Abstract
Accurate diagnosis of traumatic brain injury (TBI) is critical to ensure that patients receive appropriate follow-up care, avoid risk of subsequent injury, and are aware of possible long-term consequences. However, diagnosis of TBI, particularly in the emergency department (ED), can be difficult because the symptoms of TBI are vague and nonspecific, and patients with suspected TBI may present with additional injuries that require immediate medical attention. We performed a retrospective chart review to evaluate accuracy of TBI diagnosis in the ED. Records of 1641 patients presenting to the ED with suspected TBI and a head computed tomography (CT) were reviewed. We found only 47% of patients meeting the American Congress of Rehabilitation Medicine criteria for TBI received a documented ED diagnosis of TBI in medical records. After controlling for demographic and clinical factors, patients presenting at a level I trauma center, with cause of injury other than fall, without CT findings of TBI, and without loss of consciousness were more likely to lack documented diagnosis despite meeting diagnostic criteria for TBI. A greater proportion of patients without documented ED diagnosis of TBI were discharged home compared to those with a documented diagnosis of TBI (58% vs. 40%; p < 0.001). Together, these data suggest that many patients who have sustained a TBI are discharged home from the ED without a documented diagnosis of TBI, and that improved awareness and implementation of diagnostic criteria for TBI is important in the ED and for in- and outpatient providers.
Keywords: diagnosis, emergency department, traumatic brain injury
Introduction
National attention has focused upon traumatic brain injury (TBI) in recent years, in part because of increased awareness of the potential for long-term consequences from relatively minor TBI. In 2013, there were approximately 2.5 million TBI-related emergency department (ED) visits in the United States, contributing a significant burden to the healthcare system.1 Approximately 15% of people diagnosed with a mild TBI experience long-term effects that may include anxiety, depression, sleep disruption, headaches, cognitive impairment, or memory deficits.2–4 Patients who experience these long-term symptoms may not be able to return to work or function at their previous capacity, significantly diminishing the quality of life of these individuals.3,4 The long-term effects also impose a significant societal and economic burden given that individuals of all ages are at risk for TBI.
The diagnosis of TBI is a first step in improving awareness, care, and outcome; however, there is recognition in the field that the accurate diagnosis of TBI after TBI is problematic, particularly on the milder end of the spectrum. A 2008 study found the accuracy of TBI diagnosis in the ED to be poor; 56% of patients with clinically defined mild TBI determined by patient interview did not have a documented TBI diagnosis from the ED.5 These data suggest that many patients with TBI are being discharged without a diagnosis.5,6 Documented diagnosis of TBI is critical to ensure that patients recognize the injury they have incurred, are aware of the potential for long-lasting effects, and receive appropriate follow-up care to minimize the impact on their lives.
In the ED, diagnosis and evaluation of suspected TBI currently relies on subjective clinical assessment often augmented by a computed tomography (CT) of the head to rule out hemorrhage.7 Absent findings on the CT consistent with TBI or persistent neurological deficits, patients may be discharged home. In response to criticism that this approach may not be sensitive for patients with mild TBI,5,8–10 the 2010 American Congress of Rehabilitation Medicine (ACRM) proposed new diagnostic criteria, defining TBI as “alteration in brain function” after a TBI with at least one clinical sign: loss of consciousness (LOC), post-traumatic amnesia (PTA), an alteration in mental status (AMS) at the time of injury, neurological deficits, or evidence of brain injury using radiologic studies.11 It is unclear, however, whether ED physicians are currently using these more-objective criteria to assign a formal diagnosis to patients. When TBI does not occur in isolation, trauma to other parts of the body may confound the diagnosis of TBI, particularly when urgent intervention for higher priority injuries is required.
In the course of screening patients with acute TBI for a prospective observational study on TBI (NCT01132937), it was noted that some patients meeting ACRM criteria for TBI were found to 1) lack documentation of TBI in the medical records and 2) be unaware that they may have TBI. Furthermore, despite having documented intracranial injury observed on CT, some patients failed to attribute residual symptoms months later to the acute traumatic event.
To better understand the scope of the problem, and the potential factors contributing to documentation of TBI in the medical records, we conducted a retrospective chart review and analysis.
Methods
We performed a retrospective medical record review of patients with acute TBI presenting to a level I trauma center in Washington, DC (MedStar Health Washington Hospital Center) and a level II trauma center in Bethesda, Maryland (Johns Hopkins Suburban Hospital). The National Institutes of Health Office of Human Subjects Research Protection approved this study as an exempt medical record review, and the privacy board of Johns Hopkins Suburban Hospital and the Institutional Review Board for MedStar Health Washington Hospital Center approved this study as an expedited protocol for de-identified medical record review.
Patient population
De-identified data were collected from paper-based and electronic medical records of patients presenting to the ED at each hospital on two randomly selected days of each month between 2009 and 2013 (120 days total per site). A patient's record was reviewed and included if 1) the documented chief complaint or cause of injury was consistent with TBI (assault, falls, road traffic accidents, pedestrian struck, sports injury, and any other type of trauma such as hit/struck with object) and 2) a CT scan of the head was performed before discharge. Patients <18 years of age were excluded from the analysis.
Data collection and classification
Information was extracted from ED medical records and/or trauma intake records. For patients who were admitted to the hospital, additional information was collected from hospital inpatient admission intake records. Abstracted data included: time, day of the week, month, and year of ED admission; age; sex; race; ethnicity; cause of injury; presentation of ACRM TBI criteria; interval of injury to admission, discharge, hospitalization; drug and alcohol screening results; CT imaging results; and documented diagnoses (Supplementary Fig. 1) (see online supplementary material at http://www.liebertpub.com). The majority of data (95%) were collected and coded by two investigators (M.R.C. and A.D.M.), who were also available for questions from the investigators who collected the remaining 5%. Unclear data were resolved through consensus of the two initiating investigators.
After data collection, each patient was categorized as TBI positive (TBI+) or TBI negative (TBI−) using the ACRM diagnostic criteria. To be categorized as TBI+ according to the ACRM criteria, the patient record must indicate evidence of brain injury using radiological studies or one of the following clinical signs: 1) period of LOC or decreased LOC; 2) loss of memory for events immediately before or after the injury (PTA); or 3) any AMS at the time of injury.11 For this retrospective chart review, a patient was coded as positive for AMS if there was any documentation in the chart indicating that the patient was dazed, confused, had AMS, or had a post-injury Glasgow Coma Scale (GCS) <15 that was different from the patient's pre-injury baseline. Presence of neurological deficits (weakness, balance, vision changes, sensory loss, etc.) is an additional component of the ACRM criteria; however, these data were not well documented in patient ED medical records and were therefore not used in this study. Absent definitive evidence of meeting ACRM criteria in the medical records, a patient was classified as TBI−. At the time of the data collection, International Classification of Diseases, Ninth Revision (ICD-9) coding data were not available to the study team and were therefore not included in the analysis.
Patients were classified as having a documented ED diagnosis of TBI if the patient's medical record stated “concussion,” “post-concussive symptoms” or “PCS,” “closed head injury,” “traumatic brain injury” or “TBI,” or a reported finding on imaging consistent with TBI, such as subdural hemorrhage. All other nonspecific descriptors, such as “road traffic accident,” were classified as having no documented ED diagnosis of TBI.
For describing discord, ACRM criteria were considered the “true” condition and ED TBI diagnosis was considered the “predicted” condition. Using this convention, a patient meeting ACRM criteria for TBI (TBI+), but absent a diagnosis of TBI in the medical records (no documented ED diagnosis of TBI), was considered a false-negative documented diagnosis.
Variables examined
Variables examined for these groups included age (18–40, 41–65, and >65 years), sex, race, cause of injury, and lowest documented GCS. Dementia was noted if documented. Variables for the ACRM criteria were individually examined: LOC, AMS, PTA, and CT findings. CT results were classified as CT TBI positive when clinical radiology reports indicated presence of TBI or findings suggestive of TBI, including the presence of intracranial hemorrhage, contusion, or diffuse axonal injury. Time of injury and ED discharge location (home, intensive care unit [ICU], against medical advice [AMA], operating room [OR], floor, and transferred) were examined. Clinical diagnoses of injuries other than TBI were documented and were classified as being TBI and other, or other (e.g., trauma to an extremity, a medical diagnosis).
Statistical analysis
Descriptive statistics were used to summarize the demographics and clinical characteristics of the study population. Chi-square analyses were performed to evaluate statistical differences between the TBI+ and TBI− populations and the patients with and without a documented ED diagnosis of TBI. To determine the characteristics associated with a patient's receiving a documented ED diagnosis of TBI or no documented ED diagnosis of TBI, a binary logistic regression multi-predictor model was performed, adjusting for age, race, sex, trauma level, trauma team involvement, LOC, PTA, AMS, CT results, GCS, and cause of injury. Data are presented as number (n; %) or median (interquartile range; IQR). A two-tailed p value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS software (Version 22; SPSS, INc., Chicago, IL).
Results
Demographics of total population of charts reviewed
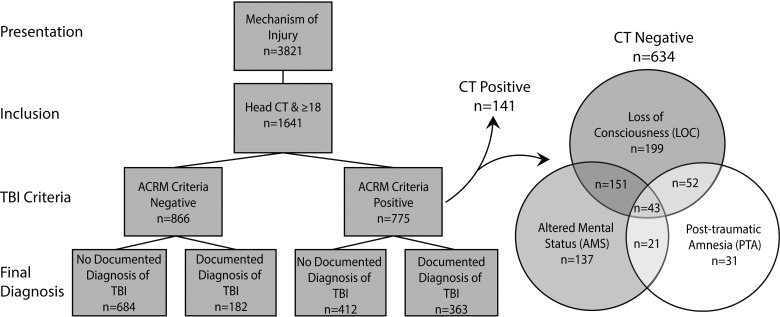
Medical records from a total of 3821 patients with a complaint or cause of injury consistent with suspected TBI were reviewed. Of these, 1641 met the inclusion criteria, were reviewed, and data were abstracted (Fig. 1). Those patients with positive head CT findings met TBI+ criteria. The diagram shows additional details of symptoms and signs in the TBI+ population with negative head CT. Table 1 describes the demographics for the total population; 53% were male with a median age of 53 (32–77), and a plurality were Caucasian (49%). The most common cause of injury was fall (49%) followed by road traffic accident (RTA; 35%).
FIG. 1.
Progression of retrospective medical record review. Left: Patients presenting to the ED with a cause of injury were screened and patients 18 or older with a head CT were included in the study. Right: clinical characteristics of patients with a negative head CT who had American Congress of Rehabilitation Medicine (ACRM) clinical criteria for traumatic brain injury (TBI). ED, emergency department; CT, computed tomography; TBI, traumatic brain injury.
Table 1.
Patient Clinical and Demographic Characteristics
| Characteristic | Total | TBI+ | TBI− | p value |
|---|---|---|---|---|
| (n = 1641) | (n = 775) | (n = 866) | ||
| Female | 769 (47%) | 285 (37%) | 484 (56%) | <0.001 |
| Age (years) (median, IQR) | 53 (32–77) | 47 (28–65) | 60 (39–81) | <0.001 |
| 18–40 | 555 (34%) | 328 (41%) | 237 (27%) | |
| 41–65 | 515 (31%) | 270 (35%) | 245 (28%) | |
| >65 | 571 (35%) | 187 (24%) | 384 (44%) | |
| Race and ethnicity | 0.004 | |||
| Caucasian | 797 (49%) | 343 (44%) | 454 (52%) | |
| African American | 502 (31%) | 256 (33%) | 246 (28%) | |
| Hispanic/Latino | 198 (12%) | 109 (14%) | 89 (10%) | |
| Other/unknown | 144 (9%) | 67 (9%) | 77 (9%) | |
| Cause of injury | <0.001 | |||
| Incidental fall | 809 (49%) | 326 (42%) | 483 (56%) | |
| Road traffic accident | 568 (35%) | 292 (38%) | 276 (32%) | |
| Violence/assault | 165 (10%) | 108 (14%) | 57 (7%) | |
| Other | 99 (6%) | 49 (6%) | 50 (6%) | |
| ED trauma level | <0.001 | |||
| Level I | 606 (37%) | 327 (42%) | 279 (32%) | |
| Level II | 1035 (63%) | 448 (58%) | 587 (68%) | |
| Trauma team involved | 704 (43%) | 477 (62%) | 227 (26%) | <0.001 |
| Blood alcohol | <0.001 | |||
| No | 436 (27%) | 270 (35%) | 166 (19%) | |
| Yes | 241 (15%) | 180 (23%) | 61 (7%) | |
| Not done | 964 (59%) | 325 (42%) | 639 (74%) | |
| Dementia | 66 (4%) | 21 (3%) | 45 (5%) | 0.01 |
| Documented diagnosis | <0.001 | |||
| TBI | 413 (25%) | 290 (37%) | 123 (14%) | |
| Other | 1096 (67%) | 412 (53%) | 684 (79%) | |
| TBI and other | 132 (8%) | 73 (9%) | 59 (7%) | |
| CT TBI positive | 141 (9%) | 141 (100%) | 0 (0%) | <0.001 |
TBI, traumatic brain injury; IQR, interquartile range; ED, emergency department; CT, computed tomography.
Demographics and clinical presentation of population determined positive for traumatic brain injury
Of patients with suspected TBI, 47% (n = 775) were classified as TBI+ (Table 1). Age, race, cause of injury, blood alcohol status, and presence of dementia were significantly associated with classification as TBI+ in univariate analysis. Notably, the proportion of men (490 of 872; 56%) meeting criteria was significantly higher than women (285 of 769; 37%; p < 0.001).
Slightly greater than 1 in 2 of the TBI+ patients (412 of 775; 53%) had no documented ED diagnosis of TBI (false negative; Fig. 1). Conversely, approximately 1 in 5 TBI− patients (182 of 866; 21%) received a documented ED diagnosis of TBI despite a lack of evidence in the medical record of meeting ACRM diagnostic criteria. The positive predictive value of a documented ED diagnosis of TBI was 0.67, and the negative predictive value was 0.62.
Table 2 shows demographic and clinical characteristics of the TBI+ population, stratified by documented ED diagnosis of TBI. Hospital trauma level, race, age, cause of injury, GCS, documented diagnoses, a clinical head CT positive for TBI, and discharge location were all significantly associated with a documented ED diagnosis of TBI. Factors such as presence of alcohol, presence of dementia, symptoms of TBI (LOC, AMS, or PTA), trauma team involvement, or sex did not differ between those with and without a documented diagnosis. The proportion of TBI+ patients discharged home was significantly higher for patients with no documented ED diagnosis of TBI (58% vs. 40%; p < 0.001; Fig. 2). Rates of documented ED diagnosis of TBI in TBI+ patients did not differ based on the day of week or time of day, and were consistent across the 5 years under study (data not shown).
Table 2.
Clinical and Demographic Characteristics of TBI+ Patients
| Characteristic | Documented ED TBI diagnosis | No documented ED TBI diagnosis | p value |
|---|---|---|---|
| (n = 363) | (n = 412) | ||
| Female | 133 (37%) | 152 (37%) | 0.942 |
| Age (years) | 0.005 | ||
| 18–40 | 133 (37%) | 185 (45%) | |
| 41–65 | 124 (34%) | 146 (35%) | |
| >65 | 106 (29%) | 81 (20%) | |
| Race and ethnicity | <0.002 | ||
| Caucasian | 180 (50%) | 163 (40%) | |
| African-American | 96 (26%) | 160 (39%) | |
| Hispanic/Latino | 50 (14%) | 59 (14%) | |
| Other/unknown | 37 (10%) | 30 (7%) | |
| ED trauma level | <0.001 | ||
| Level I | 130 (36%) | 197 (48%) | |
| Level II | 233 (64%) | 215 (52%) | |
| Trauma team involved | 222 (61%) | 255 (62%) | 0.833 |
| Cause of injury | <0.001 | ||
| Incidental fall | 180 (50%) | 146 (35%) | |
| Road traffic accident | 110 (30%) | 182 (44%) | |
| Violence/assault | 39 (11%) | 69 (17%) | |
| Other | 34 (9%) | 15 (4%) | |
| GCS | 0.034 | ||
| 13–15 | 245 (67%) | 306 (74%) | |
| 9–12 | 22 (6%) | 31 (8%) | |
| 3–8 | 40 (11%) | 26 (6%) | |
| Undetermined | 56 (15%) | 49 (12%) | |
| Loss of consciousness | 0.622 | ||
| No | 74 (20%) | 92 (22%) | |
| Yes | 217 (60%) | 229 (56%) | |
| Undocumented | 29 (8%) | 41 (10%) | |
| Suspected | 43 (12%) | 50 (12%) | |
| Post-traumatic amnesia | 0.539 | ||
| No | 35 (10%) | 32 (8%) | |
| Yes | 86 (24%) | 92 (22%) | |
| Undocumented | 242 (67%) | 288 (70%) | |
| Positive altered mental status | 212 (58%) | 227 (55%) | 0.345 |
| CT TBI positive | 126 (35%) | 15 (4%) | <0.001 |
TBI, traumatic brain injury; ED, emergency department; GCS, Glasgow Coma Scale; CT, computed tomography.
FIG. 2.
Discharge location and cause of injury for American Congress of Rehabilitation Medicine (ACRM) traumatic brain injury–positive (TBI+) patients. Number of TBI+ patients with (white) or without (gray) a documented ED TBI diagnosis by cause of injury, p < 0.001 (A) or by discharge location, p < 0.001 (B). ED, emergency department; ICU, intensive care unit; RTA, road traffic accident; TBI, traumatic brain injury.
Statistical analysis of diagnosis in traumatic brain injury–positive patients
To evaluate factors that predict whether TBI+ patients received a documented ED diagnosis of TBI, we performed a logistic regression analysis adjusting for demographic and clinical factors (Supplementary Table 1) (see online supplementary material at http://www.liebertpub.com). ED trauma level, cause of injury, CT findings, and LOC were significant predictors of a documented ED diagnosis of TBI (Supplementary Table 1) (see online supplementary material at http://www.liebertpub.com). Patients at the level I trauma center were more likely to have no documented ED diagnosis of TBI compared to patients at the level II trauma center (odds ratio, 1.88; 95% confidence interval [CI], 1.26–2.82). Compared to patients who fell, patients who were in RTAs or were assaulted were more likely to lack a documented ED diagnosis of TBI, and patients who had other causes of injury were less likely to lack a documented ED diagnosis (RTAs odds ratio, 1.95; 95% CI, 1.3–2.9; assault/violence odds ratio, 1.9; 95% CI, 1.1–3.4; Other odds ratio, 0.48; 95% CI, 0.24–0.99; p < 0.001).
Statistical analysis of computed tomography findings and discharge location
Patients with a head CT negative for TBI findings were more likely to lack a documented ED diagnosis (odds ratio, 17; 95% CI, 9–30; p < 0.001) in our logistic regression analysis. Table 3 shows the univariate analysis of all CT+ and CT− patients, demonstrating a significant correlation between CT findings consistent with TBI and discharge location (Pearson χ2(3) = 627; p < 0.0001). Within the total population, patients with CT findings consistent with TBI, 85% (120 of 141) were admitted either to the ICU or a hospital floor, in comparison to only 27% (411 of 1500) of all patients with CT findings negative for TBI. This association between head CT findings and discharge location persisted in a univariate analysis focused only on the subset of patients who met TBI+ criteria (Table 3; n = 775; Pearson χ2(3) = 314; p = 0.000). For the TBI+ patient population with CT findings negative for TBI, 62% (238 of 384) were discharged home without documented ED diagnosis of TBI (Fig. 2).
Table 3.
Discharge Locations
| Discharge location | Total population (n = 1641) | TBI+ Only (n = 775) | |
|---|---|---|---|
| CT+ (n = 141)a | CT− (n = 1500) | CT− (n = 634) | |
| Home | 10 (7%) | 1052 (70%) | 374 (59%) |
| ICU | 102 (72%) | 78 (5%) | 54 (9%) |
| Floor | 18 (13%) | 333 (22%) | 185 (29%) |
| Other | 11 (8%) | 37 (2%) | 21 (3%) |
CT+ = head CT findings consistent with TBI; ICU = intensive care unit; Other = transfer or left against medical advice; TBI+ = patients with either CT findings and/or symptoms consistent with TBI.
Analysis of traumatic brain injury population by hospital trauma level
The patient populations and care pathways differed between the two hospitals surveyed, which is reflected in the data. A higher number of patients met both screening and inclusion criteria at the level II trauma center, but a lower proportion of patients were TBI+ in comparison to the level I trauma center (448 of 1035 [43%] vs. 327 of 606 [54%]; p < 0.001). However, of patients that were TBI+, a documented ED diagnosis of TBI was recorded in 52% of patients for level 2 versus 40% for level I (p < 0.001). Age, race, sex, cause of injury, GCS, and clinical presentation (LOC, AMS, or PTA) were different between the two trauma centers (Supplementary Table 2) (see online supplementary material at http://www.liebertpub.com). Univariate analysis of each site revealed that cause of injury and CT findings consistent with TBI were significantly associated with documented ED diagnosis of TBI at both EDs (Supplementary Table 3A,B). Regression analysis performed separately for each ED found that patients without CT findings consistent with TBI, RTAs, and assaults were more likely to lack a documented diagnosis of TBI compared to those with positive CT TBI findings and fall, respectively (negative CT level I, odds ratio, 19.4; 95% CI, 8.3–45.5; p < 0.001; level II, odds ratio, 15.9; 95% CI, 6.5–38.9; p < 0.001; see Supplementary Table 3A,B) (see online supplementary material at http://www.liebertpub.com). LOC was a predictive factor for documented ED diagnosis of TBI in the regression model only at the level I trauma center (Supplementary Table 3B) (see online supplementary material at http://www.liebertpub.com).
Demographics of traumatic brain injury negative population
Characteristics of the TBI− patients stratified by documented ED diagnosis of TBI are shown in Table 4. Cause of injury, trauma team involvement, blood alcohol, and discharge location were all significantly associated with ED TBI diagnosis status. Patients with a documented ED TBI diagnosis without documented evidence of TBI in the medical record were more often discharged home, had fallen, and did not see the trauma team. The majority (73%) of TBI− patients with a documented ED TBI diagnosis had an ED diagnosis of “closed head injury” (Table 5). Conversely, a minority (27%) of the true positive diagnosis (TBI+ patients with a documented ED diagnosis of TBI) received a diagnosis of closed head injury; most of these patients were documented as “concussion” or “TBI” in medical records.
Table 4.
Clinical and Demographic Characteristics of TBI− Patients
| Characteristic | Documented ED TBI diagnosis | No documented ED TBI diagnosis | p value |
|---|---|---|---|
| (n = 182) | (n = 684) | ||
| Female | 109 (60%) | 375 (55%) | 0.221 |
| Age (years) | 0.275 | ||
| 18–40 | 45 (25%) | 192 (28%) | |
| 41–65 | 60 (33%) | 185 (27%) | |
| 65< | 77 (42%) | 307 (45%) | |
| Race and ethnicity | 0.149 | ||
| Caucasian | 108 (59%) | 346 (51%) | |
| African American | 45 (25%) | 201 (29%) | |
| Hispanic/Latino | 18 (10%) | 71 (10%) | |
| Other/Unknown | 11 (6%) | 66 (10%) | |
| Trauma center | 0.236 | ||
| Level I | 52 (29%) | 227 (33%) | |
| Level II | 130 (71%) | 457 (67%) | |
| Trauma team involved | 26 (14%) | 201 (29%) | <0.001 |
| Cause of injury | <0.001 | ||
| Incidental fall | 116 (64%) | 367 (54%) | |
| Road traffic accident | 38 (21%) | 238 (35%) | |
| Violence/assault | 9 (5%) | 48 (7%) | |
| Other | 19 (10%) | 31 (5%) | |
| GCS | 0.182 | ||
| 13–15 | 115 (63%) | 473 (69%) | |
| 9–12 | 0 (0%) | 5 (1%) | |
| 3–8 | 0 (0%) | 2 (<1%) | |
| Undetermined | 67 (37%) | 204 (30%) | |
| Blood alcohol | 0.027 | ||
| No | 23 (13%) | 143 (21%) | |
| Yes | 11 (6%) | 50 (7%) | |
| Not done | 148 (81%) | 491 (72%) | |
| Dementia | 6 (3%) | 39 (6%) | 0.194 |
TBI, traumatic brain injury; ED, emergency department; GCS, Glasgow Coma Scale.
Table 5.
Documented ED TBI Diagnoses in TBI+ and TBI− Patients
| Documented ED TBI diagnosis | TBI+ (n = 363) | TBI− (n = 182) |
|---|---|---|
| Concussion | 139 (38%) | 44 (24%) |
| TBI | 8 (2%) | 1 (1%) |
| Closed TBI | 101 (28%) | 133 (73%) |
| Imaging findings (i.e., SDH, SAH) | 115 (32%) | 4 (2%) |
TBI, traumatic brain injury; ED, emergency department; SDH, subdural hemorrhage, SAH, subarachnoid hemorrhage.
Discussion
More than half of the patients who met clinical criteria for TBI were discharged from the EDs without a documented ED diagnosis of TBI in medical records. Patients without a documented diagnosis of TBI were more often discharged home compared to patients with a documented ED diagnosis of TBI. After controlling for demographic and clinical factors, patients without CT findings consistent with TBI, RTAs, assaults, and admission to the trauma level I center were more likely to lack documented diagnosis in the ED. Although it is unclear from this retrospective review whether patients understood that they suffered a TBI, this raises concern that patients lacking documentation of their TBI may not be aware of their injury or the utility of receiving follow-up care.
The rate of false-negative documented diagnosis reported is similar to the rate in a study by Powell and colleagues in 2008 that found that 56% of ED patients who met CDC criteria for mild TBI were not diagnosed in the ED, suggesting that the rate of false-negative documented diagnosis in the ED remains steady.5 Consistent with this, we also found no change in the rate of TBI diagnosis in the 5-year span over which data were abstracted for this study.
Here, we found LOC and CT findings consistent with TBI to be predictive factors for documented ED diagnosis of TBI, consistent with the results of the 2008 study.5 The researchers suggested that these findings reflect the priorities of ED physicians to prioritize care for those patients with the most immediately life-threatening conditions. Consistent with this hypothesis, we found that the majority of TBI+ patients with no documented ED diagnosis of TBI were discharged home whereas the majority of the TBI+ patients discharged to the ICU were accurately diagnosed with TBI. Although polytrauma and other comorbidities are likely more prevalent in the population admitted to the ICU, these data also suggest that the lack of documented diagnosis of TBI in the ED may skew toward the population that presents with milder symptoms and/or comorbidities.
In contrast to the previous study, we did not find a significant correlation between ED TBI diagnosis and findings of PTA or AMS. However, these findings were often undocumented in the ED medical record and in hospital inpatient admission history and physical records, which may have affected our ability to determine a significant correlation. Our study also did not find a correlation of sex and TBI diagnosis, as was described previously.5 Differences in sex distributions between our study and the previous study may have contributed to this; our study's total population was 53% male and in the previous study was 70%. The two studies had different study designs; we performed a retrospective medical record review to identify whether patients were true positive or true negative for TBI, whereas the previous study used a prospective design and patient interviews to determine true positives and negatives. The percent of women in our study is consistent with other studies that have analyzed ED admissions using large databases, and found that men accounted for 55–60% of persons admitted to the ED for suspected TBI.8,12–14 The difference in sex ratios in the two studies may also be attributed to differences in age; the average age in the previous study was 32 and our median age was 53. The incidence of TBI in women compared to men is known to increase with age.15–17
Patient medical and billing records commonly use terms that are not specific to TBI, such as closed head injury or head injury, unspecified. Use of these terms to identify patients with a TBI diagnosis may result in the identification of patients lacking documented evidence of clinical symptoms and signs of TBI. Consistent with this, when we examined the frequency of the closed head injury diagnosis, we found that this accounted for more than 70% of TBI− patients with a documented ED diagnosis of TBI and only 27% of TBI+ patients with a documented ED diagnosis of TBI, suggesting that this descriptor may include patients without true TBI or may include patients with incomplete documentation of clinical symptoms and signs consistent with TBI.
The sensitivity of ED TBI diagnosis determined in our study was similar to the sensitivity determined using ICD-9 codes (0.47 vs. 0.46).9 Clinical documentation of ED diagnosis of TBI had a better positive predictive value (0.67 vs. 0.27) compared to ICD-9 determined TBI, whereas the negative predictive value was worse (0.62 vs. 0.99). We did not have access to ICD-9 codes at the time of the study and cannot directly compare these results. However, despite differences, both studies suggest that determining incidence of TBI using ICD-9 codes or documented ED diagnosis of TBI alone would result in an underestimate of true incidence.
The rates of undocumented diagnoses in the ED found here and reported previously5 suggest that a fraction of patients may be going home without recognizing that they sustained a TBI. Our study was a retrospective medical record review, which limited our ability to assess the patients' knowledge about their condition. It is possible that despite not having a documented ED diagnosis of TBI, patients were told that they sustained a head injury and were informed about the possible symptoms. Results from a recent prospective cohort study suggest that over half of patients with mild TBI seen in the ED with head trauma and a head CT within 24 h of injury did not receive TBI educational materials at discharge or have follow-up care within 3 months of injury.18
This underscores the importance for all care providers to be aware of the diagnostic criteria and symptoms of TBI. Whereas our study focused only upon patients ages ≥18 years, a study of pediatric TBI focused on concussion (mild TBI) found that the majority of children were diagnosed in the primary care setting.19 Moderate evidence suggests that simple early educational strategies, such as providing patients with informational booklets about post-concussive symptoms may be effective in improving outcomes.3,20,21 These educational strategies, if utilized, are unlikely to be effective in real-world experience if patients are not being accurately diagnosed.
Limitations
Our retrospective chart review used only the ACRM criteria for TBI diagnosis. The reliance on ACRM diagnostic standards may have led to an underestimation of documented ED diagnosis of TBI if ED physicians followed different guidelines for TBI. We found no difference in the rate of false-negative documented diagnosis before or after the introduction of the ACRM criteria, suggesting that this did not significantly affect ED physician diagnosis patterns. We do not think, however, that using a different criteria would have significantly affected our results, given that they correspond with another study that used a different study design and the Centers for Disease Control and Prevention criteria for TBI.5
Inclusion of only two hospitals limits the generalizability of some of the findings. For instance, the incidence of TBI causes of injury may be specific to patients admitted to the two hospitals. Consistent with this, we found differences in the demographic and clinical characteristics of patients at each ED. TBI+ patients at the ED with a trauma level I were significantly more likely to lack a documented diagnosis, suggesting differences in the rate of documenting diagnosis of TBI between hospitals. However, the factors that significantly contribute to false-negative documented diagnoses were very similar between the two hospitals. We speculate that the inaccuracy of the documented ED diagnosis of TBI with a trauma level I facility may reflect the priorities of the ED and trauma physicians who see the most critically ill patients. The role of these providers is to identify, triage, and treat those patients most in need of immediate care, and out of necessity they need to rely on inpatient teams and outpatient providers to oversee care for less-urgent and milder conditions.
The inclusion criteria for this study required the patient to have presented with a trauma-related head injury and a record of a head CT during their ED visit. This retrospective chart review focused upon the population with documented head CT for two reasons: 1) the clinical team's ordering of a head CT signaled a suspicion for head-related injury, and 2) this population with acute head CT matches the screening population for several prospective observational studies of suspected TBI patients (ClinicalTrials.Gov Identifiers NCT01132937, NCT01287156, NCT01565551, and NCT02119182). A limitation of this retrospective analysis is that our study does not assess the population with a mechanism of TBI assessed by the ED, but who did not undergo head CT. Diagnosis of mild TBI can be made by symptoms alone, in the absence of warning signs that indicate a head CT is clinically indicated.7 As a result of the requirement for head CT for inclusion in this retrospective study, the included population likely underestimates the mildest of TBI cases for which a head CT was not clinically indicated. Our data demonstrating a link between a positive head CT and discharge location may also be indicative of a higher incidence of polytrauma or other comorbidities. Investigating the accuracy of documented ED diagnosis of TBI in the ED population with a mechanism of TBI, but without clinical head CT, was beyond the scope of this retrospective chart review.
This retrospective study was limited to ED admissions, and therefore TBI diagnosed either during the course of hospitalization or in the primary care setting after discharge were not assessed. This study was not designed to calculate national incidence of TBI, but rather to determine the extent of TBI diagnosis in the ED in patients who had a clinical head CT and identify the factors that contribute to whether a patient receives a documented ED diagnosis of TBI. Without proper documentation of a TBI diagnosis, patients may not be receiving appropriate education at discharge and may not be aware of the need for follow-up care. Although our study was retrospective and not designed to assess discharge education and follow-up care, results from a prospective study indicate that more than half of patients with documented mild TBI do not receive TBI educational materials at discharge or follow-up care within 3 months.18 Future studies, performed in a prospective manner, will be better able to address the question about the relationship between diagnosis of TBI, discharge instructions, and follow-up care. Primary care physicians, hospitalists, and other members of the patient care team should also be aware of the signs and symptoms of TBI, and have a high index of suspicion for possible mild TBI in symptomatic patients with a history of trauma, but no documented TBI diagnosis, in order to accurately diagnose these patients and/or refer them for appropriate care as necessary.
Conclusions
In conclusion, our findings demonstrate that fewer than 50% of patients presenting to the ED who meet clinical criteria for TBI based on chart review receive a documented ED diagnosis of TBI. This lack of documented diagnosis may lead to complications later in a patient's care, including costly and unnecessary returns to the ED and hospital admissions. Because of the nature of the ED and the need to prioritize the most life-threatening injuries, the ED is unlikely to identify all cases of TBI, particularly mild TBI, especially in the presence of more-severe injury or illness. Although patients with mild TBI may recover with no long-term sequalae, there are patients that may experience persistent or worsening symptoms in the subacute to chronic phases after injury. As a result, it is imperative for physicians to be aware of this and to be able to appropriately document and diagnose TBI, whether they are part of the hospital team taking care of patients admitted from the ED or primary care providers doing follow-up visits. Additionally, the accuracy of ED TBI diagnosis could be improved by integrating standardized concussion assessments and automated methods to help identify patients meeting diagnostic criteria into electronic medical record systems, without increasing the burden on ED physicians. This would not only improve diagnosis of TBI, but may also improve estimates of the incidence of TBI.
Accurate documentation and diagnosis of TBI will allow physicians to treat symptoms, improve patient education, and refer patients to specialists as necessary. Improved documentation of diagnoses in TBI patients will also help researchers who seek to understand the consequences of TBI and hope to design interventional therapies for treatment.
Supplementary Material
Acknowledgments
Support for this work included funding from the Intramural Research Program at the National Institutes of Health and the Department of Defense through the Center for Neuroscience and Regenerative Medicine. We acknowledge Johns Hopkins Suburban Hospital and MedStar Health Washington Hospital Center for providing the data necessary for this study.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Taylor C.A., Bell J.M., Breiding M.J., and Likang X. (2017). Traumatic brain injury–related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill. Summ. 66, 1–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Makdissi M., Cantu R.C., Johnston K.M., McCrory P., and Meeuwisse W.H. (2013). The difficult concussion patient: what is the best approach to investigation and management of persistent (>10 days) postconcussive symptoms? Br. J. Sports Med. 47, 308–313 [DOI] [PubMed] [Google Scholar]
- 3. Levin H.S., and Diaz-Arrastia R.R. (2015). Diagnosis, prognosis, and clinical management of mild traumatic brain injury. Lancet Neurol. 14, 506–517 [DOI] [PubMed] [Google Scholar]
- 4. Carroll L.J., Cassidy J.D., Cancelliere C., Côté P., Hincapié C.A., Kristman V.L., Holm L.W., Borg J., Nygren-de Boussard C., and Hartvigsen J. (2014). Systematic review of the prognosis after mild traumatic brain injury in adults: cognitive, psychiatric, and mortality outcomes: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch. Phys. Med. Rehabil. 95, 3 Suppl., S152–S173 [DOI] [PubMed] [Google Scholar]
- 5. Powell J.M., Ferraro J.V., Dikmen S.S., Temkin N.R., and Bell K.R. (2008). Accuracy of mild traumatic brain injury diagnosis. Arch. Phys. Med. Rehabil. 89, 1550–1555 [DOI] [PubMed] [Google Scholar]
- 6. Pogoda T.K., Iverson K.M., Meterko M., Baker E., Hendricks A.M., Stolzmann K.L., Krengel M., Charns M.P., Amara J., Kimerling R., and Lew H.L. (2014). Concordance of clinician judgment of mild traumatic brain injury history with a diagnostic standard. J. Rehabil. Res. Dev. 51, 363–376 [DOI] [PubMed] [Google Scholar]
- 7. Stiell I.G., Wells G.A., Vandemheen K., Clement C., Lesiuk H., Laupacis A., McKnight R.D., Verbeek R., Brison R., Cass D., Eisenhauer M.E., Greenberg G, and Worthington J. (2001). The Canadian CT Head Rule for patients with minor head injury. Lancet Lond. Engl. 357, 1391–1396 [DOI] [PubMed] [Google Scholar]
- 8. Korley F.K., Kelen G.D., Jones C.M., and Diaz-Arrastia R. (2016). Emergency department evaluation of traumatic brain injury in the United States, 2009–2010. J. Head Trauma Rehabil. 31, 379–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bazarian J.J., Veazie P., Mookerjee S., and Lerner E.B. (2006). Accuracy of mild traumatic brain injury case ascertainment using ICD-9 codes. Acad. Emerg. Med. 13, 31–38 [DOI] [PubMed] [Google Scholar]
- 10. Yuh E.L., Mukherjee P., Lingsma H.F., Yue J.K., Ferguson A.R., Gordon W.A., Valadka A.B., Schnyer D.M. Okonkowo D.O., Maas A.I., and Manley G.T.; TRACK-TBI Investigators. (2013). Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Ann. Neurol. 73, 224–235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Menon D.K., Schwab K., Wright D.W., and Maas A.I. (2010). Position statement: definition of traumatic brain injury. Arch. Phys. Med. Rehabil. 91, 1637–1640 [DOI] [PubMed] [Google Scholar]
- 12. DiMaggio C.J., Avraham J.B., Lee D.C., Frangos S.G., and Wall S.P. (2017). The Epidemiology of emergency department trauma discharges in the United States. Acad. Emerg. Med. 24, 1244–1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gaw C.E., and Zonfrillo M.R. (2016). Emergency department visits for head trauma in the United States. BMC Emerg. Med. 16, 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bazarian J.J., Mcclung J., Shah M.N., Ting Cheng Y., Flesher W., and Kraus J. (2005). Mild traumatic brain injury in the United States, 1998–2000. Brain Inj. 19, 85–91 [DOI] [PubMed] [Google Scholar]
- 15. de Koning M.E., Scheenen M.E., van der Horn H.J, Hageman G., Roks G., Spikman J.M., and van der Naalt J. (2017). Non-hospitalized patients with mild traumatic brain injury: the forgotten minority. J. Neurotrauma. 34, 257–261 [DOI] [PubMed] [Google Scholar]
- 16. Albrecht J.S., Hirshon J.M., McCunn M., Bechtold K.T., Simoni-Wastila L., and Smith G.S. (2016). Increased rates of mild traumatic brain injury among older adults in US emergency departments, 2009–2010. J. Head Trauma Rehabil. 31, E1–E7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gardner R.C., Dams-O'Connor K., Morrissey M.R., and Manley G.T. (2018). Geriatric traumatic brain injury: epidemiology, outcomes, knowledge gaps, and future directions. J. Neurotrauma Feb 15. doi: 10.1089/neu.2017.5371. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Seabury S.A, Gaudette E., Goldman D.P., Markowitz A.J., Brooks J., McCreas M.A, Okonkwo D.O., and Manley G.T.; TRACK-TBI Investigators. (2018). Assessment of follow-up care after emergency department presentation for mild traumatic brain injury and concussion: Results from the TRACK-TBI study. JAMA Network Open 1, e180210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Arbogast K.B., Curry A.E., Pfeiffer M.R., Zonfrillo M.R., Haarbauer-Krupa J., Breiding M.J., Coronado V.G., and Master C.L. (2016). Point of health care entry for youth with concussion within a large pediatric care network. JAMA Pediatr. 170, e160294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gravel J., D'Angelo A., Carrière B., Beauchamp M.H., Chauny J.M., Wassef M., and Chaillet N. (2013). Interventions provided in the acute phase for mild traumatic brain injury: a systematic review. Syst. Rev. 2, 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Comper P., Bisschop S.M., Carnide N., and Tricco A. (2005). A systematic review of treatments for mild traumatic brain injury. Brain Inj. 19, 863–880 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.