Abstract
The vascular endothelium is an interface between the blood stream and the vessel wall. Changes in this single cell layer of the artery wall are believed of primary importance in the pathogenesis of vascular disease/atherosclerosis. The endothelium responds to humoral, neural and especially hemodynamic stimuli and regulates platelet function, inflammatory responses, vascular smooth muscle cell growth and migration, in addition to modulating vascular tone by synthesizing and releasing vasoactive substances. Compromised endothelial function contributes to the pathogenesis of cardiovascular disease; endothelial ‘dysfunction’ is associated with risk factors, correlates with disease progression, and predicts cardiovascular events. Therapies for atherosclerosis have been developed, therefore, that are directed towards improving endothelial function.
Keywords: Endothelium, Endothelial dysfunction, Atherosclerosis, Cardiovascular disease, Vessel remodeling, Clinical therapies, Review
1. Atherosclerosis
Atherosclerosis is a chronic inflammatory disease in which the artery wall thickens as a result of the accumulation of cholesterol, macrophages and smooth muscle cells (SMC), ultimately restricting blood flow through the artery. It is the main pathologic condition underlying coronary artery and cerebrovascular disease leading to heart attack and stroke, respectively. In the pathogenesis of atherosclerosis (reviewed in Ref. [1–4]), increases in plasma low density lipoprotein (LDL) leads to a proportional increase in the entry of cholesterol laden LDL particles into the arterial wall across a ‘compromised/dysfunctional’ endothelial monolayer, where it accumulates. Once there, it can become oxidized, by free radical production from adjacent endothelium, smooth muscle cells or isolated macrophages [5–8]. Oxidized LDL has numerous effects on a variety of cells, many of which are believed to cumulatively exacerbate atherothrombosis ([9] for review). These include promotion of monocyte adhesion and infiltration to the intima by causing production of monocyte chemotactic protein-1 (MCP-1) by endothelium and expression by endothelium of monocyte-binding proteins including intercellular adhesion molecule-1 (ICAM-1), foam cell formation following uptake of oxidized LDL via scavenger receptors (SR-A type I and II and CD36), and stimulation of the migration of medial SMC into the intima where they proliferate in response to growth factors such as platelet derived growth factor (PDGF) [13]. In the intima, SMC produce extracellular matrix molecules including collagen and elastin. The most common clinical complication of atherosclerosis occurs upon plaque rupture that allows blood components to come into contact with plaque lipids and tissue factor, resulting in thrombus formation. While several cell types are clearly involved in the pathogenesis of atherosclerotic plaques, endothelial compromise/dysfunction is deemed of particular importance as it is a necessary and initiating occurrence for atherogenesis to proceed. The endothelial lining can be viewed as the first line of defense between risk factors and vascular disease.
2. Arterial endothelium: structure, function
The vascular endothelium lines the entire circulatory system. In coronary arteries, this single layer, together with some extracellular matrix, comprises the tunica intima. Originally thought of simply as a passive barrier, it is now viewed as an organ whose normal functioning is crucial to maintaining vascular health, and whose dysfunction is key in the initiation, progression and clinical complications of vascular disease. Vascular endothelium acts as a selectively permeable barrier between extravascular and intravascular compartments and provides a nonthrombogenic lining for the cardiovascular system. It is poised in an anatomic location that allows interaction not only with circulating blood components and cells, but also with cells in the vessel wall. Endothelial cells are long, flat cells orientated in the long axis of the vessel. An average endothelial cell is 20–40 μM long, 10–15 μM wide and only 0.1–0.5 μM thick. Electron microscopy of arterial endothelium reveals it to be of the continuous type characterized by tight junctions at the lateral borders of each cell that restrict the movement of macromolecules, and a complex micro-vesicular system implicated in macromolecular transport. Despite its apparent morphological simplicity and relative homogeneity, there is evidence of regional and species variation manifested by differences in permeability, responsiveness and biosynthesis.
3. Barrier function
The role of the endothelium as a semipermeable barrier is one of its most basic functions. It regulates transport of macromolecules between the vascular lumen and vascular smooth muscle. There are several different mechanisms by which macromolecules cross the endothelial barrier; through the endothelial cells themselves, by diffusing laterally within the endothelial cell membrane and thus around the cell, through endothelial cell-to cell junctions, through endothelial gaps, or via vesicular transport. As most biologic molecules are large, hydrophilic, anionic molecules, which are unable to diffuse into and through bilayer membranes, most are thought to move through intercellular junctions between cells or by vesicular transport, or the formation of transient channels resulting from vesicle fusion [10]. Reorganization of the inter-cellular junctions, involving actin and myosin or direct dissolution of junctional contacts, is believed to be the primary mechanism by which endothelial permeability to water, small and large solutes is increased [11].
4. Changes in permeability
Various physiologic and pathophysiologic stimuli can induce, acutely and chronically, dramatic changes in endothelial permeability. For example thrombin, histamine and other acute inflammatory mediators can act on endothelium to stimulate opening of their intercellular junctions at the level of adherens and tight junctional complexes [12]. The signaling involved in mediating these responses include protein kinase C (PKC)–induced phosphorylation of linking proteins at the cell-cell and cell-matrix junctions, leading to actin reorganization, cell rounding and increased paracellular transport. Myosin light chain kinase (MLCK) may also be activated by inflammatory mediators leading to actin-myosin based retraction of endothelial cells [12]. Vascular endothelial growth factors (VEGFs) are key regulators of vascular permeability via nitric oxide synthase (NOS) regulation [13,14], facilitated by multiple mechanisms including gap formation and vesiculo-vacuolar organelle formation [15] (reviewed in Ref. [16]). The bacterial endotoxin lipopolysaccharide (LPS) causes endothelial hyperpermeability by stimulating the small GTPase, RhoA, and its effector Rho Kinase (ROCK) [17]. Endothelial permeability is also influenced by fluid shear stress, the tangential frictional force exerted by flowing blood [10,18]. Investigation of the relationship between albumin permeability and shear stress magnitude in vivo revealed that endothelium exposed to low wall shear stresses was more likely to have elevated macromolecule permeability [19]. Of importance with respect to vascular disease, low density lipoprotein (LDL) accumulation is greater at these more permeable areas exposed to low wall shear stress [20,21]. It is now recognized that atherosclerotic lesions preferentially develop at vessel segments exposed to low, disturbed or oscillating flow, while laminar flow and high shear stress are seemingly atheroprotective [22]. In addition to inhibition of thrombosis and inhibition of endothelial apoptosis, limitation of permeability is now a well-characterized atheroprotective mechanism of laminar flow and high shear stress [22]. Conversely, at regions of pathological low shear stress, increased endothelial permeability results in enhanced infiltration of LDL and its local accumulation, which is a critical initial event in the development of atherosclerosis [23,24]. Rozenberg et al., recently reported that Histamine, acting via its H1 receptor drives the formation of atherosclerotic lesions through an increased vascular permeability for LDL [25]. Mullick et al., showed that exposure to cigarette smoke injures the endothelium, resulting in increased arterial permeability and increased LDL accumulation [26]. A recent study provided evidence of a role for lipoxygenase and its metabolite hydroxyeicosatetraenoic acid (HETE) in ‘high fat diet’-induced endothelial tight junction disruption [27], thus providing a possible mechanistic link between lifestyle and atherosclerosis. Therefore, a wide variety of injurious stimuli (e.g., certain hemodynamic forces, inflammatory mediators, bacterial endotoxin LPS, environmental toxins, high fat diet) can contribute to endothelial dysfunction by increasing endothelial permeability and subsequently arterial lipid accumulation in the subendothelial space, thereby initiating atherosclerotic plaque development. On the other hand, factors shown to maintain endothelial barrier function include high density lipoprotein (HDL), and physical exercise (reviewed in [28]). With respect to the latter, there is considerable evidence of a direct relationship between exercise and vascular health. The effect of exercise on maintaining endothelial barrier function is likely a consequence of exercise increasing blood flow and shear stress, which in turn releases ‘vasoprotective’ molecules such as nitric oxide (NO) and prostacyclin (PGI2). It is also appreciated that Sphingosine-1-phosphate (S1P), a bioactive sphingolipid associated with HDL and found mainly in the blood and lymph, robustly promotes endothelial barrier function [29,30]. In particular, growing evidence indicates that HDL-associated S1P mediates the beneficial effects on endothelial integrity [31,32]. Other endogenous factors known to increase endothelial barrier function and decrease permeability are angiopoietin-1 [33], and the second messenger cyclic adenosine monophosphate (cAMP) and agonists such as Serotonin and β-adrenergic agonists that increase it [34,35] (Table 1).
Table 1.
Factors affecting endothelial cell permeability.
| Increase permeability | Decrease permeability |
|---|---|
| 'Low' shear stress | 'High' shear stress |
| Vascular endothelial growth factor (VEGF) | High density lipoprotein (HDL)/Sphingosine 1 phosphate(S1P) |
| Lipopolysaccharide (LPS) | |
| High fat diet | Physical exercise |
| Phospholipid oxidative products | Increased cellular cAMP (by e.g., Serotonin or β-adrenergics) |
| Inflammatory mediators (e.g., thrombin, Histamine, TGF(β) Cigarette smoke | Angiopoietin-1 |
5. Endothelial glycocalyx
Consisting of a negatively charged, organized mesh of membranous glycoproteins, proteoglycans and associated plasma proteins, the endothelial glycocalyx (100–750 nm thick) is recognized as contributing, together with the endothelium, to the protection of the vascular wall against disease (for review [36,37]). Improved fixing and imaging techniques have allowed in vivo visualization of the endothelial glycocalyx and provided evidence that there are significant reductions in its extent during acute and chronic inflammatory challenge in man. Indeed, destruction of the glycocalyx has been directly and indirectly evidenced in several studies, e.g. after ischemic challenge [38–40], during redox stress [39], and after inflammation [40,41]. Deterioration or destruction of the glycocalyx is associated with pathophysiological sequelae including increased endothelial permeability, platelet aggregation and loss of vascular responsiveness [42]. There are interesting data supporting an important role for the glycocalyx in the initiation and progression of atherosclerosis. Van den Berg et al., reported thinning of the glycocalyx in mice fed a cholesterol rich diet, and demonstrated less glycocalyx in regions of the vessel at high atherogenic risk (i.e., at branch points, areas of curvature) [43]. Moreover, the authors found an inverse relation between glycocalyx thickness and the intima-media ratio [43]. These findings support the hypothesis that diminution of the glycocalyx, perhaps as a consequence of turbulent flow/low shear stress, contributes to the vulnerability of regions that are at high atherogenic risk [44]. Vasculoprotective effects attributed to the glycocalyx include fortifying endothelial barrier function [45], inhibiting coagulation and leukocyte adhesion [46] and mediating shear stress-induced NO release [47,48]. The seemingly atheroprotective role of the gylcocalyx means that it is attracting attention as a potential novel diagnostic or therapeutic target for atherosclerosis [49,42]. Approaches to increase the glycocalyx or to reverse its damage, as well as tactics to maintain it mechanically and chemically, are being tested as viable clinical options at this stage [37,42]. Indeed, clinical trial data support a protective role for the compounds Diazoxide and Sulodexide on endothelial glycocalyx in patients after coronary bypass grafting and in those with type 2 diabetes, respectively [50,51].
6. Hemodynamic forces
Cells of the arteries are continuously exposed to pulsatile blood flow and are therefore subjected to the hemodynamic forces shear stress and cyclic strain. Shear stress is the tangential frictional force acting predominately at the endothelial cell surface, whereas cyclic strain/stretch acts perpendicular to the vessel wall and affects both endothelial and smooth muscle cells together with the underlying matrix [52]. Shear stress (ϊ) (expressed as ‘dynes/cm2’) can be calculated using the formula, ϊ = 4μQ/πr3, where μ is blood viscosity, Q is blood flow volume, π is the ratio of the circumference of a circle to its diameter, and r is the radius of the blood vessel. The pumping heart causes pulsatile changes in blood pressure that stretch the vessel wall circumferentially and create cyclic strain in vascular cells. The degree of stretch is around 9%–12% in the aorta and 1%–2% in the carotid arteries [53]. A variety of devices have been employed by research laboratories to expose cultured cells to defined mechanical forces. Those used to apply shear stress include the cone plate viscometer [54], the parallel flow chamber [55] and the perfused capillary culture system [56,57]. In the case of cyclic stretch, researchers have grown cells on a variety of elastic substrates [58] that can then be periodically stretched; e.g., the Flexercell system [59]. In order to respond to mechanical forces such as shear stress or cyclic strain and convert it into a biochemical response endothelial cells must express special receptors or ‘mechanotransducers’. Biomechanical studies have suggested many different mechanotransducer candidates including ion channels, tyrosine kinase receptors, G-protein coupled receptors, a caveolaemediated process, cell adhesion molecules, the glycocalyx and primary cilia (Reviewed in Ref. [53,60]). Certain biomechanically induced events appear to involve transcriptional regulation and shear stress-response elements have been identified in the promoters of multiple endothelial cell-expressed genes (e.g., [61]).
Recent studies have uncovered other contenders as mechanotransducers. Syndecan 4, a transmembrane heparan sulfate proteoglycan, is required for proper flow alignment in cultured endothelial cells [62]. Hypercholesterolemic mice deficient for syndecan 4 have increased atherosclerotic plaque when compared with control mice [62]. A flow-dependent GTP exchange factor called TIAM1 reportedly links platelet endothelial cell adhesion molecule 1(PECAM-1) mechanotransduction to focal activation of the small GTPase Rac1 which in turn triggers the Nuclear factor kappa B (NF-kB) pathway and production of reactive oxygen species [63]. Another mechanotransducer candidate is the ion channel protein Piezo1, a mediator of shear stress–induced calcium influx [64] Piezo1-mediated calcium influx is important for calpain activity and subsequent rearrangement of focal adhesions for flow alignment. Endothelial cells isolated from Piezol−/− mice failed to align properly when exposed to atheroprotective flow conditions [65] A role for the G protein–coupled Sphoingosine-1-phosphate receptor (S1P1) in endothelial mechanotransduction has also been put forward as the expression of S1P1 was critical for flow-mediated directional alignment in cultured endothelial cells in vitro and in vivo [66].
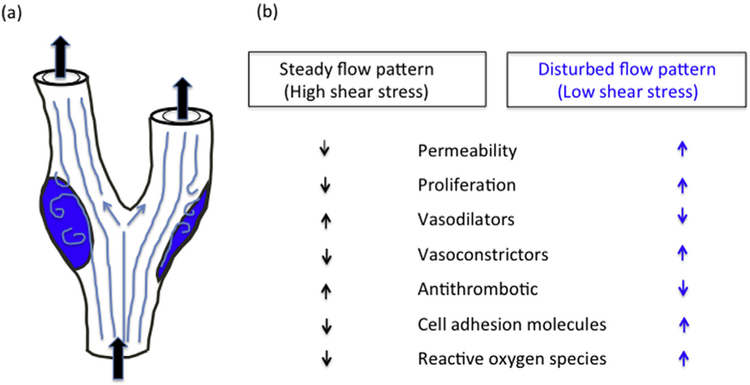
Hemodynamic forces are ubiquitous and fundamental physiologic stimuli for vascular cells, and are believed to critically influence atherogenesis by regulating endothelial cell function, smooth muscle behavior, and the interaction of endothelial cells with smooth muscle cells [67] and with leucocytes and other blood constituents [22,68,69]. Of note, flow patterns and hemodynamic forces are not uniform throughout the vasculature. While blood flow is essentially laminar throughout the arterial system, in straight parts of the arterial tree blood flow is generally steady and unidirectional and wall shear stress is high (>15 dyn/cm2; ‘physiologic flow’). At branch points and curvatures, blood flow is disturbed or oscillatory with low net wall shear stress (0–4 dyn/ cm2; ‘pathologic low flow’). Atherosclerotic lesion development generally correlates with the latter [70]. This type of observation gave rise to the concept, now accepted, that disturbed flow patterns are atherogenic whereas steady high flow patterns are atheroprotective (reviewed in Ref. [71]). Several groups have investigated the effects of various flow patterns on endothelial cell biology in vivo and in vitro over the last 30 years, and the emerging consensus is that physiologic flow favors the expression of endothelial genes and bioactive products that are protective against atherosclerosis, whereas pathologic flow stimulates genes and products that promote atherogenesis [22,68,69,70,72] (Fig. 1). Indeed, studies using DNA microarrays have revealed striking differences between the numbers and kinds of endothelial genes that respond to steady flow versus disturbed flow [73]. Of interest, it is emerging that flow modulates epigenetic DNA methylation patterns via alterations in DNA methyltransferase activity, in particular DNMT1, that may contribute to the endothelial phenotypes observed in regions of disturbed flow [74]. For example, disturbed flow patterns increase methylation of the proximal promoter of Kruppel like factor 4 (KLF4), thus inhibiting ‘atheroprotective’ KLF4 transcription in atherosclerosis-susceptible regions [75]. Findings such as these suggest that DNA methylation may play a key role in maintaining endothelial cell homeostasis and in vascular disease development and encourage continued investigation into epigenetic mechanisms relevant to vascular health and disease.
Fig. 1.
Effect of different flow patterns on (a) atherosclerotic plaque development and (b) endothelial phenotype and activity. In straight parts of the arterial tree blood flow is steady and unidirectional and wall shear stress high. At branch points and curvatures, blood flow is disturbed or oscillating and net wall shear stress is low (areas in blue in schematic of arterial bifurcation). Steady, high shear flow is atheroprotective, whereas disturbed flow, low shear is atherogenic. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
7. Hemodynamic forces and endothelium
Hemodynamic forces impact multiple aspects of endothelial cell biology and function (reviewed in Ref. [53]), all of which may influence atherosclerotic plaque initiation and development. Shear stress affects endothelial cell morphology. Endothelial cells exposed to steady rapid flow are elongated in shape and aligned with their long axis in the direction of flow, in contrast to the rounder shape and non-uniform orientation and greater permeability of EC in segments exposed to disturbed flow [76]. Shear stress plays a role in controlling endothelial cell proliferation and apoptosis; e.g., steady flow reduced EC proliferation [77], whereas disturbed flow increased EC turnover and stimulated apoptosis [78]. Cyclic strain also promotes endothelial migration and in vitro tube formation (an index of angiogenesis) [79]. Growth and migration of endothelial cells becomes important in the repair of areas denuded of endothelium as a result of injury, be it toxic or mechanical and/or iatrogenic.
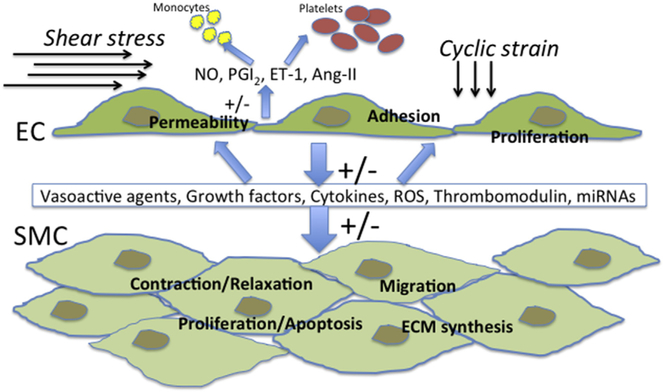
Endothelial cells respond to hemodynamic forces by altering their production of vasoactive substances (Fig. 2). Increases in shear stress generally causes vasodilation, mediated for the most part by increased endothelila nitric oxide synthase (eNOS) activity and NO production [57,80]. Indeed, shear stress is considered the premiere physiologic stimulus for this potent vasorelaxant molecule. Other endothelial-derived vasoactive substances altered by shear stress include PGI2 [81,57,82] and endothelin-1 (ET-1) [83,84]. The vasodilators NO and PGI2, and the vasoconstrictor ET-1 are not only important in regulating vascular tone at the level of vascular smooth muscle, but in addition, these agents inhibit (NO, PGI2), and stimulate (ET-1), SMC growth and migration [85–87]. Nitric oxide and PGI2 are also potent inhibitors of platelet aggregation [88,89]. Besides stimulating NO and PGI2, shear stress contributes to maintaining the endothelium as non-thrombogenic by stimulating thrombomodulin [90], heparin sulfate proteoglycans [91] and tissue type plasminogen activator (tPA) [92].
Fig. 2.
Shear stress and cyclic strain are important stimuli for endothelial cells (EC). These hemodynamic forces are sensed by mechanoreceptors that include ion channels, G protein coupled receptors, integrins, cytoskeletal components and receptor tyrosine kinases. Hemodynamic forces modulate endothelial release and expression of a myriad of substances including vasoactive agents, growth factors, cytokines, microRNAs (miRNAs), thrombomodulin and reactive oxygen species (ROS) that may affect the aggregation and adhesion of cells circulating in the blood (i.e., platelets and monocytes), the permeability, adhesivity and angiogenic potential of EC themselves, as well as the growth, migration, vasoreactivity and extracellular matrix (ECM) synthesis of the underlying vascular smooth muscle (SMC).
Hemodynamic forces also affect the production by the endothelium of a variety of growth factors and cytokines, many of which can affect the underlying smooth muscle cells, stimulating them to de-differentiate from a quiescent, contractile phenotype to the migratory and proliferative synthetic phenotype fundamental to the pathogenesis of vascular disease [93]. These include platelet-derived growth factor (PDGF) [94], basic fibroblast growth factor (bFGF) [95], transforming growth factor beta (TGFβ) [96] and Interleukin-1 and -6 [97].
Modulatory influences of shear stress on endothelial cell adhesion molecule (e.g., vascular cell adhesion molecule-1, VCAM-1) and selectin (e.g., P-selectin) expression have also been reported, effects with important implications to not only platelet aggregation [98], but also to the adhesion of leukocytes, in particular monocytes, to the endothelium [99,100]. Of note, following their adhesion, migration of monocytes across the endothelial barrier is considered a significant early event in the development of atherosclerotic lesions [1].
7.1. Reactive oxygen species
Increased production of reactive oxygen species (ROS) contributes to mechanisms of vascular/endothelial dysfunction and atherosclerosis [101,102]. ROS is a term that includes oxygen radicals such as superoxide () and hydroxyl radical (OH), as well as non-radical derivatives of O2 including hydrogen peroxide (H2O2) and Ozone (O3). Oxidative stress is mainly caused by an imbalance between the activity of endogenous pro-oxidative enzymes (such as nicotinamide adenine dinucleotide phosphate-oxidase (NADPH) oxidase and xanthine oxidase) and anti-oxidative enzymes (such as superoxide dismutase, glutathione peroxidase and heme oxygenase) in favor of the former. Modulation of ROS production from endothelium by shear stress and cyclic stretch has been reported [60,103]. For example, Chatterjee et al., showed that in response to a decrease of shear, such as occurs during ischemia, membrane depolarization via ATP-sensitive K+ channel closure initiated a signaling cascade leading to NADPH oxidase activation and ROS production [104]. In contrast, shear stress upregulated the expression of antioxidant enzymes such as peroxiredoxin 1 (PRX 1) [105]. The accepted idea, from evidence garnered over the last 20 years, is that flow patterns crucially regulate the ROS/NO balance, with steady flow (high shear) causing lower levels of ROS and greater NO bioavailability (considered anti-atherogenic), whereas disturbed flow (low shear) results in higher ROS and lower NO bioavailability (considered pro-atherogenic) (reviewed in Ref. [60]). Steady flow favors the activation of key transcription factors such as Nuclear factor (erythroid-derived 2)-like 2 (Nrf2) and Krüppel-like Factor 2 (KLF2) to promote an anti-atherogenic environment by enhancing the expression of superoxide dismutase and heme oxygenase [106], whereas irregular flow leads to activation of key transcription factors such as AP-1 and NF-κB leading to enhanced expression of pro-atherogenic agents such as monocyte chemotactic protein1 (MCP-1) and intracellular adhesion molecule 1 (ICAM-1) [60].
8. Cyclic strain
As mentioned earlier, endothelial and smooth muscle cells in vivo are also exposed to cyclic strain, a circumferential stretching synchronous with cardiac cycle-induced changes in blood pressure. Like shear stress, cyclic strain is a force of physiological and pathological interest, sensed by mechanosensors, that modulates endothelial cell intracellular signaling resulting in changes in proliferation, apoptosis [107], migration [79], angiogenic potential [79,59] and matrix remodeling [108,109,103]. Cyclic strain increases under certain pathological conditions such as hypertension and congenital heart disease. Kou et al., reported that lower (5%) cyclic strain increases, but higher (20%) cyclic strain decreases, endothelial cell survival and angiogenesis via the NAD(P)H subunit p22phox pathway [110]. Physiologic cyclic strain regulated, in a p38-and receptor tyrosine kinase-dependent manner, the release of thrombomodulin a membrane glycoprotein expressed on the lumenal surface of endothelial cells that promotes anti-coagulant and anti-inflammatory properties [111]. Liu et al., reported that cyclic strain stimulates Heme oxygenase 1 (HO-1) in a manner dependent on the production of ROS and mediated by Nrf2 [107]. They also showed that cyclic strain inhibits cytokine-mediated endothelial cell apoptosis and that HO-1 underlies this cytoprotective effect [107]. Thus, there is ample evidence that hemodynamic forces, in particular shear stress and cyclic strain, are critically important stimuli for the endothelium, affecting endothelial cell function as well as modulating the endothelial release and expression of growth factors, cytokines, vasodilators, vasoconstrictors, reactive oxygen species and cell adhesion molecules - all of which impact the underlying vascular smooth muscle and/or the interaction of circulating inflammatory and immune cells with the endothelium and thereby affect atherogenesis (Fig. 2). There is also evidence that atherosclerosis risk factors themselves (e.g. hypertension, dyslipidemia, smoking) result in altered local hemodynamic/mechanical forces that could be an underlying mechanism for the progression of atherosclerosis [112].
9. Physical exercise
Of interest, physical exercise seems to be naturally antiatherogenic, preserving vascular function with aging (reviewed in Refs. [113,114]). Some data suggest that exercise inhibits plaque development and induces the regression of coronary stenosis [115,116]. Furthermore, experimental studies have revealed that exercise prevents the conversion of plaques into a vulnerable phenotype, thus averting the appearance of fatal lesions [117]. While the molecular mechanisms involved are not yet fully understood, strong evidence supports the importance of increased shear stress, as a result of exercise-induced increased heart rate and blood flow, as the primary signal acting on the endothelium produced by exercise [118], resulting in down-regulated endothelial angiotensin II type 1 receptor expression, leading to decreases in NADPH oxidase activity and superoxide anion production, which in turn decreases ROS generation, and preserves endothelial NO bioavailability and its protective anti-atherogenic effects [119]. Of further note, atherosclerosis is a chronic inflammatory disease [120] and several studies support an inverse correlation between physical exercise and serum markers of inflammation such as Creactive protein (CRP), tumor necrosis factor-α (TNFα) and Interleukin-6 [121–123,124. In addition, recent meta analysis of 28 individual studies showed that physical exercise has several non-acute effects expected to reduce atherogenesis; i.e., decreasing adhesion molecule VCAM-1 and ICAM-1 expression, reducing the angiogenic factor VEGF, and increasing endothelial progenitor cells (EPC) [125].
10. Endothelium's vasoactive role (vasodilators)
10.1. EDRF/NO
The smooth muscle response to sympathetic/parasympathetic nerve stimulation is a major contributor to maintenance of cardiovascular tone throughout the vascular tree. However, starting with the discovery in 1980 by Furchgott and Zawadski of endothelial-derived relaxing factor (EDRF) [126], identified chemically as endogenous nitric oxide (NO) [127], endothelial cells were subsequently recognized as playing a significant role in the local regulation of vascular tone. This local regulation has implications for atherogenesis. Nitric oxide is synthesized by the heme-containing, calcium and calmodulin-dependent enzyme nitric oxide synthase in endothelial cells (eNOS) from l-arginine in a reaction that produces stoichiometric amounts of l-citrulline [128,129]. Activation of NOS and release of the free radical NO, which easily diffuses across biological membranes, results in stimulation of a soluble guanylyl cyclase leading to a profound increase in intracellular cGMP within the adjacent smooth muscle cells, thus resulting in their relaxation and consequent vasodilation [129]. NO has a wide range of actions important in maintaining vascular homeostasis. In addition to causing vasodilation, it has anti-proliferative, antioxidant and anti-inflammatory properties that inhibit atherogenesis ([130] for recent review). As mentioned previously, shear stress resulting from blood flow upregulates eNOS in endothelium. Shear stress-responsive elements have been identified in the eNOS promotor sequence on cloning of the eNOS cDNA and identification of the promotor region [131]. eNOS activity can also be stimulated by receptor mediated agonists-e.g., bradykinin, acetylcholine and thrombin via palmitoylation, binding to calmodulin/calcium, displacement of caveolin and release from the plasma membrane [132].
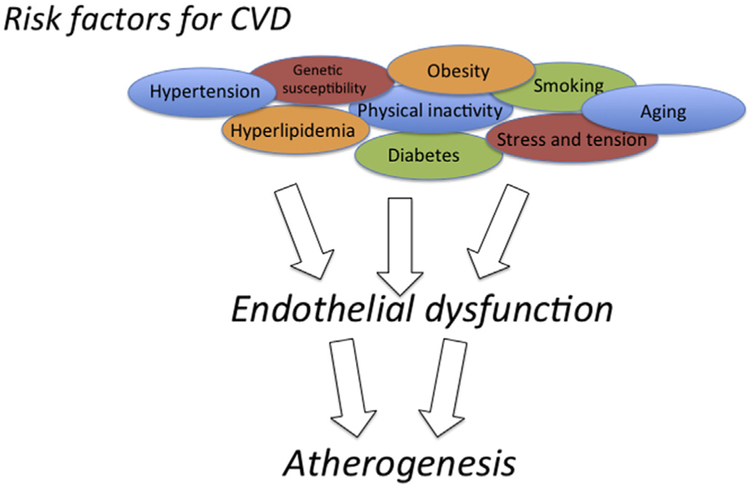
The beneficial effect of physical exercise on cardiovascular disease is believed partly due to increased NO bioavailability [119,133]. Conversely, common risk factors for cardiovascular disease such as hypercholesterolemia, hypertension, smoking and diabetes mellitus are associated with reduced NO in the arterial wall [134] (Fig. 3). Indeed, the term ‘endothelial dysfunction’ has become synonymous with reduced biological activity of NO. Because of these findings, numerous therapies have been investigated based on enhancing NO release, thereby reversing endothelial dysfunction and preventing atherogenesis. NO donors (e.g., nitroglycerin) are frequently used in cardiovascular disease patients. NO bioavailability can be restored by moderate physical exercise, antioxidants and l-arginine, the natural precursor of NO [134]. Several small-scale studies have demonstrated that intravenous l-arginine augments endothelial function and improves exercise ability in patients with cardiovascular disease by enhancing vasodilation and reducing monocyte adhesion [135]. Other agents under investigation include tetrahydrobiopterin (BH4, a co-factor required for activation of NOS) and folic acid (which may mimic BH4). Of note hormones differentially regulate eNOS and NO bioavailability, with estrogen, insulin and growth hormone increasing it, and progesterone and glucocorticoids decreasing it [136]. Antioxidants such as melatonin and Vitamin C have been found to increase blood flow via an NO-dependent mechanism [137]. Evidence is emerging that statins, a class of lipid-lowering drugs, may have differential effects on eNOS and iNOS [138–140]. Of potential interest to chocolate lovers, Taubert et al., reported that regular intake of polyphenol-rich dark chocolate increases NO bioavailability [141]. Treatment of endothelial cells in culture with alcohol increases NO production by enhancing NOS activity [142–144], and alcohol feeding in rats increases aortic NO bioavailability [145]. These NO effects might explain some of the putative cardioprotection seen with moderate alcohol consumption [146–148]. However, while there is a lot of promise in capitalizing on the pre-clinical findings with respect to NO biology, translation to new modalities for cardiovascular disease management has not been uniformly fruitful [134]. Results of dietary nitrate supplementation in clinical trials, for example, have yielded variable outcomes with some beneficial, and some with no measurable effect [149,150].
Fig. 3.
Common risk factors for cardiovascular disease (CVD) such as those listed here are associated with 'endothelial dysfunction', a condition synonymous with reduced biological activity of nitric oxide (NO), and believed to be an initiating factor for atherogenesis.
Moreover, it is important to note that certain conditions such as hypercholesterolemia, hypertension and diabetes can lead to increased vascular production of superoxide (). Superoxide can react with the increased NO also produced in such circumstances forming the strong oxidant peroxynitrite (ONOO−) that causes protein nitration, lipid peroxidation, DNA damage and cell death [151]. Excessive peroxinitrite is believed an important contributor to cardiovascular pathologies including atherosclerosis. Thus, NO must be considered a pleiotropic molecule, with both physiological and pathological potential as it has the capacity for a dual role as a protective agent, or as a target for generating harmful peroxinitrite, depending on the oxidative milieu [152,151]. As with most things in biology, it is the ’balance’ that is important and that determines physiological homeostasis or pathology development.
10.2. PGI2
Another important endothelial-derived vasodilator and athe-roprotective agent, whose release is stimulated by shear stress and in response to acetylcholine, is prostacyclin (PGI2) [153,154]. PGI2 is synthesized by cyclooxygenase-2 (COX-2) from arachidonic acid [155] and increases the second messenger cyclic adenosine monophosphate (cAMP) in smooth muscle cells as well as in platelets. PGI2 mediates its actions through specific cell surface, 7-membrane spanning, G protein-coupled receptors, known as PG12 receptor or IP [156,157]. In contrast to NO, PGI2does not appear to contribute to the maintenance of basal vascular tone of large conduit arteries. However, in patients with a decreased NO bioavailability as in atherosclerosis, COX-2-derived prostaglandins can play a compensatory role [158]. Moreover, PGI2 exerts important platelet inhibitory effects and can act synergistically with NO in this regard [159]. Like NO, PGI2 can also inhibit leukocyte adhesion and vascular smooth muscle proliferation [160] and crosstalk between the two agents exists. PGI2 facilitates the release of NO by endothelial cells [161], and conversely, the action of PGI2 in vascular smooth muscle is potentiated by NO and NO indirectly via cGMP inhibition of phosphodiesterase 3, prolongs the half-life of cAMP [162]. PGI2's effects counteract those of thromboxane (TXA2) that is synthesized through COX-1 and causes platelet aggregation, vasoconstriction and vascular proliferation, and the balance of these two prostanoids is thus important in cardiovascular hemostasis [157]. In accordance with the concept of PGI2 being atheroprotective, an orally active PGI2 stable analog, Bera-prost, or PGI2 synthase (PGIS) gene transfer inhibited neointimal formation in animal models of arterial injury [163,164]. Beraprost is widely used in therapy for pulmonary artery hypertension and chronic arterial obstruction [165]. The withdrawal of the Cox-2 inhibitor Vioxx in 2004 due to increased cardiovascular events supports the critical role of PGI2 in inhibiting atherothrombosis in humans. In a clinical study, the IP variant (R212C), which was defective in cAMP production, was closely linked to disease severity and adverse cardiovascular events in patients with cardiovascular diseases [166]. In addition to the classical IP-cAMP pathway, evidence suggests that PGI2 also mediates its effects on the vasculature via the nuclear receptor peroxisome proliferator activated receptor δ (PPAR)[167].
10.3. EDHF
Any vasodilator response that persists after combined inhibition of NO (e.g., by L-NMMA) and PGI2 (e.g., by aspirin) is attributed to substances that cause hyperpolarization of the underlying vascular smooth muscle via a mechanism involving increased potassium (K+) conductance resulting in a reduction in intracellular K+ and the subsequent depolarization of the cell and relaxation. Molecules and mediators postulated to act as EDHF include K+ [168], cytochrome P450 metabolites [169], lipoxygenase products [170], reactive oxygen species (H2O2) [171], C-type natriuretic peptide [172], and electrical coupling through myoendothelial gap junctions [173].
11. Vasoconstrictors
Opposing the action of the endothelial-derived vasodilators (NO, PGI2, EDHFs) are a number of endothelial-derived vasoconstrictors, chief among them endothelin-1 (ET-1), angiotensin-II (ANG-II) and vasoconstrictor prostaglandins.
11.1. ET-1
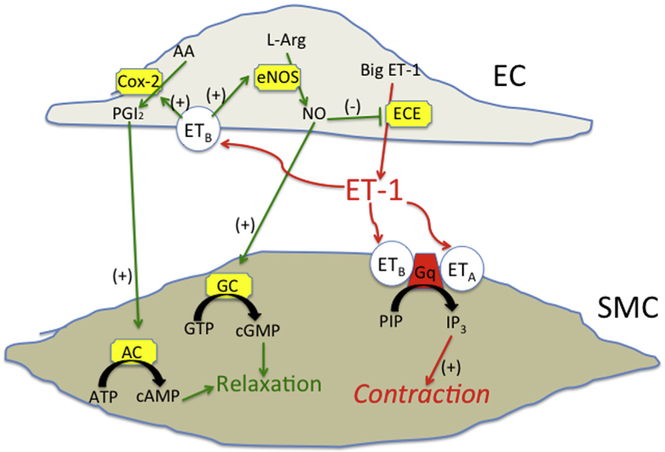
In 1988, Dr. Yanagisawa's group identified endothelin-1 (ET-1), a 21 amino acid peptide generated by the endothelin converting enzyme (ECE)-mediated cleavage of a larger precursor ‘big endo-thelin-1’ (Big ET-1), as the first endothelium-derived contracting factor [174]. ET-1 is one of the most potent endogenous vasoconstrictors (for review [175]. It is produced mainly by endothelial cells, but also by vascular smooth muscle cells, leukocytes and macrophages [175]. ET-1 and NO are functionally closely interdependent [176]; NO strongly inhibits the release of ET-1 from the endothelium and ET-1 strongly inhibits NO-mediated vasodilation and vice versa [175,177]. There are 3 isoforms of endothelin: ET-1, −2 and −3, with ET-1 most relevant in the vasculature and in contributing to the maintenance of vascular tone [178]. At elevated concentrations, associated with pathological conditions, ET-1 is also pro-inflammatory and promotes smooth muscle proliferation [179,180]. Elevated levels of ET-1 have been implicated in the pathogenesis of hypertension, vasospasm and heart failure, in addition to atherosclerosis. Increased expression of ET-1 and ECE is seen in human arteries at different stages of atherosclerosis [181]. The biological effects of ET-1 are mediated through activation of two receptors, ETA and ETB [182,183]. ETA and ETB receptors expressed on vascular smooth muscle cells mediate the vasoconstrictor effects of ET-1. The ETB receptor is also found on endothelial cells, where its activation results in vasodilation mediated by PGI2 and NO release [184] (Fig. 4). ETB also plays a role in the clearance of circulating ET-1 mediated by ligand-receptor complex internalization and intracellular degradation. Therefore, a reduction in ETB number, or ETB receptor blockade, might reduce ET-1 clearance, increasing ET-1 concentrations without altering production.Several ET receptor antagonists have been developed including mixed antagonists Bosetan and the more potent Macitentan, and the selective ETA antagonist Ambrisentan [185,186]. Restoration of the impaired activity of the NO system is seen following selective ETA receptor antagonism in a range of animal models of atherosclerosis, together with a reversal of atherosclerotic lesion development [187,188]. However mixed ETA/B receptor antagonism also seemed beneficial in inhibiting lesion development in mice [189]. Whether or not both receptors should be blocked to provide most clinical benefit in the case of cardiovascular disease is a matter of ongoing debate. More recently, combined inhibitors of ECE and neural endopeptidase (NEP) such as SLV306 (daglutril) are being widely tested in clinical trials [186].
Fig. 4.
Big endothelin-1 (inactive precursor peptide) is cleaved by endothelin converting enzyme (ECE) to form Endothelin-1 (ET-1). Endothelin receptors ETA and ETB are expressed on vascular smooth muscle cells (SMC) and mediate vasoconstriction. ETB is also expressed on endothelial cells (EC) where its activation can result in vasodilation mediated by nitric oxide (NO) and prostacyclin (PGI2) release.
11.2. Angiotensin-II/AT1R
The renin–angiotensin system (RAS) is a circulating hormonal system that regulates blood pressure, blood flow, fluid volume and electrolyte balance. Recent findings that the RAS is activated locally in the heart and vessel wall have expanded that view and it is now appreciated that it plays a critical role in the initiation and progression of atherosclerosis [190]. Indeed, with the exception of renin (which cleaves angiotensinogen to form angiotensin I), all components of the RAS are produced in the vasculature. Endothelial cells express angiotensin converting enzyme (ACE), the dipep-tidyl carboxypeptidase that converts angiotensin-1 to the physiologically active angiotensin-II (Ang-II) [191]. Both local and circulating Ang-II exert their activities through the binding to Ang-II type 1 (AT1) or type 2 (AT2) receptors. AT1 receptors are widely expressed on different cell types involved in atherogenesis and mediate most of the physiological and pathophysiological actions of Ang-II. A role for the AT2 receptor in cardiovascular disease remains controversial (for review [192]). Ang-II is a proathero-sclerotic mediator; it causes vasoconstriction and regulates not only adhesion molecule (VCAM-1, ICAM-1, P-selectin) expression but also cytokine, chemokine, and growth factor secretion within the arterial wall [193]. ACE inhibitors and angiotensin receptor blockers (ARBs) are established pharmacological tools in both primary and secondary prevention of atherosclerotic cardiovascular disease [194]. The endothelium is the main target organ for many cardiovascular drugs including ACE inhibitors, and evidence shows that their beneficial effects are not only due to blood pressure lowering but also due to a direct anti-inflammatory activity [194].
12. Antithrombotic/prothrombotic balance
The endothelium crucially maintains the lining of the blood vessel as nonthrombogenic [195]. An important pathophysiological consequence of endothelial dysfunction is a disturbed hemostatic balance of thrombotic and fibrinolytic states leading to altered blood fluidity and possible pathologic hemorrhage or clot formation at sites of vascular injury. In regard to its physiological ‘active anti-thrombotic’ role, endothelium associated factors such as the potent inhibitors of platelet aggregation PGI2 and NO, as well as heparin-like molecules, thrombomodulin, Ecto-ADPase, tissue plasminogen activator and urokinase all may contribute [196]. The endothelium is also capable of active pro-thrombotic behavior; it synthesizes thromboxane A2 (TxA2) which promotes platelet aggregation, it expresses adhesive co-factors for platelets such as von Willebrand factor, fibronectin and thrombospondin, and procoa-gulant factors such as factor V [197]. Moreover, the endothelium can be activated by various pathophysiologic stimuli to express tissue factor, a trigger for the fibrin-generating coagulation cascade [198,199]. Endothelial cells can also generate an inhibitor of the fibrinolytic pathway (plasminogen activator inibiyor-1 (PAI-1), which can reduce the rate of fibrin breakdown [200]. Thus, in physiologic conditions, the normal endothelium actively supports the fluid state of flowing blood and prevents activation of circulating cells, whereas injury to the endothelium triggers a series of biochemical and molecular reactions favoring blood arrest and vessel wall repair. In the latter case (i.e., dysfunctional endothelium), platelets may aggregate and stick to the endothelium thereby activating it and encouraging leukocyte adhesion, as well as releasing platelet-derived growth factors that stimulate intimal hyperplasia [201,202].
13. Endothelial progenitor cells
Evidence suggests that the injured endothelial monolayer may be regenerated by circulating bone marrow-derived endothelial progenitor cells (EPC), which accelerate re-endothelialization and protect against the initiation and progression of atherosclerosis [203–205,206]. EPC represent less than 1% of the cells in blood. They are generally purified from blood by density gradient centrifugation for mononuclear cells followed by attachment onto tissue culture plates, and characterized at early stages after attachment by positive expression for both an endothelial marker such as VEGFR2 and for hematopoietic stem cell markers CD133 and CD34. After expansion for several weeks they express endothelial markers including vascular endothelial (VE)-Cadherin and Von Williebrand factor (vWF) [207]. It should be noted, however, that controversy exists with respect to the identification and characterization of ‘EPC’ which may actually encompass several different populations, as well as with regard to their definitive role in the pathophysiology of atherosclerosis vs in angiogenesis [208,209]. Insufficient blood flow resulting in local tissue ischemia is recognized as a potent stimulus for recruitment of EPC [206]; EPC express chemokine receptor type 4 (CXCR-4) receptors that bind stromal-derived factor-1 (SDF-1) that is released at sites of ischemia [210]. Higher circulating levels of progenitor cells reflect greater repair capacity and have been shown to reduce the progression of atherosclerosis [211 ]. Age is a significant risk factor for the development of cardiovascular disease and interestingly, EPCs are subject to age-associated changes that diminish their number in circulation and function [212]. Decreased EPC numbers have also been associated with metabolic syndrome, which confers a high risk for cardiovascular disease [213]. Given the critical role of the endothelium in vascular health and the importance of maintaining a ‘healthy’ endothelium as opposed to a ‘dysfunctional’ one, clinical benefit may be derived from harnessing EPC that can differentiate into mature endothelial cells to use as therapy for vascular disease. With this in mind, strategies that have been employed to enhance EPC number and functionality include statins, ACE inhibitors, angiotensin receptor blockers and peroxisome proliferator-activated receptor gamma (PPAR-γ) agonists, although the mechanisms involved remain unclear [213]. Other clinical approaches involve providing exogenous EPC to the circulation to replenish numbers reduced in diseased patients [214]. Finally, the discovery of ‘resident’ stem/progenitor cells in the vessel wall that can differentiate into all types of vascular cells [215], and evidence that endothelial cells may transform into smooth muscle-like cells [216], has complicated the vascular ‘progenitor cell’ research field even further.
14. MicroRNAs (miRNAs)
Discovered in 1993, microRNAs (miRNAs) are short (19–25 nucleotides long) sequences of non-coding RNA that regulate genes at the post-transcriptional level. It is estimated that there may be up to 5000 miRs that finely tune the expression of a multitude of protein-coding genes [217], including those involved in signaling pathways controlling proliferation, differentiation and apoptosis. It is hardly surprising then, that a burgeoning role for miRNAs in endothelial dysfunction and atherogenesis has been recognized. Indeed, an expanding body of literature indicates that miRNAs affect nearly every aspect of atherosclerotic plaque initiation, development and progression including inflammation/chemo-kines, cholesterol homeostasis, cell adhesion, vascular cell proliferation/apoptosis, and EPC function (recently reviewed in Ref. [218,219]). For example, recent studies report that miR-24 targeting matrix metalloproteinase-14 (MMP-14) regulates macrophages [220], miR-126–5p promotes endothelial proliferation by suppressing Notch1 inhibitor delta-like 1 homolog (Dlk1) [221], miR-126 also inhibits VCAM-1 expression and leukocyte adhesion to endothelial cells [222], miR-145 regulates SMC differentiation and promotes plaque stability [223], miR-155 reduces inflammatory responses and enhances macrophage cholesterol efflux [224], and miR-302a modulates cholesterol homeostasis by affecting the ATP-binding cassette (ABC) transporter ABCA1 [225]. MicroRNAs are actively secreted by endothelial cells under physiological and pathophysiological conditions and can be quantified in blood. These circulating miRNA, which are very stable, are being viewed as promising biomarkers for a number of cardiovascular diseases [226]. Moreover, flow-sensitive miRNAs known as ‘mechano-miRs’ have also been identified in endothelial cells [227]. These include miR-10a, miR-23b, miR-21, miR-663, miR-92a, miR-143/145, miR-101 and miR-126; all of which regulate EC gene expression, affecting EC health or dysfuction and thus, atherogenesis. Given the important role of gene regulating miRs in endothelial function many are currently being considered as potential therapeutic targets to treat atherosclerosis. Therapies might consist of either introducing ‘atheroprotective’ miRs, or depleting ‘atherogenic’ miRs using anti-sense miRNAs.
15. Endothelial-mesenchymal transition (EndoMT)
Vascular endothelial cells can demonstrate plasticity in both developmental and pathological conditions. Generation of mesenchymal cells from endothelium, known as endothelial-mesenchymal transition (EndoMT), is a crucial step in endothelial cell differentiation to several lineages including fibroblasts, mural cells and adipocytes. EndoMT has been implicated in vascular remodeling associated with vein grafting, arteriosclerosis and atherosclerosis [228]. TGF-β has been identified as key in driving EndMT progression [229]. Murine cell lineage–tracing experiments showed that endothelial-derived cells contribute to neointimal formation through EndoMT following vein grafting which is dependent on early activation of the TGF-β Smad2/3-Slug signaling pathway [230]. Antagonism of TGF-β signaling decreased EndoMT and resulted in less neointimal formation when compared to controls. Histological examination of human vein grafts validated the murine data. Furthermore, as caveolin-1 is important for TGF-β receptor internalization and TGF-β signaling, it also appears critical for regulation of EndoMT [231]. EndoMT may be a link between factors initiating atherosclerosis, such as inflammation and disturbed flow, and the tissue remodeling that leads to plaque formation [232]. It appears that oscillatory shear stress reduces fibroblast growth factor receptor 1 (FGFR1) expression and FGF signaling, resulting in activation of endothelial TGF-β signaling and induction of EndoMT. Chen et al., demonstrated that ApoE −/−mice with disrupted ‘protective’ FGF endothelial signaling as a result of cell-specific deletion of FGF receptor substrate 2α exhibited extensive development of EndMT and increased neointima formation [232]. Moreover, in human patients the level of coronary artery disease correlated strongly with loss of endothelial FGFR1 expression, activation of endothelial TGF-β signaling, and the extent of EndoMT [232]. EndoMT is thought to promote plaque growth by increasing deposition of fibronectin and increasing expression of cell adhesion molecules ICAM and VCAM, thereby further promoting recruitment of circulating monocytes and leukocytes and inducing formation of new mesenchymal cells, leading to expansion of neointima. In a separate study, Moonen et al., reported that while steady flow inhibited EndoMT, endothelial cells exposed to disturbed flow underwent EndoMT and exhibited atherogenic differentiation. Gain- and loss-of-function studies established a pivotal role for ERK5 signaling in the inhibition of EndoMT [233]. Collectively, these data suggest that inhibition of EndoMT might prove to be a novel therapeutic strategy to treat atherosclerosis.
16. Summary
The endothelium is critical in maintaining physiological balance in the vasculature and may be considered the gatekeeper of vessel health. Endothelial cells synthesize and release many factors that locally regulate permeability, vascular tone, smooth muscle cell growth and migration, inflammatory responses and platelet function. Upsetting this tightly regulated balance, such as occurs when the endothelium becomes dysfunctional in response to a variety of different risk factors, leads to the initiation and development of atherosclerotic lesions. The endothelium is, thus, an important target for therapies, both current and in the development phase, for cardiovascular disease.
Footnotes
Conflicts of interest
Authors Profs Paul A Cahill and Eileen M Redmond, submitting the review titled “Vascular Endothelium–Gatekeeper of Vessel Health” declare no conflicts of interest.
References
- [1].Ross R, Atherosclerosis-an inflammatory disease, N. Engl. J. Med. 340 (1999) 115–126. [DOI] [PubMed] [Google Scholar]
- [2].Mestas J, Ley K, Monocyte-endothelial cell interactions in the development of atherosclerosis, Trends Cardiovasc. Med. 18 (2008) 228–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Libby P, Ridker PM, Hansson GK, Progress and challenges in translating the biology of atherosclerosis, Nature 473 (2011) 317–325. [DOI] [PubMed] [Google Scholar]
- [4].Blasi C, The autoimmune origin of atherosclerosis, Atherosclerosis 201 (2008) 17–32. [DOI] [PubMed] [Google Scholar]
- [5].Morel DW, DiCorleto PE, Chisolm GM, Endothelial and smooth muscle cells alter low density lipoprotein in vitro by free radical oxidation, Arte-riosclerosis 4 (1984) 357–364. [DOI] [PubMed] [Google Scholar]
- [6].Steinbrecher UP, Parthasarathy S, Leake DS, et al. , Modification of low density lipoprotein by endothelial cells involves lipid peroxidation and degradation of low density lipoprotein phospholipids, Proc. Natl. Acad. Sci. U. S.A. 81 (1984) 3883–3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cathcart MK, Morel DW, Chisolm GM 3rd, Monocytes and neutrophils oxidize low density lipoprotein making it cytotoxic, J. Leukoc. Biol. 38 (1985) 341–350. [DOI] [PubMed] [Google Scholar]
- [8].Parthasarathy S, Printz DJ, Boyd D, et al. , Macrophage oxidation of low density lipoprotein generates a modified form recognized by the scavenger receptor, Arteriosclerosis 6 (1986) 505–510. [DOI] [PubMed] [Google Scholar]
- [9].Mitra S, Goyal T, Mehta JL, Oxidized LDL, LOX-1 and atherosclerosis, Cardiovasc. Drugs Ther. Int. Soc. Cardiovasc. Pharmacother. 25 (2011) 419–429. [DOI] [PubMed] [Google Scholar]
- [10].Ogunrinade O, Kameya GT, Truskey GA, Effect of fluid shear stress on the permeability of the arterial endothelium, Ann. Biomed. Eng. 30 (2002) 430–446. [DOI] [PubMed] [Google Scholar]
- [11].Michel CC, Curry FE, Microvascular permeability, Physiol. Rev. 79 (1999) 703–761. [DOI] [PubMed] [Google Scholar]
- [12].Lum H, Malik AB, Mechanisms of increased endothelial permeability, Can. J. Physiol. Pharmacol. 74 (1996) 787–800. [DOI] [PubMed] [Google Scholar]
- [13].Tilton RG, Chang KC, LeJeune WS, et al. , Role for nitric oxide in the hyperpermeability and hemodynamic changes induced by intravenous VEGF, Investig. Ophthalmol. Vis. Sci. 40 (1999) 689–696. [PubMed] [Google Scholar]
- [14].Ashina K, Tsubosaka Y, Kobayashi K, et al. , VEGF-induced blood flow increase causes vascular hyper-permeability in vivo, Biochem. Biophy. Res. Commun. 464 (2015) 590–595. [DOI] [PubMed] [Google Scholar]
- [15].Wong BW, Rahmani M, Luo Z, et al. , Vascular endothelial growth factor increases human cardiac microvascular endothelial cell permeability to lowdensity lipoproteins, J. Heart Lung Transpl. 28 (2009) 950–957. [DOI] [PubMed] [Google Scholar]
- [16].Bates DO, Vascular endothelial growth factors and vascular permeability, Cardiovasc. Res. 87 (2010) 262–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Joshi AD, Dimitropoulou C, Thangjam G, et al. , Heat shock protein 90 inhibitors prevent LPS-induced endothelial barrier dysfunction by disrupting RhoA signaling, Am. J. Respir. Cell Mol. Biol. 50 (2014) 170–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Tarbell JM, Shear stress and the endothelial transport barrier, Cardiovasc. Res. 87 (2010) 320–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].LaMack JA, Himburg HA, Li XM, et al. , Interaction of wall shear stress magnitude and gradient in the prediction of arterial macromolecular permeability, Ann. Biomed. Eng. 33 (2005) 457–464. [DOI] [PubMed] [Google Scholar]
- [20].Rutledge JC, Curry FR, Lenz JF, et al. , Low density lipoprotein transport across a microvascular endothelial barrier after permeability is increased, Circ. Res. 66 (1990) 486–495. [DOI] [PubMed] [Google Scholar]
- [21].Soulis JV, Fytanidis DK, Papaioannou VC, et al. , Wall shear stress on LDL accumulation in human RCAs, Med. Eng. Phys. 32 (2010) 867–877. [DOI] [PubMed] [Google Scholar]
- [22].Berk BC, Min W, Yan C, et al. , Atheroprotective mechanisms activated by fluid shear stress in endothelial cells, Drug News Perspect. 15 (2002) 133–139. [DOI] [PubMed] [Google Scholar]
- [23].Skalen K, Gustafsson M, Rydberg EK, et al. , Subendothelial retention of atherogenic lipoproteins in early atherosclerosis, Nature 417 (2002) 750–754. [DOI] [PubMed] [Google Scholar]
- [24].Badimon L, Storey RF, Vilahur G, Update on lipids, inflammation and atherothrombosis, Thromb. Haemost. 105 (Suppl 1) (2011) S34–S42. [DOI] [PubMed] [Google Scholar]
- [25].Rozenberg I, Sluka SH, Rohrer L, et al. , Histamine H1 receptor promotes atherosclerotic lesion formation by increasing vascular permeability for lowdensity lipoproteins, Arterioscler. Thromb. Vasc. Biol. 30 (2010) 923–930. [DOI] [PubMed] [Google Scholar]
- [26].Mullick AE, McDonald JM, Melkonian G, et al. , Reactive carbonyls from tobacco smoke increase arterial endothelial layer injury, Am. J. Physiol. Heart Circ. Physiol. 283 (2002) H591–H597. [DOI] [PubMed] [Google Scholar]
- [27].Kundumani-Sridharan V, Dyukova E, Hansen DE 3rd, et al. , 12/15-Lipoxygenase mediates high-fat diet-induced endothelial tight junction disruption and monocyte transmigration: a new role for 15(S)-hydroxyeicosatetraenoic acid in endothelial cell dysfunction, J. Biol. Chem. 288 (2013) 15830–15842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Whyte JJ, Laughlin MH, The effects of acute and chronic exercise on the vasculature, Acta Physiol. Oxf. 199 (2010) 441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Garcia JG, Liu F, Verin AD, et al. , Sphingosine 1-phosphate promotes endothelial cell barrier integrity by Edg-dependent cytoskeletal rearrangement, J. Clin. Investig. 108 (2001) 689–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Xiong Y, Hla T, S1P control of endothelial integrity, Curr. Top. Microbiol. Immunol. 378 (2014) 85–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Argraves KM, Gazzolo PJ, Groh EM, et al. , High density lipoprotein-associated sphingosine 1-phosphate promotes endothelial barrier function, J. Biol. Chem. 283 (2008) 25074–25081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Wilkerson BA, Grass GD, Wing SB, et al. , Sphingosine 1-phosphate (S1P) carrier-dependent regulation of endothelial barrier: high density lipoprotein (HDL)-S1P prolongs endothelial barrier enhancement as compared with albumin-S1P via effects on levels, trafficking, and signaling of S1P1, J. Biol. Chem. 287 (2012) 44645–44653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Pizurki L, Zhou Z, Glynos K, et al. , Angiopoietin-1 inhibits endothelial permeability, neutrophil adherence and IL-8 production, Br. J. Pharmacol. 139 (2003) 329–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Langeler EG, van Hinsbergh VW, Norepinephrine and iloprost improve barrier function of human endothelial cell monolayers: role of cAMP, Am. J. Physiol. 260 (1991) C1052–C1059. [DOI] [PubMed] [Google Scholar]
- [35].Surapisitchat J, Beavo JA, Regulation of endothelial barrier function by cyclic nucleotides: the role of phosphodiesterases, Handb. Exp. Pharmacol. (2011) 193–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Chappell D, Jacob M, Paul O, et al. , The glycocalyx of the human umbilical vein endothelial cell: an impressive structure ex vivo but not in culture, Circ. Res. 104 (2009) 1313–1317. [DOI] [PubMed] [Google Scholar]
- [37].Alphonsus CS, Rodseth RN, The endothelial glycocalyx: a review of the vascular barrier, Anaesthesia 69 (2014) 777–784. [DOI] [PubMed] [Google Scholar]
- [38].Rehm M, Bruegger D, Christ F, et al. , Shedding of the endothelial glycocalyx in patients undergoing major vascular surgery with global and regional ischemia, Circulation 116 (2007) 1896–1906. [DOI] [PubMed] [Google Scholar]
- [39].Beresewicz A, Czarnowska E, Maczewski M, Ischemic preconditioning and superoxide dismutase protect against endothelial dysfunction and endothelium glycocalyx disruption in the postischemic guinea-pig hearts, Mol. Cell. Biochem. 186 (1998) 87–97. [PubMed] [Google Scholar]
- [40].Mulivor AW, Lipowsky HH, Inflammation- and ischemia-induced shedding of venular glycocalyx, Am. J. Physiol. Heart Circ. Physiol. 286 (2004) H1672–H1680. [DOI] [PubMed] [Google Scholar]
- [41].Henry CB, Duling BR, TNF-alpha increases entry of macromolecules into luminal endothelial cell glycocalyx, Am. J. Physiol. Heart Circ. Physiol. 279 (2000) H2815–H2823. [DOI] [PubMed] [Google Scholar]
- [42].Becker BF, Chappell D, Bruegger D, et al. , Therapeutic strategies targeting the endothelial glycocalyx: acute deficits, but great potential, Cardiovasc. Res. 87 (2010) 300–310. [DOI] [PubMed] [Google Scholar]
- [43].van den Berg BM, Spaan JA, Rolf TM, et al. , Atherogenic region and diet diminish glycocalyx dimension and increase intima-to-media ratios at murine carotid artery bifurcation, Am. J. Physiol. Heart Circ. Physiol. 290 (2006) H915–H920. [DOI] [PubMed] [Google Scholar]
- [44].Gouverneur M, Berg B, Nieuwdorp M, et al. , Vasculoprotective properties of the endothelial glycocalyx: effects of fluid shear stress, J. Intern. Med. 259 (2006) 393–400. [DOI] [PubMed] [Google Scholar]
- [45].Huxley VH, Williams DA, Role of a glycocalyx on coronary arteriole permeability to proteins: evidence from enzyme treatments, Am. J. Physiol. Heart Circ. Physiol. 278 (2000) H1177–H1185. [DOI] [PubMed] [Google Scholar]
- [46].Constantinescu AA, Vink H, Spaan JA, Endothelial cell glycocalyx modulates immobilization of leukocytes at the endothelial surface, Arterioscler. Thromb. Vasc. Biol. 23 (2003) 1541–1547. [DOI] [PubMed] [Google Scholar]
- [47].Mochizuki S, Vink H, Hiramatsu O, et al. , Role of hyaluronic acid glycosaminoglycans in shear-induced endothelium-derived nitric oxide release, Am. J. Physiol. Heart Circ. Physiol. 285 (2003) H722–H726. [DOI] [PubMed] [Google Scholar]
- [48].Kelly R, Ruane-O'Hora T, Noble MI, et al. , Differential inhibition by hyperglycaemia of shear stress- but not acetylcholine-mediated dilatation in the iliac artery of the anaesthetized pig, J. Physiol. 573 (2006) 133–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Drake-Holland AJ, Noble MI, The important new drug target in cardiovascular medicine-the vascular glycocalyx, Cardiovasc. Hematol. Disord. Drug Targets 9 (2009) 118–123. [DOI] [PubMed] [Google Scholar]
- [50].Mennander AA, Shalaby A, Oksala N, et al. , Diazoxide may protect endothelial glycocalyx integrity during coronary artery bypass grafting, Scand. Cardiovasc. J. 46 (2012) 339–344. [DOI] [PubMed] [Google Scholar]
- [51].Broekhuizen LN, Lemkes BA, Mooij HL, et al. , Effect of sulodexide on endothelial glycocalyx and vascular permeability in patients with type 2 diabetes mellitus, Diabetologia 53 (2010) 2646–2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Davies PF, Flow-mediated endothelial mechanotransduction, Physiol. Rev. 75 (1995) 519–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Ando J, Yamamoto K, Effects of shear stress and stretch on endothelial function, Antioxid. Redox Signal 15 (2011) 1389–1403. [DOI] [PubMed] [Google Scholar]
- [54].Ohno M, Gibbons GH, Dzau VJ, et al. , Shear stress elevates endothelial cGMP. Role of a potassium channel and G protein coupling, Circulation 88 (1993) 193–197. [DOI] [PubMed] [Google Scholar]
- [55].Koslow AR, Stromberg RR, Friedman LI, et al. , A flow system for the study of shear forces upon cultured endothelial cells, J. Biomech. Eng. 108 (1986) 338–341. [DOI] [PubMed] [Google Scholar]
- [56].Redmond EM, Cahill PA, Sitzmann JV, Perfused transcapillary smooth muscle and endothelial cell co-culture–a novel in vitro model, In Vitro Cell Dev. Biol. Anim. 31 (1995) 601–609. [DOI] [PubMed] [Google Scholar]
- [57].Redmond EM, Cahill PA, Sitzmann JV, Flow-mediated regulation of G-protein expression in cocultured vascular smooth muscle and endothelial cells, Arterioscler. Thromb. Vasc. Biol. 18 (1998) 75–83. [DOI] [PubMed] [Google Scholar]
- [58].Kanda K, Matsuda T, Behavior of arterial wall cells cultured on periodically stretched substrates, Cell Transplant. 2 (1993) 475–484. [DOI] [PubMed] [Google Scholar]
- [59].Morrow D, Cullen JP, Cahill PA, et al. , Cyclic strain regulates the Notch/CBF-1 signaling pathway in endothelial cells: role in angiogenic activity, Arterioscler. Thromb. Vasc. Biol. 27 (2007) 1289–1296. [DOI] [PubMed] [Google Scholar]
- [60].Hsieh HJ, Liu CA, Huang B, et al. , Shear-induced endothelial mechanotransduction: the interplay between reactive oxygen species (ROS) and nitric oxide (NO) and the pathophysiological implications, J. Biomed. Sci. 21 (2014) 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Resnick N, Collins T, Atkinson W, et al. , Platelet-derived growth factor B chain promoter contains a cis-acting fluid shear-stress-responsive element, Proc. Natl. Acad. Sci. U. S. A. 90 (1993) 4591–4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Baeyens N, Mulligan-Kehoe MJ, Corti F, et al. , Syndecan 4 is required for endothelial alignment in flow and atheroprotective signaling, Proc. Natl. Acad. Sci. U. S. A. 111 (2014) 17308–17313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Liu Y, Collins C, Kiosses WB, et al. , A novel pathway spatiotemporally activates Rac1 and redox signaling in response to fluid shear stress, J. Cell Biol. 201 (2013) 863–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Li J, Hou B, Beech DJ, Endothelial Piezo1: life depends on it, Channels Austin 9 (2015) 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Ranade SS, Qiu Z, Woo SH, et al. , Piezo1, a mechanically activated ion channel, is required for vascular development in mice, Proc. Natl. Acad. Sci. U. S. A. 111 (2014) 10347–10352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Jung B, Obinata H, Galvani S, et al. , Flow-regulated endothelial S1P receptor-1 signaling sustains vascular development, Dev. Cell 23 (2012) 600–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Cullen JP, Nicholl SM, Sayeed S, et al. , Plasminogen activator inhibitor-1 deficiency enhances flow-induced smooth muscle cell migration, Thromb. Res. 114 (2004) 57–65. [DOI] [PubMed] [Google Scholar]
- [68].Gimbrone MA Jr., Topper JN, Nagel T, et al. , Endothelial dysfunction, hemodynamic forces, and atherogenesis, Ann. N. Y. Acad. Sci. 902 (2000) 230–239 discussion 239–240. [DOI] [PubMed] [Google Scholar]
- [69].Pradhan S, Sumpio B, Molecular and biological effects of hemodynamics on vascular cells, Front. Biosci. J. Virtual Libr. 9 (2004) 3276–3285. [DOI] [PubMed] [Google Scholar]
- [70].Chiu JJ, Chien S, Effects of disturbed flow on vascular endothelium: pathophysiological basis and clinical perspectives, Physiol. Rev. 91 (2011) 327–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Heo KS, Fujiwara K, Abe J, Shear stress and atherosclerosis, Mol. Cells 37 (2014) 435–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Stone PH, Coskun AU, Kinlay S, et al. , Effect of endothelial shear stress on the progression of coronary artery disease, vascular remodeling, and in-stent restenosis in humans: in vivo 6-month follow-up study, Circulation 108 (2003) 438–444. [DOI] [PubMed] [Google Scholar]
- [73].Brooks AR, Lelkes PI, Rubanyi GM, Gene expression profiling of human aortic endothelial cells exposed to disturbed flow and steady laminar flow, Physiol. Genom. 9 (2002) 27–41. [DOI] [PubMed] [Google Scholar]
- [74].Dunn J, Thabet S, Jo H, Flow-dependent epigenetic DNA methylation in endothelial gene expression and atherosclerosis, Arterioscler. Thromb. Vasc. Biol. 35 (2015) 1562–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Jiang YZ, Jimenez JM, Ou K, et al. , Hemodynamic disturbed flow induces differential DNA methylation of endothelial Kruppel-Like Factor 4 promoter in vitro and in vivo, Circ. Res. 115 (2014) 32–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Langille BL, Adamson SL, Relationship between blood flow direction and endothelial cell orientation at arterial branch sites in rabbits and mice, Circ. Res. 48 (1981) 481–488. [DOI] [PubMed] [Google Scholar]
- [77].Akimoto S, Mitsumata M, Sasaguri T, et al. , Laminar shear stress inhibits vascular endothelial cell proliferation by inducing cyclin-dependent kinase inhibitor p21(Sdi1/Cip1/Waf1), Circ. Res. 86 (2000) 185–190. [DOI] [PubMed] [Google Scholar]
- [78].Davies PF, Remuzzi A, Gordon EJ, et al. , Turbulent fluid shear stress induces vascular endothelial cell turnover in vitro, Proc. Natl. Acad. Sci. U. S. A. 83 (1986) 2114–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Von Offenberg Sweeney N, Cummins PM, Cotter EJ, et al. , Cyclic strain-mediated regulation of vascular endothelial cell migration and tube formation, Biochem. Biophy. Res. Commun. 329 (2005) 573–582. [DOI] [PubMed] [Google Scholar]
- [80].Rubanyi GM, Romero JC, Vanhoutte PM, Flow-induced release of endothelium-derived relaxing factor, Am. J. Physiol. 250 (1986) H1145–H1149. [DOI] [PubMed] [Google Scholar]
- [81].Bhagyalakshmi A, Frangos JA, Mechanism of shear-induced prostacyclin production in endothelial cells, Biochem. Biophy. Res. Commun. 158 (1989) 31–37. [DOI] [PubMed] [Google Scholar]
- [82].Hendrickson RJ, Cappadona C, Yankah EN, et al. , Sustained pulsatile flow regulates endothelial nitric oxide synthase and cyclooxygenase expression in co-cultured vascular endothelial and smooth muscle cells, J. Mol. Cell Cardiol. 31 (1999) 619–629. [DOI] [PubMed] [Google Scholar]
- [83].Kuchan MJ, Frangos JA, Shear stress regulates endothelin-1 release via protein kinase C and cGMP in cultured endothelial cells, Am. J. Physiol. 264 (1993) H150–H156. [DOI] [PubMed] [Google Scholar]
- [84].Malek AM, Greene AL, Izumo S, Regulation of endothelin 1 gene by fluid shear stress is transcriptionally mediated and independent of protein kinase C and cAMP, Proc. Natl. Acad. Sci. U. S. A. 90 (1993) 5999–6003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Garg UC, Hassid A, Nitric oxide-generating vasodilators and 8-bromo-cyclic guanosine monophosphate inhibit mitogenesis and proliferation of cultured rat vascular smooth muscle cells, J. Clin. Investig. 83 (1989) 1774–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Alberts GF, Peifley KA, Johns A, et al. , Constitutive endothelin-1 over-expression promotes smooth muscle cell proliferation via an external autocrine loop, J. Biol. Chem. 269 (1994) 10112–10118. [PubMed] [Google Scholar]
- [87].Kohno M, Yokokawa K, Yasunari K, et al. , Effect of the endothelin family of peptides on human coronary artery smooth-muscle cell migration, J. Cardiovasc. Pharmacol. 31 (Suppl. 1) (1998) S84–S89. [DOI] [PubMed] [Google Scholar]
- [88].Ignarro LJ, Endothelium-derived nitric oxide: actions and properties, FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 3 (1989) 31–36. [DOI] [PubMed] [Google Scholar]
- [89].Moncada S, Prostacyclin and arterial wall biology, Arteriosclerosis 2 (1982) 193–207. [DOI] [PubMed] [Google Scholar]
- [90].Takada Y, Shinkai F, Kondo S, et al. , Fluid shear stress increases the expression of thrombomodulin by cultured human endothelial cells, Biochem. Biophy. Res. Commun. 205 (1994) 1345–1352. [DOI] [PubMed] [Google Scholar]
- [91].Arisaka T, Mitsumata M, Kawasumi M, et al. , Effects of shear stress on glycosaminoglycan synthesis in vascular endothelial cells, Ann. N. Y. Acad. Sci. 748 (1995) 543–554. [DOI] [PubMed] [Google Scholar]
- [92].Diamond SL, Eskin SG, McIntire LV, Fluid flow stimulates tissue plasminogen activator secretion by cultured human endothelial cells, Science 243 (1989) 1483–1485. [DOI] [PubMed] [Google Scholar]
- [93].Owens GK, Kumar MS, Wamhoff BR, Molecular regulation of vascular smooth muscle cell differentiation in development and disease, Physiol. Rev. 84 (2004) 767–801. [DOI] [PubMed] [Google Scholar]
- [94].Mitsumata M, Fishel RS, Nerem RM, et al. , Fluid shear stress stimulates platelet-derived growth factor expression in endothelial cells, Am. J. Physiol. 265 (1993) H3–H8. [DOI] [PubMed] [Google Scholar]
- [95].Malek AM, Gibbons GH, Dzau VJ, et al. , Fluid shear stress differentially modulates expression of genes encoding basic fibroblast growth factor and platelet-derived growth factor B chain in vascular endothelium, J. Clin. Investig.(1993) 2013–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Ohno M, Cooke JP, Dzau VJ, et al. , Fluid shear stress induces endothelial transforming growth factor beta-1 transcription and production. Modulation by potassium channel blockade, J. Clin. Investig. 95 (1995) 1363–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Sterpetti AV, Cucina A, Morena AR, et al. , Shear stress increases the release of interleukin-1 and interleukin-6 by aortic endothelial cells, Surgery 114 (1993) 911–914. [PubMed] [Google Scholar]
- [98].Merten M, Chow T, Hellums JD, et al. , A new role for P-selectin in shear-induced platelet aggregation, Circulation 102 (2000) 2045–2050. [DOI] [PubMed] [Google Scholar]
- [99].Ando J, Tsuboi H, Korenaga R, et al. , Shear stress inhibits adhesion of cultured mouse endothelial cells to lymphocytes by downregulating VCAM-1 expression, Am. J. Physiol. 267 (1994) C679–C687. [DOI] [PubMed] [Google Scholar]
- [100].Gerszten RE, Lim YC, Ding HT, et al. , Adhesion of monocytes to vascular cell adhesion molecule-1-transduced human endothelial cells: implications for atherogenesis, Circ. Res. 82 (1998) 871–878. [DOI] [PubMed] [Google Scholar]
- [101].Kaneto H, Katakami N, Matsuhisa M, et al. , Role of reactive oxygen species in the progression of type 2 diabetes and atherosclerosis, Mediat. Inflamm. 2010 (2010) 453892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Victor VM, Rocha M, Sola E, et al. , Oxidative stress, endothelial dysfunction and atherosclerosis, Curr. Pharm. Des. 15 (2009) 2988–3002. [DOI] [PubMed] [Google Scholar]
- [103].Birukov KG, Cyclic stretch, reactive oxygen species, and vascular remodeling, Antioxid. Redox Signal 11 (2009) 1651–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Chatterjee S, Browning EA, Hong N, et al. , Membrane depolarization is the trigger for PI3K/Akt activation and leads to the generation of ROS, Am. J. Physiol. Heart Circ. Physiol. 302 (2012) H105–H114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Mowbray AL, Kang DH, Rhee SG, et al. , Laminar shear stress up-regulates peroxiredoxins (PRX) in endothelial cells: PRX 1 as a mechanosensitive antioxidant, J. Biol. Chem. 283 (2008) 1622–1627. [DOI] [PubMed] [Google Scholar]
- [106].Takabe W, Warabi E, Noguchi N, Anti-atherogenic effect of laminar shear stress via Nrf2 activation, Antioxid. Redox Signal 15 (2011) 1415–1426. [DOI] [PubMed] [Google Scholar]
- [107].Liu XM, Peyton KJ, Durante W, Physiological cyclic strain promotes endothelial cell survival via the induction of heme oxygenase-1, Am. J. Physiol. Heart Circ. Physiol. 304 (2013) H1634–H1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Cummins PM, von Offenberg Sweeney N, Killeen MT, et al. , Cyclic strain-mediated matrix metalloproteinase regulation within the vascular endothelium: a force to be reckoned with, Am. J. Physiol. Heart Circ. Physiol. 292 (2007) H28–H42. [DOI] [PubMed] [Google Scholar]
- [109].Liu HB, Zhang J, Xin SY, et al. , Mechanosensitive properties in the endothelium and their roles in the regulation of endothelial function, J. Cardiovasc. Pharmacol. 61 (2013) 461–470 [DOI] [PubMed] [Google Scholar]
- [110].Kou B, Zhang J, Singer DR, Effects of cyclic strain on endothelial cell apoptosis and tubulogenesis are dependent on ROS production via NAD(P)H subunit p22phox, Microvasc. Res. 77 (2009) 125–133. [DOI] [PubMed] [Google Scholar]
- [111].Martin FA, McLoughlin A, Rochfort KD, et al. , Regulation of thrombomodulin expression and release in human aortic endothelial cells by cyclic strain, PLoS One 9 (2014) e108254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [112].Jiang Y, Kohara K, Hiwada K, Association between risk factors for atherosclerosis and mechanical forces in carotid artery, Stroke J. Cereb. Circ. 31 (2000) 2319–2324. [DOI] [PubMed] [Google Scholar]
- [113].Szostak J, Laurant P, The forgotten face of regular physical exercise: a 'natural' anti-atherogenic activity, Clin. Sci. 121 (2011) 91–106. [DOI] [PubMed] [Google Scholar]
- [114].Santos-Parker JR, LaRocca TJ, Seals DR, Aerobic exercise and other healthy lifestyle factors that influence vascular aging, Adv. Physiol. Educ. 38 (2014) 296–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Sandrock M, Schulze C, Schmitz D, et al. , Physical activity throughout life reduces the atherosclerotic wall process in the carotid artery, Br. J. Sports Med. 42 (2008) 839–844. [DOI] [PubMed] [Google Scholar]
- [116].Niebauer J, Hambrecht R, Velich T, et al. , Attenuated progression of coronary artery disease after 6 years of multifactorial risk intervention: role of physical exercise, Circulation 96 (1997) 2534–2541. [DOI] [PubMed] [Google Scholar]
- [117].Schuler F, Hambrecht R, Schlierf G, et al. , Regular physical exercise and low-fat diet. Effects on progression of coronary artery disease, Circulation 86 (1992) 1–11. [DOI] [PubMed] [Google Scholar]
- [118].Laughlin MH, Newcomer SC, Bender SB, Importance of hemodynamic forces as signals for exercise-induced changes in endothelial cell phenotype, J. Appl. Physiol. 104 (2008) 588–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Ramkhelawon B, Vilar J, Rivas D, et al. , Shear stress regulates angiotensin type 1 receptor expression in endothelial cells, Circ. Res. 105 (2009) 869–875. [DOI] [PubMed] [Google Scholar]
- [120].Libby P, Inflammation in atherosclerosis, Nature 420 (2002) 868–874. [DOI] [PubMed] [Google Scholar]
- [121].Church TS, Barlow CE, Earnest CP, et al. , Associations between cardiorespiratory fitness and C-reactive protein in men, Arterioscler. Thromb. Vasc. Biol. 22 (2002) 1869–1876. [DOI] [PubMed] [Google Scholar]
- [122].Kondo N, Nomura M, Nakaya Y, et al. , Association of inflammatory marker and highly sensitive C-reactive protein with aerobic exercise capacity, maximum oxygen uptake and insulin resistance in healthy middle-aged volunteers, Circ. J. 69 (2005) 452–457. [DOI] [PubMed] [Google Scholar]
- [123].Mora S, Cook N, Buring JE, et al. , Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms, Circulation 116 (2007) 2110–2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Gjevestad GO, Holven KB, Ulven SM, Effects of exercise on gene expression of inflammatory markers in human peripheral blood cells: a systematic review, Curr. Cardiovasc. Risk Rep. 9 (2015) 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [125].Palmefors H, DuttaRoy S, Rundqvist B, et al. , The effect of physical activity or exercise on key biomarkers in atherosclerosis–a systematic review, Atherosclerosis 235 (2014) 150–161. [DOI] [PubMed] [Google Scholar]
- [126].Furchgott RF, Zawadzki JV, The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine, Nature 288 (1980) 373–376. [DOI] [PubMed] [Google Scholar]
- [127].Ignarro LJ, Byrns RE, Buga GM, et al. , Endothelium-derived relaxing factor from pulmonary artery and vein possesses pharmacologic and chemical properties identical to those of nitric oxide radical, Circ. Res. 61 (1987) 866–879. [DOI] [PubMed] [Google Scholar]
- [128].Furchgott RF, Vanhoutte PM, Endothelium-derived relaxing and contracting factors, FASEB J. Off. Publ. Fed. Am. Soc. Exp. Biol. 3 (1989) 2007–2018. [PubMed] [Google Scholar]
- [129].Moncada S, Higgs EA, Endogenous nitric oxide: physiology, pathology and clinical relevance, Eur. J. Clin. Investig. 21 (1991) 361–374. [DOI] [PubMed] [Google Scholar]
- [130].Gkaliagkousi E, Ferro A, Nitric oxide signalling in the regulation of cardiovascular and platelet function, Front. Biosci. J. Virtual Libr. 16 (2011) 1873–1897. [DOI] [PubMed] [Google Scholar]
- [131].Sessa WC, Harrison JK, Barber CM, et al. , Molecular cloning and expression of a cDNA encoding endothelial cell nitric oxide synthase, J. Biol. Chem. 267 (1992) 15274–15276. [PubMed] [Google Scholar]
- [132].Govers R, Rabelink TJ, Cellular regulation of endothelial nitric oxide synthase, American journal of physiology, Ren. Physiol. 280 (2001) F193–F206. [DOI] [PubMed] [Google Scholar]
- [133].Schuler G, Adams V, Goto Y, Role of exercise in the prevention of cardiovascular disease: results, mechanisms, and new perspectives, Eur. Heart J. 34 (2013) 1790–1799. [DOI] [PubMed] [Google Scholar]
- [134].Yetik-Anacak G, Catravas JD, Nitric oxide and the endothelium: history and impact on cardiovascular disease, Vasc. Pharmacol. 45 (2006) 268–276. [DOI] [PubMed] [Google Scholar]
- [135].de Nigris F, Lerman LO, Ignarro SW, et al. , Beneficial effects of antioxidants and L-arginine on oxidation-sensitive gene expression and endothelial NO synthase activity at sites of disturbed shear stress, Proc. Natl. Acad. Sci. U. S. A. 100 (2003) 1420–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Duckles SP, Miller VM, Hormonal modulation of endothelial NO production, Pflugers Arch. 459 (2010) 841–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Thakor AS, Herrera EA, Seron-Ferre M, et al. , Melatonin and vitamin C increase umbilical blood flow via nitric oxide-dependent mechanisms, J. Pineal Res. 49 (2010) 399–406. [DOI] [PubMed] [Google Scholar]
- [138].Jantzen F, Konemann S, Wolff B, et al. , Isoprenoid depletion by statins antagonizes cytokine-induced down-regulation of endothelial nitric oxide expression and increases NO synthase activity in human umbilical veinendothelial cells, J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 58 (2007) 503–514. [PubMed] [Google Scholar]
- [139].Malik S, Sharma AK, Bharti S, et al. , In vivo cardioprotection by pitavastatin from ischemic-reperfusion injury through suppression of IKK/NF-kappaB and upregulation of pAkt-e-NOS, J. Cardiovasc. Pharmacol. 58 (2011) 199–206. [DOI] [PubMed] [Google Scholar]
- [140].Datar R, Kaesemeyer WH, Chandra S, et al. , Acute activation of eNOS by statins involves scavenger receptor-B1, G protein subunit Gi, phospholipase C and calcium influx, Br. J. Pharmacol. 160 (2010) 1765–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Taubert D, Roesen R, Lehmann C, et al. , Effects of low habitual cocoa intake on blood pressure and bioactive nitric oxide: a randomized controlled trial, JAMA 298 (2007) 49–60. [DOI] [PubMed] [Google Scholar]
- [142].Davda RK, Chandler LJ, Crews FT, et al. , Ethanol enhances the endothelial nitric oxide synthase response to agonists, Hypertension 21 (1993) 939–943. [DOI] [PubMed] [Google Scholar]
- [143].Hendrickson RJ, Cahill PA, Sitzmann JV, et al. , Ethanol enhances basal and flow-stimulated nitric oxide synthase activity in vitro by activating an inhibitory guanine nucleotide binding protein, J. Pharmacol. Exp. Ther. 289 (1999) 1293–1300. [PubMed] [Google Scholar]
- [144].Venkov BD, Myers PR, Tanner MA, et al. , Ethanol increases endothelial nitric oxide production through modulation of nitric oxide synthase expression, Thromb. Haemost. 81 (1999) 638–642. [PubMed] [Google Scholar]
- [145].Kleinhenz BJ, Sutliff RL, Polikandriotis JA, et al. , Chronic ethanol ingestion increases aortic endothelial nitric oxide synthase expression and nitric oxide production in the rat, Alcohol. Clin. Exp. Res. 32 (2008) 148–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [146].Mukamal KJ, Conigrave KM, Mittleman MA, et al. , Roles of drinking pattern and type of alcohol consumed in coronary heart disease in men, N. Engl. J. Med. 348 (2003) 109–118. [DOI] [PubMed] [Google Scholar]
- [147].Ronksley PE, Brien SE, Turner BJ, et al. , Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis, BMJ 342 (2011) d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [148].Cahill PA, Redmond EM, Alcohol and cardiovascular disease -modulation of vascular cell function, Nutrients 4 (2012) 297–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [149].Kapil V, Khambata RS, Robertson A, et al. , Dietary nitrate provides sustained blood pressure lowering in hypertensive patients: a randomized, phase 2, double-blind, placebo-controlled study, Hypertension 65 (2015) 320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [150].Marsch B, Theelen TL, Janssen BJ, et al. , The effect of prolonged dietary nitrate supplementation on atherosclerosis development, Atherosclerosis 245 (2015) 212–221. [DOI] [PubMed] [Google Scholar]
- [151].Fukai T, Ushio-Fukai M, Superoxide dismutases: role in redox signaling, vascular function, and diseases, Antioxid. Redox Signal 15 (2011) 1583–1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].Yamagishi S, Matsui T, Nitric oxide, a janus-faced therapeutic target for diabetic microangiopathy–Friend or foe? Pharmacol. Res. 64 (2011) 187–194. [DOI] [PubMed] [Google Scholar]
- [153].Okahara K, Sun B, Kambayashi J, Upregulation of prostacyclin synthesis-related gene expression by shear stress in vascular endothelial cells, Arterioscler. Thromb. Vasc. Biol. 18 (1998) 1922–1926. [DOI] [PubMed] [Google Scholar]
- [154].Flammer AJ, Luscher TF, Human endothelial dysfunction: EDRFs, Pflugers Arch. Eur. J. Physiol. 459 (2010) 1005–1013. [DOI] [PubMed] [Google Scholar]
- [155].Moncada S, Gryglewski R, Bunting S, et al. , An enzyme isolated from arteries transforms prostaglandin endoperoxides to an unstable substance that inhibits platelet aggregation, Nature 263 (1976) 663–665. [DOI] [PubMed] [Google Scholar]
- [156].Narumiya S, Sugimoto Y, Ushikubi F, Prostanoid receptors: structures, properties, and functions, Physiol. Rev. 79 (1999) 1193–1226. [DOI] [PubMed] [Google Scholar]
- [157].Smyth EM, Grosser T, Wang M, et al. , Prostanoids in health and disease, J. Lipid Res. 50 (Suppl. S423–428) (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Szerafin T, Erdei N, Fulop T, et al. , Increased cyclooxygenase-2 expression and prostaglandin-mediated dilation in coronary arterioles of patients with diabetes mellitus, Circ. Res. 99 (2006) e12–17. [DOI] [PubMed] [Google Scholar]
- [159].Radomski MW, Palmer RM, Moncada S, Comparative pharmacology of endothelium-derived relaxing factor, nitric oxide and prostacyclin in platelets, Br. J. Pharmacol. 92 (1987) 181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [160].Kawabe J, Ushikubi F, Hasebe N, Prostacyclin in vascular diseases. – Recent insights and future perspectives, Circ. J. Off. J. Jpn. Circ. Soc. 74 (2010) 836–843. [DOI] [PubMed] [Google Scholar]
- [161].Shimokawa H, Flavahan NA, Lorenz RR, et al. , Prostacyclin releases endothelium-derived relaxing factor and potentiates its action in coronary arteries of the pig, Br. J. Pharmacol. 95 (1988) 1197–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [162].Delpy E, Coste H, Gouville AC, Effects of cyclic GMP elevation on isoprenaline-induced increase in cyclic AMP and relaxation in rat aortic smooth muscle: role of phosphodiesterase 3, Br. J. Pharmacol. 119 (1996) 471–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].Isogaya M, Yamada N, Koike H, et al. , Inhibition of restenosis by beraprost sodium (a prostaglandin I2 analogue) in the atherosclerotic rabbit artery after angioplasty, J. Cardiovasc. Pharmacol. 25 (1995) 947–952. [DOI] [PubMed] [Google Scholar]
- [164].Numaguchi Y, Naruse K, Harada M, et al. , Prostacyclin synthase gene transfer accelerates reendothelialization and inhibits neointimal formation in rat carotid arteries after balloon injury, Arterioscler. Thromb. Vasc. Biol. 19 (1999) 727–733. [DOI] [PubMed] [Google Scholar]
- [165].Sugawara A, Kudo M, Saito A, et al. , Novel effects of beraprost sodium on vasculatures, Int. Angiol. 29 (2010) 28–32. [PubMed] [Google Scholar]
- [166].Arehart E, Stitham J, Asselbergs FW, et al. , Acceleration of cardiovascular disease by a dysfunctional prostacyclin receptor mutation: potential implications for cyclooxygenase-2 inhibition, Circ. Res. 102 (2008) 986–993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Lim H, Dey SK, A novel pathway of prostacyclin signaling-hanging out with nuclear receptors, Endocrinology 143 (2002) 3207–3210. [DOI] [PubMed] [Google Scholar]
- [168].Edwards G, Dora KA, Gardener MJ, et al. , K+ is an endothelium-derived hyperpolarizing factor in rat arteries, Nature 396 (1998) 269–272. [DOI] [PubMed] [Google Scholar]
- [169].Taddei S, Versari D, Cipriano A, et al. , Identification of a cytochrome P450 2C9-derived endothelium-derived hyperpolarizing factor in essential hypertensive patients, J. Am. Coll. Cardiol. 48 (2006) 508–515. [DOI] [PubMed] [Google Scholar]
- [170].Faraci FM, Sobey CG, Chrissobolis S, et al. , Arachidonate dilates basilar artery by lipoxygenase-dependent mechanism and activation of K(+) channels, Am. J. Physiol. Regul. Integr. Comp. Physiol. 281 (2001) R246–R253. [DOI] [PubMed] [Google Scholar]
- [171].Ellis A, Triggle CR, Endothelium-derived reactive oxygen species: their relationship to endothelium-dependent hyperpolarization and vascular tone, Can. J. Physiol. Pharmacol. 81 (2003) 1013–1028. [DOI] [PubMed] [Google Scholar]
- [172].Wei CM, Hu S, Miller VM, et al. , Vascular actions of C-type natriuretic peptide in isolated porcine coronary arteries and coronary vascular smooth muscle cells, Biochem. Biophys. Res. Commun. 205 (1994) 765–771. [DOI] [PubMed] [Google Scholar]
- [173].Griffith TM, Chaytor AT, Edwards DH, The obligatory link: role of gap junctional communication in endothelium-dependent smooth muscle hyperpolarization, Pharmacol. Res. Off. J. Italian Pharmacol. Soc. 49 (2004) 551–564. [DOI] [PubMed] [Google Scholar]
- [174].Yanagisawa M, Inoue A, Ishikawa T, et al. , Primary structure, synthesis, and biological activity of rat endothelin, an endothelium-derived vasoconstrictor peptide, Proc. Natl. Acad. Sci. U. S. A. 85 (1988) 6964–6967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [175].Thorin E, Webb DJ, Endothelium-derived endothelin-1, Pflugers Arch. Eur. J. Physiol. 459 (2010) 951–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [176].Luscher TF, Yang Z, Tschudi M, et al. , Interaction between endothelin-1 and endothelium-derived relaxing factor in human arteries and veins, Circ. Res. 66 (1990) 1088–1094. [DOI] [PubMed] [Google Scholar]
- [177].Gilbert P, Tremblay J, Thorin E, Endothelium-derived endothelin-1 reduces cerebral artery sensitivity to nitric oxide by a protein kinase C-independent pathway, Stroke J. Cereb. Circ. 32 (2001) 2351–2355. [DOI] [PubMed] [Google Scholar]
- [178].Callera G, Tostes R, Savoia C, et al. , Vasoactive peptides in cardiovascular (patho)physiology, Expert Rev. Cardiovasc. Ther. 5 (2007) 531–552. [DOI] [PubMed] [Google Scholar]
- [179].Anggrahini DW, Emoto N, Nakayama K, et al. , Vascular endothelial cellderived endothelin-1 mediates vascular inflammation and neointima formation following blood flow cessation, Cardiovasc. Res. 82 (2009) 143–151. [DOI] [PubMed] [Google Scholar]
- [180].Ivey ME, Osman N, Little PJ, Endothelin-1 signalling in vascular smooth muscle: pathways controlling cellular functions associated with atherosclerosis, Atherosclerosis 199 (2008) 237–247. [DOI] [PubMed] [Google Scholar]
- [181].Ihling C, Szombathy T, Bohrmann B, et al. , Coexpression of endothelinconverting enzyme-1 and endothelin-1 in different stages of human atherosclerosis, Circulation 104 (2001) 864–869. [DOI] [PubMed] [Google Scholar]
- [182].Arai H, Hori S, Aramori I, et al. , Cloning and expression of a cDNA encoding an endothelin receptor, Nature 348 (1990) 730–732. [DOI] [PubMed] [Google Scholar]
- [183].Sakurai T, Yanagisawa M, Takuwa Y, et al. , Cloning of a cDNA encoding a non-isopeptide-selective subtype of the endothelin receptor, Nature 348 (1990) 732–735. [DOI] [PubMed] [Google Scholar]
- [184].de Nucci G, Thomas R, D'Orleans-Juste P, et al. , Pressor effects of circulating endothelin are limited by its removal in the pulmonary circulation and by the release of prostacyclin and endothelium-derived relaxing factor, Proc. Natl. Acad. Sci. U. S. A. 85 (1988) 9797–9800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [185].Dhaun N, Pollock DM, Goddard J, et al. , Selective and mixed endothelin receptor antagonism in cardiovascular disease, Trends Pharmacol. Sci. 28 (2007) 573–579. [DOI] [PubMed] [Google Scholar]
- [186].Maguire JJ, Davenport AP, Endothelin@25-new agonists, antagonists, inhibitors and emerging research frontiers: IUPHAR Review 12, Br. J. Pharmacol. 171 (2014) 5555–5572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [187].Kowala MC, Rose PM, Stein PD, et al. , Selective blockade of the endothelin subtype A receptor decreases early atherosclerosis in hamsters fed cholesterol Am. J. Pathol. 146 (1995) 819–826. [PMC free article] [PubMed] [Google Scholar]
- [188].Barton M, Haudenschild CC, d'Uscio LV, et al. , Endothelin ETA receptor blockade restores NO-mediated endothelial function and inhibits atherosclerosis in apolipoprotein E-deficient mice, Proc. Natl. Acad. Sci. U. S. A. 95 (1998) 14367–14372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [189].Babaei S, Picard P, Ravandi A, et al. , Blockade of endothelin receptors markedly reduces atherosclerosis in LDL receptor deficient mice: role of endothelin in macrophage foam cell formation, Cardiovasc. Res. 48 (2000) 158–167. [DOI] [PubMed] [Google Scholar]
- [190].Fukuda D, Sata M, Role of bone marrow renin-angiotensin system in the pathogenesis of atherosclerosis, Pharmacol. Ther. 118 (2008) 268–276. [DOI] [PubMed] [Google Scholar]
- [191].Tirapelli CR, Bonaventura D, Tirapelli LF, et al. , Mechanisms underlying the vascular actions of endothelin 1, angiotensin II and bradykinin in the rat carotid, Pharmacology 84 (2009) 111–126. [DOI] [PubMed] [Google Scholar]
- [192].Lemarie CA, Schiffrin EL, The angiotensin II type 2 receptor in cardiovascular disease, J. Ren. Angiotensin Aldosterone System JRAAS 11 (2010) 19–31. [DOI] [PubMed] [Google Scholar]
- [193].Graninger M, Reiter R, Drucker C, et al. , Angiotensin receptor blockade decreases markers of vascular inflammation, J. Cardiovasc. Pharmacol. 44 (2004) 335–339. [DOI] [PubMed] [Google Scholar]
- [194].Montecucco F, Pende A, Mach F, The renin-angiotensin system modulates inflammatory processes in atherosclerosis: evidence from basic research and clinical studies, Mediat. Inflamm. 2009 (2009) 752406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [195].Jackson SP, Arterial thrombosiseinsidious, unpredictable and deadly, Nat. Med. 17 (2011) 1423–1436. [DOI] [PubMed] [Google Scholar]
- [196].Jin RC, Voetsch B, Loscalzo J, Endogenous mechanisms of inhibition of platelet function, Microcirculation 12 (2005) 247–258. [DOI] [PubMed] [Google Scholar]
- [197].Tanaka KA, Key NS, Levy JH, Blood coagulation: hemostasis and thrombin regulation, Anesth. Analg. 108 (2009) 1433–1446. [DOI] [PubMed] [Google Scholar]
- [198].Giesen PL, Fyfe BS, Fallon JT, et al. , Intimal tissue factor activity is released from the arterial wall after injury, Thromb. Haemost. 83 (2000) 622–628. [PubMed] [Google Scholar]
- [199].Mackman N, The many faces of tissue factor, J. Thromb. Haemost. JTH 7 (Suppl. 1) (2009) 136–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [200].Murata T, Nakashima Y, Yasunaga C, et al. , Extracellular and cell-associated localizations of plasminogen activators and plasminogen activator inhibitor-1 in cultured endothelium, Exp. Mol. Pathol. 55 (1991) 105–118. [DOI] [PubMed] [Google Scholar]
- [201].Schafer A, Bauersachs J, Endothelial dysfunction, impaired endogenous platelet inhibition and platelet activation in diabetes and atherosclerosis, Curr. Vasc. Pharmacol. 6 (2008) 52–60. [DOI] [PubMed] [Google Scholar]
- [202].Ruggeri ZM, Platelets in atherothrombosis, Nat. Med. 8 (2002) 1227–1234. [DOI] [PubMed] [Google Scholar]
- [203].Fujiyama S, Amano K, Uehira K, et al. , Bone marrow monocyte lineage cells adhere on injured endothelium in a monocyte chemoattractant protein-1-dependent manner and accelerate reendothelialization as endothelial progenitor cells, Circ. Res. 93 (2003) 980–989. [DOI] [PubMed] [Google Scholar]
- [204].Werner N, Priller J, Laufs U, et al. , Bone marrow-derived progenitor cells modulate vascular reendothelialization and neointimal formation: effect of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibition, Arterioscler. Thromb. Vasc. Biol. 22 (2002) 1567–1572. [DOI] [PubMed] [Google Scholar]
- [205].Asahara T, Murohara T, Sullivan A, et al. , Isolation of putative progenitor endothelial cells for angiogenesis, Science 275 (1997) 964–967. [DOI] [PubMed] [Google Scholar]
- [206].Williams PA, Silva EA, The role of synthetic extracellular matrices in endothelial progenitor cell homing for treatment of vascular disease, Ann. Biomed. Eng. 43 (10) (2015) 2301–2313. [DOI] [PubMed] [Google Scholar]
- [207].Hou L, Kim JJ, Woo YJ, et al. , Stem cell-based therapies to promote angiogenesis in ischemic cardiovascular disease, Am. J. Physiol. Heart Circ. Physiol. 310 (4) (2015. 15) H455–H465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [208].Madonna R, De Caterina R, Circulating endothelial progenitor cells: do they live up to their name? Vasc. Pharmacol. 67–69 (2015) 2–5. [DOI] [PubMed] [Google Scholar]
- [209].Hagensen MK, Shim J, Thim T, et al. , Circulating endothelial progenitor cells do not contribute to plaque endothelium in murine atherosclerosis, Circulation 121 (2010) 898–905. [DOI] [PubMed] [Google Scholar]
- [210].Ceradini DJ, Kulkarni AR, Callaghan MJ, et al. , Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1, Nat. Med. 10 (2004) 858–864. [DOI] [PubMed] [Google Scholar]
- [211].Liu P, Zhou B, Gu D, et al. , Endothelial progenitor cell therapy in atherosclerosis: a double-edged sword? Ageing Res. Rev. 8 (2009) 83–93. [DOI] [PubMed] [Google Scholar]
- [212].Williamson K, Stringer SE, Alexander MY, Endothelial progenitor cells enter the aging arena, Front. Physiol. 3 (2012) 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [213].Devaraj S, Jialal I, Dysfunctional endothelial progenitor cells in metabolic syndrome, Exp. Diabet. Res. 2012 (2012) 585018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [214].Fadini GP, Agostini C, Avogaro A, Autologous stem cell therapy for peripheral arterial disease meta-analysis and systematic review of the literature, Atherosclerosis 209 (2010) 10–17. [DOI] [PubMed] [Google Scholar]
- [215].Tang Z, Wang A, Yuan F, et al. , Differentiation of multipotent vascular stem cells contributes to vascular diseases, Nat. Commun. 3 (2012) 875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [216].Lao KH, Zeng L, Xu Q, Endothelial and smooth muscle cell transformation in atherosclerosis, Curr. Opin. Lipidol. 26 (5) (2015) 449–456. [DOI] [PubMed] [Google Scholar]
- [217].Londin E, Loher P, Telonis AG, et al. , Analysis of 13 cell types reveals evidence for the expression of numerous novel primate- and tissue-specific microRNAs, Proc. Natl. Acad. Sci. U. S. A. 112 (2015) E1106–E1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [218].Santovito D, Egea V, Weber C, Small but smart: MicroRNAs orchestrate atherosclerosis development and progression, Biochim. Biophys. Acta (2015). S1388–1981(15)00235–8. [DOI] [PubMed] [Google Scholar]
- [219].Schober A, Nazari-Jahantigh M, Weber C, MicroRNA-mediated mechanisms of the cellular stress response in atherosclerosis, Nat. Rev. Cardiol. 12 (2015) 361–374. [DOI] [PubMed] [Google Scholar]
- [220].Di Gregoli K, Jenkins N, Salter R, et al. , MicroRNA-24 regulates macrophage behavior and retards atherosclerosis, Arterioscler. Thromb. Vasc. Biol. 34 (2014) 1990–2000. [DOI] [PubMed] [Google Scholar]
- [221].Schober A, Nazari-Jahantigh M, Wei Y, et al. , MicroRNA-126-5p promotes endothelial proliferation and limits atherosclerosis by suppressing Dlk1, Nat. Med. 20 (2014) 368–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [222].Harris TA, Yamakuchi M, Ferlito M, et al. , MicroRNA-126 regulates endothelial expression of vascular cell adhesion molecule 1, Proc. Natl. Acad. Sci. U. S. A. 105 (2008) 1516–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [223].Lovren F, Pan Y, Quan A, et al. , MicroRNA-145 targeted therapy reduces atherosclerosis, Circulation 126 (2012) S81–S90. [DOI] [PubMed] [Google Scholar]
- [224].Du F, Yu F, Wang Y, et al. , MicroRNA-155 deficiency results in decreased macrophage inflammation and attenuated atherogenesis in apolipoprotein E-deficient mice, Arterioscler. Thromb. Vasc. Biol. 34 (2014) 759–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [225].Meiler S, Baumer Y, Toulmin E, et al. , MicroRNA 302a is a novel modulator of cholesterol homeostasis and atherosclerosis, Arterioscler. Thromb. Vasc. Biol. 35 (2015) 323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [226].Creemers EE, Tijsen AJ, Pinto YM, Circulating microRNAs: novel biomarkers and extracellular communicators in cardiovascular disease? Circ. Res. 110 (2012) 483–495. [DOI] [PubMed] [Google Scholar]
- [227].Kumar S, Kim CW, Simmons RD, et al. , Role of flow-sensitive microRNAs in endothelial dysfunction and atherosclerosis: mechanosensitive athero-miRs, Arterioscler. Thromb. Vasc. Biol. 34 (2014) 2206–2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [228].Welch-Reardon KM, Wu N, Hughes CC, A role for partial endothelialmesenchymal transitions in angiogenesis? Arterioscler. Thromb. Vasc. Biol. 35 (2015) 303–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [229].van Meeteren LA, ten Dijke P, Regulation of endothelial cell plasticity by TGF-beta, Cell Tissue Res. 347 (2012) 177–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [230].Cooley BC, Nevado J, Mellad J, et al. , TGF-beta signaling mediates endothelial-to-mesenchymal transition (EndMT) during vein graft remodeling, Sci. Transl. Med. 6 (2014) 227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [231].Li Z, Wermuth PJ, Benn BS, et al. , Caveolin-1 deficiency induces spontaneous endothelial-to-mesenchymal transition in murine pulmonary endothelial cells in vitro, Am. J. Pathol. 182 (2013) 325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [232].Chen PY, Qin L, Baeyens N, et al. , Endothelial-to-mesenchymal transition drives atherosclerosis progression, J. Clin. Investig. 2015 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [233].Moonen JR, Lee ES, Schmidt M, et al. , Endothelial-to-mesenchymal transition contributes to fibro-proliferative vascular disease and is modulated by fluid shear stress, Cardiovasc. Res. 108 (2015) 377–386. [DOI] [PubMed] [Google Scholar]