Abstract
BACKGROUND
Fundoplication, was first introduced as a surgical treatment method of gastroesophageal reflux disease. Consequently, several modifications of this method have been described, whereas laparoscopic fundoplication was recently introduced. Although single incision (SI) fundoplication was considered as an alternative to the conventional laparoscopic approach, several studies reported an increased operation duration, and high rates of multiport conversion and incisional hernia.
AIM
To provide a current overview of the technical variations and the postoperative outcomes of patients submitted to SI fundoplication.
METHODS
The present systematic review of the literature was designed and conducted on the basis of the PRISMA guidelines. A systematic screening of the electronic scholar databases (Medline, Scopus and Web of Science) was performed.
RESULTS
Literature search resulted in the identification of 19 studies. Overall, 266, 137 and 110 SI Nissen, Dor and Toupet fundoplications were reported, respectively. In the majority of the trials, standard laparoscopic instruments were used. The left liver lobe was displayed through the use of forceps, graspers, retractors, drains or even glue. Both intra-corporeal and extracorporeal suturing was described. Mean operative time was 136.3 min. Overall complication rate was 5.2% and the rate of incisional hernia was 0.9%. No mortality was reported.
CONCLUSION
Due to the methodological heterogeneity and the lack of high quality studies comparing multi to single access techniques and the several variations, we conclude that further well designed studies are necessary, in order to evaluate the role of SI fundoplication.
Keywords: Single incision, Single port, Fundoplication, Nissen, Dor, Toupet
Core tip: This systematic review summarizes all available data about the use of single incision laparoscopic fundoplication. Although the technique is not yet standardized, this study validates the safety and efficacy of the single port approach compared to conventional multiport approach.
INTRODUCTION
Fundoplication, the wrap of the gastric fundus around the distal part of the esophagus, was introduced by Nissen[1] in 1956, as a surgical treatment of gastroesophageal reflux disease (GERD), and is currently considered as the operation of choice, when conservative approaches fail[2]. Since the extent of the plication was correlated with postoperative functional complications, various modifications (e.g., Hill, Toupet) of the original technique have been described[3-5]. Besides these, fundoplication has been, also, an important restoration element in other procedures, such as, Heller myotomy for esophageal achalasia[6].
The implementation of the minimal invasive principles in fundoplication, was justified under the auspice of a better cosmetic result, reduced postoperative pain and a faster recovery[7]. However, proponents of the open approach, linked laparoscopy to increased perioperative costs, pneumoperitoneum related complications, and technical difficulties leading to a steeper learning curve, such as, narrowing of the field of vision, fixed instrument positions and loss of loss of freedom degrees[8]. Due to the fact that subsequent studies, associated laparoscopic fundoplication with a reduced length of hospital stay (LOS), return to daily activities and overall morbidity, resulted in the establishment of laparoscopy as the gold standard approach[7,9].
In order to further enhance the advantages of minimally invasive operations, single incision (SI) laparoscopic surgery was introduced. Navarra et al[10], in 1997, reported the first SI cholecystectomy, whereas Hamzaoglu et al[11], performed the first single incision laparoscopic surgery (SILS) Nissen in 2010. Single port fundoplications, although characterized by minimization of postoperative scars and better cosmesis, are more demanding in terms of laparoscopic skills, due to the inert loss of triangulation and intraoperative instrument clashing[12]. Although, initial studies comparing SILS fundoplications to the conventional multiport approaches, reported that the two techniques were comparable in terms of efficacy and safety[13,14], the increased operative time and the high rate of conversion to multiport and port-site hernia were considered as inhibitory factors for the wider acceptance of the method[13].
Therefore, taking into consideration the above mentioned body of evidence, the present systematic review of the literature was designed and conducted. Our study, mainly, focuses in providing a comprehensive appraisal of the intraoperative technical variations and the postoperative outcomes in adult patients submitted to SI fundoplication.
MATERIALS AND METHODS
Study protocol
The PRISMA guidelines were utilized for the completion of this systematic review[15].
Eligibility criteria
All human trials that reported results on SI fundoplication, with an adult study population, whose outcomes of interest were reported in English and were retrievable, were considered as eligible. Eligible studies should provide perioperative results (i.e., complication, mortality or conversion rates, operation duration and follow up) on SI fundoplication. Exclusion criteria for this systematic review were studies: (1) with a pediatric study sample; (2) with no outcome of interest; (3) with inadequate outcome data; (4) without human objects; or (5) in the form of reviews, editorials, letters, conference abstracts and expert opinions.
Literature search
A systematic screening of the literature available in the electronic scholar databases (Medline, Scopus and Web of Science) was performed. The last search date was 2/1/2019. The following keywords were used: “SILS”, “single site”, “single port”, “single incision”, “laparoendoscopic single site”, “fundoplication”.
Study selection and data collection
After the completion of the literature search, the duplicate entries were identified and removed. The next step included the screening of titles and abstracts. Finally, the remaining articles were submitted to a full text review, in order to assess consistency with the above mentioned eligibility criteria. All electronic search, study selection and data extraction were performed in duplicate and blindly by two independent investigators (PK and SC). In case of a discrepancy, through mutual discussion and revision, a consensus was reached. If the disagreement was not resolved, the opinion of a third investigator was considered (BI).
Data extraction included the recording of data regarding the included studies(first author, country and type of study, follow up, number and experience of surgeons, sample size and gender, age and body mass index (BMI) allocation of the patients), patient characteristics (ASA score, previous operations and surgery indication), technical characteristics (single port device, instrument type, liver retraction method, dissection device, boogie size, suturing method and pneumoperitoneum pressure) and perioperative outcomes (operation duration LOS, blood loss and conversion, complications, recurrence mortality and incisional hernia rates).
Only the information available in the full text article of the trials were reported. In case that the mean and the standard deviation (SD) of the continuous variables were not provided, then they were estimated from the respective median, range or interquartile range, according to the formula by Hozo et al[16]. Moreover, outcome percentages were calculated according to the following formula: Total number of events regarding a specific complication/Sum of patients sample of studies reporting the specific complication.
RESULTS
Study selection
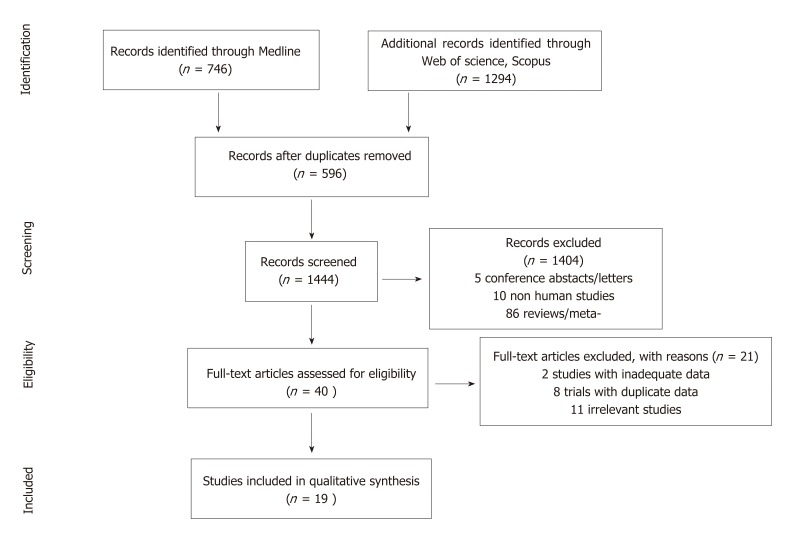
The application of the search algorithm resulted in the identification of 2040 records (Figure 1). More specifically, 746, 1102 and 192 citations were retrieved through Medline, Web of Science and Scopus, respectively. After the removal of the duplicate entries, 1444 titles and abstracts were screened. In this phase, 1404 records (5 conference abstracts or letters, 10 non human studies, 86 reviews or meta-analyses and 1303 irrelevant studies) were excluded. The next step included the full text screening of the remaining 40 articles, on the basis of the inclusion criteria. In total 21 full text articles were not considered as eligible (2 trials with inadequate data, 8 trials with duplicate patient data and 11 irrelevant studies). Therefore, 19 studies[11,12,14,17-32] were included in our systematic review.
Figure 1.
Study flow diagram.
Study characteristics
The characteristics of the included studies are summarized in Table 1. Publication year ranged from 2010[11] to 2016[14,30]. Although initial references consisted of case reports[11,12,18,23,27,29], subsequent trials included retrospective[14,19-22,24-26,30,31] and prospective[17,32] studies. All eligible trials were performed in a single institution. Regarding the operation type, 14 studies[11,12,17-26,30,31] reported on Nissen fundoplication, whereas Dor and Toupet fundoplication was performed in 6[14,25,27-29,32] and 1 trial[17], respectively. Although the number of operating surgeons ranged from 1[22,24,27] to multiple[14,19,30,32], experience in laparoendoscopic techniques was documented only in 3[24,26,27] studies. In total, 513 patients were submitted to a SI laparoscopic fundoplication. More specifically, 266, 137 and 110 SI Nissen, Heller and Dor and Toupet fundoplications were recorded, respectively. Mean age, gender and BMI allocation is, also, displayed in Table 1. Mean follow up period extended from 1 wk[11] to 60 mo[26].
Table 1.
Included studies
| Included studies | |||||||||||||
| ID | Ref. | Country | Type of study | Center | Year | Operation type | Surgeons | Experience | Sample | Gender (M/F) | Age | BMI | Follow up |
| 27417943 | Buckley et al[30] | United States | Retrospective | Single center | 2016 | Nissen | 3 | No | 21 | n/a | n/a | n/a | 34 (8.3) mo |
| 26350663 | Sukharamwala et al[17] | United States | Prospective | Single center | 2015 | Nissen | n/a | n/a | 190 | 67/123 | 55(14.7) | 27(3.9) | n/a |
| 24960483 | Agaba et al[26] | United States | Retrospective | Single center | 2014 | Nissen | 2 | Yes | 3 | n/a | n/a | n/a | 60 mo |
| 24686364 | Galvani et al[24] | United States | Retrospective | Single center | 2014 | Nissen | 1 | Yes | 2 | 0/2 | 43.4 (4) | 22(3) | n/a |
| 24615563 | Wu et al[25] | China | Retrospective | Single center | 2014 | Nissen | n/a | n/a | 5 | n/a | n/a | n/a | 1 mo |
| 23585169 | Strzalka et al[31] | Poland | Retrospective | Single center | 2013 | Nissen | n/a | n/a | 1 | n/a | n/a | n/a | n/a |
| 10.5336/medsci.2012-31954 | Yilmaz et al[22] | Turkey | Retrospective | Single center | 2013 | Nissen | 1 | n/a | 10 | 3/7 | 35(8.5) | 24.6 (3) | n/a |
| 22146016 | Eyuboglu et al[20] | Turkey | Retrospective | Single center | 2012 | Nissen | n/a | n/a | 22 | 5/17 | 28(5.75) | n/a | 8 mo |
| 20306152 | Miyazaki et al[19]1 | Japan | Retrospective | Single center | 2012 | Nissen | Surgical team | n/a | 4 | 2/2 | 52.5 (11.7) | 20.9 (1.1) | n/a |
| 22278618 | Mizuno et al [21]2 | Japan | Retrospective | Single center | 2012 | Nissen | n/a | n/a | 2 | 1/1 | 65.5 (13.4) | 30.5 (0.7) | 18 mo |
| 21991503 | Barbaros et al[18] | Turkey | Case report | Single center | 2011 | Nissen | n/a | n/a | 1 | 1/0 | 29 | n/a | n/a |
| 21059609 | Dapri et al[23] | Belgium | Case report | Single center | 2011 | Nissen | n/a | n/a | 1 | 0/1 | 21 | n/a | 6 mo |
| 21471786 | Hawasli et al[12] | United States | Case report | Single center | 2011 | Nissen | n/a | n/a | 1 | 0/1 | 36 | 29 | 1 wk |
| 20306152 | Hamzaoglu et al[11] | Turkey | Case series | Single center | 2010 | Nissen | n/a | n/a | 3 | 1/2 | 40(17.5) | 26.3 (4.93) | 1 wk |
| Total | 266 | 79/156 | 51.05 | 26.75 | 19.27 | ||||||||
| 26315292 | Fukuda et al[14] | Japan | Retrospective | Single center | 2016 | Heller and Dor | Surgical team | No | 10 | 1/9 | 53.6 (18.3) | 19.7 (2) | n/a |
| 24615563 | Wu et al[25] | China | Retrospective | Single center | 2014 | Heller and Dor | n/a | n/a | 4 | n/a | n/a | n/a | 1 mo |
| 23896255 | Ross et al[32] | United States | Prospective | Single center | 2013 | Heller and Dor | Surgical team | No | 120 | 56/64 | 53(17.4) | 25(4.7) | 33 (7.9) mo |
| 23088902 | Yamada et al[28] | Japan | Case report | Single center | 2013 | Heller and Dor | n/a | n/a | 1 | 0/1 | 56 | n/a | 12 mo |
| 22218875 | Yano et al[29] | Japan | Case report | sIngle center | 2012 | Heller and Dor | n/a | n/a | 1 | 1/0 | 31 | n/a | n/a |
| 21969159 | Nakajima et al[27] | Japan | Case report | Single center | 2011 | Heller and Dor | 1 | yes | 1 | 1/0 | 58 | n/a | 1 mo |
| Total | 137 | 59/74 | 52.9 | 24.59 | 31.5 | ||||||||
| 26350663 | Sukharamwala et al[17] | United States | Prospective | Single center | 2015 | Toupet | n/a | n/a | 110 | 28/82 | 66(13.2) | 26(3.8) | n/a |
| Total | 513 | 166/312 | 55.01 | 25.9 | 27.6 | ||||||||
Only data for Nissen extracted- Heller and Dor data duplicate;
In the study of Mizuno et al[21] only data from adult patients extracted. n/a: Not available.
Data considering the ASA classification of the included patients were systematically not provided (Table 2). The indications for performing surgery were hiatus hernia[18,25] and GERD[11,12,17,19-24,26,30,31] for the Nissen and Toupet fundoplication and achalasia[14,27-29,32] for the Heller myotomy and Dor fundoplication. Reports were inconsistent, regarding the included patients that had undergone a previous abdominal operation.
Table 2.
Patient characteristics
| Patient characteristics | |||||||
| Ref. | Operation type | ASA I | ASA II | ASA III | ASA IV | Previous operation | Indication |
| Buckley et al[30] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Sukharamwala et al[17] | Nissen | n/a | n/a | n/a | n/a | 14 | GERD |
| Agaba et al[26] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Galvani et al[24] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Wu et al[25] | Nissen | n/a | n/a | n/a | n/a | n/a | Hiatus Hernia |
| Strzalka et al[31] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Yilmaz et al[22] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Eyuboglu et al[20] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Miyazaki et al[19] * | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Mizuno et al[21]** | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Barbaros et al[18] | Nissen | n/a | n/a | n/a | n/a | n/a | Hiatus Hernia |
| Dapri et al[23] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Hawasli et al[12] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Hamzaoglu et al[11] | Nissen | n/a | n/a | n/a | n/a | n/a | GERD |
| Fukuda et al[14] | Heller and Dor | n/a | n/a | n/a | n/a | n/a | Achalasia |
| Wu et al[25] | Heller and Dor | n/a | n/a | n/a | n/a | n/a | Achalasia |
| Ross et al[32] | Heller and Dor | n/a | n/a | n/a | n/a | 5 | Achalasia |
| Yamada et al[28] | Heller and Dor | n/a | n/a | n/a | n/a | n/a | Achalasia |
| Yano et al[29] | Heller and Dor | n/a | n/a | n/a | n/a | n/a | Achalasia |
| Nakajima et al[27] | Heller and Dor | n/a | n/a | n/a | n/a | n/a | Achalasia |
| Sukharamwala et al[17] | Toupet | n/a | n/a | n/a | n/a | 14 | GERD |
n/a: Not available; ASA: American Society of Anesthesiologists; GERD: Gastroesophageal reflux disease.
Despite the fact that, in the majority of the included studies (Table 3), a commercial SP device, such as SILS™[11,18-22], Triport Plus™[32], Wrapdisk™[28], X-CONE[19], or EZ Access™[14], was applied, several trials[12,14,19,20,23,25,29,32] reported the introduction of conventional or low profile trocars through a single abdominal incision. In most operations[14,21,22,25,28,30], conventional laparoscopic instruments were used. However, the application of articulating[11,12,18,21,27,32] or curved[23] instruments has, also, been described. Heterogeneity in terms of the liver retraction method was identified. Several techniques, such as, the use of forceps[14], graspers[23], retractors[11,17,19,20,24,32], drains[28,29] or even glue[25], have been documented for the elevation and displacement of the liver left lobe. In the larger part of the included trials[11,12,14,17,18,20,22,25,27,32], commercial energy devices were applied for tissue dissection. A transesophageal boogie was used only in 4 studies[12,22,23,29], and the respective diameter ranged from 32Fr[22] to 60Fr[12]. Intracorporeal suturing with conventional sutures was documented in 4 trials[23,25,29,32]. In the remaining trials, extracorporeal suturing[22], Endostich™[12,17,18,20,32], SILS STICH[11], or V Lock™ sutures[17] were applied. The intraabdominal pneumoperitoneum pressure spanned from 8 mmHg[28] to 15 mmHg[12,26].
Table 3.
Technical characteristics
| Technical characteristics | |||||||||
| Ref. | Operation type | Single port device | Instruments | Liver retraction | Dissection device | Boogie | Suturing | Gas | Gas pressure |
| Buckley et al[30] | Nissen | SILS™ | Conventional | n/a | n/a | n/a | n/a | n/a | n/a |
| Sukharamwala et al[17] | Nissen | SILS™ | n/a | Pretzel Retractor | Monopolar or Ultrasonic dissectors | n/a | Endostich™ or V Lock™ | n/a | n/a |
| Agaba et al[26] | Nissen | SILS™ | n/a | n/a | n/a | n/a | n/a | n/a | 15mmHg |
| Galvani et al[24] | Nissen | n/a | n/a | CINCH™ retractor | n/a | n/a | n/a | n/a | n/a |
| Wu et al[25] | Nissen | Conventional trocars in a single incision | Conventional | Cyanoacrylate glue | Harmonic™ | n/a | Intracorporeal | n/a | n/a |
| Strzalka et al[31] | Nissen | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Yilmaz et al[22] | Nissen | SILS™ | Conventional | Berk technique | Harmonic™ | 32Fr | Extracorporeal | CO2 | 13mmHg |
| Eyuboglu et al[20] | Nissen | Conventional trocars in a single incision or SILS™ | n/a | Cerrahpasa retractor | Ligasure™ or Monopolar | n/a | Endostich™ | n/a | n/a |
| Miyazaki et al[19] * | Nissen | Conventional trocars in a single incision or SILS™ or X-CONE™ | n/a | Loop Retractor | n/a | n/a | n/a | n/a | n/a |
| Mizuno et al[21]** | Nissen | SILS™ | ProSeed™ and Conventional | Loop Retractor | n/a | n/a | n/a | CO2 | 8mmHg |
| Barbaros et al[18] | Nissen | SILS™ | Roticulating | Snowden Pencer™ | Ligasure™ | n/a | Endostich™ | n/a | 14mmHg |
| Dapri et al[23] | Nissen | Conventional trocars in a single incision | Dapri™ Karl Storz | Grasper | n/a | 34Fr | Intracorporeal | n/a | n/a |
| Hawasli et al[12] | Nissen | Conventional trocars in a single incision | Roticulating | Veress | Sono-surg™ | 60FR | Endostich™ | CO2 | 15mmHg |
| Hamzaoglu et al[11] | Nissen | SILS™ | Roticulating | Instanbul Technique | Harmonic™ | no | SILS™ STICH | n/a | n/a |
| Fukuda et al[14] | Heller and Dor | Conventional trocars in a single incision or SILS™ or EZ Access™ | Conventional | Mini loop Retractor™ or Forceps | Harmonic™ | n/a | n/a | CO2 | n/a |
| Wu et al[25] | Heller and Dor | Conventional trocars in a single incision | Conventional | Cyanoacrylate glue | Harmonic™ | n/a | Intracorporeal | n/a | n/a |
| Ross et al[32] | Heller and Dor | Conventional trocars in a single incision or SILS™ or Triport Plus™ | Roticulating | Retractor | Bipolar or Ultrasonic dissectors | n/a | Intracorporeal or Endostich™ | CO2 | n/a |
| Yamada et al[28] | Heller and Dor | Wrapdisk™ | Conventional | Silicon drain | Monopolar | n/a | n/a | CO2 | 8mmHg |
| Yano et al[29] | Heller and Dor | Conventional trocars in a single incision | n/a | Penrose drain | Monopolar | 56Fr | Intracorporeal | CO2 | 12mmHg |
| Nakajima et al[27] | Heller and Dor | SILS™ | Roticulating | Endo Close™ | Monopolar or Enseal™ | n/a | n/a | n/a | 10mmHg |
| Sukharamwala et al[17] | Toupet | SILS™ | n/a | Pretzel Retractor | Monopolar or Ultrasonic dissectors | n/a | Endostich™ or V Lock™ | n/a | n/a |
n/a: Not available.
Although no conversion to open was reported, the multiport conversion rates for Nissen and Dor fundoplications were 9.8% and 14%, respectively (Table 4). Mean overall operation duration was 136.3 min. The mean operative time for Nissen fundoplication was 130.7 min. Similarly pooled LOS was 2.49 d. Mean intraoperative blood loss was retained at very low levels (17.04 mL). Overall morbidity rate was estimated at the rate of 5.2%. No mortality event was documented. In all subgroups, recurrence of primary symptoms was minimal (0%). The rate of postoperative incisional hernia was calculated at the level of 0.9%.
Table 4.
Perioperative outcomes
| Perioperative outcomes | ||||||||||
| Ref. | Operation type | Open conversion | Multiport conversion | Operation duration | LOS | Blood loss | Complications | Recurrence | Mortality | Incisional hernia |
| Buckley et al[30] | Nissen | 0 | n/a | n/a | n/a | n/a | 2 | 0 | 0 | 2 |
| Sukharamwala et al[17] | Nissen | n/a | n/a | 130 (42.7) | 2 (1.1) | n/a | n/a | n/a | n/a | n/a |
| Agaba et al[26] | Nissen | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Galvani et al[24] | Nissen | 0 | 1 | 164 (83) | n/a | 23 (4) | n/a | n/a | n/a | n/a |
| Wu et al[25] | Nissen | 0 | 0 | 146 (13) | n/a | n/a | 0 | 0 | 0 | 0 |
| Strzalka et al[31] | Nissen | 0 | 0 | 100 | 1 | n/a | 0 | n/a | 0 | 0 |
| Yilmaz et al[22] | Nissen | 0 | 2 | 93 (14.1) | 2.2(0.9) | n/a | 0 | 0 | 0 | 0 |
| Eyuboglu et al[20] | Nissen | 0 | 0 | n/a | 1 | n/a | 0 | 0 | 0 | 0 |
| Miyazaki et al[19] * | Nissen | 0 | 2 | 202.7 (61.1) | 15.5 (10.6) | 25 (23) | 0 | 0 | 0 | 0 |
| Mizuno et al[21]** | Nissen | 0 | 0 | 147.5 (45.9) | 10 (2) | 10 (7) | 0 | 0 | 0 | 0 |
| Barbaros et al[18] | Nissen | 0 | 0 | 120 | 1 | n/a | 0 | 0 | 0 | 0 |
| Dapri et al[23] | Nissen | n/a | n/a | 122 | 2 | 0 | 0 | 0 | 0 | 0 |
| Hawasli et al[12] | Nissen | 0 | 0 | 52 | 1 | n/a | 0 | 0 | 0 | 0 |
| Hamzaoglu et al[11] | Nissen | 0 | 0 | 190 (17.3) | 2 | 30 (17.3) | 0 | 0 | 0 | 0 |
| 0 (0%) | 5 (9.8%) | 130.71 | 2.2 | 21.3 | 2 (2.8%) | 0 (0%) | 0 (0%) | 2 (2.8%) | ||
| Fukuda et al[14] | Heller and Dor | 0 | 7 | 223.5 (46.3) | 9.7(2.4) | 16 (17.8) | 0 | 0 | 0 | 0 |
| Wu et al[25] | Heller and Dor | 0 | 0 | 133 (20) | n/a | n/a | 0 | 0 | 0 | 0 |
| Ross et al[32] | Heller and Dor | 0 | 12 | 129 (39.2) | 2 (2.7) | n/a | 9 | n/a | 0 | 0 |
| Yamada et al[28] | Heller and Dor | n/a | n/a | 248 | 2 | 0 | 0 | 0 | 0 | 0 |
| Yano et al[29] | Heller and Dor | n/a | n/a | 236 | 4 | 0 | 0 | 0 | 0 | 0 |
| Nakajima et al[27] | Heller and Dor | 0 | 0 | 220 | 4 | 10 | 0 | 0 | 0 | 0 |
| 0 (0%) | 19 (14%) | 138.3 | 2.6 | 13.07 | 9 (6.5%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Sukharamwala et al[17] | Toupet | n/a | n/a | 145 (58.4) | 3 (5.2) | n/a | n/a | n/a | n/a | n/a |
| Total | 0 (0%) | 24 (12.9%) | 136.3 | 2.49 | 17.04 | 11 (5.2%) | 0 (0%) | 0 (0%) | 2 (0.9%) | |
n/a: Not available.
DISCUSSION
The pooled overall complication rate in SI fundoplication was calculated at the level of 5.2%, validating thus the safety profile of the single port approach. This is in accordance to the current literature, where morbidity rate of minimal invasive fundoplication is estimated at 7%-12%[7,33]. In addition to this, a very small percentage (0.9%) of the operated patients developed incisional hernia at the port site. Based on the included studies, the mean operative time was 136.3 minutes. Although SI Nissen and Dor operative times were comparable (130.71 and 138.3, respectively), the duration of SI Toupet procedure was longer (145 min). According to the study of Peters et al[7], the mean operative time of laparoscopic fundoplication was 112.59 minutes. These results, validate the elongation of the procedure time, when the SI approach is implemented. The high multiport conversion rate, reported in previous trials[14], was not confirmed in our review (12.9%). More specifically, Rao et al[34], reported that the multiport conversion rate in SI surgery ranges from 2% to 40%. In contrast to the considerable treatment failure rates (14.4%) in laparoscopic fundoplication[7], in our review, recurrence of symptoms in SI, were minimal. Similarly our findings show a comparable LOS (2.49 ds) in SI fundoplication, considering the respective hospitalization duration (4 d) in the multi port approach[7].
Despite the advantages derived from laparoscopy, minimal invasive techniques require the completion, of a steeper learning curve by the operating surgeon, in order to be performed safely and efficiently[35-37]. Through systematic repetition of the operative steps, the surgeon accumulates the necessary technical skills and achieves proficiency[36,37]. The clinical relevance of these, is that the operative volume and the location of an individual on the learning curve is directly associated with postoperative outcomes[38]. More specifically, in laparoscopic fundoplication the estimated learning curve cut-off value is approximately 20 patients[39,40]. SI fundoplication is technically more demanding and as so, a larger number of cases would be regarded as necessary for achieving adequacy. According to Ross et al[32], multiport conversion rates in SI Dor fundoplication were minimized after 60 patients, whereas the learning curve for SI Nissen and Toupet fundoplication was calculated at 25 cases[41]. In our review, single port adequacy, was scarcely reported[24,26,27]. Since previous experience is linked to perioperative endpoints, like operative time, conversion rate and morbidity, future studies should systematically report the learning curve status of the surgical team.
Although fundoplication is considered by many as a straightforward procedure, the respective minimal invasive application requires the possession of advanced skills, like laparoscopic suturing. Secure laparoscopic knot tying is a difficultly acquired dexterity and it can make the difference between an uneventful postoperative period and an increased morbidity rate[42,43]. Therefore, in order to reduce operative time and complement the inexperience of younger surgeons in intracorporeal knotting, endoscopic suturing devices have been imported in clinical practice, with comparable results[44-46]. In SILS, the limited working area, the restricted vision, the minimization of the manipulation angle and the parallelization of the optics and hand instruments increases the overall difficulty level[47,48]. In single port fundoplication, intracorporeal suturing has been extensively performed[17,23,25,29,32] with various techniques, like side-winding and the utilization of articulating graspers and needle holders[49]. Alternative approaches were the extracorporeal formation of a knot, with the subsequent completion through a suture passer[22] and the use of suturing devices[11,12,17,18,20].
Besides experience with the minimal invasive techniques, successful completion of the intracorporeal laparoscopic operative steps, like suturing or dissection, is associated with the intraoperative setting of the hand instruments. In single port surgery, the access point is usually umbilicus, through which the working ports are introduced[34]. As a result, the working angle, which should optimally be at about 60o, is significantly reduced[50,51]. Moreover, in operations like fundoplication, where the distance between the operating site and the access point is increased, the working angle further decreases, and with the synchronous alterations of the elevation angle, the derived ergonomic stress further escalates[48,49]. Therefore, in order to technically increase the manipulation angle, pre bent and articulating instruments have been introduced. Despite the fact that, simulation studies displayed a difficulty of novice surgeons in using articulating instruments[52], the combination of an dynamically bending and a pre bent tool minimizes the task completion time[53]. In the setting of SI fundoplication, both the standard[14,21,22,27,28,30] and the articulating setup[11,12,18,27,32] has been applied. Dapri et al[23,54], proposed the use of specialized reusable pre bent instruments that enabled intracorporeal and extracorporeal triangulation, thus avoiding conflict between the instruments and the scope.
Moreover, adequate exposure of the working field is another important factor for the performance of the operative tasks. The efficient displacement of the left liver lobe is a crucial step in SI fundoplication and therefore numerous techniques have been devised. The most simple method, is the use of a working instrument such as forceps[14] or graspers[23]. Commercially available retractors have been extensively utilized[17,18,32]. A long Veress needle has been, also, used as a retractor[12]. Similarly, relocating of left lobe by silicon drains and elastic loops was described in various cases[14,19,21,28,29]. Nakajima et al[27], after applying a silk thread in the left triangular ligament with a suturing device, suspended the liver lobe in the epigastric region. Furthermore, Galvani et al[24], used an internal retraction device, which after applying the retraction clip in the pars flaccida, the hook part was placed in the falciform ligament or the parietal peritoneum. The role of cyanoacrylate glue as a retracting method has been also studied[25]. According to Wu et al[25], the adhesion of the left liver lobe on the diaphragm, using cyanoacrylate glue, is a fast, safe and totally reversible technique.
Since our study is a systematic review of previously published trials, the validity of its estimations is inherently influenced by the methodology of the eligible studies. In this case, the majority of the included trials consisted of, either case reports, or retrospective analyses and only a few prospective studies were identified. In addition to this, most of these series incorporated a small sample size, thus inhibiting the strength of our results. Due to the fact that the learning curve is directly associated with the postoperative outcomes, another bias introducing factor could possibly be the inconsistent reporting of the number of the operating surgeons and their experience in single port surgery. Finally, although the identification of the various technical methodologies was considered as an endpoint in our study, the existence of these variations contributes in the overall heterogeneity levels.
Our study is an attempt to provide an overview regarding the application of SI fundoplication. Pooled results validate the safety and efficacy of the single port approach, although the technique is not yet standardized and many methodological variations have been described. The majority of the trials reporting on SI fundoplication were case reports and studies of a low quality level, without a comparison arm of the conventional multi port procedure and other methodological variations. Therefore, further randomized controlled trials, of a larger sample size are required, in order to draw a safe conclusion considering the application of SI fundoplication.
ARTICLE HIGHLIGHTS
Research background
The implementation of the minimal invasive principles in fundoplication resulted in reduced length of hospital stay, overall morbidity, and earlier return to daily activities. In order to further enhance the advantages of minimally invasive operations, single incision (SI) laparoscopic fundoplication was introduced.
Research motivation
Several studies comparing SI laparoscopic fundoplications to the conventional multiport approaches reported an increased operation duration, and high rates of multiport conversion and incisional hernia.
Research objectives
This study was designed in order to provide a comprehensive appraisal of the intraoperative technical variations and the postoperative outcomes in patients submitted to SI fundoplication.
Research methods
A systematic review of the literature available, in the electronic scholar databases (Medline, Scopus and Web of Science) was performed. All human trials that reported results on SI fundoplication, with an adult study population were considered eligible to be included in the study.
Research results
In total, 19 studies were included in this systematic review, comprising 266, 137 and 110 SI Nissen, Heller and Dor and Toupet fundoplications, respectively. Mean overall operation duration was 136.3 min. The total conversion rate to multiport laparoscopic fundoplication was 12.9%. Overall complication rate was 5.2%, while the rate of incisional hernia was 0.9%.
Research conclusions
The results of this systematic review confirm the safety and efficacy of the single port laparoscopic fundoplication, although the technique is not yet standardized.
Research perspectives
Due to the lack of high-quality studies, further well designed studies are necessary to determine the role of SI fundoplication.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: The authors declare no potential conflicts of interest.
PRISMA 2009 Checklist statement: This Systematic Review was conducted according to PRISMA Guidelines.
Peer-review started: February 11, 2019
First decision: February 26, 2019
Article in press: March 16, 2019
P-Reviewer: Amornyotin S, Morini S S-Editor: Ji FF L-Editor: A E-Editor: Zhang YL
Contributor Information
Konstantinos Perivoliotis, Department of Surgery, University Hospital of Larissa, Larissa 41110, Greece.
Chamaidi Sarakatsianou, Department of Anesthesiology, University Hospital of Larissa, Larissa 41110, Greece.
Konstantinos Tepetes, Department of Surgery, University Hospital of Larissa, Larissa 41110, Greece.
Ioannis Baloyiannis, Department of Surgery, University Hospital of Larissa, Larissa 41110, Greece. ibalogian@med.uth.gr.
References
- 1.Nissen R. [A simple operation for control of reflux esophagitis] Schweiz Med Wochenschr. 1956;86:590–592. [PubMed] [Google Scholar]
- 2.Iwakiri K, Kinoshita Y, Habu Y, Oshima T, Manabe N, Fujiwara Y, Nagahara A, Kawamura O, Iwakiri R, Ozawa S, Ashida K, Ohara S, Kashiwagi H, Adachi K, Higuchi K, Miwa H, Fujimoto K, Kusano M, Hoshihara Y, Kawano T, Haruma K, Hongo M, Sugano K, Watanabe M, Shimosegawa T. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol. 2016;51:751–767. doi: 10.1007/s00535-016-1227-8. [DOI] [PubMed] [Google Scholar]
- 3.Andolfi C, Plana A, Furno S, Fisichella PM. Paraesophageal Hernia and Reflux Prevention: Is One Fundoplication Better than the Other? World J Surg. 2017;41:2573–2582. doi: 10.1007/s00268-017-4040-5. [DOI] [PubMed] [Google Scholar]
- 4.Amer MA, Smith MD, Khoo CH, Herbison GP, McCall JL. Network meta-analysis of surgical management of gastro-oesophageal reflux disease in adults. Br J Surg. 2018;105:1398–1407. doi: 10.1002/bjs.10924. [DOI] [PubMed] [Google Scholar]
- 5.Du X, Wu JM, Hu ZW, Wang F, Wang ZG, Zhang C, Yan C, Chen MP. Laparoscopic Nissen (total) versus anterior 180° fundoplication for gastro-esophageal reflux disease: A meta-analysis and systematic review. Medicine (Baltimore) 2017;96:e8085. doi: 10.1097/MD.0000000000008085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Litle VR. Laparoscopic Heller myotomy for achalasia: a review of the controversies. Ann Thorac Surg. 2008;85:S743–S746. doi: 10.1016/j.athoracsur.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Peters MJ, Mukhtar A, Yunus RM, Khan S, Pappalardo J, Memon B, Memon MA. Meta-analysis of randomized clinical trials comparing open and laparoscopic anti-reflux surgery. Am J Gastroenterol. 2009;104:1548–61; quiz 1547, 1562. doi: 10.1038/ajg.2009.176. [DOI] [PubMed] [Google Scholar]
- 8.Westebring-van der Putten EP, Goossens RH, Jakimowicz JJ, Dankelman J. Haptics in minimally invasive surgery--a review. Minim Invasive Ther Allied Technol. 2008;17:3–16. doi: 10.1080/13645700701820242. [DOI] [PubMed] [Google Scholar]
- 9.Allaix ME, Patti MG. Heller myotomy for achalasia. From the open to the laparoscopic approach. World J Surg. 2015;39:1603–1607. doi: 10.1007/s00268-014-2914-3. [DOI] [PubMed] [Google Scholar]
- 10.Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997;84:695. doi: 10.1002/bjs.1800841126. [DOI] [PubMed] [Google Scholar]
- 11.Hamzaoglu I, Karahasanoglu T, Aytac E, Karatas A, Baca B. Transumbilical totally laparoscopic single-port Nissen fundoplication: a new method of liver retraction: the Istanbul technique. J Gastrointest Surg. 2010;14:1035–1039. doi: 10.1007/s11605-010-1183-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hawasli A, Holman AK. Single incision laparoscopic Nissen fundoplication: step by step. Surg Laparosc Endosc Percutan Tech. 2011;21:e78–e80. doi: 10.1097/SLE.0b013e31820d6491. [DOI] [PubMed] [Google Scholar]
- 13.Sharp NE, Vassaur J, Buckley FP., 3rd Single-site Nissen fundoplication versus laparoscopic Nissen fundoplication. JSLS. 2014;18:pii: e2014.00202. doi: 10.4293/JSLS.2014.00202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fukuda S, Nakajima K, Miyazaki Y, Takahashi T, Makino T, Kurokawa Y, Yamasaki M, Miyata H, Takiguchi S, Mori M, Doki Y. Laparoscopic surgery for esophageal achalasia: Multiport vs single-incision approach. Asian J Endosc Surg. 2016;9:14–20. doi: 10.1111/ases.12226. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sukharamwala P, Teta A, Ross S, Co F, Alvarez-Calderon G, Luberice K, Rosemurgy A. Over 250 Laparoendoscopic Single Site (LESS) Fundoplications: Lessons Learned. Am Surg. 2015;81:870–875. [PubMed] [Google Scholar]
- 18.Barbaros U, Demirel T, Sumer A, Deveci U, Tukenmez M, Cansunar MI, Kalayci M, Dınccag A, Seven R, Mercan S. Pure SILS Floppy Nissen Fundoplication with Hiatal Repair: A Case Report. ISRN Gastroenterol. 2011;2011:347487. doi: 10.5402/2011/347487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miyazaki Y, Nakajima K, Yamasaki M, Miyata H, Kurokawa Y, Takiguchi S, Fujiwara Y, Mori M, Doki Y. Single-port laparoscopic surgery of the distal esophagus: initial clinical experience. Surg Laparosc Endosc Percutan Tech. 2012;22:e118–e121. doi: 10.1097/SLE.0b013e318247c45f. [DOI] [PubMed] [Google Scholar]
- 20.Eyuboglu E, Ipek T, Atasoy D. Single-port laparoscopic floppy Nissen fundoplication: a novel technique with the aid of the Cerrahpasa retractor. J Laparoendosc Adv Surg Tech A. 2012;22:173–175. doi: 10.1089/lap.2011.0349. [DOI] [PubMed] [Google Scholar]
- 21.Mizuno M, Kobayashi M, Sasaki A, Nakajima J, Wakabayashi G. Early experience with single-incision laparoscopic Nissen fundoplication for gastroesophageal reflux disease in patients with mental retardation via a gastrostomy site incision: report of five cases. Surg Today. 2012;42:601–604. doi: 10.1007/s00595-012-0120-1. [DOI] [PubMed] [Google Scholar]
- 22.Yilmaz H, Alptekin H, Şahin M. Single-incision laraposcopic Nissen fundoplication for gastroesophageal reflux disease using conventional instruments. Turkiye Klin J Med Sci. 2013;33:1022–1027. doi: 10.5336/medsci.2012-31954. [DOI] [Google Scholar]
- 23.Dapri G, Bruyns J, Himpens J, Cadière GB. Single-access transumbilical laparoscopic nissen fundoplication performed with new curved reusable instruments. Surg Innov. 2011;18:61–65. doi: 10.1177/1553350610384406. [DOI] [PubMed] [Google Scholar]
- 24.Galvani CA, Garza U, Echeverria A, Kaul A, Samamé J. Multipurpose internal retractor for Single-incision surgery (SIS): single-institution case series. Surg Laparosc Endosc Percutan Tech. 2014;24:e59–e62. doi: 10.1097/SLE.0b013e31828f720d. [DOI] [PubMed] [Google Scholar]
- 25.Wu S, Yu H, Fan Y, Kong J, Yu X. Liver retraction using n-butyl-2-cyanoacrylate glue during single-incision laparoscopic upper abdominal surgery. Br J Surg. 2014;101:546–549. doi: 10.1002/bjs.9446. [DOI] [PubMed] [Google Scholar]
- 26.Agaba EA, Rainville H, Ikedilo O, Vemulapali P. Incidence of port-site incisional hernia after single-incision laparoscopic surgery. JSLS. 2014;18:204–210. doi: 10.4293/108680813X13693422518317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakajima J, Sasaki A, Obuchi T, Baba S, Umemura A, Wakabayashi G. Single-incision laparoscopic Heller myotomy and Dor fundoplication for achalasia: report of a case. Surg Today. 2011;41:1543–1547. doi: 10.1007/s00595-010-4533-4. [DOI] [PubMed] [Google Scholar]
- 28.Yamada H, Yano T. Single incision laparoscopic approach for esophageal achalasia: A case report. Int J Surg Case Rep. 2013;4:1–4. doi: 10.1016/j.ijscr.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yano F, Omura N, Tsuboi K, Hoshino M, Yamamoto SR, Kashiwagi H, Yanaga K. Single-incision laparoscopic Heller myotomy and Dor fundoplication for achalasia: report of a case. Surg Today. 2012;42:299–302. doi: 10.1007/s00595-011-0089-1. [DOI] [PubMed] [Google Scholar]
- 30.Buckley FP, 3rd, Vassaur HE, Jupiter DC, Crosby JH, Wheeless CJ, Vassaur JL. Influencing factors for port-site hernias after single-incision laparoscopy. Hernia. 2016;20:729–733. doi: 10.1007/s10029-016-1512-8. [DOI] [PubMed] [Google Scholar]
- 31.Strzałka M, Matyja M, Matłok M, Migaczewski M, Budzyński P, Budzyński A. Application of the single access technique in laparoscopic surgery. Pol Przegl Chir. 2013;85:73–77. doi: 10.2478/pjs-2013-0013. [DOI] [PubMed] [Google Scholar]
- 32.Ross SB, Luberice K, Kurian TJ, Paul H, Rosemurgy AS. Defining the learning curve of laparoendoscopic single-site Heller myotomy. Am Surg. 2013;79:837–844. doi: 10.1186/1477-7819-11-171. [DOI] [PubMed] [Google Scholar]
- 33.Rosemurgy A, Paul H, Madison L, Luberice K, Donn N, Vice M, Hernandez J, Ross SB. A single institution's experience and journey with over 1000 laparoscopic fundoplications for gastroesophageal reflux disease. Am Surg. 2012;78:917–925. [PubMed] [Google Scholar]
- 34.Rao PP, Rao PP, Bhagwat S. Single-incision laparoscopic surgery - current status and controversies. J Minim Access Surg. 2011;7:6–16. doi: 10.4103/0972-9941.72360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramsay CR, Wallace SA, Garthwaite PH, Monk AF, Russell IT, Grant AM. Assessing the learning curve effect in health technologies. Lessons from the nonclinical literature. Int J Technol Assess Health Care. 2002;18:1–10. [PubMed] [Google Scholar]
- 36.Ferrarese A, Gentile V, Bindi M, Rivelli M, Cumbo J, Solej M, Enrico S, Martino V. The learning curve of laparoscopic holecystectomy in general surgery resident training: old age of the patient may be a risk factor? Open Med (Wars) 2016;11:489–496. doi: 10.1515/med-2016-0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tekkis PP, Senagore AJ, Delaney CP, Fazio VW. Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg. 2005;242:83–91. doi: 10.1097/01.SLA.0000167857.14690.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hopper AN, Jamison MH, Lewis WG. Learning curves in surgical practice. Postgrad Med J. 2007;83:777–779. doi: 10.1136/pgmj.2007.057190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yano F, Omura N, Tsuboi K, Hoshino M, Yamamoto S, Akimoto S, Masuda T, Kashiwagi H, Yanaga K. Learning curve for laparoscopic Heller myotomy and Dor fundoplication for achalasia. PLoS One. 2017;12:e0180515. doi: 10.1371/journal.pone.0180515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Okrainec A, Ferri LE, Feldman LS, Fried GM. Defining the learning curve in laparoscopic paraesophageal hernia repair: a CUSUM analysis. Surg Endosc. 2011;25:1083–1087. doi: 10.1007/s00464-010-1321-6. [DOI] [PubMed] [Google Scholar]
- 41.Ross SB, Choung E, Teta AF, Colibao L, Luberice K, Paul H, Rosemurgy AS. The learning curve of laparoendoscopic single-Site (LESS) fundoplication: definable, short, and safe. JSLS. 2013;17:376–384. doi: 10.4293/108680813X13654754535359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amortegui JD, Restrepo H. Knot security in laparoscopic surgery. A comparative study with conventional knots. Surg Endosc. 2002;16:1598–1602. doi: 10.1007/s00464-002-8545-z. [DOI] [PubMed] [Google Scholar]
- 43.Lim S, Ghosh S, Niklewski P, Roy S. Laparoscopic Suturing as a Barrier to Broader Adoption of Laparoscopic Surgery. JSLS. 2017;21:pii: e2017.00021. doi: 10.4293/JSLS.2017.00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Coleman KA, Adams S, Smeak DD, Monnet E. Laparoscopic Gastropexy Using Knotless Unidirectional Suture and an Articulated Endoscopic Suturing Device: Seven Cases. Vet Surg. 2016;45:O95–O101. doi: 10.1111/vsu.12570. [DOI] [PubMed] [Google Scholar]
- 45.Bermas H, Fenoglio M, Haun W, Moore JT. Laparoscopic suturing and knot tying: a comparison of standard techniques to a mechanical assist device. JSLS. 2004;8:187–189. [PMC free article] [PubMed] [Google Scholar]
- 46.Coleman KA, Monnet E. Comparison of laparoscopic gastropexy performed via intracorporeal suturing with knotless unidirectional barbed suture using a needle driver versus a roticulated endoscopic suturing device: 30 cases. Vet Surg. 2017;46:1002–1007. doi: 10.1111/vsu.12722. [DOI] [PubMed] [Google Scholar]
- 47.Ekçi B. A simple technique for knot tying in single incision laparoscopic surgery (SILS) Clinics (Sao Paulo) 2010;65:1055–1057. doi: 10.1590/S1807-59322010001000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ishiyama Y, Inaki N, Bando H, Yamada T. Assessment of Intracorporeal Suturing in Single-Port Surgery Using an Experimental Suturing Model. Indian J Surg. 2017;79:137–142. doi: 10.1007/s12262-016-1445-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chung do Y. The intracorporeal knot tying using rigid instruments in single-incision laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2013;23:e90–e92. doi: 10.1097/SLE.0b013e318274b278. [DOI] [PubMed] [Google Scholar]
- 50.Meng WC, Kwok SP, Leung KL, Chung CC, Lau WY, Li AK. Optimal position of working ports in laparoscopic surgery: an in vitro study. Surg Laparosc Endosc. 1996;6:278–281. doi: 10.1097/00019509-199608000-00006. [DOI] [PubMed] [Google Scholar]
- 51.Fingerhut A, Hanna GB, Veyrie N, Ferzli G, Millat B, Alexakis N, Leandros E. Optimal trocar placement for ergonomic intracorporeal sewing and knotting in laparoscopic hiatal surgery. Am J Surg. 2010;200:519–528. doi: 10.1016/j.amjsurg.2010.01.029. [DOI] [PubMed] [Google Scholar]
- 52.Riggle JD, Miller EE, McCrory B, Meitl A, Lim E, Hallbeck MS, LaGrange CA. Ergonomic comparison of laparoscopic hand instruments in a single site surgery simulator with novices. Minim Invasive Ther Allied Technol. 2015;24:68–76. doi: 10.3109/13645706.2014.946426. [DOI] [PubMed] [Google Scholar]
- 53.Sánchez-Margallo FM, Matos-Azevedo AM, Pérez-Duarte FJ, Enciso S, Martín-Portugués ID. Performance analysis on physical simulator of four different instrument setups in laparo-endoscopic single-site (LESS) surgery. Surg Endosc. 2014;28:1479–1488. doi: 10.1007/s00464-013-3337-1. [DOI] [PubMed] [Google Scholar]
- 54.Dapri G, Casali L, Bruyns J, Himpens J, Cadiere GB. Single-access laparoscopic surgery using new curved reusable instruments: initial hundred patients. Surg Technol Int. 2010;20:21–35. doi: 10.1007/s00464-011-1678-1. [DOI] [PubMed] [Google Scholar]