Abstract
Purpose:
Federally Qualified Health Centers (FQHCs), which were expanded under the Affordable Care Act, are federally funded health centers that aim to improve access to primary care in underserved areas. With continued federal support, the number of FQHCs in the U.S. has increased >80% within a decade. However, the expansion patterns and their impact on the population served are unknown.
Methods:
A pre (2007)-post (2014) study of FQHC locations. FQHC locations were identified from the Provider of Services Files then linked to primary care service areas (PCSAs), which represent the service markets that FQHCs served. Road-based travel time was estimated from each 2007 FQHC to the nearest new FQHC as an indicator of geographic expansion in access. PCSA-level characteristics were used to compare 2007 and 2014 FQHC service markets.
Findings:
Between 2007 and 2014, there was greater expansion in the number of FQHCs (3,489 vs. 6,376; 82.7%) than in the number of service markets (1,835 vs. 2,695; 46.9%). Nearly half of 2007 FQHCs (47%) had at least one new FQHC within 30 minutes travel time. Most newly certified FQHCs (81%) were located in urban areas. Compared to 2007 service markets, the new 2014 markets (N=174) were much less likely to be in areas with >20% of the population below poverty (31.4% vs. 14.9%, P < .001).
Conclusions:
The latest expansion of FQHCs were less likely in rural or high poverty areas, suggesting the impact of expansion may have limitations in improving access to care among the most financially disadvantaged populations.
Keywords: Federally Qualified Health Centers, access, primary care, underserved
INTRODUCTION
For decades, policymakers and researchers have advocated for an effective and efficient health care delivery system that is focused on primary care.1–3 Many health care reforms and program delivery strategies have adopted the concept of a primary care centered approach and emphasized that adequate access to primary care is a fundamental condition for receiving appropriate care and improving population health.1,2,4–8 Ensuring adequate access to primary care is particularly important for areas with limited health care resources. There are many strategies in addition to increasing insurance coverage that could increase access to primary care in underserved areas, such as providing transportation to medical appointments, extending office hours to evenings or weekends, recruiting additional providers, and establishing heath centers where needed most.9
The Federally Qualified Health Center (FQHC) program is one such strategy that was established under the Omnibus Budget Reconciliation Act of 1989 to enhance care provision in underserved areas through special payment arrangements with Medicare and Medicaid.10 Although the health center program started in 1965,11 the FQHC program specifically aims to provide quality primary care for populations in underserved areas by supporting the establishment and funding of several types of clinics including community health centers, migrant health centers, health care for the homeless health centers, public housing primary care centers, health center program “look-alikes” (not receiving a grant under Section 330 of the Public Health Service Act), and outpatient health programs or facilities operated by a tribe or tribal organization or by an urban Indian organization.12 Over the past 30 years, many federal initiatives have provided financial investments to support FQHCs such as the Health Center Growth Initiative in 2002.13 Through recent federal investments in FQHCs, as part of the 2009 American Recovery and Reinvestment Act and the $11 billion Community Health Center Fund under the 2010 Affordable Care Act (ACA),14 the number of FQHC sites in the U.S. has increased to more than 8,000 and about 1 out of every 13 people in the U.S currently receive services from health centers like FQHCs.15,16
In addition to infrastructure support, the federal government also provides payment support for FQHCs providing services under both Medicare and Medicaid. Even though Medicaid is the largest source of FQHC revenue, the financial incentives in Medicare make FQHC status attractive by paying higher per visit fees to FQHCs than to other primary care providers, which may be related to the expansion in FQHCs.17 In 2011, under the original all-inclusive per visit payment system, the Medicare per visit payment to FQHCs was $109.24 in rural areas and $126.22 in urban areas, compared to $68.97 to non-FQHC providers.17 Under the ACA, Medicare transitioned FQHC payment to a Prospective Payment System (PPS) in October 2014. The new PPS includes an additional 34% payment for FQHCs providing preventive services or seeing new Medicare patients.18 In 2009, only 7.4% of 18.8 million people served by FQHCs were Medicare beneficiaries, but as the U.S. population ages, it is anticipated that FQHCs will care for more elderly Medicare beneficiaries.19 Between 2005 and 2014, the greatest increase in FQHC patients by age was those nearing Medicare eligibility (age 55–64; 132%), followed by those aged 65–74 (92%).19 Thus, in the coming years, FQHCs will have substantial impact on the care of our growing vulnerable elderly population, which will include managing multiple chronic conditions.17,20 Understanding how the confluence of incentives have influenced where FQHCs locate is important for making further revisions to policy that will increase access in the most needy areas.
To become certified as an FQHC, either as an entirely new delivery site or by making an existing health center eligible for the FQHC financial support, requires a grant application to the Health Resources and Services Administration (HRSA) Health Center Program. Grantees can operate multiple delivery sites. Examination of the expansion of FQHCs to date has been limited to examining grantees, rather than delivery sites, because the currently available dataset from HRSA, the uniform data system (UDS), is organized by grantee rather than service site. One important question about the expansion of FQHCs is whether the newly certified sites are locating in areas where there is greatest need as determined by the geographic area they serve.
In this study, we set out to determine if the large increase in the number of FQHCs between 2007 and 2014 expanded access in geographic areas that may be deemed underserved based on more recent data (2010) characteristics. To do so, we 1) measured how far the nearest newly certified FQHC delivery site location from an existing 2007 FQHCs delivery site, and 2) whether newly certified FQHC delivery site locations increased the number of FQHC service markets, as well as population characteristics of new FQHC service markets compared to the 2007 FQHC service markets. We did not use Medically Underserved Areas defined by HRSA as FQHC service markets because Medically Underserved Areas vary in size, they can be a whole county, a group of neighboring counties, or a group of urban census tracts, or a group of county of civil divisions, and there is no available information about those areas’ care resources and health outcomes. Instead, we used primary care service areas (PCSAs), a geographical unit that divides the entire U.S. into primary care markets, as FQHC service markets.21,22 We hypothesized that as expansion continued with large federal financial support, the nearest newly certified FQHCs would be farther away (more than one hour travel time) from 2007 FQHCs, and the new FQHC service markets would appear as or more underserved compared to 2007 service markets based on population characteristics, healthcare resources, Medicare utilization, and mortality.
METHODS
Data Sources
Identify FQHCs from Provider of Service files
We used Provider of Services (POS) files 2007–2014 from the Centers for Medicare & Medicaid Services (CMS) to identify each FQHC.23 The POS files are publicly available data files, updated quarterly, that detail Medicare-approved health care facilities. Each record is for a service site including facility type, 5-digit ZIP Code of location, and unique facility identification number (ID) that can be linked to Medicare claims. CMS POS files include both FQHCs and FQHC look-alikes and each site is identified by its own delivery location rather than by the grantee location. The newly certified FQHCs enter the CMS system when they apply for Medicare and Medicaid payment.
We defined the year that a FQHC was certified by the year in the POS file where the FQHC’s ID was first found rather than the year the certification was issued by HRSA, which is not available in the POS file. FQHCs with a certification year after 2007 were categorized as newly certified FQHCs. To ensure a fair comparison between 2007 and 2014, we limited FQHCs to those that continued operating until 2014, which excluded only two FQHCs.
FQHC service market areas
We used primary care service areas (PCSAs v3.1, N=7,144) as the market units for FQHCs.24 PCSAs were developed under a project funded by HRSA to create local primary care markets for the entire U.S.21 The v3.1 PCSAs were developed by aggregating 2010 Census tracts into primary care service areas based on visit patterns to primary care providers among fee-for-service Medicare beneficiaries.22 Researchers have used PCSAs as primary care markets to study primary care associated outcomes, health care policy and program implementation.24–28 The PCSA v3.1 database includes population characteristics, primary care resources, and Medicare utilization. We linked each FQHC’s 5-digit ZIP Code from the POS file to the PCSA crosswalk file to identify each FQHC’s service market. Any PCSA containing at least one FQHC represented a FQHC service market (FQHC-PCSA). We used PCSA-level measures to describe the characteristics of FQHC service markets. We did not use Medically Underserved Areas (MUAs) as the FQHC market units because there is no available up-to-date information about each MUA’s population characteristics, primary care resources, or utilization.
Road-based travel time between a 2007 FQHC and the nearest new FQHC
To have more precise FQHC locations from which to calculate road-based travel time, ideally, we would use FQHCs’ street address; however, they were not available for this study. We did not use 5-digit ZIP Code because they can cover a large area; two FQHCs in the same 5-digit ZIP Code could be 30 minutes away from each other but have the same area centroid point leading to an estimated travel time of 0. Alternatively, we used census tracts as the geographic areas, which are the smallest geographic units used by MUAs. There are 74,134 tracts, compared to 34,000 5-digit ZIP Codes. We calculated road-based travel time between two census tract population centroids. If two FQHCs are in the same tract then they will be just a few blocks away.
We obtained FQHC census tract using a crosswalk file developed by the PCSA project and obtained its population centroid from the U.S. Census. We used the SAS Google Map application29 to calculate the road-based travel time between each 2007 FQHC’s tract location and any new FQHC’s tract location. We then selected the shortest travel time for each 2007 FQHC to the nearest newly certified FQHC as the travel time that represented the minimum geographic expansion. We categorized travel time as <=30 minutes, 31–60 minutes, and more than one hour. A 30-minute travel has been used by HRSA as a threshold for reasonable travel to primary care.22,30
To reduce computation requirements, we limited the calculation of travel time to tract pairs with a straight-line distance (SLD, line distance between two geographic points without accounting for structure and flexibility of road networks) shorter than 60 miles. We classified tract pairs with SLD >= 60 miles as “more than one hour” of travel time category. A 60-mile SLD almost certainly takes longer than 60 minutes travel time given travel time incorporates road-networks and speed limits.
Characteristics of FQHC service markets (FQHC-PCSAs)
The FQHC service market characteristics were obtained from the 2010 PCSA database, We included the variables that HRSA uses to calculate the underserved criteria: 1) primary care physician supply, 2) infant mortality, 3) proportion of population with income below poverty level, and 4) proportion of population aged 65 and older.31 We applied the same area characteristics for all study years.
We reported the proportion of FQHC service markets that were high poverty areas based on whether > 20% of the area population had an income below the poverty level. The threshold of 20% of population with income below poverty level has been widely accepted and used among social scientists, demographers, the Census Bureau and several previous studies to identify high poverty areas.24,32,33 We also reported alternative measures relevant for populations with difficulty accessing care—proportion of population with income 100%−200% of poverty level, median household income, proportion of families with income below poverty level and proportion of linguistically isolated households.31 Furthermore, we evaluated % black, % Hispanic, % uninsured and % in rural. In addition, we included measures of utilization (emergency department visits, and hospitalization for ambulatory care-sensitive conditions) and mortality that were available for the Medicare population. These utilization measures and mortality were not available on a population basis for Medicaid recipients, uninsured, or privately insured residents. Utilization and mortality measures were Medicare population-adjusted to account for area demographic (age, sex, race) differences. The primary care physician supply was adjusted for total population (age and race) differences.
Statistical Analysis
We first examined trends across years in the number of FQHCs as well as in the number of FQHC-PCSAs, and their characteristics. We then focused on the newly certified FQHCs and the new FQHC-PCSAs in three periods - before ACA enactment (2008–2010), during implementation (2011–2013), and complete implementation (2014).
For the travel time analysis, we examined the proportion of 2007 FQHCs with <= 30, 31–60, and > 60 minutes travel time to the nearest newly certified FQHC. To examine the characteristics of FQHC-PCSAs, we used the median instead of the mean to present area characteristics, because PCSAs are quite varied in size, and the Kruskal-Wallis test to examine the differences between years. For all outcome measures, a significance level of 0.05 was used. Statistical analysis was performed using SAS 9.3 (SAS Institute Inc., Cary, NC). The College Institutional Review Board approved this study.
RESULTS
FQHC-PCSAs vs. non-FQHC PCSAs
Because PCSAs have not previously been used to identify service markets for FQHCs, we first evaluated whether PCSAs with FQHC service sites had characteristics consistent with being underserved areas relative to PCSAs without FQHCs. By 2014 (Table 1), more than one-third of the 7,144 PCSAs (37.7%, N=2,695) contained at least one FQHC.
Table1.
Characteristics of FQHC-PCSAs vs. non FQHC-PCSAs
| Number of PCS As | FQHC-PCSAs 2,695 | Non-FQHC PCSAs 4,449 | |
|---|---|---|---|
| Characteristics1 | |||
| % Black | 4.4 | 1.6 | <0.001 |
| % Hispanic | 5.3 | 3.5 | <0.001 |
| % Rural population | 33.5 | 42.1 | <0.001 |
| % Age 65+ | 14.0 | 15.1 | <0.001 |
| Insurance coverage | |||
| % No insurance age <18 | 1.6 | 1.2 | <0.001 |
| % No insurance age 18–64 | 13.6 | 10.3 | <0.001 |
| Poverty/Income | |||
| % Population with income 100% below poverty level | 16.0 | 10.8 | <0.001 |
| % Population with income 100%−200% of poverty level |
21.4 | 18.4 | <0.001 |
| Median household income | $ 43,859 | $ 49,277 | <0.001 |
| % Family income below poverty level | 11.7 | 7.5 | <0.001 |
| % Linguistically isolated households | 8.9 | 7.5 | <0.001 |
| % PCS As as high poverty2 areas | 27.9 | 11.8 | <0.001 |
| Mortality | |||
| Infant per 1,000 live births | 6.4 | 6.2 | 0.887 |
| Total Medicare (%) | 4.8 | 4.7 | <0.001 |
| Fee-for-service Medicare (%) | 5.1 | 4.9 | <0.001 |
| Medicare Advantage (%) | 3.5 | 2.9 | <0.001 |
| Primary care physicians per 100,000 | 70.0 | 73.1 | <0.001 |
| Medicare utilization | |||
| % Beneficiaries with primary care visits | 80.6 | 81.4 | <0.001 |
| % Beneficiaries with emergency department visits | 27.1 | 25.6 | <0.001 |
| Primary care visit rate | 3.9 | 3.8 | <0.001 |
| Emergency department visit rate | 0.5 | 0.5 | <0.001 |
| Hospitalization for ambulatory care sensitive conditions, per 1,000 | 69.6 | 66.5 | <0.001 |
Median value except % PCSAs as high poverty areas
High poverty: > 20% of area population living below the federal poverty line
Wilcoxon Score (Kruskal-Wallis Test) or Chi-Square test as appropriate
Compared to non-FQHC PCSAs (N=4,449), FQHC-PCSAs were more likely to be high poverty areas (27.9% vs. 11.8%) and with higher proportions of disadvantaged populations: minority populations (black: 4.4% vs. 1.6%; Hispanics: 5.3% vs. 3.5%), % populations with income below the poverty level (16.0% vs. 10.8%), % families with income below poverty level (11.7% vs. 7.5%), % linguistically isolated households (8.9% vs. 7.5%), and adults aged 18–64 without insurance (13.6% vs. 10.3%). The median household income was about $6,000 lower in FQHC-PCSAs ($ 43,859 vs. $ 49,277) and they were less likely to be rural (33.5% vs. 42.1%). FQHC-PCSAs also had lower primary care physician supply (70.0 physicians per 100,000 population vs. 73.1 per 100,000), fewer Medicare beneficiaries with primary care visits (80.6% vs. 81.4%), and more hospital stays for ambulatory care-sensitive conditions (69.6 per 1,000 vs. 66.5 per 1,000). All differences between FQHC-PCSAs and non-FQHC-PCSAs were statistically significant at P <0.001, except infant mortality (P = .887).
Growth in the Number of FQHCs and the Number of FQHC-PCSAs
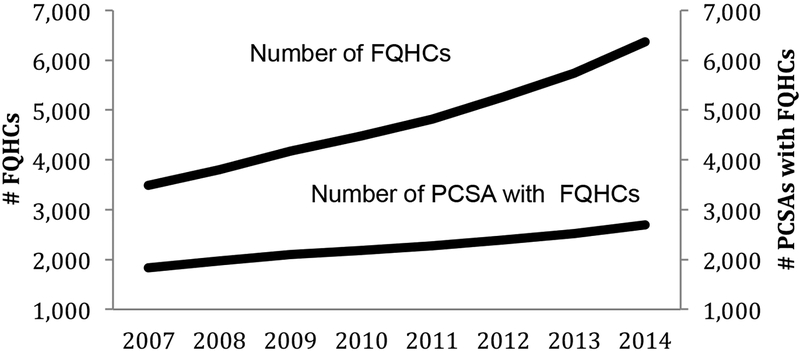
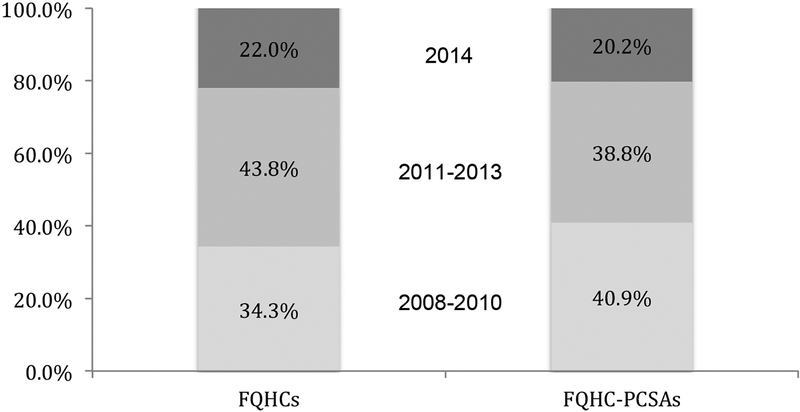
Between 2007 and 2014, there was larger growth in the number of FQHCs (82.7% increase; 3,489 FQHCs in 2007 to 6,376 in 2014) than in the number of FQHC market areas (46.9% increase; 1,835 FQHC-PCSAs in 2007 to 2,695 in 2014) (Figure 1). There were 989 (34.3%) newly certified FQHCs between 2008 and 2010 compared to 1,264 (43.8%) between 2011 and 2013 (Figure 2). The greatest single year expansion was in 2014 (22.0% growth in newly certified FQHCs and 20.2% growth in new FQHC-PCSAs).
Figure 1.
Growth of number of FQHCs and number of PCSAs with FQHCs 2007–2014
FQHCs: Federal Qualified Health Centers
PCSAs: Primary care service areas
Figure 2.
Growth among new FQHCs and new FQHC-PCSAs before and after ACA enacted
FQHCs: Federal Qualified Health Centers
PCSAs: Primary care service areas
FQHC-PCSAs: PCSAs that contained at least one FQHC, used as the service markets of FQHCs
Travel Time between 2007 FQHCs and Newly Certified FQHCs
Newly certified FQHCs were often located near FQHCs that were already certified by 2007. By 2014, 46.8% of 2007 FQHCs (N=3,489) had at least one newly certified FQHC within 30-minute travel time, and another 29.9% had one within an hour. Because the travel time calculation did not account for area population density, we further examined whether the newly certified FQHCs were located in rural or urban areas. We found that, among 2007 FQHCs, 77% were located in urban PCSAs based on the rural-urban commuting area classification. By 2014, 79% of all FQHCs were located in urban PCSAs, with 81% of all newly certified FQHCs being located in urban areas.
Characteristics of FQHC-PCSAs
Overall FQHC service markets between 2007 and 2014
Differences between all FQHC service markets in 2007 compared to all FQHC markets in 2014 were not significant, except for measures of poverty (Table 2). Compared to 2007, the FQHC service markets in 2014 had a lower % population with income below the poverty level (16.0% vs. 16.7%, P = .002), lower % population with income between 100%−200% of poverty level (21.4% vs. 21.9%, P = .016), and lower % families with income below poverty level (11.7% vs. 12.2%, P = .003). Also, fewer of the 2014 markets were high poverty areas (27.9% vs. 31.4%, P = .011).
Table2.
Characteristics of FQHC-PCSAs 2007–2014
| All | New | P* | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2007 | 2014 | 2008–2010 | 2011–2013 | 2014 | 2008–2014 | 2007 vs. 2014 | 2007 vs. new 2014 | 2007 vs. all new areas | |
| Number of FQHC-PCS As | 1,835 | 2,695 | 352 | 334 | 174 | 860 | |||
| Characteristics1 | |||||||||
| % Black | 4.0 | 4.4 | 6.5 | 4.8 | 3.6 | 5.0 | 0.656 | 0.254 | 0.307 |
| % Hispanic | 5.4 | 5.3 | 5.1 | 5.8 | 3.7 | 5.1 | 0.584 | 0.004 | 0.209 |
| % Rural population | 32.6 | 33.5 | 39.4 | 29.3 | 39.5 | 36.0 | 0.843 | 0.112 | 0.650 |
| % Age 65+ | 14.0 | 14.0 | 13.8 | 13.9 | 14.7 | 14.0 | 0.915 | 0.026 | 0.807 |
| % Without insurance coverage | |||||||||
| Age <18 | 1.5 | 1.6 | 1.6 | 1.5 | 1.6 | 1.6 | 0.999 | 0.437 | 0.999 |
| Age 18–64 | 13.9 | 13.6 | 13.6 | 12.5 | 13.0 | 13.1 | 0.097 | 0.003 | <0.001 |
| Poverty/Income | |||||||||
| % Population with income 100% below poverty level | 16.7 | 16.0 | 15.0 | 14.4 | 14.3 | 14.6 | 0.002 | <0.001 | <0.001 |
| % Population with income 100%-200% of poverty level | 21.9 | 21.4 | 21.2 | 20.3 | 20.6 | 20.7 | 0.016 | 0.009 | <0.001 |
| Median household income ($) | 43,142 | 43,859 | 44,6 41 | 46,626 | 45,47 5 | 45,49 8 | 0.035 | 0.026 | <0.001 |
| % Family income below poverty level | 12.2 | 11.7 | 11.0 | 10.5 | 10.1 | 10.6 | 0.003 | <0.001 | <0.001 |
| % Linguistically isolated households | 9.3 | 8.9 | 8.4 | 9.4 | 7.7 | 8.5 | 0.296 | 0.025 | 0.017 |
| % PCS As as high poverty2 areas | 31.4 | 27.9 | 21.9 | 21.9 | 14.9 | 20.5 | 0.011 | <0.001 | <0.001 |
| Mortality | |||||||||
| Infant per 1,000 live births | 6.4 | 6.4 | 6.3 | 6.6 | 6.3 | 6.4 | 0.640 | 0.420 | 0.276 |
| Total Medicare (%) | 4.8 | 4.8 | 5.0 | 4.9 | 4.8 | 4.9 | 0.374 | 0.561 | 0.041 |
| Fee-for-service Medicare (%) | 5.1 | 5.1 | 5.3 | 5.1 | 5.2 | 5.2 | 0.431 | 0.760 | 0.071 |
| Medicare Advantage (%) | 3.5 | 3.5 | 3.5 | 3.7 | 3.4 | 3.6 | 0.698 | 0.588 | 0.374 |
| Primary care physicians per 100,000 | 70.9 | 70.0 | 68.3 | 68.5 | 68.1 | 68.4 | 0.260 | 0.178 | 0.010 |
| Medicare utilization | |||||||||
| % Beneficiaries with primary care visits | 80.5 | 80.6 | 80.6 | 80.6 | 81.0 | 80.7 | 0.780 | 0.195 | 0.522 |
| % Beneficiaries with emergency department visits | 27.0 | 27.1 | 27.6 | 27.4 | 27.1 | 27.4 | 0.409 | 0.389 | 0.058 |
| Primary care visit rate | 3.9 | 3.9 | 3.9 | 3.8 | 3.8 | 3.8 | 0.104 | 0.021 | <0.001 |
| Emergency department visit rate | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.395 | 0.399 | 0.051 |
| Hospitalization for ambulatory care-sensitive conditions, per 1,000 | 68.4 | 69.6 | 72.4 | 70.8 | 71.7 | 71.7 | 0.189 | 0.120 | 0.003 |
Median value except % PCSAs as high poverty areas
High poverty: > 20% of area population living below the federal poverty line
Wilcoxon Score (Kruskal-Wallis Test) or Chi-Square test as appropriate
2007 existing markets vs. new markets
When directly comparing existing 2007 FQHC markets to the new service markets (Table 2), new service markets were less likely to be high poverty areas. Only a fifth of new markets were high poverty areas compared to nearly a third of existing service markets in 2007 (20.5% vs. 31.4%, P < .001). In 2014, the single year with the highest number of new FQHC-PCSAs, only 14.9% of the new service markets (N=174) were high poverty areas. Using other markers of poverty, the new markets (N=860) had lower levels of low income population—% income below the poverty level (14.6% vs. 16.7%, P < .001), % population with 100%−200% of poverty level (20.7% vs. 21.9%, P < .001), or % families with income below poverty level (10.6% vs. 12.2%, P < .001), although median household income was about $2,000 higher ($45,498 vs. $43,142, P < .001).
The new markets had slightly lower primary care supply (68.4 vs. 70.9 per 100,000 population, P = .010), more hospitalizations for ambulatory care-sensitive conditions (71.7 vs. 68.4 per 1,000 beneficiaries, P = .003), and fewer young adults (age 18–64) without insurance (13.1% vs. 13.9%, P < .001) than 2007 markets.
DISCUSSION
We found rapid expansion of FQHCs between 2007 and 2014. Many newly certified FQHC sites were in PCSAs already having an existing FQHC. Among FQHCs that were certified by 2007, nearly half of them had at least one newly certified FQHC within 30 minutes travel time by the end of 2014. Also, most newly certified FQHCs were located in urban areas. New FQHC service markets had fewer people with income below the poverty level and new markets were less likely to be high poverty areas. Although the new markets had 2.5 fewer primary care physicians per 100,000, there was no difference in Medicare outpatient utilization rates. The finding that newly certified FQHCs were less likely to be located in high poverty areas was particularly noticeable in 2014, the year that the ACA was fully implemented and the single year with the largest increase in new FQHC service market areas since 2007.
Our results indicate that the pattern of expansion may not have been optimal for improving access for some populations historically with difficult access to care because it proportionally favored markets in relative proximity to existing FQHCs and because newly certified FQHCs tended to locate in relatively less impoverished areas. While an FQHC can apply to have an area designated as underserved, it is easier for grantees to obtain a new certification in an area that has already obtained underserved status from a previous application or to add a new service site in a nearby town using the same administrative support, which may explain why many newly certified FQHCs located near existing FQHCs.
Another explanation for many newly certified FQHCs locating within 30 minutes of an existing FQHC could be that more newly certified FQHCs were in urban settings. These areas may be underserved while within reasonable travel time of other clinics based on their socioeconomic status. We found, however, that newly certified FQHCs were also less likely to be located in high poverty areas. These results suggest that the impact of expansion on increasing access among the most financially disadvantaged populations may be limited.
Although poverty is one of criteria used by HRSA to identify underserved areas, many areas were designated decades ago. With population migration and new community development, areas that were previously designated as underserved may not continue to meet the criteria with updated information. On the other hand, many areas may now be eligible to be designated as underserved. We applied the HRSA calculation formula using the 2010 U.S. population to calculate a 2010 Index of Medical Underservice (IMU) score for all v3.1 PCSAs (N=7,144), which were aggregated areas of the 2010 U.S. Census Tracts.22,31,34 Using the same IMU < 62 as the threshold for designating underserved, we identified 3,723 (52.1%) PCSAs with a 2010 IMU score less than 62, and 1,000 (26.9%) of them contained at least one FQHC in 2014. Among all FQHC service markets in 2014 (N=2,695), 37.1% had a 2010 IMU score less than 62. Among all the newly certified FQHCs since 2007 (N=2,887), only 20.7% were located in PCSAs with a 2010 IMU score less than 62 compared to 27.9% of 2007 FQHCs. Our simulation exercise indicates that the location of FQHCs may not be optimally meeting the policy goal of increasing access in the most needy areas using 2010 population data, due in at least part to the absence of a requirement for updated designation regulations and certification process that results in a tendency for new sites to locate near existing FQHC service sites.
In 2011, HRSA organized a committee to consider and develop new methodologies for the designation of being “underserved”.31 The proposed methodology estimated that 48 million people reside in areas that would be newly eligible to be designated as underserved, while 16 million of the 71 million people living in areas currently designed as underserved would lose that designation. This suggests that at least 48 million people could have increased access to primary care if newly certified FQHCs were allowed in those areas. However, the Committee (28 members) did not reach a consensus and the proposed new methodologies have been stalled. Without updated regulation for designating underserved areas that is aligned with current health care needs, newly certified FQHCs may continue to locate in areas with relatively less financially disadvantaged populations.
Our study has several limitations. We used CMS’ POS files to identify FQHCs and their locations, which could lead to results that differ from what is found in the HRSA’s UDS file.16,35,36 As noted earlier, the UDS is designed for grantees of health center programs to report their performance to HRSA and is not used by CMS for Medicare payment to delivery sites. Each CMS delivery site has unique street location but does not include grantee relationship, as a result, we were unable to distinguish between an existing grantee opening a new site and a new grantee opening its first site. In addition, we used 30-minute travel time intervals at the tract level between each 2007 FQHC and its nearest newly certified FQHC to estimate the impact on geographic access of a newly certified FQHC, a measure that is not a door-to-door measure and that does not account for the number of newly certified FQHCs or the size of newly certified FQHCs. There could be more than one newly certified FQHC within the same distance from a 2007 FQHC and with different levels of operating capacity. We were unable to account for the availability of public transportation or FQHC-provided transportation services, an enhanced FQHC service that is beyond the scope of this study.37 In addition, we defined FQHCs’ markets by FQHC locations, not where the users of FQHCs live. Our previous study showed that in 2011, 12% of Medicare FQHC users were from PCSAs that did not contain a FQHC.24 Further research to identify area characteristics for all FQHC users’ residence may provide useful information about potential area care needs. And on a related note, we studied service markets and not FQHC patients themselves, which could also be useful for identification of populations that may benefit from expansion of FQHCs.
Lastly, we were not able to report on whether newly certified FQHCs improved access to primary care from the patients’ perspective, nor did we measure patient outcomes and care quality associated with expansion. Using Medical Expenditure Panel Survey 2004–2008, Laiteerapong et al. demonstrated that FQHCs, as safety-net providers for socially and medically disadvantaged populations, reduced utilization and improved preventive care.38 Research is needed to show whether this benefit from FQHC services is still relevant in the current healthcare environment.
To be sure, there are challenges for expanding the availability of FQHCs in addition to the designation of the area as underserved, including other certification criteria that clinics have to meet (e.g. requirement of majority of board members be its own patients and a sliding fee scale to persons with income below 200 percent of the federal poverty level). Those criteria may pose barriers both administratively and financially for clinics to obtain the certification in the new areas that are currently most in need.
The expansion of FQHCs has resulted in more people seeking services at FQHCs.15 However, the geographic patterns of expansion found in this study also indicate that the pattern of expansion may not be optimal for directing these important primary care resources to financially disadvantage populations. Policy changes to further improve the provision of primary care in poor, underserved populations are needed. At least two fundamental factors could directly affect FQHC expansion to new areas—outdated underserved designation and a bureaucratically burdensome process of being certified and being financially supported by federal grants.
In conclusion, the value of primary care is widely accepted.2,3,5,25,28,39 Improved geographic access to primary care delivery location in underserved is crucial. Our study demonstrates the importance of geographic access to care in assessing policies aimed at improving primary care delivery. Future research is needed to evaluate the impact of expansion on care needs of FQHC users, including who are being served by the new FQHCs, and whether improved access is associated with better outcomes, as well as any potential unmet needs in areas with limited resources because of the expansion patterns observed in this study.
Acknowledgments
This research was supported by NIA disability supplement grant 3U01AG046830-03S2
Footnotes
All authors declare no conflict of interest to disclose.
References:
- 1.Donaldson MS, Yordy KD, Lohr KN, Vanselow NA. Primary Care: America’s Health in A New Era. Washington, DC: National Academy Press; 1996. [PubMed] [Google Scholar]
- 2.Starfield B Primary care in the United States. Int J Health Serv. 1986;16(2):179–198. [DOI] [PubMed] [Google Scholar]
- 3.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Starfield B Primary Care : Concept, Evaluation, and Policy New York: Oxford University Press; 1992. [Google Scholar]
- 5.Council on Graduate Medical Education. Twentieth Report: Advancing Primary Care. Rockville, MD: December, 2010 2010. [Google Scholar]
- 6.Council on Graduate Medical Education. Twenty-First Report: Improving Value in Graduate Medical Education. Rockville, MD: August, 2013. [Google Scholar]
- 7.Sessums LL, McHugh SJ, Rajkumar R. Medicare’s Vision for Advanced Primary Care: New Directions for Care Delivery and Payment. JAMA. June 28 2016;315(24):2665–2666. [DOI] [PubMed] [Google Scholar]
- 8.Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care--two essential elements of delivery-system reform. N Engl J Med. December 10 2009;361(24):2301–2303. [DOI] [PubMed] [Google Scholar]
- 9.Knight KE. Federally Qualified Health Centers Minimize the Impact of Loss of Frequency and Independence of Movement in Older Adult Patients through Access to Transportation Services. J Aging Res. 2011;2011:898672 PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taylor J The fundamentals of community health centers. Washington, DC: National Health Policy Forum; August 31, 2004 2004. [Google Scholar]
- 11.national Associaiton of Community Health Centers. Community Health Centers Past, Present, and Future: Building on 50 Years of Success. 2015; http://www.nachc.org/wp-content/uploads/2016/12/NACHC_50th-Report.pdf Accessed June 13, 2017, 2017. [Google Scholar]
- 12.Center for Medicare & Medicaid Services. Federally QUalified Health Center Medicare Learning Network 2017; ICN; 006397:https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/fqhcfactsheet.pdf. Accessed May 31, 2017, 2017. [Google Scholar]
- 13.Iglehart JK. Spreading the safety net--obstacles to the expansion of community health centers. N Engl J Med. March 27 2008;358(13):1321–1323. [DOI] [PubMed] [Google Scholar]
- 14.Resoruces Health and Administration Services. The Affordable Care Act and Health Centers. 2012; https://www.hrsa.gov/sites/default/files/about/news/2012tables/healthcentersacafactsheet.pdf. Accessed February 13, 2018.
- 15.Resources Health and Administration Services. Fact Sheet - Bureau of Primary Health Care - HRSA. 2016; http://bphc.hrsa.gov/about/healthcenterfactsheet.pdf. Accessed August 17, 2016.
- 16.National Association of Community Health Centers. United States Health Center Fact Sheet, 2014. Research Fact Sheets 2014. Accessed September 2, 2016. [Google Scholar]
- 17.Medicare Payment Advisory Commission. Report to the Congress: Medicare and the Health Care Delivery System: Chapter 6 Federally Qualified Health Centers.June 2011. [Google Scholar]
- 18.Center for Medicare & Medicaid Services. Federally Qualified Health Center Fact Sheet. 2016; https://www.cms.gov/Outreach-and-Education/Medicare-Learning‐Network-MLN/MLNProducts/downloads/fqhcfactsheet.pdf. Accessed March 8, 2017. [Google Scholar]
- 19.National Association of Community Health Centers. Health Centers and Medicare: Caring for America’s Seniors. Research Fact Sheets and Infographics 2016; http://nachc.org/wp-content/uploads/2015/06/Medicare-FS-2016.pdf. Accessed July 19, 2016. [Google Scholar]
- 20.Bynum JP, Chang CH, Austin A, Carmichael D, Meara E. Outcomes in Older Adults with Multimorbidity Associated with Predominant Provider of Care Specialty. J Am Geriatr Soc. April 08 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodman DC, Mick SS, Bott D, et al. Primary care service areas: a new tool for the evaluation of primary care services. Health Serv Res. February 2003;38(1 Pt 1):287–309. PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Resources Health and Administration Services. Primary Care Service Area Data Download −2010 (Census Tract Basis). https://datawarehouse.hrsa.gov/data/datadownload/pcsa2010download.aspx. Accessed April 13, 2017. [Google Scholar]
- 23.Provider of Services Current Files. https://www.cms.gov/research-statistics-data-and-systems/downloadable-publicof-use-files/provider-of-services/index.html.
- 24.Chang CH, Lewis VA, Meara E, Lurie JD, Bynum JP. Characteristics and Service Use of Medicare Beneficiaries Using Federally Qualified Health Centers. Med Care. August 2016;54(8):804–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang CH, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries’ health outcomes. JAMA. May 25 2011;305(20):2096–2104. PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wright B, Potter AJ, Trivedi A. Federally Qualified Health Center Use Among Dual Eligibles: Rates of Hospitalizations and Emergency Department Visits. Health Affairs. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cull WL, Chang CH, Goodman DC. Where do graduating pediatric residents seek practice positions? Ambul Pediatr. Jul-Aug 2005;5(4):228–234. [DOI] [PubMed] [Google Scholar]
- 28.Chang CH, O’Malley AJ, Goodman DC. Association between Temporal Changes in Primary Care Workforce and Patient Outcomes. Health Serv Res. April 2017;52(2):634–655. PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.SAS Institute Inc. Driving Distances and Drive Times using SAS and Google Maps. 2016; http://www.sascommunity.org/wiki/Driving_Distances_and_Drive_Times_using_SAS_and_Google_Maps [Google Scholar]
- 30.Health Resources and Services Administration. New Access Point Grant Awards. 2016; https://bphc.hrsa.gov/programopportunities/fundingopportunities/newaccesspoi.nts/fy2017awards/index.htm. [Google Scholar]
- 31.Negotiated Rulemaking Committee. Negotiated Rulemaking Committee on the Designation of Medically Underserved Populations and Health Professional Shortage Areas Final Report to the Secretary. 2011; http://www.hrsa.gov/advisorycommittees/shortage/nrmcfinalreport.pdf. Accessed March 8, 2017. [Google Scholar]
- 32.U.S. Census Bureau. Poverty Areas. 1995; https://www.census.gov/population/socdemo/statbriefs/povarea.html. Accessed July 23, 2018.
- 33.Colla CH, Lewis VA, Kao LS, O’Malley AJ, Chang CH, Fisher ES. Association Between Medicare Accountable Care Organization Implementation and Spending Among Clinically Vulnerable Beneficiaries. JAMA internal medicine. June 20 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Office of Rural Health Policy of Health Resoruces and Services Administration. Starting a Rural Health Clinic - A How-To Manual. In: Department of Health & Human Services, ed 2004. [Google Scholar]
- 35.The Henry J Kaiser Family Fundtaion. Community Health Centeres in an Era of Health Reform: An Overview and Key Challenges to Health Center Growh. Issue Brief 2013; https://kaiserfamilyfoundation.files.wordpress.com/2013/03/8098‐03.pdf. Accessed July 19, 2016. [Google Scholar]
- 36.Katz AB, Felland LE, Hill I, Stark LB. A long and winding road: federally qualified health centers, community variation and prospects under reform. Res Brief. November 2011(21):1–9. [PubMed] [Google Scholar]
- 37.Chen BK, Hibbert J, Cheng X, Bennett K. Travel distance and sociodemographic correlates of potentially avoidable emergency department visits in California, 2006–2010: an observational study. International journal for equity in health. March 21 2015;14:30 PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laiteerapong N, Kirby J, Gao Y, et al. Health care utilization and receipt of preventive care for patients seen at federally funded health centers compared to other sites of primary care. Health Serv Res. October 2014;49(5):1498–1518. PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shi L, Macinko J, Starfield B, Politzer R, Xu J. Primary care, race, and mortality in US states. Soc Sci Med. July 2005;61(1):65–75. [DOI] [PubMed] [Google Scholar]