Abstract
Background
High altitude illness (HAI) is a term used to describe a group of cerebral and pulmonary syndromes that can occur during travel to elevations above 2500 metres ( ˜ 8200 feet ). Acute hypoxia, acute mountain sickness (AMS), high altitude cerebral oedema (HACE) and high altitude pulmonary oedema (HAPE) are reported as potential medical problems associated with high altitude. In this review, the first in a series of three about preventive strategies for HAI, we assess the effectiveness of six of the most recommended classes of pharmacological interventions.
Objectives
To assess the clinical effectiveness and adverse events of commonly‐used pharmacological interventions for preventing acute HAI.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (OVID), Embase (OVID), LILACS and trial registries in January 2017. We adapted the MEDLINE strategy for searching the other databases. We used a combination of thesaurus‐based and free‐text terms to search.
Selection criteria
We included randomized‐controlled and cross‐over trials conducted in any setting where commonly‐used classes of drugs were used to prevent acute HAI.
Data collection and analysis
We used standard methodological procedures as expected by Cochrane.
Main results
We included 64 studies (78 references) and 4547 participants in this review, and classified 12 additional studies as ongoing. A further 12 studies await classification, as we were unable to obtain the full texts. Most of the studies were conducted in high altitude mountain areas, while the rest used low pressure (hypobaric) chambers to simulate altitude exposure. Twenty‐four trials provided the intervention between three and five days prior to the ascent, and 23 trials, between one and two days beforehand. Most of the included studies reached a final altitude of between 4001 and 5000 metres above sea level. Risks of bias were unclear for several domains, and a considerable number of studies did not report adverse events of the evaluated interventions. We found 26 comparisons, 15 of them comparing commonly‐used drugs versus placebo. We report results for the three most important comparisons:
Acetazolamide versus placebo (28 parallel studies; 2345 participants)
The risk of AMS was reduced with acetazolamide (risk ratio (RR) 0.47, 95% confidence interval (CI) 0.39 to 0.56; I2 = 0%; 16 studies; 2301 participants; moderate quality of evidence). No events of HAPE were reported and only one event of HACE (RR 0.32, 95% CI 0.01 to 7.48; 6 parallel studies; 1126 participants; moderate quality of evidence). Few studies reported side effects for this comparison, and they showed an increase in the risk of paraesthesia with the intake of acetazolamide (RR 5.53, 95% CI 2.81 to 10.88, I2 = 60%; 5 studies, 789 participants; low quality of evidence).
Budenoside versus placebo (2 parallel studies; 132 participants)
Data on budenoside showed a reduction in the incidence of AMS compared with placebo (RR 0.37, 95% CI 0.23 to 0.61; I2 = 0%; 2 studies, 132 participants; low quality of evidence). Studies included did not report events of HAPE or HACE, and they did not find side effects (low quality of evidence).
Dexamethasone versus placebo (7 parallel studies; 205 participants)
For dexamethasone, the data did not show benefits at any dosage (RR 0.60, 95% CI 0.36 to 1.00; I2 = 39%; 4 trials, 176 participants; low quality of evidence). Included studies did not report events of HAPE or HACE, and we rated the evidence about adverse events as of very low quality.
Authors' conclusions
Our assessment of the most commonly‐used pharmacological interventions suggests that acetazolamide is an effective pharmacological agent to prevent acute HAI in dosages of 250 to 750 mg/day. This information is based on evidence of moderate quality. Acetazolamide is associated with an increased risk of paraesthesia, although there are few reports about other adverse events from the available evidence. The clinical benefits and harms of other pharmacological interventions such as ibuprofen, budenoside and dexamethasone are unclear. Large multicentre studies are needed for most of the pharmacological agents evaluated in this review, to evaluate their effectiveness and safety.
Plain language summary
Drugs commonly‐used for preventing high altitude illness
Background
High altitude illness (HAI) is a term used to describe a group of brain and breathing conditions that can occur while travelling to altitudes above 2500 metres ( ˜ 8200 feet ). HAI is generally characterized by headache, nausea, vomiting and tiredness (often called acute mountain sickness), but may affect the brain or the lungs in different individuals. In this review, we assessed the most commonly‐used drugs to prevent the onset of this illness.
Study characteristics
The evidence is current to January 2017. We included 64 studies related to six different types of drugs recommended for HAI prevention. Most of the studies were conducted in high altitude mountain areas, while the rest used low pressure (hypobaric) chambers to simulate altitude exposure. The participants' ages ranged between 16 and 65 years. Eleven studies included people at a high risk of this condition due to their history of HAI or other illnesses such as asthma. Twenty‐four trials provided the intervention between three and five days prior to the ascent, and 23 trials, between one and two days beforehand. Most of the included studies reached a final altitude of between 4001 and 5000 metres above sea level. In 23 of the included studies, the source of funding was unclear. Only 18 studies declared their possible conflicts of interests. We classed 24 more studies as still ongoing or waiting for assessment.
Key results
Our findings suggest that acetazolamide is an effective treatment for the prevention of acute HAI in dosages of 250 to 750 mg/day, when this drug is compared to a placebo (i.e. a pill with no active agent). Most of the available information relates to the prevention of uncomplicated HAI (headache, nausea, vomiting and tiredness) rather than to more serious brain or lung problems. We also found that acetazolamide is associated with an increased risk of paraesthesia in the fingers (i.e. a sensation of tingling, tickling, pricking, or burning of the skin), although this outcome is not well reported in the available evidence. The benefits and harms of other drugs such as ibuprofen, budenoside and dexamethasone are unclear, due to the small number of studies.
Quality of the evidence
We rated the quality of the evidence as moderate to very low. Several studies had quality shortcomings, including their use of small numbers of participants and a lack of reporting of important outcomes such as side effects. For most of the drugs covered by the studies, additional research is required to clarify their effectiveness and safety.
Summary of findings
Background
High altitude illness (HAI) is a term used to describe a group of cerebral and pulmonary syndromes that can occur during travel to elevations above 2500 metres ( ˜ 8200 feet). HAI is arbitrarily classified as high (1500 to 3500 metres ), very high (3500 to 5500 metres or ) and extreme (above 5500 metres ) (Paralikar 2010). Because of the large number of people who ascend rapidly to between 2500 and 3500 m , high altitude illness is common in this height range (Paralikar 2010). Although the proportion of oxygen remains unchanged at 20.93%, increases in altitude result in a lower partial pressure of oxygen in the inspired air (Anonymous 1892; Wilson 2009). This reduction in the driving pressure of oxygen, along the oxygen cascade from the lungs to the tissues, can compromise the supply of oxygen to the tissues (Wilson 2009), especially the cardiovascular and pulmonary systems (Leissner 2009). The physiological responses to hypoxia and acclimatization related to HAI include hyperventilation (increased depth and rate of breathing), elevation of systemic blood pressure and tachycardia (elevations of heart rate) (Leissner 2009; Naeije 2010). However, in many instances these physiologic changes may be inadequate, such that the sojourn to altitude and the concomitant hypoxia are complicated by altitude‐associated medical illness (Palmer 2010), which is also known as high altitude illness.
Description of the condition
High altitude illness (HAI)
There are two types of mountain sicknesses: acute mountain sickness (AMS) and chronic mountain sickness (CMS), also called Monge's disease (Monge 1942). Acute hypoxia, acute mountain sickness, high altitude cerebral oedema (HACE), high altitude pulmonary oedema (HAPE), cerebrovascular syndromes, peripheral oedema, retinopathy, thromboembolism, sleep disorders and periodic breathing, high altitude pharyngitis and bronchitis, ultraviolet exposure and keratitis (snow blindness), and exacerbation of pre‐existing illness are reported as medical problems potentially associated with high altitude ascent (CATMAT 2007; Palmer 2010; Schoene 2008). Factors such as the rate of ascent, the absolute change in altitude, and individual physiology are the primary determinants of whether HAI will develop or not (Leissner 2009; Palmer 2010). The risk categories for acute mountain sickness are shown in Appendix 1 (Luks 2010).
In the 19th century, Dr Daniel Vergara, a Mexican physiologist, pioneered the studies on high altitude physiology and the physiological and anatomical mechanisms of adaptation to high elevations. Forty years later, Dr Carlos Monge, a Peruvian physiologist, reported his ideas on this issue. The work of these pioneers was summarized early this century (Rodríguez de Romo 2002). Both the physiology and pathophysiology of high altitude have recently been widely reviewed (Bärtsch 2007; Leissner 2009; Palmer 2010; Paralikar 2010). In brief, these reviews confirm both the increase in respiratory rate and increase in haemoglobin concentration on exposure to a low oxygen pressure, and that such changes are often inadequate. They identify the rate of ascent, the absolute change in altitude and individual variation in physiology as the primary determinants of whether HAI will develop or not (Palmer 2010). HAI is considered an important cause of mountain mortality (Windsor 2009).
Acute mountain sickness (AMS) or high altitude cerebral oedema (HACE)
AMS is a multisystem disorder with prominent neurological features characterized by headache, anorexia, nausea and sometimes vomiting, light‐headedness, insomnia, and fatigue (Bailey 2009a; Leissner 2009; Palmer 2010). Headache is the most prevalent symptom of acute mountain sickness. In contrast, HACE is a potentially fatal neurologic disorder and it is characterized by altered consciousness or ataxia (Bailey 2009a; Hackett 2004; Imray 2010), or both, in an individual with AMS or high altitude pulmonary oedema (HAPE). If left untreated, HACE can result in death due to cerebral oedema (Bailey 2009a). HACE is widely viewed as the end stage of AMS and is normally preceded by symptoms of AMS (Basnyat 2003), which suggest a similar pathophysiologic process (Bailey 2009a; Imray 2010; Palmer 2010). Both syndromes share a common pathophysiology linked by intracranial hypertension (Bailey 2009a; Kallenberg 2007; Schoonman 2008; Wilson 2009). The severity of AMS can be scored using the Lake Louise Questionnaire, Environmental Symptoms Questionnaire, or by the use of a simple analogue scale (Imray 2010). Headache is a very common symptom at altitude and some authors have suggested it could be viewed as a distinct clinical entity.
The definition of AMS seems to be problematic, as it will vary greatly between studies. A Lake Louise Score higher than two (including headache) is not equivalent to a criterion score of 0.70 with AMS‐C (cerebral) from the Environmental Symptoms Questionnaire (Maggiorini 1998). It has been suggested that a previous review came to an erroneous conclusion because they included a study which used the AMS‐R (respiratory) score for diagnosis of AMS. The value of the AMS‐R score is questionable for diagnosing AMS (Dumont 2000). Pathophysiology with a focus on the molecular basis of AMS and HACE has been widely described by Bailey 2009a, and advances in the genetics, molecular mechanisms, and physiology that underpin them have been extensively described by Wilson 2009.
This review treats headache as a common and early symptom of AMS. Indeed, the exact definition of what constitutes AMS will vary when using different scoring systems and when interpreted by different authors. In this review we have taken care not to pool data inappropriately where the scoring systems used cannot be directly compared.
High altitude pulmonary oedema (HAPE)
HAPE is a non‐cardiogenic pulmonary oedema (Luks 2008a; Schoene 2004; Stream 2008). It is characterized by cough, progressive dyspnoea with exertion, and decreased exercise tolerance, generally developing within two to four days after arrival at high altitude (Palmer 2010; Stream 2008). It is rare after one week of acclimatization at a particular altitude (Maggiorini 2010; Palmer 2010). Hypoxia is the trigger that results in a complex cascade of events leading to HAPE (Stream 2008). Essentially, HAPE is due to a "persistent imbalance between the forces that drive water into the airspace and the biologic mechanisms for its removal" (Scherrer 2010), with the hallmark of this condition being hypoxic pulmonary hypertension. The hypertension may be mediated by at least four mechanisms: defective pulmonary nitric oxide synthesis, exaggerated endothelin‐1 synthesis, exaggerated sympathetic activation, and a defect in alveolar transepithelial sodium transport (Scherrer 2010). An extensive review of pulmonary hypertension induced by HAI is reported by Pasha 2010.
Epidemiology of acute HAI
It has been estimated that 84% of people who fly directly to 3860 m are affected by AMS (Basnyat 2003). The incidence of HACE and HAPE is much lower than for AMS, with estimates in the range of 0.1% to 4.0% (Basnyat 2003). The rate of ascent, altitude reached (especially the sleeping altitude), and individual susceptibility are the most important risk factors for the development of HAI (Basnyat 2003; Schneider 2002). Other risk factors are a history of HAI and permanent residence lower than 900 metres, exertion in children and adults (Basnyat 2003), obesity (Ri‐Li 2003), and coronary heart disease (Dehnert 2010). It is advisable that those with asthma be sure that their condition is well controlled before they undertake exertion at altitude (CATMAT 2007).
See Appendix 2 for other medical terms.
Description of the intervention
The risk of high altitude illness (HAI) begins with a non‐acclimatized person ascending to an altitude higher than 2500 metres (Paralikar 2010). However, a susceptible individual may develop AMS at an intermediate altitude such as 2000 metres (Montgomery 1989). Several interventions to prevent HAI have been described, compiled, and published in guidelines and consensus statements (CATMAT 2007; Luks 2010). Interventions for HAI prevention can be classified as pharmacological and non‐pharmacological (Bärtsch 1992; Luks 2010; Luks 2008b; Wright 2008). The Committee to Advise on Tropical Medicine and Travel proposed a consensus for HAI in 2007, describing prevention and treatment approaches among several topics regarding this medical condition (CATMAT 2007).
In 2014, the Wilderness Medical Society (WMS) published an update of their 2010 guidelines (Luks 2010), detailing prevention and treatment directives for HAI (AMS, HACE, HAPE). This guideline was developed by an expert panel that compiled and classified all available evidence on HAI prevention and treatment. Recommendations based on evidence, using American College of Chest Physicians strategies, were agreed upon. For AMS and HACE, the experts proposed a risk classification where low‐risk people are discarded for prevention interventions. For HAPE, pharmacological prophylaxis is recommended for those with a previous diagnosis of HAI (Luks 2014). However, the document does not include all of the most frequent and broadly‐described pharmacological interventions for prevention and treatment of HAI. The most commonly suggested interventions are summarized below.
Carbonic anhydrase inhibitors: acetazolamide and methazolamide (Bernhard 1998; Carlsten 2004; Hussain 2004; Swenson 2007; Van Patot 2008; Wright 1983; Wright 2008).
Steroids: budenoside, prednisolone and dexamethasone (Basu 2002a; Basu 2002b;Ellsworth 1991; Hackett 1988; Johnson 1984; Rock 1989a).
Bronchodilator drugs: Include salmeterol, theophyline and montelukast (Sartori 2002; Kleinsasser 2002; Wright 2008).
Selective inhibitor of phosphodiesterase type 5 (PDE5): taladafil (Maggiorini 2006) and sildenafil (Bates 2007; Kleinsasser 2002; Richalet 2005).
Calcium modulators: Include nifedipine and flunarizine (Bartsch 1991; Hohenhaus 1994).
Non‐steroidal anti‐inflammatory drugs (NSAIDs) and other analgesic: aspirin, carbasalate and ibuprofen (Burtscher 1998; Burtscher 2001).
How the intervention might work
Extensive reviews of the pharmacotherapy of HAI have recently been published (Maggiorini 2010; Wright 2008). Below is a list and brief description of the common agents that have so far been suggested. Appendix 3 provides more detail, and discusses the potential adverse effects of each agent.
Carbonic anhydrase (CA) inhibitors (acetazolamide and methazolamide) generate inhibition of CA in the kidneys, resulting in increased bicarbonate excretion in the urine and metabolic acidoses. The result is an offsetting of hyperventilation‐induced respiratory alkalosis, allowing chemoreceptors to respond more fully to hypoxic stimuli at altitude (Leaf 2007). Acetazolamide can also cause pulmonary vasodilation unrelated to carbonic anhydrase inhibition (Höhne 2007; Swenson 2006).
Steroids (dexamethasone, budesonide and prednisolone): Hypoxia‐induced vasogenic oedema has been suggested as one of the major mechanisms responsible for development of AMS (Hackett 1999). Glucocorticoids blocks hypoxia‐induced endothelial dysfunction (Murata 2004; Murata 2005).
Bronchodilators (salmeterol, theophylline or aminophylline, montelukast). The human beta‐2 adrenergic receptor (B2AR) has been found to play a very important role in the pathogenesis of HAPE, and salmeterol was found to have a high binding affinity with human B2AR (Chandramoorthi 2008). Furthermore, salmeterol enhances alveolar clearance by stimulating amiloride‐sensitive sodium (Na) channels (Maggiorini 2010). Non‐selective phosphodiesterase inhibitor (theophylline or aminophylline): anti‐hypoxia and antioxidation effects of aminophylline (Yang 2007) could be responsible for reducing periodic breathing, cerebral and pulmonary microvascular permeability, and pulmonary artery pressure (Wright 2008). Montelukast is a leukotriene receptor antagonist (LTRA) that reduces the bronchoconstriction (Tintinger 2010).
Selective inhibitors of phosphodiesterase type 5 (taladafil and sildenafil) induce overproduction of nitric oxide, which attenuates pulmonary vasoconstriction during acute hypoxia (Ozaki 2001; Zhao 2001). It causes a reduction in pulmonary hypertension.
Calcium channel blockers (CCBs): calcium channel antagonists or calcium antagonists (nifedipine, flunarizine) are a group of medications that disrupt the movement of calcium (Ca2+) through calcium channels and reduce pulmonary vascular resistance (Hackett 1992), leading to a reduction of the pulmonary hypertension.
Non‐steroidal anti‐inflammatory drugs (NSAIDs) and other analgesics (aspirin, ibuprofen, carbasalate): it is postulated that prostaglandin‐mediated increases in cerebral microvascular permeability may contribute to the pathophysiology of AMS, and treatment with prostaglandin synthesis inhibitors could reduce this response (CATMAT 2007).
See Appendix 3 for adverse events of the pharmacological interventions.
Why it is important to do this review
It is important to conduct this systematic review for many reasons. First, many people all over the world travel to recreational areas located at high altitudes, putting themselves at increased risk of developing acute HAI. HAI may be severe and life‐threatening, so effective prevention is likely to be of great value both to these visitors to high‐altitude areas, and to those responsible for their treatment and rescue when required. At the other end of the spectrum, reliable prevention of minor degrees of AMS would greatly enhance the experience of many travellers. Travel to high altitudes may also aggravate underlying illnesses, particularly cardiopulmonary diseases (CATMAT 2007). Second, the true role of the many approaches for preventing acute HAI is uncertain (Adams 2004; Bärtsch 2004; CATMAT 2007; Elphick 2004), meaning that their clinical effectiveness and safety must be assessed. Third, it is necessary to answer questions such as: Are all of these interventions equally useful regardless of the type of HAI? and Is there a reason to believe that some forms are more appropriate for some persons at risk than others?. Four, an updated meta‐analysis on AMS prevention needs to be produced (Dumont 2000).
A systematic review, including a rigorous assessment of the risks of bias, of the most up‐to‐date evidence, will help clinicians make informed decisions about the use of non‐pharmacological and pharmacological interventions for preventing acute HAI. The protocol for this review included all agents to prevent high altitude illness (Martí‐Carvajal 2012), but we have decided to split the review into a series of three publications about the prevention of this condition (Part 1: Commonly‐used drugs. Part 2: Less commonly‐used drugs. Part 3: Miscellaneous and non‐pharmacological interventions). This review includes six groups of the most highly recommended agents to prevent acute HAI.
Objectives
To assess the clinical effectiveness and adverse events of commonly‐used interventions for preventing acute HAI.
Methods
Criteria for considering studies for this review
Types of studies
We include randomized controlled trials (RCTs) irrespective of publication status (trials may be unpublished or published as articles, abstracts, or letters), language (no language limitation) or country. We applied no restrictions by length of follow‐up. We also included cross‐over trials (See Differences between protocol and review and section).
We excluded quasi‐randomized studies and prospective observational studies for evaluating clinical effectiveness.
Types of participants
We include trials involving participants who are at risk of developing high altitude illness (AMS or HACE, HAPE). We include participants with and without a history of high altitude illness. We applied no age or gender restrictions.
Types of interventions
The published protocol for this review included all agents to prevent high altitude illness (Martí‐Carvajal 2012). However we decided to split the topic into a series of three publications about the prevention of this condition (See Differences between protocol and review section). This is the first of the three and includes the following six groups of the most widely recommended agents to prevent acute HAI:
Carbonic anhydrase inhibitors: Including acetazolamide and methazolamide.
Steroids: Including budenoside, prednisolone and dexamethasone.
Bronchodilator drugs: Including salmeterol, theophyline and montelukast.
Selective inhibitor of phosphodiesterase type 5 (PDE5): Including taladafil and sildenafil.
Calcium channel modulators: Including nifedipine and flunarizine.
Non‐steroidal anti‐inflammatory drugs (NSAIDs) and other analgesics: Including aspirin, carbasalate and ibuprofen.
We include trials where the relevant medication was administered before beginning the ascent. We exclude trials using these drugs during or after the ascent.
Types of outcome measures
We modified the following outcome measures from the published protocol (Martí‐Carvajal 2012). This is a departure from the protocol and it is explained in the Differences between protocol and review section.
Primary outcomes
Incidence of acute mountain sickness (AMS ‐ as defined by each study) at any time.
Secondary outcomes
Incidence of high altitude pulmonary oedema (HAPE ‐ as defined by each study) at any time.
Incidence of high altitude cerebral oedema (HACE ‐ as defined by each study), at any time.
Incidence of adverse events in general, including paraesthesia, at any time.
Differences in HAI/AMS scores at high altitude. We analysed the differences between groups by any measure of AMS severity and between 0 and 48 hours at high altitude.
Search methods for identification of studies
We used the same search methods for the identification of studies, which are common to the three reviews included in this series.
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, January 2017); MEDLINE (OVID, 1966 to January 2017); Embase (OVID, 1980 to January 2017); LILACS (1982 to January 2017). We used the specific search terms listed below in combination with the Cochrane highly sensitive search strategy for identifying randomized controlled trials (RCTs) in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Appendix 4 to Appendix 7 show the search strategies used in this set of reviews. We undertook the most recent search in January 2017.
Searching other resources
We also searched trials registries through the World Health Organization International Clinical Trials Registry Platform Search Portal (ICTRP) (see Appendix 8). We looked through the reference lists of the retrieved publications and review articles. We undertook the most recent search in January 2017.
Data collection and analysis
Data collection and analysis methods were common to the three reviews included in this series.
Selection of studies
Two review authors independently assessed each reference identified by the search against the inclusion criteria. We resolved any disagreements by discussion, and by consultation with a third review author as an arbiter if we could not reach agreement. We retrieved in full those references which appeared to meet the inclusion criteria for further independent assessment by the same three review authors.
Data extraction and management
We used a predefined form to extract the following data: eligibility criteria, demographics (age, gender, country), rate of ascent (metres/hour), final altitude reached (metres), AMS scale, design study, history of HAI, type of HAI, proposed intervention, and main outcomes, among others. See Appendix 9 for details of the data extraction form. For eligible studies, two review authors extracted the data using the selected form. We resolved discrepancies through discussion or, if required, we involved a third review author. We entered data into Review Manager 5 software and checked them for accuracy.
Assessment of risk of bias in included studies
Three review authors independently assessed risks of bias for each study, using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreement by discussion. We judged the methodological quality of each study using Cochrane’s process for assessing risk of bias, a two‐part tool that addresses the six specific domains: random sequence generation; allocation concealment; blinding of participants, personnel, and outcome assessors; incomplete outcome data; selective reporting; and other potential biases (Higgins 2011). The first part describes the risk of bias; the second part provides criteria for making judgements about the risk of bias from each of the six domains (Appendix 9). Based on this process we implemented a 'Risk of bias' worksheet to be filled out for each study. Two review authors independently assessed the risks of bias, resolving any disagreement through consultation with an additional review author. We display the results by creating a 'Risk of bias' graph and a 'Risk of bias' summary figure using RevMan 5.3 software, if appropriate. We present the risks of bias in the Results section. We also provided summary assessments of the risks of bias for each outcome within and across studies.
Measures of treatment effect
For dichotomous outcomes (such as incidence of AMS or HAPE), we show results as summary risk ratios (RRs) with 95% confidence intervals (CIs). For continuous outcomes (such as differences in AMS scores), we present the results as summary mean differences (MDs) or standardized mean differences (SMDs) as appropriate, with a 95% CI. Because we identified a considerable number of cross‐over trials, we have included these studies separately and analysed this information using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions‐ Chapter 16.4 (Elbourne 2002; Higgins 2011; Stedman 2011), specifically related to estimation of the Mantel‐Haenzel odds ratio (OR) for paired outcomes.
Unit of analysis issues
The published protocol did not include consideration of any unit of analysis issues. However, our searches identified 12 cross‐over studies and we included them in the analyses, but separately from the parallel studies. In brief, we used the methods recommended by Elbourne (Elbourne 2002; Stedman 2011). This is a departure from the protocol (Martí‐Carvajal 2012) and is explained in the Differences between protocol and review section.
Dealing with missing data
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat (ITT) basis (i.e. we attempted to include all randomized participants in the denominator of the assessed groups in the analyses). Due to the fact that we included studies with missing information (especially standard deviations) or data not suitable for planned analyses, we followed the methods recommended by the Cochrane Handbook for Systematic Reviews of Interventions‐ Chapter 16.1.3. (Higgins 2011). In brief, we transformed median values and their interquartile ranges or range extracted from included studies to means and standard deviations according to Wan and colleagues (Hozo 2005; Wan 2014). This is a departure from the protocol (Martí‐Carvajal 2012) and it is explained in the Differences between protocol and review section.
Assessment of heterogeneity
We used the I2 statistic to measure statistical heterogeneity among the trials in each analysis. When we identified substantial heterogeneity, we explored it by prespecified subgroup analysis. The I2 statistic describes the percentage of total variation across trials due to heterogeneity rather than sampling error (Higgins 2003). We considered a value for I2 greater than 50% (Higgins 2011) to be statistically significant. We assessed the clinical and methodological diversity of the included studies in a comparison for sufficient homogeneity before choosing to estimate summary effect sizes.
Assessment of reporting biases
We assessed whether the review was subject to publication bias by using a funnel plot to graphically illustrate variability between trials. If we detected asymmetry, we planned to explore causes other than publication bias. We produced a funnel plot if we could include 10 or more RCTs in a comparison.
Data synthesis
We summarized the findings using the random‐effects model (DerSimonian 1986). We carried out statistical analyses using Review Manager 5 (RevMan 5.3). We interpreted differences as important where the 95% confidence interval did not cross the value of no difference between groups. We also applied trial sequential analysis, as cumulative meta‐analyses are at risk of producing random errors due to sparse data and repetitive testing of the accumulating data (Brok 2009; Wetterslev 2008). To minimize random errors, we calculated the required information size (i.e. the number of participants needed in a meta‐analysis to detect or reject a certain intervention effect) (Wetterslev 2008). The required information size calculation also accounted for the heterogeneity or diversity present in the meta‐analysis (Wetterslev 2008). In our meta‐analysis, we based the diversity‐adjusted required information size on the event proportion in the control group; assumption of a plausible risk ratio reduction (RRR) of 20% on the RR reduction observed in the included trials with low risk of bias; a risk of type I error of 5%; a risk of type II error of 20%; and the assumed diversity of the meta‐analysis. We added the trials according to the year of publication, and if more than one trial had been published in a year, we added trials alphabetically according to the last name of the first trial author. On the basis of the required information size, we constructed trial sequential monitoring boundaries (Lan 1983; Thorlund 2009; Wetterslev 2008). These boundaries determine the statistical inference one may draw regarding the cumulative meta‐analysis that has not reached the required information size; if the trial sequential monitoring boundary is crossed before the required information size is reached, firm evidence may perhaps be established and further trials may turn out to be superfluous. On the other hand, if the boundary is not crossed, it is most probably necessary to continue doing trials in order to detect or reject a certain intervention effect. This can be determined by assessing if the cumulative Z‐curve crosses the trial sequential boundaries. Furthermore, trial sequential analysis can test the futility before the required information size has been reached, i.e. trial sequential analysis provides an area of futility. If futility boundaries are crossed, then further trials may be unnecessary (CTU 2011). We conducted TSA using software from the Copenhagen Trial Unit (CTU 2011). This is a departure from the published protocol (Martí‐Carvajal 2012). See the details in the Differences between protocol and review section.
Subgroup analysis and investigation of heterogeneity
We investigated heterogeneity by an informed clinical evaluation of each outcome, combining data only when clinically appropriate. We also investigated statistical heterogeneity using the I2 statistic, as described above. For the primary outcomes, we considered subgroup analysis for the following factors, as appropriate:
Extreme altitude exposure versus high or very high exposure (high: 1500 to 3500 metres; very high: 3500 to 5500 metres ; and extreme: above 5500 metres ) (Paralikar 2010).
Presence or absence of people at high risk of HAI.
The presence or absence of significant pre‐existing disease: cardiovascular diseases, chronic obstructive pulmonary disease (COPD), diabetes mellitus.
Sensitivity analysis
We performed a sensitivity analysis comparing the general results versus RCTs of high methodological quality (studies classified as having a 'low risk of bias' (Higgins 2011)). We chose only three core domains: generation of allocation sequence, incomplete outcome data, and selective reporting bias.
Summary of findings tables
We used the GRADE system (Guyatt 2008) to assess the quality of the body of evidence associated with primary outcomes (incidence of AMS, HAPE, HACE and adverse events), and we constructed three 'Summary of findings' tables using the GRADE profiler software for the three major comparisons in this review (acetazolamide versus placebo, budenoside versus placebo and dexamethasone versus placebo). The outcomes covered in these tables are the incidence of AMS, the incidence of HAPE, the incidence of HACE and adverse events (Table 1; Table 2; Table 3). The GRADE approach appraises the quality of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. Evaluation of the quality of a body of evidence considers within‐study risk of bias, directness of the evidence, heterogeneity of the data, precision of effect estimates and risk of publication bias (Balshem 2011; Guyatt 2011a; Guyatt 2011b; Guyatt 2011c; Guyatt 2011d; Guyatt 2011e; Guyatt 2011f; Guyatt 2011g; Guyatt 2011h).
Summary of findings for the main comparison. Acetazolamide compared with placebo for preventing high altitude illness.
| Acetazolamide compared with placebo for preventing high altitude illness | ||||||
|
Patient or population: people at risk of high altitude illness Setting: High altitude; studies undertaken in India, South America and USA. Intervention: acetazolamide Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Acetazolamide | |||||
| Incidence of acute mountain sickness (AMS)‐ Follow‐ up: From arrival to 24 hours later | 241 per 1000 | 113 per 1000 (94 to 135) | RR 0.47 (0.39 to 0.56) | 2301 (16 studies) | ⊕⊕⊕⊝ moderate1 | |
| Incidence of high altitude pulmonary oedema (HAPE)‐ Follow‐ up: From arrival to 24 hours later | See comment | See comment | Not estimable | 1138 (7 studies) | ⊕⊕⊕⊝ moderate2 | These trials reported no event |
| Incidence of high altitude cerebral oedema (HACE)‐ Follow‐ up: From arrival to 24 hours later | 2 per 1000 | 1 per 1000 (0 to 14) | RR 0.32 (0.01 to 7.48) | 1126 (6 studies) | ⊕⊕⊕⊝ moderate2 | |
| Adverse events: Paresthesias‐ Follow‐ up: From arrival to 24 hours later | 91 per 1000 | 504 per 1000 (256 to 992) | RR 5.53 (2.81 to 10.88) | 789 (5 studies) | ⊕⊕⊝⊝ Low3 |
|
| Adverse events: side effects‐ Follow‐ up: From arrival to 24 hours later | 106 per 1000 | 232 per 1000 (144 to 374) | RR 2.19 (1.36 to 3.53) | 400 (1 study) | ⊕⊕⊝⊝ Low4 | |
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Risk of bias downgraded (‐1) due to unclear selection, performance and detection bias in most of included studies. High risk of attrition bias in five studies. 2Risk of bias downgraded (‐1) due to unclear selection, performance and detection bias.
3 Risk of bias downgraded (‐2) due to unclear selection, performance and detection bias, as well as considerable heterogeneity (60%) 4Risk of bias downgraded (‐2) due to high levels of attrition bias.
Summary of findings 2. Budesonide compared with placebo for preventing high altitude illness.
| Budesonide compared with placebo for preventing high altitude illness | ||||||
|
Patient or population: people at risk of high altitude illness Setting: High altitude; studies undertaken in India, South America and USA. Intervention: budenoside Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| placebo | Budesonide | |||||
| Incidence of acute mountain sickness (AMS)‐ Follow‐ up: From arrival to 24 hours later | 606 per 1000 | 224 per 1000 (139 to 370) | RR 0.37 (0.23 to 0.61) | 132 (2 studies) | ⊕⊕⊝⊝ low1,2 | |
| Incidence of high altitude pulmonary oedema (HAPE)‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | This outcome was not reported for selected trials. |
| Incidence of high altitude cerebral oedema (HACE)‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | This outcome was not reported for selected trials. |
| Adverse events: Side effects‐ Follow‐ up: From arrival to 24 hours later | See comment | See comment | Not estimable | 40 (1 study) | ⊕⊝⊝⊝ very low3,4 | This trial reported no events |
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Risk of bias downgraded (‐1) due to high risk of performance bias in one out of two studies included. 2Imprecision downgraded (‐1) due to insufficient sample size to determine whether there are differences or not between these two groups. 3Risk of bias downgraded (‐1) due to high risk of performance bias. 4Imprecision downgraded (‐2) due to insufficient sample size to determine whether there are differences or not between these two groups.
Summary of findings 3. Dexamethasone compared with placebo for preventing high altitude illness.
| Dexamethasone compared with placebo for preventing high altitude illness | ||||||
|
Patient or population: people at risk of high altitude illness Setting: High altitude; studies undertaken in India, South America and USA. Intervention: dexamethasone Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| placebo | Dexamethasone | |||||
| Incidence of acute mountain sickness (AMS)‐ Follow‐ up: From arrival to 24 hours later | 449 per 1000 | 270 per 1000 (162 to 449) | RR 0.6 (0.36 to 1) | 176 (4 studies) | ⊕⊕⊝⊝ low1,2 | |
| Incidence of high altitude pulmonary oedema (HAPE)‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | This outcome was not reported for selected trials. |
| Incidence of high altitude cerebral oedema (HACE) ‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | This outcome was not reported for selected trials. |
| Adverse events: General‐ Follow‐ up: From arrival to 24 hours later | See comment | See comment | Not estimable | 21 (1 study) | ⊕⊝⊝⊝ very low3,4 | This trial reported no events |
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Risk of bias downgraded (‐1) due to unclear risk of selection, performance and detection bias in almost all studies included. 2Imprecision downgraded (‐1) due to insufficient sample size to determine whether there are differences or not between these two groups. 3Risk of bias downgraded (‐1) due to unclear risk of selection, performance and detection bias. 4Imprecision downgraded (‐2) due to insufficient sample size to determine whether there are differences or not between these two groups.
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies.
Results of the search
We carried out the latest search strategies in January 2017 and identified 1280 references. After reviewing the references by title and abstract, we selected 173 of the citations to review as full texts (see Figure 1). After reading the articles, we included 64 studies and 4547 participants (distributed across 78 references), excluded 38 studies (distributed in 40 references), classified 12 as ongoing studies, and 12 as studies awaiting assessment (most of them due to full text not yet available). We also identified 31 additional studies focusing on other interventions not covered by this review. We will incorporate these in subsequent reviews in this series.
1.
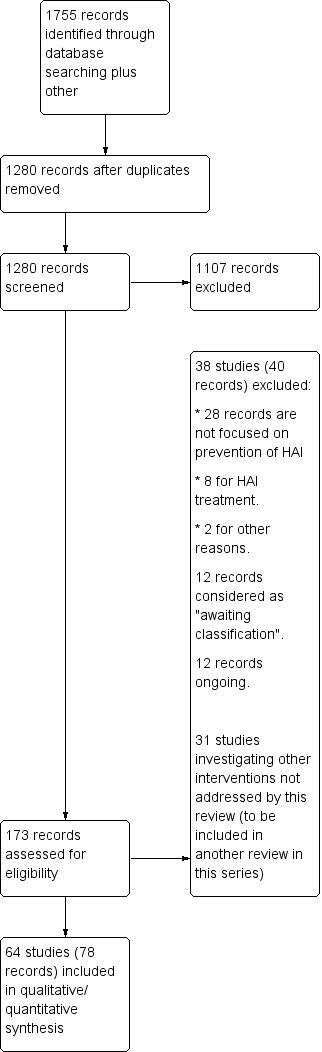
Study flow diagram.
Included studies
Twelve of 64 included studies are cross‐over trials (18.7%) that we analysed separately (Fischer 2000a; Fischer 2004; Fulco 2006; Greene 1981; Johnson 1984; Larson 1982b; Luks 2007; Muza 2004; Rock 1989a; Rock 1989b; Rock 1989c; Subudhi 2011). Fifty‐four trials were developed at high altitude (84%), and the remaining 11 were performed in hypobaric chambers (17.1%; Table 4; Baumgartner 2003; Fischer 2000a; Fischer 2004; Fulco 2006; Johnson 1984; Luks 2007; Muza 2004; Subudhi 2011; Rock 1989a; Rock 1989b; Rock 1989c).
1. Main characteristics of included studies.
| Study | High mountain | Men (%) | Increased risk of AMS, HAPE or HACE | Country | Administration timing | Trekking | Final altitude (mts) | Difference between the endpoint and the baseline altitude (mts) | Duration of ascent | Definicion de AMS | Conflict of interest |
| Anonymous 1981 | Yes | 100 | No | Ecuador | 3 days | No (Car) | 5000 | 2225 | 5 days | No definition was provided | No |
| ASCENT 2012 | Yes | 72.4 | No | Nepal | unclear | Yes | 4928 | 648 | Unclear | Lake Louise AMS score≥3 with headache | No |
| Banderet 1977 | Yes | 54.2 | No | USA | 2 days | No (Car) | 4300 | 4100 | 5 hours | No definition was provided | No |
| Bartsch 1991 | Yes | 95.2 | Previous episodes of HAPE | Italy | 4 days | No (Car) | 4559 | 3429 | 1 day | No definition was provided | No |
| Basnyat 2003 | Yes | 67.1 | No | Nepal | 2‐3 days | Yes | 4937 | 2937 | 2‐3 days | Lake Louise AMS score= headache + 1 symptom | Yes |
| Basnyat 2008 | Yes | 626 | No | Nepal | max 4 dias | Yes | 5000 | 750 | 36‐96 hours | Lake Louise AMS score≥3 with headache | Yes |
| Basu 2002a | Yes | 100 | No | India | 2 days | Yes | 3450 | 3230 | 3 days | No definition was provided | No |
| Basu 2002b | Yes | 100 | No | Nepal | 2 days | No (Flight) | 3450 | 3230 | Unclear | Lake Louise AMS score | No |
| Bates 2011 | Yes | 58 | No | Chile | 4‐5 days | 5200 | Unclear | Lake Louise AMS score≥3 | No | ||
| Baumgartner 2003 | No | 100 | No | Switzerland | 7 days | No applicable | 4559 | 4069 | 13 minutes | ESQ=AMS‐C SCORE>0,70 | No |
| Bernhard 1994 | Yes | 65.2 | 40% subjects with previous AMS mild or moderate | Bolivia | 4 days | No (Car) | 5334 | 1645 | 2 hours | Modified ESQ= 3 cerebral symptoms, one with intensity ≥2 | Yes |
| Bernhard 1998 | Yes | 69.2 | 50% of the subjects had previously visited high altitudes and had experienced mild to moderate AMS | Bolivia | 4 days | No (Car) | 5334 | 1645 | 2 hours | Modified ESQ= 3 cerebral symptoms, one with intensity ≥2 | No |
| Bradwell 1986 | Yes | 90.4 | No | Nepal | 3 days | Yes | 4846 | 3546 | 10 days | No definition was provided | No |
| Burki 1992 | Yes | Unclear | No | Pakistan | 2 days | No (Car) | 4450 | 3932 | 8 hours | No definition was provided | No |
| Burtscher 2001 | Yes | 64 | History of headache | Unclear | 2 hours | No (combination) | 3480 | 2880 | Unclear | Headache scoring | No |
| Burtscher 2014 | Yes | Unclear | History of AMS | Italy | 10 hours | No (combination) | 3800 | 3200 | Less than a day by car up to 3480, and 2.8 to 3 hours climbing from there to 3800m | Lake Louise AMS score≥3 | Yes |
| Burtscher 1998 | Yes | 58.6 | History of headache | Unclear | 1 hour | Unclear | 3480 | 2880 | Unclear | Headache scoring | Yes |
| Carlsten 2004 | Yes | 62.6 | No | Nepal | 2 hours | No (Flight) | 3630 | 3630 | 7‐8 hours | Lake Louise AMS score≥4 | Yes |
| Chen 2015 | Yes | Unclear | No | China | 3 days | No (Flight) | 3700 | 3200 | 2.5 hour | Lake Louise AMS score≥3 | No |
| Chow 2005 | Yes | 57.8 | No | USA | 5 days | No (Car) | 3800 | 2570 | 2 hours | Lake Louise AMS score≥5 | No |
| Ellsworth 1991 | Yes | 61.1 | No | USA | 1 day | No (combination) | 4392 | 3262 | 1 day | Modified ESQ= AMS‐C>0,7 + AMS‐R>0,6 | No |
| Faull 2015 | Yes | 70 | Unclear | Italy | 3 days | No (Cable‐cars or train) | 3459 | 3309 | Unclear | No definition was provided | No |
| Fischer 2000a | No | 100 | No | Germany | 3 days | No applicable | 4500 | 4500 | 30 min | No definition was provided | No |
| Fischer 2000b | Yes | 100 | No | Switzerland | 3 days | No (Cable‐cars or train) | 3454 | 3454 | 3 hours | No definition was provided | No |
| Fischer 2004 | No | 100 | No | Germany | 3 days | No applicable | 4500 | 4500 | 15 minutes | ESQ‐C score >0,5 or Lake Louise AMS score>3 | No |
| Fulco 2006 | No | 83.3 | No | USA | 1 days | No applicable | 4300 | 4300 | Unclear | Modified ESQ= AMS‐C>0,7 + AMS‐R>0,6 | No |
| Greene 1981 | Yes | 91.6 | No | Nepal | 2 days | Yes | 5895 | 3895 | 5 days | No definition was provided | No |
| Hackett 1976 | Yes | 71 | No | Nepal | 4 days | Yes | 4243 | 803 | 3‐4 days | Questionnaire clinical>2 | No |
| Hackett 1988 | Yes | 100 | No | USA | 1 hour | No (Flight) | 4400 | 4400 | 1 hour | AMS Score>2 or Modified ESQ= AMS‐C>0,7 + AMS‐R>0,6 | No |
| HEAT 2010 | Yes | 70.5 | No | Nepal | 1 day | Yes | 4928 | 648 | Unclear | No definition was provided | Yes |
| Hillenbrand 2006 | Yes | 100 | Unclear | Nepal | Unclear | Yes | 4930 | 1490 | 7 days | Lake Louise AMS score≥3 with headache | Yes |
| Hochapfel 1986 | Yes | 61,00 | No | India | 5 days | Yes | 5500 | 2100 | 9 days | No definition was provided | No |
| Hohenhaus 1994 | Yes | 86,00 | susceptibility to AMS | Italy | 3 days | No (combination) | 4559 | 4069 | 22 hours | Score clinical proposed at the International Hypoxia symposium+ Do you feel ill?=Yes | Yes |
| Hussain 2001 | Yes | 100 | No | Pakistan | 1 day | No (combination) | 4578 | 4063 | 1 day | ESQ score > = 6 | No |
| Jain 1986 | Yes | 100 | No | USA | 1 day | Unclear | 3500 | 3300 | Unclear | No definition was provided | No |
| Johnson 1984 | No | 100 | No | USA | 1 day | No applicable | 4570 | 4570 | Unclear | Modified ESQ= AMS‐C>0,7 + AMS‐R>0,6 | No |
| Kayser 2008 | Yes | unclear | No | 1 day | No (combination) | 5896 | 5896 | 7 days | Lake Louise AMS score≥3 with headache | No | |
| Ke 2013 | Yes | 100 | No | China | 3 days | No (Flight) | 3658 | Unclear | 3 hours | Presence of of headache and at least one of the symptoms of nausea or vomiting, fatigue, dizziness, or difficulty sleeping, and a total score of at least 3, | Yes |
| Küpper 2008 | Yes | 100 | No | Italia | 5 days | Yes | 4559 | 4559 | 2 days | Lake Louise AMS score≥4 | No |
| Larson 1982a | Yes | unclear | No | USA | 1 day | Yes | 4394 | 3094 | 2 days | GHAQ = Headache moderate or more and/or nausea moderate or more | No |
| Larson 1982b | Yes | 84.3 | No | USA | 1 day | Yes | 4394 | 3094 | 2 days | GHAQ = Headache moderate or more and/or nausea moderate or more | No |
| Lipman 2012 | Yes | 67.4 | No | USA | 6 hours | No (combination) | 3810 | 2570 | 12 hours | Lake Louise AMS score≥3 with headache | Yes |
| Luks 2007 | No | unclear | No | USA | 4 days | No applicable | 3900 | 2490 | Unclear | No definition was provided | Yes |
| Maggiorini 2006 | Yes | 86.2 | History of HAPE | Italia | 1 day | No (combination) | 4559 | 4069 | 2 days | Lake Louise AMS score≥4 | Yes |
| Mirrakhlmov 1993 | Yes | Unclear | Patients with asthma | Kirguistán | 2 days | No (Car) | 3200 | 2440 | 4 hours | No definition was provided | No |
| Montgomery 1989 | Yes | 74 | No | USA | 1,5 days | Unclear | 2700 | 2700 | Unclear | AMS score clinical= 3 or more symptoms with a grade 2 or greater | No |
| Moraga 2007 | Yes | 100 | No | Chile | 3 days | No (Cable‐cars or train) | 3696 | 3696 | 8,5 hours | AMS score clinical≥3 or 1 symptom=3 | No |
| Muza 2004 Def1 | No | unclear | No | USA | 1 hour | No applicable | 4300 | 4300 | Unclear | Lake Louise AMS score≥3 | Yes |
| PACE 2006 | Yes | 60 to 69 | No | Nepal | 6 days | Yes | 4928 | 1488 | Unclear | Lake Louise AMS score≥3 | No |
| Parati 2013 | Yes | 95 | No | Italy | 3 days | No (combination) | 4559 | 4437 | <28 hours | Lake Louise AMS score≥3 | Yes |
| PHAIT 2004 | Yes | 70 to 74 | No | Nepal | 2 days | Yes | 4928 | 648 | Unclear | Lake Louise AMS score≥3 with headache | Yes |
| Rock 1987 | Yes | 44 | No | USA | 2 days | No (Flight) | 4300 | 4300 | 6 hours | Modified ESQ= AMS‐C>0,7 + AMS‐R>0,6 | No |
| Rock 1989a | No | 100 | No | USA | 12 hours | No applicable | 4570 | 4570 | Unclear | Johnson Score≥1 | No |
| Rock 1989b | No | 100 | No | USA | 12 hours | No applicable | 4570 | 4570 | Unclear | Johnson Score≥1 | No |
| Rock 1989c | No | 100 | No | USA | 12 hours | No applicable | 4570 | 4570 | Unclear | Johnson Score≥1 | No |
| Sartori 2002 | Yes | unclear | susceptible to HAPE | Italy | <6 hours | No (combination) | 4559 | 3429 | 22 hours | No definition was provided | No |
| SPACE 2011 | Yes | 62 to 72 | No | Nepal | Unclear | Yes | 5000 | 700 | 30 hours‐4 days | Lake Louise AMS score= headache + 1 symptom | No |
| Subudhi 2011 | No | 80 | No | USA | 1 day | No applicable | 4875 | 3225 | 1 day | Lake Louise AMS score≥3 | Yes |
| Van Patot 2008 | Yes | 43 to 52 | No | USA | 3 days | No (Car) | 4300 | 2700 | Unclear | ESQ AMS‐C Score≥0,7 + Lake Louise AMS score≥3 with headache | Yes |
| Wang 2013 | Yes | 44 to 62 | No | Bolivia | 3 days | No (Flight) | 3561 | 3159 | 3 hours | No definition was provided | Yes |
| Wright 1983 | Yes | 95 | Previous severe AMS= 6 | Kenia | 8 days | No (combination) | 4790 | 3527 | 3 days | No definition was provided | No |
| Wright 2004 | Yes | 92 | No | Nepal | Unclear | No (Car) | 4680 | 4680 | 3 days | Lake Louise AMS score≥3 | No |
| Zell 1988 | Yes | 62 to 72 | No | Nepal | 2 days | No (combination) | 4050 | 2710 | 3 days | No definition was provided | No |
| Zheng 2014 | Yes | 100 | No | China | 1 day | No (Car) | 3900 | 3500 | 5 days | LLS includes 5 self‐reporting symptoms:headache, gastrointestinal symptoms, fatigue/weakness, dizziness/lightheadedness and difficulty in sleeping. Each symptom is scores 0‐3 | No |
Participants
The participants' ages ranged between 16 and 65 years. Nineteen of the studies included only men (29.6%; Table 4. Anonymous 1981; Basu 2002a; Basu 2002b; Baumgartner 2003; Fischer 2000a; Fischer 2000b; Fischer 2004; Hackett 1988; Hillenbrand 2006; Hussain 2001; Jain 1986; Johnson 1984; Ke 2013; Küpper 2008; Moraga 2007; Rock 1989a; Rock 1989b; Rock 1989c; Zheng 2014).
Eleven out of 64 studies included people at high risk of AMS, HAPE or HACE, due to a history of these conditions or comorbidities such as asthma (17.1%; Bartsch 1991; Bernhard 1994; Bernhard 1998; Burtscher 1998; Burtscher 2001; Burtscher 2014; Hohenhaus 1994; Maggiorini 2006; Mirrakhlmov 1993; Sartori 2002; Wright 1983).
Setting
Nineteen of the studies were undertaken in the USA (29.6%);17 were carried out in India (26.1%); and six out of 65 studies were carried out in South America (9.2%; Anonymous 1981; Bates 2011; Bernhard 1994; Bernhard 1998; Moraga 2007; Wang 2013). The remaining studies were carried out in other countries (Table 4)).
Administration of intervention to prevent AMS
Twenty‐four out of 64 studies provided the intervention between three and five days prior to the ascent (37.5%; Table 4), and 22 between one and two days prior (34.3%; Table 4). The remaining studies provided the intervention in other time intervals. Four trials did not provide information about this issue (ASCENT 2012; Hillenbrand 2006; SPACE 2011; Wright 2004). In 25% of the trials, the participants hiked to endpoint altitude (trekking), and 12 studies used a combination of means of transportation, including cars, trains, and cable‐cars (18.7%; Table 4).
Altitude
Most of the included studies reached a final altitude of between 4001 and 5000 metres above sea level (59.3%; Table 4). The most frequent difference between the endpoint and the baseline altitude was 3001 to 4000 metres (35.9%; Table 4), followed by a difference of more than 4000 metres (28.1%). The most frequent durations for ascent were of less than five hours (14 studies, 21.8%; Table 4) and three days or more (14 studies, 21.8%; Table 4). Eighteen studies did not provide information about these issues (28.1%; ASCENT 2012; Burtscher 1998; Burtscher 2001; Basu 2002a; Faull 2015; Fulco 2006; HEAT 2010; Jain 1986; Johnson 1984; Luks 2007; Montgomery 1989; Muza 2004; PACE 2006; PHAIT 2004; Rock 1989a; Rock 1989b; Rock 1989c; Van Patot 2008).
Scale used to assess AMS
The most commonly‐used scale used was the Lake Louise Score (23 trials, 35.9%), and the criterion to define AMS onset was a score three or more points in eight trials (12.5%; Table 4. Bates 2011; Burtscher 2014; Chen 2015; Muza 2004; PACE 2006; Parati 2013; Subudhi 2011; Wright 2004). In 19 studies,the criteria used to define the onset of AMS were unclear (29.6%; Anonymous 1981; Banderet 1977; Bartsch 1991; Basu 2002a; Bradwell 1986; Burki 1992; Faull 2015; Fischer 2000a; Fischer 2000b; Greene 1981; HEAT 2010; Hochapfel 1986; Jain 1986; Luks 2007; Mirrakhlmov 1993; Sartori 2002; Wright 1983; Wang 2013; Zell 1988).
Funding
In 23 of the included studies, the source of funding was unclear (35.9%; Table 4), and only 19 of 64 studies declared their possible conflicts of interests (29.6%; Basnyat 2003; Basnyat 2008; Burtscher 1998; Burtscher 2014; Carlsten 2004; HEAT 2010; Hillenbrand 2006; Hohenhaus 1994; Ke 2013; Lipman 2012; Luks 2007; Maggiorini 2006; Muza 2004; Bernhard 1994; Parati 2013; PHAIT 2004; Subudhi 2011; Van Patot 2008; Wang 2013).
Excluded studies
We excluded 38 studies (40 references) from the review. Twenty‐eight out of 38 were excluded for not focusing on HAI or AMS prevention (73.6%), but reported instead physiological or laboratory results related to altitude ascent. In eight studies, authors reported results for the treatment of HAI or AMS (21%). We excluded the remaining references for other reasons. Readers can find more information about this aspect in the Characteristics of excluded studies.
Studies awaiting classification
We classified 12 studies (Dugas 1995; Ellsworth 1987; Furian 2016; Hefti 2014; Kasic 1991; Lee 2011; Pun 2014; Roncin 1996; Swenson 1997; Utz 1970; Wang 1998; Xiangjun 2014) as awaiting assessment. We were unable to obtain the full texts from the authors, the Anaesthesia, Critical and Emergency Care Cochrane Group (ACE) or the Iberoamerican Cochrane Centre. See Characteristics of studies awaiting classification.
Ongoing studies
We considered 12 additional studies to be ongoing (ChiCTR‐TRC‐13003319; ChiCTR‐TRC‐13003590; NCT00886912; NCT01606527; NCT01682551; NCT01794078; NCT01993667; NCT02244437; NCT02450968; NCT02604173; NCT02811016; NCT02941510), given that we were only able to find them on trial registers, but we considered that they could be published shortly. See Characteristics of ongoing studies.
Risk of bias in included studies
We assessed the risks of bias for the studies across six domains. We provide a summary of our assessment of the methodological quality of included studies in Figure 2 and Figure 3.
2.
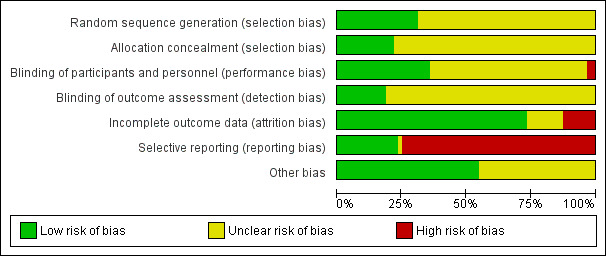
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
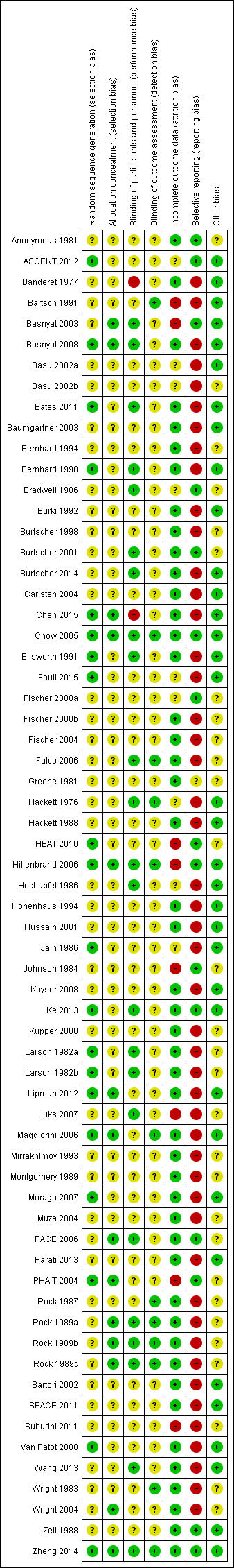
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
The authors reported a valid method of randomization in 19 studies, (ASCENT 2012; Basnyat 2008; Bates 2011; Bernhard 1998; Chen 2015; Chow 2005; Ellsworth 1991; Faull 2015; HEAT 2010; Hillenbrand 2006; Jain 1986; Ke 2013; Larson 1982a; Lipman 2012; Maggiorini 2006; Moraga 2007; PHAIT 2004; Van Patot 2008; Zheng 2014), whereas this information was not clearly reported in the remaining studies (70.3%). Similarly, 14 studies undertook and reported random allocation concealment (Basnyat 2003; Basnyat 2008; Chen 2015; Chow 2005; Hillenbrand 2006; Lipman 2012; Maggiorini 2006; PACE 2006; PHAIT 2004; Rock 1989a; Rock 1989b; Rock 1989c; Wright 2004; Zheng 2014), and the information was absent from the remaining included studies (78.1%).
Blinding
Twenty‐two studies reported blinding of participants and personnel (Basnyat 2003; Basnyat 2008; Bates 2011; Bernhard 1998; Bradwell 1986; Burtscher 2014; Chow 2005; Ellsworth 1991; Fulco 2006; Hackett 1976; Hillenbrand 2006; Hochapfel 1986; Ke 2013; Larson 1982a; Larson 1982b; Luks 2007; PACE 2006; Rock 1989a; Rock 1989b; Rock 1989c; Wang 2013; Zheng 2014). In two studies, we classified this domain as high risk (Banderet 1977; Chen 2015).
We considered the risk of detection bias to be low in 12 studies (Bartsch 1991; Chow 2005; Fulco 2006; Hackett 1976; Hillenbrand 2006; Maggiorini 2006; Rock 1987; Rock 1989a; Rock 1989b; Rock 1989c; Wright 1983; Zheng 2014), and unclear in the remaining studies (81.2%). In eight studies, we rated the risk of bias as low for both performance and detection bias (Chow 2005; Fulco 2006; Hackett 1976; Hillenbrand 2006; Rock 1989a; Rock 1989b; Rock 1989c; Zheng 2014).
Incomplete outcome data
Significant numbers of participants were lost or excluded from the final analysis of eight studies (Bartsch 1991; Basnyat 2003; HEAT 2010; Hillenbrand 2006; Johnson 1984; Luks 2007; PHAIT 2004; Subudhi 2011). Nine further studies presented unclear data (ASCENT 2012; Basu 2002a; Basu 2002b; Bradwell 1986; Faull 2015; Fischer 2000a; Hackett 1976; Hochapfel 1986; Jain 1986). In the studies with minimal attrition bias, we often found that the data analyses were undertaken on a per protocol basis, and we took this into account for data collection, including all the randomized participants in the denominators of the assessed groups.
Selective reporting
Reporting adverse events associated with the different types of interventions is fundamental to a complete assessment of their usefulness in clinical practice. We found that the majority of the studies did not report on adverse events associated with the classes of drugs commonly‐used for prevention of AMS (such as paraesthesia) (73.4%; Banderet 1977; Bartsch 1991; Basnyat 2008; Basu 2002a; Basu 2002b; Bates 2011; Baumgartner 2003; Bernhard 1994; Bernhard 1998; Burki 1992; Burtscher 1998; Burtscher 2014; Carlsten 2004; Chen 2015; Ellsworth 1991; Faull 2015; Fischer 2000b; Fischer 2004; Fulco 2006; Hackett 1976; Hackett 1988; Hochapfel 1986; Hohenhaus 1994; Jain 1986; Kayser 2008; Küpper 2008; Larson 1982a; Larson 1982b; Lipman 2012; Luks 2007; Maggiorini 2006; Mirrakhlmov 1993; Montgomery 1989; Moraga 2007; Muza 2004; Parati 2013; Rock 1987; Rock 1989a; Rock 1989b; Rock 1989c; Sartori 2002; SPACE 2011; Subudhi 2011; Van Patot 2008; Wang 2013; Wright 1983; Wright 2004).
The remaining studies reported at least one adverse event related to the assessed intervention.
Other potential sources of bias
We found a possibility of industry bias in 29 studies, mainly related to the unclear role of the sponsors in the development of the study and the unknown effect of the first phase on cross‐over trials in final results (Anonymous 1981; Basu 2002b; Bernhard 1994; Bradwell 1986; Burtscher 1998; Burtscher 2001; Fischer 2000a; Fischer 2000b; Fischer 2004; Fulco 2006; Greene 1981; HEAT 2010; Johnson 1984; Küpper 2008; Larson 1982a; Larson 1982b; Luks 2007; Mirrakhlmov 1993; Montgomery 1989; Muza 2004; PACE 2006; PHAIT 2004; Rock 1987; Rock 1989a; Rock 1989b; Rock 1989c; Subudhi 2011; Wright 1983; Wright 2004). We identified no other potential sources of risk in the remaining studies.
Effects of interventions
See: Table 1; Table 2; Table 3
See Table 1; Table 2; Table 3.
GROUP 1: Carbonic anhydrase inhibitors
Comparison 1: carbonic anhydrase inhibitors: acetazolamide versus placebo
For this comparison, we included information from 28 parallel studies (2345 participants) (Anonymous 1981; Banderet 1977; Basnyat 2003; Basnyat 2008; Bradwell 1986; Burki 1992; Burtscher 2014; Carlsten 2004; Chow 2005; Ellsworth 1991; Faull 2015; Hackett 1976; HEAT 2010; Hillenbrand 2006; Hochapfel 1986; Hussain 2001; Jain 1986; Ke 2013; Larson 1982a; Mirrakhlmov 1993; Moraga 2007; Parati 2013; PACE 2006; PHAIT 2004; SPACE 2011; Van Patot 2008; Wang 2013; Wright 2004).
All trials were performed in high mountain areas. Many of the studies administered acetazolamide or placebo between three and five days prior to ascent (13 out of 28; 46.4%) with doses of 500 mg/day (13 out of 28 studies, 46.4%; Anonymous 1981; Basnyat 2008; Bradwell 1986; Burki 1992; Chow 2005; Faull 2015; Hackett 1976; Hussain 2001; Moraga 2007; Parati 2013; PHAIT 2004; SPACE 2011; Wright 2004). For the assessment of AMS, the most widely‐used scale was the Lake Louise Score (12 out of 28 studies, 42.8%) with scores of three or more with headache as a definition of AMS (4 out of 28 trials, 14.2%; Basnyat 2008; Carlsten 2004; Hillenbrand 2006; PHAIT 2004). Two studies involved people with a history of AMS, HAPE or HACE (Burtscher 2014; Mirrakhlmov 1993).
Most of the studies reached altitudes of between 3001 to 4000 metres (Bradwell 1986; Burki 1992; Burtscher 2014; Carlsten 2004; Ellsworth 1991; Faull 2015; Jain 1986; Ke 2013; Larson 1982a; Moraga 2007; Wang 2013; Wright 2004). All but four studies included very high altitude exposure (i.e. 3500 to 5500 metres; Hochapfel 1986; Jain 1986; Mirrakhlmov 1993; Wright 2004).
Seven studies did not provide any information about any of the outcomes assessed in this review (Banderet 1977; Burki 1992; Burtscher 2014; Faull 2015; Hochapfel 1986; Jain 1986; Wang 2013). Because Carlsten 2004 and PACE 2006 evaluated two different groups that had been administered doses of acetazolamide, we included this information for the following analyses. Finally, in Carlsten 2004 two different definitions of HAI were provided and we chose information according to the second definition (Lake Louise AMS score of three or more with headache).
In addition, we analysed information from five cross‐over trials (Fischer 2004; Fulco 2006; Greene 1981; Larson 1982b; Subudhi 2011) with a total of 54 participants. Fischer 2004 only reported medians for scores of AMS, precluding the inclusion of this information in the following analysis.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Sixteen parallel studies provided information about this outcome (Basnyat 2003; Basnyat 2008; Carlsten 2004; Chow 2005; Hackett 1976; HEAT 2010; Hillenbrand 2006; Larson 1982a; Mirrakhlmov 1993; Moraga 2007; Parati 2013; PACE 2006; PHAIT 2004; SPACE 2011; Van Patot 2008; Wright 2004), registering a total of 391 events of acute mountain sickness (Incidence of AMS: 16.9%). The risk ratio (RR) for acute mountain sickness, comparing acetazolamide to placebo, was 0.47 (95% confidence interval (CI) 0.39 to 0.56; I2 = 0%; 16 trials, 2301 participants; Analysis 1.1; Figure 4).
1.1. Analysis.
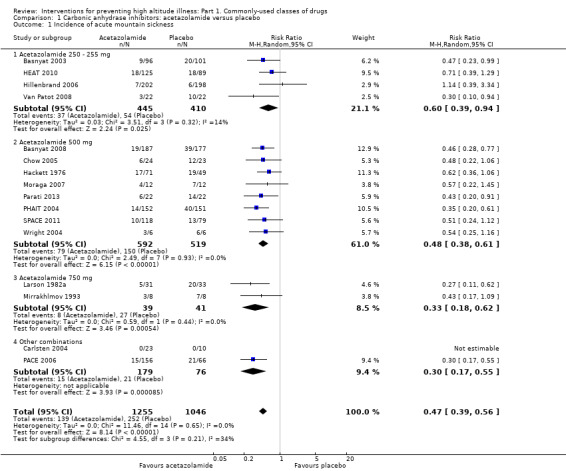
Comparison 1 Carbonic anhydrase inhibitors: acetazolamide versus placebo, Outcome 1 Incidence of acute mountain sickness.
4.
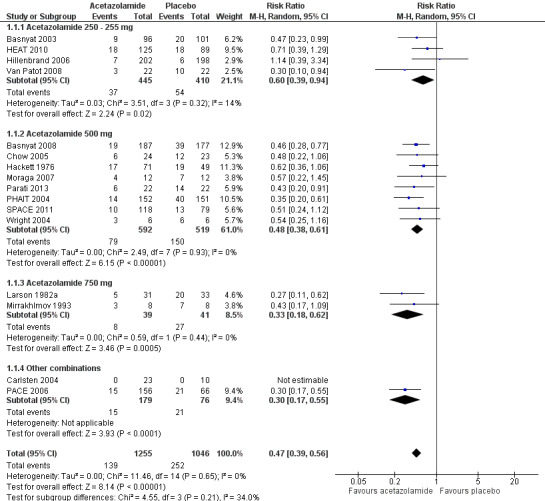
Forest plot of comparison: 1 Carbonic anhydrase inhibitors: acetazolamide versus placebo, outcome: 1.1 Incidence of acute mountain sickness.
We downgraded the quality of evidence from high to moderate, due to unclear risks of selection, detection, and performance bias in most of the included studies (See Table 1). In addition, when we considered the dosage of acetazolamide, we found a non‐statistically significant reduction in the risk of HAI in all groups (test for subgroup differences: Chi2 = 4.55, df = 3; P = 0.21; I2 = 34.0%. The RR for 250 to 255 mg is 0.60 (95% CI 0.39 to 0.94; I2 = 14%; 4 trials, 855 participants). The RR for 500 mg is 0.48 (95% CI 0.38 to 0.61; I2= 0%; 8 trials, 1111 participants). The RR for 750 mg is 0.33 (95% CI 0.18 to 0.62; I2 = 0%; 2 trials, 80 participants).The funnel plot did not show data asymmetry related to sample size (Figure 5).
5.
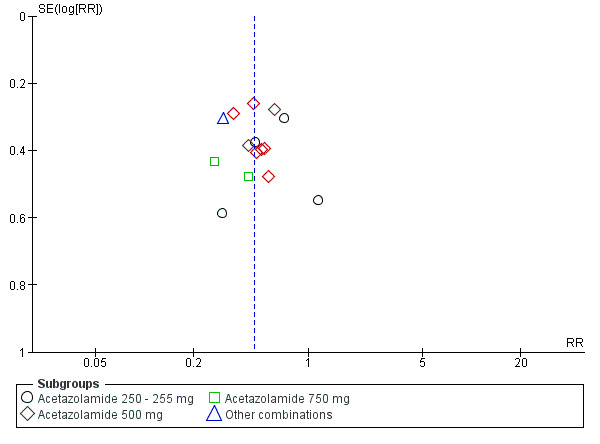
Funnel plot of comparison: 1 Carbonic anhydrase inhibitors: acetazolamide versus placebo, outcome: 1.1 Incidence of acute mountain sickness.
Regarding sensitivity analyses, only one study was at low risk of bias in the three core domains selected in the Methods section (Chow 2005). For our subgroup analyses, only one study includes an extreme altitude exposure (Wright 2004), and another includes people at high risk of HAI (Mirrakhlmov 1993). In addition, two cross‐over studies (Fulco 2006; Larson 1982b) found four events of acute mountain sickness (total incidence of AMS = 16.6%). The odds ratios ranged from 1 to 4.3. The pooled odds ratio for AMS, comparing acetazolamide to placebo, was 2.26 (95% CI 0.54 to 9.40; I2 = 56%), showing no effect of acetazolamide in the onset of HAI, but with considerable heterogeneity.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
Seven parallel studies (1138 participants) evaluated the incidence of altitude pulmonary oedema (Basnyat 2003; Basnyat 2008; Burki 1992; Chow 2005; Ke 2013; PHAIT 2004; SPACE 2011), but they did not find any events to report (Analysis 1.2). We downgraded the quality of evidence from high to moderate due to unclear risks of selection, detection, and performance bias (See Table 1).
1.2. Analysis.
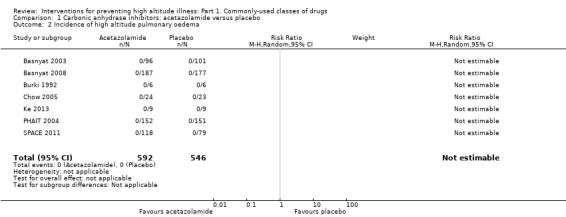
Comparison 1 Carbonic anhydrase inhibitors: acetazolamide versus placebo, Outcome 2 Incidence of high altitude pulmonary oedema.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
Six parallel studies evaluated the incidence of altitude pulmonary oedema (Basnyat 2003; Basnyat 2008; Chow 2005; Ke 2013; PHAIT 2004; SPACE 2011), but only one event was reported (incidence of HACE = 0.08%). The RR for HACE, comparing acetazolamide to placebo, was 0.32 (95% CI 0.01 to 7.48; 6 trials, 1126 participants; Analysis 1.3). We downgraded the quality of evidence from high to moderate due to unclear risks of selection, detection, and performance bias (See Table 1).
1.3. Analysis.
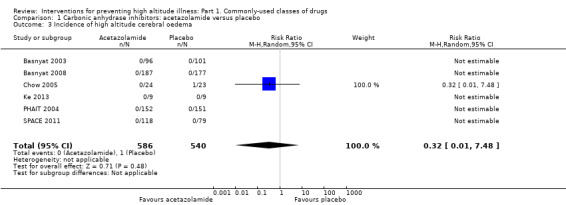
Comparison 1 Carbonic anhydrase inhibitors: acetazolamide versus placebo, Outcome 3 Incidence of high altitude cerebral oedema.
Secondary outcome 3: incidence of adverse events
Five parallel studies provide information about paraesthesias (Anonymous 1981; Basnyat 2003; Chow 2005; PACE 2006; PHAIT 2004), for 279 events (incidence of paraesthesia = 35.3%). The RR for paraesthesia, comparing acetazolamide to placebo, was 5.53 (95% CI 2.81 to 10.88; I2 = 60%; 789 participants; Analysis 1.4). This heterogeneity is reduced to 0% when the dosage of acetazolamide is taken into account (RR from 3.09 to 12.63 by dose; Analysis 1.4). We downgraded the quality of evidence from high to low due to unclear risks of selection, performance, and detection bias, as well as inconsistency (See Table 1).
1.4. Analysis.
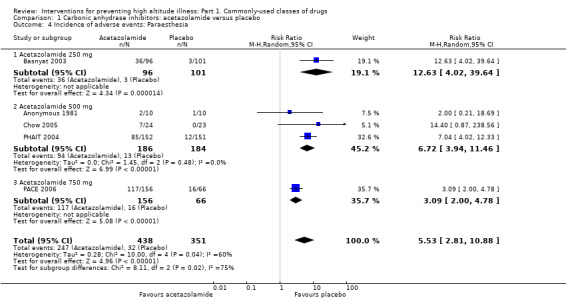
Comparison 1 Carbonic anhydrase inhibitors: acetazolamide versus placebo, Outcome 4 Incidence of adverse events: Paraesthesia.
One study (Hillenbrand 2006) evaluated the incidence of side effects in general, including paraesthesia and numbness. Sixty‐eight side effects were reported (incidence of side effects 17%). The risk of side effects, comparing acetazolamide to placebo, was 2.19 (95% CI 1.36 to 3.53) under intention‐to‐treat analysis. However, under per‐protocol analysis, the risk was 2.20 (95% CI 1.55 to 3.12). When the missing subjects were considered as cases of adverse events in both arms, the estimated risk was 1.15 (95% CI 1.08 to 1.23). We downgraded the quality of evidence from high to low due to these high levels of attrition bias (See Table 1). Another study (HEAT 2010) evaluated the incidence of major events, including drug reactions and gastrointestinal bleeding. However, authors found no major events to report. Finally, in Zell 1988 the authors reported the incidence of numbness in fingers, with six events in 32 participants.
One cross‐over study reported the incidence of tingling (Greene 1981; 24 participants). The estimated OR for this adverse event, comparing acetazolamide to placebo, was 1.44 (95% CI 0.78 to 2.68).
Secondary outcome 4: differences in HAI/AMS scores
Six parallel studies provide information about scores for AMS (Carlsten 2004; Chow 2005; Hussain 2001; Hillenbrand 2006; Moraga 2007; Wright 2004). Carlsten 2004 reported the scores for two doses of acetazolamide (250 mg and 500 mg) and compared them to a single common placebo group. To avoid double counting, we have presented the results as dosing subgroups only (Analysis 1.5). Pooling the data for all sets produced a heterogeneous effect estimate (I2 = 80.4%). The standardized mean difference between acetazolamide and placebo was 0.19 for doses of 250 mg/day (95% CI 0.01 to 0.37; I2 = 0%; 434 participants; Analysis 1.5). In contrast, the standardized mean difference between acetazolamide and placebo was ‐0.57 for doses of 500 mg/day, but with considerable heterogeneity (95% CI ‐1.20 to 0.07; I2 = 72%; 92 participants; Analysis 1.5).
1.5. Analysis.
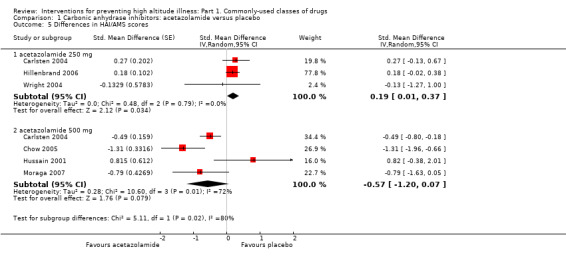
Comparison 1 Carbonic anhydrase inhibitors: acetazolamide versus placebo, Outcome 5 Differences in HAI/AMS scores.
In addition, two cross‐over studies reported differences in AMS scores, ranging from 1 to ‐2.7 (Fulco 2006; Subudhi 2011; 52 participants). The mean difference for these scores, comparing acetazolamide to placebo, was ‐1.25 (95% CI ‐4.79 to 2.29), but with considerable heterogeneity (I2 = 78%).
Trial sequential analysis for acetazolamide versus placebo
Trial sequential analysis of oral acetazolamide at any dose versus placebo for prevention of acute mountain sickness is based on the diversity‐adjusted required information size (DARIS) of 2396 participants. We calculated this DARIS based upon a proportion of participants with acute mountain sickness of 23.3% in the control group; a RRR of 20% in the experimental intervention group; an alpha of 5%; a beta of 20%; and a diversity of 0%. The cumulative Z‐curve (blue line) crossed the upper conventional alpha of 5% and the upper trial sequential alpha‐spending monitoring boundaries, showing that we have robust data for significant efficacy (Figure 6). Likewise, trial sequential analysis of oral acetazolamide at 500 mg dose versus placebo for prevention of acute mountain sickness is based on a DARIS of 1759 participants. We calculated this DARIS based upon a proportion of participants with acute mountain sickness of 29.5% in the control group; a RRR of 20% in the experimental intervention group; an alpha of 5%; a beta of 20%; and a diversity of 0%. The cumulative Z‐curve (blue line) crossed the upper conventional alpha of 5% and the upper trial sequential alpha‐spending monitoring boundaries, showing that we have robust data for significant efficacy. Finally, TSA of oral acetazolamide at 250 mg dose versus placebo for prevention of acute mountain sickness is based on a DARIS of 1777 participants. We calculated this DARIS based upon a proportion of participants with acute mountain sickness of 13.1% in the control group; a RRR of 35% in the experimental intervention group; an alpha of 5%; a beta of 20%; and a diversity of 19%. The cumulative Z‐curve (blue line) twice crossed twice the upper conventional alpha of 5%, but it did not cross the upper trial sequential alpha‐spending monitoring boundaries, indicating that new randomized controlled trials are needed. Accordingly, after only 48.1% (855/1777) of the DARIS had been attained, we were able to reject an intervention effect of 35% or larger.
6.
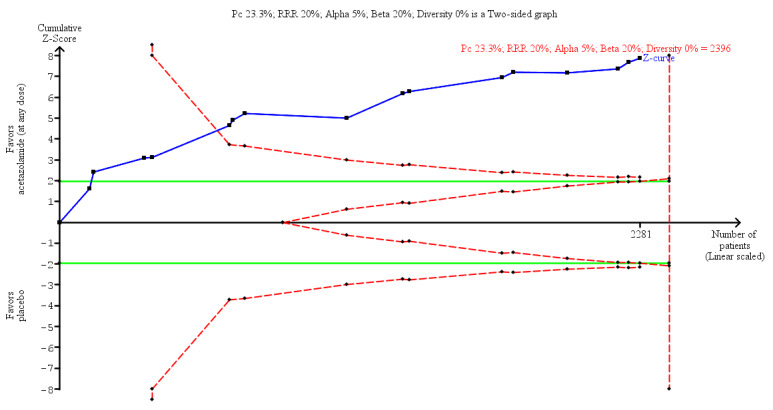
Trial sequential analysis on prevention of acute mountain illness in 16 oral acetazolamide at any dose vs placebo trials
Comparison 2: carbonic anhydrase inhibitors: acetazolamide 250 mg versus acetazolamide 500 mg
For this comparison, we analysed information from one study (Carlsten 2004) with 22 participants. This trial was carried out in the high mountain areas of Nepal, reaching a maximum altitude of 3630 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Carlsten 2004 did not identify any events of acute mountain sickness.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included study.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included study.
Secondary outcome 4: differences in HAI or AMS scores
Carlsten 2004 provided information about differences in AMS scores. The mean difference for these scores, comparing 250 mg/day of acetazolamide versus 500 mg/day of acetazolamide, was 0.76 (95% CI ‐0.16 to 1.68).
Comparison 3: carbonic anhydrase inhibitors: acetazolamide 750 mg versus acetazolamide 250mg
For this comparison, we analysed information from one study (PACE 2006) with 156 participants. This study was carried out in high mountain areas of Nepal, reaching a maximum altitude of 4928 meters.
Primary outcome 1: incidence of acute mountain sickness (AMS)
The authors of PACE 2006 found 15 events of acute mountain sickness (incidence of AMS: 9.61%).The RR for acute mountain sickness, comparing 750 mg/day versus 250 mg/day of acetazolamide, was 0.60 (95% CI 0.22 to 1.61).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included study.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
Authors of PACE 2006 reported information about paraesthesia, finding 117 events (incidence of paraesthesia: 75%). The RR for paraesthesias, comparing 750 mg/day versus 250 mg/day of acetazolamide, was 1.34 (95% CI 1.11 to 1.63).
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study.
Group 2: Steroids
Comparison 1: steroids: budenoside versus placebo
For this comparison, we analysed the information from two studies (Chen 2015; Zheng 2014) with 132 participants. Researchers administered 200 μg of inhaled budenoside twice daily in both studies. Both studies were carried out in China, reaching a maximum altitude of between 3700 to 3900 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Both studies provide information about the incidence of acute mountain sickness and found 45 events (incidence of AMS = 34%). The RR for AMS, comparing budenoside to placebo, was 0.37 (95% CI 0.23 to 0.61; I2 = 0%; Analysis 2.1). We downgraded the quality of evidence from high to low, due to a high risk of performance bias, as well as imprecision issues (See Table 2).
2.1. Analysis.
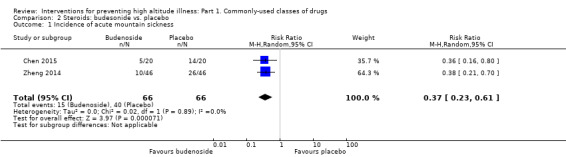
Comparison 2 Steroids: budesonide vs. placebo, Outcome 1 Incidence of acute mountain sickness.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included studies.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: incidence of adverse events
Chen 2015 assessed the incidence of side effects in general in all participants and did not find any events. We downgraded the quality of evidence from high to very low, due to a high risk of performance bias, as well as imprecision issues (See Table 2). Likewise, Zheng 2014 evaluated the onset of persistent belching but did not find any affected participants. We downgraded the quality of evidence from high to low, due to imprecision issues (See Table 2).
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included studies.
Comparison 2: steroids: dexamethasone versus placebo
For this comparison, we analysed the information from six studies in high mountain areas (Bernhard 1994; Hackett 1988; Hussain 2001; Montgomery 1989; Rock 1987; Zell 1988), with a total of 205 participants. Two studies were carried out in the USA (Hackett 1988; Montgomery 1989), two in Nepal (Rock 1987; Zell 1988), and one each in Pakistan (Hussain 2001) and Bolivia (Bernhard 1994). Hussain 2001 and Montgomery 1989 included only men. All studies used scales other than the Lake Louise Score. Bernhard 1994 included 40% of participants with previous AMS, and the altitude reached was classified as extreme (more than 5000 metres). Two studies administered 16 mg of dexamethasone (Montgomery 1989; Rock 1987), and most studies administered it during one to two days (Montgomery 1989; Rock 1987; Zell 1988).
Montgomery 1989 included the use of dexamethasone versus placebo at two different altitudes in two separate participant groups and the data for each has been presented separately (Montgomery 1989 (2,700m) and Montgomery 1989 (2,050m)).Bernhard 1994 provided two definitions for AMS, but only one (modified Environmental Symptoms Questionnaire (ESQ) = 3 cerebral symptoms, one with intensity ≥ 2) provided information for further analyses. Data from Bernhard 1994, Hackett 1988 and Hussain 2001 about AMS scores were provided as medians and standard errors, which needed transformation for the corresponding analyses (See Appendix 10).
We also analysed information from five cross‐over studies (Johnson 1984; Rock 1989a; Rock 1989b; Rock 1989c; Subudhi 2011) with a total of 53 participants. The Rock 1989 study provided information for three different doses of dexamethasone, and we extracted and analysed the data separately (Rock 1989a; Rock 1989b; Rock 1989c).
Primary outcome 1: incidence of acute mountain sickness (AMS)
Four parallel studies provided information about the incidence of acute mountain sickness (Bernhard 1994; Hackett 1988; Montgomery 1989; Rock 1987), and found a total of 60 events (incidence of AMS = 34.09%). The RR for AMS, comparing dexamethasone versus placebo, was 0.60 (95% CI 0.36 to 1.00; I2 = 39%; 176 participants; Analysis 3.1). We downgraded the quality of evidence from high to low, due to unclear risks of selection, performance, and detection bias, as well as imprecision issues (See Table 3). We found no numerical information about this outcome in the included cross‐over studies. In Subudhi 2011 the authors reported six instances of AMS, but with no information on the number in each group.
3.1. Analysis.
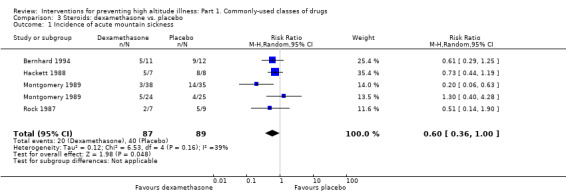
Comparison 3 Steroids: dexamethasone vs. placebo, Outcome 1 Incidence of acute mountain sickness.
Regarding sensitivity analyses, none of the studies included in this comparison present low risk of bias in all the three domains previously selected. Bernhard 1994 was the only study carried out at extreme altitude, and including a high‐risk population. Excluding this study from these analyses modified the pooled RR from 0.60 to 0.58, but increased the heterogeneity from 39% to 56%.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included studies.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: incidence of adverse events
Bernhard 1994 assessed the incidence of adverse events in general, but found no events to report. Likewise, Zell 1988 evaluated the onset of numbness in participants, but they too found no cases to report. We downgraded the quality of evidence from high to very low, due to unclear risks of selection, performance and detection bias, as well as imprecision issues (See Table 3). From the cross‐over studies, Johnson 1984 found one event of dyspepsia for this comparison (total incidence of dyspepsia = 6.25%). The RR for dyspepsia, comparing dexamethasone to placebo was 1.36 (95% CI 0.40 to 4.60).
Secondary outcome 4: differences in HAI/AMS scores
Three parallel studies provide information about AMS scores (Bernhard 1994; Hackett 1988; Hussain 2001). The standardized mean difference for these scores, comparing dexamethasone to placebo, was ‐0.46 (95% CI ‐1.21 to 0.29; I2 = 38%; 50 participants; Analysis 3.2). We downgraded the quality of evidence from high to very low, due to unclear risks of selection, performance and detection bias, as well as imprecision issues (See Table 3). Five cross‐over studies reported information about this outcome (Johnson 1984; Rock 1989a; Rock 1989b; Rock 1989c; Subudhi 2011). Mean differences ranged from ‐2.7 to 0.82 units. The MD for AMS scores, comparing dexamethasone to placebo, was ‐0.63 (95% CI ‐1.7 to 0.44), but with extreme heterogeneity (I2 = 99%).
3.2. Analysis.
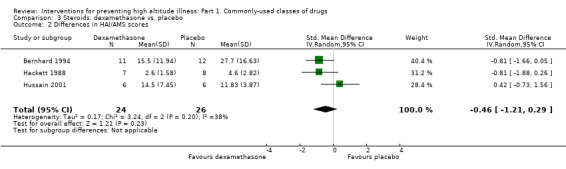
Comparison 3 Steroids: dexamethasone vs. placebo, Outcome 2 Differences in HAI/AMS scores.
Trial sequential analysis for dexamethasone versus placebo
Trial sequential analysis of dexamethazone versus placebo for prevention of acute mountain sickness is based on the diversity‐adjusted required information size (DARIS) of 517 participants. We calculated this DARIS based upon a proportion of participants with acute mountain illness of 44.9% in the control group; a RRR of 35% in the experimental intervention group; an alpha of 5%; a beta of 20%; and a diversity of 43%. After the fifth trial, the cumulative Z‐curve (blue line) crossed the upper conventional alpha of 5%, but it did not cross the upper trial sequential alpha‐spending monitoring boundaries. Accordingly, after only 34% (176/517) of the DARIS had been attained, we were able to reject an intervention effect of 35% or larger, indicating that new randomized controlled trials are needed.
Comparison 3: steroids: prednisolone versus placebo
For this comparison, we analysed the information from one study (Basu 2002b) with 40 participants. However, this study did not provide information about any of the outcomes selected for this review.
Group 3: Brochodilators
Comparison 1: bronchodilator drugs: salmeterol versus placebo
For this comparison, we analysed the information from one study (Sartori 2002) with 37 participants. Researchers administered 125 mg of inhaled salmeterol twice daily. This study was carried out in Nepal, reaching a maximum altitude of 4559 metres; all participants were susceptible to HAPE.
Primary outcome 1: incidence of acute mountain sickness (AMS)
We found no information about this outcome in the included study.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
Sartori 2002 provided information about the incidence of high‐altitude pulmonary oedema, with 20 events (incidence of HAPE = 54.05%). The RR for HAPE, comparing salmeterol to placebo, was 0.45 (95% CI 0.22 to 0.92; 37 participants).
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included study.
Secondary outcome 4: differences in HAI/AMS scores
Sartori 2002 provided information about AMS scores. The mean difference for these scores, comparing salmeterol to placebo, was ‐5.70 (95% CI ‐8.50 to ‐2.90; 37 participants).
Comparison 2: bronchodilators drugs: theophyline versus placebo
For this comparison, we identified two parallel studies with at least 20 participants (Fischer 2000a; Küpper 2008). The number of participants in Fischer 2000a was unclear, and this precludes the use of this study in further analyses. In addition, we analysed information from two cross‐over studies (Fischer 2000b; Fischer 2004) with a total of 24 participants. However, in Fischer 2004 the authors only provided information for AMS scores as medians, precluding the inclusion of this information in further analyses.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Only Küpper 2008 provided information about the incidence of acute mountain sickness, with 12 events (incidence of AMS = 60%). The RR for AMS, comparing theophyline to placebo, was 0.71 (95% CI 0.34 to 1.50; 20 male participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included studies.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included studies.
Secondary outcome 4: differences in HAI/AMS scores
Only Küpper 2008 provided information about AMS scores for the parallel studies. The standardized mean difference for these scores, comparing theophyline to placebo, was ‐0.18 (95% CI ‐1.38 to 1.02; 20 participants). Of the cross‐over studies, only Fischer 2000b reported information about scores for AMS.The mean difference between theophyline and placebo was ‐1.50 (95% CI ‐2.25 to ‐0.75).
Comparison 3: bronchodilator drugs: montelukast versus placebo
For this comparison, we analysed information from two cross‐over studies (Luks 2007; Muza 2004) with a total of 22 participants. Muza 2004 provided two definitions of AMS (Lake Louise Scale ≥ 3 and ESQ AMS‐C Score ≥ 0.7) and we selected the first one to include in analyses.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Muza 2004 found 14 events of acute mountain sickness (incidence of AMS = 58.3%). The odds ratio for AMS, comparing acetazolamide to placebo, was 1.47 (95% CI 0.61 to 3.55; 22 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included studies.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included studies.
Secondary outcome 4: differences in HAI/AMS scores
Both studies reported information about scores for AMS. Mean differences between montelukast and placebo ranged between 1.1 and ‐1.4. The mean difference between montelukast and placebo was ‐0.08 (95% CI ‐2.53 to 2.36; I2 = 81%) but with considerable heterogeneity.
Group 4: Selective inhibitors of phosphodiesterase‐5
Comparison 1: selective inhibitors of phosphodiesterase‐5: tadalafil versus placebo
For this comparison, we analysed the information from one study (Maggiorini 2006) with 19 participants. The dosage of tadalafil used was 20 mg/day. This study was carried out in Kenya, reaching a maximum altitude of 4559 metres. All participants had a history of HAPE.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Maggiorini 2006 provided information about the incidence of acute mountain sickness, with 16 events (incidence of AMS = 84.2%). The RR for AMS, comparing tadalafil to placebo, was 0.90 (95% CI 0.61 to 1.32; 29 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
Maggiorini 2006 provided information about the incidence of altitude pulmonary oedema, with eight events (incidence of HAPE = 42.1%). The RR for HAPE, comparing tadalafil to placebo, was 0.13 (95% CI 0.02 to 0.85; 29 participants).
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included study.
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study.
Comparison 2: selective inhibitors of phosphodiesterase‐5: sildenafil citrate versus placebo
For this comparison, we analysed the information from one study (Bates 2011) with 62 participants. The dosage of sildenafil citrate used was 150 mg/day. This study was carried out in Chile, reaching a maximum altitude of 5200 metres. Data about AMS scores were provided as medians and interquartile ranges, and we transformed them for further analyses (See Appendix 10).
Primary outcome 1: incidence of acute mountain sickness (AMS)
Bates 2011 provided information about the incidence of acute mountain sickness, with 39 events (incidence of AMS = 62.9%). The RR for AMS, comparing sildenafil citrate to placebo, was 1.31 (95% CI 0.91 to 1.89; 62 participants).
Secondary outcome 1 risk of altitude pulmonary oedema
We found no information about this outcome in the included study.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included study.
Secondary outcome 4: differences in HAI/AMS scores
Bates 2011 provided information about AMS scores. The standardized mean difference for these scores, comparing sildenafil to placebo, was ‐2.41 (95% CI ‐3.95 to ‐0.87; 62 participants).
Group 5: Calcium channel modulators
Comparison 1: calcium channel modulators: nifedipine versus placebo
For this comparison, we analysed the information from two studies (Bartsch 1991; Hohenhaus 1994) with a total of 48 participants. Both studies used 60 mg/day of nifedipine. Bartsch 1991 was carried out in Nepal, reaching a maximum altitude of 4559 metres, while Hohenhaus 1994 was carried out in Italy and reached the same maximum altitude. All of the participants in Bartsch 1991 had a history of HAPE, and most of the participants in Hohenhaus 1994 had susceptibility to AMS.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Hohenhaus 1994 provided information about the incidence of acute mountain sickness, with 17 events (incidence of AMS = 62.9%). The RR for AMS, comparing nifedipine to placebo, was 1.04 (95% CI 0.58 to 1.87; 27 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
Bartsch 1991 provided information about the incidence of high altitude pulmonary oedema, with eight events (incidence of HAPE = 38.09%). The RR for HAPE, comparing nifedipine to placebo, was 0.16 (95% CI 0.02 to 1.06; 21 participants).
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included studies.
Secondary outcome 4: differences in HAI/AMS scores
Both included studies provided information about AMS scores (Bartsch 1991; Hohenhaus 1994). Mean differences ranged from ‐1.25 to 0.07. The standardized mean difference for these scores, comparing nifedipine to placebo, was ‐0.56, (95% CI ‐1.85 to 0.74; I2 = 78%; 48 participants; Analysis 4.1), but with considerable heterogeneity.
4.1. Analysis.
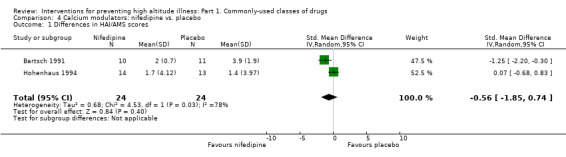
Comparison 4 Calcium modulators: nifedipine vs. placebo, Outcome 1 Differences in HAI/AMS scores.
Comparison 2: calcium channel modulators: flunarizine versus placebo
For this comparison, we analysed the information from one study (Baumgartner 2003) with 20 participants. Baumgartner 2003 used a hypobaric chamber to assess the effectiveness of 10 mg of flunarizine at 4559 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Baumgartner 2003 provided information about the incidence of acute mountain sickness and found 14 events (incidence of AMS = 70%). The RR for AMS, comparing flunarizine to placebo, was 1.00 (95% CI 0.56 to 1.78; 20 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included study.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included study.
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study.
Group 6: non‐steroidal anti‐inflammatory drugs (NSAIDs)
Comparison 1: non‐steroidal anti‐inflammatory drugs (NSAIDs) and other analgesics: aspirin versus placebo
For this comparison, we analysed the information from two studies (Burtscher 1998; Burtscher 2001) with a total of 60 participants. Both studies focused on headache at altitude, using a headache score to evaluate its onset. Aspirin 320 mg was used as a prophylaxis, given from one to two hours beforehand; both studies reached a maximum altitude of 2880 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Both studies provided information about the incidence of acute mountain sickness (Burtscher 1998; Burtscher 2001), and found a total of 31 events (incidence of AMS = 51.6%). RRs ranged from 0.13 to 0.60. The RR for AMS, comparing aspirin to placebo, was 0.35 (95% CI 0.06 to 1.95; I2 = 68%; 60 participants; Analysis 5.1), but with considerable heterogeneity.
5.1. Analysis.
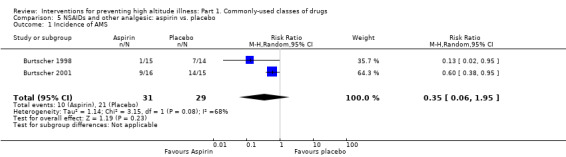
Comparison 5 NSAIDs and other analgesic: aspirin vs. placebo, Outcome 1 Incidence of AMS.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included studies.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: incidence of adverse events
Burtscher 2001 assessed the incidence of major adverse events in general, but did not find any events to report.
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included studies.
Comparison 2: non‐steroidal anti‐inflammatory drugs (NSAIDs) and other analgesics: ibuprofen versus placebo
For this comparison, we analysed the information from three studies (ASCENT 2012; HEAT 2010; Lipman 2012), with a total of 598 participants. Only ASCENT 2012 and Lipman 2012 provided a clear definition to determine the onset of AMS (Lake Louise AMS score ≥ 3 with headache). Ibuprofen dosage ranged from 600 to 1800 mg. ASCENT 2012 and HEAT 2010 were developed in Nepal, reaching a maximum altitude of 4928 metres, while Lipman 2012 was developed in the USA, reaching a maximum altitude of 3810 metres. None of these studies included high‐risk populations.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Three studies provided information about the incidence of acute mountain sickness (ASCENT 2012; HEAT 2010; Lipman 2012), and found a total of 154 events (incidence of AMS = 25.7%). The RR for AMS, comparing ibuprofen to placebo, was 0.64 (95% CI 0.49 to 0.82; I2 = 0%; 598 participants; Analysis 6.1). Regarding sensitivity analyses, none of the included studies in this comparison were at low risk of bias in the three previously selected domains. Likewise, all three studies were developed at very high altitude and none of them included a population at high risk of developing HAI/AMS.
6.1. Analysis.
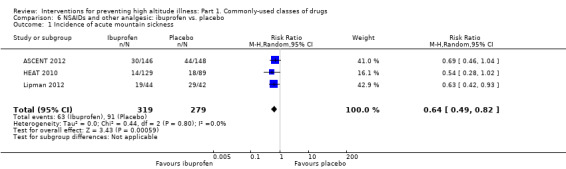
Comparison 6 NSAIDs and other analgesic: ibuprofen vs. placebo, Outcome 1 Incidence of acute mountain sickness.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
ASCENT 2012 evaluated the incidence of altitude pulmonary oedema, but did not find any events to report.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
ASCENT 2012 evaluated the incidence of altitude cerebral oedema, but did not find any events to report.
Secondary outcome 3: incidence of adverse events
HEAT 2010 assessed the incidence of major adverse events in general, but did not find any events to report. The authors of ASCENT 2012 reported one event of black stools in the ibuprofen group.
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included studies.
Trial sequential analysis for ibuprofen versus placebo
Trial sequential analysis of oral ibuprofen at any dose versus placebo for prevention of acute mountain sickness is based on a DARIS of 1532 participants. We calculated this DARIS based on a proportion of participants with acute mountain sickness of 32.6% in the control group; a RRR of 20% in the experimental intervention group; an alpha of 5%; a beta of 20%; and a diversity of 0%. After the second trial, the cumulative Z‐curve (blue line) crossed the upper conventional alpha of 5%, but it did not cross the upper trial sequential alpha‐spending monitoring boundaries, which were reached rather than crossed by the third trial. After only 39% (598/1532) of the DARIS had been reached, we were able to reject an intervention effect of 20% or larger, indicating that new randomized controlled trials are needed.
Comparison 3: non‐steroidal anti‐inflammatory drugs (NSAIDs) and other analgesics: carbasalate versus placebo
For this comparison, we analysed the information from one study (Kayser 2008) with 31 participants. Kayser 2008 defined AMS in three different ways (Lake Louise AMS score ≥ 3 with headache; Lake Louise AMS score with headache and self‐score + functional score ≥ 4; and Lake Louise AMS score with headache and self‐score + functional score + clinical score ≥ 4). We chose the first definition for the following analyses.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Kayser 2008 provided information about the incidence of acute mountain sickness and found a total of 26 events (incidence of AMS = 83.8%). The RR for AMS, comparing carbasalate to placebo, was 0.91 (95% CI 0.67 to 1.25; 31 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included study.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included study.
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study.
Group 7: Other comparisons
Comparison 1: other comparisons: acetazolamide versus dexamethasone
For this comparison, we included information from three studies (Ellsworth 1991; Hussain 2001; Zell 1988), with a total of 46 participants. In Ellsworth 1991, investigators administered 750 mg/day of acetazolamide. The study was carried out in the USA, reaching a maximum altitude of 4392 metres. Zell 1988 and Hussain 2001 used 500 mg/day of acetazolamide. Zell 1988 was carried out in Nepal, reaching a maximum altitude of 4050 metres. We also included information from a cross‐over study (Subudhi 2011), which compared acetazolamide 750 mg/day to 12 mg dexamethasone using a hypobaric chamber.
Primary outcome 1: incidence of acute mountain sickness (AMS)
We found no information about this outcome in the included studies.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included studies.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: incidence of adverse events
Zell 1988 reported information about numbness in the fingers, finding six events (Incidence of numbness: 37.5%). The RR for numbness, comparing acetazolamide to dexamethasone, was 16.25 (95% CI 1.07 to 247.19; 16 participants).
Secondary outcome 4: differences in HAI/AMS scores
Hussain 2001 provided information about differences in AMS scores at high altitude. The standardized mean difference for AMS scores, comparing acetazolamide to dexamethasone, was 0.292 (95% CI 0.06 to 0.52; 12 participants). We also found information about this outcome in Subudhi 2011. The standardized mean difference for AMS scores, comparing acetazolamide to dexamethasone, was 0.00 (95% CI ‐0.23 to 0.23; 40 participants).
Comparison 2: other comparisons: acetazolamide plus dexamethasone versus acetazolamide
For this comparison, we analysed information from three studies (Bernhard 1998; Hussain 2001; Zell 1988), with a total of 40 participants. Bernhard 1998 used 500 mg of acetazolamide/day plus 8 mg of dexamethasone/day. Forty per cent of the participants in this study had a history of previous mild or moderate AMS. This study was carried out in Italy, reaching a maximum altitude of 5334 metres. Hussain 2001 and Zell 1988 used 500 mg of acetazolamide/day plus 8 mg and 16 mg of dexamethasone/day respectively; there were no groups at risk of AMS, HAPE or HACE. Zell 1988 was carried out in Nepal, reaching a maximum altitude of 4050 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Bernhard 1998 found eight events of acute mountain sickness (incidence of AMS: 61.5%).The RR for acute mountain sickness, comparing acetazolamide plus dexamethasone to acetazolamide plus placebo, was 0.70 (95% CI 0.28 to 1.77; 13 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included studies.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: incidence of adverse events
Zell 1988 reported information about numbness in the fingers, finding 11 events (incidence of numbness: 73.3%). The RR for numbness, comparing acetazolamide plus dexamethasone to acetazolamide, was 0.73 (95% CI 0.39 to 1.35; 15 participants).
Secondary outcome 4: differences in HAI/AMS scores
Hussain 2001 provided information about differences in AMS scores at high altitude. The mean difference for AMS scores, comparing acetazolamide to dexamethasone was ‐11.47 (95% CI ‐17.63 to ‐5.31; 12 participants).
Comparison 3: other comparisons: acetazolamide plus dexamethasone versus dexamethasone
For this comparison, we included information from two studies (Hussain 2001; Zell 1988), with a total of 29 participants. In Zell 1988 500 mg of acetazolamide/day plus 16 mg of dexamethasone/day were used. This study was carried out in Nepal, reaching a maximum altitude of 4050 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
We found no information about this outcome in the included studies.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included studies.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included studies.
Secondary outcome 3: Incidence of adverse events
Zell 1988 reported information about numbness in fingers, finding five events (Incidence of numbness: 29.4%). The RR for numbness, comparing acetazolamide plus dexamethasone to dexamethasone was 12.22 (95% CI 0.78 to 191.46; 17 participants).
Secondary outcome 4: differences in HAI/AMS scores
Hussain 2001 provided information about differences in AMS scores at high altitude. The mean difference for AMS scores, comparing acetazolamide plus dexamethasone to dexamethasone was ‐9.17 (95% CI ‐15.62 to ‐2.72; 12 participants).
Comparison 4: other comparisons: acetazolamide versus ibuprofen
For this comparison, we analysed information from one study (HEAT 2010) with 254 participants. HEAT 2010 administered 225 mg of acetazolamide/day or 600 mg of ibuprofen/day.
Primary outcome 1: risk of acute mountain sickness
HEAT 2010 found 32 events of acute mountain sickness (incidence of AMS: 12.59%). The RR for AMS, comparing acetazolamide to ibuprofen, was 1.33 (95% CI 0.69 to 2.55; 163 participants).
Secondary outcome 1: risk of altitude pulmonary oedema.
We found no information about this outcome in the included study.
Secondary outcome 2: risk of high altitude cerebral oedema
We found no information about this outcome in the included study.
Secondary outcome 3: adverse events
HEAT 2010 did not identify any major adverse events.
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study.
Comparison 5: other comparisons: acetazolamide versus methazolamide
For this comparison, we analysed information from one study (Wright 1983) with 20 participants. Wright 1983 used 500 mg of acetazolamide/day and 100/150 mg of methazolamide/day. This study was carried out in high mountain areas of Nepal, reaching a maximum altitude of 4790 metres. Some participants in this study had a previous history of severe AMS.
Primary outcome 1: incidence of acute mountain sickness (AMS)
We found no information about this outcome in the included study.
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included study.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included study.
Secondary outcome 4: differences in HAI/AMS scores
Wright 1983 reported information about AMS scores.The standardized mean difference between acetazolamide and methazolamide, was ‐3.00 (95% CI ‐21.07 to 15.07; 20 participants).
Comparison 6:other comparisons: budenoside plus formoterol versus placebo
For this comparison, we analysed the information from one study (Chen 2015) with 40 participants in the relevant arms. This study was carried out in China, reaching a maximum altitude of 3700 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Chen 2015 provide information about the incidence of acute mountain sickness and found 24 events (incidence of AMS = 60%). The RR for AMS, comparing budenoside plus formoterol to placebo, was 0.71 (95% CI 0.42 to 1.21; 40 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included study.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
Chen 2015 assessed the incidence of side effects but found no events.
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study.
Comparison 7: other comparisons: budenoside versus dexamethasone
For this comparison, we analysed information from one study (Zheng 2014) with 92 participants. Zheng 2014 used 400 mg of budenoside/day and 4 mg of dexamethasone/day. This study was carried out in China, reaching a maximum altitude of 4050 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Zheng 2014 found 22 events of acute mountain sickness for this comparison (incidence of AMS = 23.9%). The RR for AMS, comparing budenoside to dexamethasone, was 0.83 (95% CI 0.40 to 1.73; 92 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included study
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
Zheng 2014 found four events of persistent belching for this comparison (incidence of persistent blenching = 4.34%). The RR for persistent blenching, comparing budenoside to dexamethasone, was 0.11 (95% CI 0.01 to 2.01; 92 participants).
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study
Comparison 8: other comparisons: budenoside versus budenoside plus formoterol
For this comparison, we analysed information from one study (Chen 2015) with 40 participants in the relevant arms. This study used 400 mg of budenoside/day and 9 mg of formoterol/day. It was carried out in China, reaching a maximum altitude of 3700 metres.
Primary outcome 1: incidence of acute mountain sickness (AMS)
Chen 2015 found 15 events of acute mountain sickness for this comparison (total incidence of AMS = 37.5%). The RR for AMS, comparing budenoside to budenoside plus formoterol, was 0.50 (95% CI 0.21 to 1.20; 40 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
We found no information about this outcome in the included study.
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
Chen 2015 did not find any side effects for this comparison.
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study.
Comparison 9: other comparisons: dexamethasone versus prednisolone
For this comparison, we analysed the information from one study (Basu 2002a) with 40 participants. However, this study did not provide information about any of outcomes selected for this review.
Comparison 10: other comparisons: tadalafil versus dexamethasone
For this comparison, we analysed information from one study (Maggiorini 2006) with 20 participants. Maggiorini 2006 used 20 mg of tadalafil/day and 16 mg of dexamethasone/day. This study was carried out in Kenya, reaching a maximum altitude of 4559 metres. All participants had a history of HAPE.
Primary outcome 1: incidence of Acute mountain sickness (AMS)
Maggiorini 2006 found 11 events of acute mountain sickness for this comparison (incidence of AMS = 55%). The RR for AMS, comparing tadalafil to dexamethasone, was 2.67 (95% CI 0.98 to 7.22; 20 participants).
Secondary outcome 1: incidence of high altitude pulmonary oedema (HAPE)
Maggiorini 2006 found one event of altitude pulmonary oedema for this comparison (incidence of AMS = 5%). The RR for HAPE, comparing tadalafil to dexamethasone, was 3.0 (95% CI 0.14 to 65.9; 20 participants).
Secondary outcome 2: incidence of high altitude cerebral oedema (HACE)
We found no information about this outcome in the included study.
Secondary outcome 3: incidence of adverse events
We found no information about this outcome in the included study
Secondary outcome 4: differences in HAI/AMS scores
We found no information about this outcome in the included study
Discussion
Summary of main results
Evidence from 65 studies showed important findings for interventions included in this review (commonly‐used pharmacological interventions). We report results for the three more important comparisons:
Acetazolamide versus placebo (28 parallel studies; 2345 participants)
Our systematic review included data from 28 parallel clinical studies (n = 2345 participants) and five cross‐over studies (n= 54 participants) that assessed the effectiveness of acetazolamide compared with a placebo for the prevention of high altitude illness. The risk of AMS was reduced with acetazolamide (RR 0.47; 95% CI 0.39 to 0.56; I2 = 0%; 16 trials; 2301 participants; moderate quality of evidence). No events of HAPE were reported and only one event of HACE (RR 0.32; 95% CI 0.01 to 7.48; 6 parallel trials; 1126 participants; moderate quality of evidence). Few studies reported side effects for this comparison, and they showed an increase in the risk of paraesthesia with the intake of acetazolamide (5 studies, 789 participants; RR from 3.09 to 12.63 by acetazolamide dosage).
Budenoside versus placebo (2 parallel studies; 132 participants)
Data on budenoside showed a reduction in the incidence of AMS compared with placebo (2 studies, 132 participants; RR 0.37; 95% CI 0.23 to 0.61; I2 = 0%; low quality of evidence). The included studies did not report any events of HAPE or HACE, and they did not find side effects (low quality of the evidence).
Dexamethasone versus placebo (7 parallel studies; 205 participants)
For dexamethasone, data did not show benefits of dexamethasone at any dosage (four studies, 176 participants; RR 0.60; 95% CI 0.36 to 1.00; I2 = 39%; low quality of evidence). The studies did not report any events of HAPE or HACE, and we rated the evidence about adverse events as of very low quality.
We did not find any studies comparing methazolamide with a placebo. We also did not find evidence of benefits of theophyline, montelukast, selective inhibitors of phosphodiesterase‐5 (such as tadalafil and sildenafil), nifedipine, flunarizine, aspirin or carbasalate in reducing the incidence of AMS. Finally, we found little information on other comparisons between different agents included in this review (i.e. ibuprofen versus placebo, acetazolamide versus dexamethasone). Combinations of these drugs did not deliver any benefits.
Overall completeness and applicability of evidence
We carried out a thorough search and identified an important number of studies addressing effectiveness and safety in the most commonly‐used pharmacological interventions for the prevention of HAI or AMS. We included 65 studies in our review, with more than 2000 participants. Those studies addressed around 15 comparisons with placebos, and 11 comparisons between different drugs. The data included participants of different age groups and both genders, as well as different high‐altitude settings, different final altitudes reached, transportation, and prophylaxis times. Our systematic search for studies and our data extraction procedures should have minimized the likelihood of missing relevant studies. The funnel plot for acetazolamide versus placebo was highly symmetrical, suggesting that the chance of having missed relevant studies was minimal, with no evidence of publication bias. Despite all this, we found a lack of reports of the duration of prophylaxis, duration of ascent, criteria to diagnose AMS, HAPE or HACE, or statistical data (such as standard deviations) in several of the included studies. The sparsity of reports of adverse events was the most frequent limitation of the included studies, as well as the wide range of criteria and scales used to determine the onset of acute mountain sickness. The identification of only one study for several of the comparisons was a common factor limiting the scope and strength of this review.
The trial sequence analyses performed with on acetazolamide for the prevention of AMS suggest we have robust data for significant efficacy, which can be applied with some confidence in the field.
Quality of the evidence
We conducted GRADE assessments on outcomes of meta‐analyses and single trials. We were unable to rate the evidence from either pooled or non‐pooled estimates as high, due to either or both of the following reasons:
small sample sizes
the risk of bias from multiple sources, including the lack of adequate randomization methods, lack of blinding, high attrition, unclear reporting of outcomes, and bias in the presentation of data, among others.
We also downgraded the evidence because of uncertainty in clinically relevant outcomes, reflected in wide confidence intervals, i.e. imprecision. See Table 1, Table 2 and Table 3 for detailed assessments and the rationale for ratings.
Potential biases in the review process
In all cases, we followed the methodology for systematic reviews outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). However, we had to made extensive modifications to the published protocol (Martí‐Carvajal 2012), due to the need to update the methods under the current methodological guidelines for Cochrane Reviews. Readers should be aware of the potential biases related to these modifications (detailed in Differences between protocol and review), as well as the decision to split the review into three parts, considering the numerous interventions assessed for HAI prevention.
In this review we undertook a comprehensive search to identify clinical trials addressing the issue of effectiveness and safety of commonly‐used classes of drugs for preventing acute HAI. Twelve studies did not provide enough information to classify them as included or excluded, because they were published only as conference proceedings, or because we did not have access to the full texts when we were completing this review. We have also considered 12 additional studies as ongoing because they are published only as protocols and we may be able to decide whether or not to include them once they have been published. A potential source of bias in the review process is that most of the studies (more than 75%), did not report adverse events associated with the classes of drugs commonly‐used for the prevention of AMS. This constitutes a lack of information about the safety profile of the drugs in question. Likewise, we did not expect to encounter any unit of analysis issues, as we did not expect to find cross‐over studies. However, we identified 12 cross‐over studies (20%). In order to avoid bias in the development of our review, we have analysed those studies separately.
Agreements and disagreements with other studies or reviews
There are several examples of published reviews evaluating different interventions to prevent high altitude illness. We found that our results are similar to other non‐Cochrane reviews (Low 2012; Kayser 2012; Ritchie 2012; Seupaul 2012; Zafren 2014), regarding HAI/AMS prevention (CATMAT 2007; Luks 2010; Luks 2014). Most of these reviews recommend acetazolamide (at doses of 500 mg/day) as the first choice for the prevention of this condition. A systematic review developed by Dumont 2000 concludes that doses of 750 mg/day are more effective than 500 mg/day; however, our findings showed that effectiveness is similar for these two options, but there is no clear information on whether the incidence of adverse events is greater, due to the lack of information in the studies for this outcome.
In 2014, Tang 2014 published evidence in favour of the use of oral dexamethasone for the prevention of AMS. The authors of this review reported that dexamethasone could reduce the incidence of AMS, with an odds ratio of 6.03 (95% CI 2.23 to 21.00), compared with placebo. While they only identified eight studies comparing dexamethasone to placebo, we found six parallel trials and five cross‐over studies. Our analysis did not produce definitive evidence about the effectiveness of dexamethasone, but we rated this evidence as being of low quality. In addition, our trial sequential analyses suggest that new randomized controlled trials are needed for this intervention. We note that current guidelines about AMS prevention include recommendations about the use of dexamethasone to prevent HAI/AMS, in 2 mg doses every six hours or 4 mg every 12 hours (Luks 2010; Luks 2014). For the use of non‐steroidal anti‐inflammatory drugs (NSAIDs), our results are similar to those published by Pandit 2014, and support the use of ibuprofen as an alternative for acetazolamide, despite the fact that they provide analyses for all pooled NSAIDs (OR 0.43; 95% CI 0.27 to 0.69, I2 = 0%). We did not find any reviews about other options such as tadalafil, sildenafil, nifedipine, flunarizine or theophylline, and these are not recommended in current clinical practice guidelines for the prevention of this condition.
Authors' conclusions
Implications for practice.
Our analysis suggests that acetazolamide, administered between three and five days prior to ascent, is an effective pharmacological agent to prevent acute altitude sickness in dosages of 250 to 750 mg/day. This information is based on evidence of moderate quality. Acetazolamide is associated with an increased risk of paraesthesia, which should be balanced against the suggested benefit. The clinical benefits and harms from other pharmacological interventions are unclear. There is little evidence relating to the prevention of HAPE and HACE, due to the low number of events reported.
Implications for research.
There is a need for further high‐quality research in this area. Future studies should be adequately powered to assess the effectiveness of these agents for the prevention of more serious forms of AMS, in combination as well as single agents. The design of future trials might be improved by the following suggestions:
Refining the clinical definition of AMS, HAPE and HACE.
Improving the reporting of statistical data related to important results, in order to avoid missing data, including information about elevation where HAI occurs.
Adding adverse events as an important endpoint in assessment of these preventive strategies.
Comparing pharmacological agents against interventions of established effectiveness (such as acetazolamide).
Finally, we suggest performing a network meta‐analysis of all interventions (pharmacological and non‐pharmacological) used for high altitude illness prevention, in order to determine which interventions are effective in avoiding the onset of new cases of this condition.
What's new
| Date | Event | Description |
|---|---|---|
| 17 December 2018 | Amended | Editorial team changed to Cochrane Emergency and Critical Care |
History
Protocol first published: Issue 4, 2012 Review first published: Issue 6, 2017
| Date | Event | Description |
|---|---|---|
| 13 March 2018 | Amended | typo corrected |
| 12 March 2018 | Amended | We amended the Differences between protocol and review section so that the changes made to the primary outcomes were clearly justified. In particular, the reason for removing mortality as an outcome. |
| 17 April 2012 | Amended | Contact details updated. |
Acknowledgements
We would like to thank Mike Bennett (content editor), Vibeke E Horstmann (statistical editor), Janne Vendt (Information Scientist), Jeffrey H Gertsch, Martin Burtscher (peer reviewers), Matiram Pun (consumer referee) and Jane Cracknell (Managing Editor) for their help and editorial advice during the preparation of this systematic review.
Appendices
Appendix 1. Risk categories for acute mountain sickness
| Risk categories | Description |
| Low | Individuals with no prior history of altitude illness and ascending to ≤ 2800 m/9186 feet. |
| Low | Individuals taking ≥ 2 days to arrive at 2500 ‐ 3000 m/8202 ‐ 9842 feet with subsequent increases in sleeping elevation < 500 m by day/ 1640 feet by day |
| Moderate | Individuals with prior history of AMS and ascending to 2500 ‐ 2800 m (8202 ‐ 9186 feet) in 1 day |
| Moderate | No history of AMS and ascending to > 2800 m (9186 feet) in 1 day |
| Moderate | All individuals ascending > 500 m/d (1640 feet) (increase in sleeping elevation) at altitudes above 3000 m/9842 feet |
| High | History of AMS and ascending to ≥ 2800 m/9186 feet in 1 day |
| High | All individuals with a prior history of HAPE or HACE |
| High | All individuals ascending to > 3500 m/11482 feet in 1 day |
| High | All individuals ascending > 500 m/1640 feet/d increase in sleeping elevation above > 3500 m/11482 feet |
| High | Very rapid ascents (e.g. Mount Kilimanjaro) |
Appendix 2. Medical terms glossary
| Term | Definition | Source |
| Anorexia | The lack or loss of appetite accompanied by an aversion to food and the inability to eat. | https://www.ncbi.nlm.nih.gov/mesh/68000855 |
| Ataxia | Impairment of the ability to perform smoothly co‐ordinated voluntary movements. | https://www.ncbi.nlm.nih.gov/mesh/68001259 |
| Dyspnoea | Difficult or laboured breathing. | https://www.ncbi.nlm.nih.gov/mesh/?term=Dyspnoea |
| Dizziness | An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. | https://www.ncbi.nlm.nih.gov/mesh/68004244 |
| Endothelium | A layer of epithelium that lines the heart, blood vessels (endothelium vascular), lymph vessels (endothelium lymphatic), and the serous cavities of the body. | https://www.ncbi.nlm.nih.gov/mesh/68004727 |
| Fatigue | The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. | https://www.ncbi.nlm.nih.gov/mesh/68005221 |
| Hallucination | Subjectively experienced sensations in the absence of an appropriate stimulus, but which are regarded by the individual as real. | https://www.ncbi.nlm.nih.gov/mesh/?term=Hallucination |
| Headache | The symptom of pain in the cranial region. | https://www.ncbi.nlm.nih.gov/mesh/68006261 |
| Hernia | Protrusion of tissue, structure, or part of an organ through the bone, muscular tissue, or the membrane by which it is normally contained. | https://www.ncbi.nlm.nih.gov/mesh/68006547 |
| Hypoxia | A disorder characterized by a reduction of oxygen in the blood. | https://www.ncbi.nlm.nih.gov/mesh/68000860 |
| Insomnia | Disorders characterized by impairment of the ability to initiate or maintain sleep. | https://www.ncbi.nlm.nih.gov/mesh/68007319 |
| Lightheadedness | See dizziness. | |
| Nausea | An unpleasant sensation in the stomach usually accompanied by the urge to vomit. | https://www.ncbi.nlm.nih.gov/mesh/68009325 |
| Pulmonary oedema | Excessive accumulation of extravascular fluid in the lung, an indication of a serious underlying disease or disorder. Pulmonary oedema prevents efficient pulmonary gas exchange in the pulmonary alveoli, and can be life‐threatening. | https://www.ncbi.nlm.nih.gov/mesh/?term=Pulmonary+oedema |
| Pulmonary alveoli | Small polyhedral outpouchings along the walls of the alveolar sacs, alveolar ducts and terminal bronchioles through the walls of which gas exchange between alveolar air and pulmonary capillary blood takes place. | https://www.ncbi.nlm.nih.gov/mesh/?term=Pulmonary+alveoli |
| Seizures | Clinical or subclinical disturbances of cortical function due to a sudden, abnormal, excessive, and disorganized discharge of brain cells. Clinical manifestations include abnormal motor, sensory and psychic phenomena. | https://www.ncbi.nlm.nih.gov/mesh/68012640 |
Appendix 3. The most frequents adverse events of the pharmacological interventions
| Drug | Description and contraindications | Adverse events | Source |
| Acetazolamide | Acetazolamide, an inhibitor of the enzyme carbonic anhydrase. Hypersensitivity to acetazolamide or any excipients in the formulation. Since acetazolamide is a sulphonamide derivative, cross sensitivity between acetazolamide, sulphonamide and other sulphonamide derivatives is possible. Acetazolamide therapy is contraindicated in situations in which sodium and/or potassium blood serum levels are depressed, in cases of marked kidney and liver disease or dysfunction, in suprarenal gland failure, and in hyperchloraemic acidoses. It is contraindicated in patients with cirrhosis because of the risk of development of hepatic encephalopathy. |
Adverse reactions, occurring most often early in therapy, include paraesthesias, particularly a “tingling” feeling in the extremities, hearing dysfunction or tinnitus, loss of appetite, taste alteration and gastrointestinal disturbances such as nausea, vomiting and diarrhoea; polyuria, and occasional instances of drowsiness and confusion | DailyMed |
| Aspirin | it is a nonsteroidal anti‐inflammatory drug. | Reye's syndrome (a rare but serious illness). Stomach bleeding |
DailyMed |
| Bosentan | It is an endothelin receptor antagonist indicated for the treatment of pulmonary arterial hypertension. Pregnancy, pre‐existing hepatic impairment. |
Elevations of liver aminotransferases (ALT, AST) and liver failure. Early liver injury may preclude future use as disease progresses. Respiratory tract infection and anaemia |
DailyMed |
| Dexamethasone | Glucocorticoids, naturally occurring and synthetic, are adrenocortical steroids that are readily absorbed from the gastrointestinal tract. Glucocorticoids cause varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli. Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have sodium‐retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analog including dexamethasone are primarily used for their anti‐inflammatory effects in disorders of many organ systems. Contraindicated in systemic fungal infections. |
Several adverse events (e.g. hyperglycaemia, fluid retention, hypokalaemic alkalosis, potassium loss, sodium retention) | DailyMed |
| Gabapentin | Gabapentin is an anticonvulsant. Gabapentin is contraindicated in patients who have demonstrated hypersensitivity to the drug or its ingredients. | Somnolence, dizziness, ataxia, fatigue, and nystagmus | DailyMed |
| Ginkgo biloba | This homeopathic product has not been evaluated by the Food and Drug Administration for safety or efficacy. FDA is not aware of scientific evidence to support homeopathy as effective. | ‐ | DailyMed |
| Methazolamide | Methazolamide is a potent inhibitor of carbonic anhydrase. Methazolamide therapy is contraindicated in situations in which sodium and/or potassium serum levels are depressed, in cases of marked kidney or liver disease or dysfunction, in adrenal gland failure, and in hyperchloraemic acidoses. In patients with cirrhosis, use may precipitate the development of hepatic encephalopathy. | Adverse reactions, occurring most often early in therapy, include paraesthesias, particularly a “tingling” feeling in the extremities; hearing dysfunction or tinnitus; fatigue; malaise; loss of appetite; taste alteration; gastrointestinal disturbances such as nausea, vomiting, and diarrhoea; polyuria; and occasional instances of drowsiness and confusion. | DailyMed |
| Nifedipine | It is a calcium channel blocker. Nifedipine must not be used in cases of cardiogenic shock. It is contraindicated in patients with a known hypersensitivity to any component of the tablet. |
Headache, flushing/heat sensation, dizziness, fatigue/asthenia, nausea | DailyMed |
| Phenytoin | Phenytoin sodium is an antiepileptic drug. Phenytoin is contraindicated in those patients who are hypersensitive to phenytoin or other hydantoins. | Central Nervous System (the most common manifestations encountered with phenytoin therapy are referable to this system and are usually dose‐related. These include nystagmus, ataxia, slurred speech, decreased coordination, and mental confusion), Gastrointestinal System ( nausea, vomiting, constipation, toxic hepatitis, and liver damage) |
DailyMed |
| Salmeterol | Long‐acting beta2‐adrenergic agonist Contraindicated in patients with asthma. It should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension. |
It increases the risk of asthma‐related death. Excessive beta‐adrenergic stimulation has been associated with seizures, angina, hypertension or hypotension, tachycardia with rates up to 200 beats/min, arrhythmias, nervousness, headache, tremor, palpitation, nausea, dizziness, fatigue, malaise, and insomnia. | DailyMed |
| Selective inhibitor of phosphodiesterase type 5 (taladafil and sildenafil) | It was shown to potentiate the hypotensive effects of nitrates, and its administration to patients who are using organic nitrates, either regularly and/or intermittently, in any form is therefore contraindicated. | Headache and flushing | DailyMed |
| Spironolactone | Aldactone oral tablets contain 25 mg, 50 mg, or 100 mg of the aldosterone antagonist spironolactone. Aldactone is contraindicated for patients with anuria, acute renal insufficiency, significant impairment of renal excretory function, or hyperkalaemia. |
Gynecomastia and hyperkalaemia | DailyMed |
| Sumatriptan | Sumatriptan is an agonist for a vascular 5‐hydroxytryptamine1 receptor subtype. It should not be given to patients with history, symptoms, or signs of Ischaemic cardiac, cerebrovascular, or peripheral vascular syndromes. | Serious cardiac events, including some that have been fatal. These events are extremely rare and most have been reported in patients with risk factors predictive of CAD. Events reported have included coronary artery vasospasm, transient myocardial ischemias, myocardial infarction, ventricular tachycardia, and ventricular fibrillation. | DailyMed |
| Theophylline | Theophylline is classified as a methylxanthine. Theophylline should be used with extreme caution in patients with the following clinical conditions due to the increased risk of exacerbation of the concurrent condition: active peptic ulcer disease, seizure disorders and cardiac arrhythmias (not including bradyarrhythmias). |
Nausea, vomiting, headache, and insomnia | DailyMed |
Appendix 4. MEDLINE (Ovid SP) search strategy
Brain edema/ or Pulmonary edema/ or ((edema or oedema) adj3 (high altitude or cerebral or pulmonary)).mp. or ((mountain or high altitude) adj3 (sickness or illness)).mp. or high altitude.ti,ab.
Exp Primary Prevention/ or exp Drug Therapy/ or (drug therap* or prevent* or acclimati?ation or nifedipine or dexamethasone or taladafil or sildenafil or theophylline or salmeterol or acetazolamide or aspirin or sumatriptan or gabapentin or phenytoin or magnesium or ginkgo biloba or ascorbic acid or alpha‐tocopherol acetate or alpha‐lipoic acid or beta‐carotene or selenium or zinc or bosentan or calcium channel blocker* or of phosphodiesterase type or nonsteroidal anti‐inflammatory drug* or steroid* or glucocorticosteroid* or corticosteroid* or non‐selective phosphodiesterase inhibitor* or carbonic anhydrase inhibitor* or beta agonist* or 5‐HT1 receptor agonist* or N‐methyl‐D‐aspartate antagonist* or antioxidant* or vitamin* or mineral* or endothelin antagonist*).mp.
((randomized controlled trial or controlled clinical trial).pt. or randomized.ab. or placebo.ab. or clinical trials as topic.sh. or randomly.ab. or trial.ti.) not (animals not (humans and animals)).sh.
1 and 2 and 3
Appendix 5. Embase (Ovid SP) search strategy
'brain edema'/exp
'lung edema'/exp
(edema OR oedema) NEXT/3 ('high altitude' OR 'altitude' OR 'cerebral' OR 'pulmonary')
('mountain' OR 'high altitude') NEXT/3 ('sickness' OR 'diseases' OR 'illness')
#1 OR #2 OR #3 OR #4
'primary prevention'/exp
'drug therapy'
'drug therap*'
'therap*'
'prevent*'
'acclimati?ation'
'nifedipine'
'dexamethasone'
'tadalafil'
'sildenafil'
'theophylline'
'salmeterol'
'acetazolamide'
'acetylsalicylic acid'
'aspirin'
'sumatriptan'
'gabapentin'
'phenytoin'
'magnesium'
'ginkgo biloba'
'ascorbic acid'
'alpha tocopherol'
'alpha‐tocopherol acetate'
'alpha‐lipoic acid'
'beta carotene'
'selenium'
'zinc'
'bosentan'
'calcium channel blocker*'
'phosphodiesterase type'
'nonsteroidal anti‐inflammatory drug*'
steroid*
glucocorticosteroid*
'non‐selective phosphodiesterase inhibitor*'
'carbonic anhydrase inhibitor*'
'beta agonist*'
'5‐ht1 receptor agonist*'
'n‐methyl‐d‐aspartate antagonist*'
antioxidant*
vitamin*
mineral*
'endothelin antagonist*'
#6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47
'randomized controlled trial'
'controlled clinical trial'
'controlled clinical trial (topic)'
#49 OR #50 OR #51
#5 AND #48 AND #52
#53 AND 'human'/de
#53 AND 'human'/de AND [embase]/lim NOT [medline]/lim
Appendix 6. CENTRAL search strategy
MeSH descriptor: [Brain Edema] explode all trees
MeSH descriptor: [Pulmonary Edema] explode all trees
(?edema near (high?altitude or cerebral or pulmonary)) or ((mountain or high?altitude) near (sickness or illness)) or high?altitude:ti,ab
(#1 or #2 or #3)
MeSH descriptor: [Secondary Prevention] explode all trees
MeSH descriptor: [Primary Prevention] explode all trees
MeSH descriptor: [Drug Therapy] explode all trees
(drug therapy or prevent* or acclimati?ation or nifedipine or dexamethasone or taladafil or sildenafil or theophylline or salmeterol or acetazolamide or aspirin or sumatriptan or gabapentin or phenytoin or magnesium or ginkgo biloba or ascorbic acid or alpha‐tocopherol acetate or alpha‐lipoic acid or beta‐carotene or selenium or zinc or bosentan or calcium channel blockers or selective inhibitor of phosphodiesterase type or nonsteroidal anti‐inflammatory drug* or steroid* or glucocorticosteroid* or corticosteroid* or non‐selective phosphodiesterase inhibitor* or carbonic anhydrase inhibitor* or beta agonist* or 5‐HT1 receptor agonist* or N‐methyl‐D‐aspartate antagonist* or antioxidant* or vitamin* or mineral* or endothelin antagonist*):ti,ab
(#5 or #6 or #7 or #8)
#4 and #9
Appendix 7. Search strategy for LILACS via BIREME interface
tw:(edema cerebral)) OR (tw:(edema pulmonar)) OR (tw:(edema))AND (tw:(enfermedad de altura)) OR (tw:(high‐altitude sickness)) OR (tw:(mal agudo de montaña)) OR (tw:(montaña enfermedad$)) OR (tw:(mal da montanha$)) OR (tw:(doença de alta altitude$)) OR (tw:(mal de altura*))
Appendix 8. WHO International Trials Registry Portal search
high‐altitude pulmonary edema
Recruitment Status: All
Appendix 9. Study eligibility screening and data extraction form.
Intervention for preventing high altitude illness
Study Selection, Quality Assessment & Data Extraction Form
| First author | Journal/Conference Proceedings etc | Year |
| |
Study eligibility
| RCT/Quasi/CCT (delete as appropriate) | Relevant participants | Relevant interventions | Relevant outcomes |
| Yes / No / Unclear |
Yes / No / Unclear |
Yes / No / Unclear |
Yes / No* / Unclear |
* Issue relates to selective reporting when authors may have taken measurements for particular outcomes, but not reported these within the paper(s). Reviewers should contact trialists for information on possible non‐reported outcomes & reasons for exclusion from publication. Study should be listed in ‘Studies awaiting assessment’ until clarified. If no clarification is received after three attempts, study should then be excluded.
| Do not proceed if any of the above answers are ‘No’. If study to be included in ‘Excluded studies’ section of the review, record below the information to be inserted into ‘Table of excluded studies’. |
| |
| Freehand space for comments on study design and treatment: |
References to trial
Check other references identified in searches. If there are further references to this trial link the papers now & list below. All references to a trial should be linked under one Study ID in RevMan.
| Code each paper | Author(s) | Journal/Conference Proceedings etc | Year |
| The paper listed above | |||
| Further papers | |||
Participants and trial characteristics
| Participant characteristics | |
| Further details | |
| Age (mean, median, range, etc) | |
| Sex of participants (numbers / %, etc) | |
| Country | |
| Other | |
| Rate of ascent (m/h) | |
| Final altitude reached (metres) | |
| AMS scale | |
| History of HAI | |
| Type of HAI reported | |
Intervention characteristics
| Intervention characteristics | |
| Further details | |
| Name | |
| Doses | |
| Administration route | |
| Time to administration | |
| Duration | |
If RCT included a combination:
| Intervention characteristics | |
| Further details | |
| Name | |
| Doses | |
| Administration route | |
| Time to administration | |
| Duration | |
If RCT included acclimatization:
| Intervention characteristics | |
| Rate of ascent (m/h) | Further details |
Methodological quality
| Allocation of intervention | |
| State here method used to generate allocation and reasons for grading | Grade (circle) |
| |
Low risk of bias (Random) |
| High risk of bias (e.g. alternate) | |
| Unclear | |
|
Concealment of allocation Process used to prevent foreknowledge of group assignment in a RCT, which should be seen as distinct from blinding | |
| State here method used to conceal allocation and reasons for grading | Grade (circle) |
| Low risk of bias | |
| High risk of bias | |
| Unclear | |
| Blinding | |
| Person responsible for participants care | Yes / No |
| Participant | Yes / No |
| Outcome assessor | Yes / No |
| Other (please specify) | Yes / No |
|
Intention‐to‐treat An intention‐to‐treat analysis is one in which all the participants in a trial are analysed according to the intervention to which they were allocated, whether they received it or not. | |
| All participants entering trial | |
| 15% or fewer excluded | |
| More than 15% excluded | |
| Not analysed as ‘intention‐to‐treat’ | |
| Unclear | |
| Free selective report | |
| State here method used to generate allocation and reasons for grading | Grade (circle) |
| |
Low risk of bias |
| High risk of bias | |
| Unclear | |
Were withdrawals described? Yes ? No ? not clear ?
Discuss if appropriate
Data extraction
|
Outcomes relevant to your review Copy and paste from ‘Types of outcome measures’ | |
| Reported in paper (circle) | |
| Incidence of AMS (headache, nausea, insomnia, dizziness, and sleep disorder) | Yes / No |
| Incidence of HACE. | Yes / No |
| Incidence of HAPE. | Yes / No |
| Safety of adverse events | Yes / No |
| Safety (adverse drug reaction) | Yes / No |
| For Dichotomous data | |||
| Code of paper | Outcomes | Intervention group (n) n = number of participants, not number of events |
Control group (n) n = number of participants, not number of events |
| A | Incidence of AMS ((headache, nausea, insomnia, dizziness, and sleep disorder) | ||
| Incidence of HACE. | |||
| Incidence of HAPE | |||
| Safety of adverse events | |||
| Safety (adverse drug reaction) | |||
|
Other information which you feel is relevant to the results Indicate if: any data were obtained from the primary author; if results were estimated from graphs etc; or calculated by you using a formula (this should be stated and the formula given). In general if results not reported in paper(s) are obtained this should be made clear here to be cited in review. |
| |
| Freehand space for writing actions such as contact with study authors and changes |
References to other trials
| Did this report include any references to published reports of potentially eligible trials not already identified for this review? | ||
| First author | Journal / Conference | Year of publication |
| Did this report include any references to unpublished data from potentially eligible trials not already identified for this review? If yes, give list contact name and details | ||
| | ||
| Trial characteristics | |
| Further details | |
| Single centre / multicentre | |
| Country / Countries | |
| How was participant eligibility defined? |
|
| How many people were randomized? | |
| Number of participants in each intervention group | |
| Number of participants who received intended treatment | |
| Number of participants who were analysed | |
| Drug treatment(s) used | |
| Dose / frequency of administration | |
| Duration of treatment (State weeks / months, etc, if cross‐over trial give length of time in each arm) | |
| Median (range) length of follow‐up reported in this paper (state weeks, months or years, or if not stated) | |
| Time‐points when measurements were taken during the study | |
| Time‐points reported in the study | |
| Time‐points you are using in RevMan | |
| Trial design (e.g. parallel / cross‐over*) | |
| Other | |
Appendix 10. Transformation of numerical data‐ Secondary outcome: Differences in HAI/AMS scores
| Study | Original data | Transformed data | Original data | Transformed data | Original data | Transformed data | Original data | Transformed data |
| Bates 2011 | Median = 4 | Mean = 4 | IQR = 2 ‐ 6 | SD = 3.19 | Median = 6.5 | Mean = 6.41 | IQR = 5 ‐ 7.75 | SD = 2.11 |
| Bernhard 1994 | SEM = 3.6 | SD = 11.94 | SEM = 4.8 | SD = 16.63 | ‐ | ‐ | ‐ | ‐ |
| Chow 2005 | Median = 2 | Mean = 2.25 | RANGE = 0 ‐ 5 | SD = 1.28 | Median = 4 | Mean = 5.5 | RANGE = 1 ‐ 13 | SD = 3.11 |
| Chow 2005 | Median = 4 | Mean = 4.75 | RANGE = 1 ‐ 10 | SD = 2.38 | ‐ | ‐ | ‐ | ‐ |
| Hackett 1988 | SEM = 0.6 | SD = 1.58 | SEM = 1.0 | SD = 2.82 | ‐ | ‐ | ‐ | ‐ |
| Hillenbrand 2006 | Median = 1.0 | Mean = 0.83 | IQR = 0 ‐ 1, 5 | SD = 1.12 | Median = 1.0 | Mean = 0.66 | IQR = 0 ‐ 1.0 | SD = 0.74 |
| Hohenhaus 1994 | SE = 2.88 | SD = 7.05 | SE = 1.1 | SD = 4.12 | SE = 1.1 | SD = 3.97 | ‐ | ‐ |
| Hussain 2001 | SE = 0.33 | SD = 1.32 | SE = 3.04 | SD = 7.45 | SE = 1.26 | SD = 3.09 | SE = 1.58 | SD = 3.87 |
| Rock 1989a | SE = 0.14 | SD = 0.59 | SE = 0.31 | SD = 1.24 | ‐ | ‐ | ‐ | ‐ |
| Rock 1989b | SE = 0.37 | SD = 1.48 | SE = 0.11 | SD = 0.47 | ‐ | ‐ | ‐ | ‐ |
| Rock 1989c | SE = 00.5 | SD = 1 | SE = 0.33 | SD = 1.32 | ‐ | ‐ | ‐ | ‐ |
| Wright 1983 | SEM = 8 | SD = 19.59 | SE = 7 | SD = 22.14 | ‐ | ‐ | ‐ | ‐ |
Data and analyses
Comparison 1. Carbonic anhydrase inhibitors: acetazolamide versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of acute mountain sickness | 16 | 2301 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.39, 0.56] |
| 1.1 Acetazolamide 250 ‐ 255 mg | 4 | 855 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.39, 0.94] |
| 1.2 Acetazolamide 500 mg | 8 | 1111 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.38, 0.61] |
| 1.3 Acetazolamide 750 mg | 2 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.18, 0.62] |
| 1.4 Other combinations | 2 | 255 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.17, 0.55] |
| 2 Incidence of high altitude pulmonary oedema | 7 | 1138 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Incidence of high altitude cerebral oedema | 6 | 1126 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.01, 7.48] |
| 4 Incidence of adverse events: Paraesthesia | 5 | 789 | Risk Ratio (M‐H, Random, 95% CI) | 5.53 [2.81, 10.88] |
| 4.1 Acetazolamide 250 mg | 1 | 197 | Risk Ratio (M‐H, Random, 95% CI) | 12.63 [4.02, 39.64] |
| 4.2 Acetazolamide 500 mg | 3 | 370 | Risk Ratio (M‐H, Random, 95% CI) | 6.72 [3.94, 11.46] |
| 4.3 Acetazolamide 750 mg | 1 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 3.09 [2.00, 4.78] |
| 5 Differences in HAI/AMS scores | 6 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 5.1 acetazolamide 250 mg | 3 | Std. Mean Difference (Random, 95% CI) | 0.19 [0.01, 0.37] | |
| 5.2 acetazolamide 500 mg | 4 | Std. Mean Difference (Random, 95% CI) | ‐0.57 [‐1.20, 0.07] |
Comparison 2. Steroids: budesonide vs. placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of acute mountain sickness | 2 | 132 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.23, 0.61] |
Comparison 3. Steroids: dexamethasone vs. placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of acute mountain sickness | 4 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.36, 1.00] |
| 2 Differences in HAI/AMS scores | 3 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐1.21, 0.29] |
Comparison 4. Calcium modulators: nifedipine vs. placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Differences in HAI/AMS scores | 2 | 48 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐1.85, 0.74] |
Comparison 5. NSAIDs and other analgesic: aspirin vs. placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of AMS | 2 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.06, 1.95] |
Comparison 6. NSAIDs and other analgesic: ibuprofen vs. placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incidence of acute mountain sickness | 3 | 598 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.49, 0.82] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Anonymous 1981.
| Methods | 1. Design: Parallel, 2 arms 2. Country: Ecuador 3. Multisite: No 4. International: No 5. Treatment duration: 3 days 6. Follow‐up: 8 days 7. Rate of ascent: unclear 8. Final altitude reached: 5000 metres 9. AMS scale: clinical arbitrary score (0 ‐ 100) 10. Randomization unit: participants 11. Analysis unit: Groups |
|
| Participants | 1. 20 participants enrolled (age 20 ‐ 52 , all normally resided at less than 200 metres, all medically qualified) Randomized to: Acetazolamide group (n = 10, 50%) Placebo group (n = 10, 50%) 2. No participant randomized was excluded 3.No participant was lost to follow‐up 4. Main characteristics of participants: Age: 20 ‐ 52 years 100% men History of AMS: not stated Percentage/number type of HAI reported: not reported |
|
| Interventions | 1. Acetazolamide group: acetazolamide 500 mg/day for 3 days, oral 2. Placebo group (control): unclear |
|
| Outcomes | This RCT did not specify its primary or secondary outcomes 1. Assesment of Acute Mountain Sickness by clinical interview: arbitrary scores (0 ‐ 100) 2. Peer review: rank order according to subjective impression 3. Blood gas measurements included: hydrogen ion concentration, oxygen tension and carbon dioxide tension |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Boehringer ingelheim ltda. Financial Mathematics Ltd. Geigy pharmaceuticals, laboratoire dëtude de recherches scientifiques lederle phamaceuticals, the Arthur Thompson Trust fund and West Midlands Regional Health Huthority and many other companies that gave financial aid 3. Role of Funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "...were randomly allocated..." (Page 181) The method of sequence generation was not specified |
| Allocation concealment (selection bias) | Unclear risk | The method of sequence generation was not specified |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote "Details of medication were concealed until after descent" (Page 181) There was insufficient information to assess whether blinding was likely to introduce bias in the results |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were reported as lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Unclear risk | Possible industry bias. The trial is sponsored by the industry or has received other kind of for‐profit support |
ASCENT 2012.
| Methods | 1. Design: A randomized, doubled‐blind, placebo‐controlled trial. 2 arms: placebo group, ibuprofen group 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: 1 day 6. Intention‐to‐treat: Yes 7. Follow‐up: 1 day after arrival 8. Rate of ascent: unclear 9. Final altitude reached: 4928 metres 10. AMS scale: Lake Louise AMS questionnaire (LLQ) |
|
| Participants | 1. 294 participants enrolled, 183 completed the entire protocol. 49 broke protocol, but allowed data collection; at the end 62 participants were lost to follow‐up 2. 232 participants completed the study. (Healthy men and women, 37 ± 12 years), recruited at 4280 or 4358 metres on the Everest approach: Placebo (109, 47%) Ibuprofen (123, 53%) 3. Main characteristics of participants: Age 36 ± 11 (placebo) 38 ± 12 (ibuprofen) Number/Percentage of women: 35 (32.4%) placebo, 46 (37.7%) ibuprofen Percentage/number history of AMS: 5/109 (4.7% placebo) 7/123 (5.8% ibuprofen) Percentage/number type of HAI reported: This study reported: Severe high altitude headache (HAH), evaluated by LLQ > 2: 16/109 (14.7% placebo) 6/123 (4.9% ibuprofen) AMS incidence evaluated by LLQ > 3: 44/109 (40.4% placebo), 30/123 (24.4% ibuprofen) |
|
| Interventions | 1. Placebo group: placebo 3 times daily orally for at least 3 doses before ascent 2. Ibuprofen group: 600 mg of ibuprofen 3 times a day orally for at least 3 doses before ascent 3. In both groups there was a period of acclimatization, approximately 3.4 ± 0.8 nights |
|
| Outcomes | Primary outcome 1. Incidence of headache, severe headache, AMS, severe AMS. Measured by a value of 2, 3 or 5 respectively on the LLQ Secondary endpoint 1. SpO2 decreased from baseline (end point SpO2%) |
|
| Notes | 1. Trial Registration “Not stated” 2. Funder: Wellcome Trust UK 3. Role of Funder: Financial support 4. A priori sample size estimation: Yes, 164 participants (84 per arm) 5. Conducted: Enrolment took place between October and November 2009; start date not specified or when the study ended 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Study medications were randomized via computer‐generated code" (Page 308) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 21% of participants randomized were not analysed (62 participants). A modified ITT analysis was performed |
| Selective reporting (reporting bias) | Low risk | Selective reporting of information was not detected |
| Other bias | Low risk | No additional biases were identified |
Banderet 1977.
| Methods | 1. Design: Paralell longitudinal study, 2 arms 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: 3 weeks 7. Rate of ascent: unclear 8. Final altitude reached: 4300 metres 9. AMS scale: The Clyde Mood Scale and the High Altitude Symptom Questionnaire 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 35 participants enrolled (volunteers) Randomized to: Treatment group (n = 18, 51%) Placebo group (n = 17, 49%) Main characteristics of participants: Age: 19 ‐ 28 years women/men: n = 16 / 19 History of AMS: none |
|
| Interventions | 1. Treatment group (intervention): acetazolamide 500 twice a day during last 2 days of staging at 1600 metres and during the first 2 days at 4300 metres 2. Placebo group (control): placebo 2 tablets twice a day each day throughout the study |
|
| Outcomes | This trial did not specify by primary or secondary outcomes Scores of Clyde Mood Scale (by symptom) |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Subjects were assigned randomly…” (Page 20) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Quote: “Subjects were assigned randomly…” (Page 20) Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: “All were informed initially that some of them would receive placebo tablets" (Page 23) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Important participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Bartsch 1991.
| Methods | 1. Design: Parallel (2 arms) 2. Country: Italy 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: unclear 7. Rate of ascent: 155 metres/hour 8. Final altitude reached: 4559 metres 9. AMS scale: AMS score 10. Randomization unit: participants 11. Analysis unit: 2roup |
|
| Participants | 21 participants enrolled (mountaineers who had radiographically‐documented episodes of high‐altitude pulmonary oedema and who had continued alpine‐style climbing to peaks above 4000 metres after there episodes of HAPE) Randomized to: Nifedipine (n = 10, 47.6%) Placebo (n = 11, 52.3%) 6 participants left the study early 1 person in placebo group left because of high‐altitude pulmonary oedema on day 2 3 people in placebo group left because of high‐altitude pulmonary oedema on day 3 1 person left the trial on the day of arrival at 4559 metres because of prodromal symptoms of pulmonary oedema 4. Main characteristics of participants: Age (mean, range): placebo group 41 years, 20 ‐ 58; nifedipine group 44 years, 23 ‐ 62 Number of women/men: 1 / 20 Number of participants with 1 episode of HAPE: 6 placebo and 6 nifedipine |
|
| Interventions | 1. Nifedipine group: administration of slow‐release preparation of nifedipine (Adalat, 20 mg) given at 10 p.m. on the third and second days before the ascent and at 8 a.m. and 10 p.m. on the day before. Starting on the day of the ascent the medication was taken 3 times daily (at 6 a.m., 2 p.m. and 10 p.m.) 2. Placebo group (control): capsules taken orally 3 times daily for 4 days |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. Presence of HAPE (documented by doppler. Susceptible mountaineers with documented histories of high‐altitude pulmonary oedema) 2. AMS score by clinical examination 3. Blood and end expiratory gas analysis: SaO2, PaO2, PaCO2, end exploratory PO2 |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: supported from the Swiss National Science Foundation 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote " ...was assigned randomly.." (Page 1285) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The clinical examination were directed toward the signs and symptoms of AMS, and were always performed by the same investigator, who was not aware of the subjects medication" (Page 1285) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 5/11 placebo participants were not included in analyses of AMS scores at 4559 metres |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Basnyat 2003.
| Methods | 1. Design: Parallel, 2 arms 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment : 2 or 3 days 6. Follow‐up: unclear 7. Rate of ascent:4.3 ± 1.1 days (range 3 ‐ 6) 8. Final altitude reached: 4937 metres 9. AMS scale: The Lake Louise Acute Mountain Sickness Scoring System 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 197 participants enrolled (healthy non‐Nepali male and female trekkers of > 18 years of age travelling between the villages from 4243 metres to 4937 metres) Exclusion criteria: Already had a diagnosis of AMS, HACE or HAPE; Had been on a high‐altitude trek 2 weeks prior to this trek; Were not trekking directly to 4937 metres; Had taken acetazolamide or ginkgo biloba in the week prior to presentation; Has diabetes, serious heart or pulmonary disease or a sulfa allergy Randomized to: Acetazolamide (n = 96, 48.7%) Placebo (n = 101, 51.2%) 2 . 42 participants lost at follow‐up (they did not retrieve the questionnaire at Lobujr): Acetazolamide group (n = 22, 22.9%) Placebo group (n = 20, 19.8%) 3. Main characteristics of participants : Age (mean; SD): acetazolamide group 35.8 ± 12.1; placebo group 33.9 ± 11.4 Percentage women/men: acetazolamide group 64.9% men/35.1% women; placebo group 69.1% men/30.9% women O2 saturation at Periche: Acetazolamide group: 86.9 ± 3.9; placebo group: 86.9 ± 4 |
|
| Interventions | 1. Acetazolamide group (intervention): acetazolamide 125 mg twice daily for 2 to 3 days before the final evaluation at 4937 metres 2. Placebo group (control): visually‐matched placebo twice daily for 2 to 3 days before the final evaluation at 4937 metres Cointerventions: None stated |
|
| Outcomes | Primary outcome: 1. Incidence and severity of AMS by the LLQ Score at Lobuje Secondary outcomes: 1. The presence or absence of high‐altitude headache 2. Diagnosis of HAPE or HACE 3. Pulse oximetry differential between 4243 metres and 4937 metres 4. Acute symptoms suggestive of infection at 4937 metres (sore throat, cough, sinusitis, diarrhoea) 5. Incidence of paraesthesias 6. Missed capsules |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: The Himalayan Rescue Association and Nepal International Clinic, Kathmandu, Nepal; and Deurali Pharmaceutical Company 3. Role of funder: Donated the placebo capsules. Study administrators paid their own expenses 4. A priori sample size estimation: No 5. Conducted: November 1 to 22 of 2001 6. Declared conflicts of interest: Yes, Page 52 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote " Random allocation occurred on site, ..." (Page 47). The method of sequence generation was not specified |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization code was drawn up by a neutral party and was securely kept in Katmandu, completely unavailable to the study administrators" Page 47 |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote " ...were visually indistinguishable, and neither study administrators nor participants knew the identity of the study capsules" (Page 47) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The results were likely to be biased due to missing data
|
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Low risk | No additional biases were identified |
Basnyat 2008.
| Methods | 1. Design: Parallel ‐ 2 arms 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: unclear 7. Rate of ascent: 36 hours to a maximum of 96 hours 8. Final altitude reached: 5000 metres 9. AMS scale: LLQ 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 364 healthy people were enrolled between the ages of 18 and 65, non‐Nepali, without AMS or any concurrent illness, and not already taking acetazolamide or any other drug for the prevention of altitude illness Exclusion criteria: Mild AMS; significantly depressed oxygen saturation; women know to be pregnant or unable to exclude the possibility of being pregnant. or having missed menses by over 7 days; individuals with a known drug allergy to acezalomide or other sulfa drugs; individuals who had spent 24 hours at altitude of 4500 metres or higher within the last 9 days; anyone know to have taken any of the following in the last 2 days: acetazolamide, steroids, theophyline or diuretics; individuals who had known intracranial space‐occupying lesions or a history of elevated intracranial pressure Randomized to: Acetazolamide group (n = 187; 51.3%) Placebo group (n = 177; 48.6%) 25 patients randomized were excluded due to: Dropped out or disqualified for stopping study drugs or taking non‐study acetazolamide Acetazolamide group (n = 13; 6.9%) Placebo group (n = 12; 6.7%) 3. Main characteristics of participants : Age (mean, SD): acetazolamide 37.9 ± 12.5; placebo 39.4 ± 12.1 Percentage/number of women/men: acetazolamide: women 42.2% (79), men 57.8% (108); placebo: women 32.2% (57), men 67.8% (120) Percentage/number history of AMS: acetazolamide: 36.4% (68), placebo; 39.5% (70) Percentage/number Type of HAI reported: placebo 21.9%, acetazolamide group 10.2% Pulse oximetry (mean, SD): acetazolamide = 86.45 ± 3.39; placebo = 85.91 ± 4.08 Heart rate (mean, SD): acetazolamide = 82.6 ± 12; placebo = 82.5 ± 12 |
|
| Interventions | 1. Acetazolamide group (intervention) = acetazolamide tablets 250 mg twice day for 4 days 2. Placebo group (control) = visually identical‐appearing placebo tablets twice day for 4 days |
|
| Outcomes | Primary outcomes: 1. HAPE diagnosis (signs and symptoms): AMS (LLS ≥ 3, at least 1 symptom) + 2 signs and 2 symptoms of pulmonary involvement Determination of pulmonary artery systolic pressure Secondary outcomes 1. Pulse oxygen saturation of < 70% in participants meeting HAPE diagnosis 2. Incidence of AMS, HAPE and HACE |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Sonosite Micromaxx, Wellcome Trust of Great Britain 3. Role of funder: Provision of ultrasonographer 4. A priori sample size estimation: Yes.(Page 211) 5. Conducted: October and November, 2006 6. Declared conflicts of interest: Yes (Page 215) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " Computer generated randomization of commercial pharmaceutical grade acetazolamide and placebo were carried out by Deuralu Janata pharmaceuticals" (Page 210) |
| Allocation concealment (selection bias) | Low risk | 3 sealed master lists of the randomization code were held by the manufacturer and independent clinicians. Only opened by an independent clinician when there was a concern (Page 211) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The code was only to be opened during the trial by an independent clinician who was not a study author when there was concern of allergic reaction or any other adverse event (...)" (Page 211) Study drug and placebo had a visually identical appearance (Page 210) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data were unlikely to make treatment effects depart from plausible values Loss to follow‐up in experimental group: 6.95% (13/187) Loss to follow‐up in control group: 6.77% (12/177) |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Basu 2002a.
| Methods | 1. Design: Parallel, 5 arms 2. Country: India 3. Multisite: No 4. International: No 5. Treatment duration: 5 days 6. Follow‐up: 7 days 7. Rate of ascent: unclear 8. Final altitude reached: 3450 metres 9. AMS scale: Lake Louise AMS scoring system 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 50 healthy men enrolled (none of them taking any medication and had not taken steroid preparations; excluded if any disorders or contraindication to steroid therapy) Patients randomized to: Group I (n = 10 , 20%) Group II (n = 10, 20%) Group III (n = 10, 20%) Group IV (n = 10, 20%) Group V (n = 10, 20%) Unclear if any people were excluded Unclear if participants were lost to follow‐up (See Table 2, only 9 participants in dexamethasone group) Main characteristics of participants: Age: 19 ‐ 24 years for all participants Percentage of men: 100% Body weight: 55 ‐ 70 kg History of AMS: Not stated |
|
| Interventions | 1. Group I (intervention): prednisolone 10 mg, oral single dose a day for 5 days 2. Group II (intervention): prednisolone 20 mg oral single dose a day for 5 days 3. Group III (intervention): prednisolone 40 mg oral single dose a day for 5 days 4. Group IV (intervention): dexamethasone IV 0.5 mg dose a day for 5 days 5. Group V (control): placebo once a day in the morning at 08:00 hours before breakfast Coninterventions: None declared |
|
| Outcomes | This RCT did not specify by primary or secondary outcomes 1. Symptoms of AMS. Score of AMS 2. Physiological variables: BP, SaO2, heart rate 3. Hormonal estimations: cortisol and ACTH |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5.Declared conflicts of interest: Not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "...randomized trial..." (Page 762) The method of sequence generation was not specified |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias Quote "The placebo and drugs looked alike..." (Page 762) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Basu 2002b.
| Methods | 1. Design: Randomized placebo controlled trial 2. Country: India 3. Multisite: No 4. International: No 5. Treatment duration: unclear 6. Follow‐up: followed over 1 week at high altitude and 2 weeks on return to sea level 7. Rate of ascent: 3450 metres by air 8. Final altitude reached: 3450 metres 9. AMS scale: Lake Louise AMS scoring system 10. Randomization unit: Participants 11. Analysis unit: Group |
|
| Participants | 40 participants enrolled. Those selected had no contraindication to steroid therapy and had not taken any steroid preparations within the preceding year Randomized to: 20 prednisolone (50%) Group I 20 placebo (50%) Group II Number randomized who were excluded: not reported Participants lost to follow‐up: not reported Main characteristics of participants: Age: 19 ‐ 26 years Percentage/number of women/men: 40 men (100%) Percentage/number history of AMS: In placebo group 11 participants showed AMS prednisolone group unclear |
|
| Interventions | Group I: received prednisolone 20 mg Group II: received placebo Once a day at 8:00 a.m. before breakfast for 2 days prior to induction, and for 3 days on arrival at high altitude |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. AMS scores 2. Circulatory levels of ACTH, cortisol, epinephrine and norepinephrine |
|
| Notes | 1.Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Unclear 6. Declared conflicts of interest: No reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The subjects were randomly divided into two groups of twenty each." (Page 319) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No participants were reported as lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such adverse events, were not reported |
| Other bias | Unclear risk | No additional biases were identified |
Bates 2011.
| Methods | 1. Design: Parallel design, 2 arms 2. Country: Bolivia 3. Multisite: No 4. International: No 5. Treatment duration: 12 days 6. Follow‐up: 12 days 7. Rate of ascent: unclear 8. Final altitude reached: 5200 metres 9. AMS scale: Lake Louise Consensus Symptom Score 10. Randomization unit: participant 11. Analysis unit: participant |
|
| Participants | This trial was conducted concurrently with a similar trial of an oral antioxidant vitamin supplement, addressing
a different aspect of altitude illness (information not included in this review) 62 healthy native lowlanders Randomized to: Sildenafil 20 (32.3%) Placebo 42 (67.7 %) 1 participant in the placebo group developed HAPE while at 3650 metres, did not ascend to the high altitude laboratory, and was excluded from the trial. Throughout the trial, it proved technically impossible to obtain satisfactory PASP measurements from 7 participants (all from the placebo group) and they were excluded from all the PASP analyses. 12 more participants were evacuated from the high altitude laboratory because of severe symptoms of AMS and thereby withdrew from the trial (5 in the sildenafil group and 7 in the placebo group). PASP and AMS data for these participants were included until their evacuation. 8 further individual PASP measurements (all at 5200 metres, 2 in the sildenafil group, 6 in the placebo group) were rejected as technically unsatisfactory following independent review after the expedition. All AMS data and PASP data from these participants at different time points are included in the analysis Main characteristics of participants: Male: placebo: 62% (26/42), sildenafil 55% (11/20) Age mean: placebo 21.5 ± 2.7 years, sildenafil 21.2 ± 3 years History of AMS: Not stated |
|
| Interventions | Sildenafil Citrate group (intervention): 50 mg/day before ascending, then 50 mg/3 times a day orally, during trek Placebo group: Unclear |
|
| Outcomes | Primary outcomes: PASP assessed by transthoracic echocardiography at 6 hours, 3 days, and 1 week following high‐altitude exposure at 5200 metres Secondary outcomes were oxygen saturations by pulse oximetry, severity of AMS using the LLS for the first 7 days at high altitude, and proportion of participants with LLS > 3 on day 2 at 5200 metres |
|
| Notes | 1. Trial Registration: NCT00627965 2. Funder: None 3. A priori sample size estimation: Stated on page 209 4. Conducted: Not stated 5. Declared conflicts of interest: No, stated on page 213 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “All 103 Apex 2 expedition participants were randomly assigned to three groups using a computer programme operated by an independent statistician, as determined…” (Page 208) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “All researchers and participants were unaware of the group assignments and independent of the individual responsible for the randomization process” “Supplies of sildenafil and masked placebo were obtained directly from the manufactures. Packs of these tablets were identically packaged in the UK under the supervision of the head of clinical trial facility, and distributed to the trial participants for personal administration.” (Page 208) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8 participants lost to follow‐up at day 2 (13%) |
| Selective reporting (reporting bias) | High risk | Patient‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Baumgartner 2003.
| Methods | 1. Design: Parallel, 2 arms 2. Country: Switzerland 3. Multisite: No 4. International: No 5. Treatment duration: 7 days 6. Follow‐up: 6 hours 7. Rate of ascent: unclear 8. Final altitude reached: 4559 metres (hypobaric chamber) 9. AMS scale: Environmental Symptom Questionnaire of Sampson 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 20 participants enrolled (Healthy white men living at altitudes below 500 metres. Men with a history of migraine or other headaches were not included) Randomized to: Flunarizine (10, 50%) Placebo (10, 50%) No participants lost to follow‐up: Main characteristics of participants: Mean age (SD; range) = 24 (4. 20 to 35) |
|
| Interventions | 1. Flunarizine group (intervention): 2 tablets of flunarizine 5 mg daily for 7 days 2. Placebo group (control): 2 tablets of placebo 5 mg daily for 7 days, identical form, colour and weight as intervention Cointerventions: Not stated |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. Assessment of HAH and symptoms of AMS 2. Static posturography 3. Memory test. 4. BP and SaO2 measurements |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: “The trial medication consisted of two tablets containing 5 mg of flunarizine or two tablets of identical form, colour and weight containing placebo” (Page 334) Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Bernhard 1994.
| Methods | 1. Design: Paralell, 2 arms 2. Country: Bolivia 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: Unclear 7. Rate of ascent: unclear 8. Final altitude reached: 5334 metres 9. AMS scale: Modified Enviromental Symptom Questionnaire 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 23 participants enrolled (healthy lowland‐living volunteers interested in high‐altitude research) Exclusion criteria: People who had been to high altitude 4 weeks prior to study; prior history of any chronic medical conditions including peptic ulcer disease, psychiatric illness or sensitivity to dexamethasone Randomized to: Dexamethasone (n = 11, 48%) Placebo (n = 12, 52%) No participants lost to follow‐up Main characteristics of participants: Age (mean, SEM ): dexamethasone 43 ± 3.9 years. placebo 32 ± 1.6 years Number of women/men: 15 women / 8 men History of AMS: 40% experienced mild to moderate AMS at altitudes less than 4000 metres |
|
| Interventions | 1. Dexamethasone group (intervention): dexamethasone capsules 4 mg every 12 hours orally for 4 days 2. Placebo group (control): placebo capsules 4 mg every 12 hours orally for 4 days (identical capsules to intervention) 3. Cointervention: None declared |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. AMS definition 1: Presence of at least 3 cerebral symptoms with a minimum of 1 symptom at intensity score > 2 2. AMS: definition 2: Scores > 0.7 for AMS‐C and 0.6 for AMS‐R 3. SaO2 and heart rate 4. Side effects |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Dr Clark Watts, Organon Inc and Nellcor Inc 3. Role of funder: Not stated; pharmaceutical supplies 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: “Subjects were randomly assigned to receive identical capsules of either dexamethasome 4 mg or placebo…” (Page 333) Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Possible industry bias: “The authors gratefully acknowledge…Organon Inc, for pharmaceutical supplies” (Page 338) |
Bernhard 1998.
| Methods | 1. Design: Paralell, 2 arms 2. Country: Bolivia 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: Unclear 7. Rate of ascent: unclear 8. Final altitude reached: 5334 metres 9. AMS scale: Modified Environmental Symptom Questionnaire. 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 13 participants enrolled (healthy volunteers, none of them normally resident at altitudes above 2000 metres, none of them had been to high altitude during the 4 weeks prior to the ascent) Randomized to: Dexamethasone + acetazolamide group (n = 6, 47%) Placebo + acetazolamide group (n = 7, 53%) No participant was lost to follow‐up Main characteristics of participants: Age (mean, SE ): dexamethasone + acetazolamide 42 ± 4.7 years. placebo + acetazolamide 44 ± 3.1 years Number of women/men: 9 men + 4 women: dexamethasone + acetazolamide 4 men + 2 women; placebo + acetazolamide 5 men + 2 women 50% of participants had experienced mild to moderate AMS |
|
| Interventions | 1. Dexamethasone group (intervention): dexamethasone capsules 4 mg twice a day and sustained 500 mg acetazolamide given once daily for 4 days 2. Placebo group (control): placebo (identical capsules ton dexamethasone) and sustained 500 mg acetazolamide capsules given once daily for 4 days 3. Cointerventions: Not stated |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. AMS definition 1: Presence of at least 3 cerebral symptoms with a minimum of 1 symptom having an intensity score of > 2 2. AMS definition 2: Scores > 0.7 for AMS‐C and 0.6 for AMS‐R 3. SaO2 and heart rate |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Using a randomized number system, subjects were assigned to two groups…” (Page 884) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Both researchers and subjects were blinded as to type of medication given” (Page 884) “… and a placebo in capsules identical to those used for the dexamethasone” (Page 884) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Bradwell 1986.
| Methods | 1. Design: Paralell, 2 arms 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: Unclear 6. Follow‐up: Unclear 7. Rate of ascent: 5 ‐ 10 miles per day 8. Final altitude reached: 4846 metres 9. AMS scale: Unclear (usual clinical criteria) 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 21 participants enrolled (all normally resident at < 200 metres, none was acclimatized to high altitude, and all were in good general health) Randomized, after being stratified by age and sex, to: Acetazolamide group (n = 11, 52.3%) Placebogroup (n = 10, 47.6%) Unclear number of participants were excluded: "These people and others who missed a test were excluded from the relevant analyses" (Page 1002) Unclear if participants were lost to follow‐up Main characteristics of participants: Age (Range): 22 ‐ 56 years Number of women/men:19 men and 2 women 12 had been on previous expedition |
|
| Interventions | 1. Acetazolamide group (intervention): Release capsules 500 mg. No further details were provided 2. Placebo group (control): No details were provided 3. Cointerventions: Not stated |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. Exercise performance tests 2. Tissue measurements 3. Blood gas measurements 4. AMS scores (unclear information) |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Wellcome Trust, Wyeth Laboratories, the Arthur Thompson Trust, Birmingham Regional Health Authority, the Samuel Scott Trust, The Royal Society, the Physiological society, Squibb Medical supplies, Lederle Laboratories, among others 3. Role of funder: Not stated 5. A priori sample size estimation: No 6. Conducted: Not stated 7. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “ At Kathmandu, subjects were randomized to acetazolamide or placebo by an independent observer after he had stratified them by age and sex” (Page 1002) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Quote: “ At Kathmandu, subjects were randomized to acetazolamide or placebo by an independent observer after he had stratified them by age and sex” (Page 1002) Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “ At Kathmandu, subjects were randomized to acetazolamide or placebo by an independent observer after he had stratified them by age and sex” (Page 1002) “Details of medication were concealed from all subjects until treatment was withdrawn” (Page 1002) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear if participants were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Unclear risk | Possible industry bias: “We thank … Wyeth laboratories… Squibb medical supplies, Lederle Laboratories, and many other societies and companies for grants ” (Page 1005) |
Burki 1992.
| Methods | 1. Design: Parallel design, 2 arms 2. Country: Pakistan (Karakorum Mountain) 3. Multisite: No 4. International: No 5. Treatment duration: 1 day 6. Follow‐up: 4 days 7. Rate of ascent: 491.5 metres/hour 8. Final altitude reached: 4450 metres 9. AMS scale: Clinical observation: Evaluation of dizziness, nausea/vomiting and headache on a scale of 0 to 2 10. Randomization unit: participant 11. Analysis unit: participant |
|
| Participants | 12 healthy men signed informed consent Randomized to: Acetazolamide: 6 (50%) Ascorbic acid: 6 (50%) 1 person in placebo group was excluded due to severe mountain sickness No losses to follow‐up reported Main characteristics of participants Age: Acetazolamide: 20.2 ± 1.5, placebo: 20.7 ± 1,4 History of AMS: Not stated |
|
| Interventions | Acetazolamide 250 mg twice daily at sea level (518 metres) Visually identical ascorbic acid 500 mg twice daily at sea level |
|
| Outcomes | Main outcomes were ventilatory response measured at sea level before and after taking the allocated drug, then another 2 measures were taken at 32 and 56 hours later at 4450 metres | |
| Notes | 1. Trial Registration: Not reported 2. Funder: Not stated 3. A priori sample size estimation: Not stated 4. Conducted: Unclear 5. Declared conflicts of interest: Not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “The subjects were randomly divided into two groups…” (Page 736) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Quote: “The subjects were randomly divided into two groups…” (Page 736) Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: “The subjects were given either the placebo tablets… or acetazolamide tablets… in a double‐blind fashion...” (Page 736) Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Burtscher 1998.
| Methods | 1. Design: Parallel, 2 arms 2. Country: Austria 3. Multisite: No 4. International: No 5. Treatment duration: 1 hour 6. Follow‐up: 24 hours 7. Rate of ascent: Unclear 8. Final altitude reached: 3480 metres 9. AMS scale: Headache scoring |
|
| Participants | 29 participants enrolled (with a history of headache) Randomized to: Aspirin group (n = 15) Placebo group (n = 14) Main characteristics of participants: Age (mean): aspirin group 38 ± 14 years, placebo group 38 ± 14 years Men: aspirin group n = 9/15, placebo group n = 8/14 History of Headache: All |
|
| Interventions | 1. Aspirin group (intervention): aspirin 320 mg, 3 tablets at 4‐hour intervals, beginning 1 hour before arrival at high altitude 2. Placebo group (control): 3 tablets at 4‐hour intervals, beginning 1 hour before arrival at high altitude |
|
| Outcomes | 1. Primary outcome Incidence and severity of headache 2. Secondary outcome Heart rate Blood pressure Arterial oxygen saturation |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Austrian Society for Mountain Medicine, the Health Section of the Austrian Alpine Club, and HoffmannLa Roche 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Yes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Twenty nine volunteers with a history of headache at high altitude were randomly assigned in a double blind fashion to receive placebo (...)" (Page 1057) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Unclear role of funder in this trial |
Burtscher 2001.
| Methods | 1. Design: Parallel, 2 arms 2. Country: Austria 3. Multisite: No 4. International: No 5. Treatment duration: 12 hours 6. Follow‐up: 2 days 7. Rate of ascent: Not clear 8. Final altitude reached: 3480 metres 9. AMS scale: Headache scoring |
|
| Participants | 31 participants enrolled (healthy men and women whose medical history contained reports of at least one episode of headache after ascent to altitudes above 2000 metres) Randomized to: Aspirin group (n = 16) Placebo group (n = 15) Main characteristics of participants: Age (median): aspirin group 39 ± 22 to 58 ; placebo group 40 ± 23 ‐ 59 Men: aspirin group n = 12/16, placebo group n = 8/15 History of AMS: None Type of HAI reported: None |
|
| Interventions | 1. Aspirin group (intervention): aspirin 320 mg with 150 ml water, 3 times at 4‐hour intervals, beginning 2 hours before arrival at high altitude 2. Placebo group (control): tablets with 150 ml water, 3 times at 4‐hour intervals, beginning 2 hours before arrival at high altitude |
|
| Outcomes | 1. Primary outcome: Incidence of headache 2. Secondary outcome: Arterial oxygen saturation |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: This study was supported by the Austrian Science Fund grant P13009‐MED, Grunenthal GMBH and Hoffmann–La Roche 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Thirty‐one subjects were randomly assigned in a double‐blind fashion to receive placebo (...)" (Page 543) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Tablets (placebo or 320 mg aspirin) were administered three times at 4‐hour intervals, beginning 2 hours before arrival at high altitude. Placebos were nearly identical to aspirin in appearance and taste. Tablets were administered by a person who was not involved in scoring or testing procedures" (Page 5430 |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Selective reporting of informations was not detected |
| Other bias | Unclear risk | Unclear role of funder in this trial |
Burtscher 2014.
| Methods | 1. Design: Parallel (two arms) 2. Country: Italy 3. Multisite: No 4. International: No 5. Treatment duration: Pills were taken 10 and 1 hour before high altitude exposure 6. Follow‐up: unclear 7. Rate of ascent: car travel from 600 to 3480 metres. Second and third day climbed 106 metres/hour 8. Final altitude reached: 3800 metres 9. AMS scale: Lake Louise Consensus scoring system 10. Randomization unit: patient 11. Analysis unit: group |
|
| Participants | 15 volunteers enrolled, all of them had history of AMS Exclusion criteria: Any type of acute or chronic illness; regular smoking (> 5 cigarettes per day); regular medications; stops at an altitude > 2500 metres during the previous 4 weeks; Age < 20 or > 60 years; pregnancy or lactation; haemoglobin concentration < 12.0 g/dL Randomized to: Acetazolamide group (n = 7, 46.6%) Placebo group (n = 8, 53.4%) No participants randomized were excluded No participants lost to follow‐up Main characteristics of participants: Age (median/mean, SD): 43.6 ± 13.4, placebo 44.7 ± 8.6 Number of men/woman: Acetazolamide: 4 men: 3 women, placebo: 4 men: 4 women |
|
| Interventions | Acetazolamide group (intervention): received 2 tablets (2 × 125 mg acetazolamide) to be taken 10 hours and 1 hour before high altitude exposure Placebo group received placebo the same way |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. AMS symptoms according to the Lake Louise Score. Participants were considered to be suffering from AMS when the score was ≥ 3 2. Physiological variables: heart rate, minute ventilation, arterial blood gases analysis |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not specified 3. Role of funder: Not specified 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: yes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote " Study participants were randomly assigned in a double blind fashion to receive placebo or acetazolamide before exposure to high altitude" (Page 4379) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Subjects received two tablets (2 × 125 mg acetazolamide or placebo) to be taken 10 hours and 1 hour before arrival at high altitude. Tablets were administered by a person who was not involved in evaluations and the timely intake of tablets has been checked” (Page 4379) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Carlsten 2004.
| Methods | 1. Design: Parallel design, 3 arms 2. Country: Bolivia 3. Multisite: No 4. International: No 5. Treatment duration: 24 hours 6. Follow‐up: 24 hours 7. Rate of ascent: Unknown 8. Final altitude reached: 3630 metres 9. AMS scale: LLS 10. Randomization unit: participant 11. Analysis unit: participant |
|
| Participants | 32 healthy vacationers who had flown from Miami to Bolivia Randomized to: Acetazolamide 250 mg: 11 (34.3%) Acetazolamide 500 mg: 11 (34.3%) Placebo (ascorbic acid): 10 (31.2%) No losses to follow‐up reported Main characteristics of participants: Not stated |
|
| Interventions | Acetazolamide 250 mg, acetazolamide 125 mg, ascorbic acid every 8 hours, 2 doses | |
| Outcomes | AMS score Absolute change from evaluation at 0 hours to evaluation at 24 hours |
|
| Notes | 1. Trial Registration: Not reported 2. Funder: Houston Award Fund, Emge Travelling Scholars programme at Stanford University School of Medicine and the Center for Latin American Studies at Stanford University 3. Role of funder: Financial support 4. A priori sample size estimation: Not stated 5. Conducted: Unclear 6. Declared conflicts of interest: Not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “33 subjects were randomly given one of three identical packets, each packet containing two tablets…” (Page 35) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Quote: “33 subjects were randomly given one of three identical packets, each packet containing two tablets…” (Page 35) Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3% of participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No additional biases were identified |
Chen 2015.
| Methods | 1. Design: Parallel, 4 arms 2. Country: China 3. Multisite: No 4. International: No 5. Treatment duration: 3 days 6. Follow‐up: unclear 7. Rate of ascent: flight from 500 metres to 3700 metres in 2½ hours 8. Final altitude reached: 3700 metres 9. AMS scale: Lake Louise Score 10. Randomization unit: participant 11. Analysis unit: group |
|
| Participants | 80 healthy young men, lowland residents of Chengdu, China Inclusion criteria: Resident at or below 500 metres; Healthy; 18 ‐ 35 years of age Exclusion criteria: HAI (> 2500 metres) exposure history in the past year; organic diseases such as congenital heart disease, dysrhythmia, liver or kidney dysfunction, or psychological or neurological disorders Randomized to: Budesonida inhaled group (n = 20, 25%) Procaterol tablet group (n = 20, 25%) Budesonida/formoterol inhaled group (n = 20, 25%) Placebo Group (n = 20, 25%) No participants randomized were excluded No participants lost to follow‐up Main characteristics of participants: Age (median/mean ± SD): budesonide 21.85 ± 3.23 procaterol 20.3 ± 2.03 budesonide/formoterol 20.6 ± 2.76 placebo 21.65 ± 3.31 Number of men/women: Not specified |
|
| Interventions | 1. Group A received Budesonide 200 mg twice daily 2. Group B received procaterol 25 mg twice daily 3. Group C received Formoterol/budesonide 160 mg 4.5 mg twice daily 4. Group D received placebo tablets, one tablet twice daily |
|
| Outcomes | Primary outcomes: 1. Symptoms of AMS at 20, 72, and 120 hours after arrival at 3700 metres altitude Secondary outcomes 1. HAPE or HACE Other outcomes: 1. Adverse reactions 2. Heart rate and SpO2 3. Pulmonary function test |
|
| Notes | 1. Trial Registration: ChiCTRPRC‐12002748 2. Funder: Special Health Research Project, Ministry of Health of P.R. China (grant No. 201002012) 3. Role of Funder: None 4. A priori sample size estimation: No 5. Conducted: between June 4 and June 16, 2012 6. Declared conflicts of interest: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote " Subjects were randomly assigned to four groups (n = 20), by a physician who did not participate in later parts of the study, using a computer‐generated random number List” (Page 198) |
| Allocation concealment (selection bias) | Low risk | Quote: “The physician who made group assignments prepared one medicine box for each subject. The physician then gave these boxes to other researchers and kept the blinding code. The subjects were fully informed and knew that they could be assigned to any of four groups and that one group would take a placebo.” (Page 198) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: “We initially intended to design a double‐blind trial. However, the procaterol tablet and placebo groups used oral tablets, and the budenoside and budesonide/formoterol groups used inhalants. So subjects might assume that they were given a different drug than those in another group, although they could not know specifically what drug they were taking” (Page 204) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no losses to follow‐up |
| Selective reporting (reporting bias) | High risk | There was no information on HAPE and HACE |
| Other bias | Low risk | No additional biases were identified |
Chow 2005.
| Methods | 1. Design: Parallel design, 3 arms 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 5 days 6. Follow‐up: 1 day 7. Rate of ascent: 1285 metres/hour 8. Final altitude reached: 3800 metres 9. AMS scale: The Lake Louise acute mountain sickness scoring system |
|
| Participants | 68 enrolled and randomized Exclusion criteria: travelled to an elevation above 2400 metres within 30 days of the study; contraindications to high altitude exposure; pregnant; pre‐existing use of acetazolamide or gingko biloba; known hypersensitivity of acetazolamide or gingko biloba; known bleeding disorders or receiving anticoagulant therapy; scheduled a surgical or dental procedure within 14 days of study participations Randomized to: Acetazolamide: 24/68 (35.3%) 3 withdrew before ascent Ginko biloba: 21/68 (30.9%) 4 withdrew before ascent Placebo: 23/68 (33.8%) 3 withdrew before ascent. 1 person in the acetazolamide group withdrew after ascent for personal reasons Main characteristics of participants Age: Acetazolamide: 32 (25 ‐ 42); Ginko biloba: 40 (25 ‐ 62): Placebo: 33.5 (24 ‐ 65) No. of men: Acetazolamide: 13 (65%); Ginko biloba: 10 (58.8%); Placebo: 10 (50%) History of AMS: Not stated |
|
| Interventions | 1. Acetazolamide 250 mg twice a day 2. Gingko Biloba 120 mg twice a day 3. Control: placebotwice a day |
|
| Outcomes | 1. Primary: LLS self‐report questionnaire score and the incidence of AMS 2. Secondary: Number of participants requesting analgesics Number of participants requesting anti‐emetics Number of participants experiencing high‐altitude pulmonary oedema or high‐altitude cerebral oedema Incidence of other symptoms |
|
| Notes | 1. Trial Registration: Not reported 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: Yes, page 298 5. Conducted: Not stated 6. Declared conflicts of interest: Not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We developed a randomization sequence by drawing cards out of a hat, using 25 labeled cards for each group" (Page 297) |
| Allocation concealment (selection bias) | Low risk | Quote: "Study medications were prepared (...) with enclosed adminisitration instructions and affixed with serial numbers" (Page 297) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "To maintain blinding, subjects in acetazolamide group started taking placebo 5 days before ascent and switched to a typical dosis for AMS prophylaxis" (Page 297) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: " in the event of an emergency, an investigator had access to the study key, which was stored within a sealed envelope" (Page 297) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Percentage of participants lost at follow‐up: 16.1% |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Low risk | No other biases were identified |
Ellsworth 1991.
| Methods | 1. Design: randomized, double‐blind, concurrent, placebo‐controlled (declared as cross‐over by authors) 2. Country: Mount Rainer, Seattle Washington (USA) 3. Multisite: No 4. International: No 5. Treatment duration: 2 days 6. Follow‐up: unclear 7. Rate of ascent: 1800 metres/7 hours, day 2 1392 metres/7 hours 8. Final altitude reached: 4392 metres 9. AMS scale: Environmental Symptoms Questionnaire, second revision (ESQ‐Ill) |
|
| Participants | 18 participants were enrolled. They normally resided at sea level and had not been exposed to high altitude within 3 weeks before the study. All were free of cardiorespiratory disease, and none had a history of diabetes mellitus, sulfa drug allergy, acid peptic disease, or psychiatric illness Randomized to: Acetazolamide 8 (44%) Dexamethasone 10 (56%) Authors did not report exclusions and losses during trial Main characteristics of participants: Age: Acetazolamide 32.6 ± 3.9; dexamethasone 36.2 ± 2.4 Percentage/number of women/men: Acetazolamide: 6 men (75%), 2 women (25%); dexamethasone: 5 men (50%) 5 women (50%) Percentage/number History of AMS: Acetazolamide: 5 (62%); dexamethasone: 3 (30%) |
|
| Interventions | 1. Acetazolamide, 250 mg (750 in 24 hours) 2. Dexamethasone, 4 mg (12 mg in 24 hours) 3. Lactose placebo |
|
| Outcomes | Outcomes were not classified as primary or secondary Incidence of AMs (unclear data) AMS‐C scores AMS‐R scores |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Unclear 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using a random numbers table (..)" (Page 289) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: " The drugs were packaged in identical appearing pink capsules by Pharmaceutical services" (Page 289) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "(...) a clinical interview and examination were conducted by one of the investigators (AJE) without knowledge of the subjects response to the questionnaire" (Page 290) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported. Report of incidence of AMS is unclear |
| Other bias | Low risk | No other biases were identified |
Faull 2015.
| Methods | 1. Design: Parallel, 2 arms 2. Country: Italy 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: 2 days 7. Rate of ascent: Unclear 8. Final altitude reached: 3459 metres 9. AMS scale: Lake Louise Score |
|
| Participants | 20 participants enrolled (healthy men and women residing at elevations between 50 metres and 150 metres, without recent (within 2 months) exposure to high altitudes) Randomized to: Acetazolamide group (n = 10) Placebo Group (n = 10) Main characteristics of participants: Age (median): total group: 43 ± 16 Men: acetazolamide group: n = 7; placebo group: n = 7 History of AMS: None Type of HAI reported: None |
|
| Interventions | 1. Acetazolamide group (intervention): acetazolamide 250 mg taken every 12 hours starting 3 days before ascent 2. Placebo group (control): tablets 250 mg taken every 12 hours starting 3 days before ascent |
|
| Outcomes | 1. Primary outcome: Prosaccadic and antisaccadic eye movements 2. Secondary outcome: Presence of AMS |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Jabbs Foundation 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Minimization was used to reduce group differences in AMS susceptibility, age,and sex.Subjects were randomly allocated to receive either 250 mg acetazolamide or identically matching placebo(...)" (Page 73) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1 participant (5%) was removed from final analysis |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Fischer 2000a.
| Methods | 1. Design: Parallel randomized design 2. Country: Switzerland 3. Multisite: No 4. International: No 5. Treatment duration: 3 hours 6. Follow‐up: unclear 7. Rate of ascent: unclear 8. Final altitude reached: 3454 metres 9. AMS scale: Acute Mountain Sickness Score |
|
| Participants | 21 participants enrolled (healthy mountaineers with normal weight and constant good health) Exclusion criteria: women, smoking, non‐compliance with studyprotocol, previous pulmonary disease Randomized to: Theophylline group (unclear) Placebo group (unclear) No participants were lost to follow‐up Main characteristics of participants: Age (median/mean): 29 ± 8 Percentage of men: 100% |
|
| Interventions | 1. Theophylline (intervention): 375 mg slow‐release tablets taken twice daily for 3 days, or 250 mg twice daily for participants < 70 kg. This was stopped 12 hours after arrived at altitude. 2. Placebo group (control): placebo tablets twice daily for 3 days |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. AMS scores by LLS 2. Measurements of respiratory frequency 3. Pulse rate 4. Oxygen saturation 5. Serum theophyline level |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Byk Gulden, Constance, Germany 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "21 subjects were randomly allocated to placebo (...)" (Page 124) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Unclear risk | Unclear role of funder |
Fischer 2000b.
| Methods | 1. Design: Cross‐over design 2. Country: Germany 3. Multisite: No 4. International: No 5. Treatment duration: first phase 3 days 6. Follow‐up: unclear 7. Rate of ascent: unclear 8. Final altitude reached: first phase 4500 metres 9. AMS scale: Acute Mountain Sickness Score |
|
| Participants | 14 participants enrolled (healthy mountaineers with normal weight and constant good health) Exclusion criteria: women, smoking, non‐compliance with study protocol, previous pulmonary disease Randomized to: Theophylline group (unclear) Placebo group (unclear) No participants were lost to follow‐up Main characteristics of participants: Age (median/mean): 29 ± 8 first study Percentage of men: 100% |
|
| Interventions | 1. Theophylline (intervention): 375 mg slow‐release tablets taken twice daily for 3 days, or 250 mg twice daily for participants < 70 kg 2. Placebo group (control): placebo tablets twice daily for 3 days |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. AMS scores by LLS 2. Measurements of respiratory frequency 3. Pulse rate 4. Oxygen saturation 5. Serum theophyline level |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Byk Gulden, Constance , Germany 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "14 subjects were randomly allocated to placebo or study medication for the first session(...)" (Page 124) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "or matched placebo tablets twice daily" (Page 124) Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Unclear role of funder. It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials |
Fischer 2004.
| Methods | 1. Design: cross‐over trial
2. Country: Germany 3. Multicentre study: No 4. Altitude setting: 4500 metres 5. AMS scale:The Lake Louise self‐assessment questionnaire (LLS) and the ESQ were used to assess symptoms of AMS at 0, 3, 6 and 9 hours |
|
| Participants | 10 participants enrolled (male volunteers) Exclusion criteria: Not provided Randomized to each group with an interval of 2 weeks between each of the three chamber sessions Theophylline group Acetazolamide group Placebo group No participants were lost to follow‐up Main characteristics of participants: Age (median/mean): 24.8 years Percentage of men: 100% |
|
| Interventions | 1. Intervention: acetazolamide (250mg twice a day) 2. Theophylline (250 mg twice a day) 3. Placebo (twice a day) |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. LLS scores 2. ESQ scores 3. PaO2, PaCO2 and PH measurements 4. Magnetic resonance imaging |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Deutsche Akademic für Flug + Radiometer Inc 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported. Numbers of participants by arm were not provided |
| Other bias | Unclear risk | Unclear role of funder. It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials |
Fulco 2006.
| Methods | 1. Design: Cross‐over trial (4 arms) 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 2 days 6. Follow‐up: unclear 7. Rate of ascent: unclear 8. Final altitude reached: 4300 metres 9. AMS scale: ESQ |
|
| Participants | 6 participants enrolled. All were born at altitude < 1500 metres and resided near sea level for at least 6 months 4‐week long definitive testing phase Randomized each week to: Sea level + placebo Sea level + acetazolamide Simulated altitude + placebo Simulated altitude + acetazolamide No participants were lost to follow‐up Main characteristics of participants: Age (median/mean): 20 ± 1 years Number of men: 5/6 |
|
| Interventions | 1. Acetazolamide 250 mg, 3 times a day for 2 days 2. Placebo group (control), 3 times a day for 2 days |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. Physiological measurements 2. ESQ scores 3. AMS‐C 4. AMS‐R |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “The presentation of the definitive exercise testing bouts…was assigned randomly for each subject” (Page 684) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Both the subjects and the investigators directly involved were blinded to drug treatment status…” (Page 684) “Acetazolamide and an identically appearing placebo capsule were prepared by a local pharmacy that had no other relationship with the study” (Page 685) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “Both the subjects and the investigators directly involved were blinded to drug treatment status…” (Page 684) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials |
Greene 1981.
| Methods | 1. Design: Cross‐over design ( 2 arms) 2. Country: Kenya 3. Multisite: No 4. International: No 5. Treatment duration: 4 weeks 6. Follow‐up: 4 weeks 7. Final altitude reached: varied 8. AMS scale: Self‐administered subjective questionnaire of AMS symptoms |
|
| Participants | 24 British climbers; none were professional sportsmen; 5 were medically trained 2. Participants were paired for age, sex and likely activities, and each member of each pair was allocated at random to 1 of 2 treatment groups: Acetazolamide 500 mg sustained release nightly Placebo: identically presented No participants were lost to follow‐up Main characteristics of participants: 2 women, 22 men History of AMS: Not reported Type of HAI reported: Not reported |
|
| Interventions | 1. Acetazolamide 500 mg nightly during 5 nights before and after exposure 2. Placebo in the same way |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. Scores for AMS from symptom cards 2. Adverse events |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Young Explorers Trust, Lederle laboratories 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “They were paired for age, sex and likely activities, and each member of each pair was allocated at random to one of two treatment groups” (Page 811) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Most of information was presented as graphs |
| Other bias | Unclear risk | Unclear role of funder. It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials |
Hackett 1976.
| Methods | 1. Design: Parallel design (2 arms) 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: Unclear 7. Final altitude reached: 4243 metres 8. AMS scale: Subjective symptoms evaluation |
|
| Participants | 278 hikers recruited in Namche Bazar (3440 metres) were included (volunteers). Number of participants assigned to each group is unclear Assigned to Acetazolamide 71 (24%) Placebo 49 (39%) No treatment controls 158 (69%): participants not taking tablets 3. Number of participants lost to follow‐up unclear. 52 questionnaires were excluded on their return Main characteristics of participants: Age: 33: 18 ‐ 71 years Men: 71% |
|
| Interventions | 1. Acetazolamide 250 mg starting at 3440 metres twice daily for 4 days 2. Placebo tablets (lactose, provided by the Royal Drug company, Kathmandu, Nepal) twice daily for 4 days |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. Acute Mountain Sickness 2. Severity: HAPE or cerebral oedema |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Unclear 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Oct 10 to Nov 10, 1975 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Those volunteering were assigned to placebo or acetazolamide groups and subjects taking no tablets were classified as controls” (Page 1150) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Tablets were packaged into small plastic bags (coded for later identification) each containing a course of medication and selected at random so that neither the subject nor the investigator knew which was being given” (Page 1150) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “Tablets were packaged into small plastic bags (coded for later identification) each containing a course of medication and selected at random so that neither the subject nor the investigator knew which was being given” (Page 1150) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Number of participants lost from each arm to follow‐up unclear |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported. HAPO and HACE results are not clearly reported in “Results” section |
| Other bias | Low risk | No other biases were identified |
Hackett 1988.
| Methods | 1. Design: Randomized double‐blind study 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 1 day 6. Follow‐up: unclear 7. Rate of ascent: 4400 metres in 1 hour, by helicopter 8. Final altitude reached: 4400 metres 9. AMS scale: AMS Symptoms Questionnaire |
|
| Participants | 15 healthy military men on no medication were enrolled; None had been to high altitude within 3 weeks before the study Randomized to: Placebo (n = 7) Dexamethasone 2 mg (n = 8) No participants were lost to follow‐up Main characteristics of participants: Men, age 28 ± 1.0 year, height 181 ± 2 cm, and weight 83±4 kg |
|
| Interventions | Dexamethasone: 2 mg dexamethasone every 6 hours starting 1 hour before flying Placebo: no details were provided |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. AMS scores and severity 2. AMS‐C 3. AMS‐R 4. Physiological measurements |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Unclear "Many people and organizations" 3. Role of funder: Unclear 4. A priori sample size estimation: No 5. Conducted: Unclear 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the 15 subjects were randomized to receive (...)" (Page 951) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
HEAT 2010.
| Methods | 1. Design: Randomized trial, parallel, 3 arms 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: 1 day 6. Intention‐to‐treat: Yes 7. Follow‐up: 1 day 8. Rate of ascent: unclear 9. Final altitude reached: 4928 metres 10. AMS scale: Lake Louise AMS questionnaire (LLS) |
|
| Participants | 343 participants enrolled (healthy men and women, 18 ‐ 65 years), to ascend from 2 villages at 4280 metres and 4358 metres respectively, to 4928 metres Exclusion criteria: headache at recrutment, diagnosis of AMS, signs or symptoms of a substantial acute infection, had slept above 4500 metres, or had taken any NSAIDs or acetazolamide within 1 day or 3 days prior to enrolment, respectively Randomized into 3 groups: Placebo (89) Ibuprofen (129) Acetazolamide (125) 48 participants randomized were excluded due to protocol violations: Placebo (12, 13%) Ibuprofen (18, 14%) Acetazolamide (18, 14%) Participants lost to follow‐up: 78 (22.7%) lost to follow‐up for unclear reasons Main characteristics of participants: Age: 39.2 ± 12.1 (placebo), 39.1 ± 12 (acetazolamide), 37 ± 11.4 (ibuprofen) Number/Percentage of men: 47/65 (72.3% placebo), 65/97 ( 67.7% acetazolamide), 75/103 (73.5% ibuprofen) Percentage/number History of AMS: 3/65 (4.6% placebo), 2/97 ( 2.1% acetazolamide), 2/103 (1.9% ibuprofen) |
|
| Interventions | 1. Placebo group: placebo 3 times a day orally for 1 day prior to the ascent 2. Ibuprofen group: 600 mg of ibuprofen 3 times a day orally Cointervention: In all 3 groups there was a period of acclimatization, approximately three nights in each group |
|
| Outcomes | Primary outcome 1. Incidence of headache at the study endpoint as calculated on the Lake Louise AMS Questionnaire (LLS) Secondary endpoints 1. Evaluation of headache severity by visual analog scale (VAS) 2. Pulse oximetry 3. AMS incidence and severity as measured by the LLS 4. Side effects |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Himalayan Rescue Association, Deurali‐Janta Pharmaceuticals of Kathmandu, Nepal and Hari Bhakta Sharma. Drs Derek and Lydia Lipman 3. Role of funder: randomization of the drugs and packaging. Drs Derek and Lydia Lipman (financial support) 4. A priori sample size estimation: Yes 5. Conducted: October 2005 to November 2005 6. Declared conflicts of interest: Yes. (Page 241) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Study medications were randomized via computer‐generated code" (Page 237) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 22.7% of participants were lost to follow‐up and not include in final analysis |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Unclear risk | Possible industry bias |
Hillenbrand 2006.
| Methods | 1. Design: Randomized, double‐blind controlled trial 2. Country: Mount Everest region of Nepal 3. Multisite: No 4. International: No 5. Follow‐up: 7 days 6. Rate of ascent : 300 metres/day 7. Final altitude reached: 4930 metres 8. AMS scale: Lake Louise AMS symptom score |
|
| Participants | 403 male Nepali porters (adults) were enrolled for 8 Nepail doctors Exclusion criteria: AMS, various medical conditions, sulphonamide allergy or any other previous drug reactions, or taking a different route that did not pass through the assessment stations 3 porters were excluded for 1 of these reasons Randomized to: Acetazolamide group = 202 (50.5%) Placebo group = 198 (49.5%) 275 porters were lost to follow‐up Most porters (275 porters; 68.75%) dropped out of the trial; 92 porters missed 1 station, 61 porters missed 2 stations, and 122 porters missed all 3 stations Treatment allocation and demographic data were similar in porters who completed the trial and in those who dropped out. 16 porters (4%) were excluded from the analysis, 8 porters for deviating from the standard trek route and 8 porters for noncompliance with medication. Three noncompliers accepted medication from a friend, 3 porters took acetazolamide, 1 porter received medicine from a trekker, and one porter simply failed to take his medication Main characteristics of participants (all groups): Age (median, range): 25, 18 ‐ 54 Percentage of men: 100% Weight: 51 kgs, 38 ‐ 66 |
|
| Interventions | 1. Acetazolamide group: 250 mg acetazolamide, orally for 7 days 2. Placebo group: 250 mg orally for 7 days |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. AMS incidence 2. Related factors 3. Side effects |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: "Jerwood Foundation and the Sir Samuel Scott of Yews Trust for grants; and the Good Hope Hospital NHS Trust Charitable Fund, the Holy Trinity Parish Church, the Royal Sutton Fun Run, and many individuals for generous donations towards the funding of this study" (Page 93) 3. Role of funder: Wyeth donated acetazolamide 4. A priori sample size estimation: Yes 5. Conducted: October to November 2001 6. Declared conflicts of interest: "The authors have no conflicting interests in this work" (Page 87) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization code was sent directly by DPH to one of the authors of this study, who was not directly involved in performing the clinical trial. He prepared the sealed envelopes containing the trial codes" (Page 88) |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomization code was sent directly by DPH to on e of the authors of this study, who was not directly involved in performing the clinical trial. He prepared the sealed envelopes containing the trial codes" (Page 88) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "(...) and a sealed envelope that was only to be opened in the event of illness (...)" (Page 88) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Porters were asked to report to them and were assessed for AMS, using the LLS AMs symptoms score." (Page 88) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 68.75% of porters dropped out of the trial |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Low risk | No other biases were identified |
Hochapfel 1986.
| Methods | 1. Design: Parallel design (2 arms) 2. Country: Nepal (Annapurna) 3. Multisite: No 4. International: No 5. Treatment duration: 9 days 6. Follow‐up: 9 days 7. Final altitude reached: 5500 metres 8. AMS scale: Self‐administered subjective questionnaire 9. Randomization unit: patient 10. Analysis unit: patient |
|
| Participants | 18 trekkers (7 women, 11 men), ages ranged 27 ‐ 53 years, were included. None of them had been at an altitude over 3000 metres over the last 12 months Randomized to: Acetazolamide group: number assigned unclear Placebo group: number assigned unclear Unclear if participants were lost to follow‐up Characteristics of participants not reported |
|
| Interventions | 1. Acetazolamide 250 mg 2. Placebo tablets: no different in form or taste from the acetazolamide tablets |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. Subjective complaints 2. Onset of headache 3. Side effects |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the batches were distributed in a random process" Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "None of participants knew the encryption(..)" "The placebo did not differ in the form nor in the taste of the Diamox tablet" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Selective reporting (reporting bias) | High risk | Unknown number of participants in each arm |
| Other bias | Low risk | No other biases were identified |
Hohenhaus 1994.
| Methods | 1. Design: Randomized trial, parallel, 2 arms 2. Country: Italy 3. Multisite: No 4. International: No 5. Treatment duration: 3 days 6. Follow‐up: 1 day 7. Rate of ascent: unclear 8. Final altitude reached: 4559 metres 9. AMS scale: Score proposed at the International Hypoxia Symposium+ "Do you feel ill?" = Yes |
|
| Participants | 27 mountaineers were recruited. 12 had increased susceptibility to AMS, 8 normal susceptibility and 7 unknown susceptibility Randomized to: Nifedipine group: 14 (51.8%) Placebo group: 13 (48.1%) No participants were lost to follow‐up Main characteristics of participants: Age 33 (24 ‐ 60) (placebo); 37 (21 ‐ 54) (nifedipine) Number of men: 9/13 (placebo); 7/14 (nifedipine) Number History of AMS/susceptible: 6/13 (placebo); 7/14 (nifedipine) |
|
| Interventions | 1. Nifedipine group: Adalat retard, 20 mg. 2. Placebo group: No details provided Medication was given at 10 P.M. on the third and second days before the ascent and at 8 A. M. and 10 P.M. on the day before. Starting on the day of ascent, medication was taken three times daily (at 6 A.M., 2 P.M. and 10 P.M.). |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. Presence of AMS 2. Blood and end‐expiratory gas analysis 3. Pulmonary artery pressure 4. HAPE |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Italian Alpine Club and Swiss Army 3. Role of funder: providing locations and transportation of the radiographic equipment 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "was assigned randomly in a double‐blind design with stratification (...)" (Page 858) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Hussain 2001.
| Methods | 1. Design: Parallel (4 arms) 2. Country: Pakistan 3. Multisite: No 4. International: No 5. Treatment duration: 6 days 6. Follow‐up: 3 days 7. Rate of ascent: 4578/24 hours 8. Final altitude reached: 4578 metres 9. AMS scale: Modified ESQ |
|
| Participants | 24 participants enrolled (healthy men, low altitude residents at < 500 metres with good health and not suffering from any acute of chronic systemic illness or psychiatric disease) Randomized to: Acetazolamide group (n = 6) Placebo Group (n = 6) Dexamethasone group (6) Acetazolamide and dexamethasone group (6) Main characteristics of participants: Age (median): global range 25 ‐ 35 years Men: 6 participants in each group History of AMS: None Type of HAI reported: None |
|
| Interventions | 1. Acetazolamide group : 250 mg every 12 hours, started 24 hours before ascent to 4578 metres and continued for 5 days 2. Placebo group: multivitamin tablet every 12 hours, started 24 hours before ascent to 4578 metres and continued for 5 days 3. Dexamethasone group (control): 4 mg tablet every 12 hours, started 24 hours before ascent to 4578 metres and continued for 5 days 4. Acetazolamide and dexamethasone: 250 mg and 4 mg every 12 hours, started 24 hours before ascent to 4578 metres and continued for 5 days |
|
| Outcomes | 1. Primary outcome: Presence of AMS 2. Secondary outcome: Oxygen saturation, severity of AMS |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study was placebo controlled and the subjects were randomized in double blind fashion into four study groups; that is, six subjects in each group" Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were reported as lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Jain 1986.
| Methods | 1. Design: Parallel trial 2. Country: Delhi, India 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: 4 days 7. Rate of ascent: Simulate 4570 metres in 1 day 8. Final altitude reached: 4570 metres 9. AMS scale: General High Altitude Questionnaire (GHAQ) 10. Randomization unit: participants 11. Analysis unit: group |
|
| Participants | 29 participants enrolled (Indian soldiers aged between 22 and 26 years having no previous experience of being at high altitude) Randomized to: Acetazolamide tablets (n = 10) Spironolactone (n = 9) Placebo (n = 10) No participant randomized was excluded or lost to follow‐up Main characteristics of participants: Age (median): global ranged 22 ‐ 26 years Men: 100% History of AMS: None Type of HAI reported: None |
|
| Interventions | 1. Acetazolamide tablets 250 mg every 6 hours beginning a day before the ascent to high altitude 2. Spironolactone tablets 25 mg every 6 hours beginning a day before the ascent to high altitude 3. Placebo tablet every 6 hours beginning a day before the ascent to high altitude |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. Presence of AMS 2. Blood and end‐expiratory gas analysis |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: No stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The subjects were initially tested at an altitude of 200 m and then divided into three groups by using a random number table" (Page 294) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No participants were reported as lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Johnson 1984.
| Methods | 1. Design: Double‐blind cross‐over 2. Country: Boston, USA 3. Multisite: No 4. International: No 5. Treatment duration: 1 day 6. Follow‐up: Unclear 7. Rate of ascent: Simulate 4570 metres in 1 day 8. Final altitude reached: 4570 metres 9. AMS scale: ESQ III, AMS‐C, and AMS‐R questionnaires |
|
| Participants | 12 participants enrolled (healthy men, 20 ‐ 26 years of age, residing at sea level). They were exposed to simulated altitude on 2 separate occasions 4 participants did not participate in the cross‐over phase Main characteristics of participants: Age (median): global ranged 22 ‐ 26 years Men: 100% History of AMS: None Type of HAI reported: None |
|
| Interventions | Dexamethasone 4 mg every 6 hours by mouth Placebo | |
| Outcomes | Outcomes were not classified as primary or secondary 1. Presence of AMS 2. AMS‐C and AMS‐R scores 3. Retinal photography 4. Biochemical and physiological measurements |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: US Army Research Institute of Environmental Medicine 3. Role of funder: Technical assistance 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The treatment order was randomly assessed" (Page 684) nsufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4 participants (33%) were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Unclear risk | It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials |
Kayser 2008.
| Methods | 1. Design: Parallel design (3 arms: 2 randomized and 1 open arm) 2. Country: Tanzania (Mount Kilimanjaro) 3. Multisite: No 4. International: No 5. Treatment duration: 5 days 6. Follow‐up: 6 days 7. Rate of ascent: 2725 metres/day 1; 1055 metres/day 2; 720 metres/day 3; 960 metres/day 4 8. Final altitude reached: 5896 metres 9. AMS scale: Lake Louise Symptom Score (LLSS) and physician assessment 10. Randomization unit: patient 11. Analysis unit: patient |
|
| Participants | 93 potential participants (non‐acclimatized, altitude‐naïve, attempting a fast climb up Mount Kilimanjaro)
Exclusion criteria: not reported. 44 participants chose prevention with acetazolamide Randomized to: Calcium carbasalate 15 (48.4%) Placebo 16 (51.6 %) No participants randomized were excluded 18 participants lost to follow‐up, refusing to participate in any data collection Main characteristics of participants: Age mean (SD): No reported History of AMS: Not stated |
|
| Interventions | Intervention: 1. acetazolamide 500 mg, oral for 5 days 2. calcium carbasalate 380 mg, 380 mg/day oral, for 5 days 3. Control: placebo |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. Prevention failure: Headache and LLS score ≥ 3; Headache and LLS + clinical score ≥ 4; Headache and LLS + clinical + functional score ≥ 4 2. HACE: Severe ataxia, vomiting, decreased consciousness 3. Disease‐free fast climb experience |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Dutch tabloid Magazine 3. Role of funder: Provide medical assistance for its readers in the organization of a climb of Mount Kilimanjaro 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The subjects who agreed to participate in the trial were randomized into two groups stratified for age and sex" (Page 16) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were reported as lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Ke 2013.
| Methods | 1. Design: Prospective randomized study 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: unclear 7. Rate of ascent: none 8. Final altitude: 3658 metres 9. AMS scale: Lake Louise Score |
|
| Participants | 1. 28 healthy lowland young men (14 ‐ 22 years old) with no altitude experiences (> 2500 metres) in the preceding 2 years Randomized into 3 groups: Acetazolamide group (n = 9, 32%) Gingko biloba (n = 10, 36%) Placebo (n = 9, 32%) Participants received 3‐day pretreatment and 1‐day treatment Main characteristics of participants: Age (mean): 19.2 (range 14 ‐ 22 years old) Percentage/number of women/men: 28 men |
|
| Interventions | 1. Acetazolamide 125 mg twice daily 2. Gingko biloba 120 mg twice daily. 3. Placebo |
|
| Outcomes | 1. The primary outcome was pulmonary artery systolic pressure (PASP) to hypoxia on the first day 2. Secondary outcomes included: AMS, arterial oxygen saturation (SaO2), mean artery pressure (MAP), heart rate (HR), and spirometry parameters (FVC, FEV1%, PEF) to hypoxia |
|
| Notes | 1. Trial Registration: not stated 2. Funder: National Key Technology R&D Program (Grant 2009BAI85B04); National Nature Science Foundation of China (Grant 81172621); and Program for Changjiang Scholars and Innovative Research Team in University 3. A priori sample size estimation: No 4. Conducted: Not stated 6. Declared conflicts of interest: Yes. None declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “The participants were randomized into three groups according to random numbers generated by using a software package with nine in the acetazolamide group, ten in the gingko biloba group and nine in the placebo group” (Page 163) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "(...) and placebo (provided by the Institute of Pharmaceuticals of the Fourth Military Medical University) were packaged in visually identical capsules at the Institute of Pharmaceuticals of the Fourth Military Medical University (...)" (Page 163) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were reported as lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Low risk | No other biases were identified |
Küpper 2008.
| Methods | 1. Design: randomized, doubled‐blind, placebo‐controlled trial 2. Country: Italy 3. Multisite: No 4. International: No 5. Follow‐up: 8 days 6. Treatment duration: 2 days 7. Intention‐to‐treat: No 8. Follow‐up: 24 hours 9. Rate of ascent: first 5 days at 1000 metres, 3440 metres ascent partial, then maximum height of 4560 10. Final altitude reached: 4559 metres 11. AMS scale: Lake Louise AMS questionnaire (LLS) |
|
| Participants | 1. 24 healthy men eligible. 4 excluded or refused to participate; the reasons for exclusion were sleep disorders, heart disease history, previous episodes of cerebral oedema or high altitude pulmonary 20 participants randomized to receive either 300 mg slow‐release theophylline tablets (n = 10) or an identical‐appearing placebo (n = 10) Participants lost to follow‐up, 1 in the theophylline group and 2 in the placebo group, were unable to ascend to Margherita hut due to adverse weather conditions Main characteristics of participants: Number/Percentage of men: 100% Percentage/number History of AMS: None of the subjects had a history of AMS. |
|
| Interventions | 1. Theophylline group (intervention): 300 mg slow‐release tablets, 1 tablet each day at 8 p.m. during 5 days prior to ascent and 2 days 1 night during ascent 2. Placebo group (control): 300 mg identical‐appearing placebo tablets, 1 tablet each day at 8 p.m. during 5 days prior to ascent and 2 days 1 night during ascent |
|
| Outcomes | This study does not establish primary or secondary outcomes 1. Incidence of AMS (AMS‐C score ≥ 4) 2. Scores of AMS 3. Theophylline levels 4. Sleep hypoxaemia and breathing pattern 5. Polysomnographic parameters |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: "This investigation was supported by an unrestricted grant of 3M Pharmaceuticals Inc., Neuss, Germany. 3M Pharmaceuticals Inc. also provided the study medication and placebo. Respironics Inc., Pittsburgh, PA, USA, provided logistic support (sleep recorders and laptops during study duration and helicopter flights for transport of this material). The Margherita hut research lab is supported by several European universities, the Italian Alpine Club, and structural and research funds of the European Union" 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Unclear 6. Declared conflicts of interest: yes. Page 312 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were randomized (random allocation; see Figure 1) to receive either 300 mg slow‐release theophylline tablets (Unilair 300; 3M Pharmaceuticals Inc., Neuss, Germany) or an identical‐appearing placebo" (Page 308) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 participants (15%) were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Possible industry bias |
Larson 1982a.
| Methods | 1. Design: Parallel (2 arms) 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 24 hours 6. Follow‐up: Until 48 hours 7. Rate of ascent: Unclear 8. Final altitude reached: 4394 metres 9. AMS scale: GHAQ modified |
|
| Participants | 64 participants enrolled (volunteers who normally resided at or near sea level, all in good general health and none had ascended to higher than 3000 metres for at least 4 weeks before participating) Randomized to: Acetazolamide (n = 31, 48.4%) Placebo (n = 33, 51.6%) 7 participants lost to follow‐up 2 participants in acetazolamide group and 3 in placebo did not leave base camp because of excessive fatigue or inadequate clothing; 5 participants in placebo group did not reach the summit, but were included in analysis because they reached at least 3000 metres Main characteristics of participants: Age: range 21 ‐ 48 years Percentage of men: 54 (84.3%) and women:10 (15.3%) Age (mean, SD): Acetazolamide = 28.7 (0.9); Placebo = 29.2 (1) Percentage of men: Acetazolamide= 87.1%; Placebo = 81.8% Pulse rate, beats per minute (mean, SD): Acetazolamide= 65.1 (1.8); Placebo = 64.0 (1.8) There is not enough information on the 6 climbers who ascended twice (cross‐over arm) |
|
| Interventions | 1. Acetazolamide group (intervention): Acetazolamide tablets 250 mg every 8 hours, beginning 1 day before ascent 2. Placebo group (control): Placebo tablets every 8 hours, beginning 1 day before ascent Cointerventions: Not reported |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. AMS assessment (GHAQ scores) at sea level, 1600 metres, 3000 metres, 4394 metres (summit) or high point attained above base camp 2. Spirometric data: resting minute ventilation, expired vital capacity and peak flow, at sea level, 1600 metres, 3000 metres and or near the summit, after resting for at least 10 minutes |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: "The acetazolamide (Diamox) and placebo used in this study were provided by Darrel Leichty, Belleuve, Wash, who is a product representative of Lederle Laboratories, Division of American Cyanamid Company, Wayne, NJ” (Page 332) 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using a random numbers table and in a double‐blind fashion" (Page 329) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Packets containing tablets and data collection forms were prepared by persons not directly involved with th study (...)" (Page 329) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Around 10% of participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Possible industry bias |
Larson 1982b.
| Methods | 1. Design: Cross‐over study 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: Unclear 6. Follow‐up: Unclear 7. Rate of ascent: Unclear 8. Final altitude reached: 4394 metres 9. AMS scale: GHAQ modified |
|
| Participants | 6 participants enrolled (volunteers who normally resided at or near sea level, all in good general health and none had ascended to higher than 3000 metres for at least 4 weeks before participating) . Approximately 1 year between the 2 climbs No participants lost to follow‐up Main characteristics of participants: No information was provided for these participants |
|
| Interventions | 1. Acetazolamide group (intervention ): Acetazolamide tablets 250 mg every 8 hours, beginning 1e day before ascent 2. Placebo group (control): Placebo tablets every 8 hours, beginning 1 day before ascent Cointerventions: None reported |
|
| Outcomes | This trial did not specify by primary or secondary outcomes: 1. AMS assessment (GHAQ scores) at sea level, 1600 metres, 3000 metres, 4394 metres (summit) or high point attained above base camp 2. Spirometric data: resting minute ventilation, expired vital capacity and peak flow, at sea level, 1600 metres, 3000 metres and or near the summit, after resting for at least 10 minutes |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: "The acetazolamide (Diamox) and placebo used in this study were provided by Darrel Leichty, Belleuve, Wash, who is a product representative of Lederle Laboratories, Division of American Cyanamid Company, Wayne, NJ” (Page 332) 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using a random numbers table and in a double‐blind fashion" (Page 329) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Packets containing tablets and data collection forms were prepared by persons not directly involved with the study (...)" (Page 329) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Around 10% of participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Possible industry bias. It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials |
Lipman 2012.
| Methods | 1. Design: Parallel design (2 arms) 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 1 day 6. Follow‐up: 1 day 7. Rate of ascent: unclear. Aprox 2305 ‐ 2356 metres every 6 hours 8. Final altitude reached: 3810 metres 9. AMS scale: Lake Louise Questionnaire Acute Mountain Sickness Score (LLQ) |
|
| Participants | 89 participants were recruited through a variety of e‐mail list‐serves with both local and national distribution, as well as posted advertisements in northern and southern California Randomized to: Placebo 42 Ibuprofeno 44 2 participants were excluded post hoc for meeting acute mountain sickness criteria at baseline, and 1 for receiving diuretic medication during the study No participants were lost to follow‐up Main characteristics of participants: Age: Placebo 34.8 (13.2), Ibuprofen 38.4 (14.5) Percentage/number of women/men: Placebo 14 women (33.3%), 28 men; Ibuprofen 14 women (31.8%), 40 men Percentage/number History of AMS: Placebo 5 (11.9%), Ibuprofeno 2 (4.6%) Percentage/number Type of HAI reported: Unclear History of headaches: Placebo 2 (4.8%), Ibuprofeno 5 (11.4%) |
|
| Interventions | 1. Ibuprofen: 600 mg 4 doses of medication at baseline, 3545 metres, 3810 metres and the next morning after descending 2. Placebo: same regimen |
|
| Outcomes | 1. Primary outcome measures: Incidence and severity of AMS as calculated on the Lake Louise Questionnaire score 2. Secondary outcome measures: headache severity by visual analogue scale and peripheral oxygen saturation by fingertip pulse oximetry (SpO2) from baseline |
|
| Notes | 1. Trial Registration: “Not stated” 2. Funder, role of funder: "This research was made possible by a Research grant from the Division of Emergency Medicine, Stanford University School of Medicine and financial support from the American Alpine Club" 3. A priori sample size estimation: Yes (page 486) 4. Conducted: July and August 2010 5. Declared conflicts of interest: Yes (page 489) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized to visually identical commercial‐grade ibuprofen 600 mg or placebo, using a computer‐generated random sequence, with the randomization code unavailable to administrators and participants" (Page 485) |
| Allocation concealment (selection bias) | Low risk | Quote: "Participants were randomized to visually identical commercial‐grade ibuprofen 600 mg or placebo, using a computer‐generated random sequence, with the randomization code unavailable to administrators and participants" (Page 485) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Luks 2007.
| Methods | 1. Design: Randomized, doubled‐blind cross‐over trial 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: Until symptoms of AMS became intolerable to the participant or they reached the maximum study duration of 8 hours. Washout time of 2 weeks between 2 observations 8. Rate of ascent (m/h): 158 metres to 3900 metres simulated in a chamber with normobaric hypoxia 9. Final altitude reached: 3900 metres 10 AMS scale: Lake Louise Acute Mountain Sickness scoring survey |
|
| Participants | Number enrolled unclear ("Healthy volunteers between the ages of 18 and 55" Page 134) Potential volunteers were excluded from the study if they had chronic pulmonary, cardiac, renal or liver disease, if they had a history of allergies or were already taking anti‐inflammatory corticosteroids or medications inhibiting leukotriene synthesis or blocking receptor binding or if they had recently been at high altitude (more than a day at an elevation of 1500 m or higher in the preceding 2 weeks) Randomized to: Montelukast group (n = 10) Placebo group (n = 10) 1 participant randomized was excluded because they completed 1 session, but did not return for the second session, because of severe symptoms during the first testing session 1 participant lost to follow‐up Main characteristics of participants: Age: 24 to 41 4 men, 6 women Percentage/number History of AMS: Not stated |
|
| Interventions | 1. Montelukast group (intervention): 10 mg tablet (Singulair, Merck and Co.) daily for 4 days 2. Placebo group (control): Similar‐appearing placebo tablet 3. Co‐interventions: for 15 minutes each hour, participants rode a stationary bicycle at a moderate pace in order to simulate the hiking or other physical activity someone might undertake at high altitude |
|
| Outcomes | 1. Primary outcome measure: Lake Louise Acute Mountain Sickness score at the end of the testing session 2. Secondary outcome measures: Score on the headache component of the Lake Louise scale, the length of time participants were able to remain in the chamber, their average heart rate and arterial blood oxygen saturations throughout their chamber exposure, and the pre‐ and post‐exposure urinary leukotriene E4 concentrations |
|
| Notes | 1. Trial Registration: Not stated 2. Funding: Merck Research Laboratories, West Point, Pennsylvania, supported this study 3. Role of sponsor: Not stated 4. A priori sample size estimation: No 5. Conducted: unclear 6. Declared conflicts of interest: Yes (Page 137) “The authors have no other financial support or conflicts of interest to disclose regarding this study” |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote " was determined by the flip of a coin..." (Page 132) Insufficient information to score this item as low or high risk of bias. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote "..neither the subject nor the investigator were aware of the assignment for a particular testing session" (Page 132) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 2 participants (20%) were excluded from further analyses |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Possible industry bias. It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials |
Maggiorini 2006.
| Methods | 1. Design: Randomized, doubled‐blind, placebo‐controlled trial 2. Countries: Italy, Switzerland 2. Multisite: Yes 3. International: Yes 4. Treatment duration: 3 days 5. Follow‐up: 48 hours 6. Rate of ascent: ascended from 1100 metres to 3200 metres by cable car, taking about 1½ hours. Continued by foot to 3600 metres, where they slept overnight, and continued the next morning to 4559 metres in about 4 hours 7. Final altitude reached: 4559 metres 8. AMS scale: Clinical examination by Lake Louise scoring protocol |
|
| Participants | 29 pants enrolled (mountaineers with a previous history of HAPE) Randomized to: Placebo group (n = 9) Tadalafil group (n = 10) Dexamethasone group (n = 10) 2 participants in the Tadalafil group were withdrawn from the study because they developed severe AMS on the evening of arrival at 4559 metres No participants were lost to follow‐up Main characteristics of participants: Age (Mean/SD): Placebo group 41/8; tadalafil group 46/3; dexamethasone group 44/3 Number of women/men: Placebo group 2/9; Tadalafil group 1/10; dexamethasone group 1/10 History of HAPE: (Interquartile range): Placebo group 1 (1 ‐ 3); tadalafil group 1 (1 ‐ 2); dexamethasone 1 (1 ‐ 2) |
|
| Interventions | 1. Tadalafil group (intervention): Tadalafil 10 mg orally, twice daily started on the morning of the day before ascent to high altitude and continued until the end of the study 2. Dexamethasone group (intervention): Dexamethasone 8 mg twice daily started on the morning of the day before ascent to high altitude and continued until the end of the study 3. Placebo group (control): White gelatin capsules, identical in appearance, containing placebo, twice daily started on the morning of the day before ascent to high altitude and continued until the end of the study |
|
| Outcomes | 1. Primary outcome: Development of HAPE 2. Secondary outcomes: Incidence of AMS |
|
| Notes | 1. Trial Registration: Clinical Trials gov identifier: NCT00274430 2. Funder: The Hartmann‐Müller Foundation, the Pierluigi Crivelli Foundation, and the Anna Fedderson‐Wagner Funds (Switzerland) 3. Role of funder: "The funding sources did not influence the study design; the collection, analysis, or interpretation of the data; or the writing of the manuscript and its submission for publicatio"n 4. A priori sample size estimation: Yes.The group was not able to recruit 54 participants and decided to perform the study after 29 participants had been enrolled 5. Conducted: Not reported 6. Declared conflicts of interest: None disclosed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "...assigned to individual participants according to a computer‐generated list" (Page 498) |
| Allocation concealment (selection bias) | Low risk | Quote: "Before the study, the pharmacist at the University Hospital Zurich packaged the medication into numbered bottles, which were assigned to individual participants according to a computer‐generated list" (Page 498) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | quote: "Two physicians who were blinded to treatment assignment performed clinical examinations according to a predefined checklist in the mornings" (Page 498) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were excluded at follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Mirrakhlmov 1993.
| Methods | 1. Design: Parallel (2 arms) 2. Country: Kirguistán 3. Multisite: No 4. International: No 5. Treatment duration: 1 day 6. Follow‐up: Unclear 7. Rate of ascent: Unclear 8. Final altitude reached: 3200 metres 9. AMS scale: No |
|
| Participants | 16 participants with bronchial asthma were recruited Randomized (single‐blinded) into 2 groups: Control group (n = 8, 50%) Intervention group (n = 8, 50%) No participants randomized were excluded from the study No participants lost to follow‐up: Main characteristics of participants: Age (range): 22 ‐ 49 years Age (mean ± SD): Intervention group: 34 ± 3; and Control group: 32 ± 3 Number of men/women: 6 men (37.5%), 10 women (62.5%) Almost all participants had daily bouts of breathlessness, which were relieved by inhaled beta2‐agonist 5 participants were treated with small doses of prednisolone |
|
| Interventions | 1. Control group: Anti‐asthmatic treatment (control group) 2. Intervention group: Anti‐asthmatic treatment plus acetazolamide 250 mg twice at day |
|
| Outcomes | Outcomes were not classified as primary or secondary 1. Severity of nocturnal hypoxaemia in asthmatic participants after the ascent to 3200 metres 2. Frequency and severity of AMS and of nocturnal hypoxaemia 3. Acclimatization to altitude by repeated overnight oximetry |
|
| Notes | 1. Trial Registration: Not stated 2. Funding: Not stated 3. Role of sponsor: Not stated 4. A priori sample size estimation: No 5. Conducted: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "..after the initial investigations, patients were randomly divided.." (Page 537) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | No other biases were identified |
Montgomery 1989.
| Methods | 1. Design: Double‐blind, randomized study 2. Country: Colorado (Snowmass, Steamboat Springs) USA 3. Multisite: Yes 4. International: No 5. Treatment duration: Unclear 6. Follow‐up: 5/6 days 7. Rate of ascent: Unclear 8. Final altitude reached: 2700 and 2050 metres 9. AMS scale: AMS score unclear |
|
| Participants | 73 persons, mainly health professionals, mostly physicians were recruited and randomized to receive: Dexamethasone (n = 38, 52%) Placebo (n = 35, 48%) No participants were lost to follow‐up or excluded Participant characteristics: Placebo n = 35 (14 women, 21 men), age 37.9 ± 7.8 years Dexamethasone n = 38 (10 women, 28 men), age 35.8 ± 6.5 years |
|
| Interventions | 4 mg of dexamethasone acetate or an identical‐appearing placebo every 6 hours for 6 doses Drug administration began within 3 hours after arrival at the ski resorts |
|
| Outcomes | AMS symptoms and incidence | |
| Notes | 1. Trial Registration: Not stated 2. Funder: Merck Sharpe & Dohme 3. Role of funder: To provided the dexamethasone and the placebo 4. A priori sample size estimation: No 5. Conducted: January 1986 and February 1987 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote " .... was randomized... " (Page 735) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Possible industry bias |
Moraga 2007.
| Methods | 1. Design: Randomized, open‐label, placebo‐controlled trial 2. Country: Chile 3. Multisite: No 4. International: Yes 5. Treatment duration: 4 days 6. Follow‐up: 4 days 7. Rate of ascent: Began 0830 hours from Antofagasta (sea level) via highway. Arrival at Calama (2400 metres) at 1230 hours was followed by a 1‐hour stop, and arrival at Ollagüe was at 1700 hours. Travel time was approximately 8½ hours 8. Final altitude reached: 3696 metres 9. AMS scale: Lake Louise Questionnaire |
|
| Participants | 50 participants enrolled (students from the Medical College at the University of Antofagasta voluntarily consented to participate in the study). 13 students were excluded for having previous experience with high altitude. 2 were evaluated by physicians and were excluded for having incidents of seizure and recent pneumonia 36 participants randomized to: Gingko biloba (12, 33%) Acetazolamide (12, 33%) Placebo (12, 33%) No participants were excluded No participants were lost to follow‐up Main characteristics of participants: Age (median/mean‐ Percentiles 5/95, SD): Placebo 22.2 ± 1.1 Acetazolamide 23.3 ± 1.2 Ginkgo biloba 22.1 ± 2.9 Percentage/number of women/men: all men Percentage/number History of AMS: None |
|
| Interventions | 1. Ginkgo biloba group (intervention): Ginkgo biloba extract Egb761 80 mg/12 hours. Administration route unspecified. At sea level a month before ascending to high altitude for 3 days, at high altitude 24 hours before ascending and continued for 3 days 2. Placebo group (control): Administration route unspecified. At sea level a month before ascending to high altitude for 3 days, at high altitude 24 hours before ascending and continued for 3 days 3. Acetazolamide group (control): Acetazolamide 250 mg/12 hours. Administration route unspecified. At sea level a month before ascending to high altitude for 3 days, at high altitude 24 hours before ascending and continued for 3 days |
|
| Outcomes | Primary outcome was assessment of AMS through the Lake Louise Questionnaire measurement at sea level and at 3696 metres | |
| Notes | 1. Trial Registration: Not stated 2. Funding: Grant PEI‐1332 Project given by the Investigation Unit at the University of Antofagasta, Chile 3. Role of sponsor: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "randomization was computer generated" (Page 252) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Muza 2004.
| Methods | 1. Design: Randomized, double‐blind, placebo‐controlled cross‐over trial 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 2 days 6. Follow‐up: 24 hours during each test phase 7. Rate of ascent : 45 mmHg/minute 8. Final altitude reached: 4300 metres 9. AMS scale: ESQ‐C score and the Lake Louise AMS Scoring System (LLS) |
|
| Participants | 12 participants enrolled (volunteers lifelong low‐altitude residents and had no exposure to altitudes greater than 1000 metres for at least 6 months immediately preceding the study. All were US Army personnel who participated in regular physical training and were of average fitness. All volunteers received medical examinations, and none was found to have any condition that would warrant exclusion from the study) 1 participant excluded. No reason given Randomized to: Montelukast (n = 11) Placebo (n = 11) No participants randomized were excluded or lost to follow‐up Main characteristics of participants: Age 24 ± 4 years 9 men, 2 women Percentage/number History of AMS: None Percentage/number Type of HAI reported: None |
|
| Interventions | 1. Intervention group: Montelukast 10 mg was given orally at 08:00 at beginning of a test phase and the second 10 mg dose was given about 24 hours later, just prior to decompressing the chamber to simulated altitude 2. Placebo group (control): An identical‐appearing tablet containing lactose was ingested on the same schedule during its corresponding test phase |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. AMS assessed by ESQ‐C score and LLS score 2. Specific ventilatory, cardiovascular,body fluid, and other physiologic parameters indicative of the early acclimatization process 3. Markers of inflammation and hypoxic stress |
|
| Notes | 1. Trial Registration: Not stated 2. Funding: This investigation was supported by the U.S. Army Medical Research and Materiel Command. Additional support was received from Merck & Co 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: received for review in July 2002 6. Declared conflicts of interest: Yes, none reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized controlled trial" (Page 413) Insufficient information to score this item as low or high risk of bias. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 participant (8.3%) was excluded from analyses |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials |
PACE 2006.
| Methods | 1. Design: Parallel (3 arms) 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: 6 days 6. Follow‐up: 24 hours 7. Rate of ascent: Average = 354 metres/day 8. Final altitude reached: 4928 metres 9. AMS scale:Lake Louise questionnaire |
|
| Participants | 222 participants enrolled (healthy non‐Nepali participants between 18 and 65 years of age with no acute infections who had not slept higher than 2700 metres or taken acetazolamide within the last 2 weeks) Randomized to: 250 mg acetazolamide group (74, 33.3%) 750‐mg group (82, 37%) Placebo (66, 29.7%) 18 participants lost to follow‐up (12%). Reasons not provided Main characteristics of participants: Age (mean, SD): placebo = 38, 11.4; 250 mg acetazolamide group = 36.8, 11; 750 mg acetazolamide group = 38.9, 12.6 Percentage of men: placebo = 69.5%; 250 mg acetazolamide group = 65.7%; 750 mg acetazolamide group = 60.3% Percentage of History of severe altitude illness: Placebo = 11.9%; 250 mg acetazolamide group = 4.5%; 750 mg acetazolamide group = 11.5% Baseline oxygen saturation (mean, SD): Placebo = 90.9, 2.8; 250 mg acetazolamide group = 91.4, 2.8; 750 mg acetazolamide group = 91.4, 3 |
|
| Interventions | 1. 250 group (intervention ): 125 mg oral twice a day for 6 days 2. 750 group (intervention ): 375 mg oral twice a day for 6 days 3. Placebo group (control): placebo capsules oral twice day for 6 days Co‐interventions : Not reported |
|
| Outcomes | Primary outcomes 1. Composite incidence and severity of AMS as measured by the LLQ (AMS = 3+ points on LLQ; severe AMS = 5+ points on LLQ) Secondary outcomes 1. Composite headache incidence and severity 2. Oxygen saturation decrease from baseline to midpoint and endpoint as measured by resting pulse oximetry |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: These studies were supported by grant 3200‐0092.8 5 from the Swiss National Science Foundation 3. Role of funder: Not stated 4. A priori sample size estimation: Yes 5. Conducted: October ‐ November 2003 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Random treatment group assignment codes were prepared by Deurali‐Janata and placed in sealed opaque envelopes" (Page 19) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Low risk | Quote: "Random treatment group assignment codes were prepared by Deurali‐Janata and placed in sealed opaque envelopes" (Page 19) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote:"The placebo substance was visually identical to the acetazolamide, and both placebo and drug were packed in identical capsules" Page 19 Quote: "(...) in sealed opaque envelopes unavailable to the study administrators who enrolled the patients" (Page 19) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 12% of participants lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Unclear risk | Possible industry bias. Quote: "Commercial pharmaceutical‐grade acetazolamide was purchased from Wyeth Pharmaceuticals and placed in capsules by Deurali‐Janata Pharmaceuticals at their processing plant in Katmandu, Nepal" (Page 19) |
Parati 2013.
| Methods | 1. Design: Parallel (2 arms) 2. Country: Italy 3. Multisite: No 4. International: No 5. Treatment duration: 5 days 6. Follow‐up: 2 days 7. Rate of ascent (m/h): 4559/28 hours 8. Final altitude reached: 4559 metres 9. AMS scale: Lake Louise Score |
|
| Participants | 44 participants enrolled (healthy lowlanders without known cardiovascular disease, no chronic cardiovascular therapy, no history of severe mountain sickness, no recent exposure to altitudes > 2000 metres, and no contraindications to acetazolamide) Randomized to: Acetazolamide group (n = 22). 3 participants not analysed Placebo group (n = 22). 2 participants not analysed Main characteristics of participants: Age (median): acetazolamide group 35.6 ± 7.1; Placebo group 37.0 ± 9.5 Men: acetazolamide group n = 9; Placebo group n = 10 History of AMS: None Type of HAI reported: None |
|
| Interventions | 1. Acetazolamide group (intervention): acetazolamide 250 mg every 12 hours for 3 days at sea level and continued for 48 hours at high altitude 2. Placebo group (control): tablets every 12 hours for 3 days at sea level and continued for 48 hours at high altitude |
|
| Outcomes | 1. Primary outcome Central blood pressure, pulse wave velocity 2. Secondary outcome Arterial oxygen saturation Acute Mountain Sickness |
|
| Notes | 1. Trial Registration: EudraCT 2010‐019986‐27 2. Funder: Ministry of Health. IRCCS instituto auxologico italiano 3. Role of funder: Not stated 4. A priori sample size estimation: Yes 5. Conducted: Not stated 6. Declared conflicts of interest: Yes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Subjects were randomly assigned to receive PL or AC, 250 mg” (Page 760) Insufficient information to assess as low or high risk of bias for this item |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to assess as low or high risk of bias for this item |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to assess as low or high risk of bias for this item |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to assess as low or high risk of bias for this item |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5 participants (11%) were excluded from final analysis |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were detected |
PHAIT 2004.
| Methods | 1. Design: Parallel (4 arms) 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: 2 days 6. Follow‐up: Unclear 7. Rate of ascent: Unclear 8. Final altitude reached: 4928 metres 9. AMS scale: Lake Louise score |
|
| Participants | 614 trekkers were enrolled. They were healthy non‐Nepali men and women aged 18 ‐ 65 years travelling directly between the baseline villages of Pheriche or Dingboche (4280 metres and 4358 metres respectively) and the end point in Lobuje (4928 metres) Participants were excluded if they had acute mountain sickness, signs and symptoms of a substantial acute infection, had slept above 4500 metres, had taken ginkgo or acetazolamide within 2 weeks before enrolment, had any known cardiac, pulmonary, or other chronic disease that would render them at increased risk of altitude illness Randomized to: Placebo group (n = 151, 24.5%) Ginko group (n = 157, 25.5%) Acetazolamida group (n = 152, 24.7%) Combined acetazolamide and ginkgo group (n = 154, 25%) No participants randomized were excluded from analysis Participants lost to follow‐up: 127 (20.7%), uniformly distributed between groups Main characteristics of participants: Age (mean, SD): Placebo group: 36.4, 10.8 Acetazolamida group: 36.4, 11 Ginko group: 36.7, 10.5 Combined acetazolamide and ginkgo group: 36.7, 11.4 Number of men, %: Placebo group: 88, 74% Acetazolamida group: 79, 67% Ginko group: 83, 67% Combined acetazolamide and ginkgo group: 88, 70% |
|
| Interventions | 1. Ginkgo 120 mg twice daily 2. Acetazolamide 250 mg twice daily 3. Combined ginkgo 120 mg and acetazolamide 250 mg twice daily 4. Placebo twice daily |
|
| Outcomes | Primary outcome measure: 1. Incidence and severity of acute mountain sickness at the study end point as judged by the Lake Louise scoring system Secondary end points: 1. Incidence and severity of headache 2. End point pulse oximetry |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Pharmaton provided financial support for study expenses 3. Role of funder: Financial support, manufactured Ginko extract 4. A priori sample size estimation: Yes 5. Conducted: between 6 October and 24 November 2002 7. Declared conflicts of interest: Yes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "the randomisation code was computer generated by Deurali‐Janta Pharmaceuticals (Kathmandu, Nepal) and held by an independent physician” (Page 2) |
| Allocation concealment (selection bias) | Low risk | Quote "the randomisation code was computer generated by Deurali‐Janta Pharmaceuticals (Kathmandu, Nepal) and held by an independent physician” (Page 2) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: “The 127 participants (20.7%) lost to follow up…” (Page 2) |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected. |
| Other bias | Unclear risk | Possible industry bias: The sponsor manufactured the Ginko extract used |
Rock 1987.
| Methods | 1. Design: Paralell (2 arms) 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 96 hours 6. Follow‐up: 6 days 7. Rate of ascent: 708.3. Travel by helicopter in < 6 hours 9. Final altitude reached: 4300 metres 10. AMS scale: ESQ‐C, ESQ‐R, Hackett score, Jhonson Score |
|
| Participants | 16 men enrolled ((volunteers; lifelong sea level residents without exposure to altitudes > 1000 metres for at least 6 months prior to their participation) Exclusion criteria: Any illness or medical contraindication to altitude exposure or to dexamethasone administration Randomized to: Control group (9, 56%) Intervention group (7, 44%) 1 participant randomized was excluded from the control group for chest pain No participants lost to follow‐up Main characteristics of participants: Age (range): 16 ‐ 26 years Number of men/women: 100% men |
|
| Interventions | 1. Treatment group (intervention): 4 mg dexamethasone orally every 6 hours for 48 hours at sea level and 48 hours after arrival at high altitude 2. Control group (control): identically‐appearing placebo orally with the same schedule |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. AMS symptoms by several scales 2. Haematocrit and haemoglobin |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Subjects had been assigned at random to either a treatment or control.." (Page 669) Insufficient information to score this item as low or high risk of bias. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "control group followed the same drug altitude schedule, but received an identically appearng placebo" (Page 669) Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "At the time of each assessment the physicians were unaware of which treatment the subject was receiving" (Page 669) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 participant (6.25%) was excluded from further analyses |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | No other biases were identified |
Rock 1989a.
| Methods | 1. Design: Cross‐over. 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 52 hours 6. Follow‐up: Unclear 7. Rate of ascent: 600 metres/minute. Hypobaric chamber 8. Final altitude reached: 4570 metres 9. AMS scale: ESQ, AMS‐C, AMS‐R, Johnson scale |
|
| Participants | 30 young, healthy men, lifelong residents at low altitude, without any prolonged exposure to altitudes > 2500 metres in the 6 months immediately preceding the study were randomized. 2 of them were unable to participate and 3 were excluded
Exclusion criteria: not stated Randomized to Dexamethasone 0.25 mg (n = 8) Placebo. Each subject served as their own control 2 participants randomized were excluded from analysis, because they were unable to participate for personal reasons, prior to the beginning of testing 3 participants lost to follow‐up: 2 were excluded for viral illness and one withdrew for administrative reasons. The data from these 3 individuals were not included in the analysis Main characteristics of participants: Age (mean, SD): 22.3, 2.4 years Number of men: 100% |
|
| Interventions | 1. Dexamethasone 0.25 mg orally every 12 hours 2. Placebo identically‐appearing, containing lactose. orally every 12 hours Exposures into the chamber were 3 weeks apart |
|
| Outcomes | This trial did not state primary or secondary outcome 1. AMS incidence 2. Physiological variables such as haemoglobin, plasma volume, urine output 3. Cortisol levels |
|
| Notes | 1. Trial Registration: Not stated. 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 4. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "30 subjects were assigned at random by an individual not involved in the data collection" (Page 569) Insufficient information to score this item as low or high risk of bias. |
| Allocation concealment (selection bias) | Low risk | Quote: "30 subjects were assigned at random by an individual not involved in the data collection" (Page 569) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Neither the subjects nor the investigators collecting the data were aware of which treatment the subjects were receiving during drug administration and data collection" (Page 569) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The clinical interview was performed by a physician (R.F.L.) who was unaware of the subject’s responses on the ESQ at the time of the interview" (Page 569) Quote: "Neither the subjects nor the investigators collecting the data were aware of which treatment the subjects were receiving during drug administration and data collection" (Page 569) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5 participants (16%) were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials. Possible industry bias |
Rock 1989b.
| Methods | 1. Design: Cross‐over. 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 52 hours 6. Follow‐up: Unclear 7. Rate of ascent: 600 metres/minute. Hypobaric chamber 8. Final altitude reached: 4570 metres 9. AMS scale: ESQ, AMS‐C, AMS‐R, Johnson scale |
|
| Participants | 1. 30 young, healthy men, lifelong residents at low altitude, without any prolonged exposure to altitudes > 2500 metres in the 6 months immediately preceding the study were randomized. 2 of them were unable to participate and 3 were excluded Exclusion criteria: not stated Dexamethasone 1 mg: 9 participants Placebo. Each participant served as their own control Two participants randomized were excluded from analysis, because they were unable to participate for personal reasons, prior to the beginning of testing 3 participants lost to follow‐up: 2 were excluded for viral illness and 1 withdrew for administrative reasons. The data from these 3 individuals were not included in the analysis 4. Main characteristics of patients: Age (mean, SD): 22.3, 2.4 years Number of men: 100% |
|
| Interventions | 1. Dexamethasone 1 mg orally every 12 hours 2. Placebo identically‐appearing, containing lactose, orally every 12 hours |
|
| Outcomes | This RCT did not state primary or secondary outcome 1. AMS incidence 2. Physiological variables such as haemoglobine, plasma volume, urine output 3. Cortisol levels |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "30 subjects were assigned at random by an individual not involved in the data collection" (Page 569) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Low risk | Quote: "30 subjects were assigned at random by an individual not involved in the data collection" (Page 569) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Neither the subjects nor the investigators collecting the data were aware of which treatment the subjects were receiving during drug administration and data collection" (Page 569) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The clinical interview was performed by a physician (R.F.L.) who was unaware of the subject’s responses on the ESQ at the time of the interview" (Page 569) Quote: "Neither the subjects nor the investigators collecting the data were aware of which treatment the subjects were receiving during drug administration and data collection" (Page 569) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5 participants (16%) were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials. Possible industry bias |
Rock 1989c.
| Methods | 1. Design: Cross‐over. 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 52 hours 6. Follow‐up: Unclear 7. Rate of ascent: 600 metres/minute. Hypobaric chamber 8. Final altitude reached: 4570 metres 9. AMS scale: ESQ, AMS‐C, AMS‐R, Johnson scale |
|
| Participants | 1. 30 young, healthy men, lifelong residents at low altitude, without any prolonged exposure to altitudes > 2500 m in the 6 months immediately preceding the study were randomized. 2 of them were unable to participate and 3 were excluded Exclusion criteria: not stated Dexamethasone 4 mg: 8 participants Placebo. Each participant served as their own control 2 participants randomized were excluded from analysis, because they were unable to participate for personal reasons, prior to the beginning of testing 3 participants lost to follow‐up: 2 were excluded for viral illness and 1e withdrew for administrative reasons. The data from these 3 individuals were not included in the analysis Main characteristics of participants: Age (mean, SD): 22.3, 2.4 years Number of men: 100% |
|
| Interventions | 1. Dexamethasone 4 mg orally every 12 hours 2. Placebo identically‐appearing, containing lactose, orally every 12 hours Exposures into the chamber were 3 weeks apart |
|
| Outcomes | This trial did not state primary or secondary outcome 1. AMS incidence 2. Physiological variables 3. Cortisol levels |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "30 subjects were assigned at random by an individual not involved in the data collection" (Page 569) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Low risk | Quote: "30 subjects were assigned at random by an individual not involved in the data collection" (Page 569) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Neither the subjects nor the investigators collecting the data were aware of which treatment the subjects were receiving during drug administration and data collection" (Page 569) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The clinical interview was performed by a physician (R.F.L.) who was unaware of the subject’s responses on the ESQ at the time of the interview" (Page 569) Quote: "Neither the subjects nor the investigators collecting the data were aware of which treatment the subjects were receiving during drug administration and data collection" (Page 569) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5 participants (16%) were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials. Possible industry bias |
Sartori 2002.
| Methods | 1. Design: parallel study (2 arms) 2. Country: Italy 3. Multisite: No 4. International: No 5. Treatment duration: 3 days 6. Follow‐up: Unclear 7. Rate of ascent: 155.8 metres/hour 8. Final altitude reached: 4559 metres 9. AMS scale: Lake Louise AMS scoring |
|
| Participants | 37 participants out of 51 with a previous event of HAPE (at least 1 radiographically‐documented episode of high‐altitude pulmonary oedema within the previous 4 years), were randomized to: Salmeterol group (n = 18, 48.6%) Placebo group (n = 19, 51.4%) No participants randomized were excluded from analysis or lost to follow‐up Main characteristics of participants: Age (mean, SD): Salmeterol group: 49.6 ± 10.2 Placebo group: 46 ± 12.6 Percentage of women/men: Salmeterol group 5/13 Placebo group 4/15 History of AMS (number of previous episodes): Salmeterol group 2.4 ± 1 Placebo group 1.9 ± 1.1 |
|
| Interventions | 1. Salmeterol group (intervention): 125 µg salmeterol every 12 hours with pressurized metred‐dose inhaler 2. Placebo group (control): inhaled placebo pressurized metred dose inhaler every 12 hours Both groups started on the morning of the day before began the ascent and continued until the end of the study Co‐interventions: Not reported |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. Incidence of HAPE 2. Lake Louise Score 3. Systolic pulmonary‐artery pressure (by echocardiography) 4. SaO2, PaO2, PaCO2 |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Swiss National Science Foundation (grants 32.46797.96 and 3238‐051157.97), the Placide Nicod Foundation, the Emma Muschamp Foundation, and the International Olympic Committee 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... were randomly assigned to inhale either..." (Page 1632) Insufficient information to score this item as low or high risk of bias. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
SPACE 2011.
| Methods | 1. Design: Parallel (3 arms) 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: 30 hours ‐ 4 days 6. Follow‐up: Unclear 7. Rate of ascent: Unclear 8. Final altitude reached: 5000 metres 9. AMS scale: Lake Louise score |
|
| Participants | 311 participants enrolled (healthy men and women between 18 and 65 years without AMS or any concurrent illness and not taking acetazolamide Exclusion criteria: Mild AMS (more than 1 mild symptom on the LLS); significantly depressed oxygen saturation (< 75%); pregnancy or those who could not exclude the possibility of being pregnant or have missed menses by over 7 days; history of allergy to acetazolamide or other sulfa drugs; individuals who were on ACE inhibitors (e.g. enalapril) or other diuretics (e.g. amiloride or triamterene); individuals who had spent 24 hours at an altitude of 4500 metres (14,000 feet) within the last 9 days; individuals known to have taken any of the following in the prior 2 days: acetazolamide (Diamox), steroids (dexamethasone, prednisone), theophylline, or diuretics (furosemide); individuals failing to provide informed consent at the study enrolment site at Pheriche Randomized to: 114 Spironolactone, 36.6% 118 Acetazolamide, 37.9% 79 Placebo , 25.4% 25 participants randomized (8%, uniformly distributed) were excluded from analysis because they violated the protocol: Acetazolamide group (8, 7,7 %) Spironolactone group (10, 9,8%) Placebo group (7, 9,8%) Participants lost to follow‐up: Acetazolamide group: n = 15, 12% Spironolactone group: n = 12, 10.5% Placebo group: n = 8, 10% Main characteristics of participants: Age (mean, SD): Acetazolamide group 37, 12.2 Spironolactone group 37.7, 12 Placebo group 39.4, 12.1 Number of men, %: Acetazolamide group 59 (62.1%) Spironolactone group 67 (62.8%) Placebo group 46 (71.9%) |
|
| Interventions | 1. Acetazolamide group (intervention): acetazolamide 250 mg twice a day orally for 4 days 2. Spironolactone group (intervention): Spironolactone 50 mg twice a day orally for 4 days 3. Placebo group (control ): placebo twice a day orally for 4 days |
|
| Outcomes | Primary outcome. Incidence and severity of AMS Secondary outcome: Incidence of headache together with severity of AMS SpO2 |
|
| Notes | 1. Trial Registration: ISRCTN77054547 2. Funder: Wellcome Trust, UK 3. Role of funder: Financial support 4. A priori sample size estimation: no 5. Conducted: October 6 and November 24, 2007 6. Declared conflicts of interest: no |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote : “randomization of spironolactone, acetazolamide, and placebo was conducted by Deurali‐Janta Pharmaceuticals Pvt. Ltd” (Page 17) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Quote : “randomization of spironolactone, acetazolamide, and placebo was conducted by Deurali‐Janta Pharmaceuticals Pvt. Ltd” (Page 17) Quote: "Three sealed master lists of the randomization code were held by the manufacturer, an independent clinician at the Nepal International Clinic in Katmandu, and an independent clinician at the aid post in Pheriche (study enrollment location)" (Page 17) |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Around 10 ‐ 12% of participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participaent‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Subudhi 2011.
| Methods | 1. Design: Cross‐over design (3 arms) 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 2 days 6. Follow‐up: Unclear 7. Final altitude reached: simulated altitude of 4875 metres 8. AMS scale: Lake Louise Score |
|
| Participants | 29 healthy volunteers who had resided at 1650 metres for at least 1 year were screened. All had to accept each treatment. Acetazolamide 250 mg Dexamethazone 4 mg Placebo Exclusion criteria: recent (1 month) exposure to altitudes above 2500 metres; medical conditions affected by hypoxia, or poor aerobic fitness 9 participants (31%) randomized dropped out of the study "due to the large time commitment required to obtain an additional trial" (Page 1220). They were excluded from the analysis Participants lost to follow‐up: None stated Main characteristics of participants: Age (mean, SD): age not stated Number of men, %: 16, 80% |
|
| Interventions | 1. Acetazolamide 250 mg every 8 hours 2. Dexamethazone 4 mg every 8 hours 3. Placebo every 8 hours |
|
| Outcomes | This trial does not state primary or secondary outcomes 1. Physiological cardiopulmonary variables: heart rate, SpO2, pulmonary function 2. Cerebral haemodynamic variables: Cerebral blood flow (doppler), critical closing pressure; resistance area product; cerebral vasomotor reactivity to CO2; cerebrovascular conductance index 3. AMS score self‐reported |
|
| Notes | 1. Trial Registration: Not reported 2. Funder: National Heart, Lung, and Blood Institute, Marren Foundation and the Altitude Research Center 3. Role of funder: Financial support 4. A priori sample size estimation: Not stated 5. Conducted: Unclear 6. Declared conflicts of interest: Yes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "Using a randomized, double‐blind, placebo controlled, crossover design, we evaluated..." (Page 1220) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 31% (9/29) of participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | It is unclear if previous events of HAI (specifically in phase 1) affected the probability of new events in second phase of cross‐over trials. Possible industry bias |
Van Patot 2008.
| Methods | 1. Design: Parallel (2 arms) 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: Unclear 7. Rate of ascent: Unclear 8. Final altitude reached: 4300 metres 9. AMS scale: Lake Louise score and ESQ AMS‐C |
|
| Participants | 44 participants who resided between 1400 and 1600 metres were randomized to: Acetazolamide n = 22, 50% Placebo n = 22, 50% Exclusion criteria: Pregnancy; history of cardiac/pulmonary disease (except asthma); alcohol consumption within 24 hours prior to ascent; current viral illness; if they had been above 2000 metres for more than 1 day in the preceding 2 weeks No participants randomized were excluded from analysis Participants lost to follow‐up: None Main characteristics of participants: Age (years): Mean (SD): Acetazolamide: 22.9 (5.37) Placebo: 23.7 (6.29) Sex (% men): 56% (18/33) Acetazolamide 52% Placebo 43% |
|
| Interventions | 1. Acetazolamide 125 mg twice a day for 3 days prior to ascent and for 24 hours while at high altitude 2. Placebo (lactulosa) twice a day for 3 days prior to ascent and for 24 hours while at high altitude |
|
| Outcomes | Primary outcome: 1. Incidence and severity of AMS based on the AMS‐C score and Lake Louise Symptom score Secondary outcome: 1. Oxygen saturation and heart rate |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Technical Sourcing International, the Wilderness Medicine Society, and the American Academy of Family Physicians Foundation 3. Role of funder: Financial support 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Yes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote "...randomized to either acetazolamide or placebo treatments using a random‐number assignment program" (Page 290) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Wang 2013.
| Methods | 1. Design: Prospective intervention study 2. Country: China 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: Unclear 7. Rate of ascent: None 8. Final altitude: 3651 metres 9. AMS scale: Lake Louise Score |
|
| Participants | 21 healthy young men (22 ‐ 26 years old) with the following characteristics were recruited: altitude of permanent residence less than 900 metres; no high‐altitude exposures (≥ 2500 metres) in the preceding 2 years; no tobacco or recreational drug use; not taking medications that might affect cognitive function or carbonic anhydrase activity; no chronic or genetic diseases; being willing to participate in the study and take the medicine provided; no history of allergy to sulfonamides Randomized to: Acetazolamide group (n = 11, 52.3%) Placebo (n = 10, 47.6%) Main characteristics of participants: Age (mean): 19.2 (range 14 ‐ 22 years old) Percentage/number of women/men: 21 men (100%) |
|
| Interventions | 1. Acetazolamide 125 mg twice daily, for 4 days 2. Placebo twice daily for 4 days |
|
| Outcomes | Outcome were not classified as primary or secondary. 1. AMS at high altitude 2. Effects of acute high‐altitude exposure on neuropsychological performance 3. Effects of acetazolamide on neuropsychological performance |
|
| Notes | 1. Trial Registration: not stated 2. Funder: "This study was sponsored by the National Key Technology R&D Program (2009BAI85B04), the National Nature Science Foundation of China (81172621), and the Program for Changjiang Scholars and Innovative Research Team in University (PCSIRT)" 3. A priori sample size estimation: No 4. Conducted: Not stated 5. Declared conflicts of interest: Yes. None declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Twenty‐one volunteers were randomized into the acetazolamide group (n = 11) and the placebo group (n = 10)” (Page 29) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Both performers and subjects were blind to treatment assignment during the trial” (Page 29) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Low risk | No other biases were identified |
Wright 1983.
| Methods | 1. Design: Parallel (2 arms) 2. Country: Kenya 3. Multisite: No. 4. International: No. 5. Treatment duration: 18 days 6. Follow‐up: 10 days 7. Rate of ascent: Unclear 8. Final altitude reached: 4985 (14 participants) or 5188 metres (6 participants) 9. AMS scale: Standard series of questions, clinical assessment |
|
| Participants | 20 participants enrolled (normally resident at less than 200 metres, none had travelled to high altitude within the previous 6 months) Exclusion criteria: not stated Randomized to: Acetazolamide group (10, 50%) Methazolomide (10, 50%) None of the participants randomized were excluded from analysis No participants lost to follow‐up Main characteristics of participants not stated Age (years): mean 36, range 22 ‐ 54 Number of men, %: 19, 95% |
|
| Interventions | 1. Acetazolamide group (intervention): 2 capsules of 250 mg of acetazolamide + inactive capsule daily 8 days before ascent and until the end of observation period (10 days) 2. Methazolomide group (control): 2 capsules of 50 mg of methazolamide + inactive capsule for the first 5 days and 3 capsules of 50 mg for the remaining 10 days |
|
| Outcomes | This RCT did not specify by primary or secondary outcomes 1. Clinical assessment of AMS 2. Blood gas measurements. PaO2, SaO2, PaCO2 3. Paraesthesia |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Lederle Laboratories, the Arthur Thompson Trust Fund, the West Midlands Regional Health Authority, and others (Page 621) 3. Role of funder: Financial support 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote " randomly allocated..." (Page 620) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Possible industry bias |
Wright 2004.
| Methods | 1. Design: Parallel (4 arms) 2. Country: Nepal 3. Multisite: No 4. International: No 5. Treatment duration: Unclear 6. Follow‐up: Unclear 7. Rate of ascent: Unclear 8. Final altitude reached: 5200 metres 9. AMS scale: Lake Louise self‐reporting AMS questionnaire |
|
| Participants | 24 participants enrolled (no information provided) Exclusion criteria: not stated Randomized to: Medroxyprogesterone group (6, 25%). Acetazolamide group (6, 25%). Acetazolamide + medroxyprogesterone group (6, 25%). Placebo group (6, 25%) 1 participant randomized to acetazolamide was excluded from analysis, because he descended with an unrelated illness No participants lost to follow‐up Main characteristics of participants not provided Age (years): range 22 ‐ 65 years Number of men, %: 92% |
|
| Interventions | 1. Medroxyprogesterone group (intervention): 3 tablets of 10 mg twice daily 2. Acetazolamide group (intervention): 250 mg twice daily + placebo (3 tablets twice daily) 3. Acetazolamide + medroxyprogesterone group (intervention): 250 mg twice daily + 3 tablets of 10 mg twice daily 4. Placebo group (control): 3 tablets of 50 mg twice daily |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. AMS incidence using LLS 2. AMS symptoms 3. Blood gases |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: The Wellcome Trust, the Arthur Thompson Trust, the Mount Everest Foundation, Ciba Corning Diagnostics UK and Upjohn Ltd (Page 30) 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not stated 6. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Study medications were randomized via computer‐generated code" (Page 237) |
| Allocation concealment (selection bias) | Low risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 22.7% of participants were lost to follow‐up and not include in final analysis |
| Selective reporting (reporting bias) | High risk | Participant‐important outcomes, such as adverse events, were not reported |
| Other bias | Unclear risk | Possible industry bias |
Zell 1988.
| Methods | 1. Design: Parallel (4 arms) 2. Country: USA 3. Multisite: No 4. International: No 5. Treatment duration: 4 days 6. Follow‐up: Unclear 7. Rate of ascent: Unclear 8. Final altitude reached: 4050 metres 9. AMS scale: ESQ |
|
| Participants | 32 participants enrolled (novice backpackers having no previous history of AMS and no recent travel to high altitudes) Exclusion criteria: Ongoing cardiopulmonary issues; Glucose intolerance or diabetes mellitus Randomized to: Dexamethasone group (n = 9) Acetazolamide (n = 7) Dexamethasone + acetazolamide group (n = 8) Placebo group (n = 8) Main characteristics of participants: Age (median): 18 ‐ 49 years for all groups Number of women/men: 12 women/20 men History of AMS: None |
|
| Interventions | 1. Dexamethasone group: dexamethasone acetate 4 mg orally every 6 hours for 96 hours 2. Acetazolamide group :Acetazolamide 250 mg twice a day oral for 96 hours 3. Placebo group: 2 vials of unmarked medications, 1 of which was taken twice a day and the other 4 times a day for 96 hours 4. Dexamethasone + acetazolamide group: Dexamethasone acetate 4 mg oral every 6 hours and acetazolamide 250 mg twice a day orally for 96 hours |
|
| Outcomes | This trial did not specify by primary or secondary outcomes 1. Incidence of AMS in recreational climbers to moderate altitudes 2. Prophylactic benefit of the 2 drugs 3. Safety profile of administering dexamethasone and acetazolamide under conditions of moderate altitudes and physical exertion |
|
| Notes | 1. Trial Registration: Not stated 2. Funder: Not stated 3. Role of funder: Not stated 4. A priori sample size estimation: No 5. Conducted: Not reported 6. Declared conflicts of interest: No |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote "Participants were randomly assigned ..." (Page 542) Insufficient information to score this item as low or high risk of bias |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information to score this item as low or high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Low risk | No other biases were identified |
Zheng 2014.
| Methods | 1. Design: Double‐blind randomized controlled trial 2. Country: China 3. Multisite: No 4. International: No 5. Treatment duration: 5 days 6. Follow‐up: Unclear 7. Rate of ascent: None 8. Final altitude: 3900 metres 9. AMS scale: Lake Louise Scoring System (LLS) |
|
| Participants | 138 healthy young men, lowland resident, were recruited Randomized into 3 groups: Budesonide group (n= 46; 33.3%) Dexamethasone (n= 46; 33.3%) Placebo (n= 46; 33.3%) 2. Loss to follow‐up: Before intervention, 10 participants were lost to follow‐up due to personal reasons (4, 3, and 3 in the budesonide, dexamethasone, and placebo groups, respectively) During intervention, 4 participants in the dexamethasone group encountered adverse reactions and discontinued medication before receiving any examination at altitude 124 participants completed the trial, whose data were included in analyses Main characteristics of participants: Age (mean): 20.3 years (range 18 ‐ 35 years old) Percentage/number of women/men: 100% men |
|
| Interventions | 1. Budesonide group: oral starch tablets + inhalation of budesonide (200 µg twice a day) 2. Dexamethasone group: empty inhalers + dexamethasone tablets (4 mg twice a day) 3. Placebo group received both inhaled and oral placebos |
|
| Outcomes | 1. Primary outcome measure was the incidence of AMS at altitude 2. Secondary outcome measures: Incidence of AMS in severe form, its severity reflected by Lake Louise Scoring System (LLS) score, heart rate, SpO2, spirometric parametres, sleep quality assessed by questionnaires, and adverse reactions related to the investigational drugs |
|
| Notes | 1. Trial Registration: not stated 2. Funder: This study was supported by the Special Health Research Project, Ministry of Health of P.R. China (grant No. 201002012) 3. A priori sample size estimation: Yes 4. Conducted: Not stated 5. Declared conflicts of interest: Yes. None declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “An independent physician randomly assigned the subjects to three groups: the budesonide, dexamethasone, and placebo groups, using a computer‐generated random number list with an allocation ratio of 1:1:1” (Page 1002) |
| Allocation concealment (selection bias) | Low risk | Quote: “An independent physician randomly assigned the subjects to three groups: the budesonide, dexamethasone, and placebo groups, using a computer‐generated random number list with an allocation ratio of 1:1:1” (Page 1002) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Empty inhalers could not be distinguished from budesonide inhalers by vision or feel. Starch tablets were similar to dexamethasone in shape, size, and color” (Page 1004) “The subjects, researchers, and other physicians were blinded” (Page 1004) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “The subjects, researchers, and other physicians were blinded” (Page 1004) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up : 4/42 in budesonide group (9.5%), 3/39 in dexamethasone group (7.7%), 3/43 in the placebo group (7%) |
| Selective reporting (reporting bias) | Low risk | Reporting bias was not detected |
| Other bias | Low risk | No other biases were identified |
ACTH = Adrenocorticotropic hormone; am = Ante meridiem/Before noon; AMS = Acute Mountain Sickness; AMS‐C = Acute Mountain Sickness score‐ cerebral subscale ; AMS‐R = Acute Mountain Sickness score‐ respiratory subscale; BP = Blood pressure; ESQ scores = Environmental Symptom Questionnaire; FVC = Forced vital capacity; g/dL = grams/decilitre; GHAQ = Generalized High Altitude Questionnaire; HACE = High altitude cerebral oedema; HAH = High altitude headache; HAI = High altitude illness; HAPE = High altitude pulmonary oedema; ITT = Intention‐to‐treat; IV = Intravenous; kg = Kilograms; LLQ = Lake Louise questionnaire; LLS = Lake Louise Scoring System; MAP = Mean artery pressure; mg = milligrams; NSAIDs = Nonsteroidal anti‐inflammatory drugs; PASP = Pulmonary Artery Systolic Pressure; PEF = Peak expiratory flow; pm = post meridiem: After noon; PH = degree of acidity or alkalinity of a solution; RCT = randomized controlled trial; SD = Standard deviation; SE = Standard error; SEM = standard error of the mean; VAS = Visual analogue scale.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACME‐1 2006 | The study is focused on treatment of high altitude illness |
| Agostoni 2013 | This study is not focused on prevention of high altitude illness |
| Bartsch 1993 | The study is focused on treatment of high altitude illness |
| Bilo 2015 | This study is not focused on prevention of high altitude illness |
| Bloch 2009 | Non‐randomized clinical trial |
| Broome 1994 | The study is focused on treatment of high altitude illness |
| Bärtsch 1994 | The study is focused on treatment of high altitude illness |
| Cain 1966 | This study is not focused on prevention of high altitude illness |
| Debevec 2015 | This study is not focused on prevention of high altitude illness |
| Dumont 1999 | This study is not focused on prevention of high altitude illness |
| Forster 1982 | This study is not focused on prevention of high altitude illness |
| Forwand 1968 | This study is not focused on prevention of high altitude illness |
| Fulco 2011 | This study is not focused on prevention of high altitude illness |
| Gertsch 2002 | This study is not focused on prevention of high altitude illness |
| Gray 1971 | The study is focused on treatment of high altitude illness |
| Harris 2003 | The study is focused on treatment of high altitude illness |
| Johnson 1988 | This study is not focused on prevention of high altitude illness |
| Jonk 2007 | This study is not focused on prevention of high altitude illness |
| Kotwal 2015 | This study is not focused on prevention of high altitude illness |
| Lalande 2009 | This study is not focused on prevention of high altitude illness |
| Lawley 2012 | The study is focused on treatment of high altitude illness |
| Levine 1989 | This study is not focused on prevention of high altitude illness |
| Liu 2013 | This study is not focused on prevention of high altitude illness |
| Mairer 2012 | This study is not focused on prevention of high altitude illness |
| McIntosh 1986 | This study is not focused on prevention of high altitude illness |
| Purkayastha 1995 | This study is not focused on prevention of high altitude illness |
| Reinhart 1994 | This study is not focused on prevention of high altitude illness |
| Sandoval 2000 | This study is not focused on prevention of high altitude illness |
| Scalzo 2015 | This study is not focused on prevention of high altitude illness |
| Serra 2001 | This study is not focused on prevention of high altitude illness |
| Siebenmann 2011 | This study is not focused on prevention of high altitude illness |
| Singh 1969 | The study is focused on treatment of high altitude illness |
| Solís 1984 | This study is not focused on prevention of high altitude illness |
| Suh 2015 | Non‐randomized clinical trial |
| Teppema 2007 | This study is not focused on prevention of high altitude illness |
| Vuyk 2006 | This study is not focused on prevention of high altitude illness |
| White 1984 | This study is not focused on prevention of high altitude illness |
| Wright 1988 | This study is not focused on prevention of high altitude illness |
Characteristics of studies awaiting assessment [ordered by study ID]
Dugas 1995.
| Methods | Double‐blind randomized study |
| Participants | 20 healthy volunteers received 5 mg of isradipine (n = 10) or placebo (n = 10) for 8 days. After 5 days of treatment in normoxia, the participants were rapidly transported to an altitude of 4350 m |
| Interventions | Israpadine (calcium channel blocker) and placebo |
| Outcomes | AMS symptom score, haemodynamic parameters and renal function |
| Notes | Full text not available (January 2016) |
Ellsworth 1987.
| Methods | Double‐blind randomized study |
| Participants | 47 climbers participated in this double‐blind, randomized trial comparing acetazolamide 250 mg, dexamethasone 4 mg, and placebo every 8 hours as prophylaxis for acute mountain sickness during rapid, active ascent of Mount Rainier (elevation 4392 metres). 42 participants (89.4 %) achieved the summit in an average of 34½ hours after leaving sea level |
| Interventions | Acetazolamide 250 mg, dexamethasone 4 mg, and placebo every 8 hours |
| Outcomes | Acute mountain sickness, symptoms reported |
| Notes | Full text not available (January 2016) |
Furian 2016.
| Methods | Double‐blind randomized placebo‐controlled trial |
| Participants | 112 COPD patients were studied in Bishkek (760 m), Kyrgyz Republic, after travelling for 6 hours to Tuja Ashu clinic (3200 m) and staying there for 3 days. |
| Interventions | Participants received dexamethasone (2 x 4 mg/d) or placebo before ascent and during stay at 3200 metres |
| Outcomes | Cumulative incidence of 1 of the following: AMS (AMSc environmental symptom cerebral score ≥ 0.7), severe hypoxaemia (SpO2 < 75% for > 30 mins) or discomfort requiring descent to low altitude. |
| Notes | Full text not available (January 2017) |
Hefti 2014.
| Methods | Double‐blind placebo‐controlled trial |
| Participants | 29 participants were assigned to a treatment group (14) receiving 800 IU vitamin E, 1000 mg vitamin C, 200,000 IU vitamin A, and 600 mg N‐acetylcystein daily, starting 2 months prior to the expedition, or to a placebo group (15) |
| Interventions | Vitamin group and placebo |
| Outcomes | AMS scores, Levels of endothelial microparticles |
| Notes | Full text not available (January 2016) |
Kasic 1991.
| Methods | Randomized study |
| Participants | 24 people who presented with acute mountain sickness |
| Interventions | A simulated descent of 1432 m (4600 ft) was attained by placing the participants in a fabric hypobaric chamber and pressurizing the chamber to 120 mmHg above ambient pressure. Participants were randomly assigned to either the hypobaric treatment or treatment with 4 litres of oxygen given by facemask; both treatments lasted for 2 hours |
| Outcomes | Mean arterial oxygen saturation (SaO2), symptoms of acute mountain sickness |
| Notes | Full text not available (January 2016) |
Lee 2011.
| Methods | Randomized trial |
| Participants | 19 adolescents aged 13 ‐ 18 years attempting an ascent of Mount Kalapatar (5500 m) |
| Interventions | Acetazolamide, methazolamide. |
| Outcomes | Incidence of AMS, oxygen saturation and pulse rate |
| Notes | Full text not available (January 2017) |
Pun 2014.
| Methods | Prospective double‐blind placebo‐controlled randomized trial |
| Participants | 358 pilgrims were recruited at Dhunche (1950 metres) and followed up at Chandanbari (3350 m), and up to the sacred lake Gosaikunda. Most of these pilgrims ascended from Dhunche to the lake in 2 ‐ 3 days |
| Interventions | Low‐dose acetazolamide (125 mg) and placebo |
| Outcomes | Lake Louise score (LLS) for AMS measurement, arterial oxygen saturation (SpO2) and heart rate |
| Notes | Full text not available (January 2016) |
Roncin 1996.
| Methods | Randomized trial |
| Participants | 44 participants were enrolled in a study of the preventive effect of Ginko biloba extract (EGb 761) on acute mountain sickness (AMS) and vasomotor changes of the extremities during a Himalayan expedition |
| Interventions | Ginko biloba extract (EGb 761) 160 mg and placebo |
| Outcomes | ESQ score and the cold gradient measured by photoplethysmography |
| Notes | Full text not available (January 2016) |
Swenson 1997.
| Methods | Randomized trial |
| Participants | 19 healthy volunteers were assessed, who ingested in randomized order both a high carbohydrate (68% CHO) or normal carbohydrate (45% CHO) diet for 4 days. On the 4th day, participants were exposed to 8 hours of 10% normobaric oxygen |
| Interventions | High carbohydrate (68% CHO) or normal carbohydrate (45% CHO) diet for 4 days |
| Outcomes | Lake Louise Consensus Questionnaire, interleukins 1 beta, 6 and 8 (IL‐1 beta, IL‐6, IL‐8) and tumour necrosis factor alpha (TNF‐alpha) |
| Notes | Full text not available (January 2016) |
Utz 1970.
| Methods | None known |
| Participants | None known |
| Interventions | None known |
| Outcomes | None known |
| Notes | Full text not available (January 2016) |
Wang 1998.
| Methods | Randomized trial |
| Participants | 65 men |
| Interventions | Conventional therapy group received oxygen, intravenous furosemide, aminophylline and dexamethasone; nifedipine group received oral nifedipine (10 mg, three times a day) in addition to conventional therapy; and participants in the nitric oxide group received nitric oxide (10 ppm) inhalation for 30 mins, in addition to oral nifedipine |
| Outcomes | Pulmonary rales on auscultation and shadows on chest radiograph |
| Notes | Full text not available (January 2016) |
Xiangjun 2014.
| Methods | Randomized trial |
| Participants | 80 healthy young male plain residents (17 ‐ 33 years old) |
| Interventions | Inhalation of budesonide (200 μg twice a day), procaterol tablet (25 μg twice a day), inhalation of budesonide/fomoterol (160 μg/4.5 μg, twice a day) or placebo (1 tablet, twice a day) |
| Outcomes | Lake Louis AMS questionnaire, blood pressure, heart rate, and oxygen saturation. |
| Notes | Full text not available (January 2017) |
AMS:Acute Mountain Sickness; CHO: Carbohydrate; EGb 761: Extract of Ginkgo biloba 761; ESQ: Environmental Symptom Questionnaire; HR: Heart rate; IL: Interleukine; LLS: Lake Louise score; mg: milligrams; min: minutes; ppm: parts per million; TNF: Tumor necrosis factor.
Characteristics of ongoing studies [ordered by study ID]
ChiCTR‐TRC‐13003319.
| Trial name or title | Oral zolpidem for improving sleep and then prevention of acute mountain sickness: a single centre, randomized, double‐blind, controlled, prospective trial |
| Methods | Interventional |
| Participants |
Inclusion criteria: 1. Aged between and including 18 and 35 years 2.People rapidly ascending to high altitude. The gender ratio depends on actual situation 3.There is no history of plateau for a long time exposure 4. Before assessment, all participants must be voluntary and sign a written informed consent Exclusion criteria: 1. Recent history of taking sleeping pills 2. Engaged in specialized sports training 3. Participants cannot take the drugs in our trial because of allergic history or other reasons. 4. Participants with bad compliance 5. Participants with serious illnesses, e.g. sleep apnoea 6. Recent history of upper respiratory tract infection 7. The driver 8. Participants with psychological or neurological disorder, and other conditions which are not appropriate for our trial Gender: both |
| Interventions | Experimental:Oral zolpidem (10 mg,qd, oral) Control: Oral placebo, the same dosage as oral zolpidem |
| Outcomes | Lake Louise Score |
| Starting date | 30 June 2013 |
| Contact information | Huang Lan |
| Notes | Recruiting |
ChiCTR‐TRC‐13003590.
| Trial name or title | The meaning of intravenous iron supplementation in acute mountain sickness: a randomized, double‐blinded, placebo‐controlled trial |
| Methods | Interventional |
| Participants |
Inclusion criteria: 1. Healthy people ready to travel from Beijing to Tibet by air 2. Participants knowing the aim of the study and giving informed consent. Exclusion criteria: 1. Not finishing the procedure 2. Coronary heart disease, uncontrolled hypertension and other severe diseases 3. Anaemia, especially iron deficiency anaemia Age minimum: 18 years old Age maximum: 65 years old Gender: Both |
| Interventions | Intervention group: Intravenous iron 200 mg Control: Placebo |
| Outcomes | Serum iron; Lake Louise score |
| Starting date | 30 July 2013 |
| Contact information | Ren Xuewen |
| Notes | Recruiting |
NCT00886912.
| Trial name or title | Prevention of acute mountain sickness by intermittent hypoxic training |
| Methods | Interventional |
| Participants |
Inclusion criteria: 1. Healthy 2. Non‐smoker 3. Endurance training minimum twice a week Exclusion criteria: 1. Any diseases 2. Previous exposure to altitudes higher than 2000 metres (last 6 weeks) Age minimum: 18 years old Age maximum: 55 years old Gender: Both |
| Interventions | 1. Hypoxia 2. Normoxia |
| Outcomes | Incidence of acute mountain sickness (time frame: after 20 hours at 4559 metres) Severity of acute mountain sickness (time frame: after 20 hours at 4559 metres) |
| Starting date | June 2008 |
| Contact information | Kai Schommer, MD |
| Notes | Recruiting |
NCT01606527.
| Trial name or title | Prospective, double‐blind, randomized, placebo‐controlled trial of ibuprofen versus placebo for prevention of neurologic forms of altitude sickness |
| Methods | Evaluating ibuprofen versus placebo for the prevention of neurological forms of altitude illness, including high altitude headache (HAH), acute mountain sickness (AMS), high altitude cerebral edema (HACE) and High Altitude Anxiety |
| Participants | The study will take place in the spring and summer of 2012 at the Marine Corps Mountain Warfare Training Center in the Eastern Sierras near Bridgeport, California. US Marines from near sea level will participate in battalion‐level training exercises at between 8500 and 11,500 feet, where some altitude illness is expected |
| Interventions | Ibuprofen 600 mg orally three times daily Placebo, same schedule |
| Outcomes | Change in the incidence of AMS as measured on the Lake Louise AMS Questionnaire
Change in High Altitude Headache measured by a visual analogue scale (VAS)
Change in cognitive performance as measured by King‐Devick
Change in the presence of anxiety and somatic symptoms using the BSI‐12 screening tool
Change in the oxygen concentration using pulse oximetry
Change in hydration status as measured by urine specific gravity
Change in HAH incidence and severity as measured on the Lake Louise AMS Questionnaire
Change in cognitive performance as measured by the Quickstick
Change in the presence of anxiety and somatic symptoms using the GAD‐2 screening tool Incidence of severe AMS as measured by a score of 6 or more on the Lake Louise AMS Questionnaire |
| Starting date | July 2012 |
| Contact information | Jeffrey Gertsch MD, Naval Health Research Center |
| Notes | The recruitment status of this study is unknown. The completion date has passed and the status has not been verified in more than 2 years. |
NCT01682551.
| Trial name or title | Evaluation of the prevention and treatment effects of Chinese medicine on high altitude illness |
| Methods | Interventional |
| Participants |
Inclusion criteria: 1. Healthy adults Exclusion criteria: 1. Chronic disease: cardiovascular disease, psychological disease, anaemia, migraine 2. Long‐term use of the following materials: Chinese herbs, steroid, antibiotics 3. Altitude acclimation: have been to mountain over 2000 metres in the past month 4. Pregnancy Age minimum: 20 years Age maximum: 70 years Gender: Both |
| Interventions | Drug: acetazolamide Drug: Chinese Medicine |
| Outcomes | Incidence of acute mountain sickness will be measured by the Lake Louise Self Report (Lake Louise Score = 4 with headache) (time frame: the Lake Louise Score will be measured at 12 pm of the second day after hiking to determine the onset of AMS) Arterial oxygen saturation (time frame: before and after the hiking) Blood pressure (time frame: before and after the hiking) Heart rate (time frame: before and after the hiking) |
| Starting date | September 2012 |
| Contact information | Not stated |
| Notes | Not yet recruiting |
NCT01794078.
| Trial name or title | A randomized, 4‐sequence, double‐blind study to test the safety of combined dosing with aminophylline and ambrisentan in exercising healthy human volunteers at simulated high altitude |
| Methods | Interventional |
| Participants |
Inclusion criteria: 1. Written informed consent to participate in the study prior to undergoing any screening procedures. The participant will be given a signed and dated copy of the informed consent 2. Participants must be healthy non‐smoking (for 6 months or longer at start of Cycle 1) adult male and female volunteers; at least 18 through 50 years at screening, with a BMI of 18 ‐ 33 kg/m2 and weighing at least 143 pounds. (65 kg). Participants' health status will be determined by medical history, physical examination, vital signs, ECG, blood chemistry, haematology, and urinalysis performed at screening 3. Be willing to fast for a minimum of 2 hours prior to screening 4. Be willing to abstain from alcohol and xanthine‐containing food and beverages from 48 hours before check‐in for each study day 5. Women who are of non‐childbearing potential must be: a) Surgically sterile (removal of both ovaries and/ or uterus at least 12 months prior to dosing) and with an FSH level at screening of 40 m IU/mL b) Naturally postmenopausal (spontaneous cessation of menses) for at least 24 consecutive months prior to dosing on Day 1, and with an FSH level at screening of 40 m IU/mL 6. Women of child‐bearing potential must have a negative serum or urine pregnancy test at screening, during the study, and must agree to avoid pregnancy during study and for 3 months after the last dose of study drug. Pregnancy is tested at screening, during check‐in of each testing cycle, during the follow‐up visit, and at any given point if deemed necessary by the physician or designate. During treatment, women of child‐bearing potential must use 2 acceptable methods of contraception at the same time unless she has had a documented tubal sterilization or chooses to use a Copper T 380A IUD or LNG 20 IUS, in which case no additional contraception is required. Abstinence is not considered a form of contraception. Medically acceptable contraceptives include: (1) documented surgical sterilization (such as a hysterectomy), (2) barrier methods (such as a condom or diaphragm) used with a spermicide, or (3) an intrauterine device (IUD) or intrauterine system (IUS) 7. Male participants must agree to take all necessary measures to avoid causing pregnancy in their sexual partners during the study and for 3 months after the last dose of study drug. Medically acceptable contraceptives include: (1) surgical sterilization (such as a vasectomy), or (2) a condom used with a spermicidal. Contraceptive measures such as Plan B (TM), sold for emergency use after unprotected sex, are not acceptable methods for routine use 8. Agree not to donate blood, platelets, or any other blood components 30 days, or plasma 90 days, prior to consenting and for 1 month after the last dose 9. Male participants must agree not to donate sperm during the study and for 12 weeks after the last dose Exclusion criteria: 1. People with laboratory results outside the normal range, if considered clinically significant by the physician or delegate. In addition, they must have a haemoglobin concentration of 12.0 g/dL 2. A mental capacity that is limited to the extent that the person cannot provide legal consent or understand information regarding the side effects of the study drug 3. Currently abusing drugs or alcohol or with a history of drug or alcohol abuse within the past 2 years 4. Unwillingness or unable to comply with the protocol, or to co‐operate fully with the physician and site personnel 5. Use of any of the following: a) Any concomitant medication including oral contraceptive hormones. People who have received any prescribed or non‐prescribed (over‐the‐counter) systemic medication, topical medications, or herbal supplements within 14 days from Day 1. St. John's Wort (hypericin) must not have been taken for at least 30 days prior to Cycle 1, Day 1 b) Any drugs, foods or substances known to be strong inhibitors or strong inducers of CYP enzymes (also known as cytochrome P450 enzymes) 6. Clinically significant ECG abnormality, in the opinion of the physician or delegate. 7. Vital signs or clinically significant laboratory values at the screening visit that in the opinion of the physician or delegate would make the person an inappropriate candidate for the study 8. A VO2 max value of less than 42 mL/kg/minute, as determined during exercise testing at screening. This value represents an educated estimate, and may be changed, to include new information, at the discretion of the physician 9. A history of, or otherwise indicated predisposition for, claustrophobia, i.e. the fear of closed, narrow spaces (because of the limited size of the high altitude chamber) 10. A history of "undeserved" altitude sickness, i.e. altitude sickness at only moderate altitude. This would consist of altitude‐related headaches, dizziness, or nausea during plane rides, or when travelling to moderately elevated locations of less than 2743.2 metres/9000 ft 11. Has taken any other investigational drug during the 30 days prior to the screening visit or is currently participating in another investigational drug clinical trial 12. Made any significant donation or had a significant loss of blood within 30, or donated plasma within 90 days of consenting 13. Receipt of a transfusion or any blood products within 90 days prior to start of Cycle 1 14. History or manifestation of clinically significant neurological, gastrointestinal, renal, hepatic, cardiovascular, psychological, pulmonary, metabolic, endocrine, haematologic or other medical disorders. For the purpose of the study, individual fitness and health are more important than family history of disease burden as a criterion for participation. For example, an individual may have significant family history of cardiovascular disease; however, the individual's active lifestyle makes a manifestation of such disease at a young age unlikely. To account for such expected variation, the ultimate decision whether to exclude or include an individual based on family history or manifestation of disease will be made by the physician. The physician may choose to use physiological assessments, such as, e.g. ECG, blood pressure, and VO2 max fitness level as an aid for decision‐making 15. Any condition that might interfere Age minimum: 18 years old Age maximum: 50 years old Gender: Both |
| Interventions | Drug: Ambrisentan 5 mg Drug: Aminophylline 400 mg |
| Outcomes | The safety of combined or single‐dose aminophylline and ambrisentan at simulated altitude in exercising adults (time frame: Safety endpoints will be measured during simulated high altitude (Cycle 2) at least 22 days post‐screening) The safety of combined or single‐dose aminophylline and ambrisentan at simulated high altitude in resting adults (time frame: Safety endpoints will be measured during an episode of simulated high altitude (Cycle 1), at least 7 days post‐screening) |
| Starting date | September 2013 |
| Contact information | Claude A Piantadosi, MD |
| Notes | Active, not recruiting |
NCT01993667.
| Trial name or title | Acetazolamide for the prevention of high altitude illness: a comparison of dosing |
| Methods | Interventional |
| Participants |
Inclusion criteria: 1. 18 years or older 2. English or Indian speaking 3. Mountaineers or trekkers who plan to climb Mount McKinley or trek to Base Camp on Mount Everest Exclusion criteria: 1. Low sodium and/potassium blood serum levels 2. Kidney disease or dysfunction 3. Liver disease, dysfunction, or cirrhosis 4. Suprarenal gland failure or dysfunction 5. Hyperchloremic acidoses 6. Angle‐closure glaucoma 7. Taking high‐dose aspirin (over 325 mg/day) 8. Any reaction to sulfa drugs or acetazolamide 9. Pregnant or lactating women |
| Interventions | Drug: Acetazolamide |
| Outcomes | Prevention of acute mountain sickness as measured by the Lake Louise Score (time frame: 1 year) Side effect profile of acetazolamide (time frame: 1 year) |
| Starting date | March 2012 |
| Contact information | Scott McIntosh, MD |
| Notes | Recruiting |
NCT02244437.
| Trial name or title | Ibuprofen versus acetaminophen in the prevention of acute mountain sickness: A double‐blind, randomized controlled trial |
| Methods | Interventional |
| Participants |
Inclusion criteria: Healthy adults between the ages of 18 and 65, men or women, non‐Nepali, without AMS or any concurrent illness, and not already taking NSAIDs and acetazolamide or any other drug for the prevention of altitude illness Exclusion criteria: Individuals not meeting inclusion criteria, including mild AMS (more than one mild symptom on the Lake Louise Questionnaire) or significantly depressed oxygen saturation (< 75%); women known to be pregnant, cannot exclude the possibility of being pregnant, or have missed menses by over 7 days; individuals who have spent 24 hours at an altitude of 4500 metres/14,000 feet within the last 9 days; anyone known to have taken any of the following in the last 2 days: acetazolamide (Diamox®), steroids (dexamethasone, prednisone), theophylline, or diuretics (Lasix®); individuals who have a known intracranial space‐occupying lesion or a history of elevated intracranial pressure, (i.e. tumours, hydrocephalus, etc) Age minimum: 18 years old Age maximum: 65 years old Gender: Both |
| Interventions | Drug: Acetaminophen Drug: Ibuprofen |
| Outcomes | Diagnosis of Acute Mountain Sickness (AMS) (Time Frame: Upon reaching 5000 metres altitude (Lobuche) of Nepal Himalaya) Blood Oxygen Saturation (SPO2) (time frame: Upon reaching 5000 metres altitude (Lobuche) of Nepal Himalaya) Heart Rate (HR) (time frame: Upon reaching 5000 metres altitude (Lobuche) of Nepal Himalaya) High Altitude Headache (HAH) (time frame: Upon reaching 5000 metres altitude (Lobuche) of Nepal Himalaya) |
| Starting date | October 2014 |
| Contact information | Nicholas C Kanaan, MD |
| Notes | Active, not recruiting |
NCT02450968.
| Trial name or title | Dexamethasone for prophylaxis of acute mountain sickness in people with chronic obstructive pulmonary disease travelling to altitude |
| Methods | Interventional |
| Participants |
Inclusion criteria: 1. Chronic obstructive pulmonary disease (COPD), GOLD criteria grade 1 ‐ 2 2. Living at low altitude (< 800 metres) Exclusion criteria: 1. COPD exacerbation 2. Severe COPD, GOLD grade 3 or 4 3. Arterial oxygen saturation < 92% at low altitude (< 800 metres) 4. Diabetes, uncontrolled cardiovascular disease such as systemic arterial hypertension, coronary artery disease; previous stroke; pneumothorax in the last 2 months 5. Untreated or symptomatic peptic ulcer disease, glaucoma, obstructive sleep apnoea 6. Internal, neurologic or psychiatric disease that interfere with protocol compliance including current heavy smoking (> 20 cigarettes a day). 7. Pregnant or nursing women Age minimum: 20 years old Age maximum: 75 years old Gender: Both |
| Interventions | Drug: Dexamethasone Drug: Placebo |
| Outcomes | Acute mountain sickness, cumulative incidence (time frame: day 3 at 3200 metres) 6 minutes walk distance (time frame: Day 2 at 3200 metres) Acute mountain sickness, severity (time frame: day 1, day 2, day 3 at 3200 metres) Arterial blood gases (time frame: Day 2 at 3200 metres) Perceived exertion (time frame: Day 2 at 3200 metres) |
| Starting date | May 2015 |
| Contact information | Talant M Sooronbaev, MD |
| Notes | Recruiting |
NCT02604173.
| Trial name or title | A randomized controlled trial of altitude sickness prevention and efficacy of comparative treatments |
| Methods | Interventional |
| Participants |
Inclusion criteria: 1. Men and women 2. Sea level‐dwelling hikers 3. Between ages 18 and 65 Exclusion criteria: 1. History of allergy to acetazolamide or budesonide (or other corticosteroids) 2. Taken NSAIDs, acetazolamide, or corticosteroids in the week prior to study enrolment 3. Hazardous medical conditions which preclude the ability to moderately hike to high altitude, including: sickle cell anaemia, asthma, or COPD, severe anaemia, or severe coronary arterial disease 4. Pregnancy or suspected pregnancy 5. Participants under 18 years of age or more than 65 6. Sleep above 4000 elevation in the preceding 1 week 7. History of asthma or COPD 8. Current symptoms of an acute upper respiratory illness 9. Unable to complete a moderately strenuous hike at high altitude Gender: Both |
| Interventions | Drug: Acetazolamide Drug: Budesonide Drug: Placebo |
| Outcomes | Oxygen saturation (time frame: 24 hours) Pulmonary function testing ‐ FEV1 (Time frame: 24 hours) Pulmonary function testing ‐ FVC (time frame: 24 hours) Pulmonary function testing ‐ PEFR (Time frame: 24 hours) |
| Starting date | August 2016 |
| Contact information | Grant S Lipman, MD |
| Notes | Not yet recruiting |
NCT02811016.
| Trial name or title | Effect of inhaled budesonide on the incidence and severity of acute mountain sickness at 4559 metres |
| Methods | Not stated |
| Participants | 51 healthy volunteers |
| Interventions | Budesonide 200 µg inhaled at 7:00 a.m. and 7 p.m. Budesonide 800 µg inhaled at 7:00 a.m. and 7 p.m. Placebo Inhalation at 7:00 a.m. and 7 p.m. |
| Outcomes | Assessment of incidence and severity of acute mountain sickness by use of 2 internationally standardized and well‐established questionnaires Venous (and capillary) blood drawings Transthoracic echocardiography for assessing pulmonary artery systolic pressure |
| Starting date | June 2016 |
| Contact information | Marc Berger, Salzburger Landeskliniken |
| Notes | This study has been completed. |
NCT02941510.
| Trial name or title | Inhaled budesonide for altitude illness prevention |
| Methods | Not stated |
| Participants | Participants will be recruited from the Denver community and prescreened for eligibility via phone. 100 participants, after consenting, will have baseline data and blood collected and will begin budesonide therapy 72 hours prior to being taken from Denver to Pikes Peak, where they will be observed at altitude for 18 hours. Participants will have the opportunity to withdraw consent at any time and will be monitored continuously by physician‐researchers |
| Interventions | Budenoside, placebo |
| Outcomes | Primary outcome measures:
|
| Starting date | April 2017 |
| Contact information | University of Colorado, Denver |
| Notes | This study is not yet open for participant recruitment. |
AMS: Acute Mountain Sickness;BMI: Body mass index; COPD: Chronic obstructive pulmonary disease ; CYP: cytochrome P450 enzymes; dL: decilitre; ECG: electrocardiogram; FEV1:forced expiratory volume in 1 second; FSH: Follicle‐stimulating hormone; ft: feet; FVC: forced expiratory vital capacity; GOLD: Global Initiative for Chronic Obstructive Lung Disease criteria,; HAH: High altitude headache; HR: hear rate; kg: kilograms; IUD: Intrauterine device; IUS: Intrauterine system; LNG 20: levonorgestrel 20 ɥg/day; ml:millilitres; Mg:milligrams; NSAIDs: Nonsteroidal anti‐inflammatory drugs ; OTC:over‐the‐counter; PEFR: peak expiratory flow rate ; qd: every day; TM:Morning‐after pill; VO2: maximal oxygen consumption.
Differences between protocol and review
1. Given that the original protocol was published in 2012, several sections needed updating to fulfil the current methodological guidelines for Cochrane Reviews. We made the following changes to the published protocol (Martí‐Carvajal 2012):
2. On the recommendation of the editors of the Cochrane Anaesthesia, Critical and Emergency Group, we split the review into three parts, considering the numerous interventions assessed for HAI prevention. This review is the first part and it focuses on commonly‐used agents to prevent this condition. Subsequent reviews will address less commonly‐used agents to prevent HAI, and non‐pharmacological interventions. This change has implications for the title and scope of this review and for later reviews in this series.
3. We updated the Background with new references to reflect current evidence about the target condition, as well as the scope of common interventions to prevent HAI.
4. The primary and secondary outcomes presented in the protocol — Martí‐Carvajal 2012) — were modified to follow the MECIR guidelines (Higgins 2016), and improve their understanding. In particular, we made the following changes.
We removed 'All‐cause mortality (by all causes or specific)' as a primary outcome of this review. This is because the risk of mortality is low in the general population, and it is not the primary goal for prevention.
We removed the outcome ' Combined incidence of AMS, HAPE or HACE (any of these alone or in combination)'. This is because this outcome is not often reported in studies, and this information can be easily calculated by the separate reporting of AMS, HAPE and HACE.
Previously the 'Risk of AMS' was a secondary outcome. It is a primary event to assess in prevention trials of HAI. We therefore moved this outcome from the list of secondary outcomes to the primary outcomes in this series of reviews. The risk of HAPE, HACE and adverse events are also important outcomes and they were included as secondary outcomes.
We included a new secondary outcome 'Difference in HAI/AMS scores at high altitude'. This is because it is frequently reported in studies, reflecting the severity of the disease
5. For this review, we selected six commonly‐used types of intervention to prevent HAI. We will address other interventions in the next two reviews belonging to this series.
6. Despite the fact that the protocol did not include any consideration of unit of analysis issues, we have identified 12 cross‐over studies in our searches. We have included them in our review to enhance the full reporting of all available evidence, and we have analysed them separately from the parallel studies.
7. We stated in the protocol that we would contact trial authors in case of missing data or selective reporting. However we were unable to conduct this task, usually due to the year of publication of the trial (most of the publications were performed too long ago and it was not possible to obtain a valid contact address or other means to contact trialists).
8. We have introduced several modifications in the Dealing with missing data section, in order to clarify the intention‐to‐treat analysis performed and to present the methods for imputing missing information (mostly related to standard deviations).
9. Under Data synthesis we added the trial sequential analysis procedure, in order to test the boundary before the required information size was reached.
10. We also made extensive modifications to the Subgroup analysis and investigation of heterogeneity section, and have selected only three variables to analyse. However, we were unable to find information about the third factor (significant pre‐existing disease) in the included trials.
Contributions of authors
Conceiving the review: AMC Co‐ordinating the review: VNE, AMC and IAR Undertaking manual searches: VNE, DMF, RDM, and IAR Screening search results: VNE, DMF, RDM and IAR Organizing retrieval of papers: VNE, DMF, RDM and IAR Screening retrieved papers against inclusion criteria: VNE, DMF, RDM and IAR Appraising quality of papers: VNE, DMF, RDM, AGG and IAR Abstracting data from papers: VNE, DMF, RDM, AGG and IAR Writing to authors of papers for additional information: Not performed Providing additional data about papers: VNE, DMF, RDM, AGG and IAR Obtaining and screening data on unpublished studies: VNE, DMF, RDM, AGG and IAR Data management for the review: IAR and RDM Entering data into Review Manager 5 (RevMan 5.3): IAR and RDM RevMan statistical data: IAR and RDM Other statistical analysis not using RevMan: AMC and IAR Interpretation of data: VNE, DMF, RDM, AGG, AMC and IAR Statistical inferences: VNE, DMF, RDM, AGG, AMC and IAR Writing the review: VNE, DMF, RDM, AGG, AMC and IAR Securing funding for the review: VNE, DMF, RDM, AGG, AMC and IAR Performing previous work that was the foundation of the present study: Not performed Guarantor for the review (one author): VNE Person responsible for reading and checking review before submission: IAR
Sources of support
Internal sources
Fundacion Universitaria de Ciencias de la Salud, Colombia.
-
Methodology Research Unit/Neonatology, Instituto Nacional de Pediatria, Mexico.
Academic.
Instituto de Evaluación Tecnológica en Salud ‐ IETS, Colombia.
External sources
-
Iberoamerican Cochrane Center, Spain.
Academic.
Declarations of interest
Victor H Nieto Estrada: nothing to declare. Daniel Molano Franco: nothing to declare. Roger David Medina: nothing to declare. Alejandro Gonzalez Garay: nothing to declare. Arturo Marti Carvajal: nothing to declare. Ingrid Arevalo‐Rodriguez: nothing to declare.
Edited (no change to conclusions)
References
References to studies included in this review
Anonymous 1981 {published data only}
- Anonymous. Acetazolamide in control of acute mountain sickness. Lancet 1981;1(8213):180‐3. [PUBMED: 6109857] [PubMed] [Google Scholar]
ASCENT 2012 {published data only}
- Gertsch JH, Corbett B, Holck PS, Mulcahy A, Watts M, Stillwagon NT, et al. Altitude Sickness in Climbers and Efficacy of NSAIDs Trial (ASCENT): randomized, controlled trial of ibuprofen versus placebo for prevention of altitude illness. Wilderness and Environmental Medicine 2012;23(4):307‐15. [DOI] [PubMed] [Google Scholar]
Banderet 1977 {published data only}
- Banderet LE. Self‐rated moods of humans at 4300 m pretreated with placebo or acetazolamide plus staging. Aviation, Space, and Environmental Medicine 1977;48(1):19‐22. [PUBMED: 831706] [PubMed] [Google Scholar]
Bartsch 1991 {published data only}
- Bartsch P, Maggiorini M, Ritter M, Noti C, Vock P, Oelz O. Prevention of high‐altitude pulmonary edema by nifedipine. New England Journal of Medicine 1991;325(18):1284‐9. [PUBMED: 1922223] [DOI] [PubMed] [Google Scholar]
- Oelz O, Maggiorini M, Ritter M, Noti C, Waber U, Vock P, et al. Prevention and treatment of high altitude pulmonary edema by a calcium channel blocker. International Journal of Sports Medicine 1992;13(1):S65‐8. [PUBMED: 1483797] [DOI] [PubMed] [Google Scholar]
Basnyat 2003 {published data only}
- Basnyat B, Gertsch JH, Johnson EW, Castro‐Marin F, Inoue Y, Yeh C. Efficacy of low‐dose acetazolamide (125 mg BID) for the prophylaxis of acute mountain sickness: a prospective, double‐blind, randomized, placebo‐controlled trial. High Altitude Medicine & Biology 2003;4(1):45‐52. [PUBMED: 12713711] [DOI] [PubMed] [Google Scholar]
Basnyat 2008 {published data only}
- Basnyat B, Hargrove J, Holck PS, Srivastav S, Alekh K, Ghimire LV, et al. Acetazolamide fails to decrease pulmonary artery pressure at high altitude in partially acclimatized humans. High Altitude Medicine & Biology 2008;9(3):209‐16. [PUBMED: 18800957] [DOI] [PubMed] [Google Scholar]
Basu 2002a {published data only}
- Basu M, Sawhney RC, Kumar S, Pal K, Prasad R, Selvamurthy W. Glucocorticoids as prophylaxis against acute mountain sickness. Clinical Endocrinology 2002;57(6):761‐7. [PUBMED: 12460326] [DOI] [PubMed] [Google Scholar]
Basu 2002b {published data only}
- Basu M, Sawhney RC, Kumar S, Pal K, Prasad R, Selvamurthy W. Hypothalamic‐pituitary‐adrenal axis following glucocorticoid prophylaxis against acute mountain sickness. Hormone and Metabolic Research 2002;34(6):318‐24. [PUBMED: 12173072] [DOI] [PubMed] [Google Scholar]
Bates 2011 {published data only}
- Bates MG, Thompson AA, Baillie JK, Sutherland AI, Irving JB, Hirani N, et al. Sildenafil citrate for the prevention of high altitude hypoxic pulmonary hypertension: double blind, randomized, placebo‐controlled trial. High Altitude Medicine & Biology 2011;12(3):207‐14. [PUBMED: 21962063] [DOI] [PubMed] [Google Scholar]
Baumgartner 2003 {published data only}
- Baumgartner RW, Keller S, Regard M, Bartsch P. Flunarizine in prevention of headache, ataxia, and memory deficits during decompression to 4559 m. High Altitude Medicine & Biology 2003;4(3):333‐9. [PUBMED: 14561238] [DOI] [PubMed] [Google Scholar]
Bernhard 1994 {published data only}
- Bernhard WN, Miller SL, Gittelsohn A. Dexamethasone for prophylaxis against acute mountain sickness during rapid ascent to 5334 m. Journal of Wilderness Medicine 1994;5(3):331‐8. [Google Scholar]
Bernhard 1998 {published data only}
- Bernhard WN, Schalick LM, Delaney PA, Bernhard TM, Barnas GM. Acetazolamide plus low‐dose dexamethasone is better than acetazolamide alone to ameliorate symptoms of acute mountain sickness. Aviation, Space, and Environmental Medicine 1998;69(9):883‐6. [PUBMED: 9737760] [PubMed] [Google Scholar]
Bradwell 1986 {published data only}
- Bradwell AR, Dykes PW, Coote JH, Forster PJ, Milles JJ, Chesner I, et al. Effect of acetazolamide on exercise performance and muscle mass at high altitude. Lancet 1986;1(8488):1001‐5. [PUBMED: 2871285] [DOI] [PubMed] [Google Scholar]
Burki 1992 {published data only}
- Burki NK, Khan SA, Hameed MA. The effects of acetazolamide on the ventilatory response to high altitude hypoxia. Chest 1992;101(3):736‐41. [PUBMED: 1541140] [DOI] [PubMed] [Google Scholar]
Burtscher 1998 {published data only}
- Burtscher M, Likar R, Nachbauer W, Philadelphy M. Aspirin for prophylaxis against headache at high altitudes: randomised, double blind, placebo controlled trial. BMJ 1998;316(7137):1057‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burtscher 2001 {published data only}
- Burtscher M, Likar R, Nachbauer W, Philadelphy M, Pühringer R, Lämmle T. Effects of aspirin during exercise on the incidence of high‐altitude headache: a randomized, double‐blind, placebo‐controlled trial. Headache 2001;41(6):542‐5. [DOI] [PubMed] [Google Scholar]
Burtscher 2014 {published data only}
- Burtscher M, Gatterer H, Faulhaber M, Burtscher J. Acetazolamide pre‐treatment before ascending to high altitudes: When to start?. International Journal of Clinical and Experimental Medicine 2014;15(11):4378‐83. [PUBMED: 25550957] [PMC free article] [PubMed] [Google Scholar]
Carlsten 2004 {published data only}
- Carlsten C, Swenson ER, Ruoss S. A dose‐response study of acetazolamide for acute mountain sickness prophylaxis in vacationing tourists at 12,000 feet (3630 m). High Altitude Medicine & Biology 2004;5(1):33‐9. [PUBMED: 15072715] [DOI] [PubMed] [Google Scholar]
Chen 2015 {published data only}
- Chen GZ, Zheng CR, Qin J, Yu J, Wang H, Zhang JH, et al. Inhaled budesonide prevents acute mountain sickness in young Chinese men. Journal of Emergency Medicine 2015;48(2):197‐206. [PUBMED: 25294611] [DOI] [PubMed] [Google Scholar]
- Xiangjun L, Lan H. Inhaled budesonide for the prevention of acute mountain sickness in unacclimatization young men: A double‐blind randomized controlled trial. Journal of the American College of Cardiology 2014;16 Suppl 1(64):C69. [Google Scholar]
Chow 2005 {published data only}
- Chow T, Browne V, Heileson HL, Wallace D, Anholm J, Green SM. Ginkgo biloba and acetazolamide prophylaxis for acute mountain sickness: a randomized, placebo‐controlled trial. Archives of Internal Medicine 2005;165(3):296‐301. [PUBMED: 15710792] [DOI] [PubMed] [Google Scholar]
Ellsworth 1991 {published data only}
- Ellsworth AJ, Meyer EF, Larson EB. Acetazolamide or dexamethasone use versus placebo to prevent acute mountain sickness on Mount Rainier. Western Journal of Medicine 1991;154(3):289‐93. [PUBMED: 2028586] [PMC free article] [PubMed] [Google Scholar]
Faull 2015 {published data only}
- Faull OK, Robertson J, Thomas O, Bradwell AR, Antoniades CA, Pattinson KTS, et al. The effect of acetazolamide on saccadic latency at 3459 meters. Wilderness and Environmental Medicine 2015;26(1):72‐7. [DOI] [PubMed] [Google Scholar]
Fischer 2000a {published data only}
- Fischer R, Hautmann H, Toepfer M, Tschoep M, Pongratz H, Huber RM. Oral slow release theophylline (oT) is effective in prevention of acute mountain sickness [abstract]. European Respiratory Journal. Supplement. 1998;12(Suppl 28):407S. [CN‐00382822] [Google Scholar]
- Fischer R, Lang SM, Steiner U, Toepfer M, Hautmann H, Pongratz H, et al. Theophylline improves acute mountain sickness. European Respiratory Journal 2000;15(1):123‐7. [PUBMED: 10678632] [DOI] [PubMed] [Google Scholar]
Fischer 2000b {published data only}
Fischer 2004 {published data only}
- Fischer R, Vollmar C, Thiere M, Born C, Leitl M, Pfluger T, et al. No evidence of cerebral oedema in severe acute mountain sickness. Cephalalgia 2004;24(1):66‐71. [PUBMED: 14687016] [DOI] [PubMed] [Google Scholar]
Fulco 2006 {published data only}
- Fulco CS, Muza SR, Ditzler D, Lammi E, Lewis SF, Cymerman A. Effect of acetazolamide on leg endurance exercise at sea level and simulated altitude. Clinical Science 2006;110(6):683‐92. [PUBMED: 16499476] [DOI] [PubMed] [Google Scholar]
Greene 1981 {published data only}
- Greene MK, Kerr AM, McIntosh IB, Prescott RJ. Acetazolamide in prevention of acute mountain sickness: a double‐blind controlled cross‐over study. BMJ 1981;283(6295):811‐3. [PUBMED: 6794709] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hackett 1976 {published data only}
- Hackett PH, Rennie D, Levine HD. The incidence, importance, and prophylaxis of acute mountain sickness. Lancet 1976;2(7996):1149‐55. [PUBMED: 62991] [DOI] [PubMed] [Google Scholar]
Hackett 1988 {published data only}
- Hackett PH, Roach RC, Wood RA, Foutch RG, Meehan RT, Rennie D, et al. Dexamethasone for prevention and treatment of acute mountain sickness. Aviation, Space, and Environmental Medicine 1988;59(10):950‐4. [PUBMED: 3190622] [PubMed] [Google Scholar]
HEAT 2010 {published data only}
- Gertsch JH, Lipman GS, Holck PS, Merritt A, Mulcahy A, Fisher RS, et al. Prospective, double‐blind, randomized, placebo‐controlled comparison of acetazolamide versus ibuprofen for prophylaxis against high altitude headache: the Headache Evaluation at Altitude Trial (HEAT). Wilderness & Environmental Medicine 2010;21(3):236‐43. [PUBMED: 20832701] [DOI] [PubMed] [Google Scholar]
Hillenbrand 2006 {published data only}
- Hillenbrand P, Pahari AK, Soon Y, Subedi D, Bajracharya R, Gurung P, et al. Prevention of acute mountain sickness by acetazolamide in Nepali porters: a double‐blind controlled trial. Wilderness & Environmental Medicine 2006;17(2):87‐93. [PUBMED: 16805144] [DOI] [PubMed] [Google Scholar]
Hochapfel 1986 {published data only}
- Hochapfel G, Schlemmer W. Prophylaxis of acute mountain sickness. Experiences with acetazolamide in Nepal. Munchener Medizinische Wochenschrift 1986;128(8):137‐8. [Google Scholar]
Hohenhaus 1994 {published data only}
- Hohenhaus E, Goerre S, Niroomand F, Oelz O, Bartsch P. Nifedipine does not prevent acute mountain sickness [abstract]. European Respiratory Journal. Supplement. 1993; Vol. 7 Suppl 17:187S. [CN‐00393692] [DOI] [PubMed]
- Hohenhaus E, Niroomand F, Goerre S, Vock P, Oelz O, Bartsch P. Nifedipine does not prevent acute mountain sickness. American Journal of Respiratory and Critical Care Medicine 1994;150(3):857‐60. [PUBMED: 8087361] [DOI] [PubMed] [Google Scholar]
Hussain 2001 {published data only}
- Hussain MM, Aslam M, Khan Z. Acute mountain sickness score and hypoxemia. Journal of the Pakistan Medical Association 2001;5(5):173‐9. [PubMed] [Google Scholar]
Jain 1986 {published data only}
- Jain SC, Singh MV, Sharma VM, Rawal SB, Tyagi AK. Amelioration of acute mountain sickness: comparative study of acetazolamide and spironolactone. International Journal of Biometeorology 1986;30(4):293‐300. [PUBMED: 3804482] [DOI] [PubMed] [Google Scholar]
Johnson 1984 {published data only}
- Johnson TS, Rock PB, Fulco CS, Trad LA, Spark RF, Maher JT. Prevention of acute mountain sickness by dexamethasone. New England Journal of Medicine 1984;310(11):683‐6. [PUBMED: 6700643] [DOI] [PubMed] [Google Scholar]
Kayser 2008 {published data only}
- Kayser B, Hulsebosch R, Bosch F. Low‐dose acetylsalicylic acid analog and acetazolamide for prevention of acute mountain sickness. High Altitude Medicine & Biology 2008;9(1):15‐23. [PUBMED: 18331216] [DOI] [PubMed] [Google Scholar]
Ke 2013 {published data only}
- Ke T, Wang J, Swenson ER, Zhang X, Hu Y, Chen Y, et al. Effect of acetazolamide and gingko biloba on the human pulmonary vascular response to an acute altitude ascent. High Altitude Medicine & Biology 2013;14(2):162‐7. [PUBMED: 23795737] [DOI] [PMC free article] [PubMed] [Google Scholar]
Küpper 2008 {published data only}
- Küpper TE, Strohl KP, Hoefer M, Gieseler U, Netzer CM, Netzer NC. Low‐dose theophylline reduces symptoms of acute mountain sickness. Journal of Travel Medicine 2008;15(5):307‐14. [PUBMED: 19006503] [DOI] [PubMed] [Google Scholar]
Larson 1982a {published data only}
- Larson EB, Roach RC, Schoene RB, Hornbein TF. Acute mountain sickness and acetazolamide. Clinical efficacy and effect on ventilation. JAMA 1982;248(3):328‐32. [PUBMED: 7045433] [PubMed] [Google Scholar]
Larson 1982b {published data only}
Lipman 2012 {published data only}
- Lipman GS, Kanaan NC, Holck P, Gertsch JH, Constance BB, Corbett B, et al. Ibuprofen prevents altitude illness: A prospective, double‐blind, randomized controlled trial. Academic Emergency Medicine 2011;18(5 Suppl 1):S15. [DOI] [PubMed] [Google Scholar]
- Lipman GS, Kanaan NC, Holck PS, Constance BB, Gertsch JH, PAINS Group. Ibuprofen prevents altitude illness: a randomized controlled trial for prevention of altitude illness with nonsteroidal anti‐inflammatories. Annals of Emergency Medicine 2012;58(6):484‐90. [PUBMED: 22440488] [DOI] [PubMed] [Google Scholar]
Luks 2007 {published data only}
- Luks AM, Henderson WR, Swenson ER. Leukotriene receptor blockade does not prevent acute mountain sickness induced by normobaric hypoxia. High Altitude Medicine & Biology 2007;8(2):131‐8. [PUBMED: 17584007] [DOI] [PubMed] [Google Scholar]
Maggiorini 2006 {published data only}
- Bernheim AM, Kiencke S, Fischler M, Dorschner L, Debrunner J, Mairbaurl H, et al. Acute changes in pulmonary artery pressures due to exercise and exposure to high altitude do not cause left ventricular diastolic dysfunction. Chest 2007;132:380‐7. [DOI] [PubMed] [Google Scholar]
- Fischler M, Maggiorini M, Dorschner L, Debrunner J, Bernheim A, Kiencke S, et al. Dexamethasone but not tadalafil improves exercise capacity in adults prone to high‐altitude pulmonary edema. American Journal of Respiratory and Critical Care Medicine 2009;180(4):346‐52. [PUBMED: 19520908] [DOI] [PubMed] [Google Scholar]
- Maggiorini M, Brunner‐La Rocca HP, Peth S, Fischler M, Bohm T, Bernheim A, et al. Both tadalafil and dexamethasone may reduce the incidence of high‐altitude pulmonary edema: a randomized trial. Annals of Internal Medicine 2006;145(7):497‐506. [PUBMED: 17015867] [DOI] [PubMed] [Google Scholar]
- Mairbaurl H, Brunner‐La Rocca HP, Peth S, Dehnert C, Fischler M, Bohm T, et al. Phosphodiesterase‐5 inhibitors and glucocorticoids prevent a high‐altitude pulmonary oedema. Deutsche Zeitschrift für Sportmedizin 2005; Vol. 56, issue 7/8:218. [CN‐00727391]
Mirrakhlmov 1993 {published data only}
- Mirrakhimov M, Brimkulov N, Cielicki J, Tobiasz M, Kudaiberdiev Z, Moldotashev I, et al. Asthma treatment at high altitude effects of acetazolamide on overnight oximetry and prevention of acute mountain sickness [Abstract]. European Respiratory Journal 1992; Vol. 5, issue Suppl 15:366s. [CN‐00494881] [PubMed]
- Mirrakhlmov M, Brimkulov N, Cieslicki J, Tobiasz M, Kudaiberdiev Z, Moldotashev I, et al. Effects of acetazolamide on overnight oxygenation and acute mountain sickness in patients with asthma. European Respiratory Journal 1993;6(4):536‐40. [PUBMED: 8491304] [PubMed] [Google Scholar]
Montgomery 1989 {published data only}
- Montgomery AB, Luce JM, Michael P, Mills J. Effects of dexamethasone on the incidence of acute mountain sickness at two intermediate altitudes. JAMA 1989;261(5):734‐6. [PUBMED: 2911170] [PubMed] [Google Scholar]
Moraga 2007 {published data only}
- Moraga FA, Flores A, Serra J, Esnaola C, Barriento C. Ginkgo biloba decreases acute mountain sickness in people ascending to high altitude at Ollague (3696 m) in northern Chile. Wilderness & Environmental Medicine 2007;18(4):251‐7. [PUBMED: 18076292] [DOI] [PubMed] [Google Scholar]
Muza 2004 {published data only}
- Muza SR, Kaminsky D, Fulco CS, Banderet LE, Cymerman A. Cysteinyl leukotriene blockade does not prevent acute mountain sickness. Aviation, Space, and Environmental Medicine 2004;75(5):413‐9. [PUBMED: 15152893] [PubMed] [Google Scholar]
PACE 2006 {published data only}
- Basnyat B, Gertsch JH, Holck PS, Johnson EW, Luks AM, Donham BP, et al. Acetazolamide 125 mg BD is not significantly different from 375 mg BD in the prevention of acute mountain sickness: the prophylactic acetazolamide dosage comparison for efficacy (PACE) trial. High Altitude Medicine & Biology 2006;7(1):17‐27. [PUBMED: 16544963] [DOI] [PubMed] [Google Scholar]
Parati 2013 {published data only}
- Caravita S, Faini A, Lombardi C, Valentini M, Gregorini F, Rossi J, et al. Sex and acetazolamide effects on chemoreflex and periodic breathing during sleep at altitude. Chest 2015;147(1):120‐31. [DOI] [PubMed] [Google Scholar]
- Parati G, Revera M, Giuliano A, Faini A, Bilo G, Gregorini F, et al. Effects of acetazolamide on central blood pressure, peripheral blood pressure, and arterial distensibility at acute high altitude exposure. European Heart Journal 2013;10(10):759‐66. [DOI] [PubMed] [Google Scholar]
- Salvi P, Revera M, Faini A, Giuliano A, Gregorini F, Agostoni, et al. Changes in subendocardial viability ratio with acute high‐altitude exposure and protective role of acetazolamide. Hypertension 2013;61(4):793‐9. [DOI] [PubMed] [Google Scholar]
PHAIT 2004 {published data only}
- Gertsch JH, Basnyat B, Johnson EW, Onopa J, Holck PS. Randomised, double blind, placebo controlled comparison of ginkgo biloba and acetazolamide for prevention of acute mountain sickness among Himalayan trekkers: the prevention of high altitude illness trial (PHAIT). BMJ 2004;328(7443):797. [PUBMED: 15070635] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rock 1987 {published data only}
- Rock PB, Johnson TS, Cymerman A, Burse RL, Falk LJ, Fulco CS. Effect of dexamethasone on symptoms of acute mountain sickness at Pikes Peak, Colorado (4,300 m). Aviation, Space,and Environmental Medicine 1987;58(7):668‐72. [PUBMED: 3619842] [PubMed] [Google Scholar]
Rock 1989a {published data only}
- Rock PB, Johnson TS, Larsen RF, Fulco CS, Trad LA, Cymerman A. Dexamethasone as prophylaxis for acute mountain sickness. Effect of dose level. Chest 1989;95(3):568‐73. [PUBMED: 2920585] [DOI] [PubMed] [Google Scholar]
Rock 1989b {published data only}
Rock 1989c {published data only}
Sartori 2002 {published data only}
- Sartori C, Allemann Y, Duplain H, Lepori M, Egli M, Lipp E, et al. Salmeterol for the prevention of high‐altitude pulmonary edema. New England Journal of Medicine 2002;346(21):1631‐6. [PUBMED: 12023995] [DOI] [PubMed] [Google Scholar]
SPACE 2011 {published data only}
- Basnyat B, Holck PS, Pun M, Halverson S, Szawarski P, Gertsch J, et al. Spironolactone does not prevent acute mountain sickness: a prospective, double‐blind, randomized, placebo‐controlled trial by SPACE Trial Group (spironolactone and acetazolamide trial in the prevention of acute mountain sickness group). Wilderness & Environmental Medicine 2011;22(1):15‐22. [PUBMED: 21377114] [DOI] [PubMed] [Google Scholar]
Subudhi 2011 {published data only}
- Julian CG, Subudhi AW, Wilson MJ, Dimmen AC, Pecha T, Roach RC. Acute mountain sickness, inflammation, and permeability: New insights from a blood biomarker study. Journal of Applied Physiology 2011;111(2):392‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subudhi AW, Dimmen AC, Julian CG, Wilson MJ, Panerai RB, Roach RC. Effects of acetazolamide and dexamethasone on cerebral hemodynamics in hypoxia. Journal of Applied Physiology 2011;110(5):1219‐25. [PUBMED: 21393464] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Patot 2008 {published data only}
- Patot MC, Leadbetter G 3rd, Keyes LE, Maakestad KM, Olson S, Hackett PH. Prophylactic low‐dose acetazolamide reduces the incidence and severity of acute mountain sickness. High Altitude Medicine & Biology 2008;9(4):289‐93. [PUBMED: 19115912] [DOI] [PubMed] [Google Scholar]
Wang 2013 {published data only}
- Wang J, Ke T, Zhang X, Chen Y, Liu M, Chen J, et al. Effects of acetazolamide on cognitive performance during high‐altitude exposure. Neurotoxicology and Teratology 2013;35:28‐33. [PUBMED: 23280141] [DOI] [PubMed] [Google Scholar]
Wright 1983 {published data only}
- Wright AD, Bradwell AR, Fletcher RF. Methazolamide and acetazolamide in acute mountain sickness. Aviation, Space, and Environmental Medicine 1983;54(7):619‐21. [PUBMED: 6349608] [PubMed] [Google Scholar]
Wright 2004 {published data only}
- Wright AD, Beazley MF, Bradwell AR, Chesner IM, Clayton RN, Forster PJ, et al. Medroxyprogesterone at high altitude. The effects on blood gases, cerebral regional oxygenation, and acute mountain sickness. Wilderness & Environmental Medicine 2004;15(1):25‐31. [PUBMED: 15040503] [DOI] [PubMed] [Google Scholar]
Zell 1988 {published data only}
- Zell SC, Goodman PH. Acetazolamide and dexamethasone in the prevention of acute mountain sickness. Western Journal of Medicine 1988;148(5):541‐5. [PUBMED: 3051673] [PMC free article] [PubMed] [Google Scholar]
Zheng 2014 {published data only}
- Zheng CR, Chen GZ, Yu J, Qin J, Song P, Bian SZ, et al. Inhaled budesonide and oral dexamethasone prevent acute mountain sickness. American Journal of Medicine 2014;127(10):1001‐9.e2. [PUBMED: 24784698] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
ACME‐1 2006 {published data only}
- Modesti PA, Vanni S, Morabito M, Modesti A, Marchetta M, Gamberi T, et al. Role of endothelin‐1 in exposure to high altitude: Acute Mountain Sickness and Endothelin‐1 (ACME‐1) study. Circulation 2006;114(13):1410‐6. [PUBMED: 16982943] [DOI] [PubMed] [Google Scholar]
Agostoni 2013 {published data only}
- Agostoni P, Swenson ER, Fumagalli R, Salvionia E, Cattadoria G, Farina S, et al. Acute high‐altitude exposure reduces lung diffusion: Data from the HIGHCARE Alps project. Respiratory Physiology & Neurobiology 2013;188(2):223‐8. [DOI] [PubMed] [Google Scholar]
Bartsch 1993 {published data only}
- Bärtsch P, Merki B, Hofstetter D, Maggiorini M, Kayser B, Oelz O. Treatment of acute mountain‐sickness by simulated descent ‐ a randomized controlled trial. BMJ 1993;306(6885):1098‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bärtsch 1994 {published data only}
- Bartsch P, Maggi S, Kleger GR, Ballmer PE, Baumgartner RW. Sumatriptan for high‐altitude headache. Lancet 1994;344(8934):1445. [PUBMED: 7968111] [DOI] [PubMed] [Google Scholar]
Bilo 2015 {published data only}
- Bilo G, Lombardi C, Revera M, Diazzi E, Giuliano A, Faini A, et al. Acetazolamide counteracts ambulatory blood pressure increase under acute exposure to high altitude. High Blood Pressure and Cardiovascular Prevention 2011;18(3):118. [Google Scholar]
- Bilo G, Villafuerte FC, Faini A, Anza‐Ramírez C, Revera M, Giuliano A, et al. Ambulatory blood pressure in untreated and treated hypertensive patients at high altitude: The High Altitude Cardiovascular Research‐Andes study. Hypertension 2015;65(6):1266‐72. [DOI] [PubMed] [Google Scholar]
- Bilo, G, Villafuerte F, Anza C, Revera, Giuliano A, Faini A, et al. Combined antihypertensive treatment and blood pressure responses to acute high altitude exposure in patients with hypertension. HIGHCARE‐ANDES Lowlanders Study. European Heart Journal 2011;34(Suppl 1):269‐70. [Google Scholar]
Bloch 2009 {published data only}
- Bloch KE, Turk AJ, Maggiorini M, Hess T, Merz T, Bosch MM, et al. Effect of ascent protocol on acute mountain sickness and success at Muztagh Ata, 7546 m. High Altitude Medicine & Biology 2009;10(1):25‐32. [PUBMED: 19326598] [DOI] [PubMed] [Google Scholar]
Broome 1994 {published data only}
- Broome JR, Stoneham MD, Beeley JM, Milledge JS, Hughes AS. High altitude headache: treatment with ibuprofen. Aviation, Space, and Environmental Medicine 1994;65(1):19‐20. [PUBMED: 8117220] [PubMed] [Google Scholar]
Cain 1966 {published data only}
- Cain SM, Dunn JE 2nd. Low doses of acetazolamide to aid accommodation of men to altitude. Journal of Applied Physiology 1966;21(4):1195‐200. [PUBMED: 5916650] [DOI] [PubMed] [Google Scholar]
Debevec 2015 {published data only}
- Debevec T, Pialoux V, Saugy J, Schmitt L, Cejuela R, Mury P, et al. Prooxidant/Antioxidant balance in hypoxia: A cross‐over study on normobaric vs. hypobaric "live high‐train low". PLoS ONE 2015;10(9):e0137957. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dumont 1999 {published data only}
- Dumont L, Mardirosoff C, Soto‐Debeuf G, Tassonyi E. Magnesium and acute mountain sickness. Aviation, Space, and Environmental Medicine 1999;70(6):625. [PUBMED: 10373058] [PubMed] [Google Scholar]
Forster 1982 {published data only}
- Forster P. Methazolamide in acute mountain sickness. Lancet 1982;1(8283):1254. [PUBMED: 6123014] [DOI] [PubMed] [Google Scholar]
Forwand 1968 {published data only}
- Forwand SA, Landowne M, Follansbee JN, Hansen JE. Effect of acetazolamide on acute mountain sickness. New England Journal of Medicine 1968;279(16):839‐45. [PUBMED: 4877992] [DOI] [PubMed] [Google Scholar]
Fulco 2011 {published data only}
- Fulco CS, Muza SR, Beidleman BA, Demes R, Staab JE, Jones JE, et al. Effect of repeated normobaric hypoxia exposures during sleep on acute mountain sickness, exercise performance, and sleep during exposure to terrestrial altitude. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology 2011;300(2):R428‐36. [PUBMED: 21123763] [DOI] [PubMed] [Google Scholar]
Gertsch 2002 {published data only}
- Gertsch JH, Seto TB, Mor J, Onopa J. Ginkgo biloba for the prevention of severe acute mountain sickness (AMS) starting one day before rapid ascent. High Altitude Medicine & Biology 2002;3(1):29‐37. [PUBMED: 12006162] [DOI] [PubMed] [Google Scholar]
Gray 1971 {published data only}
- Gray GW, Bryan AC, Frayser R, Houston CS, Rennie ID. Control of acute mountain sickness. Aerospace Medicine 1971;42(1):81‐4. [PUBMED: 4925130] [PubMed] [Google Scholar]
Harris 2003 {published data only}
- Harris NS, Wenzel RP, Thomas SH. High altitude headache: efficacy of acetaminophen vs. ibuprofen in a randomized, controlled trial. Journal of Emergency Medicine 2003;24(4):383‐7. [PUBMED: 12745039] [DOI] [PubMed] [Google Scholar]
Johnson 1988 {published data only}
- Johnson TS, Rock PB, Young JB, Fulco CS, Trad LA. Hemodynamic and sympathoadrenal responses to altitude in humans: effect of dexamethasone. Aviation, Space, and Environmental Medicine 1988;59(3):208‐12. [PUBMED: 3355474] [PubMed] [Google Scholar]
Jonk 2007 {published data only}
- Jonk AM, Berg IP, Olfert IM, Wray DW, Arai T, Hopkins SR, et al. Effect of acetazolamide on pulmonary and muscle gas exchange during normoxic and hypoxic exercise. Journal of Physiology 2007;579(Pt 3):909‐21. [PUBMED: 17218362] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kotwal 2015 {published data only}
- Kotwal J, Kotwal A, Bhalla S, Singh PK, Nair V. Effectiveness of homocysteine lowering vitamins in prevention of thrombotic tendency at high altitude area: A randomized field trial. Thrombosis Research 2015;136(4):758‐62. [DOI] [PubMed] [Google Scholar]
Lalande 2009 {published data only}
- Lalande S, Snyder EM, Olson TP, Hulsebus ML, Orban M, Somers VK, et al. The effects of sildenafil and acetazolamide on breathing efficiency and ventilatory control during hypoxic exercise. European Journal of Applied Physiology 2009;106(4):509‐15. [PUBMED: 19337745] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lawley 2012 {published data only}
- Lawley JS, Oliver SJ, Mullins P, Morris D, Junglee NA, Jelleyman C, et al. Optic nerve sheath diameter is not related to high altitude headache: A randomized controlled trial. High Altitude Medicine and Biology 2012;3:193‐9. [DOI] [PubMed] [Google Scholar]
Levine 1989 {published data only}
- Levine BD, Yoshimura K, Kobayashi T, Fukushima M, Shibamoto T, Ueda G. Dexamethasone in the treatment of acute mountain sickness. New England Journal of Medicine 1989;321(25):1707‐13. [PUBMED: 2687688] [DOI] [PubMed] [Google Scholar]
Liu 2013 {published data only}
- Liu C, Croft QP, Kalidhar S, Brooks JT, Herigstad M, Smith TG, et al. Dexamethasone mimics aspects of physiological acclimatization to 8 hours of hypoxia but suppresses plasma erythropoietin. Journal of Applied Physiology 2013;114(7):948‐56. [PUBMED: 23393065] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mairer 2012 {published data only}
- Mairer K, Gobel M, Defrancesco M, Wille M, Messner H, Loizides A, et al. MRI evidence: acute mountain sickness is not associated with cerebral edema formation during simulated high altitude. PloS One 2012;7(11):e50334. [PUBMED: 23226263] [DOI] [PMC free article] [PubMed] [Google Scholar]
McIntosh 1986 {published data only}
- McIntosh IB, Prescott RJ. Acetazolamide in prevention of acute mountain sickness. Journal of International Medical Research 1986;14(5):285‐7. [PUBMED: 3533677] [DOI] [PubMed] [Google Scholar]
Purkayastha 1995 {published data only}
- Purkayastha SS, Ray US, Arora BS, Chhabra PC, Thakur L, Bandopadhyay P, et al. Acclimatization at high altitude in gradual and acute induction. Journal of Applied Physiology 1995;79(2):487‐92. [PUBMED: 7592207] [DOI] [PubMed] [Google Scholar]
Reinhart 1994 {published data only}
- Reinhart WH, Goerre S, Bartsch P. Acetazolamide reduces the erythropoietin response to hypoxia at high altitude in humans. Journal of Wilderness Medicine 1994;5(3):312‐7. [Google Scholar]
Sandoval 2000 {published data only}
- Sandoval M, Silva J, Parra M, Cifuentes F, Maluenda R, Escobar J. Effects of consumption of antioxidants in altitude exposure [Efectos del consumo de antioxidantes en exposición a altitud]. Boletin Cientifico de la Asociacion Chilena de Seguridad 2000;2(3):67‐73. [Google Scholar]
Scalzo 2015 {published data only}
- Scalzo RL, Binns SE, Klochak AL, Giordano GR, Paris HLR, Sevits KJ, et al. Methazolamide plus aminophylline abrogates hypoxia‐mediated endurance exercise impairment. High Altitude Medicine & Biology 2015;16:331‐42. [DOI] [PubMed] [Google Scholar]
Serra 2001 {published data only}
- Serra J. Chachacoma: An alternative treatment for the prevention of acute mountain sickness? [Chachacoma ¿un tratamiento alternativo para la prevención del mal agudo de montaña?]. Revista de Ciencias de la Salud 2001;5(1):36‐42. [Google Scholar]
Siebenmann 2011 {published data only}
- Siebenmann C, Bloch KE, Lundby C, Nussbamer‐Ochsner Y, Schoeb M, Maggiorini M. Dexamethasone improves maximal exercise capacity of individuals susceptible to high altitude pulmonary edema at 4559 m. High Altitude Medicine & Biology 2011;12(2):169‐77. [PUBMED: 21718165] [DOI] [PubMed] [Google Scholar]
Singh 1969 {published data only}
- Singh I, Khanna PK, Srivastava MC, Lal M, Roy SB, Subramanyam CS. Acute mountain sickness. New England Journal of Medicine 1969;280(4):175‐84. [DOI] [PubMed] [Google Scholar]
Solís 1984 {published data only}
- Solís JV. Acetazolamide: Effects on the "acute mountain sickness", aggravated by physical activity. Boletín de la Fundación Jiménez Díaz 1984;11(3):117‐20. [Google Scholar]
Suh 2015 {published data only}
- Suh KS, Kim T, Yi NJ, Hong G. Preparation for high altitude expedition and changes in cardiopulmonary and biochemical laboratory parameters with ascent to high altitude in transplant patients and live donors. Clinical Transplantation 2015;29(11):1013‐20. [DOI] [PubMed] [Google Scholar]
Teppema 2007 {published data only}
- Teppema LJ, Balanos GM, Steinback CD, Brown AD, Foster GE, Duff HJ, et al. Effects of acetazolamide on ventilatory, cerebrovascular, and pulmonary vascular responses to hypoxia. American Journal of Respiratory and Critical Care Medicine 2007;175(3):277‐81. [PUBMED: 17095745] [DOI] [PubMed] [Google Scholar]
Vuyk 2006 {published data only}
- Vuyk J, Bos J, Terhell K, Bos R, Vletter A, Valk P, et al. Acetazolamide improves cerebral oxygenation during exercise at high altitude. High Altitude Medicine & Biology 2006;7(4):290‐301. [PUBMED: 17173514] [DOI] [PubMed] [Google Scholar]
White 1984 {published data only}
- White AJ. Cognitive impairment of acute mountain sickness and acetazolamide. Aviation, Space, and Environmental Medicine 1984;55(7):598‐603. [PUBMED: 6466255] [PubMed] [Google Scholar]
Wright 1988 {published data only}
- Wright AD, Bradwell AR, Jensen J, Lassen N. Cerebral blood flow in acute mountain sickness and treatment with acetazolamide. Clinical Science 1988;74 Suppl 18:1P. [Google Scholar]
References to studies awaiting assessment
Dugas 1995 {published data only}
- Dugas L, Dubray C, Herry JP, Olsen NV, Court‐Payen M, Hansen JM, et al. Cardiovascular effects of a calcium channel blocker in hypoxia caused by altitude [Effets cardiovasculaires d'un bloqueur calcique en hypoxie d'altitude]. Presse Medicale 1995;24(16):763‐8. [PUBMED: 7784415] [PubMed] [Google Scholar]
Ellsworth 1987 {published data only}
- Ellsworth AJ, Larson EB, Strickland D. A randomized trial of dexamethasone and acetazolamide for acute mountain sickness prophylaxis. American Journal of Medicine 1987;83(6):1024‐30. [PUBMED: 3332564] [DOI] [PubMed] [Google Scholar]
Furian 2016 {published data only}
- Furian M, Lichtblau M, Aeschbacher SS, Bisang M, Hartmann SE, Poulin M, et al. Altitude related adverse health effects in lowlanders with COPD travelling to 3,200 m. randomized trial of preventive dexamethasone treatment. Respiration 2016;91(5):415. [Google Scholar]
Hefti 2014 {published data only}
- Hefti JP, Stutz M, Geiser T, Hefti U, Merz T, Huber A. Effect of antioxidant supplements on AMS and endothelial function during a high altitude expedition: A prospective randomized double‐blind trial. High Altitude Medicine & Biology 2014;15(2):A262. [Google Scholar]
Kasic 1991 {published data only}
- Kasic JF, Yaron M, Nicholas RA, Lickteig JA, Roach R. Treatment of acute mountain‐sickness ‐ hyperbaric versus oxygen‐therapy. Annals of Emergency Medicine 1991;20(10):1109‐12. [DOI] [PubMed] [Google Scholar]
Lee 2011 {published data only}
- Lee JH, Choi PC. Comparison of methazolamide and acetazolamide for prevention of acute mountain sickness in adolescents. Journal of the Korean Society of Emergency Medicine 2011;22(5):523‐30. [Google Scholar]
Pun 2014 {published data only}
- Pun M, Neupane M, Lohani A, Thapa GB, Yadav S, Holck PS, et al. Role of low‐dose acetazolamide (125 mg BID) in prevention of acute mountain sickness in pilgrims ascending rapidly: A prospective double‐blind placebocontrolled randomized trial. High Altitude Medicine & Biology 2014;15(2):A233. [Google Scholar]
Roncin 1996 {published data only}
- Roncin JP, Schwartz F, Darbigny P. EGb 761 in control of acute mountain sickness and vascular reactivity to cold exposure. Aviation, Space, and Environmental Medicine 1996;67(5):445‐52. [PubMed] [Google Scholar]
Swenson 1997 {published data only}
- Swenson ER, Macdonald A, Vatheuer M, Maks C, Treadwell A, Allen R, et al. Acute mountain sickness is not altered by a high carbohydrate diet nor associated with elevated circulating cytokines. Aviation, Space, and Environmental Medicine 1997;68:499‐503. [PubMed] [Google Scholar]
Utz 1970 {published data only}
- Utz G, Schlierf G, Barth P, Linhart P, Wollenweber J. Prevention of acute mountain sickness using acetazolamide [Prophylaxe der akuten hohenkrankheit mit acetazolamid]. Munchener Medizinische Wochenschrift 1970;112(23):1122‐4. [PUBMED: 5467747] [PubMed] [Google Scholar]
Wang 1998 {published data only}
- Wang W, Zhang X, Ma Y. Low‐concentration nitrous oxide inhalation in the treatment of high‐altitude pulmonary edema. Chinese Journal of Tuberculosis and Respiratory Diseases 1998;21(4):212‐4. [PubMed] [Google Scholar]
Xiangjun 2014 {published data only}
- Xiangjun L, Lan H. Inhaled budesonide for the prevention of acute mountain sickness in unacclimatization young men: a double‐blind randomized controlled trial. Journal of the American College of Cardiology 2014;64(16 Suppl 1):C69. [Google Scholar]
References to ongoing studies
ChiCTR‐TRC‐13003319 {published data only}
- ChiCTR‐TRC‐13003319. Oral zolpidem for improving sleep and then prevention of acute mountain sickness: a single centre, randomized, double‐blind, controlled, prospective trial. www.chictr.org.cn/hvshowproject.aspx?id=6053 (first received 28th June 2013).
ChiCTR‐TRC‐13003590 {published data only}
- ChiCTR‐TRC‐13003590. The Meaning of Intravenous Iron Supplementation In Acute Mountain Sickness: A Randomized, Double‐Blinded, Placebo‐Controlled Trail. http://www.chictr.org.cn/showproj.aspx?proj=5970 (first published 23 June 2013).
NCT00886912 {published data only}
- NCT00886912. Prevention of Acute Mountain Sickness (AMS) by Intermittent Hypoxic Training. http://clinicaltrials.gov/show/NCT00886912 Date of registration: April 21th 2009.
NCT01606527 {published data only}
- NCT01606527. Prospective, Double‐blind, Randomized, Placebo‐controlled Trial of Ibuprofen Versus Placebo for Prevention of Neurologic Forms of Altitude Sickness. http://clinicaltrials.gov/show/NCT01606527 April 13th 2012.
NCT01682551 {published data only}
- NCT01682551. Evaluation of the Prevention and Treatment Effects of Chinese Medicine on High Altitude Illness. http://clinicaltrials.gov/show/NCT01682551 September 5th 2012.
NCT01794078 {published data only}
- NCT01794078. A Randomized, 4‐Sequence, Double‐Blind Study to Test the Safety of Combined Dosing With Aminophylline and Ambrisentan in Exercising Healthy Human Volunteers at Simulated High Altitude. https://clinicaltrials.gov/show/NCT01794078 February 10th 2013.
NCT01993667 {published data only}
- NCT01993667. Acetazolamide for the Prevention of High Altitude Illness: a Comparison of Dosing. https://clinicaltrials.gov/show/NCT01993667 November 12th 2013.
NCT02244437 {published data only}
- NCT02244437. Ibuprofen vs Acetaminophen in the Prevention of Acute Mountain Sickness: A Double Blind, Randomized Controlled Trial. https://clinicaltrials.gov/show/NCT02244437 September 14th 2014.
NCT02450968 {published data only}
- NCT02450968. Dexamethasone for Prophylaxis of Acute Mountain Sickness in Patients With Chronic Obstructive Pulmonary Disease Travelling to Altitude. https://clinicaltrials.gov/show/NCT02450968 May 18th 2015.
NCT02604173 {published data only}
- NCT02604173. A Randomized Controlled Trial of Altitude Sickness Prevention and Efficacy of Comparative Treatments. https://clinicaltrials.gov/show/NCT02604173 November 6th 2015.
NCT02811016 {published data only}
- NCT02811016. Effect of Inhaled Budesonide on the Incidence and Severity of Acute Mountain Sickness at 4559 m. https://clinicaltrials.gov/show/NCT02811016 June 14th 2016.
NCT02941510 {published data only}
- NCT02941510. Inhaled Budesonide for Altitude Illness Prevention. https://clinicaltrials.gov/show/NCT02941510 October 19th 2016.
Additional references
Adams 2004
- Adams J. Ginkgo biloba and acetazolamide for acute mountain sickness: exclusion of high risk, low status groups perpetuates discrimination and inequalities. BMJ 2004;329(7458):171. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anonymous 1892
- Anonymous. Mountain sickness. British Medical Journal 1892;1(1633):829. [PMC free article] [PubMed] [Google Scholar]
Bailey 2009a
- Bailey DM, Bärtsch P, Knauth M, Baumgartner RW. Emerging concepts in acute mountain sickness and high‐altitude cerebral edema: from the molecular to the morphological. Cellular and Molecular Life Sciences 2009;66(22):3583‐94. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Balshem 2011
- Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401‐6. [PUBMED: 21208779] [DOI] [PubMed] [Google Scholar]
Bates 2007
- Bates MG, Thompson AA, Baillie JK. Phosphodiesterase type 5 inhibitors in the treatment and prevention of high altitude pulmonary edema. Current Opinion in Investigational Drugs 2007;8(3):226‐31. [MEDLINE: ] [PubMed] [Google Scholar]
Brok 2009
- Brok J, Thorlund K, Wetterslev J, Gluud C. Apparently conclusive meta‐analyses may be inconclusive‐‐Trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta‐analyses. International Journal of Epidemiology 2009;38(1):287‐98. [PUBMED: 18824466] [DOI] [PubMed] [Google Scholar]
Bärtsch 1992
- Bärtsch P. Treatment of high altitude diseases without drugs. International Journal of Sports Medicine 1992;13 Suppl 1:71‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bärtsch 2004
- Bärtsch P, Bailey DM, Berger MM, Knauth M, Baumgartner RW. Acute mountain sickness: controversies and advances. High Altitude Medicine & Biology 2004;5(2):110‐2. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bärtsch 2007
- Bärtsch P, Gibbs JS. Effect of altitude on the heart and the lungs. Circulation 2007;116(19):2191‐202. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
CATMAT 2007
- Committee to Advise on Tropical Medicine and Travel (CATMAT). Statement on high‐altitude illnesses. An Advisory Committee Statement (ACS). Canada Communicable Disease Report (Relevé des maladies transmissibles au Canada) 2007;33(ACS‐5):1‐20. [MEDLINE: ] [PubMed] [Google Scholar]
Chandramoorthi 2008
- Chandramoorthi GD, Piramanayagam S, Marimuthu P. An insilico approach to high altitude pulmonary edema ‐ Molecular modeling of human beta2 adrenergic receptor and its interaction with salmeterol & nifedipine. Journal of Molecular Modeling 2008;14(9):849‐56. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
CTU 2011 [Computer program]
- Copenhagen Trial Unit. Trial Sequential Analysis Version. Copenhagen: Copenhagen Trial Unit, 2011.
DailyMed
- DailyMed. dailymed.nlm.nih.gov/dailymed/about.cfm 2011; Vol. (Accessed 25 May 2011).
Dehnert 2010
- Dehnert C, Bärtsch P. Can patients with coronary heart disease go to high altitude?. High Altitude Medicine & Biology 2010;11(3):183‐8. [PUBMED: 20919884] [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Dumont 2000
- Dumont L, Mardirosoff C, Tramèr MR. Efficacy and harm of pharmacological prevention of acute mountain sickness: quantitative systematic review. BMJ 2000;321(7256):267‐72. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [PUBMED: 11914310] [DOI] [PubMed] [Google Scholar]
Elphick 2004
- Elphick HL, Elphick DA. Ginkgo biloba and acetazolamide for acute mountain sickness: bias in participants may underestimate effectiveness of agents. BMJ 2004;329(7458):172. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schunemann HJ. What is "quality of evidence"and why is it important to clinicians. BMJ 2008;336(7651):995‐8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction‐GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383‐94. [PUBMED: 21195583] [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Kunz R, Atkins D, Brozek J, Vist G, et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. Journal of Clinical Epidemiology 2011;64(4):395‐400. [PUBMED: 21194891] [DOI] [PubMed] [Google Scholar]
Guyatt 2011c
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso‐Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence—imprecision. Journal of Clinical Epidemiology 2011;64(12):1283‐93. [PUBMED: 21839614] [DOI] [PubMed] [Google Scholar]
Guyatt 2011d
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence—indirectness. Journal of Clinical Epidemiology 2011;64(12):1303‐10. [PUBMED: 21802903] [DOI] [PubMed] [Google Scholar]
Guyatt 2011e
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence—inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294‐302. [PUBMED: 21803546] [DOI] [PubMed] [Google Scholar]
Guyatt 2011f
- Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence—publication bias. Journal of Clinical Epidemiology 2011;64(12):1277‐82. [PUBMED: 21802904] [DOI] [PubMed] [Google Scholar]
Guyatt 2011g
- Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso‐Coello P, et al. GRADE guidelines: 9. Rating up the quality of evidence. Journal of Clinical Epidemiology 2011;64(12):1311‐6. [PUBMED: 21802902] [DOI] [PubMed] [Google Scholar]
Guyatt 2011h
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso‐Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence—study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64(4):407‐15. [PUBMED: 21247734] [DOI] [PubMed] [Google Scholar]
Hackett 1992
- Hackett PH, Roach RC, Hartig GS, Greene ER, Levine BD. The effect of vasodilators on pulmonary hemodynamics in high altitude pulmonary edema: a comparison. International Journal of Sports Medicine 1992;13 Suppl 1:68‐71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hackett 1999
- Hackett PH. High altitude cerebral edema and acute mountain sickness. A pathophysiology update. Advances in Experimental Medicine and Biology 1999;474:23‐45. [PUBMED: 10634991] [DOI] [PubMed] [Google Scholar]
Hackett 2004
- Hackett PH, Roach RC. High altitude cerebral edema. High Altitude Medicine & Biology 2004;5(2):136‐46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. .Available from handbook.cochrane.org.
Higgins 2016
- Higgins JP, Lasserson T, Chandler J, Tovey D, Churchill R. Methodological Expectations of Cochrane Intervention Reviews. Cochrane: London, Version 1.05, 2016.
Hozo 2005
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology 2005;5:13. [PUBMED: 15840177] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hussain 2004
- Hussain MM, Aslam M. Hypoxia and pulmonary acclimatisation at 4578 m altitude: the role of acetazolamide and dexamethasone. Journal of the Pakistan Medical Association 2003;53(10):451‐8. [MEDLINE: ] [PubMed] [Google Scholar]
Höhne 2007
- Höhne C, Pickerodt PA, Francis RC, Boemke W, Swenson ER. Pulmonary vasodilation by acetazolamide during hypoxia is unrelated to carbonic anhydrase inhibition. American Journal of Physiology. Lung Cellular and Molecular Physiology 2007;292(1):L178‐84. [PUBMED: 16936246] [DOI] [PubMed] [Google Scholar]
Imray 2010
- Imray C, Wright A, Subudhi A, Roach R. Acute mountain sickness: pathophysiology, prevention, and treatment. Progress in Cardiovascular Diseases 2010;52(6):467‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kallenberg 2007
- Kallenberg K, Bailey DM, Christ S, Mohr A, Roukens R, Menold E, et al. Magnetic resonance imaging evidence of cytotoxic cerebral edema in acute mountain sickness. Journal of Cerebral Blood Flow and Metabolism 2007;27(5):1064‐71. [PUBMED: 17024110] [DOI] [PubMed] [Google Scholar]
Kayser 2012
- Kayser B, Dumont L, Lysakowski C, Combescure C, Haller G, Tramer MR. Reappraisal of acetazolamide for the prevention of acute mountain sickness: a systematic review and meta‐analysis. High Altitude Medicine & Biology 2012;13(2):82‐92. [PUBMED: 22724610] [DOI] [PubMed] [Google Scholar]
Kleinsasser 2002
- Kleinsasser A, Loeckinger A. Are sildenafil and theophylline effective in the prevention of high‐altitude pulmonary edema?. Medical Hypotheses 2002;59(2):223‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lan 1983
- Lan KKG, Demets D. Discrete sequential boundaries for clinical trials. Biometrika 1983;70(3):659‐63. [Google Scholar]
Leaf 2007
- Leaf DE, Goldfarb DS. Mechanisms of action of acetazolamide in the prophylaxis and treatment of acute mountain sickness. Journal of Applied Physiology 2007;102(4):1313‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Leissner 2009
- Leissner KB, Mahmood FU. Physiology and pathophysiology at high altitude: considerations for the anesthesiologist. International Journal of Anesthesia 2009;23(4):543‐53. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Low 2012
- Low EV, Avery AJ, Gupta V, Schedlbauer A, Grocott MP. Identifying the lowest effective dose of acetazolamide for the prophylaxis of acute mountain sickness: systematic review and meta‐analysis. BMJ (Clinical research ed.) 2012;345:e6779. [PUBMED: 23081689] [DOI] [PMC free article] [PubMed] [Google Scholar]
Luks 2008a
- Luks AM. Do we have a "best practice" for treating high altitude pulmonary edema?. High Altitude Medicine & Biology 2008;9(2):111‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Luks 2008b
- Luks AM, Swenson ER. Medication and dosage considerations in the prophylaxis and treatment of high‐altitude illness. Chest 2008;133(3):744‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Luks 2010
- Luks AM, McIntosh SE, Grissom CK, Auerbach PS, Rodway GW, Schoene RB, Wilderness Medical Society. Wilderness Medical Society consensus guidelines for the prevention and treatment of acute altitude illness. Wilderness & Environmental Medicine 2010;21(2):146‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Luks 2014
- Luks AM, McIntosh SE, Grissom CK, Auerbach PS, Rodway GW, Schoene RB, et al. Wilderness Medical Society practice guidelines for the prevention and treatment of acute altitude illness: 2014 update. Wilderness & Environmental Medicine 2014;25(4 Suppl):S4‐14. [PUBMED: 25498261] [DOI] [PubMed] [Google Scholar]
Maggiorini 1998
- Maggiorini M, Müller A, Hofstetter D, Bärtsch P, Oelz O. Assessment of acute mountain sickness by different score protocols in the Swiss Alps. Aviation, Space, and Environmental Medicine 1998;69(12):1186‐92. [PUBMED: 9856545] [PubMed] [Google Scholar]
Maggiorini 2010
- Maggiorini M. Prevention and treatment of high‐altitude pulmonary edema. Progress in Cardiovascular Diseases 2010;52(6):500‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Monge 1942
- Monge C. Life in the Andes and chronic mountain sickness. Science 1942;95(2456):79‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Murata 2004
- Murata T, Hori M, Sakamoto K, Karaki H, Ozaki H. Dexamethasone blocks hypoxia‐induced endothelial dysfunction in organ‐cultured pulmonary arteries. American Journal of Respiratory and Critical Care Medicine 2004;170(6):647‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Murata 2005
- Murata T, Suzuki N, Yamawaki H, Sato K, Hori M, Karaki H, et al. Dexamethasone prevents impairment of endothelium‐dependent relaxation in arteries cultured with fetal bovine serum. European Journal of Pharmacology 2005;515(1‐3):134‐41. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Naeije 2010
- Naeije R. Physiological adaptation of the cardiovascular system to high altitude. Progress in Cardiovascular Diseases 2010;52(6):456‐66. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ozaki 2001
- Ozaki M, Kawashima S, Yamashita T, Ohashi Y, Rikitake Y, Inoue N, et al. Reduced hypoxic pulmonary vascular remodeling by nitric oxide from the endothelium. Hypertension 2001;37(2):322‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Palmer 2010
- Palmer BF. Physiology and pathophysiology with ascent to altitude. American Journal of the Medical Sciences 2010;340(1):69‐77. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Pandit 2014
- Pandit A, Karmacharya P, Pathak R, Giri S, Aryal MR. Efficacy of NSAIDs for the prevention of acute mountain sickness: a systematic review and meta‐analysis. Journal of Community Hospital Internal Medicine Perspectives 2014;4(4):1‐7. [PUBMED: 25317267] [DOI] [PMC free article] [PubMed] [Google Scholar]
Paralikar 2010
- Paralikar SJ, Paralikar JH. High‐altitude medicine. Indian Journal of Occupational and Environmental Medicine 2010;14(1):6‐12. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pasha 2010
- Pasha MA, Newman JH. High‐altitude disorders: pulmonary hypertension: pulmonary vascular disease: the global perspective. Chest 2010;137 Suppl(6):13‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
RevMan 5.3 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3.. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ri‐Li 2003
- Ri‐Li G, Chase PJ, Witkowski S, Wyrick BL, Stone JA, Levine BD, et al. Obesity: associations with acute mountain sickness. Annals of Internal Medicine 2003;139(4):253‐7. [PUBMED: 12965980] [DOI] [PubMed] [Google Scholar]
Richalet 2005
- Richalet JP, Gratadour P, Robach P, Pham I, Déchaux M, Joncquiert‐Latarjet A, et al. Sildenafil inhibits altitude‐induced hypoxemia and pulmonary hypertension. American Journal of Respiratory and Critical Care Medicine 2005;171(3):275‐81. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ritchie 2012
- Ritchie ND, Baggott AV, Andrew Todd WT. Acetazolamide for the prevention of acute mountain sickness‐‐a systematic review and meta‐analysis. Journal of Travel Medicine 2012;19(5):298‐307. [PUBMED: 22943270] [DOI] [PubMed] [Google Scholar]
Rodríguez de Romo 2002
- Rodríguez de Romo AC. Daniel Vergara Lope and Carlos Monge Medrano: two pioneers of high altitude medicine. High Altitude Medicine & Biology 2002;3(3):299‐309. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Scherrer 2010
- Scherrer U, Rexhaj E, Jayet PY, Allemann Y, Sartori C. New insights in the pathogenesis of high‐altitude pulmonary edema. Progress in Cardiovascular Diseases 2010;52(6):485‐92. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schneider 2002
- Schneider M, Bernasch D, Weymann J, Holle R, Bärtsch P. Acute mountain sickness: influence of susceptibility, preexposure, and ascent rate. Medicine and Science in Sports and Exercise 2002;34(12):1886‐91. [PUBMED: 12471292] [DOI] [PubMed] [Google Scholar]
Schoene 2004
- Schoene RB. Unraveling the mechanism of high altitude pulmonary edema. High Altitude Medicine & Biology 2004;5(2):125‐35. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schoene 2008
- Schoene RB. Illnesses at high altitude. Chest 2008;134(2):402‐16. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schoonman 2008
- Schoonman GG, Sandor PS, Nirkko AC, Lange T, Jaermann T, Dydak U, et al. Hypoxia‐induced acute mountain sickness is associated with intracellular cerebral edema: a 3 T magnetic resonance imaging study. Journal of Cerebral Blood Flow and Metabolism 2008;28(1):198‐206. [PUBMED: 17519973] [DOI] [PubMed] [Google Scholar]
Seupaul 2012
- Seupaul RA, Welch JL, Malka ST, Emmett TW. Pharmacologic prophylaxis for acute mountain sickness: a systematic shortcut review. Annals of Emergency Medicine 2012;59(4):307‐317.e1. [PUBMED: 22153998] [DOI] [PubMed] [Google Scholar]
Stedman 2011
- Stedman MR, Curtin F, Elbourne DR, Kesselheim AS, Brookhart MA. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2011;40(6):1732‐4. [PUBMED: 20026595] [DOI] [PubMed] [Google Scholar]
Stream 2008
- Stream JO, Grissom CK. Update on high‐altitude pulmonary edema: pathogenesis, prevention, and treatment. Wilderness & Environmental Medicine 2008;19(4):293‐303. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Swenson 2006
- Swenson ER. Carbonic anhydrase inhibitors and hypoxic pulmonary vasoconstriction. Respiratory Physiology & Neurobiology 2006;151(2‐3):209‐16. [PUBMED: 16376158] [DOI] [PubMed] [Google Scholar]
Swenson 2007
- Swenson E, Teppema L. Prevention of acute mountain sickness by acetazolamide: as yet an unfinished story. Journal of Applied Physiology 2007;102(4):1305‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Tang 2014
- Tang E, Chen Y, Luo Y. Dexamethasone for the prevention of acute mountain sickness: systematic review and meta‐analysis. International Journal of Cardiology 2014;173(2):133‐8. [PUBMED: 24679688] [DOI] [PubMed] [Google Scholar]
Thorlund 2009
- Thorlund K, Devereaux PJ, Wetterslev J, Guyatt G, Ioannidis JP, Thabane L, et al. Can trial sequential monitoring boundaries reduce spurious inferences from meta‐analyses?. International Journal of Epidemiology 2009;38(1):276‐86. [PUBMED: 18824467] [DOI] [PubMed] [Google Scholar]
Tintinger 2010
- Tintinger GR, Feldman C, Theron AJ, Anderson R. Montelukast: more than a cysteinyl leukotriene receptor antagonist?. Scientific World Journal 2010;10:2403‐13. [PUBMED: 21170491] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wan 2014
- Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology 2014;14:135. [PUBMED: 25524443] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wetterslev 2008
- Wetterslev J, Thorlund K, Brok J, Gluud C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta‐analysis. Journal of Clinical Epidemiology 2008;61(1):64‐75. [PUBMED: 18083463] [DOI] [PubMed] [Google Scholar]
Wilson 2009
- Wilson MH, Newman S, Imray CH. The cerebral effects of ascent to high altitudes. Lancet Neurology 2009;8(2):175‐91. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Windsor 2009
- Windsor JS, Firth PG, Grocott MP, Rodway GW, Montgomery HE. Mountain mortality: a review of deaths that occur during recreational activities in the mountains. Postgraduate Medical Journal 2009;85(1004):316‐21. [PUBMED: 19528307] [DOI] [PubMed] [Google Scholar]
Wright 2008
- Wright A, Brearey S, Imray C. High hopes at high altitudes: pharmacotherapy for acute mountain sickness and high‐altitude cerebral and pulmonary oedema. Expert Opinion on Pharmacotherapy 2008;9(1):119‐27. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Yang 2007
- Yang B, Wang GY, Chen B, Qin RB, Xi SL, Chen L. Anti‐hypoxia and anti‐oxidation effects of aminophylline on human with acute high‐altitude exposure. Chinese Medical Sciences Journal 2007;22(1):62‐5. [PUBMED: 17441321] [PubMed] [Google Scholar]
Zafren 2014
- Zafren K. Prevention of high altitude illness. Travel Medicine and Infectious Disease 2014;12(1):29‐39. [PUBMED: 24393671] [DOI] [PubMed] [Google Scholar]
Zhao 2001
- Zhao L, Mason NA, Morrell N, Kojonazarov B, Sadykov A, Maripov A, et al. Sildenafil inhibits hypoxia‐induced pulmonary hypertension. Circulation 2001;104(4):424‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Martí‐Carvajal 2012
- Martí‐Carvajal Arturo J, Hidalgo R, Simancas‐Racines D. Interventions for preventing high altitude illness. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD009761] [DOI] [Google Scholar]


