Abstract
Background:
Cross-sectional associations between anxiety disorders and eating disorders (EDs) have been well documented; however, limited research has examined whether symptoms of anxiety disorders are prospectively associated with EDs. Identifying these longitudinal associations can aid in discerning relationships among these, often comorbid conditions and point towards a mechanistic understanding of developmental psychopathology. The current study investigated the prospective associations between parent-reported anxiety in mid-childhood (age 10) and child-reported ED behaviors and disorders in adolescence (at ages 14 and 16 years) in a population-based sample.
Methods:
Participants were individuals enrolled in the Avon Longitudinal Study of Parents and Children (ALSPAC), a population-based, prospective study of women and their children; 7,767 children whose parents provided data at age 10 were included in current analyses. An exploratory factor analysis identified latent anxiety factors at age 10, followed by a path analysis that evaluated associations between these factors and eating disorder symptoms and cognitions at age 14.
Results:
Parent-reported anxiety symptoms at age 10 yielded 5 factors: obsessive-compulsive disorder (OCD) symptoms related to symmetry and checking (Factor 1); OCD symptoms associated with aversion to dirt and germs (Factor 2); physical anxiety symptoms (Factor 3); worries (Factor 4); and social phobia symptoms (Factor 5). Factors 3 and 4 showed the most consistent, positive associations with a range of ED symptoms at age 14. Factor 3 predicted diagnosis of bulimia nervosa by age 16 (OR = 1.11, p = 0.007), while Factor 4 predicted diagnoses of anorexia nervosa (OR = 1.10, p = 0.01) and disordered eating by age 16 (OR = 1.08, p = 0.001).
Conclusions:
Results indicate that symptoms of generalized anxiety in middle childhood may predict adolescent-onset ED symptoms and ED diagnoses.
Keywords: anxiety, eating disorder, obsessive compulsive disorder, structural equation modeling, ALSPAC
Introduction
Peak onset for eating disorders occurs in adolescence and young adulthood, with over 15% of individuals experiencing an eating disorder (anorexia nervosa [AN], bulimia nervosa [BN], binge eating disorder [BED]), or subthreshold eating disorder before age 18 (Field et al., 2012; Micali et al., 2015). Although much research has evaluated cross-sectional associations between adolescent psychopathology and eating disorders, limited research has examined prospective risk factors that predict onset of eating disorders (ED). Examining childhood factors longitudinally is a necessary avenue for research to ascertain risk factors prior to ED onset, which can improve early detection and intervention for these debilitating conditions. Further, probing prospective relationships among eating disorders and related symptoms can inform developmental models of psychopathology and comorbidity.
Eating disorders are highly comorbid with other psychiatric conditions, particularly anxiety disorders. For example, more than half of individuals with an eating disorder report a lifetime anxiety disorder (AN: 47.9%, BN: 80.6%; BED: 65.1%; Hudson, Hiripi, Pope, & Kessler, 2007), a finding that replicates among adolescents (AN: 23.9%, BN: 66.2%, 65.2%; Swanson, Crow, LeGrange, Swendsen, & Merikangas, 2011). More specifically, obsessive-compulsive disorder (OCD) and social and specific phobias are among the most common comorbid psychiatric diagnoses among adolescents and adults with eating disorders (Hudson et al., 2007; Kaye, Bulik, Thornton, Barbarich, & Masters, 2004; Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011). Retrospective reports from patients also indicate that anxiety disorders often occur prior to eating disorder onset and persist after remission (Kaye et al., 2004; Raney et al., 2008).
The nature and direction of associations between anxiety and eating disorders are not entirely clear. It may be that the comorbidity between anxiety and eating disorder arises from a multiformity model of comorbidity in which one disorder (anxiety) precipitates another (eating disorder). Or it may be that this observed comorbidity is due to liability in which risk among anxiety and eating disorders stems from a shared latent factor (Neale & Kendler, 1995), with eating disorders being the presentation of this latent risk at a later developmental time point. Of note, many studies that have investigated comorbidity between eating disorders and anxiety have assessed childhood disorders retrospectively in cohorts who present with a diagnosed eating disorder (Kaye et al., 2004; Raney et al., 2008); limited research has examined temporal associations of anxiety and eating disorders prospectively. One study that examined anxiety trajectories across childhood in relationship to adolescent eating disorder pathology found no evidence that girls with high levels of maternal-reported anxiety during childhood are at increased risk for eating disorders (Zerwas, Von Holle, Watson, Gottfredson, & Bulik, 2014); however, this study did not discriminate among specific symptoms of anxiety or eating disorder pathology. Buckner, Silgado, & Lewinsohn (2010) found that, among anxiety disorder diagnoses, only obsessive-compulsive disorder (OCD) when self-reported by adolescents at age 16, predicted AN (but not BN) at age 30. Given that OCD, specifically, evidences cross-sectional and longitudinal associations with EDs, Micali et al. (2011) followed 10-year-olds presenting to a specialty clinic with an OCD diagnosis over nine years and similarly found a high prevalence (12.7%) of eating disorders at follow-up.
Some studies have also examined whether adolescent eating disorders predicted future anxiety disorders. Micali et al. (2015) found that adolescents diagnosed with full- or subthreshold eating disorders were between 2–7 times more likely to be diagnosed with an anxiety disorder over time. Further, in an examination of specific anxiety disorder diagnoses, Buckner et al. (2010) found that BN predicted later social phobia and panic disorder, providing evidence that developmental relations between eating disorders and anxiety disorders may be both symptom and disorder specific, and may include some reciprocal relations among anxiety and eating symptoms. In addition to phenotypic comorbidity between anxiety and eating disorders, there are also shared genetic underpinnings of these conditions. Studies using genetically informative designs support a relationship between eating disorders and broad anxiety disorder phenotypes (Keel, Klump, Miller, McGue & Iacono, 2005; Lilenfeld et al., 1998; Silberg & Bulik, 2005), along with relationships among specific diagnosis (e.g., AN and OCD; Anttila et al., 2016; Bellodi et al., 2001; Cederlöf et al., 2015; Lilenfeld et al., 1998, Yilmaz et al., 2017).
While the majority of research has investigated anxiety and ED comorbidity at a diagnostic level, models of comorbidity in mental illness posit that latent liability may impact symptoms of multiple disorders (Krueger and Markon, 2006), and that symptoms of disorders themselves (e.g. affective experiences, behaviors) may influence disorder presentation and progression (e.g. the likelihood that a disorder will increase in severity over time or that symptoms of comorbid psychiatric disorders will arise; Young, 2015). As such, it is pertinent to investigate comorbidity of anxiety and EDs at the symptom level. In the context of child development, examining latent factors derived from specific anxiety symptom experiences may be particularly useful, as anxiety can present in a heterogeneous manner (Broeren, Muris, Diamantopoulou, & Baker, 2013). Some research has examined how specific anxiety-related symptom factors relate to the development of eating disorders over time. Silberg and Bulik (2005) differentiated between separation anxiety, overanxious, and depressive symptoms and examined genetic and environmental associations with eating disorder symptoms in younger (8–13 year old) and older (14–17) twins, finding support for shared genetic risk among anxiety, depressive and eating disorder symptoms, but also identifying a genetic factor specific to early eating pathology, along with evidence of a shared environmental influences on separation anxiety disorder and later eating problems.
There is also evidence that individual anxiety symptoms may have specific relationships with risk for eating pathology. In the context of AN-OCD comorbidity, for example, an association between symmetry or ‘wanting things to be in an exact way’ and symptoms of AN has been supported (Degortes, Zanetti, Tenconi, Santonastaso, & Favaro, 2014; Halmi et al., 2003). With regard to physical symptoms of anxiety, research has also identified anxiety sensitivity (attentiveness and reactivity to physical anxiety symptoms) as a risk factor for eating disorders (Davey & Chapman, 2009; DeBoer, Tart, Presnell, & Powers, Baldwin, & Smits, 2012; Fulton et al., 2012; Levinson et al., 2017).
The aim of the current study was to investigate the prospective longitudinal association between parent-reported anxiety in mid-childhood (age 10) and child-reported ED behaviors along with multi-informant ED diagnoses in adolescence (at age 14 and 16 years) in a population-based sample. Given the high overlap of anxiety disorder symptoms, we aimed to identify latent factors encompassing these in childhood. Based on previous findings, we hypothesized that a range of anxiety-related symptom factors at age 10 would include multiple, meaningful symptom factors that would overlap with, but not necessarily replicate, existing diagnostic entities. Further, we anticipated that multiple of these factors would predict both eating disorder symptoms and diagnoses in adolescence, particularly those that capture OCD-related symptomatology.
Method
Participants
Participants were individuals enrolled in The Avon Longitudinal Study of Parents and Children (ALSPAC), a population-based, prospective study of women and their children (Boyd et al., 2013; Fraser et al., 2013; Golding, Pembrey, Jones, & ALSPAC, 2001). Expectant mothers (expecting to deliver between 1st April 1991 and 31st December 1992) in the area of Avon, UK were invited to take part in the study; those interested provided written informed consent. Children (n = 14,676) from 14,451 pregnancies were enrolled; at 1 year 13,988 children were alive. At age 7 years, 713 additional children were enrolled in the cohort (Boyd et al., 2013; Fraser et al., 2013). The study website contains details of all the data that are available through a fully searchable data dictionary: http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary.
In the current study, questionnaires were sent to parents of 10,441 children enrolled at age 10 years; 72% were returned. In addition, questionnaires were sent to 9,927 children at age 14 and 9,563 children at age 16; 6,811 responded at age 14 years (69%), and 5,500 at age 16 years (58%). All children with anxiety data at age 10 were included in subsequent analyses, and maximum likelihood estimation was used to adjust for missing data in path analyses.
Measures
Anxiety symptoms.
Anxiety symptoms were reported by parents of children at age 10 using the Development and Wellbeing Assessment (DAWBA; Goodman, Ford, Richards, Gatward, & Meltzer, 2000; Goodman, Heiervang, Collishaw, & Goodman, 2011). The DAWBA parent-report is a semi-structured interview used to assess psychopathology of children ages 4–16; the interviews are completed in-person or online. Eighty-three items assessed reflect diagnostic criteria and are symptom-based. The DAWBA has been shown to be externally valid and has significantly distinguished rates of anxiety disorders between psychiatric clinic and community samples (Goodman et al., 2000). Anxiety disorders, as defined by the DAWBA are reported at 43.6% in a psychiatric clinic sample, as compared to a rate of 5.5% in a community sample (Odds Ratio = 13.3). Further, in a clinic sample, there is good agreement between DAWBA and case note diagnoses (Goodman et al., 2000; Kuhn et al., 2017). A study comparing self- and parent-report versions of the DAWBA favored a parent-report format for identifying cases and discriminating clinical and community samples (Kuhn et al., 2017)
Eating disorder symptoms and cognitions.
Eating disorder symptoms were evaluated by child report at age 14 and 16 (Micali et al., 2015). Data on eating disorder behaviors were collected using questions adapted from the Youth Risk Behavior Surveillance System Questionnaire (YRBSSQ; Kann et al., 1995), validated in a population-based study of adolescents (Field, Taylor, Celio, & Colditz, 2004) inquiring about the previous year. Fourteen day test-retest reliability of the YRBSSQ indicates that the majority (72%) of items show good reliability (Brener, Collins, Kann, Warren, & Williams, 1995). Binge eating was assessed using a two-part question on occurrence and frequency of eating a very large amount of food and feeling out of control during these episodes; positive responses to both of these questions yielded a classification of engaging in binge eating. Purging was assessed by asking how often in the past year the adolescent made him/herself sick or used laxatives to lose weight or avoid gaining weight. Binge eating and purging were then categorized into ordinal frequencies of never, less than once per month, 1–3 times per month, or once per week or more. Fasting was assessed with one question: “During the past year, how often did you fast (not eat for a least a day) to lose weight or avoid gaining weight?” Fear of weight gain was evaluated by an ordinal question asking the degree to which an individual has worried about gaining a little weight in the past year, exercising to lose weight was assessed by asking if an individual had exercised to lose or avoid gaining weight, and weight concern was assessed by a question that assessed the degree to which a respondent’s weight made a difference in how they felt.
Along with categorical levels of eating disorder cognitions and behaviors assessed by the YRBSSQ, at age 14 years continuous levels of eating disorder symptoms were evaluated by self-report. Emotional eating, external eating, and restraint were assessed by several items from the Dutch Eating Behavior Questionnaire (DEBQ; Stice, Mazotti, Krebs, & Martin, 1998; Van Strien, Frijters, Bergers, & Defares, 1986). Internal consistency in the current study was acceptable (Cronbach’s α = 0.91, 0.67, and 0.72 for emotional eating, external eating, and restraint, respectively). Body dissatisfaction was assessed using the Body Dissatisfaction Scale of the Satisfaction and Dissatisfaction With Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973). This scale asks individuals to rate their satisfaction with nine body parts on a 5-point scale, from ‘extremely satisfied’ to ‘extremely dissatisfied,’ (Cronbach’s α = 0.84 in the current study). A continuous score was derived for this measure, with higher values indicating higher dissatisfaction.
Appearance-ideal internalization was assessed by items adapted from the Ideal-Body Stereotype Scale-Revised (Stice et al., 1998; Stice, Ziemba, Margolis, & Flick, 1996), with gender-specific items used to assess different aspects of appearance-ideal internalization for boys (6 items) and girls (5 items) in the current study (Calzo et al., in preparation). Pressure to lose weight was assessed using four items adapted from the Perceived Sociocultural Pressure Scale (Stice et al., 1996), which asked about pressure to lose weight from different sources: family, friends, dating partners, and the media.
Eating disorder diagnoses.
Eating disorder diagnoses (AN, BN, BED, purging disorder [PD]) were derived using questionnaire data (described above) from adolescents using DSM-5 diagnostic criteria (American Psychiatric Association, 2013; for details see [Micali et al., 2015]). Body mass index (BMI) was an objective measure collected at face-to-face assessment (median ages 13.8 and 15.5 years) and was included as a diagnostic criterion for AN. Underweight was determined using age, gender, and BMI-specific cutoffs (based on UK reference data; Cole, Flegal, Nicholls, & Jackson, 2007) corresponding to World Health Organization (WHO) grade 1 thinness.
Parental report of AN symptoms was also used at ages 14 and 16 when formulating AN diagnoses as prior research has shown that parental-report often aids in the diagnosis of AN in adolescents due to under-reporting of AN symptoms (House, Eisler, Simic, & Micali, 2008). In addition to threshold eating disorder diagnoses, we also identified youth with disordered eating cognitions and behaviors. This category included individuals who reported monthly binge eating, purging excessive exercise, or fasting, along with those who reported more sporadic disordered eating behaviors along with shape and weight concern at age 14, and those who reported eating disorder behaviors at any subthreshold level of severity at age 16 (Micali et al., 2015).
Statistical Analyses
DAWBA anxiety items were screened to assess the degree to which they would be useful in defining latent anxiety factors at age 10. Screened items were included in an exploratory factor analysis (EFA) with a Geomin rotation (oblique) to identify latent dimensions of anxiety symptoms. Prior to analyses, appropriateness of items was identified for the factor analysis. Items were excluded that were: a) related to eating; b) primarily focused on the duration or frequency of a symptom (e.g., symptom is present for at least two weeks); c) assessed functional interference secondary to symptoms (e.g., these acts or thoughts have interfered with family relationships); or d) qualified a symptom for diagnostic criteria (e.g., child recognizes fears as excessive). Items that fit poorly on all factors were also identified and removed from analyses until a final factor structure was identified.
Factor loadings from the EFA portion of the model were saved as predictors in a subsequent path analysis. This approach allowed for the estimation of effects that was consistent with an Exploratory Structural Equation Model (ESEM), and combined the EFA with the predictive modeling of path analysis. ESEM allows part of the structural model to be exploratory: latent factors are allowed to influence all manifest indicators (as opposed to being constrained in CFA) according to a predefined number of latent factors (Marsh, Morin, Parker, & Kaur, 2014). This approach was used to investigate the associations between dimensions of anxiety symptoms (age 10) and future eating disorder symptoms (age 14) and diagnoses (diagnosis at age 14 or 16). Because it was possible that relationships between anxiety and eating disorders would vary by gender, we examined model invariance by gender when predicting lifetime eating disorder diagnoses. After finding no evidence of improved model fit when grouping by gender, we collapsed the sample across genders to increase statistical power and included gender as a covariate in path analyses. Results are presented as standardized regression coefficients (ß) for the eating disorder symptoms model, in which an increase of one standard deviation on anxiety factor scores is associated with a change in ß standardized units on the outcome variable. For the lifetime eating pathology model, results are presented as standardized odds ratios.
Results
Sample Characteristics
We included youth based on three waves of data collection: at child age 10 years (Wave 10+), 14 years (Wave 14+), and 16 years (Wave 16+). Prevalence of eating disorder behaviors at age 14 and lifetime eating disorder diagnoses by age 16 along with participant demographic information are provided in Table 1.
Table 1a.
Proportion of sample endorsing eating disorder symptoms at age 14.
| %Endorsed | N (assessed) | |
|---|---|---|
| Eating Disorder Symptoms at Age 14 | ||
| Purging | 1.5% | 5180 |
| Binge eating | 5.5% | 5221 |
| Fasting | 6.4% | 5176 |
| Exercise to lose weight | 33.7% | 5036 |
| Fear of weight gain | 32.3% | 5172 |
| Weight concern | 48.5% | 5181 |
Anxiety EFA
In initial iterations of the EFA, items that assessed specific phobias did not load well onto factors, and were subsequently excluded. Items assessing fears in the classroom and school setting were also excluded as they did not cluster well with other anxiety factors; 23 items were retained in the final exploratory factor analysis, and a 5-factor solution was determined to fit the data most appropriately (RMSEA = 0.01, CFI = 0.998; see Figure 1). Factor scores obtained for the final, 5-factor, solution were subsequently used as predictors in regression models (or path analyses). Factors were identified as capturing: OCD symptoms related to symmetry and checking (Factor 1; e.g., “In the past month, child has counted to lucky numbers or avoided unlucky numbers”); OCD symptoms associated with aversion to dirt and germs (Factor 2; e.g., “In the past month, child has cleaned excessively”); physical anxiety symptoms (Factor 3; e.g., “Worries lead to child being restless, tense or on edge”); worries (Factor 4; e.g., “Child worries about the future”); and social phobia (Factor 5; e.g., “In the past month, child has been afraid of meeting new people”). Correlations among anxiety symptom factors were positive and small to moderate (0.12 [OCD dirt and germs with social phobia] - 0.36 [physical anxiety with worries]).
Figure 1.
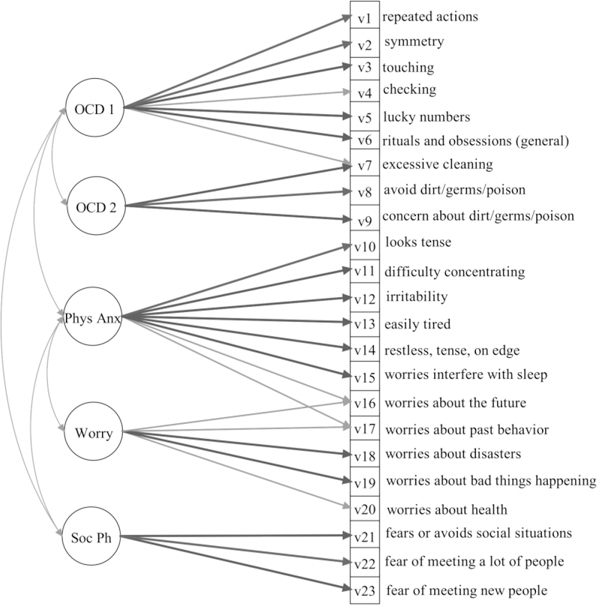
Anxiety factors at age 10. Soc Ph - social phobia. Phy Anx - physical anxiety. OCD - obsessive-compulsive disorder.
Eating Disorder Symptoms
In path analyses, missing data were allowed; however, cases where anxiety factor scores were unable to be computed (n = 31) were excluded to allow for model estimation. Thus, 7,736 cases were included. All eating disorder symptom variables were included as outcome variables in the model, and the full model is presented in Figure 2.
Figure 2.
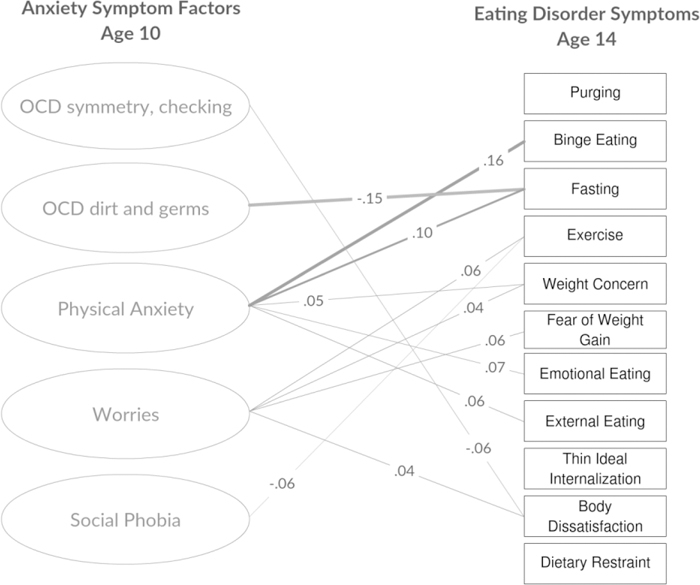
Anxiety factors at age 10 as predictors of eating disorder symptoms at age 14. Standardized regression coefficients reported. OCD – obsessive-compulsive disorder. Only significant paths included. Purging, Binge Eating, Fear of Weight Gain, Weight Concern, and Exercise reported on an ordinal scale. Fasting reported as dichotomous (present vs. absent). All other variables assessed on a continuous scale.
Female gender was associated with all eating disorder symptoms at age 14, with the exception of external eating. Factor 1 (OCD symmetry) showed a negative prospective association with body dissatisfaction (ß = −.064; SE = .02; p = .006), indicating that a stronger preference for symmetry at age 10 was associated with lower levels of body dissatisfaction in adolescence. Factor 2 (OCD dirt and germs) evidenced a negative association with fasting (ß = −0.15, SE = 0.07, p = 0.03), indicating that higher levels of obsessions and compulsions related to dirt and germs at age 10 were related to lower levels of fasting behavior at age 14. Factor 3 (physical anxiety) had positive associations with several eating disorder symptoms, including binge eating, (ß = 0.16, SE = 0.046, p = 0.001) fasting (ß = 0.10, SE = 0.045, p = 0.030), emotional eating (ß = 0.07, SE = 0.023, p = 0.001), external eating (ß = 0.06, SE = 0.023, p = 0.017), and weight concerns (ß = 0.052, SE = 0.023, p = 0.021). Factor 4 (worries) was also positively associated with several eating disorder symptoms, including fear of weight gain (ß = 0.06, SE = 0.023, p = 0.006), weight concern (ß = 0.043, SE = 0.021, p = 0.047), body dissatisfaction (ß = 0.041, SE = 0.020, p = 0.042), excessive exercise (ß = 0.07, SE = 0.023, p = 0.003), and dietary restraint (ß = 0.043, SE = 0.020, p = 0.034). Factor 5 (social phobia) had a negative association with excessive exercise (ß = −.057, SE = .021, p = .007).
Eating Disorder Diagnosis
Anxiety symptom factors were also evaluated as predictors of lifetime eating disorder diagnoses identified at either age 14 or age 16 (see Figure 3). 7,742 cases were retained in the estimation model. In this model, Factor 3 (physical anxiety) predicted a diagnosis of BN or subthreshold BN (Standardized Odds Ratio = 1.11 p = 0.007) by age 16. Factor 4 (worries) predicted diagnoses of AN (Standardized Odds Ratio = 1.10 p = 0.01) and disordered eating (Standardized Odds Ratio = 1.08, p = 0.001) by age 16.
Figure 3.
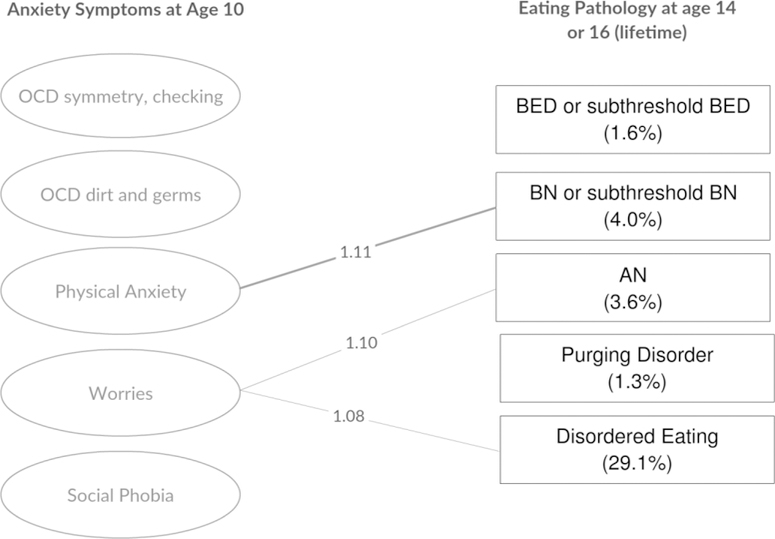
Anxiety factors at age 10 as predictors of eating pathology at age 14 or 16. OCD – obsessive-compulsive disorder. BN – bulimia nervosa. BED – binge eating disorder. AN – anorexia nervosa. Only significant paths included. Standardized odds ratios reported.
Sensitivity Analysis: Eating Disorder Risk at Age 10.
To examine the possibility that eating disorder risk at age 10 was associated with concurrent anxiety symptoms, we evaluated the relation between body image discrepancy using the Stunkard Figure Rating Scale (Stunkard, Sorenson, & Schalasinger, 1983). We examined partial correlations between this variable capturing body dissatisfaction and each of the five anxiety factors at age 10, controlling for gender. No anxiety factors at age 10 evidenced a significant partial correlation with body dissatisfaction at this assessment timepoint.
Discussion
The current study investigated prospective relations between childhood anxiety symptoms and eating disorder symptoms and diagnoses in early adolescence. We identified latent anxiety factors in childhood and allowed both factor-level and item-level correlation to most accurately capture relationships among anxiety symptoms. These five symptom factors overlapped with but did not replicate anxiety disorder diagnostic criteria. Factors that included symptoms of generalized anxiety disorder (worries and physical anxiety) related to an increased level of eating disorder cognitions and behaviors at age 14. In addition, physical anxiety predicted onset of BN, while general worries predicted later onset of AN and disordered eating.
Findings indicate that, in a general population sample of young people, childhood OCD symptoms do not prospectively relate to eating disorders in adolescence. Results contrast with previous research finding increased rates of OCD among individuals diagnosed with AN along with prospective investigations examining later development in which OCD in adolescence predicted onset of AN (Buckner et al., 2010). Key methodological differences between this investigation and previous research may account for this discrepancy. First, individuals who present in a clinical setting may represent a subset of individuals who likely have more severe and comorbid pathology. Second, we assessed only childhood OCD and relatively early onset eating disorders in this sample. A large epidemiological study indicated that mean age of onset for OCD, for instance, was 19.5 years, with an earlier age of onset in males than in females (Ruscio, Stein, Chiu, & Kessler, 2010). The mean age of onset for AN and BN in epidemiological samples occurs in the late teens (ages 15–20; Hudson et al., 2007; Kessler et al., 2013; Micali et al., 2013). In addition, the majority of cases in samples contributing to the observed genetic correlation between AN and OCD are adults (Anttila et al., 2005). Thus, different associations seen in other studies may reflect the window of risk at later developmental time points. While we did not find associations between OCD factors and eating pathology in the expected directions, there were two inverse relationships between OCD factors and eating disorder symptoms at age 14. The OCD dirt and germs factor was inversely related to fasting, and there was also an inverse relationship between OCD symmetry and checking and body dissatisfaction. While interpretation of these findings is tentative, it is possible that shared AN-OCD genetic risk may lead to divergent trajectories of psychopathology if the phenotypic symptoms serve similar functions. For example, obsessive, intrusive thoughts and compulsions may serve similar functions to some eating disorder symptoms but at-risk children who display OCD symptoms at a relatively early age may be more likely to continue exhibiting phenotypically similar symptoms over time. Additional studies that examine symptom networks over time will assist in understanding associations between specific symptoms of psychopathology across development.
Similar to findings for OCD-related factors, developmental timing may have influenced the identified associations between social phobia and future eating disorder symptoms, as median age of onset for social phobia is reported at 15–17 years old (Kessler, Petukhova, Sampson, Zaslavsky & Wittchen, 2012), thus, individuals reporting social phobia symptoms at age 10 may represent only a subset of those who go on to display these symptoms as they age. Further, while cross-sectional studies report high prevalence of social anxiety among individuals with eating disorders (Kerr-Gaffney, Harrison, & Tchanturia, 2018), fewer studies have examined these relationships prospectively. With regards to the negative association between social phobia and excessive exercise, it is possible that appearance- and competence-related anxieties coupled with the often social nature of exercise during adolescence may reduce exercise engagement, and, in turn, risk of excessive exercise, for young people with social anxiety concerns (Hartmann, Zahner, Pühse, & Schneider, 2010; Levinson, Rodebaugh, Menatti, & Weeks, 2013).
With regards to other associations, physical anxiety symptoms in childhood predicted bulimic symptoms and behaviors in adolescence. Physical anxiety symptoms included parent-report of the child looking tense, that worries lead to a child being restless, tired, irritable, having difficulty concentrating, or difficulty sleeping. Such behavioral manifestations of anxiety overlap with symptoms of depression and externalizing disorders in childhood. Physical symptoms such as restlessness, fatigue, tension, and irritability might either be diffuse, behavioral indicators of psychopathology, specific physical symptoms of anxiety, or, in some cases, might index parental misinterpretation of symptoms. Mechanisms behind this pattern of risk are unclear; it is possible that such symptoms represent early signs of difficulties with emotion regulation (Brown, Hochman, & Micali, in preparation; Castellanos-Ryan et al., 2016) or it may be that physical symptoms are more easily observable to parents and thus, more likely to be reported. There was some support for this interpretation in the current sample. We were able to compare reports of worry and physical anxiety symptoms at age 14 (parent-reported) and 15.5 (self-reported). Worry symptoms were reported at similar rates by both parents and adolescents; however, physical anxiety symptoms were more likely to be reported by parents (M = 1.13 out of 6 symptoms) than by adolescents (M = .23 out of 6 symptoms; t (4544) = 32.91, p < .001). Further, physical anxiety can include interoceptive experiences involving gastrointestinal distress, which can impact feelings of hunger and fullness. Recent reviews of the relationship between gastrointestinal symptoms and eating disorders highlight the potential for complex and reciprocal relationships between eating disorder, anxiety, and gastrointestinal symptoms (Norris, Harrison, Isserlin, Robinson, Feder, & Sampson, 2016; Conviser, Fisher, & McColley, 2018), which may be mediated by variations in gut microbiota (Glenny, Bulik-Sullivan, Tang, Bulik, & Carroll, 2017; Kleiman et al., 2015).
In addition to physical anxiety, a factor encompassing symptoms associated with worries in different areas of a child’s life (disasters, health, the future, past behavior) was prospectively associated with the development of a range of eating disorder symptoms along with diagnoses of AN and disordered eating in adolescence. Generalized anxiety symptoms are relatively common in children, and these worries may place individuals at risk for the development of a range of behaviors that serve as a reducing or worry-eliminating function. In considering mechanistic support for this hypothesis, dietary restriction may have an anxiolytic effect through a neurobiological process involved in the regulation of serotonin in some individuals (e.g. Kaye, 2008), which would offer negative reinforcement from an anxious state and lead to enhanced risk for the development of AN.
Some considerations in the current research are of note. First, we relied on parent-reported anxiety at age 10, which may not capture a child’s full experience of anxiety-related symptoms; however, there is evidence of predictive validity of parent-reported anxiety measures in the ALSPAC sample at younger ages relating to child-reported anxiety at an older age (Fisher et al., 2016) along with evidence that the parent-report version of the DAWBA outperforms the self-report version in distinguishing clinical diagnoses (Kuhn et al., 2017). In addition, parent-reported anxiety was deemed to be the most developmentally appropriate measure at this time point, particularly as parents are most likely to bring children to clinical attention. Further, research indicates that while parent and child informants often disagree regarding psychological symptoms, agreement among informants is higher in children than in adolescents (Achenbach, McConaughy, & Howell, 1987). With regards to measurement of eating disorders, measures were not designed to capture avoidant/restrictive food intake disorder as this eating disorder phenotype was not identified in diagnostic systems at the time of study design, and, as such, we were unable to assess the relationship between anxiety factors and this particular diagnostic phenotype. Further, there are some limitations to generalizability due to the characteristics of the ALSPAC sample, including a population that is mostly white and English speaking. In addition, there was some bias in retention, as those with higher levels of socioeconomic status were more likely to continue participation over time (Boyd et al., 2013). Evaluation of the degree to which the relationships observed in the current study replicate in more diverse samples of children is therefore necessary. Another consideration is that, although we included gender as a covariate, models were not evaluated separately by gender. Analyses suggested gender invariance in the eating disorder diagnosis model, though we were unable to formally test gender invariance in the eating disorder symptoms model. It is possible that some relationships between anxiety factors and eating disorder symptoms may have varied by gender, and future work might further explore this possibility. Finally, observed relationships in the current study were small in magnitude, and implications should be tempered appropriately. Future investigations aimed at identifying variables that both moderate and mediate the associations between childhood anxiety and adolescent eating disorders are necessary.
An additional consideration in the current study was the choice to use latent anxiety factor variables rather than diagnostic categories. This approach was chosen due to concerns that diagnostic criteria may not be “carving nature at its joints,” (Meehl, 1995) particularly in childhood. For example, some developmental models of psychopathology indicate that childhood disorders include diffuse and dynamic symptom presentations, which differentiate over time (Hudziak, Achenbach, Althoff, & Pine, 2007). Thus, a latent factor approach, allowing for relationships among factors and symptoms may more accurately capture symptom presentations and processes. In support of this notion, the latent anxiety factor model in the current study did not align perfectly with diagnostic classifications, yet provided an excellent fit with the observed data.
Conclusions
The current study identified childhood symptoms associated with generalized anxiety (physical anxiety symptoms and worries) as predictive of eating disorders symptoms and diagnoses in early adolescence. This investigation offers unique insight into the phenomenology of anxiety in middle childhood and the association between anxiety and the adolescent development of eating disorders in an epidemiological sample. Overall, findings indicate that early risk phenotypes for eating disorders may not present as a tendency towards specific obsessive thoughts or compulsive behaviors, but might relate to more general anxiety symptoms. Findings align with investigations in samples of individuals with eating disorders who commonly report generalized anxiety symptoms that arise prior to eating disorder onset (Raney et al., 2008). Primary care clinicians who receive parental reports of child anxiety should be attentive to weight fluctuations, changes in growth trajectory, and reports of dysregulated eating in late childhood and early adolescence. From a behavioral learning perspective, children prone to anxious feelings and worries may be more likely to develop concerns related to weight and body image and may then seek out behaviors (e.g., restriction, binge eating, purging) that offer an opportunity to mitigate these concerns. As cultural pressures may promote concern over weight gain (Schaefer et al., 2014; Stice & Shaw, 2002; Thompson & Stice, 2001), children prone to worry may be more likely to internalize specific fears related to weight and shape. Worries that have demonstrated specific relationships with eating disorders in previous studies include fear of food (Levinson, Brosof, Ma, Fewell, & Lenze, 2017), weight gain (Levinson et al., 2017), and fear of fatness (Dalley & Buunk, 2009). Future research incorporating information on genetic risk and examining potential mechanisms related to the development of specific symptoms over time (e.g. using longitudinal network analysis) will assist in further clarifying specific relationships between experiences of anxiety and the development of eating pathology. Overall, the current study provides evidence that generalized anxiety symptoms during middle childhood may specifically index risk for early onset eating disorders.
Table 1b.
Proportion of sample meeting criteria for eating pathology in adolescence.
| Proportion of Sample Meeting Criteria for Eating Pathology | |||
|---|---|---|---|
| Age 14 (N = 5256) |
Age 16 (N = 4420) |
Age 14 or 16 (N = 5823) |
|
| Binge eating disorder (BED) or subthreshold BED |
0.4% | 1.6% | 1.6% |
| Bulimia nervosa (BN) or subthreshold BN | 1.4% | 3.8% | 4.0% |
| Anorexia nervosa | 2.7% | 1.9% | 3.6% |
| Purging disorder | 0.4% | 1.4% | 1.3% |
| Disordered eating | 12.9% | 28.0% | 29.1% |
| All eating pathology (including disordered eating) |
17.9% | 36.6% | 37.0% |
| All EDs (excluding disordered eating) | 5.0% | 8.6% | 9.9% |
Note. Rates of eating disorder symptoms and diagnoses obtained by data from the Youth Risk Behavior Surveillance System Questionnaire along with objective measures of weight and height. Parent-reported data also used to determine diagnosis of anorexia nervosa. Disordered eating was defined as individuals who reported symptoms of an eating disorder but less frequent eating disordered behaviors (i.e., binge eating, purging, excessive exercise, or fasting less than once per week). Subthreshold bulimia nervosa and subthreshold binge eating disorder were defined as meeting criteria for these disorders with the exception that episodes of binge eating occurred less frequently than once per week.
Key points:
What’s Known
Patients with eating disorders report high rates of childhood-onset anxiety.
Eating disorders and anxiety disorders are often comorbid.
What’s New
Worries and physical anxiety at age 10 predict eating disorder symptoms and diagnoses in adolescence.
What’s Clinically relevant
Clinicians should be attentive to weight fluctuations and eating concerns among anxious children
Childhood worries about physical symptoms might predispose to eating and body related worries that can convert into full blown ED
Acknowledgements:
This manuscript was supported by grants from the National Institute of Mental Health (R21MH109917 and T32MH076694). The UK Medical Research Council and Wellcome (Grant ref: 102215/2/13/2) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors and they will serve as guarantors for the contents of this paper. A comprehensive list of grants funding is available on the ALSPAC website. This research was specifically funded by NIH 5R01MH073842. The authors are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. C.B.: Shire (grant recipient, Scientific Advisory Board member) and Pearson and Walker (author, royalty recipient). N.M. is supported by the National Institute of Health Research (NIHR) clinician scientist award (DHCS/08/08/012). The remaining authors have declared that they have no competing or potential conflicts of interest.
Abbreviations:
- (ALSPAC)
The Avon Longitudinal Study of Parents and Children
- (OCD)
Obsessive Compulsive Disorder
- (ED)
Eating Disorder
Footnotes
Conflict of interest statement: See Acknowledgements for full disclosures.
References
- Anttila V, Bulik-Sullivan B, Finucane HK, Bras J, Duncan L, Escott-Price V, … Neale B. (2016). Analysis of shared heritability in common disorders of the brain. Biorxiv, 10.1101/048991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Bellodi L, Cavallini MC, Bertelli S, Chiapparino D, Riboldi C, & Smeraldi E (2001). Morbidity risk for obsessive-compulsive spectrum disorders in first-degree relatives of patients with eating disorders. American Journal of Psychiatry, 158, 563–569. [DOI] [PubMed] [Google Scholar]
- Berscheid E, Walster E, & Bohrnstedt G (1973). The happy American body: A survey report. Psychology Today, 7, 119–131. [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, … Davey Smith G. (2013). Cohort Profile: the ‘children of the 90s’--the index offspring of the Avon Longitudinal Study of Parents and Children. International Journal of Epidemiology, 42, 111–127. 10.1093/ije/dys064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brener ND, Collins JL, Kann L, Warren CW, & Williams BI (1995). Reliability of the Youth Risk Behavior Survey Questionnaire. American Journal of Epidemiology, 141, 575–580. [DOI] [PubMed] [Google Scholar]
- Broeren S, Muris P, Diamantopoulou S, & Baker JR (2013). The course of childhood anxiety symptoms: developmental trajectories and child-related factors in normal children. Journal of Abnormal Child Psychology, 41, 81–95. 10.1007/s10802-012-9669-9 [DOI] [PubMed] [Google Scholar]
- Brown M, Hochman A, Micali N (in preparation). Emotional Instability as a Trait Risk Factor for Eating Disorder Behaviours in Female Adolescents: A Large-scale Prospective Study [DOI] [PubMed]
- Buckner JD, Silgado J, & Lewinsohn PM (2010). Delineation of differential temporal relations between specific eating and anxiety disorders. Journal of Psychiatric Research, 44, 781–787. 10.1016/j.jpsychires.2010.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calzo JP, Austin SB, Micali N (in preparation). Sexual Orientation Disparities in Eating Disorder Symptoms among Adolescent Boys and Girls in the United Kingdom [DOI] [PMC free article] [PubMed]
- Castellanos-Ryan N, Brière FN, O’Leary-Barrett M, Banaschewski T, Bokde A, Bromberg U, IMAGEN Consortium. (2016). The structure of psychopathology in adolescence and its common personality and cognitive correlates. Journal of Abnormal Psychology, 125(8), 1039–1052. 10.1037/abn0000193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cederlöf M, Thornton LM, Baker J, Lichtenstein P, Larsson H, Rück C, … Mataix-Cols D. (2015). Etiological overlap between obsessive-compulsive disorder and anorexia nervosa: a longitudinal cohort, multigenerational family and twin study. World Psychiatry, 14, 333–338. 10.1002/wps.20251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conviser JH, Fisher SD, & McColley SA (2018). Are children with chronic illnesses requiring dietary therapy at risk for disordered eating or eating disorders? A systematic review. International Journal of Eating Disorders, 51, 187–213. 10.1002/eat.22831 [DOI] [PubMed] [Google Scholar]
- Dalley SE, & Buunk AP (2009). “Thinspiration” vs. “fear of fat”. Using prototypes to predict frequent weight-loss dieting in females. Appetite, 52, 217–221. 10.1016/j.appet.2008.09.019 [DOI] [PubMed] [Google Scholar]
- Davey GC, & Chapman L (2009). Disgust and eating disorder symptomatology in a non-clinical population: the role of trait anxiety and anxiety sensitivity. Clin Psychol Psychother, 16, 268–275. 10.1002/cpp.623 [DOI] [PubMed] [Google Scholar]
- DeBoer LB, Tart CD, Presnell KE, Powers MB, Baldwin AS, & Smits JAJ (2012). Physical activity as a moderator of the association between anxiety sensitivity and binge eating. Eating Behaviors, 13, 194–201. 10.1016/j.eatbeh.2012.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degortes D, Zanetti T, Tenconi E, Santonastaso P, & Favaro A (2014). Childhood obsessive-compulsive traits in anorexia nervosa patients, their unaffected sisters and healthy controls: a retrospective study. European Eating Disorders Review, 22, 237–242. 10.1002/erv.2295 [DOI] [PubMed] [Google Scholar]
- Field AE, Sonneville KR, Micali N, Crosby RD, Swanson SA, Laird NM, … Horton NJ. (2012). Prospective association of common eating disorders and adverse outcomes. Pediatrics, 130, e289–95. 10.1542/peds.2011-3663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field AE, Taylor CB, Celio A, & Colditz GA (2004). Comparison of self-report to interview assessment of bulimic behaviors among preadolescent and adolescent girls and boys. International Journal of Eating Disorders, 35, 86–92. 10.1002/eat.10220. [DOI] [PubMed] [Google Scholar]
- Fisher E, Caes L, Clinch J, Tobias JH, & Eccleston C (2016). Anxiety at 13 and its effect on pain, pain-related anxiety, and pain-related disability at 17: An ALSPAC cohort longitudinal analysis. Psychology, Health, & Medicine, 21, 1–9. 10.1080/13548506.2015.1051062 [DOI] [PubMed] [Google Scholar]
- Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, Lawlor DA. (2013). Cohort Profile: The Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. International Journal of Epidemiology, 42, 97–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulton JJ, Lavender JM, Tull MT, Klein AS, Muehlenkamp JJ, & Gratz KL (2012). The relationship between anxiety sensitivity and disordered eating: the mediating role of experiential avoidance. Eating Behaviors, 13, 166–169. 10.1016/j.eatbeh.2011.12.003 [DOI] [PubMed] [Google Scholar]
- Glenny EM, Bulik-Sullivan EC, Tang Q, Bulik CM, & Carroll IM (2017). Eating Disorders and the Intestinal Microbiota: Mechanisms of Energy Homeostasis and Behavioral Influence. Current Psychiatry Reports, 19, 51 10.1007/s11920-017-0797-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golding J, Pembrey M, Jones R, & ALSPAC ST (2001). ALSPAC--the Avon Longitudinal Study of Parents and Children. I. Study methodology. Paediatr Perinat Epidemiol, 15, 74–87. [DOI] [PubMed] [Google Scholar]
- Goodman A, Heiervang E, Collishaw S, & Goodman R (2011). The ‘DAWBA bands’ as an ordered-categorical measure of child mental health: description and validation in British and Norwegian samples. Social Psychiatry and Psychiatric Epidemiology, 46, 521–532. 10.1007/s00127-010-0219-x [DOI] [PubMed] [Google Scholar]
- Goodman R, Ford T, Richards H, Gatward R, & Meltzer H (2000). The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. Journal of Child Psychology and Psychiatry, 41, 645–655. [PubMed] [Google Scholar]
- Halmi KA, Sunday SR, Klump KL, Strober M, Leckman JF, Fichter M, … Kaye WH. (2003). Obsessions and compulsions in anorexia nervosa subtypes. International Journal of Eating Disorders, 33, 308–319. 10.1002/eat.10138 [DOI] [PubMed] [Google Scholar]
- Hartmann T, Zahner L, Pühse U, Schneider S, Puder JJ, & Kriemler S (2010). Physical activity, bodyweight, health and fear of negative evaluation in primary school children. Scand J Med Sci Sports, 20, e27–34. 10.1111/j.1600-0838.2009.00888.x [DOI] [PubMed] [Google Scholar]
- House J, Eisler I, Simic M, & Micali N (2008). Diagnosing eating disorders in adolescents: a comparison of the eating disorder examination and the development and well-being assessment. International Journal of Eating Disorders, 41, 535–541. 10.1002/eat.20528 [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61, 348–358. 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudziak JJ, Achenbach TM, Althoff RR, & Pine DS (2007). A dimensional approach to developmental psychopathology. Int J Methods Psychiatr Res, 16 Suppl 1, S16–23. 10.1002/mpr.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, Warren CW, Harris WA, Collins JL, Douglas KA, Collins ME, … Kolbe LJ. (1995). Youth risk behavior surveillance--United States, 1993. J Sch Health, 65, 163–171. [DOI] [PubMed] [Google Scholar]
- Kaye WH, Bulik CM, Thornton L, Barbarich N, & Masters K (2004). Comorbidity of anxiety disorders with anorexia and bulimia nervosa. American Journal of Psychiatry, 161, 2215–2221. 10.1176/appi.ajp.161.12.2215 [DOI] [PubMed] [Google Scholar]
- Kaye W (2008). Neurobiology of anorexia and bulimia nervosa. Physiology & Behavior, 94, 121–135. 10.1016/j.physbeh.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr-Gaffney J, Harrison A, & Tchanturia K (2018). Social anxiety in the eating disorders: a systematic review and meta-analysis. Psychological Medicine, 1–15. 10.1017/S0033291718000752 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, & Wittchen HU (2012). Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res, 21, 169–184. 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, … Xavier M. (2013). The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biological Psychiatry, 73, 904–914. 10.1016/j.biopsych.2012.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman SC, Watson HJ, Bulik-Sullivan EC, Huh EY, Tarantino LM, Bulik CM, & Carroll IM (2015). The Intestinal Microbiota in Acute Anorexia Nervosa and During Renourishment: Relationship to Depression, Anxiety, and Eating Disorder Psychopathology. Psychosomatic Medicine, 77, 969–981. 10.1097/PSY.0000000000000247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, & Markon KE (2006). Reinterpreting Comorbidity: A Model-Based Approach to Understanding and Classifying Psychopathology. Annual Review of Clinical Psychology, 2, 111–133. 10.1146/annurev.clinpsy.2.022305.095213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhn C, Aebi M, Jakobsen H, Banaschewski T, Poustka L, Grimmer Y, … Steinhausen HC. (2017). Effective Mental Health Screening in Adolescents: Should We Collect Data from Youth, Parents or Both. Child Psychiatry Hum Dev, 48, 385–392. 10.1007/s10578-016-0665-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Brosof LC, Ma J, Fewell L, & Lenze EJ (2017). Fear of food prospectively predicts drive for thinness in an eating disorder sample recently discharged from intensive treatment. Eating Behaviors, 27, 45–51. 10.1016/j.eatbeh.2017.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL, Menatti AR, & Weeks JW (2013). Validation of the Social Exercise and Anxiety Measure (SEAM): Assessing fears, avoidance, and importance of social exercise. J Psychopathol Behav Assess, 35, 10.1007/s10862-012-9326-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Zerwas S, Calebs B, Forbush K, Kordy H, Watson H, Bulik CM. (2017). The Core Symptoms of Bulimia Nervosa, Anxiety, and Depression: A Network Analysis. Journal of Abnormal Psychology, 10.1037/abn0000254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilenfeld LR, Kaye WH, Greeno CG, Merikangas KR, Plotnicov K, Pollice C, Nagy L. (1998). A controlled family study of anorexia nervosa and bulimia nervosa: psychiatric disorders in first-degree relatives and effects of proband comorbidity. Archives of General Psychiatry, 55, 603–610. 10.1001/archpsyc.55.7.603 [DOI] [PubMed] [Google Scholar]
- Marsh HW, Morin AJ, Parker PD, & Kaur G (2014). Exploratory structural equation modeling: an integration of the best features of exploratory and confirmatory factor analysis. Annu Rev Clin Psychol, 10, 85–110. 10.1146/annurev-clinpsy-032813-153700 [DOI] [PubMed] [Google Scholar]
- Meehl PE (1995). Bootstraps taxometrics: Solving the classification problem in psychopathology. American Psychologist, 50, 266–275. doi: 10.1037/0003-066X.50.4.266 [DOI] [PubMed] [Google Scholar]
- Micali N, Hagberg KW, Petersen I, Treasure JL. The incidence of eating disorders in the UK in 2000–2009: findings from the General Practice Research Database. BMJ Open 2013;3(5). 10.1136/bmjopen-2013-002646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micali N, Hilton K, Nakatani E, Natatani E, Heyman I, Turner C, & Mataix-Cols D (2011). Is childhood OCD a risk factor for eating disorders later in life? A longitudinal study. Psychological Medicine, 41, 2507–2513. 10.1017/S003329171100078X [DOI] [PubMed] [Google Scholar]
- Micali N, Solmi F, Horton NJ, Crosby RD, Eddy KT, Calzo JP, … Field AE. (2015). Adolescent Eating Disorders Predict Psychiatric, High-Risk Behaviors and Weight Outcomes in Young Adulthood. Journal of the American Academy of Child and Adolescent Psychiatry, 54, 652–659.e1. 10.1016/j.jaac.2015.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neale MC, & Kendler KS (1995). Models of comorbidity for multifactorial disorders. American Journal of Human Genetics, 57, 935–953. [PMC free article] [PubMed] [Google Scholar]
- Norris ML, Harrison ME, Isserlin L, Robinson A, Feder S, & Sampson M (2016). Gastrointestinal complications associated with anorexia nervosa: A systematic review. International Journal of Eating Disorders, 49, 216–237. 10.1002/eat.22462 [DOI] [PubMed] [Google Scholar]
- Raney TJ, Thornton LM, Berrettini W, Brandt H, Crawford S, Fichter MM, … Bulik CM. (2008). Influence of overanxious disorder of childhood on the expression of anorexia nervosa. International Journal of Eating Disorders, 41(4), 326–332. 10.1002/eat.20508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, & Kessler RC (2010). The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry, 15, 53–63. 10.1038/mp.2008.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer LM, Burke NL, Thompson JK, Dedrick RF, Heinberg LJ, Calogero RM, … Swami, V. (2014). Development and Validation of the Sociocultural Attitudes Towards Appearance Questionnaire-4 (SATAQ-4). Psychol Assess, 10.1037/a0037917 [DOI] [PubMed] [Google Scholar]
- Silberg JL, & Bulik CM (2005). The developmental association between eating disorders symptoms and symptoms of depression and anxiety in juvenile twin girls. Journal of Child Psychology and Psychiatry, 46(12), 1317–1326. 10.1111/j.1469-7610.2005.01427.x [DOI] [PubMed] [Google Scholar]
- Stice E, Mazotti L, Krebs M, & Martin S (1998). Predictors of adolescent dieting behaviors: A longitudinal study. Psychology of Addictive Behaviors, 12, 195–205. 10.1037/0893-164X.12.3.195 [DOI] [Google Scholar]
- Stice E, & Shaw HE (2002). Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. Journal of Psychosomatic Research, 53, 985–993. 10.1016/S0022-3999(02)00488-9 [DOI] [PubMed] [Google Scholar]
- Stice E, Ziemba C, Margolis J, & Flick P (1996). The dual pathway model differentiates bulimics, subclinical bulimics, and controls: Testing the continuity hypothesis. Fal, 1996. Behavior Therapy, 27, 531–549. 10.1016/S0005-7894(96)80042-6 [DOI] [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, & Merikangas KR (2011). Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry, 68, 714–723. 10.1001/archgenpsychiatry.2011.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JK, & Stice E (2001). Thin-ideal internalization: Mounting evidencce for a new risk factor for body-image disturbance and eating pathology. Current Directions in Psychological Science, 10, 181–183. 10.1111/1467-8721.00144 [DOI] [Google Scholar]
- van Strien T, Frijters JER, Bergers G, & Defares PB (1986). The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. International Journal of Eating Disorders, 5, 295–315. [DOI] [Google Scholar]
- van Strien T, & Oosterveld P (2008). The children’s DEBQ for assessment of restrained, emotional, and external eating in 7- to 12-year-old children. International Journal of Eating Disorders, 41, 72–81. 10.1002/eat.20424 [DOI] [PubMed] [Google Scholar]
- Yilmaz Z, Halvorsen M, Bryois J, Yu D, Thornton LM, Zerwas S, … Crowley JJ. (2017). Examination of the shared genetic basis of anorexia nervosa and obsessive-compulsive disorder. biorxiv, 10.1101/231076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young G (2015). Causality in Psychiatry: A Hybrid Symptom Network Construct Model. Front Psychiatry, 6, 164 10.3389/fpsyt.2015.00164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerwas S, Von Holle A, Watson H, Gottfredson N, & Bulik CM (2014). Childhood anxiety trajectories and adolescent disordered eating: findings from the NICHD Study of Early Child Care and Youth Development. International Journal of Eating Disorders, 47(7), 784–792. 10.1002/eat.22318 [DOI] [PMC free article] [PubMed] [Google Scholar]


