Abstract
Background
GPs often act as gatekeepers, authorising patients’ access to specialty care. Gatekeeping is frequently perceived as lowering health service use and health expenditure. However, there is little evidence suggesting that gatekeeping is more beneficial than direct access in terms of patient- and health-related outcomes.
Aim
To establish the impact of GP gatekeeping on quality of care, health use and expenditure, and health outcomes and patient satisfaction.
Design and setting
A systematic review.
Method
The databases MEDLINE, PreMEDLINE, Embase, and the Cochrane Library were searched for relevant articles using a search strategy. Two authors independently screened search results and assessed the quality of studies.
Results
Electronic searches identified 4899 studies (after removing duplicates), of which 25 met the inclusion criteria. Gatekeeping was associated with better quality of care and appropriate referral for further hospital visits and investigation. However, one study reported unfavourable outcomes for patients with cancer under gatekeeping, and some concerns were raised about the accuracy of diagnoses made by gatekeepers. Gatekeeping resulted in fewer hospitalisations and use of specialist care, but inevitably was associated with more primary care visits. Patients were less satisfied with gatekeeping than direct-access systems.
Conclusion
Gatekeeping was associated with lower healthcare use and expenditure, and better quality of care, but with lower patient satisfaction. Survival rate of patients with cancer in gatekeeping schemes was significantly lower than those in direct access, although primary care gatekeeping was not otherwise associated with delayed patient referral. The long-term outcomes of gatekeeping arrangements should be carefully studied before devising new gatekeeping policies.
Keywords: gatekeeping, healthcare expenditure, healthcare use, patient care, primary care, referral and consultation
INTRODUCTION
Gatekeeping in health care is a response to a shortage of specialists and a need to control healthcare expenditure.1 In gatekeeping systems, patients are required to visit a GP or primary care physician to authorise access to specialty care. However, the effectiveness of gatekeeping in controlling expenditure remains unclear. On an individual patient level, one study of private health insurance found that mean annual total health expenditure was lower for patients with health insurance plans that required primary care gatekeeping to authorise specialist referrals than for those with an indemnity (non-gatekeeping) plan.2 However, the percentage of gross domestic product spent on health does not differ significantly between countries with and without gatekeeping models of health care.3
A previous review, capturing literature up to January 2010, found that gatekeeping was related to lower health service use and lower health expenditure. However, there was great variability in the magnitude and direction of the differences, and the impact on health-related and patient-related outcomes was still inconclusive.4 The question remains whether gatekeeping is linked to any adverse health effects. A few studies have suggested that gatekeeping causes delayed diagnoses of cancer.5,6 In the UK — a healthcare system with strong gatekeeping — poor survival rates for breast, colorectal, and lung cancers compared with other European countries have been partly attributed to delayed diagnoses.6
Considering the potential impact of gatekeeping policy on patients and healthcare systems,3,5 there is a need for an updated systematic review to support healthcare policy. The aim of this study was to identify the effects of primary care physician gatekeeping on quality of care, health outcomes, use and expenditure, and physician and patient attitudes.
METHOD
A systematic review was conducted according to recommendations in the Cochrane Handbook for Systematic Reviews of Interventions,7 and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement.8
Search strategy
Following scoping searches, the strategy used in a previous systematic review4 was modified to include the term ‘referral’ to increase sensitivity to studies involving gatekeeping. Terms relating to ‘primary care’ were included to limit the search to gatekeeping in this setting. ‘Quality of care’, ‘health expenditure’, and ‘health outcomes‘ and ‘patient outcomes’ were included to increase specificity.
How this fits in
Previous work has suggested an association between gatekeeping and lower healthcare use and expenditure, with inconclusive evidence for the impact on health-related and patient-related outcomes. Particular concern exists that gatekeeping causes delayed cancer diagnosis. In this systematic review, gatekeeping was associated with lower healthcare use and expenditure, and better quality of care, but with lower patient satisfaction. Primary care gatekeeping was not otherwise associated with delayed patient referral.
The research databases MEDLINE, PreMEDLINE, Embase, and the Cochrane Library were searched for relevant studies. Preliminary searches showed that gatekeeping was rarely the main objective of a study. Therefore, a comprehensive search strategy was used from the databases’ respective inception dates up to September 2017. The MEDLINE search strategy is available from the authors on request.
Eligibility criteria
The eligibility criteria were discussed and agreed by all authors (Box 1). Gatekeeping was previously defined as a requirement to visit a primary care physician, family medicine doctor, GP, general internist, or general paediatrician in a primary care setting,4 so this definition was adopted. Studies relating to patient referrals in a primary care setting were included. Gatekeeping by a primary care physician, as an intervention, was required to be implemented in patient referrals. Studies considered were systematic reviews, experimental studies, and observational studies that included outcomes of quality of care, healthcare expenditure and use, health-related and patient-related outcomes including health-related quality of life, mortality, morbidity, and patient and clinician attitudes. Studies that were published in languages other than English and those for which the abstract or full-text could not be retrieved were excluded.
Box 1. Inclusion criteria for studies in the systematic review.
Gatekeeping conducted in a primary care setting by primary care physicians including a primary care physician, family medicine doctor, GP, general internist, or general paediatrician
Outcomes of gatekeeping involve one or more of:
quality of care;
healthcare expenditure and use; and
health-related and patient-related outcomes.
Study selection
Two of the authors independently screened titles and abstracts to identify eligible studies and conducted full-text screening for eligible studies. Discrepancies were solved through discussions with other authors.
Data collection, extraction, and assessment of study quality
Two authors independently extracted the following data from the studies: study design, setting, gatekeeping arrangements, population, duration, comparison, and outcomes of studies. The extracted information was collated in a structured form, and included information reported on the gatekeeping arrangement, categories of outcomes, country, study design, population, intervention, age group, conditions, sample size, comparison (if possible), and outcomes (quality of care, health expenditure, and health-related/patient-related outcomes). Extraction forms completed by the two authors were compared, and discrepancies were discussed with the other authors and followed up with reference to the original article.
Risk of bias assessment
The methodological quality of the studies was assessed independently by two authors following the Effective Practice for Organisation of Care recommendations for review authors.9 An appropriate assessment tool relevant for each study design was chosen: the AMSTAR checklist for quality assessment of systematic reviews and meta-analyses,10 the Cochrane Risk of Bias Tool for Randomised Controlled Trials,7 and the National Institute of Health and National Heart, Lung, and Blood Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies.11 The quality of each study was based on allocation, outcome assessment, data sources, and risk of contamination and bias. As quality assessment tools specific to each study design were used, the quality of studies with different designs was not compared.
Data synthesis
Owing to the variety of measured outcomes and methodological approaches in the included studies, it was not possible to conduct a meta-analysis, and therefore a descriptive narrative synthesis was used.12
RESULTS
Study selection
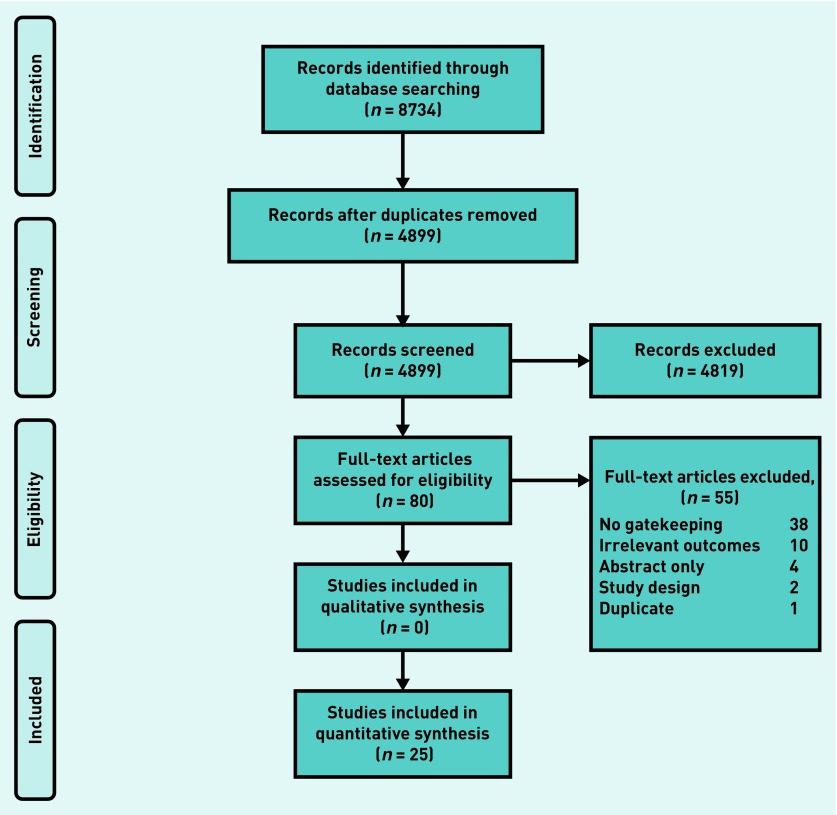
Electronic database searches yielded 8734 articles, of which 3835 were duplicates. Following title and abstract screening, 80 full-text studies were obtained. A total of 55 studies were excluded because they did not meet eligibility criteria, leaving 25 studies for analysis (Figure 1).2,4,13–35
Figure 1.
PRIMSA flow diagram for the search and selection process applied during the overview.
Study characteristics
Twenty-one observational studies, two controlled before-and-after studies, one systematic review, and one randomised controlled trial were included in the review; there were 17 studies from the US and eight from Europe, respectively (Table 1).2,4,13–35 Most of the studies included adult populations, and four included only children (<18 years old). Various health conditions were considered in the included studies. Mostly, the included studies examined the effects of gatekeeping interventions, including implementing or switching to a gatekeeping system,17,18,22 access to cancer screening services,13,20,23 emergency departments,35 and surgical departments.14,16
Table 1.
Characteristics of included studies
| Study and year | Study design | Country | Participants | Age, years | Condition | Intervention |
|---|---|---|---|---|---|---|
| Phillips et al (2004)13 | Observational | US | 13 534 | >18 | Cancer screening | Gatekeeping plan |
| Mitchell and Keenan (2008)14 | Observational | UK | 209 | 14–99 | Surgical admission | GP referral |
| Vedsted and Olesen (2011)15 | Ecological | 19 European countries | 19 countries | N/A | Cancer | Gatekeeping plan |
| Hartzell et al (2013)16 | Observational | US | 200 | N/A | Suspected hand surgical condition | Gatekeeping plan |
| Ferris et al (2002)17 | Controlled before-and-after | US | 59 952 | <18 | N/A | Gatekeeping plan |
| Pati et al (2005)2 | Observational | US | 8195 | 18–65 | N/A | Managed care with gatekeeping plan |
| Ferris et al (2001)18 | Controlled before-and-after | US | 59 997 | >18 | N/A | Without gatekeeping plan |
| Escarce et al (2001)19 | Observational | US | 55 954 | 18–64 | N/A | HMO with gatekeeping plan |
| Tye et al (2004)20 | Observational | US | 2909 | >40 | Patients without a history of breast cancer | Gatekeeping plan |
| Linden et al (2003)21 | Observational | The Netherlands and Germany | 1140 | 15–65 | Suspected psychological problems | Gatekeeping plan |
| Ferris et al (2001)22 | Observational | US | 1839 | <18 | N/A | Gatekeeping plan |
| Velasco Garrido et al (2011)4 | Systematic review | Germany | 26 studies | N/A | N/A | Gatekeeping plan |
| Haggstrom et al (2004)23 | Observational | US | 2623 | 18–65 | Mammography and cervical screening | Gatekeeping plan |
| Joyce et al (2000)24 | Observational | US | 53 011 | 18–64 | N/A | HMO with gatekeeping plan |
| Schneider et al (2016)25 | Observational | Germany | 3 616 510 | ≥18 | N/A | Coordinated care with gatekeeping plan |
| Kroneman et al (2006)26 | Observational | 18 European countries | 18 countries | N/A | N/A | Gatekeeping plan |
| Pati et al (2003)27 | Observational | US | 3254 | <18 | N/A | Gatekeeping plan |
| Delnoij et al (2000)28 | Observational | 18 OECD member countries | 18 countries | N/A | N/A | Gatekeeping plan |
| Schwenkglenks et al (2006)29 | Observational | Switzerland | 1810 | ≥18 | N/A | Gatekeeping plan |
| Kapur et al (2000)30 | Observational | US | 55 954 | 18–64 | Co-payment requirement | HMO with gatekeeping plan |
| Rask et al (1999)31 | Observational | US | 1414 | ≥30 | Patients with chest pain who were referred or self-referred to a cardiologist | Gatekeeping plan |
| Schillinger et al (2000)32 | Randomised controlled trial | US | 2293 | Adult | Required to have at least one visit to PCPs within 12 months and at least one visit to any San Francisco general hospital clinic within 6 months | Required gatekeeper |
| Halm et al (1997)33 | Observational | US | 330 | N/A | N/A | Gatekeeping plan |
| Forrest et al (2002)34 | Observational | US | 19 415 | 18–64 | N/A | Primary care authorisation for referral |
| Franco et al (1997)35 | Observational | US | 4766 | 0–13 | Visited emergency department and been triaged by a triage nurse or PCP | Primary care gatekeeper for emergency department |
HMO = health maintenance organisation. N/A = not available. OECD = Organisation for Economic Co-operation and Development. PCP = primary care physician.
Risk of bias assessment
Although most observational studies were of fair quality,2,13,19–25,27,30,31,34 experimental studies were rated at high risk of bias on the selective reporting domains.17,18,32 One systematic review scored 7 out of 11 according to AMSTAR recommendations.4 The AMSTAR checklist for methodological assessment of systematic reviews reflects bias.36 Another ecological study was not assessed because of its research design.15 Quality assessment for included studies is available from the authors on request.
Impact of gatekeeping on various indicators
Extracted outcomes from the studies are summarised in Table 2.
Table 2.
Extracted outcomes from included studies
| Study | Favouring gatekeeping | Favouring direct access |
|---|---|---|
| Phillips et al (2004)13 | Female patients in gatekeeper plans were more likely to receive mammography screening (77% versus 71%), clinical breast examination (87% versus 80%), and cervical screening (84% versus 74%). All comparisons, P<0.001 | |
| Mitchell and Keenan (2008)14 | A correct provisional diagnosis was stated in 43.6% of primary care diagnoses | |
| Vedsted and Olesen (2011)15 | Relative 1-year survival was higher compared with gatekeeper system (gatekeeper = 67.8, without gatekeeper = 73.4; P = 0.004) | |
| Hartzell et al (2013)16 | The correct diagnosis was made 31% of the time when the patient had been seen by only a primary care provider (P= 0.4) | |
| Ferris et al (2002)17 | Children visited a primary care physician an average of 2.16 times (95% CI = 2.12 to 2.19) per 6-month period before the removal of gatekeeping and 2.05 times (95% CI = 2.01 to 2.08) per 6-month period after the removal of gatekeeping. After a stable baseline period, the percentages of all visits to eligible specialists averaged 10.8% during the year before removal of gatekeeping and 11.0% during the year after removal of gatekeeping (P = 0.29) |
|
| Pati et al (2005)2 | For gatekeeping enrolees, mean annual total expenditures were US$1791 (SE = 140) compared with US$1834 (SE = 90) for those non-gatekeeping plans (P = 0.81) If both groups had similar characteristics, total mean per capita expenditures would have been US$1835 (SE = 18) for gatekeeping enrolees versus US$1959 (SE = 19) for indemnity enrolees Adults enrolled in managed care gatekeeping plans on average paid about US$110 less out of pocket than indemnity enrolees (P<0.05) |
Median per capita expenditures were higher for managed-care gatekeeping enrolees at US$561 (SE = 21) versus US$492 (SE = 22) for indemnity enrolees (not statistically significant) For outpatient expenditures, the proportion of adults with any ambulatory care expenditure was higher among care gatekeeping enrolees than among indemnity enrolees (76% versus 70%; P<0.05) Third-party payments for ambulatory services were about US$65 greater for gatekeeping enrolees than for indemnity enrolees (P<0.05) |
| Ferris et al (2001)18 | Adults visited a PCP an average of 1.21 times per 6-month period before the removal of gatekeeping and 1.19 times per 6-month period after the removal of gatekeeping (P = 0.05) After a stable baseline period, the average proportion of visits to eligible specialists as a percentage of all visits was 29.0% before the removal of gatekeeping and 29.6% during the year afterward (P = 0.39) Rates of visits to specialists were stable over the baseline period and did not change with the removal of gatekeeping |
|
| Escarce et al (2001)19 | About 83% of enrolees in the gatekeeper plan used physician services annually, compared with 74% of enrolees in the POS plan (P<0.001) About 5.7% of gatekeeper HMO members and 4.5% of POS plan members had inpatient hospital stays each year (P<0.001) 87% of enrolees in the gatekeeper HMO used some type of medical care annually, compared with 78% of enrolees in the POS plan (P<0.001) Gatekeeper enrolees had 25% higher expenditures for physician services (P<0.001), 23% higher inpatient hospital expenditures (P<0.01), 30% higher outpatient hospital expenditures (P<0.001), 43% prescription drug expenditures (P<0.001), and 41% higher expenditures for other services (P<0.001) than people in the POS plan Total medical care expenditures were 29% higher in the gatekeeper HMO (P<0.001) |
|
| Tye et al (2004)20 | Female patients in gatekeeper plans were more likely to report receiving mammography (77% versus 72%; P<0.001). The adjusted OR = 1.18 (95% CI = 1.03 to 1.36) | |
| Linden et al (2003)21 | At 3 months’ follow-up, the average total number of contacts between the enrolled patients and any other physicians in Germany was 4.56 per patient compared with 3.49 in the Netherlands | At the 12-month follow-up, hospital admissions were reported less often in Germany (15.7%) than in the Netherlands (25.4%; P<0.005) Psychiatric medication is given twice as often in Germany as in the Netherlands (16% versus 7%) |
| Ferris et al (2001)22 | Mean total expenditures for children in the gatekeeping group decreased 53% from US$486 before switching to gatekeeping to US$180 in 1994 Visits to subspecialists also declined dramatically in the gatekeeping group after the switch to gatekeeping (1.6/year in 1991 and 1992 to 0.5/year in 1994) (P<0.001 for difference) Mean annual subspecialty expenditures decreased 6% in the indemnity group and 59% in the gatekeeping group (P<0.001 for difference) Mean visits to subspecialists for children with chronic conditions decreased 57% in the gatekeeping group while increasing 31% in the indemnity group (P<0.005 for difference) Outpatient expenditures for primary care physician services declined for both the indemnity (5%) and gatekeeping (53%) groups over the period of the study (P<0.004 for difference) |
|
| Velasco Garrido et al (2011)4 | For quality of life, the study showed results favouring gatekeeping in single items (pain and role limitations), but no statistically significant differences in overall quality of life The studies with greater suitability suggest fewer hospitalisations under gatekeeping Overall, the results suggest lower use of specialist care under gatekeeping Most observations suggest 6–80% lower expenditures under gatekeeping |
The studies showed decreased satisfaction under the gatekeeping plan The diagnosis of melanoma was made without delay significantly more frequently in patients with free access, which, however, did not lead to any differences in the tumour stage at diagnosis |
| Haggstrom et al (2004)23 | Female patients in gatekeeper plans were more likely to receive screening mammography (77% versus 71%; P<0.001) and cervical screening (84% versus 74%; P<0.001) | |
| Joyce et al (2000)24 | Gatekeeper HMO members had 35% more PCP visits, 28% more specialist visits, and 33% more total visits than people in the POS plan | |
| Schneider et al (2016)25 | Averaging over age, the total difference per patient was −€ 9.65 (95% CI = −11.64 to −7.67), indicating lower costs for the gatekeeping model The prescription of psychotropic medication, measured in terms of cost, was lower in the coordinated group with total difference per patient = −€20.31 (95% CI = −26.43 to −14.46) in favour of coordinated care for these patients |
|
| Kroneman et al (2006)26 | Countries with more providers directly accessible for patients showed a higher patient satisfaction with GP services (Pearson’s r= 0.54; P = 0.05) | |
| Pati et al (2003)27 | If gatekeeping and indemnity plan enrolees had similar characteristics, total mean per capita expenditures would have been approximately 4% lower for children in gatekeeping plans at US$646 (SE 11) versus US$673 (SE 10) for indemnity plan enrolees Families of children enrolled in gatekeeping plans on average paid US$62 less out-of-pocket than indemnity plan enrolees (P<0.05) |
The proportion of children with any ambulatory care expenditures was higher among gatekeeping plan enrolees compared with indemnity plan enrolees (78% versus 74%; P<0.05) Mean total per capita annual expenditures for children in gatekeeping versus indemnity plans differed by <1% (US$887 versus US$881, respectively) Third-party expenditures for ambulatory services were on average US$45 greater for children enrolled in gatekeeping plans than for those in indemnity plans (P<0.05) |
| Delnoij et al (2000)28 | On average, per capita health spending is lower in gatekeeping systems than in non-gatekeeping systems In countries with gatekeeping GPs, ambulatory care expenditure has increased less than in non-gatekeeping systems |
|
| Schwenkglenks et al (2006)29 | Generally, health expenditure in gatekeeping group was lower than fee-for-service plans (but not statistically significant) | |
| Kapur et al (2000)30 | Expenditures tended to be higher in the gatekeeper HMO than in the POS plan, although covariate adjustment considerably narrowed the gaps observed in the unadjusted data (711 versus 564) Expenditures for PCPs’ services were significantly higher in the gatekeeper HMO (P<0.001) Total physician expenditures were 4% higher in the gatekeeper HMO (P<0.05) Total physician expenditures were 9% higher in the gatekeeper plan with US$10 co-payments for PCP and PCP-referred specialist visits than in the POS plan with US$10 and US$15 co-payments (P<0.01) |
|
| Rask et al (1999)31 | The cardiology visit rate was significantly higher in the open-access group (5.8 per 1000 open-access members versus 3.3 per 1000 gatekeeper members; P<0.01) and lower rate of echocardiograms among the gatekeeper patients (21% versus 29%; P<0.01) Gatekeeper patients with known coronary atherosclerotic heart disease were more likely to receive cardiac catheterisations (33% versus 19%; P<0.01) Gatekeeper patients as a group received cardiac catheterisation significantly sooner than did open-access patients (P = 0.05) |
|
| Schillinger et al (2000)32 | Patients in an intervention group had 0.14 fewer hospitalisations per year than a control group (P = 0.02, 95% CI = −0.26 to −0.03), representing approximately 29% fewer hospitalisations Patients in an intervention group decreased their specialty use by 0.57 visits per year more than a control group (P = 0.04, 95% CI = −1.05 to −0.01) Regarding coordination of care among ED patients (n= 734), a greater percentage of patients in an experimental group returned to general medicine clinic within a month of an ED visit, when compared with control patients (61% versus 52%; P<0.01) |
|
| Halm et al (1997)33 | Gatekeeping had a positive impact on preventive care (26% positive versus 10% negative), and knowledge over patients’ overall care (33% positive versus 8% negative) (P≤0.01). The overall cost of care was favourably affected by gatekeeping (P<0.001) | Quality of care judged to be impacted negatively (20% negative versus 6% positive; P<0.001) Gatekeeping was judged to have a negative effect on the appropriate use of hospitalisation (−0.33), laboratory tests (−0.22), specialists (−0.45), and medication choice (−0.45) (P<0.001) |
| Forrest et al (2002)34 | There is a significant difference in choice of PCP satisfaction between with and without authorisation requirement (67.1% versus 70.8%, difference = −3.7; P>0.001) | |
| Franco et al (1997)35 | There was a significant reduction of ED visits compared with 10.1% (283/2798) of clinic registrants who visited the ED during an analogous period before the intervention (P <0.001) 92% of ED visits were appropriate compared with 59% before the intervention (P<0.001) |
ED = emergency department. HMO = health maintenance organisation. OR = odds ratio. CI = confidence interval. PCP = primary care physician. POS = point of service. SE = standard error.
Quality of care
Five studies reported the impact of gatekeeping on outcome measures. In the US, patients were more likely to receive cardiac catheterisations (33% versus 19%; P<0.01) where there was primary care gatekeeping in place.31 Female patients enrolled in healthcare plans with gatekeeping were reported as having significantly more mammography screenings, clinical breast examinations, and cervical screening.13,23 They were reported as receiving more mammography in total (P<0.001; adjusted OR = 1.18; 95% CI = 1.03 to 1.36).20 However, two studies in the UK and the US indicated that primary care gatekeepers were correct in only 31%16 and 43.6%14 of diagnoses.
Health outcomes
Regarding cancer care, an ecological study reported that relative 1-year survival was higher in a direct-access system than in a gatekeeping system among patients with cancer.15 However, a pilot study included in a previous review4 demonstrated no difference in melanoma outcomes between gatekeeping and direct access, although patients in the direct-access group underwent diagnostic biopsy sooner than those in the gatekeeping group.
Healthcare use
Ten studies found effects of gatekeeping on healthcare use. The previous systematic review suggested that gatekeeping resulted in less hospitalisation and specialist use.4 In the US, a longitudinal study reported a significant reduction in emergency visits of patients following introduction of a gatekeeping system.35 Additionally, one randomised controlled trial reported that patients subject to gatekeeping decreased their healthcare use by 0.57 specialty visits and 0.14 hospitalisations per year more than patients with direct access.32
Patients made more visits to their primary care physician when gatekeeping was in place (P = 0.05).18 One cohort study reported that subspecialist visits declined in children with the gatekeeping (from 1.6/year to 0.5/year; P<0.001).22 However, one retrospective study showed that patients with healthcare plans requiring gatekeeper authorisation had 33% more total visits (primary care physician and specialist) than adults with a direct access plan.24
Health expenditure
Nine studies investigated the impact of gatekeeping on health expenditure. A previous systematic review showed health expenditure was 6–80% lower under gatekeeping than direct-access schemes.4 Two other studies also reported reduced healthcare expenditure where gatekeeping was in place,28 with lower costs than fee-for-service systems.29
A cross-sectional study reported that total mean expenditure was US$1835 for patients in a gatekeeping plan versus US$1959 for direct-access patients, and the gatekeeping patients paid US$110 less out-of-pocket.2 Moreover, the total cost difference per patient was −€9.65 (95% CI = −11.64 to −7.67), indicating lower costs for the gatekeeping model.25 However, a cross-sectional study in the US showed adults with a gatekeeping plan had 29% higher total medical expenditure.19 Another study suggested that total physician expenditure in a gatekeeping plan was 4% higher (P<0.05), especially for primary care physicians’ services (P<0.001).30
Healthcare expenditure for children was higher for those enrolled in a gatekeeping plan.27 However, if all enrolees had similar characteristics, total mean expenditure per capita would have been 4% lower for children with a gatekeeping plan.27 Similarly, another study in the US found total expenditure among children who switched to a gatekeeping plan from a direct-access plan decreased from US$486 to US$180.22
Physician attitudes
One cross-sectional study reported that primary care physicians perceived that gatekeeping had a negative impact on quality of care, and a positive impact on preventive care and knowledge of patients’ overall care.33 Primary care physicians reported that gatekeeping was significantly better at cost control than direct access. However, they believed that gatekeeping had a negative effect on the appropriate use of hospitalisation, laboratory tests, specialists, and medication choice.33
Patient satisfaction
Gatekeeping was associated with reduced patient satisfaction compared with a direct-access system.4 One study reported that patients were more satisfied with primary care physicians in a direct-access system than in a gatekeeping system.34 Similarly, a European study found that countries with more directly accessible providers showed greater patient satisfaction with GP services.26
DISCUSSION
Summary
Included studies suggest an association between gatekeeping and better quality of care, especially in terms of preventive care, and appropriate referral for specialty care and investigation. However, one study reported unfavourable outcomes of patients with cancer under gatekeeping,15 and some raised concerns about the ability of GP gatekeepers to provide a correct diagnosis.14,16 Gatekeeping resulted in fewer hospitalisations4,29,32 and lower specialist use,4,22,31 but in more primary care visits.24 Whereas some studies show that gatekeeping has lower healthcare use and expenditure,2,4,22,25,27–29,35 others suggest that gatekeeping has higher ambulatory care and outpatient expenditure.2,27 Primary care clinicians have conflicting views on gatekeeping,33 whereas patients are often less satisfied with gatekeeping schemes, preferring direct access to specialists.4,26,34
Strengths and limitations
This study aimed to summarise the current literature on an important mechanism shaping the functions of primary and secondary care, and the divide between them. It focused specifically on the gatekeeping function of primary care. The authors acknowledge that even this term has different meanings in different countries, under different healthcare models, and with different health insurance schemes, which makes comparison between studies challenging. Most of the studies included in this review are based in the US and so reflect the American healthcare system.
Although most included studies focused on gatekeeping interventions and impact on health outcomes, there may be some effects from other confounders such as cancer screening programmes, socioeconomic statuses, employments, and types of insurances that this study was unable to identify. Furthermore, the scarcity of randomised controlled trials make it challenging to attribute the observed differences merely to gatekeeping, because many other factors, such as different payment arrangements, could have affected the outcomes.
Most studies report process measures such as use, screening, or number of visits, with few reporting on patient-related and health-related outcomes, making it difficult to draw firm conclusions about the impact of gatekeeping on these areas. Finally, the findings are described in separate categories, derived from the included studies. It is likely that there is considerable inter-relation between these categories, with significant overlap, for example, between ‘quality of care’ and ‘patient experience’. Similarly, there is likely to be a complex association between patient satisfaction, gatekeeping, and healthcare use. However, the nature of the studies as reported meant that it was not possible to gain a clearer understanding of these complexities.
Comparison with existing literature
Some authors have challenged the notion of gatekeeping as an effective cost-containment system.3,27 The findings show that gatekeeping often results in lower health expenditure and health use for health services because it controls costs associated with unnecessary expensive specialist care and resource use.37
Patients are often less satisfied with gatekeeping schemes and prefer direct access to specialists, because they believe that specialists have better facilities, and because they wish to see a specialist quicker.38,39 To improve patient satisfaction, health systems should enlarge primary care capacity and decrease the gap between primary and secondary care sectors, promoting the role of primary care professionals as ‘healthcare coordinators’ between primary and secondary care.38,39
Patients in gatekeeping schemes are more likely to have preventive care in the form of cancer screening including cervical screening and mammography. However, delayed diagnosis caused by gatekeeping is believed to be one of the factors causing lower cancer survival rates in the UK. In England, nearly three-quarters of patients with cancer who visited their GPs in 200240 and 201441 were referred to a specialist after only one or two consultations, and about 60% of all referred patients saw a specialist within 2 weeks.40,41 This suggests that, at least in the UK, delayed diagnosis of cancer is not caused solely by gatekeeping, but by other healthcare system factors, patient behaviour, and healthcare provider factors.15,42–46
Implications for policy and research
Caution should be exercised in interpreting these findings to the policy context. Policymakers eager to reduce costs and use may conclude that reduction in specialist healthcare use and expenditure makes gatekeeping a favourable system. However, conclusions for policy can be drawn only when we are clear about the long-term consequences of reduced healthcare use and expenditure. Short-term reductions in specialist healthcare use may delay care, leading to worse patient outcomes.
The intended and unintended consequences of setting up gatekeeping, relaxation of gatekeeping, and use of gatekeeping should be considered in services such as investigations, and preventive and supportive services. For example, relaxation of gatekeeping may be a good strategy to improve health outcomes and patient satisfaction, but can potentially increase waiting time to secondary care.40,41
Difficulties in comparing studies and healthcare systems make it hard to draw firm conclusions from these results about the impact of gatekeeping on the outcomes examined. In particular, the long-term impact on quality of care and health outcomes remains unclear. Further studies are required to understand the impact of gatekeeping arrangements on these factors.
Continued financial and logistical challenges for healthcare systems mean that a model with potential to reduce healthcare use and expenditure while potentially improving quality of care is highly attractive. Consequently, primary care gatekeeping remains embedded in the culture of health care in many countries, including the UK. However, as this review demonstrates, the evidence of its impact on healthcare systems and patients remains far from clear and is complicated by the heterogeneity of systems and studies. Although gatekeeping may be associated with a reduction in specialist healthcare use and resulting financial benefits, a possible association with delayed diagnosis, particularly in the context of cancer care, is of significant concern. Although further research into longer-term patient- and health-related outcomes of gatekeeping would be of value, policymakers should perhaps focus more on collaborative efforts in primary and secondary care, aiming for a more unified approach to patient care.
Acknowledgments
The authors wish to thank Rebecca Jones, a specialist librarian, for her support in setting up the search strategy and retrieving the search results.
Funding
This research was supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care Northwest London (CLAHRC NWL). The views expressed in this article are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care. Poompong Sripa was supported by the Prince Mahidol Award Youth Programme. The funders have no role in shaping or drafting the manuscript.
Ethical approval
Ethical approval was not required for this study.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Loudon I. The principle of referral: the gatekeeping role of the GP. Br J Gen Pract. 2008. [DOI] [PMC free article] [PubMed]
- 2.Pati S, Shea S, Rabinowitz D, Carrasquillo O. Health expenditures for privately insured adults enrolled in managed care gatekeeping versus indemnity plans. Am J Public Health. 2005;95(2):286–291. doi: 10.2105/AJPH.2002.013466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greenfield G, Foley K, Majeed A. Rethinking primary care’s gatekeeper role. BMJ. 2016;354:i4803. doi: 10.1136/bmj.i4803. [DOI] [PubMed] [Google Scholar]
- 4.Velasco Garrido M, Zentner A, Busse R. The effects of gatekeeping: a systematic review of the literature. Scand J Prim Health Care. 2011;29(1):28–38. doi: 10.3109/02813432.2010.537015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hawkes N. The role of NHS gatekeeping in delayed diagnosis. BMJ. 2014;348:g2633. doi: 10.1136/bmj.g2633. [DOI] [PubMed] [Google Scholar]
- 6.Richards MA. The size of the prize for earlier diagnosis of cancer in England. Br J Cancer. 2009;101(Suppl 2):S125–S129. doi: 10.1038/sj.bjc.6605402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 6 [updated September 2018. 2011. https://training.cochrane.org/handbook (accessed 13 Feb 2019)
- 8.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cochrane Effective Practice and Organisation of Care (EPOC) EPOC resources for review authors. 2017. http://epoc.cochrane.org/epoc-specific-resources-review-authors (accessed 12 Feb 2019)
- 10.Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institute of Health. National Heart, Lung, and Blood Institute Study Quality Assessment Tools. Quality assessment tool for observational cohort and cross-sectional studies. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed 18 Mar 2019)
- 12.Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005;10(Suppl 1):6–20. doi: 10.1258/1355819054308576. [DOI] [PubMed] [Google Scholar]
- 13.Phillips KA, Haas JS, Liang SY, et al. Are gatekeeper requirements associated with cancer screening utilization? Health Serv Res. 2004;39(1):153–178. doi: 10.1111/j.1475-6773.2004.00220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mitchell A, Keenan RA. Are Grampian general practitioners good gatekeepers for access to emergency general surgical care? Scott Med J. 2008;53(3):33–35. doi: 10.1258/RSMSMJ.53.3.33. [DOI] [PubMed] [Google Scholar]
- 15.Vedsted P, Olesen F. Are the serious problems in cancer survival partly rooted in gatekeeper principles? An ecologic study. Br J Gen Pract. 2011. [DOI] [PMC free article] [PubMed]
- 16.Hartzell TL, Shahbazian JH, Pandey A, et al. Does the gatekeeper model work in hand surgery? Plast Reconstr Surg. 2013;132(3):381e–386e. doi: 10.1097/PRS.0b013e31829acc74. [DOI] [PubMed] [Google Scholar]
- 17.Ferris TG, Chang Y, Perrin JM, et al. Effects of removing gatekeeping on specialist utilization by children in a health maintenance organization. Arch Pediatr Adolesc Med. 2002;156(6):574–579. doi: 10.1001/archpedi.156.6.574. [DOI] [PubMed] [Google Scholar]
- 18.Ferris TG, Chang Y, Blumenthal D, Pearson SD. Leaving gatekeeping behind: effects of opening access to specialists for adults in a health maintenance organization. N Engl J Med. 2001;345(18):1312–1317. doi: 10.1056/NEJMsa010097. [DOI] [PubMed] [Google Scholar]
- 19.Escarce JJ, Kapur K, Joyce GF, Van Vorst KA. Medical care expenditures under gatekeeper and point-of-service arrangements. Health Serv Res. 2001;36(6 Pt 1):1037–1057. [PMC free article] [PubMed] [Google Scholar]
- 20.Tye S, Phillips KA, Liang SY, Haas JS. Moving beyond the typologies of managed care: the example of health plan predictors of screening mammography. Health Serv Res. 2004;39(1):179–206. doi: 10.1111/j.1475-6773.2004.00221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Linden M, Gothe H, Ormel J. Pathways to care and psychological problems of general practice patients in a ‘gate keeper’ and an ‘open access’ health care system: a comparison of Germany and the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2003;38(12):690–697. doi: 10.1007/s00127-003-0684-6. [DOI] [PubMed] [Google Scholar]
- 22.Ferris TG, Perrin JM, Manganello JA, et al. Switching to gatekeeping: changes in expenditures and utilization for children. Pediatrics. 2001;108(2):283–290. doi: 10.1542/peds.108.2.283. [DOI] [PubMed] [Google Scholar]
- 23.Haggstrom DA, Phillips KA, Liang SY, et al. Variation in screening mammography and Papanicolaou smear by primary care physician specialty and gatekeeper plan (United States) Cancer Causes Control. 2004;15(9):883–892. doi: 10.1007/s10552-004-1138-5. [DOI] [PubMed] [Google Scholar]
- 24.Joyce GF, Kapur K, Van Vorst KA, Escarce JJ. Visits to primary care physicians and to specialists under gatekeeper and point-of-service arrangements. Am J Manag Care. 2000;6(11):1189–1196. [PubMed] [Google Scholar]
- 25.Schneider A, Donnachie E, Tauscher M, et al. Costs of coordinated versus uncoordinated care in Germany: results of a routine data analysis in Bavaria. BMJ Open. 2016;6(6):e011621. doi: 10.1136/bmjopen-2016-011621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroneman MW, Maarse H, van der Zee J. Direct access in primary care and patient satisfaction: a European study. Health Policy. 2006;76(1):72–79. doi: 10.1016/j.healthpol.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Pati S, Shea S, Rabinowitz D, Carrasquillo O. Does gatekeeping control costs for privately insured children? Findings from the 1996 medical expenditure panel survey. Pediatrics. 2003;111(3):456–460. doi: 10.1542/peds.111.3.456. [DOI] [PubMed] [Google Scholar]
- 28.Delnoij D, Van Merode G, Paulus A, Groenewegen P. Does general practitioner gatekeeping curb health care expenditure? J Health Serv Res Policy. 2000;5(1):22–26. doi: 10.1177/135581960000500107. [DOI] [PubMed] [Google Scholar]
- 29.Schwenkglenks M, Preiswerk G, Lehner R, et al. Economic efficiency of gatekeeping compared with fee for service plans: a Swiss example. J Epidemiol Community Health. 2006;60(1):24–30. doi: 10.1136/jech.2005.038240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kapur K, Joyce GF, Van Vorst KA, Escarce JJ. Expenditures for physician services under alternative models of managed care. Med Care Res Rev. 2000;57(2):161–181. doi: 10.1177/107755870005700202. [DOI] [PubMed] [Google Scholar]
- 31.Rask KJ, Deaton C, Culler SD, et al. The effect of primary care gatekeepers on the management of patients with chest pain. Am J Manag Care. 1999;5(10):1274–1282. [PubMed] [Google Scholar]
- 32.Schillinger D, Bibbins-Domingo K, Vranizan K, et al. Effects of primary care coordination on public hospital patients. J Gen Intern Med. 2000;15(5):329–336. doi: 10.1046/j.1525-1497.2000.07010.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Halm EA, Causino N, Blumenthal D. Is gatekeeping better than traditional care? A survey of physicians’ attitudes. JAMA. 1997;278(20):1677–1681. [PubMed] [Google Scholar]
- 34.Forrest CB, Shi L, von Schrader S, Ng J. Managed care, primary care, and the patient–practitioner relationship. J Gen Intern Med. 2002;17(4):270–277. doi: 10.1046/j.1525-1497.2002.10309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Franco SM, Mitchell CK, Buzon RM. Primary care physician access and gatekeeping: a key to reducing emergency department use. Clin Pediatr (Phila) 1997;36(2):63–68. doi: 10.1177/000992289703600201. [DOI] [PubMed] [Google Scholar]
- 36.Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Office for National Statistics UK health accounts: 2015 Healthcare expenditure statistics, produced to the international definitions of the System of Health Accounts 2011. 2017. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthcaresystem/bulletins/ukhealthaccounts/2015 (accessed 18 Mar 2019)
- 38.Kulu-Glasgow I, Delnoij D, de Bakker D. Self-referral in a gatekeeping system: patients’ reasons for skipping the general-practitioner. Health Policy. 1998;45(3):221–238. doi: 10.1016/s0168-8510(98)00045-1. [DOI] [PubMed] [Google Scholar]
- 39.Braun BL, Fowles JB, Forrest CB, et al. Which enrollees bypass their gatekeepers in a point-of-service plan? Med Care. 2003;41(7):836–841. doi: 10.1097/00005650-200307000-00007. [DOI] [PubMed] [Google Scholar]
- 40.Barrett J, Jiwa M, Rose P, Hamilton W. Pathways to the diagnosis of colorectal cancer: an observational study in three UK cities. Fam Pract. 2006;23(1):15–19. doi: 10.1093/fampra/cmi093. [DOI] [PubMed] [Google Scholar]
- 41.Royal College of General Practitioners National audit of cancer diagnosis in primary care. http://www.rcgp.org.uk/policy/rcgp-policy-areas/national-audit-of-cancer-diagnosis-in-primary-care.aspx (accessed 18 Mar 2019)
- 42.Brown S, Castelli M, Hunter DJ, et al. How might healthcare systems influence speed of cancer diagnosis: a narrative review. Soc Sci Med. 2014;116:56–63. doi: 10.1016/j.socscimed.2014.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Harris M, Frey P, Esteva M, et al. How the probability of presentation to a primary care clinician correlates with cancer survival rates: a European survey using vignettes. Scand J Prim Health Care. 2017;35(1):27–34. doi: 10.1080/02813432.2017.1288692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hamilton W. Five misconceptions in cancer diagnosis. Br J Gen Pract. 2009. [DOI] [PMC free article] [PubMed]
- 45.Lyratzopoulos G, Vedsted P, Singh H. Understanding missed opportunities for more timely diagnosis of cancer in symptomatic patients after presentation. Br J Cancer. 2015;112(Suppl 1):S84–S91. doi: 10.1038/bjc.2015.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abel GA, Mendonca SC, McPhail S, et al. Emergency diagnosis of cancer and previous general practice consultations: insights from linked patient survey data. Br J Gen Pract. 2017. [DOI] [PMC free article] [PubMed]