Abstract
Background
Aortic valve disease is a common condition that is easily treatable with cardiac surgery. This is conventionally performed by opening the sternum longitudinally down the centre ("median sternotomy") and replacing the valve under cardiopulmonary bypass. Median sternotomy is generally well tolerated, but as less invasive options have become available, the efficacy of limited incisions has been called into question. In particular, the effects of reducing the visibility and surgical access has raised safety concerns with regards to the placement of cannulae, venting of the heart, epicardial wire placement, and de‐airing of the heart at the end of the procedure. These difficulties may increase operating times, affecting outcome. The benefits of smaller incisions are thought to include decreased pain; improved respiratory mechanics; reductions in wound infections, bleeding, and need for transfusion; shorter intensive care stay; better cosmesis; and a quicker return to normal activity.
Objectives
To assess the effects of minimally invasive aortic valve replacement via a limited sternotomy versus conventional aortic valve replacement via median sternotomy in people with aortic valve disease requiring surgical replacement.
Search methods
We performed searches of CENTRAL, MEDLINE, Embase, clinical trials registries, and manufacturers' websites from inception to July 2016, with no language limitations. We reviewed references of identified papers to identify any further studies of relevance.
Selection criteria
Randomised controlled trials comparing aortic valve replacement via a median sternotomy versus aortic valve replacement via a limited sternotomy. We excluded trials that performed other minimally invasive incisions such as mini‐thoracotomies, port access, trans‐apical, trans‐femoral or robotic procedures. Although some well‐conducted prospective and retrospective case‐control and cohort studies exist, these were not included in this review.
Data collection and analysis
Two review authors independently assessed trial papers to extract data, assess quality, and identify risk of bias. A third review author provided arbitration where required. The quality of evidence was determined using the GRADE methodology and results of patient‐relevant outcomes were summarised in a 'Summary of findings' table.
Main results
The review included seven trials with 511 participants. These included adults from centres in Austria, Spain, Italy, Germany, France, and Egypt. We performed 12 comparisons investigating the effects of minimally invasive limited upper hemi‐sternotomy on aortic valve replacement as compared to surgery performed via full median sternotomy.
There was no evidence of any effect of upper hemi‐sternotomy on mortality versus full median sternotomy (risk ratio (RR) 1.01, 95% confidence interval (CI) 0.36 to 2.82; participants = 511; studies = 7; moderate quality). There was no evidence of an increase in cardiopulmonary bypass time with aortic valve replacement performed via an upper hemi‐sternotomy (mean difference (MD) 3.02 minutes, 95% CI ‐4.10 to 10.14; participants = 311; studies = 5; low quality). There was no evidence of an increase in aortic cross‐clamp time (MD 0.95 minutes, 95% CI ‐3.45 to 5.35; participants = 391; studies = 6; low quality). None of the included studies reported major adverse cardiac and cerebrovascular events as a composite end point.
There was no evidence of an effect on length of hospital stay through limited hemi‐sternotomy (MD ‐1.31 days, 95% CI ‐2.63 to 0.01; participants = 297; studies = 5; I2 = 89%; very low quality). Postoperative blood loss was lower in the upper hemi‐sternotomy group (MD ‐158.00 mL, 95% CI ‐303.24 to ‐12.76; participants = 297; studies = 5; moderate quality). The evidence did not support a reduction in deep sternal wound infections (RR 0.71, 95% CI 0.22 to 2.30; participants = 511; studies = 7; moderate quality) or re‐exploration (RR 1.01, 95% CI 0.48 to 2.13; participants = 511; studies = 7; moderate quality). There was no change in pain scores by upper hemi‐sternotomy (standardised mean difference (SMD) ‐0.33, 95% CI ‐0.85 to 0.20; participants = 197; studies = 3; I2 = 70%; very low quality), but there was a small increase in postoperative pulmonary function tests with minimally invasive limited sternotomy (MD 1.98 % predicted FEV1, 95% CI 0.62 to 3.33; participants = 257; studies = 4; I2 = 28%; low quality). There was a small reduction in length of intensive care unit stays as a result of the minimally invasive upper hemi‐sternotomy (MD ‐0.57 days, 95% CI ‐0.93 to ‐0.20; participants = 297; studies = 5; low quality). Postoperative atrial fibrillation was not reduced with minimally invasive aortic valve replacement through limited compared to full sternotomy (RR 0.60, 95% CI 0.07 to 4.89; participants = 240; studies = 3; moderate quality), neither were postoperative ventilation times (MD ‐1.12 hours, 95% CI ‐3.43 to 1.19; participants = 297; studies = 5; low quality). None of the included studies reported cost analyses.
Authors' conclusions
The evidence in this review was assessed as generally low to moderate quality. The study sample sizes were small and underpowered to demonstrate differences in outcomes with low event rates. Clinical heterogeneity both between and within studies is a relatively fixed feature of surgical trials, and this also contributed to the need for caution in interpreting results.
Considering these limitations, there was uncertainty of the effect on mortality or extracorporeal support times with upper hemi‐sternotomy for aortic valve replacement compared to full median sternotomy. The evidence to support a reduction in total hospital length of stay or intensive care stay was low in quality. There was also uncertainty of any difference in the rates of other, secondary outcome measures or adverse events with minimally invasive limited sternotomy approaches to aortic valve replacement.
There appears to be uncertainty between minimally invasive aortic valve replacement via upper hemi‐sternotomy and conventional aortic valve replacement via a full median sternotomy. Before widespread adoption of the minimally invasive approach can be recommended, there is a need for a well‐designed and adequately powered prospective randomised controlled trial. Such a study would benefit from performing a robust cost analysis. Growing patient preference for minimally invasive techniques merits thorough quality‐of‐life analyses to be included as end points, as well as quantitative measures of physiological reserve.
Plain language summary
Heart surgery for aortic valve replacement through a small incision versus the standard full incision at the front of the chest
What question were we trying to answer?
We reviewed the evidence on the effect of a smaller "keyhole"‐type cut (instead of the usual full cut down the breastbone) on aortic valve replacement surgery in adults. We wanted to see if both were as safe and effective as each other.
Why is this important?
The aortic valve prevents blood from flowing backwards from the body back into the heart. Aortic valve disease is a common condition that is treated best with heart surgery. The usual way of performing this is by splitting the entire breastbone lengthways to gain access to the heart, but this is thought to be painful and disruptive. For nearly 20 years, some surgeons have been doing the operation through a smaller hole, cutting part of the breastbone instead of the whole length. Doing it this way makes the scar smaller, but can also make the operation more challenging because it is more difficult to see and reach the heart. This might make the operation longer and less safe, even though it looks smaller from the outside.
Which studies were included in this review?
We checked scientific databases to find published and unpublished studies that compared fully opening the breastbone (called "median sternotomy") for aortic valve replacement against opening just part of the breastbone (called "minimally invasive" or "partial" sternotomy) for the same operation. We searched all records up to July 2016 and found seven studies that answered this question that had 511 participants in them.
How were the studies designed?
The studies came from countries in Europe and North Africa. There were 511 participants, with a mixture of different conditions needing aortic valve replacement. Most of these people were 60 to 70 years old and approximately half were male. The participants in each group were similar. One of the studies was funded by a company that makes equipment for doing minimally invasive surgery.
What did the studies show?
There was no difference between the groups in the number of people who died as a result of having surgery. If 23 out of every 1000 people who had the full‐size cut in their breastbone died after the operation, around 24 (somewhere between eight and 66) in every 1000 would die using the "keyhole" operation. Because that range goes from three times less to three times more, it is difficult to say whether the operation is definitely better or worse.
The amount of time that surgeons needed to use a heart‐lung machine to support the heart while doing the operation was also not different. Neither was the amount of time that the heart was completely stopped to do the operation.
There was little difference in the amount of time participants were on the ventilator or in hospital, although the time spent on the intensive care unit was less by about half a day in the group with the smaller incision. None of the important problems that occur after heart surgery were more common in either group (infections around the heart, irregular heart rhythms or the need for an urgent reoperation because of bleeding). Participants bled slightly less after having minimally invasive surgery. In the operation with the smaller cut, the average blood loss was 158 mL less.
Quality of evidence
The quality of evidence ranged from very low to moderate. One of the main problems with the studies was that they were small and may not have picked up subtle differences between the groups. Because problems after heart surgery are rare, we need to assess lots of people having operations in order to spot small changes. Another problem is that surgeons tend to have lots of slightly different ways in which they do operations. There were also differences in practice, meaning that measurements might not have been taken at the same times, using the same ways. We need to be careful about making conclusions about which differences in the groups in this review were due to the smaller incision and which were due to other factors.
Summary of findings
Summary of findings for the main comparison. Limited upper hemi‐sternotomy versus full median sternotomy for aortic valve replacement.
| Limited upper hemi‐sternotomy versus full median sternotomy for aortic valve replacement | ||||||
| Patient or population: participants requiring aortic valve replacement Setting: cardiac surgical centres Intervention: limited sternotomy Comparison: full sternotomy | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with Full Sternotomy | Risk with Limited Sternotomy | |||||
|
Mortality Follow‐up: in‐patient stay |
Study population | RR 1.01 (0.36 to 2.82) | 511 (7 RCTs) | ⊕⊕⊕⊝ Moderate1 | ‐ | |
| 23 per 1000 | 24 per 1000 (8 to 66) | |||||
| Cardiopulmonary bypass time | The mean cardiopulmonary bypass time ranged from 71 to 107 minutes | The mean cardiopulmonary bypass time in the intervention group was 3.02 minutes more (4.1 fewer to 10.14 more) | ‐ | 311 (5 RCTs) | ⊕⊕⊝⊝ Low2,3 | Cardiopulmonary bypass times tend to have high variability between surgeons according to surgical technique. Differences of up to 15 minutes are unlikely to have clinical significance. |
| Aortic cross‐clamp time | The mean aortic cross‐clamp time ranged from 46 to 72 minutes | The mean aortic cross‐clamp time in the intervention group was 0.95 minutes more (3.45 fewer to 5.35 more) | ‐ | 391 (6 RCTs) | ⊕⊕⊝⊝ Low3,4 | Ischaemic times tend to have high variability between surgeons according to surgical technique. Differences of up to 10 minutes are unlikely to have clinical significance. |
|
Length of hospital stay Follow‐up: in‐patient stay |
The mean length of hospital stay ranged from 6.0 to 9.3 days | The mean length of hospital stay in the intervention group was 1.31 days lower (2.63 lower to 0.01 higher) | ‐ | 297 (5 RCTs) | ⊕⊝⊝⊝ Very low5,6,7 | Expediency of discharge is a quality marker in some healthcare systems, but not universally. |
|
Postoperative blood loss Follow‐up: until removal of operative drains |
The mean postoperative blood loss ranged from 280 mL to 590 mL | The mean postoperative blood loss in the intervention group was 158 mL lower (303 lower to 12 lower) | ‐ | 297 (5 RCTs) | ⊕⊕⊕⊝ Moderate8 | ‐ |
|
Deep sternal wound infection Follow‐up: not specified |
Study population | RR 0.71 (0.22 to 2.30) | 511 (7 RCTs) | ⊕⊕⊕⊝ Moderate1 | ‐ | |
| 23 per 1000 | 17 per 1000 (5 to 54) | |||||
|
Pain scores Follow‐up: 12 hours |
The mean pain scores ranged from 1.2 to 16 standard deviations | The mean pain scores in the intervention group was 0.3 standard deviations fewer (0.85 fewer to 0.2 more) | ‐ | 197 (3 RCTs) | ⊕⊝⊝⊝ Very low7,8,9 | The assessment of pain within and across studies was insufficiently standardised to make strong conclusions about effect on pain |
| Intensive care unit length of stay | The mean intensive care unit stay was 1.4 to 2.1 days | The mean intensive care unit stay in the intervention group was 0.57 days lower (0.93 lower to 0.2 lower) | ‐ | 297 (5 RCTs) | ⊕⊕⊝⊝ Low7,8 | ‐ |
|
Postoperative pulmonary function tests Follow‐up: 5 to 7 days |
The mean pulmonary function tests ranged from 53% to 82% predicted FEV1 | The mean pulmonary function tests in the intervention group was 1.98% predicted FEV1 higher (0.62 higher to 3.33 higher) | ‐ | 257 (4 RCTs) | ⊕⊕⊝⊝ Low7,10 | ‐ |
|
Re‐exploration Follow‐up: in‐patient stay |
Study population | RR 1.01 (0.48 to 2.13) | 511 (7 RCTs) | ⊕⊕⊕⊝ Moderate1 | ‐ | |
| 47 per 1000 | 47 per 1000 (22 to 99) | |||||
|
Postoperative atrial fibrillation Follow‐up: in‐patient stay |
Study population | RR 0.60 (0.07 to 4.89) | 240 (3 RCTs) | ⊕⊕⊝⊝ Low8,11 | ‐ | |
| 175 per 1000 | 105 per 1000 (12 to 856) | |||||
| Postoperative ventilation time | The mean postoperative ventilation time ranged from 5.3 to 13.2 hours | The mean postoperative ventilation time in the intervention group was 1.12 hours lower (3.43 lower to 1.19 higher) | ‐ | 297 (6 RCTs) | ⊕⊝⊝⊝ Very low7,8,11 | ‐ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; FEV1: forced expiratory volume in 1 second; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
1 Downgraded for imprecision: sample size did not meet Optimal Information Size criteria and 95% confidence intervals overlapped no effect. Optimal Information Size estimated at 4600 (to determine 1% difference using α 0.05, β 0.20). Studies all had fewer than 100 participants.
2 Downgraded for imprecision: sample size did not meet Optimal Information Size criteria and 95% confidence intervals overlapped no effect. Optimal Information Size estimated at 120 (to determine 15‐minute difference using α 0.05, β 0.80). Studies all had fewer than 100 participants.
3 Downgraded for inconsistency: use of rapid deployment valves in one study and other variations in surgical technique lead to high heterogeneity.
4 Downgraded for imprecision: sample size did not meet Optimal Information Size criteria and 95% confidence intervals overlapped no effect. Optimal Information Size estimated at 100 (to determine 10‐minute difference in mortality using α 0.05, β 0.80). Studies all had fewer than 100 participants.
5 Downgraded for imprecision: sample size did not meet Optimal Information Size criteria and 95% confidence intervals overlapped no effect. Optimal Information Size estimated at 140 (to determine 1‐day difference using α 0.05, β 0.80). Studies all had fewer than 100 participants.
6 Downgraded for indirectness: length of stay is a surrogate marker of quality and national variations exist in discharge criteria.
7 Downgraded for high risk of bias: outcome measure sensitive to lack of blinding in study.
8 Downgraded for inconsistency: variations in surgical or anaesthetic technique lead to high heterogeneity.
9 Downgraded for indirectness: different measures of pain used across studies.
10 Downgraded for inconsistency: different timing of postsurgical lung function tests across studies lead to high heterogeneity.
11 Downgraded for imprecision: wide 95% confidence intervals overlapping no effect.
Background
Aortic valve disease affects approximately 1% of the adult population in the US and comprises a range of pathologies including senile degeneration and functional regurgitation (Nkomo 2006). Of the 20 million people worldwide estimated to have rheumatic heart disease (Kumar 2013), aortic valve involvement accounts for nearly one‐third of cases (Manjunath 2014). These conditions, spanning stenosis or incompetence of the aortic valve, tend to be progressive, causing angina, breathlessness, and eventually precipitating heart failure and death. Attempts at medical management of the conditions underlying aortic valve disease have not proved fruitful (Coffey 2014; Freeman 2005; Kumar 2013; Scheuble 2005); surgical intervention remains, therefore, the gold standard in treating the condition. Aortic valve surgery has evolved significantly since its inception, such that it can be performed with relatively low mortality; attention is now directed at reducing morbidity.
Description of the condition
Since the mid‐1980s, rheumatic fever, the leading cause of valvular heart disease, has been on the decline in high‐income countries (Rose 1986). In the rest of the world, rheumatic heart disease continues to have a high burden of mortality and morbidity (Carapetis 2005). While it is relatively uncommon in North America (Dare 1993), rheumatic heart disease still represents 22% of valvular heart disease in Europe (Iung 2014). In industrialised nations, senile or degenerative aortic disease typified by aortic stenosis predominates, the incidence of which is increasing in an ageing population. The prevalence of aortic stenosis rises exponentially from the age of 50 years, affecting more than 1 in 50 adults over the age of 75 years (Thaden 2014). Aortic valve disease represents over half of the valvular heart disease in Europe (Iung 2003).
Severe aortic valve disease necessitates surgical intervention for symptomatic relief or prognostic benefit, or both. Previously it was believed that people with severe aortic stenosis maintained a long asymptomatic period with low risk of death (Ross 1968). However, even where symptoms are absent, the outlook is poor for people with severe stenosis; the majority will develop symptoms within five years (Pellikka 2005), and event‐free survival is as low as 21% at two years (Otto 1997). In the SEAS (Simvastatin and Ezetimibe in Aortic Stenosis) study from 2001 to 2004, even in people with mild or moderate aortic stenosis, 10% and 38%, respectively, progressed to surgically significant disease within five years (Gohlke‐Bärwolf 2013). It is thought that the burden of valvular heart disease will continue to increase and that indications for surgery will become broader; at present half of diagnoses of aortic stenosis are made postmortem (d'Arcy 2011).
Description of the intervention
The first total aortic valve replacement was performed in 1958 in a person in whom an attempt at repair caused disintegration of the cusps (Lillehei 1962). In the intervening half‐century, aortic valve repair has grown less common, with replacement with tissue or mechanical prosthetic valves now representing 99% of surgical management of aortic valve disease in the Euro Heart Survey (Iung 2003). It is the second‐most common cardiac surgical procedure in North America (Lee 2011). The prognostic benefit of this operation has been known for many years (Schwarz 1982), and since the early 1980s, the mortality from isolated, uncomplicated aortic valve replacement has dropped more than five‐fold to less than 1% (Carabello 2013). The long‐term freedom from serious complications is similar, even with mechanical valves requiring warfarinisation (Braunwald 2000).
Worldwide aortic valve replacement is most commonly performed via median sternotomy, an incision that extends from the sternal notch to the xiphisternum and divides the entire sternum longitudinally.
Rao and Kumar were the first to describe an aortic valve replacement through a right anterior thoracotomy (Rao 1993). The group used central cannulation and an oblique aortotomy. Subsequently, Cosgrove and Sabik used the term "minimally invasive" to describe an aortic valve procedure via a 10‐cm right anterior thoracotomy, excising the second and third costal cartilages, and employing femoral cannulation to establish cardiopulmonary bypass (CPB) (Cosgrove 1996). Various modifications have since been described, including limited upper hemi‐sternotomy in a J‐shape (Liu 1999a), inverted T‐ or Y‐shape (Cohn 1997), or lazy S (Autschbach 1998). These techniques variably allow access to cannulate the ascending aortic and right atrium ‐ as in open surgery ‐ to establish CPB. Due to the limited access, CPB and aortic cross clamp times may be longer, with theoretical effects on neurological and renal morbidity. Other modifications to the open technique may also be necessary, warranting investment in additional equipment and training (Malaisrie 2014; Walther 2006).
How the intervention might work
Median sternotomy is generally well tolerated due to fixation of the sternum on closure (Lee 2004), but the disruption can nonetheless cause pain and affect respiratory dynamics, reduce mobility, and is thought to necessitate restriction of upper body weight‐bearing (Walther 1999a). Minimally invasive surgery, by virtue of preserving the integrity of the thoracic cage, aims to improve pain, mobility and return to normal activities following discharge (Cohn 1997). These benefits are thought to offset any increase in operative time as a result of reduced surgical access, and therefore potentially reduce cost by up to 20% in all but the people at the highest risk (Cohn 1998). However, these benefits are not guaranteed, as disruption of the intercostal nerves with some approaches might paradoxically cause more pain than that associated with sternotomy (Walther 1999a), and additional port sites or groin cannulation may offset the cosmetic advantage, quality of life or satisfaction (Detter 2002a). Where people have any doubt about the efficacy of a minimally invasive approach, many choose full sternotomy (Ehrlich 2000).
Why it is important to do this review
Aortic valve replacement via full sternotomy is well tolerated and demonstrates excellent long‐term event‐free survival and quality of life. At present, few cardiac surgeons offer minimally invasive aortic valve replacement via limited sternotomy as there is uncertainty whether it offers advantages over conventional aortic valve replacement and there is clinical equipoise. If equivalence in key measures of mortality and morbidity, along with evidence of reduced pain, immobility, length of stay, and overall cost could be demonstrated, there would be momentum to make minimally invasive aortic valve replacement the gold standard. This review sought to evaluate the effect of aortic valve replacement through limited upper hemi‐sternotomy on 30‐day mortality, morbidity, health‐related quality of life, and cost compared with conventional aortic valve replacement through a full median sternotomy in people undergoing aortic valve replacement.
At present, there are no guidelines to either recommend or discourage surgeons from using minimally invasive approaches to aortic valve surgery. Neither the US nor the European guidelines on valvular heart disease make any reference to its use (Nishimura 2014; Vahanian 2012). The Society of Thoracic Surgeons Aortic Valve Guidelines for Management and Quality Measures refers to potential and future benefits of minimally invasive surgery, but makes no specific recommendations (Svensson 2013). The International Society for Minimally Invasive Cardiothoracic Surgery have no consensus guidelines on the subject of minimally invasive aortic valve replacement. As these approaches have been used for nearly two decades, however, it is likely that a dearth of strong evidence influences the decision not to offer recommendations.
Previous meta‐analyses have addressed this subject (Brown 2009; Khoshbin 2011; Murtuza 2008; Phan 2014), but results from a recently reported trial, Borger 2015, necessitates a contemporary review. The earliest of these meta‐analyses was a well‐conducted systematic review that included observational studies in order to address the dearth of randomised controlled studies (Murtuza 2008). However, the technical nature of surgery does not lend itself well to comparison in observational studies. Surgeons and centres that elect to undertake minimally invasive surgery tend to be high‐performing with low complication rates from conventional surgery. Well‐designed randomisation methods are therefore required to minimise the effects of selection biases in surgical studies. Furthermore, three randomised controlled trials have been performed since Murtuza's review (Borger 2015; Calderon 2009; Moustafa 2007), and only two of these were incorporated in subsequent reviews. In addition, the application of Cochrane methodology to the systematic review of the literature and meta‐analysis, including quality scoring, would be of benefit to readers of an updated review.
Objectives
To assess the effects of minimally invasive aortic valve replacement via a limited sternotomy versus conventional aortic valve replacement via median sternotomy in people with aortic valve disease requiring surgical replacement.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomised controlled trials. We included studies reported as full text, those published as abstract only, and unpublished data.
Types of participants
We included adults (aged 18 years or greater) with a diagnosis of aortic valve disease requiring aortic valve replacement.
Types of interventions
We included trials comparing minimally invasive aortic valve surgery through any form of hemi‐sternotomy with conventional, isolated aortic valve surgery via median sternotomy. We did not consider transapical or transfemoral aortic valve replacement, or any minimally invasive procedures performed through thoracotomies, video‐assisted thoracoscopic surgery, or other access not through a partial sternotomy. We considered any modifications to the surgical technique to facilitate this form of access including femoral cannulation, transvenous pacing, and rapid deployment/sutureless valves.
Types of outcome measures
The following were the outcome measures of interest for this study. We did not exclude studies that did not report any of the outcomes of interest, but we did comment on them, in narrative form, in the 'Discussion' section.
Primary outcomes
Mortality (i.e. all‐cause mortality).
Major adverse cardiac or cerebrovascular events (MACCE) (cardiac or cerebrovascular death, myocardial infarction, cardiac arrest, stroke, congestive cardiac failure).
Extracorporeal support times (CPB and aortic cross‐clamp).
Secondary outcomes
Organ failure requiring support (including respiratory, renal, gastrointestinal, or multi‐organ failure).
Length of hospital stay.
Postoperative blood loss.
Deep sternal wound infection.
Pain scores (as measured by visual analogue scale).
Quality of life (as measured by 36‐item Short Form (SF‐36) or any other validated scale).
Cost of surgery.
Intensive care unit length of stay.
Postoperative pulmonary function tests.
Re‐exploration.
Postoperative atrial fibrillation.
Postoperative ventilation times.
Search methods for identification of studies
Electronic searches
We identified trials through systematic searches of the following bibliographic databases on 6 July 2016:
Cochrane Central Register of Controlled Trials (CENTRAL) (2016, Issue 6);
Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, MEDLINE Daily, and MEDLINE (Ovid, 1946 to 6 July 2016);
Embase (Ovid, 1980 to week 27, 2016).
We adapted the preliminary search strategy for MEDLINE (Ovid) for use in the other databases (Appendix 1). We applied the Cochrane sensitivity‐maximising randomised controlled trial filter to MEDLINE (Ovid) and for Embase we applied terms as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011).
We also conducted a search of ClinicalTrials.gov (www.ClinicalTrials.gov), and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) Search Portal (apps.who.int/trialsearch/), which was performed on 28 December 2016.
We searched all databases from their inception and we imposed no restriction on language of publication.
Searching other resources
We checked reference lists of all primary studies and review articles for additional references. We searched relevant manufacturers' websites for trial information (performed in July 2015 and updated in January 2016):
St Jude Medical (professional‐intl.sjm.com/);
Edwards Lifesciences (www.edwards.com/products/mivs/pages/avr.aspx);
Medtronic (www.medtronic.com/for‐healthcare‐professionals/products‐therapies/cardiovascular/index.htm);
On‐X (www.onxlti.com/);
Sorin/LivaNova (www.livanova.sorin.com/).
Where the information from initial screening of papers identified studies with uncertain value for this review, we contacted authors to gain access to missing data.
Data collection and analysis
Selection of studies
Two review authors (BHK, SGJ) independently screened titles and abstracts for inclusion of all the potential studies we identified as a result of the search and coded them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. In case of disagreement, we asked a third review author (SCM) to arbitrate. We retrieved the full‐text study reports/publication, and two review authors (BHK, SGJ) independently screened the full text and identified studies for inclusion, and identified and recorded reasons for exclusion of the ineligible studies. We resolved any disagreements through discussion or, if required, by consulting a third review author (SCM). We identified and excluded duplicates and collated multiple reports of the same study so that each study, rather than each report, was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram and 'Characteristics of excluded studies' table.
Data extraction and management
We used a data collection form for study characteristics and outcome data that had been piloted on at least one study in the review. Two review authors (BHK, SGJ) extracted study characteristics from included studies. We extracted the following study characteristics.
Methods: study design, total duration of study, details of any 'run in' period, number of study centres and location, study setting, withdrawals, and date of study.
Participants: n, mean age, age range, gender, pathophysiology of aortic disease (stenotic or regurgitant), severity of condition, EuroSCORE or Society of Thoracic Surgeons score, left ventricular ejection fraction, prevalence of diabetes, baseline lung function, smoking history, inclusion criteria, and exclusion criteria.
Interventions: intervention including mode of access and modifications to cannulation strategy, comparison group, CPB time, and aortic cross‐clamp time.
Outcomes: primary and secondary outcomes as specified and collected, and time points reported.
Notes: funding for trial and notable conflicts of interest of trial authors.
Two review authors (BHK, SGJ) independently extracted outcome data from included studies. We resolved any disagreements by consensus or by involving a third review author (DC, RJNNW, SCM). One review author (BHK) transferred data into Review Manager 5 (RevMan 2014). We double‐checked that data were entered correctly by comparing the data presented in the systematic review with the study reports. A second review author (SGJ) spot‐checked study characteristics for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (BHK, SGJ) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion or by involving another review author (SCM). We assessed the risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias (e.g. industry funding or small‐study bias).
We graded each potential source of bias as high, low, or unclear risk of bias and provided a quote from the study report together with a justification for our judgement in the 'Risk of bias' table. We summarised the risk of bias judgements across different studies for each of the domains listed. Where information on risk of bias related to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
When considering treatment effects, we took into account the risk of bias for the studies that contributed to that outcome.
Assessment of bias in conducting the systematic review
We conducted the review according to a published protocol and reported any deviations from it in the 'Differences between protocol and review' section of the systematic review.
Measures of treatment effect
We analysed dichotomous data as risk ratios (RR) with 95% confidence intervals (CI). The reason we chose RRs in preference to odds ratios was because they are considered easier to interpret (Higgins 2011), and uniformly presenting data with a consistent presentation would allow simpler comparison of effects on complications or risks of surgery. We analysed continuous data as mean difference (MD) (or standardised mean difference (SMD) if different scales were used for measurement of the same outcome measure) with 95% CIs. We entered data presented as a scale with a consistent direction of effect.
We narratively described skewed data reported as medians and interquartile ranges (IQR).
Unit of analysis issues
We did not anticipate unit of analysis issues as we expected all trials to be parallel design.
Dealing with missing data
We contacted investigators or study sponsors to verify key study characteristics and to obtain missing numerical outcome data where possible (e.g. when a study was identified as abstract only). Where this was not possible, and the missing data were thought to introduce serious bias, we explored the impact of including such studies in the overall assessment of results by a sensitivity analysis.
Assessment of heterogeneity
We used the I2 statistic to measure heterogeneity among the trials in each analysis. Where we identified substantial heterogeneity (I2 greater than 50%), we reported it and explored possible causes.
Assessment of reporting biases
Where we were able to pool more than 10 trials, we planned to create and examine a funnel plot to explore possible small‐study biases for the primary outcomes.
Data synthesis
We undertook meta‐analyses only where this was meaningful: that is if the treatments, participants, and the underlying clinical question were considered similar enough for pooling to make sense.
We used a fixed‐effect model on the assumption that surgical techniques for aortic valve replacement were sufficiently standardised in the key components of the procedure to be comparable. If there was substantial heterogeneity (I2 greater than 50%), we used a random‐effects model for pooling, to account for the small but cumulative differences in surgical technique and aftercare that exist between surgeons and units.
'Summary of findings' table
We created a 'Summary of findings' table for our outcomes. We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to assess the quality of the body of evidence as it related to the studies which contributed data to the meta‐analyses for the prespecified outcomes. We used methods and recommendations described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) using GRADEpro software. We justified all decisions to downgrade or upgrade the quality of studies using footnotes and we made comments to aid readers' understanding of the review where necessary.
Subgroup analysis and investigation of heterogeneity
We did not anticipate performing any subgroup analyses.
Sensitivity analysis
We planned to carry out the following sensitivity analysis: only including studies with a low risk of bias. As none of the included studies were of overall low risk of bias, our final sensitivity analyses were performed by excluding studies evaluated to be at high risk of bias. We also performed a separate sensitivity analysis excluding studies where rapid‐deployment valves were utilised.
Reaching conclusions
We based our conclusions only on findings from the quantitative or narrative synthesis of included studies for this review. We avoided making recommendations for practice, and our implications for research suggested priorities for future research and outlined what the remaining uncertainties are in the area.
Results
Description of studies
Results of the search
We retrieved 203 references through electronic searching of CENTRAL, MEDLINE, and Embase, following de‐duplication. After review of titles and abstracts, 151 references were screened out as not relevant. From the remaining 52 references, 45 studies were excluded following full‐text review (Figure 1).
1.
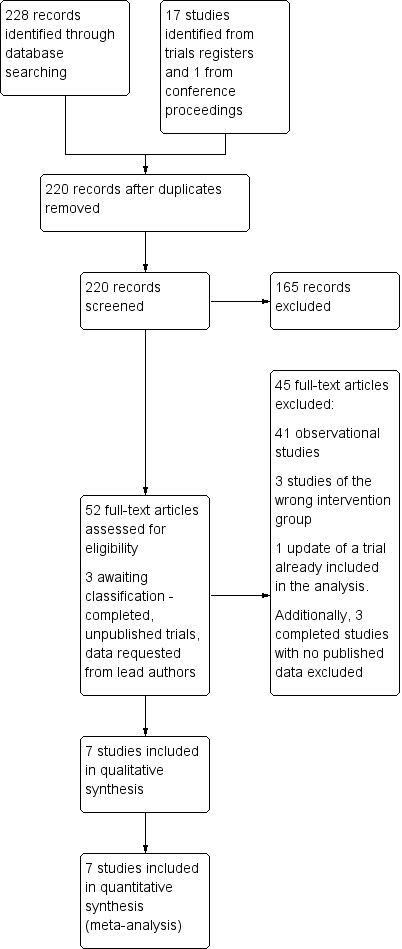
Study flow diagram.
The search for ongoing trials revealed 17 unique studies. Ten were not relevant to the current review, one had been terminated before completion (NCT00221663), one was a proposed long‐term registry (NCT02278666 (SATURNO)) and two were still recruiting (NCT02272621; NCT02726087 (QUALITY‐AVR)). Three were now completed without any published results as yet, although the primary investigators had been contacted (ISRCTN29567910 (MAVRIC); ISRCTN58128724 (MiniStern); NCT01972555 (CMILE)). These were therefore still awaiting classification. One study had been identified in conference proceedings, but excluded as it had not been prospectively randomised.
Included studies
Following the search, screening, and exclusion of irrelevant studies, we identified seven studies that met the inclusion criteria. These seven randomised controlled trials represented 511 participants in studies of between 40 and 120 participants, performed between 1999 and 2015. The studies were performed in Austria (Mächler 1999), Spain (Aris 1999a), Italy (Bonacchi 2002), Germany (Borger 2015; Dogan 2003), France (Calderon 2009), and Egypt (Moustafa 2007). All were undertaken in cardiothoracic surgical settings and only one was a multi‐centre trial, conducted by 12 surgeons across five German centres (Borger 2015).
All seven trials included participants undergoing elective, isolated aortic valve replacement. The majority of studies included both aortic stenosis and aortic regurgitation pathologies except one, which excluded participants with pure aortic regurgitation (Borger 2015). Acute pathology of the aortic valve (i.e. endocarditis), calcified ascending aorta, and other recent potential confounding comorbidities (e.g. myocardial infarction, cerebrovascular accident, significant neurological impairment) were variably described as exclusion criteria, but by definition of the inclusion criteria, all studies were likely to have excluded such participants empirically.
Variations in the participant population may have existed as three studies excluded people with very poor left ventricular ejection fraction under 25% (Bonacchi 2002; Borger 2015; Moustafa 2007). One study excluded participants with moderate left ventricular function under 40% and participants with chronic airway disease or renal impairment (Calderon 2009).
Only one of the studies reported power calculations (Calderon 2009), and four cited the outcome measures a priori in the methods (Aris 1999a; Borger 2015; Calderon 2009; Dogan 2003). All sought institutional ethical approval prior to conduct of the study.
All but one study used reversed L‐shaped upper hemi‐sternotomy as the limited sternotomy; one study used a reversed C‐shaped incision according to anatomy (Bonacchi 2002). For clarity, we will refer to the minimally invasive incision as a limited upper hemi‐sternotomy for the remainder of this review. The surgical technique remained similar between studies, with all employing aortic and right atrial cannulation, rather than femoral cannulation, to institute normothermic or mild hypothermic CPB. Cross‐clamping was exclusively across the ascending aorta and cardioplegia techniques varied in terms of delivery and type. All studies used antegrade, both as root and ostial cardioplegia, but some also gave retrograde cardioplegia for open cases. The choice of cardioplegia solution included blood and crystalloid (both St Thomas' and Bretschneider's solutions).
Choice of prostheses varied across studies. Some studies used exclusively mechanical valves (Aris 1999a; Moustafa 2007, although the former had a single participant exception), whilst others varied the valve choice dependent on participant age. The valve insertion technique was not stipulated in the majority of cases (e.g. interrupted, pledgeted, semi‐continuous, etc.) except for one study which compared rapid deployment balloon expandable stented valves for the mini‐sternotomy arm (Borger 2015). Venting strategies also varied between studies with pulmonary vein, pulmonary artery, aortic root, or no venting used.
Of the primary outcome measures, all studies reported perioperative mortality (as either in‐hospital or 30‐day mortality). Bonacchi 2002 did not provide data for CPB time and Mächler 1999 reported this as median with IQR, precluding it from inclusion in the quantitative analysis. All studies reported aortic cross‐clamp times, but again reported as median and ranges in one study (Mächler 1999), which was therefore excluded from meta‐analysis. None of the studies reported major adverse outcomes as a composite, but all reported major complications. Long‐term follow‐up beyond six months was not described.
The secondary outcome measures for the meta‐analysis were also variably reported. Studies frequently documented organ failure requiring support, but not universally in the outcome tables. All but two study reported total hospital stay (Borger 2015; Mächler 1999), both from Germany where length of stay is not considered a quality marker. Blood loss was described by several different methods which were not universally comparable. Only one study measured quality of life (Borger 2015), and no trials reported a cost analysis. Pulmonary function tests included forced expiratory volume in one second (FEV1) in all studies that reported this outcome.
None of the studies described their protocols for transfusion, return to theatre, discharge from intensive care unit, or discharge from hospital.
This information is summarised in the Characteristics of included studies tables.
Excluded studies
The Characteristics of excluded studies table effectively summarises the reasons for excluding the 45 studies not included in the meta‐analysis. Five studies were not randomised, 35 were observational, and four were not via partial sternotomies (two via thoracotomy, one port access, and one robotic).
Risk of bias in included studies
The risk of bias is summarised in the 'Risk of bias' graph (Figure 2) and 'Risk of bias' summary table (Figure 3). We made overall judgements on the risk of bias per study based on the number of domains assessed as high risk. Due to the nature of studies on surgical incisions, nearly all included studies were at high risk of bias for lack of blinding, but this will have affected the various outcome measures inconsistently (e.g. pain was likely to have been highly influenced by lack of blinding whereas deep sternal wound infection was not). Studies with risk of bias thought to be high that was not related to blinding were therefore considered high risk of bias and excluded in the sensitivity analyses.
2.
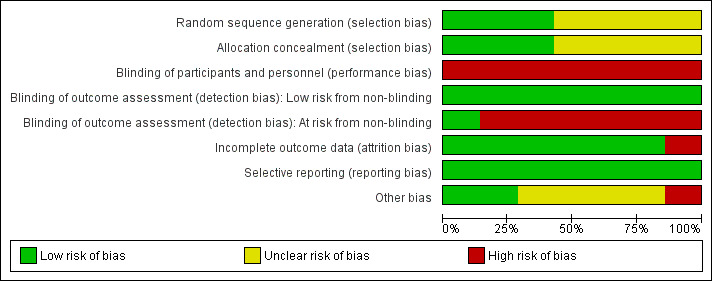
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
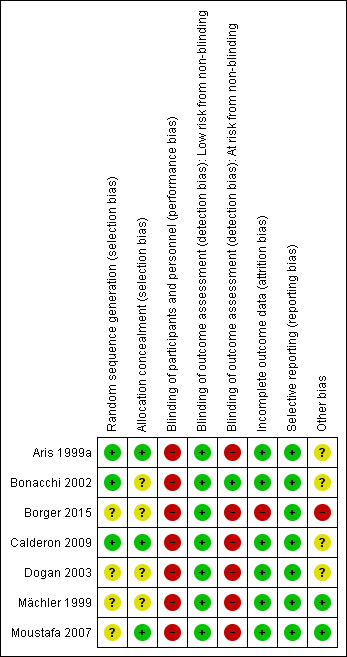
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Three studies used computer‐generated random allocation sequence generation (Aris 1999a; Bonacchi 2002; Calderon 2009); this was unclear in four studies (Borger 2015; Dogan 2003; Mächler 1999; Moustafa 2007). Three studies achieved allocation concealment by sealed enveloped opened at the time of surgery (Aris 1999a; Calderon 2009; Moustafa 2007); this was unspecified for the other four studies.
Blinding
Although blinding of the participants following minimally invasive surgery has previously been described by use of standardised dressings, none of the trials included here employed participant blinding. The surgeons were not blinded in any trial and it was not clear who the outcome assessors were in the majority of trials. Bonacchi 2002 employed blinded outcome assessors for pain score measurements, but not for any of the remaining outcomes. Nonetheless, for several quantifiable outcome measures (e.g. chest tube drainage), lack of blinding should not have significantly affected detection bias.
Incomplete outcome data
The majority of studies reported outcomes on all randomised participants (Aris 1999a; Bonacchi 2002; Calderon 2009; Dogan 2003; Mächler 1999; Moustafa 2007). In one study, there were six withdrawals from the study after randomisation (five in the limited sternotomy and one in the full sternotomy group), and the data were reported for participants who underwent treatment as intended (Borger 2015). Three of the participants in this study were withdrawn because participants randomised to minimally invasive surgery "eventually received a conventional valve because of problems with their anatomy". As such, these participants would have constituted a failure to proceed with intended surgery because of the intervention and would contribute to attrition bias.
Selective reporting
The majority of studies had not widely published a trial protocol citing their intended outcome measures. Aris and colleagues had a protocol approved with their Departmental Research Committee but did not register this with an international registry (Aris 1999a). Bonacchi and coworkers did not describe having a protocol prior to starting the trial (Bonacchi 2002). Borger and colleagues published a protocol (CADENCE‐MIS), but did not report on four prespecified secondary outcome measures (velocity‐time index, left ventricular outflow tract diameter, annular size, or septal thickness) (Borger 2015). Calderon's group had published a protocol with similar characteristics to the published study (NCT00221663), but this was updated as "Terminated ‐ due to slow recruitment" (Calderon 2009). Only one proposed outcome measure from the retracted protocol was not included (cytokine levels from tracheal aspirates). The published study described approval from the local ethics committee. Dogan and colleagues' study was approved by the institutional ethics committee but the protocol not published a priori (Dogan 2003). Mächler and coworkers did not describe a prestudy protocol and Moustafa and colleagues stated that their study had received approval from the protocol research committee at their institution, but did not have a published protocol in a registry (Mächler 1999; Moustafa 2007).
Whilst specific outcomes may have had variable reporting within studies, we adopted an approach of assessing selective reporting bias at a study‐level, in accordance with recommendations from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We considered which outcome measures for aortic valve replacement were important and could be reasonably expected to be reported and found that all studies had included information about the most important measures. We did not downgrade the judgement for Borger and colleagues' study on the basis of the missing variables as we did not consider these to be important clinical measures.
Other potential sources of bias
The minor differences in the surgical techniques between studies was not thought to have contributed a significant risk of bias, although it may have introduced so explicable heterogeneity.
Within studies, one trial had a significant confounding factor in the methodology in that the limited upper hemi‐sternotomy group also received rapid deployment balloon‐expandable valves, whereas the full‐sternotomy group received conventional surgically implanted stented prostheses (Borger 2015). This study was also funded by the manufacturer of the expanding valve.
Four studies did not report detailed demographic differences between the two groups at baseline (Aris 1999a; Bonacchi 2002; Calderon 2009; Dogan 2003), and it is unclear if this may have introduced bias.
Effects of interventions
See: Table 1
The Table 1 provides an overview of the aggregated results of the studies.
Primary outcomes
Mortality
All seven trials reported mortality either as in‐hospital or 30‐day mortality, but zero events in both groups in two trials meant that the effect was not estimable for these studies (Dogan 2003; Moustafa 2007). The overall effect estimate for 511 participants suggested no difference between limited and full sternotomy on perioperative mortality (RR 1.01, 95% CI 0.36 to 2.82; participants = 511; studies = 7; I2 = 0%; quality of evidence = moderate) (Analysis 1.1). A sensitivity analysis, removing two studies at high risk of bias (Borger 2015; Mächler 1999), did not change this outcome (RR 0.64, 95% CI 0.17 to 2.35; participants = 297; studies = 5; I2 = 0%).
1.1. Analysis.
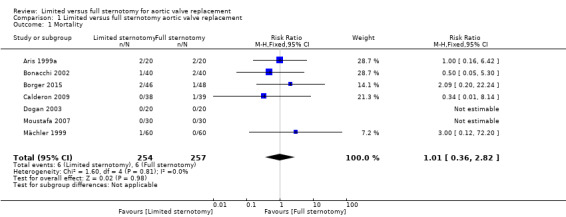
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 1 Mortality.
Major adverse cardiac or cerebrovascular events
None of the included studies reported a composite of MACCE.
Cardiopulmonary bypass time
Five studies reported CPB times in formats that could be pooled (Aris 1999a; Borger 2015; Calderon 2009; Dogan 2003; Moustafa 2007). One study did not cite CPB times but noted that there was no statistically significant difference between the two groups (Bonacchi 2002). Another study provided median CPB times, with IQR, that was not amenable to meta‐analysis (Mächler 1999).
The remainder of the studies showed significant heterogeneity, likely to represent the cumulative effects of intraoperative differences between surgeons, hospitals, and countries. It is unlikely that this clinical heterogeneity can be corrected for by trial methodology, and we therefore elected to use a random‐effects model to mitigate these differences to some degree. As CPB time is such an important surrogate marker of clinical outcome following cardiac surgery, we chose not to exclude this outcome measure completely from quantitative meta‐analysis, but downgraded the quality level of evidence. The overall effect was of no difference (MD 3.02 minutes, 95% CI ‐4.10 to 10.14; participants = 311; studies = 5; I2 = 84%; quality of evidence = low) (Analysis 1.2). Sensitivity analysis performed by exclusion of the study using rapid‐deployment valves in the limited sternotomy arm of the study did not change the results (Borger 2015).
1.2. Analysis.
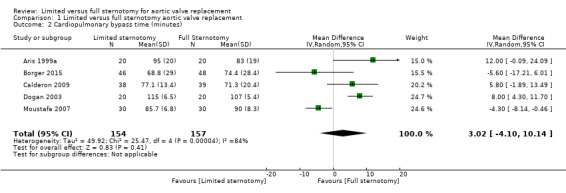
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 2 Cardiopulmonary bypass time (minutes).
Aortic cross‐clamp time
We excluded only one study in the analysis of aortic cross‐clamp times, as data were presented as median and IQR (Mächler 1999). The estimate of effect for the remaining studies suggested no difference in the outcome between limited and full sternotomy (MD 0.95 minutes, 95% CI ‐3.45 to 5.35; participants = 391; studies = 6; I2 = 82%, quality of evidence = low) (Analysis 1.3). Several explanations might exist for the heterogeneity in these studies. Because of variations in the type of aortic pathology across studies, some aortic annuli may have required more extensive decalcification than others. The use of rapid deployment valves in one study may also have affected the clinical heterogeneity (Borger 2015). Borger and colleague used Edwards Intuity rapid deployment valves which do not require aortic decalcification (unlike some other rapid deployment valves) and this will have also contributed to the reduction in aortic cross‐clamp time. As with our meta‐analysis of CPB times, we felt that the clinical importance of this measure warranted quantification with appropriate consideration of reasons for differences across studies. Sensitivity analysis, removing the study by Borger 2015, that may have been biased by the use of rapid‐deployment valves in the minimally invasive group, did not substantially change the overall effect.
1.3. Analysis.
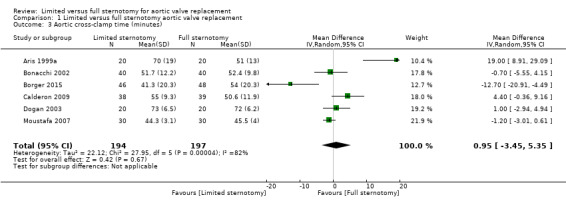
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 3 Aortic cross‐clamp time (minutes).
Secondary outcomes
Organ failure requiring support
No studies reported a composite of multi‐organ failure.
Length of hospital stay
Five studies assessed length of hospital stay following aortic valve replacement via either full or upper hemi‐sternotomy. Aris 1999a, Calderon 2009, and Dogan 2003 had results that clustered around the point of equipoise, with Bonacchi 2002 demonstrating a 95% CI that just fell in favour of surgery via limited hemi‐sternotomy. The study from Egypt showed a much greater advantage of upper hemi‐sternotomy, though the length of stay in the full sternotomy group was substantially higher than other studies (mean stay more than two weeks) (Moustafa 2007). As the discharge criteria for institutions can vary and the mean stay in this study was likely to have been affected by a long‐staying outlier, this may explain the high heterogeneity. The overall estimate of effect almost favoured limited sternotomy (MD ‐1.31 days, 95% CI ‐2.63 to 0.01; participants = 297; studies = 5; I2 = 89%; quality of evidence = very low) (Analysis 1.4). When the study by Moustafa 2007 was excluded, the heterogeneity fell considerably, but the overall effect was still of no difference (MD ‐0.30 days, 95% CI ‐0.67 to 0.08; participants = 237; studies = 4; I2 = 5%).
1.4. Analysis.
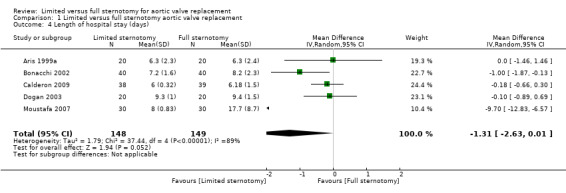
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 4 Length of hospital stay (days).
Postoperative blood loss
There was substantial heterogeneity in the results of the five studies that assessed blood loss in the postoperative period and a random‐effects model was therefore employed. The reasons for this heterogeneity were considered and the benefits of performing a quantitative meta‐analysis weighed. As the total measured blood loss may vary across studies as a result of the type of drainage tubes, haemostatic protocols, and postoperative thromboprophylaxis measures employed, this outcome measure was considered at high risk of clinical heterogeneity across cardiac surgical units. However, minimally invasive procedures are more susceptible to field flooding with small amounts of bleeding, and more meticulous haemostasis is required during dissection, which may have reduced the overall bleeding in this group. In addition, the use of transpleural drains in people undergoing upper hemi‐sternotomies (due to the sub‐xiphoid site being difficult to reach) may have allowed some pericardial bleeding to evacuate into the pleura, thereby reducing the estimated blood loss in this group. All but the oldest study by Aris 1999a demonstrated an advantage in this domain for minimally invasive surgery via limited sternotomy and the cumulative effect was that upper hemi‐sternotomy reduced postoperative bleeding (MD ‐158.00 mL, 95% CI ‐303.24 to ‐12.76; participants = 297; studies = 5; I2 = 93%, quality of evidence = moderate) (Analysis 1.5). No sensitivity analyses were performed for this outcome measure.
1.5. Analysis.
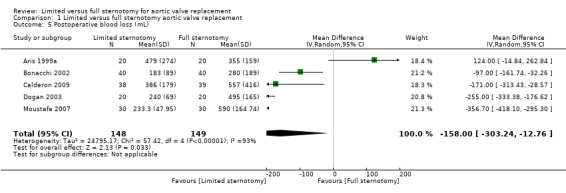
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 5 Postoperative blood loss (mL).
Deep sternal wound infection
All seven studies reported the incidence of postoperative sternal wound infections but only three had any events in either group (Bonacchi 2002; Borger 2015; Mächler 1999), increasing the possibility of a Type II error. The estimate of effect suggested no differences between full or limited sternotomy (RR 0.71, 95% CI 0.22 to 2.30; participants = 511; studies = 7; I2 = 0%, quality of evidence = moderate) (Analysis 1.6), but the wide variation in the effects both within and between studies implied that these were not powered to identify a difference. Sensitivity analyses had no effect on the estimate as removal of the studies by Borger 2015 and Mächler 1999 left only one study with events (Bonacchi 2002) that showed no difference in outcome.
1.6. Analysis.
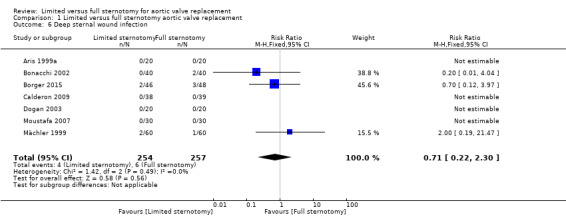
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 6 Deep sternal wound infection.
Pain scores
Three studies described pain scores between the two groups. Bonacchi 2002 used self‐reported pain scores at one and 12 hours measured by nurses blinded to the treatment groups. The figures for 12 hours were compared here. Participants experiencing moderate pain were treated with morphine and non‐steroidal anti‐inflammatory medications. Calderon 2009 employed a 40‐mm visual analogue scale for pain measurements at two days postoperatively. All participants were given paracetamol 1 g every six hours and a morphine patient‐controlled analgesia device to deliver 1‐mg boluses up to every seven minutes. Non‐steroidal analgesia was added to this regimen if participants were still in pain. Unlike the other two studies that reported pain levels, participants in this study reported more pain in the limited sternotomy group than in the full sternotomy group (not reaching statistical significance), but the analgesia usage was also lower in the upper hemi‐sternotomy group. The effects of non‐blinding may have been responsible for this disparity as participants with limited upper hemi‐sternotomy surgery may have felt that they should not require as much analgesia and therefore ended up with higher pain scores. The study by Dogan 2003 also utilised a visual analogue scale to measure pain on the second postoperative day. These were repeated at day five but not included for comparison. The overall estimate of effect using a random‐effects model for the heterogenous data did not show any advantage to surgery via limited upper hemi‐sternotomy (SMD ‐0.33, 95% CI ‐0.85 to 0.20; participants = 197; studies = 3; I2 = 70%; quality of evidence = very low) (Analysis 1.7). There were no sensitivity analyses performed.
1.7. Analysis.
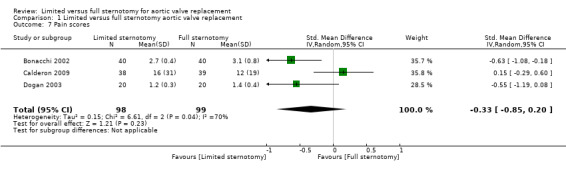
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 7 Pain scores.
Quality of life
Only one study examined quality of life using a validated tool (Borger 2015). There was no difference between full and upper hemi‐sternotomy groups (MD 0.00, 95% CI ‐0.04 to 0.04; participants = 100; studies = 1; I2 = 0%) (Analysis 1.8).
1.8. Analysis.
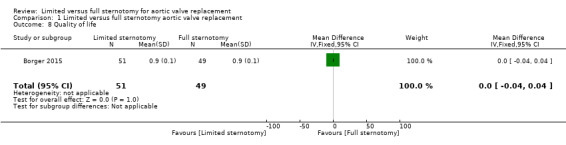
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 8 Quality of life.
Cost of surgery
None of the included studies reported cost analyses.
Intensive care unit length of stay
Five papers described intensive care stay, but due to a small standard deviation in the reporting of one paper (Calderon 2009), the analysis was weighted on the basis of the remaining four studies only (Aris 1999a; Bonacchi 2002; Dogan 2003; Moustafa 2007). All but the oldest (Aris 1999a) demonstrated an advantage of upper hemi‐sternotomy on length of stay in intensive care, though heterogeneity was high. The overall effect was of a reduction in critical care stay for participants undergoing minimally invasive surgery through limited upper hemi‐sternotomy (MD ‐0.57 days, 95% CI ‐0.93 to ‐0.20; participants = 297; studies = 5; I2 = 79%; quality of evidence = low) (Analysis 1.9). Lack of blinding was thought to have a greater influence on intensive care length of stay than some other outcome measures: trial participants undergoing limited sternotomy were likely to have been promoted for discharge from the critical care area in order to facilitate their mobilisation and recovery. In addition, clinical heterogeneity will have been influenced by the differing practices of monitoring and discharge from intensive care across surgical departments. No sensitivity analyses were performed.
1.9. Analysis.
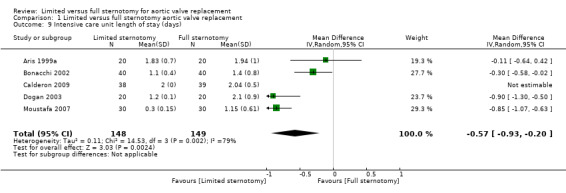
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 9 Intensive care unit length of stay (days).
Postoperative pulmonary function tests
Four papers assessed the effects of aortic valve replacement through limited upper hemi‐sternotomy on lung function, although FEV1 (either as an absolute measurement or as a percentage of predicted) was the only common parameter assessed in all these studies. Aris 1999a performed lung function tests preoperatively and again at discharge, finding a statistically significant drop in lung function following surgery, but no difference in the drop between full and upper hemi‐sternotomy groups. Bonacchi 2002 performed lung function tests at five days postoperatively and again at one to two months. The figures for the fifth postoperative day were included in this comparison. Baseline reference pulmonary function tests were not described. The study by Calderon 2009 included preoperative baseline lung function tests and again at 24 hours', 48 hours', and seven days' postoperatively. The data for day seven were used for the analysis. Moustafa 2007 also performed lung function tests at baseline (preoperative), one week, and one month. The data were not clearly annotated and the variability was assumed to be standard error (rather than standard deviation) due to the small differences and we converted it accordingly. The figures for FEV1 at one week were used in the analysis. Despite the differences in time of measurement, there was relatively little heterogeneity in the studies included and the overall effect was of an increase in FEV1 postoperatively in participants undergoing upper hemi‐sternotomy compared to full sternotomy (MD 1.98 % predicted FEV1, 95% CI 0.62 to 3.33; participants = 257; studies = 4; I2 = 28%; quality of evidence = low) (Analysis 1.10).
1.10. Analysis.
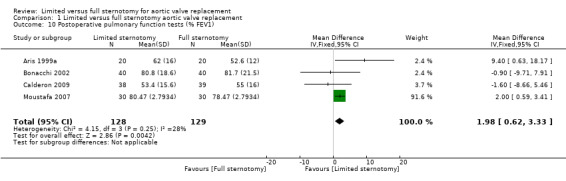
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 10 Postoperative pulmonary function tests (% FEV1).
Re‐exploration
All seven included studies described re‐exploration for bleeding, although one had no events in either group and the effect was therefore not estimable in the analysis (Aris 1999a). The CIs for each of the studies crossed over the line of no effect and therefore the net effect was of no difference between full and upper hemi‐sternotomy (RR 1.01, 95% CI 0.48 to 2.13; participants = 511; studies = 7; I2 = 0%; quality of evidence = moderate) (Analysis 1.11). The effects of a sensitivity analysis (removing Borger 2015 and Mächler 1999, the studies at highest risk of bias) did not change this outcome (RR 0.78, 95% CI 0.30 to 2.04; participants = 297; studies = 5; I2 = 29%).
1.11. Analysis.
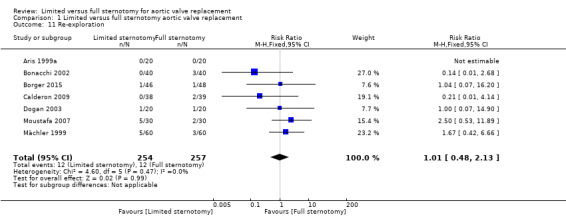
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 11 Re‐exploration.
Postoperative atrial fibrillation
Three studies included data on rates of postoperative atrial fibrillation. Management of atrial fibrillation varies considerably from surgeon to surgeon, with some adopting a prophylactic approach, most treating at onset and pharmacological options being quite wide. This, along with the cannulation strategy, choice of cardioplegia, and degree of atrial manipulation, may explain the heterogeneity in this group. There was no evidence in a combined comparison of an effect on atrial fibrillation by minimally invasive aortic valve replacement through limited hemi‐sternotomy (RR 0.60, 95% CI 0.07 to 4.89; participants = 240; studies = 3; I2 = 79%; quality of evidence = low) (Analysis 1.12). A sensitivity analysis made no change to this overall effect.
1.12. Analysis.
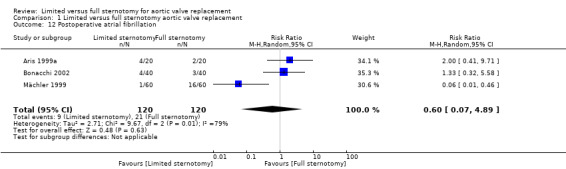
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 12 Postoperative atrial fibrillation.
Postoperative ventilation time
All but one study (Borger 2015) reported length of invasive ventilation postoperatively. The study by Mächler 1999 presented this as median and IQRs and was not included in the quantitative comparison. They found a statistically significant reduction in the postoperative ventilation time in limited compared to full sternotomy (median 7 hours (IQR 5.3 to 11) with limited versus 10 hours (IQR 8.5 to 12) with full, P < 0.0001). The data from the remaining studies were highly heterogeneous and this is likely to have been due to clinical differences in extubation protocols between units. Only one study described their criteria for extubation (Bonacchi 2002). The overall estimate of effect was of no difference (MD ‐1.12 hours, 95% CI ‐3.43 to 1.19; participants = 297; studies = 5; I2 = 97%; quality of evidence = very low) (Analysis 1.13). Making the assumption that the study by Mächler 1999 had presented normally distributed data as median and IQRs and making an approximated conversion did not change the overall effect (Section 7.7.3.5, Cochrane Handbook for Systematic Reviews of Interventions; Higgins 2011).
1.13. Analysis.
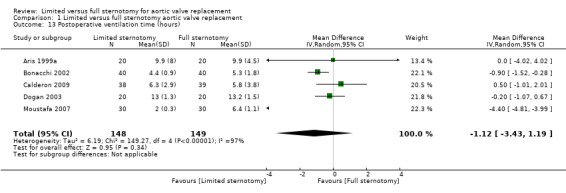
Comparison 1 Limited versus full sternotomy aortic valve replacement, Outcome 13 Postoperative ventilation time (hours).
Discussion
Summary of main results
This systematic review assessed the effects of full versus limited sternotomy on mortality, CPB time, aortic cross‐clamp time, length of hospital and intensive care unit stay, postoperative blood loss, deep sternal wound infection, pain scores, quality of life measures, pulmonary function tests, re‐exploration for bleeding, postoperative atrial fibrillation, and ventilation times. We found seven randomised controlled trials with 511 participants that answered the study question, which were generally of low‐to‐moderate quality of evidence. Some of the outcome measures were of very low quality evidence. The inherent difficulties of blinding surgical access, relatively small study sizes (and corresponding failure to meet Optimal Information Size criteria), and clinically heterogeneous populations were the main reasons for downgrading quality of evidence.
All the identified studies used upper hemi‐sternotomy as the mode of limited sternotomy. Meta‐analysis found no evidence of survival benefit, or increase in risk, with minimally invasive surgery via limited upper hemi‐sternotomy. This correlates with other, recent literature (Phan 2014). The wide CIs of the studies, including the null‐events in two of the studies demonstrate that few of these studies were powered to demonstrate differences in perioperative mortality and the aggregate effect did not cross the Optimal Information Size criteria either.
There were no treatment effects for extracorporeal support and ischaemic times between the two groups. The oldest study showed the largest difference between full and minimally invasive surgery with a significant disadvantage to performing limited sternotomy (Aris 1999a), but this was less apparent in subsequent trials, presumably as a result of the technique being refined. In one trial, the use of rapid deployment valves meant that the disadvantage of limited sternotomy on operative times was negated (Borger 2015). In fact, the advantage conferred by these valves meant that operative times were uniquely shorter for the limited sternotomy cohort in this trial. This may have confounded the comparison between the two groups and the authors acknowledged this in their discussion. Removing the study for sensitivity analysis, however, did not change the estimate of effect, which remained equivalent between the two groups.
Length of hospital stay was no shorter with minimally invasive surgery via limited sternotomy, although the effect bordered on significance. As enhanced recovery programmes and expedited discharge plans become more commonplace, even for major operations, this is expected. The analysis showed an advantage, however, in the reduction of intensive care unit stay with limited sternotomy. It was unclear why this occurred, however, as there were no differences in surgical times, pain scores, respiratory function, rates of atrial fibrillation, or return to theatre for bleeding between the two groups. A number of the studies included also described ventilator time in their outcomes, and these too showed no overall difference between limited or full sternotomy. This raises the possibility of unblinded minimally invasive patients with limited sternotomies being expedited out of the critical care unit.
Overall completeness and applicability of evidence
All the studies included in this systematic review directly addressed the review question and allowed meta‐analyses on a variety of outcome measures. The trial populations seemed to be representative of the people who might undergo aortic valve replacements, including people with aortic regurgitation and aortic stenosis. People at high risk from cardiac surgery were typically excluded (e.g. people with need for multiple or complex procedures or people with left ventricular impairment) and in the present climate, such people would not be eligible for minimally invasive surgery in any case. The surgical techniques appeared to be consistent with current practice in aortic valve implantation, with a combination of mechanical and tissue prosthetic valves implanted. One study used aprotinin routinely (Aris 1999a), which was in the interim withdrawn by the manufacturers because of an increased risk of mortality. This suspension was lifted in 2012. All studies employed aorto‐atrial CPB unless exposure dictated femoral cannulation necessary. As such, the techniques employed appeared to be relevant to modern practice, although clinically heterogeneous.
One study had an overall mortality of 10% for uncomplicated isolated aortic valve replacements via either approach (Aris 1999a). The remainder of the studies appeared to have mortality rates consistent with the expected rates for selected participants. CPB times and aortic cross‐clamp times appeared to be consistent with expected operating times. The remainder of the outcome measures in the conventional approach (full sternotomy) group appeared to correlate with equivalent data in the literature, suggesting that in all studies, the operating surgeons had already passed their learning curves for the procedures.
Quality of the evidence
This meta‐analysis represented 511 participants in seven randomised controlled studies. Most of the studies were underpowered to identify differences in the outcome measures cited. The overall quality of the evidence was low. The Table 1 demonstrated the main factors affecting quality within and between studies.
Limitations in study design and implementation
Four studies described adequate control of sequence generation and allocation concealment using computerised systems and envelopes. Blinding was not performed in any study with the exception of pain scores in the paper by Bonacchi 2002. There was no evidence of selective outcome reporting of important outcome measures, but only one study had a pretrial protocol published in an international registry (Borger 2015). This study presented data in a per‐protocol analysis rather than intention‐to‐treat. Participants who dropped out of particular arms of the study could represent failure of the procedure in that case (especially for minimally invasive approaches where the intended valve could not be deployed). The follow‐up was complete in all cases.
Indirectness of evidence
In general, there was no serious concerns of systematic bias as a result of indirectness. Two outcome measures were downgraded on quality of evidence for indirect measures. Pain was measured on a number of different scales across studies. Length of stay was also considered a poor surrogate marker of surgical outcome as different healthcare systems have different philosophies on discharging from hospital: some consider an expedited discharge an indication of participant well‐being, whereas others do not construe early discharge in this way.
Unexplained heterogeneity or inconsistency of results
Eight of the outcome measures that were amenable to quantitative analysis showed substantial heterogeneity. The individual reasons for these have been explored in the discussions for each outcome, but broadly can be attributed to the array of surgical and postoperative differences in practice across departments. Many of these cumulative, minor differences in practice were not protocolised or described in the studies and will have contributed to the clinical heterogeneity in this study. In addition, the use of a novel rapid deployment valve in the minimally invasive arm of one study introduced further heterogeneity in the results (Borger 2015), and this has been elaborated on elsewhere. Inclusion and exclusion criteria were broadly similar, but the variation in aortic valve pathology across studies may have introduced differences in operating times (due to the need for annular decalcification in stenotic valves) and different risk profiles (absence of calcium deposition in the aortic root may reduce the risk of neurological complications). The absence of clear protocols for transfusion, discharge from intensive care unit, discharge from hospital, and return to theatre may also have caused differences in outcome measures, but this should have been standardised between groups within studies. One study had within‐study differences of pain control according to which measure was used (visual analogue scale of self‐reported pain versus total dose of morphine delivered via patient‐controlled analgesia), confirming that surrogate markers may not always be reliable indicators (Calderon 2009).
Imprecision of results
The studies were all underpowered according to Optimal Information Size to measure mortality, deep sternal wound infection, and re‐exploration for bleeding. The details of this calculation are outlined in the footnotes of the Table 1.
Publication bias
A number of randomised controlled trials that had been registered but not completed may reflect attempts to perform aortic valve replacement via minimally invasive approaches that were deemed unsuccessful. There may, therefore, be some potential for publication bias if centres that have demonstrated poor results have terminated their programmes or failed to publish their results.
Potential biases in the review process
Two of the review authors have practices that include minimally invasive aortic valve replacement and one of the review authors consults for a manufacturer of minimally invasive surgical equipment. However, the literature search, review and analysis has been performed in a transparent and reproducible manner. This should have reduced any risk of bias in this review.
We had a number of postprotocol changes to the review methodology which might indicate a bias in the process resulting from prior knowledge of the findings. Several outcome measures were added following aggregation of data: these were not known to us at the time of writing the protocol and we do not believe this could have been foreseen.
Agreements and disagreements with other studies or reviews
One large meta‐analysis incorporating randomised controlled trials, propensity matched studies, and observational studies, found similar outcomes to this review (Phan 2014). They found a significant reduction in perioperative mortality for minimally invasive aortic value replacement (including but not exclusive to upper hemi‐sternotomy), but in subgroup analysis, this difference was only evident in the non‐randomised studies. Similarly, the differences in cross‐clamp and CPB times were significant only when randomised trials were excluded. With more recent studies, both mortality and operative times came closer to each other in both groups, suggesting an early learning curve to minimally invasive surgery. For other outcome measures, Phan and colleagues aggregated mini‐sternotomy and mini‐thoracotomy approaches to aortic value replacement and the comparisons are therefore not applicable for a comparison of limited versus full sternotomy.
Our findings correlated with the trend in the literature: that minimally invasive aortic valve surgery via limited upper hemi‐sternotomy can be performed at least as safely as conventional surgery via a full sternotomy. We did not identify reduction in pain as a result of less‐invasive approaches, but did find a reduction in intensive care stay and a trend towards reduction in hospital stay.
Authors' conclusions
Implications for practice.
Our review demonstrates no increase in mortality or serious morbidity with minimally invasive aortic valve replacement through limited upper hemi‐sternotomy. Concerns about the effects of longer cardiopulmonary bypass and cross‐clamp times appear to be unfounded, as increasing experience in limited sternotomy has brought these in line with extracorporeal support times with full sternotomy. There are potential benefits in postoperative bleeding rates, intensive care unit stay, and hospital length of stay. Benefits in pain relief, pulmonary function, and deep sternal wound infection rate have not been realised. This would suggest that limited‐sternotomy access is a viable and effective approach for aortic valve replacement.
Implications for research.
One significant potential improvement to future research in this field might include blinding of participants and outcome assessors using standardised dressings and a postoperative care team blinded to the approach. In this way, while the operating team would know what surgery had been performed, those making outcome assessments would not.
In addition, future trials would benefit from performing a priori sample size calculations and considering follow‐up of participants beyond discharge. In particular, return to activities of daily living or quality of life assessments to determine the mid‐term benefits (three months or more) of minimally invasive approaches such as limited upper hemi‐sternotomy would aid future decision making. Bypass and cross‐clamp times are reliable indices of the complexity of an isolated aortic valve procedure and correlate well with clinical outcomes and learning curves. In minimally invasive procedures, however, the surgical time from skin incision to skin closure can also be increased, as developing access and maintaining meticulous haemostasis are more crucial. Recording this surgical skin‐to‐skin time in future studies may, therefore, provide a reliable index of the progress of the procedures.
The most recent trial in this field compared minimally invasive aortic valve replacement using rapid deployment valves through a limited hemi‐sternotomy against conventional surgically implanted prostheses in full sternotomy. The authors of that trial argued that rapid deployment valves were a natural evolution of the minimally invasive procedure, designed to offset the increase in CPB and aortic cross‐clamp times seen in previous studies. While modifications to the technique are certainly required in order to facilitate minimally invasive approaches, the use of expanding stented valves may be too great a confounder. Future trials, therefore, might benefit from predetermined valve types to be used in both arms.
Acknowledgements
We are indebted to Nicole Martin and Cochrane Heart Group Information Specialist for her invaluable advice in formulating the search strategy and in providing timely and pragmatic advice on all aspects of the review process.
Appendices
Appendix 1. Search strategies
CENTRAL
#1 MeSH descriptor: [Aortic Valve] this term only
#2 (aortic valve* near/3 (operation* or replace* or surgery)):ti,ab,kw
#3 #1 or #2
#4 MeSH descriptor: [Minimally Invasive Surgical Procedures] this term only
#5 MeSH descriptor: [Robotics] this term only
#6 MeSH descriptor: [Thoracoscopy] explode all trees
#7 MeSH descriptor: [Sternotomy] this term only
#8 minim* invasiv*:ti,ab,kw
#9 ((surgical or surgery or surgeries or replacement* or operation*) near/3 minim*):ti,ab,kw
#10 ((surgery or surgeries or surgical) near/3 (keyhole or percutaneous or robot‐assisted)):ti,ab,kw
#11 thoracoscop*:ti,ab,kw
#12 pleuroscop*:ti,ab,kw
#13 ("hemi‐sternotomy" or "mini‐sternotomy"):ti,ab,kw
#14 #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13
#15 #3 and #14
MEDLINE Ovid
1. Aortic Valve/
2. (aortic valve* adj3 (operation* or replace* or surgery)).tw.
3. 1 or 2
4. Surgical Procedures, Minimally Invasive/
5. Robotics/
6. Thoracoscopy/
7. Sternotomy/
8. minim* invasiv*.tw.
9. ((surgical or surgery or surgeries or replacement* or operation*) adj3 minim*).tw.
10. ((surgery or surgeries or surgical) adj3 (keyhole or percutaneous or robot‐assisted)).tw.
11. thoracoscop*.tw.
12. pleuroscop*.tw.
13. ("hemi‐sternotomy" or "mini‐sternotomy").tw.
14. or/4‐13
15. 3 and 14
16. exp animals/ not humans.sh.
17. 15 not 16
18. randomized controlled trial.pt.
19. controlled clinical trial.pt.
20. randomized.ab.
21. placebo.ab.
22. drug therapy.fs.
23. randomly.ab.
24. trial.ab.
25. groups.ab.
26. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25
27. exp animals/ not humans.sh.
28. 26 not 27
29. 17 and 28
Embase Ovid
1. Aorta Valve/
2. (aortic valve* adj3 (operation* or replace* or surgery)).tw.
3. 1 or 2
4. Minimally Invasive Surgery/
5. Robotics/
6. Thoracoscopy/
7. Sternotomy/
8. minim* invasiv*.tw.
9. ((surgical or surgery or surgeries or replacement* or operation*) adj3 minim*).tw.
10. ((surgery or surgeries or surgical) adj3 (keyhole or percutaneous or robot‐assisted)).tw.
11. thoracoscop*.tw.
12. pleuroscop*.tw.
13. ("hemi‐sternotomy" or "mini‐sternotomy").tw.
14. or/4‐13
15. 3 and 14
16. exp animals/ not humans.sh.
17. 15 not 16
18. random$.tw.
19. factorial$.tw.
20. crossover$.tw.
21. cross over$.tw.
22. cross‐over$.tw.
23. placebo$.tw.
24. (doubl$ adj blind$).tw.
25. (singl$ adj blind$).tw.
26. assign$.tw.
27. allocat$.tw.
28. volunteer$.tw.
29. crossover procedure/
30. double blind procedure/
31. randomized controlled trial/
32. single blind procedure/
33. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32
34. (animal/ or nonhuman/) not human/
35. 33 not 34
36. 17 and 35
Clinicaltrials.gov
"aortic valve" AND ("minimally invasive" OR "hemi‐sternotomy" OR "mini‐sternotomy")
WHO International Clinical Trials Registry Platform
"aortic valve" AND ("minimally invasive" OR "hemi‐sternotomy" OR "mini‐sternotomy")
Data and analyses
Comparison 1. Limited versus full sternotomy aortic valve replacement.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality | 7 | 511 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.36, 2.82] |
| 2 Cardiopulmonary bypass time (minutes) | 5 | 311 | Mean Difference (IV, Random, 95% CI) | 3.02 [‐4.10, 10.14] |
| 3 Aortic cross‐clamp time (minutes) | 6 | 391 | Mean Difference (IV, Random, 95% CI) | 0.95 [‐3.45, 5.35] |
| 4 Length of hospital stay (days) | 5 | 297 | Mean Difference (IV, Random, 95% CI) | ‐1.31 [‐2.63, 0.01] |
| 5 Postoperative blood loss (mL) | 5 | 297 | Mean Difference (IV, Random, 95% CI) | ‐158.00 [‐303.24, ‐12.76] |
| 6 Deep sternal wound infection | 7 | 511 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.22, 2.30] |
| 7 Pain scores | 3 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.85, 0.20] |
| 8 Quality of life | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.04, 0.04] |
| 9 Intensive care unit length of stay (days) | 5 | 297 | Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐0.93, ‐0.20] |
| 10 Postoperative pulmonary function tests (% FEV1) | 4 | 257 | Mean Difference (IV, Fixed, 95% CI) | 1.98 [0.62, 3.33] |
| 11 Re‐exploration | 7 | 511 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.48, 2.13] |
| 12 Postoperative atrial fibrillation | 3 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.07, 4.89] |
| 13 Postoperative ventilation time (hours) | 5 | 297 | Mean Difference (IV, Random, 95% CI) | ‐1.12 [‐3.43, 1.19] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Aris 1999a.
| Methods |
Study design: prospective randomised controlled study Duration: 4 months No. of centres: single Location: Spain Setting: cardiac surgical centre Withdrawals: none Dates: not stated |
|
| Participants | 40 consecutive participants undergoing first‐time elective isolated aortic valve replacement. Exclusion criteria: none Demographics [limited / full sternotomy] Number of participants: 40 [20 / 20] Mean age (± SD) (range): 64 ± 11 years (26 to 76 years) Gender: not stated Pathophysiology: 31 AS, 9 AR Severity of disease: not stated Mean risk score: [11.6 ± 5.0 / 11.4 ± 5.5] Mean left ventricular ejection fraction: [62.3 ± 11 / 64.9 ± 13] Diabetes mellitus: not stated Preoperative lung function % predicted FEV1 : [79 ± 14 / 81 ± 21] Preoperative lung function % predicted FVC: [79 ± 14 / 80 ± 20] Smoking status: not stated |
|
| Interventions |
Limited sternotomy: reversed L‐ or reversed J‐shaped mini‐sternotomy Modifications from full sternotomy: none stated |
|
| Outcomes |
Primary outcomes: cross‐clamp and pump times, time to extubation, chest drainage (24 hours), number of blood transfusions, ICU stay, and total postoperative length of stay Secondary outcomes: pain scores (daily) and cosmetic evaluation (discharge) Other reported outcomes: none |
|
| Standard care | Standard care was aortic and right atrial cannulation, aprotinin, antegrade cold blood cardioplegia (through coronary ostia), and no left ventricular vent. Mechanical prostheses in most participants. No transoesophageal echocardiography. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Low risk | Envelope opened at time of surgery |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Blinding of outcome assessment (detection bias) Low risk from non‐blinding | Low risk | Mortality, blood loss, deep sternal wound infection, re‐exploration, and postoperative atrial fibrillation rates were unlikely to be affected by absence of blinding. |
| Blinding of outcome assessment (detection bias) At risk from non‐blinding | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence of loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Relevant outcome measures reported |
| Other bias | Unclear risk | Limited description of preoperative participant demographics |
Bonacchi 2002.
| Methods |
Study design: prospective randomised controlled study Duration: 2 years No. of centres: single Location: Italy Setting: cardiac surgery centre Withdrawals: none Dates: January 1999 to July 2001 |
|
| Participants | 80 consecutive participants with aortic valve pathology undergoing elective aortic valve replacement. Exclusion criteria: emergent surgery, concomitant coronary revascularisation, left ventricular ejection fraction < 25% or heavily calcified aorta Demographics [limited / full sternotomy] Number of participants: 80 [40/40] Mean age (± SD): [62.6 ± 9.5 years / 64 ± 12.4 years] Gender: not stated Pathophysiology (AS:AR:mixed): [12:8:20 / 10:7:23] Severity of disease (NYHA status): [2.7 ± 0.9 / 2.5 ± 0.7] Mean risk score: not stated Mean left ventricular ejection fraction: [57 ± 12 / 56 ± 13] Diabetes mellitus: not stated Preoperative lung function: not stated Smoking status: not stated |
|
| Interventions |
Limited sternotomy: reversed C‐ or reversed L‐shaped sternal incision with < 10‐cm skin incision Modifications from full sternotomy: none stated |
|
| Outcomes |
Primary outcomes: not stated Secondary outcomes: not stated Other reported outcomes: in‐hospital death, re‐exploration for bleeding, mean mediastinal drainage or bleeding > 800 mL, blood transfusion, atrial fibrillation, atelectasis, respiratory insufficiency, sternal wound infection, sternal instability, mechanical ventilation time, oxygen requirements (pre‐ and postextubation), pain scores (1 and 12 hours), analgesia requirements, ICU stay, hospital stay, spirometry (5 days and 1 to 2 months) (follow‐up time in parentheses) |
|
| Standard care | Standard care was normothermic CPB and aortic cross‐clamping with aortic and right atrial 2‐stage venous cannulation. Retrograde and ostial antegrade cold blood cardioplegia were given. A right superior pulmonary vent was used in all cases. Transverse or oblique aortotomies were utilised depending on valve choice rather than surgical approach. Transoesophageal echocardiography was employed in all cases. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) Low risk from non‐blinding | Low risk | Mortality, blood loss, deep sternal wound infection, re‐exploration, and postoperative atrial fibrillation rates are unlikely to be affected by absence of blinding. |
| Blinding of outcome assessment (detection bias) At risk from non‐blinding | Low risk | Participants and staff blinded to surgical incision |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants reported on |
| Selective reporting (reporting bias) | Low risk | Relevant outcome measures reported |
| Other bias | Unclear risk | Limited description of preoperative participant characteristics |
Borger 2015.
| Methods |
Study design: prospective randomised controlled study Duration: 9 months No. of centres: 5 centres Location: Germany Setting: cardiac surgical centres Withdrawals: 6 (5 in minimally invasive group, 1 in full sternotomy group) Dates: May 2012 to Feb 2013 |
|
| Participants | 100 participants with AS in 5 German centres. Inclusion criteria: logistic EuroSCORE < 20, NYHA ≥ 2 Exclusion criteria: pure AR, previous cardiac surgery, congenital true bicuspid valve (Sievers type 0), emergency surgery, left ventricular ejection fraction < 25%, recent myocardial infarction (≤ 90 days), or stroke or TIA ≤ 6 months Demographics [limited / full sternotomy] Number of participants: 100 randomised [46 / 48]; 6 dropouts: 1 randomised to full sternotomy withdrew; 5 randomised to minimally invasive surgery were unable to have the procedure Mean age (± SD): [73.0 ± 5.3 years / 74.2 ± 5.0 years] Male gender: [27 (58.7%) / 21 (43.7%)] Pathophysiology: AS with or without aortic insufficiency Severity of disease (NYHA ≥ III): [31 (67.4%) / 29 (60.4%)] Mean STS risk score: [1.6 ± 0.7 / 1.7 ± 0.6] Mean left ventricular ejection fraction: not stated Diabetes mellitus: [15 (32.6%) / 11 (22.9%)] Preoperative COPD: [6 (13.0%) / 7 (14.9%)] Smoking status: [22 (47.8%) / 12 (25.5%)] |
|
| Interventions |
Limited sternotomy: upper hemi‐sternotomy into 3rd or 4th intercostal space. Modifications from full sternotomy: percutaneous femoral venous cannulation if right atrial cannulation not possible. Use of rapid deployment aortic valve prosthesis ‐ Edwards Intuity valve (a stented, trileaflet bovine pericardial bioprosthesis with a balloon‐expandable cloth covered skirt frame). |
|
| Outcomes |
Primary outcomes: cross‐clamp and CPB time Secondary outcomes: haemodynamic performance, quality of life (EQ‐5D), NYHA class Safety outcomes: cardiac reoperation, thromboembolism, renal failure, paravalvular leak, permanent pacemaker insertion, resternotomy, major bleeding events, endocarditis, myocardial infarction, deep sternal wound infection, cerebrovascular accident, respiratory failure |
|
| Standard care | Standard care was full sternotomy with ascending aortic and right atrial cannulation. Normothermic or mild hypothermic CPB with antegrade crystalloid, cold or warm blood cardioplegia was given. Transverse aortotomies were employed in all cases. CO2 field flooding was used. In all full‐sternotomy participants, the valve choices were conventional stented valves. | |
| Notes | Disclosure: sponsored by Edwards Lifesciences LLC. Manuscript facilitated by Edwards Lifesciences | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) Low risk from non‐blinding | Low risk | Mortality, blood loss, deep sternal wound infection, re‐exploration, and postoperative atrial fibrillation rates were unlikely to be affected by absence of blinding. |
| Blinding of outcome assessment (detection bias) At risk from non‐blinding | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | High risk |
Quote: "three [patients] who were randomized to MIS‐RADVR [minimally invasive surgical rapid‐deployment aortic valve replacement] eventually received a conventional valve because of problems with their anatomy". Comment: these participants appeared to have been excluded following randomisation and an intention‐to‐treat analysis may have identified difficulty with the minimally invasive approach. |
| Selective reporting (reporting bias) | Low risk | Relevant outcome measures reported. 4 secondary outcome measures described in pretrial protocol were not described in the final study publication, but these were not considered clinically important measures. |
| Other bias | High risk | Significant confounder as mini‐sternotomy utilised rapid‐deployment valve and full‐sternotomy employed standard surgical valves. Study funded by manufacturer. |
Calderon 2009.
| Methods |
Study design: prospective randomised controlled study Duration: 4 years No. of centres: single Location: France Setting: university hospital Withdrawals: 1 from full sternotomy group Dates: 2003 to 2007 |
|
| Participants | 78 participants undergoing aortic valve replacement for stenotic, regurgitant, or mixed aortic valve disease by a single surgeon Inclusion criteria: adults, ASA grade ≤ 3, informed consent, left ventricular ejection fraction > 40% Exclusion criteria: redo, combined surgery, ASA ≥ 4, acute pulmonary oedema, COPD, endocarditis, chronic renal failure, antiplatelet use < 7 days before surgery, haemostatic abnormality Demographics [limited / full sternotomy] Number of participants: 78 randomised [38 / 39] Mean age (± SD): [70.9 ± 11.4 years / 70.8 ± 10.2 years] Male gender: [23 (60.5%) / 27 (69.2%)] Pathophysiology: 75% AS, 24% AR, 1% mixed Severity of disease: not stated Mean risk score: [5.4 ± 1.9 / 5.2 ± 1.8] Left ventricular ejection fraction > 50%: [36 (94.7%) / 34 (87.2%)] Diabetes mellitus: not stated Preoperative % predicted FEV1 : [73.9 ± 18.2 / 78.8 ± 21] Preoperative % predicted FVC: [81.1 ± 16.1 / 83.6 ± 19.4] Smoking status: not stated |
|
| Interventions |
Limited sternotomy: minimal sternotomy access via 6‐ to 10‐cm mid‐line skin incision and reversed L sternal incision Modifications from full sternotomy: none |
|
| Outcomes |
Primary outcomes: respiratory parameters Secondary outcomes: bleeding, transfusion, and pain status Other reported outcomes: intraoperative and postoperative blood loss, transfusion rates, CPB and cross‐clamp times, operation time, mechanical ventilation time, ICU stay, hospital stay, systemic inflammatory response syndrome, re‐exploration for bleeding, death, spirometry (1, 2, and 7 days), pain scores, cardiac output studies (follow‐up time in parentheses) |
|
| Standard care | Standard care included routine anaesthesia, aprotinin prophylaxis, right atrial appendage and ascending aortic cannulation, and Bretschneider's cardioplegia solution. Aortic root vent only was employed. | |
| Notes | Funding: French Ministry of Health | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 1:1 computer generated 6‐per‐block randomisation, designed by a statistician. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Blinding of outcome assessment (detection bias) Low risk from non‐blinding | Low risk | Mortality, blood loss, deep sternal wound infection, re‐exploration, and postoperative atrial fibrillation rates are unlikely to be affected by absence of blinding. |
| Blinding of outcome assessment (detection bias) At risk from non‐blinding | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants reported |
| Selective reporting (reporting bias) | Low risk | All relevant outcome measures reported |
| Other bias | Unclear risk | Limited description of preoperative participant characteristics |
Dogan 2003.
| Methods |
Study design: prospective randomised controlled study Duration: not stated No. of centres: single Location: Germany Setting: university hospital Withdrawals: none Dates: not stated |
|
| Participants | 40 consecutive participants scheduled for elective aortic valve replacement Exclusion criteria: stentless valves or pulmonary autograft, carotid stenosis > 50%, severe ascending aortic calcification, history of TIA or stroke, Alzheimer's or Parkinson's disease Demographics [limited / full sternotomy] Number of participants: 40 [20 / 20] Mean age (± SD): [65.7 ± 1.9 years / 64.3 ± 2.9 years] Male gender: [9 (45%) / 11 (55%)] Pathophysiology (AS:AR:mixed): [8:3:9 / 6:1:13] Severity of disease mean gradient: [57 ± 14 / 63 ± 15] Mean risk score: not stated Mean left ventricular ejection fraction: [64 ± 3 / 65 ± 2] Diabetes mellitus: [4(20%) / 3(15%)] Preoperative FEV1 : [2.3 ± 0.9 / 2.6 ± 0.8] Preoperative FVC: [3.0 ± 1.0 / 3.2 ± 1.0] Smoking status: not stated |
|
| Interventions |
Limited sternotomy: limited median skin incision (7 to 9 cm) and reversed L‐shaped upper partial sternotomy into 4th or 5th right intercostal space Modifications from full sternotomy: the venting and cardioplegia strategies in the minimally invasive cases were different. Different surgeons performed minimally invasive and full‐sternotomy operations. |
|
| Outcomes |
Primary outcomes: operative time, CPB and cross‐clamp time, postoperative ventilation, 24‐hour chest tube drainage, ICU stay, and hospital stay Secondary outcomes: spirometry (postoperative day 6 or 7), pain scores (days 2 to 3 and 6 to 7), neuropsychological and biochemical tests Other reported outcomes: none (follow‐up time in parentheses) |
|
| Standard care | Standard care was propofol anaesthesia, ascending aorta and right atrial cannulation, apical left ventricular vent, antegrade and retrograde cold blood cardioplegia. Right temporary pacing wires. | |
| Notes | No conflict of interest or funding | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Blinding of outcome assessment (detection bias) Low risk from non‐blinding | Low risk | Mortality, blood loss, deep sternal wound infection, re‐exploration, and postoperative atrial fibrillation rates are unlikely to be affected by absence of blinding. |
| Blinding of outcome assessment (detection bias) At risk from non‐blinding | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All relevant outcome measures reported |
| Other bias | Unclear risk | Some confounding aspects of surgical techniques differing between 2 groups (vent and cardioplegia techniques) |
Moustafa 2007.
| Methods |
Study design: prospective randomised controlled study Duration: not stated No. of centres:single Location: Egypt Setting: university hospital Withdrawals: none Dates: not stated |
|
| Participants | 60 consecutive participants undergoing first‐time elective aortic valve replacement for either AS or AR Exclusion criteria: emergency surgery, left ventricular ejection fraction < 25%, heavily calcified ascending aorta, redo valve surgery, other associated valve lesions Demographics [limited / full sternotomy] Number of participants: 60 [30 / 30] Mean age (± SD): [22.9 ± 2.4 / 23.8 ± 3.5] Male gender: [16 / 15] Pathophysiology (AS:AR): [15:15 / 15:15] Severity of disease: not stated Mean risk score: not stated Mean left ventricular ejection fraction: [56 ± 2.3 / 55 ± 2.6] Diabetes mellitus: not stated Preoperative lung function: not stated Smoking status: not stated |
|
| Interventions |
Limited sternotomy: reversed L‐shaped mini‐sternotomy to the 3rd intercostal space Other modifications from full sternotomy: venous drainage not specified in methods but noted to be different for mini‐sternotomy group |
|
| Outcomes |
Primary outcomes: not stated Secondary outcomes: not stated Other reported outcomes: pulmonary function tests (1 week and 1 month post), length of incision, operating time, CPB time, ventilation time, chest drainage at 24 hours, blood transfusions, ICU stay, total hospital stay, participant survey of cosmetic effect, analgesia use (follow‐up time in parentheses) |
|
| Standard care | Standard care was aortic and right atrial cannulation, coronary ostial and root antegrade cold blood cardioplegia, main pulmonary artery or left atrial appendage venting. All participants received a St Jude Medical mechanical bileaflet prosthesis. | |
| Notes | No conflict of interests declared | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Closed envelope method |
| Allocation concealment (selection bias) | Low risk | Closed envelope method |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Blinding of outcome assessment (detection bias) Low risk from non‐blinding | Low risk | Mortality, blood loss, deep sternal wound infection, re‐exploration, and postoperative atrial fibrillation rates are unlikely to be affected by absence of blinding. |
| Blinding of outcome assessment (detection bias) At risk from non‐blinding | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | All cited and relevant outcome measures reported |
| Other bias | Low risk | |
Mächler 1999.
| Methods |
Study design: prospective randomised controlled study Duration: 18 months No. of centres:single Location: Austria Setting: university hospital Withdrawals: none Dates: July 1996 to December 1997 |
|
| Participants | 120 adults requiring aortic valve procedures Exclusion criteria: acute endocarditis, concomitant procedures, reoperation Demographics [limited / full sternotomy] Number of participants: 120 [60 / 60] Median age (IQR): [65 (56 to 70) years / 65 (55 to 72) years] Male gender: [35 / 36] Pathophysiology (AS:AR): [55:5 / 54:6] Severity of disease AVA (IQR): [0.6 (0.5 to 0.7) / 0.6 (0.5 to 0.8)] Mean risk score: not stated Median left ventricular ejection fraction (IQR): [67 (60 to 71) / 63 (48 to 70)] Diabetes mellitus: not stated Preoperative lung function: not stated Smoking status: not stated |
|
| Interventions |
Limited sternotomy: mid‐line 8‐ to 10‐cm incision, L‐shaped sternotomy to 3rd or 4th right intercostal space Other modifications from full sternotomy: none |
|
| Outcomes |
Primary outcomes: not stated Secondary outcomes: not stated Other reported outcomes: cross‐clamp time, CPB time, operation time, postoperative ejection fraction, duration of ventilation, chest tube drainage at 24 hour, reoperation requirements, pericardial effusions, conversion to full sternotomy, arrhythmias, strokes, wound infection, sternal instability, sternal pain |
|
| Standard care | Standard care was isoflurane anaesthesia with bolus fentanyl, ascending and right atrial cannulation, 30 to 32 °C hypothermia on CPB, right superior pulmonary vein or pulmonary artery venting, ostial antegrade St. Thomas' cardioplegia and transvenous pacing wires if required only. | |
| Notes | Only the first 10 participants had echocardiography. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random assignation to surgeons, but no clear randomisation |
| Allocation concealment (selection bias) | Unclear risk | Concealment not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Blinding of outcome assessment (detection bias) Low risk from non‐blinding | Low risk | Mortality, blood loss, deep sternal wound infection, re‐exploration, and postoperative atrial fibrillation rates are unlikely to be affected by absence of blinding. |
| Blinding of outcome assessment (detection bias) At risk from non‐blinding | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants reported |
| Selective reporting (reporting bias) | Low risk | All relevant outcome measures reported |
| Other bias | Low risk | |
AR: aortic regurgitation; AS: aortic stenosis; ASA: American Society of Anesthesiologists; AVA: aortic valve area; CPB: cardiopulmonary bypass; COPD: chronic obstructive pulmonary disease; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; ICU: intensive care unit; IQR: interquartile range; NYHA: New York Heart Association; SD: standard deviation; TIA: transient ischaemic attack.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aris 1999b | Not randomised |
| Bakir 2014 | Not randomised |
| Baumbach 2010 | Not randomised |
| Borger 2016 | Duplicate data |
| Bruce 2014 | Intervention group was robotic surgery. |
| Canosa 1999 | Observational study |
| Chang 1999 | Observational study |
| Christiansen 1999 | Observational study |
| Concistre 2013 | Observational study |
| Corbi 2003 | Observational study |
| Dalen 2015 | Observational study (propensity matched) |
| Detter 2002b | Observational study |
| Doll 2002 | Observational study |
| Farhat 2003 | Prospective but not randomised |
| Ferdinand 2001 | Observational study |
| Foghsgaard 2009 | Prospective but not randomised |
| Frazier 1998 | Observational study |
| Gilmanov 2013 | Observational study |
| Glauber 2013 | Observational study |
| Glower 2014 | Observational study |
| Hamano 2001 | Observational study |
| Hiraoka 2011 | Observational study |
| Johnston 2012 | Observational study (propensity matched) |
| Korach 2010 | Observational study |
| Leshnower 2006 | Observational study |
| Liu 1999b | Observational study |
| Mahesh 2011 | Observational study |
| Masiello 2002 | Observational study |
| Mihos 2013 | Observational study |
| Mikus 2013 | Observational study Redo surgeries |
| Ruttmann 2010 | Observational study |
| Sansone 2012 | Mini‐thoracotomy |
| Santarpino 2012 | Observational study |
| Sener 2001 | Mini‐thoracotomy |
| Sharony 2003 | Observational study |
| Sharony 2004 | Observational study (propensity matched) |
| Sidiropolous 1999 | Observational study |
| Stamou 2003 | Observational study (propensity matched) |
| Suenaga 2004 | Observational study |
| Svensson 1998 | Observational study |
| Vanoverbeke 2004 | Observational study |
| Walther 1999b | Observational study |
| Wheatley 2004 | Port access |
| Yon 2014 | Observational study |
| You 2012 | Observational study |
Characteristics of studies awaiting assessment [ordered by study ID]
ISRCTN29567910 (MAVRIC).
| Methods |
Study design: randomised controlled trial Duration: 35 months No. of centres: single Location: UK Setting: cardiac surgical centre Dates: February 2014 to January 2017 |
| Participants | Adults receiving first‐time, non‐emergency, isolated AVR. Exclusion criteria: requiring concomitant cardiac procedure(s); haemoglobin level < 90 g/L; pregnant; unable to stop currently prescribed treatment affecting clotting; history of thrombophilia, thrombocytopenia, or other haematological conditions that would affect participation in the trial; infective endocarditis; prevented from having red blood cells and blood products according to a system of beliefs |
| Interventions | Limited sternotomy: manubrium‐limited mini‐sternotomy (intervention arm) involves a mid‐line incision in which the manubrium is divided from the sternal notch to just below the manubrio‐sternal junction. |
| Outcomes |
Primary outcomes: proportion of participants who receive a red blood cell transfusion postoperatively within 7 days of AVR surgery. Secondary outcomes: proportion of participants who receive a red blood cell transfusion during the intraoperative period, postoperative period (from admission to cardiac intensive care unit to 7 days); number of red blood cell transfusion units per participant within the 7 days following AVR surgery; proportion of participants receiving platelet transfusion or receiving fresh frozen plasma transfusion within the 7 days following AVR surgery; total number of participants receiving any blood products and the number of units transfused within the 7 days following AVR surgery and during the entire hospital stay; mean and range of postoperative blood loss within 6 and 12 hours after surgery; reoperation rates following the end of index surgery; quality of life EuroQol (EQ‐5D‐3L, EQ‐VAS) measured at baseline, day 2, 6 weeks, and 12 weeks; mean day and range of days upon which participants are deemed 'fit for discharge' from hospital; healthcare utilisation to 12 weeks postsurgery; cost and cost effectiveness; adverse event profiles related to study procedures for each arm. |
| Notes | Currently in data analysis phase |
ISRCTN58128724 (MiniStern).
| Methods |
Study design: randomised interventional treatment trial No. of centres: single |
| Participants | Participants aged > 18 years at the time of surgery; either sex; elective, first‐time, isolated AVR Exclusion criteria: documented poor left ventricular function or LVEF 30%; documented chest wall deformities; documented severe emphysema or COPD; current body mass index 35 kg/m2; concomitant cardiac surgery; redo surgery; median sternotomy indicated |
| Interventions | Comparing upper mini‐sternotomy to full median sternotomy as a surgical approach to first‐time isolated AVR. |
| Outcomes |
Primary outcomes: total length of stay in hospital for the index AVR operation measured in days Secondary outcomes: fitness for discharge; health‐related quality of life and participant satisfaction at baseline, 6 weeks, 6 months, and 12 months using the 36‐item short form health survey (SF‐36) and Coronary Revascularization Outcome Questionnaire ‐ Coronary Artery Bypass Graft (CROQ‐CABG); heart function (LVEF) by echocardiography at baseline, day of discharge, and 6 months postsurgery; procedure time: total theatre time, cross‐clamp time, cardiopulmonary bypass time, blood loss, blood transfusion; respiratory function (forced expiratory volume in 1 second) by hand‐held spirometry at baseline, day 4, day of discharge, 6 weeks, and 6 months |
| Notes | Data collection completed in October 2015. Principle Investigator contacted (April 2016) to request results. |
NCT01972555 (CMILE).
| Methods |
Study design: open‐label, randomised controlled trial Duration: 22 months No. of centres: single Location: Sweden Setting: cardiac surgical centre Dates: October 2013 to July 2015 |
| Participants | 40 consecutive participants undergoing first‐time elective isolated AVR. Exclusion criteria: LVEF < 0.45; coexisting severe valvular disorder; previous cardiac surgery; urgent or emergent surgery |
| Interventions | Limited sternotomy: either mini‐sternotomy or anterior right‐sided mini‐thoracotomy |
| Outcomes |
Primary outcomes: tricuspid annular systolic plane excursion; right ventricular fractional area change; right ventricular dimensions; pulsed wave tissue Doppler right ventricular velocity (all at postoperative days 4 and 40) Secondary outcomes: not stated (follow‐up time in parentheses) |
| Notes | Principle investigator contacted for results (October 2016). |
AVR: aortic valve replacement; COPD: chronic obstructive pulmonary disease; LVEF: left ventricular ejection fraction.
Characteristics of ongoing studies [ordered by study ID]
NCT02272621.
| Trial name or title | Surgical Trauma After Partial Upper Hemisternotomy Versus Full Sternotomy Aortic Valve Replacement |
| Methods |
Study design: open‐label, randomised, controlled trial Duration: 20 months No. of centres: single Location: Sweden Setting: cardiac surgical centre Dates: April 2014 to December 2016 |
| Participants | 40 participants scheduled for aortic valve replacement Inclusion criteria: aged ≥ 18 years; severe aortic stenosis defined as aortic valve area of < 1 cm2 or index area of 0.6 cm2/m2 by echocardiography; referred for medically indicated aortic valve replacement; sinus rhythm; provide written informed consent Exclusion criteria: left ventricular ejection fraction < 0.45; presence of any coexisting severe valvular disorder; previous cardiac surgery; urgent or emergent surgery |
| Interventions | Partial upper hemi‐sternotomy |
| Outcomes | Primary outcomes: interleukin‐6; interleukin‐8; interleukin‐10; tumour necrosis factor‐alpha. All postoperatively at 0 to 3 days |
| Starting date | April 2015 |
| Contact information | Peter Svenarud, MD, PhD +46 (0) 8 517 708 12 peter.svenarud@karolinska.se |
| Notes |
NCT02278666 (SATURNO).
| Trial name or title | Minimally Invasive Versus Conventional Aortic Valve Replacement: a Long Term Registry (SATURNO) |
| Methods |
Study design: prospective registry No. of centres: single Location: Italy Setting: cardiac surgical centre Dates: October 2014 to November 2018 |
| Participants | Estimated 1000 participants undergoing aortic valve replacement Inclusion criteria: participants undergoing isolated aortic valve surgery; written informed consent to the use of personal data Exclusion criteria: other associated cardiac surgery; emergency surgery |
| Interventions | Upper J‐ or T‐ mini‐sternotomy or right mini‐thoracotomy |
| Outcomes |
Primary outcomes: cardiopulmonary bypass time during surgery; total duration of intensive care unit stay during hospital stay, usually lasting 1 to 2 weeks; blood transfusions during hospital stay, usually lasting 1 to 2 weeks Secondary outcomes: renal insufficiency (need for haemofiltration) during hospital stay, usually lasting 1 to 2 weeks; prolonged ventilation (longer than 24 hours) during hospital stay; re‐exploration for bleeding (need of surgical revision for bleeding) during hospital stay, usually lasting 1 to 2 weeks; sepsis during hospital stay, usually lasting 1 to 2 weeks; neurological complications (stroke or transient ischaemic attacks, or both) during hospital stay, usually lasting 1 to 2 weeks; in‐hospital mortality during hospital stay, usually lasting 1 to 2 weeks; 30‐day mortality 30 days after surgery. |
| Starting date | October 2014 |
| Contact information | Elisa Mikus, MD elisamikus@yahoo.it |
| Notes |
NCT02726087 (QUALITY‐AVR).
| Trial name or title | Quality of Life After Ministernotomy Versus Full Sternotomy Aortic Valve Replacement (QUALITY‐AVR) |
| Methods |
Study design: single‐blind, all‐comer, randomised controlled trial Duration: 36 months No. of centres: single Location: Spain Setting: cardiac surgical centre Dates: March 2016 to March 2019 |
| Participants | 96 participants with isolated aortic valve replacement due to aortic stenosis Inclusion criteria: severe aortic stenosis referred for medically indicated isolated aortic valve replacement due to aortic stenosis in participants > 18 years Exclusion criteria: left ventricular ejection fraction < 40%, previous cardiac surgery, urgent/emergent surgery, infective endocarditis, need of concomitant procedures other than isolated Morrow miectomy and thorax deformity |
| Interventions | Minimally invasive aortic valve replacement with partial "J" upper hemi‐sternotomy through right 4th intercostal space |
| Outcomes |
Primary outcomes: change from baseline Questionnaire EQ‐5D‐5L Index at 1, 6, and 12 months Secondary outcomes: change from baseline Questionnaire EQ‐5D‐5L visual analogue scale for pain at 1, 6, and 12 months; early postoperative combined end point of 6 complications at 1 month (all‐cause mortality, acute myocardial infarction, cerebrovascular or transient ischaemic accident, acute renal failure (Acute Kidney Injury Classification ≥ 2), nosocomial infections (pneumonia, early endocarditis, mediastinitis, sepsis) and need of any reintervention); SATISCORE Questionnaire (satisfaction in cardiac surgery) at 1 to 6 months; change from baseline Questionnaire EQ‐5D‐5L severity index at 1, 6, and 12 months; change from baseline Questionnaire EQ‐5D‐5L health index (severity index inverse) at 1, 6, and 12 months; late postoperative combined end point of 6 complications at 1 to 5 years (all‐cause mortality, acute myocardial infarction, cerebrovascular or transient ischaemic accident, acute renal failure (Acute Kidney Injury Classification ≥ 2), nosocomial infections (pneumonia, early endocarditis, mediastinitis, sepsis), and need of any reintervention); total in‐hospital and intensive care unit stay (in days) from date of surgery until the date of discharge or date of death from any cause, whichever came first, assessed up to 1 year; cardiopulmonary bypass time in minutes and cross‐clamp ischaemic heart time in minutes needed in the surgery day 1 after surgery; mechanical ventilatory support time needed after surgery in hours at 7 days; transfusional requirements (number of red packed cells, fresh frozen plasma, and platelets) for first 72 hours after surgery; New York Heart Association functional class scale for heart failure at baseline and 1, 6, and 12 months; heart failure status between participants (number of participants alive (survival)) at 6 to 12 months; first‐year mortality (number of participants alive (survival) at 5 years; 5‐year mortality; early postoperative combined end point of 4 complications at 1 month (all‐cause mortality, acute myocardial infarction, cerebrovascular or transient ischaemic accident, and acute renal failure (Acute Kidney Injury Classification ≥ 2); late postoperative combined end point of 4 complications at 1 to 5 years (all‐cause mortality, acute myocardial infarction, cerebrovascular or transient ischaemic accident, and acute renal failure (Acute Kidney Injury Classification ≥ 2) |
| Starting date | March 2016 |
| Contact information | Emiliano A Rodriguez‐Caulo, MD, PhD, FECTS +34 951032054 erodriguezcaulo@hotmail.com |
| Notes |
Differences between protocol and review
'Summary of findings' table
We included all primary and secondary outcome measures in the 'Summary of findings' table, as these were all felt to be important patient‐related factors that should be included in the summary statement.
Additional unplanned outcome measures
We amended one of our secondary outcome measures from "Blood loss and transfusion requirements" to "Postoperative blood loss" as transfusion requirements were not stated. However, we identified three outcome measures of interest that were reported in several studies and which we proceeded to perform analysis on: intensive care unit stay, lung function tests, and re‐exploration for bleeding. Following review, we also added incidence of postoperative atrial fibrillation and ventilation time.
We renamed several outcome measures according to the wording most commonly used in the included studies, in order to bring our review in line with the accepted nomenclature. Although the clinical outcomes did not change, this allowed for a standardisation across our review. We changed all‐cause mortality to mortality; total hospital stay to length of hospital stay; sternal wound infection to deep sternal wound infection;intensive care unit length of stay to intensive care unit stay; and postoperative lung function tests to postoperative pulmonary function tests.
Sensitivity analyses
We had originally planned to include only studies with a low risk of bias as a sensitivity analysis, but no studies fulfilled this criterion. We therefore performed sensitivity analyses excluding studies at high risk of bias. We additionally identified a single study that employed rapid‐deployment aortic valves which could be a source of bias affecting intraoperative outcomes. Excluding this study was also performed as a separate sensitivity analysis for relevant outcomes.
Contributions of authors
BHK: guarantor of the review and conceived, designed, and co‐ordinated the review.
BHK, SGJ: data collection, including search strategy design, searching, screening, retrieval, appraisal, and data extraction.
BHK, SGJ: additional data from papers, unpublished data, and industry evidence.
DAC, RJNNW, SCM: review and arbitration of papers.
BHK: data entry.
All review authors: analysis and interpretation of data.
BHK, SGJ: writing the review.
DAC, RJNNW, SCM: expert advice on content of review.
Sources of support
Internal sources
-
Liverpool Heart and Chest Hospital, UK.
Financial support in retrieving relevant papers
External sources
No sources of support supplied
Declarations of interest
BHK: none known.
SGJ: none known.
SCM consults for Edwards Lifesciences, a manufacturer of equipment for minimal incision surgery. He is on the Advisory Board for Minimally Invasive Surgery, as well as being a member of the Speaker's Bureau. He is also an investigator on the PARTNER II trial, a prospective, multi‐centre, open‐label trial of people undergoing aortic valve surgery for severe aortic stenosis that includes transcatheter valve implantation strategies. As a result, he was not involved in screening of titles or abstracts, did not assess full‐texts or contribute to data‐abstraction (except for arbitration) and did not engage in assessing risk of bias or quality of evidence assessments.
DC: has a practice that includes minimally invasive aortic valve replacement.
RJNNW: has a practice that includes minimally invasive aortic valve replacement.
New
References
References to studies included in this review
Aris 1999a {published data only}
- Aris A, Camara ML, Montiel J, Delgado LJ, Galan J, Litvan H. Ministernotomy versus median sternotomy for aortic valve replacement: a prospective, randomized study. Annals of Thoracic Surgery 1999;67:1583‐7. [DOI] [PubMed] [Google Scholar]
Bonacchi 2002 {published data only}
- Bonacchi M, Prifti E, Giunti G, Frati G, Sani G. Does ministernotomy improve postoperative outcome in aortic valve operation? A prospective randomized study. Annals of Thoracic Surgery 2002;73:460‐5. [DOI] [PubMed] [Google Scholar]
Borger 2015 {published data only}
- Borger MA, Moustafine V, Conradi L, Knosalla C, Richter M, Merk DR, et al. A randomized multicenter trial of minimally invasive rapid deployment versus conventional full sternotomy aortic valve replacement. Annals of Thoracic Surgery 2015;99:17‐25. [DOI] [PubMed] [Google Scholar]
Calderon 2009 {published data only}
- Calderon J, Richebe P, Guibaud JP, Coiffic A, Branchard O, Asselineau J, et al. Prospective randomized study of early pulmonary evaluation of patients scheduled for aortic valve surgery performed by ministernotomy or total median sternotomy. Journal of Cardiothoracic and Vascular Anesthesia 2009;23:795‐801. [DOI] [PubMed] [Google Scholar]
Dogan 2003 {published data only}
- Dogan S, Dzemali O, Wimmer‐Greinecker G, Derra P, Doss M, Khan MF, et al. Minimally invasive versus conventional aortic valve replacement: a prospective randomized trial. Journal of Heart Valve Disease 2003;12:76‐80. [PubMed] [Google Scholar]
Mächler 1999 {published data only}
- Mächler HE, Bergmann P, Anelli‐Monti M, Dacar D, Rehak P, Knez I, et al. Minimally invasive versus conventional aortic valve operations: a prospective study in 120 patients. Annals of Thoracic Surgery 1999;67:1001‐5. [DOI] [PubMed] [Google Scholar]
Moustafa 2007 {published data only}
- Moustafa MA, Abdelsamad AA, Zakaria G, Omarah MM. Minimal vs median sternotomy for aortic valve replacement. Asian Cardiovascular Thoracic Annals 2007;15:472‐5. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aris 1999b {published data only}
- Aris A, Camara ML, Casan P, Litvan H. Pulmonary function following aortic valve replacement: a comparison between ministernotomy and median sternotomy. Journal of Heart Valve Disease 1999;8(6):605‐8. [PubMed] [Google Scholar]
Bakir 2014 {published data only}
- Bakir I, Casselman FP, Onan B, Praet F, Vermeulen Y, Degrieck I. Does a minimally invasive approach increase the incidence of patient‐prosthesis mismatch in aortic valve replacement?. Journal of Heart Valve Disease 2014;23(2):161‐7. [PubMed] [Google Scholar]
Baumbach 2010 {published data only}
- Baumbach H, Burger JH, Nagib R, Albert M, Ursulescu A, Franke U. Minimal invasive access‐the beneficial impact on quality of life for patients undergoing isolated aortic valve replacement. Thoracic and Cardiovascular Surgeon. Conference: 39th Annual Meeting of the German Society for Cardiovascular and Thoracic Surgery Stuttgart Germany. Conference Start 2010; Vol. 58, issue S01:V42.
Borger 2016 {published data only}
- Borger MA, Dohmen PM, Knosalla C, Hammerschmidt R, Merk DR, Richter M, et al. Haemodynamic benefits of rapid deployment aortic valve replacement via a minimally invasive approach: 1‐year results of a prospective multicentre randomized controlled trial. European Journal of Cardio‐thoracic Surgery 2016; Vol. 50, issue 4:713‐20. [DOI] [PubMed]
Bruce 2014 {published data only}
- Bruce KM, Yelland GW, Almeida AA, Smith JA, Robinson SR. Effects on cognition of conventional and robotically assisted cardiac valve operation. Annals of Thoracic Surgery 2014;97(1):48‐55. [DOI] [PubMed] [Google Scholar]
Canosa 1999 {published data only}
- Canosa C, Mariani MA, Grandjean JG, Alessandrini F, Boonstra PW, Filippo CM, et al. Aortic valve replacement via ministernotomy: early results of a two‐center study. Cardiologia 1999;44(10):925‐7. [PubMed] [Google Scholar]
Chang 1999 {published data only}
- Chang YS, Lin PJ, Chang CH, Chu JJ, Tan PP. "I" ministernotomy for aortic valve replacement. Annals of Thoracic Surgery 1999;68(1):40‐5. [DOI] [PubMed] [Google Scholar]
Christiansen 1999 {published data only}
- Christiansen S, Stypmann J, Tjan TD, Wichter T, Aken H, Scheld HH, et al. Minimally‐invasive versus conventional aortic valve replacement ‐ perioperative course and mid‐term results. European Journal of Cardio‐thoracic Surgery 1999;16(6):647‐52. [DOI] [PubMed] [Google Scholar]
Concistre 2013 {published data only}
- Concistre G, Santarpino G, Pfeiffer S, Farneti P, Miceli A, Chiaramonti F, et al. Two alternative sutureless strategies for aortic valve replacement: a two‐center experience. Innovations: Technology & Techniques in Cardiothoracic & Vascular Surgery 2013;8(4):253‐7. [DOI] [PubMed] [Google Scholar]
Corbi 2003 {published data only}
- Corbi P, Rahmati M, Donal E, Lanquetot H, Jayle C, Menu P, et al. Prospective comparison of minimally invasive and standard techniques for aortic valve replacement: initial experience in the first hundred patients. Journal of Cardiac Surgery 2003;18(2):133‐9. [DOI] [PubMed] [Google Scholar]
Dalen 2015 {published data only}
- Dalen M, Biancari F, Rubino AS, Santarpino G, Praetere H, Kasama K, et al. Ministernotomy versus full sternotomy aortic valve replacement with a sutureless bioprosthesis: a multicenter study. Annals of Thoracic Surgery 2015;99(2):524‐30. [DOI] [PubMed] [Google Scholar]
Detter 2002b {published data only}
- Detter C, Deuse T, Boehm DH, Reichenspurner H, Reichart B. Midterm results and quality of life after minimally invasive vs. conventional aortic valve replacement. Thoracic & Cardiovascular Surgeon 2002;50(6):337‐41. [DOI] [PubMed] [Google Scholar]
Doll 2002 {published data only}
- Doll N, Borger MA, Hain J, Bucerius J, Walther T, Gummert JF, et al. Minimal access aortic valve replacement: effects on morbidity and resource utilization. Annals of Thoracic Surgery 2002;74(4):S1318‐22. [DOI] [PubMed] [Google Scholar]
Farhat 2003 {published data only}
- Farhat F, Lu Z, Lefevre M, Montagna P, Mikaeloff P, Jegaden O. Prospective comparison between total sternotomy and ministernotomy for aortic valve replacement. Journal of Cardiac Surgery 2003;18(5):396‐401; discussion 402‐3. [DOI] [PubMed] [Google Scholar]
Ferdinand 2001 {published data only}
- Ferdinand FD, Sutter FP, Goldman SM. Clinical use of stentless aortic valves with standard and minimally invasive surgical techniques. Seminars in Thoracic & Cardiovascular Surgery 2001;13(3):283‐90. [DOI] [PubMed] [Google Scholar]
Foghsgaard 2009 {published data only}
- Foghsgaard S, Schmidt TA, Kjaergard HK. Minimally invasive aortic valve replacement: late conversion to full sternotomy doubles operative time. Texas Heart Institute Journal 2009;36(4):293‐7. [PMC free article] [PubMed] [Google Scholar]
Frazier 1998 {published data only}
- Frazier BL, Derrick MJ, Purewal SS, Sowka LR, Johna S. Minimally invasive aortic valve replacement. European Journal of Cardio‐thoracic Surgery 1998;14 Suppl 1:S122‐5. [DOI] [PubMed] [Google Scholar]
Gilmanov 2013 {published data only}
- Gilmanov D, Bevilacqua S, Murzi M, Cerillo AG, Gasbarri T, Kallushi E, et al. Minimally invasive and conventional aortic valve replacement: a propensity score analysis. Annals of Thoracic Surgery 2013;96(3):837‐43. [DOI] [PubMed] [Google Scholar]
Glauber 2013 {published data only}
- Glauber M, Miceli A, Gilmanov D, Ferrarini M, Bevilacqua S, Farneti PA, et al. Right anterior minithoracotomy versus conventional aortic valve replacement: a propensity score matched study. Journal of Thoracic & Cardiovascular Surgery 2013;145(5):1222‐6. [DOI] [PubMed] [Google Scholar]
Glower 2014 {published data only}
- Glower DD, Desai BS, Hughes GC, Milano CA, Gaca JG. Aortic valve replacement via right minithoracotomy versus median sternotomy: a propensity score analysis. Innovations: Technology & Techniques in Cardiothoracic & Vascular Surgery 2014;9(2):75‐81; discussion 81. [DOI] [PubMed] [Google Scholar]
Hamano 2001 {published data only}
- Hamano K, Kawamura T, Gohra H, Katoh T, Fujimura Y, Zempo N, et al. Stress caused by minimally invasive cardiac surgery versus conventional cardiac surgery: incidence of systemic inflammatory response syndrome. World Journal of Surgery 2001;25(2):117‐21. [DOI] [PubMed] [Google Scholar]
Hiraoka 2011 {published data only}
- Hiraoka A, Kuinose M, Chikazawa G, Totsugawa T, Katayama K, Yoshitaka H. Minimally invasive aortic valve replacement surgery: comparison of port‐access and conventional standard approach. Circulation Journal 2011;75(7):1656‐60. [DOI] [PubMed] [Google Scholar]
Johnston 2012 {published data only}
- Johnston DR, Atik FA, Rajeswaran J, Blackstone EH, Nowicki ER, Sabik JF 3rd, et al. Outcomes of less invasive J‐incision approach to aortic valve surgery. Journal of Thoracic & Cardiovascular Surgery 2012;144(4):852‐8.e3. [DOI] [PubMed] [Google Scholar]
Korach 2010 {published data only}
- Korach A, Shemin RJ, Hunter CT, Bao Y, Shapira OM. Minimally invasive versus conventional aortic valve replacement: a 10‐year experience. Journal of Cardiovascular Surgery 2010;51(3):417‐21. [PubMed] [Google Scholar]
Leshnower 2006 {published data only}
- Leshnower BG, Trace CS, Boova RS. Port‐access‐assisted aortic valve replacement: a comparison of minimally invasive and conventional techniques. Heart Surgery Forum 2006;9(2):E560‐4; discussion E564. [DOI] [PubMed] [Google Scholar]
Liu 1999b {published data only}
- Liu J, Sidiropoulos A, Konertz W. Minimally invasive aortic valve replacement (AVR) compared to standard AVR. European Journal of Cardio‐thoracic Surgery 1999;16 Suppl 2:S80‐3. [PubMed] [Google Scholar]
Mahesh 2011 {published data only}
- Mahesh B, Navaratnarajah M, Mensah K, Ilsley C, Amrani M. Mini‐sternotomy aortic valve replacement: is it safe and effective? Comparison with standard techniques. Journal of Heart Valve Disease 2011;20(6):650‐6. [PubMed] [Google Scholar]
Masiello 2002 {published data only}
- Masiello P, Coscioni E, Panza A, Triumbari F, Preziosi G, Benedetto G. Surgical results of aortic valve replacement via partial upper sternotomy: comparison with median sternotomy. Cardiovascular Surgery 2002;10(4):333‐8. [DOI] [PubMed] [Google Scholar]
Mihos 2013 {published data only}
- Mihos CG, Santana O, Lamas GA, Lamelas J. Incidence of postoperative atrial fibrillation in patients undergoing minimally invasive versus median sternotomy valve surgery. Journal of Thoracic & Cardiovascular Surgery 2013;146(6):1436‐41. [DOI] [PubMed] [Google Scholar]
Mikus 2013 {published data only}
- Mikus E, Calvi S, Tripodi A, Lamarra M, Giglio M. Upper 'J' ministernotomy versus full sternotomy: an easier approach for aortic valve reoperation. Journal of Heart Valve Disease 2013;22(3):295‐300. [PubMed] [Google Scholar]
Ruttmann 2010 {published data only}
- Ruttmann E, Gilhofer TS, Ulmer H, Chevtchik O, Kocher A, Schistek R, et al. Propensity score‐matched analysis of aortic valve replacement by mini‐thoracotomy. Journal of Heart Valve Disease 2010;19(5):606‐14. [PubMed] [Google Scholar]
Sansone 2012 {published data only}
- Sansone F, Punta G, Parisi F, Dato GM, Zingarelli E, Flocco R, et al. Right minithoracotomy versus full sternotomy for the aortic valve replacement: preliminary results. Heart, Lung & Circulation 2012;21(3):169‐73. [DOI] [PubMed] [Google Scholar]
Santarpino 2012 {published data only}
- Santarpino G, Pfeiffer S, Schmidt J, Concistre G, Fischlein T. Sutureless aortic valve replacement: first‐year single‐center experience. Annals of Thoracic Surgery 2012;94(2):504‐8; discussion 508‐9. [DOI] [PubMed] [Google Scholar]
Sener 2001 {published data only}
- Sener T, Gercekoglu H, Evrenkaya S, Aydin NB, Cimen S, Demirtas M, et al. Comparison of minithoracotomy with conventional sternotomy methods in valve surgery. Heart Surgery Forum 2001;4(1):26‐30. [PubMed] [Google Scholar]
Sharony 2003 {published data only}
- Sharony R, Grossi EA, Saunders PC, Schwartz CF, Ribakove GH, Culliford AT, et al. Minimally invasive aortic valve surgery in the elderly: a case‐control study. Circulation 2003;108 Suppl 1:II43‐7. [DOI] [PubMed] [Google Scholar]
Sharony 2004 {published data only}
- Sharony R, Grossi EA, Saunders PC, Schwartz CF, Ribakove GH, Baumann FG, et al. Propensity score analysis of a six‐year experience with minimally invasive isolated aortic valve replacement. Journal of Heart Valve Disease 2004;13(6):887‐93. [PubMed] [Google Scholar]
Sidiropolous 1999 {published data only}
- Sidiropolous A, Liu J, Konertz W. Minimally invasive access for aortic valve replacement (AVR). Zeitschrift fur Kardiologie 1999;88(S4):30‐4. [Google Scholar]
Stamou 2003 {published data only}
- Stamou SC, Kapetanakis EI, Lowery R, Jablonski KA, Frankel TL, Corso PJ. Allogeneic blood transfusion requirements after minimally invasive versus conventional aortic valve replacement: a risk‐adjusted analysis. Annals of Thoracic Surgery 2003;76(4):1101‐6. [DOI] [PubMed] [Google Scholar]
Suenaga 2004 {published data only}
- Suenaga E, Suda H, Katayama Y, Sato M, Fujita H, Yoshizumi K, et al. Comparison of limited and full sternotomy in aortic valve replacement. Japanese Journal of Thoracic & Cardiovascular Surgery 2004;52(6):286‐91. [DOI] [PubMed] [Google Scholar]
Svensson 1998 {published data only}
- Svensson LG, D'Agostino RS. Minimal‐access aortic and valvular operations, including the "J/j" incision. Annals of Thoracic Surgery 1998;66(2):431‐5. [DOI] [PubMed] [Google Scholar]
Vanoverbeke 2004 {published data only}
- Vanoverbeke H, Belleghem Y, Francois K, Caes F, Bove T, Nooten G. Operative outcome of minimal access aortic valve replacement versus standard procedure. Acta Chirurgica Belgica 2004;104(4):440‐4. [PubMed] [Google Scholar]
Walther 1999b {published data only}
- Walther T, Falk V, Metz S, Diegeler A, Battellini R, Autschbach R, et al. Pain and quality of life after minimally invasive versus conventional cardiac surgery. Annals of Thoracic Surgery 1999;67(6):1643‐7. [DOI] [PubMed] [Google Scholar]
Wheatley 2004 {published data only}
- Wheatley GH 3rd, Prince SL, Herbert MA, Ryan WH. Port‐access aortic valve surgery: a technique in evolution. Heart Surgery Forum 2004;7(6):E628‐31. [DOI] [PubMed] [Google Scholar]
Yon 2014 {published data only}
- Yon LCN, Totaro P, Mazzola A. Ministernotomy versus median sternotomy for isolated aortic valve replacement: is it time to define a new gold standard?. Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery 2014;9(3):241‐2. [Google Scholar]
You 2012 {published data only}
- You B, Gao F, Li P, Xu Y, Xu LL, Liu S, et al. Clinical study of minimally invasive versus conventional sternotomy for aortic valve replacement. Chung‐Hua i Hsueh Tsa Chih [Chinese Medical Journal] 2012;92(40):2859‐61. [PubMed] [Google Scholar]
References to studies awaiting assessment
ISRCTN29567910 (MAVRIC) {published data only}
- Akowuah A. Manubrium‐limited ministernotomy versus conventional sternotomy for aortic valve replacement. apps.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN29567910 (date first registered 3 February 2014). [ISRCTN29567910]
ISRCTN58128724 (MiniStern) {published data only}
- Nair S. A pragmatic, prospective, randomised controlled trial comparing upper ministernotomy to full median sternotomy as a surgical approach for aortic valve replacement. www.isrctn.com/ISRCTN58128724 (date first received 24 June 2010).
NCT01972555 (CMILE) {published data only}
- Svenarud P. Cardiac function after minimally invasive aortic valve implantation. clinicaltrials.gov/ct2/show/NCT01972555 (date first received: 21 October 2013). [NCT01972555]
References to ongoing studies
NCT02272621 {published data only}
- Surgical Trauma After Partial Upper Hemisternotomy Versus Full Sternotomy Aortic Valve Replacement. Ongoing study April 2015.
NCT02278666 (SATURNO) {published data only}
- Minimally Invasive Versus Conventional Aortic Valve Replacement: a Long Term Registry (SATURNO). Ongoing study October 2014.
NCT02726087 (QUALITY‐AVR) {published data only}
Additional references
Autschbach 1998
- Autschbach R, Walther T, Falk V, Diegeler A, Metz S, Mohr FW. S‐shaped in comparison to L‐shaped partial sternotomy for less invasive aortic valve replacement. European Journal of Cardio‐thoracic Surgery 1998;14 Suppl 1:S117‐21. [DOI] [PubMed] [Google Scholar]
Braunwald 2000
- Braunwald E. Aortic valve replacement: an update at the turn of the millennium. European Heart Journal 2000;21(13):1032‐3. [DOI] [PubMed] [Google Scholar]
Brown 2009
- Brown ML, McKellar SH, Sundt TM, Schaff HV. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta‐analysis. Journal of Thoracic and Cardiovascular Surgery 2009;137(3):670‐9.e5. [DOI] [PubMed] [Google Scholar]
Carabello 2013
- Carabello BA. Introduction to aortic stenosis. Circulation Research 2013;113(2):179‐85. [DOI] [PubMed] [Google Scholar]
Carapetis 2005
- Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infectious Diseases 2005;5(11):685‐94. [DOI] [PubMed] [Google Scholar]
Coffey 2014
- Coffey S, Cox B, Williams MJA. The prevalence, incidence, progression, and risks of aortic valve sclerosis: a systematic review and meta‐analysis. Journal of the American College of Cardiology 2014;63(25 Pt A):2852‐61. [DOI] [PubMed] [Google Scholar]
Cohn 1997
- Cohn LH, Adams DH, Couper GS, Bichell DP, Rosborough DM, Sears SP, et al. Minimally invasive cardiac valve surgery improves patient satisfaction while reducing costs of cardiac valve replacement and repair. Annals of Surgery 1997;226(4):421‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohn 1998
- Cohn LH. Minimally invasive aortic valve surgery: technical considerations and results with the parasternal approach. Journal of Cardiac Surgery 1998;13(4):302‐5. [DOI] [PubMed] [Google Scholar]
Cosgrove 1996
- Cosgrove DM, Sabik JF. Minimally invasive approach for aortic valve operations. Annals of Thoracic Surgery 1996;62(2):596‐7. [PubMed] [Google Scholar]
d'Arcy 2011
- d'Arcy JL, Prendergast BD, Chambers JB, Ray SG, Bridgewater B. Valvular heart disease: the next cardiac epidemic. Heart 2011;97(2):91‐3. [DOI] [PubMed] [Google Scholar]
Dare 1993
- Dare AJ, Veinot JP, Edwards WD, Tazelaar HD, Schaff HV. New observations on the etiology of aortic valve disease: a surgical pathologic study of 236 cases from 1990. Human Pathology 1993;24(12):1330‐8. [DOI] [PubMed] [Google Scholar]
Detter 2002a
- Detter C, Deuse T, Boehm DH, Reichenspurner H, Reichart B. Midterm results and quality of life after minimally invasive vs. conventional aortic valve replacement. Thoracic and Cardiovascular Surgeon 2002;50(6):337‐41. [DOI] [PubMed] [Google Scholar]
Ehrlich 2000
- Ehrlich W, Skwara W, Klavekorn WP, Roth M, Bauer EP. Do patients want minimally invasive aortic valve replacement?. European Journal of Cardio‐thoracic Surgery 2000;17(6):714‐7. [DOI] [PubMed] [Google Scholar]
Freeman 2005
- Freeman RV, Otto CM. Spectrum of calcific aortic valve disease pathogenesis, disease progression, and treatment strategies. Circulation 2005;111(24):3316‐26. [DOI] [PubMed] [Google Scholar]
Gohlke‐Bärwolf 2013
- Gohlke‐Bärwolf C, Minners J, Jander N, Gerdts E, Wachtell K, Ray S, et al. Natural history of mild and of moderate aortic stenosis. New insights from a large prospective European study. Current Problems in Cardiology 2013;38(9):365‐409. [DOI: 10.1016/j.cpcardiol.2013.06.003] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Iung 2003
- Iung B, Baron G, Butchart EG, Delahaye F, Gohlke‐Barwolf C, Levang OW, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. European Heart Journal 2003;24(13):1231‐43. [DOI] [PubMed] [Google Scholar]
Iung 2014
- Iung B, Vahanian A. Epidemiology of acquired valvular heart disease. Canadian Journal of Cardiology 2014;30(9):962‐70. [DOI] [PubMed] [Google Scholar]
Khoshbin 2011
- Khoshbin E, Prayaga S, Kinsella J, Sutherland FWH. Mini‐sternotomy for aortic valve replacement reduces the length of stay in the cardiac intensive care unit: meta‐analysis of randomised controlled trials. BMJ Open 2011;1(2):e000266. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumar 2013
- Kumar RK, Tandon R. Rheumatic fever & rheumatic heart disease: the last 50 years. Indian Journal of Medical Research 2013;137(4):643‐58. [PMC free article] [PubMed] [Google Scholar]
Lee 2004
- Lee BY, Gleason TG, Sonnad SS. Quality of life after aortic valve replacement. Expert Review of Pharmacoeconomics & Outcomes Research 2004;4(3):265‐75. [DOI] [PubMed] [Google Scholar]
Lee 2011
- Lee R, Li S, Rankin JS, O'Brien SM, Gammie JS, Peterson ED, et al. Fifteen‐year outcome trends for valve surgery in North America. Annals of Thoracic Surgery 2011;91(3):677‐84. [DOI: 10.1016/j.athoracsur.2010.11.009] [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Lillehei 1962
- Lillehei CW, Levy MJ, Varco RL, Wang Y, Adams P, Anderson RC. Surgical treatment of congenital aortic stenosis by cardiopulmonary bypass including methods for preoperative diagnosis of types. Circulation 1962;26(5):856‐72. [DOI] [PubMed] [Google Scholar]
Liu 1999a
- Liu J, Sidiropoulos A, Konertz W. Minimally invasive aortic valve replacement (AVR) compared to standard AVR. European Journal of Cardio‐thoracic Surgery 1999;16(Suppl 2):S80‐3. [PubMed] [Google Scholar]
Malaisrie 2014
- Malaisrie SC, Barnhart GR, Farivar RS, Mehall J, Hummel B, Rodriguez E, et al. Current era minimally invasive aortic valve replacement: techniques and practice. Journal of Thoracic and Cardiovascular Surgery 2014;147(1):6‐14. [DOI] [PubMed] [Google Scholar]
Manjunath 2014
- Manjunath CN, Srinivas P, Ravindranath KS, Dhanalakshmi C. Incidence and patterns of valvular heart disease in a tertiary care high‐volume cardiac center: a single center experience. Indian Heart Journal 2014;66(3):320‐6. [DOI: 10.1016/j.ihj.2014.03.010] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murtuza 2008
- Murtuza B, Pepper JR, Stanbridge RD, Jones C, Rao C, Darzi A, et al. Minimal access aortic valve replacement: is it worth it?. Annals of Thoracic Surgery 2008;85(3):1121‐31. [PUBMED: 18291224] [DOI] [PubMed] [Google Scholar]
Nishimura 2014
- Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; Vol. 129, issue 23:2440‐92. [DOI] [PubMed]
Nkomo 2006
- Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez‐Sarano M. Burden of valvular heart diseases: a population‐based study. Lancet 2006;368(9540):1005‐11. [DOI] [PubMed] [Google Scholar]
Otto 1997
- Otto CM, Burwash IG, Legget ME, Munt BI, Fujioka M, Healy NL, et al. Prospective study of asymptomatic valvular aortic stenosis clinical, echocardiographic, and exercise predictors of outcome. Circulation 1997;95(9):2262‐70. [DOI] [PubMed] [Google Scholar]
Pellikka 2005
- Pellikka PA, Sarano ME, Nishimura RA, Malouf JF, Bailey KR, Scott CG, et al. Outcome of 622 adults with asymptomatic, hemodynamically significant aortic stenosis during prolonged follow‐up. Circulation 2005;111(24):3290‐5. [DOI] [PubMed] [Google Scholar]
Phan 2014
- Phan K, Xie A, Di EM, Yan TD. A meta‐analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Annals of Thoracic Surgery 2014;98(4):1499‐511. [DOI] [PubMed] [Google Scholar]
Rao 1993
- Rao PN, Kumar AS. Aortic valve replacement through right thoracotomy. Texas Heart Institute Journal 1993;20(4):307‐8. [PUBMED: 8298332] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rose 1986
- Rose AG. Etiology of acquired valvular heart disease in adults. A survey of 18,132 autopsies and 100 consecutive valve‐replacement operations. Archives of Pathology & Laboratory Medicine 1986;110(5):385‐8. [PubMed] [Google Scholar]
Ross 1968
- Ross J, Braunwald E. Aortic stenosis. Circulation 1968;38(1 Suppl):61‐7. [DOI] [PubMed] [Google Scholar]
Scheuble 2005
- Scheuble A, Vahanian A. Aortic insufficiency. American Journal of Cardiovascular Drugs 2005;5(2):113‐20. [DOI] [PubMed] [Google Scholar]
Schwarz 1982
- Schwarz F, Baumann P, Manthey J, Hoffmann M, Schuler G, Mehmel HC, et al. The effect of aortic valve replacement on survival. Circulation 1982;66(5):1105‐10. [DOI] [PubMed] [Google Scholar]
Svensson 2013
- Svensson LG, Adams DH, Bonow RO, Kouchoukos NT, Miller DC, O'Gara PT, et al. Aortic valve and ascending aorta guidelines for management and quality measures: executive summary. Annals of Thoracic Surgery 2013;95(4):1491‐505. [DOI] [PubMed] [Google Scholar]
Thaden 2014
- Thaden JJ, Nkomo VT, Enriquez‐Sarano M. The global burden of aortic stenosis. Progress in Cardiovascular Diseases 2014;56(6):565‐71. [DOI] [PubMed] [Google Scholar]
Vahanian 2012
Walther 1999a
- Walther T, Falk V, Metz S, Diegeler A, Battellini R, Autschbach R, et al. Pain and quality of life after minimally invasive versus conventional cardiac surgery. Annals of Thoracic Surgery 1999;67(6):1643‐7. [DOI] [PubMed] [Google Scholar]
Walther 2006
- Walther T, Falk V, Mohr FW. Minimally invasive surgery for valve disease. Current Problems in Cardiology 2006;31(6):399‐437. [DOI: 10.1016/j.cpcardiol.2006.02.002] [DOI] [PubMed] [Google Scholar]


