Abstract
Background
Physiotherapists are currently working in primary care as first contact practitioners (FCP), assessing and managing patients with musculoskeletal conditions instead of GPs. There are no published data on these types of services.
Aim
To evaluate a new service presenting the first 2 years of data.
Design and setting
Analysis of 2 years’ data of patient outcomes and a patient experience questionnaire from two GP practices in Forth Valley NHS, UK. The service was launched in November 2015 in response to GP shortages.
Method
Data were collected from every patient contact in the first 2 years. This included outcomes of appointments, GP support, capacity of the service, referral rates to physiotherapy and orthopaedics, numbers of steroid injections, and outcomes from orthopaedic referrals. A patient experience questionnaire was also conducted.
Results
A total of 8417 patient contacts were made, with the majority managed within primary care (n = 7348; 87.3%) and 60.4% (n = 5083) requiring self-management alone. Referrals to orthopaedics were substantially reduced in both practices. Practice A from 1.1 to 0.7 per 1000 patients; practice B from 2.4 to 0.8 per 1000 patients. Of referrals to orthopaedics, 86% were considered ‘appropriate’. Extended scope physiotherapists (ESPs) asked for a GP review in 1% of patients.
Conclusion
The results suggest that patients with musculoskeletal conditions may be assessed and managed independently and effectively by physiotherapists instead of GPs. This has the potential to significantly reduce workload for GPs as the service requires minimal GP support. The majority of patients were managed within primary care, with low referral rates and highly appropriate referrals to orthopaedics. Patients reported positive views regarding the service.
Keywords: general practitioner, musculoskeletal diseases, physical therapists, primary health care, referral and consultation
INTRODUCTION
There is a crisis regarding the rapidly declining numbers of GPs across the UK and with one-third of GPs in Scotland predicted to retire within the next 5 years,1 this crisis is set to worsen. In 2015, 20% of GP training posts in Scotland were unfilled.2 In some Scottish practices, the shortage of GPs has meant that business partnerships have been dissolved and affected practices have been taken over by the local health board, leaving remaining GPs struggling to meet patient demand for appointments. This occurred in two practices in NHS Forth Valley, Scotland, in 2015; unable to recruit enough GPs into each practice to ensure a safe service, a re-design was initiated, and it was decided to take a multidisciplinary approach to meet patient needs. Advanced nurse practitioners (ANPs), extended scope physiotherapists (ESPs), and mental health nurses were employed to assess and treat some of the patients that would traditionally have been seen by a GP. The introduction of ESPs to these practices presents an innovative role within the physiotherapy profession, with ESPs in Forth Valley being among the first in the UK to take up this post.
ESPs in primary care are the first point of contact for patients with simple to complex musculoskeletal (MSK) conditions, which have been estimated to make up to 30% of a GP’s caseload.3 The prevalence of MSK conditions rises with age; and, with an ageing population, the burden on primary care services is expected to increase.4 ESPs in primary care are advanced physiotherapists who assess, diagnose, and manage patients independently, thus avoiding the GP appointments. The ESP will order investigations, refer to other services, and will often be able to administer steroid injections and/or independently prescribe medication, such as analgesia or anti-inflammatories for MSK conditions. ESPs will typically be graded as Agenda for Change band 7 or 8a and will already have several years of experience working as a specialist MSK physiotherapist. Recent publication of the scope and competencies of such roles ensures that ESP clinical practice is safe and regulated.5 Advanced physiotherapists supporting medical teams in providing assessment and treatment of patients with MSK conditions is not a new concept.6–9 Historical political drivers such as long orthopaedic waiting times7–9 and the New Deal European Working Time Directive, which resulted in reduced hours for junior doctors, led to the introduction of ESPs working in orthopaedic clinics.6 This role has rapidly expanded with ESPs in the MSK specialty working in many different clinical areas across the UK. Research has consistently shown that ESPs working in such environments can identify serious pathology,10,11 produce low referral numbers to orthopaedics,7,12,13 achieve good surgical conversion rates,8,9,13 and have high levels of patient satisfaction.4,10–14 A review of articles relating to the substitution of doctors with physiotherapists highlighted no safety concerns, though the quality of some of the research has been questioned by the same authors.10 Furthermore, GPs have expressed low confidence in their ability to diagnose and manage MSK conditions, commonly resulting in patients being referred on to secondary care when they could have been managed in primary care.12 The current challenges within primary care present a unique opportunity for the physiotherapy profession to demonstrate how ESPs can effectively, safely, and independently manage patients with MSK problems instead of a GP.
How this fits in
There are no known published studies presenting data from a service such as this, where a physiotherapist acts as a first contact practitioner for patients with musculoskeletal conditions as an alternative to a GP. These types of services are starting to emerge throughout the UK in response to shortages of GPs and difficulties in GP recruitment. This study presents the findings from the first 2 years of a new service, and results suggest that a physiotherapist can act as a first point of contact practitioner for patients with musculoskeletal conditions independently and effectively. Due to the current and predicted future pressures on GP services, physiotherapists may have much to offer general practice.
No published research presenting data from MSK services such as this were found. An unpublished audit and service evaluation of the first 3 months of the new role in primary care of the musculoskeletal practitioner, demonstrated that only 5% of patients seen were referred to orthopaedics, and patient satisfaction for the service was high (Hensman-Crook, unpublished audit, 2015; more information available from the authors on request). However, in the aforementioned study the previous orthopaedic referral rate was not reported, nor outcomes from orthopaedic referrals, and patient numbers were low (n = 168). More research into these roles, particularly the potential impact of reducing GP workload and to offer a different pathway for MSK conditions, is required.
The aims of this current study are to report:
the number of patients seen by ESPs and uptake of appointments;
outcomes of appointments with ESPs;
the numbers of prescriptions and fit notes
GPs needed to complete (for patients after seeing the ESP);
trends in referrals to orthopaedic services;
outcomes of ESP referrals to orthopaedics;
trends in referrals to musculoskeletal outpatient physiotherapy;
trends in numbers of steroid injections administered; and
patient views on the ESP service.
METHOD
The service evaluation was designed to capture data from the first 2 years of the ESP service at two GP practices in NHS Forth Valley, practice A and practice B, from 16 November 2015 to 30 November 2017 inclusive. The service was launched in November 2015 in response to GP shortages. Both practices had an approximate practice list size of around 9500 patients. Each practice had 1.2 whole time equivalent (WTE) ESPs (Agenda for Change band 8a). All ESPs had received standardised injection therapy training, and none were prescribers. Most patients were appointed directly by reception staff or after telephone triage from an ANP. All staff within the practice could appoint patients with ESPs. Patients were typically seen on the same day or within 1–2 days of requesting an appointment. ESP appointments were 20 minutes long and GP appointments were 15 minutes, within both practices. Patients were those deemed to have a potential MSK complaint and excluded the following criteria: <16 years of age, pregnancy, patients requiring a medication review or fit note only, and patients who required a home visit.
Data were collected from every patient contact and recorded on a simple data collection form that included: number of patients seen; outcomes from each patient contact, for example, self-management (such as advice or a brief intervention), injection, imaging, blood tests, physiotherapy referral, orthopaedic referral or other referral; number of patients requiring review by a GP after seeing the ESP; and numbers of patients requiring a fit note or prescription after seeing the ESP, which are actioned by the Duty GP without the GP seeing the patient.
In addition, the following were also recorded:
capacity of the service over a 20-month window (April 2016 to November 2017);
referral rates from each practice (from GPs and ESPs combined) to NHS Forth Valley physiotherapy and orthopaedics for the year preceding the introduction of the ESP role and the first 2 years of the service. Referral patterns were checked against previous years to ensure that the preceding year was a fair comparator and did not display any unusual patterns; and this was deemed to be the case;
outcomes from orthopaedic referrals (the first 18 months of the service from November 2015 to April 2017 as outcomes beyond this point were not known owing to waiting lists). In this study ‘appropriate’ was defined as investigations and/or treatment being offered that were only available in the secondary care setting or a review or open appointment being given. ‘Inappropriate’ was defined as investigations and/or treatment that could have been delivered in a primary care setting or no intervention being required; and
numbers of steroid injections administered in each practice for the year preceding the introduction of the ESP service and the first 2 years of the service.
A patient experience survey was conducted during a 2-week period, 1 March 2016 to 15 March 2016. Every patient that attended the ESP service was given a short six-item questionnaire that was similar to questions 21 and 22 from NHS England’s GP Patient Survey 201515 with replacement of the word ‘GP’ with ‘ESP’ (further details available from authors on request). Patients completed this anonymously.
RESULTS
In total, 8417 patients were seen in the first 2 years of the ESP service. There were 5999 new patients (71%) and 2418 (29%) return appointments where the patient had requested review of the same problem within 3 months, or where the ESP made a further appointment. There were 671 (8%) appointments where the patient failed to attend. Of referrals, 57 (<1%) were deemed inappropriate for the ESP service with a variety of reasons such as urinary tract infection (UTI), cellulitis, vascular issue, and pitting oedema (data not shown).
Capacity of the service
To allow for initial set up and establishment of the service, the capacity was measured after the first 5 months; from April 2016 to November 2017. This was comparable in both practices with an overall rate of 88% of appointments filled.
Outcomes of appointment with the extended scope physiotherapists (ESPs)
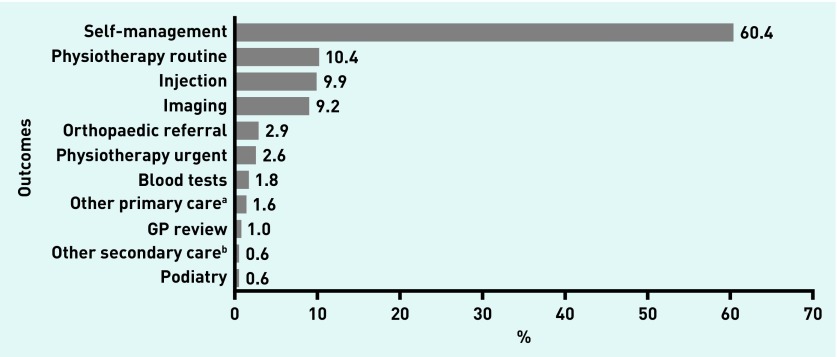
The total proportion of patients managed within primary care was 87.3% (n = 7348). Of the outcomes, 60.4% (n = 5083) of patients received self-management only, which may have involved advice or a brief intervention. Figure 1 shows the range and proportion of outcomes including referrals.
Figure 1.
Outcomes of extended scope physiotherapist appointments (N = 8417). a Other primary care: includes physiotherapy/podiatry clinic, mental health nurse, pain pharmacist, orthotics, social work and domiciliary physiotherapy/occupational therapy. b Other secondary care: includes rheumatology, neurology, oncology, A&E, and day therapy.
Support from GP
The ESPs identified 1% (n = 86) of patients as requiring a review with a GP; 12% (n = 1049) of patients required a prescription, and 3% (n = 221) required a fit note, both of which were issued by the Duty GP without the need for an appointment (data not shown).
Referral rates to orthopaedics
Referral rates for the year preceding the launch of the service and the first 2 years of the service are presented in Table 1. Referral rates for all years from both practices include both GP and ESP referrals. Referral rates to orthopaedics had lowered in both practices since the introduction of the service. In practice A, it lowered from 1.1 to 0.7 per 1000 patients (37% reduction) and, in practice B, from 2.4 to 0.8 per 1000 patients (64% reduction). This is estimated to have saved 212 referrals per annum (Table 1). In comparison, the monthly referral rate to orthopaedics across Forth Valley NHS trust was between 1.4 and 1.9 per 1000 patients across the 3-year period (data not shown).
Table 1.
Referral rates to orthopaedics from GPs and ESPs
| Study period | Average monthly referral rates to orthopaedics (relative to total practice appointments) | |||
|---|---|---|---|---|
| Practice A | Practice B | |||
| na | Per 1000 patients | na | Per 1000 patients | |
| November 2014 to October 2015 | 10 | 1.1 | 22 | 2.4 |
| November 2015 to October 2016 | 7 | 0.8 | 9 | 1.0 |
| November 2016 to October 2017 | 6 | 0.7 | 7 | 0.8 |
| Estimated annual referrals saved | 44 | 168 | ||
Nearest whole number. ESPs = Extended scope phsysiotherapists.
Outcomes from orthopaedic referrals
Over the 18-month period 165 patients were referred to orthopaedics from practice A and B combined. Of the patients that attended their appointment and where outcomes were known (n = 137), 118 (86%) were classed as appropriate and 19 (14%) were classed as inappropriate.
For 28 patients, the outcomes were not known for the following reasons: the patient had left the practice n = 10 (6%), the patient failed to attend their appointment n = 6 (4%), the patient did not respond to the offer letter n = 3 (2%), the patient had a private appointment n = 1 (1%), there was no outcome recorded in the patient records n = 6 (4%) and the patient was still on the waiting list n = 2 (1%) (data not shown).
Referral rates to physiotherapy
Referral rates for the year preceding the launch of the service and the first 2 years of the service are presented in Table 2. Referral rates for all years from both practices include both GP and ESP referrals. Referral rates to physiotherapy had increased since the introduction of the service. In practice A from 2.4 to 3.3 per 1000 patients and in practice B from 1.7 to 2.4 per 1000 patients. This has generated an estimated 216 referrals per annum from practices A and B combined. In comparison, the monthly referral rate to physiotherapy across Forth Valley NHS trust was between 2.5 and 2.9 per 1000 patients across the 3-year period (data not shown).
Table 2.
Referral rates to physiotherapy from GPs and ESPs
| Study period | Average monthly referral rates to physiotherapy (relative to total practice appointments) | |||
|---|---|---|---|---|
| Practice A | Practice B | |||
| na | Per 1000 patients | na | Per 1000 patients | |
| November 2014 to October 2015 | 22 | 2.4 | 16 | 1.7 |
| November 2015 to October 2016 | 31 | 3.4 | 29 | 3.2 |
| November 2016 to October 2017 | 30 | 3.3 | 22 | 2.4 |
| Estimated extra annual referrals | 96 | 120 | ||
Nearest whole number. ESPs = Extended scope phsysiotherapists.
Steroid injections
Data were gathered for numbers of patients who received a steroid injection from any clinician for the year preceding the launch of the ESP service and the first 2 years of the service (Table 3). The numbers of steroid injections had increased in each practice since the introduction of the service. In practice A, 43 steroid injections were carried out in the year preceding the launch of the service rising to 168 in the first year and 251 in the second year of the service. In practice B, 36 steroid injections were carried out in the year preceding the launch of the service rising to 119 in the first year and 169 in the second year of the service.
Table 3.
Numbers of steroid injections from any clinician
| Study period | Practice A, n | Practice B, n |
|---|---|---|
| November 2014 to October 2015 | 43 | 36 |
| November 2015 to October 2016 | 168 | 119 |
| November 2016 to October 2017 | 251 | 169 |
Patient experience of the ESP service
A total of 75 patients out of 182 completed the brief, anonymous questionnaire (return rate of 41%). The percentages of responses for each question are given in Table 4. Of the respondents, 92% (n = 69) marked ‘very good’ for the ESP ‘giving you enough time’ and the remaining 8% (n = 6) marked ‘good’ with no scores lower than this; 96% (n = 72) marked ‘very good’ for ‘listening to you’ and the remaining 4% (n = 3) marked ‘good’; 88% (n = 66) marked ‘very good’ for ‘explaining tests and treatments’ with 11% (n = 8) marking ‘good’, and 1% (n = 1) not applicable. Similar trends can be seen for the final three questions with the final question ‘did you have confidence and trust in the ESP you saw or spoke to’ scoring 97% (n = 73) for ‘very good’ and 3% (n = 2) for ‘good’.
Table 4.
Patient experience of the extended scope physiotherapist service, N = 75
| Patient experience of ESP service | Response, % | |||||
|---|---|---|---|---|---|---|
| Very good | Good | Neither good nor Poor | Poor | Very Poor | Not applicable | |
| Giving you enough time | 92 | 8 | 0 | 0 | 0 | 0 |
| Listening to you | 96 | 4 | 0 | 0 | 0 | 0 |
| Explaining tests and treatments | 88 | 11 | 0 | 0 | 0 | 1 |
| Involving you in decisions about your care | 89 | 11 | 0 | 0 | 0 | 0 |
| Treating you with care and concern | 91 | 9 | 0 | 0 | 0 | 0 |
| Yes, definitely | Yes, to some extent | No, not at all | Don’t know/can’t say | |||
| Did you have confidence and trust in the ESP you saw or spoke to? | 97 | 3 | 0 | 0 | ||
ESP = extended scope physiotherapist.
DISCUSSION
Summary
The majority of patients required self-management only (advice, information, or a brief intervention, Figure 1) and most patients were managed within primary care. The numbers of patients referred for imaging or blood tests were low. A negligible number of patients were inappropriate for the service or required input from a GP. The results suggest that patients could be assessed and managed independently by an ESP. Traditionally these patients would have seen a GP, and this represents a significant saving of GP time. A substantial reduction in referrals to orthopaedics and a high proportion of ‘appropriate’ referrals was reported. Referral rates to physiotherapy had risen and there was an increase in the numbers of steroid injections being provided. Results from the patient experience questionnaire showed a very positive response to the service by patients.
Strengths and limitations
The key strength of this study was the large patient sample with data from the first 2 years of the service. Data were collected from two comparable practices. The authors are not aware of any missed serious diagnoses, but no formal safety audit was completed. Additionally, reconsultation rates were not examined. It was not possible to calculate how many patients asked for, and were given, further assessment from a GP after an ESP appointment. The return rate for the patient experience questionnaire was 41% (n = 75) and, therefore, the findings should be interpreted with caution. It is also acknowledged that a definition was chosen for what was deemed ‘appropriate’ for referrals to orthopaedics and, though comparable to others,8 may not represent all reasons for referral.
Comparison with existing literature
Comparisons must be made cautiously due to differences in the service and patient population reported elsewhere.4,7,12 Other services included a screening service for patients before referral to orthopaedics,7 and an MSK triage service where GPs refer all patients with MSK conditions to advanced physiotherapists who triage, treat and/or refer on.4 Studies often had small sample sizes.4,7,12 No published studies were found reporting the results of ESPs working as first point of contact practitioners as an alternative to a GP.
In the present study, 87.3% of patients were managed entirely within primary care, similar to the systematic review by Hussenbux et al,12 and others7 (and Hensman-Crook, unpublished audit, 2015). The proportion of patients receiving self-management was higher (60%) than comparable studies (38%7 and 40% Hensman-Crook, unpublished audit, 2015); proportions of patients referred for imaging or blood tests was low and comparable to other studies7 (and Hensman-Crook, unpublished audit, 2015); and orthopaedic referral rates were lower (3%) than others (5% Hensman-Crook, unpublished audit, 2015 and 16% by Hattam and Smeatham7). However, one study7 was a screening service for orthopaedics so higher referral rates might be expected. Others lacked detail to allow comparison.4 Hussenbux et al12 report that MSK triage services could cause a 20–60% reduction in referrals to orthopaedics. Referral rates to physiotherapy and proportions of patients receiving a steroid injection are substantially lower than reported by others7 (including Hensman-Crook, unpublished audit, 2015).
Measuring the appropriateness of referrals to orthopaedics is important in view of the impact these have on secondary care. This study reports a high proportion of ‘appropriate’ referrals (86%). Other studies reported appropriate orthopaedic referrals of 71%8,12 and 74%9. Comparisons with other studies should be tentative due to possible differences in definitions, though the study by Hattam8 used similar criteria. Others (including Hensman-Crook, unpublished audit, 2015) have reported high levels of patient satisfaction in relation to ESPs working in similar roles.4,10–12,14
Implications for research and practice
Given the current crisis, services such as this could reduce burden by managing the MSK caseload within a general practice. The patient receives a specialist MSK assessment right at first presentation and GP time is released to focus on patients with other medical problems. The patient sees the right person, in the right place, at the right time.
Overburdened orthopaedic services may benefit from reduced referrals with more patients being cared for in primary care. High proportions of ‘appropriate’ orthopaedic referrals ensures less frustration for patients and clinicians. The increased number and range of steroid injections being offered as a management option for patients in primary care may avoid unnecessary secondary care referrals. However, this study has not reported outcomes from steroid injections or the long-term implications in a patient’s pathway.
Patient satisfaction is important. While it is vital to ensure that a change of role is safe, effective, and efficient, service users must also have confidence and trust in the clinician. Change can be difficult to accept and there may be barriers such as perceptions of skill level, which are not insignificant challenges. The authors of this study suggest that key factors for success in launching services such as this are: clarity and clear boundaries regarding the role; excellent communication with all staff and patients; strong leadership from the practice manager and GP team; and for posts to be based within the GP practice.
There are several other areas that may warrant further research. This study has in no way attempted to compare patient outcomes with outcomes after GP assessment or the impact of care given. No formal medical note review was completed to ensure that serious diagnoses were not missed, and no comparison has been attempted of the cost of a GP versus an ESP. Variables such as length of appointment time, salaries and differences in roles make this extremely complex. Outcomes of referrals to orthopaedic services are reported but the number of patients is relatively small in the present study, and outcomes of these referrals have not been compared to GP referrals. In light of the rapid expansion of these roles into primary care across the UK, research into these areas may be beneficial.
These results suggest that an ESP can act as a first point of contact practitioner for patients with MSK conditions, independently and effectively, as an alternative to the GP. Due to current pressures on GP services, ESPs have much to offer in relieving GPs of the MSK component of their caseloads. The number of patients given an appointment inappropriately with the ESP was very low and patients reported high satisfaction with the service. Patients may benefit from a wider range of steroid injections being offered in primary care. The service had been well utilised with some capacity to develop further. Patients with MSK conditions being managed independently and effectively by an ESP are to be welcomed. Within the current climate of significant barriers to GP provision, this will help alleviate some of the pressure. Finally, the role promotes physiotherapists as an alternative first point of contact for MSK conditions, and opens a different route for career progression for advanced physiotherapists.
Acknowledgments
The authors wish to acknowledge Richard Hendry, Senior Information Analyst; Anu Jassal, Senior Information Analyst; Laura Kenny, Information Analyst, all from NHS Forth Valley for additional support in collecting secondary care referral data.
Funding
No funding was received for this study.
Ethical approval
Ethical approval was not required as no data can be attributed to an individual patient.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.British Medical Association Over a third of GPs in Scotland plan to retire in the next five years. BMA. 2018. Dec 6, https://www.bma.org.uk/news/media-centre/press-releases/2016/december/over-a-third-of-GPs-to-retire-in-Scotland (accessed 19 Mar 2019)
- 2.Matthews-King A. Figures show widening shortfall in GP training with 20% of places unfilled. Pulse. 2015. Jul 1, http://www.pulsetoday.co.uk/news/gp-topics/education/figures-show-widening-shortfall-in-gp-training-with-20-of-places-unfilled/20010412.article (accessed 19 Mar 2019)
- 3.Thomson J, Syme G. Allied health professional (AHP) musculoskeletal pathway framework: national minimum standards. Scottish Government; 2014. https://www.gov.scot/publications/allied-health-professional-ahp-musculoskeletal-pathway-framework-national-minimum-standard/pages/2/ (accessed 6 Mar 2019) [Google Scholar]
- 4.Sephton R, Hough E, Roberts S, Oldham J. Evaluation of a primary care musculoskeletal clinical assessment service: a preliminary study. Physiotherapy. 2012;96(4):296–302. doi: 10.1016/j.physio.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Chartered Society of Physiotherapy . Advanced Practice in Physiotherapy. CSP; 2016. https://www.csp.org.uk/publications/advanced-practice-physiotherapy (accessed 6 Mar 2019) [Google Scholar]
- 6.Kersten P, McPherson K, Lattimer V, et al. Physiotherapy extended scope of practice — who is doing what and why? Physiotherapy. 2007;93(4):235–242. [Google Scholar]
- 7.Hattam P, Smeatham A. Evaluation of an orthopaedic screening service in primary care. Clin Gov. 1999;4(2):45–49. https://www.emeraldinsight.com/doi/full/10.1108/14664109910306749 (accessed 18 Mar 2019) [PubMed] [Google Scholar]
- 8.Hattam P. Effectiveness of orthopaedic triage by extended scope practitioners. Clin Gov. 2004;9(4):244–252. [Google Scholar]
- 9.Griffiths S, Taylor C, Yohannes AM. Conversion rates and perceived barriers to referral: views of extended scope practitioners in the primary care setting. Musculoskeletal Care. 2012;10(4):221–231. doi: 10.1002/msc.1023. [DOI] [PubMed] [Google Scholar]
- 10.Marks D, Comans T, Bisset L, Scuffham PA. Substitution of doctors with physiotherapists in the management of common musculoskeletal disorders: a systematic review. Physiotherapy. 2017;103(4):341–351. doi: 10.1016/j.physio.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Ludviggson ML, Enthoven P. Evaluation of physiotherapists as primary care assessors of patients with musculoskeletal disorders seeking primary health care. Physiotherapy. 2012;98(2):131–137. doi: 10.1016/j.physio.2011.04.354. [DOI] [PubMed] [Google Scholar]
- 12.Hussenbux A, Morrissey D, Joseph C, McClellan CM. Intermediate care pathways for musculoskeletal conditions — are they working? A systematic review. Physiotherapy. 2015;101(1):13–24. doi: 10.1016/j.physio.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 13.Rabey M, Morgans S, Barrett C. orthopaedic physiotherapy practitioners: surgical and radiological referral rates. Clin Gov. 2009;14(1):15–19. [Google Scholar]
- 14.Bath B, Janzen B. Patient and referring health provider satisfaction with a physiotherapy spinal triage assessment service. J Multidiscip Healthc. 2012;5:1–5. doi: 10.2147/JMDH.S26375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.NHS England GP Patient Survey 2010–2016 Survey materials: Questionnaire Jul–Sep 2015. 2015. http://www.gp-patient.co.uk/surveysandreports-10-16 (accessed 6 Mar 2019)