Abstract
Background
Caesarean delivery (CD) is a common form of delivery of a baby, rising in frequency. One reason for its performance is to preserve maternal pelvic floor function, part of which is anal continence.
Objectives
To assess the ability of CD in comparison to vaginal delivery (VD) to preserve anal continence in a systematic review
Search methods
Search terms include: "Caesarean section, Cesarean delivery, vaginal delivery, incontinence and randomised". PubMed, EMBASE and the Cochrane Central Register of Controlled Trials (Central) were searched from their inception through July, 2009.
Selection criteria
Both randomised and non‐randomised studies that allowed comparisons of post partum anal continence (both fecal and flatus) in women who had had babies delivered by either CD or VD were included.
Data collection and analysis
Mode of delivery, and when possible mode of all previous deliveries prior to the index pregnancy were extracted, as well as assessment of continence post partum of both faeces and flatus. In Non‐RCTs, available adjusted odds ratios were the primary end point sought. Incontinence of flatus is reported as a separate outcome. Summary odds ratios are not presented as no study was analysed as a randomised controlled trial. Numbers needed to treat (NNT) are presented, that is, the number of CDs needed to be performed to prevent a single case of fecal or flatus incontinence, for each individual study. Quality criteria were developed, selecting studies that allowed maternal age adjustment, studies that allowed a sufficient time after the birth of the baby for continence assessment and studies in which mode of delivery of prior pregnancies was known. Subgroup analyses were done selecting studies meeting all quality criteria and in comparisons of elective versus emergency CD, elective CD versus VD and nulliparous women versus those delivered by VD or CD, in each case again, not calculating a summary risk statistic.
Main results
Twentyone reports have been found eligible for inclusion in the review, encompassing 31,698 women having had 6,028 CDs and 25,170 VDs as the index event prior to anal continence assessment . Only one report randomised women (with breech presentation) to CD or VD, but because of extensive crossing over, 52.1%, after randomisation, it was analysed along with the other 20 studies as treated, i.e. as a non‐randomised trial. Only one of these reports demonstrated a significant benefit of CD in the preservation of anal continence, a report in which incontinence incidence was extremely high, 39% in CD and 48% in VD, questioning, relative to other reports, the timing and nature of continence assessment. The greater the quality of the report, the closer its Odds ratio approached 1.0. There was no difference in continence preservation in women have emergency versus elective CD.
Authors' conclusions
Without demonstrable benefit, preservation of anal continence should not be used as a criterion for choosing elective primary CD. The strength of this conclusion would be greatly strengthened if there were studies that randomised women with average risk pregnancies to CD versus VD.
Keywords: Female; Humans; Pregnancy; Cesarean Section; Delivery, Obstetric; Delivery, Obstetric/adverse effects; Fecal Incontinence; Fecal Incontinence/prevention & control; Flatulence; Flatulence/prevention & control
Plain language summary
How well do Cesarian or vaginal delivery of babies prevent anal incontinence?
Cesarean delivery (CD) is an ancient method of delivering a baby when there appears to be a risk to vaginal delivery; in most cases, a risk to the infant. However in modern times risk to the mother has also been considered in choosing this method of delivery, and increasingly the risk being considered is post partum pelvic floor dysfunction, which includes incontinence of flatus or faeces, together known as anal incontinence. In this systematic review of non‐randomised studies, no benefit could be demonstrated for CD over vaginal delivery (VD) in the prevention of anal incontinence. This review encompasses 21 published studies, involving 31,698 women, delivered by 6,028 CD and by 25,170 VD. No randomised studies comparing CD to VD in average risk pregnancies exist. The above conclusion is therefore based upon less than optimal evidence.
Background
Description of the condition
Anal incontinence may occur in women during the immediate post partum period and persist throughout adult life; indeed it is thought by some that labor and vaginal delivery are the principal causes of adult anal incontinence (Oberwalder 2003). It is defined as the leakage of fecal material spontaneously, solid or liquid (defining fecal incontinence) or flatus or, in many surveys, mucoid discharge (Nelson 2004). The impact of anal incontinence is dependence on protective undergarments, social isolation, and as age advances, nursing home residence (Nelson 1998). Because of the multiple facets of anal incontinence, ascertainment and prevalence have been complex, compared to urinary incontinence (wet or not wet), leading to large variance in prevalence figures in published reports (Nelson 2004), varying from 1.4% to over 11% in healthy ambulatory populations and 50% of nursing home residents (Nelson 2004). The only intervention currently employed to prevent anal incontinence is elective primary Cesarean delivery.
Description of the intervention
Over the past decade or more there has been a lively debate concerning the health benefits of elective primary Cesarean delivery (CD) (Abramowitz 2000; Amu 1998; Faridi 2002; Farrell 2002; Guise 2004; Lockwood 2004; Minkoff 2003; Nygaard 2003; Paterson‐Brown 1998; Zetterstrom 1999; Idama 1999), also known as Cesarean delivery on maternal request ((CDMR), NIH 2006), or No indicated risk Cesarean delivery, (Declercq 2005). Evidence of the diversity of opinion even among those most expert in the field is provided by a survey in London, where 31% of female obstetricians stated that they would elect to have a CD on maternal request (Paterson‐Brown 1998) although in Holland the figure among female obstetricians was only 1.4% (van Roosmalen 1999).
CD rates have been steadily rising throughout high income countries and currently. CD occurs in 24.6% in the United Kingdom (Rose 2009) and 31.1% in the USA (Tita 2009), a 50% rise in the USA in 10 years (NIH 2006). Yet, in the Netherlands it remains 9% (van Roosmalen 1999). CDMR is a component of the rising rate of CD (NIH 2006) in the United States.
Many reasons are given for a woman choosing to have a CDMR. In Taiwan timing of delivery to certain days of the week is associated with life long good fortune for the baby (Hsu 2008). Women in Brazil believe that this more aggressive and sophisticated intervention is better for the health of the baby, and that is better medicine (Behague 2002). Economic correlates with CDMR rates are evident in Brazil and Chile, where CD occurs more than twice as often in private patients, exceeding 70% of all deliveries in wealthier classes.(Behague 2002; Potter 2001; Murray 2000). However the most common reason stated for CDMR is preservation of maternal pelvic floor function, such as continence of urine, faeces, flatus and prevention of pelvic floor prolapse (Nygaard 2003; Minkoff 2003).
How the intervention might work
Cesarean delivery may prevent anal incontinence as it may preserve and protect maternal pelvic floor function by avoiding direct vaginal, sphincter and distal pelvic nerve trauma that might occur during vaginal delivery (VD).
Why it is important to do this review
However, Cesarean delivery (CD) is associated with a number of health risks when compared to Vaginal delivery (VD), including transfusion, ICU admission, hysterectomy and extended length of hospital stay. (Klein 2004; Villar 2007). In the subsequent pregnancies, there is an increased likelihood of a repeat CD and the rate of vaginal birth after CD is decreasing (NIH 2006; Greene 2004; Mollison 2005). After CD there is an increased, if small, risk in the subsequent pregnancy of uterine rupture, placenta praevia, placenta accreta and operative morbidity including peripartum hysterectomy (Landon 2004; Makoha 2004; Guise 2004; NIH 2006). The risk of intraperitoneal adhesions is increased with each CD, up to 83% in the third pregnancy, increasing the difficulty of the procedure and the risk of subsequent adhesive bowel obstruction (Morales 2007). Thromboembolism is increased following CD (Jacobsen 2004). There are also risks for the newborn, especially if the elective CD occurs before the recommended 39 weeks gestation (Tita 2009). Yet in the USA more than 50% of CD occur before the 39th week of gestation (Tita 2009; NIH 2006). This risk pulmonary difficulties in the newborn may last well into childhood, as the risk of asthma in 8 year olds has been found to be higher if they were born by CD (Roduit 2009). There is also the question of cost (Henderson 2001). In the UK it is estimated that the cost of a CD is 760 pounds more than a VD (Howard 1999). Post partum readmission to hospital is more common after CD than VD ( Liu 2005). Awareness of these risks has led insurers in the United States to increase medical insurance costs to those women having prior CDs (Grady 2008). The National Institute of Clincal Excellence (NICE) of the UK has recommended that CDMR not be done (Kmietowicz 2008).
An intervention such as CD should require rigorous evidence of efficacy in the preservation of anal continence before that specific indication can be accepted or promoted as a reason for its choice.
Objectives
To evaluate the role of CD specifically in the prevention of post partum anal incontinence.
Methods
Criteria for considering studies for this review
Types of studies
Studies were sought in which women are either randomised to CD or VD, or alternatively studies which compare in cohorts or in cross sectional surveys women having either CD or VD, in all cases for the outcome of continence after pregnancy for faeces and flatus. When possible, emergency CD was separated from elective CD in the analyses, primiparous pregnancies separated from women having prior pregnancy and, in multiparous women, CD after prior VD separated from women only having prior CD.
Types of participants
Women with a history of pregnancy and delivery of a live infant, including breech presentations and twin pregnancies.
Types of interventions
VD and CD (either electively or as an emergency).
Types of outcome measures
Incontinence of flatus and faeces, known collectively as anal incontinence, though these are reported separately in most included studies.
The timing of the measurement of the outcome was considered to be optimally more than 4 months. This timing was based upon a general belief among colorectal surgeons that sphincter control is less than normal in the presence of a healing wound such as an episiotomy, but more importantly from two pairs of publications in which incontinence rates were higher in women who were assessed at 3 months post partum than in the same women assessed several years later (MacArthur 2001; Hannah 2002; Hannah 2004; MacArthur 2005). That is, that the outcome to be measured in this review is sustained fecal or flatus incontinence rather than dysfunction associated with a healing wound.
Search methods for identification of studies
Search terms include: "Caesarean section, Cesarean delivery vaginal delivery incontinence and randomised". To identify non‐randomised studies the same search terms were used except for the term "randomised".
Electronic searches
Single institution and single practice publications were included along with cohorts recruited prior to delivery and population based surveys. Medline‐PubMed was the search engine and the date range from 1966 through July, 2009. Searches were also conducted in Embase and the Cochrane Central Register of Controlled Trials (Central) in the Cochrane Library issue 2 2009.
Searching other resources
Reference lists and authors of relevant publications were also screened for potential studies.
Data collection and analysis
Data collection and analysis was conducted in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008).
Selection of studies
RN scanned the titles and abstracts of articles retrieved by the search and excluded those that were clearly irrelevant. The full text of all potentially eligible studies were retrieved. RN examined the full text articles for compliance with the inclusion criteria and selected studies eligible for inclusion in the review. Authors correspond with study investigators if required, to clarify study eligibility (e.g. with respect to participant eligibility criteria and allocation method). Disagreements as to study eligibility were resolved by consensus or by discussion with CF.
Data extraction and management
Data were extracted from eligible studies using a data extraction form designed by the authors. Study authors were contacted by RN in order to resolve any data queries as required, for example, to obtain adjusted analyses or individual patient data requested in order to adjust their data. Two review authors (RN and CF) independently extracted the data any disagreement between these reviewer authors will be resolved by a third review author.
Assessment of risk of bias in included studies
The included studies were assessed for risk of bias using the Cochrane risk of bias assessment tool (see Appendix C) to assess RCTs: sequence generation; allocation concealment; blinding of participants, providers and outcome assessors; completeness of outcome data; selective outcome reporting; and other potential sources of bias.
However, because of the inclusion of non RCTs in this review additional risk of bias measures were included for the following items:
prospective cohort study design,
adjustment for age (the most significant risk factor for anal incontinence)
and parity (increasing parity thought to increase anal incontinence risk),
pregnancy and delivery history (to assure that those categorized as CD had not had a prior VD),
analysing emergency and elective CD separately (i.e., those mothers in labor or not), and
the timing of the assessment of outcomes after more than 4 months post partum (to assure that sustained incontinence was being assessed). Four months is an inadequate length of time for perineal healing and recovery of function, especially when there has been perineal trauma related either to the birth itself or episiotomy. Anal seepage and sphincter dysfunction are common during perineal wound healing, so that incontinence at 4 months has not been a good predictor of incontinence at 6 months, one year or six years (MacArthur 2005, Hannah 2004).
No risk of bias table is presented as no study is analysed as randomised.
Measures of treatment effect
Crude incidence data of anal incontinence were determined as well as odds ratios and 95 per cent confidence intervals for individual studies. In the only randomised study, the cross over after randomisation exceeded 50% (e.g. women randomised to VD instead treated by CD, and visa versa; see below), therefore the data from that study were presented "as treated", i.e., as a non‐randomised study.
In the non‐randomised studies, when odds ratios and confidence intervals adjusted for potential confounders, notably maternal age and parity, were available in published reports, these were extracted and used in such studies as the primary outcome measure rather than the unadjusted odds ratios.
Unit of analysis issues
There are no unit of analysis issues
Dealing with missing data
Authors were contacted to obtain missing data or analyses, especially for age adjustment.
Assessment of heterogeneity
If RCTs had been available and pooling undertaken then statistical heterogeneity would have been assessed by the measure of the I2. An I2 measurement greater than 50% will be taken to indicate a substantial heterogeneity (Higgins 2003, 2008). If substantial heterogeneity had been detected, possible explanations would have been explored in sensitivity analyses. However since no combined statistic is calculated due to the nonRCT study designs, statistical heterogeneity is not calculated herein. Clinical heterogeneity will be discussed in the Description of Studies.
Assessment of reporting biases
If the primary outcome of incontinence of faeces or flatus, or the combined outcome of anal incontinence was not assessed, this study was excluded.
Data synthesis
Meta‐analysis was not used to calculate a summary relative risk among studies because all studies are non‐randomised. Graphic representation of the results of each individual study is shown using the Revman Analysis software.
Six Forest plots are presented in Revman Analysis without summary statistics:
Fecal incontinence ‐ all studies
Incontinence of flatus ‐ all studies
Fecal incontinence in the 7 best studies, i.e. those studies which fulfilled the three following criteria: age adjustment, assessment of incontinence after 4 months postpartum and women categorized as CD with no history of prior VD.
Subgroup comparison of emergency versus elective CD for the outcome of fecal incontinence in the studies in which there was numerical delineation of these variables.
A comparison of elective CD versus non‐instrumented VD for the outcome of fecal incontinence.
A comparison of fecal incontinence in nulliparous women versus mothers delivered by CD or VD.
The number needed to treat (NNT) is presented in the Table 1 for each individual study, for fecal and flatus incontinence, that is, the number of CDs which must be done to prevent a single case of incontinence of either gas or stool. The NNT was derived from the calculated odds ratio for fecal or flatus incontinence comparing CD and VD and the risk of incontinence in the control (VD) population. No summary NNT is presented since no summary risk estimates are calculated because the included studies are all observational studies. A negative NNT denotes the number of VD needed to prevent a single case of anal incontinence relative to CD.
1. Number Needed to Treat to Prevent a Single Case of Incontinence (NNT).
| Study | NNT Feces | NNT Flatus |
| (Sultan 1993a) | ‐710 | 50 |
| (MacLennan 2000) | 40 | 39 |
| (Chaliha 2001) | ‐50 | |
| (Chaliha 1999) | ‐131 | |
| (Eason 2002) | 160 | infinity |
| (Hannah 2004) | ‐1011 | 66 |
| (Hall 2003a) | ‐40 | 20 |
| (Lal 2003) | 34 | |
| (Fornell 2004) | 104 | ‐128 |
| (Pinta 2004a) | 12 | |
| (Abramov 2005) | 13 | ‐75 |
| (Goldberg 2003) | ‐171 | |
| (Groutz 1999a) | 35 | |
| (MacArthur 2005) | ‐741 | ‐456 |
| (Varma 2006) | 130 | |
| (Altman 2007) | 444 | 12 |
| (Bharucha 2006a) | 17 | |
| (Fritel 2007) | 38 | |
| (Guise 2008) | 11 | |
| (Melville 2005) | 64 | |
| (MacArthur 1997) | 140 |
Subgroup analysis and investigation of heterogeneity
Seeking aspects of CD that might increase anal incontinence risk, the following subgroups were sought within the included studies:
1. Urgency of CD: Emergency CD and elective CD
2. Comparing Elective CD and VD.
3. Isolating those 7 studies that fulfilled all the quality assessment criteria
4. Fecal incontinence in nulliparous women in surveys that included nullips to child bearing mothers in those same surveys.
Sensitivity analysis
Since there is no summary statistic being presented in any of our outcome assessments, no sensitivity analyses to test the robustness of such a result were performed.
Results
Description of studies
Results of the search
Twenty one studies were found eligible for inclusion in the review encompassing 31,698 deliveries, 6,028 being CD and 25,170 being VD ‐ one study is awaiting classification (Burgio 2007a). There are a large number of very disparate reports included in this systematic review.
Included studies
Patient characteristics:
Maternal age: Several population‐based surveys adjusted for maternal age postpartum (MacLennan 2000; Fornell 2004; Goldberg 2003; MacArthur 2005; Abramov 2005; Varma 2006; Altman 2007; Melville 2005; Guise 2008).
Parity: Several studies included only primiparous patients (Lal 2003; Chaliha 1999; Altman 2007; Guise 2008; Pinta 2004a), so that a patient having a CD could not have had a prior VD, or they included data on prior pregnancies in multiparous patients that allowed separation of patients having a CD in the index pregnancy but no prior VDs from those that had had prior VDs. Adjustment for parity was made in some studies (MacLennan 2000; MacArthur 2005; Goldberg 2003; Altman 2007). The cohort presented by (Altman 2007) were primiparas at registration in 1995, and all subsequent deliveries were by the same mode in each cohort as the original delivery, either VD or by CD. Vaginal delivery patients were excluded if they had an instrumented delivery (by suction or forceps). Ten year follow up data with continence assessment are presented. The Hannah trial only included breech presentations (Hannah 2004). Four studies included nulliparous women in the study cohort (MacLennan 2000; Melville 2005; Varma 2006; Fritel 2007).
Multiple pregnancies: Two cohorts presented by Goldberg (Goldberg 2003) and Abramov (Abramov 2005) were of great interest as they reported twins. The first is a large group of mothers of twins and the second are identical female twin pairs discordant as to method of delivery of their babies.
Interventions and comparisons:
All studies compared CD with VD. Studies that attempted to separate the effects of pregnancy from the effects of labor reported whether the index CD was done emergently or electively were (Lal 2003; MacArthur 1997; MacArthur 2005; Abramov 2005).
Outcomes:
Ascertainment of incontinence: A variety of methods were used and included maternal self reporting to mailed questionnaires. Only five studies used an instrument specifically validated for anal continence assessment (Abramov 2005; Goldberg 2003; Hatem 2007; Guise 2008; Bharucha 2006a). Two studies failed to separate anal incontinence (Lal 2003; Guise 2008), i.e. presented a combined flatus/fecal outcome.
Timing of assessment of faecal incontinence and flatus: A number of studies made their only assessment within four months of the baby being born which we considered to be too soon for vaginal/rectal healing (Eason 2002; Hall 2003a; Hannah 2002; Lal 2003; Chaliha 1999; Chaliha 2001; MacArthur 2001; Sultan 1993a; Groutz 1999a; Guise 2008). Studies that did their continence assessment at a time greater than four months postpartum were judged to be of greater quality (MacLennan 2000; Hannah 2004; Fornell 2004; Goldberg 2003; MacArthur 2005; Abramov 2005; Varma 2006; Altman 2007; Melville 2005; Fritel 2007). Although the first publication of Hannah made the assessment less than 4 months, the two year follow‐up of that study has been published with subsequent continence data on 917 of the original 2088 enrolled presented (Hannah 2004).
Excluded studies
166 studies were found in the search, the majority of which were excluded either because they dealt with anal incontinence only after vaginal delivery, or only presented data on urinary incontinence when comparing VD and CD.
Risk of bias in included studies
Study design:
RCTs: There is only one trial that randomised women to CD or VD, but there were aspects of that report that limited the ability ana lyze it as randomised and to generalize its results to all pregnant women (Hannah 2002). Firstly, only breech presentations were included, secondly only 50 per cent of the women were primiparous and finally prior VD was not a contraindication to randomisation to CD, creating a potential classification error. Because of the breech nature of the pregnancies, there was a 43% cross over amongst the VD arm of the study to CD at the time of birth due to the obstetrician's judgment, and a 9.1% cross over from the CD arm to VD, for a total cross over of 52.1%.
The study by Eason is also a randomised trial (Eason 2002) but not randomisation to VD or CD, rather to perineal massage in the 3rd trimester. What is presented related to continence is a nested cohort within this trial that looked at different delivery methods and how they affected defecation function postpartum. Only 60 per cent of the patients were primiparous and continence assessment was also done three months after delivery.
Four of these reports present follow‐up data or analyses (Chaliha 2001; Hannah 2004; MacArthur 2005; Guise 2008) on previously published cohorts (Chaliha 1999; Hannah 2002; MacArthur 2001; Guise 2007). (Chaliha 2001) appears to be a subset of the cohort first reported in (Chaliha 1999) with additional physiologic assessments.
Population Studies: The population based surveys by MacArthur 2001, MacLennan 2000, Fornell 2004, Fritel 2007, Melville 2005 and Varma 2006 assessed continence at a time quite remote from pregnancy and delivery. A very large cross sectional population survey presented by MacArthur (MacArthur 2005) presents follow‐up data on and analyses from a multi‐continental cohort that, in the initial report (MacArthur 2001) only had a three month continence assessment. That original study included 7879 post partum women. At the six year follow‐up, with 4214 women from the original cohort responding and matched to their original data were assessed. Age adjustment was available within some of these cohorts and it is also known within the group which patients having CD and had no prior VD. Although the first publication of the RCT (Hannah 2002) made the assessment less than 4 months, the two year follow‐up of that study has been published with subsequent continence data on 917 of the original 2088 enrolled (Hannah 2004).
Overall assessment of risk of bias: As only two studies were RCTs, the assessment of risk of bias did not apply to the majority of the studies. In the methods the pre stated assessment of quality included studies that reported prospective data from cohorts, adjusted for age, considered parity, separated elective and emergent CD and reported the outcomes after 4 months. Seven studies were judged to be of greater quality based upon these criteria (Abramov 2005; Altman 2007; Goldberg 2003; MacArthur 2005; MacLennan 2000; Varma 2006; Melville 2005). Among these 7 studies only one was also a prospective cohort study (Altman 2007), providing more reliable incidence data and thus avoiding recall bias related to prevalence.
Additional details of each study can be found in the Table of Included Studies.
Effects of interventions
Reported crude incontinence rates varied greatly between reports from 1.14% (Hannah 2002) to 25.7% (Varma 2006) to 48% (Guise 2008). This variation is troubling. Variation is also often seen in prevalence studies, where apparently similar populations report widely varying rates of anal incontinence (Nelson 2004), but in no case in those reports was it as high as in the reports cited above. This may be due to variations in ascertainment techniques and the age of the assessed populations. For instance the (Hannah 2002) participants had just had babies and were clearly much younger than those assessed in (Varma 2006), who were between 40 and 69 years old. Yet in a similarly aged population to Varma 2006, Fornell 2004 presents fecal incontinence prevalence as low as 1% for solid faeces in urinary continent women. Further discussion of problems related to disease ascertainment is presented in Discussion. Comparison of rates across studies are therefore not done, though comparative rates within studies, especially when age adjustment is performed, should be more reliable than rates across studies. Results for each of the outcomes are shown in the Forest plots. In addition, summary statistics of effect are not reported as these are all non‐randomised studies, or in one case, a randomised study reported as treated (Hannah 2002; Hannah 2004) because of a cross over rate of 52.1% after randomisation.
1.Comparison: Caesarean delivery versus vaginal delivery (all studies)
Outcome: Anal incontinence
Faeces
1.11 Of the 22 studies shown in Forest plot 1.1, fecal incontinence by delivery mode, only two show a significant protective effect of CD (MacArthur 2001;Guise 2008). The (MacArthur 2001) assessed continence only 3 months post partem and in a follow up study of the same participants, the difference in prevalence of incontinence comparing CD and VD disappeared (MacArthur 2005) (OR=1.04, 0.72‐1.50), an effect also seen in comparing the early and late reports of (Hannah 2002; Hannah 2004). (Guise 2008) is a subset of (Guise 2007), the primiparous mothers from that survey, with adjustment for age, many delivery related factors and exclusion of women who reported an anal incontinence prior to the pregnancy, allowing a calculation of incidence. Also unlike the 2007 study, the more recent publication allows direct comparison of CD and VD. The protective effect of CD was very significant (OR=0.7, 0.62‐0.78) and the population large (5491), apparently giving great weight to the study. However the continence assessment tool used, the "NIH definition" of incontinence, merged both flatus and faeces. Any episode of incontinence since delivery up to three months was queried and apparently even a single episode in the early post‐partum period would classify that mother as incontinent. The incidence of incontinence in CD was 39% and in VD, 48%, levels of incontinence otherwise only seen in nursing homes (Nelson 1998). All other included studies showed prevalence numbers, despite their variation, much smaller than this, some less than 1%, especially for CD (Chaliha 2001). This adds great emphasis to the importance of continence assessment at a time remote from the delivery of the baby. In addition it also stresses the need for an assessment tool that can be more uniformly utilized in future studies and especially one that discloses a sustained disorder rather than a single event at a traumatic time.
Flatus
1.2 There are no studies that show a significant benefit of CD over VD with regard to incontinence of flatus. As mentioned above, two studies merged flatus and faeces into a single outcome variable (Guise 2008; Lal 2003) and the data from both these studies has been entered in comparison 1.1, incontinence of faeces.
2. Subgroup Comparison: Caesarean delivery versus vaginal delivery (by subgroups of quality or emergency or elective)
2.1 Incontinence of faeces in the 7 best studies. Seven studies adjusted for age, avoided misclassification or overlap of delivery mode, and assessed incontinence at an appropriate time (Abramov 2005; Altman 2007; Goldberg 2003; MacArthur 2005; MacLennan 2000; Varma 2006; Melville 2005). A validated instrument for the detection of anal incontinence was used in four of these studies (Abramov 2005; Altman 2007; Goldberg 2003; Melville 2005). None of these studies showed a significant benefit of CD over VD and aside from (Abramov 2005), the odds ratios are closely clustered around 1.0.
2.2 Emergency CD versus Elective CD
Six studies allowed comparison of elective versus emergent CD (Abramov 2005; Guise 2007; Guise 2008; Lal 2003; MacArthur 1997; MacArthur 2005). An important factor in separating the effects of pregnancy from labor is whether the CDs were done electively or in a women in labor, emergently. MacArthur presents only 3 month continence data for primips. (Odds Ratio for fecal incontinence = 0.99; 95 per cent confidence interval = 0.62‐1.52) and all women (1.14; 0.49‐2.65) (MacArthur 2001), and Abramov (Abramov 2005) a more prolonged follow‐up in discordant twins (1.07; 0.05‐24.1). (Lal 2003) had an OR of 1.57; CI 0.381‐6.486, among 184 women having either emergent or elective CDs and (MacArthur 1997) had an OR of 0.134; CI=0.007‐2.428. In none of these studies was there a significant difference in fecal incontinence between women having emergency or elective CDs. For (Guise 2007) and (Guise 2008, looking only at primiparous mothers from the 2007 population), the odds ratios were 0.92; 0.57‐1.51 and 1.20; 0.92‐1.56 respectively.
2.3 Elective CD versus VD
Four studies presented analyses that compare elective CD versus VD (Abramov 2005; Lal 2003; MacArthur 1997; MacArthur 2001), again addressing the same issue raised in comparison 2.2, whether combining elective and emergent CD in comparisons to VD might obscure a benefit of CD when done electively. There was no significant advantage of elective CD over VD in any of these four studies.
2.4 The association of pregnancy delivered by any method with fecal incontinence compared to women who have never delivered a baby is shown in this Forest plot. These are derived from the four studies (Fritel 2007; MacLennan 2000; Melville 2005; Varma 2006), encompassing 1796 nulliparous women and 7686 women who have had a baby by any delivery method. (MacLennan 2000; Varma 2006) both show a significant increase in risk of fecal incontinence in parous women.
The number needed to treat results are shown in Table 1. There was great variation between studies, in some cases with inverted numbers, that is VDs would have to be done to prevent a case of anal incontinence relative to CD (negative numbers in the Table). Summary calculations are not presented for two reasons. First summary risk data are not calculated since all included studies are observational studies. Second the prevalence risk of incontinence in the control population (VD) varied widely between studies suggesting cultural/methodological/clinical differences in these studies that would make them hard to compare. The internal validity within each study of the VD/CD comparison and NNT should not be affected by this variation.
The fecal incontinence prevalence decreased in follow‐up studies for instance from 9.6% (MacArthur 2001) in the whole cohort at 3 months to 3.6% (MacArthur 2005) at 6 years The same disappearance of an apparent insignificant benefit of CD in preservation of anal continence was found in the follow up study of the Term Breech Trial (Hannah 2002, Hannah 2004). In the (MacArthur 2005) study and the mothers of twins study (Goldberg 2003), there was an insignificant trend towards increased incontinence risk with CD (see NNT in Additonal Tables). Among the studies where follow‐up is also published, data from both the initial reports and longer follow up data are presented in the Forest plots for (Hannah 2002; Hannah 2004; MacArthur 2001; MacArthur 2005).
Discussion
Summary of main results
From the available evidence there is no demonstrable benefit of CD, apparently any CD and not just CDMR, in the preservation of anal continence.
But why doesn't CD prevent anal incontinence, especially when associating perineal trauma with loss of bowel control is not just intuitive, but sometimes visibly obvious? Certain aspects of VD are clearly causally related to anal incontinence: significant laceration, forceps, and some episiotomies (MacArthur 2005; Zetterstrom 1999). However this review demonstrates that other factors need to be explored. So one must look to pregnancy and not just labor and delivery as an initiating factor. Further evidence in favour of this comes from the sphincter repair literature cited below. The rapid decay in function suggests that another defect is present besides a gap in the sphincter that remains after the early effects of sphincter repair wear off. What this is is not yet known, though trauma at the pelvic inlet during pregnancy or in early labor (Devine 1999) seems likely.
Overall completeness and applicability of evidence
There are no randomised trials of women with average risk pregnancies.
Quality of the evidence
Many of the included reports are small studies that may not have had sufficient statistical power to demonstrate a benefit. However, the number of deliveries in some reports was quite large. Meta‐analysis is a technique that could combine these results and, among other accomplishments, overcome the problem of inadequate power by performing a combined analysis of multiple studies and so increase sample size. However, the study design needed to minimize bias in meta‐analysis is the randomised controlled trial. Bias is more likely in non‐randomized studies, in this review most likely related to subject allocation to treatment group. Women having a CD may have been on average more likely to have bigger babies, or problems during their labor, though two studies did adjust for all labor related factors (Eason 2002; Guise 2008) and the former still found that CD did not prevent anal incontinence. The latter (Guise 2008) would benefit from a follow up study more remote in time from delivery and with an alternative assessment tool that might better disclose sustained incontinence. Nor do the data shown comparing emergency CD to elective CD support the latter point. The former issue of fetal weight is not supported in the analysis of data from (MacArthur 2001), in which birth weight was not found to be a predictor of anal incontinence, though in (Guise 2008) newborn weight was a predictor of incontinence in the VD group, a group again that had an anal incontinence incidence of 48%.
This is a very significant public health issue affecting all women of birthing age. CD rates in some countries approach 50 per cent (Shorten 2007). That a randomised trial of average risk pregnancies has not yet been done suggests that such trials will not be done soon if ever. Several reports have explored why this is the case (Kotaska 2004; Lavender 2005; Turner 2008; Tilbrook 2009; PCRG 2008), all suggesting that the clinical situation is too complex and that preconceived preferences and biases among both patients and doctors would make randomisation nearly impossible. Yet in an even more complex clinical situation, breech presentation, a randomised trial has been done (Hannah 2002). Similar trials should be done among women with average risk pregnancies and hopefully with many fewer crossovers between VD and CD. It is only in this way that the separate effects of pregnancy and delivery on maternal pelvic floor function can be determined.
The next level of evidence is the prospective cohort study, a design that might provide the opportunity to establish a baseline continence status before pregnancy, labor or delivery and thus in the post partum continence assessments establish incidence rather than prevalence and so establish pregnancy factors as the etiology of the incontinence. There are six such cohorts within this review (Chaliha 1999; Eason 2002; Hannah 2002; Pinta 2004a; Altman 2007; Sultan 1993a), two of which included pre partum anal continence evaluations (Chaliha 1999; Pinta 2004a). The greatest advantage of the prospective cohort design is in studies for instance of dietary risk factors for colorectal cancer. The intervention is recorded prospectively and so was precise ‐ as dietary recall is notoriously inaccurate, and outcome also recorded as incidence, since the cohort would be ideally assured as disease free at inception by for instance an entrance colonoscopy. Subsequent disease onset is unlikely to be missed, as untreated it is lethal. In colorectal cancer studies polyps were often substituted for cancer, since investigators didn't have the patience or money to wait for cancer to occur. Polyps were thought to be good surrogates for cancer, though they have since been proven to be imperfect, especially since most polyps never evolve into cancer. So, to CD. The intervention here is CD vs. VD. It is unlikely that a woman does not accurately recall how her baby was born, each one, and if she had stitches versus no stitches and maybe even elective versus in labor.
Is outcome assessment more like to be better obtained in a prospective cohort than in a population based cross sectional survey? We have already written that sustained anal incontinence is the outcome of interest rather than transient dysfunction in the post‐partum period. Assurance that a woman was symptom free before pregnancy and before delivery would allow determination of incidence rather than prevalence and thus diminish the bias that might arise from varying prevalence in different groups. This may be better than recall years later, if earlier symptoms were assessed at all, which they were only in a minority of the included studies. Recall in this regard has not been rigorously assessed.
In addition, a healing perineum, even if unlacerated ‐ just stretched, may be prone to dysfunction, but in the context of this review, it is often transitory. Ascertainment at a time remote from delivery is key to determining if CD is protective. The prospective cohorts included in this review haven't, aside from (Altman 2007), done that.
Potential biases in the review process
see above
Agreements and disagreements with other studies or reviews
A meta‐analysis of published reports that assessed anal sphincter integrity after vaginal delivery and correlated this with continence stated that 77%‐83% (depending on parity) of anal incontinence in parous women was due to sphincter disruption (Oberwalder 2003). Three things are implied by this conclusion: first, that those not suffering sphincter disruption due to VD, specifically men, children, and nulliparous women, or women having CD, all being equally exposed to all other risk factors for anal incontinence, have a much lower risk of anal incontinence than women who have had a VD. There is scant epidemiologic evidence that this is the case (Nelson 2004). Second, it is implied that sphincter repair would be effective treatment for anal incontinence in almost all women whose incontinence follows a VD. Yet repair of disrupted sphincter has less than a perfect track record. Even more importantly, there is a reported rapid decay in function after repair that is far too great to be explained by age alone (Goffeng 1998, Guttierz 2005, Halverson 2002, Karoui 2000, Malouf 2000, Pinta 2003, Rothbart 2000, Vaizey 2004). Third, if direct trauma to the anal sphincter (and not intra‐pelvic nerves) were the major cause of anal incontinence, then CD should be effective in preventing incontinence. This review has shown that this is not the case.
An earlier version of this review as published based upon 16 reported studies and with largely the same conclusions as stated herein (Nelson2006).
Urinary incontinence has not been investigated in a Cochrane review though one systematic review has been reported (Press 2007). Sustained urinary incontinence in the studies analyzed also, as in this report, did not differ by birth mode. As with this review, this conclusion was based upon observational epidemiologic studies alone.
Authors' conclusions
Implications for practice.
No benefit for CD over VD can be demonstrated in this review of 21 non‐randomized studies. Elective primary CD in average risk women when done for the preservation of anal continence cannot be recommended. Average risk is the key factor. No doubt there are women who, due to previous trauma or pelvic reconstruction, cannot risk further trauma to the sphincter and for whom CD is appropriate. There is no evidence in included studies that such women constituted a significant number of women having CD, which could lead to a bias in favor of VD, and this situation would have been excluded in most of the best studies. In any case the results of this review state that based upon current evidence, a pregnant woman cannot be told that by having a CD she can reliably avoid anal incontinence.
Implications for research.
No adequate randomised trial of CD versus VD in average risk pregnancies with postpartum assessment of pelvic floor function, with the assessment done at an appropriate time and using an assessment tool to determine function properly has been done. Cross overs were the problem in the Term Breech Trial, a problem that should be avoidable in average risk pregnancies. There is no other issue in medicine that can approach the magnitude of this in size of population affected, cost and potential morbidity.
What's new
| Date | Event | Description |
|---|---|---|
| 17 May 2017 | Amended | PLS title changed according to feedback received in May |
History
Protocol first published: Issue 4, 2007 Review first published: Issue 2, 2010
| Date | Event | Description |
|---|---|---|
| 2 July 2009 | Amended | Subheadings in result section activated and Cindy Farquhar included as co‐author. Background and parts of the protocol have been rewritten to accommodate the new Revman subheadings but no major methodological changes were made. The study search was extended through July, 2009 |
| 26 May 2009 | Amended | Converted to new review format. |
| 18 July 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
(Eason 2002; Goldberg 2003; Hannah 2002; MacArthur 2005; MacLennan 2000; Varma 2006; Guise 2008; Hatem 2007; Altman 2007) Authors of each of these studies kindly provided additional information, data and analyses for this review.
Data and analyses
Comparison 1. Anal Incontinence, all studies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Post Partum Fecal Incontinence | 27 | Odds Ratio (Fixed, 95% CI) | Subtotals only | |
| 1.1 Feces; all studies | 27 | 55625 | Odds Ratio (Fixed, 95% CI) | 0.83 [0.73, 0.94] |
| 2 Post Partum Incontinence of Flatus | 8 | Odds Ratio (Fixed, 95% CI) | Totals not selected |
1.1. Analysis.
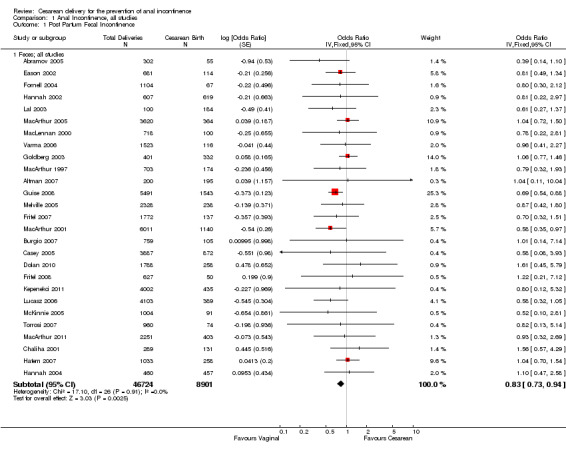
Comparison 1 Anal Incontinence, all studies, Outcome 1 Post Partum Fecal Incontinence.
1.2. Analysis.
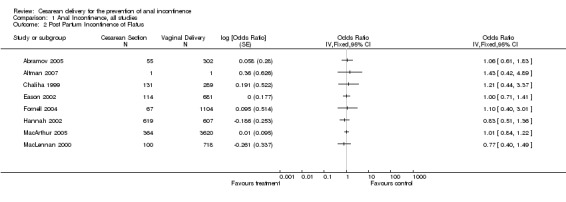
Comparison 1 Anal Incontinence, all studies, Outcome 2 Post Partum Incontinence of Flatus.
Comparison 2. Subgroup Analyses: Vaginal Delivery versus Cesarean Section.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incontinence of Feces; 13 best studies | 13 | Odds Ratio (Random, 95% CI) | 0.93 [0.77, 1.13] | |
| 2 Emergency versus Elective Cesarean Section | 6 | Odds Ratio (Fixed, 95% CI) | Totals not selected | |
| 3 Elective C. Section versus Vaginal Delivery | 4 | Odds Ratio (Fixed, 95% CI) | Totals not selected | |
| 4 Fecal Incontinence in Nulliparous versus All Deliveries | 4 | Odds Ratio (Fixed, 95% CI) | Totals not selected | |
| 5 Time Trend ‐ MacArthur | 3 | Odds Ratio (Fixed, 95% CI) | Totals not selected |
2.1. Analysis.
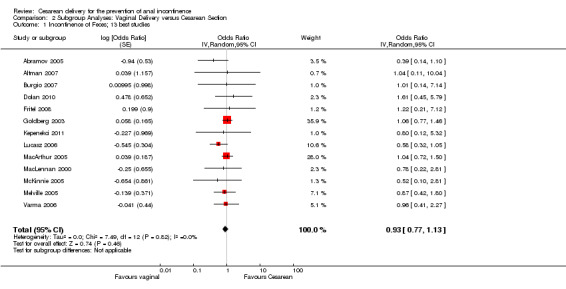
Comparison 2 Subgroup Analyses: Vaginal Delivery versus Cesarean Section, Outcome 1 Incontinence of Feces; 13 best studies.
2.2. Analysis.
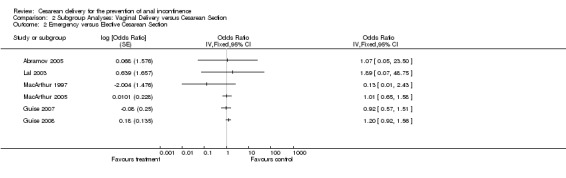
Comparison 2 Subgroup Analyses: Vaginal Delivery versus Cesarean Section, Outcome 2 Emergency versus Elective Cesarean Section.
2.3. Analysis.

Comparison 2 Subgroup Analyses: Vaginal Delivery versus Cesarean Section, Outcome 3 Elective C. Section versus Vaginal Delivery.
2.4. Analysis.
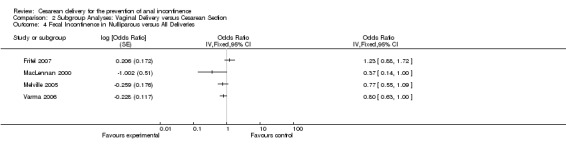
Comparison 2 Subgroup Analyses: Vaginal Delivery versus Cesarean Section, Outcome 4 Fecal Incontinence in Nulliparous versus All Deliveries.
2.5. Analysis.
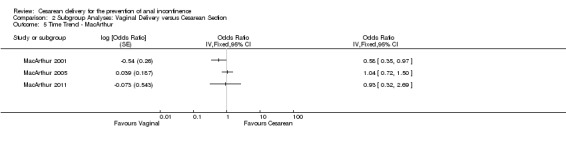
Comparison 2 Subgroup Analyses: Vaginal Delivery versus Cesarean Section, Outcome 5 Time Trend ‐ MacArthur.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abramov 2005.
| Methods | Cohort study, but with retrospective assessment of delivery methods and current incontinence assessment | |
| Participants | Discordant twin pairs | |
| Interventions | 271 identical Twin pairs that differed as to method of delivery of their babies: CD vs VD, as well as instrumented VD | |
| Outcomes | Incontinence of flatus and faeces, timing not stated | |
| Notes | validated incontinence assessment, logistic regression adjusting for major risk factors. | |
Altman 2007.
| Methods | Cohort, prospective data collection at first pregnancy with 10 year follow‐up. The only true prospective cohort study in this review. | |
| Participants | 200 women having only delivered vaginally and 195 women only delivered by CD | |
| Interventions | CD or un‐instrumented VD | |
| Outcomes | urinary or anal incontinence ‐ including gas and faeces, assessed 10 years after first delivery | |
| Notes | Regression model adjusted for age a first delivery, parity, mode of delivery, sphincter injury and interaction term between urine and anal. Prepartum incontinence excluded. | |
Borello‐France 2006.
| Methods | Multicenter cohort from the Pelvic Floor Disease Network in the USA | |
| Participants | Primiparas recruited immediately post partem | |
| Interventions | 3 types of delivery: Uncomplicated vaginal delivery n=390 Significant tear during vaginal delivery n=407 Caesarean delivery before labour n=124 |
|
| Outcomes | Flatus, Faecal and urinary incontinence at 6 weeks and 6 months post partem. | |
| Notes | Participants asked if they had incontinence of urine pre‐partem. 65% of anal incontinence resolved between 6 weeks and 6 months. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 84 drop outs at 6 weeks and 162 at 6 months VD for analysis at 6 mo= 319, CD = 105 and Tear = 335 |
Burgio 2007.
| Methods | CAPS study: Childbirth and Pelvic Symptoms study. | |
| Participants | Women from 7 cooperating centres, primiparous, with singleton pregnancies > 37 weeks gestation. | |
| Interventions | 3 cohorts: VD n=319, Sphincter tear n= 335 (repaired at delivery), and CD n=105. | |
| Outcomes | fecal and urinary incontinence | |
| Notes | no quantitative data or analyses presented to assess CD vs VD. see Borello‐France 2006 | |
Casey 2005.
| Methods | Single hospital cohort | |
| Participants | of primiparas recruited during labour. | |
| Interventions | CD n= 872, and VD n= 3015 | |
| Outcomes | Anal and urinary stress and urge incontinence at first post partem visit, said to be 5 to 7 months post partem, but in fact the mean interval was 54 days with a range of 14‐219 days. 88 had AI (2.2%). 0.67% had AI pre partem. | |
| Notes | of 10, 643 recruited, 3887 participated in the data collection at the first post partem visit. 65% got oxytocin during labour. Forceps and baby size best predictors of AI |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 37 % response rate to those initially approached. |
Chaliha 1999.
| Methods | Cohort, prospective | |
| Participants | 549 Pirimipara pregnant women | |
| Interventions | Spontaneous VD, instrumented VD or CD | |
| Outcomes | All aspects of pelvic floor function including incontinence of flatus, except fecal incontinence, assessed three months post partum | |
| Notes | Non‐adjusted | |
Chaliha 2001.
| Methods | Subset of the above cohort | |
| Participants | Primipara pregnant women | |
| Interventions | as above | |
| Outcomes | as above but with additional physiologic assessment anal function and anatomy, assessed three months post partum | |
| Notes | Non‐adjusted but in this publication was fecal incontinence by mode of delivery displayed | |
Dolan 2010.
| Methods | Cohort delivering their first baby at least 20 years earlier. | |
| Participants | Primips in 1983. Further divided into those that had more children (More) and those who did not and so had only the one pregnancy (P1). | |
| Interventions | CD, VD and forceps | |
| Outcomes | FI & UI | |
| Notes | awaiting crude numbers. Only analyses presented. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 888 of the original cohort of 3002 answered the bowel section of the questionnaire. |
Eason 2002.
| Methods | Nested cohort in an RCT | |
| Participants | 949 returned questionnaires of 1198 mailed. RCT of perineal massage in the 3rd trimester of pregnancy; pregnant women | |
| Interventions | Mode of delivery: CD vs VD. | |
| Outcomes | Incontinence of stool and flatus | |
| Notes | 60% primips. Adjusted analysis of multiple labor related factors including size of the infant, episiotomy, length of labor, mode of delivery , perineal trauma. Authors provided additional analyses including CD patients with no prior VD. Continence assessment at 3 months. | |
Fornell 2004.
| Methods | Population based survey, divided into age cohorts, retrospective | |
| Participants | 2000 Swedish women age 40 or 60 years (1000 @) | |
| Interventions | Mode of delivery: CD vs. VD | |
| Outcomes | Incontinence of faeces or flatus | |
| Notes | 1336 responses (67%). | |
Fritel 2007.
| Methods | Prospective cohort formation but retrospective data collection.. | |
| Participants | French Gazel Cohort. 20,000 Employees of the Gazel power company in 1989. 3114 women aged 45‐50 years surveyed in 1996 on perimenopausal issues and again in 2000, now age 50‐61 concerning incontinence and obstetric history. | |
| Interventions | Many health related issues including CD vs VD. | |
| Outcomes | Fecal incontinence, solid and liquid and flatus incontinence | |
| Notes | 85% response. Unadjusted odds ratios | |
Fritel 2008.
| Methods | 2 hospital cohort in France | |
| Participants | Primips in 1996 delivering at 37‐41 weeks a live baby and with an available address in 2000. n=774 | |
| Interventions | Primary outcome was comparing women in one hospital where episiotomy was routinely done to one where it was done selectively. CD = 50. VD = 368 | |
| Outcomes | Anal incontinence | |
| Notes | Adj for age, baby size, epidural, etc. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 627 returned the questionnaire (81%) |
Goldberg 2003.
| Methods | Cohort, retrospective | |
| Participants | 769 Mothers of Twins | |
| Interventions | CD vs. VD | |
| Outcomes | Incontinence of faeces, solid and liquid and flatus incontinence | |
| Notes | Age, delivery mode, parity adjusted. | |
Guise 2007.
| Methods | Cross sectional population based survey. | |
| Participants | All women delivering in the state of Oregon, USA in 2002. n=23,337 | |
| Interventions | Many delivery related variables including VD, instrumented VD, parity, infant weight, age, BMI, CD in or not in labor | |
| Outcomes | combined flatus/fecal incontinence | |
| Notes | The follow up publication (Guise 2008) allows direct comparison of CD and VD and this does not. Validated FI assessment. | |
Guise 2008.
| Methods | Cross sectional population based survey. | |
| Participants | From all women delivering in the state of Oregon, USA in 2002, those who were in their first pregnancy only. n=6152. | |
| Interventions | Many delivery related variables including VD, instrumented VD, parity, infant weight, age, BMI, CD in or not in labor | |
| Outcomes | combined flatus/fecal incontinence | |
| Notes | Odds ratios adjusted for all above factors CD incontinence 39% and VD, 48%. By far the highest of all studies. In part this is due to combined flatus/fecal incontinence, in part, since a single episode at any time since delivery was categorized as incontinence up to 3 months post partum. |
|
Hannah 2002.
| Methods | RCT ‐ Term Breech Trial | |
| Participants | Women with breech presentation pregnancies | |
| Interventions | Randomized to CD or VD | |
| Outcomes | Incontinence of faeces and flatus among many other outcomes | |
| Notes | 50% primips, 43% cross over in vaginal delivery group, 9.1% in the CD group. Outcomes therefore analysed "as treated" | |
Hannah 2004.
| Methods | RCT ‐ Term Breech Trial; | |
| Participants | Women with breech presentation pregnancies | |
| Interventions | Randomized to CD vs. VD | |
| Outcomes | Incontinence of faeces and flatus | |
| Notes | 50% primips,
43% cross over in vaginal delivery group, 9.1% in the CD group. Outcomes therefore analysed "as treated" 2 year follow‐up study of (Hannah 2002) of 44% of the initial randomised population. |
|
Hatem 2007.
| Methods | Population based survey | |
| Participants | mailed to 2492 primips 6 months post partum resident in the province of Quebec, Canada | |
| Interventions | VD or CD | |
| Outcomes | Single question for UI and AI at any time since delivery. Severity then assessed, for AI using the Vaizey score. | |
| Notes | No age adjustment. Not really a 6 month assessment as history of incontinence at any time since delivery categorized the participant as incontinent. | |
Kepenekci 2011.
| Methods | Cohort from 6 community health centres. | |
| Participants | Healthy women accompanying a friend or relative to a doctor's appointment. Excluded if pregnant, < 6 months post partem, significant illnesses. | |
| Interventions | Pregnancy history CD=435. VD 2308 | |
| Outcomes | AI, UI, Constipation, Obstructed defecation | |
| Notes | mean age 40.6 | |
Lal 2003.
| Methods | Cohort | |
| Participants | 284 primipara women | |
| Interventions | Mode of delivery, including separation of elective and emergent CD | |
| Outcomes | Incontinence of faeces (passive, urge, soiling) and flatus, interviewed 10‐12 months post partum | |
| Notes | Modified validated questionnaire and face to face interviews. Unadjusted odds ratios. | |
Lucasz 2006.
| Methods | Kaiser cohort | |
| Participants | women in 4 age cohorts. CD = 389. VD = 2927. Nullips = 787 . | |
| Interventions | among other, birth history. | |
| Outcomes | AI | |
| Notes | 25 % of cohort had AI (compared to 3.3% in | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | of 12,200 assessed for eligibility, 4103 participated (33.6%) |
MacArthur 1997.
| Methods | Single hospital cohort | |
| Participants | All women delivered in a 6 month period. n= 1606 | |
| Interventions | Mode of delivery, including separation of elective and emergent CD | |
| Outcomes | Incontinence to ? faeces? only | |
| Notes | 25+ weeks post partum postal survey. 80% response to a postal questionnaire and then follow‐up home visit and interview. Unadjusted odds ratios | |
MacArthur 2001.
| Methods | 3 single hospital cohorts cross sectional survey. | |
| Participants | All women (7879) delivered in 1 year in 3 centres in England, New Zealand and Scotland | |
| Interventions | Mode of delivery including unadjusted elective versus emergent section data. | |
| Outcomes | Only Incontinence of faeces separated by mode of delivery. 3 month postpartum assessment. | |
| Notes | Age, Mode of delivery, Race, BMI adjusted. | |
MacArthur 2005.
| Methods | Follow up of above (MacArthur2001) population cross‐sectional survey | |
| Participants | 4214 women form the previous survey | |
| Interventions | CD vs. VD | |
| Outcomes | Incontinence of faeces and flatus, 6 year assessment | |
| Notes | 6 year follow‐up of the 2001 publication (MacArthur 2001) with Age/Parity/Race, and dividing women into those that were primips, or had only previous CD adjustment. | |
MacArthur 2011.
| Methods | 12 year follow up of previously described cohort | |
| Participants | 2255 women from the previous survey | |
| Interventions | CD 403, VD 1852. Also CD in labour and CD before labour compared separatgely to VD and to each other for FI. | |
| Outcomes | UI and faecal incontinence | |
| Notes | Adj. for age/parity/BMI | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Non responders found to have similar demographics. |
MacLennan 2000.
| Methods | Population based cross sectional survey of pelvic floor dysfunction | |
| Participants | adults > 15 years old , both genders, not limited by parity. The South Australian Health Omnibus Survey of 1998. | |
| Interventions | Multiple risk factors including Mode of delivery in women who had been pregnant. | |
| Outcomes | Global pelvic floor assessment including incontinence of faeces and flatus. | |
| Notes | Authors provided raw data for Age/Parity adjustment. | |
McKinnie 2005.
| Methods | cohort from 6 gyne out patient centres. | |
| Participants | Pelvic Organ Support Study Project in the USA. mean age 42.7 +/‐ 13.8 | |
| Interventions | CD = 91. VD = 712. Nullips = 174 | |
| Outcomes | Faecal Incontinence. | |
| Notes | Foetal weight best predictor of FI. | |
Melville 2005.
| Methods | population based postal cross sectional survey. | |
| Participants | Random sample of women enrollees in the HMO Group Health Cooperative in Washington State, USA. n=6000 | |
| Interventions | A general health survey with mode of delivery, obstetrical history. | |
| Outcomes | Fecal incontinence adapted from the Wexner score. | |
| Notes | Odds Ratios adjusted for multiple factors. 3544 respondents. 7% reported fecal incontinence. | |
Torrosi 2007.
| Methods | Cohort of Primips multicentre in Italy | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Varma 2006.
| Methods | Population study randomly selected | |
| Participants | 2109 women 40‐69 years old in Kaiser Reproductive Risks for Incontinence Study with racial balancing. | |
| Interventions | Mode of Delivery | |
| Outcomes | Fecal (multiple strata of frequency) and flatus incontinence | |
| Notes | Adjusted for multiple variables including age and parity. Author provided additional analyses. | |
Williams 2007.
| Methods | ||
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bharucha 2006 | no direct comparison of CS and VD |
| Bharucha 2010 | 13 CS |
| Eogan 2011 | 85 in the cohort |
| Fynes 1998 | only injured sphincters |
| Grau 2010 | 4 FI |
| Groutz 1999 | 22 CS |
| Hall 2003 | 10 CS, 40 VD |
| Lewicki‐Gaupp 2008 | 74 in cohort |
| Okonkwo 2002 | 8 CS |
| Perry 2002 | mode of delivery not presented in parous women |
| Pinta 2004 | 24 CS, 75 VD |
| Roman 2004 | 17 AI and surveyed too early |
| Solans‐Domenech 2010 | Intrapartum FI |
| Sultan 1993 | 23 CS, 79 VD |
| Thompson 2002 | no FI |
CS; Cesarean Delivery
VD; Vaginal Delivery
FI; Faecal Incontinence
Characteristics of studies awaiting assessment [ordered by study ID]
Geissbuehler 2009.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | awaiting clarification and analyses (unpublished thesis) |
Differences between protocol and review
The search date has been extended to July, 2009, with the inclusion of 5 new studies and CF added as an author.
Contributions of authors
R. Nelson conceived of the project, did the literature search, wrote the review and did the analyses. SE Furner and M Westercamp assisted in statistical analysis and did additional analyses on individual patient data supplied by study authors.
C Farquhar assisted in the writing of the review and updating to the REVMAN 5 structure.
Declarations of interest
None known
Edited (no change to conclusions)
References
References to studies included in this review
Abramov 2005 {published data only}
- Abramov Y, Sand PK, Botros SM, Goldberg RP, et al. Risk factors for female anal incontinence: new insight through the Evanston‐Northwestern twin sisters study. Obstet. & Gynecol. 2005;106:726‐32. [DOI] [PubMed] [Google Scholar]
Altman 2007 {published data only}
- Altman D, Ekstrom A, Frosgren C, Nordenstam J, Zetterstrom J. Symptoms of anal and urinary incontinence following cesarean section or spontaneous vaginal delivery. Am J Obstet. Gynecol. 2007;197:512.e1‐e7. [DOI] [PubMed] [Google Scholar]
Borello‐France 2006 {published data only}
- Borello‐France D, Burgioo KL, Richter HE, Zycziinski H, et al. Fecal and urinary incontinence in primiparous women. Obstet Gynecol 2006;108(4):863‐72. [DOI] [PubMed] [Google Scholar]
Burgio 2007 {published data only}
- Burgio KL, Borello‐France D, Richter HE, Fitzgerals MP, et al. Risk factors for fecal and urinary incontinence after childbirth: the childbirth and pelvic symptoms study.. Am J Gastro 2007;102:1998‐2004. [DOI] [PubMed] [Google Scholar]
Casey 2005 {published data only}
- Casey BM, Schaffer JI, Bloom SL, Heartwell SF, et al. Obstetric antecedents for postpartum pelvic floor dysfunction. Am J Obstet Gynecol 2005;192:1655‐62. [DOI] [PubMed] [Google Scholar]
Chaliha 1999 {published data only}
- Chaliha C, Kalia V, Stanton SL, Monga A, Sultan AH. Antenatal prediction of postpartum urinary and fecal incontinence. Obstet. & Gynecol. 1999;94:689‐94. [DOI] [PubMed] [Google Scholar]
Chaliha 2001 {published data only}
- Chaliha C, Sultan AH, Bland JM, Monga A, Stanton SL. Anal function: effect of pregnancy and delivery. Am J Obstet. & Gynecol 2001;185:427‐32. [DOI] [PubMed] [Google Scholar]
Dolan 2010 {published data only}
- Dolan LM, Hilton P. Obstetric risk factors and pelvic floor dysfunction 20 years after first delivery. Int Urogynecol J 2010;21(5):535‐44. [DOI] [PubMed] [Google Scholar]
Eason 2002 {published data only}
- Eason E, Labrecque M, Marcoux S, Mondor M. Anal continence after childbirth. CMAJ 2002;107:326‐30. [PMC free article] [PubMed] [Google Scholar]
Fornell 2004 {published data only}
- Fornell EU, Wingren G, Kjoelhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiologic study. Acta Obstet Gynecol Scand. 2004;83:383‐9. [DOI] [PubMed] [Google Scholar]
Fritel 2007 {published data only}
- Fritel X, Ringa V, Varnous N, Zins M, Breart G. Mode of delivery and fecal incontinence at midlife. Obstet. & Gynecol. 2007;110:31‐38. [DOI] [PubMed] [Google Scholar]
Fritel 2008 {published data only}
- Fritel X, Schaal JP, Fauconnier A, Bertrand V, et al. Pelvic floor disorders 4 years after first delivery: a comparative study of restrictive versus systematic episiotomy. BJOG 2008;115(2):247‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goldberg 2003 {published data only}
- Goldberg RP, Kwon C, Gandhi S, Atkuru LV, et al. Prevalence of anal incontinence among mothers of multiples and analysis of risk factors. Am J Obstet. Gynecol. 2003;189:1627‐31. [DOI] [PubMed] [Google Scholar]
Guise 2007 {published data only}
- Guise J‐M, Morris C, Osterweil P, Li H, Rosenberg D, Greenlick M. Incidence of fecal incontinence after childbirth. Obstet. & Gynecol. 2007;109:281‐288. [DOI] [PubMed] [Google Scholar]
Guise 2008 {published data only}
- Guise J‐M, Boyles SH, Osterwel P, Li H, Eden KB, Mori M. Does cesarean protect against fecal incontinence in primiparous women?. Int. J. Urogynecol. 2008;20:61‐67. [DOI] [PubMed] [Google Scholar]
Hannah 2002 {published data only}
- Hannah ME, Hannah WJ, Hodnett ED, et al. Outcomes at 3 months after planned Cesarean vs. planned vaginal delivery for breech presentation at term. JAMA 2002;287:1822‐31. [DOI] [PubMed] [Google Scholar]
Hannah 2004 {published data only}
- Hannah ME, Whyte H, Hannah WJ, Hewson S, Amankwah K, Cheng M, Gafni A, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomised term breech trial.. Am J Obstet. Gynecol. 2004;191:917‐27. [DOI] [PubMed] [Google Scholar]
Hatem 2007 {published data only}
- Hatem M, Pasquier JC, Fraser W, Lepire E. Factors associated with postpartum urinary/anal incontinence in primiparious women in Quebec. J Obstet. Gynecol. 2007;29:232‐239. [DOI] [PubMed] [Google Scholar]
Kepenekci 2011 {published data only}
- Kepenekci I, Keskinkilic B, Akinsu F, Cakir P, Elhan AH, Erkek AB, Kuzu MA. Prevalence of pelvic floor disorders in the female population and the impact of age, mode of delivery and parity. Dis. Colon & Rectum 2011;54:85‐94. [DOI] [PubMed] [Google Scholar]
Lal 2003 {published data only}
- Lal M, Mann CH, Callender R, Radley S. Does Cesarean delivery prevent anal incontinence?. Obstet. & Gynecol. 2003;101:305‐12. [DOI] [PubMed] [Google Scholar]
Lucasz 2006 {published data only}
- Lucasz ES, Lawrence JM, Contreras R, Nager CW, Luber KM. Parity, mode of delivery and pelvic floor disorders.. Obstet Gynecol 2006;107:1253‐60. [DOI] [PubMed] [Google Scholar]
MacArthur 1997 {published data only}
- MacArthur C, Bick DE, Keithley MRB. Fecal incontinence after childbirth. Br J Obstet. & Gynecol. 1997;104:46‐50. [DOI] [PubMed] [Google Scholar]
MacArthur 2001 {published data only}
- MacArthur C, Glazener CMA, Wilson PD, Herbison GP. Obstetric practice and faecal incontinence three months after delivery.. Br J Obstet Gynecol 2001;108:678‐83. [DOI] [PubMed] [Google Scholar]
MacArthur 2005 {published data only}
- MacArthur C, Glazener CMA, Lancashire R, Herbison P, et al. Faecal incontinence and mode of first and subsequent delivery: a six‐year longitudinal study. Br J Obstet & Gynecol. 2005;112:1075‐82. [DOI] [PubMed] [Google Scholar]
MacArthur 2011 {published data only}
- MacArthur C, Glazener C, Lancashire R, Herbison P, Wilsond D. Exclusive caesarean section delivery and subsequent urinary and faecal incontinence: A 12‐year longitudinal study.. BJOG: An International Journal of Obstetrics and Gynaecology 2011;118(8):1001‐7. [DOI] [PubMed] [Google Scholar]
MacLennan 2000 {published data only}
- MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. J Obstet Gynecol. 2000;107:1460‐1470. [DOI] [PubMed] [Google Scholar]
McKinnie 2005 {published data only}
- McKinnie V, Swift S, Wang W, Woodman P, O'Boyle A, Kahn M, Valley M, Bland D, Shaffer J. The effect of pregnancy and mode of delivery on the prevalence of urinary and fecal incontinence. Am J Obstet Gynec 2005:512‐8. [DOI] [PubMed] [Google Scholar]
Melville 2005 {published data only}
- Melville JL, Fan M‐Y, Newton K, Fenner D. Fecal incontinence in US women: a population‐based study. Obstet. & Gynecol. 2005;193:2071‐2076. [DOI] [PubMed] [Google Scholar]
Torrosi 2007 {published data only}
- Torrisi G, Sampugnaro E.G, Pappalardo E.M, D'Urso E, Vecchio M, Mazza A. Postpartum urinary stress incontinence: Analysis of the associated risk factors and neurophysiological tests.. Minerva Ginecologica 2007;59(5):491‐498. [PubMed] [Google Scholar]
Varma 2006 {published data only}
- Varma MG, Brown JS, Creasman JM, Thom DH, Eeden SK, Beattie MS, Subak LL. Fecal incontinence in females older than 40 years: who is at risk?. Diseases of Colon & Rectum 2006;49(6):841‐851. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2007 {published data only}
- Williams A, Herron‐Marx S, Knibb R. The prevalence of enduring postnatal perineal morbidity and its relationship to type of birth and birth risk factors. .. Journal of Clinical Nursing 16(3), 549‐561. 2007 2007;16(3):549‐61. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bharucha 2006 {published data only}
- Bharucha AE, Zinsmeister AR, Locke GR, Seide BM, et al. Risk factors for fecal incontinence: a population based study in women. Am J Gastroent. 2006;101:1305‐1312. [DOI] [PubMed] [Google Scholar]
Bharucha 2010 {published data only}
- Bharucha AE, Zinsmeister AR, Schleck CD, Melton LJ 3rd. Bowel disturbances are the most important risk factors for late onset fecal incontinence: a population‐based case‐control study in women. Gastroenterology 2010;139(5):1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eogan 2011 {published data only}
- Eogan M, O'Brien C, Daly L, Behan M, O'Connell P.R, O'Herlihy C. The dual influences of age and obstetric history on fecal continence in parous women.. International Journal of Gynecology and Obstetrics 2011;112(2):93‐7. [DOI] [PubMed] [Google Scholar]
Fynes 1998 {published data only}
- Fynes M, Donnelly V.S, O'Connell P.R, O'Herlihy C. Cesarean delivery and anal sphincter injury.. Obstetrics and Gynecology 1998;92(41):496‐500. [DOI] [PubMed] [Google Scholar]
Grau 2010 {published data only}
- Grau J, Lacima G, Roura P, Rovira R, Estopina N, Cayuela E, Espuna M. 12 months follow‐up of post‐partum anal incontinence.. Progresos de Obstetricia y Ginecologia 2010;53(1):18‐23. [Google Scholar]
Groutz 1999 {published data only}
- Groutz A, Fait G, Lessing JB, et al. Incidence and obstetric risk factors of postpartum anal incontinence. Scan J Gastronet. 1999;34:15‐18. [DOI] [PubMed] [Google Scholar]
Hall 2003 {published data only}
- Hall W, McCracken K, Osterweil P, Guise J‐M. Frequency and predictors for postpartum fecal incontinence. AmJ Obstet. Gyencol. 2003;188:1205‐7. [DOI] [PubMed] [Google Scholar]
Lewicki‐Gaupp 2008 {published data only}
- Lewicky‐Gaupp C, Cao D.‐C, Culbertson S. Urinary and Anal Incontinence in African American Teenaged Gravidas during Pregnancy and the Puerperium.. Journal of Pediatric and Adolescent Gynecology 2008;21(1):21‐6. [DOI] [PubMed] [Google Scholar]
Okonkwo 2002 {published data only}
- Okonkwo J, Obionu C.N, Okonkwo C.V, Obiechina N.J.A. Anal incontinence among IGBO (Nigerian) women.. International Journal of Clinical Practice 2002;56(3):178‐180. [PubMed] [Google Scholar]
Perry 2002 {published data only}
- Perry S, Shaw C, McGrother C, Matthews RJ, et al. Prevalence of faecal incontinence in adults aged 40 years or more living in the community. Gut 2002;50:480‐484. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinta 2004 {published data only}
- Pinta TM, Kylanpaa M‐L, Teramo KA, Luukkonen PS. Sphincter rupture and anal incontinence after first vaginal delivery. Acta Obstet. Gynecol Scand 2004;83:917‐22. [DOI] [PubMed] [Google Scholar]
Roman 2004 {published data only}
- Roman H, Robillard P.‐Y, Payet E, Amrani R, Verspyck E, Marpeau L, Barau G. Factors associated with fecal incontinence after childbirth: Prospective study in 525 women.. Journal de Gynecologie Obstetrique et Biologie de la Reproduction 33(6 I), 497‐505. 2004. 2004;33(61):497‐505. [DOI] [PubMed] [Google Scholar]
Solans‐Domenech 2010 {published data only}
- Solans‐Domenech M, Sanchez E, Espuna‐Pons M. Urinary and anal incontinence during pregnancy and postpartum: Incidence, severity, and risk factors. .. Obstetrics and Gynecology 2010;115(3):618‐28. [DOI] [PubMed] [Google Scholar]
Sultan 1993 {published data only}
- Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartam CI. Anal sphincter disruption during vaginal delivery. N Eng J Med 1993;329:1905‐11. [DOI] [PubMed] [Google Scholar]
Thompson 2002 {published data only}
- Thompson J.F, Roberts C.L, Currie M, Ellwood D.A. Prevalence and persistence of health problems after childbirth: Associations with parity and method of birth.. Birth 2002;29(2):83‐94. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Geissbuehler 2009 {published data only}
- Geissbuehler V and Raschle M.W. International Urogynecology Journal and Pelvic Floor Dysfunction Conference: 34th Annual Meeting of the International Urogynecological Association, IUGA Lago di Como Italy. Conference Start: 20090616 Conference End: 20090620. Conference Publication:(var.pagings). Urinary stress incontinence, fecal incontinence and dyspareunia one year after first delivery. Vaginal delivery is compared with cesarean section.. Urinary stress incontinence, fecal incontinence and dyspareunia one year after first delivery. Vaginal delivery is compared with cesarean section. 2009;1:50‐1. [Google Scholar]
Additional references
Abramowitz 2000
- Abramatowitz I, Sobhani I, Ganansia R. Are sphincter defects the cause of anal incontinence after vaginal delivery? Results of a prospective survey. Dis. Colon & Rectum 2000;43:590‐6. [DOI] [PubMed] [Google Scholar]
Amu 1998
- Amu O, Rajendran S, Bolaji II. Should doctors perform an elective Cesarean section on request? Maternal choice alone should not determine method of delivery. BMJ 1998;317:463‐5. [PubMed] [Google Scholar]
Behague 2002
- Behague DP, Victoria CG, Barros FC. Consumer demand for caesarean sections in Brazil; informed decision making, patient choice or social inequality? A population based birth cohort study linking ethnographic and epidemiological methods. BMJ 2002;321:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Declercq 2005
- Declercq E, Menacker F, MacDorman M. Rise on "no indicated risk" primary caesareans in the United States, 1991‐2001: cross sectional analysis. BMJ 2005;330:71‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Devine 1999
- Devine JB, Ostergard DR, Noblett KL. Long term complications of the second stage of labor. Contemp Obstet Gyencol 1999;x:119‐26. [Google Scholar]
Faridi 2002
- Faridi FA, Willis S, Schelzig P, Siggelkow W, Schumpelick V, Rath W. Anal sphincter injury during vaginal delivery ‐ an argument for Cesarean section on request?. Perinat. Med 2002;30:379‐87. [DOI] [PubMed] [Google Scholar]
Farrell 2002
- Farrell SA. Cesarean Section versus forceps‐assisted vaginal birth: It's time to include pelvic injury in the risk benefit equation. Can. Med. Assn J 2002;155:117‐8. [PMC free article] [PubMed] [Google Scholar]
Goffeng 1998
- Goffeng AR, Andersch B, Andersson M, Berndtsson I, Hulten L, Oreslan T. Objective methods cannot predict anal incontinence after primary repair of extensive anal tears. Acta Obstet Gynecol Scand 1998;77:439‐43. [PubMed] [Google Scholar]
Grady 2008
- Grady. After Caesareans, some see higher insurance cost. New York Times 2008, issue June 1.
Greene 2004
- Greene MF. Vaginal birth after Cesarean revisited. N Eng J Med 2004;351:2647‐8. [DOI] [PubMed] [Google Scholar]
Guise 2004
- Guise JM, McDonough MS, Osterwell P, Nygren P, Chan KS, Helfand M. Systematic review of the incidence and consequences of uterine rupture in women with previous Cesarean section. BMJ 2004;329:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guttierz 2005
- Guttierz AB, Madoff RD, Lowry AC, Parker SC, Buie WD, Baxter NN. Long term results of anterior sphincteroplasty. Dis Colon & Rectum 2004;47:727‐32. [DOI] [PubMed] [Google Scholar]
Halverson 2002
- Halverson AN, Hull TL. Lon‐term outcome of overlapping anal sphincter repair. Dis Colon & Rectum 2002;45:345‐8. [DOI] [PubMed] [Google Scholar]
Henderson 2001
- Henderson J, McClandlish R, Kumiega L, Petrou S. Systematic review of economic aspects of alternative modes of delivery. Br J Obstet Gynecol 2001;108:149‐57. [DOI] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [Updated February 2008]. www.cochrane‐handbook.org The Cochrane Collaboration, 2008.
Howard 1999
- Howard RJ. Pregnant Women should have choices. BMJ 9 January, 1999; 318:122. [PubMed]
Hsu 2008
- Hsu KH, Liao PJ, Hwang CJ. Factors affecting Taiwanese women's choice of Cesarean section. Soc Sci Med 2008;66(1):201‐9. [DOI] [PubMed] [Google Scholar]
Idama 1999
- Idama TO, Lindow SW. Safest option is still to aim for vaginal delivery. Br Med J 1999;318:121. [PubMed]
Jacobsen 2004
- Jacobsen AF, Drolsum AM, Klow NE. Deep vein thrombosis after elective Cesarean section. Thrombosis res. 2004;113:283‐8. [DOI] [PubMed] [Google Scholar]
Karoui 2000
- Karoui S, Leroi AM, Koning E, Menar JF, Michot F, Dens P. Results of sphincteroplasty in 86 patients with anal incontinence. Dis Colon & Rectum 2000;43:813‐20. [DOI] [PubMed] [Google Scholar]
Klein 2004
- Klein MC. Elective Cesarean section. Can Med Assn J 2004;171:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kmietowicz 2008
- Kmietowicz Z. BMJ 2008;328;1031. [DOI] [PMC free article] [PubMed]
Kotaska 2004
- Kotaska A. Inappropriate us of randomised trials to evaluate complex phenomena: a case study. BMJ 2004;329:1039‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Landon 2004
- Landon MB, Hauth JC, Leveno KJ. Maternal and perinatal outcomes associated with a trial of labor after prior Cesarean delivery. N Eng J Med 2004;351:2581‐9. [DOI] [PubMed] [Google Scholar]
Lavender 2005
- Lavender T, Kingdon C, Hart A, Gyte G, Gabbay M, Neilson JP. Could a randomised trial answer the controversy relating to elective caesarean section? National survey of consultant obstetricians and heads of midwifery. BMJ 2005;331:490‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2005
- Liu S, Heaman M, Joseph KS, Liston RM. Risk of maternal postpartum readmission associated with mode for delivery. Obstet Gynecol 2005;105:836‐42. [DOI] [PubMed] [Google Scholar]
Lockwood 2004
- Lockwood CJ. Cesarean delivery: is it time to embrace elective procedures?. Contemp. Ob/Gyn 2004;12:8‐10. [Google Scholar]
Makoha 2004
- Makoha FW, Felimban HM, Fatthuddien MA, Roomi F, Ghabra T. Multiple cesarean section morbidity. Int J Obstet Gyencol 2004;87:227‐32. [DOI] [PubMed] [Google Scholar]
Malouf 2000
- Malouf AJ, Norton CS, Engel AF, Nicholls RJ, Kamm MA. Long‐term results of overlapping anterior anal sphincter repair for obstetrical trauma. Lancet 2000;355:260‐5. [DOI] [PubMed] [Google Scholar]
Minkoff 2003
- Minkoff H, Chervenak FA. Elective primary Cesarean delivery. N Eng J Med 2003;348:946‐50. [DOI] [PubMed] [Google Scholar]
Mollison 2005
- Mollison J, Porter M, Cambell D, Bhattacharya S. Primary mode of delivery and subsequent pregnancy. Br J Obstet Gynecol 2005;112:1061‐5. [DOI] [PubMed] [Google Scholar]
Morales 2007
- Morales KJ, Gordon MC, Bates Jr GW. Postcesarean delivery adhesions associated with delayed delivery of infant.. Am J Obstet Gynecol 2007;196:461, e1‐e6. [DOI] [PubMed] [Google Scholar]
Murray 2000
- Murray S. Relation between private health insurance and high rates of caesarean section in Chile: qualitative and quantitative study. BMJ 2000;321:1501‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 1998
- Nelson RL, Furner S, Jesudason V. Fecal incontinence in Wisconsin Nursong Homes: Prevalence and Associations. Diseases of the Colon & Rectum 1998;41:1226‐1229. [DOI] [PubMed] [Google Scholar]
Nelson 2004
- Nelson RL. Epidemiology of fecal incontinence. Gastroenterol. 2004;126:s3‐7. [DOI] [PubMed] [Google Scholar]
Nelson2006
- Nelson RL, Westercamp M, Furner SE. A systematic review of the efficacy of Cesarean section in the preservation of anal continence. Dis. Colon & Rectum 2006;49:1‐9. [DOI] [PubMed] [Google Scholar]
NIH 2006
- NIH Consensus Conference. Cesarean Delivery on Maternal Request. NIH consensus and state of the science statements; http://consensus.nih.gov/2006/CesareanStatement_Final053106.pdf 2006;23(1):1‐29. [PubMed] [Google Scholar]
Nygaard 2003
- Nygaard IE, Cruickshank FA. Should all women be offered elective Cesarean section. Obstet Gynecol. 2003;102:217‐9. [DOI] [PubMed] [Google Scholar]
Oberwalder 2003
- Oberwalder M, Connor J, Wexner SD. Meta‐analysis to determine the incidence of obstetric anal sphincter damage. Br J Surg 2003;90:1333‐37. [DOI] [PubMed] [Google Scholar]
Paterson‐Brown 1998
- Paterson‐Brown S. Should doctors perform an elective caesarean section on request? Yes, as long as the woman is fully informed.. BMJ 1998;317:462‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
PCRG 2008
- Preference Collaborative Review Group. Patients' preferences within randomised trials: systematic review and patient level meta‐analysis. BMJ 2009;338:85‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinta 2003
- Pinta T, Kyaanpaa ML, Salmi T, Jaarvinen HJ, Luukkonen P. Delayed sphincter repair for obstetric ruptures: analysis of failure. Colorectal Dis 2003;5:73‐8. [DOI] [PubMed] [Google Scholar]
Potter 2001
- Potter JE, Berquo E, Perpetuo IHO, Leal OF, Hopkins K, Souza MR, Formiga MCdeC. Unwanted caesarean sections among public and private patients in Brazil: prospective study.. Br. Med J 2001;323:1155‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Press 2007
- Press JZ, Klein MC, Kaczoroski J, Liston RM, Dadelszen P. Does Cesarean section reduce postpartum urinary incontinence? A systematic review.. Birth 2007;34(3):228‐237. [DOI] [PubMed] [Google Scholar]
Roduit 2009
- Roduit C, Scholtens S, Jongste JC, Wijga AH, Gerritsen J, Postma DS, et al. Asthma at 8 years of age in children born by caesarean section. Thorax 2009;64(2):107‐13. [DOI] [PubMed] [Google Scholar]
Rose 2009
- Rose D. Caesarean deliveries go up, despite dangers. The Times (London) 2009, issue 1 May:23.
Rothbart 2000
- Rothbart J, Bemelman WA, Meijerink WJ. Long term results of anterior anal sphincter repair for fecal incontinence due to obstetric injury. Dig. Surg 2000;17:390‐4. [DOI] [PubMed] [Google Scholar]
Shorten 2007
- Shorten A. Maternal and neonatal effects of caesarean section; More accurate estimates of benefits and harms are needed to support informed childbirth choices. Br Med J 17 November 2007;335:1003‐4. [Google Scholar]
Tilbrook 2009
- Tilbrook H. Patients' preferences within randomised trial: systematic review and patient level meta‐analysis. Br Med J 2009;338:85‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tita 2009
- Tita ATN, Landon MB, Spong CY, Lai Y, Leveno KJ, et al. Timing of elective repeat cesarean delivery at term and neonatal outcomes.. New Eng J Med 2009;360(2):111‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 2008
- Turner CE, Young JM, Solomon MJ, Ludlow, Bennes C, Phipps H. Willingness of pregnant women and clinicians to participate in a hypothetical randomized controlled trial comparing vaginal delivery and elective caesarean section. Aust New Zeal J Obstet Gynecol 2008;48:542‐6. [DOI] [PubMed] [Google Scholar]
Vaizey 2004
- Vaizey CJ, Norton C, Thornton MJ, Nicholls RJ, Kamm MA. Long term results of repeat anterior anal sphincter repair. Dis Colon & Rectum 2004;47:858‐63. [DOI] [PubMed] [Google Scholar]
van Roosmalen 1999
- Roosmalen J. Unnecessary caesarean sections should be avoided. BMJ 1999;318:121. [PubMed]
Villar 2007
- Villar J, Carroli G, Zavaleta N, Donnor A, et al. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicenter prospective study. Br Med J 17 November, 2007;335:1025‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zetterstrom 1999
- Zetterstrom J, Lopez A, Anzen B, Dolk A, Norman M, Mellgren A. Anal incontinence after vaginal delivery: a prospective study in primiparous women. Obstete Gynecol 1999;106:324‐30. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Nelson 2006
- Nelson RL, Westercamp M, Furner SE. A systematic review of cesarean section and the prevention of anal incontinence. Diseases of Colon & Rectum 2006;49:1587‐95. [DOI] [PubMed] [Google Scholar]


