Abstract
Our objective was to characterize the relationship between public housing residents’ diet/exercise habits with similar behaviors among their social network. We conducted a cross-sectional survey of randomly selected households in Baltimore, Maryland, from August 2014 to August 2015. Adult heads of household completed questions on diet, exercise, and perceived habits among network members. Our dependent variables were high added sugar intake (≥39.9 teaspoons/day), high fruit/vegetable intake (≥6.1 servings/day), and being physically active (≥moderately activity). Our network exposures were proportion of members perceived to daily consume (1) sugar-sweetened beverages, (2) sweets, (3) fruits, and (4) vegetables, as well as to weekly exercise (1) vigorously or (2) moderately. We used multivariate logistic regression to examine associations between habits with relevant network exposures. Our sample included 266 adults with mean age of 44.5 years, 86.1% women and 95.5% African American. We found a statistically significant association between study participants’ high daily intake of added sugar with perceived network exposure to daily sugar-sweetened beverages (odds ratio [OR] = 1.10, 95% confidence interval [CI] [1.02, 1.20]) and daily sweets (OR = 1.10, 95% CI [1.02, 1.20]). Greater network exposure to weekly vigorous exercise was significantly associated with personally being physically active (OR = 1.15, 95% CI [1.04, 1.28]), but not network exposure to weekly moderate exercise. Among public housing residents, associations exist between individuals’ and perceived networks’ lifestyle habits of high added sugar foods consumption and vigorous exercise, which may hold promise for future social network interventions.
Keywords: diet, exercise, health behavior, public housing, social influence
Obesity is pervasive among adults living in public housing, where the prevalence is over 50% (Ludwig et al., 2011) relative to a third of U.S. adults (Flegal, Kruszon-Moran, Carrol, Fryar, & Ogden, 2016). The U.S. Department of Housing and Urban Development estimates that 1.1 million households currently reside in public housing (U.S. Department of Housing and Urban Development, 2015). The 10-year outcomes from the “Moving to Opportunities” project suggested that public housing residents who had the opportunity to move to a higher income neighborhood had reduced prevalence of extreme obesity as compared to residents without this opportunity (Ludwig et al., 2011). This evidence implies that living in low-income public housing confers an increased risk of obesity to residents; however, mechanisms contributing to this risk remain uncertain. One goal of this study is to examine social factors that may explain this association.
Public housing developments are often located in neighborhoods with a confluence of negative environmental factors including low socioeconomic status, limited access to resources to promote healthy lifestyles, and social stressors like high crime rates. Grocery store and recreation facility availability tends to be limited in these neighborhoods, which results in poor access to healthy foods and exercise (Gordon-Larsen, Nelson, Page, & Popkin, 2006; Larsen, Story, & Nelson, 2009; Powell, Slater, Mirtcheva, Bao, & Chaloupka, 2007). Interventions attempting to address disparities in access have yielded modest benefits among low-income populations—in some cases resulting in no change in lifestyle behaviors (Gittelsohn et al., 2010), suggesting the need to examine other factors to promote behavior change.
While much research has examined the economic and built environments, less attention has focused on the social environment. An individual’s social networks can influence behaviors through social influence such as social norms and behavior modeling (Bandura, 1986). Networks can encourage certain behaviors, and members may also directly contribute to foods consumed in a household. The potential for social networks to promote change has been studied in health behaviors like smoking cessation (Christakis & Fowler, 2008; Cobb, Graham, & Abrams, 2010) and HIV risk reduction practices (Castor et al., 2010; Latkin, Sherman, & Knowlton, 2003; Tobin, Kuramoto, Davey-Rothwell, & Latkin, 2011). A prominent study suggested a link between social networks and obesity risk (Christakis & Fowler, 2007), although the results were controversial given its failure to account for contextual influences of shared surroundings (Cohen-Cole & Fletcher, 2008). Mathematical simulations have illustrated the spread of obesity through social networks and how networks might be used to mitigate the epidemic (Bahr, Browning, Wyatt, & Hill, 2009). While these prior studies may show the diffusion of obesity, research examining what specific behaviors drive this phenomenon has been limited. For example, having more close-knit relationships and friends who live nearby has been associated with healthier diets in general populations (Bot, Mackenbach, Nijpels, & Lakervald, 2016). Research is needed that specifically assesses detailed diet and exercise habits among social networks, particularly among populations with high obesity prevalence. Finally, network influence may help explain, in part, why many lifestyle interventions have been unsuccessful in sustaining behavior change (Douketis, Macie, Thabane, & Williamson, 2005). Overall, few comparative network studies exist, and additional research is needed to examine the role of networks in health disparities, particularly among impoverished populations that may rely on networks for resources (Stack, 1975).
Guided by social learning theory (Bandura, 1986), our objective was to characterize the relationship between public housing residents’ diet and exercise habits with similar lifestyle behaviors within their social network. We hypothesized that individuals who perceive a greater network exposure to daily intake of high sugar foods will have higher added sugar intake, and similarly those who perceive a greater network exposure to daily intake of fruits/vegetables will have higher fruit/vegetable intake. With regard to exercise, we hypothesized that individuals who perceive a greater network exposure to weekly moderate or vigorous exercise will have greater physical activity levels.
Method
We conducted a cross-sectional survey of randomly selected households in two public housing developments in Baltimore, Maryland, from August 2014 to August 2015. We randomized 600 addresses from a list of all residences in the two developments, of which 556 appeared occupied during neighborhood inspection and therefore eligible for inclusion. We recruited households by mailing postcards and using up to five door-knocking attempts. Up to four adults who lived in each household could participate in the survey, which were conducted in the local administrative building or residents’ homes. We relied on the head of household to verify that any additional adults were residents. Given that residential status of these additional adults could not be verified with the housing authority, we limited our analyses to the heads of household to ensure that our population only included public housing residents. We used social network software to facilitate data collection (EgoNet, MDLogix). Participants received a $40 gift card as compensation. The Johns Hopkins University School of Medicine Institutional Review Board approved this study.
Our primary dependent variables included the dietary and physical activity habits of the survey respondents or “egos.” For diet, respondents completed the National Health Interview Survey (NHIS) 5-factor dietary screener (National Cancer Institute, 2005), which we used to calculate their added sugar (teaspoons [tsp]/day) intake and their fruit/vegetable (servings/day) intake excluding fried potatoes. Per NHIS recommendations, we used standard methods to create variance-adjusted estimates (National Cancer Institute, 2005). We dichotomized each variable as “high” for values that were in the upper quartile of our sample and “not high” if otherwise. We elected to use the upper quartile values from our sample, rather than national estimates, as differences exist by income and race/ethnicity (Kruger, Yore, Solera, & Moeti, 2007; Thompson et al., 2009). In our sample, high intake was ≥39.9 tsp/day for added sugars and ≥6.1 servings/ day for fruits/vegetables. For physical activity, respondents completed a four-item exercise screener modified from an instrument previously validated in healthy adults (Ainsworth, Jacobs, & Leon, 1993), which classifies activity into four levels: high, moderate, low, and very low. As these levels increase, they have been associated with increasing cardiorespiratory fitness and leisure time exercise (Ainsworth et al., 1993). We dichotomized this variable as “high physical activity” if high or moderate and “not high physical activity” if low or very low. Being classified as “high physical activity” corresponds to regularly participating in vigorous exercise (>6 METs [metabolic equivalents]) on a weekly basis as compared to the “not high” group (Ainsworth et al., 1993), which would meet/exceed the guidelines of ≥75 minutes per week of vigorous-intensity activity (Office of Disease Prevention and Health Promotion, 2008).
Our independent variables were the perceived diet and exercise behaviors among the ego’s network members. Supplemental Table S1 (available with the article online) contains the social network questions, which were adapted from a previous survey (Pollack et al., 2014). Respondents completed an egocentric social network inventory where they were asked to generate a list of 15 people with whom they had contact with in the past year, which tends to obtain a diverse group in terms of relationships and interactions. The software then randomly selected 10 names for additional inquiry to ascertain attributes and behaviors of these individuals as perceived by the ego. This approach enables a thorough evaluation of the social network overall, while decreasing respondent burden (McCarty, Killworth, & Rennell, 2007). Egos were asked how often each person ate (1) sugar-sweetened beverages, (2) sweets, (3) fruits, and (4) vegetables (daily, weekly, monthly, never, don’t know/ refused), which we dichotomized as “daily” versus “not daily.” We included “don’t know/refused” responses into “not daily consumption.” For each ego, we then calculated the proportion of their network members who they perceived consuming (1) sugar-sweetened beverages daily, (2) sweets daily, (3) fruits daily, and (4) vegetables daily, which reflects their network exposure to each element (range 0% to 100% of network members). Egos were asked whether or not each person participated in (1) vigorous exercise at least once a week and (2) moderate exercise at least once a week. For each ego, we calculated the proportion of their network members who weekly (1) exercised vigorously and (2) exercised moderately, which reflects their network exposure to each element (range 0% to 100%). For analyses, we scaled the network exposures to these elements to represent a change in proportion of network members by 10% (rather than 1%), which is a more meaningful magnitude of network exposure change. While these network exposures were continuous variables in our primary analyses, we also explored potential exposure–response by categorizing each network exposure where “high” was the upper quartile, “mid” the median to upper quartile, and “low” less than the median based on our sample’s distributions.
We considered several ego attributes as potential covariates including age, gender, race, education, unemployment, food insecurity (Hager et al., 2010), smoking status, body mass index (BMI; calculated from measured height and weight), self-reported history of hypertension, diabetes mellitus, depressive symptoms (Kroenke, Spitzer, & Williams, 2003), season data was collected, and housing development. We considered several social network attributes as potential covariates including network size, proportion of family members, children, women, race concordant, daily contact with ego, providing emotional support (e.g., encouragement), and providing material support (e.g., money; Supplemental Table S1, available with the article online). We selected these network variables based on previous literature (Bot et al., 2016; Feunekes, de Graaf, Meyboom, & van Staveren, 1998; Gallant, 2003; Pachucki, Jacques, & Christakis, 2011; Pollack et al., 2014).
We performed descriptive analyses of all variables. To evaluate whether clustering of dependent variables occurred by housing development, we calculated intraclass correlation coefficient (ρ; Singer, 1998). No substantial clustering existed (ρ < 0.10); therefore, we did not use multilevel models. We used multivariate logistic regression to examine the association of lifestyle behaviors with relevant network exposures, which were adjusted for age, gender, BMI, and housing development (given theoretical and/or statistical potential as confounders (Supplemental Table S2, available with the article online; Aral & Nicolaides, 2017; Diez Roux, 2001; Feunekes et al., 1998; Liu et al., 2003; Wakimoto & Block, 2001). For the exploratory exposure–response analyses, we calculated predicted probabilities using the results of the adjusted logistic regression models. In sensitivity analyses, we conducted logistic regression adjusted for all the previously mentioned covariates as well as history of hypertension, diabetes mellitus, and network exposures to daily contact and material support, given their statistical significance in bivariate analyses (Supplemental Table S2, available with the article online). Because these results did not differ from the original analyses, we present only the main results. We used STATA (College Station, TX) to perform all analyses.
Results
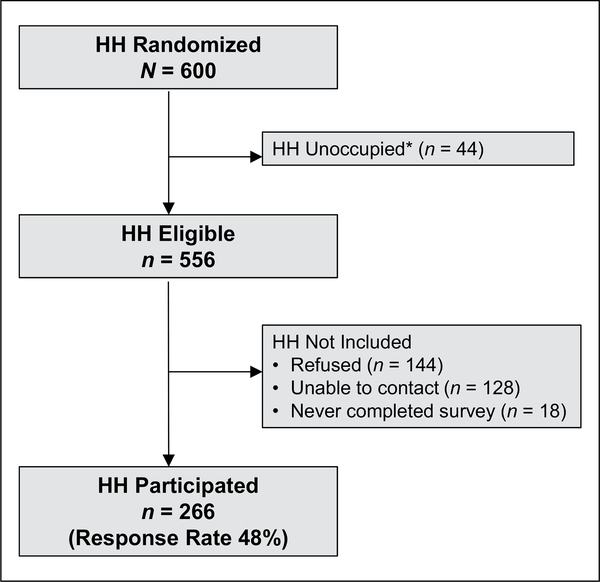
Overall, 266 heads of household (egos) participated out of the 556 eligible (47.8%; Figure 1). Participants’ mean age was 44.5 years, most were women (86.1%), and African American (95.5%; Table 1). Mean BMI was 32.6 kg/m2, and hypertension was common (56.8%). While we do not have access to demographic information of nonresponding, eligible households, our sample characteristics are similar for other studies of public housing residents in Baltimore City (Ludwig et al., 2011). Egos named a median of 15 network members (range 6–21). Only 18 participants (6.8%) reported characteristics on less than 10 network members, as they were unable to name 10 people in their network. On average, networks were composed mostly of family members (57.1%), women (61.7%), and individuals who were race concordant with the ego (94.0%; Table 1). Egos had daily contact with most network members (62.7%). Only 34.7% of network members provided material support to the ego.
Figure 1.
Recruitment of study sample. The figure displays the recruitment of our study sample from public housing developments in Baltimore, Maryland, from August 2014 to August 2015.
Note. HH = household. *Study team members inspected each randomized household during an in-person neighborhood inspection. Households with boarded up doors or external padlocks were considered unoccupied, and therefore, ineligible.
Table 1.
Characteristics of Study Sample.
| Characteristic | Head of household sample (N = 266) |
|---|---|
| Attributes of egos | |
| Age in years, M (SD) | 44.5 (12.4) |
| Women | 86.1% |
| African American race | 95.5% |
| High school graduate or equivalent | 66.2% |
| Unemployed | 33.5% |
| Food insecurea | 67.3% |
| Current cigarette smoker | 63.2% |
| BMI in kg/m2, M (SD) | 32.6 (10.1) |
| Self-reported history of hypertension | 56.8% |
| Self-reported history of diabetes mellitus | 19.9% |
| Depressive symptomsb | 47.0% |
| Season when data were collectedc | |
| Spring | 18.4% |
| Summer | 39.5% |
| Fall | 25.2% |
| Winter | 16.9% |
| Perceived attributes of social networks | |
| Small network size (<10 alters named) | 6.8% |
| % Family members, M (SD) | 57.1 (27.6) |
| % Children, M (SD) | 10.4 (13.0) |
| % Women, M (SD) | 61.7 (16.6) |
| % Race concordant with ego, M (SD) | 94.0 (20.1) |
| % Daily contact with ego, M (SD) | 62.7 (31.3) |
| % Providing emotional support, M (SD) | 64.3 (33.3) |
| % Providing material support, M (SD) | 34.7 (30.7) |
| % Living in the housing development, M (SD) | 19.0 (20.7) |
Note. BMI = body mass index.
Food insecurity assessed by two-item screener (Hager et al., 2010).
Depressive symptoms assessed by Patient Health Questionnaire–2 screener (Kroenke, Spitzer, & Williams, 2003).
Spring defined as March to May; Summer as June to August; Fall as September to November; Winter as December to February.
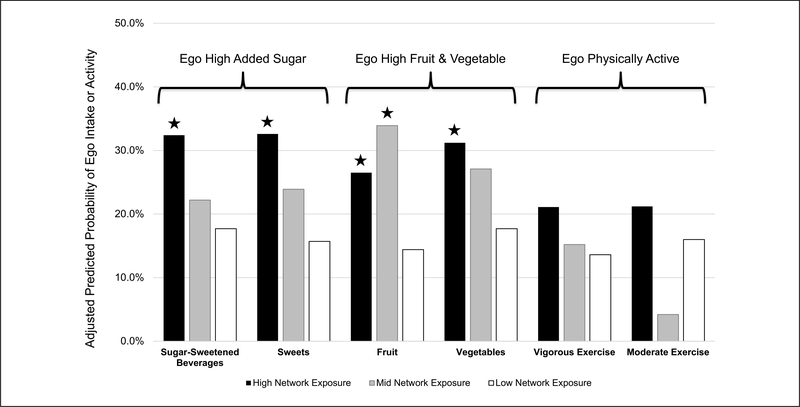
Egos’ median added sugar intake was 21.1 tsp/day (interquartile range [IQR] = 11.7–39.9), and their median fruit/ vegetable intake was 3.8 servings/day (IQR = 2.6–6.1). Overall, 24.8% met our criteria for high sugar intake (≥39.9 tsp/day) and 25.6% for high fruit/vegetable intake (≥6.1 servings/day). Egos’ perceived that 35.2% (SD = 35.6) of their networks consumed sugar-sweetened beverages daily, 28.4% (SD = 35.0) ate sweets daily, 23.1% (SD = 30.0) ate fruits daily, and 34.8% (SD = 37.6) ate vegetables daily. As the proportion of network members perceived to daily drink sugar-sweetened beverages increased by 10%, the odds that egos’ had high daily added sugar intake was statistically greater in multivariate adjusted analyses (odds ratio [OR] = 1.10, 95% confidence interval [CI] [1.02, 1.20], p = .02). Similarly, as the proportion of network members perceived to daily eat sweets increased by 10%, the odds that egos’ had high daily added sugar intake was statistically greater (OR = 1.13, 95% CI [1.05, 1.23], p < .01). There was no significant association between egos’ fruit/vegetable intake and the perceived network exposure to daily fruit (OR = 1.08, 95% CI [0.98, 1.18], p = .13) or vegetable intake (OR = 1.05, 95% CI [0.99, 1.11], p = .08). Figure 2 shows the results of our exposure–response analyses. The probability of having a high added sugar intake increases with increasing network exposure to sugar-sweetened beverages and sweets, which is significantly different between the high and low groups. There was also an exposure–response relationship for network exposure to vegetable intake (Figure 2), where the high group was significantly different from the low group. Both high and mid network exposures to fruit intake was significantly associated with ego high fruit/vegetable intake compared with the low group.
Figure 2.
Adjusted predicted probability of ego high added sugar, high fruit and vegetable intake, or physical activity by level of related network exposures to perceived behaviors.
Note. Predicted probabilities were calculated using results from logistic regression model adjusted for age, gender, body mass index, and housing development. Each network exposure is categorized as “high” to represent the upper quartile, “mid” the median to upper quartile, and “low” less than the median based on our sample’s distributions. The group of columns on the left represent the probability of egos’ high added sugar intake (≥39.9 tsp/day) by levels of network exposure to sugar-sweetened beverages and sweets. The group of columns in the middle represent the probability of egos’ high fruit and vegetable intake (≥6.1 servings/day excluding fried potatoes) by levels of network exposure to fruits and vegetables. The group of columns on the right represent the probability of egos’ being physically active (high or moderate level of activity) by levels of network exposure to weekly vigorous and weekly moderate exercise. Stars indicate that the value for this group is significantly different from the low network exposure group (p < .05). Data collected from public housing residents in Baltimore, Maryland, from August 2014 to August 2015.
Overall, 19.9% of egos met our criteria for high physical activity. On average, egos’ perceived that 27.4% (SD = 29.8) of their networks exercised vigorously at least once a week and 56.8% (SD = 37.4) of their networks exercised moderately at least once a week. As the proportion of network members perceived to vigorously exercise weekly increased by 10%, the odds that egos were physically active was statistically greater in multivariate adjusted analyses (OR = 1.15, 95% CI [1.04, 1.28], p = .01). There was no significant association between egos’ physical activity and the perceived network exposure to weekly moderate exercise (OR = 1.03, 95% CI [0.95, 1.13], p = .46). Figure 2 shows that the probability of being physically active increases with increasing network exposure to weekly vigorous exercise; however, the difference between high and low network exposure groups was not statistically significant (p = .16). No exposure–response pattern existed for network exposure to weekly moderate exercise.
Discussion
In this study, we found an association between public housing residents’ and their networks’ daily consumption of high sugar foods. We only found statistically significant associations for fruit/vegetable intake in our exposure–response analyses, where egos’ had a greater probability of high fruit/ vegetable intake if their networks had higher levels of exposure to fruits or vegetables as compared to egos with the lowest network exposure. We found an association between individuals being physically active and networks’ weekly participation in vigorous, but not moderate, exercise.
Prior research suggests a link between social networks and obesity (Bahr et al., 2009; Christakis & Fowler, 2007); however, few studies have examined diet/exercise behaviors and social networks. Dietary intake is known to correlate among family members (Bot et al., 2016; Feunekes et al., 1998; Pachucki et al., 2011). Some network characteristics have been associated with healthier diets such as having more close-knit relationships and more friends who live nearby (Bot et al., 2016). A prior survey of public housing residents in Montgomery County, Maryland, found no relationship between the proportion of network members perceived to eat “junk food like chips, candy, soda, or French fries” or “a healthy diet, meaning they eat fruits and vegetables most days of the week” with the ego’s own dietary habits (Pollack et al., 2014). We found a significant relationship between egos’ high daily added sugar intake and network exposure to daily sugar-sweetened beverage and daily sweets intake, which is different from the previous lack of association with “junk food” (Pollack et al., 2014). We found a significant relationship between individuals’ and networks’ consumption of fruits/vegetables, but only when comparing the highest to the lowest levels. The previous study did not find an association with healthy diet (Pollack et al., 2014). Our study used a validated and more detailed assessment of egos’ dietary habits (NHIS 5-factor dietary screener) than this prior study, as well as more specific measures of perceived dietary intake among network members (Supplemental Table S1, available with the article online). These differences in measures may contribute to the different findings between the two studies. Differences in the context may also contribute—Montgomery County has a higher socioeconomic status and more resources than Baltimore City, and Montgomery County public housing residents tended to be living in closer proximity to wealthier neighbors. Based on our results, future network interventions might consider targeting reduction of high sugar foods, particularly among public housing residents living in communities similar in economic status to Baltimore City.
We found a significant relationship between egos’ being physically active and network exposure to weekly vigorous exercise, but not moderate exercise in the network. A recent study of an online social network observed that running was socially contagious and varied by activity level and gender between friends (Aral & Nicolaides, 2017). In contrast, the prior network study among Montgomery County public housing residents did not find a significant relationship between egos’ being physically active and their network exposure to exercise (Pollack et al., 2014). Again, differences in measures used and differences in context noted above may contribute to the different findings between the studies of public housing residents. Future studies might consider adding objectively measured physical activity assessments rather than self-report to strengthen the evidence base. Also, our results suggest that future network interventions focus on promoting vigorous exercise, particularly among public housing residents living in communities similar in economic status to Baltimore City.
Several explanations for the associations that we observed exist including homophily, shared context, or social network influence (Christakis & Fowler, 2013). Homophily, which is the phenomenon that people with similar characteristics tend to cluster together, could explain our results. Homophily may suggest that particular social networks are important sites for interventions, such as targeting reduction of sugar-sweetened beverage or sweets among homophilous groups. Shared context is the idea that network members jointly experience unobserved exposures that cause their attributes to vary similarly. The differences that we saw between our study of public housing residents and the prior study of Montgomery County public housing residents may be explained by differences in context between these two groups, such as socioeconomic status and proximity to wealthier neighbors. Finally, social network influence may explain our results. In general, social networks influence behavior through social norms and behavior modeling (Bandura, 1986). Prior studies have found social networks may influence outcomes among participants in behavioral weight loss trials. Being part of a network with stronger social norms for unhealthy eating is associated with significantly less weight loss (Leahey, Doyle, Xu, Bihuniak, & Wing, 2015). African American and Hispanic adults have achieved greater weight loss if they reported having a child help with eating goals or coworker help with physical activity (Winston et al., 2015). Given that we found associations between individuals’ and networks’ consumption of high added sugar foods and vigorous exercise, our results may suggest that these behaviors may hold promise as targets for future social network interventions. A prior trial found no significant difference in weight loss between African Americans in a group assigned to specifically enroll with a network member as compared to a group without this support (Kumanyika et al., 2009). However, enrolling with others was associated with greater weight loss when the network member participated more and lost more weight. Therefore, future network interventions may need to target change and participation from both egos and alters to have a greater effect on behavior change.
Overall, we found that public housing residents’ diets do not meet recommendations for limitations on added sugar or promotion of fruit/vegetable intake. The American Heart Association (AHA) recommends that adults limit their added sugar intake to 6 to 9 teaspoons per day (AHA, 2017a), where the median intake in our sample was over 21 teaspoons daily. Both African American and low-income populations typically have higher intakes of added sugars (Thompson et al., 2009). The prior survey of Montgomery County public housing residents reported 58% of clustered public housing residents drank at least one sugar-sweetened beverage daily (Pollack et al., 2014). With respect to fruit/vegetable intake, the AHA recommends that adults have 8 to 10 servings of fruits/vegetables per day (AHA, 2017b). The median intake in our sample was 3.8 servings daily. Results from Behavioral Risk Factor Surveillance System data have found that few African Americans have five or more servings of fruit/vegetables daily (Kruger et al., 2007). The prior survey of Montgomery County public housing residents reported 27% had adequate fruit/vegetable intake (Pollack et al., 2014).
We also found that few residents were physically active (<20%), which is lower than prior rates reported for regular activity levels among a national sample of African Americans (45.9% for men and 36.3% for women; Kruger et al., 2007) and among Montgomery County public housing residents (43%; Pollack et al., 2014). This difference between Baltimore City and Montgomery County public housing residents is striking and may suggest that the environmental differences (e.g., higher socioeconomic status and lower crime in Montgomery County) have substantial effects on exercise. Lower income, non-White communities like Baltimore City often lack recreation facilities and have environments not conducive to exercise (Gordon-Larsen et al., 2006). Season could affect exercise (Aral & Nicolaides, 2017); however, we found no significant differences in bivariate analyses.
This study has several limitations. First, our sample was predominantly low-income African Americans from two public housing developments in Baltimore, which may limit our findings’ generalizability. Second, the response rate to our survey was 48%, although previous response rates have varied from 18% to 84% among public housing residents (Heinrich et al., 2008; Ludwig et al., 2011; Pollack et al., 2014). We do not have information on nonresponders; our sample’s characteristics were similar to those reported in the “Moving to Opportunities” project (Ludwig et al., 2011). Third, our egocentric network approach assessed perceptions rather than actual behaviors of network members, and the perceptions might differ by how often observed they were by the ego within the last year. Perceptions of network members’ behaviors are theorized to be meaningful and have implications for egos’ behavior, regardless of whether or not they are accurate (Israel, 1982). The alters’ behaviors that we assessed are easily observed by egos, which may improve their perceptions’ accuracy (Green, Hoover, Wager, Ryan, & Ssegujja, 2014), although bias may influence perceptions as respondents might desire that their networks share similar behaviors to their own. Fourth, we only ascertained perceived habits on a subset of network members rather than a participant’s whole network, which could attenuate associations. We relied on the software to select this subset at random to minimize this attenuation, although this effect could persist. Fifth, we used the NHIS five-factor dietary screener, which is a shorter and less comprehensive measure of dietary intake relative to instruments such as a 24-hour dietary recall or food frequency questionnaire. We selected this abbreviated instrument based on feedback from community members during pilot testing. We were thus unable to determine overall dietary attributes such as calorie intake. Finally, the cross-sectional design prevents us from determining casual associations or distinguishing between homophily and social network influence.
In conclusion, few Baltimore City public housing residents meet recommendations for healthy diet and physical activity. The characteristics of their social networks are linked with both unhealthy and healthy behaviors, as we saw associations with network exposure to high sugar foods and network exposure to vigorous exercise. Future research might consider engaging residents in the context of their social networks to decrease sugar-sweetened beverages, or conversely, recruiting residents and their social networks to increase vigorous physical activity.
Supplementary Material
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: KAG was supported by a career development award from the National Heart, Lung, and Blood Institute (K23HL116601). The study was also supported by small grants from the Johns Hopkins Osler Center for Clinical Excellence and the Johns Hopkins Urban Health Institute.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental Tables S1 and S2 are available with the online version of this article at http://journals.sagepub.com/home/heb.
References
- Ainsworth BE, Jacobs DR, & Leon AS (1993). Validity and reliability of self-reported physical activity status: The Lipid Research Clinics questionnaire. Medicine & Science in Sports & Exercise, 25, 92–98. [DOI] [PubMed] [Google Scholar]
- American Heart Association. (2017a). Added sugars. Retrieved from http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Nutrition/Added-Sugars_UCM_305858_Article.jsp#.WMbunBiZNBw
- American Heart Association. (2017b). Suggested servings from each food group. Retrieved from https://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/HealthyDietGoals/Suggested-Servings-from-Each-Food-Group_UCM_318186_Article.jsp?appName=MobileApp
- Aral S, & Nicolaides C (2017). Exercise contagion in a global social network. Nature Communications, 8, 14753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahr DB, Browning RC, Wyatt HR, & Hill JO (2009). Exploiting social networks to mitigate the obesity epidemic. Obesity (Silver Spring), 17, 723–728. [DOI] [PubMed] [Google Scholar]
- Bandura A (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- Bot SD, Mackenbach JD, Nijpels G, & Lakervald J (2016). Association between social network characteristics and lifestyle behaviors in adults at risk of diabetes and cardiovascular disease. PLoS One, 11, e0165041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castor D, Pilowsky DJ, Hadden B, Fuller C, Ompad DC, de Leon CL, . . . Hoover DR (2010). Sexual risk reduction among non-injection drug users: Report of a randomized controlled trial. AIDS Care, 22, 62–70. [DOI] [PubMed] [Google Scholar]
- Christakis NA, & Fowler JH (2007). The spread of obesity in a large social network over 32 years. New England Journal of Medicine, 357, 370–379. [DOI] [PubMed] [Google Scholar]
- Christakis NA, & Fowler JH (2008). The collective dynamics of smoking in a large social network. New England Journal of Medicine, 358, 2249–2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis NA, & Fowler JH (2013). Social contagion theory: Examining dynamic social networks and human behavior. Statistics in Medicine, 32, 556–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb NK, Graham AL, & Abrams DB (2010). Social network structure of a large online community for smoking cessation. American Journal of Public Health, 100, 1282–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen-Cole E, & Fletcher JM (2008). Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic. Journal of Health Economics, 27, 1382–1387. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV (2001). Investigating neighborhood and area effects on health. American Journal of Public Health, 91, 1783–1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douketis JD, Macie C, Thabane L, & Williamson DF (2005). Systematic review of long-term weight loss studies in obese adults: Clinical significance and applicability to clinical practice. International Journal of Obesity (2005), 29, 1153–1167. [DOI] [PubMed] [Google Scholar]
- Feunekes GIJ, de Graaf C, Meyboom S, & van Staveren WA (1998). Food choice and fat intake of adolescents and adults: Associations of intakes within social networks. Preventive Medicine, 27, 645–656. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Kruszon-Moran D, Carrol MD, Fryar CD, & Ogden CL (2016). Trends in obesity among adults in the United States, 2005–2014. JAMA Journal of the American Medical Association, 315, 2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallant MP (2003). The influence of social support on chronic illness self-management: A review and directions for research. Health Education & Behavior, 30, 170–195. [DOI] [PubMed] [Google Scholar]
- Gittelsohn J, Song HJ, Suratkar S, Kumar MB, Henry EG, Sharma S, . . . Anliker JA (2010). An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Education & Behavior, 37, 390–402. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, & Popkin BM (2006). Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics, 117, 417–424. [DOI] [PubMed] [Google Scholar]
- Green HD, Hoover MA, Wager GJ, Ryan GW, & Ssegujja E (2014). Measuring agreement beween egos and alters: Understanding informant accuracy in personal network studies. Field Methods, 26, 126–140. [Google Scholar]
- Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, . . . Frank DA (2010). Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics, 126, e26–e32. [DOI] [PubMed] [Google Scholar]
- Heinrich KM, Lee RE, Regan GR, Reese-Smith JY, Howard HH, Haddock CK, . . . Ahluwalia JS (2008). How does the built environment related to body mass index and obesity prevalence among public housing residents? American Journal of Health Promotion, 22, 187–194. [DOI] [PubMed] [Google Scholar]
- Israel BA (1982). Social networks and health status: Linking theory, research, and practice. Patient Counselling and Health Education, 4, 65–79. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2003). The Patient Health Questionnaire-2: Validity of a two-item depression screener. Medical Care, 41, 1284–1292. [DOI] [PubMed] [Google Scholar]
- Kruger J, Yore MM, Solera M, & Moeti R (2007). Prevalence of fruit and vegetable consumption and physical activity by race/ethnicity: United States, 2005. MMWR Morbidity and Mortality Weekly Report, 56, 301–304. [PubMed] [Google Scholar]
- Kumanyika SK, Wadden TA, Shults J, Fassbender JE, Brown SD, Bowman MA, . . . Wu X (2009). Trial of family and friend support for weight loss in African American adults. Archives of Internal Medicine, 169, 1795–1804. [DOI] [PubMed] [Google Scholar]
- Larsen NI, Story MT, & Nelson MC (2009). Neighborhood environments: Disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine, 36, 74–81. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Sherman S, & Knowlton A (2003). HIV prevention among drug users: Outcome of a network-oriented peer outreach intervention. Health Psychology, 22, 332–339. [DOI] [PubMed] [Google Scholar]
- Leahey TM, Doyle CY, Xu X, Bihuniak J, & Wing RR (2015). Social networks and social norms are associated with obesity treatment outcomes. Obesity (Silver Spring), 23, 1550–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Willett WC, Manson JE, Hu FB, Rosner B, & Colditz G (2003). Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middle-aged women. American Journal of Clinical Nutrition, 78, 920–927. [DOI] [PubMed] [Google Scholar]
- Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, . . . McDade TW (2011). Neighborhoods, obesity and diabetes: A randomized social experiment. New England Journal of Medicine, 365, 1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty C, Killworth PD, & Rennell J (2007). Impact of methods for reducing respondent burden on personal network structural measures. Social Networks, 29, 300–315. [Google Scholar]
- National Cancer Institute. (2005). Five-factor screener in the 2005 National Health Interview Survey cancer control supplement. Retrieved from http://epi.grants.cancer.gov/nhis/5factor/
- Office of Disease Prevention and Health Promotion. (2008). Physical activity guidelines for Americans. Retrieved from https://health.gov/paguidelines/guidelines/
- Pachucki MA, Jacques PF, & Christakis NA (2011). Social network concordance in food choice among spouses, friends, and siblings. American Journal of Public Health, 101, 2170–2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack CE, Green HD, Kennedy DP, Griffin BA, Kennedy-Hendricks A, Burkhauser S, & Schwartz H (2014). The impact of public housing on social networks: A natural experiment. American Journal of Public Health, 104, 1642–1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Slater S, Mirtcheva D, Bao Y, & Chaloupka FJ (2007). Food store availability and neighborhood characteristics in the United States. Preventive Medicine, 44, 189–195. [DOI] [PubMed] [Google Scholar]
- Singer JD (1998). Using SAS PROC MIXED to fit multilevel models, hierachical models, and individual growth models. Journal of Educational and Behavioral Statistics, 24, 323–355. [Google Scholar]
- Stack C (1975). All our kin: Strategies for survival in a black community. New: York, NY: Harper & Row. [Google Scholar]
- Thompson FE, McNeel TS, Dowling EC, Midthune D, Morrissette M, & Zeruto CA (2009). Interrelationships of added sugars intake, socioeconomic status, and race/ethnicity in the United States: National Health Interview Survey 2005. Journal of the American Dietetic Association, 109, 1376–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Kuramoto SJ, Davey-Rothwell MA, & Latkin CA (2011). The STEP into action study: A peer-based, personal risk network-focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction, 106, 366–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Housing and Urban Development. (2015). Picture of subsidized households. Retrieved from https://www.huduser.gov/portal/datasets/picture/yearlydata.html
- Wakimoto P, & Block G (2001). Dietary intake, dietary patterns and changes with age: Epidemiological perspective. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 56A, 65–80. [DOI] [PubMed] [Google Scholar]
- Winston GJ, Phillips EG, Wethington E, Devine C, Wells M, Peterson JC, . . . Charlson M (2015). Social network characteristics associated with weight loss among black and Hispanic adults. Obesity (Silver Spring), 23, 1570–1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.