Abstract
Background
Music therapy is a therapeutic approach that uses musical interaction as a means of communication and expression. Within the area of serious mental disorders, the aim of the therapy is to help people improve their emotional and relational competencies, and address issues they may not be able to using words alone.
Objectives
To review the effects of music therapy, or music therapy added to standard care, compared with placebo therapy, standard care or no treatment for people with serious mental disorders such as schizophrenia.
Search methods
We searched the Cochrane Schizophrenia Group’s Trials Study‐Based Register (December 2010 and 15 January, 2015) and supplemented this by contacting relevant study authors, handsearching of music therapy journals and manual searches of reference lists.
Selection criteria
All randomised controlled trials (RCTs) that compared music therapy with standard care, placebo therapy, or no treatment.
Data collection and analysis
Review authors independently selected, quality assessed and data extracted studies. We excluded data where more than 30% of participants in any group were lost to follow‐up. We synthesised non‐skewed continuous endpoint data from valid scales using a standardised mean difference (SMD). We employed a fixed‐effect model for all analyses. If statistical heterogeneity was found, we examined treatment dosage (i.e. number of therapy sessions) and treatment approach as possible sources of heterogeneity.
Main results
Ten new studies have been added to this update; 18 studies with a total 1215 participants are now included. These examined effects of music therapy over the short, medium, and long‐term, with treatment dosage varying from seven to 240 sessions. Overall, most information is from studies at low or unclear risk of bias
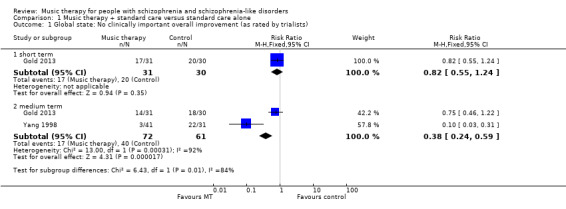
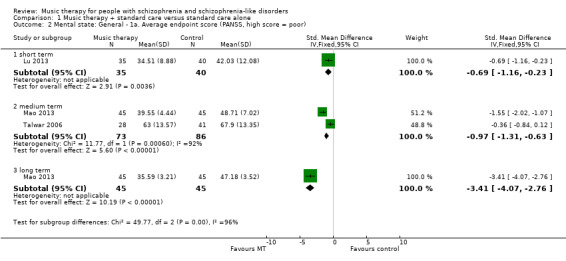
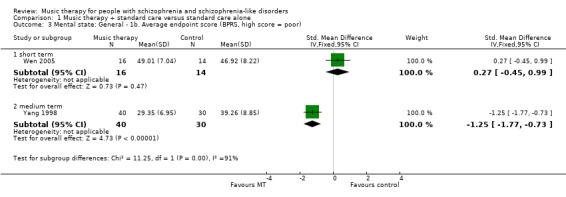
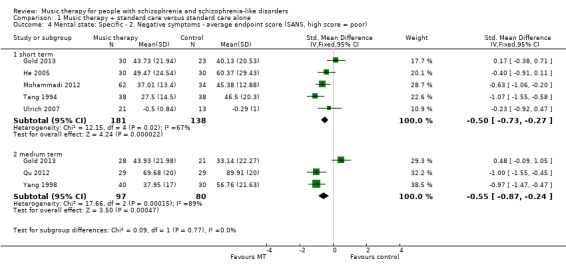
A positive effect on global state was found for music therapy compared to standard care (medium term, 2 RCTs, n = 133, RR 0.38 95% confidence interval (CI) 0.24 to 0.59, low‐quality evidence, number needed to treat for an additional beneficial outcome NNTB 2, 95% CI 2 to 4). No binary data were available for other outcomes. Medium‐term continuous data identified good effects for music therapy on negative symptoms using the Scale for the Assessment of Negative Symptoms (3 RCTs, n = 177, SMD ‐ 0.55 95% CI ‐0.87 to ‐0.24, low‐quality evidence). General mental state endpoint scores on the Positive and Negative Symptoms Scale were better for music therapy (2 RCTs, n = 159, SMD ‐0.97 95% CI ‐1.31 to ‐0.63, low‐quality evidence), as were average endpoint scores on the Brief Psychiatric Rating Scale (1 RCT, n = 70, SMD ‐1.25 95% CI ‐1.77 to ‐0.73, moderate‐quality evidence). Medium‐term average endpoint scores using the Global Assessment of Functioning showed no effect for music therapy on general functioning (2 RCTs, n = 118, SMD ‐0.19 CI ‐0.56 to 0.18, moderate‐quality evidence). However, positive effects for music therapy were found for both social functioning (Social Disability Screening Schedule scores; 2 RCTs, n = 160, SMD ‐0.72 95% CI ‐1.04 to ‐0.40), and quality of life (General Well‐Being Schedule scores: 1 RCT, n = 72, SMD 1.82 95% CI 1.27 to 2.38, moderate‐quality evidence). There were no data available for adverse effects, service use, engagement with services, or cost.
Authors' conclusions
Moderate‐ to low‐quality evidence suggests that music therapy as an addition to standard care improves the global state, mental state (including negative and general symptoms), social functioning, and quality of life of people with schizophrenia or schizophrenia‐like disorders. However, effects were inconsistent across studies and depended on the number of music therapy sessions as well as the quality of the music therapy provided. Further research should especially address the long‐term effects of music therapy, dose‐response relationships, as well as the relevance of outcome measures in relation to music therapy.
Plain language summary
Music therapy for schizophrenia or schizophrenia‐like disorders
Review Question
What are the effects of providing music therapy or adding music therapy to treatment for people with schizophrenia or schizophrenia‐like disorders?
Background
Characteristics of schizophrenia and schizophrenia‐like disorders are disordered thoughts, feelings, beliefs and perceptions. People with schizophrenia often have two main types of symptoms: the acute symptoms of hearing voices or seeing things (hallucinations) and strange beliefs (delusions), and chronic symptoms such as low mood/depression, social withdrawal, and memory problems. Music therapy is a therapeutic approach that uses music experiences to help people with serious mental disorders improve their emotional and relational competencies and addresses issues that they may not be able to using words alone.
Searching for evidence
We ran electronic searches up to January 2015 for trials randomising people with schizophrenia or schizophrenia‐like disorders to receive music therapy or standard care. We found and checked 176 potential studies.
Evidence found
Eighteen trials with a total of 1215 participants met the review requirements and provided useful data.
The evidence currently available is of low to moderate quality. The results of these studies suggest that music therapy improves global state and may also improve mental state, functioning, and quality of life if a sufficient number of music therapy sessions are provided.
Conclusions
Music therapy seems to help people with schizophrenia but further research is needed to confirm the positive effects found in this review. This research should especially address the long‐term effects of music therapy, the quality of music therapy provided and measure outcomes relevant to music therapy.
Summary of findings
for the main comparison.
| Music therapy compared with standard care for schizophrenia and schizophrenia‐like disorders | ||||||
|
Patient or population: People with schizophrenia and schizophrenia‐like disorders Settings: Individual and group setting Intervention: Music therapy (in addition to standard care) Comparison: Standard care alone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Risk with standard care | Risk difference with music therapy | |||||
|
Global state: No clinically important overall improvement (as rated by individual trials) ‐ medium term (follow‐up: 3‐6 months) |
Low risk population | RR 0.38 (0.24 to 0.59) | 133 (2 RCTs) | ⊕⊕⊝⊝ low1,2,3,4 | ||
| 300 per 1000 | 114 per 1000 (72 to 177) | |||||
| Moderate risk population | ||||||
| 655 per 1000 | 249 per 1000 (157 to 386) | |||||
| High risk population | ||||||
| 800 per 1000 | 304 per 1000 (192 to 472) | |||||
|
Mental state: specific ‐ negative symptoms ‐ average endpoint score (SANS, high score = poor) medium term (follow‐up: 3‐6 months) |
The mean mental state: specific ‐ 2. negative symptoms ‐ average endpoint score (SANS, high score = poor) in the intervention groups was 0.55 lower (0.87 lower to 0.24 lower) |
177 (3 RCTs) | ⊕⊕⊝⊝ low1, 3 | |||
| Mental state: general ‐ average endpoint score (PANSS, high score = poor) ‐ medium term, (follow‐up: 3‐6 months) | The mean mental state: general ‐ 1a. average endpoint score (PANSS, high score = poor) ‐ medium term in the intervention groups was 0.97 lower (1.31 lower to 0.63 lower) | 159 (2 RCTs) | ⊕⊕⊝⊝ low1,2,3,5 | |||
| Mental state: General ‐ average endpoint score (BPRS, high score = poor) ‐ medium term (follow‐up: 3‐6 months) | The mean mental state: general ‐ 1b. average endpoint score (BPRS, high score=poor) in the intervention groups was 1.25 lower (1.77 lower to 0.73 lower) | 70 (1 RCT) | ⊕⊕⊕⊝ moderate1,3,5 | |||
| Functioning: general ‐ average endpoint score (GAF, high score = good) medium term (follow‐up: 3‐6 months) | The mean general functioning ‐ a. average endpoint score (GAF, high score = good) in the intervention groups was 0.19 lower (0.56 lower to 0.18 higher) | 118 (2 RCTs) | ⊕⊕⊕⊝ moderate3 | |||
|
Functioning: social ‐ average endpoint score (SDSS, high score = poor) medium term, (follow‐up: 3‐6 months) |
The mean social functioning: average endpoint score (SDSS, high score = poor) ‐ medium term in the intervention groups was 0.72 lower (1.04 lower to 0.4 lower) | 160 (2 RCTs) | ⊕⊕⊕⊝ moderate1,3,5 | |||
|
Quality of life: general ‐ average endpoint score (GWB, high score = good) ‐ short term (follow‐up: less than 3 months) |
The mean quality of life: general ‐ average endpoint score (GWB, high score = good) in the intervention groups was 1.82 higher (1.27 higher to 2.38 higher) | 72 (1 RCT) | ⊕⊕⊕⊝ moderate1,3,5 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk Ratio; RCT: Randomised controlled trial; SANS: Scale for the Assessment of Negative Symptoms; SDSS: Social Disability Screening Schedule; PANSS: Positive and Negative Syndrome Scale; BPRS: The Brief Psychiatric Rating Scale; GAF: Global Assessment of Functioning; GWB: General Well‐Being Schedule. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Risk of bias ‐ limitations in study design such as poorly reported randomisation, allocation concealment, blinding or unclear outcome reporting.
2 Inconsistency ‐ heterogeneity between studies was high.
3 Imprecision ‐ the optimal information size is lower than 300 events.
4 Large effect ‐ RR < 0.5
5 Large effect ‐ the effect was in the large range according to Cohen 1988.
Background
Description of the condition
Schizophrenia is a serious mental disorder with considerable impact on individuals and their families. It may take a life‐long course, although full recovery is also observed in a proportion of cases. Symptoms of schizophrenia are usually classified as 'positive' (where something is added, such as hallucinations or paranoid ideation) and 'negative' (where something is missing, such as the ability to express oneself emotionally or to form satisfying relationships with others). The aspects of schizophrenia that are linked to losing and regaining creativity, emotional expressiveness, social relationships, and motivation may be particularly important in relation to music therapy (Gold 2009).
Description of the intervention
Music therapy is generally defined as "a systematic process of intervention wherein the therapist helps the client to promote health, using music experiences and the relationships that develop through them as dynamic forces of change (Bruscia 1998)." It often addresses intra‐ and interpsychic, as well as social processes by using musical interaction as a means of communication, expression, and transformation. Within the area of serious mental disorders, the aim of the therapy is to help people improve their emotional and relational competencies, and to address issues they may not be able to using words alone.
Music therapy as a profession (with its own academic and clinical training courses) was first introduced in North and South America in the 1940s. The first European country (Austria) followed in 1959, and soon after that many other countries followed (Maranto 1993). It is now a state‐registered profession in some countries (Austria, Latvia, UK). A survey based in Germany showed that music therapy was used in 37% of all psychiatric and psychosomatic clinics (Andritzky 1996).
Music therapy models practised today are most commonly based on psychodynamic, humanistic, cognitive behavioural or developmental theory (Gold 2009; Wigram 2002). Traditionally, behavioural models have been more prevalent in the USA, whereas psychodynamic and humanistic models have dominated in Europe; in other parts of the world there may be mixed influences. However, the various theoretical models in music therapy and their applications do not necessarily form distinct categories, but rather prototypical positions in a varied but coherent field.
Other than by their theoretical orientation, approaches in music therapy may also be described by their modality ('active' versus 'receptive'), their level of structure, and the focus on the music itself versus on verbal processing of the music experiences. The active modality includes all activities where clients are invited to play or sing. This includes a variety of activities ranging from free improvisation to reproducing songs. Receptive techniques, on the other hand, refer to clients listening to music; this may be played by the therapist for the client, or recorded music may be selected by either therapist or client. Although some models of music therapy rely exclusively on one mode of musical interaction, most models use a mixture of both.
Secondly, the level of predefined structuring may vary. Some therapists may impose a greater degree of structure than others, either by using more structured forms of music‐making or by selecting activities before the sessions, as opposed to developing these in dialogue with the client. The level of structuring may depend on the client's needs, but may also vary between music therapy models. For example, it has been observed that there are considerable differences between American and European approaches in the level of structuring (Wigram 2002). A recent review concluded that extreme positions were rarely observed and most studies used some structure as well as some flexibility (Gold 2009). A third relevant distinction concerns the focus of attention. Some music therapists and music therapy models may focus more on the processes occurring within the music itself, whereas others have a greater focus on the verbal reflection of the client's issues brought forth by these musical processes (Gold 2009).
In summary, music therapy for people with serious mental disorders often relies on a mixture of active and receptive techniques, even though musical improvisation and verbalisation of the musical interaction are often central. Music therapists working in clinical practice with this population usually have extensive training. Music therapy with patients in mental health care is usually provided either in an individual or a small group setting and is often continued over an extended period of time (Wigram 1999). Active participation is crucial for the success of music therapy. Participants do not need musical skills, but a motivation to work actively within a music therapy process is important.
How the intervention might work
Music therapy is often justified by a proposed need for a medium for communication and expression other than verbal language. Some people with serious mental disorders may be too disturbed to use verbal language alone efficiently as a therapeutic medium. Research on parent‐infant communication is often cited as a rationale for using music therapy; this body of research has shown that the earliest communication that humans develop has many 'musical' qualities (Ansdell 2010a; Stern 2010; Trevarthen 2000). More pragmatically, clinical reports have suggested that music therapy can have unique motivating, relationship‐building, and emotionally expressive qualities that may help even those who do not benefit from verbal therapy (Rolvsjord 2001; Solli 2008). The musical interaction in music therapy might also support a re‐establishment of musical resources and competencies affecting the patient's everyday life. This has been described from a patient perspective as an important factor in music therapy increasing quality of life (Ansdell 2010b).
Why it is important to do this review
In its early years, music therapy was established in selected hospitals, by enthusiastic individuals (Mössler 2011a), on the basis of successful case histories. The degree to which music therapy is available still varies greatly across and even within countries. As music therapy is becoming more established as a profession and as a service in mental health care, the need for documented evidence of its effects increases.
Objectives
To review the effects of music therapy, or music therapy added to standard care, compared with placebo therapy, standard care or no treatment for people with serious mental disorders such as schizophrenia.
Methods
Criteria for considering studies for this review
Types of studies
All relevant randomised controlled trials (RCTs). If a trial was described in a way that implied that the study was randomised, we included such trials in a sensitivity analysis. If there was no substantive difference within primary outcomes (see Types of outcome measures) when these 'implied randomisation' studies were added, then we included them in the final analysis. If there was a substantive difference, we only used randomised trials and we described the results of the sensitivity analysis in the text. We excluded quasi‐randomised studies, such as those allocating by using alternate days of the week.
Types of participants
People with schizophrenia or schizophrenia‐like disorders, diagnosed by any criteria, irrespective of gender, age or nationality.
Types of interventions
1. Music therapy or music therapy added to standard care
Music therapy is defined as "a systematic process of intervention wherein the therapist helps the client to promote health, using music experiences and the relationships that develop through them as dynamic forces of change" (Bruscia 1998). This definition of music therapy is rather broad and inclusive of different models, but distinguishes clearly from music listening alone: for it to be music therapy, there has to be a therapist, and the client‐therapist relationship as well as the music experience are relevant factors.
2. Placebo
Defined as an alternative therapy designed to control for effects of the therapist's attention.
3. Standard care or no treatment
Types of outcome measures
Where possible, we reported outcomes for the short term (up to 12 weeks), medium term (13 to 26 weeks), and long term (more than 26 weeks).
Primary outcomes
There is currently no consensus as to what should be the primary outcomes of music therapy for people with schizophrenia. Goals described by music therapists tend to describe 'soft' outcomes such as well‐being, self‐esteem, the ability to express oneself and to relate to others, or a sense of identity; outcomes such as overall symptom reduction or improved general functioning seem to be only indirectly related to those goals. However, symptom‐related outcomes are most commonly measured in research studies. Notably, measures of negative symptoms include impairments in the ability to express oneself and to relate to others, but also include other domains. Because of the importance to people with schizophrenia we regard the following as primary outcomes.
1. Global state
1.1 Clinically important change in global state ‐ as defined by individual studies
2. Mental state
2.1 Clinically important change in general mental state ‐ as defined by individual studies 2.2 Clinically important change in specific symptoms: negative symptoms ‐ as defined by individual studies
3. Functioning
3.1 Clinically important change in general functioning ‐ as defined by individual studies 3.2 Clincially important change in social functioning ‐ as defined by individual studies
Secondary outcomes
A more comprehensive and general list of relevant outcomes has been defined by the Cochrane Schizophrenia Group as follows. Most of these outcomes and their particular sub‐categories are defined as secondary outcomes for this review.
1. Global state
1.1 Relapse 1.2 Time to relapse 1.3 Any change in global state 1.4 Average endpoint global state score 1.5 Average change in global state scores 1.6 Change in medication dose
2. Mental state
2.1 Any change in general mental state 2.2 Average endpoint general mental state score 2.3 Average change in general mental state scores 2.4 Clinically important change in other specific symptoms (e.g. positive, cognitive) 2.5 Any change in specific symptoms 2.6 Average endpoint specific symptom score 2.7 Average change in specific symptom scores
3. Functioning
3.1 General
3.1.1 Any change in general functioning 3.1.2 Average endpoint general functioning score 3.1.3 Average change in general functioning scores
3.2 Specific
3.2.1 Clinically important change in other specific aspects of functioning (such as cognitive functioning or life skills) 3.2.2 Any change in specific aspects of functioning (such as cognitive functioning, social functioning or life skills) 3.2.3 Average endpoint specific aspects of functioning (such as cognitive functioning, social functioning or life skills) 3.3.4 Average change in specific aspects of functioning (such as cognitive functioning, social functioning or life skills)
4. Leaving the study early
4.1 For specific reasons 4.2 For general reasons
5. Service outcomes
5.1 Hospitalisation 5.2 Time to hospitalisation
6. Behaviour
6.1 Clinically important change in general behaviour 6.2 Any change in general behaviour 6.3 Average endpoint general behaviour score 6.4 Average change in general behaviour scores 6.5 No clinically important change in specific aspects of behaviour 6.6 Not any change in specific aspects of behaviour 6.7 Average endpoint specific aspects of behaviour 6.8 Average change in specific aspects of behaviour
7. Adverse effects/event
7.1 Clinically important general adverse effects 7.2 Any general adverse effects 7.3 Average endpoint general adverse effect score 7.4 Average change in general adverse effect scores 7.5 Clinically important change in specific adverse effects 7.6 Any change in specific adverse effects 7.7 Average endpoint specific adverse effects 7.8 Average change in specific adverse effects 7.9 Adverse event: death (suicide or natural causes)
8. Engagement with services
8.1 Clinically important engagement 8.2 Any engagement 8.3 Average endpoint engagement score 8.4 Average change in engagement scores
9. Satisfaction with treatment
9.1 Recipient of care satisfied with treatment 9.2 Recipient of care average satisfaction score 9.3 Recipient of care average change in satisfaction scores 9.4 Carer satisfied with treatment 9.5 Carer average satisfaction score 9.6 Carer average change in satisfaction scores
10. Quality of life
10.1 Clinically important change in quality of life 10.2 Any change in quality of life 10.3 Average endpoint quality of life score 10.4 Average change in quality of life scores 10.5 Clinically important change in specific aspects of quality of life 10.6 Any change in specific aspects of quality of life 10.7 Average endpoint specific aspects of quality of life 10.8 Average change in specific aspects of quality of life
11. Economic outcomes
11.1 Direct costs 11.2 Indirect costs
'Summary of findings' table
We used the GRADE approach to interpret findings (Schünemann 2011). A 'Summary of findings' table was created using the GRADE profiler into which data were imported from RevMan. This table provides outcome‐specific information concerning the overall quality of evidence from each included study and the magnitude of effect of the interventions examined. Available data on those outcomes that we rated as most important regarding patient‐care and decision making are presented in this table. We selected the following main outcomes for inclusion in the Table 1.
Global state: no clinically important overall improvement
Mental state: specific ‐ negative symptoms
Mental state: general mental state
General functioning
Social functioning
Quality of Life
Search methods for identification of studies
1. Cochrane Schizophrenia Group’s Trials Register
On January 15, 2015, the Information Specialist searched the Cochrane Schizophrenia Group’s Study‐Based Register of Trials using the following search strategy:
(*music*) in Intervention Field of STUDY.
The Cochrane Schizophrenia Group’s Registry of Trials is compiled by systematic searches of major resources (including AMED, BIOSIS, CINAHL, Embase, MEDLINE, PsycINFO, PubMed, and registries of clinical trials) and their monthly updates, handsearches, grey literature, and conference proceedings (see Group Module). There is no language, date, document type, or publication status limitations for inclusion of records into the register.
For previous searches, please see Appendix 1.
2. Handsearching
We searched the three American music therapy journals (Journal of Music Therapy, Music Therapy and Music Therapy Perspectives) as reissued on CD‐ROM by the American Music Therapy Association using the search term random* and then manually browsing through the results. The search covered the Journal of Music Therapy (1964‐1998), Music Therapy (1981‐1996) and Music Therapy Perspectives (1982‐1984, 1986‐1998).
3. Reference searching
We also inspected the references of all identified studies, included or excluded, for more studies.
4. Personal contact
We contacted corresponding authors of relevant reviews or studies to enquire about other sources of relevant information.
5. Review articles
We inspected existing review articles pertinent to the topic of this review (Oerter 2001; Silverman 2003b) for references to any additional studies.
6. Cited reference search (forward search)
We searched ISI Web of Science for articles citing any of the included studies, in order to identify any more recent studies that might have been missed.
Data collection and analysis
We have updated our methods in line with current Cochrane policy. For previous data collection and analysis methods please see Appendix 2. We have now for the most part adhered to the current template as provided by the Cochrane Schizophrenia Group (CSG). Substantial deviations from the template, in line with our protocol and previous review versions, are:
definite exclusion of therapist‐rated scales, rather than vague statement about possible exclusion (Data extraction and management);
exclusion of skewed data that cannot be transformed, rather than presenting skewed data from studies of less than 200 participants in additional tables (Data extraction and management);
use of standardised mean differences (SMDs) rather than mean differences (MDs) (Measures of treatment effect);
subgroups to be analysed (Subgroup analysis and investigation of heterogeneity).
Selection of studies
Review authors XJC, TOH, and KM independently inspected citations from the searches and identified relevant abstracts. Review author XJC first inspected study reports written in Chinese and then translated relevant sections. Those translated sections were then re‐inspected by CG, TOH and KM to ensure reliability. Where disputes arose, we acquired the full report for more detailed scrutiny. If citations met the inclusion criteria, we obtained full reports of the papers for more detailed inspection. Where it was not possible to resolve disagreement by discussion, we attempted to contact authors of the study for clarification.
Data extraction and management
1. Extraction
Review authors XJC, KM, and MG extracted data from all included studies. Any disagreement was discussed and review author CG helped to clarify any ongoing problems. We extracted data presented only in graphs and figures whenever possible, but we only included the data if two review authors independently had the same result. We reported all decisions and, if necessary, we contacted the authors of studies through an open‐ended request in order to obtain missing information or for clarification. If multi‐centre studies had been included, we would have extracted data relevant to each component centre separately where possible.
2. Management
We extracted data onto standard, simple forms. The emergence of studies with mixed samples (including eligible and non‐eligible participants) in the present update necessitated an additional decision rule. We decided to include such studies only if (i.) individual patient data or group data for the eligible subsample were available to us; (ii.) the number of eligible participants was at least as high as the sample of the smallest study with a non‐mixed sample; and (iii.) outcomes were relevant to schizophrenia (as judged by their use also in at least one non‐mixed sample).
2.1 Scale‐derived data
We included continuous data from rating scales only if: a. the psychometric properties of the measuring instrument have been described in a peer‐reviewed journal (Marshall 2000); and b. the measuring instrument has not been written or modified by one of the trialists for that particular trial.
To be considered in this review, the measuring instrument should either be i. a self‐report or ii. completed by an independent rater or relative (not the therapist). We realise that this is not often reported clearly. Therefore, detailed information on this was provided in the Characteristics of included studies section.
2.2 Endpoint versus change data
There are advantages of both endpoint and change data. Change data can remove a component of between‐person variability from the analysis. On the other hand, calculation of change needs two assessments (baseline and endpoint), which can be difficult to measure in unstable conditions such as schizophrenia. We decided primarily to use endpoint data, and would have used change data if the former had not been available.
2.3 Skewed data
Continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, we aimed to apply the following standards to all data before inclusion: a) standard deviations (SDs) and means were reported in the paper or were obtainable from the authors; b) when a scale starts from a finite number (such as zero), the SD, when multiplied by two, was less than the mean (as otherwise the mean was unlikely to be an appropriate measure of the centre of the distribution, (Altman 1996); c) if a scale started from a positive value (such as the Positive and Negative Symptoms Scale (PANSS, Kay 1986) which can have values from 30 to 210), the calculation described above was modified to take the scale starting point into account. In these cases skewness was present if 2 SD > (S‐S min), where S is the mean score and S min is the minimum score. Endpoint scores on scales often have a finite start and endpoint and these rules can be applied. When continuous data are presented on a scale that includes a possibility of negative values (such as change data), it is difficult to tell whether data are skewed or not. When individual patient data were available, we attempted to remove skewness through log‐transformation. Where this was not possible, we did not consider skewed data in this review.
2.4 Common measure
To facilitate comparison between trials, we would have converted variables that can be reported in different metrics, such as days in hospital (mean days per year, per week or per month) to a common metric (e.g. mean days per month).
2.5 Conversion of continuous to binary
Where possible, we made efforts to convert outcome measures to dichotomous data. This can be done by identifying cut‐off points on rating scales and dividing participants accordingly into 'clinically improved' or 'not clinically improved'. It is generally assumed that if there is a 50% reduction in a scale‐derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the PANSS (Kay 1986), this could be considered as a clinically significant response (Leucht 2005; Leucht 2005a). If data based on these thresholds were not available, we used the primary cut‐off presented by the original authors.
2.6 Direction of graphs
We entered data in such a way that the area to the left of the line of no effect indicated a favourable outcome for music therapy when the outcome was negative (where 'high' means 'poor'), and reversed for positive outcomes (where 'high' means 'good').
Assessment of risk of bias in included studies
Review authors XJC and KM independently assessed the risk of bias for evaluating trial quality by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). This set of criteria is based on evidence of associations between overestimate of effect and high risk of bias of the article such as sequence generation, allocation concealment, blinding, incomplete outcome data, and selective reporting. If the raters disagreed, we made the final rating by consensus with the involvement of CG. Where inadequate details of randomisation and other characteristics of trials were provided, we contacted the authors of the studies in order to obtain further information. We reported non‐concurrence in quality assessment, but if disputes arose as to which category a trial was to be allocated, again, we resolved this by discussion. We noted the level of risk of bias in both the text of the review and in the Table 1.
Measures of treatment effect
1. Binary data
For binary outcomes, we calculated a standard estimation of the fixed‐effect risk ratio (RR) and its 95% confidence interval (CI). It has been shown that RR is more intuitive (Boissel 1999) than odds ratios and that odds ratios tend to be interpreted as RR by clinicians (Deeks 2000). For statistically significant results, we calculated the number needed to treat for an additional beneficial outcome (NNTB) and the number needed to treat for an additional harmful outcome (NNTH), and its 95% CI taking account of the event rate in the control group.
2. Continuous data
For continuous outcomes, we estimated standardised mean differences (SMD) between groups. As standardised measures of effect size, these are often more readily interpretable than mean differences (MDs) on the original scale, particularly when the scale is not universally well‐known (Cohen 1988; Gold 2004). However, we also transformed the effect size back to the units of one or more of the specific instruments to further aid interpretation and to ensure comparability across schizophrenia reviews.
Unit of analysis issues
1. Cluster trials
Studies may employ 'cluster randomisation' (such as randomisation by clinician or practice), but analysis and pooling of clustered data poses problems. Authors often fail to account for intra‐class correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) where P values are spuriously low, CIs unduly narrow and statistical significance overestimated causing type I errors (Bland 1997; Gulliford 1999).
Although no cluster trials were identified for this review, the planned procedure for analysis would have been as follows. Where clustering was not accounted for in primary studies, we would have presented the data in a table, with an (*) symbol to indicate the presence of a probable unit of analysis error. We would have attempted to contact the first authors of studies to seek intra‐class correlation coefficients (ICCs) of their clustered data and to adjust for this using accepted methods (Gulliford 1999). If the intra‐class correlation was not available, we would have used an external estimate from similar studies (Higgins 2008). If clustering had been incorporated into the analysis of primary studies, we would have presented these data as if from a non‐cluster randomised study, but adjusted for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a 'design effect'. This would have been calculated using the mean number of participants per cluster (m) and the (ICC) [Design effect=1+(m‐1)*ICC] (Donner 2002). If the ICC was not reported it would have been assumed to be 0.1 (Ukoumunne 1999).
If cluster studies had been appropriately analysed taking into account ICCs and relevant data documented in the report, synthesis with other studies would have been possible using the generic inverse variance technique.
2. Cross‐over trials
A major concern of cross‐over trials is the carry‐over effect. It occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence, on entry to the second phase the participants can differ systematically from their initial state despite a wash‐out phase. For the same reason cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in severe mental illness, had we included such trials, we would only have used data from the first phase of cross‐over studies.
3. Studies with multiple treatment groups
Where a study involved more than two treatment arms, if relevant, we presented the additional treatment arms in comparisons. If data were binary, we simply added and combined the data within the two‐by‐two table. If data were continuous, we combined data following the formula in section 7.7.3.8 (Combining groups) of the Cochrane Handbook for Systematic Reviews of Interventions. Where the additional treatment arms were not relevant, we did not reproduce these data.
Dealing with missing data
1. Overall loss of credibility
At some degree of loss of follow‐up, data must lose credibility (Xia 2009). We excluded data from studies where more than 30% of participants in any group were lost to follow‐up (this did not include the outcome of 'leaving the study early'). If, however, more than 30% of those in one arm of a study were lost, but the total loss was less than 30%, we marked such data with (*) to indicate that such a result may well be prone to bias.
2. Binary
In the case where attrition for a binary outcome was between 0% and 30% and where these data were not clearly described, we presented data on a 'once‐randomised‐always‐analyse' basis (an intention‐to‐treat analysis). In studies with less than 30% dropout rate, people leaving early were considered to have had the negative outcome for dichotomous outcomes, except for the event of death and adverse effects. For these outcomes, the rate of those who stayed in the study ‐ in that particular arm of the trial ‐ would have been used for those who did not. We analysed the impact of including studies with high attrition rates (20% to 30%) in a sensitivity analysis. If inclusion of data from this latter group did result in a substantive change in the estimate of effect, we did not add these data to trials with less attrition but presented them separately.
3. Continuous
3.1 Attrition
In the case where attrition for a continuous outcome was between 0% and 30% and completer‐only data were reported, we reproduced these.
3.2 Standard deviations
If SDs were not reported in the original studies, we tried to obtain the missing values from the authors. In cases where measures of variance for continuous data were missing, but an exact standard error (SE) and CIs were available for group means and either P or t values were available for differences in mean, we would have made calculations according to the rules described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011): When only the SE is reported, SDs are calculated by the formula SD = SE * square root (n).Chapters 7.7.3 and 16.1.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) present detailed formulae for estimating SDs from P values, t or F values, CIs, ranges or other statistics. If these formulae did not apply, we calculated or estimated the SDs according to a validated imputation method which is based on the SDs of the other included studies (Furukawa 2006). Although some of these imputation strategies can introduce error, the alternative would be to exclude a given study’s outcome and thus to lose information. We nevertheless would have examined the validity of the imputations in a sensitivity analysis excluding imputed values.
3.3 Last observation carried forward
We anticipated that in some studies the method of last observation carried forward (LOCF) would be employed within the study report. As with all methods of imputation to deal with missing data, LOCF introduces uncertainty about the reliability of the results (Leucht 2007). Therefore, where LOCF data had been used in the trial, if less than 30% of the data had been assumed, we would have reproduced these data and indicated that they were the product of LOCF assumptions.
Assessment of heterogeneity
1. Clinical heterogeneity
We considered all included studies initially, without seeing comparison data, to judge clinical heterogeneity. We simply inspected all studies for outlying people or situations which we had not predicted would arise. When such situations or participant groups arose, we discussed them fully.
2. Methodological heterogeneity
We considered all included studies initially, without seeing comparison data, to judge methodological heterogeneity. We simply inspected all studies for clearly outlying methods which we had not predicted would arise. When such methodological outliers arose, we discussed them fully.
3. Statistical heterogeneity
3.1. Visual inspection
We visually inspected graphs to investigate the possibility of statistical heterogeneity.
3.2 Employing the I2 statistic
We supplemented the visual inspection primarily by employing the I2 statistic alongside the Chi2 P value. This provides an estimate of the percentage of inconsistency thought to be due to chance (Higgins 2003). The importance of the observed value of I2 depends on i. magnitude and direction of effects and ii. strength of evidence for heterogeneity (e.g. a P value from Chi2 test, or a CI for I2). We interpreted an I2 estimate greater than or equal to around 50% accompanied by a statistically significant Chi2 statistic as evidence of substantial levels of heterogeneity (Higgins 2011). When substantial levels of heterogeneity were found in the primary outcome, we explored reasons for heterogeneity (Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
We entered data from all included studies into a funnel graph (trial effect against trial size) in an attempt to investigate the likelihood of overt publication bias (Davey Smith 1997). Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). These are described in Section 10 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We are aware that funnel plots may be useful in investigating reporting biases but are of limited power to detect small‐study effects. We did not use funnel plots for outcomes where there were 10 or fewer studies, or where all studies were of similar sizes. In other cases, where funnel plots were possible, we would have sought statistical advice in their interpretation.
Data synthesis
We understand that there is no closed argument for preference for use of fixed‐effect or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This often seems to be true to us and the random‐effects model takes into account differences between studies, even if there is no statistically significant heterogeneity. There is, however, a disadvantage to the random‐effects model. It puts added weight onto small studies which often are the most biased ones. Depending on the direction of effect, these studies can either inflate or deflate the effect size. We chose fixed‐effect model for all analyses.
Subgroup analysis and investigation of heterogeneity
1. Subgroups
We anticipated no subgroup analyses.
2. Investigation of heterogeneity
If we found heterogeneity (see under Assessment of heterogeneity), we examined the following possible sources of heterogeneity:
treatment dosage (20 sessions or more versus less than 20 sessions); and
treatment approach (quality of music therapy method and training).
Sensitivity analysis
We planned to investigate the effect of including studies with high attrition rates on the primary outcomes, but no such studies were identified in this review. We did however compare the results when we included our assumptions regarding those lost to follow‐up (see Dealing with missing data) with 'completer only' analyses.
Results
Description of studies
Results of the search
The search for the first published version identified 34 potentially relevant studies (Gold 2005a). Updated searches for the version published in 2011 yielded 115 additional records (from 99 studies) for a total of 149 records (Mössler 2011b). The search for the current update yielded 31 new records for a total of 176 records. After excluding duplicates and clearly irrelevant references, a total of 115 studies (31 new for the current update) were inspected closely for possible inclusion. Of these, we included a total of 18 studies (Characteristics of included studies) and excluded 97 studies (Characteristics of excluded studies); no ongoing studies were identified (Figure 1).
1.
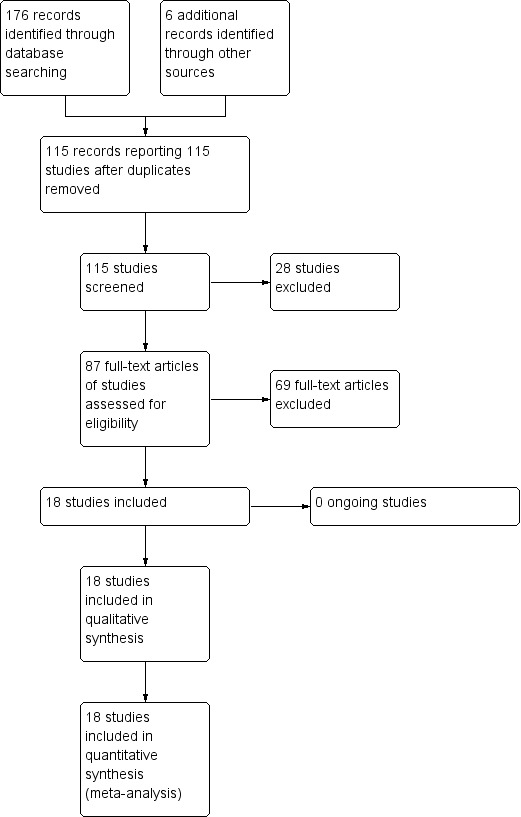
Study flow diagram (all searches)
Included studies
We included 18 studies (1215 participants) that compared music therapy added to standard care with standard care alone (Ceccato 2009; Cha 2012; Chang 2013; Fu 2013; Gold 2013; He 2005; Li 2007a; Liu 2013; Lu 2013; Mao 2013; Mohammadi 2012; Qu 2012; Talwar 2006; Tang 1994; Ulrich 2007; Wang 2013; Wen 2005; Yang 1998). The characteristics of these studies are described below (see also Additional tables 'Music therapeutic approach' and Characteristics of included studies).
1. Length of trials
The duration of studies varied from one to six months. Ten studies examined the short‐term effects of music therapy over about one to one‐and‐a‐half months (Cha 2012; Chang 2013; Fu 2013; He 2005; Li 2007a; Lu 2013; Mohammadi 2012; Tang 1994; Ulrich 2007; Wen 2005). Seven trials investigated medium‐term effects over three to four months (Ceccato 2009; Gold 2013; Liu 2013; Qu 2012; Talwar 2006; Wang 2013; Yang 1998). Two studies (Gold 2013; Mao 2013) examined the long‐term effects of music therapy over six to nine months.
2. Participants
All studies included adults with schizophrenia or related psychoses. The included studies differed somewhat with respect to diagnostic heterogeneity. Three studies included people with schizophrenia as well as people with related psychoses (Gold 2013; Talwar 2006; Ulrich 2007). The other 15 trials were more restrictive, allowing only people with schizophrenia (Ceccato 2009; Cha 2012; Chang 2013; Fu 2013; Li 2007a; Lu 2013; Mao 2013; Mohammadi 2012; Qu 2012; Wen 2005), or only a certain subtype of schizophrenia (chronic: Liu 2013; Tang 1994; Wang 2013; Yang 1998; type II: He 2005). People with acute positive symptoms were also excluded by Ulrich 2007. Diagnosis was based on three different psychiatric classification systems primarily used in the Western world (International Classification of Diseases (ICD), Diagnostic and Statistical Manual of Mental Disorders (DSM)) and China (Chinese Classification of Mental Disorders (CCMD)). The CCMD is similar in categorisation and structure to the ICD and DSM in terms of most diagnostic items, though acknowledging cultural‐related differences (Lee 2001). ICD‐10 was used in Ceccato 2009, Fu 2013, Gold 2013, Talwar 2006, and Ulrich 2007; Tang 1994 referred to the DSM‐III‐R; Cha 2012, Lu 2013, and Mohammadi 2012 referred to the DSM‐IV. The CCMD‐2 was used in Yang 1998, and the current third version of the CCMD was used as classification system in Chang 2013, He 2005, Li 2007a, Liu 2013, Mao 2013, Qu 2012, Wang 2013, and Wen 2005.
History of the disorder was reported in nine of the studies (Chang 2013: mean 6.6 years; Fu 2013: mean 3.6 years; He 2005: around nine years; Liu 2013: mean 9.7 years; Lu 2013: mean 25.0 years; Mao 2013: mean 1.8 years; Qu 2012: range 2.2 to 5 years; Wang 2013: mean 13.6 years; Yang 1998: range two to 26 years).
One study targeted a broader population of mental healthcare clients (Gold 2013); low motivation was the main inclusion criterion. Although we did include the study in the review, we examined its results separately from the other studies that were specifically targeted at schizophrenia or related psychoses.
3. Setting
Sixteen studies concerned inpatients. Ceccato 2009 and Gold 2013, however, included both in‐ and outpatients.
4. Study size
Sample sizes (of participants meeting inclusion criteria for this review) ranged from 30 to 96.
5. Interventions
5.1 Setting
All studies compared music therapy added to standard care with standard care alone. The setting of music therapy was group therapy in most of the studies; two studies (Gold 2013; Talwar 2006) used an individual setting, while two others (Wang 2013; Yang 1998) used a combination of group and individual settings.
Music therapy varied according to the use of active and receptive methods, level of structure, focus of discussions and verbal reflection. In five studies, the content of music therapy included receptive working modalities (listening to music) (Ceccato 2009; Cha 2012; He 2005; Li 2007a; Wen 2005). Four trials included exclusively active music making (improvisation, singing) (Fu 2013; Qu 2012; Talwar 2006; Ulrich 2007), and the remaining nine made use of both active and receptive ingredients (Chang 2013; Gold 2013; Liu 2013; Lu 2013; Mao 2013; Mohammadi 2012; Tang 1994; Wang 2013; Yang 1998). For all trials, except for Ceccato 2009 and Mohammadi 2012, the musical experiences were described as being accompanied by a discussion or verbal reflection of therapy contents. The focus of discussions and level of structure varied between patients, depending on their ability level (explicitly mentioned in Ulrich 2007). There was variation in music therapy methods including process‐oriented approaches and more fixed‐session structures, but overall, all were within the accepted range. There was more worrisome variation in music therapy training (Table 2; see also below: Other potential sources of bias).
1. Music therapeutic approach: Further characteristics of included studies.
| No. of sessions (offered/ received) | Adequate method | Adequate training | Modality (active/ receptive/ both) | Form of therapy | Therapy process (fixed structure/ process‐ oriented) | ||||||
| Improvisation | Playing and/or singing pre‐ composed music | Songwriting | Listening to music | Verbal discussion/reflection of therapy process | Others | ||||||
| Ceccato 2009 | Max. 16 (1/week over 4 months) | Yes | Yes | Receptive | No | No | No | Central | No | No | Fixed structure |
| Cha 2012 | Max. 12 (3/week over 4 weeks) | Yes | Unclear | Receptive | No | No | No | Yes | Yes | Music memory; Music imagery |
Process‐oriented |
| Chang 2013 | Max. 40 (5/week over 8 weeks) | Yes | Yes | Both | No | Yes | Yes | Yes | Yes | Music memory; improvisation; Musical psychodrama |
Fixed structure |
| Fu 2013 | Max. 12 (3/week over 4 weeks) | Yes | Unclear | Active | Yes | Yes | No | No | Yes | No | Fixed structure |
| Gold 2013 | 18 sessions received | Yes | Yes | Both | Yes | Yes | Yes | Yes | Yes | No | Process‐oriented |
| He 2005 | Max. 30 (5/week over 6 weeks) | Yes | Unclear | Receptive | No | No | No | Central | Yes | Dancing, reading poems with music background | Unclear |
| Li 2007a | Max. 30 (5/week over 6 weeks) | Yes | Unclear | Receptive | No | No | No | Central | Yes | No | Unclear |
| Liu 2013 | Max. 32 (2/week over 16 weeks) | Yes | Limited | Both | No | Yes | No | Yes | Yes | Recreative music therapy, Orff music therapy | Unclear |
| Lu 2013 | Max. 10 (2/week over 5 weeks) | Yes | Yes | Both | No | Yes | No | Yes | Yes | Playing percussion instruments, watching music videos | Unclear |
| Mao 2013 | Max. 240 (2/day, 5 days/week, over 6 months) | Unclear | Limited | Both | No | Yes | No | Yes | Yes | Music theory class, instrument playing, music appreciation | Unclear |
| Mohammadi 2012 | Max. 5 (weekly sessions/one month) | Yes | Unclear | Both | Yes | Yes | No | Yes | No | Making bodily movements according to the rhythm of the music | Unclear |
| Qu 2012 | Max. 224 (2/day, over 16 weeks) | Unclear | Limited | Both | No | Yes | No | Yes | Yes | Music appreciation | Unclear |
| Talwar 2006 | Max. 12 sessions (1/week over 3 months) | Yes | Yes | Active | Central | Yes | No | No | Central | No | Process‐ oriented |
| Tang 1994 | 19 sessions received | Yes | Unclear | Both | Yes | Yes | No | Central | Yes | No | Fixed structure |
| Ulrich 2007 | 7.5 sessions received | Yes | Yes | Active | Yes | Yes | No | No | Yes | No | Process‐ oriented |
| Wang 2013 | Max. 36 (3/week, over 3 months) | Unclear | Limited | Both | Yes | Yes | No | Yes | Yes | Musical appreciation, rhythm training | Unclear |
| Wen 2005 | Max. 30 (5/week over 6 weeks) | Yes | Unclear | Receptive | No | No | No | Central | Yes | Dancing | Unclear |
| Yang 1998 | Max. 78 (6/week over 3 months) | Yes | Yes | Both | Yes | Yes | No | Yes | Yes | Learning musicology | Unclear |
Adequate music therapeutic method: A "yes" indicates that the method applied considered both musical experiences and relational aspects as dynamic forces of change in music therapy. A "no" indicates that relational aspects are missing. Adequate music therapy training: A "yes" indicates that the persons conducting the music therapy have attended an appropriate music therapy training. A "no" indicates that the person conducting the music therapy had limited or even no music therapy training.
The number of sessions per week varied greatly from one (Talwar 2006) to six (Yang 1998). Where not explicitly stated, we calculated the maximum possible number of sessions received by patients from session frequency and treatment duration. The overall number of sessions offered was below 20 in seven studies which according to the a priori criteria for this review can be classified as low dosage of music therapy; in 10 studies, 20 or more studies were offered, corresponding to a high dosage; for three of these, numbers of sessions offered were much higher than in other studies (a total of 78 in Yang 1998, up to 160 in Qu 2012, and up to 240 in Mao 2013). The actual number of sessions received, however, could have been less: Talwar 2006 reported that only 58% of all participants received more than eight sessions. In one study (Cha 2012), the number of sessions offered was not reported.
There was also considerable variation in the total duration of therapy (from one to six months). Ten of the studies can be classified as short‐term music therapy (up to 12 weeks) (Cha 2012; Chang 2013; Fu 2013; He 2005; Li 2007a; Lu 2013; Mohammadi 2012; Tang 1994; Ulrich 2007; Wen 2005), seven studies as medium‐term music therapy (13 to 26 weeks) (Ceccato 2009; Gold 2013; Liu 2013; Qu 2012; Talwar 2006; Wang 2013; Yang 1998), and one (Mao 2013) as long‐term music therapy (six months).
6. Outcomes
This section describes the outcomes used in the included studies, categorised according to the list of relevant outcomes in the Methods section.
6.1 Global state
Global overall improvement, as judged by independent assessors, was rated as clinically important improvement versus no such improvement (Gold 2013; Yang 1998).
6.2 Mental state
6.2.1 General mental state
a. Positive and Negative Symptoms Scale ‐ PANSS (Kay 1987) The PANSS scale was designed to address the severity of psychopathology in patients with psychotic disorders. It consists of 30 items which belong to three subscales: positive symptoms, negative symptoms, and general psychopathology. Ratings are based on a clinical interview and additional information from caregivers or family members and clinical material. Each item is scored on a seven‐point Likert scale.
b. Brief Psychiatric Rating Scale ‐ BPRS (Overall 1988) The BPRS scale is a clinician‐rated tool designed to address severity of psychopathology in patients with psychotic disorders as well as those with severe mood disorders. The 18 items of the scale include common psychotic symptoms as well as mood disturbances. The scale is administered by an experienced clinician based on a clinical interview and observation of the patient. The items are scored on a seven‐point Likert scale.
6.2.2 Negative symptoms
Scale for the Assessment of Negative Symptoms ‐ SANS (Andreasen 1982) The SANS is a clinician‐rated instrument used to rate the presence and severity of negative symptoms, including affective flattening and blunting, alogia, avolition‐apathy, anhedonia‐associality, and attentional impairment. It consists of 20 items which are rated by trained raters using a clinical interview and additional collateral information from clinical material and family or caregivers. The items are scored using a six‐point Likert scale.
6.2.3 Positive symptoms
a. Scale for the Assessment of Positive Symptoms ‐ SAPS (Andreasen 1984)
The SAPS is a scale used to rate the presence and severity of positive symptoms, including hallucinations, delusions, bizarre behavior, and positive formal thought disorder. It consists of 30 items, which like in the SANS are rated by trained raters using a six‐point Likert scale.
6.2.4 Other specific aspects of mental state ‐ Depression
a. Self‐Rating Depression Scale ‐ SDS (Zhang 2003) The SDS scale is a self‐report instrument designed to measure levels of depression. It consists of 20 items each of which is scored on a four‐point Likert scale.
b. Hamilton Depression Scale ‐ Ham‐D (Hamilton 1960; Hamilton 2000) The Ham‐D scale is a questionnaire for clinicians designed to assess the severity of a patient's major depression.
c. Calgary Depression Scale for Schizophrenia ‐ CDSS (Addington 1992).
The CDSS is a scale to assess the severity of depression separate from positive, negative and extrapyramidal symptoms in people with schizophrenia. It is a semi‐structured interview consisting of nine items; ratings of the items are defined according to operational criteria from zero to three.
6.2.5 Other specific aspects of mental state ‐ Anxiety
Self‐Rating Anxiety Scale ‐ SAS (Zhang 2003) The SAS scale is a self‐report instrument designed to measure anxiety‐associated symptoms. It consists of 20 items each of which is scored on a four‐point Likert scale.
6.3 Leaving the study early
This outcome was available in all studies, but events occurred only in three studies (Gold 2013; Talwar 2006; Yang 1998).
6.4 Functioning
6.4.1 General functioning
a. Global Assessment of Functioning ‐ GAF (Spitzer 2000) The GAF scale is a clinician‐rated scale to rate global functioning on a continuum of mental health to mental disorder. It consists of a single item ranging from one to 100 with anchor points. It is usually rated on the basis of a clinical interview.
b. Lawton Instrumental Activities of Daily Living Scale ‐ IADL (Lawton 1969) The IADL is an instrument to assess independent living skills. It measures how a person is functioning at the present time in eight domains of function. In Mao 2013, a modified scoring procedure with four levels (one = independent to four = unable) was used where lower scores indicate better ability (personal communication, 25 July 2016).
6.4.2 Social functioning
Social Disability Screening Schedule ‐ SDSS (Wu 1998) The SDSS (in Yang 1998 referred to as Social Disability Schedule for Inpatients ‐ SDSI) is a psychiatrist‐rated scale used to rate levels of social functioning on the basis of a semi‐structured clinical interview. As only scores of subscales were reported in Fu 2013, we added up these subscale scores to a sum score, and imputed standard deviation (SDs) from subscale SDs.
6.4.3 Cognitive functioning
a. Paced Auditory Serial Addition Task ‐ PASAT (Gronwall 1977; Tombaugh 2006) The PASAT scale is a computerised serial‐addition task used to assess rate of information, processing, sustained attention, and working memory. Responses are recorded by a blinded assessor.
b. Conners Continuous Performance Task ‐ CCPT (Rosvold 1956) The CCPT is a computerised neurophysiological test assessing attention disorders and neurological functioning. Response patterns indicate, for example, inattentiveness or impulsivity, activation and arousal problems, or difficulties in maintaining vigilance.
c. Wechsler Memory Scale ‐ WMS (Saggino 1983) The WMS is a neurophysiological test assessing various memory functions including five index scores: auditory memory, visual memory, visual working memory, immediate memory, and delayed memory.
d. Clinical Memory Test ‐ CMT (Xu 1986) The CMT is a test developed for the assessment of memory. It consists of five subtests including directed memory, paired‐association learning, free recall of pictures, recognition of meaningless figures, and recall of connection between portraits and their characteristics.
e. Berg's Card Sorting Test ‐ BCST (Berg 1948; Nelson 1976) The BCST is a neurophysiological test assessing executive functions of the brain responsible for, among others, planning, cognitive flexibility, abstract thinking, or initiating appropriate actions and inhibiting inappropriate actions.
f. Wisconsin Card Sorting Test ‐ WCST (Heaton 1993) The WCST is a standard test measuring executive function. The domain "correctly completed categories" (WCST‐Cc) is a score that reflects an individual's overall level of executive functioning and the ability to utilise new information and previous experiences.
6.5 Behaviour
Nurses' Observation Scale for Inpatient Evaluation ‐ NOSIE (Honigfeld 1965) The NOSIE scale is an assessment instrument for nurses designed to assess behaviour of patients on an inpatient unit. It consists of 30 items measuring various aspects of positive behaviour (social competence, personal neatness) and negative behaviour (e.g. irritability, manifest psychosis, depression, retardation). Items are scored on a five‐point Likert scale. Scoring was reversed in one study (Li 2007a).
6.6 Patient satisfaction
Client Satisfaction Questionnaire ‐ CSQ (Atkinson 1994) The CSQ is a self‐report instrument designed to measure patients' satisfaction with care. It consists of eight items which are scored on a four‐point Likert scale.
6.7 Quality of life
6.7.1 General quality of life
a. General Well‐Being Schedule ‐ GWB (Fazio 1977) The GWB is a self‐administered questionnaire focusing on an individual's subjective feelings of well‐being and distress. The scale covers the dimensions of anxiety, depression, general health, positive well‐being, self‐control and vitality.
6.7.2 Specific aspects of quality of life
b. Skalen zur psychischen Gesundheit ‐ SPG (Tönnies 1996) The SPG scale is a self‐report instrument designed to address mental health‐related quality of life. It consists of 76 items each of which is scored on a four‐point Likert scale.
c. Social Support Questionnaire ‐ SSQ (Sarason 1983) The SSQ is a 27‐item questionnaire designed to measure perceptions of social support and satisfaction with that social support. Each item is a question that solicits a two‐part answer: Part 1 asks participants to list all the people that fit the description of the question, and Part 2 asks participants to indicate how satisfied they are, in general, with these people, on a six‐point Likert scale.
6.8 Missing outcomes
In addition to symptom and functioning scales, mainly represented here, it will be important to include more "positive" outcomes such as further quality of life measures, outcomes related with engagement with services as well as music‐related outcomes in future studies. Such outcomes might play an important role from a client perspective. Furthermore, studies focusing on cost‐effectiveness will be a next step when investigating music therapy.
Excluded studies
A total of 97 studies were excluded for the following reasons:
We excluded 38 studies because they were not randomised (14 CCTs, 20 case series, four single‐case studies).
We excluded a further 43 studies because the intervention was not music therapy. Twenty‐one of these investigated another type of therapy, e.g. art therapy, movement therapy, psychotherapy, a treatment package, or medication. Twenty‐two studies investigated the effects of music interventions that did not meet the definition of music therapy (e.g. music listening alone or Karaoke singing).
The remaining 16 studies were excluded for various reasons: We excluded one study because information needed could not be retrieved from the authors. Three studies compared music therapy with another type of therapy and we therefore excluded them. Four studies were excluded because only some of the participants were diagnosed with schizophrenia or related psychoses. Finally, no adequate outcome data were reported for eight studies (see Characteristics of excluded studies).
Awaiting assessment
There are no studies awaiting assessment.
Ongoing
We did not identify any ongoing studies.
Risk of bias in included studies
Overall, most information is from studies at low or unclear risk of bias. A summary of the risk of bias across domains, as described below, and for each included study is provided in Figure 2 and Figure 3.
2.
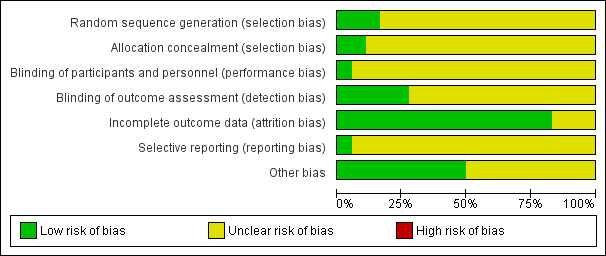
3.
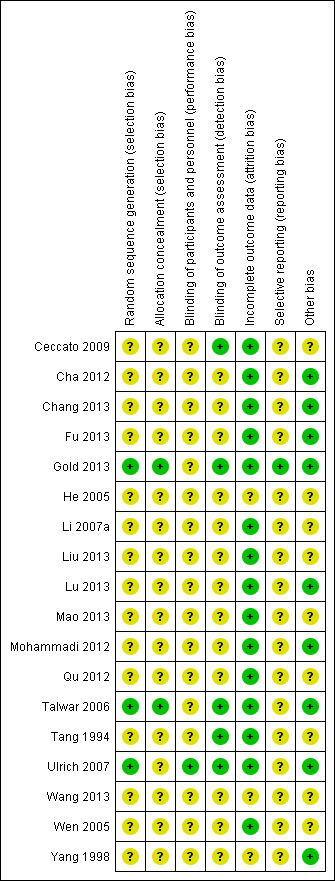
Allocation
While all studies stated that participants were randomly assigned, only 2 of them described concealment procedures. Talwar 2006 described that randomisation was concealed through a remote randomisation using a central telephone. Similarly, Gold 2013 conducted remote randomisation. An independent person who had no contact with the involved clinicians and participants provided individual allocations by e‐mail or text message. In the other studies it was unclear whether randomisation was really concealed.
Blinding
Five studies were explicitly single‐blind, using blinded assessment (Ceccato 2009; Gold 2013; Talwar 2006; Tang 1994; Ulrich 2007). For the other 13 studies it was unclear whether the persons conducting the assessments were blinded to treatment provision (Cha 2012; Chang 2013; Fu 2013; He 2005; Li 2007a; Liu 2013; Lu 2013; Mao 2013; Mohammadi 2012; Qu 2012; Wang 2013; Wen 2005; Yang 1998). Three studies tested the success of blinding. Gold 2013 verified the success of blinding and found that only in 8% of all cases assessors became aware of the participant's correct allocation. Ulrich 2007 tested whether assessors were aware of the study aim and found that they were not aware that the aim of the study had to do with music therapy. Talwar 2006 asked assessors to guess which group the participants were assigned to and identified that they guessed correctly in more than 50% of the cases. However, as this would always be the case when an experimental treatment is effective, this cannot be taken as an indication of unsuccessful blinding (Higgins 2008).
No study had a double‐blind design as the nature of the intervention does not allow to blind those who received music therapy or those who delivered it. However, in Ulrich 2007, participants were blinded to the fact that the study aim was the investigation of music therapy.
Incomplete outcome data
The majority of studies had low or zero attrition rates (Analysis 1.10). All analyses were conducted on an intention‐to‐treat basis. Gold 2013, Lu 2013, and Ulrich 2007 reported rates of missing data, i.e. participants who were followed up but where outcome data were incomplete. In Gold 2013, rates of missing data at the various outcome time points varied from 13% to 31%. Only 9% of the participants were lost for all time points of outcome assessment. The potential impact of missing data was assessed in two sensitivity analysis. For unobserved outcomes, either no change from the last observed value or no change from the baseline value was assumed. No changes in the effect were found. In Lu 2013, 6% of the participants were lost for all time points of outcome assessment. Also in this study a last observation carried forward (LOCF) procedure was applied for 3% of the missing cases. In Ulrich 2007, rates of missing data varied from 8% to 19% for the different outcome variables. All other studies had complete data for all cases that were followed up. For He 2005, the attrition rate was not reported. According to the setting (only inpatients) and apparent reporting standards in the Chinese trials (people leaving early were usually reported if there were any), we assumed that all participants had completed the trial.
1.10. Analysis.
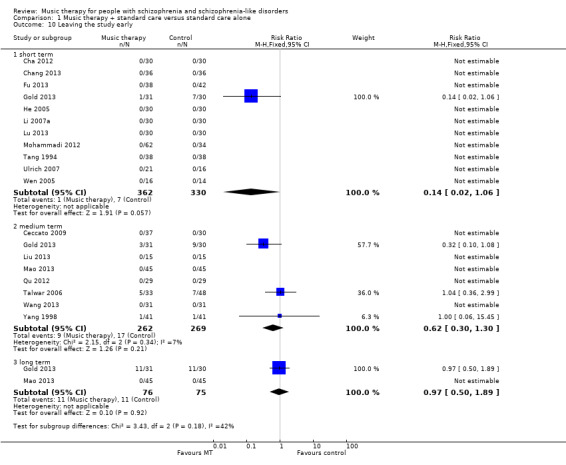
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 10 Leaving the study early.
Selective reporting
A published study protocol was only available for Gold 2013. In all the other studies, all outcomes that were described in the method section were also used for analyses. All studies reported means and SDs of both groups before and after treatment. We performed log transformation to remove skewness when this was present (as was the case with one outcome ‐ negative symptoms ‐ in Ulrich 2007). We considered all outcomes for all studies in the analyses.
Other potential sources of bias
1. Co‐intervention (treatment contamination)
For all studies, medication was reported as standard care. Tang 1994 reported a higher drop of medication level in the music therapy group than in the control group, but no significant difference at follow‐up. The other studies reported no significant differences in medication level. Standard care available to all participants included other therapies and activities (e.g. supportive counselling, occupational therapy, social activities).
2. Adequate music therapy method and training
Results may be biased if the quality of music therapy (method or training level) does not match that required in clinical practice. The quality of the music therapy methods applied was rated as satisfactory in most studies, although it was unclear in three (Table 2). The level of music therapy training was more uneven' adequate training level was ascertained only in seven of the 18 studies (Table 2).
According to the given definition of music therapy, both musical experiences and relationships developing through them could be identified as working mechanisms within these studies, although the level of intensity of the client‐therapist relationship might have varied between them. For example, Ceccato 2009 used a highly structured approach but therapists were nevertheless also instructed to "pay attention to relational atmosphere". The most prevalent modalities used were listening to music (15 studies), playing or singing pre‐composed music (13 studies), and improvisation (seven studies), along with verbal discussion of the processes (16 studies; Table 2), reflecting typical clinical practice.
Whether music therapists were adequately trained was not always clear. Some studies (e.g. Ceccato 2009, Talwar 2006, Ulrich 2007), stated that music therapy was conducted by "qualified music therapists". Some referred to quality standards in music therapy (Ulrich 2007), or approved training courses (Talwar 2006). In other studies, the level of training was clarified through personal communication (Ceccato 2009;Yang 1998). In other studies, the level of training was limited or unclear. For example, music therapy was conducted by nurses and psychiatrists who had attended a minimal music therapy training course (Tang 1994); "musicians who were employed full‐time as music therapists" (He 2005); or nurses and psychiatrists whose level of training was unclear (Li 2007a; Wen 2005).
Effects of interventions
See: Table 1
All 18 included studies are included in meta‐analysis. Outcomes are presented in the order specified in the Methods section and according to their prespecified time frame (short, medium, or long term). All comparisons concerned music therapy in addition to standard care versus standard care alone. When heterogeneity was present, we attempted to explain this via the dosage (less than 20 versus 20 or more sessions) or the adequacy of the music therapy (well‐defined versus less well‐defined music therapy; see Table 2).
COMPARISON 1: MUSIC THERAPY plus standard care versus STANDARD CARE alone
1.1 Global state
1.1.1 No clinically important overall improvement (as rated by individual trials)
Global state (no clinically important overall improvement) was addressed as a dichotomous outcome in two randomised controlled trials (RCTs) (Gold 2013; Yang 1998). There was no significant short‐term effect (1 RCT, n = 61, risk ratio (RR) 0.82 95% confidence interval (CI) 0.55 to 1.24, Analysis 1.1). There was a significant medium‐term effect favouring music therapy, suggesting that clinically important overall improvement was more likely to occur than with standard care alone (2 RCTs, n = 133, RR 0.38 95% CI 0.24 to 0.59, NNTB 2 95% CI 2 to 4). Heterogeneity was high (P = 0.0003, I² = 90%) and might be explained by high attrition in Gold 2013 (10/30 > 30% in the control group; 13/61 > 20% overall), although alternative explanations might be differences in populations (the study with the smaller effect consisted of 'low‐motivation', or treatment‐refractory, patients) or dose of therapy (the study with the smaller effect had a much smaller dose of music therapy). Excluding the study with high attrition resulted in stronger effects in favour of music therapy and no heterogeneity. In a sensitivity analysis where only complete data were used, the effects were unchanged. In the long term, no usable data were available (Gold 2013 had 24/61 > 30% attrition overall).
1.1. Analysis.
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 1 Global state: No clinically important overall improvement (as rated by trialists).
1.2 Mental state
Mental state was measured using eight continuous scales. These included endpoint scores of general mental state (PANSS and BRPS) as well as specific endpoint scores for negative (SANS) and positive (SAPS) symptoms of schizophrenia, depression (SDS, Ham‐D, CDSS), and anxiety (SAS).
1.2.1 General
Average endpoint general mental state scores using PANSS (high score = poor) were used in three studies (Lu 2013; Mao 2013; Talwar 2006). These showed significant effects in the short, medium, and long term (short term: 1 RCT, n=75, standardised mean difference (SMD) ‐0.69 95% CI ‐1.16 to ‐0.23; medium term: 2 RCTs, n = 159, SMD ‐0.97 95% CI ‐1.31 to ‐0.63; long term: 1 RCT, n = 90, SMD ‐3.41 95% CI ‐4.07 to ‐2.76, Analysis 1.2). High heterogeneity at medium term might be explained by dosage (the study with the smaller effect had a much smaller dose of music therapy; Table 2). BPRS scores (high score = poor) were used in two studies (Wen 2005; Yang 1998). On this scale, the overall effects were significant in favour of music therapy at medium term (1 RCT, n = 70, SMD ‐1.25 95% CI ‐1.77 to ‐0.73), but not at short term (1 RCT, n = 30, SMD 0.27 95% CI ‐0.45 to 0.99) (Analysis 1.3). Across both scales and all time points, it was notable that effects increased over time.
1.2. Analysis.
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 2 Mental state: General ‐ 1a. Average endpoint score (PANSS, high score = poor).
1.3. Analysis.
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 3 Mental state: General ‐ 1b. Average endpoint score (BPRS, high score = poor).
1.2.2 Specific ‐ Negative symptoms
Average endpoint scores of negative symptoms (SANS, high score = poor) were available from seven studies (Gold 2013; He 2005; Mohammadi 2012; Qu 2012; Tang 1994; Ulrich 2007;Yang 1998). As described above, the data from Ulrich 2007 were log‐transformed to remove skew, and missing SDs for Qu 2012 were estimated from those of the other studies using this outcome. The overall short‐ and medium‐term effects were significant in favour of music therapy (short term: 5 RCTs, n = 319, SMD ‐0.50 95% CI ‐0.73 to ‐0.27; medium term: 3 RCTs, n = 177, SMD ‐0.55 95% CI ‐0.87 to ‐0.24). Substantial heterogeneity between studies (short term: P=0.02, I² = 67%; medium term: P = 0.0002, I² = 89%) was removed when excluding the study on treatment‐refractory patients (Gold 2013), and the effects at both time points remained significant. In the long term, no usable data were available (Gold 2013 had 22/61 > 30% attrition overall). The effect was similar at short and medium term (Analysis 1.4).
1.4. Analysis.
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 4 Mental state: Specific ‐ 2. Negative symptoms ‐ average endpoint score (SANS, high score = poor).
1.2.3 Specific ‐ Positive symptoms
Average endpoint scores of positive symptoms (SAPS, high score = poor) were available from one study (Mohammadi 2012). Effects at short term were not significant (1 RCT, n = 96, SMD ‐0.18 95% CI ‐0.60 to 0.24, Analysis 1.5 ).
1.5. Analysis.
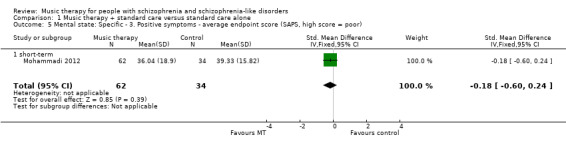
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 5 Mental state: Specific ‐ 3. Positive symptoms ‐ average endpoint score (SAPS, high score = poor).
1.2.4 Specific ‐ Depression, anxiety
Depression and anxiety were assessed in several studies using a variety of scales. Average endpoint scores of depression (SDS, high score = poor) were measured in two studies (Li 2007a; Wen 2005) and showed a significant short‐term effect in favour of music therapy (2 RCTs, n = 90, SMD ‐0.63 95% CI ‐1.06 to ‐0.21, Analysis 1.6). There was no heterogeneity between the studies (P = 0.73, I² = 0%). One of the same studies (Wen 2005), also used average endpoint depression scores using another scale (Ham‐D, high score = poor). The short‐term effect from this scale was of comparable size but did not become statistically significant from this small study alone (1 RCT, n = 30, SMD ‐0.52 95% CI ‐1.25 to 0.21, Analysis 1.7). Average endpoint depression scores on a third scale (CDSS, high score = poor) in a study of well‐defined music therapy (Lu 2013) were analysed but excluded from interpretation due to likely skewness (1 RCT, n = 75, Analysis 1.8).
1.6. Analysis.
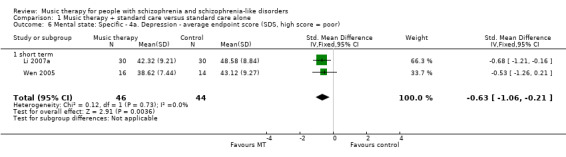
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 6 Mental state: Specific ‐ 4a. Depression ‐ average endpoint score (SDS, high score = poor).
1.7. Analysis.
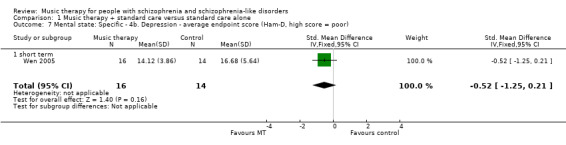
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 7 Mental state: Specific ‐ 4b. Depression ‐ average endpoint score (Ham‐D, high score = poor).
1.8. Analysis.
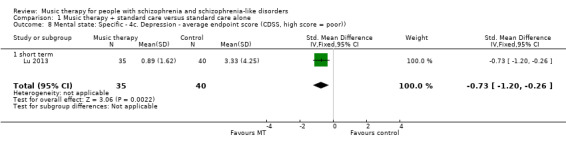
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 8 Mental state: Specific ‐ 4c. Depression ‐ average endpoint score (CDSS, high score = poor)).
Average endpoint scores of anxiety (SAS, high score = poor) were available from one study (Li 2007a), yielding a significant short‐term effect in favour of music therapy (1 RCT, n = 60, SMD ‐0.61 95% CI ‐1.13 to ‐0.09, Analysis 1.9).
1.9. Analysis.
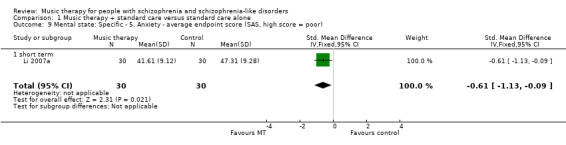
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 9 Mental state: Specific ‐ 5. Anxiety ‐ average endpoint score (SAS, high score = poor).
1.3. Leaving the study early
Data on leaving the study early were available for all 18 studies, but events occurred only in three (Gold 2013; Talwar 2006; Yang 1998). There were no significant differences on this outcome (short term: 11 RCTs, n = 692, RR 0.14 95% CI 0.02 to 1.06; medium term: 8 RCTs, n = 531, RR 0.62 95% CI 0.30 to 1.30; long term: 2 RCTs, n = 151, RR 0.97 95% CI 0.50 to 1.89, Analysis 1.10).
1.4. Functioning
1.4.1 General functioning
General functioning was measured in two studies of low‐dose music therapy (Gold 2013; Talwar 2006) using GAF scores (high score = good). No significant effects were found for the short term or medium term (short term: 1 RCT, n = 53, SMD 0.08 95% CI ‐0.47 to 0.62; medium term: 2 RCTs, n = 118, SMD ‐0.19 95% CI ‐0.56 to 0.18, Analysis 1.11 ). In the long term, no usable data were available (Gold 2013 had 22/61 > 30% attrition overall). One study of 'high‐dose' music therapy (Mao 2013) used IADL scores (high score = poor), with results showing significant effects favouring music therapy both in the medium term (1 RCT, n = 90, SMD ‐1.20 95% CI ‐1.65 to ‐0.75) and in the long term (1 RCT, n = 90, SMD ‐1.80 95% CI ‐2.29 to ‐1.30, Analysis 1.12).
1.11. Analysis.
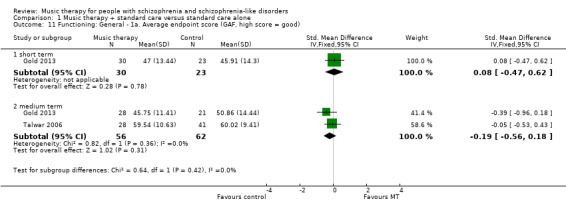
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 11 Functioning: General ‐ 1a. Average endpoint score (GAF, high score = good).
1.12. Analysis.
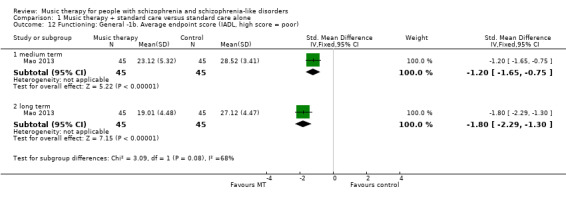
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 12 Functioning: General ‐1b. Average endpoint score (IADL, high score = poor).
1.4.2 Social functioning
Average endpoint scores of social functioning (SDSS, high score = poor) was used in three studies (Fu 2013; Mao 2013; Yang 1998). Significant effects favouring music therapy were found in the short term (1 RCT, n = 40, SMD ‐1.25 95% CI ‐1.94 to ‐0.57), medium term (2 RCTs, n = 160, SMD ‐0.72 95% CI ‐1.04 to ‐0.40), and long term (1 RCT, n = 90, SMD ‐0.56 95% CI ‐0.98 to ‐0.14, Analysis 1.13).
1.13. Analysis.
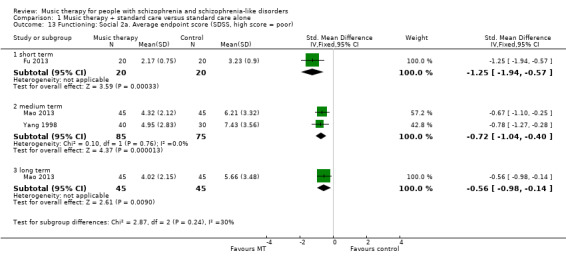
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 13 Functioning: Social 2a. Average endpoint score (SDSS, high score = poor).
No usable data were available for social functioning scores using IPROS. As this scale was only used in Qu 2012 and only scores of subscales were reported therein, we were not able to impute SDs for a total score from other studies and hence were not able to include this outcome measure in the analysis.
1.4.3 Cognitive functioning
Various aspects of cognitive functioning (attention/vigilance, memory, and abstract thinking) were addressed in three studies (Ceccato 2009; Cha 2012; Liu 2013).
Average endpoint scores of attention (PASAT, high score = good) showed a significant medium‐term effect favouring music therapy (1 RCT, n = 67, SMD 0.72 95% CI 0.22 to 1.21, P = 0.005, Analysis 1.14). However, CCPT scores measuring vigilance and attention (high score = good) in the same study, also at medium term, did not show a significant effect (1 RCT, n = 67, SMD 0.25 95% CI ‐0.23 to 0.74, Analysis 1.15).
1.14. Analysis.
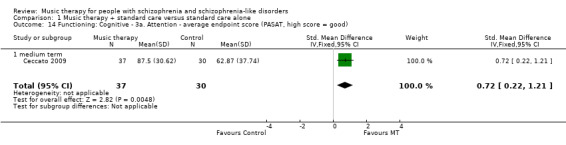
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 14 Functioning: Cognitive ‐ 3a. Attention ‐ average endpoint score (PASAT, high score = good).
1.15. Analysis.
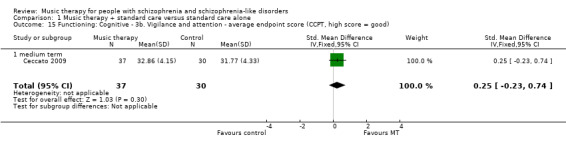
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 15 Functioning: Cognitive ‐ 3b. Vigilance and attention ‐ average endpoint score (CCPT, high score = good).
At medium term, average endpoint scores of memory (WMS, high score = good) were not significant (1 RCT, n = 67, SMD 0.43 95% CI ‐0.06 to 0.92, Analysis 1.16 ). Average endpoint scores of memory (CMT, high score = good) showed significant short‐term effects favouring music therapy (1 RCT, n = 60, SMD 0.58 95% CI 0.06 to 1.09, Analysis 1.17).
1.16. Analysis.
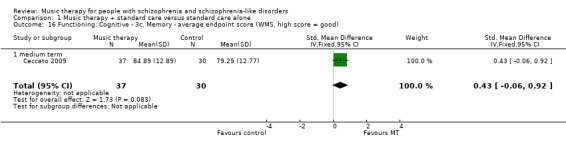
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 16 Functioning: Cognitive ‐ 3c. Memory ‐ average endpoint score (WMS, high score = good).
1.17. Analysis.
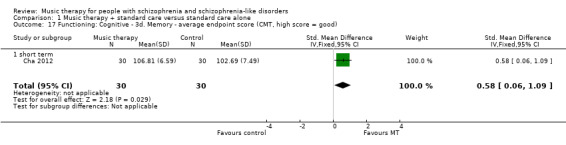
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 17 Functioning: Cognitive ‐ 3d. Memory ‐ average endpoint score (CMT, high score = good).
Average endpoint scores of abstract thinking (BCST, high score = good) were not significant at medium term (1 RCT, n = 67, SMD 0.09 95% CI ‐0.39 to 0.58, Analysis 1.18). Average endpoint scores of abstract thinking (WCST‐Cc, high score = good) showed no effects at short term (2 RCTs, n = 90, SMD ‐0.02 95% CI ‐0.07 to 0.03), but significant effects favouring music therapy at medium term (1 RCT, n = 30, SMD 1.18 95% CI 0.33 to 2.03, Analysis 1.19).
1.18. Analysis.
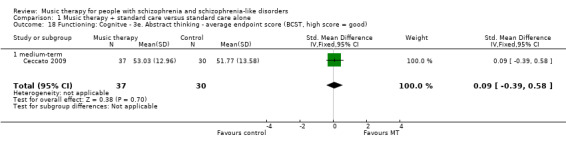
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 18 Functioning: Cognitve ‐ 3e. Abstract thinking ‐ average endpoint score (BCST, high score = good).
1.19. Analysis.
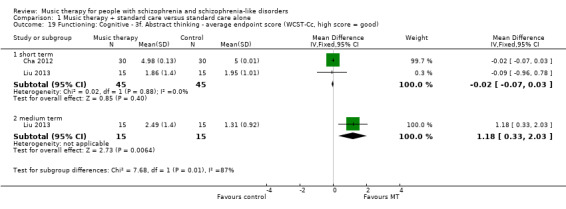
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 19 Functioning: Cognitive ‐ 3f. Abstract thinking ‐ average endpoint score (WCST‐Cc, high score = good).
1.5 Behaviour
Average endpoint scores of behaviour (NOSIE total score, high score = good; individual study data were reversed where necessary) were used in two studies, however data from both studies were not interpretable due to likely skewness (2 RCTs, n = 100, Analysis 1.20). Average change scores of behaviour of the same outcome (NOSIE total score, high score = good) were used in one 'high‐dose' study (Wang 2013), showing a significant medium‐term effect favouring music therapy (1 RCT, n = 62, SMD 0.69 95% CI 0.18 to 1.20, Analysis 1.21).
1.20. Analysis.
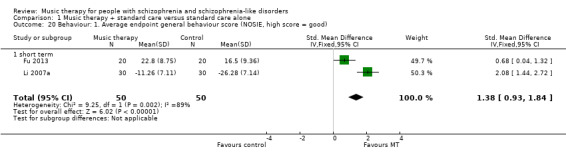
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 20 Behaviour: 1. Average endpoint general behaviour score (NOSIE, high score = good).
1.21. Analysis.
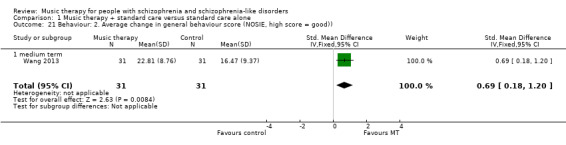
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 21 Behaviour: 2. Average change in general behaviour score (NOSIE, high score = good)).
1.6 Recipient of care satisfaction
Satisfaction with care was assessed using CSQ scores (high score = good) in one low‐dose study (12 sessions, Talwar 2006) of well‐defined music therapy. No significant effect was found (1 RCT, n = 69, SMD 0.32 95% CI ‐0.16 to 0.80, Analysis 1.22).
1.22. Analysis.
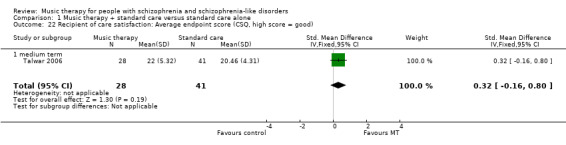
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 22 Recipient of care satisfaction: Average endpoint score (CSQ, high score = good).
1.7 Quality of life
1.7.1 General
In a 'high‐dose' study (Chang 2013), GWB scores (high score = good) showed a significant effect (1 RCT, n = 72, SMD 1.82 95% CI 1.27 to 2.38, Analysis 1.23).
1.23. Analysis.
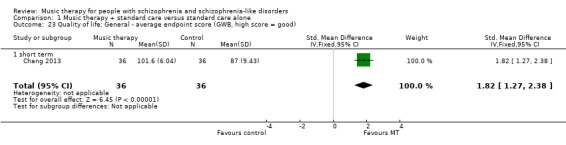
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 23 Quality of life: General ‐ average endpoint score (GWB, high score = good).
1.7.2 Specific
Average endpoint scores of mental health‐related quality of life were available from two short‐term studies. In one low‐dose study (Ulrich 2007), SPG scores (high score = good) did not show a significant effect (1 RCT, n = 31, SMD 0.05 95% CI ‐0.66 to 0.75, Analysis 1.24). Specific aspects of quality of life (social support; SSQ, high score = good) were assessed in a 'high‐dose' study (Chang 2013) and showed a significant effect favouring music therapy (1 RCT, n = 72, SMD 0.73 95% CI 0.26 to 1.21, Analysis 1.25).
1.24. Analysis.
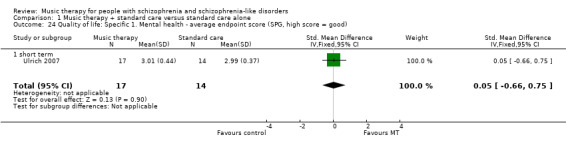
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 24 Quality of life: Specific 1. Mental health ‐ average endpoint score (SPG, high score = good).
1.25. Analysis.
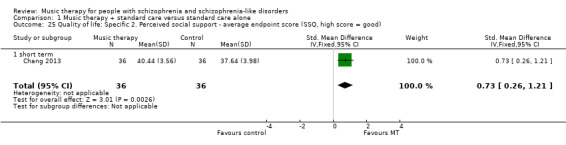
Comparison 1 Music therapy + standard care versus standard care alone, Outcome 25 Quality of life: Specific 2. Perceived social support ‐ average endpoint score (SSQ, high score = good).
Discussion
Summary of main results
COMPARISON 1: MUSIC THERAPY plus standard care versus STANDARD CARE alone
1. Global state
Although there are data from only two studies, these results suggest that music therapy has a strong effect on global state in the medium term (three to six months). The number needed to treat for an additional beneficial outcome is small (total n = 133, NNTB 2 95% CI 2 to 4). These results seem to be mediated by the number of sessions. This is an important result that should be replicated.
2. Mental state
Mental state was measured considering symptom scores of general mental state (PANSS, BPRS), negative symptoms (SANS), positive symptoms (SAPS), depression (SDS, Ham‐D) and anxiety (SAS). Significant results were found on five of the seven scales.
Effects tended to increase over time and were clearly seen in the medium term (three to six months). According to Cohen's guidelines (Cohen 1988), music therapy showed large effects (standardised mean difference (SMD) > 0.80) on general mental state (PANSS: total n = 159, SMD ‐0.97 95% confidence interval (CI) ‐1.31 to ‐0.63; BPRS: total n = 70, SMD ‐1.25 95% CI ‐1.77 to ‐0.73) and medium‐sized effects (SMD ≈ 0.50) on negative symptoms (SANS: total n = 177, SMD ‐0.55 95% CI ‐0.87 to ‐0.24).
Short‐term effects of medium size were seen for negative symptoms (total n = 319, SMD ‐0.50 95% CI ‐0.73 to ‐0.27). For other aspects of mental state (general mental state, positive symptoms, depression, and anxiety), interpretation was complicated by the use of different scales. Some scales were used only in a single small study. Differences between the results may also reflect differences in the number of sessions or differences in the quality of the music therapy applied (music therapy method and training).
Data on long‐term effects were available from one study and were strongly in favour of music therapy (total n = 90, SMD ‐3.41 95% CI ‐4.07 to ‐2.76). This is a very large effect size using general guidelines for the interpretation of intervention effects in the social sciences (Cohen 1988).
It clearly takes time for the effects of music therapy to unfold. This can be seen not only from the tendency of effects to increase over time, but also from examining the numbers of sessions provided in each of the studies. The strongest effects were found in studies that provided long‐term, high‐frequency music therapy (Table 2). This is in line with another review that specifically focused on the dose‐effect relation in music therapy (Gold 2009). Music as a medium of therapy addresses issues related to emotion and social interaction and is described as motivating. Therefore, it has been speculated earlier (e.g. Mössler 2011b) that it may be particularly well‐suited to the treatment of negative symptoms, which are related to problems in that area (affective flattening and bluntness, poor social interaction and a general lack of interest). However, the present review update suggests that effects on general mental state are at least as strong as those on negative symptoms.
In summary, large effects of music therapy were found for general symptoms and negative symptoms. The effect sizes for general symptoms in the medium and long term, corresponding to a 9‐ to 12‐point difference on the PANSS scale, were large by common standards (Cohen 1988). They were also much larger than those found in a recent systematic review of cognitive behaviour therapy (Jauhar 2015).
3. Leaving the study early
There were no differences concerning the outcome of leaving the study early. Both treatment conditions seemed to be well‐tolerated ‐ few people left either group.
4. Functioning
Functioning was measured in terms of three different aspects: general, social and cognitive functioning.
Effects on general functioning were significant and large for 'high‐dose' music therapy, both in the medium term (SMD ‐1.20 95% CI ‐1.65 to ‐0.75) and in the long term (SMD ‐1.80 95% CI ‐2.29 to ‐1.30). In contrast, low‐dose music therapy (less than 20 sessions) did not affect general functioning (short term: SMD 0.08 95% CI ‐0.47 to 0.62; medium term: SMD ‐0.19 95% CI ‐0.56 to 0.18).
Effects on social functioning were in favour of music therapy in the short, medium, and long term, with effect sizes ranging from medium to large. Results for cognitive functioning were mixed, with some scales suggesting benefit and others suggesting no effect.
Overall, it seems that music therapy can affect social functioning more quickly than general functioning. This appears plausible, given the focus of especially active music therapy on social interaction. General functioning may be harder to change. Effects of music therapy on general functioning require more sessions and more time, but can then be large (SMD > 0.80) using Cohen's guidelines (Cohen 1988). This is again in line with a previous systematic review that found increasing effects on functioning with dose of music therapy (Gold 2009).
5. Behaviour
Usable data on behaviour were limited, but suggested large effects of high‐dose music therapy in the medium term, similar to mental state and functioning.
6. Satisfaction with care
No effects on patient satisfaction with care could be identified. Data were to sparse to make any conclusions.
7. Quality of life
Quality of life (short to medium term) showed a similar pattern as other outcomes above, with high‐dose music therapy showing beneficial effects with large effect sizes, but low‐dose music therapy showing no such effects.
Overall completeness and applicability of evidence
1. Music therapy techniques
All studies used a combination of typical music therapeutic techniques: active music‐making (often improvisation, but also songs) and music listening. Verbal discussion and reflection emerging from, and connected to, the musical processes was described for all studies. The techniques of clinical music therapy were, therefore, relatively well represented.
2. Setting
In comparison to previous versions of this review, the time span of music therapy has expanded and now covers not only short‐term, but also medium‐term music therapy (from one up to six months). However, the majority of studies investigated music therapy in hospital settings, including primarily inpatients (in both acute and longer‐term wards) and some outpatients (in two studies). Therefore, direct applicability of the evidence is restricted to hospital settings. Clinical music therapy is commonly provided in such settings, but longer‐term individual and group music therapy with outpatients, also outside hospital settings, is also common. In terms of numbers of sessions, studies covered a broad range (from less than 10 to more than 200), which reflects the variety of clinical settings well. Interesting variations were found in the frequency of sessions: one to two sessions per week were common in Europe and Western Asia, whereas twice‐weekly to daily or even twice‐daily sessions were provided in East Asia. All studies were conducted in Europe, Asia or Australia.
3. Outcomes
The outcomes of included studies mainly reflect symptom and functioning scales assessing the patient's deficits. Recently, "positive" outcomes (such as quality of life, but also for example, music‐related outcomes) have been considered as well. However, there is not yet an agreement as to which outcome measures are to be preferred for those domains. This meant that we had to exclude some outcomes and even whole studies that may have been interesting (Gold 2013; Grocke 2014; Silverman 2009; Silverman 2014a; Silverman 2016). Agreement on outcomes that link more closely to processes and mechanisms of music therapy has not been reached. However, this appears to be a widespread and persistent problem in schizophrenia trials more generally (Miyar 2012).
Quality of the evidence
The included trials were of moderate quality, so at moderate risk of bias. All studies stated explicitly that randomisation was used, but concealment of allocation was unclear in most studies. There was no indication of unintended co‐intervention. In some studies (e.g. Talwar 2006), however, it was reported that some participants received less sessions than planned, which may have lowered the observed effects. Attrition rates were relatively low. All analyses were intention‐to‐treat. Blinding of assessment was reported in only a minority of studies. The adequacy of the music therapeutic approach is reflected satisfactorily by the applied music therapeutic techniques for most studies. However, the training level of music therapists was unclear in about half of the included studies. The clinical heterogeneity in music therapy may indicate the use of sensitivity analyses using random‐effects models; while this was not included in the protocol for the present version of this review, it will be considered in future updates.
Potential biases in the review process
The extensive search strategy that was undertaken for this review might make it seem likely that all relevant studies were identified. No restrictions concerning nationality or language have been made within the search process. Non‐English articles were included in the review and relevant articles were translated into English. Furthermore, dealing with data was done thoroughly and we contacted authors of relevant studies when data were insufficient.
There is, however, the possibility that our interest in this area (see Declarations of interest) or past knowledge of the literature (Gold 2005a) could have resulted in a biased view of the data. We think it would be hard to avoid some degree of similar risks of bias in the reviewing process.
Agreements and disagreements with other studies or reviews
The findings of this review are in agreement with a review of randomised and observational studies on music therapy for serious mental disorders (Gold 2009). That review confirmed and quantified the relationship between the number of sessions and the size of the effect of music therapy. Using meta‐regression, the review found that a large proportion of the variance in effects (73% to 78%) was explained by the number of sessions or its square root. A clear dose‐effect relationship strengthens the knowledge about the effects of music therapy (Higgins 2011), and might contribute to a better use of mental health resources. In contrast to that other review which drew on a broader basis and larger number of studies, meta‐regression was not considered appropriate for the present review due to the small number of studies included (Higgins 2011).
Authors' conclusions
Implications for practice.
1. For people with schizophrenia
There is evidence that music therapy, as an addition to standard care, can help people with schizophrenia improve their global state, mental state (general negative, depressive and anxiety symptoms), functioning (general and social), and quality of life over the short to medium term. Music therapy seems to address especially motivational, emotional and relational aspects, and helps patients improve regarding their social activities and roles. However, the effects of music therapy seem to depend on the number of music therapy sessions. To benefit from music therapy, it is important to participate in regular sessions over some time. The minimum number of sessions is difficult to determine and will probably vary from patient to patient.
2. For clinicians
Music therapy, as an addition to standard care, does seem to help across a wide range of measures ‐ at least over the short to medium term. Those positive effects might help support the motivation as well as emotional and relational competencies of people with schizophrenia. However, these effects seem to depend on the number of music therapy sessions provided, as well as on the quality of the therapy. The results of this review suggest that at least 20 sessions may be needed to reach clinically significant effects. This is consistent with the significant dose‐effect relationships found in Gold 2009. That review demonstrated that medium effects of music therapy on general and negative symptoms as well as functioning occur between 16 and 24 sessions. The specific techniques of music therapy, including among others adaptation of musical material to clients' needs, musical improvisation, and the discussion of personal topics emerging through the musical processes, require specialised music therapy training. Both training courses and qualified music therapists are available in many countries, but in some countries there may be a need to develop better quality training. Music therapy may be especially important for improving negative symptoms such as affective flattening and blunting, poor social relationships, and a general loss of interest and motivation. These domains may be specifically related to music therapy's strengths, but do not typically respond well to other treatment.
3. For managers/policy makers
There is a considerable amount of evidence to support music therapy for people with schizophrenia. We think that music therapy should be more widely available and that there is an evidence‐base to underpin this.
Implications for research.
1. General
Generally, there is room for improvement concerning the quality of reporting of trials in this area, and future research reports should make use of guidelines such as the CONSORT statement (Boutron 2008; Moher 2010). Replication studies are especially needed for outcomes where only one or two randomised controlled trials (RCTs) were available (e.g. global state).
2. Specific
2.1 Additional reviews
Out of necessity the search strategy for this review was broad. It revealed other music‐based interventions such as music listening that could be relevant to review. This type of music‐based intervention does not qualify as music therapy, but might play an important role in particular settings or cultures. Further reviews might also address music therapy compared with other psychosocial interventions (see Table 3).
2. Reviews suggested by excluded studies.
| Intervention | Comparison | For people with | Relevant excluded study | Relevant existing Cochrane Reviews |
| Music medicine (music listening alone, without a music therapist) | Standard care | Schizophrenia | Chambliss 1996; Glicksohn 2000; Haimov 2012; Kong 2007; Li 2011; Lin 2003; Margo 1981; Muller 2014; Ni 2002; Vadas 2012; Wang 2002a; Wang 2002b; Zhang 2010; Zhang 2013; Zhou 2003; Zhou 2006; Zhu 2002 | ‐‐ |
| Other music interventions | Hannes 1974; Hu 2004; Leung 1998; Li 2005; Tang 2002; Wang 2006a; Wang 2007; Zhang 2003a; Zhang 2005; Zincir 2011 | ‐‐ | ||
| Other creative arts therapies (art therapy, dance/movement therapy) | Standard care or other therapy | Apter 1978; Green 1987; Krajewski 1993; Su 1999 | Ren 2013; Ruddy 2005; Ruddy 2007 | |
| Treatment packages including music interventions | Barrowclough 2001; Gaszner 2009; Ji 2013; Su 2005; Tan 2009; Xiao 2005; Yang 2005 | ‐‐ | ||
| Music therapy | Other interventions | Valencia 2006; Zhang 2003b | ‐‐ | |
| Olanzapine | Placebo | Arango 2003 | Duggan 2005 | |
| Ondansetron | Placebo | Adler 2005 | ‐‐ | |
| Cognitive behaviour therapy/behaviour therapy | Standard care or other therapy | Bechdolf 2005; Drury 1996; Krajewski 1993 | Jones 2012 | |
| Family therapy | Standard care | Hogarty 1988 | Pharoah 2010; Okpokoro 2014 | |
| Music therapy | Standard care or other therapy | People in mental health care | Silverman 2011a; Silverman 2011b; Silverman 2011c | ‐‐ |
2.2 Trials
Specific areas where research is particularly needed are long‐term effects, dose‐effect relationship, and music therapy outside hospital settings. Furthermore, pragmatic trials assessing music therapy in routine use, within a changing context of mental health care, would be valuable. A suggestion for such a trial is shown in Table 4.
3. Suggestions for design of future studies.
| Methods | Allocation: randomised (could be cluster‐randomised), with sequence generation and concealment of allocation clearly described. Blindness: assessor‐blinded, success of blinding tested. Duration: at least 12 months from randomisation. |
| Participants | People with schizophrenia.* Age: any. Sex: both. History: any. N = 300 (more if cluster‐randomised).** |
| Interventions | 1. Music therapy delivered by qualified music therapist. N = 150. 2. Standard care (stratified by medication status). N = 150. |
| Outcomes | General state: relapse. Service outcomes: length of hospitalisation, number of hospital admissions. Time in work/vocational activity. General functioning (e.g. using GAF). Mental state (e.g. using PANSS). Well‐being. Quality of life (e.g. using EuroQol EQ‐5D). Adverse events: any. Compliance with/use of services offered. Economic evaluations: cost‐effectiveness, cost‐benefit. Qualitative data: interviews with service users about their experience with the treatment package. |
| Notes | * This could be diagnosed by clinical decision. If funds were permitting all participants could be screened using operational criteria, otherwise a random sample should suffice.** Size of study with sufficient power to highlight about a 10% difference between groups for primary outcome (depending on baseline risk).. *** Primary outcome. The same applies to the measure of primary outcome as for diagnosis. Not everyone may need to have operational criteria applied if clinical impression is proved to be accurate. |
GAF ‐ General Assessment of Function PANSS ‐ Positive and Negative Syndrome Scale
2.2.1 Dosage
Even though significant dose‐response relationships could be demonstrated in another review (Gold 2009), studies randomising high versus low dosage of music therapy (i.e. high versus low numbers of therapy sessions) would be required to quantify and confirm the knowledge that has been gained so far. Such studies would require considerably larger sample sizes than those represented in this study because the expected effect sizes between two active treatments will be smaller than between music therapy as an add‐on treatment and standard care alone.
2.2.2 Duration
Long‐term effects extending over more than six months have received limited attention in previous trials, and research on long‐term effects are especially necessary as schizophrenia is often a chronic condition. This may include trials of long‐term music therapy as well as long‐term follow‐up assessments of short‐ or medium‐term music therapy.
2.2.3 Core outcomes
There are currently no agreed core outcome sets for schizophrenia interventions in general (www.comet‐initiative.org) or for music therapy specifically. More co‐ordinated research is needed to identify what outcomes matter most to patients and other stakeholders. In this review, most outcomes were based on scales (such as BRPS, PANSS, SANS), which were developed primarily for research rather than clinical purposes. Although some scales (e.g. GAF) are also commonly used in clinical practice, it may be argued that the most important real‐world outcomes (such as being able to work, living independently, not being readmitted to hospital, maintaining positive relationships with significant others) are not based on scales. It may also be argued ‐ and, as we understand, has been the Cochrane Schizophrenia Group's view for a long time ‐ that the most meaningful outcomes are binary rather than continuous. In contrast to this view, recent understanding of schizophrenia as a spectrum disorder (APA 2013) also lends support to a notion where the condition as well as its outcomes can be described as continuous. There are also statistical considerations linked to choosing continuous versus binary data; analysing means, as we did for most outcomes, retains a maximum of information and therefore maximum power, but depends on a number of assumptions (as described in Methods, 2.1 Scale‐derived data). Conversely, analysing binary cut‐off values is more robust, but has less power, and necessitates a choice of cut‐off. Studies often vary in their definition of a clinically meaningful cut‐off. In conclusion, instead of further diversification of outcome measures, scales, and cut‐offs used in studies, efforts should be directed at identifying a small set of meaningful and important core outcomes, ideally in a broad consensus involving researchers, patients and other stakeholders.
What's new
| Date | Event | Description |
|---|---|---|
| 20 March 2017 | New citation required but conclusions have not changed | New data available but overall conclusions of the review remain unchanged. |
| 25 October 2016 | New search has been performed | Results of 2015 search incorporated into review. Ten new trials added to included studies table (including one previously listed as ongoing); 23 added to excluded studies table (including one previously listed as ongoing). Conclusions are unchanged. |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 2, 2005
| Date | Event | Description |
|---|---|---|
| 15 January 2015 | Amended | Search updated and 31 studies were added to 'Studies awaiting classification' section of the review. |
| 12 December 2012 | Amended | Contact details updated. |
| 31 January 2011 | New search has been performed | Updated searches resulted in four new included studies. |
| 31 January 2011 | New citation required and conclusions have changed | Conclusions changed after new data entered. |
| 24 April 2008 | Amended | Converted to new review format. |
| 24 January 2005 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The authors would like to acknowledge the help of the following people in the development of this review: Kris Bentley helped as co‐author of the original protocol (Gold 2003); Trond Dahle as co‐author of the first full review (Gold 2005a); Tony Wigram (deceased) helped with both versions (Gold 2003; Gold 2005a). The editorial team of the Cochrane Schizophrenia Group helped at all stages, but especially in developing the protocol and retrieving study reports. Jun Xia helped with translating study reports for the present update from Chinese. Claire Ghetti provided valuable comments on an earlier draft of this review. We would also like to thank Daniel Cardoso and Genevieve Gariepy for peer reviewing this version of the review.
The Cochrane Schizophrenia group now provide a template for the methods section and other parts of the protocol. We have used this template and adapted it accordingly.
Appendices
Appendix 1. Previous searches
1. 2010 search
1. Cochrane Schizophrenia Group Trials Register (December 2010)
We searched the register using the phrase:
[(*musi* or *improvis* in title, abstract, index terms of REFERENCE)] or [(music* in interventions of STUDY)]
This register is compiled by systematic searches of major databases, handsearches and conference proceedings (see Group Module).
The previous version of the review (Gold 2005a) used a slightly different search strategy:
{[* musi* or musi* or * sound* or sound* or * acou* or acou* or gim in title, abstract, index terms of REFERENCE] or [music* in interventions of STUDY]}
However, the search terms sound* and acou* were dropped in this 2011 update as they only appeared to increase the number of false positives and did not help to identify any music therapy trials.
2. Handsearching
We searched the three American music therapy journals (Journal of Music Therapy, Music Therapy and Music Therapy Perspectives) as reissued on CD Rom by the American Music Therapy Association using the search term random* and then manually browsing through the results. The search covered the Journal of Music Therapy (1964‐1998), Music Therapy (1981‐1996) and Music Therapy Perspectives (1982‐1984, 1986‐1998).
3. Reference searching
We also inspected the references of all identified studies, included or excluded, for more studies.
4. Personal contact
We contacted the contact authors of relevant reviews or studies to enquire about other sources of relevant information.
5. Review articles
We inspected existing review articles pertinent to the topic of this review (Oerter 2001; Silverman 2003b) for references to any additional studies.
6. Cited reference search (forward search)
We searched ISI Web of Science for articles citing any of the included studies, in order to identify any more recent studies that might have been missed.
Appendix 2. Previous data collection and analysis
Data collection and analysis
Selection of studies
Three review authors independently inspected the citations identified from the search. Potentially relevant abstracts were identified and full papers ordered and reassessed for inclusion and methodological quality. Any disagreement was discussed and reported.
Data extraction and management
Two revew authors independently extracted data and, where further clarification was needed, contacted the authors of trials to provide missing information.
Assessment of risk of bias in included studies
Two review authors, again working independently allocated trials to three quality categories, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). When disputes arose as to which category a trial was allocated resolution was attempted by discussion. When this was not possible and further information was necessary, data were not entered into the analyses and the study was allocated to the list of those awaiting assessment. Only trials in Category A (adequate) or B (unclear) were included in the review.
Measures of treatment effect
1. Binary data For binary outcomes, a standard estimation of the fixed‐effect risk ratio (RR) and its 95% confidence interval (CI) was calculated. The number needed to treat statistic (NNT) was also calculated. If heterogeneity was found (see under Assessment of heterogeneity), the following possible sources of heterogeneity were examined: i. treatment dosage (20 sessions or more versus less than 20 sessions); and ii. treatment approach (quality of music therapy method and training).
2. Continuous data 2.1 Skewed data: continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data the following standards were applied to all data before inclusion: (a) standard deviations (SDs) and means were reported in the paper or were obtainable from the authors; (b) when a scale started from a finite number (such as zero), the SD, when multiplied by two, was less than the mean (as otherwise the mean was unlikely to be an appropriate measure of the centre of the distribution (Altman 1996)). Endpoint scores on scales often have a finite start and endpoint and this rule can be applied to them.
2.2 Summary statistic: for continuous outcomes a SMD between groups was estimated using a fixed‐effect model. Again, if heterogeneity was found (see under Assessment of heterogeneity) possible sources of heterogeneity were examined.
2.3 Valid scales: continuous data from rating scales were included only if the measuring instrument had been described in a peer‐reviewed journal and the instrument was either a self‐report or completed by an independent rater or relative (not the therapist). Unpublished instruments are more likely to report statistically significant findings than those that have been peer reviewed and published (Marshall 2000).
2.4 Endpoint versus change data: where possible endpoint data were presented and if both endpoint and change data were available for the same outcomes then only the former were reported in this review.
Unit of analysis issues
Studies may employ 'cluster randomisation' (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems: Authors often fail to account for intra‐class correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) where P values are spuriously low, confidence intervals (CI) unduly narrow and statistical significance overestimated causing type I errors (Bland 1997; Gulliford 1999). Although no cluster trials were identified for this review, the planned procedure for analysis would have been as follows. Where clustering was not accounted for in primary studies, we would have presented the data in a table, with an (*) symbol to indicate the presence of a probable unit of analysis error. We would have attempted to contact first authors of studies to seek intra‐class correlation coefficients of their clustered data and to adjust for this using the 'design effect' (Gulliford 1999; Higgins 2008). If the intra‐class correlation was not available, we would have used an external estimate from similar studies (Higgins 2008).
Dealing with missing data
We excluded data from studies where more than 30% of participants in any group were lost to follow‐up (this did not include the outcome of 'leaving the study early'). In studies with less than 30% dropout rate, people leaving early were considered to have had the negative outcome for dichotomous outcomes, except for the event of death. We analysed the impact of including studies with high attrition rates (20% to 30%) in a sensitivity analysis. If inclusion of data from this latter group did result in a substantive change in the estimate of effect, these data were not added to trials with less attrition but presented separately.
Assessment of heterogeneity
Firstly, we considered all the included studies within any comparison to judge clinical heterogeneity. Then we visually inspected graphs to investigate the possibility of statistical heterogeneity. This was supplemented, primarily, by employing the I2 statistic. This provides an estimate of the percentage of inconsistency thought to be due to chance. Where the I2 estimate was greater than or equal to 75%, this was interpreted as evidence of high levels of heterogeneity (Higgins 2003). If it was not possible to explain this heterogeneity by i. number of sessions (20 sessions or more versus less than 20 sessions) or ii. treatment approach (quality of music therapy method and training), a random‐effects model was used to describe and account for this unexplained heterogeneity.
Assessment of reporting biases
We entered data from all included studies into a funnel graph (trial effect against trial size) in an attempt to investigate the likelihood of overt publication bias (Davey 1997).
Data synthesis
Authors entered data in such a way that the area to the left of the line of no effect indicated a favourable outcome for music therapy when the outcome was negative (where "high" means "poor"), and reversed for positive outcomes (where "high" means "good").
Sensitivity analysis
We would have analysed the effect of including studies with high attrition rates in a sensitivity analysis, but no such studies were identified in this review.
Data and analyses
Comparison 1. Music therapy + standard care versus standard care alone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Global state: No clinically important overall improvement (as rated by trialists) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 short term | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.55, 1.24] |
| 1.2 medium term | 2 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.24, 0.59] |
| 2 Mental state: General ‐ 1a. Average endpoint score (PANSS, high score = poor) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 short term | 1 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.69 [‐1.16, ‐0.23] |
| 2.2 medium term | 2 | 159 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.97 [‐1.31, ‐0.63] |
| 2.3 long term | 1 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐3.41 [‐4.07, ‐2.76] |
| 3 Mental state: General ‐ 1b. Average endpoint score (BPRS, high score = poor) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1 short term | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.27 [‐0.45, 0.99] |
| 3.2 medium term | 1 | 70 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.25 [‐1.77, ‐0.73] |
| 4 Mental state: Specific ‐ 2. Negative symptoms ‐ average endpoint score (SANS, high score = poor) | 7 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 short term | 5 | 319 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐0.73, ‐0.27] |
| 4.2 medium term | 3 | 177 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.55 [‐0.87, ‐0.24] |
| 5 Mental state: Specific ‐ 3. Positive symptoms ‐ average endpoint score (SAPS, high score = poor) | 1 | 96 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.60, 0.24] |
| 5.1 short‐term | 1 | 96 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.60, 0.24] |
| 6 Mental state: Specific ‐ 4a. Depression ‐ average endpoint score (SDS, high score = poor) | 2 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐1.06, ‐0.21] |
| 6.1 short term | 2 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐1.06, ‐0.21] |
| 7 Mental state: Specific ‐ 4b. Depression ‐ average endpoint score (Ham‐D, high score = poor) | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐1.25, 0.21] |
| 7.1 short term | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐1.25, 0.21] |
| 8 Mental state: Specific ‐ 4c. Depression ‐ average endpoint score (CDSS, high score = poor)) | 1 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.73 [‐1.20, ‐0.26] |
| 8.1 short term | 1 | 75 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.73 [‐1.20, ‐0.26] |
| 9 Mental state: Specific ‐ 5. Anxiety ‐ average endpoint score (SAS, high score = poor) | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.61 [‐1.13, ‐0.09] |
| 9.1 short term | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.61 [‐1.13, ‐0.09] |
| 10 Leaving the study early | 18 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 short term | 11 | 692 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.06] |
| 10.2 medium term | 8 | 531 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.30, 1.30] |
| 10.3 long term | 2 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.50, 1.89] |
| 11 Functioning: General ‐ 1a. Average endpoint score (GAF, high score = good) | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 short term | 1 | 53 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.47, 0.62] |
| 11.2 medium term | 2 | 118 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.56, 0.18] |
| 12 Functioning: General ‐1b. Average endpoint score (IADL, high score = poor) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 medium term | 1 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.20 [‐1.65, ‐0.75] |
| 12.2 long term | 1 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.80 [‐2.29, ‐1.30] |
| 13 Functioning: Social 2a. Average endpoint score (SDSS, high score = poor) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13.1 short term | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.25 [‐1.94, ‐0.57] |
| 13.2 medium term | 2 | 160 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.72 [‐1.04, ‐0.40] |
| 13.3 long term | 1 | 90 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐0.98, ‐0.14] |
| 14 Functioning: Cognitive ‐ 3a. Attention ‐ average endpoint score (PASAT, high score = good) | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.22, 1.21] |
| 14.1 medium term | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.72 [0.22, 1.21] |
| 15 Functioning: Cognitive ‐ 3b. Vigilance and attention ‐ average endpoint score (CCPT, high score = good) | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.23, 0.74] |
| 15.1 medium term | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.23, 0.74] |
| 16 Functioning: Cognitive ‐ 3c. Memory ‐ average endpoint score (WMS, high score = good) | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [‐0.06, 0.92] |
| 16.1 medium term | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.43 [‐0.06, 0.92] |
| 17 Functioning: Cognitive ‐ 3d. Memory ‐ average endpoint score (CMT, high score = good) | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.58 [0.06, 1.09] |
| 17.1 short term | 1 | 60 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.58 [0.06, 1.09] |
| 18 Functioning: Cognitve ‐ 3e. Abstract thinking ‐ average endpoint score (BCST, high score = good) | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.39, 0.58] |
| 18.1 medium‐term | 1 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.39, 0.58] |
| 19 Functioning: Cognitive ‐ 3f. Abstract thinking ‐ average endpoint score (WCST‐Cc, high score = good) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 19.1 short term | 2 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.07, 0.03] |
| 19.2 medium term | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 1.18 [0.33, 2.03] |
| 20 Behaviour: 1. Average endpoint general behaviour score (NOSIE, high score = good) | 2 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.38 [0.93, 1.84] |
| 20.1 short term | 2 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.38 [0.93, 1.84] |
| 21 Behaviour: 2. Average change in general behaviour score (NOSIE, high score = good)) | 1 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.69 [0.18, 1.20] |
| 21.1 medium term | 1 | 62 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.69 [0.18, 1.20] |
| 22 Recipient of care satisfaction: Average endpoint score (CSQ, high score = good) | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.16, 0.80] |
| 22.1 medium term | 1 | 69 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.32 [‐0.16, 0.80] |
| 23 Quality of life: General ‐ average endpoint score (GWB, high score = good) | 1 | 72 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.82 [1.27, 2.38] |
| 23.1 short term | 1 | 72 | Std. Mean Difference (IV, Fixed, 95% CI) | 1.82 [1.27, 2.38] |
| 24 Quality of life: Specific 1. Mental health ‐ average endpoint score (SPG, high score = good) | 1 | 31 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.66, 0.75] |
| 24.1 short term | 1 | 31 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.66, 0.75] |
| 25 Quality of life: Specific 2. Perceived social support ‐ average endpoint score (SSQ, high score = good) | 1 | 72 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.73 [0.26, 1.21] |
| 25.1 short term | 1 | 72 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.73 [0.26, 1.21] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ceccato 2009.
| Methods | Allocation: randomised. Blindness: assessors were masked to treatment. Duration: 4 months. Design: parallel group. | |
| Participants | Diagnosis: schizophrenia (ICD‐10). History: unknown. N = 67. Age: range 20 to 60 years. Sex: 41 M, 26 F. Setting: in‐ and outpatients (private clients). | |
| Interventions | 1. Group music therapy: Sound Training Attention and Memory (STAM). 1 weekly session (16 sessions in total). N = 37. 2. Standard care (medication and other therapeutic treatment indicated for schizophrenia). N = 30. | |
| Outcomes | Cognitive functioning, attention: Paced Auditory Serial Addition Test (PASAT; Gronwall 1977). Cognitive functioning, vigilance and attention: Conners Continuous Performance Task 10 (CCPT; Rosvold 1956). Cognitive functioning, memory: Wechsler Memory Scale (WMS; Saggino 1983). Cognitive functioning, abstract thinking: Bergs' Card Sorting Test (BCST; Berg 1948). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised ‐ no further details. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were masked to treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: unclear (highly structured approach, relational aspects unclear). Adequate music therapy training: yes (based on a general statement in the paper: 'qualified music therapists', and personal communication with the authors). No personal, financial, or any other interests producing bias could be found. |
Cha 2012.
| Methods | Allocation: randomised. Blindness: unknown. Duration: 4 weeks. Design: parallel group. |
|
| Participants | Diagnosis: schizophrenia (DSM‐IV). History: unknown. N = 60. Age: unknown. Sex: unknown. Setting: inpatients. | |
| Interventions | 1. Receptive music therapy: song discussion, music reminiscence, musical synchronisation, and music and imagery. N = 30. 2. Standard care (medicine, health education and occupational and recreational therapy). N = 30. |
|
| Outcomes | Cognitive functioning, abstract thinking: Wisconsin Card Sorting Test (WCST; Heaton 1993). Cognitive functioning, memory: Clinical Memory Test (CMT; Xu 1986). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no details given |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes. No financial, personal or other interests producing bias detected. |
Chang 2013.
| Methods | Allocation: randomised ‐ no further details. Blindness: unknown. Duration: 8 weeks. Design: parallel group. | |
| Participants | Diagnosis: schizophrenia (CCMD‐3). History: mean 6.6 years, SD 4.2 years. N = 72. Age: mean 34.4 years, SD 12. Sex: 49 M, 23 F. Setting: inpatients. | |
| Interventions | 1. Receptive and active group music therapy (singing, music relaxation, music reminiscence, musical story, music discussion, song creation, playing instruments; all activities were led by a music therapist). 1 hour per session, 5 sessions a week for 8 weeks (40 sessions in total). N = 36, M 25. 2. Standard care (conventional drug therapy, general occupational and recreational therapy). N = 36, M 24. |
|
| Outcomes | Quality of life, general/subjective well‐being: General Well‐Being Schedule (GWB; Fazio 1977). Qualitiy of life, social support: Social Support Questionnaire (SSQ; Sarason 1983). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | no attrition |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes. No financial, personal or other interests producing bias detected. |
Fu 2013.
| Methods | Allocation: randomised ‐ no further details. Blindness: unknown. Duration: 4 weeks. Design: parallel group. | |
| Participants | Diagnosis: schizophrenia (ICD‐10). History: mean 3.6 years, SD 0.6 years. N = 40. Age: mean 38.3 years, SD 10.3. Sex: 18 M, 22 F. Setting: inpatients. | |
| Interventions | 1. Instrumental improvisational music therapy, 45 minutes per session, 3 sessions a week for 4 weeks (12 sessions in total). 5 people formed a therapy group. N = 20. 2. Standard care, medication. N = 20. |
|
| Outcomes | Social functioning: Social Disability Screening Schedule (SDSS; Wu 1998). Behaviour: Nurses' Observation Scale for Inpatient Evaluation (NOSIE; Honigfeld 1965). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes. The intervention was implemented by a trained music therapist. No financial, personal or other interests producing bias detected. |
Gold 2013.
| Methods | Allocation: randomised. Blindness: blinded assessment. Duration: 3 months. Design: parallel groups. |
|
| Participants | Diagnosis: psychotic disorders, mood (affective disorders), neurotic, stress‐related and somatoform disorders, personality disorders, substance‐related mental disorders, behavioural syndromes associated with physiological disturbances (ICD‐10). 64 patients had one or more secondary diagnoses. History: low therapy motivation. N = 144 (of whom 61 were eligible for this review). Age: 18 to 57 years. Sex: 39 M, 22 F. Setting: in‐ and outpatients. |
|
| Interventions | 1. Individual music therapy sessions, 45 minutes per session, 2 sessions per week for a period of 3 months from the date of randomisation. N = 72 2. Treatment as usual. N = 72 |
|
| Outcomes | General functioning: General Assessment of Function (GAF; Spitzer 2000). Mental state, negative symptoms: Scale for the Assessment of Negative Symptoms (SANS; Andreasen 1982). Unable to use ‐ not used in a non‐mixed sample: Brief Symptom Inventory (BSI‐18), General Perceived Self‐Efficacy Scale (GES), Inventory of Interpersonal Problems (IIP‐32), Rosenberg Self‐Esteem Scale (RSE), SF‐36 Health Survey, University of Rhode Island Change Assessment (URICA). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computerised randomisation was conducted. |
| Allocation concealment (selection bias) | Low risk | The allocation was concealed from the clinicians and the participants. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Single‐blind, assessors were masked to treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The analysis was carried out on an intention‐to‐treat basis. |
| Selective reporting (reporting bias) | Low risk | Study protocol available. All outcome measures were considered in the analysis |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes (music therapists provided music therapy in accordance with a therapy manual). No financial, personal or other interests producing bias detected. |
He 2005.
| Methods | Allocation: randomised ‐ no further details. Blindness: unknown. Duration: 6 weeks. Design: parallel group. | |
| Participants | Diagnosis: schizophrenia type II (CCMD‐3). History: approx. 9 years. N = 60. Age: mean 35 years, SD 8. Sex: 51 M, 9 F. Setting: inpatients. | |
| Interventions | 1. Receptive and 'participative' group music therapy (music listening, or music listening in combination with reading poems or dancing, music was chosen by the participants after an "induction" given by the therapist), 1 hour per session, 5 sessions per week (30 sessions in total). N = 30. 2. Standard care (medication only). N = 30. | |
| Outcomes | Mental state, negative symptoms: Scale for the Assessment of Negative Symptoms (SANS; Andreasen 1982). Not used: Prolactin levels (biomarker for mood: high = good). | |
| Notes | Music therapy was conducted by musicians. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information about how many participants have completed the study can be found in the results or discussion part of the article. According to the study design (only inpatients) and Chinese reporting standards (people leaving early are usually reported if there are any) we assume that all participants have completed the study. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: yes. Adequate music therapy training: unclear (music therapy was conducted by musicians who worked full time as music therapists at the hospital). No personal, financial, or any other interests producing bias could be found. |
Li 2007a.
| Methods | Allocation: randomised ‐ no further details. Blindness: unknown. Duration: 6 weeks. Design: parallel group. | |
| Participants | Diagnosis: schizophrenia (CCMD‐3). History: unknown. N = 60. Age: mean 32 years, SD 12. Sex: 60 M, 0 F. Setting: inpatients. | |
| Interventions | 1. Receptive group music therapy (music listening, music listening in combination with verbal inductions given by the therapist, 'positive hypnosis'/positive imagery), 40 minutes per session, 5 sessions per week (30 sessions in total). N = 30. 2. Standard care (supportive counselling). N = 30. | |
| Outcomes | Mental state, depression: Self‐Rating Depression Scale (SDS; Zhang 2003). Mental state, anxiety: Self‐Rating Anxiety Scale (SAS; Zhang 2003). Behaviour: Nurses' Observation Scale for Inpatient Evaluation (NOSIE; Honigfeld 1965). | |
| Notes | Music therapy was conducted by nurses, unclear how much they were trained in music therapy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 60 participants completed the trial. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: yes. Adequate music therapy training: unclear (music therapy was conducted by nurses with 'music therapy ability'). No personal, financial, or any other interests producing bias could be found. |
Liu 2013.
| Methods | Allocation: randomised. Blindness: unknown. Duration: 16 weeks. Design: parallel group. | |
| Participants | Diagnosis: chronic schizophrenia in recession (CCMD‐3). History: mean 9.7 years, SD 1.1 years. N = 30. Age: mean 42.9 years, SD 10.89. Sex: 17 M, 13 F. Setting: inpatients. | |
| Interventions | 1. Group receptive and recreative music therapy, and Orff music therapy, 45 minutes per session, twice a week, for 16 weeks. N = 15. 2. Standard care. N = 15. |
|
| Outcomes | Cognitive functioning, abstract thinking: Wisconsin Card Sorting Test (WCST; Heaton 1993). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropout |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis |
| Other bias | Unclear risk | Adequate music therapy method: yes. Adequate music therapy training: limited (no information about the therapist, to the author's (XJC) knowledge, the therapist is a music therapy teacher with a medical background, but had no systematic music therapy education). No personal, financial, or any other interests producing bias could be found. |
Lu 2013.
| Methods | Allocation: randomised. Blindness: unknown. Duration: 5 weeks. Design: parallel group. |
|
| Participants | Diagnosis: schizophrenia (DSM‐IV). History: mean 24.96 years, SD 9.82 years. N = 80. Age: mean 52.02 years, SD 7.64. Sex: 59 M, 21 F. Setting: inpatients. |
|
| Interventions | 1. Group music therapy (music listening, singing popular Taiwanese songs, playing percussion instruments, watching music videos, and discussions), 60 minutes per session, twice a week for 5 weeks (10 sessions in total). The music therapy sessions were delivered by a research assistant trained in music therapy in group settings. N = 38. 2. Received prescribed medication. Usual care included 24‐hour care with activities of daily living, basic nursing care, meal provision, and social activities (watching TV, family visiting, and occasional parties for special events). N = 42. |
|
| Outcomes | Mental state, general/psychotic symptoms: The Positive and Negative Syndrome Scale (PANSS; Kay 1987). Mental state, depression: Calgary Depression Scale for Schizophrenia (CDSS; Addington 1992). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The analysis was carried out on an intention‐to‐treat basis, |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes (music therapy was conducted by research assistant with training of music therapy in group setting). No personal, financial, or any other interests producing bias could be found. |
Mao 2013.
| Methods | Allocation: randomised. Blindness: unknown. Duration: 6 months. Design: parallel group. |
|
| Participants | Diagnosis: schizophrenia (CCMD‐3). History: mean 19.5 months, SD 17.2 months. N = 90. Age: mean 35.2 years, SD 7.4. Sex: 44 M, 46 F. Setting: inpatients. |
|
| Interventions | 1. In addition to regular medical treatment, group active and receptive music activities led by a music teacher and a psychotherapist (music theory class, music singing, instrument playing, music listening and appreciation). 45 minutes per session, 2 sessions per day in the morning and afternoon respectively, 5 days per week, for 6 months in total. N = 45. 2. Received prescribed medication. N = 45. |
|
| Outcomes | Mental state, general/psychotic symptoms: The Positive and Negative Syndrome Scale (PANSS; Kay 1987). Social functioning: Activities of daily living (ADL). Social functioning: Social Disability Screening Schedule (SDSS; Wu 1998). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropout |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: unclear Adequate music therapy training: limited (music therapy was conducted by a music teacher and a psychotherapist). No personal, financial, or any other interests producing bias could be found. |
Mohammadi 2012.
| Methods | Allocation: randomised. Blindness: unknown. Duration: 1 month. Design: parallel group. |
|
| Participants | Diagnosis: schizophrenia (DSM‐IV). History: unknown. N = 96. Age: mean 34.6 years, SD 8.05. Sex: 61 M, 35 F. Setting: inpatients. |
|
| Interventions | 1. Active music therapy plus medication: playing music instruments, singing, body movements with music rhythms. 3 sessions per week for 4 weeks (12 sessions in total). N = 35. 2. 'Passive' music therapy plus medication: music listening. 3 sessions per week for 4 weeks (12 sessions in total). N = 27. Two music therapists implemented these two groups. 3. Neuroleptic medication. N = 34. |
|
| Outcomes | Mental state, negative symptoms: Scale for the Assessment of Negative Symptoms (SANS; Andreasen 1982). Mental state, positive symptoms: Scale for the Assessment of Positive Symptoms (SAPS; Andreasen 1984). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analyses |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes. Music therapy was conducted by two music therapists. No personal, financial, or any other interests producing bias could be found. |
Qu 2012.
| Methods | Allocation: randomised. Blindness: unknown. Duration: 16 weeks. Design: parallel group. |
|
| Participants | Diagnosis: schizophrenia (CCMD‐3). History: range from 2.2 to 5 years. N = 58. Age: mean 31.6 years. Sex: 43 M, 15 F Setting: inpatients. |
|
| Interventions | 1. Group music appreciation and song singing in addition to standard care: 90 minutes per session, 2 sessions per day for 16 weeks. The intervention is combined with token rewards. N = 29. 2. Standard care includes antipsychotic medication, life skill training, health education, and recreative activities. N = 29. |
|
| Outcomes | Mental state, negative symptoms: Scale for the Assessment of Negative Symptoms (SANS; Andreasen 1982). Unable to use ‐ insufficient data: Social functioning: Inpatient Psychiatric Rehabilitation Outcome Scale (IPROS). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analyses |
| Other bias | Unclear risk | Adequate music therapy method: unclear Adequate music therapy training: limited. Music therapy was conducted by a nurse with good singing skills. No personal, financial, or any other interests producing bias could be found. |
Talwar 2006.
| Methods | Allocation: randomised ‐ block randomisation with ratio of experimental treatment to control treatment 1:2. Blindness: single ‐ assessor blinded; success of blinding verified by letting assessors guess the allocated condition; more than 50% guessed correctly, but this may be confounded with treatment effect. Duration: 3 months. Design: multicenter, 4 sites. | |
| Participants | Diagnosis: schizophrenia or related psychoses (ICD‐10: F2). History: unknown. N = 81. Age: mean 37 years, range 18 to 64. Sex: 60 M, 21 F. Setting: inpatients. | |
| Interventions | 1. Active individual music therapy (improvisation, songs, dialogue), 50 minutes per session, weekly sessions (12 sessions in total). N = 33. 2. Standard care (medication, nursing care, access to occupational, social and other activities). N = 48. | |
| Outcomes | Mental state, general/psychotic symptoms: The Positive and Negative Syndrome Scale (PANSS; Kay 1987). General functioning: General Assessment of Function (GAF; Spitzer 2000). Patient satisfaction: Client Satisfaction Questionnaire (CSQ; Atkinson 1994). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers. |
| Allocation concealment (selection bias) | Low risk | Randomisation was conducted by a person independent of the researcher, and extensive steps were taken to mask the researcher to the participants' allocation status. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Interviews were conducted by a researcher masked to treatment condition; a test of the success of masking was provided: Interviewer attempted to guess the allocation status of each of the participants after three‐month follow‐up data had been collected (kappa=.31, P <. 01). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analysis was carried out on an intention‐to‐treat basis. Multiple imputation was used to account for the missing data in outcome measures at follow‐up. This method imputes m > 1 plausible values for each missing value, under the assumption of missing at random. In this review, only the actually observed data were used, not the imputed data. Multiple imputation is not recommended when only dependent variables are missing (Allison 2002, p. 54, p. 70). |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes (all music therapists attended an approved music therapy course and received fortnightly supervision). No personal, financial, or any other interests producing bias could be found. |
Tang 1994.
| Methods | Allocation: randomised ‐ no further details. Blindness: single ‐ assessor blinded. Duration: 1 month. Design: parallel group. | |
| Participants | Diagnosis: residual schizophrenia (DSM‐III‐R). History: unknown. N = 76. Age: not reported. Sex: not reported. Setting: inpatients. | |
| Interventions | 1. Active and receptive large‐group music therapy (music listening, singing and playing on instruments, discussion), 1 hour per session, 5 sessions per week (on average 19 sessions in total). N = 38. 2. Standard care (medication only). N = 38. | |
| Outcomes | Mental state, negative symptoms: Scale for the Assessment of Negative Symptoms (SANS; Andreasen 1982). Unable to use ‐ insufficient data: Disability Assessment Schedule (DAS). |
|
| Notes | Author unable to provide additional data. Music therapy was conducted by clinicians (doctor, nurses) with limited training. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Nurses who did the SANS and DAS assessment for participants were blinded to treatment status. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 76 participants completed the trial. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: yes. Adequate music therapy training: unclear (one doctor and two nurses conducted the music therapy. Two of them attended a two‐week music therapy course). No financial, personal or other interests producing bias detected. |
Ulrich 2007.
| Methods | Allocation: randomised. Blindness: single ‐ assessor blinded; assessors unaware of study aim; success of blinding verified by letting assessors guess what the study aim was; none were aware that the study aim involved music therapy. Duration: 4.8 weeks. Design: parallel group. | |
| Participants | Diagnosis: schizophrenia or related psychoses (27 of 37 had F20 in ICD‐10). History: unknown. N = 37. Age: mean 38 years, range 22 to 58. Sex: 20 M, 17 F. Setting: inpatients. | |
| Interventions | 1. Active group music therapy (focusing on musical processes and discussion of patients' problems), 60 to 105 minutes per session, on average 7.5 sessions. N = 21. 2. Standard care (medication, "other" activities ‐ no detailed description given). N = 16. | |
| Outcomes | Mental state, negative symptoms: Scale for the Assessment of Negative Symptoms (SANS; Andreasen 1982).
Quality of life, mental health: Skalen zur psychischen Gesundheit [scales about mental health] (SPG; Tönnies 1996). Unable to use ‐ unvalidated subscales of published scale: Gießentest. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A dice was thrown. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Personnel and patients were blinded to the fact that research of music therapy was the study aim. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were blinded to the research aim. Blinding was tested successfully at the end of the study. No one indicated that the aim of the study was testing the effectiveness of music therapy. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | People leaving early were reported. Intention‐to‐treat analysis was used: Participants whose diagnosis was changed after inclusion in the study were not excluded. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes (based on a general statement: 'qualified music therapists' and a reference in the article). No financial, personal or other interests producing bias detected. |
Wang 2013.
| Methods | Allocation: randomised. Blindness: unknown. Duration: 3 months. Design: parallel group. |
|
| Participants | Diagnosis: chronic schizophrenia (CCMD‐3). History: mean 13.6 years, SD 1.7 years. N = 62. Age: mean 36.7 years, SD 9.8. Sex: 39 M, 23 F. Setting: inpatients. |
|
| Interventions | 1. Group and individual music therapy, including active and receptive methods, improvisation, musical appreciation, song singing, and rhythm training in addition to standard care. 3 sessions per week for three months (36 sessions in total); no information about duration of sessions. N = 31. 2. Standard care. N = 31. |
|
| Outcomes | Behaviour: Nurses' Observation Scale for Inpatient Evaluation (NOSIE; Honigfeld 1965). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analyses |
| Other bias | Unclear risk | Adequate music therapy method: unclear. Adequate music therapy training: limited (music therapy was conducted by a nurse). No personal, financial, or any other interests producing bias could be found. |
Wen 2005.
| Methods | Allocation: randomised ‐ no further details. Blindness: unknown. Duration: 6 weeks. Design: parallel group. | |
| Participants | Diagnosis: schizophrenia (CCMD‐3). History: unknown. N = 30. Age: 15 to 50 years. Sex: 21 M, 9 F. Setting: inpatients. | |
| Interventions | 1. Receptive group music therapy (music listening, other music activities: dancing, discussion emphasising the emotional aspects of the music while listening to it), 1 hour per session, 5 sessions per week (30 sessions in total). N = 16. 2. Standard care (medication only, no anxiolytic or antidepressant). N = 14. | |
| Outcomes | Mental state, general: Brief Psychiatric Rating Scale (BPRS; Overall 1988). Mental state, depression: Self‐Rating Depression Scale (SDS); Hamilton Depression Scale (Ham‐D; Hamilton 1960). Unable to use ‐ unpublished scale: Inpatient Recovery Effect Scale. |
|
| Notes | Music therapy was conducted by the authors (probably psychiatrists) and nurses. No information given if these clinicians were trained in music therapy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed the trial. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Unclear risk | Adequate music therapy method: yes. Adequate music therapy training: unclear (no information was given, if the persons conducting music therapy, nurses and probably psychiatrists, were trained in music therapy). No financial, personal or other interests producing bias detected. |
Yang 1998.
| Methods | Allocation: randomised ‐ no further details. Blindness: unknown; assessments by two psychiatrists. Duration: 3 months. Design: parallel group. | |
| Participants | Diagnosis: schizophrenia (CCMD‐2). History: chronic, duration of disorder 2 to 26 years. N = 72. Age: range 21 to 55 years. Sex: 41 M, 29 F (reported for 70 valid cases). Setting: inpatients. | |
| Interventions | 1. Active and receptive individual and group music therapy (music listening, improvisation, discussion), 2 hours per session, 6 sessions per week (78 sessions in total). N = 41. 2. Standard care (medication only). N = 31. | |
| Outcomes | Global state: No clinically important improvement (as rated by trialists). Mental state, general: Brief Psychiatric Rating Scale (BPRS; Overall 1988). Mental state, negative symptoms: Scale for the Assessment of Negative Symptoms (SANS; Andreasen 1982). Social functioning: Social Disability Schedule for Inpatients (SDSI; Wu 1998). Unable to use ‐ insufficient data: Present State Examination Change Rating Scale (PSE). |
|
| Notes | Author unable to provide additional data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details given. |
| Allocation concealment (selection bias) | Unclear risk | No details given. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Due to the nature of the intervention it was not possible to blind those who received music therapy or those who delivered it. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details given. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Two people were reported as leaving early and the reported data are based on a total number excluding those who left early. No participants with complete data were excluded. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available. All outcome measures described in the study were considered in the analysis. |
| Other bias | Low risk | Adequate music therapy method: yes. Adequate music therapy training: yes (well‐known Chinese music therapist was involved in the project). No financial, personal or other interests producing bias detected. |
CCMD‐2/3 ‐ Chinese Classification of Mental Disorders, second/third edition DSM‐III‐R ‐ Diagnostic and Statistical Manual of Mental Disorders‐III‐R F ‐ Female ICD‐10 ‐ ICD‐10: F2 – International Classification of Diseases (version 10); ‘F’ refers to large disease sub‐categories within ICD M ‐ Male SD – Standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adler 2005 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (medication versus placebo). |
| Apter 1978 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (movement therapy, dance therapy). |
| Arango 2003 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (medication). |
| Barrowclough 2001 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (treatment package versus standard care). |
| Bean 1964 | Allocation: not randomised (all received the same intervention). |
| Bechdolf 2005 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (CBT versus supportive counselling). |
| Brotons 1987 | Allocation: unclear (unable to retrieve full report). |
| Cassity 1976 | Allocation: randomised. Participants: people with schizophrenia and other psychiatric disorders. Intervention: music therapy versus standard care. Outcomes: no usable and relevant data. |
| Castilla‐Puentes 2002 | Allocation: randomised. Participants: people with schizophrenia and other psychiatric disorders. Intervention: music therapy versus supportive talking/counselling. Outcomes: no usable data (unable to retrieve full report). |
| Ceccato 2006 | Allocation: not randomised (CCT, matched groups). |
| Chambliss 1996 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music listening). |
| Cook 1973 | Allocation: not randomised (single case study). |
| de l'Etoile 2002 | Allocation: not randomised (case series). |
| Drury 1996 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (cognitive therapy versus structured activities and informal support). |
| Gaszner 2009 | Allocation: unclear (CCT; author was contacted but we did not receive the requested information). Participants: people with schizophrenia. Interventions: not music therapy (one medication versus two or more medications versus medication and complex therapy including psychotherapy, sociotherapy, psychiatric rehabilitation). |
| Glicksohn 2000 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (only music listening). |
| Green 1987 | Allocation: randomised. Participants: people with schizophrenia and other psychiatric disorders. Interventions: not music therapy (art therapy versus standard care). |
| Grocke 2009a | Allocation: not randomised (case series). |
| Grocke 2014 | Allocation: randomized (75 of 99). Participants: people with schizophrenia (33 of 99). Interventions: music therapy. Outcomes: not relevant (Q‐LES‐Q‐18, ENRICHD, RSE, FACIT‐Sp‐12, BSI ‐ not used in a non‐mixed sample). |
| Haimov 2012 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (listening to relaxing music). |
| Hannes 1974 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (recreational therapy/socialising). |
| Hayashi 2002 | Allocation: not randomised (CCT/comparison of 2 cohorts). |
| Hodgson 1996 | not able to retrieve information needed. |
| Hogarty 1988 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (family therapy versus standard care). |
| Hu 2004 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music‐sport therapy: music listening, Karaoke, sport activities). |
| Hustig 1990 | Allocation: not randomised (case series). |
| Ji 2013 | Allocation: randomised. Participants: people with chronic schizophrenia. Intervention: group music therapy and group psychotherapy. From the design, it is not possible to separate the effects of music therapy. |
| Johnston 2002 | Allocation: not randomised (n‐of‐1‐CCT). |
| Kallert 2004 | Allocation: randomised. Participants: people with schizophrenia and other mental disorders. Interventions: not music therapy (treatment package). |
| Kong 2007 | Allocation: randomised. Participants: people with chronic schizophrenia. Interventions: not music therapy (music listening only). |
| Krajewski 1993 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (CBT versus art therapy versus CBT and art therapy). |
| Leung 1998 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (Karaoke therapy versus simple singing) |
| Li 2005 | Allocation: randomised. Participants: people with chronic schizophrenia. Interventions: not music therapy (music education, sport activities, gardening). |
| Li 2007b | Allocation: randomised. Participants: people with schizophrenia. Intervention: not music therapy (modelling and behaviour training). |
| Li 2011 | Allocation: randomised. Participants: chronic schizophrenia. Intervention: not music therapy (music listening conducted by a nurse). |
| Lin 2003 | Allocation: randomised. Participants: people with schizophrenia on recovery stage. Interventions: not music therapy (music listening only). |
| Luo 2014 | Allocation: not randomised (cohort study). |
| Margo 1981 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music listening only). |
| Martinez 2005 | Allocation: not randomised (CCT, quasi‐randomised). |
| McInnis 1990 | Allocation: not randomised (single case study). |
| Meschede 1983 | Allocation: not randomised (case series). |
| Metzner 2010 | Allocation: not randomised (single case study). |
| Moe 2000 | Allocation: not randomised (single group study). |
| Morgan 2011 | Allocation: not randomised (comparison of two consecutive cohorts). |
| Muller 2014 | Allocation: randomised. Participants: people with psychiatric symptoms. Intervention: not music therapy (music listening). |
| Murow 1997 | Allocation: not randomised (CCT, allocation by order of intake). |
| Na 2009 | Allocation: not randomised (CCT, cross‐over design). |
| Nelson 1991 | Allocation: not randomised (CCT). |
| Ni 2002 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music listening only). |
| Offer 1960 | Allocation: not randomised (CCT, allocation by different diagnoses) |
| Olbrich 1990 | Allocation: not randomised (CCT, allocation by order of intake). |
| Pavlicevic 1994 | Allocation: not randomised (CCT, matched groups). |
| Pfeiffer 1987 | Allocation: randomised. Participants: people with schizophrenia. Interventions: music therapy versus standard care. Outcomes: no usable data. |
| Pierce 2004 | Allocation: not randomised (cohort study). |
| Reker 1991 | Allocation: not randomised (case series). |
| Schmuttermayer 1983 | Allocation: not randomised (single group study). |
| Silverman 2003a | Allocation: not randomised (single case study). |
| Silverman 2009 | Allocation: randomised. Participants: people with schizophrenia and other mental disorders. Interventions: music therapy. Outcomes: not relevant (SWLS ‐ Satisfaction with Life Scale ‐ not used in a non‐mixed sample; AKIRI ‐ Adapted Knowledge of Illness and Resources Inventory ‐ modified published scale; patient satisfaction with care ‐ unpublished scale). |
| Silverman 2011a | Allocation: randomised. Participants: people with mental disorders, no specific diagnoses available. |
| Silverman 2011b | Allocation: randomised. Participants: people with mental disorders, no specific diagnoses available. |
| Silverman 2011c | Allocation: randomised. Participants: people with mental disorders, no specific diagnoses available. |
| Silverman 2013 | Allocation: randomised. Participants: people with schizophrenia and other mental disorders. Interventions: music therapy. Outcomes: not relevant (Stigma Scale (King et al., 2007) ‐ not used in a non‐mixed sample). |
| Silverman 2014a | Allocation: randomised. Participants: people with schizophrenia and other mental disorders. Interventions: music therapy. Outcomes: not relevant (MSPSS ‐ Quality of life: Multidimensional Scale of Perceived Social Support, WFPTS ‐ Wake Forest Physician Trust Scale ‐ not used in a non‐mixed sample). |
| Silverman 2014b | Allocation: randomised. Participants: people with various mental disorders. Only two had schizophrenia or related psychoses. |
| Silverman 2016 | Allocation: randomised. Participants: people with schizophrenia and other mental disorders. Interventions: music therapy. Outcomes: not relevant (POMS ‐ Profile of Mood States ‐ not used in a non‐mixed sample; AKIRI ‐ Adapted Knowledge of Illness and Resources Inventory ‐ modified published scale). |
| Skelly 1952 | Allocation: not randomised (case series). |
| Song 1994 | Allocation: not randomised (groups were matched by age, sex, education, and diagnosis). |
| Steinberg 1991 | Allocation: not randomised (case series). |
| Su 1999 | Allocation: randomised. Participants: people with chronic schizophrenia. Interventions: not music therapy (dance therapy). |
| Su 2005 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (group psychotherapy, behaviour therapy, recreational therapy, music listening, other activities). |
| Tan 2009 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (computerised cognitive remediation therapy), active control group (treatment package including occupational therapy, recreational therapy and music therapy). |
| Tang 2002 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (brainwave generator combined with electronic music instruments) |
| Thaut 1989 | Allocation: not randomised (single group study). |
| Troice 2003 | Allocation: not randomised (single group study). |
| Vadas 2012 | Allocation: randomised. Participants: psychiatric patients, including schizophrenia, schizoaffective disorder, and affective mood disorders. Intervention: not music therapy (listening to relaxing music). |
| Valencia 2006 | Allocation: not randomised to music therapy versus placebo or standard care (random allocation of participants to three active treatment conditions including music therapy; a control group (medication only) was not randomised but obtained from a waiting list). |
| Wahass 1997 | Allocation: randomised. Participants: people with schizophrenia. Intervention: not music therapy (treatment package). |
| Wang 2002a | Allocation: randomised. Participants: people with chronic schizophrenia. Interventions: not music therapy (music listening only). |
| Wang 2002b | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music listening only). |
| Wang 2005 | Allocation: not randomised (CCT, quasi‐randomised according to the date of entry). |
| Wang 2006 | Allocation: not randomised (CCT, quasi‐randomised according to the date of entry). |
| Wang 2007 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music listening, Karaoke singing by the patients, without music therapist). |
| Warren 1980 | Allocation: not randomised (all received the same stimuli within the same session); not an intervention study. |
| Wu 2000 | Allocation: not randomised (pre‐post test design). |
| Wu 2003 | Allocation: not randomised (uncontrolled pre‐post design). |
| Xiao 2005 | Allocation: randomised. Participants: people with chronic schizophrenia. Interventions: unclear if music therapy (insufficient details), and not music therapy alone (treatment package: psychotherapy, recreational therapy, music therapy versus medical treatment). |
| Yang 2005 | Allocation: randomised. Participants: people with chronic schizophrenia. Interventions: not music therapy (psychotherapy) versus active control group (recreational therapy: dance, music, reading, writing, drawing). |
| Zhang 2003a | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music listening, music appreciation, dancing). |
| Zhang 2003b | Allocation: possibly randomised, unclear. Participants: people with schizophrenia. Interventions: music therapy versus behaviour correcting therapy. |
| Zhang 2005 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (different music activities, e.g. singing, music education, dancing, watching MTV, are taking place in the patient's leisure time together with nurses who are not trained as music therapists). |
| Zhang 2010 | Allocation: randomised. Participants: refractory schizophrenia. Intervention: not music therapy (music listening played through a "music therapy" machine). |
| Zhang 2013 | Allocation: randomised. Participants: people with chronic schizophrenia. Intervention: not music therapy (music listening only, no information of the therapist). |
| Zhao 2013 | Allocation: not randomised (case series). |
| Zhou 2003 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music listening). |
| Zhou 2006 | Allocation: randomised. Participants: people with schizophrenia. Interventions: music therapy versus active control group (music listening only). |
| Zhu 2002 | Allocation: randomised. Participants: people with schizophrenia. Interventions: not music therapy (music listening only). |
| Zincir 2011 | Allocation: randomised. Participants: people with schizophrenia. Intervention: group music therapy with classic Turkish music tones, no information about the music therapist. Only abstract was available, the author's contact information has not been found. |
BSI ‐ Brief Symptom Inventory CBT – Cognitive Behavioural Therapy CCT – Controlled clinical trial ENRICHD ‐ Social Support Inventory FACIT‐Sp‐12 ‐ 12‐item Functional Assessment of Chronic Illness Therapy‐Spiritual well‐being scale MTV – Music television Q‐LES‐Q‐18 ‐ abbreviated Quality of Life Enjoyment and Satisfaction Questionnaire RSE ‐ Rosenberg Self‐Esteem Scale
Differences between protocol and review
No differences between the protocol and the 2005 publication.
In the 2011 update (2010 search), clarifications have been added concerning the definition of the intervention and methods of analysis.
In the 2015 version, the layout and numbering of outcomes has been changed for consistency across sections of the review, now a MECIR standard for Cochrane reviews, the type of outcomes remains the same.
Contributions of authors
Monika Geretsegger ‐ co‐ordinated data extraction and classification for the present update and wrote the report.
Karin Mössler ‐ co‐ordinated 'Risk of bias' assessment and 'Summary of findings' table and helped to write the report. Co‐ordinated the previous update (Mössler 2011b).
Łucja Bieleninik ‐ contributed to resolving disagreements on eligibility, helped with the 'Risk of bias' assessment and 'Summary of findings' table and helped to write the report of the present update.
Xi‐Jing Chen ‐ helped with translation, data extraction and classification of the present and the previous update (Mössler 2011b).
Tor Olav Heldal ‐ helped with data extraction and classification for the present update and previous versions (Gold 2005a; Mössler 2011b).
Christian Gold ‐ designed the protocol, co‐ordinated the reviewing, overlooked the selection of studies, extracted and analysed data, and wrote the report of the present update. Co‐ordinated previous versions (Gold 2005a; Mössler 2011b) and the original protocol (Gold 2003).
Sources of support
Internal sources
University of Bergen, Norway.
Uni Research, Bergen, Norway.
External sources
The Research Council of Norway, Norway.
Declarations of interest
Monika Geretsegger ‐ clinically trained music therapist.
Karin Mössler ‐ clinically trained music therapist and author of an included trial.
Łucja Bieleninik ‐ none.
XiJing Chen ‐ clinically trained music therapist.
Tor Olav Heldal ‐ clinically trained music therapist.
Christian Gold ‐ clinically trained music therapist and author of an included trial.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Ceccato 2009 {published data only}
- Ceccato E. Music therapy in rehabilitation for people with schizophrenia. A multicenter, single blind, randomised controlled trial testing the effectiveness of the STAM protocol (Sound Training Attention and Memory) [Musicoterapia nella riabilitazione cognitiva del paziente schizofrenico. Studio multicentrico randomizzato e controllato in singolo cieco di applicazione del protocollo STAM (Sound Training Attention and Memory)]. Master's thesis 2010.
- Ceccato E, Caneva P, Lamonaca D. Music therapy and cognitive rehabilitation in schizophrenic patients. Nordic Journal of Music Therapy 2006;15(2):111‐20. [Google Scholar]
- Ceccato E, Lamonaca D, Caneva PA, Gamba L, Poli R, Agrimi E. A multicentre study to test the effectiveness of the STAM (Sound Training Attention and Memory) protocol in the rehabilitation of patients with schizophrenia: a single blind, randomized control trial [Musicoterapia nella riabilitazione cognitiva del paziente schizofrenico. Studio multicentrico randomizzato controllatoin singolo cieco di applicazione del protocollo STAM (Sound Training Attention and Memory)]. Giornale Italiano di Psicopatologia 2009;15:395‐400. [Google Scholar]
Cha 2012 {published data only}
- Cha ZQ, Li D, Wu QF, Zhang Y, Lu JB, M ZQ. The effect of receptive music therapy on cognitive function of schizophrenia patients in remission [jie shou xing yin yue zhi liao dui jing shen fen lie huan jie qi ren zhi gong neng de ying xiang]. China Health Psychology 2012; Vol. 20, issue 07:1039‐40. [CENTRAL: 20561]
Chang 2013 {published data only}
- Chang CH, Liu FF, Xu TH, Jiao TL. A research of music therapy on subjective well‐being and social support for patients with schizophrenia [yin yue zhi liao dui jing shen fen lie huan zhe zhu guan xing fu gan yu she hui zhi chi de xiang guan yan jiu]. National Medicine 2013; Vol. 25, issue 11:25‐7.
Fu 2013 {published data only}
- Fu WJ, Zhang LF. The rehabilitation effect of improvisational music therapy on the treatment of social disability in patients with schizophrenia in recovery period [ji xing yan zou shi yin yue zhi liao dui kang fu qi jing shen fen lie huan zhe she hui gong neng que sun de kang fu xiao ying]. Sichuan Mental Health 2013; Vol. 26, issue 03:215‐8.
Gold 2013 {published and unpublished data}
- Gold C, Mossler K, Grocke D, Heldal TO, Tjemsland L, Aarre T, et al. Individual music therapy for mental health care clients with low therapy motivation: Multicentre randomised controlled trial. Psychotherapy and Psychosomatics 2013; Vol. 82, issue 5:319‐31. [DOI] [PubMed]
- Gold C, Rolvsjord R, Aaro LE, Aarre T, Tjemsland L, Stige B. Resource‐oriented music therapy for psychiatric patients with low therapy motivation: protocol for a randomised controlled trial. BMC Psychiatry 2005;5(39):1‐8. [MEDLINE: ; MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold C, Tjemsland L, Tytlandsvik M, Heskestad S, Aarre T, Stige B. Resource‐oriented music therapy for psychiatric patients with low therapy motivation: a randomised controlled trial. www.clinicaltrials.gov 2005. [DOI] [PMC free article] [PubMed]
He 2005 {published data only}
- He FR, Liu RK, Ma L. Influence of musical therapy on serum PRL of patients with schizophrenia, type II [yin yue xin li zhi liao dui ‖xing jing shen fen lie huan zhe xue qing cui ru su shui ping de ying xiang]. Shandong Archives of Psychiatry 2005;18(2):78‐9. [CAJ] [Google Scholar]
Li 2007a {published data only}
- Li YM, Ren X, Li CP, Li ZQ. The correct effect of language guided music therapy on patients with schizophrenia [yu yan you dao shi yin yue liao fa dui jing shen fen lie huan zhe de xin li jiao zhi xiao guo]. International Nurses Journal 2007;26(9):917‐8. [CHINESE: Academic Journals] [Google Scholar]
Liu 2013 {published data only}
- Liu SJ, Wu HL, Shi L. The impact of music therapy on cognitive function for patients with chronic schizophrenia in recession [yin yue zhi liao dui jing shen fen lie zheng man xing shuai tui qi huan zhe ren zhi gong neng de ying xiang]. China Rehabilitation 2013; Vol. 28, issue 03:230‐1.
Lu 2013 {published data only}
Mao 2013 {published data only}
- Mao ZQ, Li D, Zhang GF, Cha ZQ, Rong JK. The effects of music therapy on the rehabilitation of patients with chronic schizophrenia [yin yue zhi liao dui man xing jing shen fen lie zheng huan zhe de kang fu xiao guo guan cha]. China Journal of Health Psychology 2013; Vol. 21, issue 01:56‐7.
Mohammadi 2012 {published data only}
- Mohammadi AZ, Minhas LS, Haidari M, Panah FM. A study of the effects of music therapy on negative and positive symptoms in schizophrenic patients. German Journal of Psychiatry 2012; Vol. 15, issue 2:56‐62.
Qu 2012 {published data only}
- Qu YN, Huang YF, Zhou ZX, Li LH. The rehabilitation care for elderly patients with chronic schizophrenia in long‐term hospitalization [chang qi zhu yuan man xing jing shen fen lie zheng huan zhe lao nian qi de kang fu hu li]. Guide of Chinese Medicine 2012; Vol. 10, issue 09:552‐4.
Talwar 2006 {published and unpublished data}
- Crawford M. A pilot randomised controlled trial to examine the effects of individual music therapy among inpatients with schizophrenia and schizophrenia like illness. National Research Register 2004; Vol. 2.
- Gold C. Music therapy improves symptoms in adults hospitalised with schizophrenia. Evidence‐Based Mental Health 2007;10(3):77. [CINAHL: 2009752767; MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Maratos A. A pilot randomised controlled trial to examine the effects of individual music therapy among inpatients with schizophrenia and schizophrenia‐like illnesses. Unpublished study protocol 2004.
- Maratos A, Crawford M. Composing ourselves: What role might music therapy have in promoting recovery from acute schizophrenia?. London West Mental Health R&D Consortium's 9th Annual Conference. 2004.
- Talwar N, Crawford M, Maratos A. A single blind randomised controlled trial of music therapy in patients with schizophrenia and related psychoses. Thematic Conference of the World Psychiatric Association on "Treatments in Psychiatry: An Update"; 2004 Nov 10‐13; Florence, Italy. 2004.
- Talwar N, Crawford MJ, Maratos A, Nur U, McDermott O, Procter S. Music therapy for in‐patients with schizophrenia: exploratory randomised controlled trial. British Journal of Psychiatry 2006;189:405‐9. [AMED: 92246; MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Tang 1994 {published data only (unpublished sought but not used)}
- Tang W, Yao X, Zheng Z. Rehabilitative effect of music therapy for residual schizophrenia: A one‐month randomised controlled trial in Shanghai. British Journal of Psychiatry 1994;165(suppl. 24):38‐44. [PubMed] [Google Scholar]
Ulrich 2007 {unpublished data only}
- Ulrich G. De toegevoegde waarde van groepsmuziektherapie bij schizofrene patiënten: Een gerandomiseer onderzoek [The added value of group music therapy with schizophrenic patients: A randomised study]. Heerlen, NL: Open Universiteit, 2005. [Google Scholar]
- Ulrich G. [A randomised study of music therapy for schizophrenia: Study protocol]. Unpublished manuscript 2003.
- Ulrich G, Houtmans T, Gold C. The additional therapeutic effect of group music therapy for schizophrenic patients: a randomized study. Acta Psychiatrica Scandinavica 2007;116(5):362‐70. [MEDLINE: ; MEDLINE: ; PsycINFO] [DOI] [PubMed] [Google Scholar]
- Ulrich G, Houtmans T, Lechner L. [English Translation not available] [De toegevoegde waarde van groepsmuziektherapie bij schizofrene patiënten een gerandomiseerd onderzoek]. Dissertation submitted to Open Universiteit Nederland 2005.
Wang 2013 {published and unpublished data}
- Wang S. The effects of music therapy on improving social function in patients with chronic schizophrenia [man xing jing shen fen lie huan zhe fu yi yin yue zhi liao dui qi she hui gong neng de gai shan]. The National Medicine 2013; Vol. 25, issue 13:51‐2.
Wen 2005 {published data only}
- Wen SR, Cao GY, Zhou HS. The effect of music therapy on the depressive position of patients with schizophrenia [yin yue zhi liao dui jing shen fen lie huan zhe de yi yu zhuang tai de ying xiang]. Chinese Journal of Clinical Rehabilitation 2005;9(8):195. [Google Scholar]
Yang 1998 {published data only (unpublished sought but not used)}
- Yang WY, Li Z, Weng YZ, Zhang HY, Ma B. Psychosocial rehabilitation effects of music therapy in chronic schizophrenia. Hong Kong Journal of Psychiatry 1998;8(1):38‐40. [Google Scholar]
References to studies excluded from this review
Adler 2005 {published data only}
- Adler LE, Cawthra EM, Donovan KA, Harris JG, Nagamoto HT, Olincy A, et al. Improved P50 auditory gating with ondansetron in medicated schizophrenia patients. American Journal of Psychiatry 2005;162(2):386‐8. [DOI] [PubMed] [Google Scholar]
Apter 1978 {published data only}
- Apter A, Sharir I, Tyano S, Wijsenbeek H. Movement therapy with psychotic adolescents. British Journal of Medical Psychology 1978;51:155‐9. [DOI] [PubMed] [Google Scholar]
Arango 2003 {published data only}
- Arango C, Summerfelt A, Buchanan RW. Olanzapine effects on auditory sensory gating in schizophrenia. American Journal of Psychiatry 2003;160(11):2066‐8. [DOI] [PubMed] [Google Scholar]
Barrowclough 2001 {published data only}
- Barrowclough C, Haddock G, Tarrier N, Lewis SW, Moring J, O'Brien R, Schofield N, McGovern J. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. American Journal of Psychiatry 2001;158(10):1706‐13. [DOI] [PubMed] [Google Scholar]
- Haddock G, Barrowclough C, Tarrier N, Moring J, O'Brien R, Schofield N, et al. Cognitive‐behavioural therapy and motivational intervention for schizophrenia and substance misuse. 18‐month outcomes of a randomised controlled trial. British Journal of Psychiatry 2003;183:418‐26. [DOI] [PubMed] [Google Scholar]
Bean 1964 {published data only}
- Bean KL, Moore JR. Music therapy from auditory ink blots. Journal of Music Therapy 1964;1:143‐7. [Google Scholar]
Bechdolf 2005 {published data only}
- Bechdolf A. Psychological intervention for persons at risk of psychosis in the early initial prodromal state. http://www.clinicaltrials.gov.2005.
Brotons 1987 {published data only}
- Brotons M. The correlations between content of preferred music and psychiatric diagnosis of criminal offenders and effects of this music on observed behavior. Master's thesis. Tallahassee, FL: Florida State University, 1987. [Google Scholar]
- Brotons M. The correlation between content of preferred music and psychiatric diagnosis of criminal offenders and effects of this music on observed behavior. Thesis 1997. [MEDLINE: ]
Cassity 1976 {published data only}
- Cassity MD. The influence of a music therapy activity upon peer acceptance, group cohesiveness, and interpersonal relationships of adult psychiatric patients. Journal of Music Therapy 1976;13:66‐76. [Google Scholar]
Castilla‐Puentes 2002 {published data only (unpublished sought but not used)}
- Castilla RC, Perel JM. Group music therapy and medication compliance: A controlled study on patients with chronic psychotic disorders. World Journal of Biological Psychiatry 2004; Vol. 5, issue Supp 1:152.
- Castilla‐Puentes RC, Valero J, Vargas J, Gongora O, Pava C, Perel J. Music therapy and medication compliance in psychotic patients. 155th Annual Meeting of the American Psychiatric Association. 2002 May 18‐23; Philadelphia, Pennsylvania, USA.
Ceccato 2006 {published data only}
- Ceccato E, Caneva P, Lamonaca D. Music therapy and cognitive rehabilitation in schizophrenic patients. Nordic Journal of Music Therapy 2006;15(2):111‐20. [Google Scholar]
- Ceccato E, Caneva P, Lamonaca D. Music therapy and cognitive rehabilitation: A pilot study. 6th European Music Therapy Congress. Jyväskylä, Finland, 2004.
Chambliss 1996 {published data only}
- Chambliss C, Tyson K, Tracy J. Performance on the purdue pegboard and finger tapping by schizophrenics after mellow and frenetic antecedent music. Perceptual and Motor Skills 1996b;83(3):1161‐2. [DOI] [PubMed] [Google Scholar]
Cook 1973 {published data only}
- Cook M, Freethy M. The use of music as a positive reinforcer to eliminate complaining behavior. Journal of Music Therapy 1973;10:213‐6. [Google Scholar]
de l'Etoile 2002 {published data only}
- l'Etoile SK. The effectiveness of music therapy in group psychotherapy for adults with mental illness. Arts in Psychotherapy 2002;29(2):69‐78. [Google Scholar]
Drury 1996 {published data only}
- Drury V. Cognitive therapy and recovery from acute psychosis: a randomised controlled trial. PhD dissertation submitted to the University of Birmingham 1999.
- Drury V, Birchwood M, Cochrane R, MacMillan F. Cognitive therapy and recovery from acute psychosis‐a controlled trial. I. Impact on psychotic symptoms. British Journal of Psychiatry 1996;169(5):593‐601. [DOI] [PubMed] [Google Scholar]
- Drury V, Birchwood M, Cochrane R, MacMillan F. Cognitive therapy and recovery from acute psychosis‐a controlled trial. II. Impact on recovery time. British Journal of Psychiatry 1996;169(5):602‐7. [DOI] [PubMed] [Google Scholar]
- Drury V, Brichwood M, Cochrane R. Cognitive therapy and recovery from acute psychosis: a controlled trial. 3. Five‐year follow‐up. British Journal of Psychiatry 2000;177:8‐14. [DOI] [PubMed] [Google Scholar]
Gaszner 2009 {published data only}
- Gaszner P. Complex therapy of schizophrenia [A szkizofrenia komplex terapiaja]. Neuropsychopharmacologia Hungarica 2009;11(1):41‐5. [PubMed] [Google Scholar]
Glicksohn 2000 {published data only}
- Glicksohn J, Cohen Y. Can music alleviate cognitive dysfunction in schizophrenia?. Psychopathology 2000;33:43‐7. [DOI] [PubMed] [Google Scholar]
Green 1987 {published data only}
- Green BL, Wehling C, Talsky GJ. Group art therapy as an adjunct to treatment for chronic outpatients. Hospital and Community Psychiatry 1987;38(9):988‐91. [DOI] [PubMed] [Google Scholar]
Grocke 2009a {published data only}
- Grocke D. The effect of group music therapy on quality of life for participants living with a severe and enduring mental illness. Journal of Music Therapy 2009;XLVI(2):90‐104. [DOI] [PubMed] [Google Scholar]
Grocke 2014 {published data only}
- Grocke D, Bloch S, Castle D, Thompson G, Newton R, Stewart S, et al. Group music therapy for severe mental illness: a randomized embedded‐ experimental mixed methods study. Acta Psychiatrica Scandinavica 2014;130(2):144‐53. [DOI] [PubMed] [Google Scholar]
Haimov 2012 {published data only}
- Haimov I, Bloch B, Reshef A, Vadas L, Kremer I. Effects of individualised acupuncture on sleep latency, anxiety and depression among hospitalised psychiatric patients. Journal of Sleep Research 2012:353.
Hannes 1974 {published data only}
- Hannes M, Siegel HD. The short term effect of socializing on performance of schizophrenics in recreational therapy. Journal of Community Psychology 1974;2(1):51‐3. [CN‐00239038] [Google Scholar]
Hayashi 2002 {published data only}
- Hayashi N, Tanabe Y, Nakagawa S, Noguchi M, Iwata C, Koubuchi Y, et al. Effects of group musical therapy on inpatients with chronic psychoses: A controlled study. Psychiatry and Clinical Neurosciences 2002;56(2):187‐93. [DOI] [PubMed] [Google Scholar]
Hodgson 1996 {published data only}
- Hodgson NS. The effects of music therapy on the attendance rate and number of verbal prompts given to elicit attendance of adult psychiatric clients in a day treatment center. Master's thesis. Tallahassee, FL: Florida State University, 1996. [Google Scholar]
Hogarty 1988 {published data only}
- Hogarty GE, McEvoy JP, Munetz M, DiBarry AL, Cather R, Cooley SJ, et al. Dose of fluphenazine, familial expressed emotion, and outcome in schizophrenia. Results of a two‐year controlled study. Archives of General Psychiatry. 1988;45(9):797‐805. [DOI] [PubMed] [Google Scholar]
Hu 2004 {published data only}
- Hu QL, Xue LH, Gao XH. Effect of music‐sport therapy on the insight and behavioral disturbance in patients with schizophrenia [chang gui ying yong yin yue ji ti yu liao fa gai shan jing shen fen lie zheng huan zhe zi zhi li he xing wei zhang ai de zuo yong]. Chinese Journal of Clinical Rehabilitation [Zhongguo lin chuang kang fu] 2004;8(9):1626‐7. [EMBASE: 2004336037] [Google Scholar]
Hustig 1990 {published data only}
- Hustig HH, Tran DB, Hafner RJ, Miller RJ. The effect of headphone music on persistent auditory hallucinations. Behavioural Psychotherapy 1990;18:273‐81. [Google Scholar]
Ji 2013 {published data only}
- Ji JY, Zhang YR. The impact of music therapy and group psychotherapy on psychotic symptoms and social functioning of patients with chronic schizophrenia [yin yue zhi liao he tuan ti xin lin zhi liao dui man xing jing shen fen lie huan zhe jing shen zheng zhuang ji she hui gong neng ying xiang de yan jiu]. Sichuan Mental Health 2013; Vol. 26, issue 1:19‐23.
Johnston 2002 {published data only}
- Johnston O, Gallagher AG, MsMahon PJ, King DJ. The efficacy of using a personal stereo to treat auditory hallucinations: Preliminary findings. Behavior Modification 2002;26(4):537‐49. [DOI] [PubMed] [Google Scholar]
Kallert 2004 {published data only}
- Kallert TW, Matthes C, Glöckner M, Eichler T, Koch R, Schützwohl M. Acute psychiatric day hospital treatment:is the effectiveness of this treatment approach still questionable? [Akutpsychiatrische tagesklinische Behandlung: Ein effektivitätsgesichertes Versorgungsangebot?]. Psychiatrische Praxis 2004;31(8):409‐19. [DOI] [PubMed] [Google Scholar]
Kong 2007 {published data only}
- Kong YL. The effects of music therapy on patients with chronic schizophrenia [yin yue zhi liao dui man xing jing shen fen lie huan zhe de kang fu xiao guo de yan jiu]. Shandong Archives of Psychiatry 2007;20(4):225‐6. [CHINESE: Academic Journals] [Google Scholar]
Krajewski 1993 {published data only}
- Krajewski C, Classen W, Boesken S. Comparison of art and cognitive therapy (IPT) with simultaneous cognitive and art therapy for schizophrenic patients regarding the change of cognitive processes. Pharmacopsychiatry 1993;26:171. [Google Scholar]
Leung 1998 {published data only}
- Leung CM, Lee G, Cheung B, Kwong E, Wing YK, Kan CS, et al. Karaoke therapy in the rehabilitation of mental patients. Singapore Medical Journal 1998;39(4):166‐8. [PubMed] [Google Scholar]
- Ng WF. Karaoke therapy in the rehabilitation of mental patients (SMJ vol 43 issue 12 December 2002). Singapore Medical Journal 2002;43(12):643; author reply 643‐4. [PubMed] [Google Scholar]
Li 2005 {published data only}
- Li M, Wang H, Li Z. Effect of music and sport therapy as assistant treatment for schizophrenia [yin yue ti yu liao fa dui man xing jing shen fen lie zheng de fu zhu zhi liao xiao guo]. Heilongjiang Nursing Journal 2005;11(20):1677‐8. [CAJ] [Google Scholar]
Li 2007b {published data only}
- Li GR, Tang JL, Zhu WR. The application of model Law in the long‐term management of hospitalized patients with schizophrenia [shi fan fa zai chang cheng zhu yuan jing shen fen lie zheng huan zhe guan li zhong de ying yong]. Chinese Journal of Rehabilitation Medicine 2007; Vol. 22, issue 12:1105‐6.
Li 2011 {published data only}
- Li JF, Zhang XY. The effects of music therapy on hospitalised patients with chronic schizophrenia: a randomised trial [yin yue zhi liao dui man xing jing shen fen lie zheng zhu yuan huan zhe liao xiao de dui zhao yan jiu]. National Medicine 2011; Vol. 23, issue 19:2459‐60.
Lin 2003 {published data only}
- Xiao LL. The effect of music therapy on the recovery stage of different types of psychotic patients [yin yue zhi liao dui hui fu qi bu tong lei xing jing shen bing huan zhe liao xiao de yan jiu]. Journal of the Gannan Medical College 2003;23(2):183‐4. [Google Scholar]
Luo 2014 {published data only}
- Luo C, Yao DZ. The study of the brain network features in refractory schizophrenia [nan zhi xing jing shen fen lie zheng ji qi MECT zhi liao de nao wang luo te zheng yan jiu]. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=ChiCTR‐OPC‐14005339 2014.
Margo 1981 {published data only}
- Margo A, Hemsley DR, Slade PD. The effects of varying auditory input on schizophrenic hallucinations. British Journal of Psychiatry 1981;139:122‐7. [DOI] [PubMed] [Google Scholar]
Martinez 2005 {published data only}
- Martinez LRD, Soto HO, Guerrero CL, Verdugo SR, Gasca LR, Collazos MV, et al. A comprehensive rehabilitation for people with schizophrenia in Mexico: The model of the national psychiatry institute Ramón de la Fuente, group III [La rehabilitación integral del paciente esquizofrénico en México: El modelo del instituto nacional de psquiatria Ramón de la Fuente, grupo III]. Salud Mental 2005;28(6):9‐19. [Google Scholar]
McInnis 1990 {published data only}
- McInnis M, Marks I. Audiotape therapy for persistent auditory hallucinations. British Journal of Psychiatry 1990;157:913‐4. [DOI] [PubMed] [Google Scholar]
Meschede 1983 {published data only}
- Meschede HG, Bender W, Pfeiffer H. Music therapy with psychiatric problem patients [Musiktherapie mit psychiatrischen Problempatienten]. Psychotherapie, Psychosomatik, Medizinische Psychologie 1983;33(3):101‐6. [PubMed] [Google Scholar]
Metzner 2010 {published data only}
- Metzner S. About being meant: Music therapy with an in‐patient suffering from psychosis. Nordic Journal of Music Therapy 2010;19(2):133‐50. [Google Scholar]
Moe 2000 {published data only}
- Moe T, Roesen A, Raben H. Restitutional factors in group music therapy with psychiatric patients based on a modification of guided imagery and music (GIM). Nordic Journal of Music Therapy 2000;9(2):36‐50. [Google Scholar]
Morgan 2011 {published data only}
Muller 2014 {published data only}
- Muller W, Haffelder G, Schlotmann A, Schaefers AT, Teuchert‐Noodt G. Amelioration of psychiatric symptoms through exposure to music individually adapted to brain rhythm disorders ‐ a randomised clinical trial on the basis of fundamental research. Cognitive Neuropsychiatry 2014; Vol. 19, issue 5:399‐413. [DOI] [PubMed]
Murow 1997 {published data only}
- Murow E, Unikel C. Music therapy and body expression therapy in the rehabilitation of patients with chronic schizophrenia [La musicoterapia y la terapia de expresión corporal en la rehabilitación del paciente con esquizofrenia crónica]. Salud Mental 1997;20(3):35‐40. [Google Scholar]
Na 2009 {published data only}
- Na HJ, Yang S. Effects of listening to music on auditory hallucination and psychiatric symptoms in people with schizophrenia. Journal of Korean Academy of Nursing 2009;39(1):62‐71. [DOI] [PubMed] [Google Scholar]
Nelson 1991 {published data only}
- Nelson HE, Thrasher S, Barnes TRE. Practical ways of alleviating auditory hallucinations. BMJ 1991;302(6772):327. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ni 2002 {published data only}
- Ni JZ, Liu YR. Analysis of music therapy effect on patient with chronic schizophrenia [yin yue liao fa zhi liao jing shen fen lie zheng liao xiao fen xi]. Health Psychology Journal 2002;10(2):145‐6. [CBM: (Chinese Biomedical Literature); CAJ] [Google Scholar]
Offer 1960 {published data only}
Olbrich 1990 {published data only}
- Olbrich R, Mussgay L. Reduction of schizophrenic deficits by cognitive training: an evaluative study. European Archives of Psychiatry & Neurological Sciences 1990;239(6):366‐9. [MEDLINE: ; CN‐00069945] [DOI] [PubMed] [Google Scholar]
Pavlicevic 1994 {published data only}
- Pavlicevic M, Trevarthen C, Duncan J. Improvisational music therapy and the rehabilitation of persons suffering from chronic schizophrenia. Journal of Music Therapy 1994;31(2):88‐104. [Google Scholar]
Pfeiffer 1987 {published data only (unpublished sought but not used)}
- Pfeiffer H, Wunderlich S, Bender W, Elz U, Horn B. Music improvisation with schizophrenic patients ‐ a controlled study in the assessment of therapeutic effects [Freie Musikimprovisation mit schizophrenen Patienten ‐ kontrollierte Studie zur Untersuchung der therapeutischen Wirkung]. Die Rehabilitation 1987;26(4):184‐92. [PubMed] [Google Scholar]
Pierce 2004 {published data only}
- Pierce JW. The effect of music therapy and psychoeducation versus psychoeducation for mainstreaming mental health patients into society [Thesis]. Florida: University of Florida, 2004. [Google Scholar]
Reker 1991 {published data only}
- Reker T. Music therapy evaluated by schizophrenic patients. Psychiatrische Praxis 1991;18(6):216‐21. [PubMed] [Google Scholar]
Schmuttermayer 1983 {published data only}
- Schmuttermayer R. Possibilities for inclusion of group music therapeutic methods in the treatment of psychotic patients [Möglichkeit der Einbeziehung gruppentherapeutischer Methoden in die Behandung von Psychotikern]. Psychiatrie, Neurologie und Medizinische Psychologie 1983;35(1):49‐53. [PubMed] [Google Scholar]
Silverman 2003a {published data only}
- Silverman MJ. Contingency songwriting to reduce combativeness and non‐cooperation in a client with schizophrenia: A case study. The Arts in Psychotherapy 2003a;30(1):25‐33. [Google Scholar]
Silverman 2009 {published data only}
- Silverman MJ. The effect of single‐session psychoeducational music therapy on verbalizations and perceptions in.psychiatric patients. Journal of Music Therapy 2009;46(2):105‐31. [DOI] [PubMed] [Google Scholar]
Silverman 2011a {published data only}
Silverman 2011b {published data only}
Silverman 2011c {published data only}
- Silverman MJ. Effects of music therapy on psychiatric patients' proactive coping skills: two pilot studies. Arts in Psychotherapy 2011; Vol. 38, issue 2:125‐9.
Silverman 2013 {published data only}
- Silverman MJ. Effects of music therapy on self‐ and experienced stigma in patients on an acute care psychiatric unit: a randomized three group effectiveness study. Archives of Psychiatric Nursing 2013;27:223–30. [DOI] [PubMed] [Google Scholar]
Silverman 2014a {published data only}
- Silverman MJ. Effects of a live educational music therapy intervention on acute psychiatric inpatients’ perceived social support and trust in the therapist: a four‐group randomized effectiveness study. Journal of Music Therapy 2014;51(3):228–49. [DOI] [PubMed] [Google Scholar]
Silverman 2014b {published and unpublished data}
- Silverman, MJ. Effects of family‐based educational music therapy on acute care psychiatric patients and their family members: an exploratory mixed‐methods study. Nordic Journal of Music Therapy 2014;23(2):99‐122. [Google Scholar]
Silverman 2016 {published data only}
- Silverman MJ. Effects of educational music therapy on illness management knowledge and mood state in acute psychiatric inpatients: a randomized three group effectiveness study. Nordic Journal of Music Therapy 2016;25(1):57‐75. [DOI: 10.1080/08098131.2015.1008559] [DOI] [Google Scholar]
Skelly 1952 {published data only}
- Skelly CG, Haslerud GM. Music and the general activity of apathetic schizophrenics. Journal and the General Activity of Apathetic Schizophrenics 1952;47:188‐92. [DOI] [PubMed] [Google Scholar]
Song 1994 {published data only}
- Song Y, Cheng X, Fan Z. An analysis of effects of operative music therapy on emotion and social interaction of patients with chronic schizophrenia. Chinese Journal of Rehabilitation 1994;9(4):178‐9, 180‐1. [Google Scholar]
Steinberg 1991 {published data only}
- Steinberg R, Kimming V, Raith L, Gunther W, Bogner J, Timmermann T. Music psychopathology: the course of musical expression during music therapy with psychiatric inpatients. Psychopathology 1991;24:121‐9. [DOI] [PubMed] [Google Scholar]
Su 1999 {published data only}
- Su L, Fan Z, Qu Y. The effect of dance therapy for chronic schizophrenic patient [dui man xing jing shen bing huan zhe fu yi wu dao zhi liao de liao xiao guan cha]. Chinese Journal of Psychiatry 1999;32(3):167‐9. [Google Scholar]
Su 2005 {published data only}
- Su H, Zhang HD, Du XS. The synergistic effects of comprehensive rehabilitation on the negative symptoms of patients with schizophrenia [zong he xing kang fu zhi liao dui man xing fen lie zheng yin xing zheng zhuang de zeng xiao zuo yong]. Sichuan Mental Health 2005;18(3):172‐3. [CAJ] [Google Scholar]
Tan 2009 {published data only}
- Tan S, Yizhuang Z. Computerized cognitive remediation therapy for patients with schizophrenia, a multicenter randomized controlled study. ChiCTR‐TRC‐00000249.
Tang 2002 {published data only}
- Tang HYi, Zhang XY, Wu LM. The comparison study of brain function curer as a adjuvant therapy for schizophrenia patients [nao gong neng bao jian yi fu zhu zhi liao jing shen fen lie zheng de dui zhao yan jiu]. Chinese Journal of Nervous and Mental Diseases 2002;28(1):53‐4. [Google Scholar]
Thaut 1989 {published data only}
- Thaut MH. The influence of music therapy interventions on self‐rated changes in relaxation, affect, and thought in psychiatric prisoner‐patients. Journal of Music Therapy 1989;26:155‐66. [Google Scholar]
Troice 2003 {published data only}
- Troice EM, Sosa JJS. The musical experience as a curative factor in music therapy with patients with chronic schizophrenia. Salud Mental 2003;26(4):47‐58. [Google Scholar]
Vadas 2012 {published data only}
- Vadas L, Bloch B, Reshef A, Kremer I, Haimov I. The effects of acupuncture on sleep quality and emotional measures among psychiatric ward inpatients. Journal of Molecular Neuroscience 2012; Vol. 48:S119.
Valencia 2006 {published data only}
- Valencia M, Murow E, Rascón ML. Comparison of three methods of intervention in schizophrenia: psychosocial therapy, music therapy, and multiple therapies. [Comparación de tres modalidades de intervención en esquizofrenia: terapi psicosocial, musicoterapia y terapias múltiples]. Revista Latinoamericana de Psicologia 2006;38(3):535‐49. [Google Scholar]
Wahass 1997 {published data only}
- Wahass S, Kent G. The modification of psychological interventions for persistent auditory hallucinations to an Islamic culture. Behavioural and Cognitive Psychotherapy 1997;25:351‐64. [Google Scholar]
Wang 2002a {published data only}
- Wang H, Wang D, Zhou XH. The observation of the effect of music therapy on 50 chronic schizophrenia patients. [yin yue zhi liao dui 50 li man xing jing shen fen lie zheng de kang fu xiao guo guan cha]. Harbin Medical Journal 2002;22(1):33‐4. [Google Scholar]
Wang 2002b {published data only}
- Wang Aw, Shi F, Dong X. Influence of traditional pentatonic music on brain electrical activity mapping of schizophrenics [wu yin yue qu dui jing shen fen lie zheng nao dian huo dong de ying xiang]. Chinese Mental Health Journal 2002;16(7):494‐5. [Google Scholar]
Wang 2005 {published data only}
- Wang Yi‐Yun, Wang Qiu‐Yan, Cheng Ai‐Ping, Li Shui‐Xiang. The effects of music therapy on the rehabilitation of patients with chronic schizophrenia [yin yue liao fa zai man xing jing shen fen lie zheng kang fu zhi liao zhong de zuo yong]. Journal of Qiqihar Medical 2005;26(9):1011‐2. [CAJ] [Google Scholar]
- Wang Yi‐Yun, Wang Qiu‐Yan, Cheng Ai‐Ping, Li Shui‐Xiang. The effects of music therapy on the rehabilitation of patients with chronic schizophrenia [yin yue liao fa zai man xing jing shen fen lie zheng kang fu zhi liao zhong de zuo yong]. Chinese Journal of Behavioral Medical Science 2005;14(9):810. [Google Scholar]
Wang 2006 {published data only}
- Wang HM, Zhang DM. The influence of music therapy on patients' social function with chronic schizophrenia [yin yue liao fa dui man xing jing shen fen lie huan zhe de she hui gong neng de ying xiang]. Practice Nursing Care and Study Journal 2006;3(1):7‐8. [Google Scholar]
Wang 2007 {published data only}
- Wang Z, Li X. Comparative study of the music therapy on the negative symptoms of schizophrenia with native risperidone [yin yue zhi liao he bing guo chan li pei tong zhi liao jing shen fen lie zheng yin xing zheng zhuang dui zhao yan jiu]. Chinese Journal of Health Psychology 2007;15(2):155‐6. [CHINESE: Academic Journals] [Google Scholar]
Warren 1980 {published data only}
- Warren J. Paried‐associate learning in chronic institutionalised subjects using synthesized sounds, nonsense syllables, and rhythmic sounds. Journal of Music Therapy 1980;17(1):16‐25. [Google Scholar]
Wu 2000 {published data only}
- Wu LR. The effect of musical therapy on chronic schizophrenics rehabilitation [yin yue liao fa zai man xing jing shen fen lie zheng kang fu zhi liao zhong de zuo yong]. Modern Rehabilitation 2000;4(4):550‐1. [Google Scholar]
Wu 2003 {published data only}
- Wu Y, Zhao F. Effect of music and dance on recovery of schizophrenia [yin yue wu dao dui jing shen fen lie zheng kang fu de ying xiang]. Health Psychology Journal 2003;11(3):207‐8. [Google Scholar]
Xiao 2005 {published data only}
- Xiao LR, Pei XY, Wang CY. The effect factors of rehabilitation measures on the self‐managing ability and social ability of patients with schizophrenia. [yin xing jing shen fen lie huan zhe zi li he she hui neng li hui fu cuo shi ji ying xiang yin su]. Chinese Journal of Clinical Rehabilitation 2005;9(20):225. [CAJ] [Google Scholar]
Yang 2005 {published data only}
- Yang RL, Lv HX, Lou F. The effect of group psychotherapy on the recovery of patients with chronic schizophrenia [xin li xiao zu zhi liao de man xing jing shen fen lie zheng huan zhe de kang fu zuo yong]. Occupation and Health 2005;21(6):936. [CAJ] [Google Scholar]
Zhang 2003a {published data only}
- Zhang ML. The effect of active and receptive music therapy on patients with chronic schizophrenia [zhu bei dong yin yue zhi liao dui man xing jing shen fen lie zheng liao xiao fen xi]. Health Psychology Journal 2003;11(5):370‐1. [Google Scholar]
Zhang 2003b {published data only}
- Zhang Y. Effect of music therapy and behavioral therapy on schizophrenia patients. China Clinical Rehabilitation 2003;7(5):857. [Google Scholar]
Zhang 2005 {published data only}
- Zhang HJ. The effects of music therapy and physiotherapy on the negative symptoms of schizophrenia [yin ti liao fa dui jing shen fen lie yin xing zheng zhuang huan zhe de ying xiang]. Practical Journal of Medicine and Pharmacy 2005;22(9):832. [CAJ] [Google Scholar]
Zhang 2010 {published data only}
- Zhang HQ, Ma XJ, Zhao LL, Feng B, Tang ZS. The effects of music therapy in combination with electric convulsive treatment for patients with refractory schizophrenia [yin yue zhi liao lian he wu chou chu dian xiu ke zhi liao nan zhi xing jing shen fen lie zheng liao xiao fen xi]. China Practical Medicine 2010; Vol. 5, issue 32:212‐3.
Zhang 2013 {published data only}
- Zhang GP. The effects of behavioral modification training and music therapy on improving symptoms and social life function in patients with chronic schizophrenia [xing wei jiao zhi xun lian lian he yin yue zhi liao dui man xing jing shen fen lie huan zhe ji she hui sheng huo gong neng de gai shan zuo yong]. Practical Cardio‐Cerebral Pulmonary Vascular Disease 2013; Vol. 21, issue 9:85‐6.
Zhao 2013 {published data only}
- Zhao SQ, Wang JY, Li YF, L R, Liu J. The application of music appreciation for patients with schizoprenia in early rehabilitation [yin yue shang xi zai jing shen fen lie zheng zao qi kang fu zhi liao zhong de ying yong]. China Practical Medicine 2013; Vol. 8, issue 10:201‐2.
Zhou 2003 {published data only}
- Zhou B, Xu XB, Yang GZ. The effect of music therapy on the negative symptoms of patients with schizophrenia [yin yue liao fa dui jing shen fen lie zheng yin xing zheng zhuang de liao xiao fen xi]. Ningxia Medical Journal 2003;25(4):247‐8. [Google Scholar]
Zhou 2006 {published data only}
- Zhou YP, Shou YQ, Tang WZ. Comparative study of the rehabilitative effect of different types of receptive music therapy on patients with schizophrenia [bu tong gan shou shi yin yue liao fa dui jing shen fen lie zheng huan zhe de kang fu zuo yong]. Shanghai Nursing Journal 2006;6(6):12‐4. [Google Scholar]
Zhu 2002 {published data only}
- Zhu Y, Jin X. Effect of music treatment on memory decrease of patients with schizophrenia caused by clozapine [yin yue zhi liao mu dan ping suo zhi ji yi li xia jiang de dui zhao yan jiu]. Chinese Journal of Rehabilitation Theory and Practice 2002;8(11):684‐6. [CAJ; CBM] [Google Scholar]
Zincir 2011 {published data only}
- Zincir SB, Semiz UB, Yenel A, Basotlu E, Bilici M, Tulay C. Effects of group musical therapy on inpatients with schizophrenia: a preliminary study. Klinik Psikofarmakoloji Bulteni 2011:S191.
Additional references
Addington 1992
- Addington D, Addington J, Maticka‐Tyndale E, Joyce J. Reliability and validity of a depression rating scale for schizophrenics. Schizophrenia Research 1992;6:201‐8. [DOI] [PubMed] [Google Scholar]
Allison 2002
- Allison PD. Missing Data. Series: Quantitative Applications in the Social Sciences. Thousand Oaks, CA: Sage, 2002. [Google Scholar]
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313(7066):1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andreasen 1982
- Andreasen NC. Negative symptoms in schizophrenia: Definition and reliability. Archives of General Psychiatry 1982;39:784‐8. [DOI] [PubMed] [Google Scholar]
Andreasen 1984
- Andreasen NC. Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, IA, University of Iowa 1984.
Andritzky 1996
- Andritzky W. Alternative treatment in psychiatric and psychotherapy facilities in Germany [Unkonventionelle Heilweisen in psychiatrischen und psychosomatischen Kliniken in Deutschland]. Gesundheitswesen 1996;58(1):21‐30. [PubMed] [Google Scholar]
Ansdell 2010a
- Ansell G, Davidson J, Magee WL, Meehan J, Procter S. From "This F***ing life" to "that's better"...in four minutes: an interdisciplinary study of music therapy's "present moments" and their potential for affect modulation. Nordic Journal of Music Therapy 2010;19(1):3‐28. [Google Scholar]
Ansdell 2010b
- Ansdell G, Meehan J. "Some light at the end of the tunnel": Exploring users' evidence for the effectiveness of music therapy in adult mental health settings. Music and Medicine 2010;2(1):29‐40. [Google Scholar]
APA 2013
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM‐5). 5th Edition. Arlington, VA: American Psychiatric Association, 2013. [Google Scholar]
Atkinson 1994
- Atkinson C, Greenfield T. Client Satisfaction Questionnaire ‐ 8 and Service Satisfaction Scale 30. Psychological Testing: Treatment Planning and Outcome Assessment. San Francisco, CA: Lawrence Erlbaum, 1994. [Google Scholar]
Berg 1948
- Berg EA. A simple objective technique for measuring flexibility in thinking. Journal of General Psychology 1948;39:15‐22. [DOI] [PubMed] [Google Scholar]
Bland 1997
- Bland JM. Statistics notes. Trials randomised in clusters. BMJ 1997;315:600. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boissel 1999
- Boissel JP, Cucherat M, Li W, Chatellier G, Gueyffier F, Buyse M, et al. The problem of therapeutic efficacy indices. 3. Comparison of the indices and their use [Apercu sur la problematique des indices d'efficacite therapeutique, 3: comparaison des indices et utilisation. Groupe d'Etude des Indices D'efficacite]. Therapie 1999;54(4):405‐11. [PUBMED: 10667106] [PubMed] [Google Scholar]
Boutron 2008
- Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Annals of Internal Medicine 2008;148(4):295‐309. [DOI] [PubMed] [Google Scholar]
Bruscia 1998
- Bruscia KE. Defining Music Therapy. 2nd Edition. Gilsum, NH: Barcelona Publishers, 1998. [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd Edition. Hillsdale, NJ: Lawrence Erlbaum, 1988. [Google Scholar]
Davey Smith 1997
- Davey Smith G, Egger M. Meta‐analyses of randomised controlled trials. Lancet 1997;350(9085):1182. [DOI] [PubMed] [Google Scholar]
Deeks 2000
- Deeks J. Issues in the selection for meta‐analyses of binary data. Proceedings of the 8th International Cochrane Colloquium; 2000 Oct 25‐28; Cape Town. Cape Town: The Cochrane Collaboration, 2000.
Divine 1992
- Divine GW, Brown JT, Frazier LM. The unit of analysis error in studies about physicians' patient care behavior. Journal of General Internal Medicine 1992;7(6):623‐9. [DOI] [PubMed] [Google Scholar]
Donner 2002
- Donner A, Klar N. Issues in the meta‐analysis of cluster randomized trials. Statistics in Medicine 2002;21:2971‐80. [DOI] [PubMed] [Google Scholar]
Duggan 2005
- Duggan L, Fenton M, Rathbone J, Dardennes R, El‐Dosoky A, Indran S. Olanzapine for schizophrenia. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD001359.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne D, Altman DG, Higgins JPT, Curtina F, Worthingtond HV, Vaile A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [DOI] [PubMed] [Google Scholar]
Fazio 1977
- Fazio AF. A concurrent validational study of the NCHS General Well‐Being Schedule. National Center for Health Statistics. Hyattsville, MD, 1977. [PubMed]
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta‐analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59(7):7‐10. [DOI] [PubMed] [Google Scholar]
Gold 2004
- Gold C. The use of effect sizes in music therapy research. Music Therapy Perspectives 2004;22(2):91‐5. [Google Scholar]
Gold 2009
- Gold C, Solli HP, Krüger V, Lie SA. Dose‐response relationship in music therapy for people with serious mental disorders: Systematic review and meta‐analysis. Clinical Psychology Review 2009;29(3):193‐207. [DOI] [PubMed] [Google Scholar]
Gronwall 1977
- Gronwall MD. Paced auditory serial‐addition task: a measure of recovery from concussion. Perceptual & Motor Skills 1977;44:367‐73. [DOI] [PubMed] [Google Scholar]
Gulliford 1999
- Gulliford MC. Components of variance and intraclass correlations for the design of community‐based surveys and intervention studies: data from the Health Survey for England 1994. American Journal of Epidemiology 1999;149:876‐83. [DOI] [PubMed] [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry 1960;23:56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamilton 2000
- Hamilton M. Hamilton Rating Scale for Depression (Ham‐D). In: American Psychiatric Association, editor(s). Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
Heaton 1993
- Heaton R. Wisconsin Card Sorting Test Manual, Revised and Expanded. Psychological Assessment Resources, Inc.. Odessa, FL, 1993.
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester, UK: Wiley‐Blackwell, 2008. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org..
Honigfeld 1965
- Honigfeld G, Gillis RD, Klett CJ. Nurses' observation scale for inpatient evaluation: a new scale for measuring improvement in chronic schizophrenia. Journal of Clinical Psychology 1965;21:65‐71. [DOI] [PubMed] [Google Scholar]
Jauhar 2015
- Jauhar S, McKenna PJ, Radua J, Fung E, Salvador R, Laws KR. Cognitive‐behavioural therapy for the symptoms of schizophrenia: systematic review and meta‐analysis with examination of potential bias. British Journal of Psychiatry 2015;204:20‐9. [DOI] [PubMed] [Google Scholar]
Jones 2012
- Jones C, Hacker D, Cormac I, Meaden A, Irving CB. Cognitive behaviour therapy versus other psychosocial treatments for schizophrenia. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD008712.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kay 1986
- Kay SR, Opler LA, Fiszbein A. Positive and Negative Syndrome Scale (PANSS) Manual. North Tonawanda, NY: Multi‐Health Systems, 1986. [Google Scholar]
Kay 1987
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin 1987;13(2):261‐76. [DOI] [PubMed] [Google Scholar]
Lawton 1969
- Lawton MP, Brody EM. Assessment of older people: Self‐maintaining and instrumental activities of daily living. Gerontologist 1969;9(3):179‐86. [PubMed] [Google Scholar]
Lee 2001
- Lee S. From diversity to unity. The classification of mental disorders in 21st‐century China. Psychiatric Clinics of North America 2001;24(3):421‐31. [DOI] [PubMed] [Google Scholar]
Leucht 2005
- Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean?. Schizophrenia Research 2005;79(2‐3):231‐8. [PUBMED: 15982856] [DOI] [PubMed] [Google Scholar]
Leucht 2005a
- Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. Clinical implications of brief psychiatric rating scale scores. British Journal of Psychiatry 2005;187:366‐71. [PUBMED: 16199797] [DOI] [PubMed] [Google Scholar]
Leucht 2007
- Leucht S, Engel RR, Bauml J, Davis JM. Is the superior efficacy of new generation antipsychotics an artifact of LOCF?. Schizophrenia Bulletin 2007;33(1):183‐91. [PUBMED: 16905632] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maranto 1993
- Maranto CD. Music Therapy: International Perspectives. Pipersville, PA: Jeffrey, 1993. [Google Scholar]
Marshall 2000
- Marshall M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry 2000;176:249‐52. [DOI] [PubMed] [Google Scholar]
Miyar 2012
- Miyar J, Adams CE. Content and quality of 10 000 controlled trials in schizophrenia over 60 years. Schizophrenia Bulletin 2012;39(1):226‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2010
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c689. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mössler 2011a
- Mössler K. “I am a psychotherapeutically oriented music therapist.” Theory construction and its influence on professional identity formation under the example of the Viennese School of Music Therapy. Nordic Journal for Music Therapy 2011;20(2):155‐84. [Google Scholar]
Nelson 1976
- Nelson HE. A modified card sorting test sensitive to frontal lobe defects. Cortex 1976;12:313‐24. [DOI] [PubMed] [Google Scholar]
Oerter 2001
- Oerter U, Scheytt‐Holzer N, Kächele H. Music therapy in psychiatry: State of implementation and of research [Musiktherapie in der Psychiatrie: Versorgungslage und Stand der Forschung]. Nervenheilkunde 2001;20(8):428‐33. [Google Scholar]
Okpokoro 2014
- Okpokoro U, Adams CE, Sampson S. Family intervention (brief) for schizophrenia. Cochrane Database of Systematic Reviews 2014, Issue 3. [DOI: 10.1002/14651858.CD009802.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Overall 1962
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychological Reports 1962;10:799‐812. [Google Scholar]
Overall 1988
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale (BPRS): recent developments in ascertainment and scaling. Psychopharmacology Bulletin 1988;24:97‐9. [PubMed] [Google Scholar]
Pharoah 2010
- Pharoah F, Mari JJ, Rathbone J, Wong W. Family intervention for schizophrenia. Cochrane Database of Systematic Reviews 2010, Issue 12. [DOI: 10.1002/14651858.CD000088.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ren 2013
- Ren J, Xia J. Dance therapy for schizophrenia. Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD006868.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rolvsjord 2001
- Rolvsjord R. Sophie learns to play her songs of tears: A case study exploring the dialectics between didactic and psychotherapeutic music therapy practices. Nordic Journal of Music Therapy 2001;10(1):77‐85. [Google Scholar]
Rosvold 1956
- Rosvold HE, Mirsky AF, Sarason I, Bransome ED, Beck LH. A continuous performance test of brain damage. Journal of Consulting and Clinical Psychology 1956;20:343‐50. [DOI] [PubMed] [Google Scholar]
Ruddy 2005
- Ruddy R, Milnes D. Art therapy for schizophrenia or schizophrenia‐like illnesses. Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI: 10.1002/14651858.CD003728.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ruddy 2007
- Ruddy R, Dent‐Brown K. Drama therapy for schizophrenia or schizophrenia‐like illnesses. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD005378.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saggino 1983
- Saggino A. Literature review on the Wechsler Memory Scale as a clinical and research tool. [Rassegna della letterature sulla Wechsler Memory Scale come strumento clinico e di ricerca]. Bollettino di Psicologia Applicata 1983;165:37‐44. [Google Scholar]
Sarason 1983
- Sarason IG, Levine HM, Basham RB. Assessing social support: The Social Support Questionnaire. Journal of Personality and Social Psychology 1983;44:127‐39. [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Silverman 2003b
- Silverman MJ. The influence of music on the symptoms of psychosis: A meta‐analysis. Journal of Music Therapy 2003b;40(1):27‐40. [DOI] [PubMed] [Google Scholar]
Solli 2008
- Solli HP. "Shut up and play!" Improvisational use of popular music for a man with schizophrenia. Nordic Journal of Music Therapy 2008;17(1):67‐77. [Google Scholar]
Spitzer 2000
- Spitzer RL, Gibbon M, Endicott J. Global assessment scale (GAS), global assessment of functioning (GAF) scale, social and occupational functioning assessment scale (SOFAS). In: American Psychiatric Association, editor(s). Handbook of Psychiatric Measures. Washington, DC: American Psychiatric Association, 2000. [Google Scholar]
Stern 2010
- Stern D. The issue of vitality. Nordic Journal of Music Therapy 2010;19(2):88‐102. [Google Scholar]
Tombaugh 2006
- Tombaugh TN. A comprehensive review of the Paced Auditory Serial Addiction Test (PASAT). Archives of Clinical Neuropsychology 2006;21:53‐76. [DOI] [PubMed] [Google Scholar]
Trevarthen 2000
- Trevarthen C, Malloch S. The dance of wellbeing: defining the musical therapeutic effect. Nordic Journal of Music Therapy 2000;9(2):3‐17. [Google Scholar]
Tönnies 1996
- Tönnies S, Plöhn S, Krippendorf U. Skalen zur psychischen Gesundheit. Heidelberg, Germany: Roland Asanger Verlag, 1996. [Google Scholar]
Ukoumunne 1999
- Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area‐wide and organisation‐based intervention in health and health care: a systematic review. Health Technology Assessment 1999;3(5):1‐75. [PubMed] [Google Scholar]
Wigram 1999
- Wigram T, Backer J. Clinical Applications of Music Therapy in Psychiatry. London: Jessica Kingsley Publishers, 1999. [Google Scholar]
Wigram 2002
- Wigram T. Indications in music therapy: Evidence from assessment that can identify the expectations of music therapy as a treatment for autistic spectrum disorder (ASD). Meeting the challenge of evidence based practice. British Journal of Music Therapy 2002;16(1):5‐28. [Google Scholar]
Wu 1998
- Wu WY. Social Disability Screening Schedule‐Chinese version. In: Zhang MY editor(s). Handbook of Rating Scales in Psychiatry. Changsha: Hunan Science and Technology Press, 1998:163‐6. [Google Scholar]
Xia 2009
- Xia J, Adams CE, Bhagat N, Bhagat V, Bhoopathi P, El‐Sayeh H, et al. Loss to outcomes stakeholder survey: the LOSS study. Psychiatric Bulletin 2009;33(7):254‐7. [Google Scholar]
Xu 1986
- Xu SL, Wu ZY. The construction of the Clinical Memory Test. Acta Psychologica Sinica 1986;18(1):100‐8. [Google Scholar]
Zhang 2003
- Zhang MY. Mental Assessment Manual (jing shen ping ding shou ce). Human Scientific and Technical Publishers, 2003:35‐9. [Google Scholar]
References to other published versions of this review
Gold 2003
- Gold C, Bentley K, Wigram T. Music therapy for schizophrenia and schizophrenia‐like illnesses. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD004025] [DOI] [PubMed] [Google Scholar]
Gold 2005a
- Gold C, Heldal TO, Dahle T, Wigram T. Music therapy for schizophrenia or schizophrenia‐like illnesses. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD004025.pub2] [DOI] [PubMed] [Google Scholar]
Mössler 2011b
- Mössler K, Chen X, Heldal TO, Gold C. Music therapy for people with schizophrenia and schizophrenia‐like disorders. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD004025.pub3] [DOI] [PubMed] [Google Scholar]


