Abstract
Background and Purpose:
Mindfulness-based interventions (MBI) for substance use disorders (SUD) have shown promising results. However, acceptability of MBIs in the context of SUD treatment has yet to be systematically assessed across published studies. Our aims were to (a) review the literature for assessments of acceptability; (b) summarize how, when, and for whom acceptability is being measured; and (c) create suggestions for best practices in measuring acceptability of MBIs for SUD.
Methods:
Five databases were searched with key terms related to mindfulness, relapse prevention, and SUD.
Results:
Results highlight that studies of MBIs for SUD treatment lack acceptability assessment, a consistent definition of acceptability, and standardized measurements of acceptability.
Conclusion:
The lack of measurement and conceptual consistency make it difficult to conclude acceptability of MBIs for SUD treatment. It is imperative that more efforts be directed toward measurement of intervention acceptability to assess whether such interventions could be taken to scale.
Keywords: Acceptability Framework, Measurement, Mindfulness-Based Interventions, Mindfulness-Based Relapse Prevention, Substance Use Disorder, Treatment Acceptability
1. Introduction
Substance use disorder (SUD) is a significant public health problem affecting more than 20 million Americans [1]. The consequences and costs of SUD are far reaching for individuals, families, communities, and health care systems [2]. The economic impact of SUD is estimated to be more than $400 billion annually in costs related to health care, crime, and loss of work productivity [3]. Although efficacious treatments for SUD exist, many individuals who enter treatment drop out prematurely, contributing to high rates of relapse [4,5]. Accordingly, treatment and relapse prevention are long-standing and growing priorities in the field of SUD research.
In the last 10 years, interest has increased in the potential utility of mindfulness-based interventions (MBIs) as an approach to reduce relapse among individuals in SUD treatment [6]. As part of a third wave of empirically tested behavioral therapies, MBIs were preceded by behavioral therapy and cognitive behavioral therapy [7]. In contrast to the first two waves of these therapies, which focused on modification of cognitive, emotional, and behavioral processes, MBIs focus on “cultivating a non-judgmental awareness of the experience and awareness of the experience of consciousness that encompasses those same cognitive, emotional, and behavioral self-regulation processes” [8]. MBIs are designed to help modulate the stress response through increased awareness and nonjudgmental attention. Mindfulness helps individuals increase awareness of their experience in the moment, learning to respond than react to emotions or situations [9]. Recent literature supports the idea that mindfulness increases emotional regulation and self-control by increasing sensitivity to and awareness of affective cues and may be beneficial in SUD relapse prevention [10–13].
Research on the application of MBIs for SUD treatment is primarily based on adaptations of Jon Kabat-Zinn’s mindfulness-based stress reduction (MBSR) intervention [6,14] and Marlatt’s relapse prevention intervention [15]. MBIs adapted for relapse prevention are typically multiweek behavioral interventions [10,13] with session duration and frequency varying depending on the treatment setting and population. The foundation of MBIs for SUD treatment is the utilization of mindfulness as a “cultivatable skill” to help individuals learn to self-regulate both their emotions and behaviors in response to stressors that may otherwise prompt relapse [6].
Another important element of MBIs for SUD treatment is the concept of craving. In their 2013 article, Witkiewitz et al. [16] offered both a conceptual and detailed explanation of craving as the catalyst of relapse. The desire to use substances (alcohol and drugs) can be viewed as “an effort to either hold on to or avoid cognitive, affective or physical experiences” [16]. In the context of MBIs adapted for SUD relapse prevention, craving is understood as the urge or desire to experience the effects of the drug or alcohol—and is one of the greatest predictors of relapse [16,17]. MBIs for SUD are, in part, designed to help participants understand the passing or transient nature of the urge or craving that they experience and offer practices to develop strategies that support the attenuation of craving, impulsivity and compulsivity, negative mood, and stress reactivity [6,16]. Mindfulness-based skills may increase emotional regulation in response to stress and self-control in response to craving [12].
The most common type of MBI for SUD is mindfulness-based relapse prevention, which posits that it is a “novel mindfulness-based aftercare approach, [which] integrates core aspects of relapse prevention with practices adapted from MBSR and [mindfulness-based cognitive therapy] MBCT” [18]. For the purposes of this study, the authors use the abbreviation “MBI for SUD” when discussing any MBI adapted for SUD and the abbreviation MBRP only when referring to the specific program developed by Bowen et al. [16] for individuals in aftercare after completion of SUD treatment.
Although several studies showed promising results of efficacy of MBIs for SUD treatment and relapse prevention [8,11,16,18], a remaining question is whether MBIs for SUD are acceptable to end users—a key factor in broad dissemination and adoption [19,20]. It is important to assess intervention acceptability because successful implementation depends on participant acceptability; even if an intervention is efficacious, there can be issues in implementation and adoption if acceptability is low [21,22]. While there is theoretical support for the associations between acceptability and intervention enrollment, attendance, and long-term adoption of intervention practices [19–22], there remains a lack of empirical support of these associations within MBIs for SUD. This gap in knowledge can be attributed in part to the lack of systematic assessment of acceptability of MBIs for SUD across published studies.
Intervention acceptability is defined as “a multifaceted construct that reflects the extent to which people delivering or receiving a healthcare intervention consider it to be appropriate, based on anticipated or experienced cognitive and emotional responses to the intervention” [23]. From a clinical perspective, treatment acceptability is composed of multiple domains, “including perceived cruelty or unfairness, consistency with one’s beliefs about how treatment should be and whether the treatment is recommendable to others” [24].
Currently in the field of intervention research, terms are often used interchangeably with acceptability, such as fidelity, adherence, and commitment. To clarify these terms: Treatment fidelity refers to a process of monitoring the program implementation with the goal of enhancing the accuracy and consistency [25]. Participant adherence refers to the active involvement of participating in the prescribed intervention [26]. Commitment may be defined as the participants’ intention and willingness to participate in the intervention, which is a factor of acceptability but not a standalone measure [23].
The purpose of this paper is to (a) examine the literature on MBIs for SUD relapse prevention for assessments of acceptability; (b) summarize how, when, and for whom acceptability is being measured; and (c) create suggestions for the best practices of measuring acceptability of MBIs for SUD relapse prevention.
2. Methods
2.1. Data sources and selection
The authors conducted five data searches between June 1, 2018, and June 21, 2018, using the social science databases PsycINFO, PubMed, ERIC, CINHAL, and Academic Search Premiere. The database searches involved the following key terms: “mindfulness-based relapse prevention” and “substance” or “alcohol” or “drug.” The search term “substance” was added to reduce the amount of literature related to depression relapse prevention that was present without this search term. The inclusion criteria were scholarly journal articles published in English and involving adult-only populations during the past decade (2008–2018); 65 articles were identified from this search. After reviewing the abstracts, 36 articles were removed for lack of relevance, leaving 29 articles for full review. Lack of relevance includes articles focused on testing a measure not related to acceptability (psychometric studies), editorials, and studies not using an MBI for SUD. Following a full review of the articles, 11 additional papers were removed. Seventeen articles were included in the data extraction for the present study. The PRISMA flow diagram [27] was used to illustrate the detailed database search and article selection procedures (Figure 1).
Figure 1:
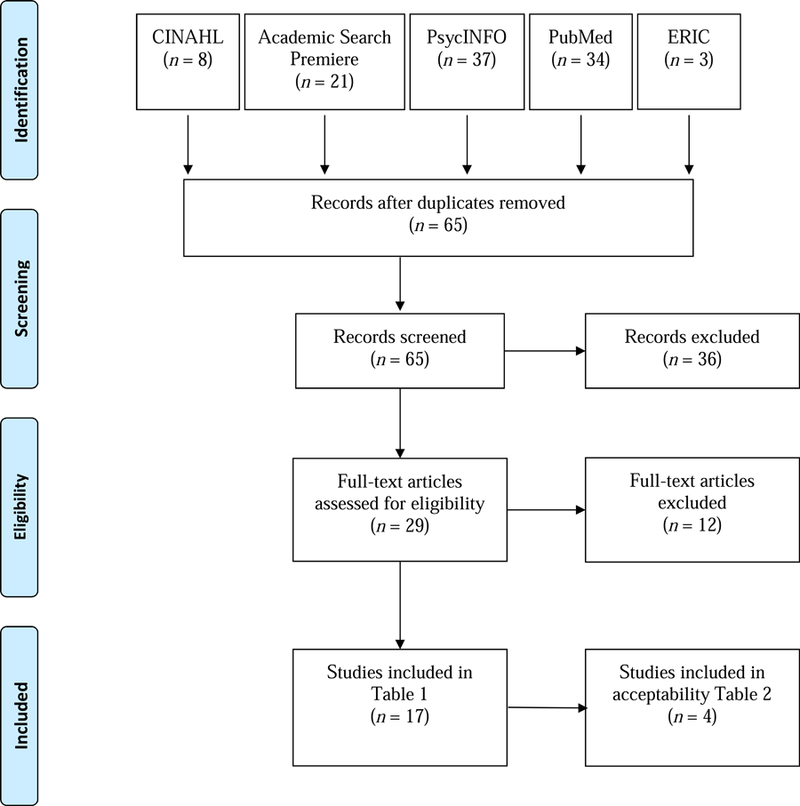
PRISMA Diagram
2.2. Data extraction
The first and second authors used identical procedures to extract data and then convened to consolidate notes regarding difficult cases. The following information was extracted from the 17 articles that met the inclusion criteria: (a) primary and secondary outcomes of the study, (b) study design, (c) sample, and (d) whether acceptability was measured. This information is displayed in Table 1. Of the 17 studies in Table 1, only four studies measured acceptability. These four studies were used to create Table 2, for which the following acceptability-related information was extracted: (a) acceptability measures utilized, (b) timing of acceptability measurement, (c) sample characteristics, (d) use of acceptability in the outcome analysis, and (e) findings related to acceptability.
Table 1:
Included studies of MBIs for SUD
| Citation | Primary and Secondary Outcomes | Design | Sample | Acceptability Measured |
|---|---|---|---|---|
| Amaro et al. [8] | Feasibility, acceptability, substance use, perceived stress, and trauma symptomology | MBRP-W nine-session (1.5–2 h per session weekly), 1–2 trained facilitators per groups of 8 to 15 women, adjunct to SUD treatment; Class 7 is a 4-h silent retreat; meditation techniques, yoga, self-regulation strategies | N = 318; 45.3% Hispanic, 34.6% non-Hispanic Black, 20.1% non-Hispanic White and other; Mage = 33.9 | Yes |
| Bowen & Kurz [31] | Changes in levels of mindfulness following MBRP | Weekly 2-h sessions with 6–10 participants | N = 93; 63% Caucasian; Mage = 40.84; 36% female; adults attending SUD inpatient treatment | No |
| Bowen et al. [18] | Feasibility and initial efficacy substance use outcomes, craving, mindfulness, and acceptance | MBRP intervention with weekly 2-h sessions with 6– 10 participants; TAU: 1–2 times weekly for 1.5 h | N = 168; Mage = 40.5; 36.3% female; adults attending SUD inpatient treatment | Yes |
| Bowen et al. [28] | Satisfaction, depression, anxiety, craving, symptoms of posttraumatic stress, and experiential avoidance | Adapted MBRP curriculum, 1x week for 6 weeks, 2 h per session; mixed-methods study (focus groups and questionnaires, surveys) | N = 15; adults from methadone clinic; Mage= 43.8; 67% female; 93% Caucasian | Yes |
| Bowen et al. [15] | Substance use relapse | MBRP and CBRP matched for dosage (8 weekly 2 h sessions), size (6–10 participants), location, and scope of homework; TAU not matched (1–2 weekly for 1.5 h); MBRP: formal MBSR, MBCT practices with integration of evidence-based practices to decrease relapse for people with SUD | N = 286; Mage = 39 for MBRP and RP, 37 for TAU; 26% 36%, and 27% female adults attending inpatient care for SUD, respectively | No |
| Enkema & Bowen [32] | Relationship between craving and substance use, moderated by practice | MBRP (8 weekly 2 h sessions, 6–10 participants), location, and scope of homework (1–2 weekly for 1.5 h) | N = 57; Mage = 38; 77.2% male; 63.16% White | No |
| Glasner et al. [11] | Stimulant use, negative affect, psychiatric severity | MBRP (n = 31) or HE (n = 32) concurrent with CM following a 4-week CM-only phase | N = 63; Mage = 45.3; 71.4% male | No |
| Glasner-Edwards et al. [33] | Stimulant use, depression, anxiety, psychiatric severity | Pilot RCT, 12-week contingency management intervention; at Week 4: randomized to MBRP or HE, measurements during intervention and 1-month posttreatment | N = 63 (MBRP = 31, HE = 32); Mage = 45.3; 71.4% male; 44.4% African American; all participants stimulant dependent | No |
| Greenfrield et al. [39] | Days of drug use and heavy drinking | MBRP (8 weekly 2 h sessions, 6–10 participants), location, and scope of homework (1–2 weekly for 1.5 h) | N = 191; Mage = 39.04; 71% male; 22 therapy groups | No |
| Grow et al. [40] | Development of mindfulness meditation home practice during and after MBRP in relation to drug use and craving | Secondary analysis from larger MBRP RCT (8 weekly 2 h sessions, 6–10 participants); TAU: 1–2 weekly for 1.5 h | N = 93; Mage = 40.84; 64.5% male; 63.4% White | No |
| Lee et al. [41] | Effectiveness of MBRP psychosocial outcomes drug use, drug avoidance, depression | RCT with 2 (baseline vs postsession) × 2 (MBRP vs. TAU) mixed design; TAU: substance use education; 10-wk MBRP, weekly meetings 1.5 h | N = 24; all male; Mage = 40.70; MBRP (n = 10); TAU (n = 14); all Taiwanese | No |
| Roos et al. [13] | Baseline SUD symptom severity patterns, depression, anxiety as moderated by MBRP, or comparison group | Latent class moderation using data from Bowen’s RCTs [15,18] | 2014: MBRP vs. TAU (N = 286; 71.8% male; Mage = 38.44); 2009: MBRP vs. TAU (N = 168; 63.7% female; Mage = 40.45) | No |
| Witkiewitz & Bowen [34] | Depressive symptoms, craving at 2-months posttest, and days of substance use | MBRP (8 weekly 2 h sessions, 6–10 participants); TAU: 1–2 weekly for 1.5 h; MBRP (adapted from MBSR) has themes of meditation practices and related RP discussions and exercises | N = 168; Mage = 40.5; 36.3% female adults attending SUD inpatient treatment | No |
| Witkiewitz et al. [16] | Mechanisms associated with MBRP that may reduce craving | MBRP RCT; Bowen [18] | N = 168; 63.7% male; Mage = 40.5; 51.8% Caucasian | No |
| Witkiewitz et al. [29] | Drug use and addiction severity | RCT of MBRP and RP for SUD; 50-minute sessions 2x weekly for 8 weeks | N = 70; all adult women in residential treatment for criminal offenders | Yes |
| Witkiewitz et al. [30] | Primary: days of substance use and substance use outcomes; secondary: family and social problems, medical problems, legal problems, psychiatric symptoms | RCT of MBRP and RP for SUD; 50-minute sessions 2x weekly for 8 weeks | N = 105; adult female population in residential treatment for criminal offenders | No |
| Zemestani & Ottaviani [42] | Cravings, depressive symptoms, anxious symptoms | MBRP and TAU matched for dose; 8 weekly, 2 h sessions | N = 74; Mage = 30.1; 79.7% male; Iranian | No |
CBRP = cognitive-based relapse prevention; HE = health education; Mage = mean age; MBIs = mindfulness-based intervention; MBRP = mindfulness-based relapse prevention; MBRP-W = mindfulness-based relapse prevention for women; N = number of participants; RCT = randomized controlled trial; RP = relapse prevention; SD = standard deviation; SUD = substance use disorder; TAU = treatment as usual.
Table 2:
MBIs for SUD studies that assessed acceptability
| Citation | Evaluation Instrument | Time of Acceptability Measurement | Sample | Acceptability Findings |
|---|---|---|---|---|
| Amaro et al. [8] | Participation (attendance) and satisfaction questionnaire | Participation: each session; satisfaction: last session | N = 318; Mage = 33.9; all female; 45.3% Hispanic, 34.6% non-Hispanic Black, 20.1% non-Hispanic White and other | 19.8% attended 1–4 sessions, 35.8% attended 5–9 sessions, 44.3% did not attend any groups; participant satisfaction was high (M = 3.4, SD = 0.3), but completion was modest (36%) |
| Bowen et al. [18] | Practice | Weekly and 4 months postintervention | N = 168; Mage = 40.5; 36.3% female adults; 51.8% Caucasian, 28.6% African American, 15.3% multiracial, 7.7% Native American | Practice reported by 86% at postintervention and 54% at 4-month follow-up; practice at 4-month follow-up: M = 4.7 days, M = 29.9 minutes per session |
| Bowen et al. [28] | Satisfaction | Immediately following last session | N = 15; adults from methadone clinic; Mage = 43.8; 67% female; 93% Caucasian | High perceived importance of course (M = 8.7, SD = 1.11); high stated likelihood of continuing formal (M = 9.0, SD = 1.2) and informal (M = 9.4, SD = 0.8) mindfulness practice; deemed feasible and acceptable, but acknowledged low attendance and retention rates |
| Witkiewitz et al. [29] | 15-week follow-up rates | 15-weeks postintervention | N = 70; adult females in residential treatment for criminal offenders; 63.8% non-Hispanic White, 17.4% African American, 13% Native American, 4.3% Asian, 1.4% Hispanic | Significantly better follow-up rates in racial and ethnic minority versus non-Hispanic White participants assigned to MBRP (85.7% vs. 52.6%); suggested MBRP may be more acceptable to minority clients |
M = Mean; Mage = mean age; MBIs = mindfulness-based intervention; MBRP = mindfulness-based relapse prevention; N = number of participants; SD = standard deviation; SUD =substance use disorder.
3. Results
3.1. Results of data synthesis
3.1.1. Measurements used to assess acceptability
The measures that authors claimed to assess acceptability were (a) satisfaction, assessed by 50% of the studies [8,28]; (b) follow-up rates of the outcome evaluation, assessed by 25% of the studies [29]; (c) evidence of utilization of intervention practices, assessed by 25% of the studies [18]; and (d) intervention session attendance, assessed by 25% of the studies [8]. Only one study [8] used attendance and satisfaction as two independent measures of acceptability. None of the studies reported the reliability or validity of the acceptability assessment tools, leaving the details of measurement unclear.
3.1.2. Timing of acceptability assessment
The most common time for measuring acceptability was during postintervention follow-up: at the end of the final intervention session [8,28], 15-week follow-up [29], and 4-month follow-up [18]. Two studies also measured acceptability weekly during the intervention [8,18].
3.1.3. Samples
Of the four studies that assessed acceptability, sample sizes ranged from 15 to 318 participants. Two studies involved only women [8,29,30]; of the two mixed-gender studies, one had a 36.3% female sample [18] and the other had a 67% female sample [28]. Only one study [29] compared racial and ethnic groups based on the measure of acceptability, indicating that follow-up rates of the outcome evaluation were higher among racial and ethnic minorities than among non-Hispanic White participants.
3.1.4. Acceptability findings
All four studies that measured acceptability concluded that the intervention was acceptable based on the various assessment used. Amaro et al. [8] reported high satisfaction and modest attendance and completion. Bowen et al. [18] indicated that 86% of the sample reported practicing at postintervention and 54% at the 4-month follow-up assessment. Frequency of use of mindfulness practices at follow-up averaged 4.7 days per week and approximately 30 minutes per practice session [18]. Bowen et al. [28] reported high satisfaction across multiple items, including perceived importance and likelihood of continuing formal and informal practice.
3.1.5. Comparable measures not used to assess acceptability
Six studies excluded from Table 2 [11,30–34] (due to not specifying acceptability assessment) were identified as using measures of practice, retention, attendance, and follow-rates as a measure of a construct other than acceptability. This is important to mention because the use of the same variables for different constructs creates confusion in defining the variables. For example, practice may be used as a measure of feasibility in Study A, then as a measure of acceptability in Study B. It is not meaningful to conclude that one approach is acceptable based on high practice, then utilize the same measure to assess feasibility in another study. What constitutes feasibility needs to be clearly defined and differentiated from acceptability.
4. Discussion
The overall lack of attention to the measurement and assessment of acceptability and inconsistent types of measures of acceptability in published articles on MBIs for treatment of SUD is concerning. A deficiency in the use of a standard definition may, in part, explain the heterogeneity of acceptability measurements that were reported. Given the significance of SUD and the high rate of relapse, directing efforts to measure program acceptability is warranted. Utilization of a standardized definition and shared conceptual framework may help researchers develop strong measurements that accurately depict and report intervention acceptability.
The lack of acceptability assessment is not exclusive to MBIs for SUD. Zimmermann, Burrell, and Jordan [35] reviewed eight MBI studies (including MBCT, MBSR, and acceptance and commitment therapy) aimed at improving psychological well-being for adults with advanced cancer. Of the eight included studies, five studies reported acceptability (two studies used a rating of intervention helpfulness as a measure of acceptability, one used qualitative data, and two did not discuss the method used for acceptability measurement) and three studies did not report acceptability.
Although assessment of treatment acceptability related to MBIs for SUD remains underdeveloped, related fields have created and implemented effective means of measurement. The work of Milosevic et al. [24] sought to evolve the field of anxiety research by establishing a valid and reliable measurement of acceptability as it relates to participant experience. The Treatment Acceptability/Adherence Scale (TAAS), a self-report questionnaire, was developed in 2015 to measure the psychometric properties associated with acceptability of and adherence to related interventions or treatments in the context of anxiety disorders. The TAAS was found to be reliable (Cronbach’s α ranging from 0.79 to 0.88, depending on the condition). Convergent and divergent validity were confirmed by significant correlations with the following measures: Endorsement and Discomfort Scale (r = 0.79, p < 0.01); Credibility/Expectancy Questionnaire, Credibility Subscale (r = 0.76, p < 0.01); Credibility/Expectancy Questionnaire, Expectancy Subscale (r = 0.66, p < 0.01); and State Anger Expression Inventory-2, State Anger Subscale (r = −0.55, p < 0.01). A similar model with rigorous testing could help establish a method to assess acceptability of MBIs for SUD treatment.
Sekhon et al. [23] reviewed 43 systematic reviews of health care interventions, none of which mentioned an acceptability theory or model. This led to the development of the theoretical framework of acceptability (TFA), which is “represented by seven component constructs: affective attitude, burden, perceived effectiveness, intervention coherence, opportunity costs, and self-efficacy” [23].
The TFA provides a good model for the measurement of acceptability as applicable to each intervention stage. It may not be necessary to assess all seven acceptability constructs in every study. For example, if an intervention is in the pilot phase, the researchers may be interested in the anticipated perceived burden among participants and facilitators, which may inform adaptations to improve fit of the intervention prior to delivery. Alternatively, during a randomized controlled trial phase, the researchers may be more interested in the participants’ experiences of self-efficacy and perceived effectiveness following exposure to the intervention.
Balance is needed between developing a consistent measure of acceptability that can be applied across studies and limiting acceptability to a single measurement. Of the MBIs for SUD studies reviewed in this paper, self-report acceptability from the participant or patient perspective was the most common. However, Sekhon et al. [23] discussed valuable information to be gained by assessing acceptability from the facilitators’ perspectives as well. For example, if an intervention has low facilitator acceptability, the facilitator may be altering the intervention, which could lead to low fidelity and potentially lower efficacy.
After reviewing the acceptability measurements used in the MBI for SUD studies included in this paper, we suggest that the term acceptability only be used when multiple constructs are used together. Otherwise, we suggest simply referring the individual construct being measured. For example, if a researcher is measuring satisfaction, adherence, and practice, those combined measures could be used to infer acceptability. If the study is only measuring satisfaction, then the researcher should only infer satisfaction, not acceptability.
Inconsistent terminology has also been noted as an issue during intervention implementation [21]. Proctor et al. [21] presented conceptual distinctions among eight implementation outcomes, including acceptability and appropriateness, which are commonly used interchangeably. According to Proctor et al. [21], these two concepts have overlapping features but “acceptability is the perception among implementation stakeholders that a given treatment, service, practice, or innovation, is agreeable, palatable, or satisfactory.” And “appropriateness is the perceived fit, relevance, or compatibility of the innovation or evidence-based practice for a given practice setting, provider, or consumer; and/or the problem.”
Based on the frameworks of Proctor et al. [21] and Sekhon et al. [23] and the intervention specifics related to MBIs for SUD treatment, we encourage the construction of acceptability scales for each intervention stage: development (Stage 1), efficacy (Stages II and III), effectiveness (Stage IV), and implementation (Stage V). The acceptability scales for Stage I should focus on anticipated ethicality (how mindfulness may complement or clash with one’s own value system) and affective attitude (feelings associated with initial impression of the MBI) prior to participating in or facilitating the intervention. The acceptability scales for Stages II and III should focus on anticipated burden (effort or time needed for the MBI) and opportunity costs (perceived value of mindfulness). The acceptability scales for Stage IV may want to consider including aspects previously mentioned (if they were not assessed in the previous stage) and assess multiple aspects over time during the intervention, acknowledging that acceptability may change with exposure to the intervention. The acceptability scales for Stage V should assess the self-efficacy of the participants or facilitators (how confident are they that they can perform the task) and the perceived effectiveness (the extent to which they believe the MBI will help in their SUD recovery and relapse prevention). Across fields, it is imperative to procure validated instruments that accurately measure treatment acceptability and reflect participants’ experiences.
4.1. Limitations of the present review
The present study was limited to empirical studies indexed in the following databases: PsycINFO, PubMed, ERIC, CINHAL, and Academic Search Premiere. The reviewed articles were restricted to English language only with adult populations. Varied measurements among the studies may not adequately capture the multiple dimensions of the latent construct of acceptability.
To the authors’ knowledge, currently there are no standardized means to assess acceptability of MBIs for SUD treatment, nor is there a way to combine multiple measurements of acceptability into a composite score. This is a promising future avenue of work for researchers in the field of MBIs for SUD.
The National Institutes of Health stage model brings attention to the importance of Stage I (intervention generation and refinement) and mentions that the stages are not linear. Intervention generations and refinement (including acceptability) should also be assessed during and after later stages, such as Stage V (implementation) to ensure acceptability in multiple settings and populations [36]. With MBIs for SUD studies still in their infancy and gaining promising evidence of efficacy, now is an opportune time for assessment of acceptability.
4.2. Future research
Future research should be conducted to advance the field of SUD relapse prevention by systematically measuring acceptability. There is a need to clearly define and differentiate the terms acceptability and feasibility to create measures that adequately capture the importance of each term and their possible influence on intervention efficacy. Assessing if and how acceptability differs by sample characteristics, such as race and ethnicity, treatment stage, and clinical profile (e.g., problem severity, comorbidity), could provide valuable insights to improve intervention retention and completion for disadvantaged individuals struggling with SUD. Further, identifying culturally specific characteristics associated with acceptability could inform appropriate adaptations of existing MBIs for SUD, potentially resulting in increased acceptability, retention, and long-term recovery. Barrera and Castro [37] discussed the importance of adapting an intervention not only to the problem (such as substance use), but also to the culture of the participants. Participant engagement (a factor of acceptability) is related to the social validity of an intervention, and generalizability of an intervention may not be possible if it is not applicable to a subcultural group [38].
4.3. Conclusion
The current review highlighted the dearth of research examining the acceptability of MBIs for SUD. Additional research is needed to develop a rigorous measurement of MBIs for SUD acceptability. There is a need to provide consistent definitions and precise language when inferring acceptability from the results of studies on MBIs for SUD. Our purpose is to bring attention to the inconsistency of acceptability measurement and provide suggestions for future assessment.
Highlights.
The most common time for measuring acceptability was during postintervention follow-up.
The overall lack of attention to the measurement and assessment of acceptability and inconsistent types of measures of acceptability in published articles on MBIs for treatment of SUD is concerning.
With MBIs for SUD studies still in their infancy and gaining promising evidence of efficacy, now is an opportune time for assessment of acceptability.
There is a need to provide consistent definitions and precise language when inferring acceptability from the results of studies on MBIs for SUD.
Acknowledgements
Special thanks to Dr. Ann Sebren for constructive comments on the manuscript conceptualization and to ASU’s Center for Mindfulness, Compassion and Resilience for their support.
Funding
This research was supported in part by NIDA and NIAAA 5R01DA038648-03 (H.A. and D.B., PI) and NIDA 5R25DA026401-08 (A.V., PI).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors have no conflict of interests to report.
References
- 1.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality, Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings, U.S. Department of Health and Human Services, Rockville, 2011. [Google Scholar]
- 2.Russell KC, Gillis HLL, Heppner W, An examination of mindfulness-based experiences through adventure in substance use disorder treatment for young adult males: a pilot study, Mindfulness 7 (2) (2015) 320–328. doi: 10.1007/s12671-015-0441-4. [DOI] [Google Scholar]
- 3.Office of National Drug Control Policy, The Economic Costs of Drug Abuse in the United States, Executive Office of the President, Office of National Drug Control Policy, Washington, DC, 2004,http://www.ncjrs.gov/ondcppubs/publications/pdf/economic_costs.pdf (accessed 15 May 2018). [Google Scholar]
- 4.McLellan AT, Lewis DC, O’Brien CP, Kleber HD, Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation, J. Am. Med. Assoc 284 (13) (2000) 1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 5.McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J, Reconsidering the evaluation of addiction treatment: from retrospective follow-up to concurrent recovery monitoring, Addiction, 100 (4) (2005) 447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- 6.Black DS, Mindfulness-based interventions: an antidote to suffering in the context of substance use, misuse, and addiction, Subst. Use Misuse 49 (5) (2014) 487–491. doi: 10.3109/10826084.2014.860749. [DOI] [PubMed] [Google Scholar]
- 7.Crane RS, Brewer J, Feldman C, et al. , What defines mindfulness-based programs? The warp and the weft, Psychol. Med 47 (6) (2017) 990–999. doi: 10.1017/S0033291716003317. [DOI] [PubMed] [Google Scholar]
- 8.Amaro H, Spear S, Vallejo Z, Conron K, Black DS, Feasibility, acceptability, and preliminary outcomes of a mindfulness-based relapse prevention intervention for culturally-diverse, low-income women in substance use disorder treatment, Subst. Use Misuse 49 (5) (2014) 547–559. doi: 10.3109/10826084.2013.852587. [DOI] [PubMed] [Google Scholar]
- 9.Kabat-Zinn J, Mindfulness-based interventions in context: past, present, and future, Clin. Psychol. Sci. Pract 10 (2) (2003) 144–156. doi: 10.1093/clipsy.bpg016. [DOI] [Google Scholar]
- 10.Collins SE, Chawla N, Hsu SH, Grow J, Otto JM, Marlatt GA, Language-based measures of mindfulness: initial validity and clinical utility, Psychol. Addict. Behav 23 (4) (2009) 743–749. doi: 10.1037/a0017579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glasner-Edwards S, Mooney LJ, Ang A, et al. , Mindfulness based relapse prevention for stimulant dependent adults: a pilot randomized clinical trial, Mindfulness 8 (1) (2017) 126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang YY, Tang R, Posner MI, Mindfulness meditation improves emotion regulation and reduces drug abuse, Drug Alcohol Depend 163 (Suppl. 1) (2016) S13–S18. doi: 10.1016/j.drugalcdep.2015.11.041. [DOI] [PubMed] [Google Scholar]
- 13.Roos CR, Bowen S, Witkiewitz K, Baseline patterns of substance use disorder severity and depression and anxiety symptoms moderate the efficacy of mindfulness-based relapse prevention, J. Consult. Clin. Psychol 85 (11) (2017) 1041–1051. doi: 10.1037/ccp0000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Britton WB, Bootzin RR, Cousins JC, Hasler BP, Peck T, Shapiro SL, The contribution of mindfulness practice to a multicomponent behavioral sleep intervention following substance abuse treatment in adolescents: a treatment-development study, Subst. Abuse 31 (2) (2010) 86–97. doi: 10.1080/08897071003641297. [DOI] [PubMed] [Google Scholar]
- 15.Bowen S, Witkiewitz K, Clifasefi SL, et al. , Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: a randomized clinical trial, JAMA Psychiatry 71 (5) (2014) 547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Witkiewitz K, Bowen S, Douglas H, Hsu SH, Mindfulness-based relapse prevention for substance craving, Addict. Behav 38 (2) (2013) 1563–1571. doi: 10.1016/j.addbeh.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sayette MA, The role of craving in substance use disorders: theoretical and methodological issues, Annu. Rev. Clin. Psychol 12 (2016) 407–433. doi: 10.1146/annurev-clinpsy-021815-093351. [DOI] [PubMed] [Google Scholar]
- 18.Bowen S, Chawla N, Collins SE, et al. , Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial, Subst. Abuse 30 (4) (2009) 295–305. doi: 10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bak M, van Dam A, Janssens R, Awareness and acceptability of pre-exposure prophylaxis (PrEP) among men who have sex with men in Kazakhstan: a mixed methods study, Cent. Asian J. Med. Sci 4 (2) (2018) 102–115. [Google Scholar]
- 20.Diepeveen S, Ling T, Suhrcke M, Roland M, Marteau TM, Public acceptability of government intervention to change health-related behaviours: a systematic review and narrative synthesis, BMC Public Health 13 (2013) 756. doi: 10.1186/1471-2458-13-756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Proctor E, Silmere H, Raghavan R, et al. , Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda, Adm. Policy Ment. Health 38 (2) (2011) 65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stok FM, de Ridder DT, de Vet E, et al. , Hungry for an intervention? Adolescents’ ratings of acceptability of eating-related intervention strategies, BMC Public Health 16 (2016) 5. doi: 10.1186/s12889-015-2665-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sekhon M, Cartwright M, Francis JJ, Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework, BMC Health Serv. Res 17 (1) (2017) 88. doi: 10.1186/s12913-017-2031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Milosevic I, Levy HC, Alcolado GM, Radomsky AS, The treatment acceptability/adherence scale: moving beyond the assessment of treatment effectiveness, Cogn. Behav. Ther 44 (6) (2015) 456–469. doi: 10.1080/16506073.2015.1053407. [DOI] [PubMed] [Google Scholar]
- 25.Bellg AJ, Borrelli B, Resnick B, et al. , Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium, Health Psychol 23 (5) (2004) 443–451. doi: 10.1037/0278-6133.23.5.443. [DOI] [PubMed] [Google Scholar]
- 26.Brawley LR, Culos-Reed SN, Studying adherence to therapeutic regimens: overview, theories, recommendations, Control. Clin. Trials 21 (5, Suppl.) (2000) 156S–163S. [DOI] [PubMed] [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, PLOS Med 6 (7) (2009) e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bowen S, Somohano VC, Rutkie RE, Manuel JA, Rehder KL, Mindfulness-based relapse prevention for methadone maintenance: a feasibility trial, J. Altern. Complement. Med 23 (7) (2017) 541–544. doi: 10.1089/acm.2016.0417. [DOI] [PubMed] [Google Scholar]
- 29.Witkiewitz K, Greenfield BL, Bowen S, Mindfulness-based relapse prevention with racial and ethnic minority women, Addict. Behav 38 (12) (2013) 2821–2824. doi: 10.1016/j.addbeh.2013.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Witkiewitz K, Warner K, Sully B, et al. , Randomized trial comparing mindfulness-based relapse prevention with relapse prevention for women offenders at a residential addiction treatment center, Subst. Use Misuse 49 (5) (2014) 536–546. doi: 10.3109/10826084.2013.856922. [DOI] [PubMed] [Google Scholar]
- 31.Bowen S, Kurz AS, Between-session practice and therapeutic alliance as predictors of mindfulness after mindfulness-based relapse prevention, J. Clin. Psychol 68 (3) (2012) 236–245. doi: 10.1002/jclp.20855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Enkema MC, Bowen S, Mindfulness practice moderates the relationship between craving and substance use in a clinical sample, Drug Alcohol Depend 179 (2017) 1–7. doi: 10.1016/j.drugalcdep.2017.05.036. [DOI] [PubMed] [Google Scholar]
- 33.Glasner-Edwards S, Mooney L, Ang A, et al. , Mindfulness based relapse prevention improves stimulant use among adults with major depression and generalized anxiety disorder, Drug Alcohol Depend 156 (2015) e80. doi: 10.1016/j.drugalcdep.2015.07.1135. [DOI] [Google Scholar]
- 34.Witkiewitz K, Bowen S, Depression, craving, and substance use following a randomized trial of mindfulness-based relapse prevention, J. Consult. Clin. Psychol 78 (3) (2010) 362–374. doi: 10.1037/a0019172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zimmermann FF, Burrell B, Jordan J, The acceptability and potential benefits of mindfulness-based interventions in improving psychological well-being for adults with advanced cancer: a systematic review, Complement. Ther. Clin. Pract 30 (2018) 68–78. doi: 10.1016/j.ctcp.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 36.Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M, Reenvisioning clinical science: unifying the discipline to improve the public health, Clin. Psychol. Sci 2 (1) (2014) 22–34. doi: 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barrera M, Castro FG, A heuristic framework for the cultural adaptation of interventions, Clin. Psychol. Sci. Pract 13 (2006) 311–316. doi: 10.1111/j.1468-2850.2006.00043.x. [DOI] [Google Scholar]
- 38.Lau AS, Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training, Clin. Psychol. Sci. Pract 13 (2006) 295–310. doi: 10.1111/j.1468-2850.2006.00042.x. [DOI] [Google Scholar]
- 39.Greenfield BL, Roos C, Hagler KJ, Stein E, Bowen S, Witkiewitz KA, Race/ethnicity and racial group composition moderate the effectiveness of mindfulness-based relapse prevention for substance use disorder, Addict. Behav 81 (2018) 96–103. doi: 10.1016/j.addbeh.2018.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grow JC, Collins SE, Harrop EN, Marlatt GA, Enactment of home practice following mindfulness-based relapse prevention and its association with substance-use outcomes, Addict. Behav 40 (2015) 16–20. doi: 10.1016/j.addbeh.2014.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee K, Bowen S, An-Fun B, Psychosocial outcomes of mindfulness-based relapse prevention in incarcerated substance abusers in Taiwan: a preliminary study, J. Subst. Use 16 (6) (2011) 476–483. doi: 10.3109/14659891.2010.505999. [DOI] [Google Scholar]
- 42.Zemestani M, Ottaviani C, Effectiveness of mindfulness-based relapse prevention for co-occurring substance use and depression disorders, Mindfulness 7 (6) (2016) 1347–1355. doi: 10.1007/s12671-016-0576-y. [DOI] [Google Scholar]


