Summary:
Improving understanding of and outcomes for Early Course Psychosis (ECP) is a recognized global mental health priority. We argue digital health technologies can advance care for ECP by better accounting for clinical heterogeneity, offering better predictive models, increasing access to early interventions, and enhancing existing treatment options.
Keywords: schizophrenia, mHealth, mobile health technology, clinical services, community mental health
Improving outcomes for Early Course Psychosis (ECP) is a recognized global mental health priority. This effort faces four key challenges: 1) accounting for and addressing heterogeneity of clinical presentation, 2) a need for better modeling of illness trajectories, 3) access and availability of early intervention, and 4) a need for new pathways to enhance utilization of existing treatments. Although there is no panacea, any solution must be scalable and cost effective to meet the global mental health need. We suggest that digital health technology-based solutions using smartphones - the swiss army knife of the 21st Century - offer a viable and scalable avenue for advancing ECP care.
Contrary to popular belief, individuals experiencing psychosis use smartphones as part of their daily life (1) and are keen to incorporate them into their treatment (2). Importantly, ECP individuals - those in the first few years of psychotic illness - are typically younger individuals raised in an increasingly digital world who are interested in technology enabled services for medication monitoring, psychoeducation, clinical scheduling, information on recovery (2), and psychosocial treatment (3). Case reports of individuals using smartphone applications (“apps”) to supplement CBT for psychosis (4) and to track auditory hallucinations(5), coupled with data indicating up to 40% of individuals with schizophrenia use their smartphone or computers to play music to block auditory hallucinations (1) underscore that ECP individuals are not waiting for the clinical community to sanction the use of digital technology in care. While not all younger people have smartphones, national data in the US suggests a mean of 94% smartphone ownership for those age 18–29 compared to 77% for the total population (6). Data on smartphone ownership and use for mental health in ECP remains scarce although small survey studies offer ownership estimates of 70% and higher (7, 8). With this generation-wide access, interest, and early adoption already occurring, the evidence suggests that today’s ECP individuals may be ready to use smartphone apps and sensors in their care.
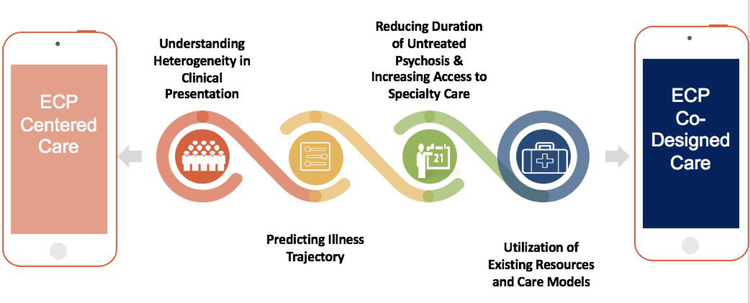
Here, as outlined in figure one, we discuss evidence to-date indicating how smartphone and related digital health technologies can advance care for ECP by better accounting for clinical heterogeneity, offering better predictive models, increasing access to early interventions, and enhancing existing treatment options. While not a comprehensive review, we underscore the potential of this growing space, acknowledge barriers to technology adoption, and offer some solutions.
Figure 1:
While no single technology or app will transform any of the fours domains necessary towards improving ECP care, the synergy of digital tools to connect domains and complement both care and research offers potential.
Understanding Heterogeneity in Clinical Presentation
Smartphones and related digital technologies offer a new strategy to approach heterogeneity of clinical presentation and produce a more personalized understanding of psychotic illness. While hallucinations and unusual thoughts/delusions are characteristic of ECP, they are also present in other illnesses and are non-specific to psychotic disorders (8). Indeed, the value of the term schizophrenia itself has been called into question as it becomes clear there is no discrete entity or single syndrome (9). Understanding this heterogeneity requires a better understanding of not only the clinical presentation of ECP, but also the lived experience. Smartphones and other wearable devices (e.g., smartwatches, fitness trackers) can now capture ecologically-valid data in real-time on key behavioral and functional indicators, including: ecological momentary assessment (EMA) data regarding symptoms and daily experiences via self-report surveys, physical activity and physiology data (e.g., heart rate, step counts), patterns of daily life like attending work and daily mobility/distance travelled, and social outcomes such as phone call and text message reciprocity. Recent work on digital phenotyping - the “moment- by-moment quantification of the individual-level human phenotype in situ, using data from personal devices such as mobile phones” - offers a practical means to achieve this. Data show that capturing spatial trajectories through GPS and social networking through call/text logs from the personal devices of those with psychotic disorders does not increase paranoia or cause known harm (10). Rather this data offers potential insights into how symptom clusters may drive clinical presentations such as social withdrawal and social anhedonia via changes in call/text reciprocity, or avolition and lethargy via changes in movement tracked through GPS in ECP(11). This wealth of easily accessible, and often automatically collected information, offers a new lens to better characterize the lived experience of those with ECP and explore new subtypes and clusters of psychosis based on new data.
Just as recent research has utilized biomarker panels including neuropsychological, stop signal, saccadic control, and evoked response paradigm metrics to identify three neurobiologically distinct psychosis biotypes (12) - smartphones offer a complementary stream of data to transform clinical heterogeneity into unique social, functional, cognitive, and physiological domains that previously have been difficult to capture or quantify.
Predicting Illness Trajectory
A long-recognized holy grail of ECP research is the ability to accurately predict illness trajectory to facilitate early intervention and prevent bad outcomes. This includes accurate prediction of: 1)-psychosis onset from a high-risk state, 2)-relapse of psychotic symptoms, and 3)-individual differences in long-term outcomes. To date, success in these three domains has been limited: only 20% to 40% of individuals identified at high-risk go on to develop a psychotic disorder (13), tools for understanding long-term outcomes are typically dichotomous and may miss important individual differences, and although there are known relapse predictors (e.g., early signs of symptom exacerbation), prediction in service of prevention is limited by a lack of real-time actionable data. It is now understood that a finegrained understanding of racial, ethnic, diversity, and social characteristics of an individuals’ environment is critical (14). Smartphones and related wearable technologies offer a feasible and scalable method to capture day-to-day fluctuations in environmental, physiological, and social indicators necessary to better understand, model, and predict illness trajectory. Preliminary data support this: Latent semantic analysis of speech samples captured via smartphone resulted in 72% accurate prediction of conversion to psychosis (15) - a significant improvement from current models, and a scalable method given the ubiquity of smartphones for capturing speech samples. For relapse prediction, longitudinal data demonstrates that monitoring relapse predictors via smartphone is feasible in ECP individuals, and that self-report surveys via smartphone are a viable and valid method for monitoring signs of relapse (16). Further, a recent pilot study suggests that two weeks prior to relapse individuals with schizophrenia demonstrate significant changes in mobility indicators derived from GPS data, sociability indicators derived from text message and call data, and symptom exacerbation indicators derived from in-app self-report surveys - indicating that we may be able to capture digital indicators of relapse with minimal burden on the individual (17). Novel technologies for monitoring medication adherence - a primary risk factor for relapse - are also emerging. In 2017, the pharmaceutical company Otsuka received FDA marketing approval for a new formulation of Aripiprazole that uses a sensor to monitors ingestion via sending a signal when the medication is in the stomach. This “digital pill” offers a low burden method for ECP individuals and providers to monitor medication adherence and problem solve non-adherence quickly to prevent relapse. Although research on predicting illness trajectory using digital technology is still in its infancy, data gathered to date support feasibility and validity, and suggest that leveraging smartphone and related wearable/sensor technologies to create data-rich models of day-to-day fluctuations in symptoms and functioning could facilitate the identification of “digital biomarkers” for ECP (10).
Reducing Duration of Untreated Psychosis & Increasing Access to Specialty Care
A prolonged duration of untreated psychosis (DUP) predicts further disability, relapse, and a higher cost of treatment over time (13). Reducing DUP requires both improved early identification and increased access to specialty care - smartphones and associated digital health tools could ameliorate both issues. For example, technology-enhanced population level screening for psychosis and automatic referral to specialty care could potentially increase early identification rates and reduce DUP. Indeed, recent reports of technology facilitated psychosis screening in schools and community health centers demonstrates high levels of acceptability with 75% of staff noting it did not increase their workload (18). Beyond early identification, preliminary feasibility and acceptability data across international settings indicate smartphone and web-based care options could also address barriers related to access to, engagement with, and continuity of ECP care. In the United States, PRIME, a smartphone and web-based peer-to-peer intervention platform for improving motivation and quality of life in ECP individuals, showed high feasibility and acceptability in preliminary testing (19). A subsequent study demonstrated that those who rarely used PRIME benefited as much as those with regularly engaged with the app, suggesting a lack of a dose effect (20). Promising pilot data have been reported for MOST, a web-based peer-to-peer intervention platform developed in Australia for improving social functioning in youth at risk for psychosis (21). Newer technologies also promise to increase access to early interventions. Research on those at high risk for psychosis and with ECP has found virtual reality interventions to be both acceptable and feasible, without adverse events such as worsening paranoia or delusions (22). While virtual reality headsets are not commonly owned today, the rapid global rise of smartphone ownership exemplifies the scalability of digital tools. These data are promising and suggest that ECP individuals in areas with no brick-and-mortar specialty care programs will be willing and able to access evidence-based treatments at scale via digital technology, independent of traditional care settings.
Utilization of Existing Resources and Care Models
Even with access to existing specialized care, up to 40% of those with ECP may disengage with services despite continued clinical needs (23). While apps are not a panacea, they can be integrated into existing care settings to offer the ECP community new tools and means to engage with care. Recent work indicates that integrating a digital technology platform in community-based ECP is feasible and perceived as valuable by clients and providers alike (24). Similarly, the Heal Your Mind app, designed for cognitive behavioral case management and symptom monitoring in ECP, has been well received by users in pilot studies (25). Preliminary efficacy data are also emerging: the app WellWave was successfully integrated into an early psychosis program to boost levels of physical activity and help users better connect with peer staff (26), and a recent study pitting two apps against treatment as usual in the U.K. indicates positive treatment effects on negative, positive, and mood symptoms (27).
Between both clinically integrated apps and self-care resources, technology-based solutions offer new avenues to increase utilization and augment existing mental health resources for ECP. New care models that take full advantage of these technologies while still preserving the clinical therapeutic relationship necessary to fully utilize these tools may be a new horizon for the optimal utilization of these apps. The ECP digital clinic models in development at Beth Israel Deaconess Medical Center (28) and piloting at UC Davis (16, 24) are examples of this novel pathway to augment and extend the impact of existing specialized care services.
Barriers
Despite these promising preliminary feasibility, acceptability, and efficacy data, three key implementation issues face the field of digital health technology in ECP care: implementation logistics, implementation costs, user-engagement and ethical issues. Logistics are particularly relevant for tools implemented as part of traditional care settings. To date, the majority of feasibility studies have been conducted in academic research settings that do not emulate real-world clinical environments. For successful dissemination in ECP care settings, the practicalities of technical support, training clinical and administrative staff, and the necessary infrastructure for data management and analysis must be addressed. This may require new partnerships between health systems and technology companies and begs the question of the second implementation issue - implementation costs. To date studies of smartphone apps for psychotic disorders have not reported cost effectiveness data. Although smartphones offer the potential to deliver scalable lower cost services, implementation still requires investment to provide smartphones (as necessary), technical support, data storage and analysis, and technology upgrades. For health systems to widely adopt digital health tools, there must be clear cost savings, either in the form of reduced cost of care as a consequence of relapse prevention or as a consequence of increased capacity to serve those in need. These technologies must be designed to be engaging as services delivered via an app will quickly loose users to dropout; app-based services that do not utilize healthcare interoperability standards for apps to transfer data to and from electronic medical records risk low engagement from the provider side. Involvement of both ECP clients and ECP care providers during product design is necessary to ensure the development of engaging digital health tools that enhance ECP care and outcomes.
Digital technology tools also raise important ethical issues regarding informed consent, privacy, and responsible data use. Recent high-profile data breaches from large social media corporations in which user data were sold to third-party corporations without user informed consent have raised suspicion amongst users and highlights the need for clear and ethical data use and privacy practices. This is particularly important when vulnerable populations and private health information are involved. Standard End User License Agreements (EULA), typically several pages long and dense with legalese, are not effective tools for informed consent and predominantly serve to protect the company but not the user. This is problematic in the case of digital health tools involving collection of massive amounts of personal data (e.g., voice and text analysis, GPS identifying where the person sleeps at night). While the purpose of this close monitoring is to improve ECP outcomes and empower ECP individuals in their care, there is also potential risk of harm from a data breach or legal subpoena. The digital health technology field should be held to the highest standards of informed consent and privacy practices and must proactively address key questions regarding data ownership and third-party data use to avoid misuse and abuse of vulnerable populations’ data. At minimum, we recommend comprehension checks for EULA and explicit agreement options for specific types of data sharing, rather than a catch-all agreement option. Importantly, treatment provision must not be contingent on an individual agreeing to digital health monitoring as this could disproportionately affect those who are most vulnerable. Other unintended consequences of digital health technology should be considered in order to build appropriate safeguards against later reuse of data for insurance coverage, employment decisions, or marketing.
An equally pressing issue is informed consent in the digital age and willingness of patients to use digital phenotyping apps outside of research studies and actually as part of care. As remote clinical studies, in which ECP individuals partake in research without ever meeting the research team, become feasible (20) it remains unclear how to ensure participants understand the risks and benefits. Research outside of ECP suggests that those with lower health literacy are more likely to have positive perceptions of the privacy afforded by health technologies, suggesting they may underestimate the risks (29). Conversely, recent survey data suggests that those with mental health disorders, including psychosis, are least comfortable sharing automatically collected GPS, phone audio, and phone text message data (30, 31). This suggests the importance of a patient-centered approach, in which the digital health technology field must work closely with ECP individuals from the inception of any digital health technology project to ensure data is collected and used in manners all stakeholders understand and agree upon.
Conclusions
Whilst digital health technology shows high feasibility and acceptability for advancing ECP care, technology alone is not a panacea. Important questions remain regarding the efficacy, privacy, usability, and stability of digital health tools. These questions would likely be best addressed via academic research and technology industry partnerships, which will in turn require a solution to the mismatched incentive structures that can impede productive and ethical collaborations.
However, we argue that these are questions worth addressing. The enormous potential and scalability of digital health technology offers an unparalleled opportunity to approach the challenge of improving ECP care with a new lens, new methods, and new interventions.
Acknowledgments
This work was supported by a Building Interdisciplinary Research Careers in Women’s Health award (K12 HD051958) awarded to LMT, funded by the National Institute of Child Health and Human Development (NICHD), Office of Research on Women’s Health, Office of Dietary Supplements, and the National Institute of Aging. JT is supported by a NIMH Career Development Award (K23 MH116130–01), a NARSAD Young Investigator Award from the Brain & Behavior Research Foundation, and the Natalia Mental Health Foundation.
Footnotes
Declaration of Interest
Dr. Tully owns shares in Safari Health Inc. - a digital health technology company. The authors declare no other potential sources of conflict of interest.
Contributor Information
John Torous, Department of Psychiatry, Beth Israel Deaconess Medical School, Harvard Medical School, Boston, MA, 02115, USA,
Jessica Woodyatt, Department of Psychology, University of Rochester, 233 Meliora Hall, Rochester NY, USA
Matcheri Keshavan, Department of Psychiatry, Beth Israel Deaconess Medical School, Harvard Medical School, Boston, MA, 02115, USA
Laura M. Tully, Department of Psychiatry, University of California, Davis., UC Davis Imaging Research Center, 4701 X Street, Sacramento CA 95817, USA
References
- 1.Gay K, Torous J, Joseph A, Pandya A, Duckworth K. Digital Technology Use Among Individuals with Schizophrenia: Results of an Online Survey. JMIR Mental Health 2016;3(2):e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lal S, Dell’Elce J, Tucci N, Fuhrer R, Tamblyn R, Malla A. Preferences of Young Adults With First-Episode Psychosis for Receiving Specialized Mental Health Services Using Technology: A Survey Study. JMIR Mental Health 2015;2(2):e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lal S, Nguyen V, Theriault J. Seeking mental health information and support online: experiences and perspectives of young people receiving treatment for first-episode psychosis. Early intervention in psychiatry. 2016. [DOI] [PubMed] [Google Scholar]
- 4.Sandoval LR, Torous J, Keshavan MS. Smartphones for Smarter Care? SelfManagement in Schizophrenia. American Journal of Psychiatry. 2017;174(8):725–8. [DOI] [PubMed] [Google Scholar]
- 5.Torous J, Roux S. Patient-Driven Innovation for Mobile Mental Health Technology: Case Report of Symptom Tracking in Schizophrenia. JMIR mental health 2017;4(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pew Research Center: Internet, Science & Tech. (2018). Demographics of Mobile Device Ownership and Adoption in the United States. [online] Available at: http://www.pewinternet.org/fact-sheet/mobile/ [Accessed 11 Nov. 2018]. [Google Scholar]
- 7.Lal S, Dell’Elce J, Tucci N, Fuhrer R, Tamblyn R, Malla A. Preferences of young adults with first-episode psychosis for receiving specialized mental health services using technology: a survey study. JMIR mental health 2015. April;2(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waters F, Fernyhough C. Hallucinations: a systematic review of points of similarity and difference across diagnostic classes. Schizophrenia bulletin 2017;43(1):32–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray RM. Mistakes I have made in my research career. Schizophrenia bulletin. 2017;43(2):253–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torous J, Staples P, Onnela J-P. Realizing the potential of mobile mental health: new methods for new data in psychiatry. Current psychiatry reports. 2015;17(8):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Torous J, Staples P, Barnett I, Sandoval LR, Keshavan M, Onnela J-P. Characterizing the clinical relevance of digital phenotyping data quality with applications to a cohort with schizophrenia. npj Digital Medicine. 2018;1(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clementz BA, Sweeney JA, Hamm JP, Ivleva EI, Ethridge LE, Pearlson GD, et al. Identification of distinct psychosis biotypes using brain-based biomarkers. American Journal of Psychiatry. 2015;173(4):373–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fusar-Poli P, McGorry PD, Kane JM. Improving outcomes of first-episode psychosis: an overview. World Psychiatry. 2017;16(3):251–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richardson L, Hameed Y, Perez J, Jones PB, Kirkbride JB. Association of environment with the risk of developing psychotic disorders in rural populations: findings from the social epidemiology of psychoses in East Anglia study. JAMA psychiatry. 2018;75(1):75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corcoran CM, Carrillo F, Fernandez-Slezak D, Bedi G, Klim C, Javitt DC, et al. Prediction of psychosis across protocols and risk cohorts using automated language analysis. World Psychiatry. 2018;17(1):67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Niendam TA, Tully LM, Iosif A-M, Kumar D, Nye KE, Denton JC, et al. Enhancing early psychosis treatment using smartphone technology: A longitudinal feasibility and validity study. Journal of Psychiatric Research. 2018;96(Supplement C):239–46. [DOI] [PubMed] [Google Scholar]
- 17.Barnett I, Torous J, Staples P, Sandoval L, Keshavan M, Onnela J-P. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Savill M, Skymba HV, Ragland JD, Niendam T, Loewy RL, Lesh TA, et al. Acceptability of Psychosis Screening and Factors Affecting Its Implementation: Interviews With Community Health Care Providers. Psychiatric Services. 2018;69(6):689–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schlosser D, Campellone T, Kim D, Truong B, Vergani S, Ward C, et al. Feasibility of PRIME: A Cognitive Neuroscience-Informed Mobile App Intervention to Enhance Motivated Behavior and Improve Quality of Life in Recent Onset Schizophrenia. JMIR Research Protocols. 2016;5(2):e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schlosser DA, Campellone TR, Truong B, Etter K, Vergani S, Komaiko K, Vinogradov S. Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia. Schizophrenia bulletin. 2018. June 22;44(5):1010–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rice S, Gleeson J, Leicester S, Bendall S, D’Alfonso S, Gilbertson T, et al. Implementation of the Enhanced Moderated Online Social Therapy (MOST+) Model Within a National Youth E-Mental Health Service (eheadspace): Protocol for a Single Group Pilot Study for Help-Seeking Young People. JMIR research protocols. 2018;7(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Canty AL, Neumann DL, Shum DHK. Using virtual reality to assess theory of mind subprocesses and error types in early and chronic schizophrenia. Schizophrenia Research: Cognition. 2017;10:15–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doyle R, Turner N, Fanning F, Brennan D, Renwick L, Lawlor E, et al. First- episode psychosis and disengagement from treatment: a systematic review. Psychiatric Services. 2014;65(5):603–11. [DOI] [PubMed] [Google Scholar]
- 24.Kumar D, Tully LM, Iosif A-M, Zakskorn LN, Nye KE, Zia A, et al. A Mobile Health Platform for Clinical Monitoring in Early Psychosis: Implementation in Community-Based Outpatient Early Psychosis Care. JMIR mental health. 2018;5(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim SW, Lee GY, Yu HY, Jung EI, Lee JY, Kim SY, et al. Development and feasibility of smartphone application for cognitive-behavioural case management of individuals with early psychosis. Early intervention in psychiatry. 2016. [DOI] [PubMed] [Google Scholar]
- 26.Macias C, Panch T, Hicks YM, Scolnick JS, Weene DL, Ongur D, et al. Using smartphone apps to promote psychiatric and physical well-being. Psychiatric Quarterly. 2015;86(4):505–19. [DOI] [PubMed] [Google Scholar]
- 27.Bucci S, Barrowclough C, Ainsworth J, Machin M, Morris R, Berry K, et al. Actissist: Proof-of-Concept Trial of a Theory-Driven Digital Intervention for Psychosis. Schizophrenia bulletin. 2018:sby032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Torous J, Hsin H. Empowering the digital therapeutic relationship: virtual clinics for digital health interventions. npj Digital Medicine. 2018;1(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mackert M, Mabry-Flynn A, Champlin S, Donovan EE, Pounders K. Health literacy and health information technology adoption: the potential for a new digital divide. Journal of medical Internet research. 2016. 0ct;18(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Di Matteo D, Fine A, Fotinos K, Rose J, Katzman M. Patient Willingness to Consent to Mobile Phone Data Collection for Mental Health Apps: Structured Questionnaire. JMIR Mental Health 2018;5(3):e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Torous J, Wisniewski H, Liu G, Keshavan M Mental Health Mobile Phone App Usage, Concerns, and Benefits in Two Distinct Urban Outpatient Psychiatry Clinics: Comparative Survey Study JMIR Mental Health 2018;5(4):e11715. [DOI] [PMC free article] [PubMed] [Google Scholar]