Abstract
Background:
Past research suggests self-harm/suicidality are more common among adults who have undergone bariatric surgery than the general population.
Objectives:
To compare prevalence of self-harm/suicidal ideation over time and identify pre-surgery risk factors for post-surgery self-harm/suicidal ideation.
Setting:
The Longitudinal Assessment of Bariatric Surgery-2 is a cohort study with pre-surgery and annual post-surgery assessments conducted at ten US hospitals.
Methods:
Adults with severe obesity undergoing bariatric surgery between March, 2006 and April, 2009 (N=2458). Five-year follow-up is reported. Self-reported history of suicidality assessed retrospectively via the Suicide Behavior Questionnaire-Revised (SBQ-R) and self-reported self-harm/suicidal ideation assessed prospectively via the Beck Depression Inventory-1 (BDI-1).
Results:
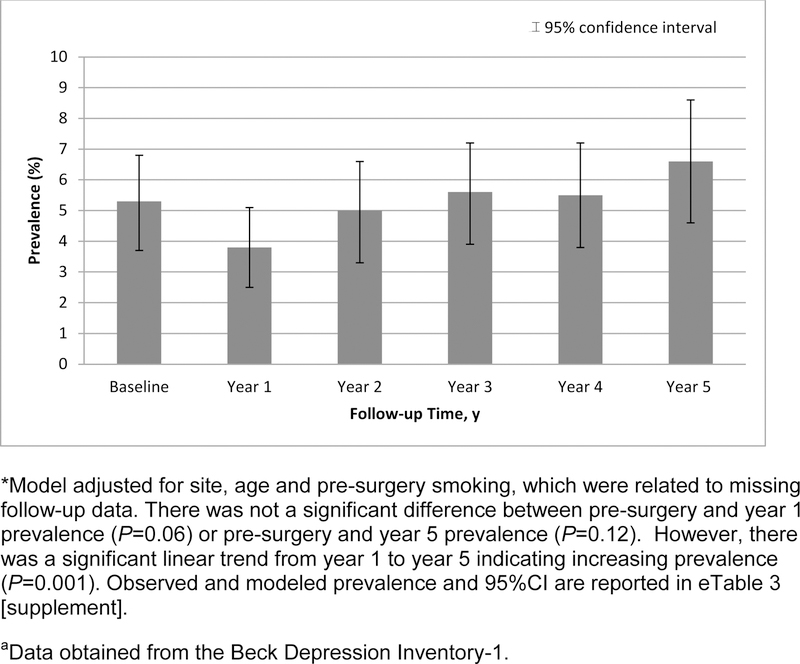
The SBQ-R was completed by 1540 participants; 2217 completed the BDI-1 pre- and post-surgery. Over 75% of participants were female, with a median age of 46 years and body mass index of 45.9 kg/m2. Approximately one-fourth of participants (395/1534) reported a pre-surgery history of suicidal thoughts and/or behavior (SBQ-R). The prevalence of self-harm/suicidal ideation (BDI-1) was 5.3% (95% CI, 3.7–6.8) pre-surgery and 3.8% (95% CI, 2.5–5.1) at year-1 post-surgery (P=.06). Prevalence increased over time post-surgery to 6.6% (95% CI, 4.6–8.6) at year-5 (P=0.001) but was not significantly different than pre-surgery (P=.12).
Conclusions:
A large cohort of adults with severe obesity who underwent bariatric surgery had a prevalence of self-harm/suicidal ideation that may have decreased in the first post-operative year but increased over time to pre-surgery levels, suggesting screening for self-harm/suicidality is warranted throughout long-term post-operative care. Several risk factors were identified that may help with enhanced monitoring.
Keywords: suicide, bariatric surgery, suicidal ideation, obesity
Approximately 15% of U.S. adults have severe obesity (body mass index; BMI≥35 kg/m²).(1) Bariatric surgery, the most effective and enduring treatment, typically results in sustained weight loss and improvement in multiple health domains with low short-term risk.(2–3) Bariatric surgery patients have reduced long-term all-cause mortality when compared to non-bariatric surgical controls with severe obesity.(4) However, concerns about suicide risk following bariatric surgery have emerged.(4,5)
A review and meta-analysis of post-bariatric surgery suicides revealed a four-fold higher rate when compared to the general population,(5) which may be attributable to bariatric surgery patients having more pre-surgery suicide risk factors than the general population.(6–10) One study(11) reported higher rates of self-harm hospitalizations among bariatric surgery patients than the general population,(12) but no change in self-harm hospitalization rates pre- to post-bariatric surgery, while another reported a higher rate of self-harm emergencies post-surgery than pre-surgery.(13) Hypothesized mechanisms for potentially elevated rates of self-harm or suicide following surgery include disappointment with weight loss or regain and changes in absorption of medication, alcohol kinetics, peptides and hormones, impulsivity, health-related quality of life, and sexual functioning.(10,14) There is also some evidence that suicide attempt risk is higher following Roux-en-Y gastric bypass [RYGB] in particular.(15) However, a recent meta-analysis did not find a difference in pooled suicide prevalence by type of bariatric surgical procedure (i.e. restrictive, malabsorptive or both).(16)
Most studies of self-harm/suicide in the bariatric surgery population have used cross-sectional/retrospective data and lack sufficient detail about suicidal intent.(14,17) Using five-year follow-up data from a multi-center longitudinal study of adults undergoing bariatric surgery, we aimed to evaluate changes in the prevalence of self-harm/suicidal ideation pre- to post-surgery and during the post-surgery period and to identify factors associated with post-surgery self-harm/suicidal ideation risk. We also examined participants’ suicidality history and described post-surgery suicides.
Methods
Participants
The Longitudinal Assessment of Bariatric Surgery-2(18) is an observational cohort study and is registered at: https://www.clinicaltrials.gov/ct2/show/NCT00465829. Adult patients seeking a first bariatric surgery by participating surgeons at 10 hospitals at 6 clinical centers throughout the U.S. were recruited between February, 2006 and February, 2009. Protocols were approved by the Institutional Review Boards at each center, and all participants provided written informed consent. By close of enrollment (April, 2009), 2458 participants underwent bariatric surgery. The flow of participants is shown in eFigure 1 [supplement].
Unless otherwise noted, measures were collected following the surgery approval process within 30 days prior to surgery and annually, following surgery. Participants were informed that their responses were confidential except in cases of potential serious harm. If participants reported suicidal ideation in the past week or any future self-harm intent, medical personnel conducted a risk assessment and contacted emergency services as necessary. Study forms are available at https://repository.niddk.nih.gov/studies/labs/Forms/.
Measures
SBQ-R.
The Suicidal Behavior Questionnaire-Revised (SBQ-R)(19) measures past suicidal thoughts/behaviors and future suicide risk. It was completed at the year-4 or year-5 assessment. One item asked if participants had “thought about or attempted to kill yourself,” any time pre-surgery and another item assessed this with a “since surgery” timeframe. Those who completed the SBQ-R at year-4 completed a past-year version of the questionnaire at year-5 that was used to update the “since surgery” status to represent the previous five years. Due to low frequencies for each of the six response categories, they were collapsed into four categories indicating ‘never,’ ‘brief passing thought,’ ‘had plan’ (combining the response options ‘I had a plan at least once to kill myself but did not try to do it’ and ‘I had a plan at least once to kill myself and really wanted to die’), and ‘had prior attempt’ (combining the response options ‘I have attempted to kill myself, but did not want to die’ and ‘I have attempted to kill myself and really hoped to die,’ with the latter three categories indicating ‘suicidality.’
BDI-1.
The Beck Depression Inventory-Version 1 (BDI-1) measures depression symptoms(20,21) and includes an item about thoughts and plans of self-harm/suicide within the past week. The response, “I don’t have any thoughts of harming myself,” was coded as ‘no self-harm/suicidal ideation.’ Due to low frequency of the other five response options, they were collapsed to indicate ‘self-harm/suicidal ideation.’
Suicide deaths.
Vital status was determined through annual study follow-up. A query of the National Death Index, a database of death records on file in state vital statistics offices (http://www.cdc.gov/nchs/ndi.htm), was performed through 2014. Causes of death were adjudicated by committee using all available sources (medical records, autopsy report, death certificate). In cases of inadequate information for adjudication, the death certificate cause was used. Suicide was defined as death adjudicated as “definite” suicide. Potential suicide was defined as death adjudicated as “probable” suicide, “definite” or “probable” alcohol or drug poisoning with unknown intent or non-adjudicated deaths with intentional self-harm or alcohol or drug poisoning as cause of death on the certificate.
Other Measures.
Sociodemographic data were self-reported on study-specific questionnaires.(18) Participants underwent weight measurement to the nearest pound and height to the nearest inch using a wall-mounted stadiometer, which was used to calculate baseline BMI (kg/m²) and percent weight loss: 100*(baseline weight-follow-up weight)/baseline weight.
Diabetes, hypertension, dyslipidemia, and sleep apnea status were determined using laboratory values, physical examination measures, participant report, and comorbid diagnoses from healthcare providers and medical records. Severe walking limitation was defined as the self-reported inability to walk 200 feet without assistance. The Medical Outcomes Study 36-item Short-Form Health Survey (SF- 36)(22) is a generic measure of functional health. Using norm-based methods, the general health and bodily pain domain scores of the Medical Outcomes Study 36-item Short-Form Health Survey (SF- 36),(22) a generic measure of functional health, were used to transform participant scores to a mean of 50 and standard deviations of 10 in the general U.S. population; higher scores indicating better functioning. Perceived social support was measured using the belonging domain score from the 12-item Interpersonal Support Evaluation List (ISEL-12); a higher score (range 1–12) indicating greater support availability.(23) Sexual dissatisfaction was defined as self-report of being “dissatisfied” or “very dissatisfied” with overall sexual life on a study-specific questionnaire.(24) Past-week depressive symptomatology was measured with the BDI-1; a higher score (range 0–63) reflected greater severity.(20)
Smoking and illicit drug use were assessed with the LABS-2 Behavioral Form.(25) Regular alcohol consumption (i.e., ≥ twice/week) and alcohol use disorder (AUD) symptoms were determined using the Alcohol Use Disorders Identification Test (AUDIT).(25,26) The therapeutic classes of prescription medications and frequency information were used to identify participants currently taking opioid analgesic medication, anti-anxiety medication, or anti-depressant medications at least daily. Past-year counseling and lifetime history of hospitalizations for psychiatric or emotional problems were assessed with the LABS-2 Psychiatric and Emotional Test Survey.(25)
Data Analytic Strategy
Analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA). All reported P values are two-tailed; P values less than 0.05 were considered statistically significant.
Potential selection bias due to missing data was examined by comparing pre-surgery characteristics of those in the SBQ-R and BDI-1 analysis samples to those not in the respective analysis samples using Pearson’s chi-squared test, the Cochran-Armitage test, or the Wilcoxon rank sum test for categorical, ordinal, and continuous variables, respectively.
A mixed-effects ordinal logistic regression model was used to determine pre-surgery predictors of suicidality in the five years post-surgery. Due to the low frequency of suicide ‘plans’ and ‘attempts,’ these two categories were collapsed resulting in three categories (i.e., no thoughts/plans/attempts, thoughts only, and plans/attempts). The parallelism assumption (constant odds of being in the next more severe category of suicidality) was tested and was not violated. Based on the literature,(5,10,14,27) these pre-surgery variables were considered: suicidality history, self-harm/suicidal ideation, age, sex, race, ethnicity, marital status, education, unemployment, household income, BMI, diabetes, hypertension, dyslipidemia, sleep apnea, severe walking limitation, SF-36 general health score, SF-36 bodily pain score, ISEL belongingness score, dissatisfaction with sexual life, BDI-1 depressive symptoms score, smoking status, regular alcohol consumption, AUD symptoms, illicit drug use, prescription opioid use, anti-anxiety medication use, anti-depressant medication use, psychiatric counseling, and lifetime history of psychiatric hospitalization. Due to the large number of variables under consideration, a model with each factor was tested first. Next, factors with P<0.20 were entered into a multivariate model with site as a random effect and surgical procedure (RYGB, LAGB, other) as a fixed effect and retained if significant.
Among those in the BDI-1 sample, longitudinal analyses were performed with mixed models with a person-level random intercept. Models controlled for site, age, and pre-surgery smoking status, which were associated with missing follow-up data(28) as fixed effects. Sensitivity analyses were performed to examine the robustness of results with respect to the missing at random assumption (eAppendix 1 [Supplement]).
A Poisson mixed model with robust error variance was used to estimate self-harm/suicidal ideation and test for differences by time point. Pairwise comparisons were made between pre-surgery vs. year-1 and pre-surgery vs. year-5. Stability in the estimates of self-harm/suicidal ideation following surgery was evaluated by testing for linear and quadratic trends from year-1 to year-5. P-values were adjusted to control for overall type I error.(29)
Poisson mixed models with robust error variance were also used to determine factors related to post-surgery self-harm/suicidal ideation with time entered as a discrete fixed effect. First, a pre-surgery model was constructed using the same pre-surgery variables and same model building strategy described above. Because the pre-surgery suicidality history was missing for approximately one-third of the BDI-1 sample, a three-category variable was created with missing recoded to unknown. A second model was constructed to identify pre-to-post-surgery changes independently associated with post-surgery self-harm/suicidal ideation, controlling for pre-surgery factors identified in the previous analysis. The following variables were considered: pre-to-post-surgery change in SF-36 general health score, SF-36 bodily pain score, ISEL belongingness score and BDI-1 depression symptoms score, with control for the corresponding pre-surgery values, post-surgery marital status, unemployment status, household income, diabetes, hypertension, dyslipidemia, sexual life dissatisfaction, smoking, regular alcohol consumption, AUD symptoms, illicit drug use, prescription opioid use, anti-anxiety medication use, anti-depressant medication use, psychiatric counseling, with consideration for pre-surgery status (e.g., became single vs. stayed married, became unemployed vs. remained employed). Interactions between time and covariates were tested and retained if significant.
Results
Sixty-three percent (n=1540) of participants completed the SBQ-R at five years post-surgery, while ninety percent (N=2217) completed the BDI-1 item pre-surgery and at least one follow-up (eFigure 1 [supplement]). A comparison of pre-surgery characteristics between those included and excluded from the analysis samples is provided in eTable 1 [supplement]. The proportion reporting self-harm/suicidal ideation at the pre-surgery assessment was similar for those who completed vs. did not complete the SBQ-R.
Characteristics of LABS-2 participants and the SBQ-R and BDI-1 analysis samples are shown in Table 1. The majority of participants (N=1738) underwent RYGB, followed by LAGB (N=610).
Table 1.
Pre-surgery Characteristics of Participants in the Longitudinal Assessment of Bariatric Surgery-2 Study and in the SBQ-R and BDI-1 Analysis Samples.
| LABS-2 sample (N=2458)a | SBQ-R analysis sample (N=1540)a | BDI-1 analysis sample (N=2217)a | |||||
|---|---|---|---|---|---|---|---|
| No. | (%)b | No. | (%)b | No. | (%)b | ||
| Age, years, median (25th, 75th) | 46.0 | (37.0, 54.0) | 48.0 | (38.0, 56.0) | 46.0 | (37.0, 55.0) | |
| Female | 1931 | (78.6) | 1220 | (79.2) | 1743 | (78.6) | |
| White racec, No./total (%) | 2102/2433 | (86.4) | 1308/1526 | (85.7) | 1897/2196 | (86.4) | |
| Hispanic/Latino ethnicity, No./total (%) | 119/2456 | (4.8) | 76/1539 | (4.9) | 106/2216 | (4.8) | |
| Married or living as married, No./total (%) | 1444/2264 | (63.8) | 907/1427 | (63.6) | 1324/2083 | (63.6) | |
| Education | (n=2334) | (n = 1428) | (n = 2082) | ||||
| High school or less | 521 | (23.0) | 344 | (24.1) | 478 | (23.0) | |
| Some college/post high school education | 918 | (40.5) | 558 | (39.1) | 844 | (40.5) | |
| College degree or higher | 825 | (36.4) | 526 | (36.8) | 760 | (36.5) | |
| Unemployed, No./total (%) | 86/2257 | (3.8) | 41/1425 | (2.9) | 79/2076 | (3.8) | |
| Household income | (n=2204) | (n = 1387) | (n = 2029) | ||||
| Less than $25,000 | 402 | (18.2) | 257 | (18.5) | 370 | (18.2) | |
| $25,000-$49,999 | 568 | (25.8) | 356 | (25.7) | 522 | (25.7) | |
| $50,000-$74,999 | 522 | (23.7) | 321 | (23.1) | 467 | (23.0) | |
| $75,000-$99,999 | 353 | (16.0) | 226 | (16.3) | 329 | (16.2) | |
| $100,000-$199,999 | 292 | (13.2) | 191 | (13.8) | 282 | (13.9) | |
| $200,000 or more | 67 | (3.0) | 36 | (2.6) | 59 | (2.9) | |
| Body mass indexd, median (25th, 75th) | 45.9 | (41.7, 51.5) | 45.8 | (41.7, 51.3) | 45.9 | (41.8, 51.3) | |
| Diabetes, No./total (%) | 774/2314 | (33.4) | 491/1452 | (33.8) | 702/2109 | (33.3) | |
| Hypertension, No./total (%) | 1601/2372 | 67.5 | 1010/1486 | (68.0) | 1466/2152 | (68.1) | |
| Dyslipidemia, No./total (%) | 1254/1976 | 63.5 | 794/1505 | (63.5) | 1141/1801 | (63.4) | |
| Sleep apnea, No./total (%) | 1288/2455 | 52.5 | 827/1540 | (53.7) | 1170/2216 | (52.8) | |
| Severe walking limitation, No./total (%) | 153/2248 | 6.8 | 102/1411 | (7.2) | 137/2040 | (6.7) | |
| SF-36 general health score | (n=2268) | (n = 1430) | (n = 2086) | ||||
| Median (25th, 75th) | 40 | (32, 49) | 40 | (32, 47) | 40 | (32, 47) | |
| SF-36 bodily pain score | (n=2261) | (n = 1424) | (n = 2079) | ||||
| Median (25th, 75th) | 40 | (32, 49) | 40 | (32, 49) | 40 | (32, 49) | |
| ISEL belongingness score | (n=2260) | (n = 1423) | (n = 2078) | ||||
| Median (25th, 75th) | 14 | (12, 16) | 14 | (12, 16) | 14 | (12, 16) | |
| Dissatisfied with sexual life, No./total (%) | 1039/2077 | (50.0) | 660/1305 | (50.6) | 952/1912 | (49.8) | |
| BDI-1 depressive symptoms score | (n=2277) | (n = 1419) | (n = 2108) | ||||
| Median (25th, 75th) | 6 | (3, 11) | 6 | (3, 11) | 6 | (3, 11) | |
| Current or recent smoker, No./total (%) | 324/2454 | (13.2) | 167/1540 | (10.8) | 278/2213 | (12.6) | |
| Regular alcohol consumption, No./total (%) 146/2262 | (6.5) | 104/1426 | (7.3) | 142/2081 | (6.8) | ||
| AUD symptoms, No./total (%) | 148/2256 | (6.6) | 95/1421 | (6.7) | 140/2075 | (6.7) | |
| Illicit drug use, No./total (%) | 100/2251 | (4.4) | 55/1419 | (3.9) | 90/2069 | (4.3) | |
| Prescription opioid use, No./total (%) | 384/2398 | (16.0) | 257/1504 | (17.1) | 348/2173 | (16.0) | |
| Anti-anxiety medication use, No./total (%) | 142/2259 | (6.3) | 87/1423 | (6.1) | 118/2070 | (5.7) | |
| Anti-depressant medication use, No./total (%) | 870/2246 | (38.7) | 535/1413 | (37.9) | 796/2060 | (38.6) | |
| Past-year psychiatric counseling, No./total (%) | 529/2246 | (23.6) | 328/1414 | (23.2) | 485/2065 | (23.5) | |
| Lifetime history of psychiatric | 229/2250 | (10.2) | 157/1419 | (11.1) | 214/2072 | (10.3) | |
| hospitalization, No./total (%) | |||||||
| Surgical procedure | |||||||
| Roux-en-Y gastric bypass | 1738 | (70.7) | 1081 | (70.2) | 1153 | (70.1) | |
| Laparoscopic adjustable gastric band | 610 | (24.8) | 382 | (24.8) | 560 | (25.3) | |
| Other | 110 | (4.5) | 77 | (5.0) | 104 | (4.7) | |
Abbreviations: AUD, alcohol use disorder; BDI-1, Beck Depression Inventory 1; BMI, body mass index, ISEL, Interpersonal Support Evaluation List; SF-36, Short-Form Health Survey-36; SBQ-R, Suicide Behavior Questionnaire-Revised.
Denominators shift between variables because of missing data.
Data are reported as No. (%) unless otherwise indicated.
Due to small numbers, non-white racial categories were combined: Asian, American Indian/Alaska Native, Black, Native Hawaiian/other Pacific Islander, multiple races.
Calculated as weight in kilograms divided by height in meters squared.
A cross-tabulation of pre- and post-surgery suicidality as measured by the SBQ-R is shown in Table 2. From retrospectively-obtained SBQ-R results, 25.7% (395/1534) of participants reported a pre-surgery suicidality history, 46.3%(183/395) of whom also reported suicidality post-surgery. Attempted suicide (vs. suicidal thoughts or plans) was far less common, reported by 4.1%(63/1534) of participants pre-surgery, 12.7% (8/63) of whom also reported post-surgery attempts. All of those who attempted suicide post-surgery (0.8%; 13/1534) had at least a brief passing thought of suicide pre-surgery. However, a small percentage of participants (2.6%; 40/1534) had post-surgery onset of suicidal thoughts or plans.
Table 2.
Suicidal Thoughts, Plans, and Attempts in the Five Years Since Bariatric Surgery by Pre-surgery Lifetime History.a
| Pre-surgery history of suicidality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Never | Brief passing thought | Had plan At least once to kill myself | Attempted to Kill myself | Since surgery totals | ||||||
|
Suicidality in the 5 years following surgery |
N | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| Never | 1099 | (71.6) | 154 | (10.0) | 37 | (2.4) | 21 | (1.4) | 1311 | (85.5) |
| Brief passing thought | 35 | (2.3) | 79 | (5.2) | 29 | (1.9) | 18 | (1.2) | 161 | (10.5) |
| Had plan at least once to kill myself | 5 | (0.3) | 10 | (0.7) | 18 | (1.2) | 16 | (1.0) | 49 | (3.2) |
| Attempted to kill myself | 0 | (0.0) | 4 | (0.3) | 1 | (0.1) | 8 | (0.5) | 13 | (0.8) |
| Prior to surgery totals | 1139 | (74.3) | 247 | (16.1) | 85 | (5.5) | 63 | (4.1) | 1534 | |
Data obtained from the Suicidal Behavior Questionnaire-Revised.
Pre-surgery suicidality history greatly increased the odds of greater severity of post-surgery suicidality (eTable 2 [supplement]). Compared to those with no pre-surgery history, those with a suicidal thought history were 17.47(95% CI, 9.58–31.88) times more likely to have more severe post-surgery suicidality. Pre-surgery past-week self-harm/suicidal ideation (AOR, 7.16, 95% CI, 2.81–18.23) and younger age (AOR, 1.32, 95% CI, 1.05–1.67, per 10 years) were also significantly associated with greater severity of post-surgery suicidality. No other pre-surgery variables or surgical procedures were independently related to suicidality in the five years post-surgery.
Prevalence of self-harm/suicidal ideation from the BDI-1 is shown in Figure 1. The prevalence of self-harm/suicidal ideation was 5.3%(95% CI, 3.7–6.8) pre-surgery and 3.8%(95% CI, 2.5–5.1) at year-1 post-surgery (P=.06). Prevalence then increased over time to 6.6%(95% CI, 4.6–8.6) at year-5 (P=0.001), but was not significantly different than pre-surgery (P=.12). Observed and modeled data by time point are reported in eTable 3 [supplement].
Figure 1.
Modeled* Prevalence of Self-harm/Suicidal Ideation in the Past Week, by Time Point.a
Pre-surgery suicidality history, self-harm/suicidal ideation, being male, smoking, greater pain severity, antidepressant medication use, psychiatric counseling, and lifetime history of psychiatric hospitalization were independently associated with greater risk of self-harm/suicidal ideation in years 1–5 post-surgery (Table 3). As indicated by a significant interaction, the magnitude of the risk of post-surgery self-harm/suicidal ideation associated with pre-surgery self-harm/suicidal ideation decreased over time. Surgical procedure type was not significantly associated with post-surgery self-harm/suicidal ideation.
Table 3.
Associations between Pre-surgery Factors and Post-surgery Self-harm/Suicidal Ideationa (N=2001)
| Pre-surgery factorsb | ARR | (95% CI) | P-value |
|---|---|---|---|
| Lifetime history of suicidality (ref=No)c | 4.50 | (3.06–6.62) | <.001 |
| Past-week self-harm/suicidal ideationd (ref=No) | <0.01 | ||
| Year 1 | 6.89 | (3.41–13.89) | |
| Year 2 | 3.55 | (1.88–6.70) | |
| Year 3 | 2.59 | (1.27–5.28) | |
| Year 4 | 2.57 | (1.30–5.08) | |
| Year 5 | 2.01 | (1.05–3.87) | |
| Male sex (ref=Female) | 1.60 | (1.16–2.20) | <0.01 |
| Age, per 10 years younger | 1.09 | (0.94–1.25) | 0.26 |
| Current smoker (ref=No) | 1.56 | (1.08–2.26) | 0.02 |
| Bodily pain score, per 5 SF-36 points lowere | 1.14 | (1.05–1.24) | 0.001 |
| Current antidepressant medication daily (ref=No) | 1.55 | (1.13–2.13) | 0.01 |
| Past-year psychiatric counseling (ref=No) | 1.70 | (1.21–2.38) | <0.01 |
| Lifetime history of psychiatric hospitalization (ref=No) | 1.72 | (1.21–2.44) | <0.01 |
| Surgical procedure | 0.57 | ||
| LAGB vs. RYGB | 1.12 | (0.56–2.24) | |
| Other vs. RYGB | 0.86 | (0.61–1.21) |
Abbreviations: ARR, adjusted relative risk; CI, confidence interval; LAGB, laparoscopic adjustable gastric band; RYGB, Roux-en-Y gastric bypass
Past week status assessed at annual assessments with the Beck Depression Inventory-1.
Site, age and pre-surgery smoking status, which were related to missing follow-up data, and surgical procedure were forced into the model. Additional pre-surgery factors were considered and retained if significant at P<.05.
There was also an association between unknown vs. no history of suicidality: 3.25 (95% CI=2.11–4.99); p<.001.
There was a significant interaction between baseline self-harm/suicidal ideation and follow-up time point, such that the risk associated with baseline self-harm/suicidal ideation was weaker with increasing time since surgery.
Lower score indicates greater pain.
Associations between pre- to post-surgery changes and post-surgery self-harm/suicidal ideation in years 1–5 are reported in Table 4. Worsening/less improvement in self-rated general health, increasing/less improvement in depressive symptoms, and starting vs. no antidepressant use were independently associated with greater relative risk of having post-surgery self-harm/suicidal ideation. Statistical power was limited to detect associations with some changes due to their low frequency (e.g., becoming single or getting married) and the low frequency of the outcome. While not representing changes, staying single vs. married and continuing antidepressant medication vs. no use were associated with having post-surgery self-harm/suicidal ideation, while continued prescription opioid use vs. no use was associated with lower risk (Table 4). Percent weight loss was not independently associated with risk of post-surgery self-harm/suicidal ideation (AOR=0.99, 95%CI, 0.93–1.05, per 5% weight loss; P=.69).
Table 4.
Independent Associations Between Pre-to-post-surgery Change and Self-harm/Suicidal Ideation Post-surgerya (N=1762)
| Pre-to-post-surgery change | ARR | (95% CI) | P-value |
|---|---|---|---|
| Marital status | 0.002 | ||
| Got married vs. stayed single | 0.53 | (0.24–1.17) | |
| Got divorced vs stayed married | 2.01 | (0.93–4.34) | |
| Stayed single vs. stayed married | 1.75 | (1.16–2.64) | |
| Decrease in general health score, per 5 SF-36 points lower | 1.07 | (1.01–1.14) | 0.02 |
| Increase in depressive symptoms score, per 5 BDI-1 points higher | 1.78 | (1.64–1.92) | <.0001 |
| Prescription opioid use | 0.04 | ||
| Stopped vs. continued | 1.45 | (0.61–3.45) | |
| Started vs. no use | 1.03 | (0.66–1.60) | |
| Continued vs no use | 0.51 | (0.27–0.94) | 0.001b |
| Anti-anxiety medication use | |||
| Stopped vs. continued | 2.07 | (0.88–4.88) | |
| Started vs. no use | 1.04 | (0.62–1.77) | |
| Continued vs no use | 1.15 | (0.50–2.65) | |
| Anti-depressant medication use | 0.01 | ||
| Stopped vs. continued | 0.74 | (0.43–1.25) | |
| Started vs. no use | 1.94 | (1.05–3.57) | |
| Continued vs no use | 1.87 | (1.11–3.13) |
Abbreviations: ARR, adjusted relative risk; CI, confidence interval; SF-36, Short-Form Health Survey-36.
Past week status assessed at annual assessments with the Beck Depression Inventory-1.
Site, age and pre-surgery smoking status, which were related to missing follow-up data, and surgical procedure were forced into the model. The model also controlled for pre-surgery factors reported in table 3 and the baseline SF-36 general health and Beck Depression Inventory-1 depressive symptoms scores.
None of the comparisons of interest were significant.
Average follow-up for vital status was 4.9 years for the 2458 participants. Among the adjudicated deaths within 5 years of surgery with assigned cause (N=40), 3 deaths were categorized as suicides (2 by drug poisonings and 1 by firearm discharge) and 2 deaths as potential suicides (1 as a definite drug poisoning with unknown intent and 1 as a probable drug poisoning with unknown intent). Among the deaths that could not be adjudicated (N=14), 2 deaths were categorized as potential suicides, both drug poisonings per the death certificate. Suicides and potential suicides occurred an average of 3.8 years and 3.9 years post-surgery, respectively. All occurred among participants who had undergone RYGB and experienced substantial weight loss (range: 19–46% of pre-surgery weight). Additional information on participants with suicide and potential suicide deaths is reported in eTable 4 [supplement].
Discussion
Among a large cohort of bariatric surgery patients, 25% reported a pre-surgery history of suicidality and 4% reported a past attempt. These rates are considerably higher than the general US population (i.e., 3.3% suicidal ideation, 0.6% suicide attempt)(30) but trend towards being lower compared to previous studies reporting pre-surgery lifetime rates. For example, in a study of 396 bariatric surgery-seeking individuals, 30.3% reported a history of suicidal ideation,(31) and lifetime prevalence of suicide attempts in bariatric surgery-seeking patients has been reported as 5.6% (among 396 patients),(31) 9.1% (among 121 patients),(32) and 11.2% (among 1020 patients).(33) A potential explanation for higher rates in previous studies is that samples of bariatric surgery-seeking individuals may include patients who were refused surgery due to history of suicidality, as current or recent suicidality is considered a contraindication for bariatric surgery,(34,35) while our study was conducted following approval for surgery. Another explanation for differences in rates may be due to sample size, as smaller studies produce less precise estimates.
In the 5 years following surgery, 15% reported suicidality, most of whom had a pre-surgery suicidality history. A significant trend in the prevalence of self-harm/suicidal ideation from years one to five post-surgery indicates self-harm/suicidal ideation may increase with time passing following bariatric surgery, perhaps due to an initial decrease in the first post-operative year. This is further supported by the timing of suicides and potential suicides, which occurred, on average, almost four years post-surgery within a five-year timeframe. A previous study identified 31 suicides following bariatric surgery over a mean follow-up of 2.8 years and reported more deaths in the third year following surgery than in the first two years combined.(36)
As expected, pre-surgery suicidality was associated with increased risk of both suicidality and self-harm/suicidal ideation in the five years post-surgery. Several additional risk factors that were independent of, or existed prior to, surgery (e.g., younger age, being male, smoking, reporting greater pain, antidepressant use, psychiatric counseling, and psychiatric hospitalizations) were identified. Consistent with these findings, two previous studies reported that most self-harm incidents following bariatric surgery occurred in patients who had pre-surgery mental health problems.(11,13) One past study found that gastrointestinal complications post-surgery were predictive of self-harm, which may be consistent with our pain finding.(11)
Getting divorced (vs. remaining married), general health decline, depression symptom increase, and starting or continuing anti-depressant medication use (vs. no use) following surgery were also related to increased risk of self-harm/suicide ideation, while use of prescription opioid medication, possibly indicative of better pain control, was associated with lower risk. After accounting for these changes, neither weight loss or surgical procedure was related to post-surgery self-harm/suicidal ideation. Studies in the general population have also found that divorce and physical illness are suicide risk factors.(8)
Although we did not have sufficient statistical power to formally evaluate factors predictive of suicide, we examined characteristics of participants who died by suicide or potential suicide within five years of surgery. Of 7 decedents, 5 were female, median age was 44, and most were non-Hispanic, White, married, and denied substance use (smoking, alcohol, and illicit drugs) pre-surgery, consistent with the characteristics of the sample in general. However, the proportion of decedents with a pre-surgery history of psychiatric treatment was high, with five of six with available data reporting anti-depressant or anti-anxiety medication, counseling, and/or hospitalizations. Additionally, all decedents underwent RYGB, perhaps because it was the most common procedure at the time. However, potential mechanisms related to RYGB should be explored in future research; these include malabsorption of antidepressant medications, changes in peptides and hormones that may affect mood, and RYGB’s association with increased risk for alcohol or substance use disorders.(10,15) In line with previous research,(13,36) overdoses accounted for two of the three suicides in our sample and four potential suicides. In contrast to their pre-surgery history, only two of five decedents with available data reported psychiatric treatment at the post-surgery assessment prior to their death. However, none reported self-harm/suicide ideation, perhaps owing to the use of a past-week measure.
Limitations to the study include lack of a control group and insufficient statistical power to evaluate suicide attempts/deaths. While self-harm emergencies are a strong predictor of suicide,(37) a recent cohort study of Danish bariatric surgery patients and non-operated controls with obesity reported bariatric surgery was associated with an increased risk of self-harm but not suicide,(38) illustrating higher risk of one does not infer higher risk of the other. Neovius and colleagues(39) found higher rates of both suicide attempts and deaths among bariatric surgery patients as compared to weight-matched controls, although they speculated that their findings could be due to a selection bias. Additional studies of adults who undergo bariatric surgery with appropriate control groups, larger sample size, and long-term follow-up are warranted.
Other important limitations include missing data that history of suicidality was assessed 5 years post-surgery. Investigation of missing data confirmed that pre-surgery factors were similar between individuals included in the analyses vs. excluded due to missing SBQ-R or BDI-1 data. Longitudinal analyses of self-harm/suicidal ideation controlled for pre-surgery factors related to missing follow-up data. Although participants were told that research data were confidential, they may have under-reported pre-surgery self-harm/suicidal ideation due to concern that their responses could affect surgery eligibility. All potentially important risk factors (e.g., family history of suicide, trauma history, impulsivity, weight loss disappointment, changes in medication absorption, peptides, and hormones)(8,10) were not assessed. The study’s strengths include the large geographically-diverse sample, standardized data collection including multiple measures related to self-harm and suicide, and longitudinal, multivariate analyses.
Among a large cohort of adults with severe obesity who underwent bariatric surgery, the post-surgery prevalence of self-harm/suicidal ideation may initially decrease in the first post-operative year but then increase over time, suggesting screening for self-harm and suicidality, with referral for treatment when indicated, is warranted throughout long-term post-operative care. Several risk factors were identified that may help with enhanced monitoring, such as younger age, being male, history of suicidality, history of psychiatric treatment, divorce, and post-surgery health decline. Because long-term monitoring by bariatric programs can be challenging due to a high loss to follow-up after surgery, it is important that monitoring suicide risk be incorporated into primary care mental health screenings.(40–43) Mental health referrals should be made for individuals found to have thoughts of self-harm/suicidality, and treatment with therapy and/or medication should be considered.
Supplementary Material
Highlights.
Bariatric surgery patients with pre-surgery suicidal ideation are at increased risk for post-surgery ideation.
Suicidal ideation slightly decreased at year-1 post surgery but returned to pre-surgery levels at year-5.
Suicide risk screening is warranted throughout long-term post-operative care.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014; 311(8): 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Courcoulas AP, Yanovski SZ, Bonds D, et al. Long-term outcomes of bariatric surgery: A National Institutes of Health Symposium. JAMA Surg 2014; 149(12): 1323–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Courcoulas AP, King WC, Belle SH, et al. Seven-year weight trajectories and health outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) study. JAMA 2017; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adams TD, Mehta TS, Davidson LE, Hunt SC. All-cause and cause-specific mortality associated with bariatric surgery: A review. Curr Atheroscler Rep 2015; 17(12): 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peterhansel C, Petroff D, Klinitzke G, Wagner B. Risk of completed suicide after bariatric surgery: a systematic review. Obesity Reviews 2013; 14(5): 369–382. [DOI] [PubMed] [Google Scholar]
- 6.Roizblatt A, Roizblatt D, Soto-Aguilar BF. Suicide risk after bariatric surgery. Rev Med Chil 2016; 144(9): 1171–1176. [DOI] [PubMed] [Google Scholar]
- 7.Mather A, Cox B, Enns M, Sareen J. Associations of obesity with psychiatric disorders and suicidal behaviors in a nationally representative sample. Journal Psychosom Res 2009; 66(4): 277–285. [DOI] [PubMed] [Google Scholar]
- 8.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite S, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychol Rev 2010; 117(2): 575–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen EY, Fettich KC, Tierney M, et al. Factors associated with suicide ideation in severely obese bariatric surgery-seeking individuals. Suicide and Life-Threatening Behavior 2012; 42(5): 541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitchell JE, Crosby RD, de Zwaan M, et al. Possible risk factors for increased suicide following bariatric surgery. Obesity 2013;21(4): 665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morgan DJR, Ho KM. Incidence and risk factors for deliberate self-harm, mental illness, and suicide following bariatric surgery: A state-wide population-based linked-data cohort study. Ann Surg 2017; 265: 244–252. [DOI] [PubMed] [Google Scholar]
- 12.Pavarin RM, Fioritti A, Fontana F, Marani S, Paparelli A, Boncompagni G. Emergency department admission and mortality rate for suicidal behavior: A follow-up study on attempted suicides referred to the ED between January 2004 and December 2010. Crisis 2014; 35(6): 406–414. [DOI] [PubMed] [Google Scholar]
- 13.Bhatti JA, Nathens AB, Thiruchelvam D, Grantcharov T, Goldstein BI, Redelmeier DA. Self-harm emergencies after bariatric surgery: A population-based cohort study. JAMA Surg 2016; 151(3): 226–232. [DOI] [PubMed] [Google Scholar]
- 14.Courcoulas A Who, why, and how? Suicide and harmful behaviors after bariatric surgery. Ann Surg 2017; 265(2): 253–254. [DOI] [PubMed] [Google Scholar]
- 15.Backman O, Stockeld D, Rasmussen F, Näslund E, Marsk R. Alcohol and substance abuse, depression and suicide attempts after Roux-en-Y gastric bypass surgery. Br J Surg 2016; 103(10): 1336–1342. [DOI] [PubMed] [Google Scholar]
- 16.Lim RBC, Zhang MWB, HO RCM. Prevalence of all-cause mortality and suicide among bariatric surgery cohorts: A meta-analysis. Int J Environ Res Public Health 2018; 15(7): 1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gribsholt SB, Thomsen RW, Svensson E, Richelsen B. Overall and cause-specific mortality after Roux-en-Y gastric bypass surgery: A nationwide cohort surgery. Surg Obes Relat Dis 2017; 13(4): 581–587. [DOI] [PubMed] [Google Scholar]
- 18.Belle SH, Berk PD, Courcoulas AP, et al. Safety and efficacy of bariatric surgery: Longitudinal Assessment of Bariatric Surgery. Surgery for Obesity and Related Diseases 2007; 3(2): 116–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): Validation with clinical and nonclinical samples, 2001; 8(4): 443–454. [DOI] [PubMed] [Google Scholar]
- 20.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory measuring depression. Arch Gen Psychiatry 1961; 4: 561–571. [DOI] [PubMed] [Google Scholar]
- 21.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review 1988; 8(1): 77–100. [Google Scholar]
- 22.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Medical Care 1992; 30(6): 473–483. [PubMed] [Google Scholar]
- 23.Brookings JB, Bolton B. Confirmatory factor analysis of the Interpersonal Support Evaluation List. Am J Community Psychol 1988; 16(1): 137–147. [DOI] [PubMed] [Google Scholar]
- 24.Steffen KJ, King WC, White GE, et al. Sexual functioning of men and women with severe obesity before bariatric surgery. Surg Obes Relat Dis 2017; 13(2): 334–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.King WC, Chen JY, Courcoulas AP, et al. Alcohol and other substance use after bariatric surgery: Prospective evidence from a U.S. multicenter cohort study [published online ahead of print March 31, 2017]. Surg Obes Relat Dis [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO Collaborative Project on early detection of persons with harmful alcohol consumption-II. Addiction 1993; 88(6): 791–804. [DOI] [PubMed] [Google Scholar]
- 27.In U.S., who is at greatest risk for suicide? 2010. Population Reference Bureau. http://www.prb.org/Publications/Articles/2010/suicides.aspx. Accessed March 23, 2017. [Google Scholar]
- 28.King WC, Chen JY, Belle SH, et al. Change in Pain and Physical Function Following Bariatric Surgery for Severe Obesity. JAMA 2016; 315(13): 1362–1371: Supplement. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edwards D, Berry JJ. The Efficiency of Simulation-Based Multiple Comparisons. Biometrics 1987; 43(4): 913–928. [PubMed] [Google Scholar]
- 30.Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA 2005; 293: 2487–2495. [DOI] [PubMed] [Google Scholar]
- 31.Chen EY, Fettich KC, McCloskey MS. Correlates of suicidal ideation and/or behavior in bariatric-surgery-seeking individuals with severe obesity. Crisis 2012; 33: 137–143. [DOI] [PubMed] [Google Scholar]
- 32.Sansone RA, Wiederman MW, Schumacher DF, Routsong-Weichers L. The prevalence of self-harm behaviors among a sample of gastric surgery candidates. J Psychosom Res 2008; 65: 441–444. [DOI] [PubMed] [Google Scholar]
- 33.Windover AK, Merrell J, Ashton K, Heinberg LJ. Prevalence and psychosocial correlates of self-reported past suicide attempts among bariatric surgery candidates. Surg Obes Relat Dis 2010; 6(6): 702–706. [DOI] [PubMed] [Google Scholar]
- 34.Fabricatore AN, Crerand CF, Wadden TA, Sarwer DB, Krasucki JL. How do mental health professionals evaluate candidates for bariatric surgery? Survey results. Obes Surg 2006; 16(5): 567–573. [DOI] [PubMed] [Google Scholar]
- 35.Bauchowitz AU, Gonder-Frederick LA, Olbrisch ME, et al. Psychosocial evaluation of bariatric surgery candidates: A survey of present practices. Psychosom Med 2005; 67(5): 825–832. [DOI] [PubMed] [Google Scholar]
- 36.Tindle HA, Omalu B, Courcoulas A, Marcus M, Hammers J, Kuller LH. Risk of suicide after long-term follow-up from bariatric surgery. Am J Med 2010; 123(11): 1036–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pavarin RM, Fioritti A, Fontana F, Marani S, Paparelli A, Boncompagni G. Emergency department admission and mortality rate for suicidal behavior: a follow-up study on attempted suicides referred to the ED between January 2004 and December 2010. Crisis 2014; 35(6): 406–414. [DOI] [PubMed] [Google Scholar]
- 38.Kovacs Z, Valentin JB, Nielsen RE. Risk of psychiatric disorders, self-harm behaviour and service use associated with bariatric surgery. Acta Psychiatr Scand 2017; 135(2): 149–158. [DOI] [PubMed] [Google Scholar]
- 39.Neovius M, Bruze G, Jacobson P, et al. Bariatric surgery & suicide: Data from two controlled matched cohort studies Paper presented at: LAT-OR-2056 The Obesity Society; November 2, 2016; New Orleans, LA. [Google Scholar]
- 40.Primary Care: A Crucial Setting for Suicide Prevention. SAMHSA-HRSA Center for Integrated Health Solutions.; https://www.integration.samhsa.gov/about-us/esolutions-newsletter/suicide-prevention-in-primary-care. Accessed November 18, 2018. [Google Scholar]
- 41.Bajaj P, Borreani E, Ghosh P, Methuen C, Patel M, Crawford MJ. Screening for suicidal thoughts in primary care: The views of patients and general practitioners. Ment Health Fam Med 2008; 5(4): 229–235. [PMC free article] [PubMed] [Google Scholar]
- 42.Ask Suicide-Screenings Questions Toolkit. National Institute of Mental Health; https://www.nimh.nih.gov/labs-at-nimh/asq-toolkit-materials/index.shtml. Accessed November 18, 2018. [Google Scholar]
- 43.van der Feltz-Cornelis CM, Sarchiapone M, Postuvan V, et al. Best practice elements of multilevel suicide prevention strategies: A review of systematic reviews. Crisis 2015; 32: 319–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.