Abstract
Excess mortality can be caused by extreme hot weather events, which are increasing in severity and frequency in Canada due to climate change. Individual and social vulnerability factors influence the mortality risk associated with a given heat exposure. We constructed heat vulnerability indices using census data from 2006 and 2011 in Canada, developed a novel design to compare spatiotemporal changes of heat vulnerability, and identified locations that may be increasingly vulnerable to heat. The results suggest that 1) urban areas in Canada are particularly vulnerable to heat, 2) suburban areas and satellite cities around major metropolitan areas show the greatest increases in vulnerability, and 3) heat vulnerability changes are driven primarily by changes in the density of older ages and infants. Our approach is applicable to heat vulnerability analyses in other countries.
Keywords: heat vulnerability, spatiotemporal modelling, climate change, demographic change, regional planning, urbanization
Introduction
Climate change is influencing the severity and frequency of heat waves in cities throughout the world (Meehi and Tebaldi, 2004, Murray & Ebi, 2012; IPCC, 2009; IPCC, 2011; Reid et al., 2009), which can in turn lead to increasing heat-related morbidity and mortality, especially during extreme heat events (Basu, 2009). Extreme heat events and the associated excess mortality are worldwide phenomena that are occurring in the tropics (Yan, 2000), subtropics (Huang et al., 2010), and temperate climate zones, including Western Europe in 2003 (Filleul et al., 2006) and major cities in Canada in 2009 and 2010 (Bustinza et al., 2013; Kosatsky et al., 2012). In order to address related public health impacts, previous studies have estimated either the spatial or temporal variability of heat-related illness/mortality (Anderson and Bell, 2010; Eisenman et al., 2016; Hattis et al., 2012; Henderson et al., 2013; Hondula et al., 2012; Jones et al., 1982; Kovach et al., 2015; Laaidi et al., 2012; Rosenthal et al., 2014; Son et al., 2012a; Son et al., 2012b; Vaneckova et al., 2010), and developed indices to locate the heat-vulnerable populations (Reid et al., 2009; Reid et al., 2012; Rinner et al., 2010; Vescovi et al., 2005).
Although previous studies have developed approaches for heat health vulnerability assessments (Chan et al. 2012; Hondula et al., 2012; Rinner et al., 2010; Tomlinson et al., 2011), most research only isolated either the spatial or the temporal vulnerability to investigate heat risk trends (Anderson and Bell, 2010; Hattis et al., 2012; Hondula et al., 2012; Tomlinson et al., 2011) but did not attempt to estimate spatio-temporally changing vulnerability for health planning based on historical datasets. Doing so will allow targeted adaptation efforts in not only the areas that are vulnerable now, but also in those areas where vulnerability is likely to rise. It is important to combine both spatial and temporal trends to investigate how changing populations in communities may influence heat vulnerability in the future (Sheridan & Dixon, 2016), and ultimately combine the resulting information with climate projections (also stated in Health Canada guideline for extreme heat and health vulnerability assessment) to facilitate extreme heat adaptation (Goldberg et al., 2007; Gosling et al., 2009; Huang et al., 2011; Jackson et al., 2010; Jeong et al., 2016). While ambient temperature largely determines the heat exposure of a population, vulnerability defines how that population is affected by the exposure, which during extreme heat events may lead to substantial excess mortality (Ho et al., 2017; Toloo et al., 2014). The relationship between heat exposure, vulnerability and risk is complicated by both short- and long-term acclimatization, as evidenced by latitudinal gradients in the temperature-mortality relationship (Henderson et al. 2013, Anderson and Bell 2009), and also by societal responses to heat such as heat emergency warning systems (Kalkstein & Sheridan, 2007; Toloo et al., 2013; Toloo et al., 2014; Tong et al., 2016). Nevertheless, quantifying spatiotemporal change in vulnerability and identifying the spatial clusters based on temporal vulnerability change could help estimating heat-related mortality or morbidity during future extreme heat events (Chow et al., 2012), especially because socio-economic vulnerability factors are substantially more important than environmental exposure levels in determining the local spatial distribution of health risk (Adger, 2006; INVS 2004; Füssel & Klein, 2006; Toloo, et al., 2013), and heat exposure is largely constrained by urban morphology and land cover (Gago et al., 2013). Most heat-related mortality does not occur in the general population, but rather in specific population groups that have elevated vulnerability due to a variety of personal, socio-economic, infrastructural or environmental factors (Reid et al., 2009; Tomlinson et al., 2011; Yardley et al., 2011). Understanding the spatiotemporal pattern of this vulnerability is therefore key to heat-related public health planning and to climate change adaptations (Ford et al., 2010). Personal vulnerability factors may include pre-existing health conditions, personal heat-adaptation habits as well as demographic characteristics such as age, gender, race, income, and educational attainment (Uejio et al., 2011; Yardley et al., 2011). Infrastructural and environmental factors include characteristics of the built and natural environment where a person resides, such as the amount of green-space, impervious surface, and microclimate characteristics (Aminipouri et al., 2016; Brown & Walker, 2008; Harlan et al., 2006; Kim & Ryu, 2015; Uejio et al., 2011; Wilhelmi & Hayden, 2010). While infrastructural and environmental factors influence vulnerability to heat, standardized data on their status and trend across large regions are rarely available, severely complicating their integration into health planning. On the other hand, information on several personal vulnerability factors is often available in the form of socio-economic data from a national census. While these data do not describe vulnerability at an individual level, they do portray both spatial and temporal trends in community-level vulnerability. Because these data primarily contain socio-economic information, and to emphasize that they are only available at the community-level, we henceforth collectively refer to them as describing socio-economic vulnerability factors. It is important to note here that such community-level variables (e.g. the average income in a census district) only represented community vulnerability, and in nature difference to the individual vulnerability such as corresponding personal characteristics (e.g. the income of a person living in that census district) and thus do not act exclusively to represent unavailable personal-level data (Diez Roux 2004).
Furthermore, although conceptual frameworks for estimating vulnerability from climate change exist (Adger et al., 2005; Ford et al., 2010; Füssel & Klein 2006; Füssel, 2007; Moses & Ekstrom, 2010), they do not allow systematic quantification of changes in heat vulnerability or risk (Toloo et al., 2014; Tong et al., 2016), for example, Vescovi et al. (2005) assumed that socioeconomic vulnerability in Quebec would not change through time. How and to what extent population distributions and redistributions (defined as “population dynamics” in this paper) influence heat vulnerability is thus unknown, and the application of statistical models that use demographic trends to quantify vulnerability and risk change is needed in order to develop policy and strategies for climate change adaptation (Berrang-Ford et al., 201; Ford et al., 2010). Several previous studies attempted to quantify relative heat risks spatially, such as Tomlinson et al. (2011) for Birmingham, UK; Buscail et al. (2012) for Rennes, France; Ho et al. (2015) and Aminipouri et al. (2016) for Vancouver, Canada; Rinner et al. (2010) for Toronto, Canada; Laverdière et al. (2015) and Vescovi et al. (2005) for Southern Quebec, Canada, and Scherer et al. (2014) for Berlin, Germany, but none of them were applied to a large region, nor to understand both the spatial and temporal dynamics. It is also important to develop a model that can compare the relative spatial difference through years, in order to incorporate with national health guidelines for extreme heat adaptation and heat vulnerability assessment.
In this study, 1) we estimate the temporal change in socio-economic vulnerability associated with heat risk in Canada, from 2006 to 2011, by combining community vulnerability data in a heat vulnerability index (Reid, 2009; Tomlinson et al., 2011; Buscail et al., 2012), and 2) we use Moran’s I to identify local clusters based on the results above, in order to locate extended areas with high temporal change. This combines existing methods to develop a simple technique that can be used to assess the spatiotemporal change of socioeconomic vulnerability related to heat risk in a national extent. Our study demonstrates current heat vulnerability trends in Canada, and may be used to target heat risk mitigation strategies in the most vulnerable areas in both the short term responses (e.g. disaster risk management, public health planning) and the long term (e.g. urban planning, regional development) (Achwarz et al., 2011; Cutter et al., 2000). The approach is easily adapted to any other country that has the necessary census data, and is following the Health Canada guideline for a complete extreme heat and health vulnerability assessment, for fulfilling the research gap to describe trends expected to influence heat-related health outcomes for assessing future risks.
Study Area
Our study area includes all 10 Canadian provinces (British Columbia, Alberta, Manitoba, Saskatchewan, Ontario, Quebec, Newfoundland and Labrador, New Brunswick, Nova Scotia, and Prince Edward Island) (Figure 1), an area with 33.4 million people or 99.7% of the Canadian population in 2011 (Geographic Research, 2015b). In southern Ontario and Quebec, the number of extremely hot days (>=30°C) at late 1990s was more than that of the summer normal since 1948 (Smoyer-Tomic et al., 2003), and similar trends have been observed in later years (Kosatsky et al., 2005; Jeong et al., 2016). During these extreme hot summer days, elevated temperature has significantly increased mortality in afflicted locations (Bustinza et al., 2013; Henderson et al., 2013; Kosatsky et al., 2005; Kosatsky et al. 2012; Smoyer-Tomic et al., 2000). For example, mortality increased by 40% for six consecutive days during the 2009 Vancouver extreme heat event (Kosatsky et al., 2012), and the number of non-traumatic deaths in Montreal on one extremely hot day in June 1994 exceeded twice the monthly mean death rate (Kosatsky et al., 2005). Heat-related mortality has also been demonstrated from cooler parts of Canada, including northern British Columbia (Henderson et al. 2013); as a result we have included all 10 Canadian provinces in our study. The three Canadian territories (Nunavut, Yukon, Northwest Territories) were excluded because the population in these regions is not known to experience adverse health effects from extreme heat (Health Canada, 2011).
Figure 1:
Population density (persons per km2) in 2011 for all Canadian provinces (British Columbia, Alberta, Manitoba, Saskatchewan, Ontario, Quebec, Newfoundland and Labrador, New Brunswick, Nova Scotia, and Prince Edward Island). Data from the 2011 Canadian census, at subdivision level.
Data and Methods
Heat Vulnerability Index
In order to quantify the relative change of vulnerability, we used a heat vulnerability index from Ho et al. (2015) that combines census data in a multi-criteria analysis (Reid, 2009; Tomlinson et al., 2011; Buscail et al., 2012). Multi-criteria analysis (MCA) is a statistical model that allows users to semi-quantitatively combine data layers in an estimation by assigning weights that represent the importance of each layer, typically based on results of meta-analysis or expert knowledge. MCA general proceeds by first assigning specific weights to each variable, then calculating a per-cell weighted average, and (optionally) discretizing the result based on percentiles or natural breaks. This method has been widely applied to environmental risk assessment (Aubrecht & Özceylan, 2013; Buscail et al., 2012; Chi, 2010; Ho et al., 2014; Ho et al., 2015).
This index of Ho et al. (2015) has considered eight groups of population that have been associated with heat vulnerability based on a literature review (Table 1): 1) older ages, 2) infants, 3) people living in old houses, 4) people in bad living environment, 5) low education population, 6) people living alone, 7) low income population, and 8) the unemployed. These eight population groups were under four dimensions of vulnerability, by each dimension with two vulnerable population groups, in which 1) and 2) were related to extreme ages, 3) and 4) were related to household characteristics, 5) and 6) were related to social status, and 7) and 8) were related to economic status. Details of association between heat vulnerability and each population group have been noted in Ho et al. (2015), with brief explanations as the followings:
Table 1:
Details of the 8 heat-related social vulnerability variables under 4 dimensions of vulnerability that used in this study.
| Dimension of Vulnerability | Variables Name | Details |
|---|---|---|
| Extreme Ages | Older ages | Population >= 55 years old |
| Infants | Population 0 – 5 years old, as to represent children under aged of elementary school’s entry | |
| Household Characteristics | People in old houses | Number of households living in housing built prior to 1960 |
| People in bad living environment | Number of households living in multi-story apartment buildings or mobile homes, as to represent population living in a location with high-risk building design during an extreme heat event | |
| Social Status | Low education population | Population with fairly low education level (without a diploma nor a degree) |
| People living alone | Number of single-person household | |
| Economic Status | Low income population | Population with household income less than $20,000 |
| Unemployed | Unemployment rate |
Older ages in this study were “people aged >= 55 years old” and infant population were “population aged from 0 – 5”, which represents young seniors, older senior and children under aged of elementary school’s entry, who need more health care and have less ability of extreme heat adaptation. People living in older people for this study was defined by “number of households living in housing built prior to 1960” and people in bad living environment were the “number of households living in multi-story apartment buildings or mobile homes”, in which the latter one representing population living in a location with high-risk building design during an extreme heat event. These are potentially important factors in some parts of Canada such as Vancouver and Calgary where the prevalence of air conditioning is low (Smoyer-Tomic et al, 2003), and have documented in studies for other countries (Tomlinson et al, 2011, Yardley et al., 2011). Low education population was defined by “people with fairly low education level (without a diploma nor a degree)”, and people living alone was defined by “number of single-person household”, in which these factors related to less knowledge and awareness for extreme heat mitigation, and associated with potential social isolation with less health care during extreme weather events. >ow income population were “people with household income less than $20,000, and unemployed was represented by “unemployment rate”, in which those were factors associated with the Vancouver Area Neighbourhood Deprivation Index (VANDIX) and VANDIX was found to be related to heat mortality in Canada (Ho et al., 2017).
In addition to highlighting common socio-economic vulnerability factors related to heat risk, vulnerability and mortality also demonstrates that there is substantial regional and temporal variation in the socio-economic factors that influence heat vulnerability. This is likely a result of variation in societal, infrastructural or demographic factors. However, information on such variability requires detailed local studies, which are not available from the majority of areas in Canada. We thus use the eight variables listed above (Table 1) across our study area while acknowledging that their relevance may vary regionally. We extracted information on each variable from the 2006 and 2011 Canadian census, at the dissemination area level, using the SimplyMap 3.0 database (Geographic Research, 2015a; Geographic Research, 2015b). In brief, dissemination area is the smallest standard geographic area with a population of 400 to 700 persons covering all the territory of Canada. Apart from the unemployment rate, all values were divided by the size of the dissemination area to obtain density values. For the census data of each year, these eight individual heat vulnerability layers were classified using the Jenks natural breaks classification method (Jenks, 1967), resulting in eight new vulnerability layers each with an index value from 1 (relative lowest vulnerability) to 9 (relative highest vulnerability). These eight layers were then combined into a single composite heat vulnerability layer by MCA by assigning equal weights (each 12.5%) to each layer (Aubrecht & Özceylan, 2013; Buscail et al., 2012; Ho et al., 2015; Tomlinson et al., 2011). This method is to follow the guideline of United Nations Environment Programme (2002) by using an unweighted quantitative aggregation with indicator standardization to avoid additional subjectivity in the index development (Aubrecht & Özceylan, 2013), opposed to the principal component analysis or ordered weighted averaging (Reid et al., 2009; Rinner et al., 2010) that potentially produced indicator weighting and composition subjectivity discussed in previous study (Aubrecht & Özceylan, 2013; Vincent, 2004). Finally, such vulnerability layers were created for 2006 and 2011 separately.
Mapping vulnerability change
For each dissemination area, we calculated the percent change in heat vulnerability from 2006 to 2011, based on the vulnerability indices above, by the following equation:
We then used Moran’s I as implemented in GeoDa to test for statistically significant clustering of heat vulnerability change, and used Moran’s local I to map spatial clusters of percent change in heat vulnerability. Spatial weights were defined using the k-nearest neighbours (KNN) algorithm (we used k=8); KNN is an asymmetrical spatial-weighting method (Getis & Aldstadt, 2010) that is particularly useful when the sizes of dissemination areas are different because it ensures that the same number of nearby dissemination areas is used in all calculations, independent of the number and size of neighbors.
The resulting map can be used to identify local patterns of spatial association, for example, detecting hot spots (clusters of increasing vulnerability) and cold spots (clusters of decreasing vulnerability) (Anselin, 1995). We then classified the map into five categories: 1) high-high cluster, i.e. a hot spot, a high value surrounded by other high values, 2) low-low cluster, i.e. a cold spot, a low value surrounded by other low values, 3) high-low correlation, an isolated high value surrounded by a cluster of low values, 4) low-high correlation, an isolated low value surrounded by a cluster of high values, and 5) areas with statistically non-significant clustering of values. This method followed the protocol of spatial heat vulnerability assessment in Canada, for example, Toronto’s heat warning system (Rinner et al., 2010), in which 1) high-high cluster in our study represented extended area with high vulnerability increase that in needed for public health actions, 2) low-low cluster indicated extended area that would have potentially lower heat vulnerability in the future, and 3) high-low and low-high correlation were to identify statistical outliners within the extended areas mapped in 1) and 2), for smoothing the decision making processes.
Comparison of seven Canadian cities
In order to study local patterns of vulnerability change, we selected 7 major cities (Toronto, Montreal, Vancouver, Ottawa, Edmonton, Calgary, and Victoria) to further investigate the temporal change in spatial patterns of vulnerability in urban areas in Canada. We used census metropolitan area (CMA) as the city boundaries, including metropolitan area (extremely urbanized), satellite cities (suburbs) and rural areas within a CMA. These 7 cities were selected based on population, also based on known extreme heat events with excess mortality found in these locations (Bélanger et al., 2014; Bustinza et al., 2013; Kosatsky et al., 2012; Smoyer-Tomic et al., 2003), and expected increases in heat-related mortality reported in climate change study (Martin et al., 2012).
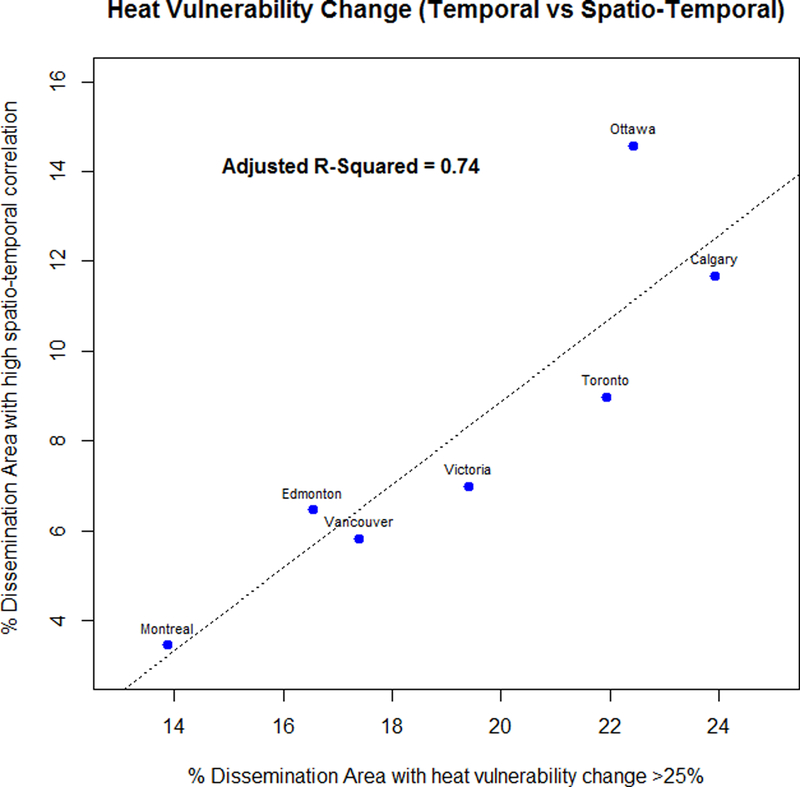
To compare the cities, we first evaluated whether a connection exists between the amount of dissemination areas undergoing high vulnerability increases and their spatial clustering. To do this, we compared the percentage of dissemination areas with high socio-economic vulnerability increase (> 25%) to the number of high-high correlation dissemination areas in each city, based on the coefficient of determination (R2). It allowed us to quantify the strength and linearity of the relationship between high vulnerability increases and spatial clustering, and also helped identify any cities deviating from this general relationship. We then conducted a visual investigation of the spatial patterns of heat vulnerability change for each city.
Secondly, we examined the change in individual vulnerability factors (table 2) in three of the seven cities to identify which socio-economic factors experience the greatest change and thus better describe the population dynamics driving change in heat vulnerability in Canada. These cities represented the metropolitan areas with relative lower, medium and higher spatial/spatiotemporal increases based on previous results. For each city, the average change of individual vulnerability factors of the dissemination areas was recalculated as percentage change following:
Table 2:
Comparison of dissemination areas with high-high correlation from Montreal, Vancouver, and Toronto.
| City | Averaged Individual Percentage Change from 2006 to 2011 (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Older ages | Infants | People in old houses | People in bad living environment | Low education population | People living alone | Low income population | Unemployed | |
| Montreal | 336 | 364 | 75 | 256 | 255 | 194 | 240 | 67 |
| Vancouver | 357 | 327 | 96 | 248 | 314 | 194 | 250 | 108 |
| Toronto | 399 | 426 | 70 | 168 | 379 | 174 | 253 | 131 |
Based on results of Moran’s I analysis from previous section, we compared the dissemination areas with high-high correlation from these three cities to examine the spatial clustering effects from changes of individual vulnerability factors.
Results
Regional vulnerability change across time and space
A broad comparison of the heat vulnerability indices shows that the social vulnerability associated with heat has generally decreased in rural areas and increased in urban areas between 2006 and 2011 (Figure 2). 14 – 24% of the dissemination areas in the selected cities had an increase in heat vulnerability of over 25% between 2006 and 2011, with the most significant changes occurring in Calgary, Ottawa, and Toronto, where at least a 25% increase in heat vulnerability was observed in 23.9%, 22.4%, and 21.9% of the dissemination areas, respectively. In comparison, only 9% dissemination areas that were not within these seven cities (Toronto, Montreal, Vancouver, Ottawa, Edmonton, Calgary, and Victoria) saw an increase in heat vulnerability of over 25% in the same period.
Figure 2:
Percentage Change of Heat Vulnerability in Canada from 2006 to 2011.
We found significant spatial clustering of heat vulnerability change across the study area, with a dominance of high-high clusters (Moran’s I: 0.44). The map of Moran’s local I shows that hot spots of high vulnerability increase are mainly found in urban areas, while both spatial and temporal correlations were low or insignificant in most rural regions (Figure 3).
Figure 3:
Clustering of the percentage change in heat vulnerability in Canada. Red indicates high increase in vulnerability in both the dissemination area and the surrounding dissemination areas. Blue indicates low increase or decrease in vulnerability in both the dissemination area and the surrounding dissemination areas. Pink indicates an isolated dissemination area with low or negative vulnerability increase, surrounded by dissemination areas with high vulnerability increases. Orange indicates an isolated dissemination area with high vulnerability increase, surrounded by dissemination areas with low vulnerability increases or vulnerability decreases. Gray indicated dissemination areas without spatial clusters.
Changes in seven cities
Out of the seven cities compared in our study, Montreal had the lowest percentage of dissemination areas located in high-high clusters of heat vulnerability (3.4%), while Ottawa has the highest percentage (14.6%). The percentage of high-high-clustered dissemination areas in a city was strongly correlated with the percentage of its dissemination areas experiencing high vulnerability increase (adjusted R2 = 0.74), with Ottawa being an outlier with unusually high clustering (Figure 4). Ottawa being an outlier may partly be a result of the structure of its administrative boundaries (Ho et al., 2015), which for Greater Ottawa include areas in two provinces (Quebec and Ontario).
Figure 4:
Comparison between the percentage of dissemination areas with heat vulnerability change of >25% and the percentages of dissemination areas with high-high clusters from LISA map in 7 cities (Toronto, Montreal, Vancouver, Ottawa, Edmonton, Calgary, and Victoria) in the Lower Canada.
We also zoomed in to visually examine the spatial patterns of heat vulnerability change in a city. Most dissemination areas in the seven cities had 5 – 25% increases in heat vulnerability from 2006 to 2011, while the dissemination areas with high vulnerability increase (> 25%) tended to be located in suburbs or in smaller cities surrounding the main metropolitan area (Figure 5). Clusters of high vulnerability increase were mainly found in suburbs and satellites cities of a city (Figure 6), especially in cities with a relatively small percentages of high vulnerability increase dissemination areas reported in figure 4 (Montreal, Vancouver, and Victoria). In addition, high vulnerability increase was also seen in some neighborhoods with an already high density of socially vulnerable people, such as Vancouver’s downtown East Side (Kerr et al., 2003), further increasing the vulnerability of these areas.
Figure 5:
Comparison of seven cities in Canada based on the temporal change of social vulnerability associated with heat risks from 2006 to 2001. Red indicates the highest increase (>25%) in vulnerability, while green indicates a decrease or a low increase (<5%) in vulnerability.
Figure 6:

Comparison of seven cities in Canada based on the spatiotemporal change of social vulnerability associated with heat risks from 2006 to 2011. Red indicates significant clusters of dissemination areas with high increase in vulnerability; grey indicates dissemination areas with either low increase in vulnerability or lack of clustering.
Comparison of Individual Vulnerability Factors
A more detailed examination of trends in individual socio-economic heat vulnerability factors was done for Montreal, Vancouver, and Toronto. These three cities were chosen because they are the most populous metropolitan areas in Canada with known extreme heat events (Bustinza et al., 2013; Kosatsky et al., 2012), and they show relatively low, medium and high increases in vulnerability, respectively (Figure 4).
The dissemination areas with high-high spatial correlation, i.e. the clusters of high heat vulnerability increase from Montreal, Vancouver, and Toronto, have seen the greatest increase in the number of infants and older ages from 2006 to 2011, and also very substantial increases in the low education and low income populations, while the number of people living in old housing and the unemployment rate have both changed relatively less (Table 2). The increases of the highest groups (infants and older ages) can be 3 to 6 times higher than the lowest group (old housing and unemployment rate). This suggests that spatiotemporal vulnerability increase in these clusters is primarily driven by an increase in older ages and family with young children, and poor and poorly educated people, rather than e.g. increases in unemployment, although all individual factors contributed to the heat vulnerability change in Canada.
Discussion
The heat vulnerability index as applied to Canadian census data from 2006 and 2011 provides a clear description of spatial patterns of change in heat vulnerability during that period. Across Canada’s 10 provinces, metropolitan areas have generally experienced a substantial increase in heat vulnerability, while changes in rural areas are more mixed. Most neighbourhoods showing large increases in heat vulnerability are found in suburbs and satellite cities surrounding metropolitan areas, possibly due to mitigation; but also include some areas of known vulnerability such as Vancouver’s downtown East Side in Vancouver with high percentage of unemployed homeless population (Kerr et al., 2003; Kosatsky et al., 2012; Smoyer-Tomic et al., 2003). In addition to these results, it is important to determine the primary drivers of the underlying population trends, and to explore whether the observed change from a retrospective study can be implemented to future planning and modelling. In the following, we discuss the results of our study in the context of the existing demographic literature and discuss the potential of our approach heat-health planning.
Implications of heat vulnerability change: migration and local growth
Our findings are strong evidence of an increase in the heat vulnerable population in urban and suburban areas (Figure 2). While we do not have detailed data on the causes of these changes, they are likely to reflect the net result of population dynamics driven by 1) workforce migration, 2) access to public transportation, 3) housing prices, and 4) natural amenities (Akbari & Avdede, 2012; Anisef et al., 2010; Ali et al., 2011; Chi, 2012; Chi & Marcouiller, 2013; Chi & Ventura, 2011; Ng & Metz, 2014; Walton-Roberts, 2012).
According to the 2006 and 2011 Canadian census data, immigration contributed to the majority of population growth (approximately 2 millions) in Canada within these 5 years (Statistics Canada 2012; Ng & Metz, 2014). This population increase contributed to an increase in housing prices (Akbari & Avdede, 2012), and specifically increased the low-income population that is relatively vulnerable to extreme heat (Hansen et al., 2013). This migration is also a contributing factor for increased unemployment rates in urban areas, and hence the social vulnerability associated with heat risk from 2006 to 2011. In addition, because of the aging of the Canadian population (Sheets & Gallagher, 2013), heat vulnerability increased rapidly in urban and suburban areas, where the majority of the elderly live, over these five years.
The cost of housing limits where the low-income population can live in a city (Waltson-Roberts, 2012), and at the same time may force a large part of the single and unemployed part of the population to live in relatively poor-quality dwellings often built in the post-war building boom or before (Smoyer-Tomic et al., 2003), with the exact location influenced by the transportation network and gasoline prices (Chi, 2012). A cluster of this heat vulnerable population group can thus be formed in a city, separately from another heat-vulnerable group, the elderly, whose residential location is to a greater extent driven by the availability of natural amenities (Chi & Marcouller, 2013). For example, an increase in heat vulnerability was observed in West End and Downtown East Side in Vancouver; both these neighbourhoods are within walking distance to downtown Vancouver and are dominated by people living alone and in high-rise buildings, and both neighbourhoods have relatively high unemployment rates and social deprivation (Andresen, 2006). Similarly, an increase in heat vulnerability was observed in Surrey Central, which is an area of known social deprivation (Bell & Hayes, 2012), and a fair public transportation network (train and bus) to downtown Vancouver. A similar pattern was found in Montreal, where there were more dissemination areas with heat vulnerability change >25% in satellite cities with good access to public transportation (subway and/or bus) and lower housing prices, such as Laval, Brossard, and Longueuil. In comparison, there was no significant increase in heat vulnerability on Montreal Island from 2006 to 2011, nor in Montreal East where housing is relatively cheap but access to downtown Montreal via public transportation is relatively poor compared to other regions. In a relatively more car-dependent, like Calgary, access to public transportation is seemingly less important, and dissemination areas with increasing heat vulnerability were commonly found within the city limit of the city itself. In summary, the factors the shape the demographic forces that in turn influence spatial patterns heat vulnerability are complex and context-dependent, and include issues such as the local housing stock and housing market, access to public transportation, and the inertia provided by existing patterns of social deprivation.
While older ages are less influenced by access to public transportation and proximity to the workplace when making relocation decisions, this large group of heat vulnerable people is generally attracted to natural amenities such as urban parks and natural spaces (Chi & Marouller, 2013), which are spatially correlated with housing prices. Suburbs and satellite cities, such as West Vancouver and Langley near Vancouver, thus saw a great increase in older ages and a corresponding increase in heat vulnerability from 2006 to 2011.
Policy implications and environmental planning for heat risk mitigation
The focus of this study was to map spatiotemporal patterns of heat vulnerability in Canada, and identify areas of particular concern to allow health agencies to focus heat risk mitigation effort in the most important locations. Previous research on heat vulnerability mapping (Hattis et al. 2012; Reid, 2009; Rinner et al., 2010; Vescovi et al., 2005) and the estimation of temperature-mortality relationships (Hondula et al., 2012) have aimed specifically at improving short-term emergency planning and disaster risk management. For example, neighborhoods with high heat vulnerability during a hot summer day could be identified in order to deploy heat mitigation measures (e.g. urban greening, increasing numbers of drinking fountains, conducting community-based workshop) for upcoming extreme hot weather events. In contrast, our study is more applicable to long-term mitigation planning as it outlines areas of increasing vulnerability. These areas, while not necessarily highly socio-economically vulnerable at present, could be targeted for heat mitigating urban planning interventions, including cooling interventions such tree planting and increasing the albedo of urban surfaces, as well as increasing health care coverage and emergency planning in the longer term. Knowledge of the drivers behind increasing vulnerability in specific dissemination areas can also help design targeted heat mitigation interventions, as older ages, families with infants, and people with poor education or low income may benefit from different heat mitigation strategies. This approach also completed the heat vulnerability assessment proposed by government, for example, in this study we followed the extreme heat and health vulnerability assessment under Health Canada guideline to first characterize community vulnerability, then to describe trends expected to influence heat-related health outcome to assess future risk, which only proposed by Health Canada guideline but not yet researched previously.
Limitations and Future Directions
In order to adapt this model from the regional to the local scale and improve its utility, a significant improvement would be a local calibration of the weights used for each social vulnerability factor in the calculation of the index. Local calibration is potentially important because the relationship between heat exposure, social vulnerability and mortality is highly variable among different cities (O’Neill et al., 2003; O’Neill et al., 2005). Such calibration can be performed with local historical weather and morbidity/mortality datasets (Bell et al., 2008; Chuang et al., 2016; Ho et al., 2017; Hu et al., 2017; Rosenthal et al., 2014; Smargiasssi et al., 2009). Furthermore, given the importance of immigration for the population growth seen from 2006 to 2011, it might be useful to include the immigrant population as an additional variable and assess its contribution to heat vulnerability in Canada. However, unlike the heat vulnerability of immigrants noted in previous studies (Yardley, 2011), the wide range of educational attainment and income levels seen in immigrants to Canada (Ng & Metz, 2014) makes immigrants a less obviously vulnerable group than is the case in other countries. A stratification of immigrants according to origin and year of immigration as well as mother tongue, educational attainment and income/wealth might be necessary to identify those immigrant groups that are especially vulnerable and to contextualize the general patterns of heat vulnerability of the immigrant population in a regional context.
Conclusions
In this study, we used Moran’s local I to detect spatial clusters of increase in vulnerability to extreme heat from 2006 to 2011, throughout the 10 Canadian provinces. Vulnerability to extreme heat was quantified using an index derived from eight census-derived social vulnerability factors using multi-criteria analysis. The results showed that increases in vulnerability are concentrated in urban and suburban areas, especially in suburbs and satellite cities surrounding the largest cities in Canada, with small negative or positive changes in most rural areas. For the spatial clusters of high increase in vulnerability found in Canada’s largest cities, the vulnerability increase is primarily driven by an increase in the number of older ages and families with infants, as well as increases in the low income and low education population. This information is useful for targeting and designing long-term heat mitigation efforts in the areas where vulnerability is growing, and is likely to continue to grow, the fastest. Local calibration of the heat vulnerability index based on long-term weather and mortality data, allowing the index to be developed from social vulnerability indicators with local pertinence, would be a significant improvement in future research.
Acknowledgements
The authors would like to acknowledge the partial support of Simon Fraser University and Pacific Institute for Climate Solutions.
Reference
- Adger WN (2006). Vulnerability. Global environmental change, 16(3), 268–281. [Google Scholar]
- Adger WN, Arnell NW, & Tompkins EL (2005). Successful adaptation to climate change across scales. Global environmental change, 15(2), 77–86. [Google Scholar]
- Ali K, Olfert MR, & Partridge MD (2011). Urban footprints in rural Canada: Employment spillovers by city size. Regional studies, 45(2), 239–260. [Google Scholar]
- Akbari AH, & Aydede Y (2012). Effects of immigration on house prices in Canada. Applied Economics, 44(13), 1645–1658. [Google Scholar]
- Aminipouri M, Knudby A, & Ho HC (2016). Using multiple disparate data sources to map heat vulnerability: Vancouver case study. The Canadian Geographer/Le Géographe canadien, 60(3), 356–368. [Google Scholar]
- Anderson G & Bell M (2010). Heat Waves in the United States: Mortality Risk during Heat Waves and Effect Modification by Heat Wave Characteristics in 43 U.S. Communities. Environmental Health Perspectives, 119(2), 210–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andresen MA (2006). A spatial analysis of crime in Vancouver, British Columbia: a synthesis of social disorganization and routine activity theory. The Canadian Geographer/Le Géographe canadien, 50(4), 487–502. [Google Scholar]
- Anisef P, Brown RS, Phythian K, Sweet R, & Walters D (2010). Early school leaving among immigrants in Toronto secondary schools. Canadian Review of Sociology/Revue canadienne de sociologie, 47(2), 103–128. [DOI] [PubMed] [Google Scholar]
- Anselin L (1995). Local indicators of spatial association-LISA. Geographical analysis, 27(2), 93–115. [Google Scholar]
- Aubrecht C, & Özceylan D (2013). Identification of heat risk patterns in the US National Capital Region by integrating heat stress and related vulnerability. Environment international, 56, 65–77. [DOI] [PubMed] [Google Scholar]
- Basu R (2009). High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environmental Health, 8:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bélanger D, Gosselin P, Valois P, & Abdous B (2014). Perceived adverse health effects of heat and their determinants in deprived neighbourhoods: a cross-sectional survey of nine cities in Canada. International journal of environmental research and public health, 11(11), 11028–11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell N, & Hayes MV (2012). The Vancouver Area Neighbourhood Deprivation Index (Vandix): a census-based tool for assessing small-area variations in health status. Canadian Journal of Public Health/Revue Canadienne de Sante’e Publique, S28–S32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrang-Ford L, Ford JD, & Paterson J (2011). Are we adapting to climate change?. Global environmental change, 21(1), 25–33. [Google Scholar]
- Brown S, & Walker G (2008). Understanding heat wave vulnerability in nursing and residential homes. Building Research & Information, 36(4), 363–372. [Google Scholar]
- Buscail C, Upegui E &Viel J-F (2012). Mapping heatwave health risk at the community level for public health action, International Journal of Health Geographics, 11:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bustinza R, Lebel G, Gosselin P, Bélanger D, & Chebana F (2013). Health impacts of the July 2010 heat wave in Quebec, Canada. BMC public health, 13(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan EYY, Goggins WB, Kim JJ, & Griffiths SM (2012). A study of intracity variation of temperature-related mortality and socioeconomic status among the Chinese population in Hong Kong. Journal of epidemiology and community health, 66(4), 322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi G (2010). Land developability: Developing an index of land use and development for population research. Journal of Maps, 6(1), 609–617. [Google Scholar]
- Chi G (2012). The impacts of transport accessibility on population change across rural, suburban and urban areas: a case study of Wisconsin at sub-county levels. Urban studies, 49(12), 2711–2731. [Google Scholar]
- Chi G, & Marcouiller DW (2013). In-migration to remote rural regions: The relative impacts of natural amenities and land developability. Landscape and Urban Planning, 117, 22–31. [Google Scholar]
- Chi G, & Ventura SJ (2011). An integrated framework of population change: Influential factors, spatial dynamics, and temporal variation. Growth and Change, 42(4), 549–570. [Google Scholar]
- Chow WT, Chuang WC, & Gober P (2012). Vulnerability to extreme heat in metropolitan Phoenix: spatial, temporal, and demographic dimensions. The Professional Geographer, 64(2), 286–302. [Google Scholar]
- Chuang WC, & Gober P (2015). Predicting hospitalization for heat-related illness at the census-tract level: Accuracy of a generic heat vulnerability index in phoenix, Arizona (USA). Environmental Health Perspectives, 123(6), 606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutter SL, Mitchell JT, & Scott MS (2000). Revealing the vulnerability of people and places: a case study of Georgetown County, South Carolina. Annals of the Association of American Geographers, 90(4), 713–737. [Google Scholar]
- Roux Diez, Ana V. 2004. The study of group-level factors in epidemiology: rethinking variables, study designs, and analytical approaches. Epidemiologic Reviews 26 (1):104–111. [DOI] [PubMed] [Google Scholar]
- Eisenman DP, Wilhalme H, Tseng CH, Chester M, English P, Pincetl S, … & Dhaliwal SK (2016). Heat death associations with the built environment, social vulnerability and their interactions with rising temperature. Health & place, 41, 89–99. [DOI] [PubMed] [Google Scholar]
- Filleul L, Cassadou S, Médina S, Fabres P, Lefranc A, Eilstein D, … & Ledrans M (2006). The relation between temperature, ozone, and mortality in nine French cities during the heat wave of 2003. Environmental Health Perspectives, 1344–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford JD, Keskitalo ECH, Smith T, Pearce T, Berrang‐Ford L, Duerden F, & Smit B (2010). Case study and analogue methodologies in climate change vulnerability research. Wiley Interdisciplinary Reviews: Climate Change, 1(3), 374–392. [Google Scholar]
- Füssel HM, & Klein RJ (2006). Climate change vulnerability assessments: an evolution of conceptual thinking. Climatic change, 75(3), 301–329. [Google Scholar]
- Füssel HM (2007). Vulnerability: a generally applicable conceptual framework for climate change research. Global environmental change, 17(2), 155–167. [Google Scholar]
- Gago EJ, Roldan J, Pacheco-Torres R, & Ordoñez J (2013). The city and urban heat islands: A review of strategies to mitigate adverse effects. Renewable and Sustainable Energy Reviews, 25, 749–758. [Google Scholar]
- Geographic Research, Inc. (2015a). Census 2006 Current Estimates Data retrieved Mar 31st, 2015, from SimplyMap database.
- Geographic Research, Inc. (2015b). Census 2011 Current Estimates Data retrieved Mar 31st, 2015, from SimplyMap database.
- Getis A, & Aldstadt J (2010). Constructing the spatial weights matrix using a local statistic In Perspectives on spatial data analysis (pp. 147–163). Springer Berlin Heidelberg. [Google Scholar]
- Goldberg RA (2007). Projecting heat-related mortality impacts under a changing climate in the New York City region. American Journal of Public Health, 97(11), 2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosling SN, McGregor GR, & Lowe JA (2009). Climate change and heat-related mortality in six cities Part 2: climate model evaluation and projected impacts from changes in the mean and variability of temperature with climate change. International journal of biometeorology, 53(1), 31–51. [DOI] [PubMed] [Google Scholar]
- Hansen A, Bi L, Saniotis A, & Nitschke M (2013). Vulnerability to extreme heat and climate change: is ethnicity a factor?. Global health action, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harlan SL, Brazel AJ, Prashad L, Stefanov WL, & Larsen L (2006). Neighborhood microclimates and vulnerability to heat stress. Social science & medicine, 63(11), 2847–2863. [DOI] [PubMed] [Google Scholar]
- Hattis D, Ogneva-Himmelberger Y & Ratick S (2012).The spatial variability of heat-related mortality in Massachusetts.Applied Geography, 33, 45–52. [Google Scholar]
- Henderson S, Wan V & Kosatsky T (2013).Differences in heat-related mortality across four ecological regions with diverse urban, rural, and remote populations in British Columbia, Canada. Health & Place, 23, 48–53. [DOI] [PubMed] [Google Scholar]
- Ho HC, Mylroie J,Infante L, and Rodgers J (2014). Fuzzy-based Spatial Modeling Approach to Predict Island Karst Distribution. Environmental Earth Sciences, 71(3), 1369–1377. [Google Scholar]
- Ho HC, Knudby A, & Huang W (2015). A Spatial Framework to Map Heat Health Risks at Multiple Scales. International journal of environmental research and public health, 12(12), 16110–16123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho HC, Knudby A, Walker BB, Henderson SB (2017). Delineation of spatial variability in the temperature-mortality relationship on extremely hot days in greater Vancouver, Canada. Environmental Health Perspectives, 125(1), 66–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hondula D, Davis R, Leisten M, Saha M, Veazey L & Wegner C (2012). Fine-scale spatial variability of heat-related mortality in Philadelphia County, USA, from 1983–2008: a case-series analysis. Environmental Health, 11:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu K, Yang X, Zhong J, Fei F, & Qi J (2017). Spatially explicit mapping of heat health risk utilizing environmental and socioeconomic data. Environmental Science & Technology. [DOI] [PubMed] [Google Scholar]
- Huang W, Kan H, & Kovats S (2010). The impact of the 2003 heat wave on mortality in Shanghai, China. Science of the Total Environment, 408(11), 2418–2420. [DOI] [PubMed] [Google Scholar]
- Huang C, Barnett AG, Wang X, Vaneckova P, FitzGerald G, & Tong S (2011). Projecting future heat-related mortality under climate change scenarios: a systematic review. Environmental health perspectives. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institut de Veille Sanitaire (2004). Étude des facteurs de risque de décès des personnes âgées résidant à domicile durant la vague de chaleur d’août 2003. Accessed 29 August 2015 from http://www.invs.sante.fr/publications/2004/chaleur2003_170904/rapport_canicule.pdf
- IPCC (2009). IPCC Fifth Assessment Report (AR5): Climate Change 2014: Impacts, Adaptation, and Vulnerability.
- IPCC (2011). IPCC Special Report on Managing the Risks of Extreme Events and Disasters to Advance Climate Change Adaptation. [DOI] [PubMed]
- Jackson JE, Yost MG, Karr C, Fitzpatrick C, Lamb BK, Chung SH, … & Fenske RA (2010). Public health impacts of climate change in Washington State: projected mortality risks due to heat events and air pollution. Climatic Change, 102(1–2), 159–186. [Google Scholar]
- Jenks G(1967). The Data Model Concept in Statistical Mapping. International Yearbook of Cartography, 7, 186–190. [Google Scholar]
- Jeong DI, Sushama L, Diro GT, Khaliq MN, Beltrami H, & Caya D (2016). Projected changes to high temperature events for Canada based on a regional climate model ensemble. Climate Dynamics, 46(9), 3163–3180 [Google Scholar]
- Jones TS, Liang AP, Kilbourne EM, Griffin MR, Patriarca PA, Wassilak SGF, … & Thacker SB (1982). Morbidity and mortality associated with the July 1980 heat wave in St Louis and Kansas City, Mo.Jama, 247(24), 3327–3331. [PubMed] [Google Scholar]
- Kalkstein AJ, & Sheridan SC (2007). The social impacts of the heat–health watch/warning system in Phoenix, Arizona: assessing the perceived risk and response of the public. International journal of biometeorology, 52(1), 43–55. [DOI] [PubMed] [Google Scholar]
- Kerr T, Wood E, Small D, Palepu A, & Tyndall MW (2003). Potential use of safer injecting facilities among injection drug users in Vancouver’s Downtown Eastside. Canadian Medical Association Journal, 169(8), 759–763. [PMC free article] [PubMed] [Google Scholar]
- Kim S, & Ryu Y (2015). Describing the spatial patterns of heat vulnerability from urban design perspectives. International Journal of Sustainable Development & World Ecology, 22(3), 189–200. [Google Scholar]
- Kosatsky T, Henderson SB, & Pollock SL (2012). Shifts in mortality during a hot weather event in Vancouver, British Columbia: rapid assessment with case-only analysis. American journal of public health, 102(12), 2367–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosatsky T, King N, & Henry B (2005). How Toronto and Montreal (Canada) respond to heat In Extreme Weather Events and Public Health Responses (pp. 167–171). Springer Berlin Heidelberg. [Google Scholar]
- Kovach MM, Konrad CE, & Fuhrmann CM (2015). Area-level risk factors for heat-related illness in rural and urban locations across North Carolina, USA. Applied Geography, 60, 175–183. [Google Scholar]
- Laaidi K, Zeghnoun A, Dousset B, Bretin P, Vandentorren S, Giraudet E &Beaudeau P (2012).The Impact of Heat Islands on Mortality in Paris during the August 2003 Heat Wave. Environmental Health Perspectives, 120(2), 254–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laverdière É, Mélissa Généreux MD, & Morais JA (2015). Prevalence of risk and protective factors associated with heat-related outcomes in Southern Quebec: A secondary analysis of the NuAge study. Canadian journal of public health, 106(5), E315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin SL, Cakmak S, Hebbern CA, Avramescu ML, & Tremblay N (2012). Climate change and future temperature-related mortality in 15 Canadian cities. International journal of biometeorology, 56(4), 605–619. [DOI] [PubMed] [Google Scholar]
- Meehi GA & Tebaldi C (2004). More Intense, More Frequent, and Longer Lasting Heat Waves in the 21st Century. Science, 305, 994–997. [DOI] [PubMed] [Google Scholar]
- Moser SC, & Ekstrom JA (2010). A framework to diagnose barriers to climate change adaptation. Proceedings of the National Academy of Sciences, 107(51), 22026–22031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray V, & Ebi KL (2012). IPCC special report on managing the risks of extreme events and disasters to advance climate change adaptation (SREX). Journal of epidemiology and community health, 66(9), 759–760. [DOI] [PubMed] [Google Scholar]
- National Post. (2012). The homelands and homes of new Canadians. The national post. Retrieved from http://nationalpostnews.files.wordpress.com/2012/02/1-na0211_immigration.pdf
- Ng ES, & Metz I (2014). Multiculturalism as a strategy for national competitiveness: The case for Canada and Australia. Journal of Business Ethics, 128(2), 253–266. [Google Scholar]
- O’Neill MS, Zanobetti A & Schwartz J (2003).Modifiers of the temperature and mortality association in seven US cities. American Journal of Epidemiology, 157, 1074–1082. [DOI] [PubMed] [Google Scholar]
- O’Neill MS, Zanobetti A, Schwartz J (2005). Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. Journal of Urban Health, 82, 191–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid CE, O’Neill MS, Gronlund CJ, Brines SJ, Brown DG, Diez-Roux AV, & Schwartz J (2009).Mapping Community Determinants of Heat Vulnerability. Environmental Health Perspectives, 117(11), 1730–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid CE, Mann J, Alfasso R, English PB, King GC, Lincoln RA, Margolis HG, Rubado DJ, Sabato JE, West NL, Woods B, Navarro. KM & Balmes JR (2012).Evaluation of a Heat Vulnerability Index on Abnormally Hot Days: An Environmental Public Health Tracking Study. Environmental Health Perspectives, 120(5), 715–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal JK, Kinney PL, & Metzger KB (2014). Intra-urban vulnerability to heat-related mortality in New York City, 1997–2006. Health & place, 30, 45–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer D, Fehrenbach U, Lakes T, Lauf S, Meier F, & Schuster C (2014). Quantification of heat-stress related mortality hazard, vulnerability and risk in Berlin, Germany. DIE ERDE–Journal of the Geographical Society of Berlin, 144(3–4), 238–259. [Google Scholar]
- Schwarz AM, Béné C, Bennett G, Boso D, Hilly Z, Paul C, … & Andrew N. (2011). Vulnerability and resilience of remote rural communities to shocks and global changes: Empirical analysis from Solomon Islands. Global Environmental Change, 21(3), 1128–1140. [Google Scholar]
- Sheets DJ, & Gallagher EM (2013). Aging in Canada: state of the art and science. The Gerontologist, 53(1), 1–8. [DOI] [PubMed] [Google Scholar]
- Sheridan SC, & Dixon PG (2016). Spatiotemporal trends in human vulnerability and adaptation to heat across the United States. Anthropocene. [Google Scholar]
- Smoyer-Tomic KE, Rainham DG, & Hewko JN (2000). Heat-stress-related mortality in five cities in Southern Ontario: 1980–1996. International Journal of Biometeorology, 44(4), 190–197. [DOI] [PubMed] [Google Scholar]
- Smoyer-Tomic KE, Kuhn R, & Hudson A (2003). Heat wave hazards: an overview of heat wave impacts in Canada. Natural hazards, 28(2–3), 465–486. [Google Scholar]
- Son J-Y, Lee J-T, Anderson B & Bell ML (2012a).The Impact of Heat Waves on Mortality in Seven Major Cities in Korea. Environmental Health Perspectives, 120(4), 566–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son J-Y, Lee J-T, Anderson B & Bell ML (2012b).Vulnerability to temperature-related mortality in Seoul, Korea. Environmental Research Letters, 6, 034027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson C, Chapman L, Thornes J & Baker C (2011).Including the urban heat island in spatial heat health risk assessment strategies: a case study for Birmingham, UK.International Journal of Health Geographic, 10:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toloo G, FitzGerald G, Aitken P, Verrall K, & Tong S (2013). Evaluating the effectiveness of heat warning systems: systematic review of epidemiological evidence. International journal of public health, 58(5), 667–681. [DOI] [PubMed] [Google Scholar]
- Toloo GS, FitzGerald G, & Tong S (2014). Managing health risks of extreme weather events: need for a systematic approach. Australian and New Zealand journal of public health, 38(1), 90–91. [DOI] [PubMed] [Google Scholar]
- Tong S, Conalonieri U, Ebi K, & Olsen J (2016). Managing and mitigating the health risks of climate change: calling for evidence-informed policy and action. Environ Health Perspect, 124, A176–A179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uejio CK, Wilhelmi OV, Golden JS, Mills DM, Gulino SP, & Samenow JP (2011). Intra-urban societal vulnerability to extreme heat: the role of heat exposure and the built environment, socioeconomics, and neighborhood stability. Health & Place, 17(2), 498–507. [DOI] [PubMed] [Google Scholar]
- United Nations Environment Programme. (2002). Assessing human vulnerability due to environmental change: concepts, issues, methods and case studies, Nairobi, Kenya [57 pp.] [Google Scholar]
- Vaneckova P, Beggs PJ, & Jacobson CR (2010). Spatial analysis of heat-related mortality among the elderly between 1993 and 2004 in Sydney, Australia. Social science & medicine, 70(2), 293–304. [DOI] [PubMed] [Google Scholar]
- Vescovi L, Rebetez M, &Rong F (2005). Assessing public health risk due to extremely high temperature events: climate and social parameters. Climate Research, 30, 71–78. [Google Scholar]
- Vincent K (2004). Creating an index of social vulnerability to climate change for Africa. Tyndall Center for Climate Change Research. Working Paper, 56, 41. [Google Scholar]
- Walton-Roberts M (2012). Regional immigration and dispersal: Lessons from small-and medium-sized urban centres in British Columbia. 3 Cities and Immigrant Integration: The Future of Second-and Third-Tier Centres,1(1,920,773), 158. [Google Scholar]
- Wilhelmi OV, & Hayden MH (2010). Connecting people and place: a new framework for reducing urban vulnerability to extreme heat. Environmental Research Letters, 5(1), 014021. [Google Scholar]
- Yan YY (2000). The influence of weather on human mortality in Hong Kong. Social science & medicine, 50(3), 419–427. [DOI] [PubMed] [Google Scholar]
- Yardley J, Sigal R & Kenny G (2011). Heat health planning: The importance of social and community factors. Global Environmental Change, 21, 670–679. [Google Scholar]