Abstract
Introduction
Anxiety is a common symptom for those experiencing dementia and is associated with worse outcomes. The aim of the study was to examine which anxiety tools have been validated compared with a gold standard diagnostic criterion in persons with dementia.
Methods
We completed a systematic review of the literature, which was registered a priori with PROSPERO (CRD42016042123). Three databases were searched, MEDLINE, EMBASE, and PsycINFO, as well as the gray literature. Abstracts and full text were searched in duplicate for inclusion. Risk of bias was assessed in duplicate.
Results
We identified 9626 citations from all sources after duplicates were removed. Many excluded studies used tools for anxiety, for which no diagnostic accuracy study was identified. Four articles were included in the final synthesis. Included articles had between 32 to 101 participants with mild to moderate dementia. The gold standard criteria focused on either generalized anxiety or all anxiety subtypes. The prevalence of anxiety was between 27.7% and 63.4%. Three tools were examined, the Geriatric Anxiety Inventory, Penn State Worry Questionnaire, and the Rating Anxiety in Dementia (RAID) scale. Sensitivity varied but was the highest in the RAID at 90% and lowest in the self-rated version of the Geriatric Anxiety Inventory (58%).
Discussion
Given how burdensome the symptoms of anxiety are to persons with dementia, valid tools are needed to help identify symptoms. We identified three validated tools, but further validation of these and other tools are needed. Practitioners should consider the use of tools with high sensitivity such as the RAID in persons with dementia.
Keywords: Dementia, Anxiety, Detection, Neuropsychiatric symptoms, Generalized anxiety disorder, Systematic review, Diagnostic accuracy
1. Introduction
Anxiety is a pervasive disorder that increases the symptom burden for persons with dementia [1]. Twenty five to seventy percent of those experiencing dementia have anxiety symptoms [1], [2]. Anxiety often correlates with poor quality of life, poor physical function, increased caregiver burden [1], cognitive impairment [3], and increased admission to nursing home [1], [4], [5]. Anxiety is more frequent when persons with dementia have an insight into their illness [6], early-onset disease, or less severe cognitive impairment [7].
Diagnosing anxiety in those experiencing dementia is often difficult because of overlapping symptoms with their primary neurodegenerative condition, other neuropsychiatric symptoms, severity of dementia, reliance on caregiver reports, and the lack of agreed-upon diagnostic criteria specific to dementia [1], [8]. There are also several subtypes of anxiety disorders including generalized anxiety disorders (GADs) [9], [10], panic disorder, and anxiety not otherwise specified [11].
Anxiety in persons with dementia is frequently underdiagnosed and undertreated, demonstrating a gap in care for these patients [12]. Given the burden associated with anxiety, it is important that practitioners have an approach to detection [13]. Brief neuropsychiatric questionnaires can be used as they ideally provide a convenient and accurate format for detection. Our objective was to examine which anxiety tools or questionnaires are valid and accurate when compared with a diagnostic standard for the detection of anxiety symptoms in those experiencing dementia. To our knowledge, there is no prior review that specifically focuses on the accuracy of anxiety tools in this population compared with a diagnostic gold standard.
2. Methods
A systematic review was conducted, following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis reporting items for diagnostic accuracy studies [14]. This systematic review protocol was registered with PROSPERO (CRD42016042123) [15].
The search strategy focused on three major clusters of terms for dementia, anxiety, and diagnostic accuracy terms (Supplementary Material 1). The databases included were MEDLINE, EMBASE, and PsycINFO. The keywords and controlled vocabulary (MeSH, EMTREE, and PsycINFO terms) were combined within the cluster with OR. Between cluster terms were combined with AND. There were no restrictions for date or language used. The search was initially constructed by a study researcher (Z.G.) and was reviewed by an experienced health sciences librarian. The search was completed on February 1, 2017.
Gray literature, literature not found in the traditional journals or databases, (listed in Supplementary Material 2) was identified using the CADTH Gray Matters Guide [16] and study authors' content knowledge. Each source was searched using dementia and anxiety terms, and results were reviewed for inclusion. References of included studies were also searched.
Six authors reviewed abstracts (Z.G., Z.I., L.S., R.S., S.C., F.A.); all abstracts were reviewed in duplicate, and any article included by either author was also included in full-text review. Abstracts were included if they discussed the use of any tool specific for anxiety or included an anxiety item within the tool and applied it on patients with dementia. Two authors (Z.G. and L.S.) reviewed all full-text articles. At the full-text stage, disagreement was resolved by discussion and a third author if needed. Full-text articles were included if the study used an anxiety tool and gold standard in patients experiencing dementia. Gold standards considered for inclusion were any criterion-based interviews (e.g., based on the Diagnostic Statistical Manual [11], any version, or International Classification of Disease, any version) [17] or a clinical interview by a trained practitioner (e.g., nurse or physician). These gold standards included represent what is the current diagnostic standard. Patients of any age, with any type of dementia, and from any setting (inpatient or outpatient) were included. If the article did not report the diagnostic accuracy outcomes (e.g., sensitivity, specificity, and so forth), authors were emailed to see if these data were available.
Risk of bias of included studies was evaluated independently by two authors (Z.G. and J.H.-L.) in duplicate using the Quality Assessment for Diagnostic Accuracy Studies-2 [18]. Any disagreement on risk-of-bias assessment was resolved by discussion.
Data were extracted from included studies with a standardized form that included study authors, year, country, sample size, tool name, clinical location, dementia severity tool, method of determining dementia diagnosis, subtypes of dementia reported mean age, percent female, prevalence of anxiety, number of items on scale used, best reported cutoff, rater of the tool, gold standard used for anxiety, subtypes of anxiety included, sensitivity, specificity, likelihood ratios, and area under the curve. Data from included full-text articles were extracted by one author (Z.G.) and verified by a second (L.S.).
Meta-analysis of prevalence, sensitivity, specificity, and likelihood ratios was planned. To do so, each tool needed to have 4 independent studies reporting these outcomes. Any statistical analyses were completed using STATA v13.
3. Results
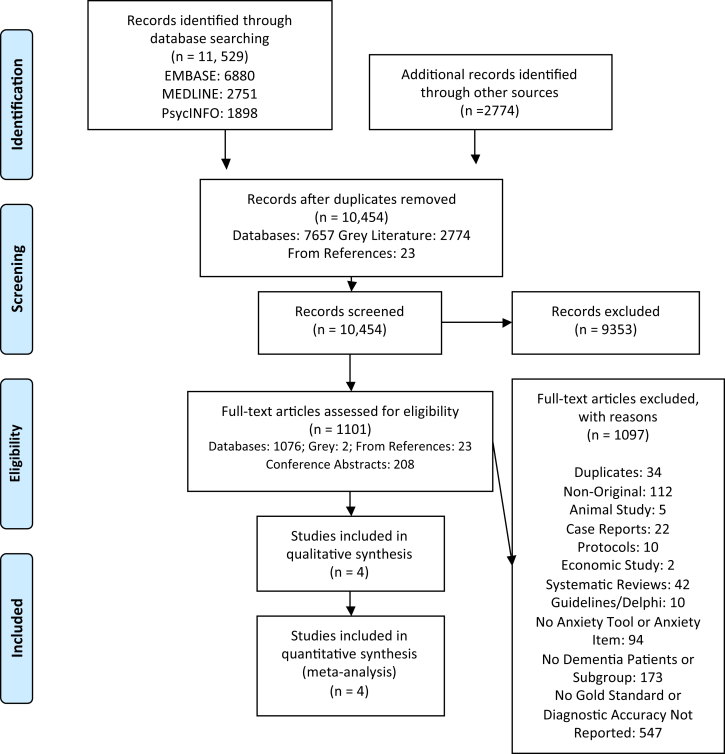
The database search retrieved 11,529 citations, with 7657 from databases once duplicates were removed (Fig. 1). There were 1969 citations from the gray literature, with a further 23 from included study references. A total of 1101 full-text articles were reviewed, and the most common reasons for exclusion were studies not using a gold standard or reporting diagnostic accuracy outcomes (n = 547), no dementia subgroup (n = 173), nonoriginal research (e.g., letters, narrative reviews) (n = 112), and no anxiety tool used (n = 94). At the full-text stage, agreement between reviewers was 98.4% (k = 0.56; 95% confidence interval, 0.37, 0.75). Four articles met inclusion criteria and were included.
Fig. 1.
PRISMA flow diagram. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
Of the 547 excluded studies that examined anxiety tools in dementia patients without a gold standard, the most commonly used tools were Neuropsychiatric Inventory (NPI) (n = 379), Behavioral Pathologic Rating Scale for Alzheimer's disease (n = 39), Rating Anxiety in Dementia (RAID) (n = 25), Hospital Anxiety and Depression Scale (n = 25), and the Hamilton Anxiety Rating Scale (n = 10).
To clarify study data, we attempted to contact 29 study authors. We were only able to contact 27 authors because two studies had no contact information. We had a return email rate of 40.7%, with 4 authors sending us further information that was reviewed.
There were several areas where risk of bias was rated as unclear on the Quality Assessment for Diagnostic Accuracy Studies-2 (Table 1). There were 2 of 4 studies with unclear risk of bias in each of the following domains: patient selection [4], [19], index tests [4], [6], and flow and timing [6], [19]. Risk of bias was unclear for the reference standard in 3 of 4 studies [4], [6], [19]. Specifically, it was not clear if the index and reference standards were interpreted independently. Flow and timing difficulties primarily reflect a lack of reporting of the time between the index and reference standards. Applicability concerns were seen in two studies [4], [19], in which there was a high risk of bias for patient selection compared with other studies as these studies recruited patients who already had a score on the NPI anxiety item of ≥4 and thus may not be representative of a general dementia population.
Table 1.
Quality assessment of diagnostic accuracy studies
| Study identification |
Risk of bias |
Applicability concerns |
|||||
|---|---|---|---|---|---|---|---|
| Author, Year | Patient selection | Index test | Reference standard | Flow and timing | Patient selection | Index test | Reference standard |
| Shankar et al., 1999 [6] | Low | Unclear | Unclear | Unclear | Low | Low | Low |
| Snow et al., 2012 [19]∗ | Unclear | Low | Unclear | Unclear | High | Low | Low |
| Bradford et al., 2013 [4]∗ | Unclear | Unclear | Unclear | Low | High | Low | Low |
| Goyal et al., 2017 [9] | Low | Low | Low | Low | Low | Low | Low |
Abbreviation: RCT, randomized controlled trial.
Snow and Bradford recruited patients from the same pilot RCT.
Studies enrolled 32 to 101 participants, who were predominately females (56.1%–78.2%), aged between 78.6 and 86 years (Table 2). Among included studies, participants had mild to moderate dementia and a variety of dementia subtypes. Studies were conducted in the UK, Norway, and United States. There were several care settings, such as subspecialty clinics, day care centers, day hospitals, nursing homes, and hospital wards.
Table 2.
Study characteristics and diagnostic accuracy outcomes
| Author, Year | n | Tool | Country | Location(s) | Dementia severity | Dementia diagnosis | Dementia types | Mean age (SD) | % Female | Prevalence of anxiety (%) | No. of items | Best cutoff∗ | Rater | Gold standard for anxiety | Type of anxiety | SN | SP | AUC | PLR | NLR | Highest SN |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bradford et al., 2013 [4]†,‡,§ | 41 | Geriatric Anxiety Inventory | USA | Neurology, Geriatrics, Psychiatry Clinics & Dementia Day Care Centers | Mild to moderate | Medical record | NR | 79 (9.1) | 56.1 | 63.4 | 20 | 8 | Trained interviewer | MINI | Any (GAD, anxiety NOS, panic disorder, PTSD) | 0.58 | 0.93 | 0.69 | 8.29 | 0.45 | 0.62 (cutoff 5) |
| Bradford et al., 2013 [4]†,‡,§ | 41 | Geriatric Anxiety Inventory Collateral | USA | Neurology, Geriatrics, Psychiatry Clinics & Dementia Day Care Centers | Mild to moderate | Medical record | NR | 79 (9.1) | 56.1 | 63.4 | 20 | 10 | Collateral | MINI | Any (GAD, anxiety NOS, panic disorder, PTSD) | 0.62 | 0.93 | 0.81 | 8.86 | 0.41 | 0.92 (cutoff 5) |
| Bradford et al., 2013 [4]†,‡,§ | 41 | Penn State Worry Questionnaire (abbreviated) | USA | Neurology, Geriatrics, Psychiatry Clinics & Dementia Day Care Centers | Mild to moderate | Medical record | NR | 79 (9.1) | 56.1 | 63.4 | 8 | 17 | Trained interviewer | MINI | Any (GAD, anxiety NOS, panic disorder, PTSD) | 0.62 | 0.73 | 0.69 | 2.30 | 0.52 | 0.77 (cutoff 13) |
| Bradford et al., 2013 [4]†,‡,§ | 41 | Penn State Worry Questionnaire (abbreviated) Collateral | USA | Neurology, Geriatrics, Psychiatry Clinics & Dementia Day Care Centers | Mild to moderate | Medical record | NR | 79 (9.1) | 56.1 | 63.4 | 8 | 22 | Collateral | MINI | Any (GAD, anxiety NOS, panic disorder, PTSD) | 0.81 | 0.73 | 0.77 | 3.00 | 0.26 | 0.92 (cutoff 13) |
| Goyal et al., 2016 [9]‡ | 101 | Rating Anxiety in Dementia (Norwegian Version) | Norway | Nursing homes | Mild to moderate | DSM V | AD, VAD, FTD, mixed (AD, VAD, LBD) | 86.0 (6.5) | 78.2 | 27.7 | 18 | 10 | Clinician | DSM V | GAD | 0.85 | 0.56 | 0.8 | 1.9 | 0.3 | 0.89 (cutoff 9) |
| Shankar et al., 1999 [6] | 24¶ | Rating Anxiety in Dementia | UK | Inpatient, day hospital/day center, long stay continuing care wards | NR (CDR done but NR) | DSM IV | AD, VAD other dementias | 79.1 (7) | 62 | 41.7 | 18 | 11 | Clinician | DSM IV | GAD | 0.90 | 0.79 | NR | 4.29 | 0.13 | |
| Snow et al., 2012 [19]†,‡ | 32 | Rating Anxiety in Dementia | USA | Geriatrics, Neurology, Primary Care Clinics, Community Day Centers | Mild to moderate | Diagnosis confirmed by provider | AD, LBD, VAD, dementia NOS | 78.6 (9.7) | 59.4 | 62.5 | 18 | 10 | Trained assessor | MINI | Any (GAD, anxiety NOS, panic disorder, PTSD) | 0.90 | 0.67 | 0.8 | 2.72 | 0.15 | 0.95 (cutoff 9) |
Abbreviations: N, sample size; NR, not reported; SN, sensitivity; SP, specificity; PLR, positive likelihood ratio; NLR, negative likelihood ratio; AUC, area under the curve; DSM, Diagnostic and Statistical Manual; MINI, Mini International Neuropsychiatric Interview; GAD, generalized anxiety disorder; NOS, not otherwise specified; PTSD, posttraumatic stress sisorder; AD, Alzheimer's disease; VAD, vascular dementia; FTD, frontotemporal dementia; LBD, Lewy body dementia; SD, standard deviation; CDR, Clinical Dementia.
Best meaning—optimal balance of sensitivity and specificity as reported by authors.
Patients recruited from the same CBT trial.
Includes patients with CDR 0.5 or minor neurocognitive disorder.
Note all rows from Bradford et al. represent the same study, with each row outlining a different tool or version of a tool.
There were 83 patients in the study but only 24 completed the DSM assessment.
The prevalence of anxiety was between 27.7% and 63.4%, based on the gold standard assessments. The anxiety gold standard was primarily the Diagnostic and Statistical Manual (DSM) versions IV or V [11]. Anxiety disorders discussed in the included articles varied. Some included only GAD, and others included any anxiety diagnosis (e.g., GAD, panic disorder, anxiety not otherwise specified, and posttraumatic Stress disorder). Meta-analysis of prevalence was not completed due to clinical heterogeneity among the types of anxiety compared.
Included tools (Table 2) were the abbreviated Penn State Worry Questionnaire (self-rating and collateral versions) (PSWQ) [4], the RAID (English and Norwegian version) [6], [9], [18], and the Geriatric Anxiety Inventory (self-rating and collateral versions) (GAI) [4] (Table 3, tool properties).
Table 3.
Anxiety tool descriptions
| Tool name | Number of items | Time frame of symptoms | Rater | Types of anxiety covered | Answer type | Availability |
|---|---|---|---|---|---|---|
| Geriatric Anxiety Inventory [4], [20] | 20 | 1 Week | Self-rater or proxy rater | GAD | Dichotomous | Copyrighted, cost for use clinically, translated to several languages |
| Penn State Worry Questionnaire, abbreviated [4], [21], [22] | 8 | 1 Week | Self or proxy rater | GAD | Likert Scale (1–5) | Not copyrighted, available in original publication |
| Rating Anxiety in Dementia [6], [9], [19] (regular and structured interview version) | 18 + 2 Descriptive items | 2 Weeks | Clinician based on patient interview, caregiver report, chart, and observations | Worry, apprehension and vigilance, motor tension, autonomic hypersensitivity, phobias, panic attacks | Likert Scale (0–3) | Not copyrighted, available in original publication |
Abbreviation: GAD, generalized anxiety disorder.
The RAID was validated in three separate studies, unlike the PSWQ and GAI that were both only validated in single studies. Among cutoffs that balance sensitivity and specificity, the RAID had the highest sensitivity at 90% across two studies [6], [19]. The PSWQ was the most specific one at 93% [4]. The area under the curve was highest for the collateral version of the GAI (0.81) and RAID (0.8). There were not enough studies per tool to complete a meta-analysis.
4. Discussion
Anxiety symptoms commonly affect those with dementia [1], and brief neuropsychiatric questionnaires provide means for detection of these symptoms. Despite this, we identified only 3 tools that have been validated compared with a gold standard. This demonstrates that there is still a gap in the literature when it comes to validating tools for anxiety disorders in patients experiencing dementia. This lack of validation is probably related, at least in part, to the absence of agreed-upon criteria for the diagnosis of anxiety disorders in those with dementia [5].
Despite this, there are some valid tools that should be considered for use in practice. The RAID was validated in 3 studies and was also commonly used in excluded studies (n = 25). This tool was developed specifically to examine anxiety in those experiencing dementia. It was constructed based on the available criteria for anxiety, such as the DSM-III-R, DSM IV, and International Criteria for Diagnosis version 10 [6], as well as available anxiety tools. For the RAID, sensitivity ranges from 85% to 90% and specificity from 56% to 79% [6], [9], [19]. The high sensitivity of this tool compared with others is ideal for detection as this confers the low false-negative rate. However, it is noted that there is a wider range in the specificity of the RAID, with the Norwegian version having the lowest at 56% [9] and the English version between 67 and 79% [6], [19]. The specificity may vary as these three articles have differing populations, with the Norwegian study focusing solely on those living in long-term care [9] and the other two English studies looking at inpatients and specialty clinics as well [6], [19]. It would be important for future studies to evaluate the differences between different locations.
The PSWQ and GAI were studied as self- and collateral-rating versions; in both cases, the collateral versions had higher sensitivity [4]. The collateral source GAI has the most items of the three tools and the highest specificity at 93% [4]. However, the sensitivity of these tools was lower than that of the RAID tool.
When it comes to application in the clinical setting, the PSWQ [4], [21], [22] has the fewest questions (8), and only the GAI is copyrighted [4], [20]. The PSWQ [4], [21], [22] and GAI [4], [20] are self-rating or proxy rating scales. The RAID has 18 rated items and 2 descriptive items, and it has been traditionally administered by trained personnel (e.g., clinician) based on multisource feedback (e.g., chart, collateral, and so forth) [6]. There is little published information on time for administration for these tools.
Caregivers often provide collateral information to health-care providers when it comes to neuropsychiatric symptoms [5]. On the one hand, this is felt to improve the accuracy of the reporting of symptoms when the person with dementia perhaps has trouble with expressing or recalling their symptoms [5]. But, on the other hand, there may be concerns that the caregiver rating may differ from the physician or patient rating [13], [23]. When anxiety was rated on the NPI in patients with Alzheimer's disease, it was seen that there were frequent disagreements between caregivers and physicians when rating anxiety (among other symptoms) [13]. This was prominent in those with mild dementia, with diminishing discrepancy as dementia severity increases [13]. Similarly, another study found that caregiver ratings of anxiety in persons with dementia had poor correlation with patient scores on anxiety tools [23]. In the included studies, the tools with the highest sensitivity are those that include a collateral source, in conjunction with information from the person living with dementia. Further work is needed to establish the comparative accuracy between the self-rated and proxy-rated anxiety tools.
Although the identified tools were validated against a gold standard for anxiety, the question remains as to what is the best gold standard for anxiety in those experiencing dementia [5]. There are currently no universally accepted criteria for anxiety disorders in those with dementia [8]. The gold standards used in the included studies were primarily based on the DSM IV or V [11]. However, certain symptoms in the DSM V for GAD, for example, “difficulty concentrating,” directly overlap with the symptoms of dementia [11]. Therefore, health-care providers need to consider these symptoms carefully when diagnosing GAD in these patients [11]. In two studies, they used a gold standard focused on GADs [6], [9], and the others included all anxiety disorders. It is not clear which of these criteria are most representative of the anxiety symptoms experienced in dementia. In addition, the study looking at the PSWQ and GAI based their anxiety diagnoses on a review of the medical record, whereas the other studies used DSM diagnoses or clinical diagnoses. These differences in anxiety diagnosis can also effect the accuracy outcomes; a study comparing the use of chart versus clinical diagnosis would confirm this.
Starkstein et al. [8] explored the validity of DSM version 4 and International Criteria for Diagnosis version 10 criteria for GAD in the setting of those experiencing dementia. Based solely on the core criteria of having “excessive anxiety and worry present for more days than not for at least 6 months causing significant distress” they found that 26% (n = 144 of 552) had these symptoms [8]. Their analysis identified that important symptoms associated with core criteria were muscle tension, fears, restlessness, irritability, and respiratory symptoms [8]. Given the lack of clarity, there needs to be further work to evaluate which gold standard is best for the diagnosis of anxiety in those with dementia, considering the construct of “clinically relevant anxiety” symptoms.
Based on the findings of this review, there are many tools being used to measure anxiety in those with dementia but only minimal studies validating their use. We were inclusive at the abstract level and found 527 articles, which examined a population of or including persons with dementia and used an anxiety tool. The primary focus of these excluded studies was examining prevalence or treatment of neuropsychiatric symptoms; thus, their focus was not on diagnostic accuracy. However, this demonstrates a wide range of tools being used as primary or secondary outcomes to measure anxiety in those with dementia, which have unclear accuracy. As a result, studies using these less validated tools may be vulnerable to inaccuracy in these main outcomes via measurement bias.
The NPI was also commonly used in studies. However, the diagnostic accuracy for the subdomain of anxiety in those experiencing dementia was not identified in this review. When measuring anxiety as an outcome, there is a dichotomy between the general neuropsychiatric scales (e.g., not focused on anxiety alone) and the specific anxiety tools. We found no studies that contrast the accuracy of general versus anxiety-specific questionnaires in dementia; thus, there is no sufficient evidence to comment on any potential differences in accuracy. However, given the general scales typically have few anxiety questions, their specificity is potentially lower.
Based on this review, there are several other possibly effective anxiety tools that have not yet been validated, and further studies should explore these (e.g., Anxiety in Cognitive Impairment and Dementia scale [24]) and could also explore direct comparison of different anxiety tools.
The accuracy of anxiety tools is not clear in those with severe dementia because the patients included in studies primarily had mild to moderate dementia. Similarly, few studies examined different languages and cultural differences in the applications of these tools. We are also not able to comment on differences in tool accuracy between subtypes of dementia or based on the participants' environment (e.g., care facility vs. home). Future work should evaluate different living settings, pathologies, and severities of dementia.
4.1. Limitations
It is possible we could be missing relevant articles; to address this, we were inclusive in our database search, gray literature search, and article inclusion. As the measured gold standards included several different types of anxiety, we did not complete a meta-analysis of prevalence because the clinical heterogeneity was perceived to be too high. Owing to too few studies, we were unable to complete a meta-analysis of diagnostic accuracy.
5. Conclusion
This review has identified three validated tools for detecting anxiety symptoms in those experiencing dementia: RAID, PSWQ, and GAI. When considering anxiety tools, practitioners need to balance tool accuracy and ease of use. The RAID has the highest sensitivity for anxiety disorders, includes a caregiver interview, and was specifically designed for those experiencing dementia. Further work is needed to examine the accuracy of different anxiety detection tools in diverse populations experiencing dementia.
Research in context.
-
1.
Systematic review: The authors of this study followed the methods of systematic review as per the Preferred Reporting Items for Systematic Reviews and Meta-Analysis checklist and registered the search in PROSPERO. Three databases, as well as several grey literature sources, were searched. Anxiety symptoms are common in persons living with dementia, and accurate tools are needed to detect these symptoms.
-
2.
Interpretation: Although anxiety is common and has adverse effects on persons living with dementia, there are few tools validated against a diagnostic gold standard for use in this population.
-
3.
Further directions: Further studies are needed to examine the validity of anxiety tools in persons living with dementia, specifically in those with severe dementia, living in long-term care or with less common pathologies.
Acknowledgments
Financial Disclosure Statement: This study received funding from the Hotchkiss Brain Institute and Department of Clinical Neurosciences at the University of Calgary. Z.G. has grant funding from the MSI foundation, Brenda Strafford Foundation, and the Hotchkiss Brain Institute. L.S., F.A., R.S., S.C., and T.P. have no relevant financial disclosures. E.E.S. receives grant funding from the Canadian Institute of Health Research and Brain Canada, and writing fees from Up-to-date and is the assistant editor for the Journal of the American Heart Association. Z.I. has no relevant financial disclosures. J.H.-L. is a research chair from the Brenda Strafford Foundation.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.dadm.2019.02.005.
Supplementary Data
References
- 1.Calleo J.S., Kunik M.E., Reid D., Kraus-Schuman C., Paukert A., Regev T. Characteristics of generalized anxiety disorder in patients with dementia. Am J Alzheimers Dis Other Demen. 2011;26:492–497. doi: 10.1177/1533317511426867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bierman E.J., Comijs H.C., Jonker C., Beekman A.T. Symptoms of anxiety and depression in the course of cognitive decline. Dement Geriatr Cogn Disord. 2007;24:213–219. doi: 10.1159/000107083. [DOI] [PubMed] [Google Scholar]
- 3.Hynninen M.J., Breitve M.H., Rongve A., Aarsland D., Nordhus I.H. The frequency and correlates of anxiety in patients with first-time diagnosed mild dementia. Int Psychogeriatr. 2012;24:1771–1778. doi: 10.1017/S1041610212001020. [DOI] [PubMed] [Google Scholar]
- 4.Bradford A., Brenes G.A., Robinson R.A., Wilson N., Snow A.L., Kunik M.E. Concordance of self- and proxy-rated worry and anxiety symptoms in older adults with dementia. J Anxiety Disord. 2013;27:125–130. doi: 10.1016/j.janxdis.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seignourel P.J., Kunik M.E., Snow L., Wilson N., Stanley M. Anxiety in dementia: a critical review. Clin Psychol Rev. 2008;28:1071–1082. doi: 10.1016/j.cpr.2008.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shankar K.K., Walker M., Frost D., Orrell M.W. The development of a valid and reliable scale for rating anxiety in dementia (RAID) Aging Ment Health. 1999;3:39–49. [Google Scholar]
- 7.Kaiser N.C., Liang L.J., Melrose R.J., Wilkins S.S., Sultzer D.L., Mendez M.F. Differences in anxiety among patients with early- versus late-onset Alzheimer's disease. J Neuropsychiatry Clin Neurosci. 2014;26:73–80. doi: 10.1176/appi.neuropsych.12100240. [DOI] [PubMed] [Google Scholar]
- 8.Starkstein S.E., Jorge R., Petracca G., Robinson R.G. The construct of generalized anxiety disorder in Alzheimer disease. Am J Geriatr Psychiatry. 2007;15:42–49. doi: 10.1097/01.JGP.0000229664.11306.b9. [DOI] [PubMed] [Google Scholar]
- 9.Goyal A.R., Bergh S., Engedal K., Kirkevold M., Kirkevold O. Norwegian version of the rating anxiety in dementia scale (RAID-N): a validity and reliability study. Aging Ment Health. 2016:1–6. doi: 10.1080/13607863.2016.1220921. [DOI] [PubMed] [Google Scholar]
- 10.Stanley M.A., Calleo J., Bush A.L., Wilson N., Snow A.L., Kraus-Schuman C. The peaceful mind program: a pilot test of a cognitive-behavioral therapy-based intervention for anxious patients with dementia. Am J Geriatr Psychiatry. 2013;21:696–708. doi: 10.1016/j.jagp.2013.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Psychiatric Association . 5th ed. American Psychiatric Publishing; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 12.Shankar K.K., Orrell M.W. Detecting and managing depression and anxiety in people with dementia. Curr Opin Psychiatry. 2000;13:55–59. [Google Scholar]
- 13.Stella F., Forlenza O.V., Laks J., de Andrade L.P., de Castilho Cação J., Govone J.S. Caregiver report versus clinician impression: disagreements in rating neuropsychiatric symptoms in Alzheimer's disease patients. Int J Geriatr Psychiatry. 2015;30:1230–1237. doi: 10.1002/gps.4278. [DOI] [PubMed] [Google Scholar]
- 14.McInnes M.D.F., Moher D., Thombs B.D., McGrath T.A., Bossuyt P.M., the PRISMA-DTA Group Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies: The PRISMA-DTA Statement. JAMA. 2018;319:388–396. doi: 10.1001/jama.2017.19163. [DOI] [PubMed] [Google Scholar]
- 15.Guidance notes for registering a systematic review protocol with PROSPERO . National Institute for Health Research; 2013. PROSPERO: International Prospective Register of Systematic Reviews Centre for Reviews and Dissemination. [Google Scholar]
- 16.Grey Matters: a practical tool for searching health-related grey literature. [online] www.cadth.ca/resources/finding-evidence Available at: Accessed February 1, 2017.
- 17.World Health Organization . World Health Organization; Geneva: 1992. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. [Google Scholar]
- 18.Whiting P.F., Rutjes A.W., Westwood M.E., Mallett S., Deeks J.J., Reitsma J.B. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 19.Snow A.L., Huddleston C., Robinson C., Kunik M.E., Bush A.L., Wilson N. Psychometric properties of a structured interview guide for the rating for anxiety in dementia. Aging Ment Health. 2012;16:592–602. doi: 10.1080/13607863.2011.644518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pachana N.A., Byrne G.J., Siddle H., Koloski N., Harley E., Arnold E. Development and validation of the Geriatric Anxiety Inventory. Int Psychogeriatr. 2007;19:103–114. doi: 10.1017/S1041610206003504. [DOI] [PubMed] [Google Scholar]
- 21.Crittendon J., Hopko D.R. Assessing worry in older and younger adults: Psychometric properties of an abbreviated Penn State Worry Questionnaire (PSWQ-A) J Anxiety Disord. 2006;20:1036–1054. doi: 10.1016/j.janxdis.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Meyer T.J., Miller M.L., Metzger R.L., Borkovec T.D. Development and validation of the Penn State Worry Questionnaire. Behav Res Ther. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 23.Gibbons L.E., Teri L., Logsdon R.G., McCurry S.M. Assessment of anxiety in dementia: an investigation into the association of different methods of measurement. J Geriatr Psychiatry Neurol. 2006;19:202–208. doi: 10.1177/0891988706292758. [DOI] [PubMed] [Google Scholar]
- 24.Gerolimatos L.A., Ciliberti C.M., Gregg J.J., Gregg J.J., Nazem S., Bamonti P.M. Development and preliminary evaluation of the anxiety in cognitive impairment and dementia (ACID) scales. Int Psychogeriatr. 2015;27:1825–1838. doi: 10.1017/S1041610215001027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.