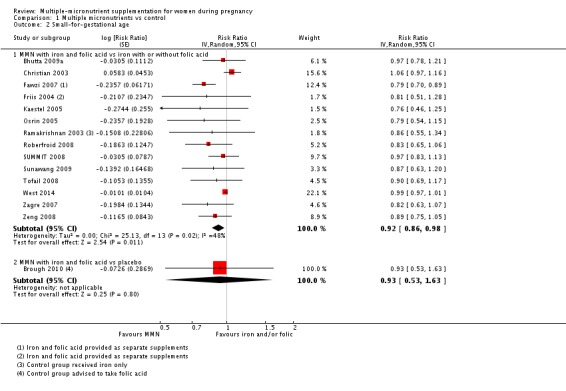
Comparison 1 Multiple micronutrients vs control, Outcome 2 Small‐for‐gestational age.
Analysis 1.3.
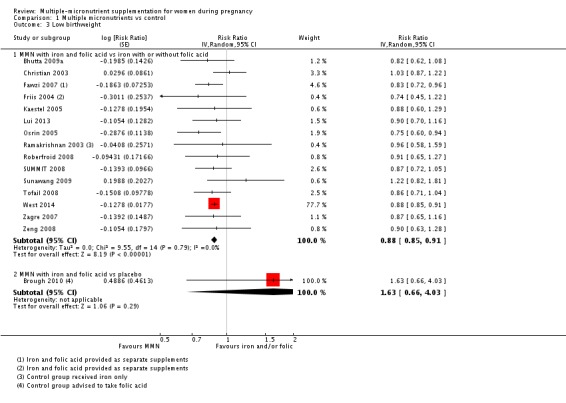
Comparison 1 Multiple micronutrients vs control, Outcome 3 Low birthweight.
Analysis 1.1.
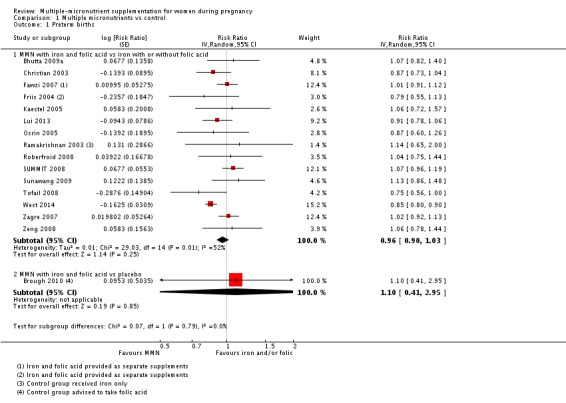
Comparison 1 Multiple micronutrients vs control, Outcome 1 Preterm births.
Analysis 1.4.
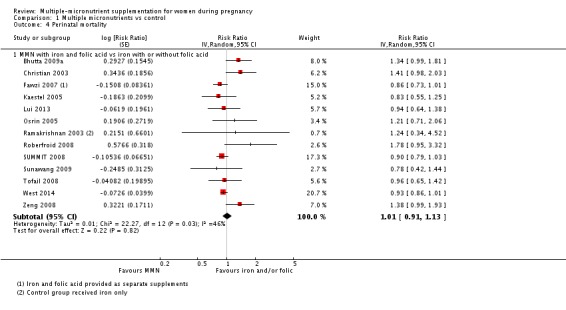
Comparison 1 Multiple micronutrients vs control, Outcome 4 Perinatal mortality.
Analysis 1.5.
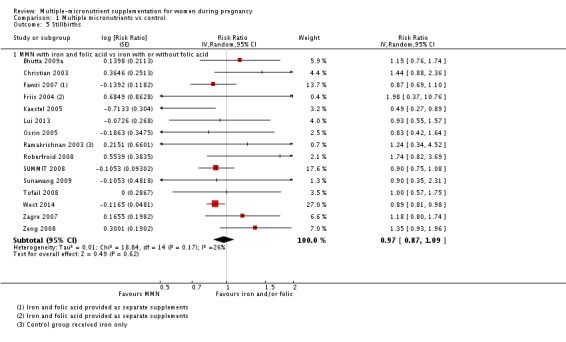
Comparison 1 Multiple micronutrients vs control, Outcome 5 Stillbirths.
Analysis 1.6.
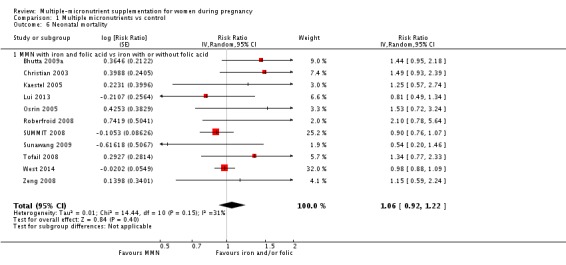
Comparison 1 Multiple micronutrients vs control, Outcome 6 Neonatal mortality.
It should be noted that the data for SGA for the following trials (Bhutta 2009a; Christian 2003; Friis 2004; Kaestel 2005; Osrin 2005; Ramakrishnan 2003; Roberfroid 2008; SUMMIT 2008; Sunawang 2009; Tofail 2008; Zagre 2007; Zeng 2008) was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial reports. For this data from the Food and Nutrition Bulletin 2009, the following were excluded: "women known to be HIV‐positive, women known to have multiple pregnancy, fetal losses before 28 weeks, stillbirths, infants with gestational age at delivery < 189 or > 314 days, and babies measured > 72 hours after birth. Only one pregnancy (the earliest) was included for each mother."
Secondary outcomes
MMN supplementation when compared against iron, with or without, folic acid showed no significant impact on maternal anaemia in the third trimester (average RR 1.03, 95% CI 0.85 to 1.24; studies = four; random‐effects, Tau² = 0.02, I² = 54%; Analysis 1.7). Similarly, no statistically significant difference was seen for the outcomes of miscarriage (average RR 0.91, 95% CI 0.80 to 1.03; studies = eight; random‐effects, Tau² = 0.00, I² = 0%; Analysis 1.8), delivery via a caesarean section (average RR 1.04, 95% CI 0.74 to 1.46; studies = four; random‐effects, Tau² = 0.00, I² = 0%; Analysis 1.13), and maternal mortality (average RR 0.97, 95% CI 0.63 to 1.48; studies = three; random‐effects, Tau² = 0.00, I² = 0%; Analysis 1.9).
Analysis 1.7.
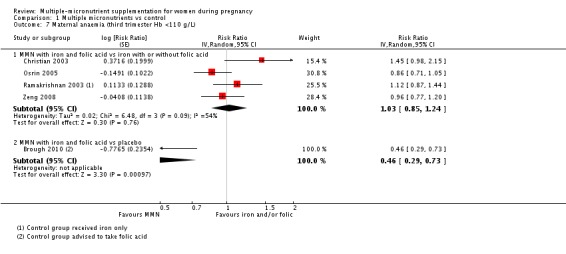
Comparison 1 Multiple micronutrients vs control, Outcome 7 Maternal anaemia (third trimester Hb <110 g/L).
Analysis 1.8.
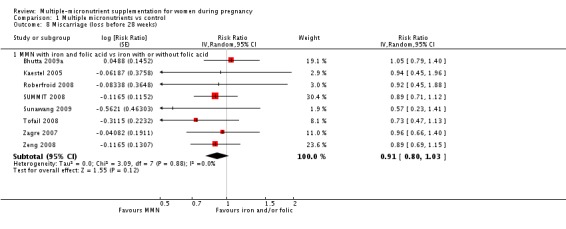
Comparison 1 Multiple micronutrients vs control, Outcome 8 Miscarriage (loss before 28 weeks).
Analysis 1.13.
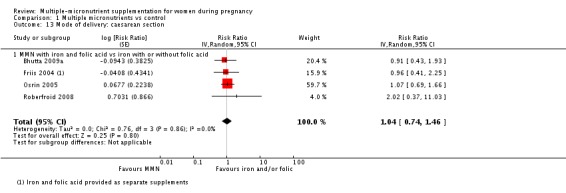
Comparison 1 Multiple micronutrients vs control, Outcome 13 Mode of delivery: caesarean section.
Analysis 1.9.
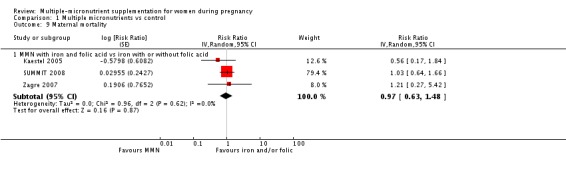
Comparison 1 Multiple micronutrients vs control, Outcome 9 Maternal mortality.
A number of prespecified clinically important outcomes could not be assessed due to insufficient data from the included trials. These included the following outcomes, which were measured either only in one trial or in none, or were presented in a format which precluded their inclusion in the analysis: placental abruption, congenital anomalies including neural tube defects (Osrin 2005), pre‐eclampsia, very preterm birth (Zeng 2008), side‐effects of MMN supplementation (Lui 2013; Tofail 2008), and neurodevelopmental delay (Zeng 2008). Additional important outcomes are: macrosomia (Roberfroid 2008), cost of supplementation, maternal well‐being or satisfaction, and nutritional status of the children (Roberfroid 2008).
Multiple micronutrients (MMN) versus placebo
Two trials conducted in the UK (Brough 2010; Theobald 1937) contributed data; in the Brough 2010 trial women in the control group were advised to take folic acid. The Theobald 1937 trial contributed data to one outcome only, and showed no clear differences between groups for pre‐eclampsia (average RR 0.67, 95% CI 0.12 to 3.74; Analysis 1.14). In the Brough 2010 trial, 402 women were randomised; women receiving supplements were at reduced risk of anaemia in the third trimester (average RR 0.46, 95% CI 0.29 to 0.73; Analysis 1.7), but there were no clear differences between women receiving supplements and those in the placebo group for any of the other outcomes reported; preterm birth (average RR1.10, 95% CI 0.41 to 2.95; Analysis 1.1); SGA (average RR 0.93, 95% CI 0.53 to1.63; Analysis 1.2); or LBW (average RR 1.63, 95% CI 0.66 to 4.03; Analysis 1.3).
Analysis 1.14.
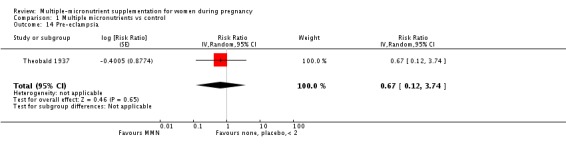
Comparison 1 Multiple micronutrients vs control, Outcome 14 Pre‐eclampsia.
Subgroup analysis (Data shown in Comparison 2) multiple micronutrients (MMN) with iron and folic acid versus iron with or without folic acid)
For the trials comparing MNN with iron and folic acid versus iron with or without folic acid (15 trials), we found substantial heterogeneity in the analyses for preterm birth, SGA, and perinatal mortality and explored its presence through subgroup analyses.
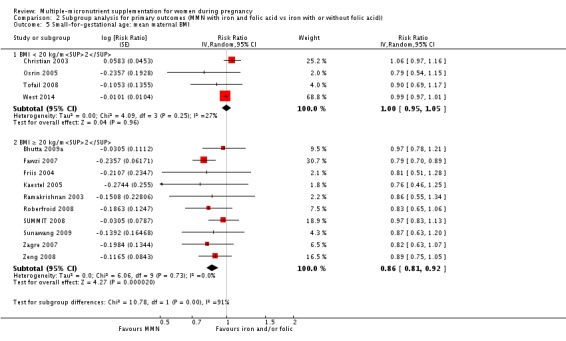
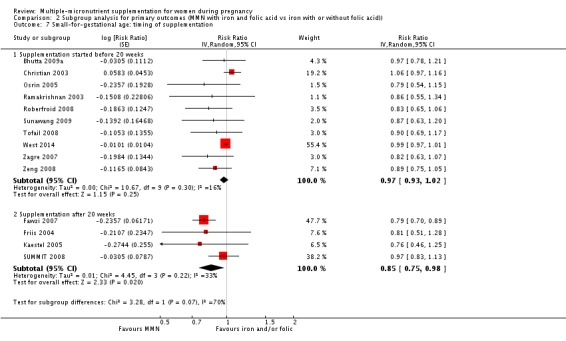
For the outcome preterm birth, MMN supplementation led to fewer preterm births for women in a subgroup of trials with mean maternal BMI of less than 20 kg/m² (average RR 0.85, 95% CI 0.80 to 0.90; studies = four), but not for women with a higher BMI (average RR 1.02, 95% CI 0.97 to 1.07; studies = 11); the test for subgroup differences was significant P < 0.00001, I² = 95.6%) Analysis 2.1. There were no group differences for the subgroups based on the timing of supplementation (Analysis 2.3), maternal height (Analysis 2.2), or for dose of iron for the outcome of preterm birth (Analysis 2.4) (all p>0.05).
Analysis 2.1.
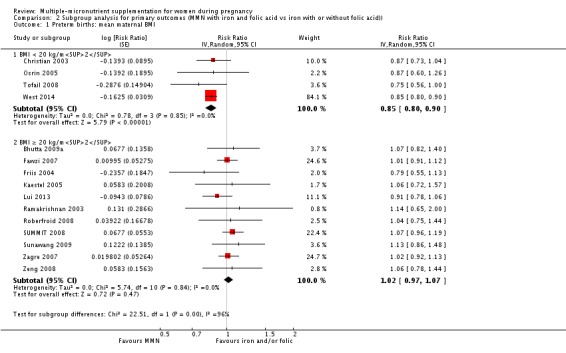
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 1 Preterm births: mean maternal BMI.
Analysis 2.3.
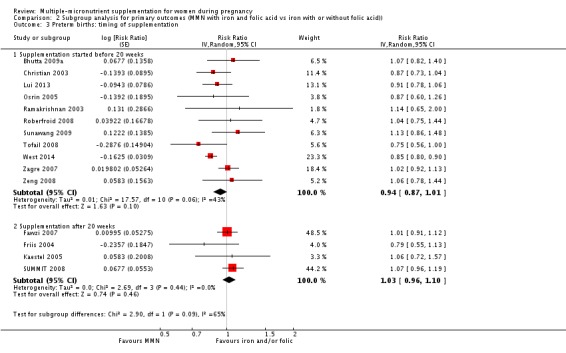
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 3 Preterm births: timing of supplementation.
Analysis 2.2.
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 2 Preterm births: mean maternal height.
Analysis 2.4.
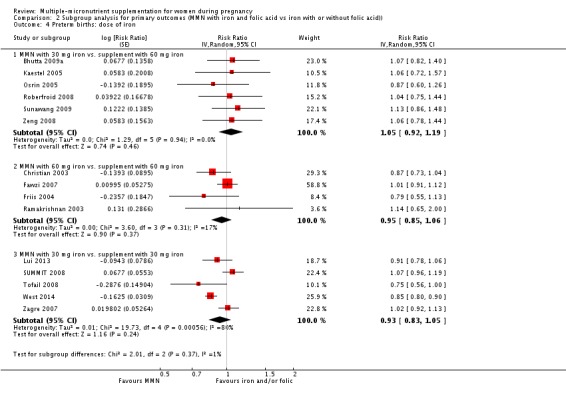
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 4 Preterm births: dose of iron.
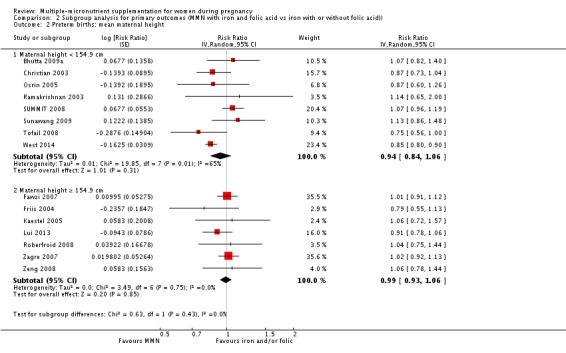
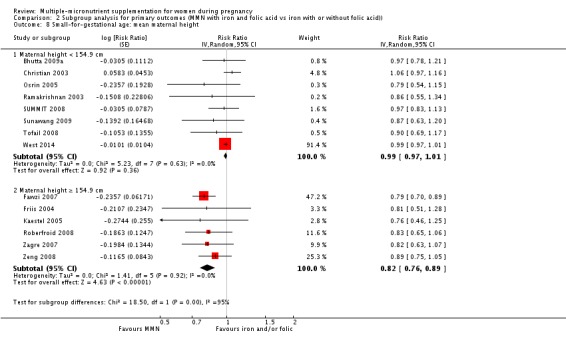
Subgroup analysis based on mean maternal BMI showed that the effect of MMN on SGA as compared to iron, with or without folic acid, was significant for the subgroup of trials with mean maternal BMI of at least 20 kg/m² (average RR 0.86, 95% CI 0.81 to 0.92; studies = 10), while it was non‐significant for the subgroup with mean maternal BMI of less than 20 kg/m² (average RR 1.00, 95% CI 0.95 to 1.05; studies = four; test for subgroup differences P = 0.001, I² = 90.7%) Analysis 2.5. Similarly, a significant difference was observed between the subgroup of studies based on maternal height (Analysis 2.8). The effect on SGA was significant in the subgroup with mean maternal height of at least 154.9 cm, while it was not significant in the subgroup with mean maternal height of less than 154.9 cm (average RR 0.82, 95% CI 0.76 to 0.89; studies = six) versus (average RR 0.99, 95% CI 0.97 to 1.01; studies = eight; test for subgroup differences P < 0.0001, I² = 94.6%), Analysis 2.8. Finally, the subgroup differences by the timing of supplementation and different doses of iron were tested and found tobe non‐significant (both p>0.05) (Analysis 2.7, Analysis 2.6, respectively).
Analysis 2.5.
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 5 Small‐for‐gestational age: mean maternal BMI.
Analysis 2.8.
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 8 Small‐for‐gestational age: mean maternal height.
Analysis 2.7.
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 7 Small‐for‐gestational age: timing of supplementation.
Analysis 2.6.
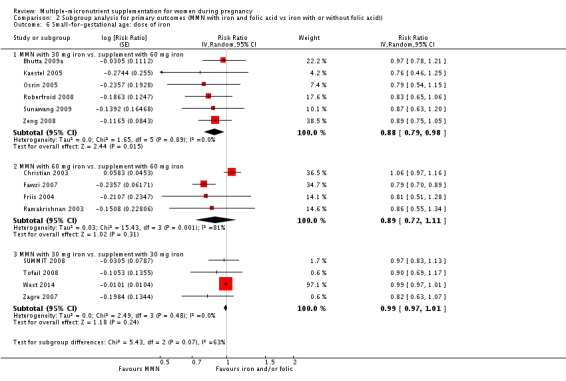
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 6 Small‐for‐gestational age: dose of iron.
The overall analysis of perinatal mortality, although showing a non‐significant effect of MMN supplements versus iron with or without folic acid, was found to have substantial statistical heterogeneity. Tests for subgroup differences did not show clear differences between subgroups based on mean maternal BMI, mean maternal height, and dose of iron (all P >0.05). However, statistically significant differences were observed between subgroups based on the timing of supplementation. The reduction in perinatal mortality was significantly higher in the subgroup with supplementation after 20 weeks (average RR 0.88, 95% CI 0.80, 0.97; studies = three), while it was non‐significant in the subgroup with supplementation before 20 weeks (average RR 1.13, 95% CI 0.96, 1.33; studies = ten), Analysis 2.11.
Analysis 2.11.
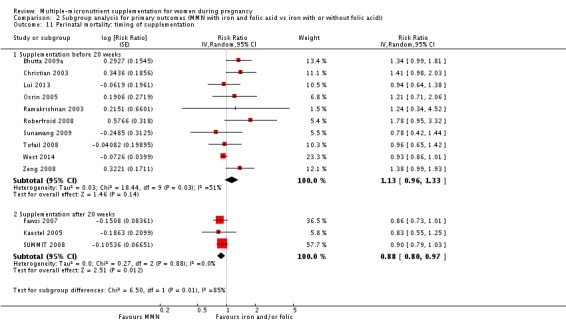
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 11 Perinatal mortality: timing of supplementation.
Sensitivity analysis (Data shown in Comparison 3)(multiple micronutrients (MMN) with iron and folic acid versus iron, with or without folic acid)
Sensitivity analysis was undertaken to study the effect of MMN supplementation on various outcomes by excluding trials with loss to follow‐up of more than 20% (Friis 2004; Kaestel 2005; Ramakrishnan 2003; Tofail 2008) from the analyses. This exclusion did not affect the significance of the findings for the outcomes.
Discussion
Summary of main results
Nineteen trials (involving 138,538 women) were identified as eligible for inclusion in this review. However, only 17 trials (involving 137,791 women) contributed data to the review. This update summarises the current evidence on the effect of multiple‐micronutrients (MMN) supplementation during pregnancy on fetal, infant, and maternal outcomes. Overall, MMN supplementation with iron and folic acid versus supplementation with iron (with or without folic acid) showed a 8% reduction in the risk of small‐for‐gestational age (SGA) births and a 12% reduction in the risk of low birthweight (LBW). A summary of the main findings for trials comparing MMN with iron and folic acid verus iron with or without folic acid is presented in Table 1.
Overall completeness and applicability of evidence
This review included a total of 19 trials evaluating the effect of MMN supplementation but only 17 contributed data. Trials conducted as early as 1937 were included in the review. All trials evaluating UNIMMAP supplement proposed in 1999 by UNICEF, UNU, and WHO and starting recruitment of participants as early as 2001 were included in the analysis. Inclusion of these and older trials, identified as a result of an extensive search of literature published over the last several decades, represents overall completeness of evidence.
As iron with folic acid are recommended for pregnant women in low and middle‐income countries, we primarily evaluated the effect of adding additional micronutrients to the iron and folic acid supplement. Most of the included trials were conducted in low‐ and middle‐income countries and included pregnant women at varying gestational stages, ranging from early pregnancy to 36 weeks of gestation. Pregnant women with serious medical conditions, such as, cardiac disease or respiratory infections, were excluded from the trials.
Comparison 1: multiple micronutrients (MMN) with iron and folic acid versus control (iron with or without folic acid) resulted in a significant decrease in the number of newborn infants identified as LBW or SGA. No significant differences were shown for other maternal and pregnancy outcomes: preterm births, maternal anaemia in the third trimester, miscarriage, maternal mortality, perinatal mortality, stillbirth, neonatal mortality, or risk of delivery via a caesarean section. A number of prespecified, clinically important outcomes could not be assessed due to insufficient or non‐available data. Single trials reported results for: very preterm birth < 34 weeks, macrosomia, side‐effects of supplements, nutritional status of children, and congenital anomalies including neural tube defects and neurodevelopmental outcome: Bayley Scales of Infant Development (BSID) scores. No trial reported pre‐eclampsia, placental abruption, premature rupture of membranes, cost of supplementation, and maternal well‐being or satisfaction.
Supplementation with MMN with iron and folic acid versus iron with or without folic acid reduced the risk of LBW and SGA. One of the postulated pathways for this finding is through an increase in birthweight; higher birthweight resulting in lower proportion of LBW and SGA births. Most of the studies included in these analyses demonstrated an increase in birthweight as a result of supplementation with MMN. During pregnancy, the increase in weight of the fetus occurs during the third trimester and this is a potential window of opportunity to improve birthweight. Importantly, a major proportion of women in these studies were taking supplements in the third trimester as several studies recruited pregnant women in the first trimester with supplementation starting in the second trimester; whereas the others recruited almost 80% of their participants by the end of the second trimester. This provides support to the postulated pathway as the intervention was in place much before the beginning of third trimester. Furthermore, since MMN supplementation did not show an impact on preterm birth, which is an underlying cause of LBW, this finding cannot be attributed to a longer duration of gestation.
Most of the studies included in this review were undertaken in low and middle‐income countries with high fertility rates, low maternal body mass index (BMI), a high prevalence of iron‐deficiency anaemia, and frequent subclinical micronutrient deficiencies (Bhutta 2008). Studies have shown that a significant proportion of pregnant women suffer from MMN deficiencies at the same time. These have been associated with poor pregnancy outcomes including LBW (Allen 2005; Keen 2003). Anaemia, especially as a result of iron deficiency, which is frequent in these women, is also possibly associated with an increased risk of infections (Oppenheimer 2001). Whilst the objective of the review was not to measure impact on the immune status or maternal infections, our findings of a significant impact on LBW and SGA as a result of MMN supplementation could be through improved nutritional status and hence better immune system and resistance to maternal infections.
Maternal anthropometry pre‐pregnancy and weight gain during pregnancy have also been associated with various neonatal and child outcomes. Maternal height seems to be a stable and easily measurable variable in the setting of low and middle‐income countries. Reviews have identified short maternal stature as an important determinant of intrauterine growth retardation and LBW (Kramer 2003; WHO 1995). Short maternal stature (short height) has been found to be significantly associated with an increased risk of child mortality, underweight infants and stunting (Ozaltin 2010; Voigt 2010). Our subgroup analyses indicate that MMN failed to show a significant effect on the SGA outcome in women with poor nutritional status at baseline, defined as maternal height less than 154.9 cm and BMI less than 20 kg/m². MMN showed a significant reduction in SGA babies among women with a mean maternal height at least 154.9 cm as compared to iron with or without folic acid, whereas the effect was non‐significant among women with a mean height less than 154.9 cm. Similarly, MMN micronutrients showed a significant reduction in SGA babies among women with a mean BMI at least 20 kg/m², whereas a non‐significant effect among those women with a mean BMI less than 20 kg/m². These findings should be interpreted with caution but suggest a possible role of MMN in preventing SGA, but only in women with good nutritional status at baseline, and an absence of similar effects in women with poor nutritional status at the time of conception. On the contrary, the findings for the subgroup analysis for preterm birth indicate a significant effect among women with low BMI but not among those with higher BMI. These differences could be explained by the different underlying causes and mechanisms leading to poor outcomes. The findings further highlight the contribution of maternal malnutrition to poor fetal anthropometry and stunting later in childhood, resulting in an intergenerational transfer of malnutrition. Though supplementation has been suggested to improve child growth and survival, there is currently no evidence that maternal MMN supplementation during pregnancy, compared to iron and folic acid, improves child growth or survival and studies with long‐term follow‐up are required.
We could not assess a number of prespecified, clinically important outcomes in this review due to insufficient or non‐available data. These include placental abruption, congenital anomalies including neural tube defects, premature rupture of membranes, macrosomia, neurodevelopmental delay, very preterm births, macrosomia, cost of supplementation, side‐effects of supplements, maternal well‐being or satisfaction, and nutritional status or growth during childhood.
Quality of the evidence
We evaluated the quality of the available evidence by using the GRADE methodology as outlined in the GRADE Handbook. We created a 'Summary of findings' table for the primary outcomes of preterm birth, SGA, LBW, stillbirths, perinatal and neonatal mortality for Comparison 1: MMN with iron and folic acid versus iron with or without folic acid supplement.
When assessed according to GRADE criteria, the quality of evidence for the review's primary outcomes overall was high. Pooled results for all primary outcomes were based on multiple trials with large sample sizes and precise estimates. For the comparison of MMN versus control (iron and/or folic acid) the following outcomes were graded to be as of high quality: preterm birth, low LBW, perinatal mortality, stillbirth and neonatal mortality. The outcome of SGA was graded to be of moderate quality, downgraded once for funnel plot asymmetry and potential publication bias.
Potential biases in the review process
This update of the review includes additional data published since the last update. An extensive literature search was conducted to identify any additional studies since the last search. The screening of the updated search, selection of eligible studies and data extraction were conducted independently by two review authors. The risk of bias was also assessed by two review authors. Given the application of the above Cochrane methodology, it is unlikely that the findings of this review are affected by biases in the review process.
Agreements and disagreements with other studies or reviews
The significant findings of reduction in the SGA and LBW risk as a result of MMN supplementation in the current review corroborate those of other systematic reviews and meta‐analyses conducted since the first version of this Cochrane review (Bhutta 2012; Kawai 2011; Margetts 2009; Ramakrishnan 2012a). A recent systematic review and meta‐analysis also reports reduction in the LBW and SGA risk; however, the effect on SGA is reported to be marginally significant (Christian 2015). This review included a smaller number of studies in the SGA analysis (studies = seven) as opposed to the current review (studies = 14), thereby explaining the difference between the estimates reported in the two reviews.
We did not find a significant effect of MMN supplements on perinatal mortality, stillbirth, and neonatal mortality in the main analyses, which are similar to the earlier version of this Cochrane review and other systematic reviews (Haider 2011; Ronsmans 2009). Christian 2015 also observed similar findings for neonatal mortality. Previously, concerns were raised regarding the possible harmful effect of MMN supplements by increasing the risk of perinatal and neonatal mortality through increased birth asphyxia in heavier babies (Christian 2005). Two earlier trials conducted in Nepal by Christian et al and Osrin et al, both had found a non‐significant increase in the risk of neonatal and perinatal mortality, but their pooled effect estimate showed a significant increase in the risk of these outcomes (Christian 2003; Osrin 2005). This concern was questioned by other researchers in the field and has not been observed in other studies (Bhutta 2009b; Huffman 2005; Shrimpton 2005). Importantly, our current findings of no impact on neonatal mortality are supported by those of two MMN supplementation trials that were individually powered to evaluate an effect on early infant mortality (SUMMIT 2008; West 2014). The recent large trial in Bangladesh did not show an increase in neonatal or early infant mortality risk in the MMN supplementation group verus iron and folic acid (West 2014). The authors, in post‐hoc analysis, however report higher neonatal mortality among boys due to birth asphyxia (West 2014). This finding should be interpreted with caution as the cause of death was ascertained by verbal autopsy with parents, which may result in misclassification of the underlying cause of death. Moreover, the trial was not powered to detect a statistically significant difference in cause‐specific mortality by gender.
The finding suggesting an increase in the risk of neonatal mortality in some settings is likely due to the absence of skilled care at delivery and the poor standard of care in the health systems in low and middle‐income countries, where the majority of births take place at home without the supervision of skilled attendants. This was also observed in a systematic review of MMN supplementation performed using the Child Health Epidemiology Research Group (CHERG) methodology (Walker 2010). While the current review showed no overall increase in the neonatal mortality risk as a result of MMN supplementation, a significantly increased risk was observed in the subgroup of populations with the majority of births at home while no effect was seen where the majority of births took place in health facilities (Haider 2011). This finding may be relevant to efforts to improve maternal nutrition and weight gain during pregnancy (and by inference fetal size) in settings where maternal care during pregnancy and childbirth may be sub optimal. We would recommend the use of MMN supplements in pregnancy principally in settings where skilled maternal care during childbirth and facility‐based births can be provided.
As noted earlier, the composition of the MMN supplements differed in several of the included trials (Table 5), and use of folic acid alone or iron with folic acid remains a standard recommendation for pregnant women in many countries globally. In order to identify the effect of a single micronutrient on pregnancy outcomes, each additional micronutrient should be evaluated against a placebo in women receiving iron with folic acid. This would, however, only be of value in populations with single or limited micronutrient deficiencies.
Table 1.
Micronutrients given to women in the intervention group
| Study ID | Iron | Folic acid | Vit A | Beta‐carotene | Vit C | Vit D | Vit E | Vit B1 | Vit B2 | Vit B3 | Vit B6 | Vit B12 | Vit K | Copper | Selenium | Zinc | Iodine | Magnesium | Calcium | Phosphorus | Biotin | Potassium | Manganese |
| Bhutta 2009 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Brough 2010 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Christian 2003 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Cogswell 2013 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Fawzi 2007 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||||||
| Friis 2004 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Hininger 2004 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||||
| Kaestel 2005 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Osrin 2005 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Ramakrishnan 2003 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||
| Roberfroid 2008 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Sood 1975 | ✓ | ✓ | ✓ | ||||||||||||||||||||
| SUMMIT 2008 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||
| Sunawang 2009 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||
| Theobald 1937 | ✓ | ✓ | ✓ | ||||||||||||||||||||
| Tofail 2008 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| West 2014 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Zagre 2007 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Zeng 2008 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
Authors' conclusions
Our findings support the effect of multiple‐micronutrient (MMN) supplements with iron and folic acid in improving birth outcomes. These findings have been consistently observed in several systematic evaluations of evidence and provide a strong basis to guide the replacement of iron and folic acid with MMN supplements for pregnant women in low and middle‐income countries where deficiencies of MMNs exist.
Efforts should focus on the integration of this intervention in maternal nutrition and antenatal care programs in low and middle‐income countries where MMN deficiencies are common among women of reproductive age.
Feedback
Professor Caroline Fall, 31 May 2016
Summary
Our comments relate mainly to the stillbirth analysis. We believe a fixed‐effect model is inappropriate for this analysis. While there was no statistical heterogeneity, the Cochrane handbook and the methods section of the review state that clinical (contextual) heterogeneity should be the main driver of the choice of model, rather than statistical heterogeneity. Contextual heterogeneity was evident in a number of aspects of these trials, including their design (individual or cluster randomized), interventions (composition of multiple micronutrient supplements and duration of supplementation), co‐interventions (for example early or late food supplementation), comparison groups (iron alone, IFA, and different doses of these, especially iron), participants (geographic location, phenotype, and gestational age at randomization) and outcome definition (definition of stillbirths varied from ≥24 weeks to ≥28 weeks gestation, including or excluding multiple births). There is inconsistency in the use of fixed or random‐effects models within the review; for example, for perinatal mortality (of which stillbirths form a sub‐set, Analysis 1.4), including 12 of the 15 trials contributing to the stillbirth analysis, a random effects meta‐analysis was used.
We think that three eligible trials have been omitted from the review (Ashorn 20151; Hanieh 20132 [protocol of this trial is cited as Biggs 2011]; and Adu‐Afarwuah 20153 [protocol cited as Dewey 2011). These are all listed in the review as ‘ongoing trials’, but they were published before the stated search date of March 2015. Inclusion of these trials makes little difference to the overall results, but a Cochrane review is expected to be complete.
The Methods section under “Unit of analysis issues” does not clearly define the strategy for comparisons in trials with factorial designs. Further, the comparisons made are unclear in places and inconsistent across studies. This issue potentially applies to 4 studies (Christian 2003; Kaestel 2005; Lui 2013; Zeng 2008), all of which had more than one eligible intervention and/or control group.
A reduction in stillbirths is the only direct benefit to health that has been reported as a result of multiple micronutrient supplements in pregnancy (as opposed to ‘metric’ outcomes like birth weight and rates of preterm birth), and is currently the only evidence sufficient to justify changing routine supplementation from IFA to MMN. A significant increase in birth weight might be expected to lead to significant health benefits (eg. reduced infant mortality) but until this review, there was no apparent effect of MMN supplementation in pregnancy on mortality. The soundness of the stillbirth evidence is therefore crucial to the policy review, and we believe that the evidence remains inconclusive.
Finally, we are curious to know how the review authors presented data for smallness for gestational age (SGA) as an outcome (Analysis 1.2) because data for SGA were not published for some of the trials.
(Summary of feedback from Harshpal Singh Sachdev, Delanjathan Devakumar, Caroline Fall, Clive Osmond, David Osrin, Jonathan Broad, Barrie Margetts, May 2016).
References
Ashorn P, Alho L, Ashorn U, Cheung YB, Dewey KG, Harjunmaa U, et al. The impact of lipid‐based nutrient supplement provision to pregnant women on newborn size in rural Malawi: a randomized controlled trial. The American Journal of Clinical Nutrition 2015; 101: 387‐97.
Hanieh S, Ha TT, Simpson JA, Casey GJ, Khuong NC, Thoang DD, et al. The effect of intermittent antenatal iron supplementation on maternal and infant outcomes in rural Viet Nam: a cluster randomised trial. PLoS Med 2013; 10: e1001470.
Adu‐Afarwuah S, Lartey A, Okronipa H, Ashorn P, Zeilani M, Peerson JM, et al. Lipid‐based nutrient supplement increases the birth size of infants of primiparous women in Ghana. The American Journal of Clinical Nutrition 2015; 101: 835‐46.
Reply
We would like to thank you and your colleagues for the detailed comments and queries on our review. We have made edits to the review to address the specific queries. We also plan to update this important review over the coming year, since the search will become out of date in March 2017.
1. Random‐effects versus fixed‐effect model – stillbirth analysis
Regarding the comment about the inconsistent use of fixed or random effects model in the review, please note we had not used these inconsistently. While we agree regarding the presence of contextual differences between the included trials, the decision to select fixed or random effects model for stillbirth analysis was based on the values of I², Tau² and/or p value, as per the methodological guidelines of Cochrane Pregnancy and Childbirth reviews: “We regarded heterogeneity as substantial if an I² was greater than 30% and either a Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity.” We have taken on board your comments and changed the stillbirth results to RR 0.97, 95% CI 0.87 to 1.09, using a random effects model. However, as our group statistician has advised, this is a very conservative approach and an interpretation of a possible reduction in stillbirth would also be valid.
2. Omission of trials
Regarding the omission of three eligible trials, namely Hanieh 2013, Ashorn 2015, and Adu‐Afarwuah 2015, we consulted the Information Specialist of Cochrane Pregnancy and Childbirth. The Information Specialist has informed us that one of the trials, Adu‐Afarwuah 2015 was not identified in the literature search conducted on 11th March 2015 – and had not been added to the Cochrane Pregnancy and Childbirth group trials register at that time. Regarding Ashorn 2015, this was in Ongoing studies, but has now been moved to Characteristics of studies awaiting classification. The review authors have requested additional data from the trial authors for Ashorn 2015, as stated in the notes section of the Characteristics of studies awaiting classification table. This trial included HIV+ patients: “This trial included women with a + HIV test: IFA = 15.6%; MMN 11.1% and LNS 14.4%. We have contacted authors to see if separate analyses for HIV‐ women are available.” Hanieh 2013 had been assigned to another review on intermittent iron, but will be re‐assessed at next update. The review authors will assess all three of these studies in the next update of this review.
3. Unit of analysis issues ‐ Trials with multiple intervention groups
We appreciate that our methods section had not detailed clearly how unit of analysis issues for trials with multiple intervention groups had been dealt with. We have made edits to address this issue, as detailed in the Unit of analysis issues section for Christian 2003; Kaestel 2005; Lui 2013; Zeng 2008. For trials with multiple intervention groups, we selected one pair of interventions and excluded the others. This is one approach recommended by the Cochrane Handbook [16.5.4]. If more than two intervention groups had met the eligibility criteria, we would have combined groups to create a single pair‐wise comparison as per [16.5.4] of the Cochrane Handbook.
4. Source of data for Small for gestational age (SGA) Unit of analysis issues ‐ Trials with multiple intervention groups
We have spoken to the Research Associate, Cochrane Pregnancy and Childbirth, who helped with the last update. The SGA data for all but three trials, came from a separate report (Food and Nutrition Bulletin 2009). Only in three trials were we able to extract SGA data directly from the trial reports (Brough 2010; Fawzi 2007; West 2014).
(Reply from Batool A Haider, Zulfiqar A Bhutta, Philippa Middleton, March 2017).
Contributors
Harshpal Singh Sachdev MD, Senior Consultant in Pediatrics and Clinical Epidemiology, Sitaram Bhartia Institute of Science and Research, New Delhi, India Delanjathan Devakumar PhD, NIHR Clinical Lecturer in Public Health, Institute for Global Health, Faculty of Population Health Sciences, University College London, London, UK Caroline Fall DM, Professor of International Paediatric Epidemiology, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton, UK Clive Osmond PhD, Professor of Biostatistics, MRC Lifecourse Epidemiology Unit, University of Southampton, Southampton, UK David Osrin PhD, Professor of Global Health, Institute for Global Health, Faculty of Population Health Sciences, University College London, London, UK Jonathan Broad MBChB, Honorary research fellow, University of Bristol, Academic Foundation Doctor, Peninsula Deanery Barrie Margetts PhD, Emeritus Professor, Population Health Sciences Research Group, Faculty of Medicine, University of Southampton, Southampton, UK
Batool A Haider, Researcher, Department of Global Health and Population, Harvard School of Public Health, Boston, MA, USA
Zulfiqar A Bhutta, Robert Harding Chair in Global Child Health & Policy, Centre for Global Child Health, Hospital for Sick Children, Toronto, Canada
Philippa Middleton, Editor, Australian Satellite of Cochrane Pregnancy and Childbirth/Principal Research Fellow, Healthy Mothers, Babies and Children, South Australian Health and Medical Research Institute, Women's and Children's Hospital, Adelaide, Australia
Acknowledgements
This review was prepared in part during the Fellowship Programme organised by the Cochrane Infectious Diseases Group in July 2003 and March 2005. The Department for International Development (UK) supports this programme through the Effective Health Care Research Programme Consortium at the Liverpool Tropical School of Medicine. The views expressed are not necessarily those of the Department for International Development.
This update was made possible through an unrestricted sub‐grant under a Program Cooperative Agreement between UNICEF (Headquarters) and the Centre for Global Child Health, The Hospital for Sick Children, Toronto, Canada.
We would like to thank Ms Lynn Hampson for her assistance with the literature search, and Professor James Neilson who provided support and guidance for previous versions of the review. We would also like to thank Nabila Hossain, Anoosh Moin, Nancy Medley, and Nasreen Aflaifel for their assistance with the screening of search results and data extraction, and Roland Kupka from UNICEF for comments on the review. Nancy Medley created the 'Summary of findings' table for the review. We would also like to thank Therese Dowswell for making edits in response to feedback from the Editor.
Nancy Medley and Nasreen Aflaifel's work was financially supported by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization. The named authors alone are responsible for the views expressed in this publication (2015 update).
As part of the prepublication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team) and the Group's Statistical Adviser (2015 update).
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Data and analyses
Comparison 1.
Multiple micronutrients vs control
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Preterm births | 16 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 MMN with iron and folic acid vs iron with or without folic acid | 15 | Risk Ratio (Random, 95% CI) | 0.96 [0.90, 1.03] | |
| 1.2 MMN with iron and folic acid vs placebo | 1 | Risk Ratio (Random, 95% CI) | 1.10 [0.41, 2.95] | |
| 2 Small‐for‐gestational age | 15 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 MMN with iron and folic acid vs iron with or without folic acid | 14 | Risk Ratio (Random, 95% CI) | 0.92 [0.86, 0.98] | |
| 2.2 MMN with iron and folic acid vs placebo | 1 | Risk Ratio (Random, 95% CI) | 0.93 [0.53, 1.63] | |
| 3 Low birthweight | 16 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 3.1 MMN with iron and folic acid vs iron with or without folic acid | 15 | Risk Ratio (Random, 95% CI) | 0.88 [0.85, 0.91] | |
| 3.2 MMN with iron and folic acid vs placebo | 1 | Risk Ratio (Random, 95% CI) | 1.63 [0.66, 4.03] | |
| 4 Perinatal mortality | 13 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 4.1 MMN with iron and folic acid vs iron with or without folic acid | 13 | Risk Ratio (Random, 95% CI) | 1.01 [0.91, 1.13] | |
| 5 Stillbirths | 15 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 5.1 MMN with iron and folic acid vs iron with or without folic acid | 15 | Risk Ratio (Random, 95% CI) | 0.97 [0.87, 1.09] | |
| 6 Neonatal mortality | 11 | Risk Ratio (Random, 95% CI) | 1.06 [0.92, 1.22] | |
| 6.1 MMN with iron and folic acid vs iron with or without folic acid | 11 | Risk Ratio (Random, 95% CI) | 1.06 [0.92, 1.22] | |
| 7 Maternal anaemia (third trimester Hb <110 g/L) | 5 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 7.1 MMN with iron and folic acid vs iron with or without folic acid | 4 | Risk Ratio (Random, 95% CI) | 1.03 [0.85, 1.24] | |
| 7.2 MMN with iron and folic acid vs placebo | 1 | Risk Ratio (Random, 95% CI) | 0.46 [0.29, 0.73] | |
| 8 Miscarriage (loss before 28 weeks) | 8 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 8.1 MMN with iron and folic acid vs iron with or without folic acid | 8 | Risk Ratio (Random, 95% CI) | 0.91 [0.80, 1.03] | |
| 9 Maternal mortality | 3 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 9.1 MMN with iron and folic acid vs iron with or without folic acid | 3 | Risk Ratio (Random, 95% CI) | 0.97 [0.63, 1.48] | |
| 10 Very preterm birth (before 34 weeks of gestation) | 1 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 10.1 MMN with iron and FA vs iron with or without folic acid | 1 | Risk Ratio (Random, 95% CI) | 1.30 [0.67, 2.54] | |
| 11 Congenital anomalies | 1 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 11.1 MMN with iron and folic acid vs iron with or without folic acid | 1 | Risk Ratio (Random, 95% CI) | 0.99 [0.14, 7.00] | |
| 12 Neurodevelopmental outcome: BSID scores | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Mental development scores at 6 months of age: new subgroup | 1 | 770 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐6.78, 6.74] |
| 12.2 Mental development scores at 12 months of age | 1 | 744 | Mean Difference (IV, Random, 95% CI) | 1.21 [‐5.06, 7.48] |
| 12.3 Psychomotor development scores ar 6 months of age | 1 | 770 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐3.91, 3.59] |
| 12.4 Psychomotor development scores at 12 months of age | 1 | 744 | Mean Difference (IV, Random, 95% CI) | 0.34 [‐2.73, 3.41] |
| 13 Mode of delivery: caesarean section | 4 | Risk Ratio (Random, 95% CI) | 1.04 [0.74, 1.46] | |
| 13.1 MMN with iron and folic acid vs iron with or without folic acid | 4 | Risk Ratio (Random, 95% CI) | 1.04 [0.74, 1.46] | |
| 14 Pre‐eclampsia | 1 | Risk Ratio (Random, 95% CI) | 0.67 [0.12, 3.74] |
Analysis 1.10.
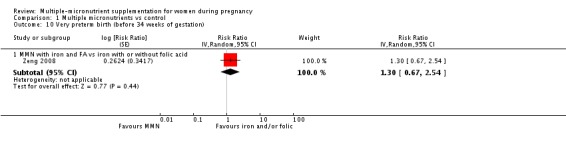
Comparison 1 Multiple micronutrients vs control, Outcome 10 Very preterm birth (before 34 weeks of gestation).
Analysis 1.11.
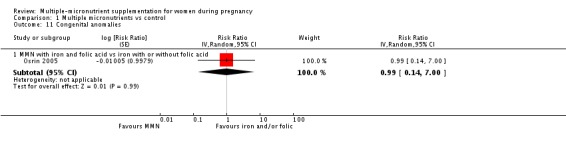
Comparison 1 Multiple micronutrients vs control, Outcome 11 Congenital anomalies.
Analysis 1.12.
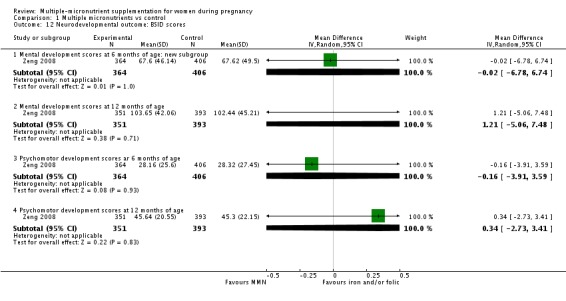
Comparison 1 Multiple micronutrients vs control, Outcome 12 Neurodevelopmental outcome: BSID scores.
Comparison 2.
Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid))
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Preterm births: mean maternal BMI | 15 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 1.1 BMI < 20 kg/m2 | 4 | Risk Ratio (Random, 95% CI) | 0.85 [0.80, 0.90] | |
| 1.2 BMI ≥ 20 kg/m2 | 11 | Risk Ratio (Random, 95% CI) | 1.02 [0.97, 1.07] | |
| 2 Preterm births: mean maternal height | 15 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Maternal height < 154.9 cm | 8 | Risk Ratio (Random, 95% CI) | 0.94 [0.84, 1.06] | |
| 2.2 Maternal height ≥ 154.9 cm | 7 | Risk Ratio (Random, 95% CI) | 0.99 [0.93, 1.06] | |
| 3 Preterm births: timing of supplementation | 15 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 3.1 Supplementation started before 20 weeks | 11 | Risk Ratio (Random, 95% CI) | 0.94 [0.87, 1.01] | |
| 3.2 Supplementation after 20 weeks | 4 | Risk Ratio (Random, 95% CI) | 1.03 [0.96, 1.10] | |
| 4 Preterm births: dose of iron | 15 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 4.1 MMN with 30 mg iron vs. supplement with 60 mg iron | 6 | Risk Ratio (Random, 95% CI) | 1.05 [0.92, 1.19] | |
| 4.2 MMN with 60 mg iron vs. supplement with 60 mg iron | 4 | Risk Ratio (Random, 95% CI) | 0.95 [0.85, 1.06] | |
| 4.3 MMN with 30 mg iron vs. supplement with 30 mg iron | 5 | Risk Ratio (Random, 95% CI) | 0.93 [0.83, 1.05] | |
| 5 Small‐for‐gestational age: mean maternal BMI | 14 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 5.1 BMI < 20 kg/m2 | 4 | Risk Ratio (Random, 95% CI) | 1.00 [0.95, 1.05] | |
| 5.2 BMI ≥ 20 kg/m2 | 10 | Risk Ratio (Random, 95% CI) | 0.86 [0.81, 0.92] | |
| 6 Small‐for‐gestational age: dose of iron | 14 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 6.1 MMN with 30 mg iron vs. supplement with 60 mg iron | 6 | Risk Ratio (Random, 95% CI) | 0.88 [0.79, 0.98] | |
| 6.2 MMN with 60 mg iron vs. supplement with 60 mg iron | 4 | Risk Ratio (Random, 95% CI) | 0.89 [0.72, 1.11] | |
| 6.3 MMN with 30 mg iron vs. supplement with 30 mg iron | 4 | Risk Ratio (Random, 95% CI) | 0.99 [0.97, 1.01] | |
| 7 Small‐for‐gestational age: timing of supplementation | 14 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 7.1 Supplementation started before 20 weeks | 10 | Risk Ratio (Random, 95% CI) | 0.97 [0.93, 1.02] | |
| 7.2 Supplementation after 20 weeks | 4 | Risk Ratio (Random, 95% CI) | 0.85 [0.75, 0.98] | |
| 8 Small‐for‐gestational age: mean maternal height | 14 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 8.1 Maternal height < 154.9 cm | 8 | Risk Ratio (Random, 95% CI) | 0.99 [0.97, 1.01] | |
| 8.2 Maternal height ≥ 154.9 cm | 6 | Risk Ratio (Random, 95% CI) | 0.82 [0.76, 0.89] | |
| 9 Perinatal mortality: mean maternal BMI | 13 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 9.1 BMI < 20 kg/m² | 4 | Risk Ratio (Random, 95% CI) | 1.05 [0.85, 1.29] | |
| 9.2 BMI ≥ 20 kg/m² | 9 | Risk Ratio (Random, 95% CI) | 1.02 [0.87, 1.19] | |
| 10 Perinatal mortality: mean maternal height | 13 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 10.1 Maternal height < 154.9 cm | 8 | Risk Ratio (Random, 95% CI) | 1.01 [0.89, 1.14] | |
| 10.2 Maternal height ≥ 154.9 cm | 5 | Risk Ratio (Random, 95% CI) | 1.04 [0.81, 1.34] | |
| 11 Perinatal mortality: timing of supplementation | 13 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 11.1 Supplementation before 20 weeks | 10 | Risk Ratio (Random, 95% CI) | 1.13 [0.96, 1.33] | |
| 11.2 Supplementation after 20 weeks | 3 | Risk Ratio (Random, 95% CI) | 0.88 [0.80, 0.97] | |
| 12 Perinatal mortality: dose of iron | 13 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 12.1 MMN with 30 mg iron vs. supplement with 60 mg iron | 6 | Risk Ratio (Random, 95% CI) | 1.19 [0.95, 1.48] | |
| 12.2 MMN with 60 mg iron vs. supplement with 60 mg iron | 3 | Risk Ratio (Random, 95% CI) | 1.08 [0.71, 1.63] | |
| 12.3 MMN with 30 mg iron vs. supplement with 30 mg iron | 4 | Risk Ratio (Random, 95% CI) | 0.92 [0.87, 0.99] |
Analysis 2.9.
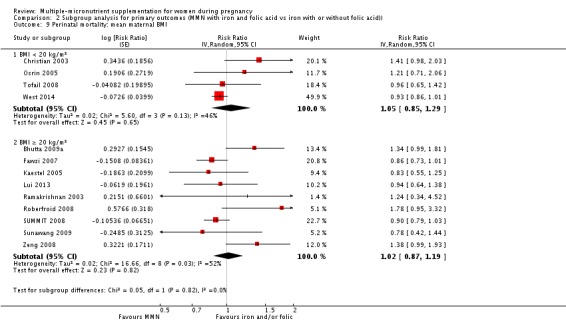
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 9 Perinatal mortality: mean maternal BMI.
Analysis 2.10.
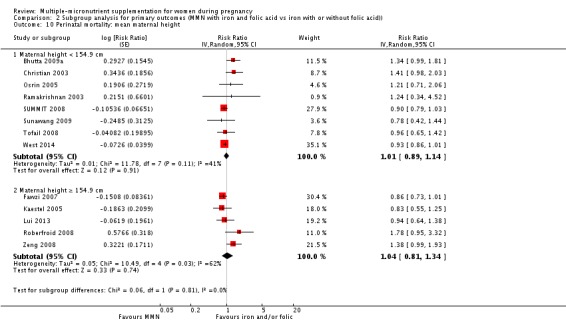
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 10 Perinatal mortality: mean maternal height.
Analysis 2.12.
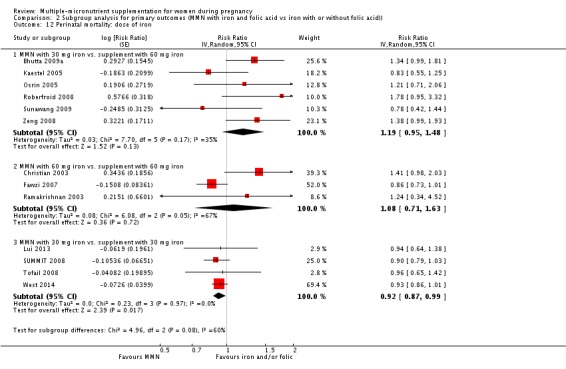
Comparison 2 Subgroup analysis for primary outcomes (MMN with iron and folic acid vs iron with or without folic acid)), Outcome 12 Perinatal mortality: dose of iron.
Comparison 3.
Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Preterm births | 10 | Risk Ratio (Random, 95% CI) | 0.97 [0.90, 1.04] | |
| 2 Small‐for‐gestational age | 8 | Risk Ratio (Random, 95% CI) | 0.91 [0.84, 1.00] | |
| 3 Low birthweight | 11 | Risk Ratio (Random, 95% CI) | 0.88 [0.85, 0.91] | |
| 4 Perinatal mortality | 10 | Risk Ratio (Random, 95% CI) | 1.04 [0.92, 1.17] | |
| 5 Stillbirths | 11 | Risk Ratio (Random, 95% CI) | 0.98 [0.88, 1.09] | |
| 6 Neonatal mortality | 11 | Risk Ratio (Random, 95% CI) | 1.06 [0.92, 1.22] | |
| 7 Maternal anaemia (third trimester Hb <110 g/L) | 3 | Risk Ratio (Random, 95% CI) | 1.01 [0.79, 1.29] | |
| 8 Miscarriage (loss before 28 weeks) | 6 | Risk Ratio (Random, 95% CI) | 0.92 [0.81, 1.05] | |
| 9 Maternal mortality | 2 | Risk Ratio (Random, 95% CI) | 1.05 [0.66, 1.64] | |
| 10 Very preterm birth (before 34 weeks of gestation) | 1 | Risk Ratio (Random, 95% CI) | 1.30 [0.67, 2.54] | |
| 11 Congenital anomalies | 1 | Risk Ratio (Random, 95% CI) | 0.99 [0.14, 7.00] | |
| 12 Neurodevelopmental outcome: BSID scores | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Mental development scores at 6 months of age: new subgroup | 1 | 770 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐6.78, 6.74] |
| 12.2 Mental development scores at 12 months of age | 1 | 744 | Mean Difference (IV, Random, 95% CI) | 1.21 [‐5.06, 7.48] |
| 12.3 Psychomotor development scores ar 6 months of age | 1 | 770 | Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐3.91, 3.59] |
| 12.4 Psychomotor development scores at 12 months of age | 1 | 744 | Mean Difference (IV, Random, 95% CI) | 0.34 [‐2.73, 3.41] |
| 13 Mode of delivery: caesarean section | 4 | Risk Ratio (Random, 95% CI) | 1.04 [0.74, 1.46] |
Analysis 3.1.
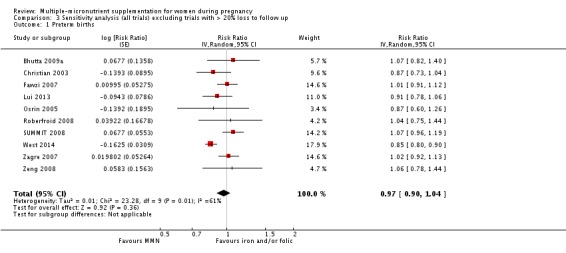
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 1 Preterm births.
Analysis 3.2.
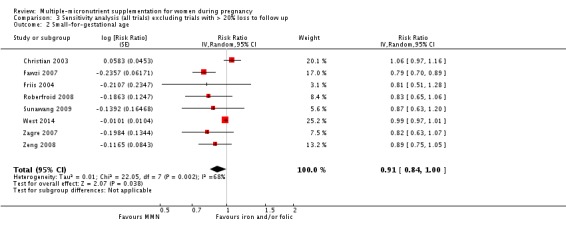
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 2 Small‐for‐gestational age.
Analysis 3.3.
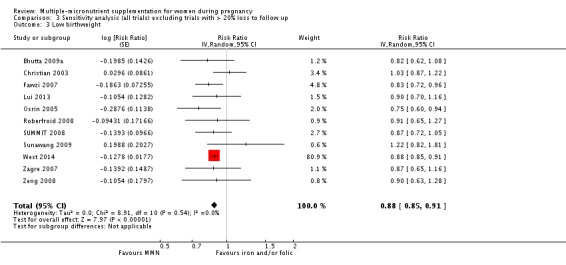
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 3 Low birthweight.
Analysis 3.4.
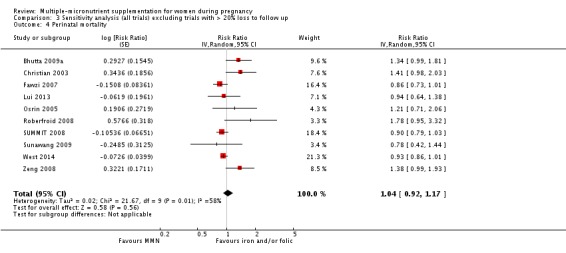
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 4 Perinatal mortality.
Analysis 3.5.
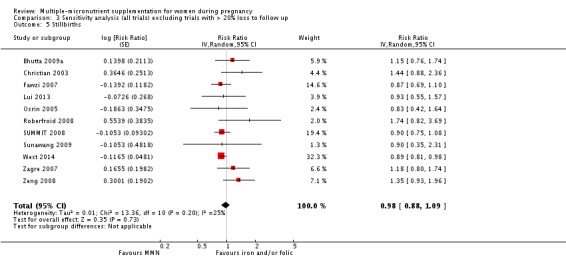
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 5 Stillbirths.
Analysis 3.6.
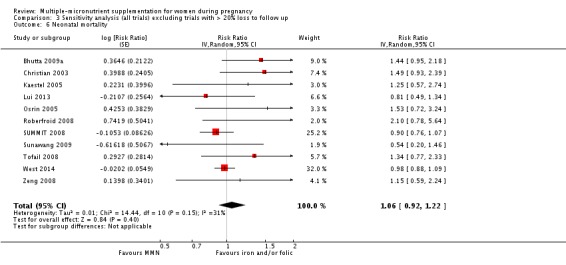
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 6 Neonatal mortality.
Analysis 3.7.
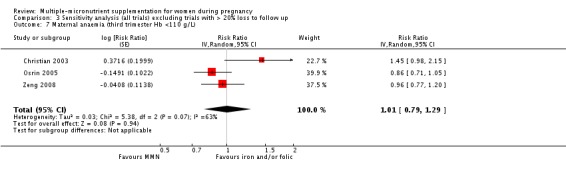
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 7 Maternal anaemia (third trimester Hb <110 g/L).
Analysis 3.8.
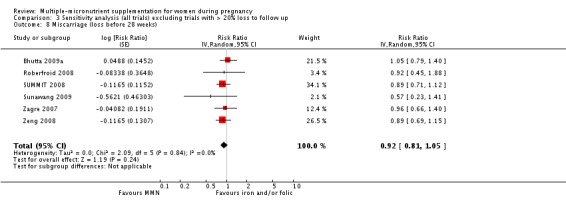
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 8 Miscarriage (loss before 28 weeks).
Analysis 3.9.
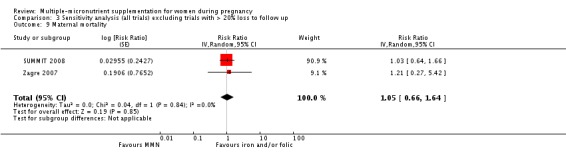
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 9 Maternal mortality.
Analysis 3.10.
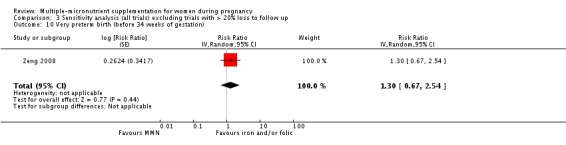
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 10 Very preterm birth (before 34 weeks of gestation).
Analysis 3.11.
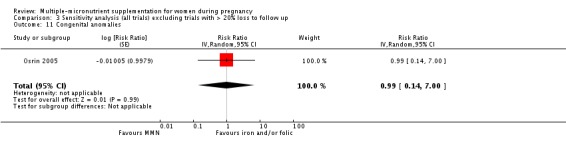
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 11 Congenital anomalies.
Analysis 3.12.
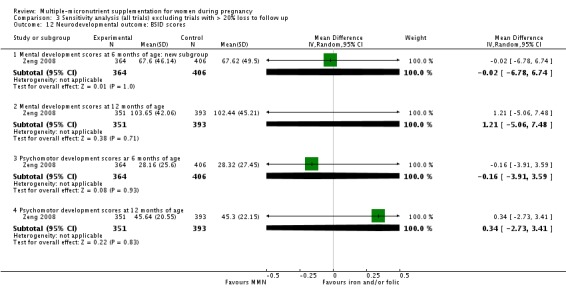
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 12 Neurodevelopmental outcome: BSID scores.
Analysis 3.13.
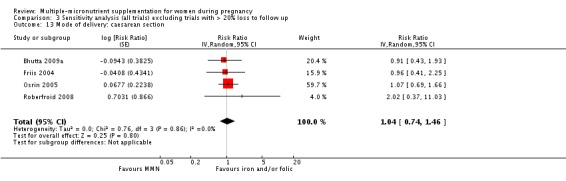
Comparison 3 Sensitivity analysis (all trials) excluding trials with > 20% loss to follow up, Outcome 13 Mode of delivery: caesarean section.
What's new
Last assessed as up‐to‐date: 11 March 2015.
| Date | Event | Description |
|---|---|---|
| 7 April 2017 | Amended | Summary of amendments: 10 November 2015 We have corrected I² values for footnotes 1 and 2 in the Table 1. 22 March 2016 We have corrected the stillbirth data for Friis 2004 and corrected the data for preterm birth, SGA, LBW, stillbirth, perinatal mortality, neonatal mortality, maternal anaemia, caesarian section, and miscarriage for Bhutta 2009a. 16 March 2017 Estimates for Christian 2003 trial were updated. In response to feedback received from Professor Caroline Fall, all analyses have now been changed to random‐effects models, given the clinical heterogeneity amongst the included trials. The Unit of Analysis section has been updated to describe the inclusion of data from trials with more than two intervention groups. All feedback has been incorporated and addressed. |
| 7 April 2017 | New citation required but conclusions have not changed | There have been a number of cumulative amendments since the last published version in 2015. The overall conclusions remain unchanged. |
History
Protocol first published: Issue 3, 2004 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 22 March 2016 | Amended | We have corrected the stillbirth data for Friis 2004 and corrected the data for preterm birth, SGA, LBW, stillbirth, perinatal mortality, neonatal mortality, maternal anaemia, caesarian section, and miscarriage for Bhutta 2009a. |
| 10 November 2015 | Amended | We have corrected I² values for footnotes 1 and 2 in the Table 1. |
| 11 March 2015 | New search has been performed | Search updated and two new trials included (Lui 2013 and West 2014) and 51 new studies excluded. Six trials included in previous versions of the review have now been excluded: four trials assessed the effect of fortification with multiple micronutrients (MMN) (Dieckmann 1944; Jarvenpaa 2007; Tatala 2002; Vadillo‐Ortega 2011) and two trials included high‐risk women (Gupta 2007; Rumiris 2006). A 'Summary of findings' table has been added. Two new outcomes, mode of delivery and macrosomia, have been added to the review. The list of primary outcomes has been modified. |
| 11 March 2015 | New citation required and conclusions have changed | It is now explicit that the review focuses on oral supplements and trials examining parenteral provision of multiple micronutrients (MMN) or MMN via food fortification are now not included. The updated review includes 19 studies. There is now evidence to suggest that women who receive MMN are at lower risk of having a stillbirth. |
| 17 February 2012 | New search has been performed | Search updated. For this update we have added 17 new included studies (Bhutta 2009a; Brough 2010; Fawzi 2007; Gupta 2007a; Hininger 2004; Jarvenpaa 2007; Kaestel 2005; Roberfroid 2008; Rumiris 2006a; Sood 1975; SUMMIT 2008; Sunawang 2009; Theobald 1937; Tofail 2008; Vadillo‐Ortega 2011; Zagre 2007; Zeng 2008) and 15 new excluded studies. We have also identified six ongoing studies (Biggs 2011; Cogswell 2006a; Dewey 2011; Fall 2007a; Moore 2011; West 2011a). This review is now comprised of 23 included studies; 64 excluded studies and six ongoing studies. The methods have been updated. Conclusions have not changed. |
| 17 February 2012 | New citation required but conclusions have not changed | Review updated. Conclusions not changed. |
| 20 September 2008 | Amended | Converted to new review format. |
Differences between protocol and review
The methods have been updated to reflect the latest Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The prespecified subgroup analysis 'duration of treatment' has been merged with another prespecified subgroup analysis 'gestational age at which supplementation was started' because it uses the same information. We also deleted a subgroup 'micronutrient interactions'.
Two new secondary outcomes have been included; these are macrosomia and mode of delivery. The list of primary outcomes has been modified so that it now includes some outcomes that were earlier included as secondary outcomes. The changes to the primary and secondary outcomes have been made to address issues identified in the recent literature, by experts in the field and given their importance from the policy perspective.
It is now explicit that the review focuses on oral supplements and trials examining parenteral provision of multiple micronutrients (MMN) or MMN via food fortification are now not included.
A 'Summary of findings' table has been added.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | This cluster‐randomised trial was conducted in urban and rural areas in Pakistan. | |
| Participants | Pregnant women with gestational age < 16 weeks were eligible for enrolment. MMN group (n = 1148), iron folic acid group (n = 1230). | |
| Interventions | MMN group received vitamin A 800 mcg, D 200 IU, E 10 mg, C 70 mg, B1 1.4 mg, B2 1.4 mg, niacin 18 mg, B6 1.9 mg, B12 2.6 mg, folic acid 400 mcg, iron 30 mg, zinc 15 mg, copper 2 mg, selenium 65 mcg and iodine 150 mcg. Iron folic acid group received 60 mg iron and 400 mcg folic acid. |
|
| Outcomes | Size at birth, gestational age at birth, perinatal mortality, maternal anaemia (Hb < 11 g/ dl), mode of delivery (caesarean section). It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | MMN and MMN + nutritional education groups were compared with iron folic acid and iron folic acid + nutritional education group. Iron folic acid given to all participants. Maternal malnutrition, vitamin A deficiency, anaemia and iron deficiency were common. 2 methods of community outreach were implemented that is, basic nutrition along with antenatal care messages and quarterly community‐based group sessions conducted by CHWs and social scientist. There was no significant difference in baseline characteristics between 2 groups. Data for caesarean section were presented (intervention 18/743; control 22/832). It was not included in the analysis as this was a cluster RCT. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a cluster‐based allocation strategy of supplements (either IF or MMN supplementation) by respective CHWs was implemented". Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Comment: "allocated to either the IF or MMN supplements according to their respective location and allocation by the AKU Pharmacy". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition (15.8%) and exclusion (around 1%) along with their reasons were reported. Attrition and exclusions were balanced across the treatment arms. |
| Selective reporting (reporting bias) | Low risk | Comment: results of all outcomes mentioned in methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Both tablets were identical in colour, shape and packaging" and "field staff (medical officers, CHWs, social scientists and data collection team) remained completely blinded as to the supplements allocation. All pregnant women were allocated a unique code and allocated a uniquely labelled and numerically coded specific supplement supply". Comment: participants and caregivers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Both tablets were identical in colour, shape and packaging" and "field staff (medical officers, CHWs, social scientists and data collection team) remained completely blinded as to the supplements allocation". Comment: outcome assessors were probably blinded to the treatment assignment. |
| Methods | This randomised trial was conducted in a socially deprived, multi‐ethnic population in east London, United Kingdom. | |
| Participants | Participants included women aged 16 years or older with a singleton pregnancy. Exclusion criteria included a gestation of greater than 13 weeks of gestation, chronic disease or use of micronutrient supplements (excluding folic acid and iron). MMN group n = 207 and placebo n = 195. | |
| Interventions | Participants were randomised to receive either MMN supplements, known as Pregnacare, or a placebo comprising starch with an iron oxide coating. MMN supplement contained beta‐carotene 3 mg, thiamin (as thiamin mononitrate, 3·6 mg) 3 mg, riboflavin 2 mg, niacin (as nicotinamide) 20 mg, vitamin B6 (as pyridoxine HCl) 10mg, vitamin B12 (as cyanocobalamin) 6 mcg, folic acid 400 mcg, vitamin C (as ascorbic acid, 73 mg) 70 mg, vitamin D (as cholecalciferol, 200 IU) 5 mcg, vitamin E (as D‐a‐tocopheryl acid succinate, 21 mg) 20 mg, vitamin K 70 mcg, Fe (as ferrous fumarate, 63·3 mg) 20 mg, zinc (as zinc sulphate H2O, 41 mg) 15 mg, Mg (as magnesium hydroxide, 372 mg) 150 mg, Iodine (as potassium iodide, 183 mg) 140 mcg and copper (as copper sulphate H2O, 2·8 mg) 1 mg. | |
| Outcomes | Birthweight, preterm birth, SGA, head circumference, Hb. | |
| Notes | Women not using folic acid were also given 400 mcg folic acid to take daily until 12 weeks of gestation. There were no significant differences in age, height, weight, BMI or parity regarding treatment group allocation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "a randomised, double‐blind, placebo‐controlled trial" and "Participants were randomised to receive either multiple‐micronutrient supplements, known as Pregnacare, or a visually identical placebo". Comment: insufficient information about the sequence generation process to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "a randomised, double‐blind, placebo‐controlled trial". Comment: insufficient information to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusion (8.7%) and attrition (12.2%) was reported along with their reasons. |
| Selective reporting (reporting bias) | Low risk | Comment: results of all outcomes mentioned in methods were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Participants were randomised to receive either multiple micronutrient supplements, known as Pregnacare, or visually identical placebo comprising starch with an iron oxide coating. All tablets were provided by Vitabiotics (London, UK) and packaged to allow double blinding. Only Vitabiotics knew the code and it was not broken until statistical analysis had been completed". Comment: participants and caregivers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All tablets were provided by Vitabiotics (London, UK) and packaged to allow double blinding. Only Vitabiotics knew the code and it was not broken until statistical analysis had been completed". Comment: outcome assessors were probably blinded to the treatment assignment. |
| Methods | This was a double‐blind cluster‐randomised trial, carried out in rural Nepal from December 1998 to April 2001. | |
| Participants | A total of 4926 pregnant women were enrolled in the study. The women were randomised into 5 groups as follows: group 1 (n = 941), group 2 (n = 957), group 3 (n = 999), group 4 (n = 1050) and group 5 (n = 1051). Women who were currently pregnant or those who were breastfeeding an infant less than 9 months old were excluded from the study. Also excluded were menopausal, sterilised or widowed women. | |
| Interventions | Group 1 received folic acid 400 mcg and vitamin A. Group 2 received folic acid 400 mcg, iron 60 mg as ferrous fumerate and vitamin A. Group 3 contained the same minerals as group 2 in addition to 30 mg of zinc as zinc sulphate. Group 4 received similar micronutrients as group 3 in addition to vitamin D 10 mcg, vitamin E 10 mg, vitamin B1 1.6 mg, vitamin B2 1.8 mg, niacin 20 mg, vitamin B6 2.2 mg, vitamin B12 2.6 mcg, vitamin C 100 mg, vitamin K 65 mcg, copper 2 mg and magnesium 100 mg. Group 5 (control group) received 1000 mcg of vitamin A only. All supplements were given orally from the time of pregnancy detection until 12 weeks after a live birth or 5 weeks after a still birth or a miscarriage. |
|
| Outcomes | Preterm births, SGA (weight < 10 percentile of gestational age), LBW (< 2500 g), side‐effects, fetal loss, perinatal mortality, neonatal mortality, 3‐month infant mortality. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | All women were offered 2, 400 mg single dose albendazole in the second and third trimester of pregnancy because of the high prevalence of hookworm infestation in this population. Hookworm infestation and vitamin A deficiency are one of the major causes of anaemia in this population. Due to this reason, vitamin A was given to all the participants including the control group. Baseline characteristics did not differ significantly among the various randomisation groups except for ethnicity and land holding. In this review, we used the group 4 data for the MMN group and group 2 data for the control group. All the estimates were adjusted for the cluster design and provided by the authors. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was done in blocks of five within each village development community by the senior study investigators, who drew numbered chips from a hat". Comment: probably done. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization was done in blocks of five within each village development community by the senior study investigators, who drew numbered chips from a hat". Comment: insufficient information to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusion (1.43%) and attrition (6.9%) was reported along with their reasons. |
| Selective reporting (reporting bias) | Low risk | Comment: results of all outcomes mentioned in methods were presented in the various publications of this trial. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "participants, investigators, field staff and statisticians did not know supplement codes", "supplements, which were of identical shape, size, and color" and "code allocation was kept locked at the Johns Hopkins University, Baltimore". Comment: participants and caregivers were blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "participants, investigators, field staff and statisticians did not know supplement codes". Comment: outcome assessors were blinded to the treatment assignment. |
| Methods | This was a double‐blind trial in Dar es Salam, Tanzania. Pregnant women who attended antenatal clinics between August 2001 and July 2004 were included. | |
| Participants | Pregnant women who attended antenatal clinics, had a negative test for HIV infection, planned to stay in the city until delivery and for 1 year thereafter with gestational age between 12 and 27 weeks according to LMP were included. The study groups were similar with respect to baseline characteristics. | |
| Interventions | Intervention group (n = 4214) received vitamin B1 20 mg, B2 20 mg, B6 25 mg, B12 50 μg, C 500 mg, E 30 mg niacin 100 mg, folic acid 0.8 mg. Control group (n = 4214) received placebo. Women were randomly assigned to receive either MM or control from the time of enrolment until 6 weeks after delivery. | |
| Outcomes | LBW (< 2500 g), preterm delivery (< 37 weeks of gestation), very LBW (< 2000 g), extremely preterm delivery (< 34 weeks of gestation), SGA (< 10th percentile for gestational age), fetal death, death in first 6 weeks, length, head circumference, placental weight, risk of caesarean section, maternal mortality, haematological status (Hb < 11 g/dL and < 8.5 g/dL, immune status (CD4 count < 775 per cubic mm, CD8 count < 480 per cubic mm and CD3 count < 1350 per cubic mm). | |
| Notes | All women irrespective of group received iron 60 mg and folic acid 0.25 mg. Malaria prophylaxis (sulphadoxine‐pyrimethamine tablets) at 20 and 30 weeks of gestation was given to all. The study groups were similar with respect to baseline characteristics. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A list was prepared according to a randomization sequence in blocks of 20; at enrolment, each eligible women was assigned to the next numbered bottle" and computerised random number generator was used (personal communication). Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "Each eligible women was assigned to the next numbered bottle". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusion (0.5%) and attrition (5.4%) were reported with reasons in each arm. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Active tablets and placebo were similar in shape, size and color and were packaged in identical coded bottles" and "Each eligible women was assigned to the next numbered bottle". Comment: participants and caregivers were blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "research assistants who assessed the study outcome were unaware of the intervention group". Comment: outcome assessors were blinded. |
| Methods | This trial was carried out in Zimbabwe in 1996‐1997. | |
| Participants | Pregnant women who were between 22 and 36 weeks of gestation were eligible for enrolment. Participants 1669 were randomised into 2 groups, MMN group n = 837 and placebo n = 832. Out of the 1106 women that were followed, 725 were HIV+ve and 360 were HIV‐ve. | |
| Interventions | MMN group received daily supplementation of vitamin A 3000 mcg RE, beta carotene 3.5 mg, thiamine 1.5 mg, riboflavin 1.6 mg, B6 2.2 mg, B12 4 mcg, niacin 17 mg, C 80 mg, D 10 mcg, E 10 mg, zinc 15 mg, copper 1.2 mcg and selenium 65 mcg while the other group received a placebo. An iron folic acid supplement was given separately as part of the routine antenatal care and was not part of the MMN tablet. Tablets were given from the day of enrolment until delivery. | |
| Outcomes | Gestational age, birthweight, birth length, head circumference, preterm delivery (< 37 weeks of gestation), LBW (< 2500 g), IUGR‐LBW (> 37 weeks' gestational age and < 2500 g birthweight). It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Study intervention was approximately the RDA for pregnant or lactating women, except for vitamin A for which a higher amount was given. Out of 1106 women who were followed, 725 were HIV‐ve whereas 360 were HIV+ve and HIV status of 21 was indeterminate. We have used data of HIV‐ve women only in this review. The intervention and the placebo groups were comparable at baseline except for the higher proportion of primigravida in the placebo group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Allocation to daily supplementation with multimicronutrient or identical‐looking placebo tablets was based on simple blocked randomization. The digits 0–5 in a computer‐generated random sequence were replaced by 6 preassigned permuted blocks of 4: AABB, ABAB, ABBA, BABA, BBAA, and BAAB; the digits 6–9 were deleted". Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "Containers with 110 multimicronutrient or placebo tablets, which were coded A or B, respectively, were delivered by the manufacturer together with the code in 2 sealed envelopes. Duplicate containers, which corresponded to the random sequence, were consecutively numbered from 1 to 1800. The study participants were numbered consecutively at recruitment". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was > 20% and reasons for it were reported. Exclusions were not reported in the study. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "double blind", "multimicronutrient or identical‐looking placebo tablets". Comment: study participants and care providers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "double blind", "multimicronutrient or identical‐looking placebo tablets". Comment: investigators were probably blinded to the treatment assignment. |
| Methods | A double‐blind, randomised placebo‐controlled trial. The study was conducted at Obstetric Departments of Grenoble and Lyon Hospitals in France. | |
| Participants | A total of 100 apparently healthy women receiving prenatal care between 12 and 16 weeks of gestation were enrolled. | |
| Interventions | The intervention group received a MMN supplement and the control group received a placebo. The MMN supplement contained vitamin C (60 mg), b‐carotene (4.8 mg), vitamin E (10 mg), thiamin (1.4 mg), riboflavin (1.6 mg), niacin (15 mg), pantothenic acid (6 mg), folic acid (200 mg), cobalamin (1 mg), Zn (15mg as citrate), Mg (87.5 mg as glycerophosphate), Ca (100 mg as carbonate). The supplement was given for an average of 14 ± 2 weeks of gestation till delivery. | |
| Outcomes | Effect of MMN supplementation on maternal blood vitamin concentrations, mineral and trace element concentrations and oxidative stress indexes concentrations. Maternal weight gain, gestational age of baby at birth, birthweight and head circumference were also assessed. | |
| Notes | The MMN supplement was iron‐free, due to its oxidative potential effect. Baseline characteristics and vitamin mineral status of the enrolled participants were comparable in both groups. Outcomes measured were presented in a format that precluded its inclusion in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Pregnant women were randomly assigned" and "randomized, placebo‐controlled trial". Comment: method used to generate the randomisation sequence is not described in sufficient detail to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information to permit judgment. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Reasons for attrition (35%) were not described in the study. There were no exclusions reported. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes in the methods section were presented in the paper. |
| Other bias | Low risk | comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The subjects, the hospital staff and the investigators were blinded to the coding scheme until analyses of the data were completed". Comment: participants and caregivers were blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The subjects, the hospital staff and the investigators were blinded to the coding scheme until analyses of the data were completed". Comment: outcome assessors were blinded to the treatment assignment. |
| Methods | This study was conducted in Guinea‐Bissau. | |
| Participants | Pregnant women with less than 37 weeks of gestation were eligible for enrolment. A total of 2100 women were randomised into 3 groups, MMN RDA group, MMN 2 RDA group and 60 mg iron 400 mcg folic acid group. | |
| Interventions | 15 micronutrients were included in the supplement at RDA level, except for folic acid that was included at 400 mcg level. Supplement consisted of vitamin A 800 mcg, D 200 IU, E 10 mg, C 70 mg, B1 1.4 mg, B2 1.4 mg, niacin 18 mg, B6 1.9 mg, B12 2.6 mg, folic acid 400 mcg, iron 30 mg, zinc 15 mg, copper 2 mg, selenium 65 mcg and iodine 150 mcg. Intervention group (n = 1392) received MMN supplements (supplement RDA n = 695, supplement 2 RDA n = 697) while the other group received folic acid 400 mcg and iron 60 mg n = 708. | |
| Outcomes | Size at birth, gestational age at birth, preterm birth (< 37 weeks of gestation), LBW (< 2500 g), miscarriage (fetal loss before 28 completed weeks of gestation), perinatal mortality (fetal loss between 28 weeks of gestation and first 7 days of life), neonatal mortality (deaths within the first 28 days of life), maternal Hb, anaemia (Hb < 100 g/L) and maternal death (death during pregnancy or within 42 days after termination of pregnancy), childhood mortality. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Malaria is endemic but HIV prevalence is relatively low. Iron folic acid given to all participants. There was no significant difference in baseline characteristics between randomisation groups. We used the 1 RDA and control groups in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Simple block randomisation with a block size of 150 was managed as follows: at entry, the project midwife randomly drew 1 piece of coloured paper corresponding to the colour code on the tablet containers from envelopes with initially 50 pieces of each of the three colours". Comment: probably done. |
| Allocation concealment (selection bias) | High risk | Quote: "at entry, the project midwife randomly drew one piece of coloured paper corresponding to the colour code on the tablet containers from envelopes with initially 50 pieces of each of the three colours". Comment: probably not done. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Exclusion (3.1%) and attrition (20.4%) data was reported along with their reasons. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "three identical‐looking micronutrient supplements", "code was kept secret from study participants, study personnel, and data analysts until data cleaning and preliminary data analysis had been carried out." and "the health workers who collected outcome data after delivery did not have any knowledge of intervention group of the women". Comment: participants and caregivers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "three identical‐looking micronutrient supplements", "code was kept secret from study participants, study personnel, and data analysts until data cleaning and preliminary data analysis had been carried out." and "the health workers who collected outcome data after delivery did not have any knowledge of intervention group of the women". Comment: outcome assessors were probably blinded to the treatment assignment. |
| Methods | This was a double ‐blind randomised controlled trial conducted in five rural counties in Hebei Provinve, China. Women were enrolled from May 2006 to April 2009. |
|
| Participants | Pregnant women who recorded dates of their menstruation for 2 or more months before they became pregnant, were nulliparous, at least 20 years old, not more than 20 weeks' gestation, legally competent, had not consumed micronutrient supplements other than folic acid in the prior 6 months, had a Hb level greater than 10.0 g/dL, resided in and received prenatal care in 1 of 5 counties, and consented to participate were eligible. 18,775 pregnant women with singleton pregnancies were randomised to group A (n = 6261), group B (n = 6252), and group C (n = 6262). | |
| Interventions | The study has 3 arms. Group A received folic acid 400 μg, group B received folic acid 400 μg and iron 30 mg, and group C received the UNICEF formulation containing folic acid 400 μg, Fe 30 mg, vitamin A 800 μg, E 10 mg, D 5 mcg, C 70 mg, B1 1.4 mg, B2 1.4 mg, B6 1.9 mg, B12 2.6 μg, niacin 18 mg, Zn 15 mg, Cu 2 mg, iodine 150 μg, selenium 65 μg. Supplements were take from enrolment until delivery. | |
| Outcomes | Perinatal mortality, neonatal mortality, infant mortality, maternal Hb and anaemia at 24 to 28 weeks of gestation, gestational age at birth, preterm birth, LBW, birthweight, low weight for height, low weight for age, low height for age, infant anaemia, gastrointestinal side‐effects (nausea, vomiting, or other mild gastrointestinal discomfort) at monthly visits. | |
| Notes | There were no significant differences at baseline between the groups Data for side‐effects: 6% (n = 355) in the MMN group while 3.6% (n = 212) in the iron folic acid group. We used the estimates for the comparison of MMN vs. IFA groups in this review. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A statistician external to the study randomly assigned ten 4‐digit lot numbers to each of the 3 supplement types (masked to the formulation and allocation) and generated the assignment list for each county proportional to the expected number of participants; within each county and block, lot numbers were randomly assigned using RANUNI in SAS statistics software (SAS Institute Inc)". Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: " A statistician external to the study randomly assigned ten 4‐digit lot numbers to each of the 3 supplement types (masked to the formulation and allocation)". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate (6.2%) was less than 20% and reasons for attrition and exclusions were provided. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned were reported. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Aside from a pharmaceutical engineer who ensured allocation of lot numbers to the correct supplement formulations, all others (i.e., participants, local physicians, study personnel, and investigators) were masked to the identity of the supplements". Comment: probably done. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Treatment codes were broken after completion of the study and main analyses.", " double blind". Comment: probably done. |
| Methods | This study was undertaken in Nepal. All women attending a designated antenatal clinic at Janakpur zonal hospital were considered for enrolment. | |
| Participants | Women were eligible for enrolment if an ultrasound examination confirmed a singleton pregnancy, a gestational age between 12 to 20 completed weeks, no notable fetal abnormality, no existing maternal illness of a severity that could compromise the outcome of pregnancy; and the participant lived in an area of Dhanusha or the adjoining district of Mohattari accessible for home visits. Participants received supplements throughout pregnancy until delivery. | |
| Interventions | The MMN group (n = 600) received tablets containing vitamin A 800 mcg, vitamin E 10 mg, vitamin D 5 mcg, B1 1.4 mg, B2 1.4 mg, niacin 18 mg, B6 1.9 mg, B12 2.6 mcg, folic acid 400 mcg, vitamin C 70 mg, iron 30 mg, zinc 15 mg, copper 2 mg, selenium 65 mcg, and iodine 150 mcg. Control group (n = 600) received tablets containing iron 60 mg and folic acid 400 mcg. There were 2 prespecified deviations from the protocol: if a participant's enrolment blood Hb concentration was less than 70 g/L, she was given an extra 60 mg of iron daily, anthelmintic treatment, and her Hb was rechecked after 1 month; and if a participant described night blindness at any time, she was given 2000 ug of vitamin A daily and referred for medical follow up. | |
| Outcomes | Birthweight, LBW (< 2500 g), gestational duration, preterm delivery (< 37 weeks of gestation), miscarriage, stillbirth, early and late neonatal death, infant length, head circumference. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Infants were followed up to 3 months. Both groups of participants were comparable at baseline. There is a discrepancy in the number of neonatal deaths reported. Figure: 'Study profile' in the Devakumar 2014 Lancet publication (p e655) reports 12 neonatal deaths in the control group and Osrin 2005 reports 11 neonatal deaths in the control group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomly allocated 1200 participant identification numbers by computer into two groups in permuted blocks of 50". Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "We did randomisation in advance of recruitment", "The allocation code was kept on file in Kathmandu and London. We allocated every identification number a supplement container to last throughout the trial. Containers were filled with either intervention or control tablets in Kathmandu by a team member who was otherwise uninvolved in the trial; these containers were then marked only with identification numbers and transported to the study centre in Janakpur" and "After screening, consent, and enrolment, one of us (YS) allocated participants sequential identification numbers and the corresponding supplement containers". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was 5% and reasons for it were reported. Exclusion was 39.5% and reasons were not reported. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The allocation code was kept on file in Kathmandu and London" and "Containers were filled with either intervention or control tablets in Kathmandu by a team member who was otherwise uninvolved in the trial; these containers were then marked only with identification numbers and transported to the study centre in Janakpur. Intervention and control supplements were manufactured to look, smell, and taste identical". Comment: participants and caregivers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The allocation code was kept on file in Kathmandu and London" and "Containers were filled with either intervention or control tablets in Kathmandu by a team member who was otherwise uninvolved in the trial; these containers were then marked only with identification numbers and transported to the study centre in Janakpur. Intervention and control supplements were manufactured to look, smell, and taste identical". Comment: outcome assessors were probably blinded to the treatment assignment. |
| Methods | This randomised controlled trial was carried out during 1997‐2000 in Mexico. | |
| Participants | Pregnant women who were less than 13 weeks' pregnant, were not receiving MMN supplementation and who agreed to participate were included in the study. A total of 873 women were randomised into the MMN group (n = 435, mean age 23.09 ± 5.48) and the iron only group (n = 438, mean age 23.00 ± 5.08). | |
| Interventions | MMN tablets included the following vitamins and minerals: iron 60 mg as ferrous sulphate, folic acid 215 mcg, vitamin A 2150 IU, vitamin D3 309 IU, vitamin E 5.73 IU, thiamin 0.93 mg, riboflavin 1.87 mg, niacin 15.5 mg, vitamin B6 1.94 mg, vitamin B12 2.04 mcg, vitamin C 66.5 mg, zinc 12.9 mg, magnesium 252 mg. The controls were given iron only tablets with 60 mg of iron as iron sulphate. All were given orally, from recruitment 6 days a week until delivery. | |
| Outcomes | Preterm births (< 37 weeks of gestation), SGA (below the 10th percentile for birthweight‐for‐gestational age), LBW (< 2500 g), perinatal mortality, mean Hb concentration, mean serum ferritin. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Data on birth outcomes were only available for 656 pregnancies (MMN group n = 328 and control group, iron only n = 326). The 2 groups did not differ significantly in most of the characteristics at recruitment, except for marital status (more single mothers in MMN supplementation group) and mean BMI (significantly lower in the MMN supplementation group). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was carried out by using 4 color‐coded groups (2 per treatment) that were assigned a priori with the use of a computer‐generated list". Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "Four colors were used to ensure masking and were assigned at random before the study began to a list of serial numbers from 1 to 1000" and "pregnant women were allocated to the pre‐assigned color code as they were added to this list at the time of recruitment". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Exclusion was 5.2% but reasons for it were not reported. Attrition (26.2%) along with their reasons were reported. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the various publications of this trial. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All study personnel and investigators were blinded to the group assignment, the details of which were kept at Emory University and the INSP in sealed envelopes that were opened only after preliminary data analysis was completed". Comment: participants and caregivers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All study personnel and investigators were blinded to the group assignment, the details of which were kept at Emory University and the INSP in sealed envelopes that were opened only after preliminary data analysis was completed". Comment: outcome assessors were probably blinded to the treatment assignment. |
| Methods | This was a factorial, double‐blind, randomised controlled trial from March 2004 to October 2006 in the Hounde health district of Burkina Faso. | |
| Participants | Pregnant women irrespective of gestational age. Exclusion criterion was if women planned to leave area within 2 years. | |
| Interventions | Intervention group (n = 714) received vitamin A 800 mcg, D 200 IU, E 10 mg, B1 1.4 mg, B2 1.4 mg, niacin 18 mg, folic acid 400 mg, B6 1.9 mg, B12 2.6 mcg, C 70 mg, zinc 15 mg, iron 30 mg, copper 2 mg, selenium 65 mcg, iodine 150 mcg. Placebo group (n = 712) received folic acid 400 mcg and iron 60 mg. | |
| Outcomes | Stillbirths (fetal death between 28 weeks of gestation till birth), neonatal deaths, perinatal death, gestation age, preterm births (< 37 weeks of gestation), birthweight, LBW (< 2500 g), SGA (birthweight less than 10 percentile of a reference population), LGA, birth length, Rohrer index, arm circumference, chest circumference, head circumference, Hb in cord blood, soluble serum transferrin receptor, stunting, wasting, underweight, and infant mortality during the first year of life. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Supplement intake was observed directly and were given till 3 months after delivery. Participants were also randomly assigned to receive either malaria chemoprophylaxis (300 mg cholorquine/week) or intermittent preventive treatment (1500 mg sulfadoxine and 75 mg pyrimethamine once in the second and third trimester). All participants received albendazole 400 mg during second and third trimester. Severely anaemic women received ferrous sulphate 200 mg and folic acid 0.25 mg twice daily for 3 months regardless of their allocation groups. The study groups were similar with respect to baseline characteristics except for small difference in Hb (lower in intervention group) and BMI (lower in control group). Stunting, wasting, underweight, and infant mortality during the first year of life were presented as hazard ratios and could not be included in the analysis of outcome using risk ratios. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization scheme was generated by a computer program in permuted blocks of 4". Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization numbers were sealed in opaque envelopes. At each inclusion, the consulting physician opened the next sealed envelope and transmitted the randomisation number to a pharmacist managing the allocation sequence and the packaging of drugs in Center Muraz. The pharmacist was also blinded to the intervention. Individual plastic zip bags contained 31 tablets each and were labelled with the participant’s name, address, and identification numbers only". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was 7.5% and reason for it was provided. Only 1 woman was excluded because of therapeutic abortion. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "double blind", "Intervention and control micronutrient tablets were identical in appearance" and "code was kept secret from study participants and staff until completion of preliminary data analysis" and "Pharmacist was also blinded to the intervention". Comment: participants and caregivers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "double blind", "Intervention and control micronutrient tablets were identical in appearance" and "code was kept secret from study participants and staff until completion of preliminary data analysis" and "Pharmacist was also blinded to the intervention". Comment: outcome assessors were probably blinded to the treatment assignment. |
| Methods | Trial conducted in New Dehli and Tamil Nadu, India. | |
| Participants | Pregnant women with gestational age 22 ± 2 were eligible to participate in the trial. A total of 647 pregnant women participated in the trial. Women with chronic diseases like heart diseases, tuberculosis, leprosy, chronic diarrhoea and a Hb < 5 g/100 mL were excluded from the study. | |
| Interventions | There were total of 7 study groups. 2 in the control group and 5 in the intervention group. 1 of the control groups received placebo and other received vitamin B12 and folic acid alone. 4 intervention groups received vitamin B12, folic acid and iron in a range of 30 to 240 mg. The fifth intervention group received 120 mg of iron without vitamin B12 and folate. Supplementation was given for 10‐12 weeks. | |
| Outcomes | Outcomes were improvement in maternal Hb/haematocrit, iron absorption from maternal gut, fetal birthweight, maternal and fetal Hb 3 months postpartum, hookworm infestation in mother and side‐effects of supplementation. | |
| Notes | None of the outcomes were reported in a format that allowed inclusion of the data in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "By reference to previously prepared random tables the women were allocated to one of the two streams A or B" and "within each stratum subjects were allotted to final treatment groups according to a set of random numbers". Comment: probably done. |
| Allocation concealment (selection bias) | High risk | Quote: "By reference to previously prepared random tables the women were allocated to one of the two streams A or B" and "within each stratum subjects were allotted to final treatment groups according to a, set of random numbers". Comment: probably not done. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was 30% and reasons for it were reported. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All the tablets had the same appearance and had the daily folic acid and iron dose divided into two tablets". Comment: participants, caregivers probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All the tablets had the same appearance and had the daily folic acid and iron dose divided into two tablets". Comment: outcome assessors probably blinded to the treatment assignment. |
| Methods | A double‐blind cluster‐randomised trial conducted at Lombok island of Indonesia between July 1, 2001 and April 1, 2004. | |
| Participants | Pregnant women of any gestational age assessed by physical exam and reported LMP. | |
| Interventions | MMN group (n = 15804)) received iron 30 mg, folic acid 400 mcg, vitamin A 800 mcg, D 200 IU, E 10 mg, C 70 mg, B1 1.4 mg, B6 1.9 mg, B12 2.6 mcg, zinc 15 mg, copper 2 mg, selenium 65 mcg, iodine 150 mcg and niacin 18 mg. Placebo group (n = 15,486) received iron 30 mg and folic acid 400 mcg. | |
| Outcomes | Early infant mortality (death within 12 weeks of birth), neonatal mortality (death within 28 days of birth), early neonatal mortality (death within 7 days of birth), late neonatal mortality (death between 7 and 28 days of birth), postneonatal mortality (death between 28 days and 12 weeks of birth), fetal loss, abortions (fetal loss before 28 weeks of gestation), still births (death between 28 weeks and before delivery), perinatal mortality (still birth or death within 7 days of birth), maternal mortality related to pregnancy up to 12 weeks postpartum, maternal cognition and mood, and child cognition (motor, cognitive and socioeconomic abilities) at 42 months of age. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Women in both groups received supplements throughout pregnancy until 90 days postpartum. Intervention and placebo groups were comparable in terms of baseline characteristics. Study was stopped early due to insufficient funds. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Before enrolment, midwife identification numbers were sequentially allocated to computer‐generated, randomly permuted blocks of groups numbered one to eight, stratified by community health centre or village health clinic". Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "midwives at village health centres and community health centres were assigned midwife identification numbers" and "Before enrolment, midwife identification numbers were sequentially allocated to computer‐generated, randomly permuted blocks of groups numbered one to eight, stratified by community health centre or village health clinic". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusion (25.2%) and attrition (5%) were reported along with their reasons. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Unclear risk | Study was stopped early due to insufficient funds. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All study scientists and personnel, government staff and enrolees were unaware of the allocation." and "The code to indicate which strip was IFA or MMN was known only by the manufacturing production manager and a quality control officer from UNICEF, Copenhagen, neither of whom had any connection to the study or its personnel". Comment: participants and caregivers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All study scientists and personnel, government staff and enrolees were unaware of the allocation." and "The code to indicate which strip was IFA or MMN was known only by the manufacturing production manager and a quality control officer from UNICEF, Copenhagen, neither of whom had any connection to the study or its personnel". Comment: outcome assessors were probably blinded to the treatment assignment. |
| Methods | A cluster‐randomised trial conducted in 2 subdistricts of Indramayu district of west Java province of Indonesia from May 2000 till August 2003. | |
| Participants | Pregnant women irrespective of gestational age. Women suffering from diabetes mellitus, coronary heart disease and tuberculosis were excluded. | |
| Interventions | Intervention group (n = 432) received RDA of 15 micronutrients according to the UNICEF/UNU/WHO recommended formula, including 30 mg of ferrous fumarate. Control group (n = 411) received ferrous sulphate 60 mg and folic acid 0.25 mg. | |
| Outcomes | Birthweight, birth length, head and chest circumference, Hb, serum ferritin, serum zinc, serum retinol and urinary Iodine, miscarriage, stillbirths, neonatal mortality. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Study groups were similar with respect to baseline characteristics. Supplements were given from the time of enrolment at 12‐20 weeks' gestation and continued up to 30 days postpartum. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We restructured the 157 hamlets into 160 dwelling clusters.", "these 160 clusters (and the pregnant women living within them) were randomly assigned into 4 blocks of 40 clusters each". Comment: method used for generating the randomisation sequence is not described in sufficient detail to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Comment:method used for allocation concealment is not described in sufficient detail to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusion (< 1%) and attrition (10.4%) were reported along with their reasons. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "This study had a single‐blind design, since the supplement for the treatment and control group looked different physically. However, participants residing in each cluster received the same supplement, so they were not aware that other participants from other clusters received a different supplement". Comment: study participants were blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: " This study had a single‐blind design" comment: Blinding of outcome assessors probably not done. |
| Methods | This study was conducted at St. Mary Abbots hospital, London during 1936. | |
| Participants | Pregnant women less than 24 weeks of gestation. No baseline characteristics comparison was performed. | |
| Interventions | Intervention group (n = 50) received calcium lactate 20 grains, vitamin A 11,000 IU, D 450 IU. Placebo group did not receive any intervention. | |
| Outcomes | Albuminuria + hypertension, hypertension, albuminuria, hyperemeses, oedema, headache, cramps, insomnia. | |
| Notes | There was no proof that all the patients in intervention took capsules (vitamin A and D) and tablets (calcium lactate) regularly. Outcomes included in this study were not of review interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "An equal number of blue and white beads were placed in a box. Each women accepted for the experiment was asked to draw a bead from the box. Those who drew blue beads were placed in group A while those who drew white beads were placed in group B." Comment: probably done. |
| Allocation concealment (selection bias) | High risk | Comment: probably not done. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No exclusion and attrition were reported. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "participants were divided into 2 groups, the intervention group received extra vitamins and the control did not receive any intervention". Comment: probably not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "symptoms were recorded by independent antenatal officers who had no knowledge as to which patients were receiving the additional substances". Comment: outcome assessors were blinded to the treatment assignment. |
| Methods | The study was conducted in Matlab, a rural subdistrict in the east central plain of Bangladesh from November 2001 till December 2003. | |
| Participants | Pregnant women with gestational age 6‐8 weeks, Hb greater than equal to 80 g/L and no serious disease were eligible for enrolment. | |
| Interventions | MMN group (n = 1224) received vitamin A 800 mcg, D 200 IU, E 10 mg, C 70 mg, B1 1.4 mg, B2 1.4 mg, niacin 18 mg, B6 1.9 mg, B12 2.6 mg, folic acid 400 mcg, iron 30 mg, zinc 15 mg, copper 2 mg, selenium 65 mcg and iodine 150 mcg, while the other group received folic acid and iron (60 mg iron 400 mcg folic acid n = 1265 and 30 mg iron 400 mcg folic acid n = 1248). | |
| Outcomes | Size at birth, gestational age at birth, perinatal mortality, maternal Hb at 30 weeks, birthweight, spontaneous abortions, infant mortality, motor development and behavioural development, infant micronutrient status, under 5 child mortality, blood pressure and kidney function in children, child growth outcomes, and adverse effects. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Women were divided into 2 groups, that is, early food group and usual food group. Each food group was divided into 3 subgroups of MMN and iron folic acid groups. Iron folic acid given to all participants. There was no significant difference in baseline characteristics between randomisation groups. Maternal malnutrition was prevalent. Control group with 30 mg iron is included in this review. Data for child growth outcomes presented in a manner which precluded its inclusion in the analysis. Adverse effects included nausea (MMN supplementation 154/786, 30FeFA 126/763), vomiting (MMN 91/787, 30FeFA 54/762), loose motions (MMN 19/786, 30FeFA 18/763), heartburn (MMN 86/786, 30FeFA 83/763), and constipation (MMN 219/788, 30FeFA 227/762). Other trial (Gupta 2007) measuring this outcome presents data for all side‐effects using a composite measure. Analyses for individual side‐effects will be presented once additional trials are available. Cost data are published in Shaheen 2013. Stunting data relevant to this review are presented in Kahn 2013. The data for the Fe30F group are presented in Figure 1, a line graph, and we will contact the authors to clarify the exact numbers for inclusion in the next update. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "individual randomisation was done in blocks of 12" and "After enrolment, women were randomly assigned to 6 intervention groups". Comment: method used for generating the randomisation sequence was not described in sufficient detail to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Comment: method used for allocation concealment was not described to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was (26%) reported along with their reasons. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "pills were identical in appearance, and monthly supplies were provided in identical bottles", " the mothers were unaware of their micronutrient supplement" and "double masking was practiced". Comment: study participants and caregivers were blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "pills were identical in appearance, and monthly supplies were provided in identical bottles", "the testers were unaware of children’s groups" and "double masking was practiced". Comment: outcome assessors were blinded to the treatment assignment. |
| Methods | Community‐based, cluster‐randomised, double‐blind trial to examine whether a daily antenatal and postnatal MMN supplement given to women will enhance newborn and infant survival and health and other birth outcomes in a rural setting in northwestern Bangladesh. | |
| Participants | Pregnant women, aged 12‐45 years, consenting to participate were recruited (n = 45,000). Women not interviewed for consent within 12 consecutive weeks after being ascertained as pregnant by urine testing were excluded. | |
| Interventions | Dietary supplement: MMN containing 15 micronutrients all at an RDA including: vitamin A (770 ug retinol equivalents, vitamin D (5 ug), vitamin E (15 mg), folic acid (600 ug), thiamin (1.4 mg), riboflavin (1.4 mg), niacin (18 mg), vitamin B‐12 (2.6 mg), vitamin B‐6 (1.9 mg), vitamin C (85 mg), iron (27 mg), zinc (12 mg), iodine (220 ug), copper (1000 ug), selenium (60 ug). Control supplement contained iron (27 mg) ‐ folic acid (600 ug) (providing the current standard of care during pregnancy). Mothers instructed to take 1 tablet per day, from the 1st trimester through 12 weeks postpartum. | |
| Outcomes | Infant mortality through 6 months of age, perinatal mortality, neonatal mortality, birth size (weight, length, circumferences), gestational age at birth, infant health outcomes, maternal morbidity, obstetric complications, body composition, nutritional status. Christian 2014a reports length‐for‐age Z score and stunting at 1 and 3 months in an abstract. | |
| Notes | The composition of the MMN supplement followed the UN MMN preparation, except with higher amounts as needed to meet the RDA from the Institute of Medicine. The substudy area was selected to be representative of the parent trial across a range of factors, including sociodemographic and geographic variations, which were evaluated during an earlier trial in the same area. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomized", "study area was divided into 596 sectors of comparable size that were used as units of randomization". Comment: probably done. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "cluster‐randomized", "Allocation: Randomized". Comment: insufficient information to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete information was not available as the main trial has not been published; however, attrition is reported to be < 20% (trial presentations). |
| Selective reporting (reporting bias) | Low risk | Comment: reports from the study are still being published. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "double‐masked", "Double Blind (Subject, Caregiver, Investigator, Outcomes Assessor)", "received daily supplementation, so treatment effect (still blinded due to the ongoing trial)". Comment: probably done. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "double‐masked", "Double Blind (Subject, Caregiver, Investigator, Outcomes Assessor)", "received daily supplementation, so treatment effect (still blinded due to the ongoing trial)". Comment: probably done. |
| Methods | This study was a cluster‐randomised, double‐blind controlled programmatic study in rural Niger aiming to compare MMN supplementation versus iron and folic acid. | |
| Participants | Women residing in target villages and experiencing amenorrhoea for less than 12 weeks were eligible for recruitment. All villages within the coverage of the 17 health centres of Mayahi district were included. Women with night blindness and/or signs of severe anaemia were excluded. | |
| Interventions | Micronutrient group (n = 1893) received vitamin A 800 mcg, D 200 IU, E 10 mg, C 70 mg, B1 1.4 mg, B2 1.4 mg, B3 18 mg, B6 1.9 mg, B12 2.6 mg, folic acid 400 mcg, iron 30 mg, zinc 15 mg, copper 2 mg, selenium 65 mcg, iodine 150 mcg. Control (n = 1777) received iron and folic acid. | |
| Outcomes | Birthweight and incidence of LBW, miscarriage, stillbirth, maternal mortality. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | Study participants received reproductive health services including malaria chemoprophylaxis, behavior change communication activities to increase awareness and adoption of better lifestyles (feeding and rest during pregnancy). Outreach prenatal care sessions were also conducted throughout intervention villages. Randomisation resulted in comparable groups for most baseline characteristics except for households and more preventive measures against malaria (more in MMN group) and less education and more poverty in iron/folic acid group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Villages ‐ not individuals were randomly assigned to one treatment group or the other". Comment: method used for generating the randomisation sequence was not described in sufficient detail to permit judgement. |
| Allocation concealment (selection bias) | Unclear risk | Comment: method used for allocation concealment was not described to permit judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was 18%. Reasons for attrition were reported. Exclusion data were not reported. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Because the two supplements did not look identical and may have been recognizable, a coding system was put in place by the SONIPHAR pharmaceutical company in Niger. six codes were assigned to the treatments: three for iron/folic acid and three for multimicronutrient supplements. SONIPHAR packaged the supplements in boxes with identical labelling except for the supplement code. Health workers, traditional midwives, and data collectors were informed that each supplement came in two sizes and colors, so that the code letter did not distinguish which supplement was used". Comment: participants and caregivers were probably blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Because the two supplements did not look identical and may have been recognizable, a coding system was put in place by the SONIPHAR pharmaceutical company in Niger. six codes were assigned to the treatments: three for iron/folic acid and three for multimicronutrient supplements. SONIPHAR packaged the supplements in boxes with identical labelling except for the supplement code. Health workers, traditional midwives, and data collectors were informed that each supplement came in two sizes and colors, so that the code letter did not distinguish which supplement was used". Comment: outcome assessors were probably blinded to the treatment assignment. |
| Methods | Community‐based cluster‐randomised trial conducted in 2 poor rural counties in Shaanxi province of north west China between August 2002 and January 2006. | |
| Participants | Pregnant women of less than 28 weeks' gestation between August 2002 and January 2006. Pregnancy was confirmed using last menstrual period (LMP) and urine pregnancy test. | |
| Interventions | Group A (n = 2017) received folic acid 0.4 mg. Group B (n = 1912) received iron 60 mg and folic acid 0.4 mg. Group C (n = 1899) received iron 30 mg, folic acid 0.4 mg, zinc 15 mg, copper 2 mg, selenium 0.65 mg, iodine 0.15 mg, vitamin A 0.8 mg, B1 1.4 mg, B2 1.4 mg, B6 1.9, B12 0.026 mg, D 0.05 mg, C 70 mg, E 10 mg, niacin 18 mg. | |
| Outcomes | Birthweight, LBW (< 2500 g), SGA (weight < 10 percentile for gestational age), preterm birth (< 37 weeks of gestation), very preterm birth (< 34 weeks of gestation), gestational age, birth length, head circumference, Hb, anaemia (Hb < 110 g/L in third trimester), neonatal deaths (death within 28 days of delivery), early neonatal deaths (death within 7 days of delivery), perinatal deaths (fetal death after 28 weeks of gestation plus early neonatal deaths); and mental and psychomotor development outcomes until 1 year of age by using the Bayley Scales of Infant Development, and growth outcomes (stunting, underweight, and wasting) in children in the first 30 months of life. It should be noted that the data for SGA was obtained from a separate report (Food and Nutrition Bulletin 2009) and not from the individual trial report. |
|
| Notes | For review purpose, MMN and iron folate groups are used. Intervention was administered till 6 weeks postpartum. Baseline characteristics at enrolment and both cluster and individual level baseline characteristics were balanced by treatment groups. Stunting, underweight, and wasting data presented as odds ratio and could not be included in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation schedule was generated off site with a pseudo‐random number generator in SAS". Comment: probably done. |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomisation schedule was generated off site with a pseudo‐random number generator in SAS version 6 (SAS Institute, Cary, NC). A treatment colour code was assigned to each village based on the treatment allocation schedule". Comment: probably done. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusion (4.8%) and attrition (2.3%) were reported along with their reasons. |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes mentioned in the methods section were presented in the paper. |
| Other bias | Low risk | Comment: no other bias was identified. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "double blind", "treatment colour code was assigned to each village based on the treatment allocation schedule. The treatment codes were opened only once all data had been collected and blinded analysis of the primary hypothesis was completed" and "were of identical appearance and packaged in blister packs". Comment: participants and caregivers were blinded to the treatment assignment. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "double blind", "treatment colour code was assigned to each village based on the treatment allocation schedule. The treatment codes were opened only once all data had been collected and blinded analysis of the primary hypothesis was completed". Comment: outcome assessors were blinded to the treatment assignment. |
BMI: body mass index Hb: haemoglobin HIV: human immunodeficiency virus IU: international unit IUGR: intrauterine growth retardation LBW: low birthweight LGA: large‐for‐gestational age LMP: last menstrual period mcg: microgram mg: milligram Mg: magnesium MMN: multiple micronutrient RCT: randomised controlled trial RDA: recommended daily allowance SGA: small‐for‐gestational age
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agarwal 2012 | Abstract only; similar micronutrients given for different durations. |
| Aguayo 2005 | Not a RCT. Assessing acceptability of MMN supplements by pregnant and lactating women. |
| Ahn 2006 | Comparing 2 MMN supplements. |
| An 2001 | Compares different doses of iron (35 mg vs 60 mg). |
| Arsenault 2010 | Includes HIV‐1 positive women. |
| Asemi 2014 | Single‐blind trial comparing multivitamin vs multivitamin‐mineral. Supplements differed in composition and dose. |
| Beazley 2002 | Assesses vitamin C and E supplementation only. |
| Bergmann 2006 | Assesses docosahexaenoic acid and fructo‐oligosaccharide. |
| Biswas 1984 | Cross‐over design, measuring only serum iron levels after single doses of different vitamin formulations. |
| Carrasco 1962 | Study has assessed the impact of D‐sorbitol on the absorption of MMNs in pregnant women. |
| Caulfield 1999 | Only assesses zinc supplementation. |
| Caulfield 1999a | Only assesses zinc supplementation. |
| Chames 2002 | Only assesses calcium supplementation. |
| Choudhury 2012 | Comparing micronutrient powder (home fortification) containing iron, folic acid, vitamin C and zinc vs iron folic acid tablet to study impact on anaemia during pregnancy. |
| Christian 2009 | Assesses the effectiveness of the standard of care (iron folic acid and single‐dose mebendazole) for the treatment of severe anaemia (haemoglobin < 70 g/L) along with enhanced regimens. |
| Cooper 2012 | Evaluates periconceptional MMN supplementation only (no MMNs given during pregnancy) (same as Khulan 2012). |
| Czeizel 1996 | Assesses periconceptional supplementation of 18 micronutrients against 4 micronutrients. |
| Dawson 1987 | Assesses supplementation of 14 micronutrients against 11 micronutrients. |
| Dawson 1998 | Assesses supplementation of different doses of 12 to 17 micronutrients. |
| Dieckmann 1944 | Fortification trial. |
| Fall 2007 | This is not a trial evaluating micronutrient supplementation. |
| Fawzi 1998 | Includes pregnant women who are HIV‐1 positive. |
| Feyi‐Waboso 2005 | Parenteral preparation. |
| Fleming 1986 | Only assesses iron, folate and vitamin B in different combinations. |
| Goldenberg 1995 | Only assesses zinc supplementation. |
| Gopalan 2004 | Evaluates effect of soya oil. |
| Graham 2007 | Study has looked at the impact of vitamin A fortified rice with and without iron and riboflavin supplementation in night‐blinded women. |
| Guldholt 1991 | Only assesses high‐dose vs low‐dose iron supplementation. |
| Gupta 2007 | Women with BMI < 18.5 and/or haemoglobin level of 7‐9 g/dL were included. |
| Hambidge 2014 | Protocol of a study comparing nutrition intervention (MMN fortified lipid‐based supplement) in pre‐conceptional and peri‐conceptional stage. |
| Hillman 1963 | Only assesses pyridoxine supplementation. |
| Holly 1955 | Only assesses iron and cobalt supplementation. |
| Hossain 2014 | Trial evaluates the effect of vitamin D supplementation. Both groups received iron and calcium. |
| Hunt 1983 | Only assesses zinc supplementation. |
| Hunt 1984 | Only assesses zinc supplementation. |
| Hunt 1985 | Only assesses zinc supplementation. |
| Huybregts 2009 | Assesses impact of balanced energy, protein dietary supplement. |
| Huybregts 2013 | Trial compares prenatal LNS vs MMN. Follow‐up of primary trial excluded (Huybregts 2009). |
| Iannotti 2008 | Only assesses zinc supplementation. |
| ICMR 2000 | Assesses periconceptional supplementation of folic acid containing vitamins. |
| Itam 2003 | Not a randomised trial. |
| Jarvenpaa 2007 | Fortification trial. |
| Kabir 2009 | This is the same cohort as Tofail 2008. However, all pregnant women were again randomised to breastfeeding counselling or a control (standard health message) group. Effect was evaluated on anthropometric outcomes in children. |
| Kable 2012 | Trial in women consuming alcohol during pregnancy evaluating effect of MMNs in ameliorating the impact of prenatal alcohol exposure in infants. |
| Khavari 2014 | The trial recruited HIV positive women. |
| Khulan 2012 | Evaluates periconceptional MMN supplementation only (no MMNs given during pregnancy). |
| Kubik 2004 | Original papers in Polish. Translated versions of the papers show that this study is not a randomised trial. |
| Kynast 1986 | Study presented at a conference. Abstract does not indicate that it as a randomised trial. |
| Lanou 2014 | Evaluated the effect of a lipid‐based nutrient supplement LNS. |
| Leroy 2010 | The study compares a traditional food assisted MCHN program vs a newly designed approach to prevent malnutrition in children. |
| Li 2014 | The study evaluates the effect of supplementation with folic acid and milk. |
| Lindström 2011 | Describing prevalence of micronutrient deficiencies at baseline and its determinants. |
| Ling 1996 | Evaluating the impact of traditional Chinese tonics with nutrients. |
| Lucia 2007 | Evaluating impact of docosahexaenoic acid and fructo‐oligosaccharide. |
| Ma 2008 | Evaluating retinol and riboflavin supplementation. |
| Magon 2014 | The trial evaluating the effect of use of fortified snacks during pregnancy. Both groups received the same micronutrients (i.e., iron, folic acid, beta‐ carotene, and calcium), however, the dose of micronutrients in the intervention group was higher than the control group. |
| Malvasi 2014 | Study evaluating the effect of myoinositol, d‐chiro inositol, folic acid and manganese during pregnancy on maternal blood pressure, glycaemic and cholesterol parameters. Inositol is not an essential nutrient. |
| Mardones 2007 | Impact of fortification of fortified dairy product with polyunsaturated fatty acids. |
| Marya 1987 | Only assesses calcium and vitamin D supplementation. |
| Mathan 1979 | Assesses supplementation of vitamin C and protein. |
| Menon 1962 | Not a RCT. |
| Merchant 2005 | Includes pregnant women who are HIV‐1 positive. |
| Merialdi 1999 | Only assesses zinc supplementation. |
| Muslimatun 2001a | Only assesses vitamin A supplementation. |
| Muslimatun 2001b | Evaluates vitamin A supplementation. |
| Nguyen 2012 | Protocol of a study evaluating pre‐conceptional MMN vs IFA supplements. |
| Nwagha 2010 | Micronutrients given via injection. |
| Ochoa‐Brust 2007 | Assesses impact of vitamin C only. |
| Olofin 2014 | The trial included HIV‐positive women. |
| Park 1999 | Study design does not satisfy the eligibility criteria of the review. |
| Patimah 2013 | Not a randomised trial. |
| People's League 1946 | Quasi‐randomised trial. Women were divided into 2 groups by placing them alternately on separate lists. |
| Ramirez‐Velez 2011 | Intervention group receives 9 micronutrients and control group receives 3 micronutrients. |
| Raqib 2013 | Evaluated the effect of vitamin B12 only. |
| Robertson 1991 | Only assesses zinc supplementation. |
| Rumiris 2006 | Pregnant women with superoxidedismutase (SOD) levels below 1102 U/gHb included in the study. |
| Sachdeva 1993 | Evaluated calcium supplementation. |
| Sagaonkar 2009 | Comparison of 4 micronutrients with 3. |
| Salzano 2001 | Evaluated supplementation with calcium and fatty acids (linoleic acid, mono and poly unsaturated fatty acids) vs control. |
| Schmidt 2001 | Only assesses vitamin A supplementation. |
| Schmidt 2002 | Only assesses vitamin A supplementation. |
| Semba 2000 | A trial of vitamin A supplementation in HIV‐infected women. |
| Semba 2001 | Only assesses vitamin A supplementation. |
| Suharno 1993 | Only assesses vitamin A supplementation. |
| Sun 2010 | Quasi‐randomised trial. Women were allocated to 4 groups in the order of enrolment. |
| Suprapto 2002 | Only assesses vitamin A and riboflavin supplementation. |
| Taghizadeh 2014 | Comparing 2 different MMN supplements (13 micronutrients vs 10 micronutrients). |
| Tanumihardjo 2002 | Only assesses vitamin A and iron supplementation. |
| Tatala 2002 | Fortification trial. |
| Thauvin 1992 | Not a randomised trial. |
| Vadillo‐Ortega 2011 | Fortification trial |
| Webb 2009 | Participants include HIV‐positive women. |
| Wibowo 2012 | Evaluating effect of milk fortified with different doses of minerals and vitamins. |
| Wijaya‐Erhardt 2011 | Evaluated weekly food provision (optimised diet) vs the control. |
| Wijaya‐Erhardt 2014 | Evaluated educational intervention using a pre‐post design. |
| Young 2010 | Study assessed the acceptability of a micronutrient powder (Sprinkles), a fortified food (Nutrivida), and tablets by the participants. All supplements has similar composition of micronutrients. |
| Zavaleta 2000 | Only assesses zinc supplementation. |
BMI: body mass index IFA: iron and folic acid LNS: lipid‐based nutrient supplement MMN: multiple micronutrient RCT: randomised controlled trial vs: versus
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Parallel randomised trial recruiting at 4 sites in Malawi. Setting: 1 public district hospital (Mangochi), 1 semiprivate hospital (Malindi), and 2 public health centres (Lungwena and Namwera) in Mangochi District, southern Malawi. |
| Participants | Inclusion: ultrasound‐confirmed pregnancy of no more than 20 completed gestation weeks, residence in the defined catchment area, availability during the period of the study, and signed or thumb‐printed informed consent. Exclusion: age younger than 15 years, need for frequent medical attention due to a chronic health condition, diagnosed asthma treated with regular medication, severe illness warranting hospital referral, history of allergy toward peanuts, history of anaphylaxis or serious allergic reaction to any substance, requiring emergency medical care, pregnancy complications evident at enrolment visit (moderate to severe edema, blood Hb concentration, 50 g/L, systolic blood pressure .160 mm Hg or diastolic blood pressure .100 mm Hg), earlier participation in the iLiNS‐DYAD‐M trial (during a previous pregnancy), or concurrent participation in any other clinical trial. 1391 women randomised. (IFA – 463; MMN 466; LNS – 462). Lost to follow‐up (IFA 26; MMN 32; LNS 26). Group demographic characteristics similar. |
| Interventions | Intervention: Group 1: IFA – 1 capsule containing 60 mg iron and 400 mcg folic acid and 2 doses of intermittent preventive malaria treatment with sulfadoxine‐pyrimethamine. Group 2: MMN – malaria treatment as above plus 1 capsule containing IFA and 16 micronutrients. Group 3: LNS – malaria treatment as above and sachets of SQ‐LNS containing the same micronutrients as group 2 plus 4 additional minerals, protein and fat (118 kcal). All supplements to be taken daily. Follow‐up until 6 weeks postpartum. Data collectors delivered supplements fortnightly. Participants were invited to antennal care visits at the clinic at 32 and 36 weeks and 1‐2 weeks postpartum. Participants were given mobile phones and airtime so that they could inform of deliveries outside of clinics. |
| Outcomes | Primary outcomes: birthweight and newborn length (within 6 weeks of birth). Secondary outcomes: newborn weight, head circumference, mid‐upper arm circumference (MUAC), and the duration of pregnancy, as well as the incidence of maternal or newborn SAEs. Several other maternal and infant outcomes are reported. |
| Notes | Due to testing of LNS products for a bacteria, 160 pregnant women in the LNS group missed out their supplement for 1‐20 days during August 2012. 127 of these women were provided with IFA tablets at this time, while 33 were not available for contact. Adverse events were recorded separately and monitored, and a study physician determined if the participant should continue with the allocated supplement. Analysis modified ITT = participants with missing data for an outcome were excluded from analysis of that outcome. 12 twin pregnancies were excluded from all analyses. This trial included women with a + HIV test: IFA = 15.6%; MMN 11.1% and LNS 14.4% We have contacted authors to see if separate analyses for HIV‐ women are available. Authors have agreed to provide these data for inclusion in the next update of this review. |
| Methods | Randomised controlled trial. |
| Participants | Pregnancy women 12‐14 weeks' gestation. Fetal malformation excluded. Total number randomised 560. Group denominators not stated. |
| Interventions | MMN versus iron 100 mg and folic acid 500 mcg. MMN not described. |
| Outcomes | Mean birthweight, low birthweight. |
| Notes | No usable data due to missing group denominators. Authors contacted (g_gathwala@hotmail.com) in hopes of adding data in next update. |
MMN: multiple micronutrient
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A randomised controlled trial to compare the impact on birthweight of daily iron folic acid, twice weekly iron folic acid and twice weekly multiple‐micronutrient supplementation for pregnant women in Ha Nam province, Vietnam. |
| Methods | Randomised controlled trial. Communes agreeing to participate in the study will be randomly assigned to 1 of the 3 treatment arms. The commune was chosen as the cluster unit of randomisation to reduce the likelihood of interactions between the intervention groups. All eligible women in each commune will be invited to participate in the study. The pharmaceutical manufacturer and the Chairman of the DSMC will retain the allocation code. |
| Participants | Healthy pregnant women 16 weeks' gestation or less were included. Women with complicated pregnancies (e.g. twins, diabetes, other medical conditions), or Hb ≤ 8.0 will be excluded. |
| Interventions | Study has 3 arms. Group 1 will receive elemental iron 60 mg and folic acid 1.5 mg taken orally twice weekly, group 2 will receive multiple micronutrients (modified 2xUNIMAPP) taken orally twice weekly, and group 3 will receive elemental iron 60 mg and folic acid 0.4 mg taken orally once daily. All supplements will be provided for the duration of pregnancy and 3 months postpartum. |
| Outcomes | Birthweight, maternal Hb and ferritin, infant cognitive development, infant height, Hb. |
| Starting date | September 2010. |
| Contact information | Beverley‐Ann Biggs Department of Medicine Royal Melbourne Hospital Parkville, Victoria, 3050 Australia. Tel # 61383443256 Email: babiggs@unimelbi.edu.au |
| Notes |
| Trial name or title | ILINS‐DYAD ‐ Ghana population. Protocol identifier: NCT00970866. Dewey 2011 title (abstract): Efficacy of Lipid‐Based Nutrient Supplements (LNS) for pregnant and lactating women and their Infants. |
| Methods | This study will be a community‐based, randomised controlled trial with 3 intervention groups. |
| Participants | Inclusion criteria
Exclusion criteria
|
| Interventions | 1. Dietary supplement: iron and folic acid (IFA): pregnant women will receive 1 (1) iron (60 mg) and folic acid (400 mcg) (IFA) tablet daily during pregnancy, and a tablet containing calcium (Ca) only (akin to a placebo) during lactation; there will be no supplementation for infants born to the women. The Fe/FA tablets will be taken each day with water after meals. 2. Dietary supplement: multiple micronutrient (MMN) group. Pregnant women will receive 1 (1) multiple‐micronutrient tablet daily during pregnancy and the first 6 months of lactation; there will be no supplementation for infants born to the women. The MMN tablets will be taken each day with water after meals. 3. Dietary supplement: lipid‐based nutrient supplements (LNS) group. Pregnant women will receive 20 g of LNS‐P&L daily during pregnancy and the first 6 months of lactation, whilst infants born to the women will receive 20 g of LNS‐20 g daily from 6 to 18 months of age. |
| Outcomes | Primary outcome is child length at birth, length‐for‐age Z‐score (LAZ, based on WHO 2006 growth standards) at 18 months of age. Secondary outcomes include the following. i. Maternal
ii. Child
|
| Starting date | November 2009. |
| Contact information | Kathryn G Dewey, UC Davis |
| Notes | Sample size = 864. For the 2015 update of this review, we identified 3 further reports related to the ILINS‐DYAD Ghana trial: Adu‐Afarwuah 2013, Adu‐Afarwuah 2014 and Oaks 2014. These reports are abstracts; the full report of pregnancy outcome data has not yet been published. |
| Trial name or title | Protocol identifier: NCT02190565. Supplementation with WellnessPack mama during pregnancy and lactation ‐ a randomized double‐blind, placebo‐controlled study. |
| Methods | Parallel randomised, double‐blind trial investigating food supplementation for the primary prevention of anaemia. |
| Participants | Inclusion criteria:
Exclusion criteria:
Upon miscarriage or transfer to prenatal care specialist, the participant is excluded from the study. |
| Interventions | Placebo comparator: placebo. Placebo consisting of 2 sham multivitamin and mineral tablets and 2 capsules of oil. Active comparator: food supplement. Food supplement consisting of fish oil (omega 3 fatty acids DHA and EPA) and multivitamin and mineral tablets with extra iron and folic acid. Intervention: Dietary Supplement: Food supplement. |
| Outcomes | Primary outcome: prevalence of anaemia in active and placebo groups [Time Frame: pregnancy weeks 28‐30] [Designated as safety issue: No] Blood will be analysed for Hb and ferritin values. We will compare how many women in each group (active vs placebo) are ordinated iron supplementation due to anaemia by mid‐pregnancy. Secondary outcome: Levels of nutritional biomarkers in maternal blood and breast milk [Time Frame: 6‐10 weeks after delivery] [ Designated as safety issue: No] Levels of nutritional biomarkers such as DHA and vitamin D in maternal blood and breast milk will be measured in active and placebo groups. |
| Starting date | October 2014 ‐ January 2016. |
| Contact information | Professor Angelica Lindén Hirschberg: Angelica.Hirschberg.Linden@ki.se |
| Notes | Sudy sponsor: Oriflame Cosmetics AB. Collaborators: Karonlinska Institutet. |
| Trial name or title | Investigating the effects of prenatal and infancy nutritional supplementation on infant immune development in The Gambia: The Early Nutrition and Immune Development (ENID) Trial. |
| Methods | A randomised trial to investigate the effects of prenatal and infancy nutritional supplementation on infant immune development. |
| Participants | Women (aged 18 to 45 years) resident in rural Kiang West Region, the Gambia, with pregnancy confirmed by urine test and ultrasound examination and with gestational age approximately 10‐20 weeks will be recruited. Women currently enrolled in another MRC study or current pregnancy (beyond 20 weeks on ultrasound assessment), with severe anaemia (Hb less than 7 g/dL), reported onset of menopause will be excluded. |
| Interventions | 4 pregnancy interventions, to be given daily from 12 weeks' gestation until delivery: 1. FeFol: Iron‐folate, 60 mg iron 400 µg folate, representing the usual standard of care during pregnancy, as per Gambian Government guidelines (control group). 2. MMN: multiple micronutrients. A combination of 15 micronutrients, specifically designed for use during pregnancy, and as formulated by UNICEF. A single tablet provides the recommended dietary allowance (RDA) for each micronutrient, but we will supplement women in this arm of the trial with 2 daily MMN tablets. 3. PE + FeFol: protein‐energy and iron‐folate. A food‐based supplement developed by Valid International, providing a comparable level of iron and folate to the FeFol only arm, but with the addition of energy, protein and lipids. 4. PE + MMN: protein‐energy and multiple micronutrients. A micronutrient fortified food‐based supplement also developed by Valid International, and providing comparable levels of micronutrients to the MMN arm (including FeFol), in addition to the energy and protein and lipid content. From 6 months of age, infants will further be randomised to receive either a lipid‐based nutritional supplement, with or without additional MMN, or placebo from 6 to 12 months of age. |
| Outcomes | Primary outcomes: 1. Thymic index at 1, 8, 24 and 52 weeks of age. 2. Antibody response to EPI vaccines (diphtheria, tetanus toxoid, HiB, measles). Secondary outcomes: cellular markers of immunity in a randomly selected subcohort of infants, stratified by treatment group. The secondary outcome measurements will be assessed when the infants are 12, 24 and 52 weeks of age. Subsidiary studies to the main trial will additionally assess the impact of supplementation on infant growth and development to 24 months of age. |
| Starting date | October 1, 2009. |
| Contact information | Sophie Moore MRC Keneba MRC Laboratories Fajara, Banjul Gambia PO Box 273 Email: smoore@mrc.gm |
| Notes | 800 mother‐infant pairs. |
| Trial name or title | Rang‐Din Nutrition Study. Mridha 2014 (abstract) title: Lipid‐based nutrient supplements for pregnant women reduce newborn stunting in Bangladesh. Protocol identifier: NCT01715038. Harding 2014 documents trial methods and compliance. |
| Methods | Cluster‐randomised effectiveness trial |
| Participants | 4011 pregnant women recruited. Inclusion criteria
Exclusion criteria
|
| Interventions | 1. Experimental: Comprehensive "Comprehensive" LNS: LNS‐PLW provided daily to mothers during pregnancy and postpartum lactation (a total of at least 11 months, starting by 20 weeks' gestation and ending at 6 months postpartum) and LNS developed for infants and young children (LNS‐child) provided daily to their infants (beginning at 6 months of age for a period of 18 months i.e. from 6‐24 months of age). 2. Experimental: child‐only LNS "Child‐only" LNS: daily LNS‐child supplementation of the child starting at 6 months of age and ending at 24 months of age (18 months total). Women will be provided with iron and folic acid (IFA) tablets during pregnancy and for 3 months postpartum. 3. Experimental: child‐only MNP "Child‐only" MNP: daily MNP supplementation of the child starting at 6 months of age and ending at 24 months of age (18 months total). Women will be provided with iron and folic acid (IFA) tablets during pregnancy and for 3 months postpartum. 4. Active comparator: control: IFA. Control: no additional nutrient supplementation for the child will be provided through the study, but the regular nutrition education and visits provided by the program frontline staff will continue. Women will be provided with IFA tablets during pregnancy and for 3 months postpartum. |
| Outcomes | Primary outcome measures: 1. Birthweight [Time Frame: Within 48 hours (or back calculated from later measurements).] [Designated as safety issue: No]. Birthweight of the infants (women who received LNS‐PLW vs. women who received IFA tablets). Pre‐defined tests for interaction will be done for: baseline maternal characteristics (age, height, BMI, education, primiparity, food insecurity, wealth and gestational age at enrolment), time of year when outcome was assessed and child sex. 2. Birth length [Time Frame: Within 48 hours (or back calculated from later measurements)] [Designated as safety issue: No]. Birth length of the infants (women who received LNS‐PLW vs. women who received IFA tablets). Pre‐defined tests for interaction will be done for: baseline maternal characteristics (age, height, BMI, education, primiparity, food insecurity, wealth and gestational age at enrolment), time of year when outcome was assessed and sex of child. 3. Child linear growth status at 24 months [Time Frame: 24 months] [Designated as safety issue: No]. Linear growth (the "comprehensive" LNS approach vs. the "child‐only" LNS approach vs. "child‐only" MNP) vis‐à‐vis one another and vis‐à‐vis the control group. Pre‐defined tests for interaction will be done for: baseline maternal characteristics (age, height, BMI, education, primiparity, food insecurity, wealth and gestational age at enrolment), time of year when outcome was assessed and sex of child. Secondary outcome measures: There are many additional maternal and neonatal outcomes listed on the protocol. |
| Starting date | October 2011 ‐ April 2015. |
| Contact information | Kathryn Dewey, University of California, Davis. |
| Notes | Study sponsors: University of California, Davis US Agency for International Development Family Health International 360 International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR,B) World Mission Prayer League (LAMB) FANTA |
| Trial name or title | Impact of pre‐pregnancy micronutrient supplementation on maternal and child outcomes. Protocol identifier: NCT01665378. Setting: Vietnam. |
| Methods | Parallel, double‐blind randomised trial. |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | Arms 1 and 2: experimental: multiple micronutrients. Multiple micronutrient groups receive: vitamin A (μg) 800 vitamin D (IU) 600 vitamin E (mg) 10 vitamin C (mg) 70 thiamine (mg) 1.4 riboflavin (mg) 1.4 niacin (mg) 18 vitamin B6 (mg) 1.9 vitamin B12 (μg) 2.6 folic acid (μg)* 2800 Iron (mg)* 60 zinc (mg) 15 copper (mg) 2 selenium (μg) 65 iodine (μg) 150. Arm 3 and 4: active comparator: iron and folic acid. Iron and folic acid groups receive: iron (60 mg) and folic acid (2800 μg), based on current WHO recommendations for WRA. Arm 5 and 6: placebo comparator: folic acid. Folic acid groups receive: 2800 μg FA once a week during the pre‐pregnancy period. |
| Outcomes | Primary outcomes: 1. Birth Size [Time Frame: At birth] [Designated as safety issue: No] Infants' weight, length and head circumference will be measured as early as possible within 24 hours after birth using standard procedures. All measurements will be obtained in duplicate by the same data collector. Weight‐for‐age and length‐for‐age z scores will be calculated using the 2006 WHO reference data. 2. Gestational Age [Time Frame: At birth] [Designated as safety issue: No] Gestational age will be calculated based on the date of last menstrual period. This method has been shown to be reliable in previous work and we expect precise estimates since we will be visiting women weekly from baseline during the pre‐pregnancy period and will exclude women who may be have delivered in the past 6 months. Secondary outcomes: Maternal and infant iron status. |
| Starting date | October 2011 ‐ September 2014. |
| Contact information | Dr. Usha Ramakrishnan, Emory University. |
| Notes | Sponsor: Emory University. Collaborator: MicroNutrient Initiative. |
| Trial name or title | Effect of animal‐source food supplement prior to and during pregnancy on birthweight and prematurity in rural Vietnam. |
| Methods | Cluster‐randomised trial recruiting women from 29 communes in Vietnam. |
| Participants | Women recruited when registering for marriage. |
| Interventions | I) Food supplement 5 days/week from marriage to term (˜18 months). II) Food supplement 5 days/week from 16 weeks' gestation to term (˜5 months). III) Routine prenatal care. |
| Outcomes | The primary outcome is birthweight and the secondary outcome is the prevalence of prematurity. Other outcomes include maternal micronutrient status (iron, zinc, folic acid, vitamins A and B12), the incidence of infections; infant growth and infections from 0‐6 months of age are also assessed. Maternal data and information are measured at recruitment, 16, and 34 weeks' gestation. Infant anthropometric status is measured at birth, 1, 3, and 6 months. Infant gestational age is assessed at birth to determine the prevalence of pre‐term deliveries, and the mother’s activity or physical work during pregnancy is also determined. |
| Starting date | Not stated. |
| Contact information | N. Tu, Vietnam Nutrition Association, Hanoi, Vietnam. C. King, Children's Hospital Oakland Research Institute, Oakland, CA, USA. |
| Notes |
BMI: body mass index DHA: docosahexaenoic acid EPA: eicosapentaenoic acid Hb: haemoglobin IFA: iron and folic acid ITT: intention‐to‐treat LNS: lipid‐based nutrient supplement mcg: microgram MMN: multiple micronutrient RDA: recommended daily allowance SAE: serious adverse event
Contributions of authors
Batool A Haider (BAH) and Zulfiqar A Bhutta (ZAB) undertook the current 2015 update of the 2012 Cochrane Review. BAH undertook the revised analysis with input from ZAB. Both authors approved the final version of the review.
ZAB was the principal investigator of Bhutta 2009a, and data extraction was undertaken by BAH and Arjumand Rizvi for this trial. BAH created the comparisons, did the analysis and wrote the text of the review. ZAB provided guidance and approved the review.
Sources of support
Internal sources
The Aga Khan University Hospital, Pakistan.
External sources
Department for International Development, UK.
United Nations Children's Fund (UNICEF), USA.
UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Batool A Haider: none.
Zulfiqar A Bhutta was the principal investigator of the UNIMAPP trial conducted in Pakistan (Bhutta 2009a). He was not involved in the screening and data extraction for this paper, which was conducted by other review authors acknowledged above.
Edited (no change to conclusions)
References
References to studies included in this review
- Bhutta ZA, Rizvi A, Raza F, Hotwani S, Zaidi S, Soofi S, et al. A comparative evaluation of multiple micronutrient and iron‐folate supplementation during pregnancy in Pakistan: impact on pregnancy outcomes. Food and Nutrition Bulletin 2009;30(4):S496‐S505. [DOI] [PubMed] [Google Scholar]; Persson LA, Eneroth H, Ekstrom EC. Multiple micronutrient supplementation during pregnancy: a review of effects on birth size, maternal haemoglobin and perinatal mortality demonstrated in trials in Bangladesh, Guinea‐Bissau and Pakistan. Report for UNICEF/UNU/WHO2004.
- Brough L, Rees GA, Crawford MA, Morton RH, Dorman EK. Effect of multiple‐micronutrient supplementation on maternal nutrient status, infant birth weight and gestational age at birth in a low‐income, multi‐ethnic population. British Journal of Nutrition 2010;104(3):437‐45. [DOI] [PubMed] [Google Scholar]
- Christian P, Darmstadt GL, Wu L, Khatry SK, LeClerq SC, Katz J, et al. The effect of maternal micronutrient supplementation on early neonatal morbidity in rural Nepal: a randomised, controlled, community trial. Archives of Disease in Childhood 2008;93(8):660‐4. [DOI] [PubMed] [Google Scholar]; Christian P, Jiang T, Khatry SK, LeClerq SC, Shrestha SR, West KP Jr. Antenatal supplementation with micronutrients and biochemical indicators of status and subclinical infection in rural Nepal. American Journal of Clinical Nutrition 2006;83:788‐94. [DOI] [PubMed] [Google Scholar]; Christian P, Khatry SK, Katz J, Pradhan EK, LeClerq SC, Shrestha SR, et al. Effects of alternative maternal micronutrient supplements on low birth weight in rural Nepal: double blind randomised community trial. BMJ 2003;326:571. [DOI] [PMC free article] [PubMed] [Google Scholar]; Christian P, Khatry SK, LeClerq SC, Dali SM. Effects of prenatal micronutrient supplementation on complications of labor and delivery and puerperal morbidity in rural Nepal. International Journal of Gynaecology and Obstetrics 2009;106(1):3‐7. [DOI] [PubMed] [Google Scholar]; Christian P, Murray‐Kolb LE, Khatry SK, Katz J, Schaefer BA, Cole PM, et al. Prenatal micronutrient supplementation and intellectual and motor function in early school‐aged children in Nepal. JAMA 2010;304(24):2716‐23. [DOI] [PubMed] [Google Scholar]; Christian P, Nanayakkara‐Bind A, Schulze K, Wu L, LeClerq SC, Khatry SK. Antenatal micronutrient supplementation and third trimester cortisol and erythropoietin concentrations. Maternal & Child Nutrition 2014 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]; Christian P, Shrestha J, LeClerq SC, Khatry SK, Jiang T, Wagner T, et al. Supplementation with micronutrients in addition to iron and folic acid does not further improve the hematologic status of pregnant women in rural Nepal. Journal of Nutrition 2003;133:3492‐8. [DOI] [PubMed] [Google Scholar]; Christian P, Stewart CP, LeClerq SC, Wu L, Katz J, West KP Jr, et al. Antenatal and postnatal iron supplementation and childhood mortality in rural Nepal: a prospective follow‐up in a randomized, controlled community trial. American Journal of Epidemiology 2009;170(9):1127‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]; Christian P, West KP Jr, Khatry SK, LeClerq SC, Pradhan EK, Katz J, et al. Effects of maternal micronutrient supplementation on fetal loss and infant mortality: a cluster‐randomised trial in Nepal. American Journal of Clinical Nutrition 2003;78:1194‐202. [DOI] [PubMed] [Google Scholar]; Katz J, Christian P, Dominici F, Zeger SL. Treatment effects of maternal micronutrient supplementation vary by percentiles of the birth weight distribution in rural Nepal. Journal of Nutrition 2006;136:1389‐94. [DOI] [PubMed] [Google Scholar]; Kulkarni B, Christian P, LeClerq SC, Khatry SK. Determinants of compliance to antenatal micronutrient supplementation and women's perceptions of supplement use in rural Nepal. Public Health Nutrition 2010;13(1):82‐90. [DOI] [PubMed] [Google Scholar]; Murray‐Kolb L, Bahnfleth C, Hurley K, Cole P, Khatry S, LeClerq S, et al. Micronutrient supplementation during pregnancy and the preschool years and child behavior at 7‐9 years of age. FASEB Journal 2014;28(1 Suppl):Abstract no: 619.3. [Google Scholar]; Nanayakkara‐Bind A, Schulze K, Wu L, Le SC, Khatry SK, Christian P. Effects of antenatal micronutrient supplementation on cortisol and erythropoietin in pregnant Nepalese women. FASEB Journal 2011;25:Abstract no: 779.15. [Google Scholar]; Stewart CP, Christian P, LeClerq SC, West KP Jr, Khatry SK. Antenatal supplementation with folic acid + iron + zinc improves linear growth and reduces peripheral adiposity in school‐age children in rural Nepal. American Journal of Clinical Nutrition 2009;90(1):132‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]; Stewart CP, Christian P, Schulze KJ, Arguello M, Leclerq SC, Khatry SK, et al. Low maternal vitamin B‐12 status is associated with offspring insulin resistance regardless of antenatal micronutrient supplementation in rural Nepal. Journal of Nutrition 2011;141(10):1912‐7. [DOI] [PubMed] [Google Scholar]; Stewart CP, Christian P, Schulze KJ, Leclerq SC, West KP Jr, Khatry SK. Antenatal micronutrient supplementation reduces metabolic syndrome in 6‐ to 8‐year‐old children in rural Nepal. Journal of Nutrition 2009;139(8):1575‐81. [DOI] [PubMed] [Google Scholar]
- Fawzi WW, Msamanga GI, Urassa W, Hertzmark E, Petraro P, Willett WC, et al. Vitamins and perinatal outcomes among HIV‐negative women in Tanzania. New England Journal of Medicine 2007;356(14):1423‐31. [DOI] [PubMed] [Google Scholar]
- Friis H, Gomo E, Nyazema N, Ndhlovu P, Krarup H, Kaestel P, et al. Effect of micronutrient supplementation on gestational length and birth size: a randomized, placebo‐controlled, double‐blind effectiveness trial in Zimbabwe. American Journal of Clinical Nutrition 2004;80:178‐84. [DOI] [PubMed] [Google Scholar]
- Hininger I, Favier M, Arnaud J, Faure H, Thoulon JM, Hariveau E, et al. Beneficial effects of a combined micronutrient supplementation on maternal oxidative stress and newborn anthropometric measurements: a randomised double blind, placebo‐controlled trial in healthy pregnant women. 21st Conference on Priorities in Perinatal Care in South Africa; 2002 March 5‐8; Eastern Cape, South Africa. 2002. [Google Scholar]; Hininger I, Favier M, Arnaud J, Faure H, Thoulon JM, Hariveau E, et al. Effects of a combined micronutrient supplementation on maternal biological status and newborn anthropometric measurements: a randomized double‐blind, placebo‐controlled trial in apparently healthy pregnant women. European Journal of Clinical Nutrition 2004;58:52‐9. [DOI] [PubMed] [Google Scholar]
- Andersen GS, Friis H, Michaelsen KF, Rodrigues A, Benn CS, Aaby P, et al. Effects of maternal micronutrient supplementation on fetal loss and under‐2‐years child mortality: long‐term follow‐up of a randomised controlled trial from Guinea‐Bissau. African Journal of Reproductive Health 2010;14(2):17‐26. [PubMed] [Google Scholar]; Kaestel P, Michaelsen KF, Aaby P, Friis H. Effects of prenatal multimicronutrient supplements on birth weight and perinatal mortality: a randomised, controlled trial in Guinea‐Bissau. European Journal of Clinical Nutrition 2005;59(9):1081‐9. [DOI] [PubMed] [Google Scholar]
- Cogswell ME. Impact of prenatal vitamin/mineral supplements on perinatal mortality (planned trial). ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 21 March 2006)2006. ; Li HT, Mei Z, Ren A, Serdula M, Cogswell M, Liu JM. Impact of iron‐containing micronutrient supplementation on high hemoglobin concentration during pregnancy. FASEB Journal 2012;26:Abstract no. 1021.2. [Google Scholar]; Liu JM, Mei Z, Ye R, Serdula M, Li HT, Cogswell M. Impact of iron‐contained micronutrient supplementation on macrosomia and large for gestational age births. FASEB Journal 2012;26:1021.2. [Google Scholar]; Liu JM, Mei Z, Ye R, Serdula MK, Ren A, Cogswell ME. Micronutrient supplementation and pregnancy outcomes: Double‐blind randomized controlled trial in China. JAMA Internal Medicine 2013;173(4):276‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mei Z, Serdula MK, Liu JM, Flores‐Ayala RC, Wang L, Ye R, et al. Iron‐containing micronutrient supplementation of Chinese women with no or mild anemia during pregnancy improved iron status but did not affect perinatal anemia. Journal of Nutrition 2014;144(6):943‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devakumar D, Chaube SS, Wells JC, Saville NM, Ayres JG, Manandhar DS, et al. Effect of antenatal multiple micronutrient supplementation on anthropometry and blood pressure in mid‐childhood in Nepal: follow‐up of a double‐blind randomised controlled trial. Lancet. Global Health 2014;2(11):e654‐e663. [DOI] [PMC free article] [PubMed] [Google Scholar]; Devakumar D, Stocks J, Ayres JG, Kirkby J, Yadav SK, Saville NM, et al. Effects of antenatal multiple micronutrient supplementation on lung function in mid‐childhood: follow‐up of a double‐blind randomised controlled trial in Nepal. European Respiratory Journal 2015 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]; Devakumar D, Wells JCK, Chaube SS, Saville NM, Manandhar DS, Costello A, et al. The phenotypic effects of antenatal multiple micronutrient supplementation in Nepalese children. Archives of Disease in Childhood 2014;99(Suppl 1):A2, Abstract no: P04. [Google Scholar]; Hindle LJ, Gitau R, Filteau SM, Newens KJ, Osrin D, Costello AM, et al. Effect of multiple micronutrient supplementation during pregnancy on inflammatory markers in Nepalese women. American Journal of Clinical Nutrition 2006;84:1086‐92. [DOI] [PubMed] [Google Scholar]; MIRA (Mother Infant Research Unit). MIRA Janakpur. Multiple micronutrient supplementation study. The effects of multiple micronutrient supplementation on birthweight, gestation and infection: a double blind, randomised controlled trial conducted in Nepal. Personal communication2003:1‐18. ; Osrin D, Vaidya A, Shrestha Y, Baniya RB, Manandhar DS, Adhikari RK, et al. Effects of antenatal micronutrient supplementation on birthweight and gestational duration in Nepal: double‐blind, randomised controlled trial. Lancet 2005;365:955‐62. [DOI] [PubMed] [Google Scholar]; Vaidya A, Saville N, Shrestha BP, Costello AM, Manandhar DS, Osrin D. Effects of antenatal multiple micronutrient supplementation on children's weight and size at 2 years of age in Nepal: follow‐up of a double‐blind randomised controlled trial. Lancet 2008;371(9611):492‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia‐Guerra A, Neufeld LM, Hernandez‐Cordero S, Rivera J, Martorell R, Ramakrishnan U. Prenatal multiple micronutrient supplementation impact on biochemical indicators during pregnancy and postpartum. Salud Publica de Mexico 2009;51(4):327‐35. [DOI] [PubMed] [Google Scholar]; Ramakrishnan U, Cossio TG, Neufeld LM, Rivera J, Martorell R. Effect of prenatal multiple micronutrient supplements on maternal weight and skinfold changes: A randomized double‐blind clinical trial in Mexico. Food and Nutrition Bulletin 2005;26(3):273‐80. [DOI] [PubMed] [Google Scholar]; Ramakrishnan U, Gonzalez‐Cossio T, Neufeld LM, Rivera J, Martorell R. Multiple micronutrient supplementation during pregnancy does not lead to greater infant birth size than does iron‐only supplementation: a randomized controlled trial in a semirural community in Mexico. American Journal of Clinical Nutrition 2003;77:720‐5. [DOI] [PubMed] [Google Scholar]; Ramakrishnan U, Neufeld LM, Gonzalez‐Cossio T, Villalpando S, Garcia‐Guerrra A, Juan R, et al. Multiple micronutrient supplements during pregnancy do not reduce anemia or improve iron status compared to iron‐only supplements in semirural Mexico. Journal of Nutrition 2004;134:898‐903. [DOI] [PubMed] [Google Scholar]; Lourdes Flores M, Neufeld LM, Gonzalez‐Cossio T, Rivera J, Martorell R, Ramakrishnan U. Multiple micronutrient supplementation and dietary energy intake in pregnant women. Salud Publica de Mexico 2007;49(3):190‐8. [DOI] [PubMed] [Google Scholar]
- Huybregts L, Roberfroid D, Lanou H, Kolsteren P, Camp J. Prenatal lipid‐based nutrient supplements increase cord leptin concentration in pregnant women from rural Burkina Faso. Annals of Nutrition & Metabolism 2013;63(Suppl 1):799, Abstract no: PO1134. [DOI] [PubMed] [Google Scholar]; Lanou H, Huybregts L, Roberfroid D, Kolsteren P. Effect of prenatal lipid‐based nutrient supplementation on gestational weight gain. Annals of Nutrition & Metabolism 2013;63(Suppl 1):783, Abstract no: PO1099. [Google Scholar]; Roberfroid D, Huybregts L, Habicht JP, Lanou H, Henry MC, Meda N, et al. Randomized controlled trial of 2 prenatal iron supplements: is there a dose‐response relation with maternal hemoglobin?. American Journal of Clinical Nutrition 2011;93:1012‐8. [DOI] [PubMed] [Google Scholar]; Roberfroid D, Huybregts L, Lanou H, Habicht JP, Henry MC, Meda N, et al. Prenatal micronutrient supplements cumulatively increase fetal growth. Journal of Nutrition 2012;142(3):548‐54. [DOI] [PubMed] [Google Scholar]; Roberfroid D, Huybregts L, Lanou H, Henry MC, Meda N, Kolsteren FP, et al. Effect of maternal multiple micronutrient supplements on cord blood hormones: a randomized controlled trial. American Journal of Clinical Nutrition 2010;91(6):1649‐58. [DOI] [PubMed] [Google Scholar]; Roberfroid D, Huybregts L, Lanou H, Henry MC, Meda N, Menten J, et al. Effects of maternal multiple micronutrient supplementation on fetal growth: a double‐blind randomized controlled trial in rural Burkina Faso. American Journal of Clinical Nutrition 2008;88:1330‐40. [DOI] [PubMed] [Google Scholar]; Roberfroid D, Huybregts L, Lanou H, Ouedraogo L, Henry MC, Meda N, et al. Impact of prenatal multiple micronutrients on survival and growth during infancy: a randomized controlled trial. American Journal of Clinical Nutrition 2012;95(4):916‐24. [DOI] [PubMed] [Google Scholar]
- Sood SK, Ramachandran K, Mathur M, Gupta K, Ramalingaswami V, Swarnbai C, et al. WHO sponsored collaborative study on nutritional anemia in India. Quarterly Journal of Medicine, New Series XLIV 1975;174:241‐58. [PubMed] [Google Scholar]
- Prado EL, Alcock KJ, Muadz H, Ullman MT, Shankar AH, for the SUMMIT Study Group. Maternal multiple micronutrient supplements and child cognition: a randomized trial in Indonesia. Pediatrics 2012;130(3):e536‐46. [DOI] [PubMed] [Google Scholar]; Prado EL, Ullman MT, Muadz H, Alcock KJ, Shankar AH. The effect of maternal multiple micronutrient supplementation on cognition and mood during pregnancy and postpartum in Indonesia: a randomized trial. PLoS ONE 2012;7(3):e32519. [DOI] [PMC free article] [PubMed] [Google Scholar]; Sebayang SK, Dibley MJ, Kelly P, Shankar AV, Shankar AH. Modifying effect of maternal nutritional status on the impact of maternal multiple micronutrient supplementation on birthweight in Indonesia. European Journal of Clinical Nutrition 2011;65(10):1110‐7. [DOI] [PubMed] [Google Scholar]; Shankar AV, Asrilla Z, Kadha JK, Sebayang S, Apriatni M, Sulastri A, et al. Programmatic effects of a large‐scale multiple‐micronutrient supplementation trial in Indonesia: using community facilitators as intermediaries for behavior change. Food and Nutrition Bulletin 2009;30(2 Suppl):S207‐S214. [DOI] [PubMed] [Google Scholar]; The Supplementation with Multiple Micronutrients Intervention Trial (SUMMIT) Study Group, Shankar AH, Jahari AB, Sebayang SK, Aditiawarman, Apriatni M, et al. Effect of maternal multiple micronutrient supplementation on fetal loss and infant death in Indonesia: a double‐blind cluster‐randomised trial. Lancet 2008;371(9608):215‐27. [DOI] [PubMed] [Google Scholar]
- Sunawang, Utomo B, Hidayat A, Kusharisupeni, Subarkah. Preventing low birth weight through maternal multiple micronutrient supplementation: a cluster‐randomized controlled trial in Indramayu, West Java. Food and Nutrition Bulletin 2009;30(4):S488‐S495. [DOI] [PubMed] [Google Scholar]
- Theobald GW, Camb MD. Effect of calcium and vitamins A and D on incidence of pregnancy toxaemia. Lancet 1937;2:1397‐9. [Google Scholar]
- Ekstrom EC, Eneroth H, Arifeen SE, Persson L. Efficacy of micronutrient supplement intake in increasing hemoglobin in pregnancy: dose‐effect comparisons with multiple micronutrient in the MINIMat trial in rural Bangladesh. FASEB Journal 2013;27 Suppl:Abstract no: 845.25. [Google Scholar]; Eneroth H, Arifeen S, Persson LA, Lonnerdal B, Hossain MB, Stephensen CB, et al. Maternal multiple micronutrient supplementation has limited impact on micronutrient status of Bangladeshi infants compared with standard iron and folic acid supplementation. Journal of Nutrition 2010;140(3):618‐24. [DOI] [PubMed] [Google Scholar]; Eneroth H, Persson LA, Arifeen S, Ekstrom EC. Infant anaemia is associated with infection, low birthweight and iron deficiency in rural Bangladesh. Acta Paediatrica 2011;100(2):220‐5. [DOI] [PubMed] [Google Scholar]; Hawkesworth S, Wagatsuma Y, Kahn AI, Hawlader MD, Fulford AJ, Arifeen SE, et al. Combined food and micronutrient supplements during pregnancy have limited impact on child blood pressure and kidney function in rural Bangladesh. Journal of Nutrition 2013;143(5):728‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]; Khan A, Kabir I, Ekstrom EC, Asling‐Monemi K, Alam D, Frongillo EA, et al. Effects of prenatal food and micronutrient supplementation on child growth from birth to 54 months of age: A randomized trial in Bangladesh. Nutrition Journal 2011;10(1):134. [DOI] [PMC free article] [PubMed] [Google Scholar]; Khan AI. Effects of pre‐ and postnatal nutrition interventions on child growth and body composition: the MINIMat trial in rural Bangladesh. Global Health Action 2013;6:22476. [DOI] [PMC free article] [PubMed] [Google Scholar]; Khan AI, Hawkesworth S, Ekstrom EC, Arifeen S, Moore SE, Frongillo EA, et al. Effects of exclusive breastfeeding intervention on child growth and body composition: The MINIMat trial, Bangladesh. Acta Paediatrica 2013;102(8):815‐23. [DOI] [PubMed] [Google Scholar]; Moore SE, Fulford AJ, Wagatsuma Y, Persson LA, Arifeen SE, Prentice AM. Thymus development and infant and child mortality in rural Bangladesh. International Journal of Epidemiology 2014;43:216‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]; Persson LA, Arifeen S, Ekstrom EC, Rasmussen KM, Frongillo EA, Yunus M. Effects of prenatal micronutrient and early food supplementation on maternal hemoglobin, birth weight, and infant mortality among children in Bangladesh: The MINIMat randomized trial. JAMA 2012;307(19):2050‐9. [DOI] [PubMed] [Google Scholar]; Persson LA, Eneroth H, Ekstrom EC. Multiple Micronutrient supplementation during pregnancy: A review of effects on birth size, maternal haemoglobin and perinatal mortality demonstrated in trials in Bangladesh, Guinea‐Bissau and Pakistan. Report for UNICEF/UNU/WHO2004. ; Shaheen R, Persson LA, Ahmed S, Lindholm L. Early invitation to prenatal food combined with multiple micronutrients is cost‐effective compared to iron‐folic acid supplementations: Results from MINIMat trial. Tropical Medicine and International Health 2013;18(Suppl 1):88. [Google Scholar]; Shaheen R, Streatfield PK, Naved RT, Lindholm L, Persson LA. Equity in adherence to and effect of prenatal food and micronutrient supplementation on child mortality: results from the MINIMat randomized trial, Bangladesh. BMC Public Health 2014;14:5. [DOI] [PMC free article] [PubMed] [Google Scholar]; Tofail F, Persson LA, Arifeen SE, Hamadani JD, Mehrin F, Ridout D, et al. Effects of prenatal food and micronutrient supplementation on infant development: a randomized trial from maternal and infant nutrition intervention, Matlab (MINIMat) study. American Journal of Clinical Nutrition 2008;87:704‐11. [DOI] [PubMed] [Google Scholar]
- Christian P, Shamim A, Shaikh S, Ali H, Mehra S, Lee W, et al. Antenatal multiple micronutrient supplementation and growth in the first two years of life and cognitive function at 24 months in rural Bangladesh. FASEB Journal 2014;28(1 Suppl 1):Abstract no. 256.5. [Google Scholar]; Gernand A, Schulze K, Shaikh S, Shamim A, Ali H, Wu L, et al. The effect of prenatal multiple micronutrient supplementation on biomarkers of placental angiogenesis in rural Bangladesh. FASEB Journal 2014;28(1 Suppl 1):Abstract no: 804.2. [Google Scholar]; Gernand AD, Christian P, Paul RR, Shaikh S, Labrique AB, Schulze KJ, et al. Maternal weight and body composition during pregnancy are associated with placental and birth weight in rural Bangladesh. Journal of Nutrition 2012;142(11):2010‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gernand AD, Christian P, Schulze KJ, Shaikh S, Labrique AB, Shamim AA, et al. Maternal nutritional status in early pregnancy is associated with body water and plasma volume changes in a pregnancy cohort in rural Bangladesh. Journal of Nutrition 2012;142(6):1109‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gernand AD, Paul RR, Shaikh S, Shamim AA, Schulze K, Labrique AB, et al. Maternal gestational weight and body composition are associated with placental weight in rural Bangladesh. FASEB Journal 2011;25:Abstract no: 780.7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Mehra S, Schulze KJ, Merrill RD, Shaikh S, Ali H, Shamim AA, et al. Exploration of non‐nutritional factors associated with stunting in 24 month old children of rural Bangladesh. FASEB Journal 2013;27 Suppl:Abstract no: 618.8. [Google Scholar]; West KP. Antenatal micronutrient supplementation and infant survival (JiVitA‐3). ClinicalTrials.gov (http://clinicaltrials.gov) (accessed 8 July 2011). ; West KP Jr, Shamim AA, Mehra S, Labrique AB, Ali H, Shaikh S, et al. Effect of maternal multiple micronutrient vs iron–folic acid supplementation on infant mortality and adverse birth outcomes in rural Bangladesh: the JiVitA‐3 randomized trial. JAMA 2014;312(24):2649‐58. [DOI] [PubMed] [Google Scholar]; West KP, Shamim AA, Labrique AB, Ali H, Shaikh S, Mehra S, et al. Efficacy of antenatal multiple micronutrient (MM) vs iron‐folic acid (IFA) supplementation in improving gestational and postnatal viability in rural Bangladesh: the JiVitA‐3 trial. FASEB Journal 2013;27 Suppl:Abstract no: 358.6. [Google Scholar]
- Zagre NM, Desplats G, Adou P, Mamadoultaibou A, Aguayo VM. Prenatal multiple micronutrient supplementation has greater impact on birthweight than supplementation with iron and folic acid: a cluster‐randomized, double‐blind, controlled programmatic study in rural Niger. Food and Nutrition Bulletin 2007;28(3):317‐27. [DOI] [PubMed] [Google Scholar]
- Cao Y, Wang T, Zeng L. Risk of childhood malnutrition at 24 months related to small for gestational age and low birth weight in rural Western China. Annals of Nutrition & Metabolism 2013;63(Suppl 1):556, Abstract no: PO619. [Google Scholar]; Chang S, Zeng L, Brouwer ID, Kok FJ, Yan H. Effect of iron deficiency anemia in pregnancy on child mental development in rural china. Pediatrics 2013;131(3):e755‐63. [DOI] [PubMed] [Google Scholar]; Li Q, Yan H, Zeng L, Cheng Y, Liang W, Dang S, et al. Effects of maternal multimicronutrient supplementation on the mental development of infants in rural western China: follow‐up evaluation of a double‐blind, randomized, controlled trial. Pediatrics 2009;123(4):e685‐e692. [DOI] [PubMed] [Google Scholar]; Wang W, Yan H, Zeng L, Cheng Y, Wang D, Li Q. No effect of maternal micronutrient supplementation on early childhood growth in rural western China: 30 month follow‐up evaluation of a double blind, cluster randomized controlled trial. European Journal of Clinical Nutrition 2012;66(2):261‐8. [DOI] [PubMed] [Google Scholar]; Yan H. Impact of iron/folate versus multi‐micronutrient supplementation during pregnancy on birth weight: a randomised controlled trial in rural Western China. Current Controlled Trials (www.controlled‐trials.com) (accessed 15 February 2007). ; Zeng L, Cheng Y, Dang S, Yan H, Dibley MJ, Chang S, et al. Impact of micronutrient supplementation during pregnancy on birth weight, duration of gestation and perinatal mortality in rural western China: double blind cluster randomised controlled trial. BMJ 2008;337:a2001. [DOI] [PMC free article] [PubMed] [Google Scholar]; Zeng L, Yan H, Cheng Y, Dang S, Dibley MJ. Adherence and costs of micronutrient supplementation in pregnancy in a double‐blind, randomized, controlled trial in rural western China. Food and Nutrition Bulletin 2009;30(4):S480‐S487. [DOI] [PubMed] [Google Scholar]; Zeng L, Yan H, Cheng Y, Dibley M. Modifying effects of maternal nutrition status on the response to multiple micronutrients supplementation on preterm and neonatal mortality in China. Annals of Nutrition & Metabolism 2013;63(Suppl 1):859‐60, Abstract no: PO1241. [Google Scholar]; Zeng L, Yan H, Cheng Y, Dibley MJ. Modifying effects of wealth on the response to nutrient supplementation in pregnancy on birth weight, duration of gestation and perinatal mortality in rural western China: double‐blind cluster randomized controlled trial. International Journal of Epidemiology 2011;40(2):350‐62. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Agarwal N, Dora S, Kriplani A, Garg P, Vivekanandhan S, Kulshrestha V. Response of therapy with vitamin B6, B12 and folic acid on homocysteine level and pregnancy outcome in hyperhomocysteinemia with unexplained recurrent abortions. International Journal of Gynecology and Obstetrics 2012;119(Suppl 3):S759. [Google Scholar]
- Aguayo VM, Kone D, Bamba SI, Diallo B, Sidibe Y, Traore D, et al. Acceptability of multiple micronutrient supplements by pregnant and lactating women in Mali. Public Health Nutrition 2005;8(1):33‐7. [DOI] [PubMed] [Google Scholar]
- Ahn E, Pairaudeau N, Pairaudeau N, Cerat Y, Couturier B, Fortier A, et al. A randomized cross over trial of tolerability and compliance of a micronutrient supplement with low iron separated from calcium vs high iron combined with calcium in pregnant women. BMC Pregnancy and Childbirth 2006;6:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An H, Yin S, Xu Q. Effects of supplementing calcium, iron and zinc on the fetus development and growth during pregnancy. Chinese Journal of Preventive Medicine 2001;35(6):370‐3. [PubMed] [Google Scholar]
- Arsenault JE, Aboud S, Manji KP, Fawzi WW, Villamor E. Vitamin supplementation increases risk of subclinical mastitis in HIV‐infected women. Journal of Nutrition 2010;140(10):1788‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asemi Z, Samimi M, Tabassi Z, Ahmad E. Multivitamin versus multivitamin‐mineral supplementation and pregnancy outcomes: a single‐blind randomized clinical trial. International Journal of Preventive Medicine 2014;5(4):439‐46. [PMC free article] [PubMed] [Google Scholar]
- Beazley D, Ahokas R, Livingston J, Griggs M, Scroggs M, Sibai B. Effects of vitamin C and E supplementation on total antioxidant status (TAS) and 8‐isoprostane (IP) levels in women at high risk for preeclampsia. American Journal of Obstetrics and Gynecology 2002;187(6 Pt 2):S76. [DOI] [PubMed] [Google Scholar]; Beazley D, Livingston J, Kao L, Sibai L. Vitamin C and E supplementation in women at high risk for preeclampsia: a double‐blind placebo controlled trial. American Journal of Obstetrics and Gynecology 2002;187(6 Pt 2):S216. [DOI] [PubMed] [Google Scholar]
- Bergmann RL, Haschke‐Becher, Bergmann KE, Dudenhausen JW, Haschke F. Low dose docosahexaenoic acid supplementation improves the DHA status of pregnant women. Pediatric Academic Societies Annual Meeting; 2006 April 29‐May 2; San Francisco, CA, USA. 2006. [Google Scholar]
- Biswas MK, Pernoll MJ, Mabie WC. A placebo controlled comparative trial of various prenatal vitamin formulations in pregnant women. Clinical Therapeutics 1984;6(6):763‐9. [PubMed] [Google Scholar]
- Carrasco EO, Jose FR, Samson GD, Germar E, Padilla B. Effect of D‐sorbitol on the absorption and transfer of nutrients from mother to fetus. American Journal of Clinical Nutrition 1962;11:533‐6. [DOI] [PubMed] [Google Scholar]
- Caulfield LE, Zavaleta N, Figueroa A, Leon Z. Maternal zinc supplementation does not affect size at birth or pregnancy duration in Peru. Journal of Nutrition 1999;129(8):1563‐8. [DOI] [PubMed] [Google Scholar]
- Caulfield LE Zavaleta N, Figueroa A. Adding zinc to prenatal iron and folate supplements improves maternal and neonatal zinc status in a Peruvian population. American Journal of Clinical Nutrition 1999;69:1257‐63. [DOI] [PubMed] [Google Scholar]
- Chames M, Liu H, Bendich A, Bogden J, Sibai B, Prada J. A randomized trial of calcium supplementation effects on blood lead levels in pregnancy. American Journal of Obstetrics and Gynecology 2002;187(6 Pt 2):S137. [Google Scholar]
- Choudhury N, Aimone A, Hyder SM, Zlotkin SH. Relative efficacy of micronutrient powders versus iron‐folic acid tablets in controlling anemia in women in the second trimester of pregnancy. Food & Nutrition Bulletin 2012;33(2):142‐9. [DOI] [PubMed] [Google Scholar]
- Bhutta Z. Severe anemia treatment trials, Pakistan (ongoing trial). ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 21 March 2006)2006. ; Christian P, Shahid F, Rizvi A, Klemm RDW, Bhutta ZA. Treatment response to standard of care for severe anemia in pregnant women and effect of multivitamins and enhanced anthelminthics. American Journal of Clinical Nutrition 2009;89:853‐61. [DOI] [PubMed] [Google Scholar]
- Cooper WN, Khulan B, Owens S, Elks CE, Seidel V, Prentice AM, et al. DNA methylation profiling at imprinted loci after periconceptional micronutrient supplementation in humans: Results of a pilot randomized controlled trial. FASEB Journal 2012;26(5):1782‐90. [DOI] [PubMed] [Google Scholar]
- Czeizel AE. Controlled studies of multivitamin supplementation on pregnancy outcomes. Annals of New York Academy of Sciences 1993;678:266‐75. [DOI] [PubMed] [Google Scholar]; Czeizel AE. Prevention of congenital abnormalities by periconceptional multivitamin supplementation. BMJ 1993;306:1645‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]; Czeizel AE. Reduction of urinary tract and cardiovascular defects by periconceptional multivitamin supplementation. American Journal of Medical Genetics 1996;62:179‐83. [DOI] [PubMed] [Google Scholar]; Czeizel AE, Dudas I. Prevention of the first occurrence of neural tube defects by periconceptional vitamin supplementation. New England Journal of Medicine 1992;327:1832‐5. [DOI] [PubMed] [Google Scholar]; Czeizel AE, Dudas I, Fritz G, Tecsoi A, Hanck A, Kunovits G. The effect of periconceptional multivitamin ‐mineral supplementation on vertigo, nausea and vomiting in the first trimester of pregnancy. Archives of Gynecology and Obstetrics 1992;251:181‐5. [DOI] [PubMed] [Google Scholar]; Czeizel AE, Dudas I, Metneki J. Pregnancy outcomes in a randomized controlled trial of periconceptional multivitamin supplementation. Archives of Gynecology and Obstetrics 1994;255:131‐9. [DOI] [PubMed] [Google Scholar]; Czeizel AE, Metneki J, Dudas I. The effect of preconceptional multivitamin supplementation on fertility. International Journal of Vitamin and Nutrition Research 1996;66:55‐8. [PubMed] [Google Scholar]
- Dawson EB, McGanity WJ. Protection of maternal iron stores in pregnancy. Journal of Reproductive Medicine 1987;32(6):478‐87. [PubMed] [Google Scholar]
- Dawson EB, Dawson R, Behrens J, DeVora M, McGanity WJ. Iron in prenatal multivitamin/multimineral supplements. Journal of Reproductive Medicine 1998;43:133‐40. [PubMed] [Google Scholar]
- Dieckmann WJ, Adair FL, Michel H, Kramer S, Dunkle F, Arthur B, et al. Calcium, phosphorus, iron and nitrogen balances in pregnant women. American Journal of Obstetrics and Gynecology 1944;47:357‐68. [Google Scholar]
- Fall C. Mumbai maternal nutrition project. Current Controlled Trials (http://controlled‐trials.com) (accessed 15 February 2007)2007. ; Potdar RD, Sahariah SA, Gandhi M, Kehoe SH, Brown N, Sane H, et al. Improving women's diet quality preconceptionally and during gestation: effects on birth weight and prevalence of low birth weight‐a randomized controlled efficacy trial in India (Mumbai Maternal Nutrition Project). American Journal of Clinical Nutrition 2014;100(5):1257‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawzi W, Msamanga G, Antelman G, Xu C, Hertzmark E, Spiegelman D, et al. Effect of prenatal vitamin supplementation on lower genital levels of HIV type 1 and interleukin type 1 beta at 36 weeks of gestation. Clinical Infectious Diseases 2004;38(5):716‐22. [DOI] [PubMed] [Google Scholar]; Fawzi WW, Msamanga G, Hunter D, Urassa E, Renjifo B, Mwakagile D, et al. Randomized trial of vitamin supplements in relation to vertical transmission of HIV‐1 in Tanzania. Journal of Acquired Immune Deficiency Syndromes 2000;23(3):246‐54. [DOI] [PubMed] [Google Scholar]; Fawzi WW, Msamanga G, Spiegelman D, Wei R, Kapiga S, Villamor E, et al. A randomised trial of multivitamin supplements and HIV disease progression and mortality. New England Journal of Medicine 2004;351(1):23‐32. [DOI] [PubMed] [Google Scholar]; Fawzi WW, Msamanga GI, Kupka R, Spiegelman D, Villamor E, Mugusi F, et al. Multivitamin supplementation improves hematologic status in HIV‐infected women and their children in Tanzania. American Journal of Clinical Nutrition 2007;85(5):1335‐43. [DOI] [PubMed] [Google Scholar]; Fawzi WW, Msamanga GI, Spiegelman D, Urassa EJN, McGarth N, Mwakagile D, et al. Randomized controlled trial of the effects of vitamin supplements on pregnancy outcomes and T cell counts in HIV ‐1 infected women in Tanzania. Lancet 1998;351:1477‐82. [DOI] [PubMed] [Google Scholar]; Kawai K, Kupka R, Mugusi F, Aboud S, Okuma J, Villamor E, et al. A randomized trial to determine the optimal dosage of multivitamin supplements to reduce adverse pregnancy outcomes among HIV‐infected women in Tanzania. American Journal of Clinical Nutrition 2010;91(2):391‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Kawai K, Msamanga G, Manji K, Villamor E, Bosch RJ, Hertzmark E, et al. Sex differences in the effects of maternal vitamin supplements on mortality and morbidity among children born to HIV‐infected women in Tanzania. British Journal of Nutrition 2010;103(12):1784‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]; Villamor E, Koulinska IN, Aboud S, Murrin C, Bosch RJ, Manji KP, et al. Effect of vitamin supplements on HIV shedding in breast milk. American Journal of Clinical Nutrition 2010;92(4):881‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]; Villamor E, Msamanga G, Saathoff E, Manji K, Fawzi WW. Effect of vitamin supplements on the incidence of malaria among children born to HIV‐infected Women. FASEB Journal 2006;20(4 Pt 1):A125. [PubMed] [Google Scholar]; Villamor E, Msamanga G, Spiegelman D, Antelman G, Peterson KE, Hunter DJ, et al. Effect of multivitamin and vitamin A supplements on weight gain during pregnancy among HIV‐1 infected women. American Journal of Clinical Nutrition 2002;76:1082‐90. [DOI] [PubMed] [Google Scholar]; Villamor E, Saathoff E, Bosch RJ, Hertzmark E, Baylin A, Manji K, et al. Vitamin supplementation of HIV‐infected women improves postnatal child growth. American Journal of Clinial Nutrition 2005;81(4):880‐8. [DOI] [PubMed] [Google Scholar]
- Feyi‐Waboso PA, Chris A, Nwaogu GC, Archibong EI, Ejikem EC. The role of parenteral multivitamin preparation (Eldervit‐12) in the prevention of anaemia in pregnancy. Tropical Journal of Obstetrics and Gynaecology 2005;22(2):159‐63. [Google Scholar]
- Fleming AF, Ghatoura GBS, Harrison KA, Briggs ND, Dunn DT. The prevention of anemia in pregnancy in primigravidae in the Guinea Savana of Nigeria. Annals of Tropical Medicine and Parasitology 1986;80(2):211‐33. [DOI] [PubMed] [Google Scholar]
- Goldenberg R, Tamura T, Neggers Y, Copper R, Johnston K, DuBard M, et al. Maternal zinc supplementation increases birthweight and head circumference. American Journal of Obstetrics and Gynecology 1995;172(1 Pt 2):368. [Google Scholar]
- Gopalan S, Patnaik R, Ganesh K. Feasible strategies to combat low birth weight and intra‐uterine growth retardation. Journal of Pediatric Gastroenterology and Nutrition 2004;39 Suppl 1:S37. [Google Scholar]
- Graham JM, Haskell MJ, Pandey P, Shrestha RK, Brown KH, Allen LH. Supplementation with iron and riboflavin enhances dark adaptation response to vitamin A‐fortified rice in iron‐deficient, pregnant, nightblind Nepali women. American Journal of Clinical Nutrition 2007;85(5):1375‐84. [DOI] [PubMed] [Google Scholar]
- Guldholt IS, Trolle BG, Hvidman LE. Iron supplementation during pregnancy. Acta Obstetricia et Gynecologica Scandinavica 1991;70:9‐12. [DOI] [PubMed] [Google Scholar]
- Gupta P, Ray M, Dua T, Radhakrishnan G, Kumar R, Sachdev HP. Multimicronutrient supplementation for undernourished pregnant women and the birth size of their offspring: a double‐blind, randomized, placebo‐controlled trial. Archives of Pediatrics and Adolescent Medicine 2007;161(1):58‐64. [DOI] [PubMed] [Google Scholar]
- Hambidge KM, Krebs NF, Westcott JE, Garces A, Goudar SS, Kodkany BS, et al. Preconception maternal nutrition: a multi‐site randomized controlled trial. BMC Pregnancy and Childbirth 2014;14(1):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillman RW, Cabaud PE, Nilsson DE, Arpin PD, Tufano RJ. Pyridoxine supplementation during pregnancy. American Journal of Clinical Nutrition 1963;12:427‐30. [DOI] [PubMed] [Google Scholar]
- Holly RG. Anemia in pregnancy. Obstetrics and Gynecology 1955;5:562‐9. [PubMed] [Google Scholar]
- Hossain N, Kanani FH, Ramzan S, Kausar R, Ayaz S, Khanani R, et al. Obstetric and neonatal outcomes of maternal vitamin D supplementation: results of an open label randomized controlled trial of antenatal vitamin D supplementation in Pakistani women. Journal of Clinical Endocrinology and Metabolism 2014;99(7):2448‐55. [DOI] [PubMed] [Google Scholar]
- Hunt IF, Murphy NJ, Cleaver AE, Faraji B, Swendseid ME, Coulson AH, et al. Zinc supplementation during pregnancy: zinc concentration of serum and hair from low‐income women of Mexican descent. American Journal of Clinical Nutrition 1983;37:572‐82. [DOI] [PubMed] [Google Scholar]
- Hunt IF, Murphy NJ, Cleaver AE, Faraji B, Swendseid ME, Coulson AH, et al. Zinc supplementation during pregnancy: effects on selected blood constituents and on progress and outcome of pregnancy in low‐income women of Mexican descent. American Journal of Clinical Nutrition 1984;40:508‐21. [DOI] [PubMed] [Google Scholar]
- Hunt IF, Murphy NJ, Cleaver AE, Faraji B, Swendseid ME, Browdy BL, et al. Zinc supplementation during pregnancy in low‐income teenagers of Mexican descent: effects on selected blood constituents and on progress and outcome of pregnancy. American Journal of Clinical Nutrition 1985;42:815‐28. [DOI] [PubMed] [Google Scholar]
- Huybregts L, Roberfroid D, Lanou H, Menten J, Meda N, Camp J, et al. Prenatal food supplementation fortified with multiple micronutrients increases birth length: a randomized controlled trial in rural Burkina Faso. American Journal of Clinical Nutrition 2009;90(6):1593‐600. [DOI] [PubMed] [Google Scholar]
- Huybregts L, Roberfroid D, Lanou H, Meda N, Taes Y, Valea I, et al. Prenatal lipid‐based nutrient supplements increase cord leptin concentration in pregnant women from rural Burkina Faso. Journal of Nutrition 2013;143(5):576‐83. [DOI] [PubMed] [Google Scholar]
- Iannotti LL, Zavaleta N, Leon Z, Shankar AH, Caulfield LE. Maternal zinc supplementation and growth in Peruvian infants. American Journal of Clinical Nutrition 2008;88(1):154‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indian Council of Medical Research (ICMR) Collaborating Centers, Central Technical Co‐ordinating Unit. Multicentric study of efficacy of periconceptional folic acid containing vitamin supplementation in prevention of open neural tube defects in India. Indian Journal of Medical Research 2000;112:206‐11. [PubMed] [Google Scholar]
- Itam IH. The effect of "Chemiron" on haematological parameters and ferritin levels in pregnant Nigerian women in Calabar. Mary Slessor Journal of Medicine 2003;3(2):17‐24. [Google Scholar]
- Jarvenpaa J, Schwab U, Lappalainen T, Pakkila M, Niskanen L, Punnonen K, et al. Fortified mineral water improves folate status and decreases plasma homocysteine concentration in pregnant women. Journal of Perinatal Medicine 2007;35(2):108‐14. [DOI] [PubMed] [Google Scholar]; Jarvenpaa J, Schwab U, Lappalainen T, Pakkila M, Niskanen L, Punnonen K, et al. Mineral water fortified with folic acid and vitamins B6, B12, D and calcium improves folate status and decreases plasma homocysteine concentration in pregnant women. 35th Nordic Congress of Obstetrics and Gynecology; 2006 May 23‐25; Goteburg, Sweden. 2008:55. [Google Scholar]
- Kabir I, Khan AI, Arifeen S, Alam DS, Persson LA. Effects of prenatal food and micronutrient supplementation and breastfeeding counseling on postnatal growth of rural Bangladeshi children. Pediatric Academic Societies Annual Meeting; 2009 May 2‐5; Baltimore, USA. 2009. [Google Scholar]
- Chambers C, Yevtushok L, Zymak‐Zakutnya N, Wertelecki W, Jones KL, Keen CL, et al. Maternal alcohol consumption during pregnancy, nutritional status and impact on infant outcomes. Alcohol and Alcoholism 2013;48 Suppl:i21‐i22. [Google Scholar]; Coles C, Yevtushok L, Zymak‐Zakutnya N, Wertelecki W, Keen CL, Y YJ, et al. Micronutrient supplements can mitigate the teratogenic effects of prenatal alcohol exposure on Ukrainian infants at 6 months. Alcohol and Alcoholism 2013;48 Suppl:i22. [Google Scholar]; Coles CD, Chambers CD, Yevtushok L, Zymak‐Zakutnya N, Wertelecki W, Keen CL, et al. Micronutrient supplements can mitigate the teratogenic effects of prenatal alcohol exposure on Ukrainian infants at six months. Birth Defects Research Part A ‐ Clinical and Molecular Teratology 2012;94(5):361. [Google Scholar]; Kable J, Coles C, Chambers C, Keen C, Uriu‐Adams J, Jones K, et al. Preliminary analysis of the impact of micronutrient supplements on neurophysiological encoding and memory in Ukranian infants 12‐18 months postpartum. Alcoholism: Clinical and Experimental Research 2012;36(S1):212A. [Google Scholar]; Kable J, Coles C, Chambers C, Keen C, Uriu‐Adams J, Jones K, et al. The impact of micronutrient supplementation in alcohol‐exposed pregnancies on information processing skills in Ukrainian infants. Alcohol and Alcoholism 2013;48 Suppl:i22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khavari N, Jiang H, Manji K, Msamanga G, Spiegelman D, Fawzi W, et al. Maternal multivitamin supplementation reduces the risk of diarrhoea among HIV‐exposed children through age 5 years. International Health 2014;6:298‐305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khulan B, Cooper WN, Skinner BM, Bauer J, Owens S, Prentice AM, et al. Periconceptional maternal micronutrient supplementation is associated with widespread gender related changes in the epigenome: A study of a unique resource in the Gambia. Human Molecular Genetics 2012;21(9):2086‐101. [DOI] [PubMed] [Google Scholar]
- Chelchowska M, Laskowska‐Klita T, Kubik P, Leibschang J. The effect of vitamin‐mineral supplementation on the level of MDA and activity of glutathione peroxidase and superoxide dismutase in blood of matched maternal‐cord pairs [Wplyw suplementacji witaminowo‐mineralnej na poziom MDA oraz aktywnosc peroksydazy glutationowej i dysmutazy ponadtlenkowej w krwi kobiet ciezarnych i krwi pepowinowej ich dzieci]. Przeglad Lekarski 2004;61(7):760‐3. [PubMed] [Google Scholar]; Kubik P, Kowalska B, Laskowska‐Klita T, Chelchowska M, Leibschang J. Effect of vitamin‐mineral supplementation on the status of some microelements in pregnant women. Przeglad Lekarski 2004;61(7):764‐8. [PubMed] [Google Scholar]; Laskowska‐Klita T, Chelchowska M, Ambroszkiewicz J, Kubik P, Leibschang J. The effect of vitamin‐mineral supplementation on vitamins D, A (beta‐carotene) and E concentration in blood of matched maternal‐cord pairs [Wplyw suplementacji witaminowo‐mineralnej na stezenie witamin D, A (beta‐karoten) i E w krwi kobiet ciezarnych i krwi pqpowinowej ich dzieci.]. Przeglad Lekarski 2004;61(7):755‐9. [PubMed] [Google Scholar]
- Kynast G, Langner K, Saling E. Clinical results of oral application of trace elements in risk pregnancies. Proceedings of 10th European Congress of Perinatal Medicine; 1986 Aug 12‐16; Leipzig, Germany. 1986. [Google Scholar]
- Lanou H, Huybregts L, Roberfroid D, Nikiema L, Kouanda S, Camp J, et al. Prenatal nutrient supplementation and postnatal growth in a developing nation: an RCT. Pediatrics 2014;133(4):e1001‐e1008. [DOI] [PubMed] [Google Scholar]
- Leroy JL. Preventing malnutrition in children under two years of age approach. ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 18 October 2014)2010. ; Richter SM, Leroy JL, Olney D, Quinones E, Ruel M. Strengthening and Evaluating the Preventing Malnutrition in Children under 2 Approach in Guatemala: Report of the Enrollment Survey. Washington DC: FHI 360, 2013. [Google Scholar]
- Li YF, Hu NS, Tian XB, Li L, Wang SM, Xu XB, et al. Effect of daily milk supplementation on serum and umbilical cord blood folic acid concentrations in pregnant Han and Mongolian women and birth characteristics in China. Asia Pacific Journal of Clinical Nutrition 2014;23(4):567‐74. [DOI] [PubMed] [Google Scholar]
- Lindström E, Hossain MB, Lönnerdal B, Raqib R, Arifeen S, Ekström EC. Prevalence of anemia and micronutrient deficiencies in early pregnancy in rural Bangladesh, the MINIMat trial. Acta Obstetricia et Gynecologica Scandinavica 2011;90(1):47‐56. [DOI] [PubMed] [Google Scholar]
- Ling CD, Zhang ZJ, Chen ZL. Studies on nutritional effects of traditional Chinese tonics with strengthened nutrients on pregnant women and rats. Chung‐Kuo Chung Hsi i Chieh Ho Tsa Chih 1996;16:270‐3. [PubMed] [Google Scholar]
- Lucia Bergmann R, Bergmann KE, Haschke‐Becher E, Richter R, Dudenhausen JW, Barclay D, et al. Does maternal docosahexaenoic acid supplementation during pregnancy and lactation lower BMI in late infancy?. Journal of Perinatal Medicine 2007;35(4):295‐300. [DOI] [PubMed] [Google Scholar]
- Ma AG, Schouten EG, Zhang FZ, Kok FJ, Yang F, Jiang DC, et al. Retinol and riboflavin supplementation decreases the prevalence of anemia in Chinese pregnant women taking iron and folic acid supplements. Journal of Nutrition 2008;138(10):1946‐50. [DOI] [PubMed] [Google Scholar]
- Magon A, Collin SM, Joshi P, Davys Late G, Attlee A, Mathur B. Leaf concentrate fortification of antenatal protein‐calorie snacks improves pregnancy outcomes. Journal of Health, Population and Nutrition 2014;32(3):430‐40. [PMC free article] [PubMed] [Google Scholar]
- Malvasi A, Casciaro F, Minervini MM, Kosmas I, Mynbaev OA, Pacella E, et al. Myo‐inositol, D‐chiro‐inositol, folic acid and manganese in second trimester of pregnancy: a preliminary investigation. European Review for Medical and Pharmacological Sciences 2014;18(2):270‐4. [PubMed] [Google Scholar]
- Mardones F, Urrutia MT, Villarroel L, Rioseco A, Castillo O, Rozowski J, et al. Effects of a dairy product fortified with multiple micronutrients and omega‐3 fatty acids on birth weight and gestation duration in pregnant Chilean women. Public Health Nutrition 2007;11(1):30‐40. [DOI] [PubMed] [Google Scholar]
- Marya RK, Rathee S, Manrow M. Effect of calcium and vitamin D supplementation on toxaemia of pregnancy. Gynecologic and Obstetric Investigation 1987;24:38‐42. [DOI] [PubMed] [Google Scholar]
- Mathan BVI, Baker SH, Sood SK, Ramachandran K, Ramalingaswami V. WHO sponsored collaborative studies on nutritional anaemia in India. The effects of ascorbic acid and protein supplementation on the response of pregnant women to iron, pteroyglutamic acid and cyanocobalamin therapy. British Journal of Nutrition 1979;42:391‐8. [DOI] [PubMed] [Google Scholar]
- Menon MKK, Rajan L. Prophylaxis of anaemia in pregnancy. British Journal of Obstetrics and Gynaecology of the British Commonwealth 1962;12:382‐9. [Google Scholar]
- Merchant AT, Msamanga G, Villamor E, Saathoff E, O'Brien M, Hertzmark E, et al. Multivitamin supplementation of HIV‐ positive women during pregnancy reduces hypertension. Journal of Nutrition 2005;135(7):1776‐81. [DOI] [PubMed] [Google Scholar]
- Merialdi M, Caulfield LE, Zavaleta N, Figueroa A, DiPietro JA. Adding zinc to prenatal iron and folate tablets improves fetal neurobehavioral development. American Journal of Obstetrics and Gynecology 1999;180(2 Pt 1):483‐90. [DOI] [PubMed] [Google Scholar]
- Muslimatun S, Schmidt MK, Schultink W, West CE, Hautvast JGAJ, Gross R, et al. Weekly supplementation with iron and vitamin A during pregnancy increases hemoglobin concentration but decreases serum ferritin concentration in Indonesian pregnant women. Journal of Nutrition 2001;131(1):85‐90. [DOI] [PubMed] [Google Scholar]
- Muslimatun S, Schmidt MK, West CE, Schultink W, Hautvast JG, Karyadi D. Weekly vitamin A and iron supplementation during pregnancy increases vitamin A concentration of breast milk but not iron status in Indonesian lactating women. Journal of Nutrition 2001;131(10):2664‐9. [DOI] [PubMed] [Google Scholar]
- Nguyen PH, Lowe AE, Martorell R, Nguyen H, Pham H, Nguyen S, et al. Rationale, design, methodology and sample characteristics for the Vietnam pre‐conceptual micronutrient supplementation trial (PRECONCEPT): a randomized controlled study. BMC Public Health 2012;12:898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwagha UI, Okeji N, Clems‐Anunwa O, Ejezie FE, Nwagha TU, Iyare E. The role of some micronutrients (eldervit) in the management of the anaemic pregnant Nigerian women: a preliminary report. Tropical Journal of Obstetrics & Gynaecology 2010;27(2):34‐9. [Google Scholar]
- Ochoa‐Brust GJ, Fernandez AR, Villanueva‐Ruiz GJ, Velasco R, Trujillo‐Hernandez B, Vasquez C. Daily intake of 100 mg ascorbic acid as urinary tract infection prophylactic agent during pregnancy. Acta Obstetricia et Gynecologica Scandinavica. 2007;86(7):783‐7. [DOI] [PubMed] [Google Scholar]
- Olofin IO, Spiegelman D, Aboud S, Duggan C, Danaei G, Fawzi WW. Supplementation with multivitamins and vitamin A and incidence of malaria among HIV‐infected Tanzanian women. Journal of Acquired Immune Deficiency Syndromes (1999) 2014;67(Suppl 4):S173‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park E, Wagenbichler P, Elmadfa I. Effects of multivitamin/mineral supplementation, at nutritional doses, on plasma antioxidant status and DNA damage estimated by sister chromatid exchanges in lymphocytes in pregnant women. International Journal for Vitamin and Nutrition Research 1999;69:396‐402. [DOI] [PubMed] [Google Scholar]
- Patimah S, As'ad S, Jusoff K, Hadju V, Razak A, Bahar B. The influence of multiple micronutrient supplementations on hemoglobin and serum ferritin levels of pregnant women. World Journal of Medical Sciences 2013;8(3):177‐85. [Google Scholar]
- People's League of Health. Nutrition of expectant and nursing mothers: interim report. Lancet 1942;2:10‐2. [Google Scholar]; People's League of Health. The nutrition of expectant and nursing mothers in relation to maternal and infant mortality and morbidity. Journal of Obstetrics and Gynaecology of the British Empire 1946;53:498‐509. [DOI] [PubMed] [Google Scholar]
- Ramirez‐Velez R, Romero M, Echeverri I, Ortega JG, Mosquera M, Salazar B, et al. A factorial randomized controlled trial to evaluate the effect of micronutrients supplementation and regular aerobic exercise on maternal endothelium‐dependent vasodilatation and oxidative stress of the newborn. Trials 2011;12:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raqib R. Role of vitamin B12 supplementation during pregnancy and postpartum to reduce nutritional anemia and improve immunity in Bangladeshi women and their infants. ClinicalTrials.gov (https://clinicaltrials.gov/) (accessed 21 May 2013)2013.
- Robertson JS, Heywood B, Atkinson SM. Zinc supplementation during pregnancy. Journal of Public Health Medicine 1991;13:227‐9. [DOI] [PubMed] [Google Scholar]
- Rumiris D, Purwosunu Y, Wibowo N, Farina A, Sekizawa A. Lower rate of preeclampsia after antioxidant supplementation in pregnant women with low antioxidant status. Hypertension in Pregnancy 2006;25:241‐53. [DOI] [PubMed] [Google Scholar]
- Sachdeva R, Mann SK. Impact of nutrition education and medical supervision on pregnancy outcome. Indian Pediatrics 1993;30(11):1309‐14. [PubMed] [Google Scholar]
- Sagaonkar S, Sukhija S, Tayal R, Sagaonkar PD. Pregnancy induced iron deficiency and the evaluation and comparison of the efficacy and safety of ferrous fumarate and carbonyl iron in its treatment ‐ PERFECT trial. Journal of Obstetrics and Gynecology of India 2009;59(6):552‐62. [Google Scholar]
- Salzano P, Felicetti M, Laboccetta A, Borrelli P, Domenico A, Borrelli A. Prevention of gestational hypertension with calcium, linoleic acid, mono and polyunsaturated fatty acid supplements. Minerva Ginecologica 2001;53(4):235‐8. [PubMed] [Google Scholar]
- Schmidt MK, Muslimatun S, West CE, Schultink W, Hautvast JG. Vitamin A and iron supplementation of Indonesian pregnant women benefits vitamin A status of their infants. British Journal of Nutrition 2001;86(5):607‐15. [DOI] [PubMed] [Google Scholar]
- Schmidt MK, Muslimatun S, Schultink W, West CE, Hautvast JG. Randomised double‐blind trial of the effect of vitamin A supplementation of Indonesian pregnant women on morbidity and growth of their infants during the first year of life. European Journal of Clinical Nutrition 2002;56(4):338‐46. [DOI] [PubMed] [Google Scholar]
- Semba RD, Kumwenda N, Taha TE, Mtimavalye L, Broadhead R, Miotti PG, et al. Plasma and breast milk vitamin A as indicators of vitamin A status in pregnant women. International Journal for Vitamin and Nutrition Research 2000;70(6):271‐7. [DOI] [PubMed] [Google Scholar]
- Semba RD, Kumwenda N, Taha TE, Mtimavalye L, Broadhead R, Garrett E, et al. Impact of vitamin A supplementation on anaemia and plasma erythropoietin concentrations in pregnant women: a controlled clinical trial. European Journal of Haematology 2001;66(6):389‐95. [DOI] [PubMed] [Google Scholar]
- Suharno D, West CE, Muhilal, Karyadi D, Hautvast JGA. Supplementation with vitamin A and iron for nutritional anaemia in pregnant women in West Java, Indonesia. Lancet 1993;342:1325‐8. [DOI] [PubMed] [Google Scholar]
- Sun YY, Ma AG, Yang F, Zhang FZ, Luo YB, Jiang DC, et al. A combination of iron and retinol supplementation benefits iron status, IL‐2 level and lymphocyte proliferation in anemic pregnant women. Asia Pacific Journal of Clinical Nutrition 2010;19(4):513‐9. [PubMed] [Google Scholar]
- Suprapto B, Widardo, Suhanantyo. Effect of low‐dosage vitamin A and riboflavin on iron‐folate supplementation in anaemic pregnant women. Asia Pacific Journal of Clinical Nutrition 2002;11(4):263‐7. [DOI] [PubMed] [Google Scholar]
- Taghizadeh M, Samimi M, Tabassi Z, Heidarzadeh Z, Asemi Z. Effect of multivitamin‐mineral versus multivitamin supplementation on maternal, newborns' biochemical indicators and birth size: a double‐blind randomized clinical trial. Oman Medical Journal 2014;29(2):123‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanumihardjo SA. Vitamin A and iron status are improved by vitamin A and iron supplementation in pregnant Indonesian women. Journal of Nutrition 2002;132:1909‐12. [DOI] [PubMed] [Google Scholar]
- Makola D, Ask DM, Tatala SR, Latham MC, Ndossi G, Mehansho H. A micronutrient‐fortified beverage prevents iron deficiency, reduces anemia and improves the hemoglobin concentration in pregnant Tanzanian women. Journal of Nutrition 2003;133:1339‐46. [DOI] [PubMed] [Google Scholar]; Tatala SR, Ash D, Makola D, Latham M, Ndosi G, Grohn Y. Effect of micronutrient fortified beverage on nutritional anaemia during pregnancy. East African Medical Journal 2002;79(11):598‐603. [DOI] [PubMed] [Google Scholar]
- Thauvin E, Fusselier M, Arnaud J, Faure H, Favier M, Coudray C, et al. Effects of multivitamin mineral supplement on zinc and copper status during pregnancy. Biological Trace Element Research 1992;32:405‐14. [DOI] [PubMed] [Google Scholar]
- Vadillo‐Ortega F, Perichart‐Perera O, Espino S, Avila‐Vergara MA, Ibarra I, Ahued R, et al. Effect of supplementation during pregnancy with L‐arginine and antioxidant vitamins in medical food on pre‐eclampsia in high risk population: randomised controlled trial. BMJ 2011;342:d2901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb AL, Aboud S, Furtado J, Murrin C, Campos H, Fawzi WW, et al. Effect of vitamin supplementation on breast milk concentrations of retinol, carotenoids and tocopherols in HIV‐infected Tanzanian women. European Journal of Clinical Nutrition 2009;63(3):332‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wibowo N, Purwosunu Y, Sekizawa A, Farina A, Idriansyah L, Fitriana I. Antioxidant supplementation in pregnant women with low antioxidant status. Journal of Obstetrics & Gynaecology Research 2012;38(9):1152‐61. [DOI] [PubMed] [Google Scholar]
- Wijaya‐Erhardt M, Muslimatun S, Erhardt JG. Fermented soyabean and vitamin C‐rich fruit: a possibility to circumvent the further decrease of iron status among iron‐deficient pregnant women in Indonesia. Public Health Nutrition 2011;14(12):2185‐96. [DOI] [PubMed] [Google Scholar]
- Wijaya‐Erhardt M, Muslimatun S, Erhardt G. Effect of an educational intervention related to health and nutrition on pregnant women in the villages of Central Java Province, Indonesia. Health Education Journal 2014;73(4):370‐81. [Google Scholar]
- Hernandez A, Garcia‐Guerra A, Dominguez CP, Garcia‐Feregrino R, Neufeld LM. Effect of three supplements with identical micronutrient content on anemia in pregnant Mexican women. FASEB Journal 2008;22:Abstract no: 677.8. [Google Scholar]; Young SL, Blanco I, Hernandez‐Cordero S, Pelto GH, Neufeld LM. Organoleptic properties, ease of use, and perceived health effects are determinants of acceptability of micronutrient supplements among poor Mexican women. Journal of Nutrition 2010;140(3):605‐11. [DOI] [PubMed] [Google Scholar]
- Zavaleta N, Caulfield LE, Garcia T. Changes in iron status during pregnancy in peruvian women receiving prenatal iron and folic acid supplements with or without zinc. American Journal of Clinical Nutrition 2000;71(4):956‐61. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
- Adu‐Afarwuah S, Lartey A, Okronipa H, Maleta K, Ashorn P, Ashorn U, et al. Efficacy of LNS products for pregnant and lactating women: pregnancy outcomes from the iLiNS‐dyad studies in Ghana and Malawi. Annals of Nutrition and Metabolism 2013;63:24‐5. [Google Scholar]; Ashorn P, Alho L, Ashorn U, Cheung YB, Dewey KG, Harjunmaa U, et al. The impact of lipid‐based nutrient supplement provision to pregnant women on newborn size in rural Malawi: a randomized controlled trial. American Journal of Clinical Nutrition 2015;101(2):387‐97. [DOI] [PubMed] [Google Scholar]
- Gathwala G. Effect of antenatal multiple micronutrient supplementation of mothers on the birthweight of their infants. Journal of Paediatrics and Child Health 2012;48(Suppl 1):47‐8. [Google Scholar]
References to ongoing studies
- Biggs BA. A randomised controlled trial to compare the impact on birth weight of daily iron‐folic acid, twice weekly iron‐folic acid and twice weekly multiple micronutrient supplementation for pregnant women in Ha Nam province, Vietnam. Australian New Zealand Clinical Trials Registry (www.anzctr.org.au) (accessed 16 February 2011)2011.
- Adu‐Afarwuah S, Lartey A, Okronipa H, Maleta K, Ashorn P, Ashorn U, et al. Efficacy of LNS products for pregnant and lactating women: Pregnancy outcomes from the iLiNS‐dyad studies in Ghana and Malawi. Annals of Nutrition and Metabolism 2013;63:24‐5. [Google Scholar]; Adu‐Afarwuah S, Lartey A, Okronipa H, Peerson J, Vosti S, Ashorn P, et al. Lipid‐based nutrient supplement for pregnant women improve birth outcomes among primiparous but not multiparous women in Ghana. FASEB Journal 2014;28(1 Suppl 1):Abstract no: 256.7. [Google Scholar]; Dewey KG. Efficacy of lipid‐based nutrient supplements (LNS) for pregnant and lactating women and their infants. ClinicalTrials.gov (http://clinicaltrials.gov/) (accessed 15 February 2011)2011. [DOI] [PMC free article] [PubMed]; Oaks B, Adu‐Afarwuah S, Lartey A, Stewart C, Ashorn P, Vosti S, et al. Lipid‐based nutrient supplementation during pregnancy decreases maternal cortisol in younger women. FASEB Journal 2014;28(1 Suppl 1):Abstract no. 389.6. [Google Scholar]
- Hirschberg AL. Supplementation with WellnessPack mama during pregnancy and lactation‐ a randomized double‐blind, placebo‐controlled study. ClinicalTrials.gov (http://clinicaltrials.gov/) [accessed 2 September 2014]2014.
- Jobarteh ML, Moore S, Kennedy C, Gambling L, McArdle HJ. The effect of nutritional supplementation during pregnancy on placental transporter expression in placentas from gambian women. Placenta 2013;34(9):A81‐2. [Google Scholar]; Moore S. Investigating the effects of pre‐natal and infancy nutritional supplementation on infant immune development in The Gambia: the Early Nutrition and Immune Development (ENID) trial. Current Clinical Trials (http://www.current‐trials.com) (accessed 8 July 2011). [DOI] [PMC free article] [PubMed]; Moore SE, Fulford AJC, Darboe MK, Jobarteh ML, Jarjou LM, Prentice AM. A randomized trial to investigate the effects of pre‐natal and infant nutritional supplementation on infant immune development in rural Gambia: The ENID trial: Early Nutrition and Immune Development. BMC Pregnancy and Childbirth 2012;12:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harding KL, Matias SL, Moniruzzaman M, Stewart CP, Mridha MK, Vosti SA, et al. Rang‐Din Nutrition Study: assessment of participant adherence to lipid‐based nutrient and iron‐folic acid supplements among pregnant and lactating women in the context of a study on the effectiveness of supplements in Bangladesh. FHI 360/FANTA. Washington, DC: US Agency for International Development (USAID), 2014. [Google Scholar]; Mridha M, Chaparro C, Paul R, Hussain S, Vosti S, Matias S, et al. Lipid‐based nutrient supplements for pregnant women reduce newborn stunting in Bangladesh. FASEB Journal 2014;28(1 Suppl):Abstract no: 256.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramakrishnan U. Impact of pre‐pregnancy micronutrient supplementation on maternal and child outcomes. ClinicalTrials.gov (https://clinicaltrials.gov/) (accessed 20 September 2012)2012.
- Tu N, King JC, Dean D, Dirren H. Effect of food‐based supplement prior to and during pregnancy on birth weight and prematurity in rural Vietnam (VINAVAC study). Annals of Nutrition & Metabolism 2013;63(Suppl 1):806, Abstract no: PO3314. [Google Scholar]; Tu N, King JC, Dirren H, Thu HN, Ngoc QP, Diep AN. Effect of animal‐source food supplement prior to and during pregnancy on birthweight and prematurity in rural Vietnam: a brief study description. Food and Nutrition Bulletin 2014;35(4 Suppl):S205‐S208. [DOI] [PubMed] [Google Scholar]
Additional references
- Allen LH. Multiple micronutrients in pregnancy and lactation: an overview. American Journal of Clinical Nutrition 2005;81(5):1206S–1212S. [DOI] [PubMed] [Google Scholar]
- WHO Secretariat, Andersson M, Benoist B, Delange F, Zupan J. Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2‐years‐old: conclusions and recommendations of the technical consultation. Public Health Nutrition 2007;10(12A):1606‐11. [DOI] [PubMed] [Google Scholar]
- Benoist B, McLean E, Andersson M, Rogers L. Iodine deficiency in 2007: global progress since 2003. Food and Nutrition Bulletin 2008;29(3):195‐202. [DOI] [PubMed] [Google Scholar]
- Berti C, Biesalski HK, Gärtner R, Lapillonne A, Pietrzik K, Poston L, et al. Micronutrients in pregnancy: current knowledge and unresolved questions. Clinical Nutrition (Edinburgh, Scotland) 2011;30(6):689‐701. [DOI] [PubMed] [Google Scholar]
- Bhutta ZA, Haider BA. Maternal micronutrient deficiencies in developing countries. Lancet 2008;371(9608):186‐7. [DOI] [PubMed] [Google Scholar]
- Bhutta ZA, Haider BA. Prenatal micronutrient supplementation: Are we there yet?. CMAJ : Canadian Medical Association Journal 2009;180(12):1188‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta ZA, Imdad A, Ramakrishnan U, Martorell R. Is it time to replace iron folate supplements in pregnancy with multiple micronutrients?. Paediatric and Perinatal Epidemiology 2012;26 Suppl 1:27‐35. [DOI] [PubMed] [Google Scholar]
- Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence‐based interventions for improvement of maternal and child nutrition: what can be done and at what cost?. Lancet 2013;382(9890):452‐77. [DOI] [PubMed] [Google Scholar]
- Black RE. Micronutrients in pregnancy. British Journal of Nutrition 2001;85 Suppl 2:S193‐S197. [DOI] [PubMed] [Google Scholar]
- Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, Onis M, et al. Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet 2013;382:427‐51. [DOI] [PubMed] [Google Scholar]
- Caulfield L, Zavaleta N, Shankur AH, Merialdi M. Potential contribution of maternal zinc supplementation during pregnancy to maternal and child survival. American Journal of Clinical Nutrition 1998;65:S499‐S508. [DOI] [PubMed] [Google Scholar]
- Christian P, Osrin D, Manandhar DS, Khatry SK, L Costello AM, West KP Jr. Antenatal micronutrient supplements in Nepal. Lancet 2005;366:711‐2. [DOI] [PubMed] [Google Scholar]
- Christian P. Evidence of multiple micronutrient supplementation (MMS) in pregnancy. Sight and Life 2015;29(1):28‐34. [Google Scholar]
- Datta S, Alfaham M, Davies DP, Dunstan F, Woodhead S, Evans J, et al. Vitamin D deficiency in pregnant women from a non‐European ethnic minority population‐‐an interventional study. BJOG: an international journal of obstetrics and gynaecology 2002;109(8):905‐8. [DOI] [PubMed] [Google Scholar]
- De‐Regil LM, Fernandez‐Gaxiola AC, Dowswell T, Pena‐Rosas JP. Effects and safety of periconceptional folate supplementation for preventing birth defects. Cochrane Database of Systematic Reviews 2010, Issue 10. [DOI: 10.1002/14651858.CD007950.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn JT. Iodine supplementation and the prevention of cretinism. Annals of New York Academy of Sciences 1993;678:158‐68. [DOI] [PubMed] [Google Scholar]
- Edmond K, Hurt L, Fenty J, Amenga‐Etego S, Zandoh C, Hurt C, et al. Effect of vitamin A supplementation in women of reproductive age on cause‐specific early and late infant mortality in rural Ghana: ObaapaVitA double‐blind, cluster‐randomised, placebo‐controlled trial. BMJ Open 2012;2(1):e000658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fall CH, Fisher DJ, Osmond C, Margetts BM, Maternal Micronutrient Supplementation Study Group. Multiple micronutrient supplementation during pregnancy in low‐income countries: a meta‐analysis of effects on birth size and length of gestation. Food and Nutrition Bulletin 2009;30(4 Suppl):S533‐S546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO/WHO. Vitamin and mineral requirements in human nutrition. 2nd ed.World Health Organization and Food and Agriculture Organization of theUnited Nations; 2004.. Vitamin and mineral requirements in human nutrition. 2nd Edition. World Health Organization and Food and Agriculture Organization of the United Nation, 2004. [Google Scholar]
- Food, Nutrition Bulletin. Multiple Micronutrient Supplementation During Pregnancy in Developing Country Settings. www.cmamforum.org/Pool/Resources/Multiple‐micronutrient‐suppl‐during‐pregnancy‐FNB‐2009.pdf (accessed 11 March 2015):Table 1: S538. [DOI] [PubMed]
- Ginde AA, Sullivan AF, Mansbach JM, Camargo CA Jr. Vitamin D insufficiency in pregnant and nonpregnant women of childbearing age in the United States. American Journal of Obstetrics and Gynecology 2010;202(5):436.e1‐436.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider BA, Yakoob MY, Bhutta ZA. Effect of multiple micronutrient supplementation during pregnancy on maternal and birth outcomes. BMC Public Health 2011;11 Suppl 3:S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider BA, Olofin I, Wang M, Spiegelman D, Ezzati M, Fawzi WW, et al. Anaemia, prenatal iron use, and risk of adverse pregnancy outcomes: systematic review and meta‐analysis. BMJ 2013;346:f3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess SY, King JC. Effects of maternal zinc supplementation on pregnancy and lactation outcomes. Food and Nutrition Bulletin 2009;30(1):S60‐S78. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
- Huffman SL, Baker J, Shumann J, Zehner ER. The case for promoting multiple vitamin/mineral supplements for women of reproductive age in developing countries. The LINKAGES Project (www.linkagesproject.org) (accessed 26 April 2003)1998.
- Huffman SL, Habicht JP, Scrimshaw N. Micronutrient supplementation in pregnancy. Lancet 2005;366:2001. [DOI] [PubMed] [Google Scholar]
- Jiang T, Christian P, Khatry SK, Wu L, West KP Jr. Micronutrient deficiencies in early pregnancy are common, concurrent, and vary by season among rural Nepali pregnant women. Journal of Nutrition 2005;135(5):1106‐12. [DOI] [PubMed] [Google Scholar]
- Kawai K, Spiegelman D, Shankar AH, Fawzi WW. Maternal multiple micronutrient supplementation and pregnancy outcomes in developing countries: meta‐analysis and meta‐regression. Bulletin of the World Health Organization 2011;89(6):402‐411B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keen CL, Clegg MS, Hanna LA, Lanoue L, Rogers JM, Daston GP, et al. The plausibility of micronutrient deficiencies being a significant contributing factor to the occurrence of pregnancy complications. Journal of Nutrition 2003;133:1597S–1605S. [DOI] [PubMed] [Google Scholar]
- Kramer MS. The epidemiology of adverse pregnancy outcomes: an overview. Journal of Nutrition 2003;133:1592S–1596S. [DOI] [PubMed] [Google Scholar]
- Margetts BM, Fall CH, Ronsmans C, Allen LH, Fisher DJ, Maternal Micronutrient Supplementation Study Group. Multiple micronutrient supplementation during pregnancy in low‐income countries: review of methods and characteristics of studies included in the meta‐analyses. Food and Nutrition Bulletin 2009;30(4 Suppl):S517‐S526. [DOI] [PubMed] [Google Scholar]
- McArdle HJ, Ashworth CJ. Micronutrients in fetal growth and development. British Medical Bulletin 1999;55:499‐510. [DOI] [PubMed] [Google Scholar]
- Murray‐Kolb LE, Chen L, Chen P, Shapiro M, Caulfield L. CHERG iron report: maternal mortality, child mortality, perinatal mortality, child cognition, and estimates of prevalence of anemia due to iron deficiency. CHERG Iron Report (cherg.org/publications/iron‐report.pdf) (accessed 3 February 2015)2013.
- Oppenheimer SJ. Iron and its relation to immunity and infectious disease. Journal of Nutrition 2001;131:616S–635S. [DOI] [PubMed] [Google Scholar]
- Oriji VK, Enyindah CE, Nyeche S. Factors determining compliance to routine iron supplementation in pregnancy at the University of Portharcout Teaching Hospital. Nigerian Journal of Medicine 2011;20(1):131‐4. [PubMed] [Google Scholar]
- Ota E, Mori R, Middleton P, Tobe‐Gai R, Mahomed K, Miyazaki C, et al. Zinc supplementation for improving pregnancy and infant outcome. Cochrane Database of Systematic Reviews 2015, Issue 2. [DOI: 10.1002/14651858.CD000230.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozaltin E, Hill K, Subramanian SV. Association of maternal stature with offspring mortality, underweight, and stunting in low‐ to middle‐income countries. JAMA 2010;303(15):1507‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathak P, Kapil U, Kapoor SK, Saxena R, Kumar A, Gupta N, et al. Prevalence of multiple micronutrient deficiencies amongst pregnant women in a rural area of Haryana. Indian Journal of Pediatrics 2004;71(11):1007‐14. [DOI] [PubMed] [Google Scholar]
- Peña‐Rosas JP, De‐Regil LM, Garcia‐Casal MN, Dowswell T. Daily oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD004736.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramakrishnan U, Grant FK, Goldenberg T, Bui V, Imdad A, Bhutta ZA. Effect of multiple micronutrient supplementation on pregnancy and infant outcomes: a systematic review. Paediatric and Perinatal Epidemiology 2012;26(suppl):153‐67. [DOI] [PubMed] [Google Scholar]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- Ronsmans C, Fisher DJ, Osmond C, Margetts BM, Fall CH, Maternal Micronutrient Supplementation Study Group. Multiple micronutrient supplementation during pregnancy in low‐income countries: a meta‐analysis of effects on stillbirths and on early and late neonatal mortality. Food and Nutrition Bulletin 2009;30(4 Suppl):S547‐S555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachan A, Gupta R, Das V, Agarwal A, Awasthi PK, Bhatia V. High prevalence of vitamin D deficiency among pregnant womenand their newborns in northern India. American Journal of Clinical Nutrition 2005;81(5):1060‐4. [DOI] [PubMed] [Google Scholar]
- Seck BC, Jackson RT. Determinants of compliance with iron supplementation among pregnant women in Senegal. Public Health Nutrition 2008;11(6):596‐605. [DOI] [PubMed] [Google Scholar]
- Shrimpton R, Dalmiya N, Danton‐Hill I, Gross R. Micronutrient supplementation in pregnancy. Lancet 2005;366:2001‐2. [DOI] [PubMed] [Google Scholar]
- Siegfried N, Irlam JH, Visser ME, Rollins NN. Micronutrient supplementation in pregnant women with HIV infection. Cochrane Database of Systematic Reviews 2012, Issue 3. [DOI: 10.1002/14651858.CD009755] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens G, Finucane M, De‐Regil L, Paciorek C, Flaxman S, Branca F, et al. Global,regional, and national trends in total and severe anaemia prevalence in children and pregnant and non‐pregnant women. Lancet Global Health 2013;1(1):e16‐e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tielsch JM, Rahmathullah L, Katz J, Thulasiraj RD, Coles C, Sheeladevi S, et al. Maternal night blindness during pregnancy is associated with low birthweight, morbidity, and poor growth in South India. Journal of Nutrition 2008;138:787–92. [DOI] [PubMed] [Google Scholar]
- UNICEF. Composition of a multi‐micronutrient supplement to be used in pilot programmes among pregnant women in developing countries 1999. UNICEF (www.UNICEF.org) (accessed 25 April 2003)1999.
- Voigt M, Rochow N, Jährig K, Straube S, Hufnagel S, Jorch G. Dependence of neonatal small and large for gestational age rates on maternal height and weight ‐ an analysis of the German Perinatal Survey. Journal of Perinatal Medicine 2010;38(4):425‐30. [DOI] [PubMed] [Google Scholar]
- Walker N, Fischer‐Walker C, Bryce J, Bahl R, Cousens S. Standards for CHERG reviews of intervention effects on child survival. International Journal of Epidemiology 2010;39 Suppl 1:i21–i31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessells KR, Brown KH. Estimating the global prevalence of zinc deficiency: results based on zinc availability in national food supplies and the prevalence of stunting. PloS One 2012;7:e50568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Iron deficiency anaemias: report of a WHO study group. WHO Technical Report Series (http://whqlibdoc.who.int/trs/WHO_TRS_182.pdf) (accessed 1 February 2014)1959; Vol. 182. [PubMed]
- Kelly A, Kevanya J, Onis M, Shah PM. A WHO collaborative study of maternal anthropometry and pregnancy outcomes. International Journal of Gynecology & Obstetrics 1996;53:219‐33. [DOI] [PubMed] [Google Scholar]
- FAO/WHO. Vitamin and Mineral Requirements in Human Nutrition: Joint FAO/WHO Expert Consultation. 2nd Edition. WHO/FAO, 2004. [Google Scholar]
- WHO. Global Prevalence of Vitamin A Deficiency in Populations at Risk 1995–2005. WHO Global Database on Vitamin A Deficiency. Geneva: World Health Organization, 2009. [Google Scholar]
- WHO. Guideline: Daily Iron and Folic Acid Supplementation in Pregnant Women. Geneva: World Health Organization, 2012. [PubMed] [Google Scholar]
References to other published versions of this review
- Haider BA, Bhutta ZA. Multiple‐micronutrient supplementation for women during pregnancy. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD004905.pub2] [DOI] [PubMed] [Google Scholar]
- Haider BA, Bhutta ZA. Multiple‐micronutrient supplementation for women during pregnancy. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD004905.pub3] [DOI] [PubMed] [Google Scholar]


