Abstract
Background
Current guidelines recommend oral anticoagulation therapy for patients with atrial fibrillation (AF) with one or more risk factors for stroke; however, anticoagulation control (time in therapeutic range (TTR)) with vitamin K antagonists (VKAs) is dependent on many factors. Educational and behavioural interventions may impact patients' ability to maintain their international normalised ratio (INR) control. This is an updated version of the original review first published in 2013.
Objectives
To evaluate the effects of educational and behavioural interventions for oral anticoagulation therapy (OAT) on TTR in patients with AF.
Search methods
We updated searches from the previous review by searching the Cochrane Central Register of Controlled Trials (CENTRAL) and the Database of Abstracts of Reviews of Effects (DARE) in The Cochrane Library (January 2016, Issue 1), MEDLINE Ovid (1949 to February week 1 2016), EMBASE Classic + EMBASE Ovid (1980 to Week 7 2016), PsycINFO Ovid (1806 to Week 1 February 2016) and CINAHL Plus with Full Text EBSCO (1937 to 16/02/2016). We applied no language restrictions.
Selection criteria
We included randomised controlled trials evaluating the effect of any educational and behavioural intervention compared with usual care, no intervention, or intervention in combination with other self‐management techniques among adults with AF who were eligible for, or currently receiving, OAT.
Data collection and analysis
Two of the review authors independently selected studies and extracted data. Risk of bias was assessed using the Cochrane 'Risk of bias' tool. We included outcome data on TTR, decision conflict (patient's uncertainty in making health‐related decisions), percentage of INRs in the therapeutic range, major bleeding, stroke and thromboembolic events, patient knowledge, patient satisfaction, quality of life (QoL), beliefs about medication, illness perceptions, and anxiety and depression. We pooled data for three outcomes ‐ TTR, anxiety and depression, and decision conflict ‐ and reported mean differences (MD). Where insufficient data were present to conduct a meta‐analysis, we reported effect sizes and confidence intervals (CI) from the included studies. We evaluated the quality of evidence using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) framework.
Main results
Eleven trials with a total of 2246 AF patients (ranging from 14 to 712 by study) were included within the review. Studies included education, decision aids, and self‐monitoring plus education interventions. The effect of self‐monitoring plus education on TTR was uncertain compared with usual care (MD 6.31, 95% CI ‐5.63 to 18.25, I2 = 0%, 2 trials, 69 participants, very low‐quality evidence). We found small but positive effects of education on anxiety (MD ‐0.62, 95% CI ‐1.21 to ‐0.04, I2 = 0%, 2 trials, 587 participants, low‐quality evidence) and depression (MD ‐0.74, 95% CI ‐1.34 to ‐0.14, I2 = 0%, 2 trials, 587 participants, low‐quality evidence) compared with usual care. The effect of decision aids on decision conflict favoured usual care (MD ‐0.1, 95% CI ‐0.17 to ‐0.02, I2 = 0%, 2 trials, 721 participants, low‐quality evidence).
Authors' conclusions
This review demonstrates that there is insufficient evidence to draw definitive conclusions regarding the impact of educational or behavioural interventions on TTR in AF patients receiving OAT. Thus, more trials are needed to examine the impact of interventions on anticoagulation control in AF patients and the mechanisms by which they are successful. It is also important to explore the psychological implications for patients suffering from this long‐term chronic condition.
Keywords: Aged; Humans; Middle Aged; Administration, Oral; Anticoagulants; Anticoagulants/administration & dosage; Anticoagulants/adverse effects; Anxiety; Anxiety/prevention & control; Atrial Fibrillation; Atrial Fibrillation/blood; Atrial Fibrillation/complications; Chronic Disease; Decision Support Techniques; Drug Monitoring; Drug Monitoring/methods; Drug Monitoring/standards; International Normalized Ratio; International Normalized Ratio/standards; Medication Adherence; Patient Education as Topic; Randomized Controlled Trials as Topic; Self Care; Self Care/methods; Stroke; Stroke/blood; Stroke/etiology; Stroke/prevention & control
Plain language summary
Educational and behavioural interventions to increase the time in the therapeutic range for patients with atrial fibrillation on anticoagulant therapy
Review question
We reviewed the evidence about the effects of educational and behavioural interventions in patients with atrial fibrillation who are taking oral anticoagulant medication.
Background
Atrial fibrillation is characterised by an irregular heartbeat and places people at greater risk of forming blood clots and having a stroke. To reduce stroke risk, medication that 'thins the blood' is used, known as oral anticoagulants. For patients taking warfarin, regular patient monitoring assesses the time it takes for blood to clot, known as the international normalised ratio (INR), to ensure that the target therapeutic range of 2.0 to 3.0 is maintained. This is often difficult to achieve due to the many factors that can affect INR control such as alcohol intake, other medications, and food.
Educational and behavioural interventions may play an important role in improving the ability of people with atrial fibrillation to maintain their INR control, by increasing patient knowledge and understanding.
Study characteristics
This is an update of the original review first published in 2013. We searched scientific databases in February 2016 and found 11 randomised clinical trials including 2246 adults with atrial fibrillation who were taking oral anticoagulant medication. The trials we found compared education, decision aids, and self‐monitoring plus education to usual care, over any length of time.
Key results
Few studies had comparable groups and data. There was uncertainty about the effect of self‐monitoring plus education on the percentage of time the INR was within the therapeutic range because the proportion or time in the therapeutic range was similar between individuals who received self‐monitoring plus education and those who did not. There were small and positive effects on anxiety and depression in individuals who received education compared to those who received usual care. There were small and negative effects on decision conflict in individuals who received decision aids compared to those who received usual care.
Quality of the evidence
The evidence should be interpreted with caution as the quality of the evidence ranged from very low to low across different outcomes because of the limitations of individual studies. It is likely that further high‐quality trials may affect these reported results.
Summary of findings
Summary of findings for the main comparison. Education, self‐monitoring plus education, and decision aids compared to usual care for oral anticoagulant therapy in patients with atrial fibrillation.
| Education, self‐monitoring plus education, and decision aids compared to usual care for oral anticoagulant therapy in patients with atrial fibrillation | |||||||
| Patient or population: oral anticoagulant therapy in patients with atrial fibrillation Setting: hospital, anticoagulation clinic, general physician practice, or research clinic Intervention: education, self‐monitoring plus education, or decision aid as noted Comparison: usual care | |||||||
| Outcomes | Intervention | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with usual care | Risk with Intervention | ||||||
| Percentage of time within the therapeutic range | Self‐monitoring plus education | The mean time in therapeutic INR range was 0 | MD 6.31 higher (5.63 lower to 18.25 higher) | Not estimable | 69 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | Indirect comparison as self‐monitoring was compared to placebo and self‐management was compared to placebo, but self‐monitoring and self‐management were not directly compared. |
| HADS anxiety | Education | The mean HADS anxiety was 0 | MD 0.62 lower (1.21 lower to 0.04 lower) | Not estimable | 587 (2 RCTs) | ⊕⊕⊝⊝ LOW 2 3 | |
| HADS depression | Education | The mean HADS depression was 0 | MD 0.74 lower (1.34 lower to 0.14 lower) | Not estimable | 587 (2 RCTs) | ⊕⊕⊝⊝ LOW 2 3 | |
| Decision conflict | Decision aid | The mean decision conflict was 0 | MD 0.1 lower (0.17 lower to 0.02 lower) | Not estimable | 721 (2 RCTs) | ⊕⊕⊝⊝ LOW 2 4 | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; INR: international normalised ratio; MD: mean difference; RCT: randomised controlled trial; HADS: Hospital Anxiety and Depression Scale | |||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||||
1Downgraded due to study limitations including small study bias (all patients had to be eligible for self‐management of oral anticoagulation and therefore may not be representative of all AF patients requiring oral anticoagulation)
2Downgraded due to attrition bias
3Downgraded due to selection bias
4Downgraded due to performance bias
Background
Description of the condition
Atrial fibrillation (AF) is the most common arrhythmia in clinical practice (Kirchhof 2016). The lifetime risk of developing AF is approximately one in four among people aged 40 years or older (Lloyd‐Jones 2004; McManus 2012). The incidence and prevalence of AF is rising (Chugh 2014; Colilla 2013; Krijthe 2013).The prevalence of AF dramatically increases with age, rising from 0.5% at 40 to 50 years of age to 5% to 15% at 80 years (Chugh 2014; Colilla 2013; Heeringa 2006; Krijthe 2013; Lane 2017; Lloyd‐Jones 2004; Miyasaka 2006), with the prevalence being slightly higher in men than in women (Lloyd‐Jones 2004; McManus 2012). One US population‐based study (N = 4618) found the age‐ and sex‐adjusted incidence of AF per 1000 person‐years was 3.04 (95% CI 2.78 to 3.31) in 1980, increasing to 3.68 (95% CI 3.42 to 3.95) in 2000, amounting to a relative increase of 12.6% (Miyasaka 2006). Similar findings in the European Rotterdam Study (N = 6806) found that the overall prevalence of AF was 5.5% to 6.0% in men and 5.1% in women (Heeringa 2006). Recent analyses of the Clinical Practice Research Datalink in the UK demonstrate a constant yearly rise in the prevalence of AF nationally, increasing from 700,000 patients in 2010 to a projected prevalence of between 1.3 million and 1.8 million patients by 2060 (Lane 2017). AF is associated with a five‐fold greater risk of stroke and thromboembolism (Wolf 1991), and the incidence of stroke attributable to AF also increases with age (Lip 2006). AF‐related stroke is likely to be more severe than non‐AF related stroke (Sheikh 2015; Wolf 1991). When including hospital admissions, treatment costs, and long‐term nursing home care, AF accounts for 1% of the total UK healthcare expenditure (Sheikh 2015). Given the increasing incidence and prevalence of AF, these figures are likely to rise.
Patients with an increased risk of stroke (as determined by stroke risk stratification models) should receive long‐term oral anticoagulant therapy (OAT): either vitamin K antagonists (VKA) such as warfarin, or non‐vitamin K antagonist oral anticoagulants (NOAC) such as apixaban, dabigatran, edoxaban, or rivaroxaban, unless contraindicated. In a meta‐analysis, dose‐adjusted OAT, resulting in international normalized ratio (INR) values in the range of 2.0 to 3.0, significantly reduced the risk of ischaemic stroke or thromboembolism in patients with non‐valvular AF by 39% (95% CI 22% to 52%) and 64% (95% CI 41% to 62%), respectively, compared with either aspirin or placebo (Hart 2007). Whilst OAT dramatically reduces stroke risk, the therapeutic range of the INR is narrow and must be maintained. This can be problematic, with INRs greater than 3.0 increasing the risk of major and minor bleeding and INRs less than 2.0 increasing the risk of thromboembolism (Lip 2006). Regular INR monitoring is essential and patients need to carefully adhere to dietary and lifestyle restrictions (Ansell 2004). A retrospective analysis of OAT in the UK demonstrated that only patients with the greatest INR control increased their time to stroke occurrence, with only patients spending over 71% of their time in the target therapeutic range (TTR) benefiting (Morgan 2009). In practice, 51% of patients at high risk of stroke (CHADS2 score 2 or more) remained outside of the target therapeutic range for at least 50% of the time (Morgan 2009). Further, a post hoc analysis of patients enrolled in the Atrial Fibrillation Clopidogrel Trial With Irbesartan for Prevention of Vascular Events (ACTIVE), which randomised AF patients with one additional stroke risk factor to receive clopidogrel 75 mg/day plus aspirin (75 to 100 mg/day recommended dose) or OAT, found that patients with a TTR less than 58% gained no benefit from OAT. The INR must be within the therapeutic range for at least 58% of the time to confer benefit in terms of stroke risk reduction (Connolly 2008). Thus, maintenance of INR is a major concern for both AF patients and healthcare professionals. Furthermore, whilst interventions targeting this patient group ultimately aim to reduce the risk of stroke, patients' TTR is a good short‐term indicator of whether the patients will experience adverse events in the long‐term, thus presenting a useful trial endpoint.
The inherent difficulties associated with VKAs (narrow therapeutic range; drug, alcohol, and food interactions; regular blood tests) have led to the development of NOACs, which have sought to overcome these problems by providing an efficacious and safe alternative treatment that does not require regular monitoring. Several NOACs are now available (apixaban, dabigatran, edoxaban, and rivaroxaban) and all are non‐inferior to warfarin for the prevention of stroke and systemic embolism, with similar (for dabigatran 150 mg twice daily and rivaroxaban) or better safety profiles (dabigatran 110 mg twice daily, apixaban, and edoxaban) and a significant reduction in intracranial haemorrhage for all NOACs (Connolly 2009; Giugliano 2013; Granger 2011; Patel 2011). The use of NOACs may shift the focus of interventions for this patient group, but VKAs (i.e. warfarin) are still widely used in AF patients and it is important to investigate ways in which we can improve the outcomes of patients still taking VKAs and whether the principles used for interventions with this group are also relevant for those taking NOACs.
Given that AF is a chronic condition that places patients at increased risk of mortality and morbidity ‐ particularly from stroke ‐ and often requires life‐long treatment, including chronic OAT, the educational materials and the support given to patients when they are first prescribed OAT are crucial for the maintenance of their treatment regimens.
Description of the intervention
Attempts to support behaviour change can take numerous forms. At the individual level they almost always fall into the category of 'education or communication' and may use one or more behaviour change techniques (Michie 2011; NICE 2007). While some interventions are designed to target regimen simplicity or access to testing, education is vital to enable patient uptake and adherence (to medication, treatment regimen, and lifestyle changes). Indeed, patient education for OAT has attempted to influence behaviour by improving knowledge, attitudes, and practices that are necessary to improve health outcomes (Wofford 2008). Yet very few studies define their intervention components in a standardised way, despite novel guidelines that give explicit guidance on how to do so (Michie 2011).
In recent years increased attention has been paid to the classification of behaviour change techniques to aid the development and design of interventions. The behaviour change taxonomy describes 93 distinct techniques that can be applied to understanding a range of health‐related behaviours. The taxonomy was validated using obesity and tobacco use as examples, but can be applied to a range of health behaviours including adherence. Defining an intervention using these techniques at the development stage could influence the success of the intervention (Michie 2009; Michie 2013).
Techniques used in delivering patient education cover a wide spectrum, including the use of booklets and videos as media to transmit information either alone or in addition to self‐management interventions (such as INR self‐monitoring) and interventions that use decision aids (Khan 2004; Man‐Son‐Hing 1999). Patient knowledge surrounding OAT varies with age, with elderly patients (> 75 years) demonstrating poorer knowledge (Tang 2003). In one study, less than half of participants were able to name even one specific benefit, risk, or lifestyle change associated with warfarin (Coehlo‐Dantas 2004). In several cases, spouses were more knowledgeable than the patients and appeared to play a vital role in monitoring the individuals' treatment regimens (Coehlo‐Dantas 2004). Therefore, educational interventions for this patient group may prove to be particularly beneficial.
Other interventions focus on behavioural and practical aspects of lifestyle change and treatment. Behavioural interventions aim to modify patients’ behaviour towards treatment and symptoms (NICE 2007). Interventions that use these principles to promote change include cognitive behavioural therapy (CBT), motivational interviewing, and heart rate variability biofeedback. CBT is a goal‐oriented, systematic procedure which aims to solve problems concerning dysfunctional emotions, behaviours, and cognitions and to promote positive attitude, self efficacy, and planning. However, with any complex intervention it is difficult to determine which component has influenced the behavioural outcome, as researchers often do not define the active components of the intervention and interventions vary in duration and levels of support. Clearly it is important for trials to be explicit about the content and delivery of their interventions and to choose appropriate evaluative tools in order to examine how and why their interventions are successful, by using an applied behaviour change model (Kok 2016; Michie 2011).
How the intervention might work
Interventions for patients with AF who receive OAT should ultimately aim to improve clinical outcomes, primarily reducing the prevalence of stroke and mortality. However, in the short‐term we can aim to increase patients' TTR by focusing on factors that affect treatment adherence. Many factors can affect INR control, such as drug‐drug interactions and variable dietary vitamin K intake (Holbrook 2005), but with adequate knowledge surrounding treatment and lifestyle factors, interventions should aim to encourage behaviour change.
It has been suggested that several factors influence adherence (Horne 2013; Lane 2015; Thrall 2004), and these factors are either intentional or unintentional. Intentional non‐adherence can occur when patients make a decision not to take their treatment as a result of their personal motivations or beliefs, or both (Horne 2013). Unintentional non‐adherence refers to an individual’s skills or ability to take his or her medications (for example problems with remembering to take tablets). Poor INR control could result from both unintentional and intentional non‐adherence (Horne 2013). Where patients' knowledge of their condition and their OAT is limited, this may impact on their practical ability to manage treatment (unintentional) and their perceptions surrounding treatment necessity (intentional). Indeed several studies have demonstrated that patients have poor knowledge of AF and its treatment (Lane 2006; Lip 2002; Nadar 2003; Tang 2003).
There is evidence that patient knowledge correlates significantly with TTR (Tang 2003), with more knowledgeable patients having a better TTR. Thus if education can demonstrate an improvement in TTR, it could have important clinical benefits (that is the reduction of adverse events such as stroke and major bleeding). Decision aids are informative interventions designed to help people make specific choices surrounding their medications, and they may also increase patient knowledge. These interventions aim to reduce decision conflict, which refers to the patient's uncertainty in making health‐related decisions and the factors relating to that uncertainty, which may subsequently impact on treatment uptake and adherence.
Intentional non‐adherence may be more difficult to target and interventions need to focus on inaccurate perceptions of medications. The common sense model (Horne 1999) suggests that patients hold beliefs about the necessity of their prescribed medication (Specific‐Necessity) and concerns about prescribed medication based on beliefs about the danger of dependence and long‐term toxicity as well as the disruptive effects of the medication (Specific‐Concerns). The model also describes general beliefs about medication, assessing beliefs that medicines are addictive and harmful (General‐Harm) and that medicines are over‐prescribed by doctors (General‐Overuse). These beliefs, and the way in which patients balance their concern about medications, have been widely used in predicting medication adherence in a variety of chronic conditions including rheumatoid arthritis (Neame 2005), asthma (Jessop 2003), type II diabetes (Farmer 2006), and depression (Aikens 2005).
A comparison of beliefs about medications between adherent, unintentional non‐adherent, and intentionally non‐adherent patients found significant differences in medication‐related beliefs in patients with a range of chronic illnesses after being newly prescribed medication for the last 10 days (Clifford 2008). Compared with adherers, intentional non‐adherers had significantly lower scores on the necessity sub‐scale of the Beliefs about Medication Questionnaire (P = 0.012), higher scores on the concerns sub scale (P = 0.008), and lower scores on the necessity‐concerns differential (P = 0.001). There were no significant differences between adherers and unintentional non‐adherers (Clifford 2008). Evidently, whilst unintentional non‐adherers may benefit from memory aids (that is reminders, tablet dosettes), intentional non‐adherers may need to address both their perceptions of their medication and misinformation, which may be achieved by increasing patient education surrounding their treatment. Intentional non‐adherers appear to doubt their personal need for their medication and have concerns about taking it when compared to adherers.
More recent models critique the categories of ‘intentional’ and ‘unintentional’, as there is overlap between the categories. For example, whilst forgetting is unintentional it may be influenced by intentional or motivational factors (McHorney 2011). The capability, opportunity and motivation (COM‐B) model of behaviour was developed in order to choose interventions that are most likely to be effective and specific for the individual behaviour (Jackson 2014). This model hypothesises that the interaction between an individual’s capability, opportunity and motivation (COM) cause the performance of behaviour (B). Thus the model provides explanations for why patients do not adhere to treatment regimens. Patient’s capability includes their psychological and physical capacity to engage in necessary thought processes including disease comprehension, cognitive functioning (e.g. memory capacity) and executive function (e.g. capacity to plan). A complex medication regimen, such as with a VKA (i.e. warfarin), might be beyond the psychological planning capabilities of some patients. Motivation is defined as brain processes that energise and direct behaviour such as the perception of illness, beliefs about treatment, self‐efficacy and outcome expectancies. Some evidence suggests that individuals with complex regimens for several conditions choose to take the medication that offers the most symptom relief, or is treating the most feared condition (Nunes 2009). Opportunity is defined as the physical opportunity provided by the environment including cost, access, physical characteristics of the medicine, regimen complexity, social support and the relationship with the health‐care provider (HCP). For VKAs this may include the barriers to regular INR testing, and the social support required to attend appointments and make and maintain lifestyle changes. This model provides a more precise method of defining the causes of non‐adherence, going beyond the dichotomies of intentional and unintentional, and thus may prove to be a useful model when developing interventions with this patient group.
Research suggests that interventions with the greatest likelihood of success are theoretically underpinned, and precisely describe the behavioural change techniques employed to address the needs of target patient group (Michie 2009; Michie 2013).
Why it is important to do this review
AF is a condition that is increasing in prevalence (Chugh 2014; Lane 2017; Miyasaka 2006) and requires treatment with OAT to reduce associated stroke risk. However, patients on VKAs need to maintain a narrow therapeutic INR range, which may be difficult to achieve in practice (Morgan 2009). Patients need sufficient information to make informed choices and actively participate in the management of their own treatment (Lane 2015; Thrall 2004). Patient education aims to influence patient behaviour and improve knowledge, attitudes, and practices that are necessary to improve health outcomes (Wofford 2008), but the efficacy of patient interventions designed to improve AF patient adherence to OAT is not clear. By increasing patient knowledge and understanding surrounding AF and OAT we may reduce the prevalence of intentional and unintentional non‐adherence, and increase patient motivation to adhere, in addition to providing patients with the tools to improve their planning and capability to incorporate the regimen required with VKA therapy into their lifestyle (Jackson 2014), which may subsequently increase TTR. TTR is important and has been shown to be a predictor of thromboembolic or haemorrhagic complications, although it is a surrogate for the hard endpoints such as reductions in mortality and stroke that OAT is aimed at achieving. Many factors influence TTR, including adherence to medication and lifestyle factors (e.g., alcohol intake, diet and other medications), however, TTR does give an indication as to whether patients are adhering to the regimen required for VKA therapy, which should translate into a reduction in stroke and major bleeding events. We updated our previous review (Clarkesmith 2013) to evaluate the value of educational and behavioural interventions for patients with AF who were currently prescribed VKA (mainly warfarin), including the impact on TTR and secondary outcomes such as decision conflict, patient knowledge, and quality of life.
Objectives
To evaluate the effects on TTR of educational and behavioural interventions for OAT in patients with AF.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) of educational or behavioural interventions with any length of follow‐up and in any language.
Types of participants
Adults (aged 18 years or older) with AF, categorised according to the European Society of Cardiology (ESC) guidelines (Kirchhof 2016), including:
newly diagnosed AF;
paroxysmal AF, defined as episodes that usually terminate spontaneously (usually in less than 48 hours), but may last for up to seven days;
persistent AF, characterised by an episode lasting more than seven days or requiring termination via cardioversion;
long‐standing persistent AF, where AF has been present for > one year (i.e. permanent AF) but where a rhythm control strategy is adopted;
permanent AF, where AF has been continuous for more than one year and accepted as the 'normal' heart rhythm by the patient and the physician (hence no rhythm control adopted).
AF was diagnosed and documented by electrocardiogram (12‐lead or Holter monitoring). Patients that were eligible for, or currently receiving, OAT were considered for inclusion in this review. We also included studies which included AF patients with other medical conditions in this review. The studies were RCTs comparing at least one intervention with a control group, and including patients with AF as either the study population or a specified subgroup. We only included studies where patients were grouped per indication, that is for patients taking oral anticoagulants for AF, deep vein thrombosis (DVT) or pulmonary embolism (PE), valve replacements, etc, we only included AF patient data within the analysis.
Types of interventions
We considered all types of educational and behavioural interventions given to AF patients who were taking OAT for this systematic review. Educational interventions included those that delivered patient information, such as:
educational booklets;
videos as media to transmit additional information;
self‐management interventions (such as INR self‐monitoring) that also educated patients;
decision aids;
talking interventions.
Behavioural interventions included techniques that attempted to modify patients’ behaviour towards treatment and symptoms, such as:
cognitive behavioural therapy (CBT);
self‐monitoring or management interventions that include significant educational components;
motivational interviewing;
heart rate variability biofeedback.
Interventions could target adults on the individual level or as a group. The intervention may have taken place in the emergency department, a hospital, the home, or in the community and could have been delivered by a nurse, pharmacist, educator, health or medical practitioner, or a multidisciplinary team associated with the hospital or referred to by the hospital. The intervention could have been undertaken at any time point from diagnosis of AF or initiation of OAT (that is not only newly diagnosed AF patients or those newly referred for anticoagulant therapy). We only considered trials where the comparison groups were usual care, no intervention, or the intervention in combination with other self‐management techniques. We defined usual care as standard anticoagulation clinic practice, where patients attended routine INR checks (defined as usual care by the author). We included any length of follow‐up. We have endeavoured to ensure that our review is clearly distinct from the Garcia‐Alamino 2010 review, which exclusively evaluated the effects of self‐monitoring or self‐management of OAT compared to standard monitoring. In particular, we have only included self‐monitoring interventions where they include a clear and distinct educational component (in addition to training on the use of the self‐monitoring device); this should include topics in addition to self‐testing, such as risk information, lifestyle changes, and information pertaining to their condition.
Types of outcome measures
Primary outcomes
The primary outcome measure was TTR, as defined by Rosendaal 1993 (INR 2.0 to 3.0).
Secondary outcomes
The secondary outcomes were:
major bleeding (defined as bleeds that result in death, are life threatening, cause chronic sequelae, or consume major healthcare resources) and minor bleeding (Schulman 2004);
stroke and thromboembolic events;
increased knowledge with regard to AF and anticoagulation therapy;
patient satisfaction;
acceptability of the anticoagulant therapy;
quality of life; psychological well‐being (anxiety and depression);
changes in perception towards AF and INR control;
changes in the patients’ illness beliefs and illness representations;
self‐reported adherence to treatment and a change in the patients’ beliefs about medications;
economic costs of the intervention (cost‐effectiveness);
decision conflict*.
*We included decision conflict as a secondary outcome in the final analysis. Whilst not specified as an outcome of interest in the original protocol, it was highlighted as a common secondary outcome measure in three of the studies included in the final review. For this reason, we decided to include these data within the results. Decision conflict measures (1) healthcare consumers' uncertainty in making a health‐related decision; (2) the factors contributing to the uncertainty; and (3) healthcare consumers' perceived effective decision making.
These outcomes were quantified using validated or non‐validated questionnaires, ratings, or scales.
Search methods for identification of studies
Electronic searches
We updated searches from the previous review (Clarkesmith 2013) by searching the Cochrane Central Register of Controlled Trials (CENTRAL) and the Database of Abstracts of Reviews of Effects (DARE) in The Cochrane Library (January 2016, Issue 1 of 12), MEDLINE Ovid (1949 to February week 1 2016), EMBASE Classic + EMBASE Ovid (1980 to Week 7 2016), PsycINFO Ovid (1806 to Week 1 February 2016) and CINAHL Plus with Full Text EBSCO (1937 to 16/02/2016). See Appendix 1 for the search strategies.
Searching other resources
We handsearched abstract books from national and international cardiology, psychology, and psychiatry conferences to include meetings relating to AF and meetings that discussed the development of educational and behaviour change interventions, including:
European Society of Cardiology;
American College of Cardiology;
American Heart Association;
Society for Behavioural Medicine and the Division of Health Psychology Conference;
European Health Psychology Conference;
Royal College of Psychiatrists Annual Meeting.
We also searched dissertation abstracts (UMI ProQuest Digital Dissertations) and reference lists of all relevant papers to identify other potentially relevant articles.
We did not apply any language restrictions to the searches.
Data collection and analysis
Selection of studies
Two authors (Clarkesmith and Lane) independently scrutinised the titles found from the search and decided on inclusion or exclusion. For the 2016 update, two authors (Clarkesmith and Khaing) independently reviewed the abstracts and papers for inclusion and exclusion. We used Cohen's kappa statistic to assess agreement between the two authors on the selection of articles for inclusion. At the first review stage (June 2010), the kappa coefficient was 98.4%. Following the updated search in 2012, the kappa coefficient was 95%. For the current update, the kappa coefficient was 85%. Where disagreements arose, the full‐text article was accessed to determine whether the study met the inclusion and exclusion criteria and a third author reviewed the studies (Lane). The authors discussed the article and agreement was reached by consensus.
Data extraction and management
Two review authors independently extracted the data. For each trial, the following data were extracted (where available) using a specially designed data extraction form: participants (sample size, age, sex, ethnicity, marital status, type of AF); type of anticoagulation therapy (VKA, i.e.,warfarin, other); type and duration of the interventions (intervention versus usual care or no intervention, other combinations); primary (TTR) and secondary outcomes (increase in knowledge with regard to AF and anticoagulation therapy, decision conflict, time within the therapeutic INR range, patient satisfaction, acceptability of the anticoagulant therapy, quality of life, changes in perception towards AF and INR control, changes in the patients’ illness beliefs and illness representations, changes in the patients’ beliefs about medications, self‐reported adherence, psychological well‐being); length of follow‐up; statistical methods employed; the effect size and its precision. Studies were included in this review if they reported any of the primary or secondary outcomes of interest, regardless of whether the original study's primary or secondary outcomes corresponded with the review's primary or secondary outcomes. For example, if a study reported TTR as a secondary outcome, we included the TTR in this review as part of the primary outcome.
Assessment of risk of bias in included studies
Two review authors (Clarkesmith and Lane) independently assessed the risk of bias of each trial in accordance with guidance in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We determined the risk of bias using the Cochrane 'Risk of bias' tool. We assessed the following criteria.
Random sequence generation (selection bias).
Allocation concealment (selection bias).
Blinding of participants and personnel (performance bias) and of outcome assessors (detection bias).
Incomplete outcome data (attrition bias).
Selective reporting (reporting bias).
Other sources of bias.
We judged each criteria as low risk, high risk, or unclear risk.
Sequence generation
Low risk, if the allocation sequence was generated using techniques such as a random number table; a computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; or cluster randomisation.
High risk, if the allocation sequence was generated using techniques such as odd or even date of birth; date (or day) of admission; hospital or clinic record number.
Unclear risk, if there was insufficient information about the sequence generation process to permit judgement.
Allocation concealment
Low risk, if the allocation concealment used methods such as central allocation (including telephone, web‐based, and pharmacy‐controlled randomisation); sequentially numbered drug containers of identical appearance; sequentially numbered opaque, sealed envelopes.
High risk, if the participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque, or not sequentially numbered); alternation or rotation; date of birth; case record number.
Unclear risk, if the method of concealment was not described or not described in sufficient detail to allow a definite judgement (e.g. if the use of assignment envelopes was described but it remained unclear whether envelopes were sequentially numbered, opaque, and sealed).
Where the method of allocation was unclear, we contacted study authors to provide further details.
Blinding
Low risk, if there was no blinding but the review authors judged that the outcome and the outcome measurement were not likely to be influenced by lack of blinding; if blinding of participants and key study personnel was ensured and it was unlikely that the blinding could have been broken; if either participants or some key study personnel were not blinded but outcome assessment was blinded and the non‐blinding of others was unlikely to introduce bias.
High risk, if there was no blinding or incomplete blinding and the outcome or outcome measurement was likely to be influenced by lack of blinding; if blinding of key study participants and personnel was attempted but it was likely that the blinding could have been broken; if either participants or some key study personnel were not blinded and the non‐blinding of others was likely to introduce bias.
Unclear risk, if there was insufficient information to permit judgement or the study did not address this outcome (e.g. where the blinding was described only as double‐blind without any other details).
Incomplete data assessment (loss of participants, for example with withdrawals, dropouts, protocol deviations)
-
Low risk, if there were no missing outcome data; reasons for missing outcome data were unlikely to be related to the true outcome; missing outcome data were balanced in numbers across intervention groups with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk was not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes was not enough to have a clinically relevant impact on observed effect size; missing data were imputed using appropriate methods; for cluster randomised trials, an error made in statistical analysis when the analysis does not take account of the unit of allocation.
In some studies, the unit of allocation is not a person but is instead a group of people. Sometimes the data from these studies are analysed as if people had been allocated individually. Using individuals as the unit of analysis when groups of people are allocated can result in overly narrow confidence intervals. Thus, where included in meta‐analysis, it can result in studies receiving more weight than is appropriate and this must be accounted for.
High risk, if the reasons for missing outcome data were likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups; for dichotomous outcome data, the proportion of missing outcomes compared with observed event risk was enough to introduce clinically relevant bias in the intervention effect estimate; for continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes was enough to introduce clinically relevant bias in observed effect size; ‘as‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomisation; potentially inappropriate application of simple imputation.
Unclear risk, if there was insufficient reporting of attrition or exclusions to permit judgement (e.g. numbers randomised were not stated, no reasons for missing data were provided), or the study did not address this.
Selective outcome reporting
Low risk, if the study protocol was available and all of the study’s pre‐specified (primary and secondary) outcomes that were of interest in the review were reported in the pre‐specified way; the study protocol was not available, but it was clear that the published reports included all expected outcomes including those that were pre‐specified.
High risk, if not all of the study’s pre‐specified primary outcomes were reported; one or more primary outcomes were reported using measurements, analysis methods, or subsets of the data (e.g. sub scales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting was provided, such as an unexpected adverse effect); one or more outcomes of interest in the review were reported incompletely so that they could not be entered in a meta‐analysis; the study report failed to include results for a key outcome that would be expected to have been reported for such a study.
Unclear risk, if there was insufficient information to permit judgement.
Other sources of bias
Low risk, if the study appeared to be free of other sources of bias.
High risk, if there was at least one important risk of bias (e.g. the study had a potential source of bias related to the specific study design used; stopped early due to some data‐dependent process (including a formal stopping rule); had extreme baseline imbalance; had been claimed to be fraudulent; had some other problem).
Unclear, if there was either insufficient information to assess whether an important risk of bias existed or if there was insufficient rationale or evidence that an identified problem would not introduce bias.
Measures of treatment effect
We undertook statistical analyses as follows. For continuous variables (for example changes in illness perception questionnaire or changes in TTR), we calculated the mean difference (MD) with 95% confidence interval (CI). Had we been able to pool any dichotomous variables, we would have calculated odds ratios (OR) with 95% CI.
Dealing with missing data
Where the article indicated inclusion of AF patients, but data were not included by subgroup, we contacted the authors of the included studies to gather AF‐specific data. We also contacted authors where there was insufficient detail on the demographic data for AF patients or the content of the intervention. We received responses and additional data from several authors (Beyth 2000; Christensen 2007; Clarkesmith 2013; Gadisseur 2003; Hendriks 2013; Polek 2012; Thomson 2007; Vormfelde 2014). For fifteen studies the authors could not be contacted (Al‐Meshal 2013; Lakshmi 2013; Moore 2013; Sawicki 1999; Stone 1989; Verret 2012; Watzke 2000) or did not respond to e‐mail or written requests for unpublished data (Barcellona 2006; Chan 2006; Gardiner 2006; Jank 2009; Menendez‐Jandula 2005; Ryan 2009; Siebenhofer 2007; Yildirim 2015). For two studies, we successfully contacted the authors but the data were unavailable (Machtinger 2007; Moss 2014). If authors responded with data that were incomplete, we contacted them again for further details.
Assessment of heterogeneity
We assessed heterogeneity of studies included in the meta‐analysis using the I2 statistic and Chi2 test for heterogeneity. Data were considered heterogenous if the P value was less than or equal to 0.10, for which random‐effect models were used. Fixed‐effect models were used where the P value was greater than 0.10.
Assessment of reporting biases
There were not enough studies in this review to test for reporting bias, thus we discuss the findings narratively. However, future revisions will test for bias using a funnel plot based on the data for the primary outcome of TTR. Asymmetry of the funnel plot will be taken as an indication of publication bias. Other causes of asymmetry of the funnel plot will also be explored, such as clinical heterogeneity between studies (for example, different control event rates) or methodological heterogeneity between studies (for example, failure to conceal allocation). We summarised information on blinding during both the collection and analysis of study data in a narrative review; this information informed the risk of bias assessments. We also summarised the completeness of the reported data, including any concerns over the exclusion of participants or excessive dropouts. We also reported concerns over the selective reporting of outcomes, time points, or subgroups.
Data synthesis
We combined results of individual studies within a narrative review. Where possible and appropriate, we used meta‐analysis to statistically combine results. We included TTR data if directly reported using the Rosendaal method of calculation (Rosendaal 1993), or where available from personal communication with the authors. For the analysis we used Review Manager to calculate the summary statistics (RevMan 2014). We examined heterogeneity using the Chi2 and the I2 statistics (Higgins 2011). We evaluated the quality of evidence using the GRADE approach (Higgins 2011), and we employed GRADE profiler to to create a 'Summary of findings' table GRADEpro 2015.
Subgroup analysis and investigation of heterogeneity
We carried out subgroup analyses looking at the type of intervention (educational alone, behavioural alone, and a combination of education and behavioural versus usual care). Future revisions may also examine frequency (one session versus multiple sessions) and duration (less than six months versus more than six months) of the intervention, length of time on OAT, men versus women, individual versus group interventions, and age of participant groups, dependant upon the availability of such data in the included study reports.
Sensitivity analysis
There were insufficient studies to carry out sensitivity analyses. However, future revisions of the review may employ sensitivity analyses to examine factors that may lead to differences between the results of individual trials: poor quality versus good quality trials.
Results
Description of studies
Results of the search
The search retrieved 1560 de‐duplicated articles from all sources. Of these, we excluded 1451 by assessing the titles and abstracts. We obtained 109 full‐text articles for consideration.
We excluded 86 articles based on review of the full‐texts. Of these, we included one new study as an ongoing trial. Of the three ongoing trials included in the previous version of this review (Clarkesmith 2013), we included two as studies in this review and excluded one based on subsequent information in the published results suggesting the trial was not randomised (further details are given in the Excluded studies section). We included a total of 20 articles reporting on 11 studies in this review (Figure 1). A further three articles relating to the included studies were found subsequent to the searches and are included as references.
1.
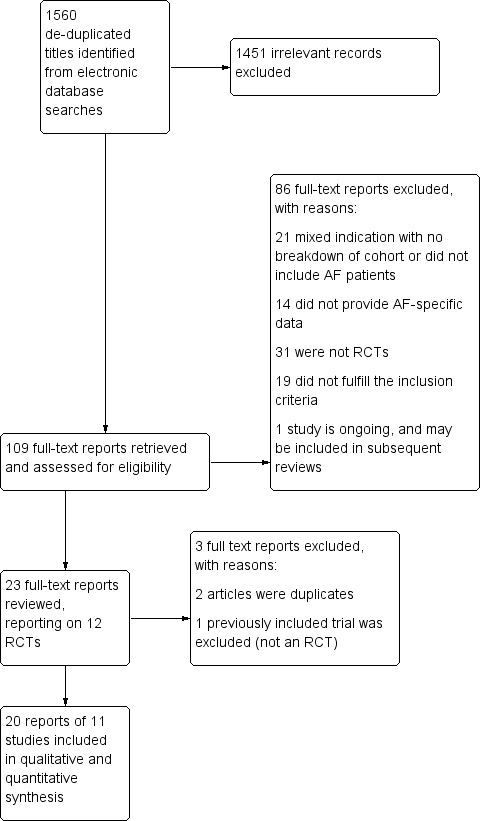
PRIMSA flow chart of included studies.
Included studies
Thirteen articles reporting on eight studies were included in the original Cochrane review (Beyth 2000; Christensen 2007; Gadisseur 2003; Man‐Son‐Hing 1999; McAlister 2005; Polek 2012; Thomson 2007; Voller 2005). For this update we have identified a further ten articles reporting on three studies (Clarkesmith 2013; Hendriks 2013; Vormfelde 2014). Two of these studies were included in the previous review (Clarkesmith 2013) as ongoing trials and now have published results (Clarkesmith 2013; Vormfelde 2014). Features of the interventions are included in the Characteristics of included studies. See the PRISMA flow chart for the inclusion process (Figure 1).
Methods
The 11 included studies were randomised controlled trials. Six of the studies specifically recruited AF patients (Clarkesmith 2013; Hendriks 2013; Man‐Son‐Hing 1999; McAlister 2005; Thomson 2007; Voller 2005). A further five 'mixed' trials recruited patients with a range of indications for OAT (for example AF, venous thromboembolism, cardiovascular disease, heart valve prosthesis, peripheral vascular disease, or myocardial infarction) and the authors provided unpublished data on the AF patients (Beyth 2000; Christensen 2007; Gadisseur 2003; Polek 2012; Vormfelde 2014). Two trials were cluster randomised studies (McAlister 2005; Vormfelde 2014), and one used a Zelen design (Gadisseur 2003).
Participants
The total sample size of 2246 AF patients, including published and unpublished data, varied by trial from 14 to 712 participants (Polek 2012 (unpublished), and Hendriks 2013, respectively). The mean age of the trial participants, from studies that reported age, ranged from 59 to 75 years. One trial did not provide any demographic information for their AF patients (Gadisseur 2003).
Patients were included if they had AF (Clarkesmith 2013; Hendriks 2013; McAlister 2005; Thomson 2007; Voller 2005); had ECG documented AF (Clarkesmith 2013; Hendriks 2013); were receiving intravenous heparin (Beyth 2000); were aged 18 years or over (Christensen 2007; Clarkesmith 2013; Hendriks 2013; McAlister 2005), 60 years or over (Thomson 2007), 65 years or over (Beyth 2000), or 18 to 75 years (Gadisseur 2003); planned to start warfarin (Beyth 2000; Gadisseur 2003; Polek 2012; Thomson 2007); had been taking warfarin for any length of time (Thomson 2007; Vormfelde 2014), greater than three months (Gadisseur 2003), less than 3 months (Clarkesmith 2013), or greater than eight months (Christensen 2007); were accessible via telephone (Polek 2012); and had German language skills (Vormfelde 2014).
Patients were excluded if they had been treated with warfarin at any time in the previous six months (Beyth 2000); had contraindications for warfarin (Clarkesmith 2013); previously received warfarin (Clarkesmith 2013); were admitted from a nursing home (Beyth 2000; Polek 2012); were enrolled in another clinical trial (Beyth 2000; Voller 2005); were too ill to give consent (Beyth 2000) or did not speak English (Beyth 2000; Clarkesmith 2013; McAlister 2005; Polek 2012; Thomson 2007); had previously used self‐management for INR (Christensen 2007); had antiphospholipid syndrome (Gadisseur 2003), a life threatening illness (Gadisseur 2003), life expectancy less than or equal to one year (Clarkesmith 2013; Gadisseur 2003; McAlister 2005), cognitive impairment (Clarkesmith 2013; Gadisseur 2003; McAlister 2005; Polek 2012; Thomson 2007), physical limitations making successful participation impossible (Gadisseur 2003), or poor hearing or eyesight (Voller 2005); had experienced a major haemorrhage in a previous trial (Man‐Son‐Hing 1999); were taking warfarin for another condition (McAlister 2005; Thomson 2007; Voller 2005); were scheduled for cardioversion (McAlister 2005; Thomson 2007) or cardiac surgery (Vormfelde 2014); had a history of psychotic disorder (Polek 2012), previous stroke or transient ischaemic attack (TIA; Thomson 2007), valvular heart disease (Clarkesmith 2013), unstable or uncontrolled hypertension (Vormfelde 2014), unstable heart failure (Vormfelde 2014), untreated hyperthyroidsim (Vormfelde 2014), current or forseen pacemaker (Vormfelde 2014), internal cardioverter defibrillator (Vormfelde 2014), or alcohol or other addiction (Voller 2005).
Types of studies
Of the eleven studies that were identified, five compared education with usual care (Clarkesmith 2013; Gadisseur 2003; Hendriks 2013; Polek 2012) or usual care with an educational booklet (Vormfelde 2014), four compared self‐monitoring plus education with usual care (Beyth 2000; Christensen 2007; Gadisseur 2003; Voller 2005), and one also included a self‐management group (Gadisseur 2003). A further three trials focused on the use of a decision support aid versus usual care (Man‐Son‐Hing 1999; McAlister 2005) or a 'guideline evidence' comparison group (Thomson 2007).
Types of interventions
Interventions were either one to one (Beyth 2000; Hendriks 2013; McAlister 2005; Polek 2012; Vormfelde 2014) or group training sessions (Gadisseur 2003; Voller 2005), or both (Clarkesmith 2013). Three of the trials did not explicitly specify a group or individual intervention type (Christensen 2007; Man‐Son‐Hing 1999; Thomson 2007).
All of the interventions included an educational element, usually consisting of a description of the consequences of minor or major stroke and major haemorrhage, the blood monitoring required for VKA (i.e. warfarin), and the probability of stroke and major haemorrhage for patients taking a VKA. Most interventions also included information regarding the lifestyle factors influencing VKA control and provided written educational materials or a booklet. Two of the interventions also included a video component (Clarkesmith 2013; Vormfelde 2014). Self‐monitoring interventions included training on the use of INR monitoring devices (Beyth 2000; Christensen 2007; Gadisseur 2003; Voller 2005).
Decision aid interventions offered more detailed information on the risks of bleeding and thromboembolism (Man‐Son‐Hing 1999; McAlister 2005; Thomson 2007). All three trials using a decision support aid employed pictograms to depict the risk of stroke and bleeding on either placebo, aspirin, or warfarin; two utilised paper‐based charts (Man‐Son‐Hing 1999; McAlister 2005) and the third used a computerised version (Thomson 2007). The decision aid was presented and patients were asked to select which treatment they would prefer on the basis of the risk information presented in the pictogram (probability trade‐off technique). For example, the consequences of a minor stroke, a major stroke, and minor and major bleeding were described along with the probability of those events occurring whilst taking different treatment options. This gave patients the opportunity to make informed decisions (Man‐Son‐Hing 1999); in this trial patients completed a worksheet which summarised the information following use of the decision aid.
Duration of the intervention
The duration of the educational training element of the interventions varied. Seven trials reported a one‐off consultation of 30 to 60 minutes (Beyth 2000; Clarkesmith 2013; Thomson 2007; Vormfelde 2014) or three to four sessions each lasting 30 to 120 minutes (Gadisseur 2003; Hendriks 2013; Voller 2005). The other four trials did not specify how long the intervention lasted or the number of sessions (Christensen 2007; Man‐Son‐Hing 1999McAlister 2005; Polek 2012).
Intervention facilitator
Two studies did not specify the type of facilitator (Christensen 2007; Voller 2005). Of those that did, facilitators included a lay educator (Beyth 2000); a physician, pharmacist, or healthcare professional (Gadisseur 2003; McAlister 2005; Polek 2012); a computerised audio tool (Man‐Son‐Hing 1999; Thomson 2007); a trainee health psychologist (Clarkesmith 2013); a practice nurse (Vormfelde 2014); and a nurse specialist (Hendriks 2013).
Country
The geographical settings of the studies were: Denmark (Christensen 2007), the Netherlands (Gadisseur 2003; Hendriks 2013), Germany (Voller 2005; Vormfelde 2014), USA (Beyth 2000; Man‐Son‐Hing 1999; Polek 2012), Canada (McAlister 2005), and the UK (Thomson 2007; Clarkesmith 2013).
Setting for the intervention
Most of the interventions were conducted in a hospital or anticoagulation clinic setting (Beyth 2000; Christensen 2007; Clarkesmith 2013; Gadisseur 2003; Hendriks 2013; Man‐Son‐Hing 1999; Polek 2012). Two of the trials took place in general practitioner (GP) practices (McAlister 2005; Vormfelde 2014), with another taking place in a research clinic with patients from general practices (Thomson 2007). One of the trials did not describe the intervention setting (Voller 2005).
Follow‐up
Assessment of the impact of the intervention on outcomes was at three (Polek 2012), six (Beyth 2000; Christensen 2007; Clarkesmith 2013; Gadisseur 2003; Man‐Son‐Hing 1999; Vormfelde 2014), and 12 months (Clarkesmith 2013; Hendriks 2013; McAlister 2005; Thomson 2007).
Funding
Four of the trials declared some funding input by drug companies (Clarkesmith 2013; Gadisseur 2003; Man‐Son‐Hing 1999; Voller 2005).
Excluded studies
We excluded 86 studies for the following reasons.
1. Twenty‐one studies were excluded for not providing a breakdown of a mixed indication cohort per indication (Al‐Meshal 2013; McCahon 2011; Moore 2013; Nilsson 2011; Suriano 2014; Vadher 1996; Vadher 1997; Verret 2012), or not including AF patients (Baker 1991; Bump 1977; Claes 2005; Claes 2006; Cordasco 2009; Cromheecke 2000; Cromheecke 2001; Fitzmaurice 2005; Holbrook 2007; Landefeld 1992; Mazor 2007; Pernod 2008; Waterman 2001).
2. Fourteen studies did not provide AF‐specific findings, and attempts to obtain the specific data from the authors were unsuccessful. For twelve of these studies the authors could not be contacted (Lakshmi 2013; Stone 1989; Sawicki 1999; Watzke 2000), or did not respond to e‐mail or written requests for unpublished data (Barcellona 2006; Chan 2006; Gardiner 2006; Jank 2009; Menendez‐Jandula 2005; Ryan 2009; Siebenhofer 2007; Yildirim 2015). For two studies, the author was successfully contacted but the data were unavailable (Machtinger 2007; Moss 2014).
3. Thirty‐one studies were not RCTs (Armstrong 2011; Bajorek 2005; Blaise 2009; Bloomfield 2011; Burns 2009; Castelino 2010; Corbella 2009; Davis 2005; Duran‐Parrondo 2011; Fraenkel 2011; Hasan 2011; Heidbuchel 2015; Krause 2010; Leger 2004; Megden 1999; Morin 2015; Nedaz 2002; Polzien 2007; Qvist 2016; Reverdin 2011; Saokaew 2010; Satger 2009; Sawicki 2003; Stafford 2011; Taylor 1997; Tuiskula 2011; Turc‐Dessertine 2005; Winans 2010; Witt 2005; Woodend 2005; Wurster 2006).
4. Nineteen studies did not fulfil other predefined inclusion criteria. Seven did not include an educational or behavioural intervention (Field 2010; Fitzmaurice 1996; Fitzmaurice 2000; Gouin‐Thibault 2010; Matchar 2005; Trivalle 2010; Waterman 2001 b). Five studies provided education on self‐monitoring alone with no additional education on AF and the risks and benefits of OAT (Christensen 2011; Dolor 2010; Grunau 2011; Matchar 2010; Sunderji 2005). None of the studies were excluded for including participants <18 years of age. Five studies did not report any of the pre‐specified outcomes (Batty 2001; Jackson 2004; O'Sullivan 2016; PRISM Study group 2003; Peng 2014). One of the studies did not randomise their usual care group (Khan 2004). One of the studies did not have a separate control group; patients acted as their own historical control (Bereznicki 2013).
5. One study eligible for inclusion is an ongoing trial and the results are not yet available (Siebenhofer 2012).
Two studies that were excluded from a previous version of this review as they were ongoing trials are now included (Clarkesmith 2013; Vormfelde 2014), and one has been excluded as it was not an RCT (Stafford 2011).
Risk of bias in included studies
The risk of bias for each of the included studies is summarised in Figure 2 and Figure 3. Individual domains are summarized below, with detailed information for each in the Characteristics of included studies tables.
2.
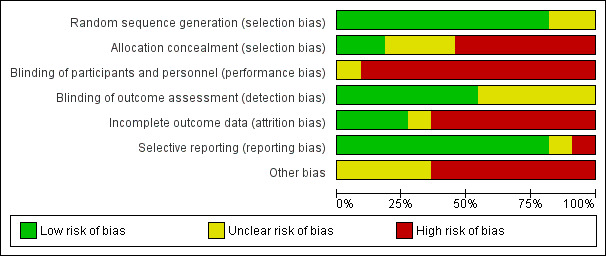
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
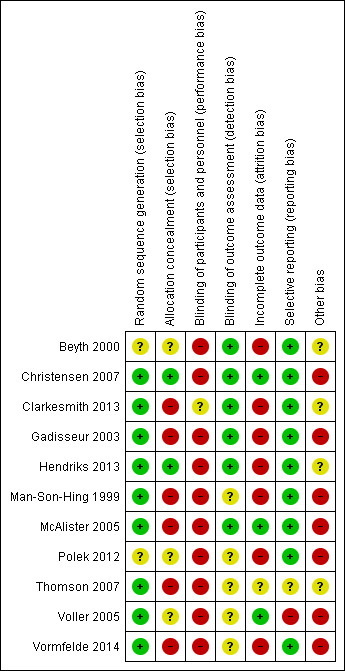
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Nine of the included trials provided information about adequate sequence generation. For the majority of trials this consisted of randomisation to the intervention or usual care according to: a computer‐generated sequence using block randomisation (Christensen 2007; Clarkesmith 2013; Man‐Son‐Hing 1999; McAlister 2005; Thomson 2007); one‐to one randomisation (Hendriks 2013); a random numbers table (Voller 2005); or a two‐step partial‐Zelen design (Gadisseur 2003). The other two trials did not provide details of sequence generation (Beyth 2000; Polek 2012).
Two studies used cluster randomisation at the level of the family physician (McAlister 2005; Vormfelde 2014). All eligible patients within any one physician's practice were allocated to the intervention or usual care practices. This process avoided contamination that may have occurred if the same physician delivering the intervention also delivered usual care.
All of the studies reported the number of eligible participants; however, for the mixed cohort trials it was difficult to retrospectively assess which of the screened patients had AF. Of those trials specifically recruiting AF patients, the percentage of eligible patients randomised ranged from 15% to 94% (Clarkesmith 2013 and Hendriks 2013, respectively). In the mixed indication cohort trials this percentage ranged from 18% to 95% (Gadisseur 2003 and Christensen 2007, respectively). Thus, some of the trials were more representative than others. Those trials that included less than 50% of the eligible participants were at risk of selection bias (Clarkesmith 2013; Gadisseur 2003; Man‐Son‐Hing 1999; McAlister 2005; Thomson 2007; Vormfelde 2014), whereby patient characteristics may affect the study outcomes. For example, those patients that participated may have been more motivated or willing to participate. One study did not report how many participants were eligible for the study (Voller 2005).
Blinding
Blinding patients to the intervention they were receiving was not possible with these types of interventions, nor was it possible to blind the intervention facilitator to which arm the patients were in. This inevitably raises the risk of bias for all studies. Experimenter bias could have occurred in these trials, whereby the individuals delivering the intervention and usual care could behave differently towards a group inadvertently, affecting the study outcome. There was one exception to this (Clarkesmith 2013), where all INR monitoring (primary outcome) was undertaken at an independent anticoagulation clinic where the employees were not aware of the treatment allocation. However, blinding of the outcome assessors (the data analysts or researchers) regarding to which intervention arm the patient was assigned was possible, in principle, and was undertaken in six trials (Beyth 2000; Clarkesmith 2013; Christensen 2007; Gadisseur 2003; Hendriks 2013; McAlister 2005). Five trials did not state whether their outcome assessor was blinded to the group to which the patients were randomised (Man‐Son‐Hing 1999; Polek 2012; Thomson 2007; Voller 2005; Vormfelde 2014) or indeed whether the individual delivering the intervention also carried out the analysis, which inevitably increases the risk of bias.
Incomplete outcome data
The percentage of patients completing the final follow‐up with data available for all outcomes ranged from 55% to 100% (Clarkesmith 2013 and Voller 2005, respectively). Attrition greater than 20% was considered to indicate high risk of bias. Attrition was greater for questionnaire follow‐ups than clinical follow‐ups (such as those trials reporting TTR or cardiovascular death as their primary outcome). If attrition is related to any feature of the study design or instrumentation, or leads to bias between groups, this will increase the risk of bias. Some of the self‐monitoring and decision aid studies reported participants as lost to follow‐up due to an inability to perform the tests or to understand the decision aid. Other reasons included discontinuing warfarin, moving away from the area, death, illness, and hospitalisation. Where patients were unable to use the intervention, this could lead to a high risk of bias, compared to a more 'capable' sample.
Selective reporting
Five of the studies published a protocol paper (Clarkesmith 2013; Hendriks 2013; McAlister 2005; Voller 2005; Vormfelde 2014). McAlister and Hendriks reported on all but one of the pre‐specified outcomes (patient satisfaction). Two studies reported on all of their pre‐specified outcomes (Voller 2005; Vormfelde 2014), although one trial was ended early due to insufficient participant numbers to power the primary outcome (Voller 2005), Clarkesmith reported on all pre‐specified outcomes other than cost‐effectiveness (Clarkesmith 2013). A further six studies did not publish protocol papers (Beyth 2000; Christensen 2007; Gadisseur 2003; Man‐Son‐Hing 1999; Polek 2012; Thomson 2007), but reported on all the outcomes specified within their method section.
Other potential sources of bias
Over the course of the study, participant characteristics may change. With increasing age the participants in these studies were likely to have suffered from additional comorbidities and started taking new medications. These trial designs cannot control for the impact of concomitant medications or the additional burden of new medication regimens across the study period, thus this may have increased the risk of bias for all trials. Four trials required patients to be able to undertake self‐monitoring and/or self‐management of INR (Beyth 2000; Christensen 2007; Gadisseur 2003; Voller 2005), and therefore these patients may not be representative of all patients requiring OAT; however, in one study all patients were aged 65 years or older so the results of this study may be more generalisable to the mainly elderly AF population (Beyth 2000). In two trials there was a difference at baseline between groups in terms of the antithrombotic therapy that patients were receiving (those already receiving warfarin and those not) which could have affected patients' ability to make decisions about treatment (one of the outcomes was decision conflict; McAlister 2005; Thomson 2007). In one study, improvement in knowledge was dependent on the GP practice where the patient education was delivered, most probably due to differences in the patient‐nurse discussions after the video presentation (Vormfelde 2014). In one trial, there was the possibility of contamination between the intervention and usual care groups, as physicians could have provided similar information contained within the educational booklet to the usual care group during routine clinic visits (Man‐Son‐Hing 1999). In two trials, the type of intervention (comprehensive nurse‐led; Hendriks 2013) or the intervention facilitator (health psychologist; Clarkesmith 2013), could suggest that the results may not be applicable outside these settings.
Effects of interventions
See: Table 1
Various methods of measuring outcomes were employed; this was the main obstacle when comparing study findings. This was further complicated by the different time points at which measurements were taken, depending on the length of the trial. Further, the included studies differed in type (behavioural and decision aids) and in their comparator group. Where data were comparable ‐ that is, using the same measurement tool and type of intervention ‐ we requested AF‐specific data if it was not provided in the published article. We report key results in Table 1, and summarize them below by outcome and intervention.
Primary outcomes
TTR
The TTR (INR of 2.0 to 3.0) was reported by five trials (Beyth 2000; Christensen 2007; Clarkesmith 2013; Gadisseur 2003; Vormfelde 2014) as outlined by the Rosendaal method (Rosendaal 1993). One trial reported the TTR in days (Voller 2005). Three trials reported other indicators of INR control: percentage of in‐range INRs (McAlister 2005; Voller 2005), and combined INR and complications outcomes (Christensen 2007). Of those studies reporting TTR, all tested self‐monitoring plus education or education only interventions (Beyth 2000; Christensen 2007; Gadisseur 2003; Vormfelde 2014), but only two published AF‐specific data (Voller 2005; Clarkesmith 2013) and one of those trials did not use the Rosendaal method (Voller 2005). Thus, we contacted the remaining trial authors for AF‐specific data, which were provided by three of the authors (Christensen 2007; Gadisseur 2003; Vormfelde 2014). We did not request AF‐specific data for outcomes that were not comparable; that is, combined INR and complications outcomes (Christensen 2007).
Education intervention
Four of the included trials compared education only and usual care (Clarkesmith 2013; Gadisseur 2003; Polek 2012; Vormfelde 2014). Three of these trials reported TTR (Clarkesmith 2013; Gadisseur 2003; Vormfelde 2014).
Gadisseur 2003 studied a cohort with a mixed indication for OAT and provided additional unpublished data on the AF cohort for the three arms of the trial who received INR self‐monitoring training including education: self‐management, self‐measurement, and routine care in educated patients. They found that the TTR was highest in the educated usual care group (mean 75.0%, SD 18.5%), followed by the self‐measurement group (mean 70.3%, SD 18.7%), followed by the educated usual care group (mean 67.1%, SD 26.4%) and lowest in the self‐management group (mean 64.7%, SD 18.3%). These groups were not comparable to Vormfelde 2014, as there was no control comparator in Vormfelde 2014 that did not receive education. These groups were also not comparable to Clarkesmith 2013 as the education in Gadisseur 2003 was not AF‐specific.
Clarkesmith 2013 studied an AF cohort and found significantly higher TTR in the intervention group (median 76.2%, interquartile range (IQR) 64.1% to 97.3% ) than the usual care group (median 71.3%, IQR 51.2% to 84.7%) at six months, but no significant difference between the groups at 12 months (median 76.0%, IQR 60.5% to 85.0% versus median 70.0%, IQR 62.0% to 79.0%, respectively).
Vormfelde 2014 recruited a mixed indication cohort, but provided unpublished AF‐specific data. TTR was significantly higher in the intervention group (mean 69%, SD 25.1%) compared to the brochure only group (mean 64%, 28.2%) at 6‐months.
Self‐monitoring plus education intervention
Four trials examined the impact of self‐monitoring plus education (Beyth 2000; Christensen 2007; Gadisseur 2003; Voller 2005).
Christensen 2007 recruited patients with multiple indications for OAT, with only 20 AF patients: 11 receiving self‐management plus education and nine in the usual care group. INR control was slightly higher in the intervention group (mean 77.3%, SD 11.6%) than in the usual care group (mean 67.9%, SD 23.5%; MD 9.3%, 95% CI ‐7.5% to 26.2%; not significant).
Gadisseur 2003 was also a mixed cohort trial where the authors provided unpublished data on AF patients. TTR in the self‐monitoring plus education group (mean 70.3%, SD 18.7%) was slightly higher than in the usual care group (mean 67.1%, SD 26.4%; MD 3.2%, 95% CI ‐13.7% to 20.2%; not significant).
Beyth 2000 did not provide AF‐specific data on TTR outcomes and thus could not be included in these analyses.
Voller 2005 reported cumulative percentage of time in INR rather than TTR by the Rosendaal method. TTR in the self‐monitoring group (mean 67.8%, SD 17.6%) was significantly higher than in the usual care group (mean 58.5%, SD 19.8%).
The fixed‐effects pooled analysis of the two studies reporting TTR using the Rosendaal method of calculation demonstrated that self‐monitoring plus education did not significantly improve TTR when compared to usual care (MD 6.3%, 95% CI ‐5.63% to 18.25%; Christensen 2007; Gadisseur 2003; Analysis 1.1; Figure 4).
1.1. Analysis.
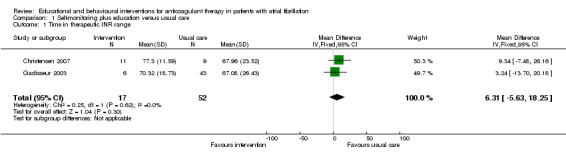
Comparison 1 Self‐monitoring plus education versus usual care, Outcome 1 Time in therapeutic INR range.
4.
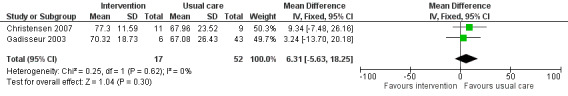
Forest plot of comparison: self‐monitoring plus education versus usual care on time in therapeutic INR range.
Education versus self‐monitoring plus education intervention
One trial compared self‐monitoring plus education with education only (Gadisseur 2003).
Gadisseur 2003 provided unpublished data on AF patients that suggested the TTR was slightly higher in the education only group (mean 75.0%, SD 18.5%) than in the self‐monitoring plus education group (mean 70.3%, SD 18.7%).
Decision aid intervention
One trial reported the percentage of INRs in range (McAlister 2005).
Percentage of INRs within the therapeutic range differed from TTR as the outcome was not calculated using the Rosendaal method (Rosendaal 1993). McAlister 2005 found that INR control deteriorated in the usual care arm over time (INRs were between 2.0 and 3.0 on 66% of the days at three months versus 70% of the days at baseline), while INR control improved in the intervention arm (INRs were between 2.0 and 3.0 on 72% of the days at three months versus 65% at baseline). The between group difference was statistically significant (P = 0.02). By 12 months, INR control in both arms had regressed back to baseline levels. However, the usual care and intervention groups were not well matched at baseline.
Secondary outcomes
Major and minor bleeding, stroke, and thromboembolic events
Two studies reported major bleeding, stroke, and thromboembolic events (Beyth 2000; Clarkesmith 2013), and one provided unpublished AF‐specific data (Beyth 2000). None of the studies reported on minor bleeding. Two studies reported mortality (Beyth 2000; Hendriks 2013), one specified cardiovascular death (Hendriks 2013), but the other did not specify if death was due to a cardiovascular cause (Beyth 2000). Three studies reported the number of thromboembolic or haemorrhagic complications (Clarkesmith 2013; Voller 2005; Vormfelde 2014), with one reporting specifically on those requiring medical treatment (Voller 2005).
Self‐monitoring plus education intervention
One study provided unpublished AF data on major bleeding, stroke, and thromboembolic events (Beyth 2000). This study found the number of cases of major bleeding in the self‐monitoring plus education group (n = 1, 1.8% of total AF cohort) was similar to the number of cases in the usual care group (n = 2, 3.7% of total AF cohort). There were also very few cases of stroke and thromboembolic events in the self‐monitoring plus education (n = 1, 1.8% of total AF cohort) and usual care (n = 2, 3.7% of total AF cohort) groups (Beyth 2000). Voller 2005 measured thromboembolic and bleeding events. Two severe haemorrhages occurred in one patient in the self‐monitoring group, and one thromboembolic event occurred in the usual care group.
Increased knowledge with regard to AF and anticoagulation therapy
Seven trials reported on patient knowledge (Clarkesmith 2013; Hendriks 2013; Man‐Son‐Hing 1999; McAlister 2005; Polek 2012; Thomson 2007; Vormfelde 2014). Five trials assessed knowledge before and after the intervention (Clarkesmith 2013; Hendriks 2013; Man‐Son‐Hing 1999; Thomson 2007; Vormfelde 2014), and two only tested knowledge after the intervention (McAlister 2005; Polek 2012). All trials used different measurement tools for assessing knowledge.
Education intervention
Four trials reported on patient knowledge (Clarkesmith 2013; Hendriks 2013; Polek 2012; Vormfelde 2014). All trials used different knowledge questionnaires and therefore data could not be pooled.
Two trials reported on mixed indication cohorts (Polek 2012; Vormfelde 2014). One trial provided unpublished AF data on knowledge outcomes (Polek 2012). They found slightly higher knowledge scores in the intervention group (mean 11.2, SD 1.6) than the usual care group (mean 10.1, SD 1.7) at the 12‐week follow‐up. However, the number of AF patients in this mixed cohort was too small to draw definitive conclusions. Vormfelde 2014 did not provide AF‐specific data on patient knowledge to include in this review.
Hendriks 2013 found a greater improvement in knowledge between baseline and 12‐month follow‐up in the intervention group (mean 7.21, SD 2.30 versus mean 8.23, SD 2.16, respectively) than the usual care group (mean 6.91, SD 2.54 versus mean 7.66, SD 2.09, respectively). Between‐group differences were significant at follow‐up (P = 0.028).
Clarkesmith 2013 found no significant differences in knowledge between baseline and six‐month follow‐up for the intervention or usual care groups (median (IQR) score at baseline 6 (5 to 7) in the intervention group versus 6 (4 to 7) in the usual care group; at six‐month follow‐up 7 (6 to 7) versus 7 (4 to 7), respectively).
Decision aid intervention
Two trials reported on patient knowledge (Man‐Son‐Hing 1999; Thomson 2007).
Thomson 2007 used an extension of the decision conflict scale (O'Connor 1995), and found that although knowledge scores after the intervention had improved slightly, by three‐month follow‐up they had returned to pre‐intervention levels. There was no significant difference between the decision aid and guidelines groups at any point.
Man‐Son‐Hing 1999 used a non‐validated scale and demonstrated that patients in the decision aid group had significantly greater knowledge of treatment‐related information than those in the usual care group (aspirin‐related knowledge MD 15.9, 95% CI 4.6 to 27.2, P < 0.001; warfarin‐related knowledge MD 14.9, 95% CI 4.6 to 25.2, P < 0.001).
Patient satisfaction
Four trials included patient satisfaction as a specified outcome (Gadisseur 2003; Hendriks 2013; Man‐Son‐Hing 1999; McAlister 2005). However, one trial did not report results for this outcome (McAlister 2005).
Education intervention
One education trial reported patient satisfaction; however, the authors did not provide AF‐specific data for this outcome (Gadisseur 2003).
Decision aid intervention
One trial using a decision aid intervention reported patient satisfaction as an outcome (Man‐Son‐Hing 1999). They found that the use of the decision aid did not significantly affect patients' satisfaction with their physician consultations.
QoL: psychological well‐being (anxiety and depression)
Three studies reported on QoL as an outcome (Clarkesmith 2013; Gadisseur 2003; Hendriks 2013), using three different measurement tools (Brazier 1992; Badia 2007; Sawicki 1999). One of the trials did not publish AF‐specific data for QoL (Gadisseur 2003). Two trials reported anxiety and depression outcomes (Clarkesmith 2013; Hendriks 2013), measured by the Hospital Anxiety and Depression Scale (Zigmond 1983). One study reported on anxiety alone (Thomson 2007), using a different measurement tool (Spielberger 1969).
Education intervention
Two trials reported on anxiety (Clarkesmith 2013; Hendriks 2013). Both trials used the Hospital Anxiety and Depression Scale to measure anxiety (Zigmond 1983).
Clarkesmith 2013 provided unpublished scores for anxiety. They found a greater increase in anxiety from baseline to 6 months in the intervention group (mean 6.14, SD 5.13) than the usual care group (mean 3.86, SD 6.36), but these differences were not significant (P = 0.14). There were no significant differences in anxiety between baseline and 12 months in either the intervention (mean 2.41, SD 5.28) or usual care (mean 2.71, SD 5.86) groups (P = 0.86). Between 6 and 12 months there was a slight, but non‐significant (P = 0.24), decrease in anxiety in both the intervention (mean ‐3.00, SD 5.33) and usual care (mean ‐0.35, SD 5.86) groups.
Hendriks 2013 reported no significant changes in anxiety from baseline (median 5, IQR 3 to 9) to 12 months (median 5, IQR 3 to 8) in the intervention group. In the usual care group there were no significant changes in scores from baseline (median 5, IQR 3 to 9) to 12 months (median 4, IQR 2 to 7). They found no significant differences in anxiety between groups, but a significant increase within both the intervention (median change ‐1, IQR ‐3 to 1) and usual care (median change ‐1, IQR ‐2 to 1) groups across time (P < 0.001).
The fixed‐effects pooled analysis of the two studies reporting anxiety using the Hospital Anxiety and Depression Scale (HADS) demonstrated that education had a small but positive impact on anxiety when compared to usual care (MD ‐0.62, 95% CI ‐1.21 to ‐0.04, P = 0.04; Clarkesmith 2013; Hendriks 2013; Analysis 2.1; Figure 5).
2.1. Analysis.
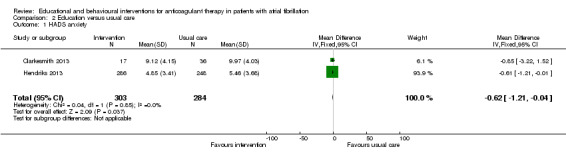
Comparison 2 Education versus usual care, Outcome 1 HADS anxiety.
5.

Forest plot of comparison: education versus usual care on HADS anxiety.
Clarkesmith 2013 provided unpublished data for depression. The found a similar increase in depression from baseline to 6 months for the intervention (mean 4.32, SD 3.20) and usual care (mean 4.00, SD 3.20) groups; these differences were not significant (P = 0.71). The difference in depression was less between baseline and 12 months in both the intervention (mean 2.88, SD 4.1) and usual care (mean 2.88, SD 5.15) groups (P = 1.00). Between 6 and 12 months there was a slight, but non‐significant (P = 0.55) decrease in depression in both the intervention (mean ‐1.73, SD 3.10) and usual care (mean ‐1.06, SD 2.66) groups.
Hendriks 2013 also provided unpublished data for depression and found no significant change in depression from baseline to 12 months in the intervention (median 4, IQR 1 to 7 versus median 3, IQR 1 to 6) and usual care groups (median 4, IQR 2 to 7 versus median 4, IQR 2 to 7).
The fixed‐effects pooled analysis of the two studies reporting depression using the HADS questionnaire demonstrated that education had a small but positive impact on depression when compared to usual care (MD ‐0.74, 95% CI ‐1.34 to ‐0.14, P = 0.02; Clarkesmith 2013; Hendriks 2013; Analysis 2.2; Figure 6).
2.2. Analysis.
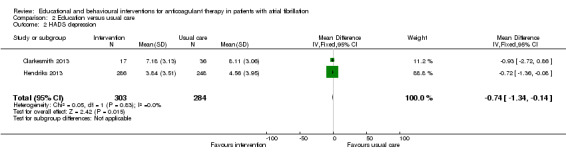
Comparison 2 Education versus usual care, Outcome 2 HADS depression.
6.
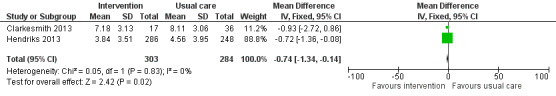
Forest plot of comparison: education versus usual care on HADS depression.
Two trials reported on QoL (Clarkesmith 2013; Hendriks 2013). Hendriks and colleagues used the SF‐36 questionnaire (Ware 1992), whilst the other used the AF‐QoL questionnaire (Badia 2007).
Hendriks 2013 found no significant differences between groups on any of the SF‐36 sub‐scales. There were significant changes within groups across time for vitality (intervention: P = 0.008; usual care: P < 0.00), physical role (usual care: P = 0.004), bodily pain (usual care: P = 0.002), emotional role (intervention: P = 0.004), and mental health (intervention: P = 0.001).
Clarkesmith 2013 found no significant differences between or within groups on any of the AF‐QoL subscales.
Decision aid intervention
Only one trial reported anxiety as an outcome (Thomson 2007). Anxiety fell significantly in both groups pre‐ to post‐clinic, (MD ‐4.57, 95% CI ‐6.30 to ‐2.84), but there was no evidence of a significant difference in anxiety between the two groups (F (1, 95) = 0.001; P = 0.98).
Changes in the patients’ illness beliefs and illness representations
One study reported on illness perceptions, and beliefs about medications (Clarkesmith 2013).
Education intervention
One study reported on illness perceptions (Clarkesmith 2013). They found no significant differences between the intervention and usual care groups on any of the sub‐scales.
One study reported on beliefs about medication (Clarkesmith 2013). The usual care group scored higher than the intervention group on specific concerns about medication and general harm scales at all time points. There was also a significant difference between groups in the perception of general harm (F (1, 28) = 4.4; P < 0.05) and an interaction between time and group for patients' concerns regarding medication (F (4, 27) = 2.9; P = 0.02). There was a significant interaction between group and time for patients' perceptions of the overuse of medication (F (4, 28) = 2.4, P = 0.04). The usual care group perceived medication as more overused than the intervention group. Scores on the Specific‐Necessity sub‐scale of the Beliefs about Medicines Questionnaire were similar for both groups, but there were no significant differences across time or between groups.
Economic costs of the intervention (cost‐effectiveness)
Two studies measured cost‐effectiveness of the intervention (Clarkesmith 2013; Hendriks 2013), but one study did not report on this outcome and did not provide data (Clarkesmith 2013).
Education intervention
Hendriks 2013 found the cost‐effectiveness acceptability curve for cost per quality‐adjusted life year demonstrated that if willingness to pay is set at €20 000, the possibility of nurse‐led care being cost‐effective is 99% compared with usual care. For cost per life‐year a probability of 92.5% is reached at a willingness to pay of €20 000.
Decision conflict
Three studies reported on decision conflict (Man‐Son‐Hing 1999; McAlister 2005; Thomson 2007). One of the studies did not have a usual care arm and therefore was not included in the pooled data analysis (Thomson 2007).
Decision aid intervention
Three studies (Man‐Son‐Hing 1999; McAlister 2005; Thomson 2007) reported decision conflict, and all used the decision conflict scale (O'Connor 1995).
Man‐Son‐Hing 1999 found that the usual care arm (mean 1.74, SD 0.5) scored slightly higher on decision conflict than the decision aid arm (mean 1.6, SD 0.4; MD ‐0.09, 95% CI ‐0.2 to 0.02).
McAlister 2005 found that the usual care arm (mean 1.7, SD 0.5) scored slightly higher on decision conflict than the decision aid arm (mean 1.6, SD 0.5; MD ‐0.10, 95% CI ‐0.19 to ‐0.01).
Although three studies reported decision conflict as an outcome, only two compared differences in the usual care and decision aid intervention groups (Man‐Son‐Hing 1999; McAlister 2005). The third compared the decision aid with a guideline comparison group and therefore was not included in the meta‐analysis (Thomson 2007). Data from the two trials were pooled and the random‐effects analysis favoured usual care in terms of reducing decision conflict (MD ‐0.10, 95% CI ‐0.17 to ‐0.02; Man‐Son‐Hing 1999; McAlister 2005; Analysis 3.1; Figure 7).
3.1. Analysis.
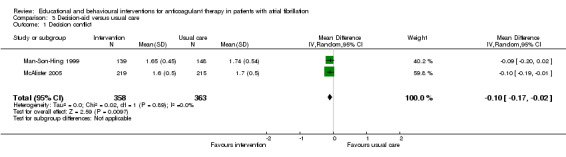
Comparison 3 Decision‐aid versus usual care, Outcome 1 Decision conflict.
7.
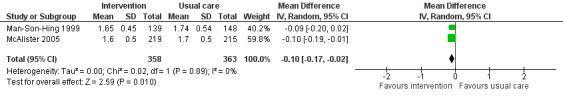
Forest plot of comparison: decision‐aid versus usual care on decision conflict.
Other outcomes
None of the studies reported on:
patient acceptability of anticoagulant therapy;
changes in perception towards AF and INR control;
self‐reported adherence to treatment
Discussion
Summary of main results
This review found eleven RCTs of behavioural and educational interventions for anticoagulant therapy in patients with AF (Beyth 2000; Christensen 2007; Clarkesmith 2013; Gadisseur 2003; Hendriks 2013; Man‐Son‐Hing 1999; McAlister 2005; Polek 2012; Thomson 2007; Voller 2005; Vormfelde 2014). Five trials compared education with usual care (Clarkesmith 2013; Gadisseur 2003; Hendriks 2013; Polek 2012; Vormfelde 2014), four compared self‐monitoring plus education with usual care (Beyth 2000; Christensen 2007; Gadisseur 2003; Voller 2005), and one trial also compared a self‐management group (consisting of self‐testing and self‐dosing; Gadisseur 2003). Three trials focused on the use of a decision support aid versus usual care (Man‐Son‐Hing 1999; McAlister 2005) or a comparison group (Thomson 2007). The analyses included a small number of trials with small sample sizes, thus more evidence is needed to draw definitive conclusions.
Education
We have summarised the findings from the education trials in Table 1. Two trials comparing education and usual care reported on anxiety and depression (Hendriks 2013; Clarkesmith 2013). Pooled data demonstrated that education had a small but positive impact on anxiety (MD ‐0.62, 95% CI ‐1.21 to ‐0.04, P = 0.04) and depression (MD ‐0.74, 95% CI ‐1.34 to ‐0.14, P = 0.02) when compared to usual care over 12 months (Analysis 2.1; Analysis 2.2; Figure 5; Figure 6). These findings are influenced by the weighting of the trial by Hendriks and colleagues, and the 12 month follow‐up data for both trials, as Clarkesmith 2013 found a decline in both anxiety and depression in both groups at the 6 month follow‐up. Evidently patients may feel more anxious and depressed in the initial months following diagnosis and treatment commencement.
Self‐monitoring plus education versus usual care
We have summarised the findings from the self‐monitoring trials in Table 1. Two self‐monitoring plus education trials reported TTR (Christensen 2007; Gadisseur 2003). Pooled data for the AF patients demonstrated that self‐monitoring plus education did not significantly improve TTR when compared to usual care (MD 6.3, 95% CI ‐5.63 to 18.25; Analysis 1.1; Figure 4). One previous Cochrane Review compared self‐management (monitoring and dosing) and self‐monitoring (monitoring only) interventions for mixed indication patients taking OAT (Garcia‐Alamino 2010). In their pooled data analysis, self‐management interventions showed significant reductions in both thromboembolic events (RR 0.50, 95% CI 0.36 to 0.69) and all‐cause mortality (RR 0.64, 95% CI 0.46 to 0.89), but self‐monitoring did not. The findings from the current review support those by Garcia‐Alamino 2010 that in an AF cohort, self‐monitoring is no more successful in increasing INR control than usual care.
Decision aids
We have summarised the findings from the decision aid trials in Table 1. Decision aid trials favoured usual care over the intervention in minimising decision conflict (MD ‐0.10, 95% Cl ‐0.17 to ‐0.02; Analysis 3.1; Figure 7). The use of a decision aid did not have a significant impact on AF patients' anxiety levels (Thomson 2007) or patient satisfaction (Man‐Son‐Hing 1999). This suggests that patients that took part in the decision aid trial were uncertain as to which treatment they were going to choose.
Overall completeness and applicability of evidence
Five of the included trials had mixed indication cohorts (Beyth 2000; Christensen 2007; Gadisseur 2003; Polek 2012; Vormfelde 2014 ), and 14 further trials were excluded as they did not provide AF‐specific data (Barcellona 2006; Chan 2006; Gardiner 2006; Jank 2009; Lakshmi 2013; Machtinger 2007; Menendez‐Jandula 2005; Moss 2014; Ryan 2009; Sawicki 2003; Siebenhofer 2007; Stone 1989; Watzke 2000; Yildirim 2015). Recruiting patients with mixed indications for a VKA can be problematic. Patients often have different INR ranges (for example with valve replacements) and each patient group is unique in their lifestyle and treatment recommendations. AF patients are often older (Kannel 1998), prescribed treatment on a long‐term basis (NICE 2006), and susceptible to inaccurate beliefs surrounding their illness (Steed 2010) due to their symptoms being irregular and often unrecognised (Fuster 2006). Thus, it is essential that interventions are disease specific, yet only three of the included trials specifically mentioned educating the patients about AF (Clarkesmith 2013; Hendriks 2013; McAlister 2005). Without discussing the illness itself, patients may not understand the need for treatment and the associated risks of their condition. Those interventions that are disease specific may prove more successful in targeting the particular concerns of the target population.
A further consideration is that the participants in these trial cohorts may exhibit a number of co‐morbidities which have not been accounted for; thus, they may have received similar behaviour change interventions in the past for conditions such as diabetes, potentially increasing their knowledge and awareness of risk. Therefore, the results of these trials may not be representative of the effect a behavioural or educational intervention may have on a sample of VKA‐naive AF‐only patients, and we cannot draw conclusions on the use of interventions for newly referred patients who are at greatest risk of complications. The majority of AF patients are elderly and are likely to have had some prior experience making treatment decisions for other conditions, although the VKA regimen is more complex than simply taking medication.
The primary outcome of this review was time spent in therapeutic range (TTR). Whilst pooled data from the self‐monitoring trials found no improvement in TTR when compared to usual care, some evidence from the educational intervention trials suggests providing face‐to‐face support and resources can significantly improve TTR when compared to usual care. Indeed, one decision aid trial, also providing education, found INR control deteriorated in the usual care arm over time, but improved in the intervention group (McAlister 2005). The clinical implications of improving INR control are important as the effectiveness of treatment, including warfarin, is often undermined by low levels of adherence, and maintaining the therapeutic range of 2.0 to 3.0 is imperative for stroke risk reduction (Kirchhof 2016; Morgan 2009; White 2007). More evidence is needed to identify the specific intervention components that help to improve INR control, so that these behaviour change techniques can be adopted in the future. It is important that researchers specify intervention components in detail, utilising the behaviour change taxonomy, to enable the progression of research in the field (Michie 2009; Michie 2011; Michie 2013).
Patients that self‐monitor are also educated to ensure they are able to perform the tests accurately and safely. It is therefore difficult to determine whether the education or the self‐monitoring is improving health outcomes. Further, patients selected for self‐monitoring tend to be younger, healthier, and better educated. Thus, they may not be representative of a general AF population (Garcia‐Alamino 2010). Similarly, decision aids provide patients with education regarding treatment choices; thus, it is difficult to determine whether increases in knowledge alone may have the same effect. The delivery of the intervention could also influence the outcomes. A group‐based intervention provides opportunity for social comparison, which influences patient attitudes towards their treatment and their perception of social norms.
Most trials recruited patients that had been previously taking OAT. Whilst some trials included VKA‐naive patients (Clarkesmith 2013; Hendriks 2013; Thomson 2007) or inpatients starting OAT (Beyth 2000; Polek 2012), only one of the trial cohorts were exclusively VKA‐naive (Clarkesmith 2013). Experience of taking a VKA could increase the risk of poor internal validity as patients may had been receiving OAT treatment long term, for up to 5.5 years prior to receiving the intervention (Christensen 2007), and may be influenced by their treatment history (for example side effects). Previous experience of the treatment may also influence adherence to recommendations, and a patient’s decision to start taking the treatment in the first place (Holbrook 2005; Lip 2011). Patients may develop specific beliefs about their medications that influence the decision‐making process, such as the inconvenience of regular blood tests, need for reductions in or abstinence from alcohol, and dietary restrictions (Dantas 2004; Lane 2006; Lip 2007; Lip 2011). Patients may also feel a level of protection from harm by taking a treatment (Lip 2011), thus increasing their likelihood of adopting one treatment over another. One of the trials in this review recruited patients that had previously taken part in Man‐Son‐Hing 1999. All of these patients had previously taken either an antiplatelet drug (60% of decision aid group versus 60% of the usual care group) or OAT (37% of the decision aid group versus 38% of the usual care group). The participants within this trial are unlikely to be representative of patients that are making treatment decisions for the first time. Firstly, they are ex‐trial patients and may be more likely to have had prior treatment‐related education and, secondly, they have had first‐hand experience of one or both treatments. One study found that more patients chose warfarin in a decision aid trial when the drug name was blinded than when it was unblinded (Holbrook 2007), suggesting that patients are influenced by prior knowledge, beliefs surrounding medications, and perhaps any adverse events they may have suffered from. In two studies included in this review (McAlister 2005; Thomson 2007), there was a difference at baseline between groups regarding the antithrombotic therapy that patients were receiving (those already receiving warfarin and those not) which could have affected patients' ability to make decisions about treatment, as one of the outcomes was decision conflict. Research suggests that patients are more likely to choose their current treatment over and above another; it has been suggested that this act prevents cognitive dissonance (that is the stress of choosing a preferred treatment over actual treatment choice; Fuller 2004; Holbrook 2007; Howitt 1999; Protheroe 2000).
Quality of the evidence
Two types of bias were most prevalent within the studies. Firstly, blinding of patients to the intervention received was not possible, nor was it possible to blind the intervention facilitator, inevitably raising the risk of bias. It is unclear whether the researchers may have biased patient outcomes by treating the patients in the intervention arm differently from those in the control group. Blinding the outcome assessor (data analyst or researchers) regarding to which intervention arm the patient was assigned was undertaken in six trials (Beyth 2000; Christensen 2007; Clarkesmith 2013; Gadisseur 2003; Hendriks 2013; McAlister 2005). Trial authors must be explicit when reporting their methods and procedures to ensure accurate assessment of blinding bias and enable comparison of trials.
Inclusion bias was also evident in many studies, where the trial participants may not have been representative of the eligible participants. The percentage of eligible patients randomised was as low as 15% in the exclusively AF populations (Clarkesmith 2013), and 18% in one of the mixed cohort trials (Gadisseur 2003). Perhaps the reluctance of individuals to participate may relate to the extensive training required, particularly for self‐monitoring trials, or questionnaire burden. Furthermore, many patients may refuse consent due to physical limitations, the time commitment associated with multiple training sessions or multiple follow‐ups, or psychological barriers to performing self‐monitoring. AF patients in particular are mostly elderly (Kannel 1998), and often highly symptomatic (Lip 2011), thus trial participation may be a burden. This could explain the small AF sample sizes in the included mixed OAT indication trials, as patients with other indications may be younger and with fewer co‐morbidities.
The quality of care in the control groups may vary substantially within and between countries, and the lack of a 'standard' of usual care is one of the key limitations of the studies in this field. There is no standard provision of anticoagulation monitoring, thus trials are often comparing an intervention with an unknown entity. The educational element of the intervention may be one of the key factors in improving TTR. However, trials varied in the intensity, duration, and number of education sessions, and the education facilitator; thus, we cannot draw conclusions about the influence of each of the educational components or the facilitator of these interventions on outcomes.
Five studies did not record patients' level of education (Christensen 2007; Gadisseur 2003; Polek 2012; Thomson 2007; Voller 2005), a factor which may impact on knowledge uptake and treatment control. Research suggests that patients with greater knowledge of their treatment spend more time in the therapeutic range (Tang 2003). Thus, the results of the trials that do not indicate education level may be influenced by individual differences in educational achievement between trial groups.
Whilst the educational components of the interventions did focus on important areas of risk (that is, side effects and medication recommendations), only three of the trials included education specific to the patient’s indication for treatment (Clarkesmith 2013; Hendriks 2013; McAlister 2005). Studies suggest that AF patients have limited knowledge of their condition (Coehlo‐Dantas 2004; Lane 2006; Lane 2015; Nadar 2003; Tang 2003), which may influence the perceptions they form about their illness and their treatment (Steed 2010). Thus, it is essential that patients form accurate concepts of their illness and make appropriate lifestyle changes.
Few studies provided AF‐specific data on psychological outcomes such as anxiety, depression, and QoL. Those that did found elevated levels of anxiety and depression for AF patients in both the intervention and usual care groups (Clarkesmith 2013; Hendriks 2013). Whilst levels decreased over time, there is no evidence that this change is specifically related to the intervention. The decision aid trial that reported anxiety as an outcome also found that anxiety fell significantly in both groups from pre‐ to post‐clinic (MD ‐4.57, 95% CI ‐6.30 to ‐2.84), but there was no evidence of a significant difference in anxiety between the two groups (F (1, 95) = 0.001; P = 0.98; Thomson 2007). While there is evidence to suggest that AF patients suffer from high levels of anxiety (Thrall 2004), none of the interventions in this review were designed with this in mind. Thus the trials exhibit small reductions in anxiety in the intervention groups versus usual care. As evidence suggests that AF patients often have inaccurate illness representations (Steed 2010), more trials of interventions that include targeted psychological components and outcome measures are needed.
Potential biases in the review process
Our search strategy included a comprehensive search of several electronic databases, meticulous handsearching of reference lists of included and excluded papers, recent conference proceedings, and personal communications with experts in this area. In addition, we wrote to all the authors of included studies requesting AF‐specific data and further demographic and clinical details on the included cohorts. Further, the titles and abstracts of all studies identified by the search strategy were reviewed independently by two review authors and disagreements were resolved by consensus. Data extraction of the included studies was also undertaken independently by two review authors. Therefore, we believe that the potential for bias in the review process was minimal and that it is unlikely that we have missed important studies. It is also important to note that the authors of Clarkesmith 2013 are also authors of this review; for further details see the Declarations of interest.
Authors' conclusions
Implications for practice.
Patients participating in both educational interventions and self‐monitoring interventions (with education) appear to spend more time within the therapeutic INR range, but pooled analyses of the AF data did not significantly favour self‐monitoring plus education over usual care. Evidence is limited, as there were few trials with small samples of AF patients. More trials are needed to examine the impact of intensive educational interventions on anticoagulation control in AF patients and the impact on TTR. Self‐monitoring may not be a feasible option for many patients, particularly as it requires additional training and is costly (Fitzmaurice 2000), and new anticoagulants are now available which do not require monitoring (Lip 2011; Shantsila 2010). Further, NOAC trials ‐ for example, where dabigatran was compared with warfarin ‐ examined the TTR of those patients taking warfarin and compared the event rates by quartile of centre TTR (cTTR; Wallentin 2010). Despite very good cTTR (> 72.6%), both doses of dabigatran were associated with fewer adverse events than warfarin. Despite the increasing use of NOACs there are still be some patients for whom the NOACs are not suitable (for example, those with severe renal impairment), where a VKA would be the only alternative OAT treatment. However, no study to date has compared self‐monitoring with a VKA to treatment with NOACs on adverse events (stroke and major bleeding) and therefore it is unclear whether there would be a benefit of self‐monitoring with a VKA (in the appropriate patient) over treatment with NOACs. Given that NOACs are increasingly used to treat AF patients, there is a need for interventions to provide effective illness‐specific educational tools, which incorporate relevant behaviour change techniques (Michie 2011; Michie 2013).
Implications for research.
This review highlights the need for AF‐specific trials of educational/behavioural interventions in larger cohorts and the development of psychological interventions for psychological morbidity in this population. Further, interventions should specifically state which behaviour change techniques they have used (and why) and their effect, in order to allow conclusions about which factors are likely to impact upon adherence. The number of VKA‐naive AF patients within the trials was limited, with most patients being VKA‐experienced. Trials also need to consider the use of disease‐specific measuring tools, which may provide a more accurate assessment of the impact of the intervention. In addition, such trials should account for the potential confounding effects of level of education and the quality of the care in the control group.
Ongoing trials
A trial focusing on self‐management is currently being undertaken (Siebenhofer 2012). This trial may provide additional evidence for later review updates. We will update this review once the results from this study are published. In addition, for the results to be generalisable to the AF population there is a need for population‐based studies that collect data on adverse event rates, time in therapeutic range, and cost effectiveness, and factors that impinge on successful educational and behavioural interventions. Future studies should set out to understand the mechanisms by which interventions are successful by exploring the psychological and practical implications for AF patients commencing OAT treatment.
What's new
| Date | Event | Description |
|---|---|---|
| 1 November 2016 | New search has been performed | This is an update of the original search and review published in 2013. This update has added an additional 10 articles based on 3 studies (Clarkesmith 2013; Hendriks 2013; Vormfelde 2014). The additional studies were all educational interventions. Data from two of these trials (Hendriks 2013; Clarkesmith 2013) on anxiety and depression were pooled (Analysis 2.1; Analysis 2.2). Data from the additional trials were also included (but not pooled) for time in therapeutic range, education, quality of life, beliefs about medication, and cost effectiveness. A summary of findings table has been added to the update (Table 1). |
| 1 November 2016 | New citation required and conclusions have changed | Three additional trials reported in this update compared with 2013 review. Additional data contributed to novel synthesis of analysis of effects on anxiety and depression. |
Acknowledgements
We would like to thank Dr Hendriks, Dr Friede, Dr Christensen, Dr Beyth, Dr Gadisseur, Dr Fradette, Dr Polek, and Dr Thomson for providing unpublished AF data, which we have included within the review. We would also like to thank all the authors whose articles were not included, but who provided unpublished manuscripts and data for review. In addition, the authors would like to thank Professor Lip and Mr Borg Xuereb for their contributions to the protocol used to conduct this review.
Appendices
Appendix 1. Search strategy
The Cochrane Library
#1 MeSH descriptor patient education as topic this term only #2 MeSH descriptor attitude to health explode all trees #3 MeSH descriptor patient participation this term only #4 MeSH descriptor behavior therapy this term only #5 MeSH descriptor cognitive therapy this term only #6 MeSH descriptor counseling explode all trees #7 MeSH descriptor motivation this term only #8 MeSH descriptor goals this term only #9 MeSH descriptor Biofeedback (Psychology) this term only #10 MeSH descriptor decision support techniques this term only #11 MeSH descriptor Communications Media explode all trees #12 education in All Text #13 (training in All Text or train in All Text) #14 (teaching in All Text or teach in All Text) #15 (behaviour* in All Text or behavior* in All Text) #16 "patient knowledge" in All Text #17 counsel* in All Text #18 (cognitiv* in All Text near/3 therapy in All Text) #19 (cognitiv* in All Text near/3 intervention* in All Text) #20 motivation* in All Text #21 contingency next management in All Text #22 (biofeedback in All Text or bio‐feedback in All Text) #23 (goal in All Text or goals in All Text) #24 (decision* in All Text near/3 aid* in All Text) #25 pamphlet* in All Text #26 booklet* in All Text #27 video* in All Text #28 decision next aid* in All Text #29 "patient participation" in All Text #30 (#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10) #31 (#11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20) #32 (#21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29) #33 (#30 or #31 or #32) #34 MeSH descriptor warfarin this term only #35 MeSH descriptor Coumarins explode all trees #36 MeSH descriptor anticoagulants this term only #37 MeSH descriptor vitamin k explode all trees with qualifiers: AI #38 oral next anticoagula* in All Text #39 Oral next anti‐coagula* in All Text #40 ("vitamin K" in All Text and (antagonist* in All Text or inhibitor* in All Text) ) #41 "antivitamin K" in All Text #42 "anti‐vitamin K" in All Text #43 warfarin in All Text #44 acenocoumarol in All Text #45 sintrom in All Text #46 sinthrome in All Text #47 jantoven in All Text #48 marevan in All Text #49 coumadin* in All Text #50 waran in All Text #51 phenprocoumon in All Text #52 nicoumalone in All Text #53 VKA in All Text #54 coumarin* in All Text #55 dicoumarol in All Text #56 dicumarol in All Text #57 (#34 or #35 or #36 or #37 or #38 or #39 or #40 or #41 or #42 or #43) #58 (#44 or #45 or #46 or #47 or #48 or #49 or #50 or #51 or #52 or #53 or #54 or #55 or #56) #59 (#57 or #58) #60 (#33 and #59)
MEDLINE on Ovid
1. Warfarin/ 2. acenocoumarol/ 3. Coumarins/ 4. Phenindione/ 5. Dicumarol/ 6. Anticoagulants/ 7. oral anticoagula$.tw. 8. exp Vitamin K/ai [Antagonists & Inhibitors] 9. warfarin.tw. 10. acenocoumarol.tw. 11. sintrom.tw. 12. sinthrome.tw. 13. jantoven.tw. 14. marevan.tw. 15. coumadin$.tw. 16. waran.tw. 17. Phenprocoumon/ 18. nicoumalone.tw. 19. (vitamin k adj3 antagonist$).tw. 20. vitamin k inhibitor$.tw. 21. oral anticoagula$.tw. 22. oral anti‐coagula$.tw. 23. vka.tw. 24. antivitamin k.tw. 25. anti‐vitamin k.tw. 26. or/1‐25 27. Patient Education as Topic/ 28. exp Attitude to Health/ 29. Patient Participation/ 30. ((educat$ or train$ or teach$) adj3 (program$ or intervention$)).tw. 31. (patient$ adj3 (train$ or teach$ or educat$ or inform$)).tw. 32. patient knowledge.tw. 33. Behavior Therapy/ 34. Cognitive Therapy/ 35. exp counseling/ 36. (behavi$ adj3 (therap$ or manage$ or modif$ or chang$ or intervention$)).tw. 37. (cogniti$ adj3 (therap$ or intervention$)).tw. 38. counsel$.tw. 39. Motivation/ 40. motivational interview$.tw. 41. contingency management.tw. 42. biofeedback.tw. 43. bio‐feedback.tw. 44. goals/ 45. (goal$ adj3 set$).tw. 46. decision support techniques/ 47. decision$ aid$.tw. 48. exp communications media/ 49. pamphlet$.tw. 50. booklet$.tw. 51. video$.tw. 52. or/27‐51 53. 26 and 52 54. randomized controlled trial.pt. 55. controlled clinical trial.pt. 56. randomized.ab. 57. placebo.ab. 58. clinical trials as topic.sh. 59. randomly.ab. 60. trial.ti. 61. 54 or 55 or 56 or 57 or 58 or 59 or 60 62. exp animals/ not humans.sh. 63. 61 not 62 64. 53 and 63
EMBASE Ovid
RCT filter as recommended in the Cochrane Handbook (Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 (updated September 2009). The Cochrane Collaboration, 2009. Available from www.cochrane‐handbook.org.) applied.
1. phenindione/ 2. antivitamin K/ 3. exp coumarin anticoagulant/ 4. anticoagulant agent/ 5. warfarin.tw. 6. acenocoumarol.tw. 7. sintrom.tw. 8. sinthrome.tw. 9. jantoven.tw. 10. marevan.tw. 11. coumadin$.tw. 12. waran.tw. 13. nicoumalone.tw. 14. (vitamin k adj3 antagonist$).tw. 15. vitamin k inhibitor$.tw. 16. oral anticoagula$.tw. 17. oral anti‐coagula$.tw. 18. vka*.tw. 19. antivitamin k.tw. 20. anti‐vitamin k.tw. 21. coumarin$.tw. 22. vitamin K group/po [Oral Drug Administration] 23. or/1‐22 24. patient education/ 25. attitude to health/ 26. patient participation/ 27. ((educat$ or train$ or teach$) adj3 (program$ or intervention$)).tw. 28. (patient$ adj3 (train$ or teach$ or educat$ or inform$)).tw. 29. patient knowledge.tw. 30. behavior therapy/ 31. cognitive therapy/ 32. exp counseling/ 33. (behavi$ adj3 (therap$ or manage$ or modif$ or chang$ or intervention$)).tw. 34. (cogniti$ adj3 (therap$ or intervention$)).tw. 35. counsel$.tw. 36. motivation/ 37. motivational interview$.tw. 38. contingency management.tw. 39. biofeedback.tw. 40. bio‐feedback.tw. 41. (goal$ adj3 set$).tw. 42. decision support system/ 43. decision$ aid$.tw. 44. (decision$ adj3 support).tw. 45. mass medium/ 46. pamphlet$.tw. 47. booklet$.tw. 48. video$.tw. 49. or/24‐48 50. random$.tw. 51. factorial$.tw. 52. crossover$.tw. 53. cross over$.tw. 54. cross‐over$.tw. 55. placebo$.tw. 56. (doubl$ adj blind$).tw. 57. (singl$ adj blind$).tw. 58. assign$.tw. 59. allocat$.tw. 60. volunteer$.tw. 61. crossover procedure/ 62. double blind procedure/ 63. randomized controlled trial/ 64. single blind procedure/ 65. or/50‐64 66. (animal/ or nonhuman/) not human/ 67. 65 not 66 68. 23 and 49 and 67
PsycINFO
1. anticoagulant drugs/ 2. warfarin.tw. 3. acenocoumarol.tw. 4. coumadin$.tw. 5. waran.tw. 6. nicoumalone.tw. 7. (vitamin k adj3 antagonist$).tw. 8. oral anticoagula$.tw. 9. vka*.tw. 10. coumarin$.tw. 11. or/1‐10 12. client education/ 13. client participation/ 14. behavior therapy/ 15. cognitive therapy/ 16. exp counseling/ 17. motivation/ 18. exp goals/ 19. biofeedback/ 20. decision making/ 21. exp communications media/ 22. ((educat$ or train$ or teach$) adj3 (program$ or intervention$)).tw. 23. (patient$ adj3 (train$ or teach$ or educat$ or inform$)).tw. 24. patient knowledge.tw. 25. health knowledge/ 26. (behavi$ adj3 (therap$ or manage$ or modif$ or chang$ or intervention$)).tw. 27. (cogniti$ adj3 (therap$ or intervention$)).tw. 28. health attitudes/ 29. counsel$.tw. 30. motivational interview$.tw. 31. contingency management.tw. 32. biofeedback.tw. 33. bio‐feedback.tw. 34. (goal$ adj3 set$).tw. 35. decision$ aid$.tw. 36. (decision$ adj3 support).tw. 37. pamphlet$.tw. 38. booklet$.tw. 39. video$.tw. 40. or/12‐39 41. 11 and 40 42. random$.tw. 43. factorial$.tw. 44. crossover$.tw. 45. cross‐over$.tw. 46. placebo$.tw. 47. (doubl$ adj blind$).tw. 48. (singl$ adj blind$).tw. 49. assign$.tw. 50. allocat$.tw. 51. volunteer$.tw. 52. control*.tw. 53. "2000".md. 54. or/42‐53 55. 41 and 54
CINAHL
as run on 9 August 2012:
S72 S52 and S71 S71 S53 or S54 or S55 or S56 or S57 or S58 or S59 or S60 or S61 or S62 or S63 or S64 or S65 or S66 or S67 or S68 or S69 Limiters ‐ Published Date from: 20100501‐20120931 S70 S53 or S54 or S55 or S56 or S57 or S58 or S59 or S60 or S61 or S62 or S63 or S64 or S65 or S66 or S67 or S68 or S69 S69 cross‐over* S68 crossover* S67 volunteer* S66 (MH "Crossover Design") S65 allocat* S64 control* S63 assign* S62 placebo* S61 (MH "Placebos") S60 random* S59 (doubl* N1 mask*) S58 (singl* N1 mask*) S57 (doubl* N1 blind*) S56 (singl* N1 blind) S55 (clinic* N1 trial?) S54 PT clinical trial S53 (MH "Clinical Trials") S52 S25 and S51 S51 S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 or S41 or S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 S50 video* S49 booklet* S48 pamphlet* S47 (MH "Communications Media") S46 (decision* aid*) S45 (MH "Decision Support Techniques") S44 (goal* N3 set*) S43 (MH "Goals and Objectives") S42 bio‐feedback S41 biofeedback S40 contingency management S39 motivational interview* S38 (MH "Motivation") S37 counsel* S36 (cogniti* N3 (therap* or intervention*)) S35 (behavi* N3 (therap* or manage* or modif* or chang* or intervention*)) S34 (MH "Counseling") S33 (MH "Cognitive Therapy") S32 (MH "Behavior Therapy") S31 patient knowledge S30 (patient* N3 (train* or teach* or educat* or inform*)) S29 ((educat* or train* or teach*) N3 (program* or intervention*)) S28 (MH "Consumer Participation") S27 (MH "Attitude to Health") S26 (MH "Patient Education") S25 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 S24 anti‐vitamin k S23 antivitamin k S22 vka* S21 oral anti‐coagula* S20 oral anticoagula* S19 vitamin k inhibitor* S18 (vitamin k N3 antagonist*) S17 nicoumalone S16 "Phenprocoumon" S15 waran S14 coumadin* S13 marevan S12 jantoven S11 sinthrome S10 sintrom S9 warfarin S8 (MH "Vitamin K") S7 oral anticoagula* S6 (MH "Anticoagulants") S5 "Dicumarol" S4 "Phenindione" S3 "Coumarins" S2 "acenocoumarol" S1 (MH "Warfarin")
as run on 21 June 2010:
S76 S57 and S75 S75 S58 or S59 or S60 or S61 or S62 or S63 or S64 or S65 or S66 or S67 or S68 or S69 or S70 or S71 or S72 or S73 or S74 S74 TX cross‐over* S73 TX crossover* S72 TX volunteer* S71 (MH "Crossover Design") S70 TX allocat* S69 TX control* S68 TX assign* S67 TX placebo* S66 (MH "Placebos") S65 TX random* S64 TX (doubl* N1 mask*) S63 TX (singl* N1 mask*) S62 TX (doubl* N1 blind*) S61 TX (singl* N1 blind*) S60 TX (clinic* N1 trial?) S59 PT clinical trial S58 (MH "Clinical Trials+") S57 S17 and S56 S56 S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 or S41 or S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 or S51 or S52 or S53 or S54 or S55 S55 (TI video*) or (AB video*) S54 (TI booklet*) or (AB booklet*) S53 (TI pamphlet*) or (AB pamphlet*) S52 (MH "Communications Media+") S51 (TI decision* N3 support) or (AB decision* N3 support) S50 (TI "decision* aid*") or (AB "decision* aid*") S49 (MH "Decision Support Techniques+") S48 (TI goal* N3 set*) or (AB goal* N3 set*) S47 (TI bio‐feedback) or (AB bio‐feedback) S46 (TI biofeedback) or (AB biofeedback) S45 (TI "contingency management") or (AB "contingency management") S44 (TI "motivational interview*") or (AB "motivational interview*") S43 (MH "Motivation+") S42 (TI counsel*) or (AB counsel*) S41 (TI cogniti* N3 intervention*) or (AB cogniti* N3 intervention*) S40 (TI cogniti* N3 therap*) or (AB cogniti* N3 therap*) S39 (TI behavi* N3 intervention*) or (AB behavi* N3 intervention*) S38 (TI behavi* N3 chang*) or (AB behavi* N3 chang*) S37 (TI behavi* N3 modif*) or (AB behavi* N3 modif*) S36 (TI behavi* N3 manage*) or (AB behavi* N3 manage*) S35 (TI behavi* N3 therap*) or (AB behavi* N3 therap*) S34 (MH "Counseling+") S33 (MH "Cognitive Therapy") S32 (MH "Behavior Therapy") S31 (TI "patient knowledge") or (AB "patient knowledge") S30 (TI patient* N3 inform*) or (AB patient* N3 inform*) S29 (TI patient* N3 educat*) or (AB patient* N3 educat*) S28 (TI patient* N3 teach*) or (AB patient* N3 teach*) S27 (TI patient* N3 train*) or (AB patient* N3 train*) S26 (TI teach* N3 intervention*) or (AB teach* N3 intervention*) S25 (TI teach* N3 program*) or (AB teach* N3 program*) S24 (TI train* N3 intervention*) or (AB train* N3 intervention*) S23 (TI train* N3 program*) or (AB train* N3 program*) S22 (TI educat* N3 intervention*) or (AB educat* N3 intervention*) S21 (TI educat* N3 program*) or (AB educat* N3 program*) S20 (MH "Consumer Participation") S19 (MH "Attitude to Health") S18 (MH "Patient Education") S17 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 S16 (TI dicumarol) or (AB dicumarol) S15 (TI dicoumarol) or (AB dicoumarol) S14 (TI coumarin*) or (AB coumarin*) S13 (TI VKA*) or (AB VKA*) S12 (TI phenprocoumon) or (AB phenprocoumon) S11 (TI coumadin*) or (AB coumadin*) S10 (TI sintrom) or (AB sintrom) S9 (TI acenocoumarol) or (AB acenocoumarol) S8 (TI warfarin) or (AB warfarin) S7 (TI "antivitamin K") or (AB "antivitamin K") S6 (TI "vitamin K" N2 inhibitor*) or (AB "vitamin K" N2 inhibitor*) S5 (TI "vitamin K" N2 antagonist*) or (AB "vitamin K" N2 antagonist*) S4 (TI oral N2 anti‐coagula*) or (AB oral N2 anti‐coagula*) S3 (TI oral N2 anticoagula*) or (AB oral N2 anticoagula*) S2 (MH "Warfarin") S1 (MH "Anticoagulants")
Data and analyses
Comparison 1. Self‐monitoring plus education versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Time in therapeutic INR range | 2 | 69 | Mean Difference (IV, Fixed, 95% CI) | 6.31 [‐5.63, 18.25] |
Comparison 2. Education versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HADS anxiety | 2 | 587 | Mean Difference (IV, Fixed, 95% CI) | ‐0.62 [‐1.21, ‐0.04] |
| 2 HADS depression | 2 | 587 | Mean Difference (IV, Fixed, 95% CI) | ‐0.74 [‐1.34, ‐0.14] |
Comparison 3. Decision‐aid versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Decision conflict | 2 | 721 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.17, ‐0.02] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beyth 2000.
| Methods | Randomised, controlled, parallel‐groups design | |
| Participants |
N randomised: 132 versus 162 usual care Diagnosis of patients: AF n = 54 (16.6%) for the intervention group and usual care groups. Other indications include VTE, cerebrovascular disease, heart valve prosthesis, peripheral vascular disease, myocardial infarction Demographics for total cohort: Age: 74.9±6.9 intervention versus 74.5±6.6 usual care % female: 55% intervention versus 59% usual care % white: 69% intervention versus 65% usual care Mean number of school years 12.1±4.4 intervention versus 12.1±4.1 usual care Demographics for AF patients: Age: 74.6±6.8 intervention versus 75.5± 6.2 usual care % female: 40% intervention versus 66% usual care % white: 77% intervention versus 77% usual care Mean number of school years 14.5±4.9 intervention versus 12.0±3.9 usual care Inclusion/exclusion criteria: Patients hospitalised and receiving 10,000 units or more of intravenous heparin, were 65 years or over, for whom warfarin treatment was planned for 10 days or more. Patients were excluded if they had been treated with warfarin at any time in the previous six months, were admitted from a nursing home, were enrolled in another clinical trial, were too ill to give consent, or did not speak English. |
|
| Interventions |
Type: Guideline‐based consultation, education and self‐monitoring Content: A consultation that assessed the patients' indication for therapy and potential risks for warfarin‐related bleeding (a method used by the researchers previously). This included specific recommendations about modifiable risk factors, such as use of non‐steroidal anti‐inflammatory drugs. The other component included patient education, coaching, and self monitoring. Patient education consisted of one to one teaching by a lay educator using a specifically formatted workbook for older adults to teach them about warfarin, indications for its use, drug and food interactions, and the signs and symptoms of bleeding. Coaching aimed to increase patients' participation in their care and improve information‐seeking skills. Self‐monitoring of prothrombin time (grounded in social learning theory). Patients were instructed to monitor 3 times in the first week and once weekly after that. Duration: 30 minutes to one hour (consultation) Facilitator: lay educator Setting: hospital |
|
| Outcomes | incidence of major bleeding excessive anticoagulation rates of VTE |
|
| Country | Cleveland, Ohio, USA | |
| Comparison | usual care group | |
| Length follow‐up | six months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were stratified according to their baseline risk for major bleeding by using the outpatient bleeding risk index. The index includes four independent risk factors for major bleeding: age 65 or older, history of gastrointestinal bleeding, history of stroke, and one or more of four specific comorbid conditions (myocardial infarction, hematocrit < 30%, creatinine concentration> 133µmol/L (1.5mg/dL), or diabetes mellitus). Patients with one or two risk factors were classified as intermediate risk, and those with three or more risk factors were classified as high risk; estimated frequencies of major bleeding in six months were 6% and 35% respectively. Details on how patients were assigned to treatment groups was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Of the 426 eligible patients identified, 294 (69.0%) received either usual care or the intervention. Details on how patients were assigned to treatment groups was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants cannot be blinded to which arm of the trial they receive. Neither can the personnel delivering the intervention be blinded. However, the educational intervention was delivered by a lay educator who was not involved in the treatment of the patients. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Trained abstractors who were not involved with the intervention component of the study collected data from the medical chart at the start of OAT, and by blinded interview at enrolment, at one, three, and six months after enrolment, and every six months thereafter. Whenever an event was reported, the clinical characteristics of the bleeding or thromboembolic episode were determined by review of the relevant medical record and abstracted, without identifying the patient, onto a standard form. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the 163 patients assigned to the intervention group, 81% (n = 132) participated in the intervention; 12 patients felt more comfortable with venepuncture, three stopped warfarin during hospitalisation, and one was discharged to a nursing home that precluded the use of a portable monitor. At six months, 21 patients (13%) in the intervention group and 26 (16%) of the usual care group had died. |
| Selective reporting (reporting bias) | Low risk | The method section describes the primary outcome as first major bleeding event during the six month intervention period. Secondary outcomes were death and recurrent VTE at six months; major bleeding after six months, and INR control during the first six months of therapy. The authors report data on all of these outcomes. |
| Other bias | Unclear risk | All patients had to be able to self‐monitor their INR and therefore the patients may not be representative of all patients requiring oral anticoagulation. However, all patients were aged 65 years or older, which is representative of an AF cohort. |
Christensen 2007.
| Methods | Open‐label randomised controlled trial, cross‐over (six months) | |
| Participants |
N randomised: 47 versus 45 (usual care/conventional management) AF: n = 11 versus n = 9 (usual care); other indications include mechanical heart valve, coagulopathies, VTE, synthetic vascular graft Demographics for total cohort: Age: 51.5±14.4 intervention versus 46.3±13.4 usual care % female: 23% intervention versus 44% usual care % white: not stated % education above primary level: not stated Demographics for AF cohort: Age: 59±18 intervention versus 51±12 usual care % female: 0% intervention versus 7% usual care % white: 100% in both groups % high school or greater: 4% intervention versus 3% usual care Inclusion/exclusion criteria: Patients were eligible if they were referred for patient self‐management by a general practitioner or hospital department, treated with oral anticoagulants > 8 months, 18 years or over, and willing to be randomised. Patients were excluded if they had previously used self‐management or lived abroad. |
|
| Interventions |
Type: teaching lesson (not explained in detail) and patient self‐management Content: The group used Coagucheck, which displays the INR value after the application of a drop of blood. Self‐management training included the patient practicing analysis of blood specimens. The patient gradually assumed management of OAT. After 27 weeks, patients took an exam; if passed, patient went on to self‐manage. After six months the conventional management group started the same training. Duration: not stated Facilitator: not stated Setting: hospital |
|
| Outcomes | major complications (bleeding and thromboembolism requiring intervention) death and/or discontinuation of the study primary endpoint: variance of INR in trial and control samples TTR |
|
| Country | Aarhus, Denmark | |
| Comparison | conventional management | |
| Length follow‐up | Observation period 1) 8 to 12 months before randomisation 2) primary observation period was 6 months of either patient self‐management or conventional management 3) patient self‐management training was 27 weeks |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomly assigned to patient self‐management using a computerised, prospective randomisation schedule. Randomisation in blocks with various sizes in numbers of two, four, and six was used. |
| Allocation concealment (selection bias) | Low risk | Of the 105 patients who were eligible to take part in the study, 100 patients were randomised (95%), therefore there is a low risk of selection bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the intervention, the participants receiving the intervention and the personnel delivering it cannot be blinded to which arm of the intervention they are in. It was unclear whether the personnel delivering the intervention were also involved in treating the usual care arm. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | External control blood samples were blinded. The results of the INR analysis were blinded for all except one secretary who would ensure the safety of the patient by contacting the managing physician if the INR value was below 1.5 or above 4.5. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | In the self‐management arm, three patients dropped out, two during the training period, and one died. In the usual care arm of the study, one patient was withdrawn by the physician and four dropped out during the self‐management training. Thus 92% of original cohort participants were included in the analysis. |
| Selective reporting (reporting bias) | Low risk | The endpoints were the variance (mean square of standard deviation) of the INR value, the median INR value (using a blinded control sample analysed monthly by a reference laboratory) and the coumarin dose. All outcomes were reported. |
| Other bias | High risk | All participants had to be eligible for self‐management of oral anticoagulation and therefore may not be representative of all patients requiring oral anticoagulation. |
Clarkesmith 2013.
| Methods | Randomised controlled trial | |
| Participants |
N randomised: 46 intervention versus 51 usual care Diagnosis of patients: All warfarin‐naive AF patients Demographics for total cohort: Age: 72.0±8.2 intervention versus 73.7±8.1 usual care % female: 32.6% intervention versus 37.3% usual care % white: 100% intervention versus 98% usual care % education above primary level: not stated Inclusion/exclusion criteria: Newly diagnosed AF patients referred for warfarin therapy, with ECG‐documented AF. Patients were excluded if they were aged < 18 years, had any contraindication to warfarin, had previously received warfarin, had valvular heart disease, were cognitively impaired, were unable to speak or read English, or had any disease likely to cause their death within 12 months. |
|
| Interventions |
Type: one‐off, group (one to six patients), theory‐driven educational intervention Content: The intervention involved one group session for one hour where patients were shown a DVD containing information about the need for OAT, risks and benefits, potential interactions with food, drugs and alcohol, and the importance of monitoring and control of their INR. Patients were encouraged to ask questions and complete a worksheet‐based exercise following each 10 minute DVD section. They were then given educational materials such as a booklet and a self‐monitoring INR and lifestyle diary to take home. Usual care involved patients receiving the standard 'yellow booklet' which contains generic information for all patients taking OAT and key safety information. Duration: one hour session Facilitator: health psychologist (could be delivered by trained lay educator) Setting: hospital outpatients clinic |
|
| Outcomes | TTR, knowledge, illness perceptions, beliefs about medication, anxiety and depression, quality of life, stroke, thromboembolic events, major and minor bleeding | |
| Country | United Kingdom | |
| Comparison | usual care | |
| Length follow‐up | 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer generated list stratified by (a) age (< 70 and > 70 years)/sex and (b) specialist AF clinic versus ‘general’ cardiology clinic, in blocks of four, randomised patients on an individual basis to receive either ‘usual care’ or the intensive educational intervention in addition to ‘usual care’. The randomisation schedule was designed by an independent trials unit. |
| Allocation concealment (selection bias) | High risk | Of the 646 patients who were eligible for the study, 97 patients participated (15%); 234 (36.2%) eligible patients declined to participate, primarily due to the questionnaire burden. Due to the number of patients declining to participate, there is an increased risk of selection bias. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention, the patients and staff delivering the intervention could not be blinded regarding to which arm of the trial participants were assigned. However, monitoring of the INR (for the primary outcome, TTR) was undertaken independent of the study, by the Anticoagulation Services at the hospitals (who were not aware of the patients' allocation to intervention or usual care). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The researcher analysing the data was blinded regarding to which arm of the intervention patients were randomised. A researcher not involved in the data analysis or intervention delivery matched patient ID numbers with randomisation codes and checked follow‐up questionnaires for completeness. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Ninety‐seven patients were randomised to the study; one discontinued from the intervention arm due to mental health problems and one discontinued from the usual care arm due to questionnaire burden. Results were analysed based on the intention‐to‐treat analysis for the primary outcome (TTR). The number of patients returning questionnaires assessing the secondary outcomes was 62.9% at six months and 54.6% at twelve months. |
| Selective reporting (reporting bias) | Low risk | All specified outcomes other than cost‐effectiveness were reported. |
| Other bias | Unclear risk | The intervention was delivered by a health psychologist and therefore the results may not be generalisable to different intervention facilitators. |
Gadisseur 2003.
| Methods | Multicentre randomised study, four arms | |
| Participants |
N randomised: A) weekly self‐measurement n = 52; B) weekly self measurement and self‐dosing n = 47; C) educated routine care n = 60; D) existing routine care (not trained) n = 161. This study used a Zelen design. Diagnosis of patients: AF patients in group A = 6 (11.6%); group B = 9 (19.2%), group C = 10 (16.6%), and group D = 43 (26.7%). Other indications included deep vein thrombosis, pulmonary embolism, artificial heart valves, and vascular prosthesis. Demographics for total cohort: Age: mean in group A = 54.8 (25 to 74), B = 53.9 (24 to 75), C = 56 (21 to 73), D = 62 (32 to 75) % female: A = 23%, B = 32%, C = 40%, D = 46% % white: not stated % education above primary level: not stated Demographics for the AF patients: not provided Inclusion/exclusion criteria: At least three months of OAT experience, need for long‐term OAT, and aged 18 to 75 years. Patients were excluded if they had antiphospholipid syndrome, a life threatening illness, life expectancy ≤ 1 year, diminished understanding, and physical limitations making successful participation impossible. |
|
| Interventions |
Type: self‐management and self‐dosing including education Content: They received information about the study, the blood coagulation system, OAT, and the effects of some substances (e.g. alcohol, certain medications, and foods rich in vitamin K) on OAT. They were also taught how to use the Coagucheck device, and instructed on oral self‐dosing of phenprocoumon and acenocoumarol. This also contained practical information about working with the Coagucheck, information about the coagulation system, and theoretical and practical self‐dosing training. They were also given written information on all the topics discussed. Group A: weekly INR self‐measurement, but dosing was performed by anticoagulation clinic physicians. Patients reported their INR values by telephone to the anticoagulation clinics. Dosing schedules were communicated via telephone. Group B: this group self‐managed their OAT, patients informed the anticoagulation clinic of their INR measurements, proposed dosing schedules, and reported any relevant information or complications. Patients were contacted via telephone to confirm whether they could adhere to their proposed dosing schedule or if they needed to adjust it. Group C: patients were trained for inclusion in groups A or B but stayed with the routine care system. Measurements of INR and dosing were done by anticoagulation clinic physicians, and the interval between INR measurements depended on the stability of the INR values. Group D: patients in this group were unaware of their participation in the study, representing the existing care system. Duration: three training sessions, groups of four to five, 90 to 120 minutes Facilitator: delivered by physician, paramedical person Setting: hospital |
|
| Outcomes | Quality of OAT determined by number of INR readings in target range; occurrence of thromboembolic and haemorrhagic complications; patients ability to independently perform anticoagulant self‐dosing | |
| Country | Netherlands | |
| Comparison | A) weekly self‐measurement B) weekly self‐measurement and self‐dosing C) educated routine care D) existing routine care (not trained) |
|
| Length follow‐up | mean follow‐up time 24.5 weeks | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The patients were selected by groups of 40 and randomised to four treatment groups (A, B, C, and D) following a 2‐step partial Zelen design. |
| Allocation concealment (selection bias) | High risk | Of the 881 eligible participants, 159 (18%) were randomised, therefore this study is at high risk of inclusion bias. 916 patients were randomly selected by a computer; 35 (3.9%) were excluded because of intellectual or physical limitations or because of a life expectancy of < 1 year. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Patients who were not randomised to group D were sent a letter with written information about the study (thus not blinded). Knowledge of the composition of the different groups was restricted to a few nurses who were also responsible for anonymously transferring the dosing schedules for group A and group B patients to standard forms and faxing them to the other participating anticoagulation clinics. The patients and staff could not be blinded regarding to which arm of the trial participants were assigned. The authors do not state whether those physicians delivering the intervention also treated the usual care arm. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The physicians evaluating and correcting the proposed dosing schedules for group A and B were unaware of the originators of these schedules. The INR values of the patients in routine care groups C and D were entered into the routine computerised system in such a way that the dosing physicians could not distinguish between these and the general patient population. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the original 180 patients randomised to the study, 116 (64%) completed the quality of life questionnaires at baseline and follow‐up; 21 patients were withdrawn or ineligible and the remainder were lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified endpoints were (1) quality of OAT represented by the number of INR readings within target range (TTR); (2) patients' ability to independently perform anticoagulant self‐dosing, by number of dosage corrections made. All specified outcomes were reported. |
| Other bias | High risk | All participants had to be eligible for self‐management of oral anticoagulation and therefore may not be representative of all patients requiring oral anticoagulation. |
Hendriks 2013.
| Methods | Randomised controlled trial | |
| Participants |
N randomised: 356 intervention versus 356 usual care Diagnosis of patients: all AF patients Demographics for total cohort: Age: 66±13 intervention versus 67±12 usual care % female: 44.7% intervention versus 37.9% usual care % white: not stated % education above primary level: not stated Inclusion/exclusion criteria: All patients of at least 18 years of age who were referred for AF (documented on ECG) by GPs or non‐cardiology specialists to their outpatient department were included. Exclusion criteria were any comorbidity which is unsatisfactorily treated, unstable heart failure defined as New York Heart Association IV or necessitating hospital admission < 3 months before inclusion, untreated hyperthyroidism, current or foreseen pacemaker, internal cardioverter defibrillator or cardio resynchronisation therapy, or cardiac surgery < 3 months before inclusion. |
|
| Interventions |
Type: enhanced educational intervention Content: The intervention consisted of nurse‐led outpatient care steered by decision support software based on the guidelines and supervised by a cardiologist. During the visits, the nurse specialist informed patients about the pathophysiology of AF, its symptoms and possible complications, the results of the diagnostic tests, and treatment options. The dedicated software CardioConsult AF was used to determine the individual patient profile based on symptoms, type of AF, and stroke risk, and it proposed the most appropriate management. Follow‐up visits were scheduled at 3, 6, and 12 months, and every 6 months thereafter. Patients could contact the nurse in person or by telephone between planned visited as needed. Patients in the control group received usual care by a cardiologist in the outpatient clinic during visits. Duration: 30 minutes per visit Facilitator: nurse specialist Setting: Maastricht University medical centre |
|
| Outcomes |
Primary endpoint: composite endpoint of cardiovascular hospitalisation or cardiovascular death Secondary endpoints: guideline adherence, patient knowledge on AF, quality of life, patient satisfaction, cost‐effectiveness |
|
| Country | The Netherlands | |
| Comparison | usual care (outpatient visits with cardiologist) | |
| Length follow‐up | at least 12 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomly assigned to nurse‐led care or usual care by a computer generated one to one randomisation. |
| Allocation concealment (selection bias) | Low risk | Out of 760 eligible patients, 712 patients participated (94%). Therefore there is a low risk of inclusion bias. The groups were well matched without significant differences in baseline characteristics. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The nurse, patients, and the supervising cardiologist were not blinded due to the nature of the intervention. The authors do not state whether those physicians involved in delivering the intervention also treated the usual care arm. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | There was an independent panel of specialists to assess the primary endpoint. This committee was blinded to assignment and interim study outcomes. They reviewed each case independently and held a meeting at the end. If the decision was non‐unanimous, the endpoint was established by the study chair. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The final sample included all of the original patients that were randomised to the study. None of the patients were lost to follow‐up. Patients (n = 178) who did not complete the SF‐36 at both time‐points were excluded. There is a suggestion that more usual care arm patients did not complete the SF‐36 questionnaires. |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported with the exception of patient satisfaction. |
| Other bias | Unclear risk | This was a nurse‐led comprehensive intervention and therefore the results may not be applicable outside this setting. |
Man‐Son‐Hing 1999.
| Methods | Randomized controlled trial 20 possible SPAF trial centres invited, 14 participated |
|
| Participants |
N randomised: n = 139 intervention (10 lost to follow‐up) versus n = 148 control (14 lost to follow‐up) Diagnosis of patients: all AF patients Demographics of cohort: Age: intervention mean = 65 versus control mean = 65 % female: intervention 24% versus control 24% % white: not stated % education above primary level: intervention 90% high school education or greater versus control 91% high school education or greater Inclusion/exclusion criteria: All participants were in the SPAF III aspirin cohort study and were eligible unless they had high risk criteria or had a major haemorrhage during the study. |
|
| Interventions |
Type: decision aid Content: 29 page booklet, a personal worksheet (complete pre‐intervention), and a 20‐minute audiotape that guided the patient through the booklet and worksheet. The intervention included a description of the consequences of minor/major stroke and major haemorrhage, the blood monitoring required for warfarin and the 2‐year probability of stroke and major haemorrhage for patients taking aspirin/warfarin using pictograms. Duration: not stated Facilitator: physician/audio tape Setting: hospital |
|
| Outcomes | One to four days after meeting with their physicians patients completed questionnaires: Patient choices (strength of their decisional input, five‐point Likert scale, unvalidated) Knowledge (23 questions about AF, stroke and treatment, unvalidated) Expectations (four questions regarding patient expectations of stroke/haemorrhage, unvalidated) Decisional conflict (decisional conflict scale; O'Connor 1995) Satisfaction (six questions, five‐point Likert scale, unvalidated) Six‐month adherence to their treatment decisions (self‐report brief questionnaire, administered via telephone, unvalidated) |
|
| Country | US | |
| Comparison | Control group, usual care, i.e. no change was made to the usual manner in which each centre communicated the results of the SPAF III study or the way in which the decision regarding type of antithrombotic was made. | |
| Length follow‐up | six‐month follow‐up | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated scheme, administered from a central location to block sequence from previewing. Stratified by centre and the presence of a history of hypertension. |
| Allocation concealment (selection bias) | High risk | Of the 657 patients who were eligible for the trial, 287 participated (43%), giving a substantial risk of inclusion bias; 24 participants were lost to follow‐up. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The authors do not state whether the researcher or personnel were blinded regarding to which arm the participants were randomised. However, we can assume that participants and physicians were not blinded to treatment allocation due to the nature of the intervention. The authors do not state whether those physicians delivering the intervention also treated the usual care arm. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The authors do not state whether the personnel scoring and analysing the questionnaires were blinded to the treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | From 139 patients participating, 87 (63%) worksheets were completed. However, all of the 139 patients randomised to the decision aid were included in the study analysis of decision conflict. |
| Selective reporting (reporting bias) | Low risk | Outcome measures were patients' ability to make choices regarding antithrombotic therapy, six‐month adherence to decision, knowledge, decision conflict and satisfaction. There was no protocol paper for this study. Only one of the pre‐specified outcome variables in the method section was not reported (patient satisfaction). |
| Other bias | High risk | This was a sub‐set of the SPAF III trial and all patients were receiving aspirin. The SPAF III study excluded those who had 'high‐risk criteria' (without explanation of this) and those who had major haemorrhage, both of which are likely to affect opinion about oral anticoagulation and the ability to make decisions about treatment. Those who participated had a greater proportion with better education (high school or greater) compared to those who declined participation and this could have influenced the ability to make a decision. There was the possibility of contamination between the intervention and comparator arms as physicians could have provided similar information which was contained in the educational booklet during routine clinic visits to patients in the usual care group. |
McAlister 2005.
| Methods | Prospective, multicentre, two‐arm, cluster randomised trial | |
| Participants |
N randomised: intervention n = 219 versus control n = 215 Fifty GP practices were randomised to the decision aid group and 52 were randomised to usual care. Diagnosis of patients: All NVAF (also broken down by type of AF; see paper) Demographics of cohort: Age: intervention 73±9 versus control 71±10 % female: intervention 43% versus control 34% % white: not stated % completed high school: intervention n = 84 (38%) versus control n = 72 (33%) Inclusion/exclusion criteria: Community‐dwelling patients over the age of 18 were included in this study if they had a diagnosis of NVAF (intermittent or chronic) confirmed by ECG, or prescription for digoxin. They were excluded if they 1) had valvular AF; 2) were taking warfarin for another condition; 3) were scheduled for cardioversion; 3) had a contraindication for warfarin or aspirin; 4) had cognitive impairment; 5) had a life expectancy less than 12 months; 6) could not understand/converse in English. |
|
| Interventions |
Type: general education session plus patient decision aid and physician's manual Content: 30‐page decision aid booklet, personal worksheet, 50‐minute audiotape to guide participants through the booklet and worksheet, and a seven‐page physician's manual summarising the evidence discussed in the patient booklet with a focus on the 2001 ACCP risk stratification schema and recommendations for antithrombotic therapy. Four versions of the decision aid were available depending on patients' baseline stroke risk. All four versions provide the same background information about AF; the potential consequences of stroke and major haemorrhage; relative efficacy/bleeding risks with warfarin and aspirin therapy. Key points are further elaborated upon in the audio‐tape. The one‐page worksheet is to be completed by the patient after reviewing the booklet to clarify their personal values regarding desired outcomes, the therapy they are inclined to take, their preferred role in the decision process, and any questions they have for their physician. Duration: not stated Facilitator: physician Setting: GP practices |
|
| Outcomes | Use of appropriate antithrombotic therapy at three months, as defined by the 2001 ACCP recommendations. Secondary outcomes include (1) appropriate antithrombotic therapy at 6 months and 12 months, (2) patient’s readiness to make a choice at baseline (previously validated questionnaire), (3) patient knowledge after the intervention (multiple‐choice responses used in a previous trial), (4) decisional conflict (decision conflict scale; O'Connor 1995), (5) acceptability of decision aid (9 questions with variable responses on a five‐point Likert scale), (6) satisfaction (five‐point Likert scale), (7) adherence with therapy (validated Morisky scale with modified five‐point Likert scale response). | |
| Country | Canada | |
| Comparison | usual care | |
| Length follow‐up | one‐year follow‐up | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation to intervention or usual care was carried out according to a computer‐generated sequence using clustered block randomisation (block size of four) with allocation concealment. |
| Allocation concealment (selection bias) | High risk | Of the 904 patients who were eligible for the study, 446 were randomised (49%). Due to the number of patients declining screening, there is an increased risk of inclusion bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The authors do not state whether the researchers or personnel were blinded regarding to which arm the participants were randomised. However, we can assume that participants and physicians were not blinded to treatment allocation due to the nature of the intervention. Physicians who delivered the intervention did not treat the usual care arm. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The outcome assessment was carried out by an independent statistician who was blinded to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 446 eligible participants who were randomised, 434 (97%) were included in the three‐month follow‐up evaluation. |
| Selective reporting (reporting bias) | Low risk | The primary endpoint was use of appropriate antithrombotic therapy; other endpoints include TTR, patient's readiness to make choices, knowledge, decision conflict, acceptability of decision aid, satisfaction, and adherence. Adherence and satisfaction scales data are not explained in detail. However, authors report the majority of data from the protocol paper including key primary and secondary outcomes. |
| Other bias | High risk | There was an imbalance at baseline in antithrombotic therapy between the intervention and usual care groups which could have influenced the patients' ability to make decisions regarding antithrombotic therapy thereby affecting the outcomes. In addition, a greater proportion of patients were unwilling to consider changing treatment at baseline in the decision aid group compared to usual care (41% versus 36%) and more patients in the decision aid group felt that their physician should make the decision regarding antithrombotic therapy than those in the usual care (52% versus 40%); both of which could have affected patients' decisional conflict. The study was underpowered as the protocol paper suggested that 814 participants were required (N = 434 included). |
Polek 2012.
| Methods | Nested randomised controlled trial | |
| Participants |
N randomised: intervention = 25 versus usual care = 28 Diagnosis of patients: mixed indication cohort Demographics of the cohort: Age: mean 63.71 (SD 16.04) % female: not stated % white: not stated % education above primary level: not stated Demographics of the AF patients: N = 14 Treatment group n = 5; usual care n = 9 Age: mean intervention = 73.6 (SD 11.1) versus mean usual care = 76 (SD 13.4) % female: intervention = 4/5 (80%) versus usual care = 3/9 (33%) % white: intervention = 3/5 (60%) versus usual care = 5/9 (55%) % educated above primary school level: not available Inclusion criteria: patients discharged to home on OAT, alert and orientated, able to speak and understand English, and accessible via telephone Exclusion criteria: patients discharged to a nursing home or rehabilitation facility, history of psychotic disorder or cognitive impairment |
|
| Interventions |
Type: enhanced educational intervention Content: face‐to‐face warfarin education, printed materials, instruction, medical alert bracelet. The intervention was based on Banduras social cognitive model and aimed to improve self‐efficacy. Four post‐discharge phone calls assessing knowledge post‐intervention and correcting incorrect answers. Duration: not stated Facilitator: pharmacist Setting: hospital |
|
| Outcomes | warfarin knowledge self‐efficacy |
|
| Country | USA | |
| Comparison | usual care | |
| Length follow‐up | 12 weeks | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Patients were randomly assigned to the intervention or usual care group after receiving patient education from the pharmacist. Authors do not describe the sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | Of 66 patients who were screened and offered participation in the study, there were 53 included in the original randomised sample (80% of those screened), with a low risk of inclusion bias. Only 42/53 (79%) received the intervention or usual care; 42/66 of eligible patients were therefore included (64%). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The authors do not state whether the researchers or personnel were blinded regarding to which arm the participants were randomised. However, we can assume that participants and physicians were not blinded to treatment allocation due to the nature of the intervention. The authors do not state whether the personnel delivering the intervention also treated the usual care arm. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Authors do not state whether the person scoring the questionnaires was blinded to the treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The final sample included 42 (79%) of the original 53 patients that were randomised to the study. Attrition was 36% and therefore designated as high risk of bias. |
| Selective reporting (reporting bias) | Low risk | The authors describe two outcomes in their method section: (1) warfarin knowledge and (2) self‐efficacy. The authors report on both outcomes in their results section. There was no published protocol paper, thus we cannot determine whether those outcomes reported reflect those that were included in the study. |
| Other bias | High risk | Very small sample size (N = 42 in total) |
Thomson 2007.
| Methods | Three/two‐armed open, randomised controlled efficacy trial | |
| Participants |
N randomised: 69 decision aid versus 67 guidelines Diagnosis of patients: all AF patients Demographics of cohort: Age: 73.1±6.7 decision aid versus 73.7±6.2 guidelines % female: 43.4 decision aid versus 44.6 guidelines % white: not stated % education above primary level: not stated Inclusion/exclusion criteria: Patients were recruited if they were already taking warfarin or if they were considering taking warfarin for the first time. Patients were eligible if they were aged 60 or over and had either chronic NVAF or PAF. Patients were excluded if they had acute onset AF requiring cardioversion, previous stroke or TIA, contraindications for warfarin, or cognitive impairment, or were taking warfarin for other indications, non‐English speaking, or at risk of cerebral bleed. |
|
| Interventions |
Type: decision aid Content: included individual risk and benefit presentation and a section to support shared decision making Two different decision aids: 1. Used explicit value elicitation employing the standard gamble method and Markov decision analysis “explicit tool” 2. Included only risk/benefit presentation “implicit tool” (computerised decision aid). The doctor was trained to use the computerised decision aid. Early in the trial, the observation study (running alongside the trial) found the first decision aid to be difficult, so this arm was discontinued (gamble method) and the paper describes the results of the second arm versus evidence‐based paper guidelines. The intervention arm included benefits and harms of warfarin treatment, advantages and disadvantages, and personalised risk assessment (using the Framingham equation). The presentation used graphical and numerical forms of presentation. Duration: mean 31 minutes long (range 16 to 41) Facilitator: computerised tool Setting: research clinic |
|
| Outcomes | decision conflict knowledge state trait anxiety inventory Degner’s decision making preference scale |
|
| Country | Newcastle, UK | |
| Comparison | guideline‐based consultation | |
| Length follow‐up | three months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised to either computerised decision aid (intervention) or evidence‐based paper guidelines (control), using electronically‐generated random permuted blocks via a web‐based randomisation service provided by the Centre for Health Services Research. |
| Allocation concealment (selection bias) | High risk | Of 483 patients who were eligible for the study, 145 patients were eventually randomised (30%). Thus there is a substantial risk of inclusion bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The authors do not state whether the researchers or personnel were blinded regarding to which arm the participants were randomised. However, we can assume that participants and physicians were not blinded to treatment allocation due to the nature of the intervention. The authors do not state whether those physicians delivering the intervention also treated the usual care arm. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The authors do not state whether the person scoring the questionnaires was blinded to the treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Of the 69 patients allocated to the decision aid tool, 16 (23%) did not receive the intervention. Of the 67 patients allocated to the guidelines group, 11 (16%) did not receive the intervention. In total, 19% of patients randomised did not receive the intervention. More patients randomised to the decision aid tool did not receive the intervention although the overall attrition rate was < 20%. Reasons included withdrawal of consent, death, illness, surgery, alcoholism, and inability to use the tool. |
| Selective reporting (reporting bias) | Unclear risk | The primary outcome was decision conflict. Secondary outcomes were state and trait anxiety, knowledge, and decision making preference. Decision conflict outcomes were reported, but there was no tabulated report of the scale breakdown. All of the outcomes were reported, but mean scores and numbers of patients per group were not. |
| Other bias | Unclear risk | There was a difference at baseline between the groups in the number of patients not already receiving warfarin which may have influenced patients' ability/willingness to make treatment decisions which may have affected the primary outcome (decisional conflict). |
Voller 2005.
| Methods | Prospective multicentre randomised controlled trial | |
| Participants |
N randomised: 101 self‐management versus 101 family doctor group Diagnosis of patients: all NVAF patients Demographics of cohort: Age: 64.6±9.6 self‐management versus 64.1±8.9 family doctor % female: 28.6 self‐management versus 38.6 family doctor % white: not stated % education above primary level: not stated Inclusion/exclusion criteria: All patients for whom long‐term anticoagulation was indicated because of permanent non‐valvular AF were included into the investigation. Exclusion criteria were lack of suitability for INR self‐management, participation in another study, alcohol or other addiction, a mechanical heart valve replacement or anticoagulant treatment already administered for another indication, and diseases such as AIDS or carcinomas. Patients with visual impairment were also excluded. |
|
| Interventions |
Content: educational session following the standards of the Working Group for the Study of Patient Self‐Management of Oral Anticoagulation, based on the intervention session developed by Sawicki and colleagues. The programme consisted of three consecutive weekly teaching sessions for groups of three to six patients. Topics included anticoagulation in general, INR self‐monitoring, preventing bleeding, effects of diet and other medication, reducing or increasing dose, problems that may be encountered with operations, illness, exercise, pregnancy, etc. Duration: 60 to 90 minutes (based on Sawicki's description) Facilitator: not stated Setting: not stated |
|
| Outcomes |
Primary endpoint: number of thromboembolic or hemorrhagic complications requiring treatment Secondary endpoints: the degree of handicap after stroke, the degree of severity of haemorrhage, the proportion as well as cumulative time of the INR values in the individual target range, INR variance, time course of complications, and the cost efficiency of self‐measurement compared to conventional procedures |
|
| Country | Germany | |
| Comparison | family doctor group | |
| Length follow‐up | Overall observation period (retrospective): self‐management 37.34±5.93 years family doctor 40.25±6.07 years |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation list developed before beginning of the study with SAS software PROC PLAN procedure |
| Allocation concealment (selection bias) | Unclear risk | Authors do not report how many participants were eligible for the study |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The authors do not state whether the researcher or personnel were blinded regarding to which arm the participants were randomised. However, we can assume that participants and physicians were not blinded to treatment allocation due to the nature of the intervention. The authors do not state whether those physicians delivering the intervention also treated the usual care arm. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The authors do not state whether the person scoring the questionnaires was blinded to the treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All of the 202 patients who were randomised to the study were included in the final analysis. |
| Selective reporting (reporting bias) | High risk | The study was discontinued because the number of cases was too small, and the group comparison was confined to the evaluation of the number of INR values measured and the total period for which the patients remained outside, above, and below the target range. |
| Other bias | High risk | All patients had to be eligible for self‐management of oral anticoagulation and therefore may not be representative of all AF patients requiring oral anticoagulation. The mean age was 64 years which is fairly young for an AF population. In addition, there were only three primary outcome events (two haemorrhages in the self‐management group and one thromboembolic event in the family doctor group). |
Vormfelde 2014.
| Methods | Cluster randomised controlled trial of 22 GP practices | |
| Participants |
N randomised: intervention = 185 patients versus comparator = 134 patients Diagnosis of patients: AF, thrombosis, pulmonary embolism, heart valve replacement, unknown Demographics for total cohort: Age: 73±10 intervention versus 72±10 usual care % female: 56% intervention versus 58% usual care % white: not stated % education above primary level: not stated Demographics of the AF patients: N = 14 Treatment group n = 141 versus usual care n = 81 Age: intervention mean 74.5 (SD 8.0) versus usual care mean 72.9 (SD 9.4) Female: intervention = 72 (45.6%) versus usual care = 38 (46.9%) ≥ 10 years education: intervention 32 (20.3%) versus usual care 28 (34.6%) Inclusion/exclusion criteria: All patients taking OAT (with a range of indications) with ability to consent to participation and adequate German language skills were included. Exclusion criteria included residence in a nursing home and patients in cross coverage. |
|
| Interventions |
Type: parallell randomised controlled trial Content: Practice nurses delivered the educational intervention session consisting of a 20‐minute video presentation, an eight‐page brochure, and a corresponding questionnaire. The information was on 13 topics pertaining to oral anticoagulation with phenprocoumon according to the internationally recognised model and recommendations. Usual care included patients who were only given a brochure. Duration: one hour Facilitator: practice nurse Setting: general practice |
|
| Outcomes | Primary outcome: number of correctly answered questions from the 13‐item OAT questionnaire Secondary outcomes: time spent in therapeutic range, subjective feelings of safety and complications related to OAT |
|
| Country | Germany | |
| Comparison | patients who were only given the brochure | |
| Length follow‐up | six months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The first 22 GPs that agreed to participate were included. The Institute for Medical Statistics randomised these 22 practices into two equal‐sized trial groups (intervention versus control) by random permutation. |
| Allocation concealment (selection bias) | High risk | Of the 85 general medical practices contacted, 22 general medical practices agreed to participate (26%). There is risk of bias from participation of more highly motivated and better educated individuals than average, who knew they were being tested. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The authors do not state whether the researchers or personnel were blinded regarding to which arm the participants were randomised. However, we can assume that participants and practice nurses were not blinded to treatment allocation due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The authors do not state whether their data analysis was blinded regarding to which group the patients were randomised. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the 979 anticoagulated patients who were identified in the 22 practices, 319 completed the trial (33%). During follow‐up, for the intervention arm (n = 194), nine (5%) did not complete the trial as eight moved away and one died. For the control arm (n = 151), 17 (11%) patients did not complete the trial as six moved away, three died, and eight chose to drop out. INR analysis was possible in 157/194 (81%) patients in the intervention group and 91/151 (60%) in the control arm; overall attrition was greater than 20% and more patients in the control group did not have INR data at follow‐up available for the analyses. |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | High risk | Improvement in knowledge was dependent on the practice where the patient education was delivered which was probably due to differences in the discussion with the nurse after the video presentation. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Al‐Meshal 2013 | No breakdown of patient group |
| Armstrong 2011 | Not an RCT |
| Bajorek 2005 | Not an RCT, no control group |
| Baker 1991 | Wrong patient group, no AF |
| Barcellona 2006 | No unpublished AF data provided on request |
| Batty 2001 | Does not measure any of the required outcomes |
| Bereznicki 2013 | No separate control group, patients acted as their own historical control |
| Blaise 2009 | Not an RCT, retrospective study |
| Bloomfield 2011 | Meta‐analysis, not an RCT |
| Bump 1977 | No AF patients |
| Burns 2009 | Not an RCT, review paper |
| Castelino 2010 | Not an RCT |
| Chan 2006 | No unpublished AF data provided on request |
| Christensen 2011 | Limited education, specific to self‐testing |
| Claes 2005 | No AF patients |
| Claes 2006 | No AF patients |
| Corbella 2009 | Not an RCT |
| Cordasco 2009 | No AF patients |
| Cromheecke 2000 | No AF patients |
| Cromheecke 2001 | No AF patients |
| Davis 2005 | Not an RCT, survey |
| Dolor 2010 | No education other than instruction to self‐test |
| Duran‐Parrondo 2011 | Trial is not randomised |
| Field 2010 | Training is for staff not patients |
| Fitzmaurice 1996 | Not a patient intervention |
| Fitzmaurice 2000 | Did not include an educational or behavioural intervention |
| Fitzmaurice 2005 | No AF patients |
| Fraenkel 2011 | Not compared to usual care, not an RCT |
| Gardiner 2006 | No unpublished AF data provided on request |
| Gouin‐Thibault 2010 | Intervention for staff not patients |
| Grunau 2011 | Patients were educated on self‐monitoring only |
| Hasan 2011 | Not an RCT |
| Heidbuchel 2015 | Not an RCT, review article |
| Holbrook 2007 | No AF patients |
| Jackson 2004 | Does not measure any of the required outcomes |
| Jank 2009 | No unpublished AF data provided on request |
| Khan 2004 | Randomisation procedure did not meet inclusion criteria |
| Krause 2010 | Systematic review not an RCT |
| Lakshmi 2013 | No unpublished AF data provided on request |
| Landefeld 1992 | No AF patients |
| Leger 2004 | Not an RCT, wrong patient group |
| Machtinger 2007 | No unpublished AF data provided on request |
| Matchar 2005 | No education or behaviour change within the intervention |
| Matchar 2010 | Self‐monitoring only, no educational or behavioural intervention |
| Mazor 2007 | No AF patients |
| McCahon 2011 | No breakdown of patient group |
| Megden 1999 | Not an RCT |
| Menendez‐Jandula 2005 | No unpublished AF data provided on request |
| Moore 2013 | No breakdown of patient group |
| Morin 2015 | Not an RCT, research model |
| Moss 2014 | No unpublished AF data provided on request |
| Nedaz 2002 | Not an RCT, this paper is a commentary |
| Nilsson 2011 | Abstract only, no mention of AF patients |
| O'Sullivan 2016 | Does not include any of the primary or secondary outcomes |
| Peng 2014 | Does not include any of the primary or secondary outcomes |
| Pernod 2008 | No AF patients |
| Polzien 2007 | Not an RCT, commentary |
| PRISM Study group 2003 | Does not include any of the primary or secondary outcomes |
| Qvist 2016 | Not an RCT, no comparison group |
| Reverdin 2011 | Not an RCT |
| Ryan 2009 | No unpublished AF data provided on request |
| Saokaew 2010 | Systematic review and meta‐analysis, not an RCT |
| Satger 2009 | Not an RCT, review article |
| Sawicki 1999 | No unpublished AF data provided on request |
| Sawicki 2003 | Not an RCT, no comparison group |
| Siebenhofer 2007 | No unpublished AF data provided on request |
| Stafford 2011 | Not a randomised trial |
| Stone 1989 | No unpublished AF data provided on request |
| Sunderji 2005 | Education only relates to self‐monitoring |
| Suriano 2014 | No breakdown of patient group |
| Taylor 1997 | Not an RCT |
| Trivalle 2010 | Education of staff not patients |
| Tuiskula 2011 | Not an RCT |
| Turc‐Dessertine 2005 | Not an RCT, survey. No intervention or control group |
| Vadher 1996 | No breakdown of patient group |
| Vadher 1997 | No breakdown of patient group |
| Verret 2012 | No breakdown of patient group |
| Waterman 2001 | No AF patients, no comparison group |
| Waterman 2001 b | No patient intervention |
| Watzke 2000 | No unpublished AF data provided on request |
| Winans 2010 | Not an RCT |
| Witt 2005 | Not an RCT, retrospective, observational cohort study |
| Woodend 2005 | Not an RCT (commentary) |
| Wurster 2006 | Not an RCT |
| Yildirim 2015 | No unpublished AF data provided on request |
Characteristics of ongoing studies [ordered by study ID]
Siebenhofer 2012.
| Trial name or title | Primary Care Management for Optimized Antithrombotic Treatment [PICANT] |
| Methods | Cluster randomised controlled trial |
| Participants | Patients with an indication for oral anticoagulation |
| Interventions | Patient information leaflet and a video developed by Vormfelde 2014, treatment monitoring via the Coagulation Monitoring List, and encouragement to participate in a self‐management course where they will learn how to carry out self‐testing and self‐dosing. |
| Outcomes |
Primary outcome: combined endpoint of all thromboembolic events requiring hospitalisation and all major bleeding complications. Secondary outcomes: mortality, hospitalisation, stroke, major bleeding and thromboembolic complications, severe treatment interactions, number of adverse events, quality of anticoagulation, health‐related quality of life, and costs. |
| Starting date | July 2012 |
| Contact information | siebenhofer@allgemeinmedizin.uni‐frankfurt.de |
| Notes |
ACCP: American College of Clinical Pharmacy AF: atrial fibrillation ECG: Electrocardiography GP: general practitioner INR: international normalised ratio NVAF: nonvalvular atrial fibrillation OAT: oral anticoagulation therapy PAF: paroxysmal atrial fibrillation SPAF Stroke Prevention in Atrial Fibrillation Study TIA: transient ischemic attack TTR: time in therapeutic range VTE: venous thromboembolism
Differences between protocol and review
1. Contributions of the authors
The contributions of authors has changed from the original protocol (see contributions of authors section).
2. Decision conflict as a secondary outcome
Decision conflict was included as a secondary outcome in the final analysis. Whilst not specified as an outcome of interest in the original protocol, it was highlighted as a common secondary outcome measure in three of the studies included in the final review. For this reason, the authors decided to include these data within the results.
Contributions of authors
Data collection, paper searches, screening and appraisal, and data extraction were conducted by Miss Khaing and Drs Clarkesmith and Lane. Dr Clarkesmith wrote the initial draft of the Introduction and Methods of the review paper, which was edited by Dr Lane. Drs Clarkesmith and Lane performed the data analysis together and drafted the Results and Discussion sections. Both Dr Clarkesmith and Dr Lane revised and commented on subsequent drafts. Professor Pattison contributed to the interpretation of the analyses and provided critical revision of drafts of the review.
Sources of support
Internal sources
No sources of support supplied
External sources
University of Birmingham Centre for Cardiovascular Sciences, City Hospital, UK.
Aston University, UK.
Declarations of interest
Dr Clarkesmith completed a PhD studentship that was funded by an Investigator‐Initiated Educational Grant from Bayer Healthcare and Aston University when the original review was conducted, but currently works as a post‐doctoral researcher with no conflicts of interest. Miss Khaing reports no conflicts of interest. Dr Lane was the principal grant holder for the 'TRial of an Educational intervention on patients' knowledge of Atrial fibrillation and anticoagulant therapy, INR control, and outcome of Treatment with warfarin' (TREAT). Dr Clarkesmith was the primary investigator for TREAT. Dr Lane and Professor Pattison were the educational supervisors of Dr Clarkesmith for the TREAT study. This review is not funded by Bayer Healthcare.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Beyth 2000 {published data only}
- Beyth RJ, Landefeld CS. Multicomponent comprehensive care was as effective as usual care for decreasing major bleeding in older patients on warfarin. Evidence Based Medicine 2001;6:116. [Google Scholar]
- Beyth RJ, Quinn L, Landefeld S. A multicomponent intervention to prevent major bleeding complications in older patients receiving warfarin. Annals of Internal Medicine 2000;133(9):687‐95. [DOI] [PubMed] [Google Scholar]
Christensen 2007 {published data only}
- Christensen TD, Maegaard M, Sorensen HT, Hjortdal VE, Hasenkam. Self‐versus conventional management of oral anticoagulant therapy. American Journal of Cardiovascular Drugs 2007;7(3):191‐7. [DOI] [PubMed] [Google Scholar]
- Christensen TD, Maegaard M, Sorensen HT, Hjortdal VE, Hasenkam JM. Self‐management versus conventional management of oral anticoagulant therapy: A randomised, controlled trial. European Journal of Internal Medicine 2006;17:260‐6. [DOI] [PubMed] [Google Scholar]
Clarkesmith 2013 {published data only}
- Clarkesmith DE, Pattison HM, Lip GYH, Lane DA. Educational intervention improves anticoagulation control in atrial fibrillation patient. PLoS One 2013;8(9):e74037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DE, Borg Xuereb C, Pattison HM, Lip GYH, Lane DA. TRial of an Educational intervention on patients' knowledge of Atrial fibrillation and anticoagulant therapy, INR control and outcome of Treatment with warfarin (TREAT). BMC Cardiovascular Disorders 2010;10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gadisseur 2003 {published data only}
- Gadisseur APA, Breukink‐Enghers WGM, Meer FJM, Besselaar AMH, Sturk A, Rosendaal FR. Comparison of the quality of oral anticoagulant therapy through patient self‐management by specialized anticoagulation clinics in the Netherlands. Archives of Internal Medicine 2003;163(24):2639‐46. [DOI] [PubMed] [Google Scholar]
- Gadisseur APA, Kaptein AA, Breukink‐Engbers WGM, meer FJM, Rosendaal FR. Patient self‐management of oral anticoagulant care vs. management by specialized anticoagulation clinics: positive effects on quality of care. Journal of Thrombosis and Haemostasis 2004;2:584‐91. [DOI] [PubMed] [Google Scholar]
Hendriks 2013 {published data only}
- Hendriks J, Crijins H, Wit R, Vrijhoef H, Tieleman R. A disease management program in atrial fibrillation: a guidelines‐based, nurse‐driven, ICT‐supported outpatient clinic. Acta Cardiologica 2009;64(1):144‐5. [Google Scholar]
- Hendriks J, Tomini F, Asselt T, Crijins H, Vrijhoef H. Cost‐effectiveness of a specialized atrial fibrillation clinic vs. usual care in patients with atrial fibrillation. Europace 2013;15:1128‐35. [DOI] [PubMed] [Google Scholar]
- Hendriks JML, Crijins HJGM, Vrijhoef HJM. Integrated chronic care management for patients with atrial fibrillation: a rationale for redesigning atrial fibrillation care. Journal of Atrial Fibrillation 2015;7(5):45‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendriks JML, Vrijhoef HJM, Crijins HJGM, Brunner‐La Rocca HP. The effect of a nurse‐led integrated chronic care approach on quality of life in patients with atrial fibrillation. Europace 2014;16:491‐9. [DOI] [PubMed] [Google Scholar]
- Hendriks JML, Wit R, Crijins HJGM, Vrijhoef HJM, Prins MH, Pisters R, et al. Nurse‐led care vs. usual care for patients with atrial fibrillation: results of a randomized trial of integrated chronis care vs. routine clinical care in ambulatory patients with atrial fibrillation. European Heart Journal 2012;33:2692‐9. [DOI] [PubMed] [Google Scholar]
- Hendriks JML, Wit R, Vrijhoef HJM, Tieleman RF, Crijins HJGM. An integrated chronic care program for patients with atrial fibrillation: Study protocol and methodology for an ongoing prospective randomised controlled trial. International Journal of Nursing Studies 2010;47:1310‐16. [DOI] [PubMed] [Google Scholar]
Man‐Son‐Hing 1999 {published data only}
- Man‐Son‐Hing M, Laupacis A, O'Connor AM. A patient decision aid regarding antithrombotic therapy for stroke prevention in atrial fibrillation: A randomized controlled trial. JAMA 1999;282(8):737‐43. [DOI: 10.1001/jama.282.8.737] [DOI] [PubMed] [Google Scholar]
McAlister 2005 {published data only}
- McAlister FA, Man‐Son‐Hing M, Straus SE, Ghali WA, Anderson D, Majumdar SR, et al. Impact of a patient decision aid on care among patients with nonvalvular atrial fibrillation: a cluster randomised trial. Canadian Medical Association Journal 2005;173(5):496‐501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlister FA, Man‐Son‐Hing M, Straus SE, Ghali WA, Gibson P, Anderson D, et al. A randomised trial to assess the impact of an antithrombotic decision aid in patients with nonvalvular atrial fibrillation: the DAAFI trial protocol [ISRCTNI4429643]. BMC Cardiovascular Disorders 2004;4:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Polek 2012 {published data only}
- Polek C, Hardie T. Warfarin use post hospitalization: pilot comparative effectiveness of telephone follow‐up. Rehabilitation Nursing 2012;37(2):80‐7. [DOI] [PubMed] [Google Scholar]
Thomson 2007 {published data only}
- Thomson RG, Eccles MP, Steen IN, Greenaway J, Stobbart L, Murtagh MJ, et al. A patient decision aid to support shared decision‐making on anti‐thrombotic treatment of patients with atrial fibrillation: a randomised controlled trial. Quality and Safety in Health Care 2007;16:216‐23. [DOI: 10.1136/qshc.2006.018481] [DOI] [PMC free article] [PubMed] [Google Scholar]
Voller 2005 {published data only}
- Voller H, Glatz J, Taborski U, Bernado A, Dovifat C, Bunkard G, et al. Background and test plan of the study for self‐management of anticoagulation in patients with non‐ventricular atrial fibrillation [Hintergrund und Prufplan der studie zum Selbstmanagement der Antikoagulation bei Patient mit nichtvalvularem Vorhofflimern (SMAAF‐studie)]. Zeitschrift fur Kardiologie 2000;89:284‐8. [DOI] [PubMed] [Google Scholar]
- Voller H, Glatz J, Taborski U, Bernardo A, Dovifat C, Heidinger K. Self‐management of oral anticoagulation in nonvalvular atrial fibrillation (SMAAF study) [Selbstmanagement de antikoagulation bei patienten mit nichtvalvularem vorhofflimmern]. Zeitschrift fur Kardiologie 2005;94(3):183‐6. [DOI] [PubMed] [Google Scholar]
Vormfelde 2014 {published data only}
- Hua TD, Vormfelde SV, Abed MA, Schneider‐Rudt H, Sobotta P, Friede T, et al. Practice nurse‐based, individual and video assisted patient education in oral anticoagulation ‐ Protocol of a cluster‐randomized controlled trial. BMC Family Practice 2011;12:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vormfelde SV, Abu Abed M, Hua TD, Schneider S, Friede T, Chenot JF. Educating orally anticoagulated patients in drug safety‐ a cluster randomized study in general practice. Dtsch Arztebl Int 2014;111:607‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Al‐Meshal 2013 {published data only}
- Al‐Meshal N, Al‐Sultan R, Al Moones S, Al‐Sudaus H, Bawazeer G, Zayed E, et al. The impact of a structured educational program on patient knowledge about their warfarin therapy. International Journal of Pharmacy Practice 2013;21:28. [Google Scholar]
Armstrong 2011 {published data only}
- Armstrong EP, Chemodurow L, Christensen S, Johnson ES. A pre‐ post‐evaluation of implementing an inpatient monitoring and education program. Pharmacy Practice 2011;9(2):101‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bajorek 2005 {published data only}
- Bajorek BV, Krass I, Ogle SJ, Duguid MJ, Shenfield GM. Optimizing the use of antithrombotic therapy for atrial fibrillation in older people: A pharmacist‐led mutlidisciplinary intervention. Journal of the American Geriatrics Society 2005;53:1912‐20. [DOI: 10.1111/j.1532-5415.2005.53564.x] [DOI] [PubMed] [Google Scholar]
Baker 1991 {published data only}
- Baker D, Roberts DE, Newcombe RG, Fox KAA. Evaluation of drug information for cardiology patients. British Journal of Clinical Pharmacy 1991;31:525‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Barcellona 2006 {published data only}
- Barcellona D, Contu P, Marongiu F. A two‐step educational approach for patients taking oral anticoagulants does not improve therapy control. Journal of Thrombosis and Thrombolysis 2006;22:185‐90. [DOI: 10.1007/s11239-006-9027-2] [DOI] [PubMed] [Google Scholar]
Batty 2001 {published data only}
- Batty G, Oborne CA, Hooper R, Jackson S. Investigation of intervention strategies to increase the appropriate use of antithrombotics in elderly hospital inpatients with atrial fibrillation. The Journal of Clinical Governance 2001;9:115‐22. [Google Scholar]
Bereznicki 2013 {published data only}
- Bereznicki L, Jackson S, Peterson G. Supervised patient self‐testing of warfarin therapy using an online system. Journal of Medical Internet Research 2013;15:e138. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blaise 2009 {published data only}
- Blaise S, Satger B, Fontaine M, Yver J, Rastel D, Toffin L, et al. Evaluation of an education program for patients taking oral anticoagulants: Experience of the GRANTED network in Isere [Evaluation d'un programme d'education therapeutique pour les traitments anticoagulants oraux: exerience du reseau Ville‐Hopital GRANTED du secteur Sud‐Isere]. Journal des Maladies Vasculaires 2009;34:346‐53. [DOI: 10.1016/j.jmv.2009.07.088] [DOI] [PubMed] [Google Scholar]
Bloomfield 2011 {published data only}
- Bloomfield HE, Krause A, Greer N, Taylor BC, MacDonald R, Rutks I, et al. Meta‐analysis: effect of patient self‐testing and self‐management of long‐term anticoagulation on major clinical outcomes. Annals of Internal Medicine 2011;154(7):472‐w‐160. [DOI] [PubMed] [Google Scholar]
Bump 1977 {published data only}
- Bump CM, Campbell JG. The relationship of patient education to the clinical course of patients receiving anticoagulants. Abstracts of Hospital Management Studies 1977;14(2):18091. [Google Scholar]
Burns 2009 {published data only}
- Burns S. Application of the theory of planned behavior to oral anticoagulation therapy. Nursing and Health Sciences 2009;11:98‐101. [DOI: 10.1111/j.1442-2018.2009.00426.x] [DOI] [PubMed] [Google Scholar]
Castelino 2010 {published data only}
- Castelino RL, Chen TF, Guddattu V, Bajorek BV. Use of evidence‐based therapy for the prevention of cardiovascular events among older people. Evaluation & the Health Professions 2010;33(3):276‐301. [DOI] [PubMed] [Google Scholar]
Chan 2006 {published data only}
- Chan FWH, Wong RSM, Lau WH, Chan TYK, Cheng G, You JHS. Management of Chinese patients on warfarin therapy in two models of anticoagulation service ‐ a prospective randomized trial. British Journal of Clinical Pharmacology 2006;62(5):601‐9. [DOI: 10.1111/j.1365-2125.2006.02693.x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Christensen 2011 {published data only}
- Christensen H, Lautertein JJ, Sorensen PD, Petersen ERB, Madsen JS, Brandslund I. Home management of oral anticoagulation via telemedicine versus conventional hospital‐based treatment. Telemedicine and e‐Health 2011;17(3):169‐76. [DOI: 10.1089/tmj.2010.0128] [DOI] [PMC free article] [PubMed] [Google Scholar]
Claes 2005 {published data only}
- Claes N, Buntinx F, Vijgen J, Arnout J, Vermylen J, Fieuws S, et al. The Belgian improvement study on oral anticoagulation therapy: a randomized clinical trial. European Heart Journal 2005;26(20):2159‐65. [DOI] [PubMed] [Google Scholar]
Claes 2006 {published data only}
- Claes N, Moeremans K, Frank B, Jef A, Jos V, Herman VL, et al. Estimating the cost‐effectiveness of quality‐improving interventions in oral anticoagulation management within general practice. Value in Health 2006;9(6):369‐76. [DOI: 10.1111/j.1524-4733.2006.00129] [DOI] [PubMed] [Google Scholar]
Corbella 2009 {published data only}
- Corbella A, Bottari L, Cevasco I, Giacobbe S, Roba I, Rossini S, et al. Patients in chronic anticoagulation therapy: the organization of an educational program run by nurses and the assessment of patients' satisfaction [Le persone in Terapia Anticoagulante Orale (TAO): costruzione di un intervento gestito dagli infermieri e valutazione del gradimento]. Assistenza Infermieristica e Ricerca 2009;28(2):65‐72. [PubMed] [Google Scholar]
Cordasco 2009 {published data only}
- Cordasco KM, Asch SM, Bell DS, Guterman JJ, Gross‐Schulman S, Ramer L, et al. A low‐literacy medication education tool for safety‐net hospital patients. American Journal of Preventative Medicine 2009;37(6 Suppl 1):S209‐16. [DOI: 10.1016/j.amepre.2009.08.018] [DOI] [PubMed] [Google Scholar]
Cromheecke 2000 {published data only}
- Cromheecke ME, Levi M, Colly LP, Mol BJM, Prins MH, Hutten BA, et al. Oral anticoagulation self‐management and management by a specialist anticoagulation clinic: a randomised cross‐over comparison. Lancet 2000;356(8):97‐102. [DOI] [PubMed] [Google Scholar]
Cromheecke 2001 {published data only}
- Cromheecke ME, Levi M, Colly LP. Self management of long term oral anticoagulation was as effective as specialist anticoagulation clinic management. Evidence‐Based Medicine 2001;6(2):41. [Google Scholar]
Davis 2005 {published data only}
- Davis NJ, Billett HH, Cohen HW, Arnsten JH. Impact of adherence, knowledge, and quality of life on anticoagulation control. Annals of Pharmacotherapy 2005;39(4):632‐6. [DOI] [PubMed] [Google Scholar]
Dolor 2010 {published data only}
- Dolor RJ, Ruybalid RL, Uyeda L, Edson RG, Phibbs C, Vertrees JE, et al. An evaluation of patient self‐testing competency of prothrombin time for managing anticoagulation: pre‐randomization results of VA cooperative study #481 ‐ The home INR study (THINRS). Journal of Thrombosis and Thrombolysis 2010;30:263‐75. [DOI] [PubMed] [Google Scholar]
Duran‐Parrondo 2011 {published data only}
- Duran‐Parrondo C, Vazquez‐Lago JM, Campos‐Lopez AM, Figueras A. Impact of a pharmacotherapeutic programme on control and safety of long‐term anticoagulation treatment. Drug Safety 2011;34(6):489‐500. [DOI] [PubMed] [Google Scholar]
Field 2010 {published data only}
- Field TS, Tjia J, Mazor KM, Donovan JL, Kanaan AO, Harrold LR, et al. Randomized trial of a warfarin communication protocol for nursing homes: an SBAR‐based approach. The American Journal of Medicine 2011;124:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fitzmaurice 1996 {published data only}
- Fitzmaurice DA, Hobbs FDR, Murray ET, Bradley CP, Holder R. Evaluation of computerized decision support for oral anticoagulation management based in primary care. British Journal of General Practice 1996;46:533‐5. [PMC free article] [PubMed] [Google Scholar]
Fitzmaurice 2000 {published data only}
- Fitzmaurice DA, Hobbs FD, Murray ET. A nurse led clinic and computer decision support software for anticoagulation decisions were as effective as a hospital clinic. Evidence Based Medicine 2001;6:61. [Google Scholar]
- Fitzmaurice DA, Hobbs FD, Murray ET, Holder RL, Allan TF, Rose PE. Oral anticoagulation management in primary care with the use of computerized decision support and near‐patient testing: a randomised, controlled trial. Archives of Internal Medicine 2000;160(15):2343‐8. [DOI] [PubMed] [Google Scholar]
Fitzmaurice 2005 {published data only}
- Fitzmaurice DA, Murray ET, Gee KM. A randomised controlled trial of patient self management of oral anticoagulation treatment compared with primary care management. Journal of Clinical Pathology 2002;55:845‐9. [DOI: 10.1136/jcp.55.11.845] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzmaurice DA, Murray ET, McCahon MD, Holder R, Raferty JP, Hussain S, et al. Self management of oral anticoagulation: randomised trial. BMJ 2005;331(7524):1057. Erratum in: BMJ 2005 331(7528):1330. [DOI: 10.1136/bmj.38618.580903.AE; ISRCTN 19313375] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E, Fitzmaurice D, MaCahon D, Fuller C, Sandhur H. Training for patients in a randomised controlled trial of self management of warfarin treatment. BMJ 2004;328(21):437. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fraenkel 2011 {published data only}
- Fraenkel L, Street RL, Fried TR. Development of a tool to improve the quality of decision making in atrial fibrillation. BMC Medical Informatics and Decision Making 2011;11:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gardiner 2006 {published data only}
- Gardiner C, Williams K, Longair I, Mackie IJ, Machin SJ, Cohen H. A randomised control trial of patient self‐management of oral anticoagulation compared with patient self‐testing. British Journal of Haematology 2006;132:598‐603. [DOI: 10.1111/j.1365-2141.2005.05899] [DOI] [PubMed] [Google Scholar]
Gouin‐Thibault 2010 {published data only}
- Gouin‐Thibault I, Levy C, Pautas E, Cambus JP, Drouet L, Mahe I, et al. Improving anticoagulation control in hospitalized elderly patients on warfarin. Journal of the American Geriatrics Society 2010;58:242‐7. [DOI] [PubMed] [Google Scholar]
Grunau 2011 {published data only}
- Grunau B, Wiens MO, Harder KK. Patient self‐management of warfarin therapy. Canadian Family Physician 2011;57:292‐8. [PMC free article] [PubMed] [Google Scholar]
Hasan 2011 {published data only}
- Hasan SS, Sharmala R, Syed IA, Basariah N, Chong DWK, Mei TK, et al. Factors affecting warfarin‐related knowledge and INR control of patients attending physician‐ and pharmacist‐managed anticoagulation clinics. Journal of Pharmacy Practice 2011;24(5):485‐93. [DOI] [PubMed] [Google Scholar]
Heidbuchel 2015 {published data only}
- Heidbuchel H, Berti D, Campos M, Destenghe L, Freixo A, Nunes A, et al. Implementation of non‐vitamin K antagonist oral anticoagulants in daily practice: the need for comprehensive education for professionals and patients. Thrombosis Journal 2015;13:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Holbrook 2007 {published data only}
- Holbrook A, Labiris R, Goldsmith CH, Ota K, Harb S, Sebaldt RJ. Influence of decision aids on patient preferences for anticoagulant therapy: a randomized trial. Canadian Medical Association Journal 2007;176(11):1583‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2004 {published data only}
- Jackson SL, Peterson M, Vial JH. A community‐based educational intervention to improve antithrombotic drug use in atrial fibrillation. The Annals of Pharmacotherapy 2004;38:1794‐9. [DOI: 10.1345/aph.1E152] [DOI] [PubMed] [Google Scholar]
Jank 2009 {published data only}
- Jank S, Kappler M, Markmann A, Bertsche T, Klimm HD, Haefeli WE. Impact of an individualised computer‐assisted educational intervention on management of anticoagulation therapy. Basic and Clinical Pharmacology and Toxicology 2009;106(6):526. [Google Scholar]
Khan 2004 {published data only}
- Khan TI, Kamali F, Kesteven P, Avery P, Wynne H. The value of education and self‐monitoring in the management of warfarin therapy in older patients with unstable control of anticoagulation. British Journal of Haematology 2004;126:557‐64. [DOI] [PubMed] [Google Scholar]
Krause 2010 {published data only}
- Krause A, Bloomfield H, Wilt T. Safety and effectiveness of patient‐managed outpatient anticoagulation: A systematic review. Journal of General Internal Medicine 2010;25:S387. [Google Scholar]
Lakshmi 2013 {published data only}
- Lakshmi R, James E, Kirthivasan R. Study on the impact of clinical pharmacist's interventions in the optimal use of oral anticoagulants in stroke patients. Indian Journal of Pharmaceutical Sciences 2013;75:53‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Landefeld 1992 {published data only}
- Landefeld CS, Anderson PA. Guideline‐based consultation to prevent anticoagulation‐related bleeding. Annals of Internal Medicine 1992;116(10):829‐37. [DOI] [PubMed] [Google Scholar]
Leger 2004 {published data only}
- Leger S, Allenet B, Pichot O, Figari G, Calop J, Carpentier P, et al. Impact of an education program on patient behaviour favoring prevention of drug‐related adverse events: a pilot study in patients receiving oral anticoagulants for thromboembolic venous disease [Impact d'un pragramme d'education therapeutique sur les attitudes de prevention vis‐s‐vis du risque iatrogene: etude pilote controlee visant les patients sous‐anticoagulants oraux pour maladie thromboembolique veineuse]. Journal des Maladies Vasculaires 2004;29(3):152‐8. [DOI] [PubMed] [Google Scholar]
Machtinger 2007 {published data only}
- Machtinger EL, Wang F, Chen LL, Rodriguez M, Wu S, Schilinger D. A visual medication schedule to improve anticoagulation control: A randomised controlled trial. The Joint Commission Journal on Quality and Patient Safety 2007;33(10):625‐35. [DOI] [PubMed] [Google Scholar]
Matchar 2005 {published data only}
- Matchar DB, Jacobson AK, Edson RG, Lavori PW, Ansell JE, Ezekowitz MD, et al. The impact of patient self‐testing of prothrombin time for managing anticoagulation: Rationale and design of VA cooperative study #481 ‐ the home INR study (THINRS). Journal of Thrombosis and Thrombolysis 2005;19(3):163‐72. [DOI] [PubMed] [Google Scholar]
Matchar 2010 {published data only}
- Matchar DB, Jacobson A, Dolor R, Edson R, Uyeda L, Phibbs CS, et al. Effect of home testing of international normalised ratio on clinical events. The New England Journal of Medicine 2010;363(17):1608‐20. [DOI] [PubMed] [Google Scholar]
Mazor 2007 {published data only}
- Mazor KM, Baril J, Dugan E, Spencer F, Burgwinkle P, Gurwitz JH. Patient education about anticoagulant medication: Is narrative evidence or statistical evidence more effective?. Patient Education and Counseling 2007;69:145‐57. [DOI: 10.1016/j.pec.2007.08.010] [DOI] [PubMed] [Google Scholar]
McCahon 2011 {published data only}
- McCahon D, Fitzmaurice DA, Murray ET, Fuller CJ, Hobbs RFD, Allan TF, Raferty JP. SMART: Self‐management of anticoagulation, a randomised trial. BMC Family Practice 2003;4:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCahon D, Murray ET, Murray K, Holder RL, Fitzmaurice DA. Does self‐management of oral anticoagulation therapy improve quality of life and anxiety?. Family Practice 2011;28(2):134‐40. [DOI] [PubMed] [Google Scholar]
Megden 1999 {published data only}
- Megden TH, Heidgen FJ, Vetter H. Optimization of long term control of oral anticoagulation by patient self‐management [Verbesserung der langzeitkontrolle der oralen antikoagulation durch patienten‐selbstmanagement]. Herz Kreislauf 1999;31(10):393‐7. [Google Scholar]
Menendez‐Jandula 2005 {published data only}
- Menendez‐Jandula B, Souto J, Oliver A, Monserrat I, Quintana M, Gich I, et al. Comparing self‐management of oral anticoagulant therapy with clinic management. Annals of Internal Medicine 2005;145:1‐10. [DOI] [PubMed] [Google Scholar]
- Menendez‐Jandula B, Souto JC, Oliver A. Patient self management of anticoagulants resulted in fewer major complications than clinic‐based management. Evidence Based Nursing 2005;142:1‐10. [DOI] [PubMed] [Google Scholar]
Moore 2013 {published data only}
- Moore SJ, Blair EA, Steeb D, Reed BN, Hull JH, Crisp B, et al. Use of video technology to improve pharmacist efficiency and patient comprehension of anticoagulation education. Pharmacotherapy 2013;33(10):e264. [Google Scholar]
- Moore SJ, Blair EA, Steeb DR, Reed BN, Hull JH, Rodgers JE. Impact of video technology on efficiency of pharmacist‐provided anticoagulation counseling and patient comprehension. Annals of Pharmacotherapy 2015;49:631‐8. [DOI] [PubMed] [Google Scholar]
Morin 2015 {published data only}
- Morin MM, Weimer CA. Design and implementation of an ambulatory anticoagulation therapy program using RN: Pharmacy model. Journal of Thrombosis and Thrombolysis 2015;39(3):413. [Google Scholar]
Moss 2014 {published data only}
- Moss RC, Lowe GC, Frampton CA, Revell P. A nurse‐led randomised controlled trial of a structured educational programme for patients starting warfarin therapy. Journal of Research in Nursing 2014;19:402‐12. [Google Scholar]
Nedaz 2002 {published data only}
- Nedaz M. Atrial fibrillation, anticoagulation and shared decision making [Fibrillation auriculaire et partage avec le patient de la decision d'anticoaguler]. Medecine et Hygiene 2002;60(2412):2054‐8. [Google Scholar]
Nilsson 2011 {published data only}
- Nilsson N, Eide TH, Kjeldhy C, Refsum N, Dahle G. What knowledge do patients on warfarin have about their treatment, and may patient education by a pharmacist improve their knowledge?. International Journal of Clinical Pharmacy 2011;33:418. [Google Scholar]
O'Sullivan 2016 {published data only}
- O'Sullivan D, Mahony D, O'Connor MN, Gallagher P, Gallagher J, Cullinan S, et al. Prevention of adverse drug reactions in hospitalised older patients using a software‐supported structured pharmacist intervention: a cluster randomised controlled trial. Drugs and Ageing 2016;33:63‐73. [DOI] [PubMed] [Google Scholar]
Peng 2014 {published data only}
- Peng B, Ni J, Anderson CS, Zhu Y, Wang Y, Pu C, et al. Implementation of a structured guideline‐based program for the secondary prevention of ischemic stroke in China. Stroke 2014;45:515‐9. [DOI] [PubMed] [Google Scholar]
Pernod 2008 {published data only}
- Pernod G, Labarere J, Yver J, Satger B, Allenet B, Berremili T, et al. EDUC'AVK: Reduction of oral anticoagulant‐related adverse events after patient education: A prospective multicenter open randomized study. Journal of General Internal Medicine 2008;23(9):1441‐6. [DOI: 10.1007/s11606-008-0690-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Polzien 2007 {published data only}
- Polzien G. Prevent medication errors: a new year's resolution. Home Healthcare Nurse 2007;25(1):59‐62. [DOI] [PubMed] [Google Scholar]
PRISM Study group 2003 {published data only}
- Lees KR, Sim I, Wier CJ, Erwin L, McAlpine C, Rodger J, et al. Cluster‐randomized, controlled trial of computer‐based decision support for selecting long‐term anti‐thrombotic therapy after acute ischaemic stroke. QJM: An International Journal of Medicine 2003;96:143‐53. [DOI: 10.1093/qjmed/hcg019] [DOI] [PubMed] [Google Scholar]
Qvist 2016 {published data only}
- Qvist I, Hendriks JML, Moeller DS, Albertsen AE, Mogensen HM, Oddershede GD, et al. Effectiveness of structured, hospital‐based, nurse‐led atrial fibrillation clinics: a comparison between a real‐world population and a clinical trial population. Open Heart 2016;3:e000335. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reverdin 2011 {published data only}
- Reverdin S, Schnetzler B, Gagneux G, Gavignet C, Boehlen F, Moerloose P. Implementation of an INR self‐testing and self‐management programme in common ambulatory private practice: our experience with 90 patients. Swiss Medical Weekly 2011;141:w13199. [DOI] [PubMed] [Google Scholar]
Ryan 2009 {published data only}
- Ryan F, Byrne S, OShea S. Randomized controlled trial of supervised patient self‐testing of warfarin therapy using an internet‐based expert system. Journal of Thrombosis and Haemostasis 2009;7:1284‐90. [DOI] [PubMed] [Google Scholar]
Saokaew 2010 {published data only}
- Saokaew S, Permsuwan U, Chaiyakunapruk N, Nathisuwan S, Sukonthasarn A. Effectiveness of pharmacist‐participated warfarin therapy management: a systematic review and meta‐analysis. Journal of Thrombosis and Haemostasis 2010;8:2418‐27. [DOI] [PubMed] [Google Scholar]
Satger 2009 {published data only}
- Satger B, Blaise S, Fontaine M, Yver J, Allenet B, Baudrant M, et al. Therapy education for patients receiving oral anti‐coagulants vitamin K antagonists [Education therapeutique des patients traites par anticoagulants oraux antivitamines k]. La Presse Medicale 2009;38(12):1780‐7. [DOI: 10.1016/j.lmp.2009.07.019] [DOI] [PubMed] [Google Scholar]
Sawicki 1999 {published data only}
- Sawicki PT, for the working group for the study of patient self‐management of oral anticoagulation. A structured teaching and self‐management program for patients receiving oral anticoagulation. JAMA 1999;281(2):145‐50. [DOI] [PubMed] [Google Scholar]
Sawicki 2003 {published data only}
- Sawicki PT, Blaser B, Didjurgeit U, Kaiser T, Kleepies C, Schmitz N, et al. Long‐term results of patient's self‐management of oral anticoagulation. Journal of Clinical and Basic Cardiology 2003;6(1‐4):59‐62. [DOI] [PubMed] [Google Scholar]
Siebenhofer 2007 {published data only}
- Siebenhofer, A, Rakovac I, Kleepies C, Piso B, Didjurgeit U. Self‐management of oral anticoagulation in the elderly: Rationale, design, baselines and oral anticoagulation control after one year follow‐up. Blood Coagulation, Fibrinolysis and Cellular Haemostasis 2007;97:408‐16. [DOI: 10.1160/TH06-08-0482] [DOI] [PubMed] [Google Scholar]
Stafford 2011 {published data only}
- Stafford L, Peterson GM, Bereznicki LRE, Jackson S. A role for pharmacists in community‐based post‐discharge warfarin management: protocol for the 'role of community pharmacy in post hospital management of patients initiated on warfarin' study. BMC Health Services Research 2011;11:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stone 1989 {published data only}
- Stone S, Holden A, Knapic N, Ansell J. Comparison between videotape and personalized patient education for anticoagulant therapy. The Journal of Family Practice 1989;29(1):55‐7. [PubMed] [Google Scholar]
Sunderji 2005 {published data only}
- Sunderji R, Gin K, Shalansky K, Carter C, Chambers K, Davies C, et al. Clinic impact of point‐of‐care vs laboratory measurement of anticoagulation. American Journal of Clinical Pathology 2005;123:184‐8. [PubMed] [Google Scholar]
Suriano 2014 {published data only}
- Suriano M, Tavelli A, Anania S, Braham S, Moia M, Moja EA. Improvement of the time in the therapeutic range (TTR) after a psycho‐educational course in patients on oral anticoagulant therapy (OAT). Thrombosis Research 2014;134:S12. [Google Scholar]
Taylor 1997 {published data only}
- Taylor FC, Gray A, Cohen H, Gaminara L, Ramsay M. Costs and effectiveness of a nurse specialist anticoagulant service. Journal of Clinical Pathology 1997;50:823‐8. [DOI: 10.1136/jcp.50.10.823] [DOI] [PMC free article] [PubMed] [Google Scholar]
Trivalle 2010 {published data only}
- Trivalle C, Cartier T, Verny C, Mathieu AM, Davrinche P, Agostini H, et al. Identifying and preventing adverse drug events in elderly hospitalised patients: a randomised trial of a program to reduce adverse drug effects. The Journal of Nutrition, Health and Ageing 2010;14(1):57‐61. [DOI] [PubMed] [Google Scholar]
Tuiskula 2011 {published data only}
- Tuiskula KA, Sullivan KM, Abraham G, Lahoz MR. Revising warfarin patient education materials to meet a national patient safety goal. American Journal Health‐System Pharmacy 2011;68:974‐6. [DOI] [PubMed] [Google Scholar]
Turc‐Dessertine 2005 {published data only}
- Turc‐Dessertine C. Evaluation of the therapeutic education of the patients under anti‐vitamins K treatment in cardiology service/intensive care unit. Recherche en Soins Infirmiers 2005;1(80):59‐75. [PubMed] [Google Scholar]
Vadher 1996 {published data only}
- Vadher B, Patterson DLH, Leaning M. Comparison of oral anticoagulant control by nurse‐practitioner using a decision‐aid with that by clinicians. British Journal of Haematology 1996;93(1):31. [PubMed] [Google Scholar]
Vadher 1997 {published data only}
- Vadher B, Patterson DLH, Leaning M. Evaluation of a decision support system for initiation and control of oral anticoagulation in a randomised trial. BMJ 1997;314:1252‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Verret 2012 {published data only}
- Verret L, Couturier J, Rozon A, Saudrais‐Janecek S, St‐Onge A, Nguyen A, et al. Impact of a pharmacist‐led warfarin self‐management program on quality of life and anticoagulation control: a randomized trial. Pharmacotherapy: The Journal of Human Pharmacology & Drug Therapy 2012;32:871‐9. [DOI] [PubMed] [Google Scholar]
Waterman 2001 {published data only}
- Waterman AD, Miligan PE, Banet GA, Gatchel SK, Gage BF. Establishing and running an effective telephone‐based anticoagulation service. Journal of Vascular Nursing 2001;19:4. [DOI] [PubMed] [Google Scholar]
Waterman 2001 b {published data only}
- Waterman AD, Banet G, Miligan PE, Frazier A, Verzino E, Walton B, et al. Patient and physician satisfaction with a telephone‐based anticoagulation service. Journal of General Internal Medicine 2001;16:460‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watzke 2000 {published data only}
- Watzke HH, Forberg E, Svolba G. A prospective controlled trial comparing weekly self‐testing and self‐dosing with the standard management of patients on stable oral anticoagulation. Thrombosis and Haemostasis 2000;83:661‐5. [PubMed] [Google Scholar]
Winans 2010 {published data only}
- Winans ARM, Rudd KM, Triller D. Assessing anticoagulation knowledge in patients new to warfarin therapy. The Annals of Pharmacotherapy 2010;44:1152‐7. [DOI] [PubMed] [Google Scholar]
Witt 2005 {published data only}
- Witt DM, Sadler MA, Shanahan RL, Mazzoli G, Tillman DJ. Effect of a centralized clinical pharmacy anticoagulation service on the outcomes of anticoagulation therapy. Chest 2005;127:1515‐22. [DOI: 10.1378/chest.127.5.1515] [DOI] [PubMed] [Google Scholar]
Woodend 2005 {published data only}
- Woodend AK. Patient self management of anticoagulants resulted in fewer major complications than clinic‐based management. Evidence‐Based Nursing 2005;8(3):87. [DOI] [PubMed] [Google Scholar]
Wurster 2006 {published data only}
- Wurster M, Doran T. Anticoagulation management: A new approach. Disease Mangement 2006;9(4):201‐9. [DOI] [PubMed] [Google Scholar]
Yildirim 2015 {published data only}
- Yildirim JG, Temel AB. The effect of nurse home‐support programme on self‐management of the patients receiving oral anticoagulation (Warfarin) therapy. Anadolu Kardiyoloji Dergisi 2015;15:20. [Google Scholar]
References to ongoing studies
Siebenhofer 2012 {published data only}
- Siebenhofer A, Ulrich LR, Mergenthal K, Roehl I, Rauk S, Berghold A, et al. Primary care management for optimized antithrombotic treatment [PICANT]: study protocol for a cluster randomized controlled trial. Implementation Science 2012;7:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulrich LR, Mergenthal K, Petersen JJ, Roehl I, Rauk S, Kemperdick B, et al. Anticoagulant treatment in germany family practices‐ screening results from a cluster randomized controlled trial. BMC Family Practice 2014;15:170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulrich LR, Petersen JJ, Roehl I, Rauck S, Erler A, Kemperdick B, et al. A monitoring list for oral anticoagulation case management in primary care [Eine monitoring‐liste fur ein hausarztliches case management bei oraler antikoagulation]. Continuing Medical Education 2013;89(4):165‐74. [Google Scholar]
Additional references
Aikens 2005
- Aikens JE, Nease DE, Nau PD, Klinkman MS, Schwenk TL. Adherence to maintenance‐phase antidepressant medication as a function of patient beliefs about medication. Annals of Family Medicine 2005;3:23‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ansell 2004
- Ansell J, Hirsh J, Poller L, Bussey H, Jacobsen A, Hylek E. The pharmacology and management of the vitamin K antagonists. Chest 2004;126:204‐33. [DOI] [PubMed] [Google Scholar]
Badia 2007
- Badia X, Arribas F, Ormaetxe JM, Peinado R, Terreros MS. Development of a questionnaire to measure health‐related quality of life (HRQoL) in patients with atrial fibrillation (AF‐QoL).. Health and Quality of Life Outcomes 2007;5(37):1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brazier 1992
- Brazier JE, Harper R, Jones NMB, O'Cathain A, Thomas KJ, Usherwood T. Validating the SF‐36 health survey questionnaire new outcome measure for primary care. British Medical Journal 1992;305:160‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chugh 2014
- Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJ. Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation 2014;129:837‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clifford 2008
- Clifford S, Barber N, Horne R. Understanding different beliefs held by adherers, unintentional non‐adherers: application of the necessity‐concerns framework. Journal of Psychosomatic Research 2008;64:41‐6. [DOI] [PubMed] [Google Scholar]
Coehlo‐Dantas 2004
- Coehlo‐Dantas G, Thomson BV, Manson JA, Tracy CS, Upshur REG. Patients' perspectives on taking warfarin: qualitative study in family practice. BMC Family Practice 2004;5:15. [DOI: 10.1186/1471-2296-5-15] [DOI] [PMC free article] [PubMed] [Google Scholar]
Colilla 2013
- Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. American Journal of Cardiology 2013;112:1142‐1147. [DOI] [PubMed] [Google Scholar]
Connolly 2009
- Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L, RE‐LY steering commitee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. New England Journal of Medicine 2009;361:1139‐1151. [DOI] [PubMed] [Google Scholar]
Connolly 2008
- Connolly SJ, Pogue J, Eikelboom J, Flaker G, Commerford P, Franzosi MG, et al. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalised ratio control achieved by centres and countries as measured by time in therapeutic range. Circulation 2008;118:2029‐37. [DOI] [PubMed] [Google Scholar]
Dantas 2004
- Dantas GC, Thomson BV, Manson JA, Tracy CS, Upshur RE. Patients' perspectives on taking warfarin: qualitative study in family practice. BMC Family Practice 2004;5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Farmer 2006
- Farmer A, Kinmonth AL, Sutton S. Measuring beliefs about taking hypoglycaemic medication. Diabetic Medicine 2006;23:265‐70. [DOI] [PubMed] [Google Scholar]
Fuller 2004
- Fuller R, Dudley N, Blacktop J. Avoidance hierarchies and preferences for anticoagulation‐semi‐qualitative analysis of older patients' views about stroke prevention and the use of warfarin. Age and Ageing 2004;33:608‐11. [DOI] [PubMed] [Google Scholar]
Fuster 2006
- Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation). Circulation 2006;114:257‐354. [DOI] [PubMed] [Google Scholar]
Garcia‐Alamino 2010
- Garcia‐Alamino JM, Ward AM, Alonso‐Coello P, Perera R, Bankhead C, Fitzmaurice D, Heneghan CJ. Self‐monitoring and self‐management of oral anticoagulation: Review. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD003839.pub3] [DOI] [PubMed] [Google Scholar]
Giugliano 2013
- Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Spinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patiel I, Hanyok JJ, Mercuri M, Antman EM, Inverstigators EA‐T. Edoxaban versus warfarin in patients with atrial fibrillation. New England Journal of Medicine 2013;369:2093‐2104. [DOI] [PubMed] [Google Scholar]
GRADEpro 2015 [Computer program]
- GRADE Working Group, McMaster University. GRADEpro GDT. Version accessed 10 December 2016. Hamilton (ON): GRADE Working Group, McMaster University, 2014.
Granger 2011
- Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek E, Hanna M. Apixaban versus warfarin in patients with atrial fibrillation. The New England Journal of Medicine 2011;365:981‐92. [DOI] [PubMed] [Google Scholar]
Hart 2007
- Hart RG, Pearce LA, Aguilar MI. Meta‐analysis: antithrombotic therapy to prevent stroke in patients who have non‐valvular atrial fibrillation. Annals of Internal Medicine 2007;146:857‐67. [DOI] [PubMed] [Google Scholar]
Heeringa 2006
- Heeringa J, Kuip DA, Hofman A, Herpen G, Stricker BH, Stijnen J, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. European Heart Journal 2006;27:949‐53. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. The Cochrane Collaboration, March 2011. [Google Scholar]
Holbrook 2005
- Holbrook AM, Pereira JA, Labiris R, McDonald H, Douketis JD, Crowther M. Systematic overview of warfarin and its drug and food interactions. Archives of Internal Medicine 2005;165:1095‐106. [DOI] [PubMed] [Google Scholar]
Horne 1999
- Horne R, Weinman J. Patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. Journal of Psychosomatic Research 1999;47(6):555‐67. [DOI] [PubMed] [Google Scholar]
Horne 2013
- Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients' adherence‐related beliefs about medicines prescribed for long‐term conditions: a meta‐analytic review of the Necessity‐Concerns Framework.. PLoS One. 2013; Dec 2;8(12):e80633. [DOI: 10.1371/journal.pone.0080633] [DOI] [PMC free article] [PubMed] [Google Scholar]
Howitt 1999
- Howitt A, Armstrong D. Implementing evidence based medicine in general practice: audit and qualitative study of antithrombotic treatment for atrial fibrillation. BMJ 1999;318:1324‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2014
- Jackson C, Eliasson L, Barber N, Weinmann J. Applying COM‐B to medication adherence: a suggested framework for research and interventions. European Health Psychologist 2014;16(1):_. [Google Scholar]
Jessop 2003
- Jessop DC, Rutter DR. Adherence to asthma medications: the role of illness representations. Psychology and Health 2003;18(5):595‐612. [Google Scholar]
Kannel 1998
- Kannel WB, Wolf PA, Benjamin EJ, Levy D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population‐based estimates. American Journal of Cardiology 1998;82(8A):2‐9. [DOI] [PubMed] [Google Scholar]
Kirchhof 2016
- Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, Hindricks G, Manolis AS, Oldgren J, Popescu BA, Schotten U, Vardas P. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. European Heart Journal 2016;27(August):1‐90. [DOI] [PubMed] [Google Scholar]
Kok 2016
- Kok G, Gottleib NH, Peters GJY, Mullen PD, Parecl GS, Ruiter RAC, Fernandez ME, Markham C, Bartholomew K. A taxonomy of behaviour change methods: an intervention mapping approach. Health Psychology Review 2016;10(3):297‐312. [DOI] [PMC free article] [PubMed] [Google Scholar]
Krijthe 2013
- Krijthe BP, Kunst A, Benjamin EJ, Lip GY, Franco OH, Hofman A, Witteman JC, Stricker BH, Heeringa J. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. European Heart Journal 2013;34:2746‐2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lane 2006
- Lane DA, Ponsford J, Shelley A, Sirpal A, Lip GYH. Patient knowledge and perceptions of atrial fibrillation and anticoagulant therapy. Journal of Thrombosis and Haemostasis 2006;110:354‐8. [DOI] [PubMed] [Google Scholar]
Lane 2015
- Lane DA, Aguinaga L, Blomstrom‐Lundqvist C, Boriani G, Hills MT, Hylek EM, LaHaye SA, Lip GY, Lobban T, Madrola J, McCabe PJ, Pedersen SS, Pisters R, Stewart S, Wood K, Potpara TS, Gorenek B, Conti JB, Keegan R, Power S, Hendriks J, Ritter P, Calkins H, Violi F, Hurwitz J. Cardiac tachyarrhythmias and patients values and preferences for their management: the European Heart Rhythm Association (EHRA) consensus document endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), and Sociedad Lationamericana de Estimulacion Cardiaca y Electrofisiologia (SOLEACE). Europace 2015;17:1747‐1769. [DOI] [PubMed] [Google Scholar]
Lane 2017
- Lane DA, Skjøth F, Lip GYH, Larsen TB, Kotecha D. Temporal trends in incidence, prevalence and mortality of atrial fibrillation in primary care.. Journal of the American Heart Association 2017;in Press. [DOI: 10.1161/JAHA.116.005155] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lip 2002
- Lip GYH, Kamath S, Jafri M, Mohammed A, Bareford D, McAlister FA. Ethnic differences in patient perceptions of atrial fibrillation and anticoagulation therapy: the West Birmingham Atrial Fibrillation Project. Stroke 2002;33:238‐44. [DOI] [PubMed] [Google Scholar]
Lip 2006
- Lip GY, Edwards SJ. Stroke prevention with aspirin, warfarin and ximelagatran in patients with non‐valvular atrial fibrillation: a systematic review and meta‐analysis. Thrombosis Research 2006;118:321‐33. [DOI] [PubMed] [Google Scholar]
Lip 2007
- Lip GYH, Agnelli G, Thach AA, Knight E, Rost D, Tangelder MJ. Oral anticoagulation in atrial fibrillation: a Pan‐European Patient Survey. European Journal of Internal Medicine 2007;18:202‐8. [DOI] [PubMed] [Google Scholar]
Lip 2011
- Lip GYH, Andreotti F, Fauchier L, Huber K, Hylek E, Knight E, et al. Bleeding risk assessment and management in atrial fibrillation patients: a position document from the European Heart Rhythm Association, endorsed by the European Society of Cardiology Working Group on Thrombosis. Europace 2011;13:723‐46. [DOI: 10.1093/europace/eur126] [DOI] [PubMed] [Google Scholar]
Lloyd‐Jones 2004
- Lloyd‐Jones DM, Wang TJ, Leip EP, Larson MG, Levy D, Vasan RS, et al. Lifetime risk for developing atrial fibrillation: The Framingham Heart Study. Circulation 2004;110:1042‐6. [DOI] [PubMed] [Google Scholar]
McHorney 2011
- McHorney CA, Spain CV. Frequency of and reasons for medication non‐fulfilment and non‐persistence among American adults with chronic disease. Health Expectations 2011;14(3):307‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
McManus 2012
- McManus DD, Rienstra N, Benjamin AA. An update on the progress of patients with atrial fibrillation. Circulation 2012;126:e143‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Michie 2009
- Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta‐regression. Health Psychology 2009;28(6):690‐701. [DOI: 10.1037/a0016136] [DOI] [PubMed] [Google Scholar]
Michie 2011
- Michie S, Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation Science 2011;6(42). [DOI] [PMC free article] [PubMed] [Google Scholar]
Michie 2013
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behaviour change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Annals of Behavioral Medicine 2013;46(1):81‐95. [DOI: 10.1007/s12160-013-9486-6] [DOI] [PubMed] [Google Scholar]
Miyasaka 2006
- Miyasaka Y, Barnes ME, Gersh BJ. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 2006;114:119‐25. [DOI] [PubMed] [Google Scholar]
Morgan 2009
- Morgan CL, McEwan P, Tukiendorf A, Robinson PA, Clemens A, Plumb JM. Warfarin treatment in patients with atrial fibrillation: Observing outcomes associated with varying levels of INR control. Thrombosis 2009;124:37‐41. [DOI] [PubMed] [Google Scholar]
Nadar 2003
- Nadar S, Begum N, Kaur B, Sandhu S, Lip GYH. Patients understanding of anticoagulation therapy in a multiethnic population. Journal of the Royal Society of Medicine 2003;96:175‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Neame 2005
- Neame R, Hammond A. Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis. Rheumatology 2005;44:762‐7. [DOI] [PubMed] [Google Scholar]
NICE 2006
- National Collaborating Centre for Chronic Conditions. Atrial fibrillation: national clinical guideline for management in primary and secondary care. London: Royal College of Physicians 2006. [PubMed]
NICE 2007
- Behaviour change at population, community and individual levels. NICE Public Health Guidelines 6 2007.
Nunes 2009
- Nunes V, Neilson J, O'Flynn N, Calvert N, Kuntze S, Smithson H, et al. Clinical guidelines and evidence for review for medicines adherence: involving patients in decisions about prescribed medicines and supporting adherence. National Collaborating Centre for Primary care and Royal College of General Practitioners 2009. [PubMed]
O'Connor 1995
- O'Connor AM. Validation of a decision conflict scale. Medical Decision Making 1995;15(1):25‐30. [DOI: 10.1177/0272989X9501500105] [DOI] [PubMed] [Google Scholar]
Patel 2011
- Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. The New England Journal of Medicine 2011;365:883‐91. [DOI] [PubMed] [Google Scholar]
Protheroe 2000
- Protheroe J, Fahey T, Montgomery AA, Peters TJ. The impact of patients' preferences on treatment of atrial fibrillation: observational study of patient based decision analysis. BMJ 2000;320:1380‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rosendaal 1993
- Rosendaal FR, Cannegieter SC, Meer FJM, Briet E. A method to determine the optimal intensity of oral anticoagulant therapy. Thrombosis and Haemostasis 1993;69(3):236‐9. [PubMed] [Google Scholar]
Schulman 2004
- Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non‐surgical patients. Journal of Thrombosis and Haemostasis 2005;3:692‐4. [DOI] [PubMed] [Google Scholar]
Shantsila 2010
- Shantsila A, Lip GYH. Towards (cost) effective cardiovascular risk management: using new drugs vs. the better use of available ones. International Journal of Clinical Practice 2009;64(2):138‐40. [DOI: 10.1111/j.1742-1241.2009.02233.x] [DOI] [PubMed] [Google Scholar]
Sheikh 2015
- Sheikh A, Patel NJ, Nalluri N, Agnihotri K, Spagnola J, Patel A, et al. Trends in hospitalization for atrial fibrillation: epidemiology, cost and implications for the future. Progree in Cardiovascular Diseases 2015;58(2):105‐16. [DOI] [PubMed] [Google Scholar]
Spielberger 1969
- Spielberger CD, Gorsuch RL, Lushene RE. The stait‐trait anxiety inventory. Consulting Psychiatrists Press. California: Palo Alto, 1969. [Google Scholar]
Steed 2010
- Steed L, Newman SP, Hardman SMC. An examination of the self‐regulation model in atrial fibrillation. British Journal of Health Psychology 2010;4(4):337‐47. [DOI: 10.1348/135910799168687] [DOI] [Google Scholar]
Tang 2003
- Tang E, Lai C, Lee K, Wong RSM, Cheng G, Chan TYK. Relationship between patients warfarin knowledge and anticoagulation control. Annals of Pharmacotherapy 2003;37:34‐9. [DOI] [PubMed] [Google Scholar]
Thrall 2004
- Thrall G, Lip GYH, Lane D. Compliance with pharmacological therapy in hypertension: can we do better, and how?. Journal of Human Hypertension 2004;18:595‐7. [DOI] [PubMed] [Google Scholar]
Wallentin 2010
- Wallentin L, Yusuf S, Ezekowitz MD, Alings M, Flather M, Franzosi MG, et al. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: analysis of the RE‐LY trial. Lancet 2010;376(9745):975‐83. [DOI] [PubMed] [Google Scholar]
Ware 1992
- Ware JE, Sherbourne CD. The MOS 36‐Item Short‐Form Health Survey (SF‐36). Medical Care 1992;30(6):473‐83. [PubMed] [Google Scholar]
White 2007
- White HD, Gruber M, Feyzi J, Kaatz S, Tse HF, Husted S, Albers GW. Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulation control: results from SPORTIF III and V. Archives of Internal Medicine 2007;167(3):239‐45. [DOI] [PubMed] [Google Scholar]
Wofford 2008
- Wofford JL, Wells MD, Singh S. Best strategies for patient education about anticoagulation with warfarin: a systematic review. BMC Health Service Research 2008;8:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolf 1991
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22(8):983‐8. [DOI] [PubMed] [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 1983;67:361‐70. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Clarkesmith 2013
- Clarkesmith DE, Pattison HM, Lane DA. Educational and behavioural interventions for anticoagulant therapy in patients with atrial fibrillation. Cochrane Database of Systematic Reviews 2013, Issue 6. [DOI: 10.1002/14651858.CD008600.pub2] [DOI] [PubMed] [Google Scholar]


