Abstract
OBJECTIVE
Vancomycin is often used in the pediatric cardiac surgical population, but few pharmacokinetic data are available to guide dosing.
METHODS
A retrospective, population pharmacokinetic study was performed for patients <19 years of age initiated on vancomycin after cardiac surgery in the cardiac intensive care unit from 2011–2016 in our institution. Patient data were summarized by using descriptive statistical methods, and population pharmacokinetic analysis was performed by using NONMEM. Simulation was performed to determine a dosing strategy that most frequently obtained an AUC0–24:MIC (minimum inhibitory concentration) ratio of >400.
RESULTS
A total of 261 patients (281 cardiac surgical procedures, cardiopulmonary bypass 82.3%) met inclusion criteria (60.1% male, median age 0.31 [IQR, 0.07–0.77] years). Vancomycin (14.5 ± 1.7 mg/kg/dose) was administered at median postoperative day 9 (IQR, 4–14), with a mean serum concentration of 11.5 ± 5.5 mg/L at 8.9 ± 3.8 hours after a dose. Population pharmacokinetic analysis demonstrated that a 1-compartment proportional error model with allometrically scaled weight best fit the data, with creatinine clearance and postmenstrual age as significant covariates. Simulation identified that a dosing regimen of 20 mg/kg/dose every 8 hours was most likely to achieve an AUC0–24:MIC ratio > 400 at a mean trough serum concentration of 12.9 ± 3.2 mg/L.
CONCLUSIONS
Vancomycin dosing in the postoperative pediatric cardiac surgical population should incorporate postmenstrual age and creatinine clearance. A vancomycin dose of 20 mg/kg every 8 hours is a reasonable empiric strategy.
Keywords: cardiac surgery, NONMEM, pediatrics, population pharmacokinetics, simulation, vancomycin
Objective
Vancomycin is a widely used glycopeptide antimicrobial for the treatment and prophylaxis of Gram-positive infections in children. Multiple pharmacokinetic studies have been performed with vancomycin in the general pediatric population and pediatric subpopulations, such as patients with malignancy or critical illness.1–6 Each of these subpopulations has unique characteristics that could potentially alter the pharmacokinetics of vancomycin, resulting in suboptimal outcomes. Pediatric patients who have undergone a cardiac surgical procedure are known to have alterations in physiology, such as volume status and kidney function, that could potentially affect vancomycin disposition, as vancomycin is primarily excreted through glomerular filtration and 80% to 90% of the drug is recovered unchanged in the urine.7–10
After cardiac surgery patients are at a high risk for acute kidney injury for a multitude of reasons including low cardiac output syndrome, venous congestion, and impaired kidney perfusion.7 The use of cardiopulmonary bypass induces an inflammatory state that alters vascular permeability and end-organ perfusion, further contributing to acute kidney injury.11 Patients often receive large doses of diuretics in the postoperative period and subsequently can have rapid shifts in fluid status and changes in urine output.12 Patients may also experience acute kidney injury due to nephrotoxin exposure in the postoperative period. Because vancomycin is a potential nephrotoxin, particularly in the setting of other nephrotoxic medications, a careful dosing strategy is necessary to optimize vancomycin concentrations while avoiding toxicity.7
For these reasons, an analysis of the pharmacokinetics of vancomycin in the postoperative pediatric cardiac surgical population is warranted. Description of the pharmacokinetic parameters in this patient population and covariates that alter vancomycin pharmacokinetics can be used to develop empiric dosing regimens that achieve therapeutic endpoints while minimizing adverse events.
Methods
The study was approved by the Baylor College of Medicine Institutional Review Board. A retrospective descriptive population pharmacokinetic study was designed and patients were identified by querying the hospital pharmacy system from 2011–2016. Patients were included in the study if they were <19 years of age, initiated on vancomycin therapy in the cardiac intensive care unit at our institution after a cardiac surgical procedure, and had 1 or more serum vancomycin concentrations sampled. Patients were excluded if they were undergoing any type of renal replacement therapy, including peritoneal dialysis for fluid mobilization, or mechanical circulatory support (including ventricular assist devices) or had vancomycin administered intra-operatively while undergoing cardiopulmonary bypass.
Data collection included patient date of birth, gestational age, weight, height, cardiac surgical procedure and date of surgical procedure, use of cardiopulmonary bypass (CPB), length of CPB in minutes, serum creatinine (SCr) values throughout the vancomycin course, urine output during the previous 12 hours, vancomycin dose, and vancomycin serum concentrations. Presence of delayed sternal closure in the intensive care unit was also noted. Patient data were collected for up to 30 days after the cardiac surgical procedure.
Vancomycin serum concentrations were collected in either a 1 × 0.6 mL Amber Microtainer with Gel or 1 × 1 mL Red/Black Serum Separator Vacutainer. The vancomycin assay was performed by using the VIT-ROS Chemistry Products VANC Reagent in conjunction with the VITROS Chemistry Products Calibrator Kit 11 on the VITROS 5600 Integrated System (Ortho Clinical Diagnostics, Raritan, NJ). The assay is based on competition between vancomycin in the sample and vancomycin labeled with Glucose-6-phosphate dehydrogenase (G6P-DH) for antibody binding sites. Activity of G6P-DH decreases upon binding to the antibody; therefore, vancomycin concentration in the sample can be measured in terms of G6P-DH activity. The analytic measurement range was 5 to 50 mg/L. The coefficient of variation was <6%.
Descriptive Analysis. The patient population was described by using percentages, mean, standard deviation, median, and range, for normally and non-normally distributed data, as appropriate. Postmenstrual age (PMA) was calculated in weeks. Creatinine clearance (CrCL) was calculated according to the bedside Schwartz equation.13 Graphical representation of the initial data was also used. Statistical analyses were performed by using Stata IC v.12 (StataCorp, College Station, TX) and Excel 2013 (Microsoft Corp, Redmond, WA).
Pharmacokinetic Analysis. Population pharmacokinetic analysis was performed with NONMEM v.7.3 (Icon PLC, Dublin, Ireland) and PDx-Pop 5.1 (Icon PLC) by using first-order conditional estimation with interaction. The base model was developed through analysis of prior literature and visually evaluating graphs of serum concentrations of vancomycin after dosing (Figure 1). Interindividual variability was modeled exponentially.
Figure 1.
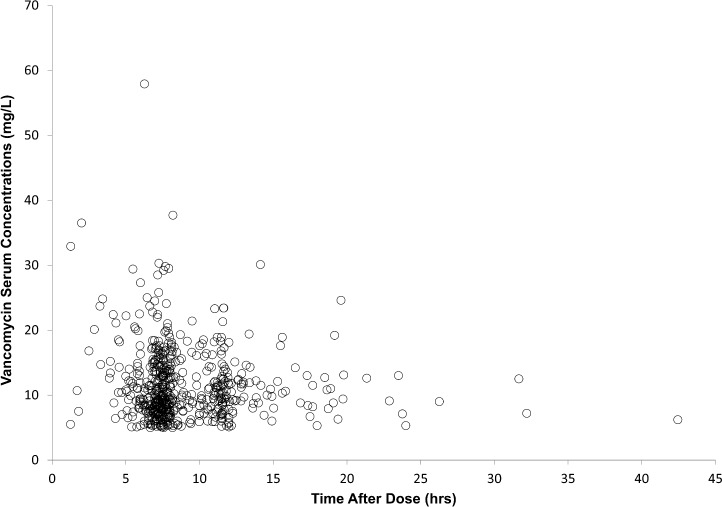
Vancomycin serum concentrations versus time after a vancomycin dose.
Potentially significant covariates were plotted against pharmacokinetic parameters to initially evaluate suitability for inclusion in the model. Power, linear, and linear proportional models were evaluated with continuous covariates. Categorical covariates were modeled exponentially. Covariates were included in the base model if a reduction in the objective function value (OFV) was >3.84, signifying statistical significance (p < 0.05). After significant covariates were identified, a full model, containing all significant covariates, was developed. Individual covariates were then removed from the model and were then considered to be retained in the model if the OFV increased by >10.83, which has a significance level of p < 0.001.
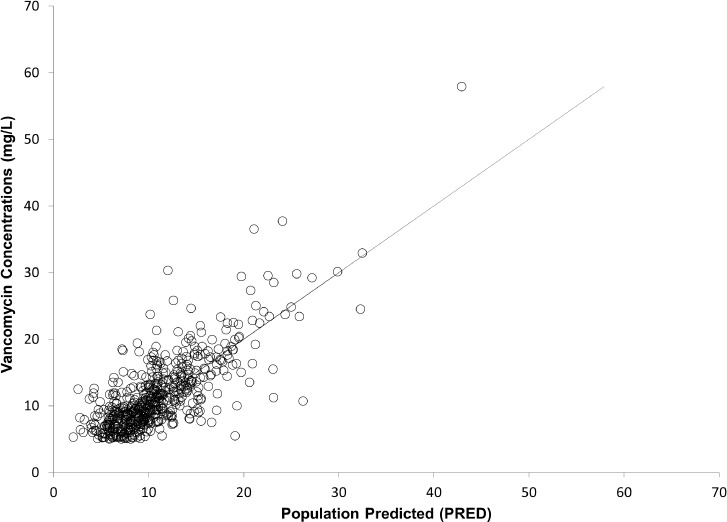
Scatter plots of dependent variables versus individual-predicted (IPRE) and population-predicted (PRED) vancomycin serum concentrations, as well as conditional weighted residuals (CWRES) versus predicted (PRED) concentrations and time after dose, were created to evaluate model goodness of fit and detect bias. Bootstrap simulations were performed (n = 1000) on the final model with calculation of 95% confidence intervals.
A simulation was run (n = 10,000 replications) on the final model from a virtual patient, developed from median values of covariates to identify potential empiric dosing recommendations. Median values were chosen for a simulation, as this would be representative of patients undergoing cardiac surgery at our institution. Five different dosing regimens were evaluated: 10 mg/kg/dose every 6 hours, 15 mg/kg/dose every 8 hours, 15 mg/kg/dose every 6 hours, 20 mg/kg/dose every 8 hours, and 20 mg/kg/dose every 8 hours. Samples in the simulation were drawn before the fourth dose for every 8-hour dosing, and before the fifth dose for every 6-hour dosing. An AUC0–24:MIC (minimum inhibitory concentration) ratio was calculated as based on a Staphylococcus aureus MIC of 1. Dosing strategies were identified that obtained a high percentage of simulations that had an AUC0–24:MIC ratio of >400 while maintaining trough serum concentrations of <15 mg/L.
Results
Demographics. A total of 261 patients underwent 281 cardiac surgical procedures and met inclusion criteria (Tables 1 and 2). In total, most patients were younger than 1 year, 67 patients (25.7%) were >1 year of age, and 8 patients (3.1%) were ≥13 years of age. Patients received the following continuous infusion inotropic/vasopressor medications while on vancomycin therapy: milrinone (58.6%), epinephrine (24.9%), vasopressin (14.5%), and calcium chloride (7.6%). Patients received a mean vancomycin dose of 14.5 ± 1.7 mg/kg/dose. Serum concentrations below the limit of quantification (5 mg/L) were <10% of the total serum concentrations and were excluded from the analysis, resulting in 578 serum vancomycin concentrations analyzed. The mean serum concentration was 11.5 ± 5.5 mg/L, which was drawn at a mean of 8.9 ± 3.8 hours after a dose.
Table 1.
Demographic Variables
| Category (N = 261) | Value |
|---|---|
| Male, % | 60.1 |
| Gestational age, wk, median (IQR) | 38.7 (37.1–40) |
| Age, yr, median (IQR) | 0.31 (0.07–0.77) |
| Postmenstrual age, wk, median (IQR) | 54.6 (42.6–76.9) |
| Height, cm, median (IQR) | 58 (51.5–67.1) |
| Weight, kg, median (IQR) | 4.8 (3.4–7.4) |
| Postoperative day, median (IQR) | 9 (4–14) |
| Cardiopulmonary bypass, % | 82.3 |
| Cardiopulmonary bypass time, min, mean ± SD | 207 ± 88 |
| Open sternum post surgery, % | 3.1 |
| Serum creatinine, mg/dL, median (IQR) | 0.32 (0.25–0.41) |
| Creatinine clearance, mL/min/1.73 m2, median (IQR) | 84 (58–108) |
| Urine output over previous 12 hr, mL, median (IQR) | 226 (150–345) |
| Urine output over previous 12 hr, mL/kg/hr, mean ± SD | 3.9 ± 2.1 |
Table 2.
Cardiac Surgical Procedures
| Cardiac Surgical Procedure (N = 281) | n (%) |
|---|---|
| Bidirectional Glenn | 31 (11.0) |
| Norwood | 29 (10.3) |
| Tetralogy of Fallot repair | 21 (7.5) |
| Ventricular septal defect closure | 20 (7.1) |
| Complete atrioventricular canal | 18 (6.4) |
| Blalock-Taussig shunt placement | 13 (4.6) |
| Mitral valve repair | 13 (4.6) |
| Aortic arch advancement | 12 (4.3) |
| Fontan | 12 (4.3) |
| Coarctation of the aorta repair via thoracotomy | 10 (3.6) |
| Orthotopic heart transplant | 10 (3.6) |
| Arterial switch operation | 9 (3.2) |
| Placement of pulmonary artery band | 9 (3.2) |
| RV-PA conduit placement | 9 (3.2) |
| Pacemaker placement | 6 (2.1) |
| Aortic valve replacement | 5 (1.8) |
| Repair of total anomalous pulmonary venous return | 5 (1.8) |
| ALCAPA repair | 4 (1.4) |
| Atrial septal defect/ventricular septal defect repair | 4 (1.4) |
| Mee shunt placement | 4 (1.4) |
| Repair of interrupted aortic arch | 3 (1.1) |
| Ligation of patient ductus arteriosus | 3 (1.1) |
| Rastelli procedure | 3 (1.1) |
| Other | 28 (10.0) |
ALCAPA, Anomalous Left Coronary Artery to Pulmonary Artery; RV-PA, Right ventricular to Pulmonary Artery
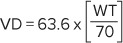
Pharmacokinetic Modeling. A 1-compartment proportional error model, using first-order conditional estimation with interaction, best fit the data. Weight with allometric scaling on clearance (CL) (0.75) and volume of distribution (VD) (1) was added to the model with a subsequent reduction in the OFV of −302.446. The model with allometrically scaled weight was used for further covariate analysis. Covariates were added to the model one at a time and were considered to have a significant effect on the model if the OFV was reduced by >3.84 (Table 3). After backwards elimination of covariates, the remaining covariates were CrCL and PMA on CL, and this model resulted in a difference in OFV from the full model of 24.524. Urine output over the previous 12 hours had a strong association with CL graphically but did not meet criteria during the backwards stepwise removal of covariates. The final model consisted of weight with allometric scaling on CL and VD, and PMA and CrCL on CL (Table 4). Diagnostic plots demonstrated good model fit with low bias (Figures 2 through 5). Bootstrap analysis of 1000 runs was performed and 99.8% of runs successfully minimized (Table 5).
Table 3.
Individual Covariate Analysis
| 1-Compartment Model (N = 261) | OFV (change from base model) | |
| CL = (WT/70) ^ 0.75; VD = WT/70 | 2721.201 | |
| Clearance (change from allometric WT) | ||
| *(SCr/0.4) ^ Θ | 2111.387 (−307.368) | |
| *(CrCL/84) ^ Θ | 1827.299 (−893.902) | |
| * Θ ^ (OPNSTR) | 2411.002 (−7.753) | |
| * Θ ^ (CPB) | 2403.192 (−15.563) | |
| * Θ ^ ((UOP + 1)/293) | 2393.425 (−25.33) | |
| *(1/(1 + (PMA/50) ^ Θ)) | 2305.798 (−112.957) | |
| * Θ ^ (LOG((POD + 0.01)/9)) | 2406.806 (−11.949) | |
| Volume of Distribution (change from allometric WT) | ||
| * Θ ^ ((UOP + 1)/293) | 2414.172 (−4.583) | |
| * Θ ^ (LN((POD + 0.01)/9)) | 2418.754 (−0.001) | |
| *(AGEYRS/1.5) ^ Θ | 2398.898 (−19.857) | |
| * Θ ^ OPNSTR | 2415.669 (−3.086) | |
| * Θ ^ CPB | 2418.735 (−0.02) | |
| * Θ ^ M | 2416.777 (−1.978) | |
Θ, estimate; AGEYRS, age in years; CL, clearance; CPB, cardiopulmonary bypass; CrCL, creatinine clearance; LN, natural log; M, male; OFV, objective function value; OPNSTR, open sternum; PMA, postmenstrual age (wk); POD, postoperative day; SCr, serum creatinine (mg/dL); UOP, urine output over the previous 12 hours (mL); VD, volume of distribution; WT, weight (kg)
Table 4.
Final Model and Variability
| Model (n = 261) | IIV, % | Residual Variability, % |
|---|---|---|
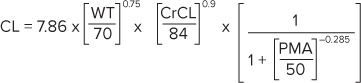 |
17.4 | 19.9 |
 |
25.5 |
CL, clearance (L/hr); CrCL, creatinine clearance; IIV, interindividual variability; PMA, postmenstrual age (wk); VD, volume of distribution (L); WT, weight (kg)
Figure 2.
Dependent variables versus population-predicted concentrations. There is agreement along the line of unity.
Figure 5.
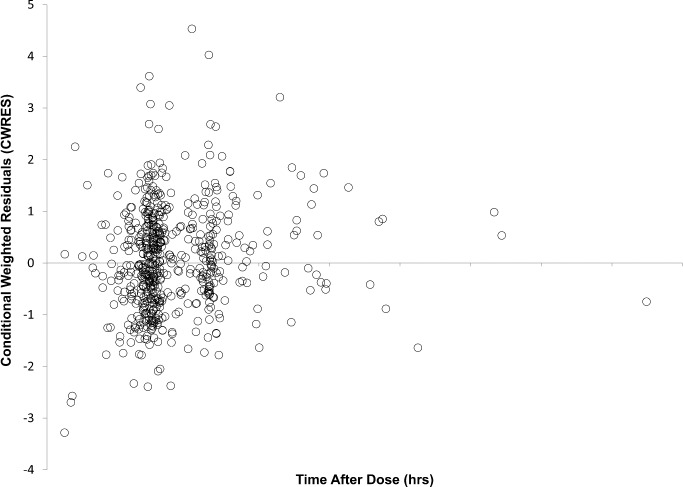
Conditional weighted residuals versus time after dose. There is no apparent bias.
Table 5.
Bootstrap Analysis
| n = 261 | 1-Compartment Model | 1000 Bootstrap | ||
|---|---|---|---|---|
| Parameter | Estimate (RSE %) | 95% CI | Median (RSE %) | 95% CI |
| CL, L/hr |
7.86 (2.06) | 7.54–8.18 | 7.85 (2.06) | 7.53–8.14 |
| VD, L | 63.6 (5.08) | 57.3–69.9 | 63.7 (4.92) | 57.8–70.1 |
| Creatinine clearance, mL/min/1.73 m2 | 0.90 (5.67) | 0.80–1.0 | 0.90 (6.05) | 0.79–0.99 |
| PMA, wk | −0.29 (32.2) | −0.46 to −0.11 | −0.30 (33.1) | −0.52 to −0.13 |
| ω1, % | 17.4 (15.4) | 14.5–19.8 | 17.1 (16.0) | 14.2–19.6 |
| ω2, % | 25.5 (35.2) | 14.2–33.0 | 24.7 (38.7) | 12.1–32.9 |
| Proportional error, % | 10.2 (19.9) | 18.4–22.6 | 19.9 (9.81) | 17.8–21.8 |
ω1, interindividual error on CL; ω2, interindividual error on VD; CL, clearance (L/hr); PMA, postmenstrual age; RSE%, relative standard error; VD, volume of distribution (L)
Figure 3.
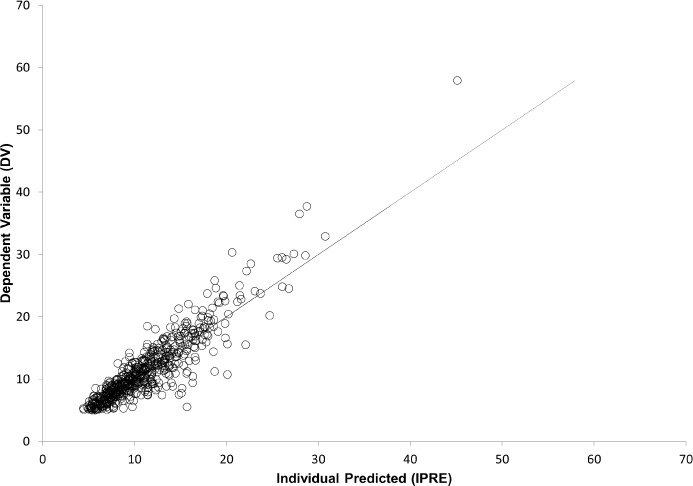
Dependent variables versus individual-predicted concentrations.
Figure 4.
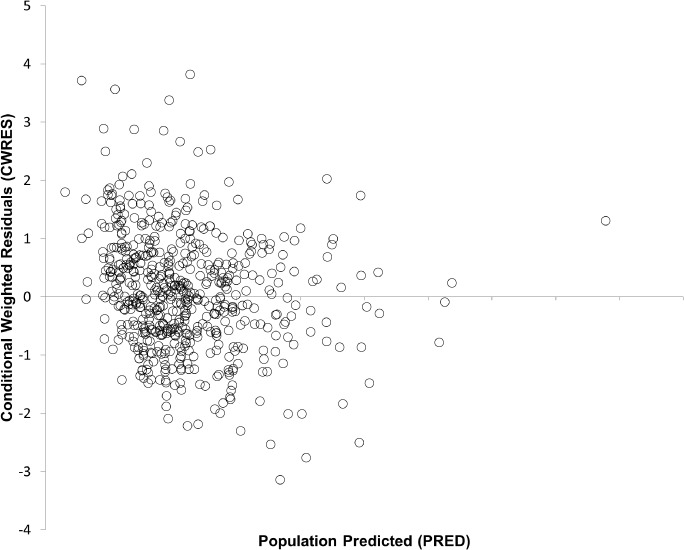
Conditional weighted residuals versus predicted values. There is no apparent bias.
Simulation was performed (n = 10,000) on median values obtained from the dataset for weight (4.025 kg), PMA (51.5 weeks), and SCr (0.32 mg/dL, CrCL 75 mL/min/1.73 m2) for a patient initiated on vancomycin at postoperative day 9 (the median postoperative day in the dataset). Samples were simulated to be drawn before the fourth dose for every 8-hour dosing, and before the fifth dose for every 6-hour dosing (Table 6). A dose of 20 mg/kg/dose every 8 hours had the highest attainment of an AUC0–24:MIC ratio of >400 while maintaining the greatest percentage of patients who had a trough serum concentration < 15 mg/L. Clearance was estimated at 0.105 ± 0.019 L/kg/hr, VD was 0.95 ± 0.25 L/kg, and mean estimated half-life was calculated at 6.5 ± 2.1 hours.
Table 6.
Simulation of Vancomycin Dosing
| Simulation (n = 10000) | Dose, mg/kg/dose | Schedule | Area Under the Curve, mg × L/hr | Attainment of AUC0–24: MIC > 400, % | Serum Concentration, mg/L (%) |
|---|---|---|---|---|---|
| Total cohort | 10 | every 6 hr | 377 ± 66 | 33.2 | 9.9 ± 2.2 (98.8) |
| 15 | every 8 hr | 425 ± 75 | 60.0 | 9.7 ± 2.5 (98.2) | |
| 15 | every 6 hr | 565 ± 98 | 97.2 | 14.8 ± 3.2 (53.2) | |
| 20 | every 8 hr | 565 ± 99 | 96.9 | 12.9 ± 3.2 (74.4) | |
| 20 | every 12 hr | 378 ± 66 | 33.9 | 7.0 ± 2.5 (99.8) |
MIC, minimum inhibitory concentration
Discussion
This is the largest analysis of vancomycin pharmacokinetics in the pediatric cardiac surgical population published to date. The estimates that have been derived from this analysis are similar to other reports of vancomycin pharmacokinetics in the pediatric, neonatal, and pediatric cardiac intensive care population.14–17 Benefield et al18 described the pharmacokinetics of vancomycin in the postoperative pediatric cardiac surgical population, using a non-parametric approach. The calculated values for CL (0.089 ± 0.106 L/kg/hr) were slightly lower than our estimates, with higher estimates for VD (1.2 ± 0.8 L/kg). These reported values, and our estimates, are higher than the values reported by Marlowe et al17 of pediatric cardiology patients with a CL of 0.0513 ± 0.14 L/kg/hr and a VD of 0.40 ± 0.12 L/kg.17 Variation in intraoperative and postoperative patient management strategies and patient acuity are likely to have resulted in the differences noted in estimates. Additionally, most of the patient population used for building the pharmacokinetic model was <1 year of age. Extrapolation to older patients should occur with appropriate caution, particularly when dosing by body weight, using institutional norms for maximum single doses. Patient variability in the postoperative cardiac intensive care population can be great, and application of the results of these analyses should be tailored to individual patient care scenarios.
Postmenstrual age, as opposed to postnatal age, was a significant covariate for describing vancomycin CL. Development of renal maturation has been reported to be associated with PMA.19 The use of PMA as a covariate has been previously reported in neonates,15 and our analysis supports the effect that PMA has on vancomycin pharmacokinetics. The CL of vancomycin was demonstrated to occur in a sigmoidal pattern, with CL approaching 50% of the population value at approximately 50 weeks' PMA. Clinically, this demonstrates that vancomycin CL should be expected to be lower in patients with a lower PMA, independent of SCr, only approaching full CL values at ~100 weeks' PMA. Daily dose reductions, as characterized by extended dosing intervals, would be more likely in patients of low PMA. As most patients undergoing pediatric cardiac surgical procedures are neonates and infants, PMA should be considered when prescribing vancomycin therapy in the pediatric cardiac surgical patient.
Kidney function, as characterized by CrCL, was a significant covariate for vancomycin CL in our analysis. This is expected, as prior publications have demonstrated similar results, and as vancomycin is primarily renally eliminated.6,14,17,20,21 As decreases in CrCL occur, it is important for clinicians to recognize that CL of vancomycin will also decrease, necessitating increases in dosing intervals and more frequent serum concentration monitoring. The simulation performed used a CrCL of 75 mL/min/1.73 m2, and values lower than this would be expected to have extended dosing intervals beyond every 8 hours. The inc7orporation of kidney function in vancomycin dosing in this patient population is particularly important in the pediatric cardiac surgical population. Though non-significant on the final analysis, the impact of kidney function on vancomycin CL was also demonstrated with the graphical relationship between urine output and vancomycin CL. Acute kidney injury is common in patients undergoing CPB, even though CPB was non-significant as a covariate for vancomycin CL in our patient population.7,22 The acute kidney injury caused by CPB in this population was likely reflected in the changes in SCr and CrCL in the postoperative period. The study inclusion/exclusion criteria have also likely minimized the effect of CPB as a covariate in our analysis. Peritoneal dialysis is a common strategy for managing fluid and removing inflammatory mediators in the immediate postoperative period in the youngest and often most critically ill patients who have undergone CPB; however, the dialysis would alter vancomycin CL, so these patients were excluded from the analysis.23,24 The median postoperative day for vancomycin therapy was day 9, which would diminish the acute effects of CPB (such as acute kidney injury) that are more likely to occur earlier in the postoperative course.22 This median postoperative day for vancomycin initiation likely reflects the identification of potential infectious illness, as patients have postoperative antimicrobial prophylaxis for the first 48 hours, and fever is a common adverse event associated with cardiopulmonary bypass. Overall, many factors could alter kidney function in the postoperative pediatric cardiac surgical patient and careful assessment of patient kidney function is necessary when selecting empiric vancomycin dosing regimens.
We simulated common dosing regimens to evaluate their ability to achieve an adequate AUC0–24:MIC ratio for treatment of methicillin-resistant S aureus infections with an MIC of 1 mg/L and acceptable trough concentrations to minimize vancomycin exposure and prevent acute kidney injury. Our analysis generated a total daily dose of 60 mg/kg/day to achieve the goal AUC0–24:MIC ratio, which is similar to prior publications.16 However, we would recommend an extended dosing interval, every 8 hours as opposed to every 6 hours, as based on the simulation result. The younger age group of the patient population (primarily infants and neonates) and the potential for diminished kidney function and decreased CL of vancomycin necessitate an extended dosing interval as compared with pediatric non-cardiac surgical patients. Maintaining as low a trough concentration as possible while still achieving a goal AUC0–24:MIC ratio should be considered in order to prevent acute kidney injury in this patient population. Vancomycin is associated with acute kidney injury in the general pediatric and pediatric cardiac surgical population, and minimizing exposure to vancomycin is a strategy to potentially prevent acute kidney injury in this population.25,26
The limitations associated with this investigation are those germane to retrospective reviews of data collected in the normal course of patient care. We excluded patients receiving renal replacement therapy, including peritoneal dialysis, which are modalities commonly used in the postoperative pediatric cardiac surgical population.23,24 As mentioned previously, the median postoperative day for vancomycin therapy initiation was well beyond the time typically considered most critical for patients undergoing cardiopulmonary bypass during surgery, and this should be taken into account. Additionally, we did not capture a continuous infusion vasoactive/inotropic medication score, incorporating doses of these medications, which could further quantify patient acuity. Though urine output was not significant in our analysis, it is clear that urine output should be monitored closely in the pediatric cardiac surgical population in order to achieve therapeutic goals with vancomycin therapy. Individual patient disposition, institutional strategies for managing postoperative cardiac surgical patients, and goals of therapy should be taken into account when evaluating the clinical application of these analyses.
Conclusions
Vancomycin pharmacokinetics in the pediatric cardiac surgical population is influenced by kidney function and PMA, and dosing should incorporate these variables. A vancomycin dose of 20 mg/kg/dose every 8 hours was identified as an empiric dosing strategy in this patient population.
ABBREVIATIONS
- CL
clearance
- CPB
cardiopulmonary bypass
- CrCL
creatinine clearance
- CWRES
conditional weighted residuals
- DV
dependent variable
- G6P-DH
glucose-6-phosphate dehydrogenase
- IIV
interindividual variability
- IPRE
individual predicted
- MIC
minimum inhibitory concentration
- OFV
objective function value
- PMA
postmenstrual age
- PRED
population predicted
- SCr
serum creatinine
- UOP
urine output
- VD
volume of distribution
- WT
weight
Footnotes
Disclosure The authors declare no conflicts or financial interest in any product or service mentioned in the manuscript, including grants, equipment, medications, employment, gifts, and honoraria. The authors had full access to all the data and take responsibility for the integrity and accuracy of the data analysis.
REFERENCES
- 1.Abdel Hadi O, Al Omar S, Nazer LH et al. Vancomycin pharmacokinetics and predicted dosage requirements in pediatric cancer patients. J Oncol Pharm Pract. 2016;22(3):448–453. doi: 10.1177/1078155215591386. [DOI] [PubMed] [Google Scholar]
- 2.Anderson BJ, Allegaert K, Van den Anker JN et al. Vancomycin pharmacokinetics in preterm neonates and the prediction of adult clearance. Br J Clin Pharmacol. 2007;63(1):75–84. doi: 10.1111/j.1365-2125.2006.02725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Asbury WH, Darsey EH, Rose WB et al. Vancomycin pharmacokinetics in neonates and infants: a retrospective evaluation. Ann Pharmacother. 1993;27(4):490–496. doi: 10.1177/106002809302700417. [DOI] [PubMed] [Google Scholar]
- 4.Guilhaumou R, Marsot A, Dupouey J et al. Pediatric patients with solid or hematological tumor disease: vancomycin population pharmacokinetics and dosage optimization. Ther Drug Monit. 2016;38(5):559–566. doi: 10.1097/FTD.0000000000000318. [DOI] [PubMed] [Google Scholar]
- 5.Le J, Capparelli EV, Wahid U et al. Bayesian estimation of vancomycin pharmacokinetics in obese children: matched case-control study. Clin Ther. 2015;37(6):1340–1351. doi: 10.1016/j.clinthera.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marques-Minana MR, Saadeddin A, Peris JE. Population pharmacokinetic analysis of vancomycin in neonates: a new proposal of initial dosage guideline. Br J Clin Pharmacol. 2010;70(5):713–720. doi: 10.1111/j.1365-2125.2010.03736.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blinder JJ, Asaro LA, Wypij D et al. Acute kidney injury after pediatric cardiac surgery: a secondary analysis of the safe pediatric euglycemia after cardiac surgery trial. Pediatr Crit Care Med. 2017;18(7):638–646. doi: 10.1097/PCC.0000000000001185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pea F, Pavan F, Furlanut M. Clinical relevance of pharmacokinetics and pharmacodynamics in cardiac critical care patients. Clin Pharmacokinet. 2008;47(7):449–462. doi: 10.2165/00003088-200847070-00002. [DOI] [PubMed] [Google Scholar]
- 9.Sherwin J, Heath T, Watt K. Pharmacokinetics and dosing of anti-infective drugs in patients on extracorporeal membrane oxygenation: a review of the current literature. Clin Ther. 2016;38(9):1976–1994. doi: 10.1016/j.clinthera.2016.07.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Saet A, de Wildt SN, Knibbe CA et al. The effect of adult and pediatric cardiopulmonary bypass on pharmacokinetic and pharmacodynamic parameters. Curr Clin Pharmacol. 2013;8(4):297–318. doi: 10.2174/15748847113089990067. [DOI] [PubMed] [Google Scholar]
- 11.Bautista-Hernandez V, Karamanlidis G, McCully JD et al. Cellular and molecular mechanisms of low cardiac output syndrome after pediatric cardiac surgery. Curr Vasc Pharmacol. 2016;14(1):5–13. doi: 10.2174/1570161113666151014122557. [DOI] [PubMed] [Google Scholar]
- 12.Ricci Z, Haiberger R, Pezzella C et al. Furosemide versus ethacrynic acid in pediatric patients undergoing cardiac surgery: a randomized controlled trial. Crit Care. 2015;19:2. doi: 10.1186/s13054-014-0724-5. doi:10.1186/s13054-014-0724-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwartz GJ, Munoz A, Schneider MF et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20(3):629–637. doi: 10.1681/ASN.2008030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Hoog M, Schoemaker RC, Mouton JW et al. Vancomycin population pharmacokinetics in neonates. Clin Pharmacol Ther. 2000;67(4):360–367. doi: 10.1067/mcp.2000.105353. [DOI] [PubMed] [Google Scholar]
- 15.Frymoyer A, Hersh AL, El-Komy MH et al. Association between vancomycin trough concentration and area under the concentration-time curve in neonates. Antimicrob Agents Chemother. 2014;58(11):6454–6461. doi: 10.1128/AAC.03620-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Le J, Bradley JS, Murray W et al. Improved vancomycin dosing in children using area under the curve exposure. Pediatr Infect Dis J. 2013;32(4):e155–e163. doi: 10.1097/INF.0b013e318286378e. doi:10.1097/INF.0b013e318286378e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marlowe KF, Chicella MF, Claridge TE et al. An assessment of vancomycin pharmacokinetic variability in pediatric cardiology patients. J Pediatr Pharmacol Ther. 2003;8(2):132–136. doi: 10.5863/1551-6776-8.2.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benefield EC, Hagemann TM, Allen HC et al. Vancomycin dosing and pharmacokinetics in postoperative pediatric cardiothoracic surgery patients. J Pediatr Pharmacol Ther. 2016;21(1):66–74. doi: 10.5863/1551-6776-21.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson BJ, Holford NH. Understanding dosing: children are small adults, neonates are immature children. Arch Dis Child. 2013;98(9):737–744. doi: 10.1136/archdischild-2013-303720. [DOI] [PubMed] [Google Scholar]
- 20.Le J, Vaida F, Nguyen E et al. Population-based pharmacokinetic modeling of vancomycin in children with renal insufficiency. J Pharmacol Clin Toxicol. 2014;2(1):1017–1026. [PMC free article] [PubMed] [Google Scholar]
- 21.Staatz CE, Byrne C, Thomson AH. Population pharmacokinetic modelling of gentamicin and vancomycin in patients with unstable renal function following cardiothoracic surgery. Br J Clin Pharmacol. 2006;61(2):164–176. doi: 10.1111/j.1365-2125.2005.02547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park SK, Hur M, Kim E et al. Risk factors for acute kidney injury after congenital cardiac surgery in infants and children: a retrospective observational study. PLoS One. 2016;11(11) doi: 10.1371/journal.pone.0166328. e0166328. doi:10.1371/journal.pone.0166328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sorof JM, Stromberg D, Brewer ED et al. Early initiation of peritoneal dialysis after surgical repair of congenital heart disease. Pediatr Nephrol. 1999;13(8):641–645. doi: 10.1007/s004670050672. [DOI] [PubMed] [Google Scholar]
- 24.Stromberg D, Fraser CD, Jr, Sorof JM et al. Peritoneal dialysis: an adjunct to pediatric postcardiotomy fluid management. Tex Heart Inst J. 1997;24(4):269–277. [PMC free article] [PubMed] [Google Scholar]
- 25.Moffett BS, Hilvers PS, Dinh K et al. Vancomycin-associated acute kidney injury in pediatric cardiac intensive care patients. Congenit Heart Dis. 2015;10(1):e6–e10. doi: 10.1111/chd.12187. doi:10.1111/chd.12187. [DOI] [PubMed] [Google Scholar]
- 26.Sinclair EA, Yenokyan G, McMunn A et al. Factors associated with acute kidney injury in children receiving vancomycin. Ann Pharmacother. 2014;48(12):1555–1562. doi: 10.1177/1060028014549185. [DOI] [PubMed] [Google Scholar]


