Abstract
Pancreatic ductal adenocarcinoma (PDAC) remains a deadly disease with no efficacious treatment options. PDAC incidence is projected to increase, which may be caused at least partially by the obesity epidemic. Significantly enhanced efforts to prevent or intercept this cancer are clearly warranted. Oncogenic KRAS mutations are recognized initiating events in PDAC development, however, they are not entirely sufficient for the development of fully invasive PDAC. Additional genetic alterations and/or environmental, nutritional, and metabolic signals, as present in obesity, type-2 diabetes mellitus, and inflammation, are required for full PDAC formation. We hypothesize that oncogenic KRAS increases the intensity and duration of the growth-promoting signaling network. Recent exciting studies from different laboratories indicate that the activity of the transcriptional co-activators Yes-associated protein (YAP) and WW-domain-containing transcriptional co-activator with PDZ-binding motif (TAZ) play a critical role in the promotion and maintenance of PDAC operating as key downstream target of KRAS signaling. While initially thought to be primarily an effector of the tumor-suppressive Hippo pathway, more recent studies revealed that YAP/TAZ subcellular localization and co-transcriptional activity is regulated by multiple upstream signals. Overall, YAP has emerged as a central node of transcriptional convergence in growth-promoting signaling in PDAC cells. Indeed, YAP expression is an independent unfavorable prognostic marker for overall survival of PDAC. In what follows, we will review studies implicating YAP/TAZ in pancreatic cancer development and consider different approaches to target these transcriptional regulators.
Keywords: Pancreatic cancer, Yes-associated protein and WW-domain-containing transcriptional co-activator with PDZ-binding motif, Oncogenic Kras, Obesity, Signaling network and loops
Core tip: The identification of signaling networks that underlie risk factor promoted pancreatic cancer development and progression is of paramount importance to prevent or intercept this lethal disease. Accumulating evidence suggests that several core signaling pathways downstream of oncogenic Kras, augmented by environmental conditions, e.g., obesity, converge on Yes-associated protein (YAP) and WW-domain-containing transcriptional co-activator with PDZ-binding motif (TAZ), transcriptional co-activators in the Hippo pathway. Statins and metformin, widely used Food and Drug Administration-approved drugs, show great promise to intercept this disease by disrupting or inhibiting this amplifying network at multiple points converging onto YAP/TAZ.
INTRODUCTION
Despite advances in our understanding of genetics and basic biology, imaging, surgical treatments, and adjuvant therapy, pancreatic ductal adenocarcinoma (PDAC), which represents 90% of all pancreatic cancers, is a disease with dismal prognosis with an overall 5-year survival rate of only about 7%[1]. The incidence in the general population is estimated to be 8 cases per 100000 person-years, and the worldwide mortality about 7 deaths per 100000 person-years[2,3]. PDAC is already the 3rd leading cause of cancer-related mortalities in the United States[4]. Indeed, deaths due to PDAC are predicted to increase markedly. Indeed, the disease is expected to become the 2nd leading cause of cancer-related mortality in the United States in the next few years[5]. Given that only a minority of patients diagnosed with PDAC are eligible for surgical intervention, the research is gradually shifting to identify novel approaches in early diagnosis, prevention and interception, a novel concept, which attempts stopping transformed cells from progressing to frank cancer[6-10]. The elucidation of the molecular mechanisms of risk-factor associated PDAC promotion will be of paramount importance to facilitate the discovery of novel targets and agents for prevention and identify robust biomarkers to stratify patients for selective and individualized therapeutics.
KRAS MUTATIONS AND PDAC
Oncogenic KRAS mutations were first reported to be associated with PDAC more than 30 years ago[11,12]. Although the genetic landscape of PDAC is complex, since the initial reports extensive research in both humans and mice have substantiated the critical significance of KRAS mutations in the early stages of PDAC. In fact, many studies have confirmed that over 90% of PDAC harbors KRAS mutations[13,14] and KRAS signaling is one of the core signaling pathways in human PDAC[13]. Most KRAS mutations in PDAC are found at position G12, of which the single amino acid replacement G12D is the most predominant[15]. Mutations at position G13 or Q61 have been detected at lower frequency, 21% or 28%, respectively[15]. Using deep whole exome sequencing an integrated genomic characterization of PDAC revealed several different KRAS mutations in a subset of tumors, with some PDACs showing biallelic mutations[16]. Mechanistically, mutations at position G12 with a single amino acid substitution induce conformational changes that interfere with the intrinsic GTPase activity of KRAS and prevent the interactions between KRAS and GTPase-activating proteins (GAPs), which stimulate the conversion of KRAS-GTP (active state) to KRAS-GDP (inactive state), thereby ending KRAS activation. In this manner, the KRAS mutations lead to its prolonged activation and consequently to the persistent stimulation of downstream signaling effectors[15,17]. It is becoming clear that different mutations of G12 lead to different conformational states that differ in their affinity for interacting effectors[18]. Although mutations in KRAS is an early and essential step in PDAC, it is insufficient to stimulate development of frank, invasive PDAC. Activation of other pathways by additional mutations (e.g., in tumor suppressor genes, including p53, p16 and SMAD4) or environmental stimuli, including obesity and metabolic syndrome are required for the promotion of invasive PDAC[19-24].
In addition, the “efficacy” of oncogenic KRAS to initiate and promote PDAC is influenced and modulated by the presence of common susceptibility genes. Recent genome-wide association studies (GWAS) of PDACs in populations of European ancestry have identified additional common pancreatic cancer risk loci carrying pancreatic cancer risk signals, including NR5A2, PDX1, AB0, NOC2L, HNF1B, GRP[25-28]. Moreover, an elegant study demonstrated that variations in oncogenic dosage have a critical role in PDAC biology and phenotypic diversification[29], with the highest oncogenic Kras levels underlying aggressive undifferentiated phenotypes. Activation of other pro-oncogenic pathways, including Myc, Yap1 or Nfkb2, which collaborate with heterozygous mutant Kras in driving tumorigenesis have been shown to have a lower metastatic potential[29]. It seems that evolutionary constraints direct oncogenic dosage gain and variation along defined routes to drive the early progression of PDAC and shape its downstream biology[29]. Integrated genomic and global gene expression analyses have classified human pancreatic cancers into several distinct subtypes that may dictate and predict clinical outcomes and therapeutic responses. Collison and colleagues defined three subtypes: classical, quasi mesenchymal, and exocrine-like[30], while Bailey et al[31] classified four subtypes: squamous, pancreatic progenitor, immunogenic, and aberrantly differentiated endocrine exocrine (ADEX). By separating tumor cells and stromal components, Moffitt and colleagues identified two stromal subtypes: normal and activated, and two tumor-specific subtypes: classical and basal-like[32]. Using whole genome sequencing and copy number variation analysis Waddell et al[33] categorized PDAC into four subclasses based on patterns of structural variation (variation in chromosomal structure): stable, locally rearranged, scattered, and unstable. Taken together, these large genomic efforts clearly demonstrate that pancreatic cancer is a genetically complex and heterogeneous disease, which has significant implications in prognosis and therapeutic response, and classifying pancreatic cancers into subtypes may assist and pave the way to more efficacious personalized treatment strategies.
PROGRESSION MODEL OF PDAC
It is estimated that PDACs develop over many years from non-invasive precursor lesions. The non-cystic lesion is called pancreatic intraepithelial neoplasia (PanIN) and is usually diagnosed in histological preparation of tissue removed during surgery or in biopsy specimens[34-37]. These PanINs progress from early PanIN-1 lesions to advanced PanIN-3 (carcinoma in situ) and finally to frank invasive PDAC. Besides this classical view of gradual step-wise PanIN progression and PDAC formation, in at least a subset of PDACs there seem to be catastrophic genetic events (e.g., chromothripsis) necessary for the transition from preinvasive to invasive PDAC (punctuated equilibrium)[38-41]. The pathological characteristics of cystic precursor lesions, including intraductal papillary mucinous neoplasm (IPMN) have been recently reviewed elsewhere[42]. Most low-grade PanIN lesions contain oncogenic KRAS mutations[43]. This finding provided further evidence in support of the step-wise carcinogenesis model, in which KRAS mutations are envisioned as initiating events[15,44,45].
Genetically engineered mouse models of PDAC have corroborated this paradigm[46-49]. In the KC model, mutated Kras is expressed from its endogenous locus (by crossing LSL-KrasG12D mice with PDX-1-Cre or p48-Cre mice, i.e., KC model)[48-50]. This KC mouse model shares similar histopathologic and genetic features to the human disease including the development and progression of PanINs[46]. In addition to the role of oncogenic KRAS in the initiation of PDAC, Kras mutations have also been shown to be important for PDAC maintenance[51,52]. In line with the notion that mutated Kras is necessary but not fully sufficient for the development of invasive PDAC, only few animals (5%-10%) in the KC model (without additional genetic alterations) develop frank PDAC very late (usually after 9 mo)[46]. Cell senescence has been proposed as a barrier to the malignant progression of tumors[53]. The formation of PDAC can be greatly accelerated by the presence of another mutation (e.g., Trp53)[47,54].
Besides additional genetic mutations, several studies have convincingly demonstrated that environmental, nutritional, and metabolic factors, including obesity, type-2 diabetes mellitus (T2DM) and inflammation efficiently promote PDAC formation[55-59]. This notion is substantiated by several preclinical studies. Expression of physiologic levels of oncogenic Kras in murine models efficiently transformed only a small percentage of cells[60]. KRAS downstream signaling molecules, including the ERKs were not activated when oncogenic Kras was expressed from its endogenous locus[61]. Accordingly, cell culture studies have shown that incubating PDAC cells in a serum-free medium failed to display activated ERK despite the presence of KRAS activating mutations in these cells. However, ERK activation could be induced by adding growth factors to the culture medium[62-64]. In mouse models, oncogenic Kras in adult mice was insufficient to induce PDAC, while concomitant induction of pancreatic inflammation (e.g., by administration of the cholecystokinin analog cerulein) stimulated the formation of PanINs and cancers[65]. Our own studies have clearly demonstrated that an obesogenic diet accelerated early PanIN progression and PDAC development in KC mice, which was associated with metabolic disturbances (e.g., hyperinsulinemia), increased pancreatic inflammation, and desmoplasia[55,56]. Taken together, the current evidence indicates that oncogenic Kras is indispensable but not sufficient to induce malignant pancreatic cells. Additional genetic or environmental factors (obesity, T2DM, inflammation) are required to elevate KRAS activity[52] and/or stimulate additional signaling pathways to promote PDAC formation[66].
Recent elegant gene-environment interaction studies have demonstrated that the increased risk of developing PDAC by environmental stimuli and conditions may be influenced by the presence of common genetic variations. A GWAS data analysis has found that genetic variations in inflammatory responses and insulin resistance may affect the risk of obesity- and diabetes-related pancreatic cancer[67]. It is apparent that a detailed understanding of the gene-regulatory networks that integrate signaling by KRAS and cooperating pathways to drive an oncogenic program in pancreatic cancer is of fundamental importance to design novel strategies to target this aggressive disease. Recent exciting studies from different laboratories indicate that the activity of the transcriptional regulators yes-associated Protein (YAP) and WW-domain-containing transcriptional co-activator with PDZ-binding motif (TAZ) play a critical role in the promotion and maintenance of PDAC. In what follows, we will review studies implicating YAP/TAZ in pancreatic cancer development and consider possible approaches to target these transcriptional regulators with emphasis in repurposing drugs that are currently in clinical use.
YAP/TAZ IN PANCREATIC CANCER
The Hippo pathway
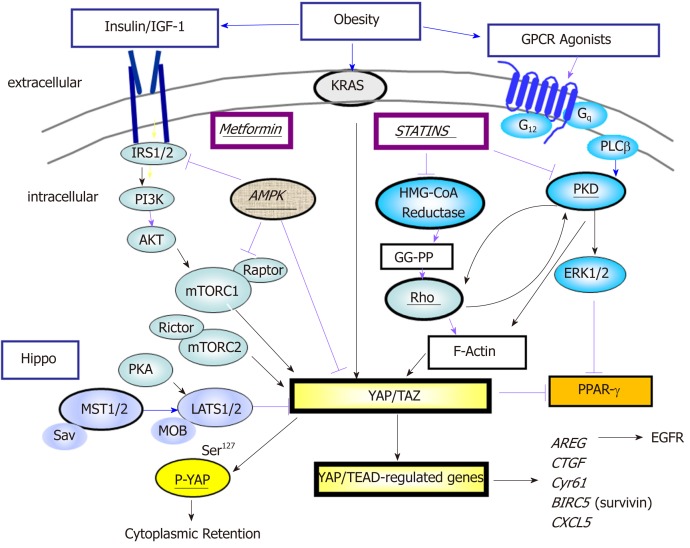
The highly conserved Hippo pathway, originally identified and characterized as potent growth-suppressive pathway in Drosophila[68], is a key regulatory mechanism in development, organ-size, tissue regeneration and tumorigenesis[68,69]. Canonical Hippo signals are transmitted via the serine/threonine kinases mammalian Ste20-like kinases 1/2 (Mst1/2), in complex with the scaffold protein salvador homolog 1 (Sav1), phosphorylate and activate large tumor suppressor 1/2 (Lats1/2), in complex with its regulatory protein Mps One binder 1/2 (MOB1/2)[69]. As shown in Figure 1, Lats1/2 then phosphorylates the transcriptional co-activators YAP and TAZ which also can function as novel sensors of the mevalonate and glycolytic pathways[70-72].
Figure 1.
Yes-associated protein and WW-domain-containing transcriptional co-activator with PDZ-binding motif is a point of convergence in signaling pathways. A network that involves activated Ras, G protein-coupled receptors (GPCRs) and tyrosine kinase receptors positively regulates Yes-associated protein and WW-domain-containing transcriptional co-activator with PDZ-binding motif (YAP/TAZ) activity via Rho/PKD/organization of the actin cytoskeleton and PI3K/AKT/mTORC1. The interaction of mTORC1 and YAP is explained in the text. In addition, the localization and activity of YAP/TAZ is negatively impacted by the Hippo pathway which mediates phosphorylation of YAP and thereby its cytoplasmic sequestration. Metformin and statins inhibit YAP/TAZ activity at different sites in the network. Stimulatory effects are shown by black arrows whereas inhibitory effects are indicated by red arrows. YAP/TAZ: Yes-associated protein and WW-domain-containing transcriptional co-activator with PDZ-binding motif; GPCR: G protein-coupled receptor.
The residues Ser127 and Ser397 of YAP are positioned within a consensus sequence (HXRXXS) phosphorylated by Lats1/2. The phosphorylation of YAP at these sites, restricts its cellular localization to the cytoplasm, reduces its stability, and inhibits its co-transcriptional activity. In addition to Lats1/2, YAP and TAZ can be phosphorylated by other protein kinases[68]. Although YAP and TAZ have very similar structural topologies, share nearly half of the overall amino acid sequence, and are thought to be largely redundant, they may differ in their regulation and downstream functions[73].
When the Hippo pathway is not functional, YAP localizes to the nucleus where it interacts with the TEA-domain DNA-binding transcription factors (TEAD 1-4). YAP/TEAD-regulated genes encode for proteins implicated many critical cellular processes, e.g., autocrine/paracrine proliferation via EGFR (AREG) and G protein-coupled receptors (EDN2), and interact with other developmental pathways activated in PDAC, including Wnt, Notch, and Hedgehog[74]. YAP/TAZ also induces epithelial-to-mesenchymal transition (EMT) and induces a more undifferentiated state to malignant cells. Accordingly, YAP/TAZ play an important role in pancreas development, which has implications for pancreatic regeneration, cancer, and diabetes[75]. It is accepted that YAP/TAZ acts as a potent oncogene in multiple cell types, including PDAC[76] and also contributes to the strong immunosuppressive microenvironment characteristic of mouse and human pancreatic cancer[77]. Recent findings indicate that YAP/TAZ opposes Ras-induced senescence by increasing the expression of the key enzymes involved in deoxyribonucleotide biosynthesis which are critical for DNA replication[78].
As indicated above, YAP and TAZ do not bind directly to DNA but act by enhancing the activity of transcription factors or other proteins that interact with DNA. Although TEAD family members are the major DNA-binding partners, YAP/TAZ can also bind to other transcription factors, e.g., RUNXs, p73, Smad1, Klf4, AP-1 to elicit context-specific functions[74,79,80]. It is important to point out that YAP and TAZ not only act as co-activators of transcription factors that bind to promoter sites contiguous to the gene that they control but exert regulatory effects via distant enhancer elements[81,82]. Furthermore, recent studies indicate that YAP/TAZ-bound to enhancers mediate the recruitment of the general coactivator bromodomain-containing protein 4 (BRD4) and RNA polymerase II at promoters regulated by YAP/TAZ, thereby enhancing expression of multiple growth-regulating genes[83]. It is evident that YAP and TAZ control gene-regulatory programs through a variety of mechanism, further supporting their fundamental role in cell signaling.
Regulation of YAP/TAZ in PDAC
Recent studies demonstrated that YAP is required for acinar-to-ductal metaplasia (ADM), an early event that precedes PanIN progression into PDAC in genetically engineered mouse models[84,85]. In addition, YAP is a major mediator of pro-oncogenic mutant p53[86] and p53 deficiency promotes YAP signaling trough Ptpn14[87]. Also, YAP confers resistance to RAF/MEK inhibitors[88] and chemotherapy in PDAC[89]. While initially thought to be primarily an effector of the tumor-suppressive Hippo pathway, more recent studies revealed that YAP/TAZ subcellular localization and co-transcriptional activity is regulated by multiple upstream signals including those mediated by various G protein-coupled receptors (GPCRs), tyrosine kinase receptors (EGFR, MET, Insulin/IGF-1 receptor), integrins, PI3K, mTOR, PKC, PKD, RHO and actin cytoskeleton, all of which stimulate YAP/TAZ transcriptional co-activator activity[66,69,76,90-92]. Recently, Src kinases, downstream of KRAS, have been shown to inhibit the Hippo pathway by directly phosphorylating Lats1 thereby activating YAP[93]. Interestingly, some of the tumor suppressive effects of wild type p53 appear to be exerted via inhibition of YAP1 function[87].
In human PDAC cells, YAP functions as a downstream effector of the crosstalk between insulin/IGF-1 receptor and GPCR systems[94] (Figure 1). We have demonstrated that stimulation with insulin and the GPCR agonist neurotensin induced rapid YAP nuclear import and markedly augmented the mRNA levels of YAP/TEAD-regulated genes, including CTGF and Cyr61. The growth-promoting agonists regulated YAP activity via PI3K and PKD in PANC-1 and MiaPaCa-2[94], human cell lines that correspond to the squamous/quasi mesenchymal/ basal-like sub-type of PDAC. In other cell types, several studies have also been shown that PI3K activation inhibits the Hippo pathway[95,96] thereby promoting YAP activity, and PKD mediates YAP nuclear localization and activation of YAP/TEAD-regulated gene expression[90]. Overall, YAP has emerged as a central node of transcriptional convergence in growth-promoting signaling in PDAC cells (Figure 1). In addition to rapid regulation via phosphorylation and sub-cellular localization, additional pathways and epigenetic stimuli modulate YAP/TAZ protein expression. In this context, it has been shown that the RAS pathway, independently of the Hippo cascade, enhances YAP1 stability through downregulation of the ubiquitin ligase complex substrate recognition factors SOCS5/6[97]. Moreover, the eukaryotic translation initiation factor 5A (eIF5A), which is up-regulated by KRAS in PDAC, interacts with the tyrosine kinase PEAK1 leading to enhanced YAP expression[98].
The nutrient sensor mTORC1, a central downstream component of the PI3K/AKT and RAF/MEK/ERK pathways, is implicated in the development of multiple types of cancer, including PDAC[99]. Interestingly, YAP and mTORC1 form a positive feedback loop that leads to enhanced YAP protein expression. Specifically, YAP stimulates mTORC1 via increasing the activity of the PI3K pathway[100] and augmented amino acid transport[101,102]. In turn, mTORC1 activation leads to YAP accumulation at least in part, via decreased autophagy[103]. Importantly, amplification and overexpression of YAP has been shown to bypass the need of mutant Kras in murine PDAC[104] and other cancer cell types[105] though the mechanism(s) differ(s), probably reflecting cell-context factors[106]. These finding indicates that YAP not only acts downstream of KRAS but also that YAP can sidestep the need of KRAS mutant expression in PDAC[107].
Several studies in different cell types demonstrated that an increase in the intracellular level of cAMP inhibits YAP activation, at least in part through activation of protein kinases of the Hippo pathway[108,109]. Interestingly, concomitant expression of mutated (R201C) GNAS, which encodes for stimulatory G-protein alpha subunit that increases cAMP synthesis, with oncogenic Kras in mice, induced the formation of pancreatic cystic neoplasms, resembling human intraductal papillary mucinous neoplasms (IPMN), a less aggressive histological subtype of pancreatic tumors, by inhibiting YAP signaling[110]. These recent findings underscore the importance of YAP activation in the development of specifically PDAC. In this regard, it is of great interest that YAP function has been associated with the squamous/quasi mesenchymal/basal-like sub-type of PDAC (discussed above), considered the most clinically aggressive form. The significance of YAP expression in human PDAC is discussed in the next section.
An important feature of human and murine PDAC is an extensive desmoplastic stroma[111] that increases the stiffness of the extracellular matrix (ECM) surrounding the epithelial cancer cells[42]. The Hippo/YAP pathway has been recognized to play a critical role in mechano-transduction[112,113] and in sensing ECM stiffness[114] but the mechanisms involved are not fully understood. Recently, the Ras-related GTPase RAP2 has been identified as a major sensor of mechanical cues from the ECM. At low stiffness, RAP2 activates the Hippo kinases Lats1/2 thereby inhibiting YAP/TAZ activity[115]. Therefore, high stiffness leads to inhibition of the Hippo tumor suppressive pathway, thus enhancing the co-activator activity of YAP and TAZ. Reciprocally, increased expression of a number of YAP/TEAD-regulated genes, including CTGF, Cyr61 and CXCL5 contribute to shaping the stroma of PDAC, thus establishing an important amplification loop involving the tumor microenvironment leading to the stimulation of PDAC development.
YAP and human PDAC
Several studies reported that YAP and TAZ are over-expressed and over-active in human PDAC[104,116,117] and identified YAP expression as an independent prognostic marker for survival of PDAC[118]. We have examined the prognostic value not only of YAP but also of upstream and downstream components of the YAP-driven network in pancreatic cancer[119]. We confirmed that higher expression of YAP is significantly associated with unfavorable prognosis (survival) in PDAC[120]. Indeed, none of the patients of the population with higher levels of YAP mRNA expression survived for 5 years while 32% of the subset with the lower levels of YAP mRNA survived for 5 years or more. In addition, multiple genes regulated by YAP/TEAD, including AJUBA, ANLN, AREG, ARHGAP19, ARHGAP29, AURKA, BUB1, CCND1, CDK6, CXCL5, DKK1, JAG1, NOTCH2 and RHAMM were significantly associated with unfavorable prognosis in PDAC[120]. In a further analysis of the data, we verified that the expression of each of these genes was positively and significantly correlated with the expression of YAP in PDAC. In contrast, genes in pathways, e.g., LKB/AMPK and cAMP/PKA, that oppose YAP action, including STRAD, MARK1, PKA, are associated with favorable prognosis in PDAC patients[120]. Similar results were obtained using other web-based tools, such as Gene Expression Profiling Interactive Analysis[121].
YAP and obesity
Besides its recognized role in the regulation of growth and development, recent studies show that Hippo kinases and YAP/TAZ transcriptional coactivators, are regulated by metabolism and conversely that the Hippo/YAP pathway controls metabolic processes in physiological and pathologic conditions, including obesity and T2DM[122,123]. In fact, cellular metabolites and metabolic pathways, e.g., glucose and free fatty acids, regulate the Hippo pathway. Glucose metabolism through the glycolytic pathway activates phosphofructokinase 1 (PFK1), a key rate-limiting enzyme of glycolysis. In turn, PFK1 interacts with TEAD, thereby regulating YAP/TEAD complex formation and expression of YAP/TEAD-regulated genes[70]. Furthermore, O-linked β-N-acetylglucosamine (O-GlcNAc) is another post-translational mechanism by which a sugar is attached to serine residues of nuclear or cytoplasmic proteins and modifies protein activity[124]. Indeed, the attachment of O-GlcNAc to Ser109 of YAP stimulates its transcriptional co-activator activity by interfering with the interaction of YAP with Lats1/2, thus protecting YAP from inhibitory phosphorylation and providing a novel mechanism linking glucose availability to YAP activity[125]. This multilayered regulation of YAP activity by glucose metabolism is potentially important in the obese state, which often is accompanied by insulin resistance and elevated glucose levels.
A characteristic and defining feature of obesity is the enlargement of adipose tissue depots, which is often accompanied by adipose tissue (AT) inflammation[126]. Dysfunctional adipose tissue with alterations of adipokine production, ectopic fat storage, and AT inflammation are thought to be critical, pathophysiological processes underlying the development of insulin resistance. Adipocytes and adipose tissue macrophages are central cellular players of AT inflammation[127-132]. The Hippo pathway has been shown to modulate adipocyte proliferation and differentiation, with YAP/TAZ nuclear localization stimulating proliferation and suppressing adipogenesis[133-136]. As depicted in Figure 1, nuclear YAP/TAZ interacts with and inhibits PPAR-γ, a major pro-adipogenic transcription factor, thereby suppressing adipocyte differentiation[133,137]. In that context, hyperglycemia and advanced glycation end products impair adipogenesis by upregulating and activating YAP[138].
There are few studies investigating the importance of YAP/TAZ in macrophage polarization[139]. It has been shown that the cell shape, independent of cytokines present in the micromilieu, has a profound influence on macrophage polarization via the actin cytoskeleton[140], which strongly suggests an important role of YAP/TAZ in this process due to the critical function or YAP/TAZ as mechano-sensors and mechano-transducers[112,113]. In addition, adipose tissue in obese subjects is characterized by peri-adipocyte fibrosis with elevated levels of CTGF (connective tissue growth factor)[141], a recognized product of YAP/TEAD transcriptional activity. Our own studies have shown that YAP is overexpressed in mesenteric adipose tissue of obese KC mice (unpublished). Taken together, an important role of YAP/TAZ in adipose tissue inflammation during obesity emerges, which might have important implications in the PDAC promoting effects of obesity[142,143].
Strategies to inhibit YAP/TAZ in pancreatic cancer
As indicated above, YAP hyper-activation can evade the need of KRAS mutant expression in PDAC[107]. Thus, even if Ras could be effectively inhibited by new therapies, YAP amplification could provide a potential pathway to tumor recurrence. Given that YAP is as a key element not only downstream of Ras but also an alternative route to bypass the need of this oncogene for tumor relapse, YAP is emerging as a fundamental target in PDAC. Although targeting transcription factors or their co-activators has proven difficult, recent studies suggest novel approaches to inhibit YAP/TAZ activity with drugs in clinical use, including statins and metformin in PDAC and other malignancies.
Statins
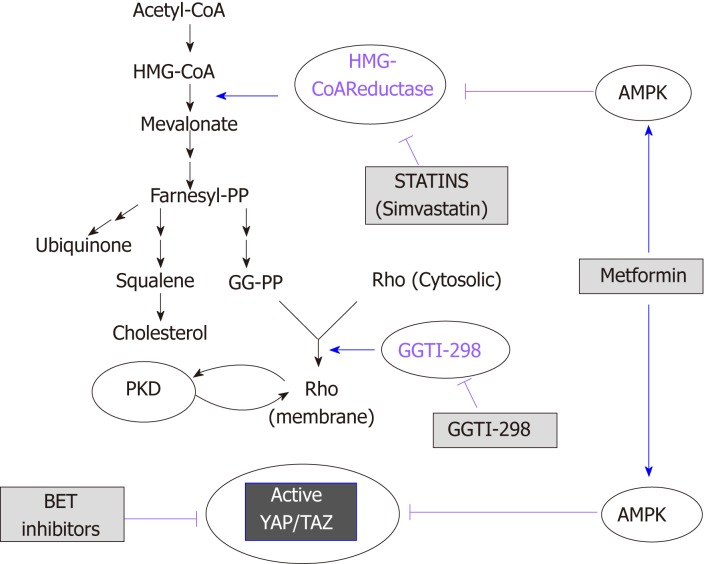
Several studies demonstrated activation of the pathway leading to mevalonate biosynthesis in epithelial cancers through mutant p53[144-146] and AKT/mTORC1[146]. Statins, which have been used to treat dyslipidemia and prevent heart diseases, selectively inhibit 3-hydroxy-methylglutaryl (HMG) CoA reductase[147], the rate-limiting enzyme in the generation of mevalonate (Figure 2). Mevalonate is a precursor for the generation of important lipids and lipid intermediates, including farnesyl pyrophosphate (FPP), geranylgeranyl pyrophosphate (GG-PP) and cholesterol. The function and activity of small GTPases of the Rho family, including Rho A and C, depend on the transfer of the geranylgeranyl moiety of GG-PP to a cysteine in their COOH-terminal region. Active Rho plays a critical role in YAP/TAZ activation through actin remodeling in several cell populations[69] (Figure 2). Accordingly, increased expression of RHOA and RHOC is associated with unfavorable prognosis in patients with PDAC.
Figure 2.
Schematic overview of the mevalonate pathway. The scheme illustrates the site of action of statins, metformin and bromodomain and extra-terminal domain inhibitors (see text for details). BET: Bromodomain and extra-terminal domain; AMPK: AMP-activated protein kinase; GG-PP: Geranylgeranyl pyrophosphate.
Numerous epidemiological studies have concluded that statin use is correlated with beneficial effects in PDAC[148-156], especially in men[151,152]. A large study demonstrated that statins were associated with a significantly reduced PDAC risk (by 34%) with a stronger effect in males[151]. The beneficial effects of statins depend on the type of statins used, with several reports showing positive associations with lipophilic (and not hydrophilic) statins and reduced cancer risk[157-160]. However, a recent study, in which statin use was self-reported and the type of statins was not documented in early cohorts, failed to detect an effect of statins in lowering PDAC risk[161]. The same authors published a follow up study of the same dataset, in which they reported an increased survival in PDAC patients with regular pre-diagnosis use of statins[162]. Recently, a meta-analysis of PDAC risk that included more than 3 million participants and 170000 pancreatic cancer patients has been published[163]. This study indicates a significant decrease in pancreatic cancer risk with statin use, thus reinforcing the conclusion that statin administration is associated with beneficial effects in PDAC patients. In addition to their potential efficacy in primary prevention and interception, statins may improve the outcome of patients after surgical removal of their primary PDAC[148,149,164], indicating a possible role of statins in the prevention of PDAC recurrence.
In preclinical studies[165,166], statins delayed progression of PDAC in mice harboring KrasG12D. Statins were identified as potential YAP inhibitors by screens of molecules that changed the nuclear/cytoplasmic distribution of YAP[167]. Our own experiments using PDAC cells also indicated that lipophilic statins induce cytoplasmic localization of YAP and markedly inhibited YAP/TEAD-regulated genes, proliferation, and colony formation by PDAC cells (submitted for publication). Taken together, converging evidence from epidemiological and preclinical studies indicates a protective effect of statins in PDAC.
Metformin
1,1-dimethylbiguanide hydrochloride (metformin) is the most widely administered drug for the treatment of T2DM worldwide[168,169]. The anti-diabetic, i.e., lowering the blood glucose levels, actions of metformin are mediated systemically by a reduction of hepatic glucose production and output into the circulation and improvement of insulin sensitivity via increasing cellular uptake of glucose in skeletal muscles and adipose tissue[170]. In addition to lowering blood glucose levels, metformin decreased the levels of insulin and IGF-1 in both diabetic and non-diabetic patients[171,172]. Multiple epidemiological studies showed an association of metformin with reduced incidence, recurrence and mortality of cancer in patients with T2DM[173-182]. However, a therapeutic efficacy of metformin has not been observed in all studies[183], in particular in late-stage, advanced cases of cancer. In that context, recent meta-analyses supported the notion that the beneficial effects of metformin depend on the stage of the tumor, with a substantially enhanced survival in patients with local, non-metastatic, disease[178,184]. Further reports indicated that metformin administered to T2DM patients could be also beneficial in secondary chemoprevention, i.e. after surgical resection of the cancer in the pancreas[185,186].
The mechanism of action of metformin remains incompletely understood. Besides its systemic (glucose lowering) effects, at the cellular level metformin indirectly activates AMP-activated protein kinase (AMPK)[187], though other AMPK-independent mechanisms are also operational[188,189]. AMPK is activated by phosphorylation by the tumor suppressor LKB-1/STK11 in the activation loop[190] when cellular ATP levels decrease and 5’-AMP and ADP concentrations increase[169]. It generally thought that metformin leads to AMPK activation by directly inhibiting complex I of the mitochondrial respiratory chain[191,192], which leads to a decrease in ATP synthesis resulting in increased AMP and ADP thereby leading to AMPK activation. AMPK suppresses cellular proliferation by inhibiting the function of mTORC1 through several mechanisms. AMPK activates TSC2 by phosphorylation on Ser1345[193-195], which leads to an accumulation of inactive Rheb-GDP thereby inhibiting mTORC1. AMPK can also inhibit mTORC1 function by phosphorylation of Raptor, which disrupts its complex with mTOR[196]. In addition, mTORC1 activation induced by insulin/IGF-1 signaling is also inhibited via phosphorylation of IRS-1 on Ser794 by AMPK, a phosphorylation that impedes PI3K activation[197,198]. We demonstrated that metformin, at low concentrations, activates AMPK in PDAC cells[199,200] and inhibits mTORC1, ERK and DNA synthesis via AMPK[199-201]. Metformin also reduced the rate of growth of PDAC xenografts[202,203]. Furthermore, we recently reported that oral administration of metformin strikingly prevented the increase in PDAC incidence in KC mice with diet-induced obesity[204]. This effect was associated with an increase in pancreatic AMPK activity (as measured by ACC Ser79 phosphorylation), and decrease in phospho MEK1/2 (Ser217/221), phospho S6 (Ser235/236), and phospho ERK1/2 (Thr202, Tyr204)[204]. In that context, berberine, a natural compound that activates AMPK and inhibits ATP production, also inhibited mTORC1, ERK, DNA synthesis and proliferation of pancreatic cancer cells and reduced the growth of PDAC xenografts[201].
Recent evidence indicates that AMPK also opposes YAP activity via multiple mechanisms, including direct YAP phosphorylation on Ser94[205,206], a residue that is important for the interaction of YAP with TEAD. In addition, AMPK has been shown to phosphorylate HMG-CoA reductase (Ser872), thereby inhibiting its activity and reducing mevalonic acid synthesis[207]. Furthermore, AMPK phosphorylates and activates upstream regulators of the Hippo pathway[208]. The inhibitory effects of AMPK on the YAP/TAZ pathway is illustrated in Figure 2. These studies suggest an important direct link among adenine nucleotide levels, AMPK and YAP/TAZ activity. In studies from our laboratories, we found recently that diet-induced obesity markedly increased pancreatic TAZ expression in KC mice and that oral metformin prevented the increase in YAP/TAZ[204]. Given that statins and metformin inhibit YAP activation through different mechanisms, it is logical to speculate that administration of a combination of these FDA-approved drugs will suppress YAP/TAZ activity and exerts PDAC-protective activity. The scheme presented in Figure 1 dramatizes this notion by showing that statins and metformin reach YAP through different pathways.
Inhibitors of BRD4: A new approach for targeting YAP/TAZ
BRD4, which interacts with acetyl-lysine, acts as a critical regulator of the expression of selected subsets of genes. Bromodomain and extra-terminal domain (BET) inhibitors interfere with the proliferation of PDAC cells, raising the possibility that BET proteins may be new targets for PDAC therapy[209]. A recent elegant study demonstrated a direct physical interaction between YAP or TAZ and BRD4, as revealed by co-immunoprecipitation experiments. The data imply that YAP, TEAD and BRET-containing proteins (e.g., BRD4, BRD2) form a multi-molecular complex in the nucleus[83]. Consistent with the notion that BRD4 plays a critical role in YAP/TAZ function, the BET cell-permeable inhibitor JQ1[210] downregulates the expression of YAP/TAZ-regulated genes[83]. Considerable efforts are being made to develop new inhibitors of BRD proteins and thus this field will develop rapidly[211]. These new findings suggest a novel approach to target YAP/TAZ that remains to be tested experimentally in vivo, using models of PDAC. As suggested by Figure 2, the possibility of using BET inhibitors in combination with statins and/or metformin is attractive and warrants further experimental work.
Feedback loops and effect of pathway inhibitors
Most signaling pathways are subjected to potent feedback loops that adjust the activity and function of the signaling network. There is evidence that besides their stimulating effects on mitogenic signaling the mTORC1/S6K and RAF/MEK/ERK pathways also mediate robust negative feedback loops that restrict the activity of insulin/IGF-1, EGFR, and other tyrosine kinase receptors[99]. In that context, the mTORC1/S6K pathway inhibits the function of IRS-1 by phosphorylating several residues (Ser636/639 by mTORC1 and Ser307/636/1001 by S6K)[212]. Inhibitors of mTORC1/S6K or MEK/ERK suppress these feedback loops, which in turn causes a compensatory activation of upstream signaling molecules, e.g., PI3K, AKT, and ERK that as a consequence strongly counteract the anti-proliferative actions of these inhibitors[99,200,213]. The up-regulation of these pathways conceivably can promote YAP activity leading to drug resistance. Therefore, a detailed understanding of feedback mechanisms that regulate upstream signaling is critical and will enable the identification of rational drug combinations that will circumvent drug resistance produced by unleashing the activity of alternative pathways.
CONCLUSION
Despite major advances in defining the molecular mutations driving PDAC, this disease remains universally lethal with an overall 5-year survival rate of only about 7%-8%. More efficacious therapeutic strategies are clearly needed but given the late presentation and early dissemination of the disease, substantial efforts should be concentrated on prevention and interception. Hereby, detailed knowledge of the molecular mechanisms underlying risk-factor promoted PDAC will surely facilitate and enable the discovery of novel molecular targets and agents for primary or secondary prevention. Epidemiological studies convincingly demonstrate that obesity is a risk factor for PDAC development, the importance of which takes an added level given the epidemic proportions of metabolic diseases. It is also recognized that almost all PDACs harbor an oncogenic KRAS mutation, which seems necessary but not sufficient for complete PDAC formation. Besides additional mutations, which greatly accelerate PDAC progression in mice, environmental conditions, including obesity, T2DM, and inflammation, have been shown to also promote PDAC in murine models. As illustrated in Figure 1, we propose that PI3K/mTORC1 and PKD/ERK are critical nodes in the network activated by GPCRs, EGFR and insulin/IGF-1 receptor in PDAC. These signaling modules are responsive to obesogenic signals and reinforce KRAS signaling. In turn, oncogenic KRAS mutations potentiate the intensity of signaling network emanating from GPCRs, EGFR, and insulin/IGF-1 receptors by activating PI3K/AKT and Raf/MEK/ERK, the most prominent downstream pathways of oncogenic KRAS.
We also postulate that YAP/TAZ transcriptional co-activators are central and critical players in this amplification network, further intensifying positive feedback loops. GPCRs, EGFR, and insulin/IGF-1 receptor signaling rapidly stimulate nuclear import and transcriptional co-activator activity of YAP/TAZ, while oncogenic KRAS increases the levels of YAP protein. In turn, YAP stimulates signaling via autocrine/paracrine stimulation of EGFR via increased production of EGFR ligands (e.g., amphiregulin), thereby further propagating and enhancing KRAS activity, as well as creating an immunosuppressive microenvironment. We hypothesize that oncogenic KRAS potentiates a signaling network that is stimulated and sustained by environmental factors. As YAP/TAZ play a central role in the signaling network, targeting this network at different sites with FDA-approved drugs, including statins and metformin (Figure 2), is therefore a compelling approach, especially in obese patients at higher risk of developing PDAC.
Footnotes
Conflict-of-interest statement: All authors declare no conflicts-of-interest related to this article.
Peer-review started: February 6, 2019
First decision: March 5, 2019
Article in press: March 25, 2019
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fekaj E, Şendur MAN S-Editor: Ma RY L-Editor: A E-Editor: Ma YJ
Contributor Information
Enrique Rozengurt, Department of Medicine, David Geffen School of Medicine, University of California at Los Angeles, Los Angeles, CA 90095, United States; CURE: Digestive Diseases Research Center, Los Angeles, CA 90095, United States.
Guido Eibl, Department of Surgery, David Geffen School of Medicine, University of California at Los Angeles, Los Angeles, CA 90095, United States; CURE: Digestive Diseases Research Center, Los Angeles, CA 90095, United States.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 2.Xiao AY, Tan ML, Wu LM, Asrani VM, Windsor JA, Yadav D, Petrov MS. Global incidence and mortality of pancreatic diseases: a systematic review, meta-analysis, and meta-regression of population-based cohort studies. Lancet Gastroenterol Hepatol. 2016;1:45–55. doi: 10.1016/S2468-1253(16)30004-8. [DOI] [PubMed] [Google Scholar]
- 3.Whitcomb DC, Shelton CA, Brand RE. Genetics and Genetic Testing in Pancreatic Cancer. Gastroenterology. 2015;149:1252–1264.e4. doi: 10.1053/j.gastro.2015.07.057. [DOI] [PubMed] [Google Scholar]
- 4.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68:7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 5.Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74:2913–2921. doi: 10.1158/0008-5472.CAN-14-0155. [DOI] [PubMed] [Google Scholar]
- 6.Meyskens FL, Jr, Mukhtar H, Rock CL, Cuzick J, Kensler TW, Yang CS, Ramsey SD, Lippman SM, Alberts DS. Cancer Prevention: Obstacles, Challenges and the Road Ahead. J Natl Cancer Inst. 2015;108 doi: 10.1093/jnci/djv309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kensler TW, Spira A, Garber JE, Szabo E, Lee JJ, Dong Z, Dannenberg AJ, Hait WN, Blackburn E, Davidson NE, Foti M, Lippman SM. Transforming Cancer Prevention through Precision Medicine and Immune-oncology. Cancer Prev Res (Phila) 2016;9:2–10. doi: 10.1158/1940-6207.CAPR-15-0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Albini A, DeCensi A, Cavalli F, Costa A. Cancer Prevention and Interception: A New Era for Chemopreventive Approaches. Clin Cancer Res. 2016;22:4322–4327. doi: 10.1158/1078-0432.CCR-16-0695. [DOI] [PubMed] [Google Scholar]
- 9.Umar A, Dunn BK, Greenwald P. Future directions in cancer prevention. Nat Rev Cancer. 2012;12:835–848. doi: 10.1038/nrc3397. [DOI] [PubMed] [Google Scholar]
- 10.Miller MS, Allen P, Brentnall TA, Goggins M, Hruban RH, Petersen GM, Rao CV, Whitcomb DC, Brand RE, Chari ST, Klein AP, Lubman DM, Rhim AD, Simeone DM, Wolpin BM, Umar A, Srivastava S, Steele VE, Rinaudo JA. Pancreatic Cancer Chemoprevention Translational Workshop: Meeting Report. Pancreas. 2016;45:1080–1091. doi: 10.1097/MPA.0000000000000705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, Perucho M. Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell. 1988;53:549–554. doi: 10.1016/0092-8674(88)90571-5. [DOI] [PubMed] [Google Scholar]
- 12.Smit VT, Boot AJ, Smits AM, Fleuren GJ, Cornelisse CJ, Bos JL. KRAS codon 12 mutations occur very frequently in pancreatic adenocarcinomas. Nucleic Acids Res. 1988;16:7773–7782. doi: 10.1093/nar/16.16.7773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones S, Zhang X, Parsons DW, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Kamiyama H, Jimeno A, Hong SM, Fu B, Lin MT, Calhoun ES, Kamiyama M, Walter K, Nikolskaya T, Nikolsky Y, Hartigan J, Smith DR, Hidalgo M, Leach SD, Klein AP, Jaffee EM, Goggins M, Maitra A, Iacobuzio-Donahue C, Eshleman JR, Kern SE, Hruban RH, Karchin R, Papadopoulos N, Parmigiani G, Vogelstein B, Velculescu VE, Kinzler KW. Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science. 2008;321:1801–1806. doi: 10.1126/science.1164368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biankin AV, Waddell N, Kassahn KS, Gingras MC, Muthuswamy LB, Johns AL, Miller DK, Wilson PJ, Patch AM, Wu J, Chang DK, Cowley MJ, Gardiner BB, Song S, Harliwong I, Idrisoglu S, Nourse C, Nourbakhsh E, Manning S, Wani S, Gongora M, Pajic M, Scarlett CJ, Gill AJ, Pinho AV, Rooman I, Anderson M, Holmes O, Leonard C, Taylor D, Wood S, Xu Q, Nones K, Fink JL, Christ A, Bruxner T, Cloonan N, Kolle G, Newell F, Pinese M, Mead RS, Humphris JL, Kaplan W, Jones MD, Colvin EK, Nagrial AM, Humphrey ES, Chou A, Chin VT, Chantrill LA, Mawson A, Samra JS, Kench JG, Lovell JA, Daly RJ, Merrett ND, Toon C, Epari K, Nguyen NQ, Barbour A, Zeps N Australian Pancreatic Cancer Genome Initiative, Kakkar N, Zhao F, Wu YQ, Wang M, Muzny DM, Fisher WE, Brunicardi FC, Hodges SE, Reid JG, Drummond J, Chang K, Han Y, Lewis LR, Dinh H, Buhay CJ, Beck T, Timms L, Sam M, Begley K, Brown A, Pai D, Panchal A, Buchner N, De Borja R, Denroche RE, Yung CK, Serra S, Onetto N, Mukhopadhyay D, Tsao MS, Shaw PA, Petersen GM, Gallinger S, Hruban RH, Maitra A, Iacobuzio-Donahue CA, Schulick RD, Wolfgang CL, Morgan RA, Lawlor RT, Capelli P, Corbo V, Scardoni M, Tortora G, Tempero MA, Mann KM, Jenkins NA, Perez-Mancera PA, Adams DJ, Largaespada DA, Wessels LF, Rust AG, Stein LD, Tuveson DA, Copeland NG, Musgrove EA, Scarpa A, Eshleman JR, Hudson TJ, Sutherland RL, Wheeler DA, Pearson JV, McPherson JD, Gibbs RA, Grimmond SM. Pancreatic cancer genomes reveal aberrations in axon guidance pathway genes. Nature. 2012;491:399–405. doi: 10.1038/nature11547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bryant KL, Mancias JD, Kimmelman AC, Der CJ. KRAS: feeding pancreatic cancer proliferation. Trends Biochem Sci. 2014;39:91–100. doi: 10.1016/j.tibs.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cancer Genome Atlas Research Network; Cancer Genome Atlas Research Network. Electronic address: andrew_aguirre@dfci.harvard.edu. Integrated Genomic Characterization of Pancreatic Ductal Adenocarcinoma. Cancer Cell. 2017;32:185–203.e13. doi: 10.1016/j.ccell.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pylayeva-Gupta Y, Grabocka E, Bar-Sagi D. RAS oncogenes: weaving a tumorigenic web. Nat Rev Cancer. 2011;11:761–774. doi: 10.1038/nrc3106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pantsar T, Rissanen S, Dauch D, Laitinen T, Vattulainen I, Poso A. Assessment of mutation probabilities of KRAS G12 missense mutants and their long-timescale dynamics by atomistic molecular simulations and Markov state modeling. PLoS Comput Biol. 2018;14:e1006458. doi: 10.1371/journal.pcbi.1006458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eibl G, Cruz-Monserrate Z, Korc M, Petrov MS, Goodarzi MO, Fisher WE, Habtezion A, Lugea A, Pandol SJ, Hart PA, Andersen DK Consortium for the Study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer. Diabetes Mellitus and Obesity as Risk Factors for Pancreatic Cancer. J Acad Nutr Diet. 2018;118:555–567. doi: 10.1016/j.jand.2017.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu M, Jung X, Hines OJ, Eibl G, Chen Y. Obesity and Pancreatic Cancer: Overview of Epidemiology and Potential Prevention by Weight Loss. Pancreas. 2018;47:158–162. doi: 10.1097/MPA.0000000000000974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abbruzzese JL, Andersen DK, Borrebaeck CAK, Chari ST, Costello E, Cruz-Monserrate Z, Eibl G, Engleman EG, Fisher WE, Habtezion A, Kim SK, Korc M, Logsdon C, Lyssiotis CA, Pandol SJ, Rustgi A, Wolfe BM, Zheng L, Powers AC. The Interface of Pancreatic Cancer With Diabetes, Obesity, and Inflammation: Research Gaps and Opportunities: Summary of a National Institute of Diabetes and Digestive and Kidney Diseases Workshop. Pancreas. 2018;47:516–525. doi: 10.1097/MPA.0000000000001037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersen DK, Korc M, Petersen GM, Eibl G, Li D, Rickels MR, Chari ST, Abbruzzese JL. Diabetes, Pancreatogenic Diabetes, and Pancreatic Cancer. Diabetes. 2017;66:1103–1110. doi: 10.2337/db16-1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Y, Dutson E, Eibl G. Strategies to Prevent Obesity-Related Cancer. JAMA. 2018;319:2442. doi: 10.1001/jama.2018.4942. [DOI] [PubMed] [Google Scholar]
- 24.Juo YY, Gibbons MAM, Dutson E, Lin AY, Yanagawa J, Hines OJ, Eibl G, Chen Y. Obesity Is Associated with Early Onset of Gastrointestinal Cancers in California. J Obes. 2018;2018:7014073. doi: 10.1155/2018/7014073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klein AP, Wolpin BM, Risch HA, Stolzenberg-Solomon RZ, Mocci E, Zhang M, Canzian F, Childs EJ, Hoskins JW, Jermusyk A, Zhong J, Chen F, Albanes D, Andreotti G, Arslan AA, Babic A, Bamlet WR, Beane-Freeman L, Berndt SI, Blackford A, Borges M, Borgida A, Bracci PM, Brais L, Brennan P, Brenner H, Bueno-de-Mesquita B, Buring J, Campa D, Capurso G, Cavestro GM, Chaffee KG, Chung CC, Cleary S, Cotterchio M, Dijk F, Duell EJ, Foretova L, Fuchs C, Funel N, Gallinger S, M Gaziano JM, Gazouli M, Giles GG, Giovannucci E, Goggins M, Goodman GE, Goodman PJ, Hackert T, Haiman C, Hartge P, Hasan M, Hegyi P, Helzlsouer KJ, Herman J, Holcatova I, Holly EA, Hoover R, Hung RJ, Jacobs EJ, Jamroziak K, Janout V, Kaaks R, Khaw KT, Klein EA, Kogevinas M, Kooperberg C, Kulke MH, Kupcinskas J, Kurtz RJ, Laheru D, Landi S, Lawlor RT, Lee IM, LeMarchand L, Lu L, Malats N, Mambrini A, Mannisto S, Milne RL, Mohelníková-Duchoňová B, Neale RE, Neoptolemos JP, Oberg AL, Olson SH, Orlow I, Pasquali C, Patel AV, Peters U, Pezzilli R, Porta M, Real FX, Rothman N, Scelo G, Sesso HD, Severi G, Shu XO, Silverman D, Smith JP, Soucek P, Sund M, Talar-Wojnarowska R, Tavano F, Thornquist MD, Tobias GS, Van Den Eeden SK, Vashist Y, Visvanathan K, Vodicka P, Wactawski-Wende J, Wang Z, Wentzensen N, White E, Yu H, Yu K, Zeleniuch-Jacquotte A, Zheng W, Kraft P, Li D, Chanock S, Obazee O, Petersen GM, Amundadottir LT. Genome-wide meta-analysis identifies five new susceptibility loci for pancreatic cancer. Nat Commun. 2018;9:556. doi: 10.1038/s41467-018-02942-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Childs EJ, Mocci E, Campa D, Bracci PM, Gallinger S, Goggins M, Li D, Neale RE, Olson SH, Scelo G, Amundadottir LT, Bamlet WR, Bijlsma MF, Blackford A, Borges M, Brennan P, Brenner H, Bueno-de-Mesquita HB, Canzian F, Capurso G, Cavestro GM, Chaffee KG, Chanock SJ, Cleary SP, Cotterchio M, Foretova L, Fuchs C, Funel N, Gazouli M, Hassan M, Herman JM, Holcatova I, Holly EA, Hoover RN, Hung RJ, Janout V, Key TJ, Kupcinskas J, Kurtz RC, Landi S, Lu L, Malecka-Panas E, Mambrini A, Mohelnikova-Duchonova B, Neoptolemos JP, Oberg AL, Orlow I, Pasquali C, Pezzilli R, Rizzato C, Saldia A, Scarpa A, Stolzenberg-Solomon RZ, Strobel O, Tavano F, Vashist YK, Vodicka P, Wolpin BM, Yu H, Petersen GM, Risch HA, Klein AP. Common variation at 2p13.3, 3q29, 7p13 and 17q25.1 associated with susceptibility to pancreatic cancer. Nat Genet. 2015;47:911–916. doi: 10.1038/ng.3341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolpin BM, Rizzato C, Kraft P, Kooperberg C, Petersen GM, Wang Z, Arslan AA, Beane-Freeman L, Bracci PM, Buring J, Canzian F, Duell EJ, Gallinger S, Giles GG, Goodman GE, Goodman PJ, Jacobs EJ, Kamineni A, Klein AP, Kolonel LN, Kulke MH, Li D, Malats N, Olson SH, Risch HA, Sesso HD, Visvanathan K, White E, Zheng W, Abnet CC, Albanes D, Andreotti G, Austin MA, Barfield R, Basso D, Berndt SI, Boutron-Ruault MC, Brotzman M, Büchler MW, Bueno-de-Mesquita HB, Bugert P, Burdette L, Campa D, Caporaso NE, Capurso G, Chung C, Cotterchio M, Costello E, Elena J, Funel N, Gaziano JM, Giese NA, Giovannucci EL, Goggins M, Gorman MJ, Gross M, Haiman CA, Hassan M, Helzlsouer KJ, Henderson BE, Holly EA, Hu N, Hunter DJ, Innocenti F, Jenab M, Kaaks R, Key TJ, Khaw KT, Klein EA, Kogevinas M, Krogh V, Kupcinskas J, Kurtz RC, LaCroix A, Landi MT, Landi S, Le Marchand L, Mambrini A, Mannisto S, Milne RL, Nakamura Y, Oberg AL, Owzar K, Patel AV, Peeters PH, Peters U, Pezzilli R, Piepoli A, Porta M, Real FX, Riboli E, Rothman N, Scarpa A, Shu XO, Silverman DT, Soucek P, Sund M, Talar-Wojnarowska R, Taylor PR, Theodoropoulos GE, Thornquist M, Tjønneland A, Tobias GS, Trichopoulos D, Vodicka P, Wactawski-Wende J, Wentzensen N, Wu C, Yu H, Yu K, Zeleniuch-Jacquotte A, Hoover R, Hartge P, Fuchs C, Chanock SJ, Stolzenberg-Solomon RS, Amundadottir LT. Genome-wide association study identifies multiple susceptibility loci for pancreatic cancer. Nat Genet. 2014;46:994–1000. doi: 10.1038/ng.3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Petersen GM, Amundadottir L, Fuchs CS, Kraft P, Stolzenberg-Solomon RZ, Jacobs KB, Arslan AA, Bueno-de-Mesquita HB, Gallinger S, Gross M, Helzlsouer K, Holly EA, Jacobs EJ, Klein AP, LaCroix A, Li D, Mandelson MT, Olson SH, Risch HA, Zheng W, Albanes D, Bamlet WR, Berg CD, Boutron-Ruault MC, Buring JE, Bracci PM, Canzian F, Clipp S, Cotterchio M, de Andrade M, Duell EJ, Gaziano JM, Giovannucci EL, Goggins M, Hallmans G, Hankinson SE, Hassan M, Howard B, Hunter DJ, Hutchinson A, Jenab M, Kaaks R, Kooperberg C, Krogh V, Kurtz RC, Lynch SM, McWilliams RR, Mendelsohn JB, Michaud DS, Parikh H, Patel AV, Peeters PH, Rajkovic A, Riboli E, Rodriguez L, Seminara D, Shu XO, Thomas G, Tjønneland A, Tobias GS, Trichopoulos D, Van Den Eeden SK, Virtamo J, Wactawski-Wende J, Wang Z, Wolpin BM, Yu H, Yu K, Zeleniuch-Jacquotte A, Fraumeni JF, Jr, Hoover RN, Hartge P, Chanock SJ. A genome-wide association study identifies pancreatic cancer susceptibility loci on chromosomes 13q22.1, 1q32.1 and 5p15.33. Nat Genet. 2010;42:224–228. doi: 10.1038/ng.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mueller S, Engleitner T, Maresch R, Zukowska M, Lange S, Kaltenbacher T, Konukiewitz B, Öllinger R, Zwiebel M, Strong A, Yen HY, Banerjee R, Louzada S, Fu B, Seidler B, Götzfried J, Schuck K, Hassan Z, Arbeiter A, Schönhuber N, Klein S, Veltkamp C, Friedrich M, Rad L, Barenboim M, Ziegenhain C, Hess J, Dovey OM, Eser S, Parekh S, Constantino-Casas F, de la Rosa J, Sierra MI, Fraga M, Mayerle J, Klöppel G, Cadiñanos J, Liu P, Vassiliou G, Weichert W, Steiger K, Enard W, Schmid RM, Yang F, Unger K, Schneider G, Varela I, Bradley A, Saur D, Rad R. Evolutionary routes and KRAS dosage define pancreatic cancer phenotypes. Nature. 2018;554:62–68. doi: 10.1038/nature25459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Collisson EA, Sadanandam A, Olson P, Gibb WJ, Truitt M, Gu S, Cooc J, Weinkle J, Kim GE, Jakkula L, Feiler HS, Ko AH, Olshen AB, Danenberg KL, Tempero MA, Spellman PT, Hanahan D, Gray JW. Subtypes of pancreatic ductal adenocarcinoma and their differing responses to therapy. Nat Med. 2011;17:500–503. doi: 10.1038/nm.2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bailey P, Chang DK, Nones K, Johns AL, Patch AM, Gingras MC, Miller DK, Christ AN, Bruxner TJ, Quinn MC, Nourse C, Murtaugh LC, Harliwong I, Idrisoglu S, Manning S, Nourbakhsh E, Wani S, Fink L, Holmes O, Chin V, Anderson MJ, Kazakoff S, Leonard C, Newell F, Waddell N, Wood S, Xu Q, Wilson PJ, Cloonan N, Kassahn KS, Taylor D, Quek K, Robertson A, Pantano L, Mincarelli L, Sanchez LN, Evers L, Wu J, Pinese M, Cowley MJ, Jones MD, Colvin EK, Nagrial AM, Humphrey ES, Chantrill LA, Mawson A, Humphris J, Chou A, Pajic M, Scarlett CJ, Pinho AV, Giry-Laterriere M, Rooman I, Samra JS, Kench JG, Lovell JA, Merrett ND, Toon CW, Epari K, Nguyen NQ, Barbour A, Zeps N, Moran-Jones K, Jamieson NB, Graham JS, Duthie F, Oien K, Hair J, Grützmann R, Maitra A, Iacobuzio-Donahue CA, Wolfgang CL, Morgan RA, Lawlor RT, Corbo V, Bassi C, Rusev B, Capelli P, Salvia R, Tortora G, Mukhopadhyay D, Petersen GM Australian Pancreatic Cancer Genome Initiative, Munzy DM, Fisher WE, Karim SA, Eshleman JR, Hruban RH, Pilarsky C, Morton JP, Sansom OJ, Scarpa A, Musgrove EA, Bailey UM, Hofmann O, Sutherland RL, Wheeler DA, Gill AJ, Gibbs RA, Pearson JV, Waddell N, Biankin AV, Grimmond SM. Genomic analyses identify molecular subtypes of pancreatic cancer. Nature. 2016;531:47–52. doi: 10.1038/nature16965. [DOI] [PubMed] [Google Scholar]
- 32.Moffitt RA, Marayati R, Flate EL, Volmar KE, Loeza SG, Hoadley KA, Rashid NU, Williams LA, Eaton SC, Chung AH, Smyla JK, Anderson JM, Kim HJ, Bentrem DJ, Talamonti MS, Iacobuzio-Donahue CA, Hollingsworth MA, Yeh JJ. Virtual microdissection identifies distinct tumor- and stroma-specific subtypes of pancreatic ductal adenocarcinoma. Nat Genet. 2015;47:1168–1178. doi: 10.1038/ng.3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Waddell N, Pajic M, Patch AM, Chang DK, Kassahn KS, Bailey P, Johns AL, Miller D, Nones K, Quek K, Quinn MC, Robertson AJ, Fadlullah MZ, Bruxner TJ, Christ AN, Harliwong I, Idrisoglu S, Manning S, Nourse C, Nourbakhsh E, Wani S, Wilson PJ, Markham E, Cloonan N, Anderson MJ, Fink JL, Holmes O, Kazakoff SH, Leonard C, Newell F, Poudel B, Song S, Taylor D, Waddell N, Wood S, Xu Q, Wu J, Pinese M, Cowley MJ, Lee HC, Jones MD, Nagrial AM, Humphris J, Chantrill LA, Chin V, Steinmann AM, Mawson A, Humphrey ES, Colvin EK, Chou A, Scarlett CJ, Pinho AV, Giry-Laterriere M, Rooman I, Samra JS, Kench JG, Pettitt JA, Merrett ND, Toon C, Epari K, Nguyen NQ, Barbour A, Zeps N, Jamieson NB, Graham JS, Niclou SP, Bjerkvig R, Grützmann R, Aust D, Hruban RH, Maitra A, Iacobuzio-Donahue CA, Wolfgang CL, Morgan RA, Lawlor RT, Corbo V, Bassi C, Falconi M, Zamboni G, Tortora G, Tempero MA Australian Pancreatic Cancer Genome Initiative, Gill AJ, Eshleman JR, Pilarsky C, Scarpa A, Musgrove EA, Pearson JV, Biankin AV, Grimmond SM. Whole genomes redefine the mutational landscape of pancreatic cancer. Nature. 2015;518:495–501. doi: 10.1038/nature14169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hansel DE, Kern SE, Hruban RH. Molecular pathogenesis of pancreatic cancer. Annu Rev Genomics Hum Genet. 2003;4:237–256. doi: 10.1146/annurev.genom.4.070802.110341. [DOI] [PubMed] [Google Scholar]
- 35.Hruban RH, Adsay NV, Albores-Saavedra J, Compton C, Garrett ES, Goodman SN, Kern SE, Klimstra DS, Klöppel G, Longnecker DS, Lüttges J, Offerhaus GJ. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am J Surg Pathol. 2001;25:579–586. doi: 10.1097/00000478-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Maitra A, Fukushima N, Takaori K, Hruban RH. Precursors to invasive pancreatic cancer. Adv Anat Pathol. 2005;12:81–91. doi: 10.1097/01.pap.0000155055.14238.25. [DOI] [PubMed] [Google Scholar]
- 37.Hruban RH, Goggins M, Parsons J, Kern SE. Progression model for pancreatic cancer. Clin Cancer Res. 2000;6:2969–2972. [PubMed] [Google Scholar]
- 38.Real FX, de Andrés MP. Mutant Kras Dosage and Chromothripsis: The Right Ingredients for a Pancreatic Cancer Catastrophe. Trends Cancer. 2018;4:399–401. doi: 10.1016/j.trecan.2018.04.004. [DOI] [PubMed] [Google Scholar]
- 39.Notta F, Hahn SA, Real FX. A genetic roadmap of pancreatic cancer: still evolving. Gut. 2017;66:2170–2178. doi: 10.1136/gutjnl-2016-313317. [DOI] [PubMed] [Google Scholar]
- 40.Notta F, Chan-Seng-Yue M, Lemire M, Li Y, Wilson GW, Connor AA, Denroche RE, Liang SB, Brown AM, Kim JC, Wang T, Simpson JT, Beck T, Borgida A, Buchner N, Chadwick D, Hafezi-Bakhtiari S, Dick JE, Heisler L, Hollingsworth MA, Ibrahimov E, Jang GH, Johns J, Jorgensen LG, Law C, Ludkovski O, Lungu I, Ng K, Pasternack D, Petersen GM, Shlush LI, Timms L, Tsao MS, Wilson JM, Yung CK, Zogopoulos G, Bartlett JM, Alexandrov LB, Real FX, Cleary SP, Roehrl MH, McPherson JD, Stein LD, Hudson TJ, Campbell PJ, Gallinger S. A renewed model of pancreatic cancer evolution based on genomic rearrangement patterns. Nature. 2016;538:378–382. doi: 10.1038/nature19823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Real FX, Cibrián-Uhalte E, Martinelli P. Pancreatic cancer development and progression: remodeling the model. Gastroenterology. 2008;135:724–728. doi: 10.1053/j.gastro.2008.07.033. [DOI] [PubMed] [Google Scholar]
- 42.Ren B, Liu X, Suriawinata AA. Pancreatic Ductal Adenocarcinoma and Its Precursor Lesions: Histopathology, Cytopathology, and Molecular Pathology. Am J Pathol. 2019;189:9–21. doi: 10.1016/j.ajpath.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 43.Kanda M, Matthaei H, Wu J, Hong SM, Yu J, Borges M, Hruban RH, Maitra A, Kinzler K, Vogelstein B, Goggins M. Presence of somatic mutations in most early-stage pancreatic intraepithelial neoplasia. Gastroenterology. 2012;142:730–733.e9. doi: 10.1053/j.gastro.2011.12.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Deramaudt T, Rustgi AK. Mutant KRAS in the initiation of pancreatic cancer. Biochim Biophys Acta. 2005;1756:97–101. doi: 10.1016/j.bbcan.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 45.Logsdon CD, Lu W. The Significance of Ras Activity in Pancreatic Cancer Initiation. Int J Biol Sci. 2016;12:338–346. doi: 10.7150/ijbs.15020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hingorani SR, Petricoin EF, Maitra A, Rajapakse V, King C, Jacobetz MA, Ross S, Conrads TP, Veenstra TD, Hitt BA, Kawaguchi Y, Johann D, Liotta LA, Crawford HC, Putt ME, Jacks T, Wright CV, Hruban RH, Lowy AM, Tuveson DA. Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell. 2003;4:437–450. doi: 10.1016/s1535-6108(03)00309-x. [DOI] [PubMed] [Google Scholar]
- 47.Hingorani SR, Wang L, Multani AS, Combs C, Deramaudt TB, Hruban RH, Rustgi AK, Chang S, Tuveson DA. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell. 2005;7:469–483. doi: 10.1016/j.ccr.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 48.Hruban RH, Adsay NV, Albores-Saavedra J, Anver MR, Biankin AV, Boivin GP, Furth EE, Furukawa T, Klein A, Klimstra DS, Kloppel G, Lauwers GY, Longnecker DS, Luttges J, Maitra A, Offerhaus GJ, Pérez-Gallego L, Redston M, Tuveson DA. Pathology of genetically engineered mouse models of pancreatic exocrine cancer: consensus report and recommendations. Cancer Res. 2006;66:95–106. doi: 10.1158/0008-5472.CAN-05-2168. [DOI] [PubMed] [Google Scholar]
- 49.Hruban RH, Rustgi AK, Brentnall TA, Tempero MA, Wright CV, Tuveson DA. Pancreatic cancer in mice and man: the Penn Workshop 2004. Cancer Res. 2006;66:14–17. doi: 10.1158/0008-5472.CAN-05-3914. [DOI] [PubMed] [Google Scholar]
- 50.Funahashi H, Satake M, Dawson D, Huynh NA, Reber HA, Hines OJ, Eibl G. Delayed progression of pancreatic intraepithelial neoplasia in a conditional Kras(G12D) mouse model by a selective cyclooxygenase-2 inhibitor. Cancer Res. 2007;67:7068–7071. doi: 10.1158/0008-5472.CAN-07-0970. [DOI] [PubMed] [Google Scholar]
- 51.Collins MA, Bednar F, Zhang Y, Brisset JC, Galbán S, Galbán CJ, Rakshit S, Flannagan KS, Adsay NV, Pasca di Magliano M. Oncogenic Kras is required for both the initiation and maintenance of pancreatic cancer in mice. J Clin Invest. 2012;122:639–653. doi: 10.1172/JCI59227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.di Magliano MP, Logsdon CD. Roles for KRAS in pancreatic tumor development and progression. Gastroenterology. 2013;144:1220–1229. doi: 10.1053/j.gastro.2013.01.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Porciuncula A, Hajdu C, David G. The Dual Role of Senescence in Pancreatic Ductal Adenocarcinoma. Adv Cancer Res. 2016;131:1–20. doi: 10.1016/bs.acr.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 54.Aguirre AJ, Bardeesy N, Sinha M, Lopez L, Tuveson DA, Horner J, Redston MS, DePinho RA. Activated Kras and Ink4a/Arf deficiency cooperate to produce metastatic pancreatic ductal adenocarcinoma. Genes Dev. 2003;17:3112–3126. doi: 10.1101/gad.1158703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chang HH, Moro A, Takakura K, Su HY, Mo A, Nakanishi M, Waldron RT, French SW, Dawson DW, Hines OJ, Li G, Go VLW, Sinnett-Smith J, Pandol SJ, Lugea A, Gukovskaya AS, Duff MO, Rosenberg DW, Rozengurt E, Eibl G. Incidence of pancreatic cancer is dramatically increased by a high fat, high calorie diet in KrasG12D mice. PLoS One. 2017;12:e0184455. doi: 10.1371/journal.pone.0184455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dawson DW, Hertzer K, Moro A, Donald G, Chang HH, Go VL, Pandol SJ, Lugea A, Gukovskaya AS, Li G, Hines OJ, Rozengurt E, Eibl G. High-fat, high-calorie diet promotes early pancreatic neoplasia in the conditional KrasG12D mouse model. Cancer Prev Res (Phila) 2013;6:1064–1073. doi: 10.1158/1940-6207.CAPR-13-0065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lashinger LM, Harrison LM, Rasmussen AJ, Logsdon CD, Fischer SM, McArthur MJ, Hursting SD. Dietary energy balance modulation of Kras- and Ink4a/Arf+/--driven pancreatic cancer: the role of insulin-like growth factor-I. Cancer Prev Res (Phila) 2013;6:1046–1055. doi: 10.1158/1940-6207.CAPR-13-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Philip B, Roland CL, Daniluk J, Liu Y, Chatterjee D, Gomez SB, Ji B, Huang H, Wang H, Fleming JB, Logsdon CD, Cruz-Monserrate Z. A high-fat diet activates oncogenic Kras and COX2 to induce development of pancreatic ductal adenocarcinoma in mice. Gastroenterology. 2013;145:1449–1458. doi: 10.1053/j.gastro.2013.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Harvey AE, Lashinger LM, Hays D, Harrison LM, Lewis K, Fischer SM, Hursting SD. Calorie restriction decreases murine and human pancreatic tumor cell growth, nuclear factor-κB activation, and inflammation-related gene expression in an insulin-like growth factor-1-dependent manner. PLoS One. 2014;9:e94151. doi: 10.1371/journal.pone.0094151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Campbell PM, Singh A, Williams FJ, Frantz K, Ulkü AS, Kelley GG, Der CJ. Genetic and pharmacologic dissection of Ras effector utilization in oncogenesis. Methods Enzymol. 2006;407:195–217. doi: 10.1016/S0076-6879(05)07017-5. [DOI] [PubMed] [Google Scholar]
- 61.Daniluk J, Liu Y, Deng D, Chu J, Huang H, Gaiser S, Cruz-Monserrate Z, Wang H, Ji B, Logsdon CD. An NF-κB pathway-mediated positive feedback loop amplifies Ras activity to pathological levels in mice. J Clin Invest. 2012;122:1519–1528. doi: 10.1172/JCI59743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Seufferlein T, Van Lint J, Liptay S, Adler G, Schmid RM. Transforming growth factor alpha activates Ha-Ras in human pancreatic cancer cells with Ki-ras mutations. Gastroenterology. 1999;116:1441–1452. doi: 10.1016/s0016-5085(99)70509-3. [DOI] [PubMed] [Google Scholar]
- 63.Ryder NM, Guha S, Hines OJ, Reber HA, Rozengurt E. G protein-coupled receptor signaling in human ductal pancreatic cancer cells: neurotensin responsiveness and mitogenic stimulation. J Cell Physiol. 2001;186:53–64. doi: 10.1002/1097-4652(200101)186:1<53::AID-JCP1004>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 64.Guha S, Rey O, Rozengurt E. Neurotensin induces protein kinase C-dependent protein kinase D activation and DNA synthesis in human pancreatic carcinoma cell line PANC-1. Cancer Res. 2002;62:1632–1640. [PubMed] [Google Scholar]
- 65.Guerra C, Schuhmacher AJ, Cañamero M, Grippo PJ, Verdaguer L, Pérez-Gallego L, Dubus P, Sandgren EP, Barbacid M. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell. 2007;11:291–302. doi: 10.1016/j.ccr.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 66.Eibl G, Rozengurt E. KRAS, YAP, and obesity in pancreatic cancer: A signaling network with multiple loops. Semin Cancer Biol. 2019;54:50–62. doi: 10.1016/j.semcancer.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tang H, Wei P, Duell EJ, Risch HA, Olson SH, Bueno-de-Mesquita HB, Gallinger S, Holly EA, Petersen GM, Bracci PM, McWilliams RR, Jenab M, Riboli E, Tjønneland A, Boutron-Ruault MC, Kaaks R, Trichopoulos D, Panico S, Sund M, Peeters PH, Khaw KT, Amos CI, Li D. Genes-environment interactions in obesity- and diabetes-associated pancreatic cancer: a GWAS data analysis. Cancer Epidemiol Biomarkers Prev. 2014;23:98–106. doi: 10.1158/1055-9965.EPI-13-0437-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Misra JR, Irvine KD. The Hippo Signaling Network and Its Biological Functions. Annu Rev Genet. 2018;52:65–87. doi: 10.1146/annurev-genet-120417-031621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Meng Z, Moroishi T, Guan KL. Mechanisms of Hippo pathway regulation. Genes Dev. 2016;30:1–17. doi: 10.1101/gad.274027.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Enzo E, Santinon G, Pocaterra A, Aragona M, Bresolin S, Forcato M, Grifoni D, Pession A, Zanconato F, Guzzo G, Bicciato S, Dupont S. Aerobic glycolysis tunes YAP/TAZ transcriptional activity. EMBO J. 2015;34:1349–1370. doi: 10.15252/embj.201490379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang Z, Wu Y, Wang H, Zhang Y, Mei L, Fang X, Zhang X, Zhang F, Chen H, Liu Y, Jiang Y, Sun S, Zheng Y, Li N, Huang L. Interplay of mevalonate and Hippo pathways regulates RHAMM transcription via YAP to modulate breast cancer cell motility. Proc Natl Acad Sci U S A. 2014;111:E89–E98. doi: 10.1073/pnas.1319190110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Santinon G, Pocaterra A, Dupont S. Control of YAP/TAZ Activity by Metabolic and Nutrient-Sensing Pathways. Trends Cell Biol. 2016;26:289–299. doi: 10.1016/j.tcb.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 73.Plouffe SW, Lin KC, Moore JL, 3rd, Tan FE, Ma S, Ye Z, Qiu Y, Ren B, Guan KL. The Hippo pathway effector proteins YAP and TAZ have both distinct and overlapping functions in the cell. J Biol Chem. 2018;293:11230–11240. doi: 10.1074/jbc.RA118.002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim MK, Jang JW, Bae SC. DNA binding partners of YAP/TAZ. BMB Rep. 2018;51:126–133. doi: 10.5483/BMBRep.2018.51.3.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cebola I, Rodríguez-Seguí SA, Cho CH, Bessa J, Rovira M, Luengo M, Chhatriwala M, Berry A, Ponsa-Cobas J, Maestro MA, Jennings RE, Pasquali L, Morán I, Castro N, Hanley NA, Gomez-Skarmeta JL, Vallier L, Ferrer J. TEAD and YAP regulate the enhancer network of human embryonic pancreatic progenitors. Nat Cell Biol. 2015;17:615–626. doi: 10.1038/ncb3160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Moroishi T, Hansen CG, Guan KL. The emerging roles of YAP and TAZ in cancer. Nat Rev Cancer. 2015;15:73–79. doi: 10.1038/nrc3876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Murakami S, Shahbazian D, Surana R, Zhang W, Chen H, Graham GT, White SM, Weiner LM, Yi C. Yes-associated protein mediates immune reprogramming in pancreatic ductal adenocarcinoma. Oncogene. 2017;36:1232–1244. doi: 10.1038/onc.2016.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Santinon G, Brian I, Pocaterra A, Romani P, Franzolin E, Rampazzo C, Bicciato S, Dupont S. dNTP metabolism links mechanical cues and YAP/TAZ to cell growth and oncogene-induced senescence. EMBO J. 2018;37 doi: 10.15252/embj.201797780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhao B, Li L, Lei Q, Guan KL. The Hippo-YAP pathway in organ size control and tumorigenesis: an updated version. Genes Dev. 2010;24:862–874. doi: 10.1101/gad.1909210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Imajo M, Ebisuya M, Nishida E. Dual role of YAP and TAZ in renewal of the intestinal epithelium. Nat Cell Biol. 2015;17:7–19. doi: 10.1038/ncb3084. [DOI] [PubMed] [Google Scholar]
- 81.Zanconato F, Forcato M, Battilana G, Azzolin L, Quaranta E, Bodega B, Rosato A, Bicciato S, Cordenonsi M, Piccolo S. Genome-wide association between YAP/TAZ/TEAD and AP-1 at enhancers drives oncogenic growth. Nat Cell Biol. 2015;17:1218–1227. doi: 10.1038/ncb3216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Stein C, Bardet AF, Roma G, Bergling S, Clay I, Ruchti A, Agarinis C, Schmelzle T, Bouwmeester T, Schübeler D, Bauer A. YAP1 Exerts Its Transcriptional Control via TEAD-Mediated Activation of Enhancers. PLoS Genet. 2015;11:e1005465. doi: 10.1371/journal.pgen.1005465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zanconato F, Battilana G, Forcato M, Filippi L, Azzolin L, Manfrin A, Quaranta E, Di Biagio D, Sigismondo G, Guzzardo V, Lejeune P, Haendler B, Krijgsveld J, Fassan M, Bicciato S, Cordenonsi M, Piccolo S. Transcriptional addiction in cancer cells is mediated by YAP/TAZ through BRD4. Nat Med. 2018;24:1599–1610. doi: 10.1038/s41591-018-0158-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang W, Nandakumar N, Shi Y, Manzano M, Smith A, Graham G, Gupta S, Vietsch EE, Laughlin SZ, Wadhwa M, Chetram M, Joshi M, Wang F, Kallakury B, Toretsky J, Wellstein A, Yi C. Downstream of mutant KRAS, the transcription regulator YAP is essential for neoplastic progression to pancreatic ductal adenocarcinoma. Sci Signal. 2014;7:ra42. doi: 10.1126/scisignal.2005049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gruber R, Panayiotou R, Nye E, Spencer-Dene B, Stamp G, Behrens A. YAP1 and TAZ Control Pancreatic Cancer Initiation in Mice by Direct Up-regulation of JAK-STAT3 Signaling. Gastroenterology. 2016;151:526–539. doi: 10.1053/j.gastro.2016.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Di Agostino S, Sorrentino G, Ingallina E, Valenti F, Ferraiuolo M, Bicciato S, Piazza S, Strano S, Del Sal G, Blandino G. YAP enhances the pro-proliferative transcriptional activity of mutant p53 proteins. EMBO Rep. 2016;17:188–201. doi: 10.15252/embr.201540488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mello SS, Valente LJ, Raj N, Seoane JA, Flowers BM, McClendon J, Bieging-Rolett KT, Lee J, Ivanochko D, Kozak MM, Chang DT, Longacre TA, Koong AC, Arrowsmith CH, Kim SK, Vogel H, Wood LD, Hruban RH, Curtis C, Attardi LD. A p53 Super-tumor Suppressor Reveals a Tumor Suppressive p53-Ptpn14-Yap Axis in Pancreatic Cancer. Cancer Cell. 2017;32:460–473.e6. doi: 10.1016/j.ccell.2017.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lin L, Sabnis AJ, Chan E, Olivas V, Cade L, Pazarentzos E, Asthana S, Neel D, Yan JJ, Lu X, Pham L, Wang MM, Karachaliou N, Cao MG, Manzano JL, Ramirez JL, Torres JM, Buttitta F, Rudin CM, Collisson EA, Algazi A, Robinson E, Osman I, Muñoz-Couselo E, Cortes J, Frederick DT, Cooper ZA, McMahon M, Marchetti A, Rosell R, Flaherty KT, Wargo JA, Bivona TG. The Hippo effector YAP promotes resistance to RAF- and MEK-targeted cancer therapies. Nat Genet. 2015;47:250–256. doi: 10.1038/ng.3218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Neesse A, Frese KK, Bapiro TE, Nakagawa T, Sternlicht MD, Seeley TW, Pilarsky C, Jodrell DI, Spong SM, Tuveson DA. CTGF antagonism with mAb FG-3019 enhances chemotherapy response without increasing drug delivery in murine ductal pancreas cancer. Proc Natl Acad Sci USA. 2013;110:12325–12330. doi: 10.1073/pnas.1300415110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang J, Sinnett-Smith J, Stevens JV, Young SH, Rozengurt E. Biphasic Regulation of Yes-associated Protein (YAP) Cellular Localization, Phosphorylation, and Activity by G Protein-coupled Receptor Agonists in Intestinal Epithelial Cells: A NOVEL ROLE FOR PROTEIN KINASE D (PKD) J Biol Chem. 2016;291:17988–18005. doi: 10.1074/jbc.M115.711275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yu FX, Guan KL. The Hippo pathway: regulators and regulations. Genes Dev. 2013;27:355–371. doi: 10.1101/gad.210773.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Straßburger K, Tiebe M, Pinna F, Breuhahn K, Teleman AA. Insulin/IGF signaling drives cell proliferation in part via Yorkie/YAP. Dev Biol. 2012;367:187–196. doi: 10.1016/j.ydbio.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 93.Si Y, Ji X, Cao X, Dai X, Xu L, Zhao H, Guo X, Yan H, Zhang H, Zhu C, Zhou Q, Tang M, Xia Z, Li L, Cong YS, Ye S, Liang T, Feng XH, Zhao B. Src Inhibits the Hippo Tumor Suppressor Pathway through Tyrosine Phosphorylation of Lats1. Cancer Res. 2017;77:4868–4880. doi: 10.1158/0008-5472.CAN-17-0391. [DOI] [PubMed] [Google Scholar]
- 94.Hao F, Xu Q, Zhao Y, Stevens JV, Young SH, Sinnett-Smith J, Rozengurt E. Insulin Receptor and GPCR Crosstalk Stimulates YAP via PI3K and PKD in Pancreatic Cancer Cells. Mol Cancer Res. 2017;15:929–941. doi: 10.1158/1541-7786.MCR-17-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fan R, Kim NG, Gumbiner BM. Regulation of Hippo pathway by mitogenic growth factors via phosphoinositide 3-kinase and phosphoinositide-dependent kinase-1. Proc Natl Acad Sci USA. 2013;110:2569–2574. doi: 10.1073/pnas.1216462110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kim NG, Gumbiner BM. Adhesion to fibronectin regulates Hippo signaling via the FAK-Src-PI3K pathway. J Cell Biol. 2015;210:503–515. doi: 10.1083/jcb.201501025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hong X, Nguyen HT, Chen Q, Zhang R, Hagman Z, Voorhoeve PM, Cohen SM. Opposing activities of the Ras and Hippo pathways converge on regulation of YAP protein turnover. EMBO J. 2014;33:2447–2457. doi: 10.15252/embj.201489385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Strnadel J, Choi S, Fujimura K, Wang H, Zhang W, Wyse M, Wright T, Gross E, Peinado C, Park HW, Bui J, Kelber J, Bouvet M, Guan KL, Klemke RL. eIF5A-PEAK1 Signaling Regulates YAP1/TAZ Protein Expression and Pancreatic Cancer Cell Growth. Cancer Res. 2017;77:1997–2007. doi: 10.1158/0008-5472.CAN-16-2594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rozengurt E, Soares HP, Sinnet-Smith J. Suppression of feedback loops mediated by PI3K/mTOR induces multiple overactivation of compensatory pathways: an unintended consequence leading to drug resistance. Mol Cancer Ther. 2014;13:2477–2488. doi: 10.1158/1535-7163.MCT-14-0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tumaneng K, Schlegelmilch K, Russell RC, Yimlamai D, Basnet H, Mahadevan N, Fitamant J, Bardeesy N, Camargo FD, Guan KL. YAP mediates crosstalk between the Hippo and PI(3)K–TOR pathways by suppressing PTEN via miR-29. Nat Cell Biol. 2012;14:1322–1329. doi: 10.1038/ncb2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Park YY, Sohn BH, Johnson RL, Kang MH, Kim SB, Shim JJ, Mangala LS, Kim JH, Yoo JE, Rodriguez-Aguayo C, Pradeep S, Hwang JE, Jang HJ, Lee HS, Rupaimoole R, Lopez-Berestein G, Jeong W, Park IS, Park YN, Sood AK, Mills GB, Lee JS. Yes-associated protein 1 and transcriptional coactivator with PDZ-binding motif activate the mammalian target of rapamycin complex 1 pathway by regulating amino acid transporters in hepatocellular carcinoma. Hepatology. 2016;63:159–172. doi: 10.1002/hep.28223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hansen CG, Ng YL, Lam WL, Plouffe SW, Guan KL. The Hippo pathway effectors YAP and TAZ promote cell growth by modulating amino acid signaling to mTORC1. Cell Res. 2015;25:1299–1313. doi: 10.1038/cr.2015.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Liang N, Zhang C, Dill P, Panasyuk G, Pion D, Koka V, Gallazzini M, Olson EN, Lam H, Henske EP, Dong Z, Apte U, Pallet N, Johnson RL, Terzi F, Kwiatkowski DJ, Scoazec JY, Martignoni G, Pende M. Regulation of YAP by mTOR and autophagy reveals a therapeutic target of tuberous sclerosis complex. J Exp Med. 2014;211:2249–2263. doi: 10.1084/jem.20140341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kapoor A, Yao W, Ying H, Hua S, Liewen A, Wang Q, Zhong Y, Wu CJ, Sadanandam A, Hu B, Chang Q, Chu GC, Al-Khalil R, Jiang S, Xia H, Fletcher-Sananikone E, Lim C, Horwitz GI, Viale A, Pettazzoni P, Sanchez N, Wang H, Protopopov A, Zhang J, Heffernan T, Johnson RL, Chin L, Wang YA, Draetta G, DePinho RA. Yap1 activation enables bypass of oncogenic Kras addiction in pancreatic cancer. Cell. 2014;158:185–197. doi: 10.1016/j.cell.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Shao DD, Xue W, Krall EB, Bhutkar A, Piccioni F, Wang X, Schinzel AC, Sood S, Rosenbluh J, Kim JW, Zwang Y, Roberts TM, Root DE, Jacks T, Hahn WC. KRAS and YAP1 converge to regulate EMT and tumor survival. Cell. 2014;158:171–184. doi: 10.1016/j.cell.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Greten FR. YAP1 takes over when oncogenic K-Ras slumbers. Cell. 2014;158:11–12. doi: 10.1016/j.cell.2014.06.021. [DOI] [PubMed] [Google Scholar]
- 107.Ying H, Dey P, Yao W, Kimmelman AC, Draetta GF, Maitra A, DePinho RA. Genetics and biology of pancreatic ductal adenocarcinoma. Genes Dev. 2016;30:355–385. doi: 10.1101/gad.275776.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yu FX, Zhang Y, Park HW, Jewell JL, Chen Q, Deng Y, Pan D, Taylor SS, Lai ZC, Guan KL. Protein kinase A activates the Hippo pathway to modulate cell proliferation and differentiation. Genes Dev. 2013;27:1223–1232. doi: 10.1101/gad.219402.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim M, Kim M, Lee S, Kuninaka S, Saya H, Lee H, Lee S, Lim DS. cAMP/PKA signalling reinforces the LATS-YAP pathway to fully suppress YAP in response to actin cytoskeletal changes. EMBO J. 2013;32:1543–1555. doi: 10.1038/emboj.2013.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ideno N, Yamaguchi H, Ghosh B, Gupta S, Okumura T, Steffen DJ, Fisher CG, Wood LD, Singhi AD, Nakamura M, Gutkind JS, Maitra A. GNASR201C Induces Pancreatic Cystic Neoplasms in Mice That Express Activated KRAS by Inhibiting YAP1 Signaling. Gastroenterology. 2018;155:1593–1607.e12. doi: 10.1053/j.gastro.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Suklabaidya S, Dash P, Das B, Suresh V, Sasmal PK, Senapati S. Experimental models of pancreatic cancer desmoplasia. Lab Invest. 2018;98:27–40. doi: 10.1038/labinvest.2017.127. [DOI] [PubMed] [Google Scholar]
- 112.Panciera T, Azzolin L, Cordenonsi M, Piccolo S. Mechanobiology of YAP and TAZ in physiology and disease. Nat Rev Mol Cell Biol. 2017;18:758–770. doi: 10.1038/nrm.2017.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Low BC, Pan CQ, Shivashankar GV, Bershadsky A, Sudol M, Sheetz M. YAP/TAZ as mechanosensors and mechanotransducers in regulating organ size and tumor growth. FEBS Lett. 2014;588:2663–2670. doi: 10.1016/j.febslet.2014.04.012. [DOI] [PubMed] [Google Scholar]
- 114.Ibar C, Irvine KD. Rapping about Mechanotransduction. Dev Cell. 2018;46:678–679. doi: 10.1016/j.devcel.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 115.Meng Z, Qiu Y, Lin KC, Kumar A, Placone JK, Fang C, Wang KC, Lu S, Pan M, Hong AW, Moroishi T, Luo M, Plouffe SW, Diao Y, Ye Z, Park HW, Wang X, Yu FX, Chien S, Wang CY, Ren B, Engler AJ, Guan KL. RAP2 mediates mechanoresponses of the Hippo pathway. Nature. 2018;560:655–660. doi: 10.1038/s41586-018-0444-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yang S, Zhang L, Purohit V, Shukla SK, Chen X, Yu F, Fu K, Chen Y, Solheim J, Singh PK, Song W, Dong J. Active YAP promotes pancreatic cancer cell motility, invasion and tumorigenesis in a mitotic phosphorylation-dependent manner through LPAR3. Oncotarget. 2015;6:36019–36031. doi: 10.18632/oncotarget.5935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Xie D, Cui J, Xia T, Jia Z, Wang L, Wei W, Zhu A, Gao Y, Xie K, Quan M. Hippo transducer TAZ promotes epithelial mesenchymal transition and supports pancreatic cancer progression. Oncotarget. 2015;6:35949–35963. doi: 10.18632/oncotarget.5772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Salcedo Allende MT, Zeron-Medina J, Hernandez J, Macarulla T, Balsells J, Merino X, Allende H, Tabernero J, Ramon Y Cajal S. Overexpression of Yes Associated Protein 1, an Independent Prognostic Marker in Patients With Pancreatic Ductal Adenocarcinoma, Correlated With Liver Metastasis and Poor Prognosis. Pancreas. 2017;46:913–920. doi: 10.1097/MPA.0000000000000867. [DOI] [PubMed] [Google Scholar]
- 119.Uhlen M, Zhang C, Lee S, Sjöstedt E, Fagerberg L, Bidkhori G, Benfeitas R, Arif M, Liu Z, Edfors F, Sanli K, von Feilitzen K, Oksvold P, Lundberg E, Hober S, Nilsson P, Mattsson J, Schwenk JM, Brunnström H, Glimelius B, Sjöblom T, Edqvist PH, Djureinovic D, Micke P, Lindskog C, Mardinoglu A, Ponten F. A pathology atlas of the human cancer transcriptome. Science. 2017:357. doi: 10.1126/science.aan2507. [DOI] [PubMed] [Google Scholar]
- 120.Rozengurt E, Sinnett-Smith J, Eibl G. Yes-associated protein (YAP) in pancreatic cancer: at the epicenter of a targetable signaling network associated with patient survival. Signal Transduct Target Ther. 2018;3:11. doi: 10.1038/s41392-017-0005-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Tang Z, Li C, Kang B, Gao G, Li C, Zhang Z. GEPIA: a web server for cancer and normal gene expression profiling and interactive analyses. Nucleic Acids Res. 2017;45:W98–W102. doi: 10.1093/nar/gkx247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ardestani A, Lupse B, Maedler K. Hippo Signaling: Key Emerging Pathway in Cellular and Whole-Body Metabolism. Trends Endocrinol Metab. 2018;29:492–509. doi: 10.1016/j.tem.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 123.Koo JH, Guan KL. Interplay between YAP/TAZ and Metabolism. Cell Metab. 2018;28:196–206. doi: 10.1016/j.cmet.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 124.Jóźwiak P, Forma E, Bryś M, Krześlak A. O-GlcNAcylation and Metabolic Reprograming in Cancer. Front Endocrinol (Lausanne) 2014;5:145. doi: 10.3389/fendo.2014.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Peng C, Zhu Y, Zhang W, Liao Q, Chen Y, Zhao X, Guo Q, Shen P, Zhen B, Qian X, Yang D, Zhang JS, Xiao D, Qin W, Pei H. Regulation of the Hippo-YAP Pathway by Glucose Sensor O-GlcNAcylation. Mol Cell. 2017;68:591–604.e5. doi: 10.1016/j.molcel.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 126.Kammoun HL, Kraakman MJ, Febbraio MA. Adipose tissue inflammation in glucose metabolism. Rev Endocr Metab Disord. 2014;15:31–44. doi: 10.1007/s11154-013-9274-4. [DOI] [PubMed] [Google Scholar]
- 127.Bai Y, Sun Q. Macrophage recruitment in obese adipose tissue. Obes Rev. 2015;16:127–136. doi: 10.1111/obr.12242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Boutens L, Stienstra R. Adipose tissue macrophages: going off track during obesity. Diabetologia. 2016;59:879–894. doi: 10.1007/s00125-016-3904-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Castoldi A, Naffah de Souza C, Câmara NO, Moraes-Vieira PM. The Macrophage Switch in Obesity Development. Front Immunol. 2016;6:637. doi: 10.3389/fimmu.2015.00637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hill AA, Reid Bolus W, Hasty AH. A decade of progress in adipose tissue macrophage biology. Immunol Rev. 2014;262:134–152. doi: 10.1111/imr.12216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Reilly SM, Saltiel AR. Adapting to obesity with adipose tissue inflammation. Nat Rev Endocrinol. 2017;13:633–643. doi: 10.1038/nrendo.2017.90. [DOI] [PubMed] [Google Scholar]
- 132.Wensveen FM, Valentić S, Šestan M, Turk Wensveen T, Polić B. The "Big Bang" in obese fat: Events initiating obesity-induced adipose tissue inflammation. Eur J Immunol. 2015;45:2446–2456. doi: 10.1002/eji.201545502. [DOI] [PubMed] [Google Scholar]
- 133.An Y, Kang Q, Zhao Y, Hu X, Li N. Lats2 modulates adipocyte proliferation and differentiation via hippo signaling. PLoS One. 2013;8:e72042. doi: 10.1371/journal.pone.0072042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Seo E, Basu-Roy U, Gunaratne PH, Coarfa C, Lim DS, Basilico C, Mansukhani A. SOX2 regulates YAP1 to maintain stemness and determine cell fate in the osteo-adipo lineage. Cell Rep. 2013;3:2075–2087. doi: 10.1016/j.celrep.2013.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kuroda M, Wada H, Kimura Y, Ueda K, Kioka N. Vinculin promotes nuclear localization of TAZ to inhibit ECM stiffness-dependent differentiation into adipocytes. J Cell Sci. 2017;130:989–1002. doi: 10.1242/jcs.194779. [DOI] [PubMed] [Google Scholar]
- 136.Li Y, Du J, Zhu E, Zhang J, Han J, Zhao W, Sun B, Tian D. Liraglutide suppresses proliferation and induces adipogenic differentiation of 3T3-L1 cells via the Hippo-YAP signaling pathway. Mol Med Rep. 2018;17:4499–4507. doi: 10.3892/mmr.2018.8438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Basu-Roy U, Han E, Rattanakorn K, Gadi A, Verma N, Maurizi G, Gunaratne PH, Coarfa C, Kennedy OD, Garabedian MJ, Basilico C, Mansukhani A. PPARγ agonists promote differentiation of cancer stem cells by restraining YAP transcriptional activity. Oncotarget. 2016;7:60954–60970. doi: 10.18632/oncotarget.11273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Chang CC, Chen CY, Chang GD, Chen TH, Chen WL, Wen HC, Huang CY, Chang CH. Hyperglycemia and advanced glycation end products (AGEs) suppress the differentiation of 3T3-L1 preadipocytes. Oncotarget. 2017;8:55039–55050. doi: 10.18632/oncotarget.18993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Huang YJ, Yang CK, Wei PL, Huynh TT, Whang-Peng J, Meng TC, Hsiao M, Tzeng YM, Wu AT, Yen Y. Ovatodiolide suppresses colon tumorigenesis and prevents polarization of M2 tumor-associated macrophages through YAP oncogenic pathways. J Hematol Oncol. 2017;10:60. doi: 10.1186/s13045-017-0421-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.McWhorter FY, Wang T, Nguyen P, Chung T, Liu WF. Modulation of macrophage phenotype by cell shape. Proc Natl Acad Sci USA. 2013;110:17253–17258. doi: 10.1073/pnas.1308887110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pellegrinelli V, Heuvingh J, du Roure O, Rouault C, Devulder A, Klein C, Lacasa M, Clément E, Lacasa D, Clément K. Human adipocyte function is impacted by mechanical cues. J Pathol. 2014;233:183–195. doi: 10.1002/path.4347. [DOI] [PubMed] [Google Scholar]
- 142.Hertzer KM, Xu M, Moro A, Dawson DW, Du L, Li G, Chang HH, Stark AP, Jung X, Hines OJ, Eibl G. Robust Early Inflammation of the Peripancreatic Visceral Adipose Tissue During Diet-Induced Obesity in the KrasG12D Model of Pancreatic Cancer. Pancreas. 2016;45:458–465. doi: 10.1097/MPA.0000000000000497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Xu M, Chang HH, Jung X, Moro A, Chou CEN, King J, Hines OJ, Sinnett-Smith J, Rozengurt E, Eibl G. Deficiency in hormone-sensitive lipase accelerates the development of pancreatic cancer in conditional KrasG12D mice. BMC Cancer. 2018;18:797. doi: 10.1186/s12885-018-4713-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Freed-Pastor WA, Mizuno H, Zhao X, Langerød A, Moon SH, Rodriguez-Barrueco R, Barsotti A, Chicas A, Li W, Polotskaia A, Bissell MJ, Osborne TF, Tian B, Lowe SW, Silva JM, Børresen-Dale AL, Levine AJ, Bargonetti J, Prives C. Mutant p53 disrupts mammary tissue architecture via the mevalonate pathway. Cell. 2012;148:244–258. doi: 10.1016/j.cell.2011.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Clendening JW, Pandyra A, Boutros PC, El Ghamrasni S, Khosravi F, Trentin GA, Martirosyan A, Hakem A, Hakem R, Jurisica I, Penn LZ. Dysregulation of the mevalonate pathway promotes transformation. Proc Natl Acad Sci USA. 2010;107:15051–15056. doi: 10.1073/pnas.0910258107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kuzu OF, Noory MA, Robertson GP. The Role of Cholesterol in Cancer. Cancer Res. 2016;76:2063–2070. doi: 10.1158/0008-5472.CAN-15-2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Istvan ES, Deisenhofer J. Structural mechanism for statin inhibition of HMG-CoA reductase. Science. 2001;292:1160–1164. doi: 10.1126/science.1059344. [DOI] [PubMed] [Google Scholar]
- 148.Jeon CY, Pandol SJ, Wu B, Cook-Wiens G, Gottlieb RA, Merz CN, Goodman MT. The association of statin use after cancer diagnosis with survival in pancreatic cancer patients: a SEER-medicare analysis. PLoS One. 2015;10:e0121783. doi: 10.1371/journal.pone.0121783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wu BU, Chang J, Jeon CY, Pandol SJ, Huang B, Ngor EW, Difronzo AL, Cooper RM. Impact of statin use on survival in patients undergoing resection for early-stage pancreatic cancer. Am J Gastroenterol. 2015;110:1233–1239. doi: 10.1038/ajg.2015.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Chen MJ, Tsan YT, Liou JM, Lee YC, Wu MS, Chiu HM, Wang HP, Chen PC. Statins and the risk of pancreatic cancer in Type 2 diabetic patients--A population-based cohort study. Int J Cancer. 2016;138:594–603. doi: 10.1002/ijc.29813. [DOI] [PubMed] [Google Scholar]
- 151.Walker EJ, Ko AH, Holly EA, Bracci PM. Statin use and risk of pancreatic cancer: results from a large, clinic-based case-control study. Cancer. 2015;121:1287–1294. doi: 10.1002/cncr.29256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Carey FJ, Little MW, Pugh TF, Ndokera R, Ing H, Clark A, Dennison A, Metcalfe MS, Robinson RJ, Hart AR. The differential effects of statins on the risk of developing pancreatic cancer: a case-control study in two centres in the United Kingdom. Dig Dis Sci. 2013;58:3308–3312. doi: 10.1007/s10620-013-2778-7. [DOI] [PubMed] [Google Scholar]
- 153.E JY, Lu SE, Lin Y, Graber JM, Rotter D, Zhang L, Petersen GM, Demissie K, Lu-Yao G, Tan XL. Differential and Joint Effects of Metformin and Statins on Overall Survival of Elderly Patients with Pancreatic Adenocarcinoma: A Large Population-Based Study. Cancer Epidemiol Biomarkers Prev. 2017;26:1225–1232. doi: 10.1158/1055-9965.EPI-17-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Iarrobino NA, Gill B, Bernard ME, Mishra MV, Champ CE. Targeting Tumor Metabolism With Statins During Treatment for Advanced-stage Pancreatic Cancer. Am J Clin Oncol. 2018 doi: 10.1097/COC.0000000000000433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Jian-Yu E, Graber JM, Lu SE, Lin Y, Lu-Yao G, Tan XL. Effect of Metformin and Statin Use on Survival in Pancreatic Cancer Patients: a Systematic Literature Review and Meta-analysis. Curr Med Chem. 2018;25:2595–2607. doi: 10.2174/0929867324666170412145232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bang UC, Watanabe T, Bendtsen F. The relationship between the use of statins and mortality, severity, and pancreatic cancer in Danish patients with chronic pancreatitis. Eur J Gastroenterol Hepatol. 2018;30:346–351. doi: 10.1097/MEG.0000000000001060. [DOI] [PubMed] [Google Scholar]
- 157.Liu Y, Tang W, Wang J, Xie L, Li T, He Y, Deng Y, Peng Q, Li S, Qin X. Association between statin use and colorectal cancer risk: a meta-analysis of 42 studies. Cancer Causes Control. 2014;25:237–249. doi: 10.1007/s10552-013-0326-6. [DOI] [PubMed] [Google Scholar]
- 158.Manthravadi S, Shrestha A, Madhusudhana S. Impact of statin use on cancer recurrence and mortality in breast cancer: A systematic review and meta-analysis. Int J Cancer. 2016;139:1281–1288. doi: 10.1002/ijc.30185. [DOI] [PubMed] [Google Scholar]
- 159.Anothaisintawee T, Udomsubpayakul U, McEvoy M, Lerdsitthichai P, Attia J, Thakkinstian A. Effect of Lipophilic and Hydrophilic Statins on Breast Cancer Risk in Thai Women: A Cross-sectional Study. J Cancer. 2016;7:1163–1168. doi: 10.7150/jca.14941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Liu B, Yi Z, Guan X, Zeng YX, Ma F. The relationship between statins and breast cancer prognosis varies by statin type and exposure time: a meta-analysis. Breast Cancer Res Treat. 2017;164:1–11. doi: 10.1007/s10549-017-4246-0. [DOI] [PubMed] [Google Scholar]
- 161.Hamada T, Khalaf N, Yuan C, Babic A, Morales-Oyarvide V, Qian ZR, Nowak JA, Ng K, Kraft P, Rubinson DA, Stampfer MJ, Giovannucci EL, Fuchs CS, Ogino S, Wolpin BM. Statin use and pancreatic cancer risk in two prospective cohort studies. J Gastroenterol. 2018;53:959–966. doi: 10.1007/s00535-018-1430-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hamada T, Khalaf N, Yuan C, Morales-Oyarvide V, Babic A, Nowak JA, Qian ZR, Ng K, Rubinson DA, Kraft P, Giovannucci EL, Stampfer MJ, Fuchs CS, Ogino S, Wolpin BM. Prediagnosis Use of Statins Associates With Increased Survival Times of Patients With Pancreatic Cancer. Clin Gastroenterol Hepatol. 2018;16:1300–1306.e3. doi: 10.1016/j.cgh.2018.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Zhang Y, Liang M, Sun C, Qu G, Shi T, Min M, Wu Y, Sun Y. Statin Use and Risk of Pancreatic Cancer: An Updated Meta-analysis of 26 Studies. Pancreas. 2019;48:142–150. doi: 10.1097/MPA.0000000000001226. [DOI] [PubMed] [Google Scholar]
- 164.Lee HS, Lee SH, Lee HJ, Chung MJ, Park JY, Park SW, Song SY, Bang S. Statin Use and Its Impact on Survival in Pancreatic Cancer Patients. Medicine (Baltimore) 2016;95:e3607. doi: 10.1097/MD.0000000000003607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Mohammed A, Qian L, Janakiram NB, Lightfoot S, Steele VE, Rao CV. Atorvastatin delays progression of pancreatic lesions to carcinoma by regulating PI3/AKT signaling in p48Cre/+ LSL-KrasG12D/+ mice. Int J Cancer. 2012;131:1951–1962. doi: 10.1002/ijc.27456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Fendrich V, Sparn M, Lauth M, Knoop R, Plassmeier L, Bartsch DK, Waldmann J. Simvastatin delay progression of pancreatic intraepithelial neoplasia and cancer formation in a genetically engineered mouse model of pancreatic cancer. Pancreatology. 2013;13:502–507. doi: 10.1016/j.pan.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 167.Sorrentino G, Ruggeri N, Specchia V, Cordenonsi M, Mano M, Dupont S, Manfrin A, Ingallina E, Sommaggio R, Piazza S, Rosato A, Piccolo S, Del Sal G. Metabolic control of YAP and TAZ by the mevalonate pathway. Nat Cell Biol. 2014;16:357–366. doi: 10.1038/ncb2936. [DOI] [PubMed] [Google Scholar]
- 168.Witters LA. The blooming of the French lilac. J Clin Invest. 2001;108:1105–1107. doi: 10.1172/JCI14178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Kahn BB, Alquier T, Carling D, Hardie DG. AMP-activated protein kinase: ancient energy gauge provides clues to modern understanding of metabolism. Cell Metab. 2005;1:15–25. doi: 10.1016/j.cmet.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 170.Shaw RJ, Lamia KA, Vasquez D, Koo SH, Bardeesy N, Depinho RA, Montminy M, Cantley LC. The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin. Science. 2005;310:1642–1646. doi: 10.1126/science.1120781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Berker B, Emral R, Demirel C, Corapcioglu D, Unlu C, Kose K. Increased insulin-like growth factor-I levels in women with polycystic ovary syndrome, and beneficial effects of metformin therapy. Gynecol Endocrinol. 2004;19:125–133. doi: 10.1080/09513590400007309. [DOI] [PubMed] [Google Scholar]
- 172.Goodwin PJ, Pritchard KI, Ennis M, Clemons M, Graham M, Fantus IG. Insulin-lowering effects of metformin in women with early breast cancer. Clin Breast Cancer. 2008;8:501–505. doi: 10.3816/CBC.2008.n.060. [DOI] [PubMed] [Google Scholar]
- 173.Evans JM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD. Metformin and reduced risk of cancer in diabetic patients. BMJ. 2005;330:1304–1305. doi: 10.1136/bmj.38415.708634.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Li D, Yeung SC, Hassan MM, Konopleva M, Abbruzzese JL. Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology. 2009;137:482–488. doi: 10.1053/j.gastro.2009.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Libby G, Donnelly LA, Donnan PT, Alessi DR, Morris AD, Evans JM. New users of metformin are at low risk of incident cancer: a cohort study among people with type 2 diabetes. Diabetes Care. 2009;32:1620–1625. doi: 10.2337/dc08-2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ben Sahra I, Le Marchand-Brustel Y, Tanti JF, Bost F. Metformin in cancer therapy: a new perspective for an old antidiabetic drug? Mol Cancer Ther. 2010;9:1092–1099. doi: 10.1158/1535-7163.MCT-09-1186. [DOI] [PubMed] [Google Scholar]
- 177.Sadeghi N, Abbruzzese JL, Yeung SC, Hassan M, Li D. Metformin use is associated with better survival of diabetic patients with pancreatic cancer. Clin Cancer Res. 2012;18:2905–2912. doi: 10.1158/1078-0432.CCR-11-2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Li X, Li T, Liu Z, Gou S, Wang C. The effect of metformin on survival of patients with pancreatic cancer: a meta-analysis. Sci Rep. 2017;7:5825. doi: 10.1038/s41598-017-06207-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Lega IC, Shah PS, Margel D, Beyene J, Rochon PA, Lipscombe LL. The effect of metformin on mortality following cancer among patients with diabetes. Cancer Epidemiol Biomarkers Prev. 2014;23:1974–1984. doi: 10.1158/1055-9965.EPI-14-0327. [DOI] [PubMed] [Google Scholar]
- 180.Amin S, Mhango G, Lin J, Aronson A, Wisnivesky J, Boffetta P, Lucas AL. Metformin Improves Survival in Patients with Pancreatic Ductal Adenocarcinoma and Pre-Existing Diabetes: A Propensity Score Analysis. Am J Gastroenterol. 2016;111:1350–1357. doi: 10.1038/ajg.2016.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Lee DY, Yu JH, Park S, Han K, Kim NH, Yoo HJ, Choi KM, Baik SH, Kim NH, Seo JA. The influence of diabetes and antidiabetic medications on the risk of pancreatic cancer: a nationwide population-based study in Korea. Sci Rep. 2018;8:9719. doi: 10.1038/s41598-018-27965-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Xin W, Fang L, Fang Q, Zheng X, Huang P. Effects of metformin on survival outcomes of pancreatic cancer patients with diabetes: A meta-analysis. Mol Clin Oncol. 2018;8:483–488. doi: 10.3892/mco.2017.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Suissa S, Azoulay L. Metformin and cancer: mounting evidence against an association. Diabetes Care. 2014;37:1786–1788. doi: 10.2337/dc14-0500. [DOI] [PubMed] [Google Scholar]
- 184.Wan G, Sun X, Li F, Wang X, Li C, Li H, Yu X, Cao F. Survival Benefit of Metformin Adjuvant Treatment For Pancreatic Cancer Patients: a Systematic Review and Meta-Analysis. Cell Physiol Biochem. 2018;49:837–847. doi: 10.1159/000493214. [DOI] [PubMed] [Google Scholar]
- 185.Jang WI, Kim MS, Kang SH, Jo AJ, Kim YJ, Tchoe HJ, Park CM, Kim HJ, Choi JA, Choi HJ, Paik EK, Seo YS, Yoo HJ, Kang JK, Han CJ, Kim YJ, Kim SB, Ko MJ. Association between metformin use and mortality in patients with type 2 diabetes mellitus and localized resectable pancreatic cancer: a nationwide population-based study in korea. Oncotarget. 2017;8:9587–9596. doi: 10.18632/oncotarget.14525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Cerullo M, Gani F, Chen SY, Canner J, Pawlik TM. Metformin Use Is Associated with Improved Survival in Patients Undergoing Resection for Pancreatic Cancer. J Gastrointest Surg. 2016;20:1572–1580. doi: 10.1007/s11605-016-3173-4. [DOI] [PubMed] [Google Scholar]
- 187.Hawley SA, Ross FA, Chevtzoff C, Green KA, Evans A, Fogarty S, Towler MC, Brown LJ, Ogunbayo OA, Evans AM, Hardie DG. Use of cells expressing gamma subunit variants to identify diverse mechanisms of AMPK activation. Cell Metab. 2010;11:554–565. doi: 10.1016/j.cmet.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Ben Sahra I, Laurent K, Loubat A, Giorgetti-Peraldi S, Colosetti P, Auberger P, Tanti JF, Le Marchand-Brustel Y, Bost F. The antidiabetic drug metformin exerts an antitumoral effect in vitro and in vivo through a decrease of cyclin D1 level. Oncogene. 2008;27:3576–3586. doi: 10.1038/sj.onc.1211024. [DOI] [PubMed] [Google Scholar]
- 189.Kalender A, Selvaraj A, Kim SY, Gulati P, Brûlé S, Viollet B, Kemp BE, Bardeesy N, Dennis P, Schlager JJ, Marette A, Kozma SC, Thomas G. Metformin, independent of AMPK, inhibits mTORC1 in a rag GTPase-dependent manner. Cell Metab. 2010;11:390–401. doi: 10.1016/j.cmet.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Hezel AF, Bardeesy N. LKB1; linking cell structure and tumor suppression. Oncogene. 2008;27:6908–6919. doi: 10.1038/onc.2008.342. [DOI] [PubMed] [Google Scholar]
- 191.Owen MR, Doran E, Halestrap AP. Evidence that metformin exerts its anti-diabetic effects through inhibition of complex 1 of the mitochondrial respiratory chain. Biochem J. 2000;348 Pt 3:607–614. [PMC free article] [PubMed] [Google Scholar]
- 192.El-Mir MY, Nogueira V, Fontaine E, Avéret N, Rigoulet M, Leverve X. Dimethylbiguanide inhibits cell respiration via an indirect effect targeted on the respiratory chain complex I. J Biol Chem. 2000;275:223–228. doi: 10.1074/jbc.275.1.223. [DOI] [PubMed] [Google Scholar]
- 193.Inoki K, Zhu T, Guan KL. TSC2 mediates cellular energy response to control cell growth and survival. Cell. 2003;115:577–590. doi: 10.1016/s0092-8674(03)00929-2. [DOI] [PubMed] [Google Scholar]
- 194.Shaw RJ, Bardeesy N, Manning BD, Lopez L, Kosmatka M, DePinho RA, Cantley LC. The LKB1 tumor suppressor negatively regulates mTOR signaling. Cancer Cell. 2004;6:91–99. doi: 10.1016/j.ccr.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 195.Inoki K, Ouyang H, Zhu T, Lindvall C, Wang Y, Zhang X, Yang Q, Bennett C, Harada Y, Stankunas K, Wang CY, He X, MacDougald OA, You M, Williams BO, Guan KL. TSC2 integrates Wnt and energy signals via a coordinated phosphorylation by AMPK and GSK3 to regulate cell growth. Cell. 2006;126:955–968. doi: 10.1016/j.cell.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 196.Gwinn DM, Shackelford DB, Egan DF, Mihaylova MM, Mery A, Vasquez DS, Turk BE, Shaw RJ. AMPK phosphorylation of raptor mediates a metabolic checkpoint. Mol Cell. 2008;30:214–226. doi: 10.1016/j.molcel.2008.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Tzatsos A, Tsichlis PN. Energy depletion inhibits phosphatidylinositol 3-kinase/Akt signaling and induces apoptosis via AMP-activated protein kinase-dependent phosphorylation of IRS-1 at Ser-794. J Biol Chem. 2007;282:18069–18082. doi: 10.1074/jbc.M610101200. [DOI] [PubMed] [Google Scholar]
- 198.Ning J, Clemmons DR. AMP-activated protein kinase inhibits IGF-I signaling and protein synthesis in vascular smooth muscle cells via stimulation of insulin receptor substrate 1 S794 and tuberous sclerosis 2 S1345 phosphorylation. Mol Endocrinol. 2010;24:1218–1229. doi: 10.1210/me.2009-0474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Sinnett-Smith J, Kisfalvi K, Kui R, Rozengurt E. Metformin inhibition of mTORC1 activation, DNA synthesis and proliferation in pancreatic cancer cells: dependence on glucose concentration and role of AMPK. Biochem Biophys Res Commun. 2013;430:352–357. doi: 10.1016/j.bbrc.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Soares HP, Ni Y, Kisfalvi K, Sinnett-Smith J, Rozengurt E. Different patterns of Akt and ERK feedback activation in response to rapamycin, active-site mTOR inhibitors and metformin in pancreatic cancer cells. PLoS One. 2013;8:e57289. doi: 10.1371/journal.pone.0057289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Ming M, Sinnett-Smith J, Wang J, Soares HP, Young SH, Eibl G, Rozengurt E. Dose-Dependent AMPK-Dependent and Independent Mechanisms of Berberine and Metformin Inhibition of mTORC1, ERK, DNA Synthesis and Proliferation in Pancreatic Cancer Cells. PLoS One. 2014;9:e114573. doi: 10.1371/journal.pone.0114573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Kisfalvi K, Eibl G, Sinnett-Smith J, Rozengurt E. Metformin disrupts crosstalk between G protein-coupled receptor and insulin receptor signaling systems and inhibits pancreatic cancer growth. Cancer Res. 2009;69:6539–6545. doi: 10.1158/0008-5472.CAN-09-0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Kisfalvi K, Moro A, Sinnett-Smith J, Eibl G, Rozengurt E. Metformin inhibits the growth of human pancreatic cancer xenografts. Pancreas. 2013;42:781–785. doi: 10.1097/MPA.0b013e31827aec40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Chang HH, Moro A, Chou CEN, Dawson DW, French S, Schmidt AI, Sinnett-Smith J, Hao F, Hines OJ, Eibl G, Rozengurt E. Metformin Decreases the Incidence of Pancreatic Ductal Adenocarcinoma Promoted by Diet-induced Obesity in the Conditional KrasG12D Mouse Model. Sci Rep. 2018;8:5899. doi: 10.1038/s41598-018-24337-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Mo JS, Meng Z, Kim YC, Park HW, Hansen CG, Kim S, Lim DS, Guan KL. Cellular energy stress induces AMPK-mediated regulation of YAP and the Hippo pathway. Nat Cell Biol. 2015;17:500–510. doi: 10.1038/ncb3111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wang W, Xiao ZD, Li X, Aziz KE, Gan B, Johnson RL, Chen J. AMPK modulates Hippo pathway activity to regulate energy homeostasis. Nat Cell Biol. 2015;17:490–499. doi: 10.1038/ncb3113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Omkumar RV, Darnay BG, Rodwell VW. Modulation of Syrian hamster 3-hydroxy-3-methylglutaryl-CoA reductase activity by phosphorylation. Role of serine 871. J Biol Chem. 1994;269:6810–6814. [PubMed] [Google Scholar]
- 208.DeRan M, Yang J, Shen CH, Peters EC, Fitamant J, Chan P, Hsieh M, Zhu S, Asara JM, Zheng B, Bardeesy N, Liu J, Wu X. Energy stress regulates hippo-YAP signaling involving AMPK-mediated regulation of angiomotin-like 1 protein. Cell Rep. 2014;9:495–503. doi: 10.1016/j.celrep.2014.09.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sahai V, Kumar K, Knab LM, Chow CR, Raza SS, Bentrem DJ, Ebine K, Munshi HG. BET bromodomain inhibitors block growth of pancreatic cancer cells in three-dimensional collagen. Mol Cancer Ther. 2014;13:1907–1917. doi: 10.1158/1535-7163.MCT-13-0925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Filippakopoulos P, Qi J, Picaud S, Shen Y, Smith WB, Fedorov O, Morse EM, Keates T, Hickman TT, Felletar I, Philpott M, Munro S, McKeown MR, Wang Y, Christie AL, West N, Cameron MJ, Schwartz B, Heightman TD, La Thangue N, French CA, Wiest O, Kung AL, Knapp S, Bradner JE. Selective inhibition of BET bromodomains. Nature. 2010;468:1067–1073. doi: 10.1038/nature09504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Liu Z, Wang P, Chen H, Wold EA, Tian B, Brasier AR, Zhou J. Drug Discovery Targeting Bromodomain-Containing Protein 4. J Med Chem. 2017;60:4533–4558. doi: 10.1021/acs.jmedchem.6b01761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Tanti JF, Jager J. Cellular mechanisms of insulin resistance: role of stress-regulated serine kinases and insulin receptor substrates (IRS) serine phosphorylation. Curr Opin Pharmacol. 2009;9:753–762. doi: 10.1016/j.coph.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 213.Soares HP, Ming M, Mellon M, Young SH, Han L, Sinnet-Smith J, Rozengurt E. Dual PI3K/mTOR Inhibitors Induce Rapid Overactivation of the MEK/ERK Pathway in Human Pancreatic Cancer Cells through Suppression of mTORC2. Mol Cancer Ther. 2015;14:1014–1023. doi: 10.1158/1535-7163.MCT-14-0669. [DOI] [PMC free article] [PubMed] [Google Scholar]