Abstract
Objective:
To identify a brain-based predictor of cocaine abstinence using a recently developed machine learning approach, connectome-based predictive modeling (CPM). CPM is a predictive tool and a method of identifying networks that underlie specific behaviors (‘neural fingerprints’).
Methods:
Fifty-three individuals participated in neuroimaging protocols at the start of treatment for cocaine-use disorder, and again at the end of 12-week treatment. CPM with leave-one-out cross-validation was run to identify pre-treatment networks that predicted abstinence (percent cocaine-negative urines during treatment). Networks were applied to post-treatment fMRI data to assess changes over time and ability to predict abstinence during follow-up. The predictive ability of identified networks was then tested in separate, heterogeneous sample of individuals scanned prior to treatment for cocaine use disorder (n=45).
Results:
CPM predicted abstinence during treatment, as indicated by a high correspondence between predicted and actual abstinence values (r(df=52)=0.42, p=0.001). Identified networks included connections within and between canonical networks implicated in cognitive/ executive control (frontoparietal, medial frontal) and in reward responsiveness (subcortical, salience, motor/sensory). Connectivity strength did not change with treatment, and strength at post-treatment also predicted abstinence during follow-up (r(df=39)=0.34, p=0.03). Network strength in the independent sample predicted treatment response with 64% accuracy by itself, and with 71% accuracy when combined with baseline cocaine-use.
Conclusions:
These data demonstrate that individual differences in large-scale neural networks contribute to variability in treatment outcomes for cocaine use disorder. They identify specific abstinence networks that may be targeted in novel interventions.
Introduction
Addictions are a leading cause of disability worldwide. Despite advances, the effectiveness of most substance-use interventions remains highly variable across individuals and multiple quit-attempts are standard. While a growing body of research suggests that variability in treatment response is linked to individual differences in neural functioning (1-6), the search for brain-based predictors has yet to yield a reliable indicator of future treatment response or abstinence (7, 8). Identification of brain-based predictors of abstinence may not only expand existing biological knowledge of addictions pathophysiology (which may itself be used to refine existing interventions), but may ultimately be used to directly inform real-world clinical practice via assignment of patients to therapies based on individual patterns of neural function; i.e., neuromarkers (7, 9, 10).
In most cases, treatment-oriented neuroimaging studies in addiction, and other disorders, rely on prospective associations (1–4), where the term ‘predicts’ is often inaccurately used to refer to correlation or regression (11, 12). However, true predictive models require application of the model to novel data (8, 11, 13–15). Newly available alternatives such as machine-learning allow for actual prediction (9, 11, 12), but have not yet been used to identify pre-treatment predictors of abstinence. Nonetheless, prior research indicates that alterations within well-established neural networks – e.g., frontoparietal, salience, default mode – likely contribute to individual differences in treatment outcomes for cocaine-use disorder (3, 5, 16). For example, functional connectivity strength between the medial prefrontal cortex and temporal pole, when combined with years of education, has been identified as a predictor of relapse (5). However, no prior study has used a whole-brain, machine learning approach to identify neuromarkers of future abstinence.
Connectome-based predictive modeling (CPM) (13, 17) is a machine learning approach for generating brain-behavior models from whole-brain, functional connectivity data (‘connectomes’). Unlike correlation or regression models, CPM with built-in cross validation protects against over-fitting by testing the strength of the relationship in a novel sample, increasing the likelihood of replication in future studies and thus the applicability to other clinical samples (13). Unlike other machine-learning approaches previously employed to study addictions, CPM is entirely data-driven and requires no a priori selection of networks. It is therefore both a predictive tool as well as a method of identifying networks that subserve specific behaviors – referred to as ‘neural fingerprints’ – and thus may also be used to identify novel treatment targets (13, 17). CPM has previously been used to identify neural fingerprints of IQ and attention using whole-brain functional connectivity data acquired during neurocognitive task performance (17–19), but has not been previously used to predict future behaviors or a clinical outcome.
Here, we use dimensional CPM to identify neural networks predictive of future abstinence from cocaine by applying CPM to fMRI reward task data acquired at the start of a 12-week treatment for cocaine-use-disorder. We further test the stability of these networks over time and in relation to post-treatment abstinence. Finally, we test the ability of identified networks to predict treatment response in a heterogeneous replication sample. Based on prior work focusing on selected networks (5, 16), we hypothesized that increased connectivity within- and between medial frontal, frontoparietal and salience networks would positively predict abstinence.
Methods
Participants and recruitment
Participants (n=74) were recruited from a randomized controlled trial of behavioral therapy plus galantamine or placebo treatment for cocaine-use disorder (20). Demographic and clinical characteristics are shown in Table 1. In addition to seeking treatment for cocaine, all participants were currently enrolled in methadone maintenance treatment for opioid-use disorder. Consistent with the parent trial (20), the fMRI sample was predominantly male (63.5%) and unemployed (73.0%), with multiple prior treatment attempts (outpatient: 2.97± 3.63, inpatient: 3.16±5.24) and legal problems (lifetime arrests: 5.46±6.29). Following exclusion of individuals with incomplete data (n=4) or excessive motion during scanning (n=17; further details below), the final sample used for CPM analyses consisted of 53 individuals (73.6% male). Further details on motion controls and follow-up analyses controlling for time of scanning are provided in the Supplemental Materials. As shown in Table 1, included versus excluded participants did not differ in years of cocaine-use, treatment assignment or other clinical variables with the exception of sex (p=.004). As in our prior work (2, 4), abstinence during treatment was determined based on results of biweekly urine testing and defined as the percentage of urines negative for cocaine provided during treatment. All participants provided written informed consent following a complete description of study procedures.
Table 1 –
Demographic and clinical characteristics of methadone-maintained, cocaine-dependent participants (N=74)
| fMRI data included in CPM* |
||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Total (N=74) | Yes (n=53) | No (n=21) | F or X2 | p-value | |||
| Female, No. (%) | 27 | 36.5 | 14 | 26.4 | 13 | 61.9 | 8.18 | 0.004 |
| Methadone dose at baseline (mg), mean (SD) | 73 | 24.4 | 74.7 | 23.1 | 69 | 27.5 | 0.81 | 0.37 |
| Days in treatment at fMRI scan, mean (SD) | 1.9 | 7.3 | 1.5 | 6.7 | 2.9 | 8.6 | 0.55 | 0.46 |
| Completed High School, No. (%) | 53 | 71.6 | 37 | 69.8 | 16 | 76.2 | 0.3 | 0.58 |
| Unemployed, No. (%) | 54 | 73 | 36 | 71.7 | 16 | 76.2 | 0.15 | 0.7 |
| Age, mean (SD) | 36.3 | 9.4 | 35.2 | 9.4 | 39.3 | 9.1 | 2.95 | 0.09 |
| Days opioid use, past 28, mean (SD) | 3.6 | 5.8 | 3.8 | 6.1 | 3.1 | 5 | 0.23 | 0.63 |
| Days marijuana use, past 28, mean (SD) | 2 | 5.5 | 1.9 | 5.9 | 2.2 | 4.2 | 0.04 | 0.85 |
| Days cocaine use, past 28, mean (SD) | 16.2 | 8.1 | 16.9 | 8.3 | 14.5 | 7.4 | 1.33 | 0.25 |
| Days cigarette use, past 28, mean (SD) | 26.1 | 6.6 | 25.6 | 7.6 | 27.4 | 2.8 | 1.06 | 0.31 |
| Days alcohol use, past 28, mean (SD) | 2.4 | 5.9 | 2.1 | 5.1 | 3.2 | 7.7 | 0.56 | 0.46 |
| Years of regular cocaine use, mean (SD) | 9 | 7.8 | 8.1 | 6.5 | 11.3 | 10.2 | 2.6 | 0.11 |
| No. prior outpatient drug treatments, mean (SD) | 3 | 3.6 | 3 | 3.8 | 2.9 | 3.4 | 0.01 | 0.92 |
| No. prior inpatient drug treatments, mean (SD) | 3.2 | 5.2 | 3 | 4.7 | 3.6 | 6.6 | 0.18 | 0.68 |
| Lifetime No. of arrests, mean (SD) | 5.5 | 6.3 | 5.3 | 6.1 | 5.8 | 6.9 | 0.07 | 0.8 |
| Estimated IQ (Shipley), mean (SD) | 90.5 | 12.8 | 90.1 | 12.8 | 91.2 | 13.2 | 0.11 | 0.74 |
| Route of Cocaine Use | ||||||||
| Smoke, No. (%) | 52 | 70.3 | 37 | 69.8 | 15 | 71.4 | 0.5 | 0.92 |
| Snort, No. (%) | 15 | 20.3 | 11 | 20.8 | 4 | 19 | ||
| IV, No. (%) | 6 | 8.1 | 4 | 7.5 | 2 | 9.5 | ||
| Speedball, No. (%) | 1 | 1.4 | 1 | 1.9 | 0 | 0 | ||
| Percent cocaine negative urines, mean (SD) | 21.6 | 28.9 | 23 | 28 | 18 | 31.5 | 0.46 | 0.5 |
4 individuals were excluded due to incomplete or missing data; 17 were excluded due to excessive motion during scannin
Neuroimaging data acquisition
fMRI data were acquired during performance of a well-validated Monetary Incentive Delay task (21) (Supplemental Figure 1; details on acquisition in Supplemental Materials). Preprocessing was conducted using SPM8 and the BioImage Suite and is described in the Supplemental Materials.
Functional connectivity
Whole-brain functional connectivity analyses were conducted using the BioImage suite, using previously described methods (17–19). Network nodes were defined using the Shen 268-node brain atlas which includes the cortex, subcortex and cerebellum (22), as in other prior CPM work (17–19) (further details in Supplemental Materials). Task connectivity was calculated based on the ‘raw’ task timecourses, with no regression of task-evoked activity (18, 23). This involved computation of mean time courses for each of the 268 nodes (i.e., average time course of voxels within the node) for use in node-by-node pairwise Pearson’s correlations. Resultant r-values were transformed using Fisher’s z-transformation to create symmetric 268x268 connectivity matrices in which each element of the matrix represents the strength of connection between two individual nodes (hereafter referred to as an edge) (13, 19).
Connectome-based predictive modeling (CPM)
CPM was conducted using previously validated custom MATLAB scripts (13). A schematic diagram of CPM is shown in Supplemental Figure 2. Briefly, CPM takes group connectivity matrices and behavioral data (in this case, percentage of cocaine-negative urines during treatment) as input to generate a predictive model of the behavioral data from connectivity matrices (13). Edges and behavioral data from the training dataset are correlated using regression analyses (here using either Pearson’s correlation or partial correlation) to identify positive and negative predictive networks. Positive networks are networks for which increased edge weights (increased connectivity) are associated with the variable of interest, whereas negative networks are networks for which decreased edge weights (decreased connectivity) are associated with the variable of interest. While both networks are used for predicting the same variable, they are by definition independent - as a single edge cannot be both a positive and negative predictor. Single subject summary statistics are then created as the sum of the significant edge weights in each network and entered into predictive models assuming linear relationships with behavioral data. Resultant polynomial coefficients (linear equation including slope and intercept) are then applied to the test dataset to predict behaviors. In the case of leave-one-out cross-validation (used here), a single participant’s predicted value (i.e., the ‘left-out’ participant) is generated by taking the data from all other participants as the training dataset in an iterative manner until all participants have a predicted value.
Model performance (i.e., correspondence between predicted and actual values) was assessed using Spearman’s rho correlations. When using leave-one-out cross-validation, analyses in the leave-one-out folds are not wholly independent and the number of degrees of freedom is thus overestimated for parametric p-values based on correlation. Instead of parametric testing, we therefore performed permutation testing. To generate null distributions for significance testing, we randomly shuffled the correspondence between behavior variables and connectivity matrices 5,000 times and re-ran the CPM analysis with the shuffled data. Based on these null distributions, the p-values for leave-one-out predictions were calculated as in prior work (13, 18). Details on characterization of resultant network anatomy are provided in the Supplemental Materials.
Results
Associations between baseline variables and abstinence
Spearman’s correlation analyses indicated no significant associations between baseline clinical variables (years-of-use, past-month-use, methadone dose) and within-treatment abstinence (p’s>.05). For comparison with CPM findings, a machine learning analysis (i.e., support vector regression; SVR) of baseline clinical data (details in Supplemental Materials) was also conducted. As CPM is optimized for neuroimaging data, SVR was selected over CPM for this analysis. SVR incorporating baseline clinical variables did not predict within-treatment abstinence (p>.05).
Predicting within-treatment abstinence
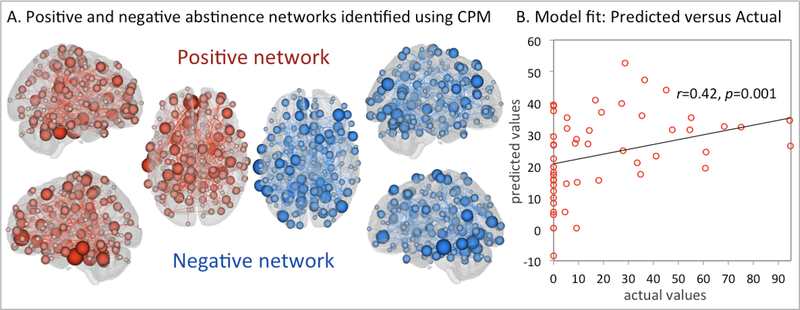
To control for putative effects of residual motion, CPM analyses were conducted both with and without motion as a covariate. Both approaches yielded similar results (further details in Supplemental Materials). For simplicity, findings including motion as a covariate are presented here unless otherwise specified. The overall CPM model successfully predicted abstinence (cocaine-negative urines; Figure 1A: combined: r(df=52)=0.42, p=0.001), as did connectivity within the positive (r(df=52)=0.43, p<0.001) and negative (r(df=52)=0.40 p=0.003) networks separately.
Figure 1 – CPM model performance and positive and negative abstinence networks.
Figure 1A shows positive (red) and negative (blue) abstinence networks. For the positive network, increased edge weights (i.e., increased functional connectivity) predict more within-treatment abstinence. For the negative network, decreased edge weights (i.e., decreased functional connectivity) predict more within-treatment abstinence. Larger (smaller) spheres indicate nodes with more (less) edges. Figure 1B shows the correspondence between actual (x-axis) and predicted (y-axis) abstinence values generated using CPM. Abstinence values correspond to the percentage of urines negative for cocaine provided during treatment. Despite the clinical complexity of the population (Table 1), CPM successfully predicted within-treatment abstinence (p’s<.005). Predictions remained significant in follow-up analyses controlling for clinical variables including years-of-cocaine-use and treatment retention (Supplementary Materials).
Follow-up comparisons controlling for methadone dose, medication group (galantamine/ placebo), cocaine-use history (years of use, days of past-month use), other alcohol/drug-use, smoking status, and timing of fMRI scanning with respect to treatment initiation also successfully predicted abstinence (r’s>0.400, p’s<.003) and are presented in the Supplementary Materials. Post-hoc correlations indicated significant correspondence between network strengths and other abstinence indices (e.g., percent days self-reported abstinence, maximum days of consecutive abstinence) and are provided in the Supplemental Materials.
Network anatomy
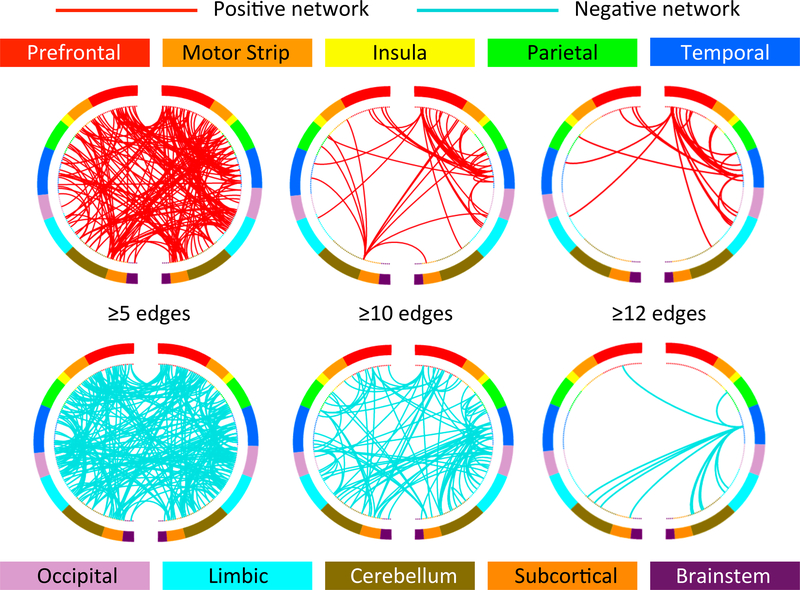
Figure 2 summarizes positive and negative abstinence networks based on connectivity between macroscale brain regions (note that brain regions are presented in approximate anatomical order, such that longer range connections are represented by longer lines). Consistent with prior CPM work (17–19), network anatomies for both networks were complex and included connections between frontal, parietal, occipital and temporal lobes. Despite this complexity, the spatial extent of both positive and negative networks together included only 539 edges (266 positive, 263 negative), or less than 1% of possible connections. Highest degree nodes (i.e., nodes with the most connections) for the positive network included a prefrontal node with connections to limbic, temporal, parietal, cerebellar and other prefrontal nodes, and a temporal node with connections to limbic, parietal, motor and prefrontal nodes. Highest degree nodes for the negative network also included a temporal node with connections to limbic, parietal and prefrontal nodes, as well as with connections to cerebellar and subcortical nodes. Both abstinence networks included short- and long-range connections. However, the positive network was characterized by relatively more long-range connections (56% long-range; 44% short-range), while the negative network included more short-range connections (42% long-range; 58% short-range).
Figure 2 – Positive and negative abstinence networks summarized by connectivity between macroscale brain regions.
Figure 2 summarizes positive and negative abstinence networks based on connectivity between macroscale brain regions. From top, brain regions are presented in approximate anatomical order, such that longer range connections are represented by longer lines.
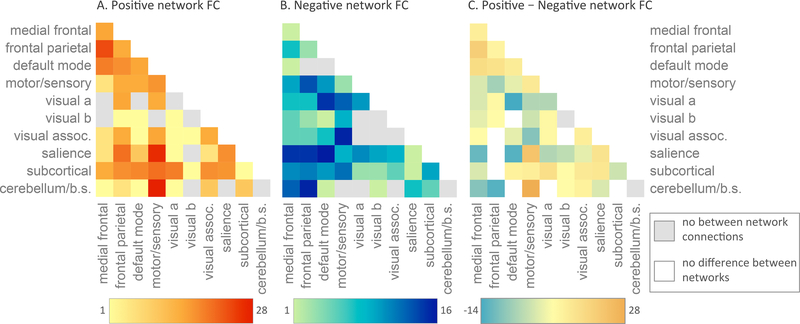
Overlap with canonical neural networks
To facilitate characterization of identified abstinence networks, Figure 3 summarizes connectivity based on the number of connections within and between canonical neural networks (e.g., frontoparietal, motor/sensory) for the positive (3A) and negative (3B) networks. By definition, positive and negative networks do not contain overlapping connections (as a single edge cannot be both a positive and negative predictor). However, positive and negative abstinence networks included connections within and between similar large-scale canonical neural networks. Comparison of networks (Figure 3C) indicated that the positive network included relatively more connections between medial frontal and frontoparietal and default mode networks; between motor/sensory and cerebellar and salience networks; and between subcortical and motor/sensory and salience networks. The negative network included relatively more connections between medial frontal and salience networks; between medial frontal and subcortical networks; between medial frontal and motor/sensory networks; between default mode and salience networks; and between frontoparietal and motor/sensory networks. The positive network was further characterized by more within-network connections across medial frontal, frontoparietal, default mode, motor/sensory, visual association and salience networks, whereas the negative network included more within-network connections for occipital and subcortical networks.
Figure 3 – Positive and negative abstinence networks summarized by overlap with canonical neural networks.
Within- and between-network connectivity for the positive network (A), negative network (B) and for positive – negative networks (C) are summarized based on overlap with canonical neural networks. For A and B, cells represent the total number of edges connecting nodes within (and between) each network with darker colors indicating a greater number of edges. For C, cells represent the number of positive versus negative edges connecting nodes within (and between) each network with warmer colors (orange/yellow) indicating more edges in the positive network and cooler colors (blue/green) indicating more edges in the negative network. Despite this visual simplification, it is important to note that, by definition positive and negative networks do not contain overlapping edges (for further information on network definitions, see Supplemental Materials).
Relationship to post-treatment abstinence
Individuals enrolled in the trial were also invited to participate in post-treatment fMRI scanning. Following exclusion for excess motion (as described above) this included 40 participants. To determine the extension of our networks to predict abstinence following treatment, individual participant network summary scores were created as the sum of connectivity strengths within positive and negative networks (negative network values were first sign-flipped so that higher values indicated ‘better’ networks). Resultant scores from post-treatment matrices were entered into correlation analyses with abstinence during 6month follow-up (as defined via self-report using the timeline follow-back method, assessed at monthly intervals). Post-treatment connectivity strengths were significantly associated with abstinence during follow-up (r(df=39)=0.34, p=0.03). Comparison of pre- versus post-treatment networks indicated no significant changes in connectivity strength (t(df=38)=0.81, p=0.42).
Out-of-sample replication and binary prediction
To determine the generalizability of our findings, we tested the ability of the identified networks to predict cocaine-negative urine urine toxicology outcomes in a heterogeneous sample of cocaine-dependent individuals (n=45). This included previously excluded individuals with excess motion during scanning (n=17; Table 1) and individuals from an independent, previously published randomized controlled trial (n=28) (2). As in our original analyses, residual motion was included as a covariate. Further details on exclusion for motion and related analyses are provided in the supplemental materials.
As the practical clinical utility of biomarkers is unlikely to rely on their ability to generate continuous indices of treatment outcome, but rather on their ability to a priori identify treatment responders from non-responders in a binary manner, we further tested the ability of the identified networks to predict abstinence in a binary manner (yes/no, any drugfree urine specimens) in our replication sample. Individual participant summary scores were extracted from functional-connectivity matrices, as above, and entered into regression analyses with within-treatment abstinence values.
Pre-treatment network strength in the independent sample predicted abstinence during treatment for both continuous (percent cocaine-negative urines during treatment; r(df=44)=0.36, p=.016) and binary (yes/no, any cocaine-negative urine; 64% accuracy, x2(df=2)=5.99, p=0.014; 82% specificity; 35% sensitivity) outcomes. For binary prediction, accuracy was increased to 71% following inclusion of baseline cocaine-use (days of use in month prior to treatment) in the model (x2(df=2)=6.20, p=0.02; 89% sensitivity; 41% specificity; Supplemental Figure 4). As shown in Supplemental Figure 4, binarization across different levels of use (≥25% drug-free urines, ≥75% drug-free urines) decreased sensitivity (57%, 25%, respectively) but increased specificity (71%, 89%, respectively).
Discussion
The translation of brain imaging findings into real-world clinical settings is one of the primary challenges of modern neuropsychiatry (7–9, 12, 13, 24). Here, we demonstrate the ability of a recently developed connectome-based machine learning approach to predict treatment outcomes (abstinence from cocaine during 12-week treatment) using baseline patterns of connectivity. We further demonstrate that post-treatment patterns of connectivity within these networks predict abstinence during six-month follow-up. Finally, we demonstrate that the same networks can be used to predict treatment response in an independent, heterogeneous sample. Despite this predictive ability, identified networks could be considered potential treatment targets (3, 5, 16), and further replication and model refinement is needed prior to direct application of findings to clinical decision-making.
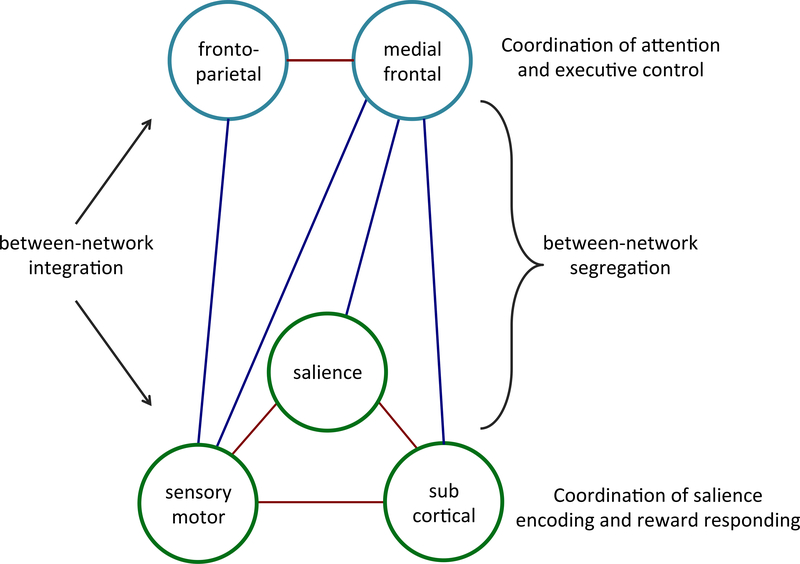
Consistent with the connectome-based approach, abstinence networks were complex and included connections between multiple well-established neural networks (17, 18). The positive network included more frontoparietal-medial frontal-default mode connections as well as more salience-subcortical-motor/sensory-connections. In contrast, the negative network (network for which increased connectivity is negatively associated with abstinence) included more connections between the medial frontal network and salience, subcortical, and motor/sensory networks, as well as more salience-default mode connections. Based on these findings, Figure 4 presents a theoretical network model of abstinence. We propose that abstinence is: (i) positively predicted by integration of an cognitive/executive control system involving increased connectivity between frontoparietal and medial frontal networks; (ii) by integration of a reward responsiveness system involving increased connectivity between salience, motor/sensory and subcortical networks; and (iii) by segregation (decreased connectivity) between these two systems. This model builds on prior models of addiction emphasizing separation of frontoparietal and salience networks (25, 26) but also incorporates medial frontal, motor/sensory and subcortical networks to provide a theoretical framework for future research.
Figure 4 – Five network model of abstinence.
Large-scale patterns of between-network connectivity for abstinence networks identified using CPM are summarized based on relative number of connections within positive (red) versus negative (blue) networks. Stronger connectivity (i.e., network integration) between frontoparietal and medial-frontal networks (top) and between sensory-motor, salience and subcortical networks (bottom) positively predicted within treatment abstinence. Weaker connectivity between these two systems (i.e., network segregation) also predicted more within treatment abstinence.
Within the above context, cognitive/executive control networks are theorized to contribute to abstinence via coordination of top-down processes necessary for treatment engagement (e.g., acquisition of new skills, enhanced control over impulsive behavior), whereas integration of reward networks may support motivational processes relevant to treatment (e.g., willingness to change, attending to alternate rewards) (3, 27). In addition, based on prior resting state work in cocaine-use disorder (28), appropriate separation between these two systems is theorized to relate to greater behavioral flexibility (or to decreased compulsivity), as would be required for behavior change during treatment.
While we did not model specific events-of-interest but rather used ‘raw’ time courses, our findings are nonetheless intuitive when considered within the context of reward task performance - which requires coordination of both attentional and cognitive control processes as well as of salience encoding and reward response behaviors (29, 30). Findings are further consistent with recent data prospectively linking medial prefrontal, frontoparietal and salience networks to cocaine relapse (5, 16), as well as with data from activation-based studies linking individual differences in brain reward responses to treatment outcomes in addiction (2, 6, 31). They further suggest that segregation of executive control/attention and salience/reward response systems within the context of MID task performance may be optimal for achieving abstinence from cocaine. More generally, these data add to emerging evidence that manipulation of brain states (e.g., via reward task performance) may be helpful in detecting individual differences in brain-behavior relationships (23). For example, CPMs derived from task-based data have consistently out-performed those derived from resting state data in non-addicted populations (32). However, further work across different brain states and in relation to diverse substance-use behaviors is needed to test this hypothesis within the specific context of addictions.
Connectivity strength within abstinence networks did not differ from pre- to posttreatment. Prior activation-based studies have demonstrated changes in neural responses following substance-use treatments; however, comparatively little is known about network-level changes with treatment. For example, individual differences in connectivity have been found to predict subsequent relapse to cocaine (5, 16, 33), yet no prior study has compared connectivity before and after treatment for cocaine-use-disorder. Our findings suggest relative stability of identified networks over 12-week treatment, raising the possibility that abstinence may be more closely linked to pre-treatment neural function than to within-treatment neuroplasticity. Within this context, it is possible that pre-treatment interventions influencing connectivity within the identified networks (e.g., cognitive training, targeted pharmacotherapies) may be helpful in promoting abstinence during treatment (34–37). For example, prior CPM work has demonstrated that connectivity strength within networks predictive of ADHD symptoms is changed following methylphenidate administration (19). Thus it is possible that effective treatments for addictions might also influence connectivity within complex networks.
It is further possible that networks contributing to treatment response are distinct from those directly implicated in disease pathology or that change with treatment. Brain regions predictive of treatment responses in other disorders often have limited overlap with regions consistently found to differentiate patients from controls (38). Clinically, factors that predict treatment response (e.g., motivation to change) may be distinct from those that change with treatment (e.g., acquisition of new skills). Thus, the same may be true for neural networks. Further, it is possible that changes within abstinence networks may take time to emerge and thus may only be detectable following treatment, as would be consistent with data indicating protracted emergence of treatment effects (39). Additional work is therefore needed to characterize network-level changes over time and in relation to addiction pathology, per se. Similarly, future studies should consider how ‘positive’ versus ‘negative’ networks might change over the course of treatment.
While continuous prediction approaches, which maximize individual differences, are optimal for feature selection in heterogeneous clinical samples (11), the practical value of predictive modeling within a clinical context will likely involve binary prediction (e.g., treatment responder versus non-responder). We therefore tested the ability of the identified networks to predict categorical outcomes (yes/no, drug negative urine), as well as to predict dimensional (percent drug negative urines) within-treatment abstinence in an independent, heterogeneous sample of individuals with cocaine-use disorder with and without concurrent methadone treatment. Connectivity within the identified networks successfully predicted both categorical and dimensional treatment response in our replication sample.
In our replication sample, our model had high sensitivity but low specificity. In this instance, low sensitivity would translate to under identification of responders (and thus under assignment of individuals to effective treatment), whereas low specificity would translate to under identification of non-responders (over-assignment to ineffective treatment). Given that multiple failed treatment attempts are common in addictions – and that only resources are lost in the instance of over assignment to ineffective treatment – maximizing sensitivity in this instance appears paramount.
Strengths and limitations
This study has several strengths, including use of a recently developed whole-brain predictive modeling approach, multiple time point fMRI data (pre- and post-treatment) and out-of-sample replication. However, several limitations should be noted. Some participants were excluded for missing data or excess motion during scanning, resulting in a relatively modest sample size for our primary analysis (N=53); thus, further work in larger samples is warranted, as noted above. In addition, the functional significance of the identified networks in relation to other aspects of substance-use pathology remains to be determined. While networks were relatively robust and not significantly changed in follow-up analyses controlling for other factors, we cannot entirely exclude the effects of other clinical variables, such as concurrent use of other substances or even acute intoxication, on connectivity strength. Given the relatively limited temporal specificity of urine toxicology analyses, future studies should consider incorporation of salivary testing for acute drug effects. In addition, further work will be needed to determine generalizability of these findings to fMRI data acquired during performance of different tasks and/or while the brain is ‘at-rest’. To avoid circularity, we did not test the ability of pre-treatment data to predict abstinence during follow-up; however, this will be an important next step for future studies (5). To facilitate replication, we have made the positive and negative abstinence network masks publicly available at our website (to be posted upon manuscript publication) (40).
Identified networks accounted for just under 20% of the variance in within treatment abstinence for novel subjects. While arguably somewhat modest, it is important to note that effect sizes estimates derived from ‘traditional’ statistical approaches – i.e., statistics applied to test explanatory hypotheses – are typically larger than those derived from machine learning approaches – i.e., statistics applied to predict unknown information (17, 41). Predictive models are less likely to overfit a specific dataset, leading to both increased likelihood of outof-sample-replication as well as typically decreased (more realistic) effect size estimates (42–44). Similarly, small effect sizes are found in mega-analyses with ~10,000 subjects (e.g., findings from the EGINMA project).
Conclusions
This study demonstrates that baseline patterns of whole-brain connectivity can predict a complex clinical outcome – in this case, cocaine abstinence. Consistent with the parent randomized controlled trial (20), participants had significant addiction histories including multiple prior quit-attempts, legal problems and concurrent methadone treatment for opioid-use disorder. Despite this clinically rich profile, baseline connectivity within the identified networks successfully predicted within-treatment abstinence, even after controlling for other baseline variables including other drug-use history and treatment assignment.
The predictive ability of these networks translated to a separate, heterogeneous sample of individuals (including non-methadone maintained individuals with cocaine-use disorder scanned prior to enrollment in a different treatment trial). These data demonstrate that individual differences in connectivity within large-scale neural networks implicated in cognitive/executive control and reward responsiveness processes contribute to variability in cocaine-use outcomes. As such, these ‘neural fingerprints’ may be an appropriate target for future intervention efforts.
Supplementary Material
Acknowledgment section:
The authors would like to thank Charla Nich and Karen Hunkele for help with non-imaging statistical analyses.
Disclosure of financial relationships: Drs. Yip and Scheinost report no financial relationships with commercial interest. Dr. Carroll is a member in trust of CBT4CBT LLC. Dr. Potenza has received financial support or compensation for the following: Dr. Potenza has consulted for and advised Lundbeck, Ironwood, Shire, INSYS, RiverMend Health, Opiant/Lakelight Therapeutics, and Jazz Pharmaceuticals; has received unrestricted research support from Mohegan Sun Casino and grant support from the National Center for Responsible Gaming and Pfizer pharmaceuticals; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; has consulted for legal and gambling entities on issues related to impulse control disorders; provides clinical care in the Connecticut Department of Mental Health and Addiction Services Problem Gambling Services Program; has performed grant reviews for the National Institutes of Health and other agencies; has edited journals and journal sections; has given academic lectures in grand rounds, CME events and other clinical or scientific venues; and has generated books or book chapters for publishers of mental health texts.
Funding: This work was supported by grants K01DA039299, P50DA09241 and R01DA035058 from the National Institute on Drug Abuse and by the National Center on Addiction and Substance Abuse.
References
- 1.Marhe R, Luijten M, van de Wetering BJ, Smits M, Franken IH: Individual differences in anterior cingulate activation associated with attentional bias predict cocaine use after treatment. Neuropsychopharmacol. 2013;38:1085–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balodis IM, Kober H, Worhunsky PD, Stevens MC, Pearlson GD, Carroll KM, Potenza MN: Neurofunctional Reward Processing Changes in Cocaine Dependence During Recovery. Neuropsychopharmacol. 2016;41:2112–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worhunsky PD, Stevens MC, Carroll KM, Rounsaville BJ, Calhoun VD, Pearlson GD, Potenza MN: Functional brain networks associated with cognitive control, cocaine dependence, and treatment outcome. Psychol Addict Behav. 2013;27:477–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yip SW, DeVito EE, Kober H, Worhunsky PD, Carroll KM, Potenza MN: Anticipatory reward processing among cocaine-dependent individuals with and without concurrent methadone-maintenance treatment: Relationship to treatment response. Drug Alcohol Depend. 2016;166:134–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Geng X, Hu Y, Gu H, Salmeron BJ, Adinoff B, Stein EA, Yang Y: Salience and default mode network dysregulation in chronic cocaine users predict treatment outcome. Brain. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moeller SJ, Paulus MP: Toward biomarkers of the addicted human brain: Using neuroimaging to predict relapse and sustained abstinence in substance use disorder. Progress in neuro-psychopharmacology & biological psychiatry. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yip S, Carroll K, Potenza M: An overview of translational approaches to the treatment of addictions in Neuroimaging and Psychosocial Addiction Treatment: An Integrative Guide for Researchers and Clinicians. Edited by Feldstein Ewing S, Witkiewitz K, Filbey F, Palgrave; 2015. [Google Scholar]
- 8.Garavan H, Brennan KL, Hester R, Whelan R: The neurobiology of successful abstinence. Curr Opin Neurobiol. 2013;23:668–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitfield-Gabrieli S, Ghosh SS, Nieto-Castanon A, Saygin Z, Doehrmann O, Chai XJ, Reynolds GO, Hofmann SG, Pollack MH, Gabrieli JD: Brain connectomics predict response to treatment in social anxiety disorder. Mol Psychiatry. 2016;21:680–685. [DOI] [PubMed] [Google Scholar]
- 10.Chung T, Noronha A, Carroll KM, Potenza MN, Hutchison K, Calhoun VD, Gabrieli JD, Morgenstern J, Nixon SJ, Wexler BE, Brewer J, Ray L, Filbey F, Strauman TJ, Kober H, Feldstein Ewing SW: Brain mechanisms of Change in Addictions Treatment: Models, Methods, and Emerging Findings. Current addiction reports. 2016;3:332–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gabrieli John DE, Ghosh Satrajit S, Whitfield-Gabrieli S: Prediction as a Humanitarian and Pragmatic Contribution from Human Cognitive Neuroscience. Neuron. 2015;85:11–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whelan R, Garavan H: When Optimism Hurts: Inflated Predictions in Psychiatric Neuroimaging. Biol Psychiatry. 2014;75:746–748. [DOI] [PubMed] [Google Scholar]
- 13.Shen X, Finn ES, Scheinost D, Rosenberg MD, Chun MM, Papademetris X, Constable RT: Using connectome-based predictive modeling to predict individual behavior from brain connectivity. Nat Protocols. 2017;12:506–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vul E, Harris C, Winkielman P, Pashler H: Puzzlingly High Correlations in fMRI Studies of Emotion, Personality, and Social Cognition. Perspectives on psychological science : a journal of the Association for Psychological Science. 2009;4:274–290. [DOI] [PubMed] [Google Scholar]
- 15.O'Halloran L, Nymberg C, Jollans L, Garavan H, Whelan R: The potential of neuroimaging for identifying predictors of adolescent alcohol use initiation and misuse. Addiction. 2017;112:719–726. [DOI] [PubMed] [Google Scholar]
- 16.McHugh MJ, Gu H, Yang Y, Adinoff B, Stein EA: Executive control network connectivity strength protects against relapse to cocaine use. Addict Biol. 2016. [DOI] [PubMed] [Google Scholar]
- 17.Finn ES, Shen X, Scheinost D, Rosenberg MD, Huang J, Chun MM, Papademetris X, Constable RT: Functional connectome fingerprinting: identifying individuals using patterns of brain connectivity. Nat Neurosci. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenberg MD, Finn ES, Scheinost D, Papademetris X, Shen X, Constable RT, Chun MM: A neuromarker of sustained attention from whole-brain functional connectivity. Nat Neurosci. 2016;19:165–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenberg MD, Zhang S, Hsu WT, Scheinost D, Finn ES, Shen X, Constable RT, Li CS, Chun MM: Methylphenidate Modulates Functional Network Connectivity to Enhance Attention. J Neurosci. 2016;36:9547–9557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carroll KM, Nich C, Devito EE, Shi JM, Sofuoglu M: Galantamine and Computerized Cognitive Behavioral Therapy for Cocaine Dependence: A Randomized Clinical Trial. J Clincal Psychiatry. 2018;doi: 10.4088/JCP.17m11669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andrews MM, Meda SA, Thomas AD, Potenza MN, Krystal JH, Worhunsky P, Stevens MC, O'Malley S, Book GA, Reynolds B, Pearlson GD: Individuals Family History Positive for Alcoholism Show Functional Magnetic Resonance Imaging Differences in Reward Sensitivity That Are Related to Impulsivity Factors. Biol Psychiatry. 2011;69:675–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shen X, Tokoglu F, Papademetris X, Constable RT: Groupwise whole-brain parcellation from resting-state fMRI data for network node identification. Neuroimage. 2013;82:403–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Finn ES, Scheinost D, Finn DM, Shen X, Papademetris X, Constable RT: Can brain state be manipulated to emphasize individual differences in functional connectivity? Neuroimage. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gabrieli JD, Ghosh SS, Whitfield-Gabrieli S: Prediction as a humanitarian and pragmatic contribution from human cognitive neuroscience. Neuron. 2015;85:11–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sutherland MT, McHugh M, Pariyadath V, Stein EA: Resting State Functional Connectivity in Addiction: Lessons Learned and a Road Ahead. NeuroImage. 2012;62:2281–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pariyadath V, Gowin JL, Stein EA: Chapter 8 - Resting state functional connectivity analysis for addiction medicine: From individual loci to complex networks in Progress in brain research. Edited by Hamed E, Martin PP, Elsevier; 2016. pp. 155–173. [DOI] [PubMed] [Google Scholar]
- 27.Carroll KM, Rounsaville BJ: Behavioral therapies: The glass would be half full if only we had a glass. in Rethinking Substance Abuse: What the Science Shows, and What We Should Do About It Edited by Miller W, Carroll K. New York, The Guilford Press; 2006. pp. 223–239. [Google Scholar]
- 28.Hu Y, Salmeron B, Gu H, Stein EA, Yang Y: Impaired functional connectivity within and between frontostriatal circuits and its association with compulsive drug use and trait impulsivity in cocaine addiction. JAMA psychiatry. 2015;72:584–592. [DOI] [PubMed] [Google Scholar]
- 29.Balodis IM, Potenza MN: Anticipatory Reward Processing in Addicted Populations: A Focus on the Monetary Incentive Delay Task. Biol Psychiatry. 2015;77:434–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Knutson B, Fong GW, Adams CM, Varner JL, Hommer D: Dissociation of reward anticipation and outcome with event-related fMRI. Neuroreport. 2001;12:3683–3687. [DOI] [PubMed] [Google Scholar]
- 31.Moeller SJ, Tomasi D, Woicik PA, Maloney T, Alia-Klein N, Honorio J, Telang F, Wang GJ, Wang R, Sinha R, Carise D, Astone-Twerell J, Bolger J, Volkow ND, Goldstein RZ: Enhanced midbrain response at 6-month follow-up in cocaine addiction, association with reduced drug-related choice. Addict Biol. 2012;17:1013–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greene A, Gao S, Scheinost D, Constable R: Task-induced brain state manipulation improves prediction of individual traits. Nature communications. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McHugh MJ, Demers CH, Salmeron BJ, Devous MD, Stein EA, Adinoff B: CorticoAmygdala Coupling as a Marker of Early Relapse Risk in Cocaine-Addicted Individuals. Front Psychiatry. 2014;5:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Konova AB, Moeller SJ, Tomasi D, Goldstein RZ: Effects of chronic and acute stimulants on brain functional connectivity hubs. Brain Res. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sofuoglu M, DeVito EE, Waters AJ, Carroll KM: Cognitive enhancement as a treatment for drug addictions. Neuropharmacol. 2013;64:452–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kiluk BD, Buck MB, Devore KA, Babuscio TA, Nich C, Carroll KM: Performance-Based Contingency Management in Cognitive Remediation Training: A Pilot Study. J Subst Abuse Treat. 2017;72:80–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bickel WK, Yi R, Landes RD, Hill PF, Baxter C: Remember the future: working memory training decreases delay discounting among stimulant addicts. Biol Psychiatry. 2011;69:260–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Doehrmann O, Ghosh SS, Polli FE, Reynolds GO, Horn F, Keshavan A, Triantafyllou C, Saygin ZM, Whitfield-Gabrieli S, Hofmann SG, Pollack M, Gabrieli JD: Predicting treatment response in social anxiety disorder from functional magnetic resonance imaging. JAMA psychiatry. 2013;70:87–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carroll K, Nich C, Ball SA, McCance-Katz EF, Frankforter TF, Rounsaville BJ: One year follow-up of disulfiram and psychotherapy for cocaine-alcohol abusers: Sustained effects of treatment. Addiction. 2000;95:1335–1349. [DOI] [PubMed] [Google Scholar]
- 40.Woo C-W, Chang LJ, Lindquist MA, Wager TD: Building better biomarkers: brain models in translational neuroimaging. Nat Neurosci. 2017;20:365–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shmueli G: To Explain or to Predict? Statistical Science. 2010;25:289–310. [Google Scholar]
- 42.Whelan R, Garavan H: When optimism hurts: inflated predictions in psychiatric neuroimaging. Biol Psychiatry. 2014;75:746–748. [DOI] [PubMed] [Google Scholar]
- 43.Yarkoni T, Westfall J: Choosing Prediction Over Explanation in Psychology: Lessons From Machine Learning. Perspectives on psychological science : a journal of the Association for Psychological Science. 2017;12:1100–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cremers HR, Wager TD, Yarkoni T: The relation between statistical power and inference in fMRI. PLoS One. 2017;12:e0184923. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.