Summary
Background
Abortion-related mortality is one of the main causes of maternal mortality worldwide. Laws often restrict the provision of safe abortion care, yet post-abortion care is a service that all countries have committed to provide to manage abortion complications. There is minimal evidence on the capacity of national health systems to provide post-abortion care.
Methods
We did a multicountry analysis of data from nationally representative Service Provision Assessment surveys done between 2007 to 2017 in ten countries across three regions (Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Tanzania, and Uganda). Data were available for all ten countries from 2007 to 2015. We included facilities offering childbirth delivery services and classified facilities as primary or referral level. We measured signal functions for post-abortion care (the availability of key equipment and ability to perform services) to assess the proportion of primary-level and referral-level facilities in each country with the capacity to provide basic and comprehensive post-abortion care, respectively. We calculated the proportion of facilities providing each post-abortion care signal function to examine specific gaps in service provision.
Findings
There are critical gaps in the provision of post-abortion care at all facilities that offer delivery services. In seven (70%) of ten countries, less than 10% of primary-level facilities could provide basic post-abortion care, and in eight (80%) of ten countries less than 40% of referral-level facilities could provide comprehensive post-abortion care. In no country could all referral facilities provide all the essential services that need to be included in basic post-abortion care.
Interpretation
The capacity of primary-level and referral-level health facilities to provide basic and comprehensive post-abortion care, respectively, is low. The results highlight the gap between political commitments to address the consequences of unsafe abortion and the capacity of health systems to provide post-abortion care. Increasing the provision of good-quality post-abortion care is essential to reduce the level of abortion-related morbidity and mortality.
Introduction
Abortion-related complications are an important and preventable cause of maternal deaths, accounting for 8–9% of maternal deaths worldwide between the early 2000s and 2016.1,2 In places where there is little or restricted access to safe abortion care, abortion-related complications can also result in severe morbidity. A review3 of 70 studies from 28 countries estimated that at least 9% of women admitted to hospital for abortion-related reasons had a near-miss event, where a woman had complications, such as severe haemorrhage, that would have most likely resulted in death had she not made it to hospital.
Although the availability of safe methods for terminating pregnancy such as manual vacuum aspiration and access to medical abortion are expanding in many countries, many abortions are still done under unsafe conditions. Recent estimates for 2010–14 showed that 45% of the 56 million induced abortions done worldwide each year are unsafe, with 31% considered less safe (ie, they were done either without using a WHO-recommended method appropriate for the pregnancy duration or by someone who was not appropriately trained) and 14% classified as least safe (ie, involving both inappropriate methods and inappropriately trained providers).4 In several regions of the world, women have a high risk of adverse health outcomes associated with unsafe abortion: eg, in four of the five regions of Africa, an estimated 44% or more of abortions are classified as least safe.4
All countries globally have made long-standing political commitments to address abortion-related morbidity and mortality through the provision of quality health services for the management of complications from abortion.5 The term post-abortion care refers to a group of essential emergency interventions that should be provided to women who present with complications from unsafe or incomplete abortions. Although the risk of complications requiring treatment is low with spontaneous abortions or safely induced abortions, incomplete abortions requiring post-abortion care also arise in a small proportion of these cases.
Post-abortion care consists of both curative care (treating incomplete abortion and its complications) and preventive care (contraceptive counselling and services), and both components are essential to ensure that high-quality care is received by women who require these services. When high-quality post-abortion care is available, the morbidity and mortality associated with unsafe or incomplete abortions can be greatly reduced.6,7 The best clinical approaches to providing post-abortion care include treating complications of early pregnancy loss, task shifting clinical care to mid-level providers, and providing family planning counselling.8 However, evidence on the capacity of national health systems to provide this life-saving service and assess the quality of the care given is scarce.8
The quality of post-abortion care has been assessed by using structural and process indicators that examine the availability of its key components at health facilities.9 One such approach is to measure signal functions for post-abortion care. Signal functions were initially developed by the UN to monitor provision of emergency obstetric care, in this case consisting of eight key medical interventions used to treat the obstetric complications that most commonly lead to maternal death. The signal functions were used to generate aggregate measures that delineate two levels of care: basic emergency obstetric care and comprehensive emergency obstetric care, which roughly correspond to care that should be provided at both the primary level (defined as health centres and likely to be staffed with midwives) and at the first referral hospital level (staffed with doctors), respectively.10 This approach has been adapted for post-abortion care10,11 with relevant signal functions covering treatments for the most common abortion complications leading to mortality (ie, haemorrhage, sepsis, and intra-abdominal injury). Signal functions for post-abortion care have also been successfully applied to assess the status of post-abortion-care services in Ethiopia and Zambia.10,12
A first step towards improving the health-system quality of post-abortion care is to measure it and determine which of its key services are being provided at health facilities and which are absent. The signal functions of post-abortion care succinctly summarise its key preventive and curative components with aggregate indicators of basic and comprehensive capability such that they can be compared across countries and with other maternal health services that have been similarly assessed. We used this signal-functions approach to provide a multicountry assessment of the status of post-abortion care services, and to document gaps in the quality of post-abortion care provision from a health-systems perspective.
Methods
Data sources
We did a multicountry analysis of data from nationally representative Service Provision Assessment (SPA) surveys done between 2007 and 2017 by the Demographic and Health Surveys programme for ten countries across three regions (sub-Saharan Africa, south Asia, and the Caribbean): Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Tanzania, and Uganda (appendix). Data were available for all ten countries from 2007 to 2015. The SPA are cross-sectional surveys of health facilities, staff, and clients, and collect information on the overall availability and delivery of a range of services and commodities in a country. The surveys typically include 400–700 public and non-public health facilities sampled from a comprehensive list of facilities. The core questionnaire reflects generally accepted standards for health-care services, and interviewers verify the existence of items that are assessed; eg, whether the supplies or medicines available were functional or expired at the time of the visit.
We used data from the SPA facility inventory module, which includes questions about abortion-related services if the health facility offers services for deliveries or care of newborn babies.10 Facilities providing delivery services should theoretically be able to provide post-abortion care services based on the overlap between provider training and equipment required for the two sets of services. All health facilities with completed interviews and that reported offering delivery services were included in our analysis. The proportion of facilities capable of providing delivery services ranged widely, from 200 (14%) of 1463 (95% CI 11–16) in Bangladesh in 2014 to 350 (77%) of 455 (72–81) in Senegal in 2015 for primary-level facilities, and from 65 (71%) of 91 (62–79) in Nepal in 2015 to 46 (98%) of 47 (95–99) in Uganda in 2007 for referral- level facilities (appendix).
We classified the facilities in each health-care system as primary or referral level using each country’s SPA survey reports (appendix). One exception was Bangladesh, for which we used the 2015 Bangladesh health system review13 because the necessary information was not available from the SPA report. We also used information from the WHO and UN global abortion policies database14 and documents from each country’s ministry of health to check country-specific policy guidance on post-abortion care (appendix).
Signal functions
For this analysis, we constructed aggregate indicators of the health facilities’ capacity to provide basic and comprehensive post-abortion care using a signal functions approach. By assessing the availability of specific health interventions that are key to post-abortion care—ie, the signal functions—we could measure the capacity for, and quality of, post-abortion care from a health systems perspective.
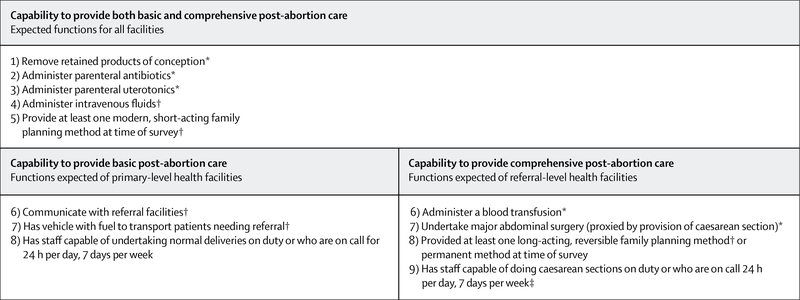
This analysis provided indicators of the availability of basic and comprehensive post-abortion care signal functions, adapted from Campbell and colleagues10 (figure 1). The signal functions approach, along with other approaches that focus on infrastructure and process indicators, do not directly reflect client experiences with health services or their health outcomes.
Figure 1: Signal functions for basic and comprehensive post-abortion care.
*Assessed on the basis of facility reporting if they had ever provided the service. †Assessed on the basis of the availability and validity or functionality of a given item (drug or equipment) at the time of survey. ‡We assumed that staff who were capable of doing caesarean sections were also capable of doing normal deliveries, and therefore did not include this factor in comprehensive capability.
Basic post-abortion care is expected to be available at all facilities that provide delivery care. The capacity to provide basic post-abortion care was measured through eight signal functions: four on specific treatment services, three on staffing and referral, and one on the preventive service of post-abortion contraception (figure 1). Short-acting, modern methods of contraception included hormonal methods (pills and injectables) and non-hormonal methods (male and female condoms, diaphragms, spermicides, and fertility awareness-based methods).
Comprehensive post-abortion care is expected to be available at referral-level facilities. We measured the capacity to provide comprehensive post-abortion care through nine signal functions: five of the signal functions for basic post-abortion care (removal of retained products of conception; administration of parenteral antibiotics, parenteral uterotonics, and intravenous fluids; and provision of at least one modern, short-acting family planning method at the time of the survey; figure 1), the capacity to provide blood transfusions and do major abdominal surgery (ie, laparotomy and hysterectomy; this function was proxied by capacity to provide caesareans), the availability of health professionals capable of doing caesareans 24 h per day, 7 days per week, and the availability of a long-acting contraceptive method (intrauterine devices or hormonal implants) on the day of the survey or facility provision of permanent contraceptive methods (ie, female and male sterilisation). Referral-level facilities were not required to have communication or transportation capacity as they were assumed to have the capacity to provide the breadth of care required to manage severe complications.
We did not include all the staffing signal functions that Campbell and colleagues recommend.10 For measurement of basic post-abortion care, we assumed that our signal function of availability of staff capable of doing vaginal deliveries 24 h per day, 7 days per week encompassed the following signal functions: the facility was open 24 h per day, 7 days per week with at least one health professional on duty and at least three health professionals registered for basic post-abortion care. Likewise, for comprehensive post-abortion care, we assumed that availability of staff capable of providing caesareans encompassed the following signal functions: the facility was open 24 h per day, 7 days per week, with at least one medical doctor on duty and at least three medical doctors registered for comprehensive post-abortion care.
Five signal functions were based on facilities reporting if they had ever provided the requisite service (ie, removal of retained products of conception, provision of parenteral antibiotics and parenteral uterotonics, blood transfusions, and surgical capability). We chose the duration of ever instead of the past 3-month period preferred by most signal-function studies because health systems and patient flow might have varied in the chosen countries, and we wanted to ensure a period long enough for facilities to have encountered patients needing these services. Five signal functions were assessed based on the availability and functionality of a given item (drug or equipment) at the time of the survey (ie, provision of intravenous fluids, provision of short-acting or long- acting reversible or permanent contraceptive methods, communication, and transportation capabilities for referral). We calculated the proportion of facilities providing each post-abortion care signal function to examine specific gaps in service provision.
Statistical analysis
We calculated country-level statistics for primary-level and referral-level facilities that did deliveries, and applied facility sample weights that were specific to the survey. Surveys in Bangladesh, Kenya, Nepal, Senegal, Tanzania, and Uganda were based on nationally representative samples of health facilities; those in Haiti, Malawi, and Namibia were based on facility censuses, whereas Rwanda was based on a near-census of facilities. Survey weights accounted for stratification as described in the country’s report (typically by a subnational, geographical unit such as a region or province, and by an administrative unit, such as facility type or managing authority for facilities). They also accounted for over-sampling of specific facility types, non-response, and facility closures (appendix).
We created composite indicators for measuring the health system’s capacity to provide basic and comprehensive post-abortion care based on the signal functions described earlier (figure 1). We also constructed two less-restrictive composite indicators for basic and comprehensive provision of post-abortion care on the basis of evidence from other studies that appropriate referral in obstetric care,15–17 sufficient trained health staff,16 and provision of post-abortion family planning counselling remains a challenge for facilities8,10 in many low-income countries. For the first less-restrictive composite indicator of basic post-abortion care, the signal function of staff availability was excluded. For the second less-restrictive measure, we excluded staff availability and the two signal functions for the capacity to refer patients (ie, communication capacity and transport), and expanded the criteria for post-abortion family planning services to include at least one short-acting or long-acting method available on the day of the survey. For comprehensive post-abortion care, the first less-restrictive composite indicator excluded the requirement for staff availability. For the second less-restrictive measure, we excluded the signal function for staff availability and used the same expanded criteria for post-abortion family planning services as for basic post-abortion care.
We calculated the percentage of facilities in each country that met each set of signal functions in the composite indicators to measure the proportion of primary-level and referral-level health facilities capable of providing basic post-abortion care, and the proportion of referral-level facilities capable of providing comprehensive post-abortion care. We examined how countries’ proportions of facilities capable of providing basic and comprehensive post-abortion care differed across the composite indicators. We also calculated the proportion of primary-level and referral-level facilities in each country that provide each individual signal function to ascertain specific gaps in service capability and provision. We used Stata version 15.0 for the statistical analysis.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
The ten countries included in this analysis had broadly different contexts in which abortion-related morbidity and mortality occurred, including the legal conditions for pregnancy termination; the abortion rate, treatment rate for abortion-related complications, and maternal mortality rate; and national policies and guidelines on the provision of post-abortion care (appendix table 3). Six (60%) of the ten countries included in the analysis (Kenya, Malawi, Rwanda, Senegal, Tanzania, and Uganda) are in regions of Africa where 24% or less of induced abortions are considered safe.4 Maternal mortality levels were consistently high across all countries, with estimates of 121 or more maternal deaths per 100 000 livebirths in 2016. National policies and guidelines indicated that provision of post-abortion care was explicitly allowed at the primary level in five (50%) of the ten countries (Haiti, Namibia, Nepal, Senegal, and Uganda) and at the referral level in six (60%) of the ten countries (Bangladesh, Haiti, Namibia, Nepal, Senegal, and Uganda). Post-abortion counselling for contraceptive methods was included in post-abortion care policies or national guidelines for nine (90%) of the ten countries (Bangladesh, Haiti, Kenya, Malawi, Nepal, Rwanda, Senegal, Tanzania, Uganda; appendix).
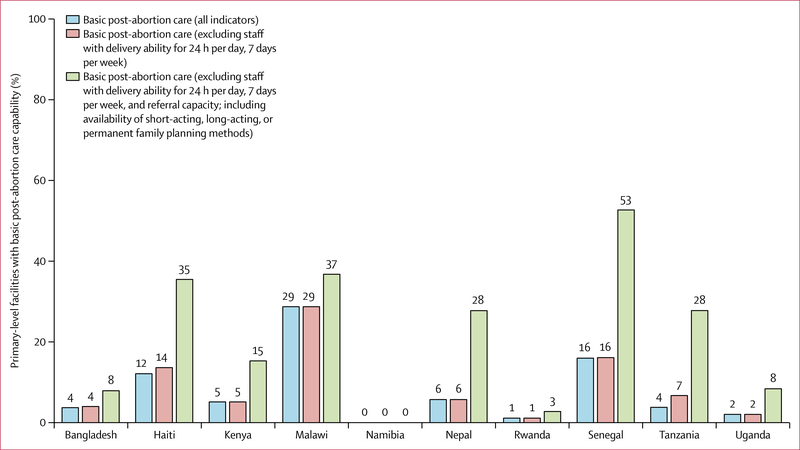
Data for the availability and distribution of post-abortion care services across the ten countries showed an alarming state of health care for women who had complications from either induced or spontaneous abortion and sought treatment. The proportion of primary-level facilities with basic post-abortion care capability, based on providing all eight signal functions, ranged from 0 of 213 in Namibia to 136 (29%) of 472 (95% CI 25–33) in Malawi, and was less than 10% in seven (70%) of ten countries (figure 2). When we used a less restrictive composite indicator of basic post-abortion care by excluding staff availability and the two signal functions for the capacity to refer patients, and expanding the criteria of post-abortion family planning services to provision of either long-acting or short-acting contraceptives, the proportion of primary-level facilities with basic post-abortion care capability increased in every country except Namibia. This proportion ranged from ten (3%) of 365 (95% CI 1–5) of primary-level facilities in Rwanda to 184 (53%) of 350 (47–58) in Senegal (figure 2). Even with this circumscribed set of post-abortion care services, in nine (90%) of the ten countries fewer than half of the primary-level facilities that provided delivery services could also provide basic post-abortion care.
Figure 2: Basic post-abortion care capability among primary-level facilities in ten countries providing deliveries, 2007–15.
Data presented compare three aggregate indicators of basic post-abortion care.
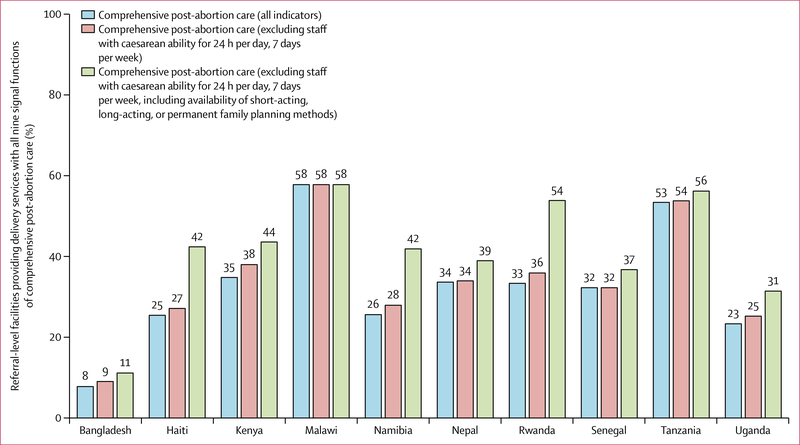
In eight (80%) of the ten countries, less than 40% of referral-level facilities that provided delivery services could provide all nine signal functions of comprehensive post-abortion care, with comprehensive capacity levels ranging from six (8%) of 80 (95% CI 5–11) in Bangladesh to 32 (58%) of 55 (45–70) in Malawi (figure 3). By use of a less-restrictive indicator of comprehensive provision of post-abortion care that excluded staff availability and expanded the criteria for post-abortion family planning services to at least one long-acting or short-acting method, the overall capacity of referral-level health facilities to provide comprehensive post-abortion care increased in all countries except Malawi (which remained at 58%; figure 3). Yet, even under these criteria fewer than half of all referral-level facilities that provided delivery services could provide comprehensive post-abortion care in seven of the ten countries.
Figure 3: Comprehensive post-abortion care capability among referral-level facilities in ten countries providing deliveries, 2007–15.
Data presented compare three aggregate indicators of basic post-abortion care.
Data for the individual signal functions for basic post-abortion care indicated where there might have been strengths or challenges in delivering basic post-abortion care at the primary level, and whether these were common across the countries (table). Relative strengths compared with other signal functions were post-abortion family planning, staffing, and provision of intravenous fluids. Almost all primary-level facilities that provided deliveries in the ten countries (98–100%) had a short-acting contraceptive method available at the time of the survey. More than half the primary-level facilities in all countries except Bangladesh had availability of staff capable of providing delivery services 24 h per day, 7 days per week and providing intravenous fluids. The most commonly absent signal function for basic post-abortion care was the means to transport a patient to a referral- level facility: in five (50%) of the ten countries, less than 20% of primary-level facilities could do so. Other services related to basic post-abortion care that were missing in many primary-level facilities were the capacity to remove products of conception and to administer parenteral antibiotics.
Table:
Country-specific capability to provide post-abortion care, 2007–15
| Bangladesh | Haiti | Kenya | Malawi | Namibia | Nepal | Rwanda | Senegal | Tanzania | Uganda | |
|---|---|---|---|---|---|---|---|---|---|---|
| Capability to provide basic post-abortion care signal functions among primary-level facilities | ||||||||||
| Removal of retained products of conception | 26% | 61% | 44% | 48% | 1% | 51% | 13% | 84% | 52% | 30% |
| Administer parenteral antibiotics | 31% | 64% | 58% | 88% | 13% | 49% | 55% | 82% | 52% | 59% |
| Administer parenteral uterotonics | 44% | 73% | 81% | 99% | 16% | 97% | 22% | 80% | 90% | 59% |
| Administer intravenous fluids | 28% | 86% | 84% | 96% | 84% | 99% | 78% | 97% | 86% | 63% |
| Modern short-acting family planning methods available | 100% | 100% | 100% | 99% | 100% | 100% | 98% | 98% | 99% | 99% |
| Capacity to communicate with referral facilities | 25% | 67% | 92% | 81% | 95% | 17% | 90% | 30% | 26% | 79% |
| Means of referral (vehicle with fuel) | 15% | 45% | 17% | 88% | 15% | 57% | 18% | 50% | 60% | 8% |
| Staff capable of undertaking vaginal deliveries available 24 h per day, 7 days per week | 41% | 71% | 78% | 99% | 64% | 91% | 100% | 97% | 58% | 87% |
| Capability to provide comprehensive post-abortion care signal functions among referral-level facilities | ||||||||||
| Removal of retained products of conception | 70% | 80% | 91% | 75% | 86% | 74% | 95% | 86% | 83% | 78% |
| Administer parenteral antibiotics | 90% | 100% | 88% | 98% | 79% | 87% | 97% | 98% | 95% | 89% |
| Administer parenteral uterotonics | 88% | 100% | 96% | 98% | 93% | 94% | 100% | 100% | 98% | 82% |
| Administer intravenous fluids | 95% | 100% | 92% | 100% | 98% | 94% | 100% | 93% | 93% | 88% |
| Modern short-acting family planning methods available | 100% | 100% | 100% | 100% | 93% | 95% | 71% | 87% | 99% | 100% |
| Administer blood transfusion | 44% | 78% | 60% | 95% | 95% | 69% | 100% | 41% | 87% | 53% |
| Surgical capability | 63% | 90% | 55% | 91% | 81% | 68% | 100% | 75% | 88% | 50% |
| Long-acting or permanent family planning methods available | 88% | 60% | 82% | 96% | 55% | 73% | 88% | 65% | 96% | 52% |
| Staff capable of undertaking caesareans available 24 h per day, 7 days per week | 56% | 80% | 50% | 89% | 74% | 68% | 87% | 75% | 88% | 44% |
Generally across the ten countries, referral-level facilities had greater capacity than primary-level facilities to provide basic post-abortion care signal functions, ranging from 24 referral-level facilities (30%) of 80 (95% CI 25–35) in Bangladesh to eight (60%) of 13 (38–78) in Senegal (appendix). More than 70% of referral facilities in all ten countries administered parenteral antibiotics, parenteral uterotonics, and intravenous fluids, and had at least one short-acting contraceptive method available (table). The proportion of referral-level facilities that had ever removed retained products of conception ranged from 56 (70%) of 80 (95% CI 64–76) in Bangladesh to 37 (95%) of 39 (81–99) in Rwanda.
There were larger gaps between countries in the signal functions for comprehensive post-abortion care than for the basic version. For example, blood transfusion capability ranged from five (41%) of 13 referral-level facilities (95% CI 24–61) in Senegal to 39 (100%) of 39 in Rwanda; a similar gap was noted for surgical capability, with 55% or less of referral facilities in Kenya and Uganda having ever done caesareans compared with more than 80% of referral facilities in Haiti, Malawi, Rwanda, Namibia, and Tanzania (table).
Countries showed inconsistent capacity to provide postabortion care across the signal functions. For example, although only 41% of referral facilities in Senegal provided blood transfusions, nearly all provided parenteral antibiotics and uterotonics. The different levels of capacity across essential post-abortion care services within each country produced the consistently low levels found in the composite measures of comprehensive post-abortion care across all ten countries.
Discussion
This was the first multicountry analysis using standardised, nationally representative data, and a signal functions approach to assess the capacity of national health systems to provide post-abortion care. Although post-abortion care is an essential emergency service, less than 10% of primary-level facilities in seven countries had the capability to provide basic post-abortion care and less than 40% of referral-level facilities in eight countries could provide comprehensive post-abortion care. Considering that the results pertained only to facilities offering delivery services, the proportion of facilities with basic and comprehensive post-abortion care capability would be even lower if all facilities were considered. Our results showing poor quality of post-abortion care were consistent with country-specific studies examining post-abortion care in Zambia,10 Kenya,18 and Nepal.19
Facility admissions for abortion-related complications due to induced or spontaneous abortions commonly occur in many of the countries included in our study,20 and moderate to severe complications have higher risks of morbidity and mortality.3,21,22 In emergencies, primary- level facilities are usually easier for women to access geographically, particularly in rural or poorer urban areas. In such areas, women might be more likely to delay seeking care for complications from spontaneous or induced abortion, thus further increasing the risk of complications becoming more severe.23 Our study suggests that most women would be unable to receive appropriate care at the theoretically closest-available health facilities in these countries. Furthermore, even those women who can access referral-level facilities, either via referral from primary care or through bypassing primary care altogether, are not guaranteed appropriate management of their complications at that level.
The provision of essential services at facilities varied considerably between countries. This most likely reflected the structure of the health system and tasks expected at each level of facility within it, regardless of our broad classification into primary and referral levels for analysis. Although we attempted to accommodate the disparity in health-facility classifications across countries by restricting our analysis to facilities that provided deliveries and using the country SPA reports to classify them, a wide range of facilities with varying capabilities were included in both groups. This is reflected in the varying proportions of referral-level facilities that had surgical and blood transfusion capability in each country. However, all facilities that undertake deliveries should have the capacity to provide basic care for common obstetric complications that include abortion-related complications.
The pattern of lower availability of a broad range of contraceptive methods (short-acting and long-acting, reversible methods and permanent methods) at referral- level facilities in many countries is similar to results from a study in Zambia.10 This finding might also be an artifact of the health system, where women are sent to primary-level care to obtain contraceptive methods as a way of reducing staff workload at the referral level and to improve continuation of care. However, evidence shows that post-abortion family planning is best provided at the same time and location as clinical treatment for complications,8 and that when post-abortion family planning counselling is provided, it increases the uptake of contraceptive methods by women and thus protects them against the risk of future unintended pregnancies.24,25
Our study had several limitations. First, question wording in the SPA surveys has changed over time such that our analysis included data based on slightly different questions (appendix). Second, SPA surveys only collect data related to post-abortion care from facilities providing delivery services; hence, we relied on information collected about delivery services or general hospital services (such as communication and referral). This approach could have possibly excluded from the analysis some hospitals that provide post-abortion care but do not do deliveries. Respondents’ answers also might not have taken post-abortion care into consideration and might have differed if the survey had specifically asked about post-abortion care. Furthermore, having staff trained to provide delivery care and emergency obstetric care does not guarantee their willingness to provide post-abortion care. Provider stigma and refusal to provide women with abortion care have been documented as challenges that women face within health systems.26 Additionally, we relied on certain delivery indicators as proxies for the ability to provide an essential signal function of post-abortion care. Third, we relied on facilities ever having done a function and did not limit signal function availability to performance of a function in the past 3 or 12 months. Similarly, because of inconsistencies in question phrasing across country surveys, we relied on both observed and reported availability and functionality of commodities (appendix). These two decisions could have resulted in an overestimation of actual capabilities of the facility at the time of survey. Considering these limitations, our results are a conservative scenario of post-abortion care availability and quality in the countries considered, despite the relatively dismal results. A fourth limitation of the study is that our characterisation of the quality of post-abortion care is from a health-system perspective alone and based on structural indicators of care provision and if essential services have ever been delivered. The evidence we used cannot account for other important aspects of the quality of abortion-related care, especially patient-centred measures. Because Rwanda’s SPA was a near census, we might have underestimated the signal functions in private facilities with three to four providers. However, from a health- systems perspective, these facilities account for a very small proportion of the total and are not likely to be major providers of post-abortion care services.
Future prospective studies are needed to build on this approach, to continue to track availability and quality of post-abortion care, to link them to women’s outcomes and to test interventions to improve services. Although post-abortion care is part of overall emergency obstetric care, information on the availability of services related to post-abortion care should be collected specifically for assessing the provision of abortion-related care. These services were probably reported more for deliveries, as part of emergency obstetric care, than management of early pregnancy loss (induced and spontaneous). Since 2012, SPA facility inventory data have been collected to enable calculation of WHO and USAID service readiness indicators in the service availability and readiness assessment methodology. Improving public accessibility to more recent health system datasets, such as the country-level service availability and readiness assessment microdata that can be used to measure capacity of post-abortion care and are standardised with the SPA, will allow for better information to track changes in availability of post-abortion care and quality over time.
Providing high-quality post-abortion care in all facilities is an ethical and humanitarian imperative.27 High-quality post-abortion care can lead to reductions in the levels of abortion-related morbidity and mortality from induced and spontaneous abortion and encompasses interventions that are part of comprehensive health-care delivery efforts to achieve universal health coverage.28 It is particularly crucial that governments increase the capacity of all health facilities to deliver basic post-abortion care because numerous studies of basic emergency obstetric care have noted that population coverage of basic care is often deficient compared with emergency care.29–31 The evidence from this study points to the substantial gap between political commitments to address the consequences of unsafe abortion through the provision of quality post-abortion care and the capacity of national health systems to provide this life-saving service.
Contributors
OOO and AB planned the study. OOO and HSW did the statistical analyses. OOO and AB wrote the first draft of the Article, which was revised and critically reviewed by all authors. All authors had access to the publicly accessible microdata, contributed to the discussion, and approved the final version of the manuscript.
Supplementary Material
Research in context.
Evidence before this study
The provision of quality post-abortion care can lead to reductions in morbidity and mortality from complications due to incomplete abortions or abortions done under unsafe conditions. Post-abortion care includes the treatment of complications and prevention of unintended pregnancy. We searched MEDLINE with the terms “postabortion”, “postabortion care*”, “postabortion health services*”, “postabortion complications”, “postabortion use”, or “postabortion services*” for published articles, observational studies, reviews, or systematic reviews published in any language before Feb 28, 2018. We also searched Demographic and Health Surveys publications that used data from the Service Provision Assessment survey. We did not identify any multicountry analyses of the capacity of health systems to provide essential elements of post-abortion care. Relevant studies tended to focus either on a single country (or subnational areas within a country) or on a particular element of post-abortion care (eg, post-abortion contraception).
Added value of this study
Ours is the first multicountry analysis using standardised, nationally representative data to assess the capacity of primary-level and referral-level health facilities that offer delivery services to provide post-abortion care. We used comparable indicators of the key elements of basic and comprehensive post-abortion care services (termed as signal functions). Our results reflected the quality of post-abortion care from a health-systems perspective, and we documented the particular components of post-abortion care for which countries had stronger or weaker capacity.
Implications of all the available evidence
Our findings for ten countries across three geographical regions showed that the capacity of primary-level and referral-level health facilities to provide basic and comprehensive post-abortion care, respectively, is low. The analysis was limited to health facilities that offer delivery services, so the results indicated a large gap between governmental commitments to provide post-abortion care and the relevant health facilities that can do so adequately. Our study showed the need for increased investment by governments in the capacity of health facilities to deliver essential post-abortion care, including the treatment of complications, referral to higher-level facilities, and the provision of contraceptive counselling and a broad range of methods, and to continue to monitor the availability and quality of post-abortion care.
Acknowledgments
Funding UK Aid from the UK Government.
Footnotes
Declaration of interests
OOO, AB, and HSW report a grant by UK Aid from the UK Government; however, the views expressed do not necessarily reflect the UK Governments official policies.
References
- 1.Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2016 (GBD 2016) Results. Seattle: Institute for Health Metrics and Evaluation (IHME), 2017. http://ghdx.healthdata.org/gbd-results-tool (accessed Feb 1, 2018). [Google Scholar]
- 2.Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a Who systematic analysis. Lancet Glob Health 2014; 2: e323–33. [DOI] [PubMed] [Google Scholar]
- 3.Calvert C, Owolabi OO, Yeung F, et al. The magnitude and severity of abortion-related morbidity in settings with limited access to abortion services: a systematic review and meta-regression. BMJ Glob Health 2018; 3: e000692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganatra B, Gerdts C, Rossier C, et al. Global, regional, and subregional classification of abortions by safety, 2010–14: Estimates from a Bayesian hierarchical model. Lancet 2017; 390: 2372–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UN. Report of the International Conference on Population and Development, Cairo, 5–13 September 1994 New York: United Nations, 1994. [PubMed] [Google Scholar]
- 6.WHO. Safe abortion: technical and policy guidance for health systems, 2nd edn. Geneva: World Health Organization, 2012. [PubMed] [Google Scholar]
- 7.Postabortion Care (PAC) consortium. PAC model. Postabortion Care (PAC) Consortium, 2015. http://pac-consortium.org/ (accessed Feb 28, 2018). [Google Scholar]
- 8.Huber D, Curtis C, Irani L, Pappa S, Arrington L. Postabortion care: 20 years of strong evidence on emergency treatment, family planning, and other programming components. Glob Health Sci Pract 2016; 4: 481–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dennis A, Blanchard K, Bessenaar T. Identifying indicators for quality abortion care: a systematic literature review. J Fam Plann Reprod Health Care 2017; 43: 7–15. [DOI] [PubMed] [Google Scholar]
- 10.Campbell OMR, Aquino EML, Vwalika B, Gabrysch S. Signal functions for measuring the ability of health facilities to provide abortion services: an illustrative analysis using a health facility census in Zambia. BMC Pregnancy Childbirth 2016; 16: 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Healy J, Otsea K, Benson J. Counting abortions so that abortion counts: Indicators for monitoring the availability and use of abortion care services. Int J Gynaecol Obstet 2006; 95: 209–20. [DOI] [PubMed] [Google Scholar]
- 12.Dibaba Y, Dijkerman S, Fetters T, et al. A decade of progress providing safe abortion services in Ethiopia: results of national assessments in 2008 and 2014. BMC Pregnancy Childbirth 2017; 17: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed SM, Naheed A, WHO. Bangladesh health system review. World Health Organization, Regional Office for the Western Pacific, Asia Pacific Observatory on Health Systems and Policies, 2015. [Google Scholar]
- 14.WHO. Global Abortion Policies Database. Geneva: World Health Organization, 2017. https://srhr.org/abortion-policies/ (accessed Feb 17, 2018). [Google Scholar]
- 15.Murray SF, Pearson SC. Maternity referral systems in developing countries: Current knowledge and future research needs.Soc Sci Med 2006; 62: 2205–15. [DOI] [PubMed] [Google Scholar]
- 16.Kyei-Nimakoh M, Carolan-Olah M, McCann TV. Access barriers to obstetric care at health facilities in sub-Saharan Africa—a systematic review. Syst Rev 2017; 6: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ndihokubwayo JB, Coulibaly SO, Cherian MN, et al. Strengthening surgical and anaesthetic services at district level in the African region: issues, challenges and proposed actions. East Cent Afr J Surg 2017; 22: 21–27. [Google Scholar]
- 18.Mutua MM, Achia TNO, Maina BW, Izugbara CO. A cross-sectional analysis of Kenyan postabortion care services using a nationally representative sample. Int J Gynaecol Obstet 2017; 138: 276. [DOI] [PubMed] [Google Scholar]
- 19.Bell SO, Zimmerman L, Choi Y, Hindin MJ. Legal but limited? Abortion service availability and readiness assessment in Nepal. Health Policy Plan 2018; 33: 99–106. [DOI] [PubMed] [Google Scholar]
- 20.Singh S, Maddow-Zimet I. Facility-based treatment for medical complications resulting from unsafe pregnancy termination in the developing world, 2012: a review of evidence from 26 countries. BJOG 2016; 123: 1489–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalilani-Phiri L, Gebreselassie H, Levandowski BA, Kuchingale E, Kachale F, Kangaude G. The severity of abortion complications in Malawi. Int J Gynaecol Obstet 2015; 128: 160–64. [DOI] [PubMed] [Google Scholar]
- 22.Ziraba AK, Izugbara C, Levandowski BA, et al. Unsafe abortion in Kenya: a cross-sectional study of abortion complication severity and associated factors. BMC Pregnancy Childbirth 2015; 15: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mutua MM. Delayed post abortion care and complications from unsafe abortions in Kenya. Int J Epidemiol 2015; 44: i47. [Google Scholar]
- 24.USAID. High impact practices in family planning (HIP). Postabortion family planning: strengthening the family planning component of postabortion care. Washington DC: USAID, 2012. https://www.fphighimpactpractices.org/briefs/postabortion-family-planning/ (accessed Feb 26, 2018). [Google Scholar]
- 25.Johnson BR, Ndhlovu S, Farr SL, Chipato T. Reducing unplanned pregnancy and abortion in Zimbabwe through postabortion contraception. Stud Fam Plann 2002; 33: 195–202. [DOI] [PubMed] [Google Scholar]
- 26.Gemzell-Danielsson K, Cleeve A. Estimating abortion safety: advancements and challenges. Lancet 2017; 390: 2333–34. [DOI] [PubMed] [Google Scholar]
- 27.Kulczycki A The imperative to expand provision, access and use of misoprostol for post-abortion care in sub-Saharan Africa. Afr J Reprod Health 2016; 20: 22–25. [DOI] [PubMed] [Google Scholar]
- 28.Stenberg K, Hanssen O, Edejer TT-T, et al. Financing transformative health systems towards achievement of the health Sustainable Development Goals: a model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob Health 2017; 5: e875–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pearson L, Shoo R. Availability and use of emergency obstetric services: Kenya, Rwanda, Southern Sudan, and Uganda. Int J Gynaecol Obstet 2005; 88: 208–15. [DOI] [PubMed] [Google Scholar]
- 30.Paxton A, Bailey P, Lobis S, Fry D. Global patterns in availability of emergency obstetric care. Int J Gynaecol Obstet 2006; 93: 300–07. [DOI] [PubMed] [Google Scholar]
- 31.Ameh C, Msuya S, Hofman J, Raven J, Mathai M, van den Broek N. Status of emergency obstetric care in six developing countries five years before the MDG targets for maternal and newborn health. PLoS One 2012; 7: e49938. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.