Abstract
For patients, the social and emotional repercussions of stroke include shame, personality changes, and upheavals experienced by the couple (i.e. patient and main family caregiver). These impacts on the couple ‘patient/family caregiver’ are scarcely documented. Focusing on the perceptions of the patients and the family caregivers living at home, two years after a stroke occurrence, the aims of the study were to analyse the concordance of attitudes towards the emotional and social repercussions of stroke and to determine the profiles of the differing dyads. Two researchers conducted separate face-to-face structured interviews with stroke survivors and their family caregivers. Eleven items, identified through a content analysis of interviews and after a qualitative process of generating questionnaire items, assessed the commonly experienced impact of stroke on the family, the social repercussions of stroke, and its emotional effects on the stroke survivors. The kappa concordance coefficient was used to determine the response convergence between patients and family caregivers. Four items, selected by a panel of experts, were included in logistic regressions (i.e., demographic characteristics and patients’ impaired functions) to identify the differing dyadic profiles. Family caregivers’ and patients’ attitudes towards the social repercussions of stroke were similar. Patients with motor deficiencies tended to underestimate the upheaval brought to their couple by stroke, whereas caregivers of language-impaired patients tended to underestimate their feelings of shame and demeaning. Communication disturbances, but also residual physical disabilities in stroke survivors, may affect the understanding of each other’s attitudes within dyads. In order to avoid dysfunctional relationships between family caregivers and patients, healthcare professionals need to pay special attention to this issue, especially in cases of aphasia and motor deficiencies.
Introduction
Stroke is one of the main causes of acquired disability in most developed countries and considerably affects the life course of the victims [1]. Depending on the affected brain area, stroke can leave long-term impairments of motor, sensory, and/or cognitive functions, but is also associated with social changes [2]. At the occupational level, an average of two out of five stroke victims working at the time of occurrence were able to return to work; at the personal level, stroke can affect the relationships with children and the partners—including the sexual sphere—as well as deteriorate family dynamics and decrease participation in social activities [3, 4].
Since a majority of the survivors return home, their family caregivers, mainly their partners, also experience these social repercussions of stroke. Expected to provide complex care at home in addition to having new responsibilities (increased home tasks and duties, management of relationships with the professionals, etc.), these dependency workers [5] pose a risk for the healthcare system while their exhaustion increases and their cultural, social, and leisure activities decrease [6, 7]. This workload, in addition to their continual adaptation to the limitations of the patient, may isolate them socially. Thus, when they themselves are affected by the repercussions of the stroke as the caregiver, their capacity to remain healthy becomes a challenge for public health and health policies [8, 9].
Patient-caregiver dyad as a unit in and of itself
A strong association exists between the experiences of the patients and their family caregivers thus allowing the patient-caregiver dyads to be considered as entities [10] based on both feelings and caring [11]. After a stroke event, the quality of the relationship plays a key role on the respective well-being of the patient and the family caregiver.
The usefulness of identifying closeness of attitudes
Highlighting the concordance between patients and caregivers is challenging: studies on mutual trust [12] and harmony in social relations [13] have shown that when stroke patients and their family caregivers share similar opinions, the psychological health of patients is higher. In couples, the positively perceived quality of communication is generally associated with higher satisfaction of partners with their relationship [14] and helps to enhance the dyadic adjustment during a chronic illness [15]. Yet, while the patient-caregiver relationship should be considered as a balance between giving and taking [16], social support appears to be rather unidirectional, favouring the patient [17]. Thus, there is a need to investigate the link between patients’ and family caregivers’ attitudes towards a situation commonly shared, such as the social repercussions of stroke.
In this study, emphasis was made on the concordance of three impacts of stroke on patients and their family caregivers: changes in the patient’s personality and emotions due to stroke, effects of stroke on the family members, and the extended social repercussions of stroke.
Change in personality of stroke survivors and its impact on family caregivers
Personality change of the stroke patient is one of family caregivers’ recurring complaints [18], resulting either directly from stroke sequelae [18] or reflecting the stroke survivor’s way of adapting to this potentially traumatic event [11, 19].
Detecting personality change is particularly useful since affective disorders have been shown to play a more important role than motor impairments or pain on their family caregivers’ quality of life and satisfaction with life [6]. Moreover, family caregivers reporting personality changes in their stroke relatives have more frequently reported experiencing emotional distress [18].
Emotions felt and shared by stroke victims
Being a stroke survivor triggers a multitude of emotions. Bitterness, shame, and grief are commonly reported after the onset of a stroke [20]. Some patients feel relief that its severity was not worse; recovery gains instil pride [21]. Although sharing one’s emotions allows understanding and learning from difficult situations and helps strengthen social bonds [22], shame is one of the least shared emotions [23]. In addition, to protect their family caregivers, some patients tend to minimise the impact severity of stroke [24]. As a result, the ability of the family caregivers to detect their relatives’ ill-being and, furthermore, to support them is made more difficult.
To evaluate the potential interventions that would decrease the impact of stroke on dyadic communication, there is a need to determine the extent to which the attitudes of dyad members differ with regard to the emotional effects of stroke on the survivors.
Attitude concordance within dyads
Concordance is the agreement between the attitudes of two persons. Most of the literature on concordance has assessed the reliability of resorting to caregivers as proxy respondents for patients with limited ability due to their chronic illness [25–28]; in these studies, caregivers tend to overestimate patient symptoms and underestimate patient quality of life.
No previous literature has explored the attitudes of both patients and their caregivers regarding the social repercussions of stroke, experienced jointly during the chronic phase, nor has it identified the profiles of the differing dyads. Three important aspects reflect the quality of the dyadic interactions between stroke patients and their caregivers: (1) concordant attitudes resulting from prior communication, (2) concordant attitudes regarding commonly experienced psychosocial impacts of stroke, and (3) the psychological repercussions experienced by the stroke patients.
Objectives
Focusing on the perceptions of the stroke survivors and their family caregivers living at home two years after the stroke occurrence, the aims of the study were to analyse the concordance of attitudes on the emotional and social repercussions of stroke and to determine the differing dyadic profiles.
Materials and methods
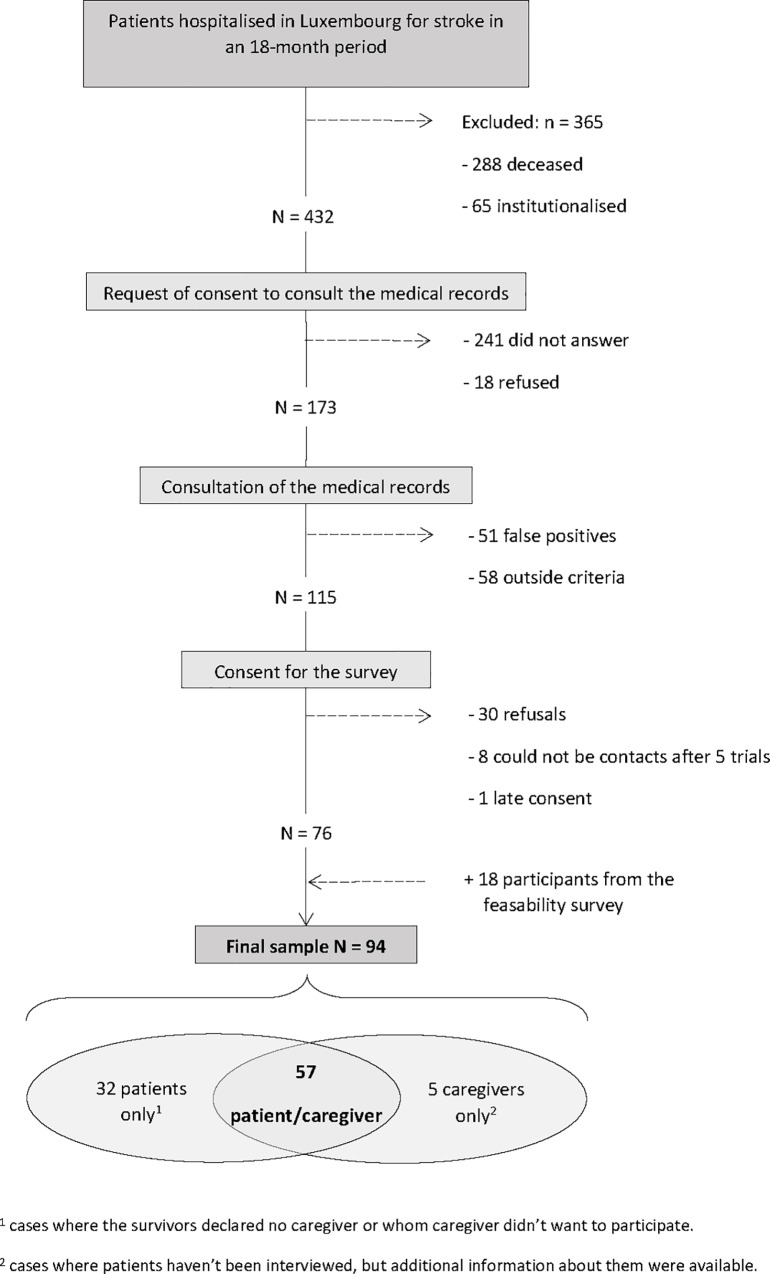
This study is part of a larger national survey on living at home two years after stroke in Luxembourg, conducted among all adult (≥18 years) survivors of stroke and their main family caregivers. Over a period of 18 months, the records of all the patients hospitalised two years earlier in Luxembourg (N = 797) were analysed (e.g., Fig 1).
Fig 1. Description of the sampling process.
Their status—living or deceased—was obtained from the Civil Status Registry. Survivors were drawn from the list compiled by the ‘Inspection Générale de la Sécurité Sociale’ of Luxembourg. Among the 432 eligible persons (living, not institutionnalised, residing in Luxembourg, contact information available), 173 gave their informed consent to have their medical records consulted by a practitioner investigator of the Research Centre for Health in Luxembourg. This step allowed to confirm the stroke diagnosis in 115 cases (the others were false positives or did not complete the clinical criteria of stroke). When returning an informed consent form to participate to a face-to-face interview, these were asked to identify their main caregivers as ‘the person[s] who mostly takes care of [them] since the stroke’. The final sample was composed of 94 participants, including 57 stroke survivor / caregiver dyads. Appointments was organised at their homes. Two researchers separately conducted face-to-face structured interviews supported by two distinct questionnaires: one for the survivors and one for the caregivers.
Ethical aspects
The protocol was approved by the National Committee of Research Ethics (CNER) and reported to the Committee for Data Protection of Luxembourg.
Data collected from both stroke survivors and family caregivers
The attitudes towards the most frequently experienced emotional and social repercussions of stroke were assessed by 11 items [6] identified through a content analysis of 10 interviews and after a qualitative process of generating questionnaire items [29]. The items measured three effects of stroke on the patient (character change, feeling demeaned, and feeling ashamed to see friends), four impacts on the family (whether stroke led to an upheaval in the family and in the couple, children distancing, and strengthening of family bonds), and four extended social repercussions (whether they received expressions of sympathy, whether friendship bonds were strengthened, whether they lost friends, and whether their social life was maintained as before). The attitudes were measured on a 4-point Likert scale ranging from ‘totally disagree’ to ‘completely agree’.
The following socio-demographic characteristics were assessed: age, sex, educational level (below 12th grade; 12th grade and above), occupational activity at the time of stroke onset (never employed; manual worker; employee/executive manager/technician; manager/liberal profession), changes in financial situation due to stroke (yes; no).
Data collected from stroke survivors
Neurological impairments of the motor, sensory, and visual functions, incontinence, and memory and language impairments were assessed, as identified by the American Heart Association Stroke Outcome Classification (AHA.SOC) [30]. The number of affected domains was expressed in four categories: ‘no impaired domain’, ‘one impaired domain’, ‘two impaired domains’, and ‘more than two impaired domains’.
Statistical analysis
The items assessing the emotional and social repercussions of stroke were dichotomised into ‘agree’ and ‘disagree’. The response distribution was analysed using percentages, means, and standard deviations when appropriate. The concordance between patients’ and caregivers’ attitudes was measured using the kappa concordance coefficient. A significant kappa indicates that the response distribution is not due to chance. A non-significant kappa indicates that there are substantial discordance among the responses, but does not provide information regarding the type of discordance—do patients tend to agree and caregivers disagree or vice versa versus both patients and caregivers agreeing or disagreeing at the same frequency? In order to complete the discordance analysis, a panel of experts composed of psychologists, neurologists, and members of the research unit jointly selected items to be analysed more deeply to illustrate the situation [29]. After presenting the response distribution, a group of discordant dyads was isolated by creating a binary variable (i.e. ‘caregiver agrees and patient disagrees’ vs. ‘others’) and entered as the dependent variable of a logistic regression. This method allowed us to identify the weight of each adjusted independent variable relative to the others. The independent variables were sex and age of the patients and the caregivers, the patients’ impaired motor, visual, and sensory functions, incontinence, and residual language and memory disabilities.
Results
Among the 57 patient-caregiver dyads, one patient did not respond to any of the items; thus, the sample size decreased to 56 dyads. Of these, 50 dyads were composed of couples (89.3%), and 32 (64%) had wife caregivers and 18 (36%) husband caregivers. In the six remaining dyads, five caregivers were women (83.3%), mainly daughters caring for a parent, and one was another family member—not specified. A majority of households had completed at least 12 years of education.
Profiles of the respondents and the dyads
Two-thirds of the affected individuals were men, with an average age of 63.3 years. Two years after stroke occurrence, 50% had residual sensory impairments, primarily pain. Nearly one-third had language and memory disorders, and 39.3% had sustained motor deficiencies. Nearly 43% of stroke survivors reported three or more impaired domains.
Among the caregivers, two-thirds were women, with an average age of 59 years. About 90% of these were the patients’ spouses. Results are detailed in Table 1.
Table 1. Socio-demographic and health characteristics of the 56 dyad members.
| Patients | Caregivers | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | % | n | % | ||||||
| Sex | Women | 21 | 37.5 | 36 | 64.3 | ||||
| Men | 35 | 62.5 | 20 | 35.7 | |||||
| Relationship to patient | Spouse | 50 | 89.3 | ||||||
| Child | 5 | 8.9 | |||||||
| Other | 1 | 1.8 | |||||||
| Educational level | Below 12th grade | 25 | 44.6 | 24 | 42.9 | ||||
| 12th grade and above | 31 | 55.4 | 32 | 57.1 | |||||
| Residual impairment domains | Motor | 22 | 39.3 | ||||||
| Vision | 12 | 21.4 | |||||||
| Sensory | 28 | 50.0 | |||||||
| Language | 18 | 32.1 | |||||||
| Memory | 21 | 37.5 | |||||||
| Character | 9 | 16.1 | |||||||
| Incontinence | 6 | 10.7 | |||||||
| Number of deficiencies | 0 | 13 | 23.2 | ||||||
| 1 | 10 | 17.9 | |||||||
| 2 | 9 | 16.1 | |||||||
| 3 or more | 24 | 42.9 | |||||||
| Age (mean, sd) | 63.3 (15.3) | 59.1 (13.8) | |||||||
Attitudes regarding emotional and social repercussions of stroke
Response distribution
As shown in Table 2, a majority of patients and caregivers reported that stroke had helped strengthen their bonds with their friends: They not only received expressions of sympathy, they were also able to maintain their social life as before the stroke.
Table 2. Patients' and caregivers' attitudes towards stroke repercussions and dyad concordance.
| Patients (n = 56) |
Caregivers (n = 56) |
||||||
|---|---|---|---|---|---|---|---|
| Agree | Disagree | Agree | Disagree | Concordance | |||
| % | % | % | % | % | K | P | |
| Social repercussions | |||||||
| 1. Upheaval in the family | 55.4 | 44.5 | 64.3 | 35.7 | 76.8 | 0.52 | 0.000*** |
| 2. Upheaval in the couple | 22.6 | 77.4 | 38.9 | 61.1 | 62.9 | 0.39 | 0.002** |
| 3. Distance with children | 08.2 | 91.8 | 09.8 | 90.2 | 66.1 | 0.14 | 0.319 |
| 4. Expressions of sympathy | 83.9 | 16.1 | 75.9 | 24.1 | 71.0 | 0.43 | 0.001*** |
| 5. Family bonds strengthened | 66.1 | 33.9 | 69.2 | 30.8 | 54.8 | 0.21 | 0.120 |
| 6. Friend bonds strengthened | 87.3 | 12.7 | 90.9 | 09.1 | 71.0 | 0.07 | 0.623 |
| 7. Loss of friends | 09.3 | 90.7 | 08.9 | 91.1 | 79.0 | 0.39 | 0.003** |
| 8. Social life maintained | 73.2 | 26.8 | 80.4 | 19.6 | 67.6 | 0.30 | 0.020* |
| Emotional repercussions on the patient | |||||||
| 9. Patient feels demeaned | 44.6 | 55.4 | 25.5 | 74.5 | 51.6 | 0.20 | 0.121 |
| 10. Patient’s personality changed | 42.9 | 57.1 | 53.6 | 46.4 | 64.5 | 0.43 | 0.001*** |
| 11. Patient ashamed of seeing friends | 12.5 | 87.5 | 03.6 | 96.4 | 79.0 | 0.18 | 0.102 |
Significance levels:
*p<0.05
**p<0.01
***p≤0.001.
In contrast, patients as well as caregivers mostly disagreed with the statements that the patient was ashamed of seeing friends, the stroke had put a distance between them and their children, and they had lost friends.
However, more than half of the caregivers stated that the personality of the affected person had changed vs. 43% of the patients. Nearly 45% of the survivors felt demeaned vs. only 25.5% of their caregivers.
More than 55% of the survivors (vs. 64.3% of the caregivers) felt that the stroke had brought an upheaval in their family while 22.6% (vs. 38.9%) reported that stroke had brought an upheaval in their couple relationship.
Concordance
Percentage of concordance between patients and their caregivers’ statements (Table 2) ranged from 51.6% (patient’s feeling demeaned) to 79% (shame of seeing friends and loss of friends).
The most concordant items concerned the attitude towards the upheaval the stroke had brought to the family (κ = .52), the patient’s personality change and expressions of sympathy (κ = .43), and upheaval the stroke had brought to the couple and loss of friends (κ = .39).
In contrast, attitudes of caregivers and patients were less concordant with regard to whether the stroke had strengthened bonds with friends (κ = .07), led to children distancing (κ = .14), and whether the patients felt demeaned (κ = .20).
Illustration and discordant dyad profiles
Patients’ and caregivers’ responses to the items questioning the patients’ feeling demeaned and ashamed, the patients’ personality change, and upheaval in the couple are shown in Table 3.
Table 3. Response distribution for the four illustrative items.
| The patient feels demeaned | ||||
| Patients | ||||
| Agree | Disagree | Total | ||
| Caregivers | Agree | 08 | 05 | 13 |
| Disagree | 14 | 24 | 38 | |
| Total | 22 | 29 | 51 | |
| The patient is ashamed of seeing friends | ||||
| Patients | ||||
| Agree | Disagree | Total | ||
| Caregivers | Agree | 1 | 01 | 02 |
| Disagree | 6 | 48 | 54 | |
| Total | 7 | 49 | 56 | |
| The patient’s personality changed | ||||
| Patients | ||||
| Agree | Disagree | Total | ||
| Caregivers | Agree | 19 | 11 | 30 |
| Disagree | 05 | 21 | 26 | |
| Total | 24 | 32 | 56 | |
| Stroke brought serious upheaval in our couple | ||||
| Patients | ||||
| Agree | Disagree | Total | ||
| Caregivers | Agree | 09 | 11 | 20 |
| Disagree | 03 | 30 | 33 | |
| Total | 12 | 41 | 53 | |
The results of logistic regressions of these four items on discordant dyads are presented in Table 4.
Table 4. Logistic regressions of the discordant groups for the four items.
|
The stroke-affected person feels demeaned |
The patient is ashamed to see friends |
The patient’s personality is changed |
Stroke brought serious upheaval in our couple relationship | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | S.E. | p | B | S.E. | p | B | S.E. | p | B | S. E. | p | ||
| Intercept | -2.04 | 2.91 | 0.482 | -8.92 | 4.47 | 0.046 | -1.75 | 4.32 | 0.686 | -1.97 | 2.11 | 0.350 | |
| Age of the caregiver | -0.06 | 0.05 | 0.235 | -0.01 | 0.07 | 0.930 | 0.04 | 0.06 | 0.432 | -0.08 | 0.06 | 0.226 | |
| Age of the patient | 0.03 | 0.04 | 0.455 | 0.03 | 0.06 | 0.603 | -0.04 | 0.05 | 0.442 | 0.06 | 0.06 | 0.272 | |
| Sex of the caregiver | Women | 1.69 | 2.12 | 0.424 | 2.82 | 2.80 | 0.313 | 0.95 | 3.91 | 0.809 | - | - | |
| Men | - | - | - | - | - | ||||||||
| Sex of the patient | Women | 1.17 | 1.98 | 0.554 | 2.31 | 2.31 | 0.316 | -1.62 | 3.87 | 0.675 | - | - | |
| Men | - | - | - | - | - | ||||||||
| Motor impairment | Yes | 0.60 | 0.90 | 0.507 | 0.35 | 1.37 | 0.798 | 0.38 | 0.95 | 0.691 | 2.14 | 1.00 | 0.027* |
| No | - | - | - | 0 | - | ||||||||
| Vision impairment | Yes | -0.52 | 1.05 | 0.622 | 0.48 | 1.18 | 0.686 | -0.38 | 1.08 | 0.725 | -1.83 | 1.24 | 0.142 |
| No | - | - | - | 0 | - | ||||||||
| Sensory impairment | Yes | 0.28 | 0.97 | 0.773 | 0.63 | 1.70 | 0.710 | 0.71 | 0.91 | 0.434 | 0.10 | 1.00 | 0.922 |
| No | - | - | - | 0 | - | ||||||||
| Language impairment | Yes | 2.11 | 1.00 | 0.036* | 2.56 | 1.37 | 0.063# | -0.25 | 1.01 | 0.808 | -1.04 | 1.09 | 0.342 |
| No | - | - | - | 0 | - | ||||||||
| Memory impairment | Yes | -0.86 | 1.00 | 0.393 | 0.17 | 1.21 | 0.887 | -1.01 | 1.03 | 0.331 | 1.38 | 0.88 | 0.115 |
| No | - | - | - | 0 | - | ||||||||
| Incontinence | Yes | 2.73 | 1.47 | 0.064# | -1.37 | 2.05 | 0.505 | -0.79 | 1.41 | 0.574 | - | - | |
| No | - | - | - | - | - | ||||||||
Significance levels:
#p<0.1
*p<0.05.
Demeaning
Among the 22 dyads in which the patients stated that he/she felt demeaned, 14 caregivers disagreed with this assessment. Dyads with a higher probability of reporting this type of discordance were those consisting of stroke survivors suffering from language impairments and incontinence.
Shame
Among the seven dyads with patients reporting that they felt ashamed to see friends, only one caregiver corroborated this feeling. Discordance was rather observed in dyads whose patient presented language impairments.
Personality change
Even though 30 caregivers reported that the personality of the stroke survivor had changed, 11 of the patients they cared for felt their personality was the same as before the stroke. In our analyses, this discordance type was not associated with any socio-demographic feature or type of impairment of the patient.
Couple upheaval
In our sample, 20 caregivers declared that stroke had brought an upheaval in their couple relationship, while 11 of their patients did not agree. This discordance type only occurred in dyads where the caregiver was female and the patient male, and particularly when the patient suffered from motor impairments. No such discordance appeared when the patient was incontinent.
Discussion
Our study analysed the concordance of attitudes between patients and their caregivers towards the emotional and social repercussions of stroke and determined the differing dyadic profiles. The attitudes of both family caregivers and stroke survivors towards the social repercussions of stroke were similar. Stroke patients with motor deficiencies tended to underestimate the upheaval brought to their couple relationship due to the event, whereas caregivers of language-impaired relatives tended to underestimate their feelings of shame and feeling demeaned. Caregivers generally tended to overestimate the upheaval on the couple and the patients’ personality change. Thus, communication disturbances, but also residual physical disabilities, may affect the understanding of each other’s attitudes within dyads.
Couple upheaval was more of a concern for family caregivers than for patients. Similarly, family caregivers also perceived a change in their stroke-affected relatives’ personality. Our study shows that family caregivers, more than the patients, experience the relationship with the other as discontinuous compared to the pre-stroke period, suggesting that becoming family caregivers can be experienced as a biographical disruption [31] which may impair their sense of coherence and thus alter their health behaviours [32]. Research analysing the distortions between individual and dyadic strategies revealed that ill persons received more social support from their caregiver than the opposite [33]. Our findings may reflect that the caregivers are making noticeable efforts to maintain a normal lifestyle for the stroke survivors. Another possible interpretation of our results is that the patients’ relationship with their partners is not a priority for them because they already have to cope with functional impairments (particularly in the motor dimension), a decrease in their quality of life, socio-economic problems [34], and the fear of suffering a new stroke [35].
Our findings also show that it can be difficult for some family caregivers to detect negative affect (such as shame and feeling demeaned) in stroke patients, especially when the stroke survivors suffer from language impairments. Shame is known to be one of the least shared emotions [36]. In the context of chronic disease, shame can be elicited by moralising health professionals [36] or the weight of social norms. In the latter condition, shame is a response to a social vulnerability to stigma [37, 38], as is reported by patients with Parkinson’s disease or lung cancer. In order to maintain their self-esteem and not add an additional burden of social support to be provided by their caregivers, some affected patients may hide their negative affect in front of others [24]. The frequency of discordant attitudes indicates that shame is an intimate feeling, but also suggests that some stroke survivors are confronted with a stigmatisation of their handicaps/disabilities [6]. Experiencing shame has been shown to have positive effects on the survivors’ motivation towards health behaviours [39]. However, further studies are necessary to identify to what extent keeping this emotion to themselves is actually beneficial or not for their wellbeing, and whether it indicates the quality of the relationship with their partners. On the other hand, one should be attentive to the possibility that some caregivers have set up a negative dyadic coping strategy consisting of not paying attention to the survivors’ affects, as observed in depressed individuals [37]. Our findings should also not obscure the fact that a majority of the patients did not report feeling ashamed in front of friends.
Of the four analysed discordant socio-demographic dyadic profiles, one was strongly related to the gender of caregivers; indeed, gender studies report that discordance regarding the level of quality of life of survivors is higher in couples where the caregiver is a woman [26], and that female spouses tend to be overprotective towards their ill counterpart [38]. The discordance of attitudes towards the upheaval in the couple only occurs in female caregiver/male patient dyads. Based on a feminist approach, this tendency of withholding their own feelings is typically observed in women, as a study describing shame in women with chronic pain has shown [40]. Accordingly, the patients may not even notice the magnitude of the changes. This finding underscores the notion that the caregiving role still has gendered specificities [41].
The social repercussions of stroke affected the survivors and the caregivers similarly. Our results show that while family caregivers do not carry the effects of stroke within them, they are affected by its social impacts. In addition to impairing their physical [42] and psychological [43–45] health, caring can also deteriorate its social dimension. Attending to social networks may require an additional effort on their part, especially when they fear leaving the patients alone [6].
None of the attitudes regarding the social repercussions experienced in common by the survivors and caregivers received total concordance. The recent interest for analysing the patient/caregiver as an entity [11] must not obscure the fact that patients and caregivers perceive their reality individually through their own filters [46]. Can such discordances be beneficial to the dyads’ balance? One can assume that caregivers who identify the accurate emotions of the survivors will probably be better able to respond adequately, which will in turn improve the quality of their relationship. For example, caregivers who do not perceive that their relatives feel ashamed in front of friends can interpret their desire to stay at home as laziness or unwillingness. This competence has been, for example, conceptualised through family caregiving skills, and includes accurate monitoring and interpretation [47].
The dissimilarities in attitudes observed in our study indubitably draw attention on the need to provide information to both survivors and caregivers. Actions addressed to dyads can improve the content of the relationship and the caregivers’ health [48]. Moreover, a high reciprocity and exchange in regard to feelings between patients and their caregivers has been shown to decrease the caregiving burden [49]. Eliciting communication among the dyads could enhance the experience of living after a stroke, for both the patients and their caregivers.
Limitations
Inherent limitations to our study are linked to the small size of our sample and the high rate of mortality two years post-stroke as well as to the size of the Luxembourg, which is one of the smallest countries in Europe. In particular, it results in low power for the tests performed. We did not made any adjustment to take into account for the multiple tests.
From a methodological standpoint, some limits should be acknowledged, such as the drawbacks of the kappa concordance coefficient. For example, concordance rates of only 63% for the ‘upheaval in the couple’ and ‘patient’s personality change’ were significant. This phenomenon has been described in the literature as a paradox [50, 51]. The microanalyses performed here nevertheless overcame these drawbacks and allowed a more in-depth understanding of our results.
In addition, the Luxembourg national survey did not gather information on comorbidities, especially of mental health—such as comorbid depression, anxiety, and psychological distress—which could explain, at least to some extent, the differences that were obtained here [52]. Therefore, for further research, the consequences of the emotional states of stroke patients and their caregivers should be controlled with respect to mental health variables to enable a more careful interpretation of the results.
Practice implications
Patient education in the chronic phase of stroke could be improved by addressing dyads as a whole, rather than only one of the members. Initiatives have already been taken in the field of psychological distress, which consist of regular meetings between survivors, caregivers, and health professionals. These ‘trialogues’ help people interact, understand each other, and find innovative solutions to their daily challenges [53].
Our recommendations focus on the need for professionals to accompany survivors and their caregivers in their lives after stroke, in the sense of more reciprocity and mutual comprehension. For this purpose, proposing services aimed at promoting communication of emotions within the dyads would help to harmonise the giving-receiving balance, including facilitating emotion sharing as well as developing the caregivers’ caregiving skills and, empowerment, and to reduce the stigmatizsation [54]. Healthcare professionals should also be attentive to those dyads where the survivors suffer from language impairments, especially in cases of aphasia, since they are more vulnerable to misunderstandings while sharing their emotions.
A satisfactory relationship with an ill partner is associated with less caregiving burden. It is also related to better communication within the couple [55]. Thus, actions aimed at promoting communication between partners are expected to improve the wellbeing of caregivers. Although each partner should have the choice to maintain some level of intimacy, it is the duty of the healthcare and social practitioners to create the best environment possible to promote fruitful exchange within the dyad.
Conclusions
In the chronic phase following stroke, family caregivers’ and survivors’ attitudes towards social repercussions of stroke are similar. The upheaval felt on the level of the couple was even higher for caregivers than for the survivors. Together, they have to cope with the social isolation potentially incurred by the stroke. Negative affects experienced by the survivors, such as shame and feeling demeaned, are not necessarily perceived by their caregivers, which may be associated with inadequate responses to the survivors’ needs. The dissimilarities in attitudes raise the question as to the quality of the relationship between two relatives where one takes care of the other. Further research may help in finding means to enhance the communication between the members of the dyads, which would help reinforce their respective health capability [56].
Supporting information
(DOCX)
Data Availability
Data are available from the IRSEI for researchers who meet the criteria for access to INSIDE Data. These criteria are similar to those fixed by Eurostat. http://ec.europa.eu/eurostat/web/microdata/overview. Researchers may contact the management board and Pr Michèle Baumann, Unit INSIDE, Institute IRSEI, Maison des Sciences Humaines, 11 Porte des Sciences. L-4366 Esch/sur/Alzette, Luxembourg.
Funding Statement
The authors are grateful for the financial support received from the Luxembourg National Research Fund, the grant number of the project was FNR/VIVRE/06/06/06. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO. Global status report on non-communicable diseases. Report World Health Organization Geneva, Switzerland, 2014. ISBN 978 92 4 156485 4 [http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf]
- 2.OECD. Health at a Glance 2017: OECD Indicators, OECD Publishing, Paris: [ 10.1787/health_glance-2017-en] [DOI] [Google Scholar]
- 3.Baumann M, Lurbe-Puerto K, Bucki B. Harmony and divergences in couples. Family and social implications two years post-stroke. Sc. Ann Alexandru Ioan Cuza Univ New Ser Sociol Soc Work Sect. 2012; 5: 155–173. [Google Scholar]
- 4.Baumann M, Couffignal S, Le Bihan E, Chau N. Life satisfaction two-years after stroke onset: the effect of gender, occupational status, memory function and quality of life among patients (Newsqol) and their family caregivers (Whoqol-bref) in Luxembourg. BMC Neurol 2012; 12: 105–116. 10.1186/1471-2377-12-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Standing Committee for the Social Sciences. Developing a new understanding of enabling health and wellbeing in Europe, European Science Foundation; Ed. Strasbourg; 2013. [https://ec.europa.eu/eip/ageing/library/developing-new-understanding-enabling-health-and-wellbeing-europeharmonising-health-and_en] [Google Scholar]
- 6.Lurbe-Puerto K, Leandro ME, Baumann M. Experiences of caregiving, satisfaction of life, and social repercussions among family caregivers, two years post-stroke. Soc. Work Health Care 2012; 51: 725–742. 10.1080/00981389.2012.692351 [DOI] [PubMed] [Google Scholar]
- 7.Bucki B. Health capability: an attempt to clarify an alternative approach for health sociology. Sc. Ann Alexandru Ioan Cuza Univ. New Ser Sociol Soc Work Sect 2014; 7: 19–31. [Google Scholar]
- 8.Ruger JP. Health capability: conceptualization and operationalization. Am J Public Health 2010; 100: 41–49. 10.2105/AJPH.2008.143651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Untas A, Koleck M, Rascle N, Bruchon-Schweitzer M. From the transactional model to a dyadic approach in health psychology. Psychol Fr. 2012; 57: 97–110. [Google Scholar]
- 10.Baumann M, Bucki B. Lifestyle as a health risk for family caregivers with least life satisfaction, in home-based post-stroke caring. Healthcare Policy 2013; 9: 98–111. [PMC free article] [PubMed] [Google Scholar]
- 11.Molloy GJ, Johnston M, Johnston DW, Pollard B, Morrison V, Bonetti D, Joice S & MacWalter R. Spousal caregiver confidence and recovery from ambulatory activity limitations in stroke survivors. Health Psychol 2008; 27: 286–290. 10.1037/0278-6133.27.2.286 [DOI] [PubMed] [Google Scholar]
- 12.Visser-Meily A, Post M, van de Port I, Maas C, Forsberg-Wärleby G, Lindeman E. Psychosocial functioning of spouses of patients with stroke: from initial inpatient rehabilitation to 3 years poststroke course and relations with coping strategies. Stroke 2009; 40: 1399–1404. 10.1161/STROKEAHA.108.516682 [DOI] [PubMed] [Google Scholar]
- 13.Meeks BS, Hendrick SS, Hendrick C. Communication, love and relationship satisfaction. J Soc Pers Relatsh 1998; 15: 755–773. [Google Scholar]
- 14.Badr H, Acitelli LK. Dyadic Adjustment in chronic illness: does relationship talk matter? J Fam Psychol 2005; 19: 465–469. 10.1037/0893-3200.19.3.465 [DOI] [PubMed] [Google Scholar]
- 15.Warner LM, Schüz B, Wurm S, Ziegelmann JP, Tesch-Römer C. Giving and taking—differential effects of providing, receiving and anticipating emotional support on quality of life in adults with multiple illnesses. J Health Psychol 2010; 15: 660–670. 10.1177/1359105310368186 [DOI] [PubMed] [Google Scholar]
- 16.Spitz E, Sordes Ader F. Qualité de vie, entourage, soutien social, in: Qualité de Vie et Maladies Rénales Chroniques: Satisfaction Des Soins et Autres Patient-Reported Outcomes. 2007: 109–123. [Google Scholar]
- 17.Stone J, Townend E, Kwan J, Haga K, Dennis MS, Sharpe M. Personality change after stroke: some preliminary observations. J Neurol Neurosurg Psychiatry 2004; 75: 1708–1713. 10.1136/jnnp.2004.037887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baumann M, Le Bihan E, Chau K, Chau N. Associations between quality of life and socioeconomic factors, functional impairments and dissatisfaction with received information and home-care services among survivors living at home two years after stroke onset. BMC Neurol 2014; 14: 92–103. 10.1186/1471-2377-14-92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baumann M, Lurbe-Puerto K, Alzahouri K, Aïach P. Increased residual disability among poststroke survivors and the repercussions for the lives of informal caregivers. Top Stroke Rehabil 2011; 18: 162–171. 10.1310/tsr1802-162 [DOI] [PubMed] [Google Scholar]
- 20.Kvigne K, Kirkevold M, Gjengedal E. Fighting back-struggling to continue life and preserve the self-following a stroke. Health Care Women Int 2004; 25: 370–387. 10.1080/07399330490278376 [DOI] [PubMed] [Google Scholar]
- 21.Reed M, Harrington R, Duggan A, Wood VA. Meeting stroke survivors’ perceived needs: a qualitative study of a community-based exercise and education scheme. Clin Rehab 2010; 24: 16–25. [DOI] [PubMed] [Google Scholar]
- 22.Rimé B. Should we talk about emotions? [Faut-il parler de ses émotions ?]. Sci Hum 2000; 16–20. [Google Scholar]
- 23.Finkenauer C, Rimé B. Socially shared emotional experiences vs. emotional experiences kept secret: Differential characteristics and consequences. J Soc Clin Psychol 1998; 17: 295–318. [Google Scholar]
- 24.McPherson CJ, Wilson KG, Murray MA. Feeling like a burden: Exploring the perspectives of patients at the end of life. Soc Sci Med 2007; 64: 417–427. 10.1016/j.socscimed.2006.09.013 [DOI] [PubMed] [Google Scholar]
- 25.Jette AM, Ni P, Rasch EK, Appelman J, Sandel ME, Terdiman J, Chan L. Evaluation of patient and proxy responses on the activity measure for postacute care. Stroke 2012; 43: 824–829. 10.1161/STROKEAHA.111.619643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Low G, Gutman G. Couples’ Ratings of chronic obstructive pulmonary disease patients’ quality of life Clin Nurs Res 2003; 12: 28–48. 10.1177/1054773803238739 [DOI] [PubMed] [Google Scholar]
- 27.Silveira MJ, Given CW, Given B, Rosland AM, Piette JD. Patient-caregiver concordance in symptom assessment and improvement in outcomes for patients undergoing cancer chemotherapy. Chronic Illness 2010; 6: 46–56. 10.1177/1742395309359208 [DOI] [PubMed] [Google Scholar]
- 28.Sneeuw KC, Aaronson NK, Osoba D, Muller MJ, Hsu MA, Yung WK, Brada M, Newlands ES. The use of significant others as proxy raters of the quality of life of patients with brain cancer. Med Care 1997; 35: 490–506. [DOI] [PubMed] [Google Scholar]
- 29.Ricci L, Lanfranchi JB, Lemetayer F, Rotonda C, Guillemin F, Coste J, Spitz E. Qualitative methods used to generate questionnaire items: A systematic review. Qualitative Health Res 2018. 10.1177/1049732318783186. [DOI] [PubMed] [Google Scholar]
- 30.Kelly-Hayes M, Robertson JT, Broderick JP, Duncan PW, Hershey LA, Roth EJ, Thies WH, Trombly CA. The American heart association stroke outcome classification. Stroke 1998; 29: 1274–1280. [DOI] [PubMed] [Google Scholar]
- 31.Bury M. Chronic illness as biographical disruption. Sociol Health Illn 1982; 4: 167–182. [DOI] [PubMed] [Google Scholar]
- 32.Silarova B, Nagyova I, Rosenberger J, Studencan M, Ondusova D, Reijneveld SA, van Dijk JP. Sense of coherence as a predictor of health-related behaviours among patients with coronary heart disease. Eur J Cardiovasc Nurs 2013; 13(4): 345–356. 10.1177/1474515113497136 [DOI] [PubMed] [Google Scholar]
- 33.Meier C, Bodenmann G, Moergeli H, Peter-Wight M, Martin M, Buechi S, Jenewein J. Dyadic coping among couples with COPD: A pilot study. J Clin Psychol Med Settings 2012; 19: 243–254. 10.1007/s10880-011-9279-7 [DOI] [PubMed] [Google Scholar]
- 34.Baumann M, Lurbe K, Leandro ME, Chau N. Life satisfaction of two-year post-stroke survivors: Effects of socio-economic factors, motor impairment, NEWcastle Stroke-specific Quality Of Life measure and World Health Organization Quality Of Life–bref of informal caregivers in Luxembourg and a rural area in Portugal. Cerebrovasc Dis 2012; 33: 219–230. 10.1159/000333408 [DOI] [PubMed] [Google Scholar]
- 35.Salter K, Hellings C, Foley N, Teasell R. The experience of living with stroke: a qualitative meta-synthesis. J Rehabil Med 2008; 40: 595–602. 10.2340/16501977-0238 [DOI] [PubMed] [Google Scholar]
- 36.Rimé B. Emotion elicits the social sharing of emotion: Theory and empirical review. Emot Rev 2009; 1: 60–85. [Google Scholar]
- 37.Bodenmann G, Charvoz L, Widmer K, Bradbury TN. Differences in individual and dyadic coping among low and high depressed, partially remitted, and nondepressed persons. J. Psychopathol Behav Assess 2004; 26: 75–85. [Google Scholar]
- 38.Green TL, King KM. Experiences of male patients and wife-caregivers in the first year post-discharge following minor stroke: a descriptive qualitative study. Int J Nurs Stud 2009; 46; 1194–1200. 10.1016/j.ijnurstu.2009.02.008 [DOI] [PubMed] [Google Scholar]
- 39.Frich JC, Malterud K, Fugelli P. Experiences of guilt and shame in patients with familial hypercholesterolemia: a qualitative interview study. Patient Educ Couns 2007; 69: 108 10.1016/j.pec.2007.08.001 [DOI] [PubMed] [Google Scholar]
- 40.Werner A, Isaksen LW, Malterud K. “I am not the kind of woman who complains of everything”: Illness stories on self and shame in women with chronic pain. Soc Sci Med 2004; 59: 1035–1046. 10.1016/j.socscimed.2003.12.001 [DOI] [PubMed] [Google Scholar]
- 41.Bucki B, Spitz E, Baumann M. [Caring for a stroke victim: the emotional reactions of male and female caregivers]. Santé Publique 2012; 24: 143–156. [PubMed] [Google Scholar]
- 42.Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull 2003; 129: 946–972. 10.1037/0033-2909.129.6.946 [DOI] [PubMed] [Google Scholar]
- 43.Franzén-Dahlin A, Larson J, Murray V, Wredling R, Billing E. Predictors of psychological health in spouses of persons affected by stroke. J Clin Nurs 2007; 16: 885–891. 10.1111/j.1365-2702.2006.01744.x [DOI] [PubMed] [Google Scholar]
- 44.Han B, Haley WE. Family caregiving for patients with stroke review and analysis. Stroke 1999; 30: 1478–1485. [DOI] [PubMed] [Google Scholar]
- 45.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging 2003; 18: 250–267. [DOI] [PubMed] [Google Scholar]
- 46.Hafsteinsdóttir TB. Educational needs of patients with a stroke and their caregivers: a systematic review of the literature. Patient Educ Couns 2011; 851: 14–25. [DOI] [PubMed] [Google Scholar]
- 47.Schumacher KL, Stewart BJ, Archbold PG, Dodd MJ, Dibble SL. Family caregiving skill: development of the concept. Res Nurs Health 2000; 23: 191–203. [DOI] [PubMed] [Google Scholar]
- 48.Sebern MD, Woda A. Shared care dyadic intervention outcome patterns for heart failure care partners. West J Nurs Res 2012; 34: 289–316. 10.1177/0193945911399088 [DOI] [PubMed] [Google Scholar]
- 49.Reid CE, Moss S, Hyman G. Caregiver Reciprocity: The effect of reciprocity, carer self-esteem and motivation on the experience of caregiver burden. Aust J Psychol 2005; 57: 186–196. [Google Scholar]
- 50.Blum A, Feldmann L, Bresler F, Jouanny P, Briançon S, Régent D. [Measuring agreement as an evaluation of a diagnostic imaging method]. J Radiol 1995; 76: 441–443. [PubMed] [Google Scholar]
- 51.Feinstein AR, Cicchetti DV. High agreement but low kappa: I. the problems of two paradoxes. J Clin Epidemiol 1990; 43: 543–549. [DOI] [PubMed] [Google Scholar]
- 52.Möller-Leimkühler AM. Gender differences in cardiovascular disease and comorbid depression. Dialogues Clin Neurosci 2007; 9(1): 71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Amering M. Trialog-an exercise in communication between consumers, carers and professional mental health workers beyond role stereotypes. Int J Integr Care 2010; 10: Suppl, e014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Corrigan PW. Best practices: Strategic stigma change (SSC): Five principles for social marketing campaigns to reduce stigma. Psychiatr Serv 2011; 62(8): 824–826. 10.1176/ps.62.8.pss6208_0824 [DOI] [PubMed] [Google Scholar]
- 55.Steadman PL, Tremont G, Davis JD. Premorbid relationship satisfaction and caregiver burden in dementia caregivers. J Geriatr Psychiatry Neurol 2007; 20: 115–119. 10.1177/0891988706298624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bucki B, Spitz E, Etienne AM, Le Bihan E & Baumann M. Health capability of family caregivers: How different factors interrelate and their respective contributions using a Bayesian approach. BMC Public Health 2016; 16: 364 10.1186/s12889-016-3027-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Data are available from the IRSEI for researchers who meet the criteria for access to INSIDE Data. These criteria are similar to those fixed by Eurostat. http://ec.europa.eu/eurostat/web/microdata/overview. Researchers may contact the management board and Pr Michèle Baumann, Unit INSIDE, Institute IRSEI, Maison des Sciences Humaines, 11 Porte des Sciences. L-4366 Esch/sur/Alzette, Luxembourg.