Short abstract
Objectives
This study aimed to identify, assess and summarize available scientific evidence on tailored text messaging interventions focused on type 2 diabetes self-management. The systematic review concentrated on message design and delivery features, and tailoring strategies. The meta-analysis assessed the moderators of the effectiveness of tailored text messaging interventions.
Methods
A comprehensive search strategy included major electronic databases, key journal searches and reference list searching for related studies. PRISMA and Cochrane Collaboration's guidelines and recommended tools for data extraction, quality appraisal and data analysis were followed. Data were extracted on participant characteristics (age, gender, ethnicity), and interventional and methodological characteristics (study design, study setting, study length, choice of modality, comparison group, message type, format, content, use of interactivity, message frequency, message timing, message delivery, tailoring strategies and theory use). Outcome measures included diet, physical activity, medication adherence and glycated hemoglobin data (HbA1C). Where possible, a random effects meta-analysis was performed to pool data on the effectiveness of the tailored text messaging interventions and moderator variables.
Results
The search returned 13 eligible trials for the systematic review and 11 eligible trials for the meta-analysis. The majority of the studies were randomized controlled trials, conducted in high-income settings, used multi-modalities, and mostly delivered informative, educational messages through an automated message delivery system. Tailored text messaging interventions produced a substantial effect (g = 0.54, 95% CI = 0.08–0.99, p < 0.001) on HbA1C values for a total of 949 patients. Subgroup analyses revealed the importance of some moderators such as message delivery (QB = 18.72, df = 1, p = 0.001), message direction (QB = 5.26, df = 1, p = 0.022), message frequency (QB = 18.72, df = 1, p = 0.000) and using multi-modalities (QB = 6.18, df = 1, p = 0.013).
Conclusions
Tailored mobile text messaging interventions can improve glycemic control in type 2 diabetes patients. However, more rigorous interventions with larger samples and longer follow-ups are required to confirm these findings and explore the effects of tailored text messaging on other self-management outcomes.
Keywords: Text messaging, type 2 diabetes, systematic review, meta-analysis, tailoring, message design, health behavior, self-management
Introduction
The rapid growth of type 2 diabetes in the world is a serious concern.1 Type 2 diabetes is a life-threatening condition, but it is possible to prevent the development of illness, delay or even reverse its complications through effective diabetes management.2 Because the major part of diabetes management (nearly 95%) is executed by the patients,3 it is highly critical to increasing patients’ self-management skills. More often, mobile health technologies (mHealth) are being used to provide support to these patients who often fail to follow traditional self-management practices.4,5 Particularly, mobile text messaging offers customized, cost-effective and convenient support and can help patients to track their medical and behavioral outcomes continuously.6
Despite the expanding use of mobile text messaging, there is still a lack of knowledge on the optimal way to create and deliver mobile text messages that could stimulate behavior change.7–11 Previous research so far provided mixed evidence for the moderators of the effective text messaging interventions such as frequent messaging,12,13 infrequent messaging,14 one-way messaging,13,14 two-way messaging8 and using multi-modalities (text messaging, WEB portal, assessment devices, etc.).12,15,16 There were also studies revealing no effects of some moderators, such as message direction (whether one-way or two-way messaging)7 or choice of modality (whether text messaging only or text messaging plus).14
The limited space and design opportunities provided by mobile text messaging may also make it difficult to craft effective messages for behavior change. Using different message design elements such as message appeal (e.g. fear, guilt, humor), message tone (e.g. authoritarian vs. friendly, directive vs. passive), message format (e.g. textese) or use of evidence (e.g. statistical evidence, testimonial evidence) persuasively might create important differences in receivers’ message involvement, message receptivity and message retention.17–19 Previous research20 also demonstrated that health messages can be framed to emphasize either the benefits of performing a specific behavior (a gain-frame) or the costs of not performing a specific behavior (a loss-frame). Gain-framed messages are more associated with prevention behaviors, while loss-framed messages are more appropriate to detection behaviors.
According to Elaboration Likelihood Model,21 the messages including personally relevant features increase one’s motivation and ability to elaborate on the message content, enhance his/her involvement with the message and thereby increase persuasion. Rather than providing a standard self-management program for patients with type 2 diabetes, tailoring the intervention message and delivery based on their psychosocial needs (e.g. awareness, perceived risk, self-efficacy), their performance (e.g. providing individual feedback), preferences (e.g. time and frequency of messages) or demographics (e.g. young Latino-American women) could be an effective way of changing behavior and its maintenance.2,7,12,14 For example, text messaging interventions targeted at young people and children were more successful if they were using personalized messages (e.g. using the child’s name), using informal short message services (SMS) content and texts (e.g. “ur goal is 2 eat less sugary things 2 get ur blood down!”).22
The Transtheoretical Model (TTM) has frequently been used in interventions to address the specific needs and expectations of patients in different stages of behavior change.23 For example, in a text messaging intervention, message content can be tailored to eliminate the barriers at the initial pre-contemplation stage or reward the desired behavior for patients in the latter action stage.
The Health Belief Model (HBM) has also been used for tailoring messages and other components in behavior change interventions. The HBM assumes that the perceptions of the threat coming from a health problem and the benefits of avoiding the risk influence one’s readiness to act.23 If messages are specifically designed to target individual characteristics, perceived barriers, perceived benefits, perceived susceptibility, cues to action and self-efficacy, they can induce behavior change. Tailoring on 4-5 theoretical constructs can be more effective than tailoring on fewer theoretical constructs (0–3).18 Computer-tailored interventions were effective on health behavior change,24,25 but there is a lack of knowledge in tailoring message design and delivery mode and other intervention components in these interventions.24
Previously, tailoring was considered as a “unitary construct” as opposed to either personalized and/or standardized messages.13–15 However, different types of tailoring strategies with changing effects on behavior are available, and personalization is also a form of tailoring.26–28 Personalization frames the information to create a perception in the participants as if the message is specifically designed for them, and it is not specifically related to the content of the message. Using the name or other identifiers of participants such as age or ethnicity while delivering a generic message could increase the message’s persuasiveness. Another commonly applied tailoring strategy is Feedback. It includes providing descriptive, comparative and evaluative messages to participants about their psychological and behavioral conditions during the intervention. Content-matching is an advanced level of tailoring where key theoretical constructs are used to match personal needs, goals and interests of participants. It can be used to guide patients as they move through different stages of behavior change.26,27 Especially in the age of computer-tailored interventions where employing different types and combinations of tailoring are possible, there is a strong need for understanding which type of tailoring strategies and message-specific elements are more important in a specific context and for a specific group of people.
Various demographic, medical, motivational and behavioral factors can influence type 2 diabetes self-management.29–31 Therefore, it is necessary to understand the underlying mechanism of tailoring for patients with type 2 diabetes. To our knowledge, no existing reviews of mobile text messaging in the area of type 2 diabetes management have focused on tailored interventions and synthesizing the evidence for the optimal tailoring strategies, message design and delivery features in these interventions. Hence, the main purposes of this systematic review and meta-analysis were (a) to identify, assess and summarize available scientific evidence for tailored mobile text messaging interventions focused on type 2 diabetes self-management, (b) to examine the characteristics of tailored interventions by concentrating on their message design features, tailoring strategies and message delivery features, (c) to explore a link between tailoring strategies and self-management outcomes which were specified as glycated hemoglobin monitoring (HbA1C), diet, physical activity and medication adherence, (d) to assess the effect of tailored mobile text messaging interventions on specified type 2 diabetes self-management outcomes and (e) to identify the moderators of the effectiveness of the interventions to define the optimal tailored mobile messaging strategies and intervention characteristics for type 2 diabetes self-management.
Method
The systematic review and meta-analysis were planned, conducted and reported according to the process described in the Methodological Expectations of Cochrane Intervention Reviews (MECIR)32 and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.33
Inclusion/exclusion criteria
Eligible interventions were tailored randomized trials focused on type 2 diabetes self-management via mobile phone-based text messaging that involved the delivery of behavior change content through SMS, multimedia message services (MMS) or instant messaging (i.e. WhatsApp). The interventions that used at least one type of tailoring variables such as personalized message or feedback on behavior and included a non-tailored control/comparison group were considered. To be able to include all the relevant studies, no additional filter was applied to limit study participants regarding ethnicity, age, religion, occupation, income or any other demographic variables. No specific time limit was applied either. Table 1 presents the eligibility criteria developed for considering the studies in the systematic review.
Table 1.
Eligibility criteria for considering the studies in the review.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Types of studies | • Randomized trials• Written in English | Unpublished studies, conference abstracts/posters |
| Types of participants | • People with type 2 diabetes• The studies with a mixed population, such as individuals with type 1 and type 2 diabetes were only considered if separate data for type 2 diabetes patients were provided | • Interventions that focused on patients with type 1 diabetes or gestational diabetes or diabetic retinopathy• The studies whose participants included healthcare providers or other stakeholders rather than patients or consumers of health care services |
| Types of interventions | • Mobile phone-based text messaging interventions that involved the delivery of behavior change content through short message services (SMS), multimedia message services (MMS) or instant messaging using mobile messaging apps like WhatsApp• Interventions that used at least one type of tailoring variable such as personalized message or feedback on behavior• Interventions including a non-tailored control/comparison group | • Mobile app or web-based interventions without any mobile-phone-based text messaging component to deliver behavior change messages• The studies delivered generic (standard) messages or only included the appointment and simple medication reminders (prompts) or instructions for medication use (i.e. insulin dose adjustment) • The studies used audio or voice message (including Interactive Voice Response (IVR) messages) without using any mobile text messaging component• The interventions delivered generic (standard) messages• The studies whose messages included only the appointment and simple medication reminders (prompts) or instructions for medication use (i.e. insulin dose adjustment) |
| Types of outcomes | • At least one of the measures of self-management behaviors described by Diabetes Canada2 diet (including nutrition, healthy eating, calorie intake), physical activity, medication adherence or glycated hemoglobin monitoring (HbA1C) | • Clinical measures other than HbA1C, and attitudinal and behavioral variables related to intervention development or process/implementation evaluations such as usability, feasibility and cost-effectiveness |
Search strategy
A comprehensive search strategy was conducted between 18 and 29 January 2018. The search strategy included major electronic database searches, key journal searches and hand searches of reference lists from recent systematic reviews and meta-analyses (Appendix I). Combinations of key terms, MeSH terms and CINAHL subject headings were searched across the selected electronic databases (Appendix II). The PubMed search strategy, which was modified for other databases, is provided in Appendix III.
Selecting studies and collecting data
Search results from different sources were exported to the Zotero 5.0 Citation Manager34 where duplicates were removed, and the titles and abstracts of the remaining citations were examined against the eligibility criteria. In cases where the abstracts were not available or explanatory, full-text reviews were conducted to assess the eligibility of the studies. Further, full-texts of all the studies that passed the initial title–abstract screening were scrutinized.
Using a structured form adapted from the Cochrane Handbook for Systematic Reviews of Interventions,32 data were extracted on a number of variables including participants’ characteristics, interventional and methodological components (Table 2). Tailoring strategies were identified using the guideline developed based on Noar and Harrington (2016),26 Dijkstra (2016)27 and Hawkins et al. (2008).28 The guideline (Appendix IV) includes detailed descriptions and examples of each tailoring strategy. For the classification of trial setting (high-income or low- and middle-income country setting), the World Bank’s country classification was used.35
Table 2.
Variables examined in the reviewed studies.
| Participants’ characteristics |
|
| Interventional and methodological components |
|
| Intervention outcomes |
|
The first author and two reviewers with a doctorate and masters level qualifications and specific research interests in mobile communication and behavior change worked independently during the screening, assessment and data extraction processes. Any disagreement was discussed until consensus was reached and the reasons for excluded studies were recorded.
Assessing risk of bias
The methodological validity and risk of bias in the selected studies were checked based on the Cochrane Handbook for Systematic Reviews of Interventions.32 If available, study protocols and trial registry sites were examined to improve the judgment on the bias. The first author and the reviewer independently assessed the risk of bias in the studies and discussed any discrepancies until consensus was reached. The risk was judged as high, low and unclear, and the rationale for each judgment was recorded.
Data synthesis and analysis
Quantitative data, where possible, were pooled in a statistical meta-analysis to estimate the size of the effects of tailored interventions in the outcomes of mobile text messaging interventions on type 2 diabetes management.
For categorical data, odds ratio and for continuous data, weighted mean differences and confidence intervals (95%) were selected to express the effect sizes. Random effects meta-analytical procedures were followed. Effect sizes were weighted by their inverse variance weight in calculating mean effect sizes. As an estimate of the effect size for each study, Hedges g was used.36 The effect sizes 0.20, 0.50 and 0.80 are used as a threshold for the effect sizes of small, medium and large, respectively.37 Based on the findings of the previous text messaging reviews,14–15 a small to moderate effect of the tailored text messaging interventions on type 2 diabetes self-management outcomes was expected.
Following the Cochrane guideline,32 the mean, standard deviation (SD), and the number of participants in the intervention and control groups of the last follow-up measurement from each study and for each outcome were collected. Authors were contacted if related data were missing in the studies. Some datasets38 were derived from another review,7 and necessary calculations were made by the formula provided in the Cochrane Handbook32 using the same correlation coefficient (0.5) (please see the Supplementary Note). The data provided as median and range were converted into a mean and SDs based on the estimates provided by Hozo et al. (2005).39
Publication bias analysis was performed to assess the robustness of results by applying funnel plot asymmetry test and using “trim-and-fill” method. Egger Regression and Begg and Mazumdar Rank Correlation tests40 were also performed to detect any possible bias in the data. Heterogeneity was assessed statistically using the I2 statistic, where I2 >50% was accepted as the indicator of substantial heterogeneity.32 For pre-specified 11 moderators (Appendix V), subgroup analyses were performed to examine potential sources of heterogeneity, and Cochrane Q statistic was used to identify statistically significant differences between interventions.
A software program (Meta-Essentials 1.2)40 was used to perform the meta-analysis. As a result of the impracticality of statistical pooling, the findings were presented in narrative form.
Results
The combined database searches returned 2187 records, and with 35 records from other sources, a total of 2222 records were collected. After duplicates were removed, 1598 records were screened for eligibility using title and abstract. A total of 127 articles were shortlisted for eligibility, and full-text screening resulted in 13 eligible trials for systematic review and 11 trials for meta-analysis. Appendix VI lists the excluded studies with their reasons. Search results are summarized in the PRISMA flow diagram (Figure 1).
Figure 1.
Study selection flow diagram based on the Preferred Reporting Item for Systematic Reviews and Meta-Analyses (PRISMA) guideline.
Some articles were evaluated together with their related studies (Arora et al. (2014)41 with Burner et al. (2013),42 Capozza et al. (2015)38 with Abebe et al. (2013),43 Fortmann et al. (2017)44 with Philis-Tsimikas et al. (2011),45 Gatwood et al. (2016)46 with Gatwood et al. (2014)47) to provide a more thorough assessment about their message content and tailoring strategies. Among the studies reported on the same trial, preliminary studies were excluded (e.g. Kim and Song (2008),48 Agboola et al. (201349) and final studies with the maximal treatment results were included (e.g. Kim and Kim (2008)50, Agboola et al. (2016)51, respectively).
Risk of bias
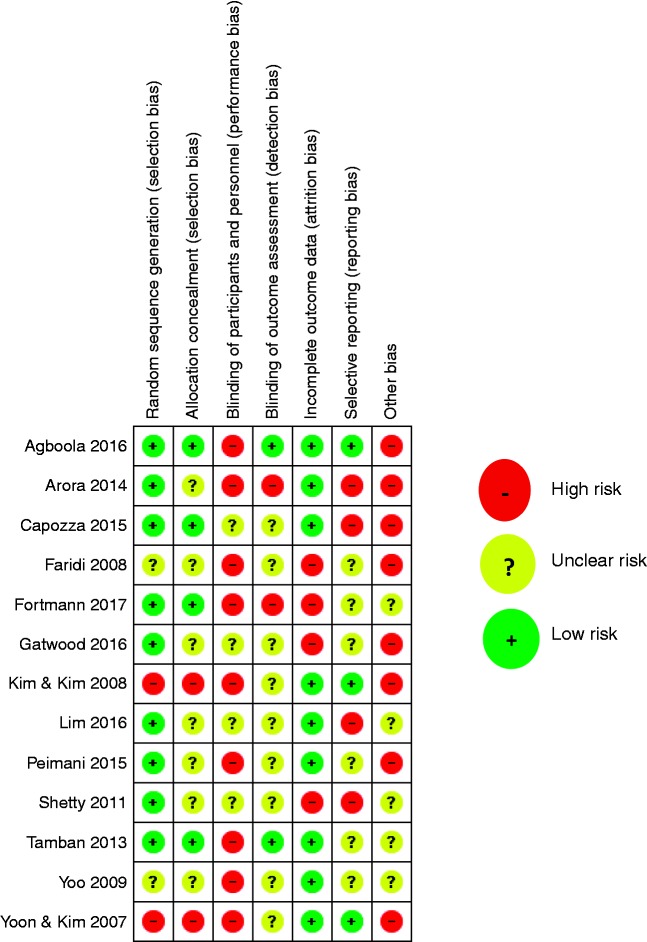
The most commonly observed high-risk bias was related to performance bias where blinding of participants and personnel to the intervention were often impossible due to the nature of the interventions. For example, when participants received pedometers, they were more likely to understand that the intervention related to physical activity. In the majority of the studies (62%, n = 8), there was a high risk of some other form of bias, mostly related to small sampling size and poor methodology. Figure 2 summarizes the risk of bias assessment for each included study and Figure 3 demonstrates the portion of each risk of bias, as low, unclear and high. Also, Appendix VII presents the detailed risk of bias estimates for each study and the rationale given for each judgment.
Figure 2.
Risk of bias summary: reviewers' judgments about each risk of bias item for each included study.
Figure 3.
Risk of bias presented as percentages across all included studies.
Characteristics of the included studies
All articles reported on only one trial. Eleven trials were randomized controlled trials (RCTs), whereas the remaining two used pre-test–post-test control group design.50,52 On average, length of intervention was 6.5 months. Ten trials were conducted in high-income settings, whereas three interventions were carried out in low- and middle-income settings. A total of 1.328 participants enrolled in these trials (mean = 102; range = 30 to 215). Each included only adult type 2 diabetes patients (51.2% female) and with a mean age ranging from 47 to 65 years of age and with HbA1C values at baseline ranging from 6.5 to 8%.
SMS text messaging was the primary mode of communication to deliver the intervention messages in all studies. Seven trials used multi-modalities (text messaging plus), whereas six trials either only used text messaging or combined it with usual care. Twelve studies provided usual care to their comparison groups, while four studies also provided usual care to their treatment groups. In four studies usual care included regular clinic visits and consults with a healthcare provider (i.e. endocrinologist, physician).
In all trials, message content included educational, behavioral and/or motivational features to induce behavior change. In general, messages were created based on the recommendations of reference institutions such as the American Diabetes Association. The intervention messages were not customized using the framing effect or any other message-specific elements (e.g. humor, fear, directive, passive tone).
Varying frequencies were used for the delivery of the messages in the trials. They were broadly grouped into two categories, as frequent messaging and infrequent messaging. Frequent messaging was conceptualized as sending at least one message per day, whereas infrequent messaging was described as sending three messages per week or less. Nine trials delivered messages frequently and four trials delivered messages infrequently.
Five studies implemented two-way messaging, while the remaining eight studies used one-way messaging. The majority of the interventions (n = 8) delivered automated messages which mostly included immediate feedback and recommendations provided by a decision algorithm in response to patients’ uploaded data, whereas in three studies tailored messages were sent directly from a health care provider or an investigator.
The personalization strategy employed in the interventions (n = 4) included adaptation of timing53 and number and frequency of messages41,50 based on participants’ preferences, identifying areas of specific interest in the self-management of diabetes and providing options to select message categories (i.e. diet or exercise-related messages)41,44,50 and presenting options for message language.41,44 Six studies employed psychosocial-behavioral tailoring. The messages included specific recommendations, reminders and feedback that matched with participants’ uploaded measurements or health records. Three studies38,47,51 demonstrated the use of all tailoring types in their intervention.
The use of theory was reported in only four studies.41,47,51,67 The Transtheoretical model, Health Belief Model, Self-determination Theory, Social Cognitive Theory and Information-Motivation-Behavioral Skills model were used to guide the tailoring of intervention components and message content in the interventions. Only one study47 employed multiple behavioral theories and used the Technology Acceptance Model for measuring the acceptability of text messaging. Table 3 presents the characteristics of the included studies in this systematic review.
Table 3.
Characteristics of the interventions included in the review.
| Study author name, year | Study/Design/Duration | Sample characteristics/Size (baseline); Female ratio/Age (baseline mean (SD))/Country: level of income | Intervention modality | Comparison | Message type/Format/Design features | Message Frequency/Timing/Delivery | Tailoring method & strategies | Use of theory |
|---|---|---|---|---|---|---|---|---|
| Agboola et al., 201651 | RCTParallel 2 arms6 months | Adults with T2D (HbA1C>7%)n = 126; 32.5% femaleAge: 51.45 (11.6) USA: High income | Pedometer, mobile phone text messaging, telephone reminders, web portal, and usual care | Pedometer, telephone reminders, web portal and usual care (No text messaging) | Two-way messagingSMS textTEXT to Move study:• Morning messages provided feedback based on the previous day’s activity• Afternoon and evening messages included coaching themes, such as support, health education, motivation and reminders to engage in healthy behaviors• Some of the interactive messages focused on satisfaction with the program, health status, knowledge of physical activity, food intake and medication adherence | At least two messages per day• Morning messages at9 a.m., EST on weekdays & 11 am EST on weekends• Evening messages at 6 p.m. ESTMessages were delivered automatically | Combination of personalization and Psychosocial-Behavioral TailoringBased on language preferences (English or Spanish) and demographic and behavioral information obtained at baseline, web portal content, training materials and text messaging were personalizedBehavioral feedback, and educational, motivational messages were sent to induce behavior changeExample: “as of 8:27 a.m., you were active for 45 mins yesterday which is 75% of your daily goal” | Transtheoretical ModelThe theory was used to assess participants’ stage of change and design the corresponding message content |
| Arora et al., 201441 | RCTParallel 2 arms6 months | Adults with T2D (HbA1C>8%)n = 128; 64% femaleAge: 50.7 (10.2) USA: High income | Mobile phone text messaging and usual care | Usual care | One-way messagingSMS textTExT-MED intervention:• Educational/motivational messages (1 per day)• Medication reminders (3 per week)• Challenge messages on healthy living (2 per week)• Trivia (2 per week) | 2 messages per dayat 9 a.m. and 5 p.m. Messages were delivered automatically | PersonalizationText messages were designed based on the language preferences (English or Spanish). Optimal message frequency and content (knowledge gaps/topic preferences) for the target group were identified in the previous studyExample: “Having diabetes can lead to a heart attack and stroke! But it doesn’t have to” | Health Belief ModelThe theory was used in the development of TExT-MED program to develop message contents to address specific barriers and knowledge gaps of T2D patients |
| Capozza et al., 201538 | RCTParallel 2 arms6 months | Adults with T2D (HbA1C>8%)n = 93; 61.5% femaleAge: 53.25 (10.95) USA: High income | Mobile phone text messaging and usual care | Usual care | Two-way messagingSMS textCare4Life Intervention:• Unidirectional and generic messages on diabetes education and health improvement were sent each day• Patients were able to activate optional two-way messaging protocols (totally 6) including medication reminders, glucose testing reminders, BP monitoring reminders, and tracking and encouragement for exercise and diet | 1–7 text messages per dayOne text messaging per day was mandatory, others depended on the use and preferences of patientsMessages were delivered automatically | Combination of Personalization and Psychosocial-Behavioral TailoringBased on the language preferences (English or Spanish) messages were personalized. Patients were able to control the type and frequency of the messages. Also based on their uploaded data, patients received some reminders and feedback messagesExample: “How are you? Feeling stressed about diabetes is normal. Getting support will help you feel better and control glucose. Ask for help when you need it” | None reported |
| Faridi et al., 200856 | RCTParallel 2 arms3 months | Adults with T2D (HbA1C <8%)n = 30; 63.4% femaleAge: 56.45 (9.6) USA: High income | Web-based system (NICHE technology), Mobile phone text messaging and biometric wireless assessment devices (glucose meter and pedometer) | Usual care and pedometer | Two-way messagingSMS textAutomated feedback messages based on patients’ uploaded HbA1C and physical activity dataThe content aimed to enhance diabetes self-management and self-efficacy | At least one daily, the real-time feedback message(Participants are requested to upload their data each day) Messages were delivered automatically | Psychosocial -Behavioral TailoringMessages were tailored to provide feedback on specific patient data. The content was arranged to enhance diabetes self-management skills and diabetes care self-efficacyNo example was provided | None reported |
| Fortmann et al., 201744 | RCTParallel 2 arms6 months | Hispanic adults with T2D(HbA1C > or = 7.5%)n = 126; 75%femaleAge: 48.4 (9.8) USA: High income | Mobile phone text messaging, blood glucose meter and usual care | Usual care and blood glucose meter | One-way messagingSMS textEducational, motivational and call-to-action messages on diabetes self-care and medication reminders and blood glucose monitoring prompts | 2–3 messages per day (at the beginning) Message timing was standardized for all patientsMessages were delivered automatically | PersonalizationMessages were culturally tailored to the needs of the specific population(Project Dulce curriculum was used which aimed to address cultural barriers and beliefs about diabetes) Example: “Use small plates! Portions will look larger and you may feel more satisfied after eating” “It takes a team! Get the support you need, family, friends and support groups can help you to succeed” | None reported |
| Gatwood et al., 201647 | RCTParallel 2 arms3 months | Adults with T2D (HbA1C >8%)n = 48, 50% femaleAge: 47.0 (11.7) USA: High income | Mobile phone text messaging | Usual care and a monthly “check-in” text message | One-way messagesSMS textMessages were designed to increase patients’ knowledge and motivation for improvement in their medication adherence and diabetes-related health beliefsA total of 168 theory-based messages (84 self-determination theory messages, 96 health belief model messages) and 128 tailored medication-specific messages were used | At least one message per dayOrdering and timing of the message were arranged based on the patient’s daily medication scheduleMessages were delivered automatically | Combination of Personalization and Psychosocial-Behavioral Tailoring• The subject’s name was used in every message and their age was used sporadically• Some details about the patient’s current diabetes medications, including the name of the medications, number of times taken each day, number of pills taken at each dose, and time of day the medication was taken for tailoring the text message delivery and arranging messages specifically to each subject’s treatment (benefits, safety and mechanism of action)• The name of medications was also included in some theory-driven messagesExample: “It may be tough to see but taking your diabetes medications is vital to your health. Taking them as directed may help you see their value” | Health Belief ModelSelf-Determination TheoryBoth theories were used to develop content for the mobile messaging interventionTechnology Acceptance Model was used to guide questionnaire items to assess the acceptance of text messaging |
| Kim &Kim 200850 | Pre-test–Post-test Control group design12 months | Adults with T2D and obesity (HbA1C>7%)n = 34, 53% femaleAge: 47 (8.6) Korea: High income | Website platform, mobile phone text messaging, wired internet and usual care including 4-5 visits to an endocrinologist | Usual care including 4–5 visits to an endocrinologist | One-way messagingSMS textMessages on continuous education and reinforcement of diet, exercise, medication adjustment and frequent monitoring of blood glucose levels | Weekly messagesMessages were delivered by a healthcare professional | Psychosocial-Behavioral TailoringFeedback messages and recommendations were sent based on patient-specific uploaded dataExample: “Your glucose control seems to be good” or “Please add one tablet of sulfonylurea in the evening” or “lack of exercise may be the cause of the aggravated glucose level” | None reported |
| Lim et al., 201655 | RCTParallel 2 arms6 months | Adults with T2D (HbA1C 7 -10.5%)n = 100, 25% femaleAge: 65.0 (4.9) Korea: High income | Website, physical activity monitor, glucometer and mobile phone messaging | Usual care and glucometer | Two-way messagingSMS textU-Healthcare intervention: Feedback messages and instructions on medication adjustments, diet pattern, physical activity and other lifestyle modifications | For each message type, a different schedule was applied. Weekly average glucose levels were sent on: Mondays at 10.00 a.m., monthly average glucose levels were sent on the last day of every month at 11.00 a.m., reminder messages were sent every Tuesday at 10.00 a.m., etc. Messages were delivered automatically | Psychosocial-Behavioral TailoringSpecific feedback messages, instructions, and recommendations based on patients’ uploaded data were generated by the decision rule engine and sent back to the patient immediatelyAlso, reminder messages on glucose monitoring, diet and physical activity were sent regularlyNo example was provided | None reported |
| Peimani et al., 201557 | RCTParallel 3 arms3 months | Adults with T2D (HbA1C not specified) n = 150, 46% femaleAge: 52.5 (10.9) Iran: Upper middle income | 2 intervention groups:Tailored text messaging group vs. non-tailored messaging group | No treatment-no messaging | One-way messagingSMS textEducational and motivational messages on diet, exercise, medication adjustment and self-monitoring of blood glucose levels | On average seven messages per week for both treatment groupsAutomated messages were delivered | Psychosocial-Behavioral TailoringTailored messages were motivational and persuasive and focused on increasing awareness of each self-management behavior. 75% of the messages addressed patients’ specific barriers to adhering prescribed diet, exercise or medication. No example was provided | Self-efficacy/Social Cognitive TheoryThe theory was used to tailor the intervention message content |
| Shetty et al., 201154 | RCTParallel 2 arms12 months | Adults with T2D (HbA1C 7-10%)n = 215, the gender ratio was not providedAge: 50.3 (9.1) India: Low middle income | Mobile text messaging | Usual care including appropriate prescriptions of drugs based on clinical and laboratory investigations and advice on diet modification and physical activity | One-way messagingSMS textEducational and motivational messages on diet, physical activity, medication adherence and healthy living | Once every 3 daysFrequency of messages varied as per patients’ preferencesUnclear information about how messages were delivered | PersonalizationMobile text messages were personalized based on patients’ preferred frequency of receiving messages and preferred content/topic including instructions on medical nutrition, physical activity, reminders for medication adherence and healthy living habitsNo example was provided | None reported |
| Tamban, et al., 201353 | RCTParallel 2 arms6 months | Adults with T2D (HbA1C >7) n = 104, 46% femaleAge: 49.5 (7.1) Philippines: Lower middle income | Mobile text messaging and usual care | Usual care including scheduled consults with an endocrinologist and visit to a DM educator | One-way messagingSMS textMessages on diet, physical activity and other self-management issues | 3 messages per weekMondays: Messages about dietWednesdays: Messages about exerciseFridays: Messages about the consequences of nonadherence to diabetes self-careMessages delivered by a research assistant | PersonalizationMessages were delivered based on patients preferred timingSMS messages included two sentences. First one included facts about proper diet and exercise, the second sentence acted as a reminder for adhering diet and exercise given by diabetes educatorExample: “Calorie counting is good for diabetics. Ask your dietitian how to do it and follow her advice” | None reported |
| Yoo, et al., 200958 | RCT2 parallel arms3 months | Adults with T2D (HbA1C>6.5–10) n = 123; 41% femaleAge: 58.2 (8.7) Korea Rep: High income | The Ubiquitous Chronic Disease Care System includes mobile text messaging and using assessment devices (i.e. glucometer) and a web-based physician communication | Usual care including clinic visits and regular consults with physicians | Two-way messagingSMS textMotivational messages on a healthy diet, exercise and glucose monitoring along with general information about diabetes, hypertension and obesity | 3 messages per dayAutomated feedback messages were sent immediately after patients uploaded their measurementsMessages were delivered automatically | Psychosocial-Behavioral TailoringRecommendations and reminders were sent immediately after patients uploaded their specific data, and motivational and educational messages were sent three times a dayExample: “Your fasting blood glucose level is very high compared with the appropriate target level for type 2 diabetes (<7.2. mmol/l)…Reduce your calorie intake and avoid foods high in fat. In addition, plan for regular exercise after your meals” | None reported |
| Yoon & Kim, 200752 | Pre-test–post-testControl group design12 months | Korean adults with T2D (HbA1C>7%)n =51, 57% femaleAge 47.1 (8.9) Korea Republic: High income | The website, wired internet and mobile messaging | Usual care including clinic visits and consults with an endocrinologist | One-way messagingSMS textInformative and motivating messages on continuous education and reinforcement of diet, exercise, medication adjustment and frequent monitoring of blood glucose levels | Once a week, on average 52 times in a yearMessages were sent by healthcare professionals | Psychosocial-Behavioral TailoringFeedback messages and recommendations based on patient-specific uploaded data on diet, exercise, medication or glucose monitoringExample: “Please check the amount that you eat”, “Your glucose control seems to be good” | None reported |
The effect of tailored text messaging interventions on self-management outcomes
Only two interventions41,54 assessed all the specified diabetes self-management outcomes while one study47 measured only medication adherence. Six studies measured the effect of the intervention on physical activity, and two studies49,55 reported statistically significant improvements. Five studies measured the effect of the intervention on dietary habits of participants, and two studies found statistically significant increases in dietary adherence.49,55 Medication adherence was assessed in three studies, and one study41 reported a statistically significant effect of the treatment. According to the tailoring strategies, no meaningful difference was observed between the interventions on physical activity, diet and medication adherence outcomes. The interventions also measured a limited number of attitudinal and behavioral outcomes related to diabetes self-management, such as acceptability, knowledge, health belief, self-determination and self-efficacy. Satisfaction with the intervention was measured in four studies which reported high satisfaction scores (more than 94%) with their interventions (Appendix VIII).
Due to the insufficient number of interventions reporting the effect of interventions on physical activity, diet and medication adherence, and the inconsistent scale of measurements (i.e. rates, counts, means), the data on these self-management outcomes could not be pooled in a meta-analysis. However, data from 11 trials that provided the effect of the intervention on glycated hemoglobin monitoring (HbA1C) were pooled in a meta-analysis. One study54 was excluded from the meta-analysis due to data inconsistency.
A meta-analysis: the effect of tailored interventions on glycated hemoglobin monitoring
The effect of 11 eligible tailored interventions on HbA1C values of a total of 949 type 2 diabetes patients showed a moderate and statistically significant weighted mean effect size, g = 0.54 (95% CI = 0.08–0.99, p < 0.001). Table 4 presents information on combined effect size, point estimates with confidence intervals and weights calculated for each study, and Figure 4 illustrates the forest plot diagram of the results.
Table 4.
Effects of tailored text messaging interventions on glycemic control.
| Study name | Hedges' g | CI lower limit | CI upper limit | Weight |
|---|---|---|---|---|
| Agboola et al., 2016“Text to Move” Intervention | −0.26 | −0.61 | 0.09 | 10.09% |
| Arora et al., 2014“TExT-MED” Intervention | 0.05 | −0.30 | 0.40 | 10.12% |
| Capozza et al., 2015“Care4Life” Intervention | −0.02 | −0.44 | 0.40 | 9.61% |
| Faridi et al., 2008“NICHE” pilot study | 0.66 | −0.07 | 1.43 | 7.32% |
| Fortmann et al., 2017“Dulce Digital” intervention | 0.53 | 0.15 | 0.92 | 9.87% |
| Kim & Kim, 2008“Mobile and internet” intervention | 2.21 | 1.39 | 3.14 | 6.44% |
| Lim et al., 2016“Multifactorial intervention” | 0.56 | 0.13 | 1.00 | 9.51% |
| Peimani et al., 2015“SMS-based intervention” | 0.35 | −0.04 | 0.75 | 9.78% |
| Tamban et al., 2013“The SMS intervention” | 0.40 | −0.04 | 0.84 | 9.46% |
| Yoo et al., 2009“The UCDC intervention” | 0.55 | 0.17 | 0.93 | 9.89% |
| Yoon & Kim, 2007“The SMS intervention” | 1.75 | 1.12 | 2.43 | 7.91% |
| Combined effect size | ||||
| Hedges' g | 0.54 | |||
| Standard error | 0.20 | |||
| CI lower limit | 0.08 | |||
| CI upper limit | 0.99 | |||
| PI lower limit | −0.64 | |||
| PI upper limit | 1.72 | |||
Note: CI: confidence interval; PI: prediction interval.
Figure 4.
Forest plot of tailored text messaging interventions’ effect on glycemic control.
Publication bias analysis revealed a small degree of asymmetry of data (p = 0.052 in Begg and Mazumdar test, and p = 0.002 in the Egger regression test). Trim-and-fill analysis imputed one study to the left of the mean resulting in a decrease in the effect size to g = 0.38 (95% CI = −0.15, 0.91). Figure 5 illustrates the funnel plot demonstrating combined and adjusted effect sizes and imputed data point.
Figure 5.
Funnel plot assessment of asymmetry in data.
Performing a leave-one-out sensitivity analysis by removing one study each time showed that the combined effect size was in minimum at g = 0.4150 and in maximum at g = 0.62.51 Removing two studies which were assessed as low quality due to their study design and sampling size50,52 did not have a significant effect on the data asymmetry. Funnel plot analysis still demonstrated a need for an imputed data point on the left side of the mean and a substantial degree of heterogeneity among studies (I2 = 55.52); therefore these studies were not excluded from the analysis.
The sample of studies indicated a significant level of heterogeneity (Q11 = 58.4, p<0.00, I2 = 82.8%), and a priori subgroup analyses with random effects model were conducted to investigate the reasons for the heterogeneity and possible effects of interventional and methodological components on the combined effect size.
Subgroup analyses
Subgroup analyses were conducted for the interventional and methodological moderators. The pre-specified subgroups related to participant characteristics (age, gender and ethnicity/race) and study design could not be analyzed quantitatively due to insufficient data.
The studies significantly differed in terms of their message frequencies (QB = 18.72, df = 1, p = 0.000), message direction (QB = 5.26, df = 1, p = 0.022), message delivery (QB = 18.72, df = 1, p = 0.000) and choice of modality (QB = 6.18, df = 1, p = 0.013). We had hypothesized that the studies using interactive (two-way) messages, mixed modalities (i.e. SMS and Web portal) and non-automated message delivery will produce larger effect sizes than their counterparts. The results confirmed our hypotheses on these variables. However, we had to reject our hypothesis on message direction because one-way messaging produced a larger effect size than two-way messaging. The interventions did not significantly differ according to their tailoring strategies, study lengths and study settings (Table 5).
Table 5.
Weighted mean effect size by moderating variables.
| Subgroups | n | Hedges’ g (95% CI) | p-value | Q B |
|---|---|---|---|---|
| Tailoring strategies | ||||
| Advanced | 8 | 0.66 (CI:0.09–1.22) | 0.00 | |
| Basic | 3 | 0.31 (CI: 0.02–0.60) | 0.17 | |
| 0.55 (p = 0.457) | ||||
| Message frequency | ||||
| Frequent messaging | 8 | 0.27 (CI: 0.04–0.51) | 0.01* | |
| Infrequent messaging | 3 | 1.41 (CI: 0.33–2.50) | 0.00* | |
| 18.72 (p = 0.000*) | ||||
| Message direction | ||||
| One-way messaging | 6 | 0.79 (0.13–1.46) | 0.00* | |
| Two-way messaging | 5 | 0.27 (−0.10–0.63) | 0.00* | |
| 5.26 (p = 0.022*) | ||||
| Message delivery | ||||
| Automated | 8 | 0.27 (CI:0.04–0.51) | 0.01* | |
| Non-automated | 3 | 1.41 (CI:0.33–2.50) | 0.00* | |
| 18.72 (p = 0.000*) | ||||
| Intervention modality | ||||
| Text messaging | 4 | 0.18 (CI:-0.02–0.38) | 0.38 | |
| Multi-modality | 7 | 0.79 (CI:0.19–1.39) | 0.00* | |
| 6.18 (p = 0.013*) | ||||
| Study length | ||||
| Short-term (3 months) | 3 | 0.48 (CI: 0.32–0.64) | 0.68 | |
| Long-term (6 months or more) | 8 | 0.57 (CI:0.00–1.14) | 0.00 | |
| 1.04 (p = 0.309) | ||||
| Study setting | ||||
| High income | 9 | 0.59 (CI: 0.09–1.10) | 0.00 | |
| Low and middle income | 2 | 0.37 (0.33–0.41) | 0.89 | |
| 0.04 (p = 0.975) | ||||
Note: n = number of studies in each group, g= weighted mean effect size.
CI: confidence interval; p < 0.05: statistical significance.
*Statistically significant, QB: the difference between groups based on combined effect size.
Discussion
This study presented a comprehensive review and a meta-analysis of tailored mobile text messaging interventions on type 2 diabetes self-management. The main characteristics of tailored interventions and their moderators of effectiveness were analyzed. This study acknowledged that different tailoring strategies are available, and by proposing a guideline for classifying tailoring strategies, it attempted to increase the comparability of the findings across reviews. Therefore, this study not only contributes to the growing field of type 2 diabetes self-management but also offers a useful framework for other text messaging interventions.
The majority of the trials were RCTs, conducted in high-income settings, and used multi-modalities for the delivery of interventions. All interventions targeted people with type 2 diabetes and used SMS as the form of text messaging.
Text messaging content in the reviewed studies generally included cognitive and rational attributes aiming to increase awareness and knowledge about diabetes self-management. For example, “Having diabetes can lead to a heart attack and stroke! But it doesn’t have to”,41 “Calorie counting is good for diabetics. Ask your dietitian how to do it and follow her advice”,49 and “How are you? Feeling stressed about diabetes is normal. Getting support will help you feel better and control glucose. Ask for help when you need it”.38 However, behavior change also has affective and conative aspects,59 and integrating cognitive and affective interventions can increase self-management skills of patients and lower their HbA1C.31
Further, a randomized controlled trial revealed that type 2 diabetes patients should receive more specific messages about what to do about medications, tests or treatment goals instead of receiving simple educational messages.60 Also, the educational and informative messages used in the interventions mostly relied on standard guidelines. The effectiveness of educational and informative components of diabetes self-management increases when they are customized.31
Another important result was the lack of message-specific elements or the framing effect in the message design considerations of the interventions. Considering the rapid growth of type 2 diabetes and the ineffectiveness of traditional self-management practices and insufficient evidence provided by previous research,7,30 there is a strong need for employing more persuasive message strategies in the interventions that will be guided by communication and persuasion theories.
The previously identified lack of a theoretical grounding in mHealth-based studies7,30,61 was confirmed by this systematic review. Although these behavioral theories have been the most frequently used theories in behavior change interventions,62 they may be limited in addressing the adaptive, customized and contextual nature of mHealth-based studies.4,63,64
As expected, tailored text messaging interventions had a moderate, positive, significant effect on HbA1C values. This result is consistent with the findings of the previous meta-analyses,7,13,14 which indicated small to moderate effects of text messaging interventions.
The subgroup analysis revealed that one-way, non-automated messages that are supported by additional modalities and sent infrequently are likely to be more effective for glycemic control in type 2 diabetes patients than other text messaging strategies. It was expected that patients would prefer less frequent messaging, but contrary to our hypothesis, they may not prefer interactive communication either.
Previous reviews have provided mixed results on the effectiveness of multi-modalities (text messaging, WEB portal, assessment devices, etc.).12,14,15 The findings of this study support our hypothesis and are also consistent with the mass media and communication studies that the seamless integration of multiple channels to reach a specific audience leads to more effective outcomes.65
The effectiveness of non-automated messages on HbA1C control could be an indication of how patients value tailoring and personalized communication. Non-automated message delivery may create a personalization tailoring effect and increase the engagement with the intervention. Although too much interactivity and message frequency appear less impactful, messages designed specifically for participants and coming from real people (i.e. healthcare provider, nurse and dietitian) are likely to be more effective.
There were some limitations to the study that should be noted. First, a meta-analysis could not be implemented on physical activity, diet and medication adherence because of the insufficient data provided for these outcomes. Due to the same reason, the relative effectiveness of different tailoring strategies used in the interventions could not be assessed. Because our focus was to examine the message design features, we included only the English articles. Further, the data provided about the tailoring strategies and the message content in this review were limited by the short explanations or examples provided in the articles.
The majority of the interventions included some risks of bias mainly due to the small sample sizes and insufficient blinding, and therefore it might have increased the possibility of publication bias in the meta-analysis. Trim-and-fill method revealed an imputed study that would be placed at the lower left side of the funnel to correct the asymmetry of data. It probably relates to the poor methodological designs in trials with small sample sizes which can cause an absence of studies on the left-hand side at the base of the funnel.32,66 However, by the correction of asymmetry, the tailored interventions still produced a substantial combined effect (g = 0.38) on glycemic control. Although a significant heterogeneity among the studies was observed, the random effects model was used, and subgroup analyses with a priori moderators were performed to understand how and to what degree the interventions differed from each other.
This study has significant implications for future research. Investigating the effects of different tailoring strategies for diabetes self-management is important and future research should further explore the relationships between tailoring strategies and other intervention components. Patients’ attitudes and behaviors toward message design factors in mobile text messaging need to be explored further by focusing on demographic and psychographic differences of patients.
The comparative effectiveness of automated, rule-based systems and non-automated message delivery should be examined in more detail considering the rapid increase in the use of automated systems and our challenging results.
Comparisons with previous reviews
Previous related studies on type 2 diabetes management either particularly focused on lifestyle behaviors (diet and physical activity)7 or medication adherence16 or glycated hemoglobin control.30,67 This study examined all these self-management outcomes and therefore provided a more comprehensive approach to understanding the effects of text messaging interventions on type 2 diabetes self-management. However, the main goal of this study was to identify the characteristics of tailored text messaging interventions and to examine their tailoring strategies and message design and delivery features. Therefore, this study differs from the other reviews as it only included tailored interventions. Although Dobson et al.’s30 systematic review provided information on tailoring where available, our study provided an in-depth analysis of tailoring strategies used in the interventions and further elaborated on message design strategies. Contrary to their results, our meta-analysis found support for the previous research7 and reported a significant effect of tailored mobile text messages on glycemic control of patients with type 2 diabetes.
Another important difference of this study is that it included both automated and non-automated text messaging interventions. By comparing the message delivery types, it was revealed that non-automated message delivery could be more effective than automated message delivery.
The meta-analysis examined the effects of a large number of moderators and found significant effects of message frequency, message direction and intervention modality on glycated hemoglobin control. In their meta-analysis, Arambepola et al.7 found no significant difference between the effect on unidirectional and bidirectional messages on glycated hemoglobin control. Our study found that in tailored interventions one-way (unidirectional) messaging could be more effective than two-way (bidirectional) messages and provided support for the previous text messaging reviews.13,14 Unlike Farmer et al. findings,16 this study revealed that using multi-modalities (i.e. web portal and text messaging) could be more effective than using only text messaging and provided support for previous research.15,18
Conclusions
Tailored mobile text messaging interventions were mostly RCTs, focused on adult patients, conducted in high-income settings, and used SMS to deliver intervention messages which mainly aimed to increase awareness and knowledge about type 2 diabetes management. The review highlighted the use of different tailoring strategies that addressed the participants’ preferences and needs. However, there is still a need for using more persuasive message design elements and comprehensive and dynamic theoretical approaches in these interventions.
The meta-analysis concluded that tailored mobile text messaging interventions can improve glycemic control in type 2 diabetes patients. Patients seem to prefer direct and personalized communication, but do not necessarily favor frequent contact and interactivity. Also, when combined with other modes of interaction (web page, assessment devices, etc.) the effects of tailored text messaging interventions on glycemic control can increase. However, more rigorous interventions with larger and carefully selected samples and longer follow-ups are required to confirm these findings and to explore the effects of tailored text messaging on other self-management behaviors.
Supplementary Material
Acknowledgements
The authors would like to thank to the reviewers for their kind reviews and valuable contributions to this study.
Contributorship
The first author designed the study with input from the other authors. Decisions regarding study inclusion, the risk of bias and data extraction were made by the first author and two independent reviewers. The first author analyzed the data and drafted the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Declaration of Conflicting Interests
The authors declare that there is no conflict of interest regarding the publication of this manuscript.
Ethical approval
Not applicable.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor
CS
Peer review
This manuscript was reviewed by two individuals who have chosen to remain anonymous.
Supplemental material
A supplementary file relating to this article is attached.
References
- 1.International Diabetes Federation (IDF). IDF diabetes atlas. 7th ed. Available from http://www.diabetesatlas.org (2017, accessed 5 April 2019).
- 2.Canadian Diabetes Association (CDA). Type 2 diabetes: the basics. Available from: https://www.diabetes.ca/DiabetesCanadaWebsite/media/Managing-My-Diabetes/Tools%20and%20Resources/type-2-diabetes-the-basics.pdf?ext=.pdf (2019, accessed 8 April 2019).
- 3.Diabetes UK. Supported self-management. Available from https://www.diabetes.org.uk/professionals/position-statements-reports/diagnosis-ongoing-management-monitoring/supported-self-management (2009, accessed 5 April 2019).
- 4.Spruijt-Metz D, Nilsen W, Pavel M. mHealth for behavior change and monitoring In. Adibi S. (ed.) mHealth. Multidisciplinary verticals. Boca Raton: CRC Press, 2015; pp. 120–128. [Google Scholar]
- 5.Hood M, Wilson R, Corsica J, et al. What do we know about mobile applications for diabetes self-management? A review of reviews. J Behav Med [Internet]. Springer US; 2016; 2015. Available from: http://link.springer.com/10.1007/s10865-016-9765-3 [DOI] [PubMed]
- 6.de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, et al. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 2012; 12 :CD007459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arambepola C, Ricci-Cabello I, Manikavasagam P, et al. The impact of automated brief messages promoting lifestyle changes delivered via mobile devices to people with type 2 diabetes: a systematic literature review and meta-analysis of controlled trials. J Med Internet Res [Internet]. 2016. Apr 19 [cited 2017 Sep 15]; 18(4): e86 Available from: http://www.ncbi.nlm.nih.gov/pubmed/27095386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall AK, Cole-Lewis HBJ, Hall AK, et al. Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health. 2015; 36(20): 393–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gatwood J, Balkrishnan R, Erickson SR, et al. Mobile phone use and perspectives on tailored texting in adults in diabetes. JMTM 2015; 4(3): 2–12. [Google Scholar]
- 10.Suffoletto B. Text message behavioral interventions: From here to where? Curr Opin Psychol 2016; 9: 16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muench F, Baumel A. More than a text message: dismantling digital triggers to curate behavior change in patient-centered health interventions. J Med Internet Res 2017; 19(5): e147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kitsiou S, Paré G, Jaana M, et al. Effectiveness of mHealth interventions for patients with diabetes: An overview of systematic reviews. PLoS One 2017; 12(3): 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orr JA, King RJ. Mobile phone SMS messages can enhance healthy behaviour: a meta-analysis of randomised controlled trials. Health Psychol Rev [Internet] 2015; 9(4): 397–416. Available from: 10.1080/17437199.2015.1022847 [DOI] [PubMed] [Google Scholar]
- 14.Head KJ, Noar SM, Iannarino NT, et al. Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Soc Sci Med [Internet] 2013; 97: 41–48. Available from: 10.1016/j.socscimed.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 15.Armanasco AA, Miller YD, Fjeldsoe BS, et al. Preventive health behavior change text message interventions: A meta-analysis. Am J Prev Med [Internet]. 2017; 52(3): 391–402. Available from: 10.1016/j.amepre.2016.10.042 [DOI] [PubMed] [Google Scholar]
- 16.Farmer AJ, McSharry J, Rowbotham S, et al. Effects of interventions promoting monitoring of medication use and brief messaging on medication adherence for people with Type 2 diabetes: a systematic review of randomized trials. Diabet Med 2016; 33(5): 565–579. [DOI] [PubMed] [Google Scholar]
- 17.O'Keefe DJ. Persuasion: Theory and research. 2nd ed Thousand Oaks: Sage Publications, 2002. [Google Scholar]
- 18.Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull 2007; 133(4): 673–693. [DOI] [PubMed] [Google Scholar]
- 19.Muench F, van Stolk-Cooke K, Morgenstern J, et al. Understanding messaging preferences to inform development of mobile goal-directed behavioral interventions. J Med Internet Res 2014; 16(2): e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rothman AJ, Bartels RD, Wlaschin J, et al. The strategic use of gain- and loss-framed messages to promote healthy behavior: How theory can inform practice. J Commun 2006; 56(Suppl): 202–220. [Google Scholar]
- 21.Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. Adv Exp Soc Psychol 1986; 19: 123–205. [Google Scholar]
- 22.Militello LK, Kelly SA, Melnyk BM. Systematic review of text-messaging interventions to promote healthy behaviors in pediatric and adolescent populations: implications for clinical practice and research. Worldviews Evid Based Nurs 2012; 9(2): 66–77. [DOI] [PubMed] [Google Scholar]
- 23.Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Ann Rev Pub Health 2010; 31: 399–418. [DOI] [PubMed] [Google Scholar]
- 24.Lustria MLA, Noar SM, Cortese J, et al. A meta-analysis of web-delivered tailored health behavior change interventions. J Health Comm 2013; 18(9): 1039–1069. [DOI] [PubMed] [Google Scholar]
- 25.Krebs P, Prochaska JO, Rossi JS. Defining what works in tailoring: A meta-analysis of computer-tailored interventions for health behavior change. Prevent Med 2010; 51(3-4): 214–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Noar SM, Harrington NG. Tailored communications for health-related decision-making and behavior change In Diefenbach MA, Miller-Halegoua S, Bowen DJ. (eds) Handbook of health decision science. New York: Springer Science + Business Media, 2016, pp. 251–263. [Google Scholar]
- 27.Dijkstra A. Personalization/computer-tailoring in persuasive technology: tailoring ingredients target psychological processes. Persuas Technol [Internet] 2016; 5–4 Available from: http://ceur-ws.org (2016, accessed 15 September 2017). [Google Scholar]
- 28.Hawkins RP, Kreuter M, Resnicow K, et al. Understanding tailoring in communicating about health. Health Educ Res 2008; 23(3): 454–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pal K, Dack C, Ross J, et al. Digital health interventions for adults with type 2 diabetes: qualitative study of patient perspectives on diabetes self-management education and support. J Med Internet Res 2018; 20(2): e40. doi:10.2196/jmir.8439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dobson R, Whittaker R, Pfaeffli Dale L, et al. The effectiveness of text message-based self-management interventions for poorly-controlled diabetes: A systematic review. Digit Health [Internet] 2017; 3: 205520761774031 Available from: http://journals.sagepub.com/doi/10.1177/2055207617740315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sherifali D, Berard LD, Gucciardi E, et al. Self-management education and support. Diabetes Canada Clinical Practice Guidelines Expert Committee. Can J Diabetes 2018; 42: S36–S41. [DOI] [PubMed] [Google Scholar]
- 32.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org.
- 33.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev [Internet] 2015; 4(1): 1 Available from http://systematicreviewsjournal.biomedcentral.com/articles/10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zotero.org. Zotero 5.0 Citation manager. Available from https://www.zotero.org.
- 35.World Bank Group. New country classifications by income level: 2017-2018. Available from https://blogs.worldbank.org/opendata/new-country-classifications-income-level-2017-2018 (2018, accessed 5 April 2019).
- 36.Borenstein M, Hedges LV, Higgins JPT, et al. Introduction to meta-analysis. West Sussex: Wiley, 2009. [Google Scholar]
- 37.Cohen J. A power primer. Psychol Bull 1992; 112: 155–159. [DOI] [PubMed] [Google Scholar]
- 38.Capozza K, Woolsey S, Georgsson M, et al. Going mobile with diabetes support: A randomized study of a text message-based personalized behavioral intervention for type 2 diabetes self-care. Diabetes Spectr [Internet] 2015; 28(2): 83–91. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/734/CN-01154734/frame.html [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Method 2005; 5: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suurmond R, van Rhee H, Hak T. Introduction, comparison, and validation of Meta-Essentials: a free and simple tool for meta-analysis. Res Synth Meth 2017; 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Arora S, Peters AL, Burner E, et al. Trial to examine text message–based mhealth in emergency department patients with diabetes (text-med): A randomized controlled trial. Ann Emerg Med 2014. ; 63(6): 745–754.e6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24225332 [DOI] [PubMed] [Google Scholar]
- 42.Burner E, Menchine M, Taylor E, et al. Gender differences in diabetes self-management: a mixed-methods analysis of a mobile health intervention for inner-city Latino patients. J Diabetes Sci Technol 2013; 7(1): 111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abebe NA, Capozza KL, Des Jardins TR, et al. Considerations for community-based mHealth initiatives: insights from three Beacon Communities. J Med Internet Res 2013; 15(10): e221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fortmann AL, Gallo LC, Garcia MI, et al. Dulce Digital: an mHealth SMS-based intervention improves glycemic control in hispanics with type 2 diabetes. Diabetes Care 2017; 40(10): 1349–1355. doi: 10.2337/dc17-0230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Philis-Tsimikas A, Fortmann A, Lleva-Ocana L, et al. Peer-led diabetes education programs in high-risk Mexican Americans improve glycemic control compared with standard approaches. Diabetes Care 2011; 34(9): 1926–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gatwood J, Balkrishnan R, Erickson SR, et al. The impact of tailored text messages on health beliefs and medication adherence in adults with diabetes: A randomized pilot study. Res Soc Adm Pharm 2016; 12(1): 130–140. [DOI] [PubMed] [Google Scholar]
- 47.Gatwood J, Balkrishnan R, Erickson SR, et al. Addressing medication nonadherence by mobile phone: Development and delivery of tailored messages. Res Soc Adm Pharm 2014; 10(6): 809–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim H, Song M. Technological intervention for obese patients with type 2 diabetes. Appl Nurs Res 2008; 21(2): 84–89. [DOI] [PubMed] [Google Scholar]
- 49.Agboola S, Lopez L, Searl M, et al. Text to move: randomized controlled trial of personalized text messaging to improve physical activity in a diverse patient population with type 2 diabetes mellitus. J Mobile Tech Med 2013; 2(4s): 8. [Google Scholar]
- 50.Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform 2008; 77(6): 399–404. [DOI] [PubMed] [Google Scholar]
- 51.Agboola S, Jethwani K, Lopez L, et al. Text to Move: a randomized controlled trial of a text-messaging program to improve physical activity behaviors in patients with type 2 diabetes mellitus. J Med Internet Res 2016; 18(11): e307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yoon K, Kim H. A short message service by cellular phone in type 2 diabetic patients for 12 months. Diabetes Res Clin Pract [Internet] 2008; 79(2) :256–261. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/322/CN-00628322/frame.html [DOI] [PubMed] [Google Scholar]
- 53.Tamban C, Isip-Tan I, Jimeno C. Use of short message services (SMS) for the management of type 2 diabetes mellitus: a randomized controlled trial. J SEAN Fed Endocr Soc [Internet] 2013; 28(2): 143 Available from: http://www.asean-endocrinejournal.org/index.php/JAFES/article/view/68/132 [Google Scholar]
- 54.Shetty AS, Chamukuttan S, Nanditha A. Reinforcement of adherence to prescription recommendations in Asian Indian diabetes patients using short message. A pilot study. J Assoc Physicians India 2011; 59: 711–714. [PubMed] [Google Scholar]
- 55.Lim S, et al. Multifactorial intervention in diabetes care using real-time monitoring and tailored feedback in type 2 diabetes. Acta Diabetologica 2016; 53: 189–198. [DOI] [PubMed] [Google Scholar]
- 56.Faridi Z, Liberti L, Shuval K, et al. Evaluating the impact of mobile telephone technology on type 2 diabetic patients’ self-management: The NICHE pilot study. J Eval Clin Pract 2008; 14(3): 465–469. [DOI] [PubMed] [Google Scholar]
- 57.Peimani M, Rambod C, Omidvar M, et al. Effectiveness of short message service-based intervention (SMS) on self-care in type 2 diabetes: A feasibility study. Prim Care Diabetes [Internet] 2014; 10(4): 251–258. Available from: 10.1016/j.pcd.2015.11.001 [DOI] [PubMed] [Google Scholar]
- 58.Yoo H, Park M, Kim T, et al. A ubiquitous chronic disease care system using cellular phones and the internet. Diabet Med [Internet] 2009; 26(6) :628–635. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/290/CN-00729290/frame.html [DOI] [PubMed] [Google Scholar]
- 59.Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Reading, MA: Addison-Wesley, 1975. [Google Scholar]
- 60.Adams SY, Crawford AG, Rimal RN, et al. The effects of a computer-tailored message on secondary prevention in type 2 diabetes: a randomized trial. Popul Health Manag 2009; 12(4): 197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Medicine 2013; 10(1). 10.1371/journal.pmed.1001362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Glanz K, Rimer BK, Lewis FM. (eds) The scope of health behavior and health education. In: Health behavior and health education: Theory, research, and practice San Francisco: Jossey-Bass, 2002, pp. 3–21.
- 63.Saranummi N, Spruijt-Metz D, Intille SS, et al. Moving the science of behavior change into the 21st century: novel solutions to prevent disease and promote health. IEEE Pulse, 2013; 4: 22–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Davis R, Campbell R, Hildon Z, et al. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev 2015; 9(3): 323–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kotler P. Marketing management. 14th ed Upper Saddle River: Prentice Hall, 2003, p. 21. [Google Scholar]
- 66.Sedgwick P. Meta-analyses: how to read a funnel plot. BMJ 2013; 346: f1342. [DOI] [PubMed] [Google Scholar]
- 67.Faruque LI, Wiebe N, Ehteshami-Afsha A. Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. Can Med Assoc J 2017; 189(9): E341–E364. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.