ABSTRACT
The cytological and biochemical examination of cerebrospinal fluid (CSF) has been used for the presumed diagnosis of bacterial meningitis until the final microbiological results are achieved. We assessed the ability of CSF lactate in comparison with other CSF parameters to discriminate bacterial and enteroviral community acquired meningitis. We included 1,187 CSF samples of acute community-acquired meningitis, being 662 cases of bacterial and 525 of enteroviral meningitis. Lactate concentration (mg/dL), leukocyte count/mm3, protein (mg/dL), and glucose (mg/dL) were compared between bacterial and viral meningitis. Receiver operator characteristic (ROC) curves were used to assess diagnostic performance. CSF leukocytes, CSF protein and CSF lactate were significantly higher in bacterial meningitis cases (P<0.0001). CSF glucose was significantly lower in bacterial meningitis cases (P<0.0001). CSF lactate showed the best predictive ability with an area under the curve of 0.944 (95% CI 0.929 – 0.959). Considering a cut off of CSF lactate of 30 mg/dL, the sensitivity and specificity for bacterial meningitis were 84.1% and 99%, respectively. In the cytological and biochemical CSF analysis, CSF lactate was the most accurate marker for bacterial meningitis.
KEYWORDS: Meningitis, Bacterial meningitis, Cerebrospinal fluid, Lactate
Bacteria and enteroviruses are the main cause of acute community-acquired meningitis. Bacterial meningitis is associated with high morbidity and mortality. Prompt treatment with appropriate antibiotics is essential to optimize outcomes. Early diagnosis is therefore crucial for selecting patients who need antibiotics 1 – 3 . On the other hand, the course of viral meningitis is in general benign and there is usually no specific treatment 4 .
The diagnosis of bacterial meningitis is based on blood and cerebrospinal fluid cultures, Gram staining and bacterial antigen detection by latex agglutination. Gram staining and latex agglutination may lead to false-negative results and culture may take a few days for a definitive result 1 – 3 ; therefore, empiric antibiotic treatment is often initiated until the final etiologic determination is accomplished. Cytological and biochemical analysis of cerebrospinal fluid (CSF) may contribute in this way since there are findings that indicate greater likelihood of bacterial etiology 5 . Highly elevated white blood cell (WBC) count with predominance of neutrophils, decreased CSF/serum glucose ratio and increased CSF protein concentration are suggestive of bacterial meningitis 6 . High CSF lactate has also been pointed out as an early marker of bacterial meningitis 7 . However, the precise diagnostic value of lactate compared to other CSF parameters has not yet been established 8 – 11 .
In the present study we aimed to evaluate the sensitivity of CSF lactate determination in the distinction between bacterial meningitis and enteroviral meningitis in comparison with other CSF parameters.
CSF samples collected from patients with acute meningitis from 2013 to 2017 were included in the analysis. The CSF samples were obtained from patients with suspected meningitis. The CSF collection and analyzes were all performed by Senne Líquor Diagnóstico. CSF analysis included cytological, biochemicaland microbiological evaluation. Data included in the present analysis were obtained from the Senne Líquor Diagnóstico database and included leukocyte count (mm3), protein (mg/dL), glucose (mg/dL) and lactate concentration (mg/dL).
The definition of bacterial meningitis took into account the bacterioscopy, bacterial antigen latex agglutination testand CSF bacterial culture. CSF positivity in at least one of these three methods for Streptococcus pneumoniae, Neisseria meningitidisor Haemophilus influenza was considered bacterial meningitis.
The definition of enterovirus meningitis was achieved by means of enterovirus PCR. PCR was performed according to a previous description 12 . The cases in which PCR was positive were considered of enteroviral etiology. Cases of non enterovirus meningitis were not included in this analysis.
An informed consent form was applied to study participants. The normality of data was assessed by the Kolmogorov-Smirnov test. Mean CSF leukocyte, protein, glucose and lactate of bacterial and enteroviral meningitis were compared with the t test. A sensitivity analysis was conducted to compare the ability of these four variables to predict bacterial meningitis. The area under the receiver operator characteristic curves (AUROC) and 95% confidence intervals (CI) were used to calculate the predictive ability of parameters. Statistical analysis was performed using the SPSS version 17.0 for Windows (IBM, USA). The significance level was set at P<0.05.
CSF samples from 1,187 patients were included in the analysis, 662 had bacterial meningitis and 525 had enteroviral meningitis. The mean patients age was 16.3619.21 for bacterial meningitis and 12.48±12.41 for enterovirus meningitis (P=0.263). In the bacterial meningitis group, the percentage of male patients was 56.7% and in the bacterial meningitis group 78.6% (P=0.119). The mean±SD values of leukocytes, protein, glucose and lactate in bacterial and enteroviral meningitis are shown in Table 1.
Table 1. Comparison of cytological and biochemical parameters between bacterial and viral meningitis.
| CSF parameter | Etiology | Mean±SD | P |
|---|---|---|---|
| Leukocytes/mm3 | Bacterial | 5,749.88±27,512.03 | <0.0001 |
| Viral | 306.40±424.38 | ||
| Protein (mg/dL) | Bacterial | 424.09±645.91 | <0.0001 |
| Viral | 46.76±29.05 | ||
| Glucose (mg/dL) | Bacterial | 30.68±31.22 | <0.0001 |
| Viral | 52.80±13.45 | ||
| Lactate (mg/dL) | Bacterial | 87.28±58.85 | <0.0001 |
| Viral | 17.76±4.55 |
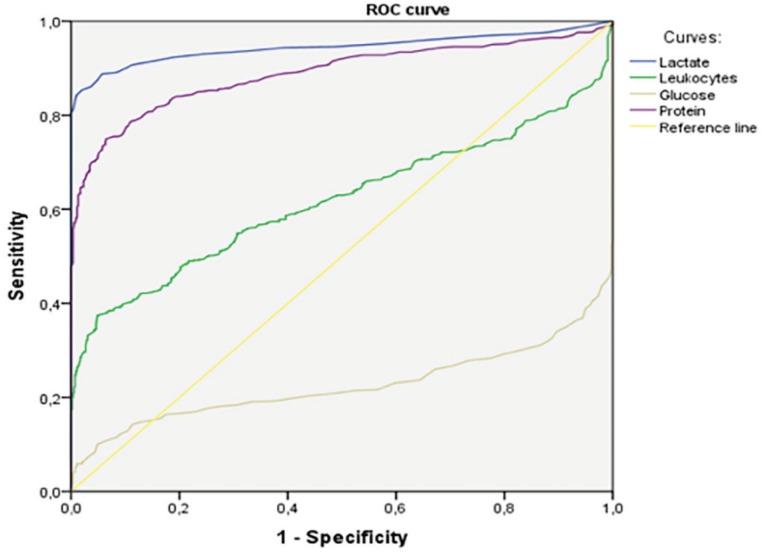
Receiver operator characteristic curves were used to assess the diagnostic accuracy for bacterial meningitis of cytological and biochemical parameters. Figure 1 shows the area under the curve (AUC) for CSF leukocytes, CSF glucose and CSF lactate. The best performing parameter was the CSF lactate.
Figure 1. Receiver Operator Characteristic (ROC) curves of CSF biomarkers. Areas under the curve (AUC) of cerebrospinal fluid markers of bacterial meningitis were: CSF lactate (AUC 0.944; 95% CI 0.929 – 0.959), CSF leukocytes (AUC 0.620; 95% CI 0.588 – 0.653), CSF protein (AUC 0.889; 95% CI 0.869 – 0.909) and CSF glucose (AUC 0.225; 95% CI 0.196 – 0.254).
CSF lactate showed to be the best single CSF parameter to predict bacterial meningitis. CSF lactate above 30 mg/dL was very sensitive and highly specific for the diagnosis of bacterial meningitis. These findings are in line with previous studies 8 – 11 . Li and cols. found higher CSF lactate levels in patients with bacterial meningitis than in patients with viral meningitis. However, that study included only post-neurosurgical bacterial meningitis and not community acquired meningitis 11 . In a prospective observational study, Buch et al. 9 showed that lactate was more accurate than other CSF markers to identify bacterial meningitis. However, the authors compared CSF lactate between patients with bacterial meningitis and patients with aseptic meningitis, including in this last category patients with proven viral etiology and patients with aseptic meningitis of unknown etiology 11 . Pires et al. 10 found lactate as the best single CSF marker of bacterial meningitis with high sensitivity and specificity of CSF lactate above 30 mg/dL in a pediatric population. Our findings confirm the findings of previous studies showing CSF lactate as the best CSF marker of bacterial meningitis. Unlike the study from Buch et al. 9 , we only included cases with proven bacterial or enteroviral etiology and we did not include patients with meningitis of unknown etiology. In addition, we did not limit our study to the pediatric population. Furthermore, we included only community-acquired meningitis, excluding hospital-acquired and post-neurosurgical meningitis. Therefore, our data strongly reinforce the high positive predictive value of CSF lactate for diagnosing acute bacterial meningitis.
Our study has limitations that deserve to be mentioned. The present study was retrospective and did not include clinical data. However, the significant number of CSF samples analyzed and the strict definition criteria used for bacterial and viral etiologies could be considered as a strength of the study. We did not include other etiologies of viral meningitis than enteroviruses; therefore, we were unable to compare CSF parameters including lactate between bacterial and aseptic meningitis of other etiologies. However, enterovirus meningitis comprises the majority of aseptic meningitis in our country 13 . This choice of including only enterovirus confirmed cases was made because many of the non-enteroviral suspected meningitis of viral etiology are not confirmed and remain presumed. Moreover, other meningitis-associated virus, such as Flaviviruses, are not systematically tested in our laboratory. Other viruses, such as herpes viruses, are frequently associated with encephalitis rather than meningitis. The inclusion of aseptic meningitis of unknown etiology or cases of encephalitis could reduce the accuracy of CSF data comparison between viral and bacterial community-acquired meningitis etiologies.
In conclusion, CSF lactate, whose determination is simple and fast, has great value in the discrimination between bacterial and viral meningitis.
REFERENCES
- 1.van Ettekoven CN, van de Beek D, Brouwer MC. Update on community-acquired bacterial meningitis guidance and challenges. Clin Microbiol Infect. 2017;23:601–606. doi: 10.1016/j.cmi.2017.04.019. [DOI] [PubMed] [Google Scholar]
- 2.van de Beek D, de Gans J, Tunkel AR, Wijdicks EF. Community-acquired bacterial meningitis in adults. N Engl J Med. 2006;354:44–53. doi: 10.1056/NEJMra052116. [DOI] [PubMed] [Google Scholar]
- 3.van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med. 2004;351:1849–1859. doi: 10.1056/NEJMoa040845. [DOI] [PubMed] [Google Scholar]
- 4.McGill F, Griffiths MJ, Solomon T. Viral meningitis current issues in diagnosis and treatment. Curr Opin Infect Dis. 2017;30:248–256. doi: 10.1097/QCO.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 5.Heckenberg SG, Brouwer MC, van de Beek D. Bacterial meningitis. Handb Clin Neurol. 2014;121:1361–1375. doi: 10.1016/B978-0-7020-4088-7.00093-6. [DOI] [PubMed] [Google Scholar]
- 6.Mount HR, Boyle SD. Aseptic and bacterial meningitis: evaluation, treatment, and prevention. Am Fam Physician. 2017;96:314–322. [PubMed] [Google Scholar]
- 7.Nazir M, Wani WA, Malik MA, Mir MR, Ashraf Y, Kawoosa K, et al. Cerebrospinal fluid lactate a differential biomarker for bacterial and viral meningitis in children. J Pediatr (Rio J). 2018;94:88–92. doi: 10.1016/j.jped.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 8.Sanaei Dashti A, Alizadeh S, Karimi A, Khalifeh M, Shoja SA. Diagnostic value of lactate, procalcitonin, ferritin, serum-C-reactive protein, and other biomarkers in bacterial and viral meningitis a cross-sectional study. Medicine (Baltimore). 2017;96:e7637. doi: 10.1097/MD.0000000000007637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buch K, Bodilsen J, Knudsen A, Larsen L, Helweg-Larsen J, Storgaard M, et al. Cerebrospinal fluid lactate as a marker to differentiate between community-acquired acute bacterial meningitis and aseptic meningitis/encephalitis in adults a Danish prospective observational cohort study. Infect Dis (Lond). 2018;50:514–521. doi: 10.1080/23744235.2018.1441539. [DOI] [PubMed] [Google Scholar]
- 10.Pires FR, Franco AC, Gilio AE, Troster EJ. Use of score and cerebrospinal fluid lactate dosage in the differential diagnosis of bacterial and aseptic meningitis. Rev Paul Pediatr. 2017;35:369–374. doi: 10.1590/1984-0462/;2017;35;4;00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Y, Zhang G, Ma R, Du Y, Zhang L, Li F, Fang F, et al. The diagnostic value of cerebrospinal fluids procalcitonin and lactate for the differential diagnosis of post-neurosurgical bacterial meningitis and aseptic meningitis. Clin Biochem. 2015;48:50–54. doi: 10.1016/j.clinbiochem.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Casaroto E, Marra AR, Coelho FM, Pinho JR, Sitnik R, Colombari F, et al. Improving the diagnosis of meningitis due to enterovirus and herpes simplex virus I and II in a tertiary care hospital. BMC Infect Dis. 2013;13:487–487. doi: 10.1186/1471-2334-13-487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Soares CN, Cabral-Castro MJ, Peralta JM, de Freitas MR, Zalis M, Puccioni-Sohler M. Review of the etiologies of viral meningitis and encephalitis in a dengue endemic region. J Neurol Sci. 2011;303:75–79. doi: 10.1016/j.jns.2011.01.012. [DOI] [PubMed] [Google Scholar]