Abstract
Objective
We perform a systematically search, appraise and synthesize of the best available evidence on the effectiveness of Progressive Muscle Relaxation (PMR) in the adults with schizophrenia, in any setting, regarding anxiety, personal and social functioning, cognition, and well-being.
Method
Major databases were searched to find both published and unpublished studies from inception until April 2017, using Schizophren* AND Relax* as keywords, and studies published in Portuguese, English, Spanish, Italian, French were considered for inclusion in this review. Methodological quality was assessed by two independent reviewers using the Critical Appraisal Checklist for Randomized Controlled Trials from the Joanna Briggs Institute.
Results
From a total of 1172 studies, five studies, involving 216 adults with schizophrenia, met the inclusion criteria for this systematic review after assessment of their methodological quality. These studies reported benefits in experimental group participants after PMR intervention on anxiety (assessed with State anxiety inventory, Beck Anxiety Inventory and Spielberger Trait Anxiety Inventory), well-being (assessed with Subjective Exercise Experiences Scale) and personal and social functioning (assessed with Sheehan Disability Scale and Therapist Rating Scale).
Conclusions
Evidence suggests that PMR was effective in adults diagnosed with schizophrenia, except in one study where was only effective when combined with education. Thus, PMR may be useful to decrease state anxiety, improve well-being and social functioning in adults diagnosed with schizophrenia. However, due to the diversity of clinical intervention designs of PMR (different number and length of sessions) and outcome assessment scales, no strong evidence was found in this systematic review.
Keywords: Psychiatry, Rehabilitation, Nursing
1. Introduction
Schizophrenia is a major psychiatric disorder characterized by a presence of positive and negative symptoms that affect various domains of individual functioning, including work, interpersonal relations, and self-care. The positive symptoms may include delusions, hallucinations, disorganized speech and/or grossly disorganized or catatonic behavior. The negative symptoms may be expressed in form of diminished emotional expression, abulia, anhedonia, avolition or other (American Psychiatric Association, 2013). The acute manifestations of schizophrenia are usually preceded by a long prodromal phase during which the cognition, behavior, communication and/or affect become gradually impaired (NICE, 2010; Tandon et al., 2009), namely in affective domain may be reflected through anxiety, irritability and depression. During this early phase of schizophrenia, the person may additionally experience sleep disturbance and loss of energy. The emergence of bizarre ideas, the excessive preoccupation with new ideas, social withdrawal and impaired role functioning are also frequent (NICE, 2010; Tandon et al., 2009; Meijel, 2003; Melo-Dias and Silva, 2015).
Typically, the inability to fully recover a daily and social functioning may lead to the feeling of poor quality of life (Narvaez et al., 2008), and to the experience of anxiety and depression (Karow et al., 2014; Castle and Bosanac, 2012; Lysaker and Salyers, 2007), that, in turn, can cause psychological distress and burden of the illness. Regarding symptoms of anxiety, they were shown to have an impact on subjective quality of life, with higher ratings of anxiety being associated with lower satisfaction with daily activities, family, health and social relationship (Huppert et al., 2001). The subjective feelings of poor quality of life and symptoms of anxiety and depression are considered as relevant risk factors for the exacerbation of remitted psychotic symptoms and for triggering the evolution of the new acute episode (Tandon et al., 2009).
Symptoms of anxiety can appear early in the course of schizophrenia, affecting negatively the existing prodromal psychotic symptoms and accelerating the onset of psychosis (American Psychiatric Association, 2013; Tandon et al., 2009). Moreover, there is a growing evidence showing that patients with schizophrenia, as compared to general population, have an increased risk of comorbid lifetime anxiety disorders, with prevalence rates ranging from 3.6% to 39.5% (Pallanti et al., 2013; Achim et al., 2011). The anxiety disorders can cause functional disability, being associated to an increased risk of suicide, poorer quality of life, poorer social functioning and lower self-esteem (Pallanti et al., 2013).
The successive exposure on the situations that induce stress or anxiety may trigger hypersensitivity for unpleasant stimuli and lead to the more accelerated and more intense activation of biological mechanisms that are responsible for maintaining homeostasis (McEwen, 1998). Over-activation of these mechanisms may cause over-tension of skeletal musculature that provokes dysregulation in various physiological systems, including central nervous, autonomic, neuroendocrine, cardiovascular and immune systems (McGuigan and Lehrer, 2007) developing a form of subclinical inflammatory state, enhanced oxidative stress level, decreased level of neurotrophins and/or impaired hypothalamic-pituitary-adrenal axis response, driving to significant impact on the health of schizophrenic patients (Misiak et al., 2014).
One of the methods used to reverse the process of prolonged and heightened skeletal muscle tension and to relieve the anxiety and stress is relaxation (McGuigan and Lehrer, 2007; Jacobson, 1976; Vickers and Zollman, 1999). Relaxation consists of complex responses at motor, visceral and behavioral levels. Motor and visceral responses involve tensing a group of muscles while breathing in, holding the contractions for a short period of time (for example, 15 seconds) and then releasing the muscles while breathing out (Vickers and Zollman, 1999). Behavioral responses involve observation, discrimination and verbalization of existing changes in the neuromuscular system and allow the development of skills of conscious releasing of tension and the generalization of this learning effect for the other groups of muscle (Jacobson, 1976; Vickers and Zollman, 1999; Payne, 2005).
The Progressive Muscle Relaxation of Jacobson (PMR) is one of the relaxation techniques widely used for the relief of stress and anxiety (Vickers and Zollman, 1999). The PMR is easily learned and its beneficial effects include, but are not limited to, reduction of anxiety and depression, enhancement of feelings of self-control and enhancement of coping abilities in the stressful situations (McGuigan and Lehrer, 2007; Chen et al., 2009). Studies including schizophrenic patients have also evidenced the beneficial impact of the PMR, with positive changes being observed through the alleviation of anxiety, reduction of psychological stress and increase in psychological well-being (Chen et al., 2009; Georgiev et al., 2012).
To date, one systematic review (SR) assessing the effectiveness of the PMR in schizophrenic patients was conducted (Vancampfort et al., 2013), based on the findings from three randomized controlled trials (RCTs) involving 146 schizophrenic patients, the SR authors concluded that the PMR is a promising intervention for the reduction of anxiety and psychological distress, and the improvement of subjective well-being, being potentially useful in acute and chronic impatient settings (Vancampfort et al., 2013). Nevertheless, the referred SR only searched for randomized controlled trials and focused on a very restricted set of outcomes. The effects of the PMR were not controlled for the confounding variables, such as age, severity of the disorder, and the presence/absence of the acute psychotic symptoms, and also didn't compare the effects of the PMR with the effects of other relaxation or stress-reducing techniques. Because of all these reasons and also updating of the existing evidence, there is a need for a new SR on the effectiveness of the PMR in patients with schizophrenia, in order to identify additional research aiming the effectiveness of progressive muscle relaxation on the anxiety in adults with schizophrenia.
Therefore, the objective of this review was to systematically search, appraise and synthesize the best available evidence on the effectiveness of Progressive Muscle Relaxation (PMR) in the adults with schizophrenia, in any setting, regarding anxiety, personal and social functioning, and well-being and other outcomes.
More specifically, the review focused on the following question: What is the effectiveness of PMR training on anxiety, social isolation, personal and social functioning, cognition, conversation, and well-being in adults with schizophrenia?
In this systematic review the set of objectives, inclusion criteria and methods of analysis for this review were specified in a priori published protocol (Melo-Dias et al., 2014).
2. Main text
2.1. Methods
This systematic review was guided by JBI methodology for Systematic reviews of effectiveness (Tufanaru et al., 2017).
2.1.1. Inclusion criteria
Population: adults (aged 18 and over), with current DSM-IV Schizophrenia diagnosis, in any setting.
Intervention: PMR (Jacobson's Model) regardless of the number and duration of sessions.
Comparator: No intervention (usual care) or another type of intervention referred to as relaxation intervention.
Outcomes: Primary outcomes – anxiety, social isolation, personal and social functioning, published protocol cognition, sadness, conversation, and well-being; Secondary outcomes – Physiological measurement/vital signs and others (respiratory rate, blood pressure, heart rate, skin temperature), and structured observation of tense/relaxed postures.
Study design: randomized controlled trials, quasi-experimental, before and after studies, prospective and retrospective cohort studies, case control studies, and analytical cross-sectional studies.
2.1.2. Search strategy
The search strategy aimed to find both published and unpublished studies. A three-step search strategy was used in this review. An initial limited search of MEDLINE and CINAHL was undertaken, followed by an analysis of the text words in the title and abstract and the index terms used to describe the article. A second search using all identified keywords and index terms was then undertaken in April 2017 across all included databases (see search strategies by databases in Table 1). Thirdly, the reference list of all identified reports and articles was searched for additional studies. Studies published in Portuguese, English, Spanish, Italian, French were considered for inclusion in this review.
Table 1.
Search strategies by databases, conducted on April, 2017.
| Database | Query | Items found |
|---|---|---|
| Medline (via PubMed) | Search ((((Schizophren*[Title/Abstract]) OR "dementia praecox"[Title/Abstract]) OR "Schizophrenia"[Mesh])) AND ((((Relax*[Title/Abstract]) OR "Relaxation"[Mesh]) OR "Relaxation Therapy"[Mesh]) OR "Muscle Relaxation"[Mesh]) Filters: English; French; Italian; Portuguese; Spanish | 416 |
| CINAHL (via EBSCO) | (TI schizophren* OR AB schizophren*) OR (TI "dementia praecox" OR AB "dementia praecox") OR (TI relax* OR AB relax*) OR (MH "Relaxation") OR (MH "Muscle Relaxation") OR (MH "Simple Relaxation Therapy (Iowa NIC)") OR (MH "Relaxation Techniques+") OR (MH "Progressive Muscle Relaxation (Iowa NIC)") OR (MH "Schizophrenia+") Limiters - Language: English, French, Italian, Portuguese, Spanish |
111 |
| Directory of Open Access Journals (DOAJ) | Article: Abstract (Schizophren* AND relax*) | 13 |
| ERIC | (TI schizophren* OR AB schizophren*) OR (TI "dementia praecox" OR AB "dementia praecox") OR (TI relax* OR AB relax*) | 3 |
| PsycNET - PsycARTICLES | ((Title:(Relax*)) OR (Abstract:(Relax*))) AND ((Title:(Schizophren*)) OR (Abstract:(Schizophren*)) OR (Title:("dementia praecox")) OR (Abstract:("dementia praecox"))) | 10 |
| Scielo Citation Index | (Title: (schizophren*) OR Topic: (schizophren*)) AND (Title: (relax*) OR Topic: (relax*)) | 3 |
| The Cochrane Library | ((Schizophren*:ti,ab,kw) OR ("dementia praecox":ti,ab,kw) OR (MeSH descriptor: [Schizophrenia])) AND ((Relax*:ti,ab,kw) OR (MeSH descriptor: [Relaxation]) OR (MeSH descriptor: [Relaxation Therapy]) OR (MeSH descriptor: [Muscle Relaxation]) | 48 |
| Embase | 'dementia praecox':ab,ti OR schizophren*:ab,ti OR 'schizophrenia'/exp AND (relax*:ab,ti OR 'relaxation training'/exp OR 'muscle relaxation'/exp) | 537 |
| PEDro | Abstract and Title (schizophren* AND relax*) | 16 |
| CAPES | Schizophren* AND Relax* | 4 |
| RCAAP – Scientific Open Access Repository of Portugal | Description (schizophren* AND relax*) | 11 |
| total | 1172 |
The search was conducted with no time limits to include in this review all existing studies about this topic. The searched databases include: CINAHL (via EBSCO), Directory of Open Access Journals (DOAJ), ERIC, Medline (via PubMed), PsycNET, Scielo Citation Index, The Cochrane Central Register of Controlled Trials, Embase, PEDro. Also, the search for unpublished studies was conducted in the following databases: CAPES (www.capes.gov.br) and RCAAP – Scientific Open Access Repository of Portugal (http://www.rcaap.pt).
2.1.3. Study screening and selection
Search results were included in an Endnote file and then the duplicates were removed. All identified studies were assessed by two independent reviewers based on title and abstract according the inclusion criteria. All full-text papers that did not present sufficiently data on title or abstract to make a decision, were assessed by two independent reviewers to check whether they met the inclusion criteria described above. Any disagreements that arose between the reviewers were solved through discussion.
2.1.4. Assessment of methodological quality
Quantitative papers selected for retrieval were assessed by two independent reviewers for methodological validity prior to inclusion in the review using JBI Critical Appraisal Checklist for Randomized Controlled Trials (Tufanaru et al., 2017). The disagreements that arose between the reviewers were resolved with a third reviewer. Authors of primary studies were contacted to clarify information.
Before the assessment of methodological quality, the reviewers decided to include all studies that meet the inclusion criteria and discussed the methodological fragilities of the studies.
2.1.5. Data extraction
The two reviewers extracted data from studies independently, using the standardized data extraction tool from JBI-SUMARI (JBI, 2014) which included participant characteristics, intervention characteristics and methods of the study, assessment characteristics and outcomes of significance to the review question.
2.1.6. Data synthesis
Significant differences were found between participants, interventions, outcome measures (clinical heterogeneity) and designs (methodological heterogeneity) (Tufanaru et al., 2015). For these reasons, we were unable to perform a meta-analysis. Thus, the synthesis is presented in narrative form according to the outcomes of interest (Tufanaru et al., 2017).
2.2. Results
2.2.1. Study selection and inclusion process
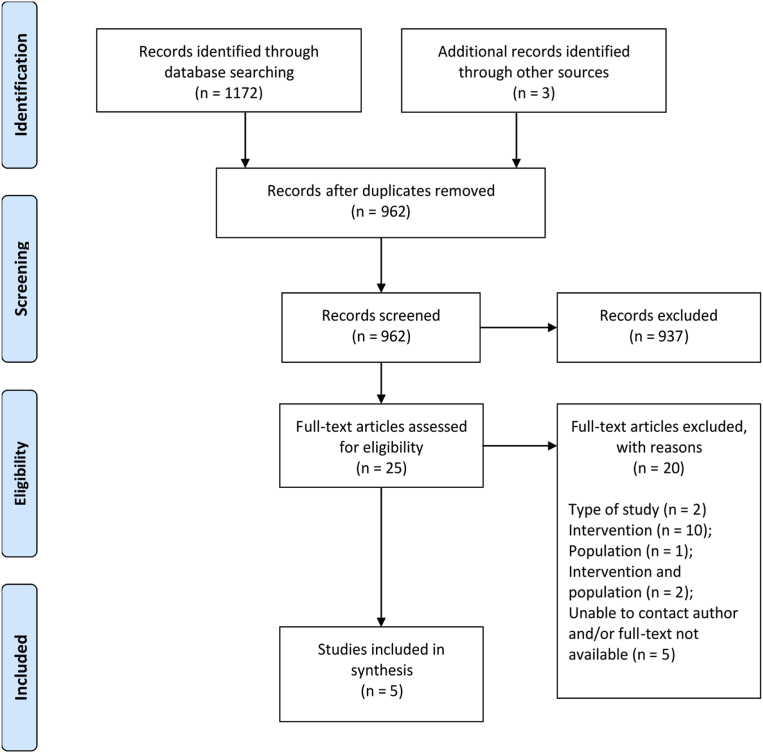
A total of 1172 potentially relevant studies were identified through database searching, and three additional studies found in other sources (reference list of articles). Of those, 213 were duplicates. Of the remaining 962 articles, 937 were excluded after screening by title and abstract. From the 25 remaining articles, 20 were excluded after the full-text analysis revealed that they did not meet the inclusion criteria. The methodological quality of the remaining five studies was assessed and all of them were included in the synthesis. The five studies included 216 adults with schizophrenia. Fig. 1 illustrates this process.
Fig. 1.
Flowchart of the search and study selection process.
2.2.2. Methodological quality of included studies
Two independent reviewers assessed the five studies (Table 2).
Table 2.
Assessment of the methodological quality of included studies (randomized controlled trial).
| Citation | Hassel et al., 1982 | Chen et al., 2009 | Vancampfort et al., 2011 | Georgiev et al., 2012 | Wang et al., 2015 | % |
|---|---|---|---|---|---|---|
| Q1. Was true randomization used for assignment of participants to treatment groups? | Y | U | Y | Y | U | 60.00 |
| Q2. Was allocation to treatment groups concealed? | Y | U | U | Y | U | 40.00 |
| Q3. Were treatment groups similar at the baseline? | Y | Y | Y | Y | Y | 100.00 |
| Q4. Were participants blind to treatment assignment? | Y | U | U | U | U | 20.00 |
| Q5. Were those delivering treatment blind to treatment assignment? | Y | U | U | U | U | 20.00 |
| Q6. Were outcomes assessors blind to treatment assignment? | N | U | U | Y | U | 20.00 |
| Q7. Were treatment groups treated identically other than the intervention of interest? | Y | Y | Y | Y | Y | 100.00 |
| Q8. Was follow up complete and if not, were differences between groups in terms of their follow up adequately described and analyzed? | U | N | Y | Y | Y | 60.00 |
| Q9. Were participants analyzed in the groups to which they were randomized? | U | N | N | N | N | 0.00 |
| Q10. Were outcomes measured in the same way for treatment groups? | Y | Y | Y | Y | Y | 100.00 |
| Q11. Were outcomes measured in a reliable way? | U | N | U | U | U | 0.00 |
| Q12. Was appropriate statistical analysis used? | Y | Y | Y | Y | Y | 100.00 |
| Q13. Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial? | Y | Y | Y | Y | Y | 100.00 |
Y = yes; N = no; U = nuclear.
In three studies, the authors were contacted to obtain more information, and all authors answered about assignment to treatment groups, methods used in randomization, blindness to treatment and to assessment strategies.
All five studies showed similarity at baseline between groups (experimental and control) concerning the demographic characteristics of the population and outcomes of interest, with the exception of Georgiev et al. (2012), where anxiety scores (assessed by SAI) were not similar at baseline between groups.
The information related to true randomization and participant blinding was always unclear. Due to the nature of the intervention, the practical difficulties of blinding participants to the interventions were recognized.
2.2.3. Findings of the review
We present a narrative synthesis of the five included studies (Hassel et al., 1982; Chen et al., 2009; Vancampfort et al., 2011; Georgiev et al., 2012; Wang et al., 2015). Full details of the included studies reported by the authors are presented in Table 3.
Table 3.
Characteristics of included studies.
| Study | Methods | Participants | Intervention A | Intervention B | Measured outcomes, Instruments, assessment periods, Limitations of the studies |
|---|---|---|---|---|---|
| Van Hassel J.H., Bloom L.J., Gonzalez A.M. (1982) USA |
RCT | 39 individuals (37 male, 2 female) served as Ss (Study Subjects). All Ss carried schizophrenic diagnoses in their outpatient records, with 62% classified as chronic undifferentiated subtype, 28% as paranoid subtype, and 10% as other forms of schizophrenia. Ages ranged from 23 to 70, with a mean age of 47.5. Most Ss (72%) were receiving antipsychotic or tranquilizing medication during the period of the study. Setting: Denver Veterans Administrations Hospital |
13 Ss in the Applied Relaxation (R) group Description: Initial training in deep muscle relaxation (Jacobson). Groups patients were required to practice relaxation exercises at home. The group continued to practice standard relaxation procedures throughout the 6-week period and engaged in discussions of how to apply the techniques to life stresses. No stressful imagery was used, nor were Ss encouraged to attend to anxiety cues. Emphasis was placed on using standard relaxation procedures in stressful situations encountered away from the hospital. Ss were seen in groups of 3–8, dependent upon scheduling constraints. Number of sessions: 6 total sessions Frequency: once per week Duration: 45 minutes |
14 Ss in the Anxiety Management Training (AMT) group Description: The training was conducted in three stages. In the first stage, patients were taught standard deep muscle relaxation (Jacobson). Groups patients were required to practice relaxation exercises at home. In the second stage, patients were stressed via stressful imagery and encouraged to pay attention to exactly where and how the tension was registered. The third stage, patients were stressed and then taught to reduce tension via cue-controlled relaxation. Groups completed post-training assessment scales. Ss were seen in groups of 3–8, dependent upon scheduling constraints. Number of sessions: 6 total sessions Frequency: once per week Duration: 45 minutes Intervention C 12 Ss in the Wait List (WL) group Description: The group met once to complete pre-training assessment scales and to have the goals and procedures of the training explained to them. They were informed that their group would not begin meeting for approximately 6 weeks. After the 6-week waiting period, the WL group met again. At that time the WL, AMT,and R groups completed post-training assessment scales. Post-training therapist rating scales also were completed at this time. Once the scales were complete, the WL group began the AMT training program. After 6 weeks of AMT training, the remaining 8 WL group Ss once again completed post-training questionnaires. |
The nature, purposes, and requirements of the study were explained fully to each S prior to inclusion in the program. Pretests were administered to the Ss (STAI) and their therapists (Therapist Rating Scale). Measured Outcomes:
Assessment periods: Pretests were administered to the Ss (STAI) and their therapists (Therapist Rating Scale). Therapists were instructed to consider only the preceding 30 days when they were rating their patients; After 6 weeks of training WL, AMT, and R groups completed post-training assessment scales. Post-training therapist rating scales also were completed. Limitations of the studies: Because of constraints imposed by the hospital administration, it was not possible to alter the patient's regular therapy program or medication regime for purposes of this study. |
|
Chen et al., 2009 Taiwan |
RCT | Eighteen patients were block randomised and then assigned to an experimental or control group. Only 14 Patients with DSM-IV diagnosis of schizophrenia. (4 male and 10 female) completed the study. Setting: Acute psychiatric ward of a medical center in Taiwan. |
Progressive muscle relaxation (n = 8; 1 male and 7 female) Progressive muscle relaxation training. One session of PMRT was applied to the experimental group per day at a set time each morning for 11 consecutive days, during 40 minutes each. Subjects were led into a sound-proof therapy room and asked to sit in a half recumbent position on a therapy chair with no distractions. Each person was covered with a comfortable sheet and the room lights were then dimmed. The air-conditioned temperature of the room was set at 23 °C. The volume of the instructions played to the experimental group was set between 40–50 decibels, which was an acceptable sound level. To ensure program standardization, the PMRT audiotape employing Jacobson's progressive muscle relaxation protocol included progressive relaxation of groups of muscles and deep breathing for 25 minutes. The PMRT tape contained instructions for systematic tensing and relaxation of specific muscle groups, starting with the groups of muscles in the upper body and progressing down to the lower part of the body. Number of sessions: 11 total sessions Frequency: once a day (11 consecutive days) Duration: 40 minutes |
Control group (n = 6; 3 male and 3 female) Control group patients received a placebo intervention (they were quietly led to a therapy chair in the same therapy room, at the same set time each morning, with no other interventions given). |
Measured outcomes: anxiety, positive symptoms, most frequently diagnosed psychiatric illness/disorder; patient's perceived overall disease status, finger temperature. Despite the positive findings, we must underline the potential biases related to the blindness, randomization methods, and therapist's factors. We must also underline the fact of this clinical evaluation was conducted from 11 consecutive sessions of during 40 minutes of progressive muscle relaxation intervention. Beck Anxiety Inventory (BAI). The BAI developed by Aaron Beck in 1988 includes 21 questions, each question having four possible scores between 0–3. When the scores are summed, 0–7 points are normal, 8–15 points indicate mild anxiety, 16–25 points indicate moderate anxiety and 26–63 points indicate severe anxiety (Julian, 2011). Scale for the assessment of positive symptoms (SAPS). The semi-structured questionnaire assesses characteristics of hallucinations, delusions, bizarre behaviours, aggressive and anxious behaviours and impaired active reasoning. Each question is evaluated at six levels, from ‘problem non-existent’ to ‘extremely severe’ (Chen et al. 2009). Mini-international neuropsychiatric interview is a structural interview scale that assesses for the most frequently diagnosed psychiatric illness/disorder. It is based upon the Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (DSM-IV) and the tenth edition of the International Classification of Diseases (ICD-10). Clinical global impression. Developed by Guy in 1976, this tool measures the patient's perceived overall disease status. Disease severity has seven levels, from ‘no disease’ to ‘extremely severe’. Changes in the progression of the disease are divided into seven levels, from ‘improved greatly’ to ‘very bad’. Treatment efficacy is divided into four levels, from ‘improved greatly’ to ‘no improvements’ (Chen et al. 2009). During the baseline procedure, finger temperature was continuously recorded for five minutes allowing the subjects to stabilize from previous activities and thus reducing arousal associated with the experimental setting. The first two minutes of baseline were discounted; the remaining three minutes were averaged and obtained as the baseline levels. Assessment periods: On the day prior to commencement of the intervention, the following instruments were administered the Mini-international neuropsychiatric interview (MINI); the scale for the assessment of positive symptoms (SAPS); clinical global impression (CGI) and the BAI. The BAI and the SAPS were again completed at the end of 11 days of PMRT or control intervention and one week after cessation of PMRT or control intervention. Finger temperature was measured prior to and three minutes after each PMRT session. |
|
Vancampfort et al., 2011 Belgium |
RCT | 64 out of 88 eligible patients with schizophrenia met the inclusion criteria. Only 52 Patients (31 male and 21 female) completed the study. Setting: Acute inpatient care unit University Psychiatric Centre of the Catholic University of Leuven, Belgium. |
Progressive muscle relaxation (n = 27; 18 male and 9 female) Progressive muscle relaxation was offered one time in a week and lasted approximately 25 minutes. Training consisted of successive tensing and relaxing at least five major muscle groups, beginning with the upper body and proceeding to the lower parts. Tensing for about 8 seconds and relaxing for about 30 seconds of each muscle group was practiced twice prior to proceeding to a subsequent muscle group. Number of sessions: 1 session Frequency: once a week Duration: 25 minutes |
Resting control condition (n = 25; 13 male and 12 female) Resting control condition sat quietly in a room for 25 minutes and was told that they could read. Reading material was provided for participants who did not bring their own material. The same physiotherapist was also here present in the room and only left during completion of the questionnaires |
Measured outcomes: State anxiety; Stress and subjective well-being; schizophrenia symptoms. Despite the positive findings, we must underline the potential biases related to the blindness, randomization methods, and therapist's factors. We highlight also that the Cutoff point for inclusion of the study's in the review were established by reviewers in five mandatory "yes" answers to questions in the standardized critical appraisal instrument from JBI-MAStARI. We must also underline the fact of this clinical evaluation was conducted from one only 25 minutes session of progressive muscle relaxation intervention. Progressive muscle relaxation is part of a larger clinical physiotherapy program consisting of aquatic sessions (once a week), walking (twice a week), yoga training (once a week), fitness training (twice a week), psycho-education about an active lifestyle (once every two weeks) and group-related movement sessions with psychosocial and cognitive objectives (twice a week). Progressive muscle relaxation was offered once a week and lasted approximately 25 minutes. Instruments: State Anxiety Inventory. State anxiety was assessed by the State Anxiety Inventory of Spielberger. The range of possible total scores is 20–80. Higher scores indicate higher levels of anxiety. Subjective Exercise Experiences Scale. Stress, subjective well-being and fatigue were measured using the Subjective Exercise Experiences Scale. Each subscale contains four items, which are scored on a scale from 0 (not at all) to 7 (entirely). Higher scores on a subscale indicate a higher perception for this factor. The psychosis evaluation tool for common use by caregivers. The psychosis evaluation tool for common use by caregivers was used by an independent and well-trained nurse to evaluate schizophrenia symptoms. It evaluates 20 symptom items on a 7-point scale, resulting in an overall score ranging from 20 to 140. Symptoms are grouped in five factors: positive (hallucinations, delusions, unusual thought content, grandiosity), negative (poor rapport, passive/apathetic withdrawal, blunted affect, motor retardation), depressive (anxiety, depression, feelings of guilt, somatic concerns), cognitive (poor attention, disorientation, difficulties with abstract thinking, conceptual disorganization) and excitatory (poor impulse control, lack of cooperation, hostility, excitement) symptoms. The scores for each factor range from 4 to 28. Assessment periods: Before and after the single interventions the State anxiety inventory and the subjective exercise experiences scale were completed. Effect sizes were calculated. |
|
Georgiev et al., 2012 Bulgaria |
RCT | Out of 78 patients with schizophrenia, 64 met the inclusion criteria. Only 59 Patients (28 male and 21 female) completed the study. Setting: Chronic department of the State Psychiatric Hospital in Tzerova Koria, Bulgaria. |
Progressive muscle relaxation (n = 31; 15 male and 16 female) Progressive muscle relaxation was offered one time in a week and lasted approximately 25 minutes. Training consisted of successive tensing and relaxing at least five major muscle groups, beginning with the upper body and proceeding to the lower parts. Tensing for about 8 seconds and relaxing for about 30 seconds of each muscle group was practiced twice prior to proceeding to a subsequent muscle group. Number of sessions: 1 session Frequency: once a week Duration: 25 minutes |
Resting control condition (n = 28; 13 male and 15 female) Resting control condition sat quietly in a room for 25 minutes and was told that they could read. Reading material was provided for participants who did not bring their own material. |
Measured outcomes: State anxiety; Stress and subjective well-being Despite the positive findings, we must underline the potential biases related to the blindness, randomization methods, and therapist's factors. We must also underline the fact of this clinical evaluation was conducted from one only 25 minute of progressive muscle relaxation intervention. During two weeks participants undertook one weekly habituation session in order to get used to the environment and the protocol. The PMR is part of a larger clinical physiotherapy program consisting of aquatic sessions (once a week), walking (twice a week), yoga training (once a week), fitness training (twice a week), psychoeducation about an active lifestyle (once every two weeks) and group related movement sessions with psychosocial and cognitive objectives (twice a week). Scales: State anxiety was assessed by the State anxiety inventory (SAI) of Spielberger. The range of possible total scores is 20–80. Higher scores indicate higher levels of anxiety. Subjective Exercise Experiences Scale. Stress, subjective well-being and fatigue were measured using the Subjective Exercise Experiences Scale. Each subscale contains four items, which are scored on a scale from 0 (not at all) to 7 (entirely). Higher scores on a subscale indicate a higher perception for this factor. Assessment periods: During the week of the test condition also psychiatric symptoms were administered. |
|
Wang et al., 2015 China |
RCT | Sixty-four patients with acute schizophrenia were randomly assigned to four groups. Only 52 Patients (29 male and 23 female) completed the study. Setting: Acute psychiatric ward of Changsha Psychiatric Hospital, Changsha, China. |
Progressive muscle relaxation (n = 12; 7 male and 5 female) Progressive muscle relaxation (PMR) group. This technique involved systematically relaxing major muscle groups of the body with the goal of physical and mental relaxation. The PMR group received ten 30-minute group PMR practice sessions, in two sessions per week, during 5 weeks of PMR training. Each session preceded by a 15-minute group discussion of PMR experiences. Self-practice of PMR at least once per day and recording of relaxation experiences on a specific form. Brochure describing the mechanisms and benefits of relaxation. Relaxation audio CD providing a guide for self-practice of PMR. Dedicated e-mail address where patients could communicate with the intervention staff about PMR experiences. Number of sessions: 10 total sessions Frequency: twice per week Duration: 30minutes + 15 minutes = 45 minutes Intervention C Education plus progressive muscle relaxation (n = 13; 7 male and 6 female) Combination of intervention activities and materials in education and PMR groups. Group PMR practice and group education provided on separate days each week. Group PMR practice Number of sessions: 5 total sessions Frequency: one per week Duration: 30minutes + 15 minutes = 45 minutes Group education Number of sessions: 5 total sessions Frequency: one per week Duration: 30minutes + 15 minutes = 45 minutes |
Education (n = 14; 7 male and 7 female) Five 30-minute group education sessions respectively covering five topics: illness, treatment, well-being, support, and patients' rights; one session per week; each session followed by a 15-minute group discussion of the contents taught. Brochure summarizing topics in the group education sessions. Video CD containing a 30-minute video showing typical stories told by other patients with acute schizophrenia. Dedicated e-mail address where patients could send e-mails to the intervention staff for counseling. Number of sessions: 5 total sessions Frequency: one per week Duration: 30minutes + 15 minutes = 45 minutes Intervention D Control (n = 13; 8 male and 5 female) Patient education according to usual ward procedures Ten 30-minute group exercise sessions; two sessions per week; Each session preceded by 15-minute free group chat. Number of sessions: 10 total sessions Frequency: twice per week Duration: 30minutes + 15 minutes = 45 minutes |
Measured outcomes: Quality of Life; Functional disability; Severity of positive schizophrenia symptoms Despite the positive findings, we must underline the potential biases related to the blindness, randomization methods, and therapist's factors. We must also underline the fact of this clinical evaluation was conducted from ten 30 minute sessions of progressive muscle relaxation. Quality of Life Enjoyment and Satisfaction Questionnaire Short Form (Q-LES-Q-SF), a self-report instrument developed to assess the degree of enjoyment and satisfaction experienced by respondents.13 The Q-LES-Q-SF, with 16 items, is identical to the General Activities subscale of the larger QLES- Q instrument. Each question is scored on a 5-point scale (1 = very poor degree of enjoyment or satisfaction, 5 = very good degree of enjoyment or satisfaction). The first 14 items are summed to produce a global QoL index with a maximum of 70 points. The last two questions concern medication and overall life satisfaction. Functional disability was assessed with the Sheehan Disability Scale (SDS), which was developed to measure impairment in functioning of psychiatric patients in treatment outcome studies. The SDS is a self-report instrument assessing patient functioning using three items (work/study, social life, family life/home responsibilities). Each item is rated on a 10- point visual analogue scale (0 = no disability, 1–3 = mild, 4–6 = moderate, 7–9 = marked, and 10 = extreme disability). SDS has been used previously in studies of patients with schizophrenia. Scale for the Assessment of Positive Symptoms (SAPS). This semi-structured questionnaire assesses characteristics of hallucinations, delusions, bizarre behaviors, aggressive and anxious behaviors, and impaired active reasoning. Each question is evaluated at six levels, from ‘‘problem nonexistent’’ to ‘‘extremely severe.’’ Assessment periods: All patients were evaluated at baseline (within 72 hours before the interventions) and at the end of weeks 5 (when the interventions ended) and week 15 (a 10-week follow-up after the interventions). |
2.2.4. Outcomes
2.2.4.1. Primary outcome: state anxiety
Four of the five studies included in this systematic review assessed the state anxiety but using different methods/instruments. In the studies of Vancampfort et al. (2011) and Georgiev et al. (2012) anxiety was assessed with the State anxiety inventory (SAI) [The range of possible total scores is 20–80. Higher scores indicate higher levels of anxiety]. Chen et al. (2009), used the Beck Anxiety Inventory (BAI), and in turn Hassel et al. (1982) used the Spielberger Trait Anxiety Inventory (STAI).
Georgiev et al. (2012) and also Vancampfort et al. (2011) reported a significant decreased state anxiety within the PMR group, respectively 51.77 ± 6.0 SD to 47.74 ± 4.71 SD and 45.22 ± 10.31 SD to 33.44 ± 8.64 SD, and also mentioning that there were no significant pre-post changes within the Control Group (CG) (Table 4). This decrease was emphasized by effect sizes for PMR that in Georgiev et al. (2012) were -0.22 (95%CI = -0.73 to 0.19) and in Vancampfort et al. (2011) were -1.25 (95% CI = -1.83 to -0.63) both for state anxiety (Table 4).
Table 4.
Anxiety scores at baseline and post-intervention after PMR versus control condition.
| Study | Outcome | PMR group (Assessment Moments) |
CG (Assessment Moments) |
||
|---|---|---|---|---|---|
| Baseline | Post-intervention | Baseline | Post-intervention | ||
| Georgiev et al., 2012 | State Anxiety [assessed with SAI] | n = 31 51.77 ± 6.0 |
n = 31 47.74 ± 4.71 |
n = 28 47.92 ± 7.36 |
n = 28 49.17 ± 7.84 |
| Vancampfort et al., 2011 | State Anxiety [assessed with SAI] | n = 27 45.22 ± 10.31 |
n = 27 33.44 ± 8.64 |
n = 25 45.24 ± 11.80 |
n = 25 45.68 ± 10.97 |
| Chen et al., 2009 | State Anxiety [assessed with BAI] | n = 8 16.4 ± 4.4 |
n = 8 5.8 |
n = 6 15.0 ± 3.9 |
n = 6 13 |
| Hassel et al. (1982) | State Anxiety [assessed with STAI] | [group AMT] n = 14 49.70 |
[group AMT] n = 14 ? |
n = 12 58.5 |
n = 12 ? |
| [group R] n = 13 51.57 |
[group R] n = 13 ? |
||||
Note: Values presented as mean ± SD.
Chen et al. (2009), described similar tendency of decreased state anxiety, namely in the experimental group (EG), the Beck Anxiety Inventory (BAI) range prior to intervention 9–21 points and the mean was 16,4 ± 4.4 SD. In the control group (CG), the BAI range 11–20 points and the mean were 15 (Table 4).
Each question of BAI scale scores from zero to three, with totals be considered normal from 0 to 7, mild anxiety from 8 to 15, and moderate anxiety from 16 to 25, and severe anxiety from 26 to 63.
Anxiety baseline on Beck score was moderate (16 points) in EG patients and mild (15 points) in CG patients, anxiety at one-week post-intervention was normal (7 points) in EG and mild (13 points) in CG.
The difference in the severity of anxiety between both groups was significant after 11 days of PMR intervention (Z = -4.1, p < 0.0001). Follow up after the 11 days of intervention, mean anxiety severity was still lower in the experimental group than in the control group (Z = -2.0, p = 0.0446).
The degree of anxiety improvement was significantly higher in the progressive muscle relaxation training group than in the control group after progressive muscle relaxation training intervention (p < 0.0001) and at follow-up (p = 0.0446); the mean BAI score fell from 16.4 pretest to 5.8 post-test.
Clarification for the post-intervention means and SD of the experimental group was requested by email to the author Kueiru Chou (Chen et al., 2009), but he did not answer.
Another study also assess anxiety, was Hassel et al. (1982) using the Spielberger Trait Anxiety Inventory (STAI).
The STAI is a commonly used measure of trait and state anxiety, has 40 items, 20 items allocated to each of the S-Anxiety and T-Anxiety subscales. Range of scores for each subtest is 20–80, the higher score indicating greater anxiety. A cut point of 39–40 has been suggested to detect clinically significant symptoms for the S-Anxiety scale; however, other studies have suggested a higher cut score of 54–55 for older adults (Julian, 2011; American Psychological Association, 2018).
Covariance and post-hoc Newman-Keuls analysis was carry out on STAI scores reporting the following adjusted means, group AMT (Anxiety Management Training) = 49.70; group R (Applied Relaxation) = 51.57, and group WL (Wait List) = 58.50 (Table 4).
This analysis point out that the group WL mean (p < .05) was greater than the group AMT and group R, and within these means was similar to each other.
Consequently, the mean of the WL group (non-treated) contrasting with the group AMT and group R means significant decrement in STAI scores, show effects of treatments in reduction of generalized anxiety (Hassel et al., 1982).
Correspondingly expressive decrement in STAI scores on the group AMT and group R contrasting with the group WL show effects of treatments in reduction of generalized anxiety.
Clarification for the data of post-intervention means of all groups involved in investigation was requested by email to the author Larry J. Bloom, that respond to all questions about quality assessment of the study except the data and values requested about of post-intervention assessment.
2.2.4.2. Primary outcome: personal and social functioning
Two of the five studies included in this systematic review assessed personal and social functioning.
Specifically, Hassel et al. (1982) assessed with the Therapist Rating Scale, both abilities to achieve personal goals and social ability.
The Therapist Rating Scale contained eight items, namely, reported anxiety, observed anxiety, ability to work effectively in therapy, social ability, ability to manage anger, ability to manage emotions, ability to achieve personal goals, and psychiatric status (Hassel et al., 1982, p.281) and all three groups means were subject to Newman-Keuls multiple comparison analysis for significance. Therefore, main effects of treatment were important to abilities to achieve personal goals (item 7), F (3, 35) = 6.02, p < .01, and without significance on social ability (item 4) F (2, 35) = .29, p < .05.
AMT, R, and WL groups show 2.70, 3.07, and 4.44, respectively for the adjusted means, and post-hoc analysis point out that AMT group and R group don't differ from each other, and consequently (because of treatment) significantly less that the WL group mean, p < .05.
In turn Wang et al. (2015) assessed Functional disability with a self-report instrument, the Sheehan Disability Scale (SDS) that assess work or study, social life, family life or home responsibilities with a 10-point visual analogue scale, from extreme disability (10) to no disability (0).
In this study treatment major effect was on all SDS scores and also in other outcomes, namely schizophrenia positive symptoms and also Quality of Life (Table 5).
Table 5.
SDS scores at baseline (within 72 hours before the interventions), the end of weeks 5 (when the interventions ended) and week 15 (a 10-week follow-up after the interventions).
| Wang et al., 2015 | SDS: work/study |
SDS: social life |
SDS: family life/home responsibilities |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PMR | Control | Education + PMR | Education | PMR | Control | Education + PMR | Education | PMR | Control | Education + PMR | Education | |
| Baseline | n = 12 6.3 ± 2.9 |
n = 13 6.2 ± 2.9 |
n = 13 6.2 ± 3.0 |
n = 14 6.0 ± 3.2 |
n = 12 6.3 ± 2.8 |
n = 13 6.2 ± 2.6 |
n = 13 6.3 ± 2.7 |
n = 14 6.0 ± 2.4 |
n = 12 6.0 ± 2.7 |
n = 13 5.9 ± 2.5 |
n = 13 6.0 ± 2.5 |
n = 14 5.8 ± 2.3 |
| Post-intervention | n = 12 5.2 ± 2.7 |
n = 13 6.2 ± 3.0 |
n = 13 3.6 ± 2.6 |
n = 14 5.2 ± 2.8 |
n = 12 5.3 ± 2.6 |
n = 13 6.1 ± 2.7 |
n = 13 3.9 ± 2.8 |
n = 14 5.0 ± 2.6 |
n = 12 5.0 ± 2.6 |
n = 13 5.9 ± 2.7 |
n = 13 3.7 ± 2.7 |
n = 14 5.0 ± 2.4 |
| Follow-up 15 weeks | n = 12 5.4 ± 2.8 |
n = 13 6.2 ± 2.8 |
n = 13 4.6 ± 2.7 |
n = 14 5.0 ± 2.9 |
n = 12 5.3 ± 2.9 |
n = 13 6.2 ± 2.5 |
n = 13 4.9 ± 2.9 |
n = 14 5.0 ± 2.8 |
n = 12 5.1 ± 2.9 |
n = 13 5.8 ± 2.6 |
n = 13 4.1 ± 2.9 |
n = 14 4.8 ± 2.6 |
Therefore, differences were found between treatments on functional disability, Quality of Life and schizophrenia positive symptoms, with the major effect on Quality of Life, proceed from functional disability, and at last schizophrenia positive symptoms.
Comparing the different treatments, Wang et al. (2015) demonstrated in Table 5 no significant effects form education and PMR alone, but the combined intervention of education with PMR had statistically significantly better effects on SDS score at the end of experimental group then the control group.
2.2.4.3. Primary outcome: well-being
Two of the five studies included in this systematic review assessed Well-being.
In the studies of Vancampfort et al. (2011) and Georgiev et al. (2012) well-being (and also stress and fatigue) was assessed with the Subjective Exercise Experiences Scale (SEES). The SEES represent one of the most reliable and valid instruments for assessing subjective well-being in exercise settings and subdivides in two subscales, psychological stress and positive well-being. Each subscale contains four items, which are scored on a scale from 0 (not at all) to 7 (entirely). Higher scores on a subscale indicate a higher perception for this factor.
Vancampfort et al. (2011) reports that Scheffé post-hoc analysis revealed that within the progressive muscle relaxation group significantly increased subjective well-being could be observed, and effect sizes for progressive muscle relaxation were +1.26 (95% CI = 0.65 to 1.84) for subjective well-being. Table 6 presents the well-being scores before and after progressive muscle relation and control condition where can see the clear tendency of increased well-being responses.
Table 6.
SEES scores at baseline and post-intervention after PMR versus resting control condition.
| Study | Outcome | PMR group (Assessment Moments) |
CG (Assessment Moments) |
||
|---|---|---|---|---|---|
| Baseline | Post-intervention | Baseline | Post-intervention | ||
| Georgiev et al., 2012 | Well-being | n = 31 14.26 ± 4.80 |
n = 31 19.90 ± 5.19 |
n = 28 14.71 ± 4.13 |
n = 28 15.21 ± 3.98 |
| Vancampfort et al., 2011 | Well-being | n = 27 16.70 ± 5.30 |
n = 27 21.52 ± 4.12 |
n = 25 15.68 ± 5.94 |
n = 25 15.36 ± 5.57 |
Note: Values presented as mean ± SD.
In turn in Georgiev et al. (2012) study we can acknowledge as well that increase on well-being (Table 6) and reported effect sizes for PMR as +1.01 (95%CI = 0.45 to 1.54) for subjective well-being.
With regard to all remaining primary outcomes: Social Isolation, Cognition, Sadness and Conversation, although originally outlined in the review protocol, none included study reported results related to this outcome.
2.2.4.4. Secondary outcome: skin temperature
Only one of the five studies included in this systematic review assessed skin temperature. Chen et al. (2009) report that the Mann-Whitney U-test showed after 11 days of PMR, the mean increase in finger temperature was significantly greater in the experimental group than in the control group, 0.4 and 0.2 °C respectively (U = 29.5, p < 0.05). The authors presented the physiological explanation for an increase in finger temperature: “when a subject is anxious, subcutaneous arteriole vasoconstriction reduces the amount of heat lost in the periphery which results in a decreased skin temperature and cold extremities” (p. 2189).
With regard to all remaining secondary outcomes: physiological measurement/vital signs (respiratory rate, blood pressure, heart rate) and structured observation of tense/relaxed postures, although originally outlined in the review protocol, none included study reported results related to these outcomes.
2.3. Discussion
This review set out examine the effectiveness of progressive muscle relaxation training for adults diagnosed with schizophrenia additionally aiming to determine if there is enough information to provide answers to questions of the impact the effectiveness of PMR in levels the anxiety, personal and social functioning, and well-being in adults with schizophrenia.
As primary findings from the five selected randomized controlled trials studies with 216 adults with schizophrenia it is evident from this review the increased well-being in participants as well as the significantly decreased state of anxiety. Among these, the studies revealed some of the diverse outcomes of interest, namely state of anxiety (assessed by SAI (Vancampfort et al., 2011; Georgiev et al., 2012) and BAI (Chen et al., 2009)), personal and social functioning (assessed by SDS (Wang et al., 2015) and Therapist Rating Scale (Hassel et al., 1982), well-being (assessed by SEES (Vancampfort et al., 2011; Georgiev et al., 2012)), and finally skin temperature (measured with equipment) (Chen et al., 2009).
Four studies assessed anxiety (Hassel et al., 1982; Chen et al., 2009; Vancampfort et al., 2011; and Georgiev et al., 2012). As stated before, symptoms of anxiety were shown to have an impact on subjective quality of life, with higher ratings of anxiety being associated with lower satisfaction with daily activities, family, health and social relationship. Within anxiety disorders comorbidity can cause functional disability, poorer quality of life, poorer social functioning and lower self-esteem (American Psychiatric Association, 2013; Pallanti et al., 2013), and for that one of the methods used to reverse the process of prolonged muscle tension and to relieve the anxiety and stress is relaxation, as we acknowledge with this review that in all studies, anxiety decreased significantly.
Chen et al. (2009) report that the Mann-Whitney U-test showed after 11 days of PMR, the mean increase in finger temperature was significantly greater in the experimental group than in the control group, 0.4 and 0.2 °C respectively (U = 29.5, p < 0.05).
As presented, schizophrenia affect various domains of individual functioning with social withdrawal and impaired role functioning (American Psychiatric Association, 2013; NICE, 2010; Tandon et al., 2009; Meijel, 2003; Melo-Dias and Silva, 2015), therefore this inability is leading to poor quality of life and to the experience of anxiety (Narvaez et al., 2008; Karow et al., 2014; Castle and Bosanac, 2012; Lysaker and Salyers, 2007), the needed clarification of outcomes related with psychosocial functioning is also important to the treatment of patients with schizophrenia.
Two studies Wang et al. (2015) and Hassel et al. (1982) presented data for this outcome. The first study assessed psychosocial functioning with SDS, referring that PMR (stand-alone intervention) showed no significant effects on the scores of functional disability over time compared with baseline scores. The second study assess with Therapist Rating Scale and, from several items of personal functioning, only reports benefits on ability to achieve personal goals.
Schizophrenic patients are often associated negatively with depressive and anxiety symptoms having impact on subjective quality of life with lower satisfaction with daily activities, family, health and social relationship (Strauss et al., 2012; Huppert et al., 2001), two studies (Vancampfort et al., 2011; Georgiev et al., 2012) stated that PMR improved and increased subjective well-being in participants.
We must also underline the fact that the different studies have different clinical intervention designs of PMR. Two studies (Vancampfort et al., 2011; Georgiev et al., 2012) analyzed the effects of a single-session of PMR; another study (Chen et al., 2009) verified the effects of 11 sessions in consecutive days; and the other study (Wang et al., 2015) used 10 sessions but delivered them twice a week during five weeks, and finally another Hassel et al. (1982) used 6 sessions delivered once per week.
Vickers and Zollman (1999) indicated that “most relaxation techniques need to be practiced daily, and typically, patients learn a relaxation technique over the course of eight weekly classes, so it can be problematized whether the design of the programs of PMR have their effects on effectiveness of the intervention.
It can also be argued the fact that the studies not cover all outcomes considered classical in assessing results of this type of relaxation interventions, particularly including vital signs (respiratory rate, blood pressure, heart rate), self-rating of relaxation, and self-rating/self-report from participants using preset descriptive phrases about relaxation/anxiety, structured observation of tense/relaxed postures, as mentioned in the review protocol (Melo-Dias et al., 2014), in order to increase the possibility to provide more meaningful results of the PMR intervention.
Prospective randomized controlled trials in this area need to be more robust in order to guarantee clear evidence of benefits within specific PMR intervention granted by physiological, psychological, affective and behavioral outcomes.
2.3.1. Limitations of the included studies
The sample sizes of the included studies ranged from ranged from 8 to 31 participants in experimental groups (PMR) and from 6 to 28 participants in control groups. This range of sample size, the lack of sample size calculation as to the lack of statistical power and effect size in the included studies was also a limitation.
According to the CONSORT statement, sample size calculation should be reported and justified in all published RCTs. Ideally, a study should be large enough to have a high probability (power) of detecting as statistically significant a clinically important difference of a given size if such a difference exists.27
Nevertheless, two studies (Chen et al., 2009; Vancampfort et al., 2013) reported the small sample size as problematic and potentially affecting the generalizability of the findings. The other two studies (Georgiev et al., 2012; Wang et al., 2015) considered an adequate sample size for this type of studies and intervention. Despite these considerations, the majority of the studies reported that further studies with larger samples should be conducted.
2.3.2. Limitations of the review
The methodological quality of all included studies was a major limitation. The studies were unclear about the methods of true random assignment; allocation concealment; and blindness related to treatment allocation of participants and the researchers who assessed the outcomes. Additionally, no study described and included the outcomes of people who withdrew in the analysis.
Although it was exactly the same core intervention – PMR – the studies presented different outcomes to assess effectiveness, and sometimes used different measurement scales to assess the same or similar constructs, and also report different number of sessions and duration of the intervention.
In conclusion, schizophrenia and its course show prodromal deterioration in affective domain that may be reflected through anxiety and depression. The inability to fully recover a daily and social functioning may lead to the feeling of poor quality of life, and to the experience of anxiety and depression, that, in turn, can cause psychological distress and burden of the illness. Specifically, regarding symptoms of anxiety, they were shown to have an impact on subjective quality of life, with lower satisfaction with daily activities, family, health and social relationship, and therefore considered as relevant risk factors for the exacerbation of remitted psychotic symptoms and of the new acute episode.
Is well know that PMR is one of the relaxation techniques widely used for the relief of stress and anxiety, with beneficial effects on reduction of anxiety and depression, enhancement of feelings of self-control and enhancement of coping abilities in the stressful situations.
The studies included in the systematic review provide results on the effectiveness of PMR training on the human responses of adults diagnosed with schizophrenia. Evidence is positive in all five studies, although can be fragile due the diversity of clinical intervention designs of PMR (different number and length of sessions) and the diversity of outcome assessment scales.
Nevertheless, the few results specifically about decreasing state anxiety and improving well-being are optimistic about the effectiveness of PMR in adults diagnosed with schizophrenia.
Based on this synthesis and in the in-depth analysis of the selected studies for this review, we highlight four core clinical practice implications/recommendations:
First, clarity should be ensured and a description of PMR program routine of systematic tensing and relaxing specific muscle groups; Second, PMR sessions should be standardized as much as possible, avoiding excess of variations on audio, voice and a specific therapy script; Third, the design of this PMR clinical intervention, namely the frequency and number of sessions, should be in tune with the daily or weekly routines of social, professional and personal behaviors; Fourth, as a health professional, Nurses may and should deliver PMR as an autonomous nursing intervention to adults diagnosed with schizophrenia, as this variables are sensitive to nursing interventions.
About the Implications for research, additional high quality RCTs (using CONSORT guidelines) are required to strengthen the current evidence of PMR training for adults diagnosed with schizophrenia.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
About Schizophrenia and Progressive Muscle Relaxation – a systematic review of effectiveness.
On behalf of our team work and resilience I'd like to thank to each of you co-authors, Professor Rosa Cristina Lopes, Nurse researcher Daniela Filipa Batista Cardoso, Psychologist researcher Elzbieta Bobrowicz-Campos, and Professor João Luís Alves Apóstolo, for the hours of hard work and sympathy of spending some time of your life's to develop and finalize this systematic review “Schizophrenia and Progressive Muscle Relaxation – a systematic review of effectiveness”, thank you all!
References
- Achim A.M., Maziade M., Raymond E., Olivier D., Mérette C., Roy M.-A. How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophr. Bull. 2011;37(4):811–821. doi: 10.1093/schbul/sbp148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . fifth ed. American Psychiatric Association; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- American Psychological Association . 2018. The State-Trait Anxiety Inventory (STAI)http://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/trait-state.aspx Retrieved from. [Google Scholar]
- Castle D., Bosanac P. Depression and schizophrenia. Adv. Psychiatr. Treat. 2012;18(4):280–288. [Google Scholar]
- Chen W.C., Chu H., Lu R.B., Chou Y.H., Chen C.H., Chang Y.C. Efficacy of progressive muscle relaxation training in reducing anxiety in patients with acute schizophrenia. J. Clin. Nurs. 2009;18(15):2187–2196. doi: 10.1111/j.1365-2702.2008.02773.x. [DOI] [PubMed] [Google Scholar]
- Georgiev A., Probst M., De Hert M., Genova V., Tonkova A., Vancampfort D. Acute effects of progressive muscle relaxation on state anxiety and subjective well-being in chronic Bulgarian patients with schizophrenia. Psychiatr. Danub. 2012;24(4):367–372. PubMed PMID: 23132187. [PubMed] [Google Scholar]
- Hassel J.H.V., Bloom L.J., Gonzalez A.M. Anxiety management with schizophrenic outpatients. J. Clin. Psychol. 1982;38(2):280–285. doi: 10.1002/1097-4679(198204)38:2<280::aid-jclp2270380208>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Huppert J.D., Weiss K.A., Lim R., Pratt S., Smith T.E. Quality of life in schizophrenia: contributions of anxiety and depression. Schizophr. Res. 2001;51:171–180. doi: 10.1016/s0920-9964(99)00151-6. [DOI] [PubMed] [Google Scholar]
- Jacobson E. fifth ed. Mcgraw-Hill; London: 1976. You Must Relax. [Google Scholar]
- JBI – Joanna Briggs Institute . The University of Adelaide; South Australia (Australia): 2014. Joanna Briggs Institute Reviewers’ Manual: 2014 Edition. [Google Scholar]
- Julian L.J. Measures of anxiety: state-trait anxiety inventory (STAI), Beck anxiety inventory (Bai), and hospital anxiety and depression scale-anxiety (HADS-A) Arthritis Care Res (Hoboken). Nov; 2011;63(Suppl 11):S467–S472. doi: 10.1002/acr.20561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karow A., Wittmann L., Schöttle D., Schäfer I., Lambert M. The assessment of quality of life in clinical practice in patients with schizophrenia. Dialogues Clin. Neurosci. 2014;16(2):185–195. doi: 10.31887/DCNS.2014.16.2/akarow. PMID: 25152657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lysaker P.H., Salyers M.P. Anxiety symptoms in schizophrenia spectrum disorders: associations with social function, positive and negative symptoms, hope and trauma history. Acta Psychiatr. Scand. 2007;116:290–298. doi: 10.1111/j.1600-0447.2007.01067.x. [DOI] [PubMed] [Google Scholar]
- McEwen B.S. Stress, adaptation, and disease. Allostasis and allostatic load. Ann. N. Y. Acad. Sci. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McGuigan F.J., Lehrer P.M. Progressive relaxation. Origins, principles, and clinical applications. In: Lehrer P.M., Woolfolk R.L., Sime W.E., editors. Principles and Practice of Stress Management. third ed. Guilford Press; New York: 2007. pp. 59–86. [Google Scholar]
- Meijel B. Thesis University Utrecht; Utrecht: 2003. Relapse Prevention in Patients with Schizophrenia: A Nursing Intervention Study. Labor Grafimedia BV, Utrecht. [Google Scholar]
- Melo-Dias C., Silva C.F. Esquizofrenia. Revista Investigação em Enfermagem. 2015;10(2):69–76. ISSN: 2182-9764. [Google Scholar]
- Melo-Dias C., Apóstolo J., Cardoso D. Effectiveness of progressive muscle relaxation training for adults diagnosed with schizophrenia: a systematic review protocol. JBI Database Syst. Rev Implement Rep. 2014;12(10):85–97. [Google Scholar]
- Misiak B., Frydecka D., Zawadzki M., Krefft M., Kiejna A. Review. Refining and integrating schizophrenia pathophysiology – relevance of the allostatic load concept. Neurosci. Biobehav. Rev. 2014;45:183–201. doi: 10.1016/j.neubiorev.2014.06.004. [DOI] [PubMed] [Google Scholar]
- Narvaez J.M., Twamley E.W., McKibbin C.H.L., Heaton R.K., Patterson T.L. Subjective and objective quality of life in schizophrenia. Schizophr. Res. 2008;98:201–208. doi: 10.1016/j.schres.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NICE – National Institute for Clinical Excellence . Update edition. RCPsych Publications; London: 2010. Schizophrenia: the NICE Guideline on Core Interventions in the Treatment and Management of Schizophrenia in Adults in Primary and Secondary Care. PMID: 20704054. [Google Scholar]
- Pallanti S., Cantisani A., Grassi G. Anxiety as a core aspect of schizophrenia. Curr. Psychiatr. Rep. 2013;15:354. doi: 10.1007/s11920-013-0354-7. [DOI] [PubMed] [Google Scholar]
- Payne R.A. third ed. Churchill Livingstone: Elsevier Limited; 2005. Relaxation Techniques: A Practical Handbook for the Health Care Professional. [Google Scholar]
- Strauss G.P., Sandt A.R., Catalano L.T., Allen D.N. Negative symptoms and depression predict lower psychological well-being in individuals with schizophrenia. Compr Psychiatry. 2012;53(8):1137–1144. doi: 10.1016/j.comppsych.2012.05.009. [DOI] [PubMed] [Google Scholar]
- Tandon R., Nasrallah H.A., Keshavan M.S. Schizophrenia, "just the facts" 4. Clinical features and conceptualization. Schizophr. Res. 2009;110(1):1–23. doi: 10.1016/j.schres.2009.03.005. [DOI] [PubMed] [Google Scholar]
- Tufanaru C., Munn Z., Stephenson M., Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int. J. Evid. Based Healthc. 2015;13(3):196–207. doi: 10.1097/XEB.0000000000000065. [DOI] [PubMed] [Google Scholar]
- Tufanaru C., Munn Z., Aromataris E., Campbell J., Hopp L. Chapter 3: systematic reviews of effectiveness. In: Aromataris E., Munn Z., editors. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute; 2017. https://reviewersmanual.joannabriggs.org/ Available from. [Google Scholar]
- Vancampfort D., De Hert M., Knapen J., Maurissen K., Raepsaet J., Deckx S. Effects of progressive muscle relaxation on state anxiety and subjective well-being in people with schizophrenia: a randomized controlled trial. Clin. Rehabil. 2011;25(6):567–575. doi: 10.1177/0269215510395633. [DOI] [PubMed] [Google Scholar]
- Vancampfort D., Correll C.U., Scheewe T.W., Probst M., De Herdt A., Knapen J. Progressive muscle relaxation in persons with schizophrenia: a systematic review of randomized controlled trials. Clin. Rehabil. 2013;27(4):291–298. doi: 10.1177/0269215512455531. [DOI] [PubMed] [Google Scholar]
- Vickers A., Zollman C. ABC of complementary medicine: hypnosis and relaxation therapies. BMJ. 1999;319(7221):1346–1349. doi: 10.1136/bmj.319.7221.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F.-Z., Luo D., Kan W., Wang Y. Combined intervention with education and progressive muscle relaxation on quality of life, functional disability, and positive symptoms in patients with acute schizophrenia. J. Altern. Complement. Med. 2015;21(3):159–165. doi: 10.1089/acm.2014.0128. [DOI] [PubMed] [Google Scholar]