This cohort study evaluates the risk of depression and anxiety in patients with chronic rhinosinusitis by disease phenotype (with and without nasal polyps) in a nationwide insurance data set.
Key Points
Question
Is chronic rhinosinusitis associated with the risk of depression and anxiety?
Findings
In this cohort study of 48 672 participants in a nationwide insurance data set, the overall incidence of depression and anxiety during the 11-year follow-up was higher in the group with chronic rhinosinusitis than in the comparison group. The adjusted hazard ratio for development of depression and anxiety was higher in the chronic rhinosinusitis group without nasal polyps vs those with nasal polyps.
Meaning
An increased incidence of depression and anxiety appears to be associated with chronic rhinosinusitis, and patients without nasal polyps seem to be at a higher risk of developing depression and anxiety than those with nasal polyps.
Abstract
Importance
Chronic rhinosinusitis (CRS) is associated with a decreased quality of life, affecting physical and emotional aspects of daily function, the latter of which could manifest as depression and anxiety.
Objective
To evaluate the risk of depression and anxiety in CRS, depending on the CRS phenotype (CRS without nasal polyps [CRSsNP] and CRS with nasal polyps [CRSwNP]).
Design, Setting, and Participants
This retrospective nationwide cohort study used population-based insurance data (consisting of data from approximately 1 million patients). The study population included 16 224 patients with CRS and 32 448 individuals without CRS, with propensity score matching between groups according to sociodemographic factors and enrollment year. Data were collected from January 1, 2002, through December 31, 2013, and analyzed from July 1 through November 15, 2018.
Main Outcomes and Measures
Survival analysis, the log-rank test, and Cox proportional hazards regression models were used to calculate the incidence, survival rate, and hazard ratio (HR) of depression and anxiety for each group.
Results
Among the 48 672 individuals included in the study population (58.8% female), the overall incidence of depression during the 11-year follow-up was 1.51-fold higher in the CRS group than in the non-CRS group (24.2 vs 16.0 per 1000 person-years; adjusted HR, 1.54; 95% CI, 1.48-1.61). The incidence of anxiety was also higher in the CRS group than in the comparison group (42.2 vs 27.8 per 1000 person-years; adjusted HR, 1.57; 95% CI, 1.52-1.62). Moreover, the adjusted HRs of developing depression (CRSsNP, 1.61 [95% CI, 1.54-1.69]; CRSwNP, 1.41 [95% CI, 1.32-1.50]) and anxiety (CRSsNP, 1.63 [95% CI, 1.57-1.69]; CRSwNP, 1.45 [95% CI, 1.38-1.52]) were greater in patients with CRSsNP than in those with CRSwNP.
Conclusions and Relevance
This observational study suggests that CRS is associated with an increased incidence of depression and anxiety. Specifically, findings from this study found that patients without nasal polyps showed a higher risk of developing depression and anxiety than those with nasal polyps.
Introduction
Chronic rhinosinusitis (CRS) is one of the most prevalent chronic diseases and consists of a group of disorders characterized by inflammation of the sinonasal mucosa lasting for more than 12 weeks.1,2 The cause of CRS is likely multifactorial, with various contributory inflammatory mechanisms that ultimately determine the clinical phenotype that manifests.3,4 Chronic rhinosinusitis is clinically classified into 2 phenotypes (based on the nasal endoscopic findings with regard to nasal polyps), that is, CRS with nasal polyps (CRSwNP) or CRS without nasal polyps (CRSsNP). The CRSwNP phenotype is usually associated with greater severity of clinical disease.2
It is well known that CRS places a considerable burden on society and the health care system in terms of direct health care costs and other indirect costs.5,6 In addition, CRS can have a considerable effect on the patient’s health-related quality of life by causing physical, social, emotional, and cognitive impairment. Moreover, CRS can be associated with a range of therapy-induced adverse effects and exert a financial influence on the patient.6,7 Mental health problems related to CRS, such as depression and anxiety, also affect the patient’s health-related quality of life and can create challenges in medical management.8,9,10
The severity of CRS based on nasal endoscopy and computed tomographic imaging findings correlates poorly with symptom scores. One of the potential causes for this discordance is the presence of mental health problems, such as depression and anxiety. Such comorbid mental health problems in patients with CRS are usually associated with increased use of health care resources, antibiotic use, and missed workdays.11 Furthermore, mental health problems may present as physical complaints with or without objective findings, leading to patient and physician confusion and frustration.12,13 Sometimes, exploration of emotional issues may be uncomfortable for a physician who has yet to establish a strong relationship with the patient.12 Several previous cross-sectional studies9,11,14,15 have reported that depression and anxiety are quite common in patients with CRS. However, the causal relationship between CRS and mental health conditions is not yet fully understood. Whether patients report higher levels of CRS symptoms because of their depression and/or anxiety or whether the effects of CRS on quality of life contribute to depression and anxiety remains unclear.
Therefore, in the present study, we aimed to investigate the association between CRS and prospective risk of developing mental health problems, such as depression and anxiety. We used a nationwide representative sample of 1 025 340 adults from the 2002-2013 National Sample Cohort of the Korea National Health Insurance Service (KNHIS-NSC) in South Korea. Because this nationwide population-based data set contains information about the history of use of medical services for more than 1 million Koreans, we could examine the association between each CRS phenotype and the risk of mental health problems while adjusting for clinical and demographic factors.
Methods
Korea National Health Insurance Service
National health insurance has provided health coverage to the entire South Korean population since 1989. Therefore, every South Korean is enrolled in the KNHIS and nearly all data from the health care system are stored in large central databases. The KNHIS controls all medical costs among beneficiaries, medical providers, and the government. Almost all medical data, including diagnostic codes, procedures, prescription drugs, and personal information, are included in the KNHIS database. Each South Korean resident is assigned a unique identification number at birth, and this number is used by the KNHIS to identify individuals. Thus, health care claim data are not omitted or duplicated. The Korean Classification of Diseases (KCD), a system similar to the International Classification of Diseases, is used in the KNHIS to assign diagnostic codes. In the present study, we used KNHIS-NSC data collected from January 1, 2002, through December 31, 2013, consisting of information from a nationally representative sample of 1 025 340 random individuals and accounting for approximately 2.2% of the South Korean population in 2002. In 2002, we conducted stratified random sampling among the South Korean population of 46 million with 1476 strata by age (18 groups), sex (2 groups), and income level (41 groups, including 40 health insurance and 1 medical aid beneficiary). Study protocols adhered to the tenets of the Declaration of Helsinki and used KNHIS-NSC data (NHIS-2017-2-556) from the KNHIS. This study was also approved by the institutional review board of Hallym Medical University, Chuncheon Sacred Hospital, Chuncheon, Republic of Korea, which waived the need for written informed consent because the KNHIS-NSC data set consisted of deidentified secondary data for research purposes.
Study Population
The CRS group included all patients who received inpatient and outpatient care for an initial diagnosis of CRS from January 1, 2002, through December 31, 2004. To improve the accuracy of the diagnostic code, the operational definition of CRS in the present study included CRS (KCD code J32 [CRSsNP] or KCD code J33 [CRSwNP]) diagnosed more than once at intervals of 3 months or more. This definition was used because the diagnosis of CRS requires that it is clinically persistent for more than 12 weeks. Also, we included only patients who underwent nasal endoscopy in this period. Patients who fit this criterion were included in the study. The exclusion criteria were as follows: (1) younger than 18 years; (2) a diagnosis of depression and anxiety from January 1, 2002, to December 31, 2004, before the diagnosis of CRS; (3) death from any cause from January 1, 2002, through December 31, 2004; and (4) a diagnosis of CRS (KCD codes J32 or J33) before January 1, 2002. The comparison group (2 patients for every 1 patient with CRS) was selected with propensity score matching according to age, sex, residential area, and household income. Finally, we enrolled 16 224 eligible patients with CRS (10 763 with CRSsNP and 5461 with CRSwNP). Each patient was tracked until December 31, 2013, or until the occurrence of depression and anxiety, according to KCD codes (eTable 1 in the Supplement). In addition, we included only patients who were diagnosed with depression and anxiety by a psychiatrist and those who visited clinics more than 2 times within 3 months.
Variables and Operational Definition of CRS
Details of patients’ age, sex, residence, household income, and comorbidities were obtained from the database. The study population was divided into 3 age groups (<45, 45-64, and >64 years), 3 income groups (low [≤30.0% of the national median]; middle [30.1%-69.9% of the national median]; and high [≥70.0% of the national median]), and 3 residential areas (Seoul, the largest metropolitan region in South Korea; other metropolitan cities in South Korea; and small cities and rural areas).
The operational definitions of the study end points were all-cause mortality or the incidence of depression and anxiety. Patients were censored after December 31, 2013, if they did not experience any events and if they were alive until that date. Risks for depression and anxiety were compared between the CRS and non-CRS groups based on person-years at risk, which was defined as the duration from the date of CRS diagnosis or January 1, 2002 (for the comparison group), to the end point. We presented the amount of missing data on eTable 2 in the Supplement.
Statistical Analysis
Data were analyzed from July 1 to November 15, 2018. Descriptive and χ2 analyses were conducted to identify sex, age groups, residence, and household income and evaluate the difference in variables of study participants. To calculate the effect size for χ2 analysis, we used the Φ or Cramer V statistic; the Monte Carlo method was applied to extract 95% CIs of exact significance. We explained that no difference occurs in variables for the χ2 test when values of effect size are less than the reference values (small effect size: 0.10 [df = 1] vs 0.07 [df = 2]). Kaplan-Meier analysis was performed to identify the difference of survival functions among study groups. The overall depression- and anxiety-free survival rates for the observation period were determined with the Kaplan-Meier survival curve. To identify whether CRS increased the risk of occurrence of depression and anxiety, we used Cox proportional hazards regression analyses to calculate the hazard ratio (HR) and 95% CI, adjusting for other outcome variables. Incidence rates per 1000 person-years for depression and anxiety were obtained by dividing the number of patients with depression and anxiety by person-years at risk. All statistical analyses were performed with R software (version 3.4.3; R Foundation for Statistical Computing). Two-sided P < .05 was considered statistically significant.
Results
The present study consisted of 10 763 patients with CRSsNP, 5461 with CRSwNP, and 32 448 non-CRS controls for a total study population of 48 672 (41.2% male and 58.8% female). Similar distributions of sex, age, residential area, household income, and comorbidities were observed in the the 3 groups. In addition, these variables have no difference between study groups because they have very small effect size values. Therefore, they were used for sample matching so that group matching could be performed appropriately. Table 1 presents the characteristics of the study population for the 3 cohorts.
Table 1. Characteristics of Study Participants.
| Variable | Study Group, No. (%) | Effect Size (95% CI) | χ2 | ||
|---|---|---|---|---|---|
| Comparison (n = 32 448) | CRS (n = 16 224) | ||||
| CRSsNP (n = 10 763) | CRSwNP (n = 5461) | ||||
| Sex | |||||
| Male | 13 357 (41.2) | 3753 (34.9) | 2929 (53.6) | 0.000 (0.967-0.970) | 0.002 |
| Female | 19 091 (58.8) | 7010 (65.1) | 2532 (46.4) | ||
| Age, y | |||||
| <45 | 19 990 (61.6) | 6891 (64.0) | 3050 (55.9) | 0.006 (0.384-0.394) | 1.911 |
| 45-64 | 9880 (30.4) | 3047 (28.3) | 1889 (34.6) | ||
| >64 | 2578 (7.9) | 825 (7.7) | 522 (9.6) | ||
| Residence area | |||||
| Seoul | 8789 (27.1) | 3143 (29.2) | 1226 (22.5) | 0.007 (0.257-0.265) | 2.677 |
| Other metropolitan | 8545 (26.3) | 2940 (27.3) | 1444 (26.4) | ||
| Rural and small city | 15 114 (46.6) | 4680 (43.5) | 2791 (51.1) | ||
| Household income, % of national median | |||||
| ≤30.0 (low) | 5700 (17.6) | 1861 (17.3) | 1031 (18.9) | 0.003 (0.776-0.784) | 0.501 |
| 30.1-69.9 (middle) | 12 244 (37.7) | 4000 (37.2) | 2106 (38.6) | ||
| ≥70.0 (high) | 14 504 (44.7) | 4902 (45.5) | 2324 (42.6) | ||
Abbreviations: CRS, chronic rhinosinusitis; CRSwNP, CRS with nasal polyps; CRSsNP, CRS without nasal polyps.
We used univariate and multiple Cox regression models to analyze the HRs for the development of depression and anxiety during the 11-year follow-up period. The overall incidence of depression was significantly higher in the CRS group (24.2 per 1000 person-years) than in the comparison group (16.0 per 1000 person-years), with an adjusted HR of 1.54 (95% CI, 1.48-1.61). In addition, we observed a significantly higher incidence of anxiety in the CRS group (42.2 per 1000 person-years) than in the comparison group (27.8 per 1000 person-years) with an adjusted HR of 1.57 (95% CI, 1.52-1.62).
When we performed the subgroup analysis according to CRS phenotypes, a significantly higher incidence of depression and anxiety occurred in the CRSsNP group compared with the CRSwNP group (Table 2 and Table 3). Thus, the incidences of depression and anxiety in the CRSsNP group were 25.2 and 43.7 per 1000 person-years, respectively, whereas incidences in the CRSwNP group were 22.1 and 39.2 per 1000 person-years, respectively. After adjusting for sociodemographic factors (sex, age, residential area, and household income) and comorbidities, we found that patients with CRSsNP had a significant likelihood of prospective development of depression and anxiety (adjusted HR for depression, 1.61 [95% CI, 1.54-1.69]; adjusted HR for anxiety, 1.63 [95% CI, 1.57-1.69]), as indicated by the results of multiple Cox proportional hazards regression analyses of all variables. Meanwhile, in the CRSwNP group, the adjusted HRs for depression and anxiety were 1.41 (95% CI, 1.32-1.50) and 1.45 (95% CI, 1.38-1.52), respectively.
Table 2. Incidence per 1000 Person-Years and Hazard Ratios for Depression During an 11-Year Follow-up Period.
| Variable | No. of Participants | No. of Cases | Incidence per 1000 Person-Years | HR (95% CI) | |
|---|---|---|---|---|---|
| Unadjusted | Adjusted | ||||
| Group | |||||
| Comparison | 32 448 | 5202 | 16.0 | 1 [Reference] | 1 [Reference] |
| CRSsNP | 10 763 | 2618 | 25.2 | 1.59 (1.52-1.67) | 1.61 (1.54-1.69) |
| CRSwNP | 5461 | 1154 | 22.1 | 1.40 (1.31-1.49) | 1.41 (1.32-1.50) |
| Sex | |||||
| Male | 20 039 | 2805 | 13.9 | 1 [Reference] | 1 [Reference] |
| Female | 28 633 | 6169 | 22.0 | 1.59 (1.52-1.66) | 1.62 (1.55-1.70) |
| Age, y | |||||
| <45 | 29 931 | 3804 | 12.3 | 1 [Reference] | 1 [Reference] |
| 45-64 | 14 816 | 3846 | 27.3 | 2.25 (2.15-2.35) | 2.33 (2.22-2.43) |
| >64 | 3925 | 1324 | 40.7 | 3.46 (3.25-3.68) | 3.39 (3.18-3.61) |
| Residence area | |||||
| Seoul | 13 158 | 2376 | 18.2 | 1 [Reference] | 1 [Reference] |
| Other metropolitan | 12 929 | 2313 | 17.9 | 0.98 (0.93-1.04) | 1.00 (0.94-1.06) |
| Rural and small city | 22 585 | 4285 | 19.3 | 1.06 (1.01-1.11) | 1.08 (1.03-1.13) |
| Household income, % of national median | |||||
| ≤30.0 (low) | 8592 | 1585 | 18.7 | 1 [Reference] | 1 [Reference] |
| 30.1-69.9 (middle) | 18 350 | 3124 | 17.0 | 0.91 (0.85-0.96) | 1.01 (0.95-1.08) |
| ≥70.0 (high) | 21 730 | 4265 | 19.9 | 1.07 (1.01-1.13) | 1.09 (1.03-1.16) |
Abbreviations: CRS, chronic rhinosinusitis; CRSwNP, CRS with nasal polyps; CRSsNP, CRS without nasal polyps; HR, hazard ratio.
Table 3. Incidence per 1000 Person-Years and Hazard Ratios for Anxiety During an 11-Year Follow-up Period.
| Variables | No. of Participants | No. of Cases | Incidence per 1000 Person-Years | HR (95% CI) | |
|---|---|---|---|---|---|
| Unadjusted | Adjusted | ||||
| Group | |||||
| Comparison | 32 448 | 8587 | 27.8 | 1 [Reference] | 1 [Reference] |
| CRSsNP | 10 763 | 4165 | 43.7 | 1.60 (1.54-1.66) | 1.63 (1.57-1.69) |
| CRSwNP | 5461 | 1902 | 39.2 | 1.43(1.36-1.50) | 1.45 (1.38-1.52) |
| Sex | |||||
| Male | 20 039 | 4586 | 23.8 | 1 [Reference] | 1 [Reference] |
| Female | 28 633 | 10 068 | 38.8 | 1.65 (1.59-1.71) | 1.72 (1.66-1.78) |
| Age, y | |||||
| <45 | 29 931 | 6644 | 22.5 | 1 [Reference] | 1 [Reference] |
| 45-64 | 14 816 | 6131 | 47.8 | 2.19 (2.11-2.26) | 2.31 (2.23-2.39) |
| >64 | 3925 | 1879 | 64.5 | 3.06 (2.91-3.22) | 3.04 (2.88-3.20) |
| Residence area | |||||
| Seoul | 13 158 | 3681 | 29.6 | 1 [Reference] | 1 [Reference] |
| Other metropolitan | 12 929 | 3863 | 31.9 | 1.08 (1.03-1.13) | 1.10 (1.05-1.15) |
| Rural and small city | 22 585 | 7110 | 34.3 | 1.16 (1.12-1.21) | 1.20 (1.15-1.25) |
| Household income, % of national median | |||||
| ≤30.0 (low) | 8592 | 2669 | 33.6 | 1 [Reference] | 1 [Reference] |
| 30.1-69.9 (middle) | 18 350 | 5257 | 30.5 | 0.90 (0.86-0.95) | 1.00 (0.96-1.05) |
| ≥70.0 (high) | 21 730 | 6728 | 33.5 | 1.00 (0.95-1.04) | 1.04 (0.99-1.08) |
Abbreviations: CRS, chronic rhinosinusitis; CRSsNP, chronic rhinosinusitis without nasal polyps; CRSwNP, chronic rhinosinusitis with nasal polyps; HR, hazard ratio.
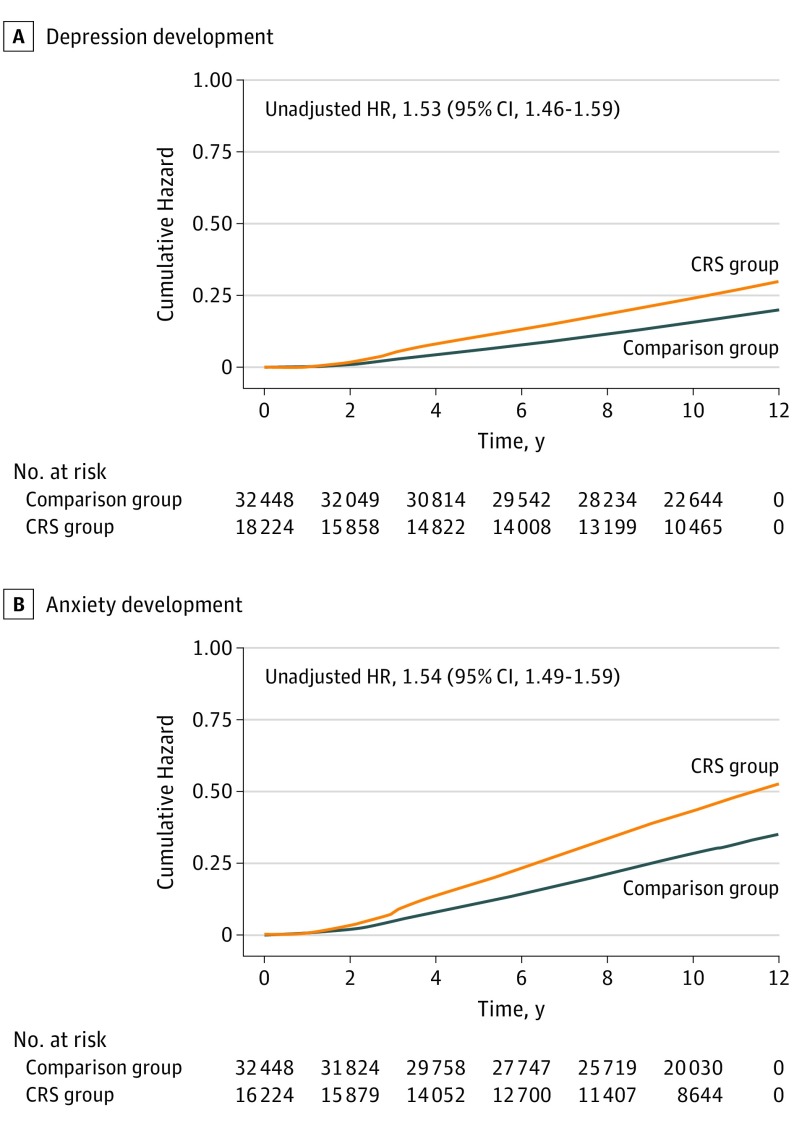
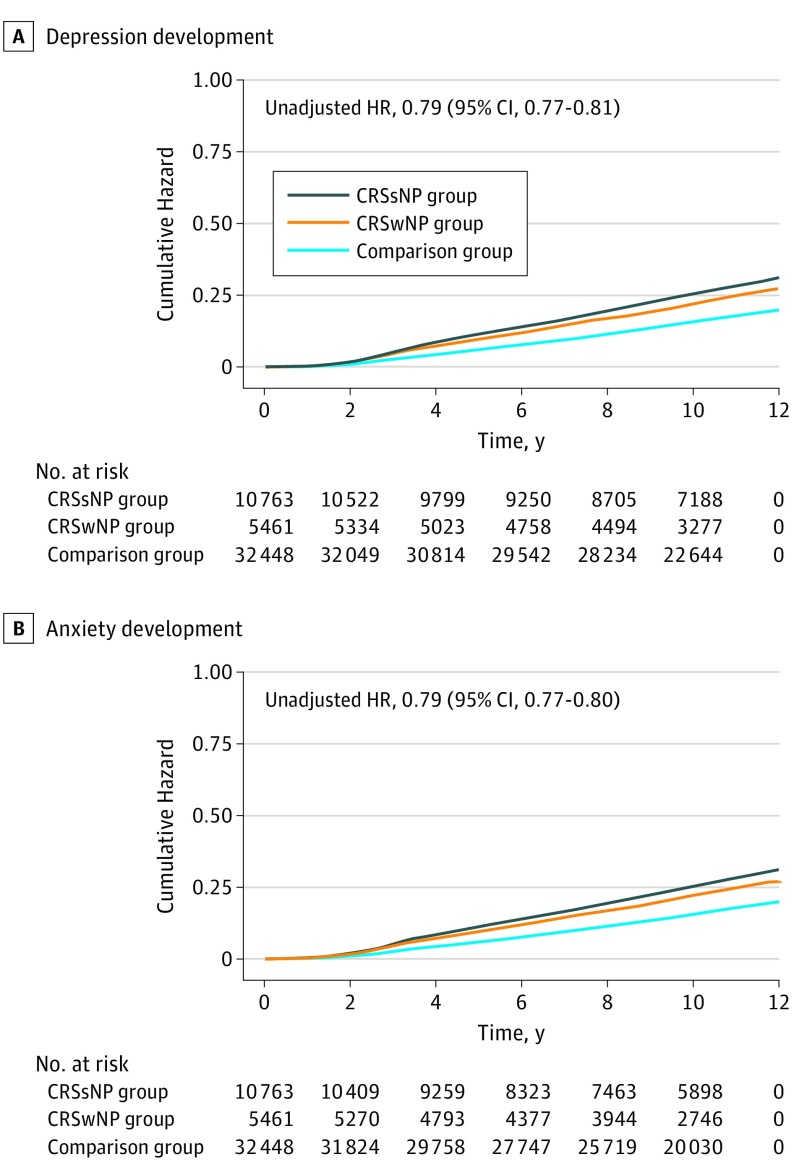
Figure 1 and Figure 2 present Kaplan-Meier survival curves with log-rank tests for the 11-year follow-up period. The results of the log-rank test indicated that patients with CRS developed depression (HR, 1.53; 95% CI, 1.46-1.59) and anxiety (HR, 1.54; 95% CI, 1.49-1.59) more frequently compared with those from the comparison group (Figure 1). Moreover, subgroup analysis revealed lower 11-year depression-free (HR, 0.79; 95% CI, 0.77-0.80) and anxiety-free (HR, 0.79; 95% CI, 0.77-0.81) survival rates in the CRSsNP group than in the CRSwNP group (Figure 2).
Figure 1. Survival Curves in Patients With and Without Chronic Rhinosinusitis (CRS).
Data are analyzed using Kaplan-Meier survival curve and log-rank test analysis. HR indicates hazard ratio.
Figure 2. Survival Curves in Patients With Chronic Rhinosinusitis (CRS) Phenotypes vs Comparison Patients Without CRS.
Data are analyzed using Kaplan-Meier survival curve and log-rank test analysis. CRSsNP indicates CRS without nasal polyps; CRSwNP, CRS with nasal polyps; HR, hazard ratio.
Discussion
In this study, we used nationwide population insurance data to conduct a retrospective cohort study to evaluate the risk of depression and anxiety in CRS depending on the CRS phenotype. We observed an association between CRS and an increased incidence of depression and anxiety. Specifically, CRSsNP was associated with a higher risk of developing depression and anxiety than was CRSwNP.
Chronic rhinosinusitis is one of the common rhinologic diseases and, despite receiving optimal medical and surgical treatment, some patients with CRS have repeated, persistent symptoms that make this condition challenging to manage. Specifically, patients with CRS combined with comorbid mental health problems usually show significantly worse pain and energy levels, as well as difficulty with daily activities, than do patients with CRS without mental health problems.16 Anxiety and depression are the 2 most common mental health disorders in patients with CRS.11,14,17 Previous studies9,14,15 also have demonstrated higher prevalence rates of depression and anxiety in patients with CRS. Thus, these psychiatric comorbidities may influence not only the diagnosis of CRS but also its therapeutic and surgical outcomes.18
Despite its clinical importance, the causal association between CRS and psychiatric comorbidities is not fully understood. For example, whether depression and anxiety amplify the symptoms of CRS or whether these conditions are the consequence of CRS is unknown. Recently, a cohort study using Taiwan National Health Insurance data19 demonstrated that CRS was associated with a significant increase in the risk of depression. The study reported that patients with CRS have a 1.51-fold higher risk of developing depression, but with no difference in the incidence of depression between CRSsNP and CRSwNP groups.19 However, no study, to our knowledge, has reported evaluating the risk of developing anxiety in CRS. Thus, to date this study is the first nationwide, population-based retrospective cohort study to evaluate the incidence of depression and anxiety in CRS, according to the different phenotypes of CRS.
To confirm the link between CRS and mental health problems, we used data from the KNHIS-NSC. Several previous studies using these data have also been published.20,21,22,23,24 In the present longitudinal study, we examined the association between CRS and mental health problems using sociodemographically matched individuals extracted from a nationwide 11-year longitudinal cohort database of 1 025 340 South Korean patients. Consistent with previous reports, we found that patients with CRS had a significantly higher risk of depression and anxiety, with HRs of 1.54 and 1.57, respectively, after adjusting for sociodemographic factors and comorbidities. We also found that patients with CRSsNP and CRSwNP had a significantly higher risk of developing depression and anxiety. However, adjusted HRs for depression and anxiety in patients with CRSsNP were higher than those in patients with CRSwNP. Thus, in this study, patients with CRSsNP appear to have a higher likelihood of developing mental health problems, such as depression and anxiety. Similarly, a previous cross-sectional study17 reported that emotional well-being was worse in patients with CRSsNP than in those with CRSwNP. Moreover, another study25 reported that facial pain and headache, which are known to be associated with depression and anxiety, were more common in patients with CRSsNP than in those with CRSwNP.A possible reason for this could be that patients with CRSwNP are more likely to visit the clinic sooner and begin treatment earlier because CRSwNP is frequently associated with asthma and allergic rhinitis. Another possible reason could be that patients with CRSwNP tend to visit the hospital continuously as they often undergo endoscopic sinus surgery. Therefore, prevention and treatment of complications are easier.
Strengths and Limitations
The present study has several unique strengths. First, it has a relatively long follow-up period (11 years) and uses a large national population-based database, which enables us to analyze all events associated with depression and anxiety effectively. Second, to improve diagnostic accuracy, we include only patients with CRS diagnosed by otolaryngologists and patients with anxiety or depression diagnosed by psychiatrists. Nasal endoscopy and psychiatric counseling therapy can only be performed by otolaryngologists and psychiatrists. Third, the present study is designed to evaluate the differences in the risk of developing depression and anxiety in patients with CRS, according to the precise phenotype. Chronic rhinosinusitis is a highly heterogeneous disease and is currently classified based on nasal endoscopic findings such as CRSwNP or CRSsNP.2 However, the clinical phenotype does not adequately reflect the pathophysiologic diversity of patients with CRS.26,27,28 Evidence from several studies suggests that CRSsNP is characterized by a predominant helper T 1 (TH1) inflammatory response, whereas CRSwNP is driven by TH2 inflammation and increased eosinophil infiltration.26,27,28 Thus, investigating the differences associated with the risk of development of mental diseases for each phenotype is important from the point of view of personalized medicine in this field. Our findings suggest that CRS increases the risk of depression and anxiety, regardless of phenotype. Nonetheless, CRSsNP is associated with a higher risk of depression and anxiety than is CRSwNP.
Our study also has some limitations. First, we do not have access to data regarding smoking, alcohol intake, and body mass index. Therefore, we cannot adjust for these potential confounding factors in the analysis. Second, the diagnosis of CRS depends on the KCD diagnostic codes, which might be less accurate than diagnoses based on information from a medical record that included the medical history, results of physical examination, or nasal endoscopy findings. Third, data regarding disease severity, such as computed tomographic images, are lacking in our registry. Fourth, the terms of depression and anxiety include a wide variety of disease states. Our diagnostic code system has errors that are too simplistic. Therefore, we cannot investigate whether patients with severe CRS are at a higher risk of depression and anxiety compared with patients with mild CRS. Finally, because this is a retrospective cohort study, we cannot directly examine and analyze the mechanisms underlying the association between CRS and depression or anxiety. Future clinical studies investigating a wider range of factors, diagnostic criteria, and disease severity can provide additional evidence for the link between CRS and depression or anxiety.
Conclusions
The present study investigated a possible link between CRS and the development of depression and anxiety during an 11-year follow-up period. Our findings suggest that patients with CRS had a higher risk of depression and anxiety, regardless of the CRS phenotype. In addition, depression and anxiety appeared to occur more frequently in patients without nasal polyps compared with those with nasal polyps. Therefore, this study provides new insight into the effects of CRS on mental health problems. Physicians should be aware of the potential comorbidities observed in patients with CRS and provide therapy to reduce the risk of depression and anxiety in these patients.
eTable 1. Diagnostic Codes Used in the Korean National Health Insurance Service (KNHIS)
eTable 2. Missing Data in the Retrospective Cohort Study
References
- 1.Anand VK. Epidemiology and economic impact of rhinosinusitis. Ann Otol Rhinol Laryngol Suppl. 2004;193:3-5. doi: 10.1177/00034894041130S502 [DOI] [PubMed] [Google Scholar]
- 2.Fokkens WJ, Lund VJ, Mullol J, et al. . EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012: a summary for otorhinolaryngologists. Rhinology. 2012;50(1):1-12. doi: 10.4193/Rhino50E2 [DOI] [PubMed] [Google Scholar]
- 3.Stevens WW, Lee RJ, Schleimer RP, Cohen NA. Chronic rhinosinusitis pathogenesis. J Allergy Clin Immunol. 2015;136(6):1442-1453. doi: 10.1016/j.jaci.2015.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kato A. Immunopathology of chronic rhinosinusitis. Allergol Int. 2015;64(2):121-130. doi: 10.1016/j.alit.2014.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caulley L, Thavorn K, Rudmik L, Cameron C, Kilty SJ. Direct costs of adult chronic rhinosinusitis by using 4 methods of estimation: results of the US Medical Expenditure Panel Survey. J Allergy Clin Immunol. 2015;136(6):1517-1522. doi: 10.1016/j.jaci.2015.08.037 [DOI] [PubMed] [Google Scholar]
- 6.Halawi AM, Smith SS, Chandra RK. Chronic rhinosinusitis: epidemiology and cost. Allergy Asthma Proc. 2013;34(4):328-334. doi: 10.2500/aap.2013.34.3675 [DOI] [PubMed] [Google Scholar]
- 7.Bhattacharyya N. Contemporary assessment of the disease burden of sinusitis. Am J Rhinol Allergy. 2009;23(4):392-395. doi: 10.2500/ajra.2009.23.3355a [DOI] [PubMed] [Google Scholar]
- 8.Litvack JR, Mace J, Smith TL. Role of depression in outcomes of endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2011;144(3):446-451. doi: 10.1177/0194599810391625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis GE, Yueh B, Walker E, Katon W, Koepsell TD, Weymuller EA. Psychiatric distress amplifies symptoms after surgery for chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2005;132(2):189-196. doi: 10.1016/j.otohns.2004.09.135 [DOI] [PubMed] [Google Scholar]
- 10.Mace J, Michael YL, Carlson NE, Litvack JR, Smith TL. Effects of depression on quality of life improvement after endoscopic sinus surgery. Laryngoscope. 2008;118(3):528-534. doi: 10.1097/MLG.0b013e31815d74bb [DOI] [PubMed] [Google Scholar]
- 11.Tomoum MO, Klattcromwell C, DelSignore A, Ebert C, Senior BA. Depression and anxiety in chronic rhinosinusitis. Int Forum Allergy Rhinol. 2015;5(8):674-681. doi: 10.1002/alr.21528 [DOI] [PubMed] [Google Scholar]
- 12.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317-325. doi: 10.7326/0003-4819-146-5-200703060-00004 [DOI] [PubMed] [Google Scholar]
- 13.Baijens LW, Verdonschot R, Vanbelle S, et al. . Medically unexplained otorhinolaryngological symptoms: towards integrated psychiatric care. Laryngoscope. 2015;125(7):1583-1587. doi: 10.1002/lary.25082 [DOI] [PubMed] [Google Scholar]
- 14.Nanayakkara JP, Igwe C, Roberts D, Hopkins C. The impact of mental health on chronic rhinosinusitis symptom scores. Eur Arch Otorhinolaryngol. 2013;270(4):1361-1364. doi: 10.1007/s00405-012-2230-1 [DOI] [PubMed] [Google Scholar]
- 15.Wasan A, Fernandez E, Jamison RN, Bhattacharyya N. Association of anxiety and depression with reported disease severity in patients undergoing evaluation for chronic rhinosinusitis. Ann Otol Rhinol Laryngol. 2007;116(7):491-497. doi: 10.1177/000348940711600703 [DOI] [PubMed] [Google Scholar]
- 16.Brandsted R, Sindwani R. Impact of depression on disease-specific symptoms and quality of life in patients with chronic rhinosinusitis. Am J Rhinol. 2007;21(1):50-54. doi: 10.2500/ajr.2007.21.2987 [DOI] [PubMed] [Google Scholar]
- 17.Erskine SE, Hopkins C, Clark A, et al. . Chronic rhinosinusitis and mood disturbance. Rhinology. 2017;55(2):113-119. doi: 10.4193/Rhin16.111 [DOI] [PubMed] [Google Scholar]
- 18.Bhattacharyya N. Radiographic stage fails to predict symptom outcomes after endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2006;116(1):18-22. doi: 10.1097/01.mlg.0000192284.22703.04 [DOI] [PubMed] [Google Scholar]
- 19.Hsu CL, Wang TC, Shen TC, Huang YJ, Lin CL, Sung FC. Risk of depression in patients with chronic rhinosinusitis: a nationwide population-based retrospective cohort study. J Affect Disord. 2016;206:294-299. doi: 10.1016/j.jad.2016.09.001 [DOI] [PubMed] [Google Scholar]
- 20.Kim JY, Lee JW, Kim M, Kim MJ, Kim DK. Association of idiopathic sudden sensorineural hearing loss with affective disorders. JAMA Otolaryngol Head Neck Surg. 2018;144(7):614-621. doi: 10.1001/jamaoto.2018.0658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim JY, Hong JY, Kim DK. Association of sudden sensorineural hearing loss with risk of cardiocerebrovascular disease: a study using data from the Korea National Health Insurance Service. JAMA Otolaryngol Head Neck Surg. 2018;144(2):129-135. doi: 10.1001/jamaoto.2017.2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park SJ, Choi NK, Yang BR, Park KH, Woo SJ. Risk of stroke in retinal vein occlusion. Neurology. 2015;85(18):1578-1584. doi: 10.1212/WNL.0000000000002085 [DOI] [PubMed] [Google Scholar]
- 23.Shin JY, Roughead EE, Park BJ, Pratt NL. Cardiovascular safety of methylphenidate among children and young people with attention-deficit/hyperactivity disorder (ADHD): nationwide self controlled case series study. BMJ. 2016;353:i2550. doi: 10.1136/bmj.i2550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim SH, Jeong HY, Yang DH, Kim J, Lee SY. Beneficial effect of statins in patients receiving chronic hemodialysis following percutaneous coronary intervention: a nationwide retrospective cohort study. Sci Rep. 2018;8(1):9692. doi: 10.1038/s41598-018-27941-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Durr DG, Desrosiers MY, Dassa C. Impact of rhinosinusitis in health care delivery: the Quebec experience. J Otolaryngol. 2001;30(2):93-97. doi: 10.2310/7070.2001.20813 [DOI] [PubMed] [Google Scholar]
- 26.Van Zele T, Claeys S, Gevaert P, et al. . Differentiation of chronic sinus diseases by measurement of inflammatory mediators. Allergy. 2006;61(11):1280-1289. doi: 10.1111/j.1398-9995.2006.01225.x [DOI] [PubMed] [Google Scholar]
- 27.Polzehl D, Moeller P, Riechelmann H, Perner S. Distinct features of chronic rhinosinusitis with and without nasal polyps. Allergy. 2006;61(11):1275-1279. doi: 10.1111/j.1398-9995.2006.01132.x [DOI] [PubMed] [Google Scholar]
- 28.Van Bruaene N, Pérez-Novo CA, Basinski TM, et al. . T-cell regulation in chronic paranasal sinus disease. J Allergy Clin Immunol. 2008;121(6):1435-1441, 1441.e1-1441.e3. doi: 10.1016/j.jaci.2008.02.018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Diagnostic Codes Used in the Korean National Health Insurance Service (KNHIS)
eTable 2. Missing Data in the Retrospective Cohort Study