Abstract
Cryptococcal meningitis is considered one of the AIDS-defining illness and has been reported to be associated with neurological sequels. However, acute vision loss as presenting complaint is rare in Cryptococcal meningitis. Management of Cryptococcal meningitis with antifungal therapy may not lead to favourable outcomes and may necessitate the need for invasive intervention. We report a case of acute bilateral visual loss secondary to Cryptococcal meningitis.
Keywords: Cryptococcal meningitis, HIV/AIDS, Vision loss, Ocular complications, Amphotericin B
1. Introduction
Cryptococcal meningitis (CM) is a severe opportunistic central nervous system fungal infection primarily seen in immune compromised patients with human immunodeficiency virus (HIV) [1]. Nearly 40% of patients with Cryptococcal meningitis will develop ocular involvement [2]. However, visual loss as presenting complaint in HIV patients secondary to Cryptococcal meningitis is uncommon [2,3]. Around 10% of the patients with Acquired Immunodeficiency Syndrome (AIDS) patients and Cryptococcus infection and often associated with other comorbidities, such as Cytomegalovirus (CMV) retinitis [4]. The etiology of the vision complications associated with Cryptococcal meningitis remains unclear. Possible explanations for vision loss with Cryptococcal infection include direct infiltration or perineuritic arachnoiditis and invasion of the optic nerve or optic tracts by the fungus leading to vision loss [2,5]. Also, inflammatory compression of optic never, adhesive arachnoiditis, cerebral vasculitis, intracranial hypertension, and amphotericin B toxicity can also lead to vision loss [[6], [7], [8], [9]]. Raised intracranial pressure leading to visual loss is considered the most common mechanism of vision loss [10,11]. Antifungal therapeutics may not be sufficient even with early detection of infection, necessitating aggressive interventions to lower the intracranial pressure to reduce the visual complications and may also prevent permanent visual loss [7].
Here, we report a case of a patient presented with bilateral vision loss secondary to Cryptococcal meningitis in an AIDS patient.
2. The case
A 35-year-old patient brought to the hospital after being found unconscious in the bathroom. He reported having a severe headache from the past two months and also having a sore throat, neck pain and night sweating from past two weeks. This was associated with progressive vision deterioration and acute blindness. The patient also reported having a body rash and recurrent oral ulcers in the past. He denied alcohol or smoking use ever, however, gave a history of unprotected sex with multiple partners.
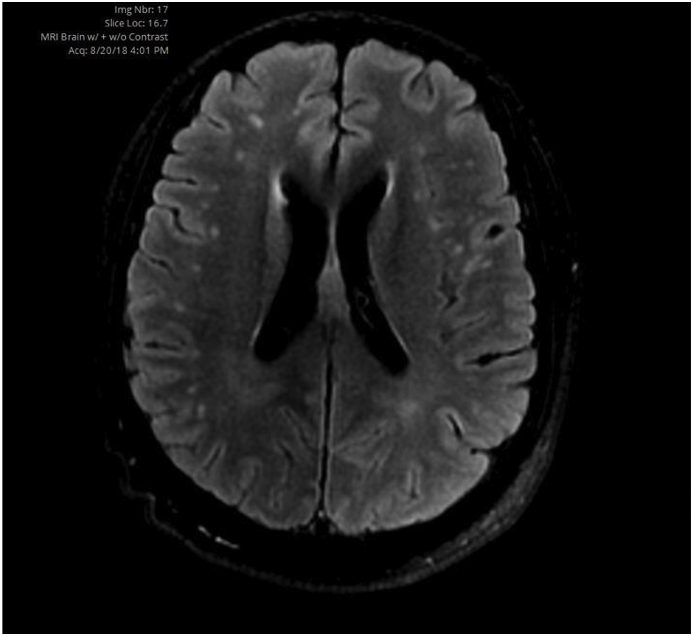
In the emergency department, the CT scan showed leptomeningeal enhancement suggestive of acute meningitis. Lumbar puncture was performed in the emergency room which revealed the protein of 0.6 g/L, nucleated cells of 4 × 106 L, glucose of 3 mmol/L (54 mg/dl) as shown in Table 1. The cerebrospinal fluid (CSF) and blood cultures grew Cryptococcus neoformans which were also supported by positive India Ink test. Following admission, the patient was diagnosed positive HIV1 in the ELISA and Western Blot tests, and his HIV viral load was 288,054 copies while his CD4 cell count was 15 cells. During hospitalization, MRI scan was performed and showed patchy white matter changes in the supratentorial area mainly subcortical white matters with some periventricular signal changes, but no visual pathway defects were noticed [Fig. 1] (see Fig. 2).
Table 1.
Initial CSF analysis.
| Cerebrospinal Fluid Analysis | |
|---|---|
| Appearance | Crystal Clear |
| RBC CSF | 2,000 × 106/L |
| Nucleated Cells CSF | 4 × 106/L |
| Protein CSF | 0.6 g/L |
| Glucose CSF | 3 mmol/L |
Fig. 1.
MRI scan on prior to commencing treatment.
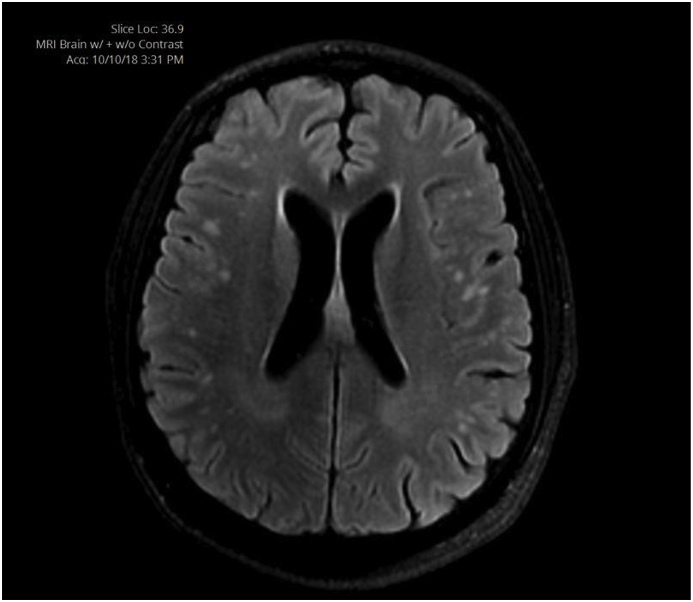
Fig. 2.
MRI scan after one month of treatment.
An ophthalmology consultation was obtained, which revealed complete vision loss in both eyes and partial sixth never palsy on the right. The fundoscopic examination identified bitemporal optic disc paleness with right temporal optic disc atrophy, no evidence of papilledema nor CMV retinitis. There was no chorioretinitis or vitritis seen on examination.
The patient was treated with intravenous (IV) Liposomal amphotericin B (6 mg/kg) and fluconazole (800 mg/day) beginning on the day of admission and was continued for three weeks. He has a persistently growing Cryptococcus neoformans noticed in the CSF culture and also showed a positive India Ink tests at week 2 of the therapy. At week 3, another CSF analysis was done and showed negative to Cryptococcus neoformans. At discharge, Fluconazole was continued for seven weeks, and the patient showed dramatic improvement in the form of resolution of a headache, but unfortunately, he had permanent vision loss. Furthermore, MRI scan was performed after one month of therapy and showed persistent white matter changes, but no meningeal enhancement.
3. Discussion
Cryptococcus meningitis has become more prevalent as an opportunistic infection in HIV/AIDS patients. Although Cryptococcal meningitis associated with neurological complications and intracranial hypertension, however ocular complications due to Cryptococcal meningitis in patients with HIV/AIDS are uncommon. Kenstelyn et al. reported four cases of bilateral vision loss in patients with AIDS; however, most of them had other concurrent opportunistic infections (CMV retinitis) [9]. In a 12-years retrospective study from Australia on Cryptococcus meningitis identified 10% of patients developed permanent blindness due to a chronic increase in intracranial pressure. In our case, the patient has reported persistent headache from the past two months with gradual visual deterioration over four days that lead to permanent vision loss. It is noteworthy that our patient presented with vision loss secondary to Cryptococcus meningitis, however, such occurrences are rare.
The etiological mechanism for the rapid onset of vision loss (<3 days) was thought to result from direct infiltration of the optic nerves or adhesive or inflammatory arachnoiditis [5,9]. In our patient, the mechanism for vision loss may be due to direct infiltration of optic nerve or damage to the pathway, although this was not supported by the MRI scan. Studies suggested that the direct infection of the optic nerve with Cryptococcus can also result in rapidly progressing optic neuropathy and permanent damage to the optic nerve [3,10]. However, compared to other case reports, it is important to mention that our patient did not have visual pathway affection in the MRI scan nor papilledema on examination. Studies suggested that MRI of the optic nerve can be a useful indicator of optic nerve infiltration. However, it is complex process, and compression of optic nerve without other endophthalmitis was also observed in some cases [11].
The recommended therapy for Cryptococcal meningitis comprises 2-week induction treatment with liposomal amphotericin B accompanied by fluconazole or flucytosine [12]. After 2-weeks of treatment, our patient still showed culture positive that forced us to extend the liposomal amphotericin B with fluconazole for another week. The patient showed well tolerance to medications and did not report any adverse reactions reported during treatment.
In summary, Cryptococcal meningitis is a serious infection that is considered an AIDS-defining illness, is associated with significant neurological and ophthalmic complications, including vision loss. Our case highlights the severity and irreversibility of the vision loss that is caused by Cryptococcal meningitis. Despite, the availability of antifungal therapy, eradication of the infection can be challenging and warranting invasive intervention.
Conflict of interest
The authors declare no conflict of interest in this study.
Funding
No source of fundings.
Acknowledgment
We thank our colleague Kukkady, M, Radiologist, for retrieving the images of the MRI scan.
Contributor Information
Wafa Ali Aldhaleei, Email: wafa.ali.aldhaleei@gmail.com.
Akshaya Srikanth Bhagavathula, Email: akshaypharmd@gmail.com.
Ameera Alhajeri, Email: amalhajeri@seha.ae.
References
- 1.Armstrong-James D., Meintjes G., Brown G.D. A neglected epidemic: fungal infections in HIV/AIDS. Trends Microbiol. 2014;22(3):120–127. doi: 10.1016/j.tim.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Aderman C.M., Gorovoy I.R., Chao D.L., Bloomer M.M., Obeid A., Stewart J.M. Cryptococcal choroiditis in advanced AIDS with clinicopathologic correlation. Am. J. Ophthalmol. Case Rep. 2018;10:51–54. doi: 10.1016/j.ajoc.2018.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuriakose C., Mishra A., Vanjare H., Raju A., Abraham O. Visual disturbance in patients with cryptococcal meningitis: the road ahead. J. Neurosci. Rural Pract. 2017;8(1):151. doi: 10.4103/0976-3147.193560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kestelyn P.G., Cunningham E.T., Jr. HIV/AIDS and blindness. Bull. World Health Organ. 2001;79(3):208–213. [PMC free article] [PubMed] [Google Scholar]
- 5.Duggan J., Walls H.M. Ocular complications of cryptococcal meningitis in patients with HIV: report of two cases and review of the literature. J. Int. Assoc. Phys. AIDS Care. 2012;11(5):283–288. doi: 10.1177/1545109712448537. [DOI] [PubMed] [Google Scholar]
- 6.Cohen D.B., Glasgow B.J. Bilateral optic nerve cryptococcosis in sudden blindness in patients with acquired immune deficiency syndrome. Ophthalmology. 1993;100(11):1689–1694. doi: 10.1016/s0161-6420(93)31416-8. [DOI] [PubMed] [Google Scholar]
- 7.More A., Garg R., Malhotra H., Kumar N., Uniyal R. Acute vision loss in post-partum period as presenting symptom of HIV-associated cryptococcal meningitis–an unusual case report. BMC Infect. Dis. 2016;16(1):582. doi: 10.1186/s12879-016-1925-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Claus J.J., Portegies P. Reversible blindness in AIDS-related cryptococcal meningitis. Clin. Neurol. Neurosurg. 1998;100(1):51–52. doi: 10.1016/s0303-8467(97)00119-4. [DOI] [PubMed] [Google Scholar]
- 9.Curi AL, Lazera M, Vasconcelos-Santos DV. Cryptococcosis. Intraocular Inflammation 2016 (pp. 1277-1283). Springer, Berlin, Heidelberg.
- 10.Vieira M.A., Cavalcanti M.D., Costa D.L., Eulálio K.D., Vale O.C., Vieira C.P., Costa C.H. Visual evoked potentials show strong positive association with intracranial pressure in patients with cryptococcal meningitis. Arquivos de neuro-psiquiatria. 2015;73(4):309–313. doi: 10.1590/0004-282X20150002. [DOI] [PubMed] [Google Scholar]
- 11.Ghatalia P.A., Vick A., Vattoth S., Roberson G.H., Pappas P.G. Reversible blindness in cryptococcal meningitis with normal intracranial pressure: case report and review of the literature. Clin. Infect. Dis. 2014;59(2):310–313. doi: 10.1093/cid/ciu216. [DOI] [PubMed] [Google Scholar]
- 12.Kestelyn P., Taelman H., Bogaerts J., Kagame A., Aziz M.A., Batungwanayo J., Stevens A.M., Van de Perre P. Ophthalmic manifestations of infections with Cryptococcus neoformans in patients with the acquired immunodeficiency syndrome. Am. J. Ophthalmol. 1993;116(6):721–727. doi: 10.1016/s0002-9394(14)73472-5. [DOI] [PubMed] [Google Scholar]