Abstract
Objective
To study the current status and applications of additive manufacturing (AM) in dentistry along with various technologies, benefits and future scope.
Methods
A significant number of relevant research papers on the additive manufacturing application in dentistry are identified through Scopus and studied using bibliometric analysis that shows an increasing trend of research in this field. This paper briefly describes various types of AM technologies with their accuracy, pros and cons along with different dental materials. Paper also discusses various benefits of AM in dentistry and steps used to create 3D printed dental model using this technology. Further, ten major AM applications in dentistry are identified along with primary references and objectives.
Results
Additive manufacturing is an innovative technique moving towards the customised production of dental implants and other dental tools using computer-aided design (CAD) data. This technology is used to manufacture elaborate dental crowns, bridges, orthodontic braces and can also various other models, devices and instruments with lesser time and cost. With the help of this disruptive innovation, dental implants are fabricated accurately as per patient data captured by the dental 3D scanner. The application of this technology is also being explored for the precise manufacturing of removal prosthetics, aligners, surgical templates for implants and produce models that for the planning of treatment and preoperative positioning of the jaws.
Keywords: Additive manufacturing (AM), 3D scanning, Dentistry, Applications, Implants
1. Introduction
Additive manufacturing is used to create a 3D solid object directly from the digital 3D CAD data under computer control. Various areas of manufacturing such as industries, defence, aerospace, art, medical and design are adopting by additive manufacturing for customisation and rapid production. Nowadays, it has various applications in the field of dentistry in which manufacturing of personalised dentistry models is possible. The technology successfully produces drill guides for dental implants.1,2
AM process starts with a virtual image which is created by a 3D scanner or CAD software and generates product by different AM technologies. AM technologies fulfil the complex challenges in medical as well as in dentistry. These technologies are now available to improve patient outcomes. The two leading technologies prominent in the area of dentistry are stereolithography (SLA) generally used for aligner fabrication, and another is direct metal laser sintering (DMLS) which is capable of producing high-quality metal dental crown and appliance frames.3, 4, 5
Implant surgeries are performed mostly by hand. During this procedure, dentists first scan the patient's jaw and drill the patient's mouth by taking help of scanned image. This technique works on imagination so it is not so accurate.6,7 Additive manufacturing is a sophisticated method for pinpointing the best location to drill. It improves the accuracy of surgery by correctly creating an entire set of denture that comfortably fit in the patient's mouth. AM technology is now becoming accessible. It provides better health care and offers needful information for diagnosis and treatment to the dentist. It also has different applications in medical areas during performing of complex surgery which is helpful to improve patient outcome.8, 9, 10
2. Types of additive manufacturing technologies
The fundamental principle of AM is to directly create a 3D physical model by adding layer by layer technique from CAD model (generated with the help of designing software or by the 3D scanner, CT, MRI). There are various AM technologies used to build product layer by layer; each adopts different methods of production of the physical model as discussed below:
-
➢
Stereolithography (SLA): Products are built with the application of ultraviolet laser inside a vat of resin. Limited availability of materials useable with this technology as it uses light-sensitive polymers. It gives better surface finish and has lesser wastage of raw material.11,12
-
➢
Selective laser sintering (SLS): In this additive manufacturing technology, it accomplishes sintering with the application of a laser beam. The material used is in the form of powder, and laser sinters the powder.13,14
-
➢
Fused deposition modelling (FDM): Product is manufactured as similar to the extrusion process, where a heated thermoplastic material is added layer by layer to fabricate a model. In this process, the print head consists of multi-nozzle and extrudes different types of material at the same time.15,16
-
➢
Direct metal laser sintering (DMLS): This technology is used to produce metal parts with high accuracy and better mechanical strength. In this technology, the metal material is added layer by layer and a laser beam is used to fuse powder at a definite point.17,18
-
➢
Polyjet 3D printing (PJP): Undertaking the manufacture of part through UV-curable acrylic plastic. It uses various types of printing materials. In medical and dentistry field, model printed by this technology provides a better understanding of patient anatomy.19,20
-
➢
Inkjet 3D printing (IJP): This technology use different fluids such as polymer solution provided in the form of liquid and deposited layer by layer to built a product. It prints varieties of materials with less time and cost.21,22
-
➢
Laminated Object Manufacturing (LOM): 3D models are fabricated by adding layers of the defined sheet of materials. A laser is used to cut sheet material as per the required cross-section. Adhesives are used to combine the layers and generated by repeating the steps.23,24
-
➢
Colour-Jet-Printing (CJP): This technology uses powder as a core material, and binder as a resin and the part is built through spreading of core material in the layer, over the build platform using a roller. Printing head jets/spray binder (adhesive) on the powder layer at specified points as decided by the CAD software, thus a colourful product is built (printed) which has extensive usage in the medical field.25,26
-
➢
Electron Beam Melting (EBM): Powerful electron beam is used to build product layer by layer using a metal powder by command of the CAD model with exact geometry. Under a vacuum, the raw material is stored and fused by an electron beam.27,28
-
➢
Multi-Jet-Printing (MJP): In this technology, nozzles are used to spray binding of liquid onto metallic or ceramic powder to create a thin solid layer. After production of the model, it must be sintered in the furnace to increase the strength.29,30
All these additive manufacturing technologies offer different dental materials having different accuracy. Table 1 describes the different dental material, accuracy along with the pros and cons of each AM technology.
Table 1.
Additive manufacturing technologies with accuracy and its pros and cons with different dental materials.
| S No | AM technology | Approximate Accuracy | Dental Material | Pros | Cons |
|---|---|---|---|---|---|
| 1 | Stereolithography | 50–55 μm |
|
|
|
| 2 | Selective laser sintering | 45–50 μm |
|
|
|
| 3 | Fused deposition modelling | 35–40 μm |
|
|
|
| 4 | Direct metal laser sintering | 20–35 μm |
|
|
|
| 5 | Polyjet 3D printing | 20–85 μm |
|
|
|
| 6 | Inkjet 3D printing | 35–40 μm |
|
|
|
| 7 | Laminated Object Manufacturing | 60–70 μm |
|
|
|
| 8 | Colour-Jet-Printing | 23–30 μm |
|
|
|
| 9 | Electron Beam Melting | 40–50 μm |
|
|
|
| 10 | Multi-Jet Printing | 25–35 μm |
|
|
|
3D physical model printed by AM provides an accurate perception of a patient's anatomy to the dentist and the surgeon. Implants of a specific patient are created with geometric freedom and solve day to day challenges in dentistry.
3. Research questions
This article addresses the following research questions:
RQ1: To study different technologies of additive manufacturing, their accuracy, pros and cons with different dental materials.
RQ2: To identify relevant research papers on the additive manufacturing application in dentistry through Scopus and studied using bibliometric analysis.
RQ3: To study various benefits and steps used to create a 3D printed dental model using this technology.
RQ4: To identify significance applications of additive manufacturing in dentistry along with primary references and objectives.
4. Benefits of additive manufacturing in dentistry
In dentistry, there are various requirements for the patients; such as crown, implants and bridges. Various AM technologies are beneficial for dentistry. Binding jet technology is used to manufacture dental prostheses. Various parameters are taken such as drying powder level, binder amount, drying time and powder spreading speed. The result shows that it provides an accurate implant with low cost and better strength.31 Additive manufacturing is used to manufacture patient specific eruption guidance appliances, thereby increasing patient comfort and reducing overall cost of the model.32 Binding Jet 3D printing technology is used to produce partial denture by using metallic powder. Micro-computed tomography is used to scan the existing framework for obtaining a 3D printed model. The result shows that it helps to achieve more than 99% density with controlled shrinkage at a lesser cost. It is highly compatible to produce complex shape dental implant with exact dimensions.33 The comparison of the accuracy of dental restoration manufactured through additive manufacturing and subtractive manufacturing method using wax or zirconia milling is undertaken. The result shows that the accuracy of dental restorations manufactured by additive manufacturing technique is higher than that of subtractive methods. AM is also a digital method which stores inventory in digital form; as a result, it also reduced inventory cost.34 The experimental analysis for dimensional accuracy is done for teeth manufactured by FDM technique. The intraoral 3D scanner is used to create a 3D digital model and manufactured model by three different layer thicknesses. Dimensional accuracy of the model is evaluated by GOM Inspect software, which shows that the reducing layer thickness easily achieves a high level of accuracy.35 Additive manufacturing fulfils the customised requirements of dentistry in lesser time and cost.2,6,8,10 Following are the significant benefits obtained through the adoption of AM in dentistry:
-
•
Faster and accurate service
-
•
Cost-effective
-
•
Determine depth and width of teeth
-
•
Easily fabricate customised implants
-
•
Reduce fabrication time
-
•
With its digital storage, there is considerable inventory reduction of physical models
-
•
Rapidly produce custom design
-
•
Accurate sizing for implants
By using AM, the dentist can now use a variety of materials for prosthodontics such as ceramics and metal alloys. It produces dental model optimally with high accuracy.
5. Research status on additive manufacturing applications in dentistry
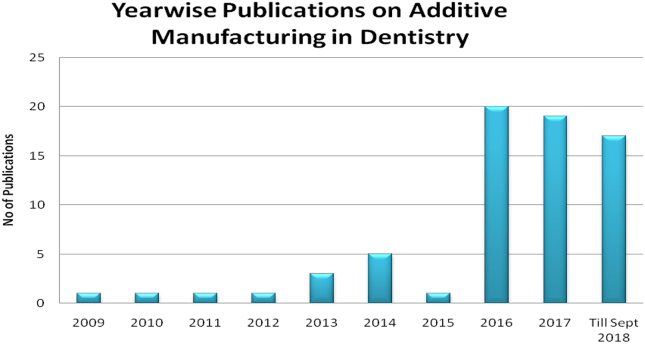
Identified research article related to this area through Scopus database till September 2018 by searching keywords as “Additive Manufacturing” Dentistry” and found 70 research articles published in this field. Here we observed from the data, that first paper got published in 2009, and now the number of publications has risen. Fig. 1 shows year-wise publications from 2009 to September 2018.
Fig. 1.
Additive manufacturing applications in dentistry: Year-wise publications (Source: Scopus).
Journal of Prosthetic Dentistry have highest publications of nine in this field by the application of AM. Dental Materials journal have two publications is at position 2. Biomed Research International, Rapid Prototyping Journal, Journal of Dental Research and various other journals have one each. By the application of AM in the field of dentistry, engineering area has maximum utilisation of 27%. However, dentistry contributes 23%, Materials Science 16%, Biochemistry, Genetics and Molecular Biology 11%, Medicine 5%, Computer science 3% and other areas also contribute 14%.
From Scopus data, it has analysed that applications of additive manufacturing are increasing in the area of dentistry. Thus these technologies/machines are becoming commercially viable and acceptable in the field of dentistry.
6. Steps used to create a 3D printed dental model using additive manufacturing
3D physical models build by the additive manufacturing technologies provide complete and better information to the surgeon. Table 2 discusses the various steps used to create 3D printed dental models.
Table 2.
Steps to create a 3D printed dental model by using additive manufacturing.
| S. No | Step used | Description | References |
|---|---|---|---|
| 1 | Digital 3D model of the patient's mouth |
|
Haleem and Javaid 201836; Kumar et al., 201837 |
| 2 | Modification in design |
|
Azari and Nikzad 200938; Tahmaseb et al., 201439 |
| 3 | 3D printing |
|
Kumar et al., 201640; Chang et al., 201541; Javaid and Haleem 201842 |
| 4 | Testing and Implementation |
|
Chen et al., 201443; Francisco et al., 201644 |
Dental 3D scanners are now available for designing implants (denture, prosthetics, or aligners). It consists of a light source and camera/s. Projector project light on the surface of the patient part and camera capture the data in the point cloud. It captures multiple images of the patient part and further merged these images to form a complete 3D digital model. This 3D digital model easily modifies design through the use of different software and easily printed by AM technologies.
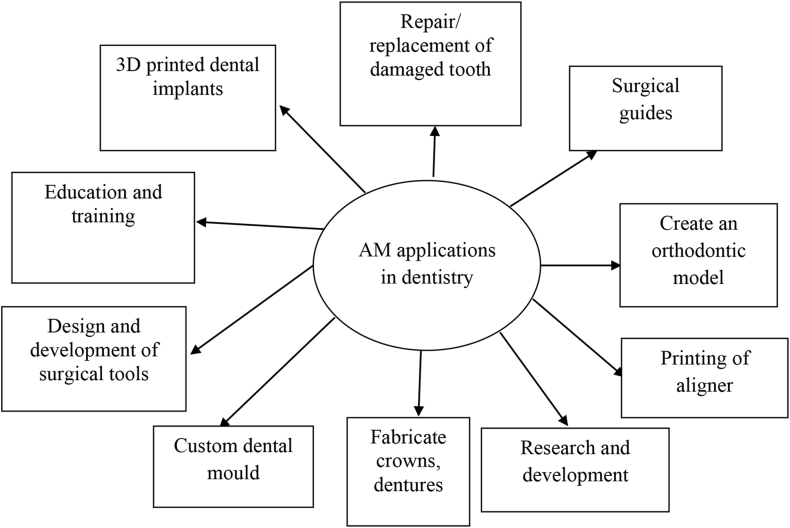
7. Applications of additive manufacturing in dentistry
Applications of AM help dental professional to fabricate any implant and dental devices. Technology can precisely help to improve the daily work of a dentist. It provides development in the medical field, and now it explores its applications in dentistry. Before performing actual surgery, preoperation can also be performed on the 3D model and analysed it. Fig. 2 shows ten major applications of additive manufacturing in dentistry.
Fig. 2.
-
•3D printed dental implants: During dental implant surgery, AM plays an essential role to provide the best solution for creating a template of 3D model which is helpful for the replacement of missing tooth. It improves the accuracy of the surgery as compared to the traditional method. This technique is economical and comfortable in which the dental model gets an excellent surface finish.45, 46, 47, 48
- •
- •
- •
- •
- •
-
•Fabricate crowns, dentures: This technology is used to fabricate crown rapidly. Patient teeth are scan and crown is directly printed that save time, and further can also be modified. It prints complete denture with gum and teeth. Multi-material is used to print and all kinds of dental implants and models. It uses explicit material for the printing process.63, 64, 65
- •
- •
-
•Education and training: It is important to train medical students for performing various clinical trial and practices. Product manufactured by this technology provide a better demonstration, as model fabricated by this technology is colourful, so it is useful in dentistry for teaching.71, 72, 73, 74
In dentistry, AM applications are used to improve patient outcomes. It is used for preoperative planning, education, custom manufacturing and make reliable operation. It produces permanent dentistry implants and devices for the patient.75,76
8. Discussion
Upcoming research & development is towards the production of elaborate dental crowns, aligner, surgical templates, bridges, and orthodontic braces as per requirement of the individual patient. This technology creates an on-demand production of customised dental implants. It has the potential to design & develop tools for dentist and surgeons. AM can help produce complex shaped dental implants/prototype with a wide variety of materials which makes surgeon's job easier with minimum side effects because a 3D printed model gives a better understanding of complex pathology & anatomy of patients which is also suitable for surgical training. Observed there is an improvement in the quality of patient life and efficiently solve different problems in dentistry. Surgeons can now print an implant to practice before the surgery. The dentist can convert need/idea into a reality which provides a comprehensive opportunity to manufacture modified dental implant as per requirement of the patient. It save time for the dental technician and provides improved opportunities to create a new dental product.
9. Future scope
In future, AM can print low-cost, functional dentures using multiple biocompatible materials. It can give a fully printable denture solution. AM is rapidly evolving with new materials. Prosthodontics physical models and any customised, low-cost dental implants seem to be viable. AM technologies can enable collaboration among clinician and laboratory and help to provide a perfect solution for the production of various types of customised medical and dentistry models. The potential of this technology is that if any model does not fit, we can make design changes as per requirement and then print it. In future, this technology rapidly will create digital dentistry.
10. Conclusion
Additive manufacturing technologies provide innovation in the manufacturing of complex and mass customised dental implants with negligible wastages. Easy scanning of the Patient-specific dental parts by the dental 3D scanner assists quick printing of personalised dental model with high accuracy. The dentist uses this digital technology for research purpose in which a prototype is created and tested. In upcoming years, this technology will bring a more dental product for a dentistry lab. The dentist can take advantages of this technology for replacement of teeth, crown, braces, dentures, veneers and aligner. Now the dentist can scan the patient mouth, and directly email the scanned file to the 3D printer lab and hence create a 3D printed model which fits the patient's mouth. It will be quite helpful during complicated cases when different surgical guide models are possible for the surgeon dentist. AM seems to have the potential to solve various problems in this field such as customised requirement, denture positioning and denture retention and improve existing dental implants.
Conflict to interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jobcr.2019.04.004.
Contributor Information
Mohd Javaid, Email: mjavaid@jmi.ac.in, https://scholar.google.co.in/citations?user=rfyiwvsAAAAJ&hl=en.
Abid Haleem, Email: ahaleem@jmi.ac.in, https://scholar.google.co.in/citations?user=4047148AAAAJ&hl=en.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Javaid M., Haleem A. Additive manufacturing applications in medical cases: a literature-based review. Alexandria J Med. 2017;54(4):411–422. doi: 10.1016/j.ajme.2017.09.003. [DOI] [Google Scholar]
- 2.Duta M., Caraiane A. vol. 3. 2017. Advances in 3D printing in dentistry; pp. 49–54. (4th International Multidisciplinary Scientific Conference on Social Sciences and Arts SGEM). [Google Scholar]
- 3.Centenero S.A., Hernandez-Alfaro F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results - our experience in 16 cases. J Cranio-Maxillofacial Surg. 2012;40(2):162–168. doi: 10.1016/j.jcms.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 4.Logozzo S., Zanetti E.M., Franceschini G., Makynen A. Recent advances in dental optics – Part I: 3D intraoral scanners for restorative dentistry. Optic Laser Eng. 2014;54:203–221. [Google Scholar]
- 5.Chang Y.C., Shieh Y.S., Lee S.P. Chronic osteomyelitis with proliferative periostitis in the lower jaw. J Dent Sci. 2015;10:450–455. [Google Scholar]
- 6.Dawood A., Marti B.M., Sauret-Jackson V., Darwood A. 3D printing in dentistry. Br Dent J. 2015;219(11):521–529. doi: 10.1038/sj.bdj.2015.914. [DOI] [PubMed] [Google Scholar]
- 7.Esposito M., Ardebili Y., Worthington H.V. Interventions for replacing missing teeth: different types of dental implants. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD003815.pub4. [DOI] [PubMed] [Google Scholar]
- 8.Chawla K. 3D bioprinting: technology in dentistry. Int J Dent Res Oral Sci. 2017;2(2):63–64. [Google Scholar]
- 9.Javaid M., Haleem A. Additive manufacturing applications in orthopaedics: a review. J Clin Orthop Trauma. 2018;9(3):202–2006. doi: 10.1016/j.jcot.2018.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coachman C., Calamita M.A., Coachman F.G., Coachman R.G., Sesma N. Facially generated and cephalometric guided 3D digital design for complete mouth implant rehabilitation: a clinical report. J Prosthet Dent. 2017;117(5):577–586. doi: 10.1016/j.prosdent.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Zheng Y., Wang Y., Chen R.K. Tissue transformation mold design and stereolithography fabrication. Rapid Prototyp J. 2017;23(1):162–168. [Google Scholar]
- 12.Ye H., Venketeswaran A., Das S., Zhou C. Investigation of separation force for constrained-surface stereolithography process from mechanics perspective. Rapid Prototyp J. 2017;23(4):696–710. [Google Scholar]
- 13.Mazzoli A., Ferretti C., Gigante A., Salvolini E., Mattioli-Belmonte M. Selective laser sintering manufacturing of polycaprolactone bone scaffolds for applications in bone tissue engineering. Rapid Prototyp J. 2015;21(4):386–392. [Google Scholar]
- 14.Butler J. Using selective laser sintering for manufacturing. Assemb Autom. 2011;31(3):212–219. [Google Scholar]
- 15.Taylor A.C., Beirne S., Alici G., Wallace G.G. System and process development for coaxial extrusion in fused deposition modelling. Rapid Prototyp J. 2017;23(3):543–550. [Google Scholar]
- 16.Heras E.S., Haro F.B., Burgo J.M.A., Marcos M.E.I. Plate auto-level system for fused deposition modelling (FDM) 3D printers. Rapid Prototyp J. 2017;23(2):401–413. [Google Scholar]
- 17.Alsalla H.H., Smith C., Hao L. The effect of different build orientations on the consolidation, tensile and fracture toughness properties of direct metal laser sintering Ti-6Al-4V. Rapid Prototyp J. 2018;24(2):276–284. [Google Scholar]
- 18.Salmi M., Tuomi J., Paloheimo K.S. Patient-specific reconstruction with 3D modeling and DMLS additive manufacturing. Rapid Prototyp J. 2012;18:209–214. [Google Scholar]
- 19.Javaid M., Kumar L., Kumar V., Haleem A. Product design and development using Polyjet rapid prototyping technology. Int J Control Theory Inf. 2015;5:12–19. [Google Scholar]
- 20.Moore J.P., Williams C.B. Fatigue properties of parts printed by PolyJet material jetting. Rapid Prototyp J. 2015;21:675–685. [Google Scholar]
- 21.Begines B., Hook A.L., Alexander M.R., Tuck C.J., Wildman R.D. Development, printability and post-curing studies of formulations of materials resistant to microbial attachment for use in inkjet-based 3D printing. Rapid Prototyp J. 2016;22(5):835–841. [Google Scholar]
- 22.Cummins G., Desmulliez M.P.Y. Inkjet printing of conductive materials: a review. Circuit World. 2012;38(4):193–213. [Google Scholar]
- 23.Chiu Y.Y., Liao Y.S. Laser path planning of burn‐out rule for LOM process. Rapid Prototyp J. 2003;9(4):201–211. [Google Scholar]
- 24.Kechagias J., Maropoulos S., Karagiannis S. Process build‐time estimator algorithm for laminated object manufacturing. Rapid Prototyp J. 2004;10(5):297–304. [Google Scholar]
- 25.Yuan J., Zhu M., Xu B., Chen G. Review on processes and color quality evaluation of color 3D printing. Rapid Prototyp J. 2018;24(2):409–415. [Google Scholar]
- 26.Gardan J. Method for characterization and enhancement of 3D printing by binder jetting applied to the textures quality. Assemb Autom. 2017;37(2):162–169. [Google Scholar]
- 27.Cronskär M., Bäckström M., Rännar L.E. Production of customized hip stem prostheses – a comparison between conventional machining and electron beam melting (EBM) Rapid Prototyp J. 2013;19(5):365–372. [Google Scholar]
- 28.Petrovic V., Niñerola R. Powder recyclability in electron beam melting for aeronautical use. Aircraft Eng Aero Technol: Int J. 2015;87(2):147–155. [Google Scholar]
- 29.Bass L., Meisel N.A., Williams C.B. Exploring variability of orientation and aging effects in material properties of multi-material jetting parts. Rapid Prototyp J. 2016;22(5):826–834. [Google Scholar]
- 30.Chen H., Zhao Y.F. Process parameters optimization for improving surface quality and manufacturing accuracy of binder jetting additive manufacturing process. Rapid Prototyp J. 2016;22(3):527–538. [Google Scholar]
- 31.Miyanaji H., Zhang S., Lassell A., Zandinejad A., Yang L. Process development of porcelain ceramic material with binder jetting process for dental applications. Miner. Met.Mater.Soc. 2016;68(3):831–841. [Google Scholar]
- 32.Barone S., Neri P., Paoli A., Razionale A.V. Design and manufacturing of patient-specific orthodontic appliances by computer-aided engineering techniques. J Eng Med. 2018;232(1):54–66. doi: 10.1177/0954411917742945. [DOI] [PubMed] [Google Scholar]
- 33.Mostafaei A., Stevens E.L., Ference J.J., Schmidt D.E., Chmielus M. 2018. Binder Jetting of a Complex-Shaped Metal Partial Denture Framework. Additive manufacturing. [DOI] [Google Scholar]
- 34.Bae E.J., Jeong D., Kim W.C., Kim J.H. A comparative study of additive and subtractive manufacturing for dental restorations. J Prosthet Dent. 2017;118(2):187–193. doi: 10.1016/j.prosdent.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 35.Milde J., Morovic L., BlahaJ Influence of the layer thickness in the Fused Deposition Modeling process on the dimensional and shape accuracy of the upper teeth model. MATEC Web Conf. 2017 [Google Scholar]
- 36.Haleem A., Javaid M. 3D scanning applications in medical field: a literature-based review. Clin Epidemiol Global Health. 2018 doi: 10.1016/j.cegh.2018.05.006. [DOI] [Google Scholar]
- 37.Kumar L., Shuaib M., Tanveer Q., Kumar V., Javaid M., Haleem A. 3 D scanner integration with product development. Int J Eng Technol. 2018;7(2):220–225. [Google Scholar]
- 38.Azari A., Nikzad S. The evolution of rapid prototyping in dentistry: a review. Rapid Prototyp J. 2009;15:216–222. [Google Scholar]
- 39.Tahmaseb A., Wismeijer D., Coucke W., Derksen W. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implant. 2014;29:25–42. doi: 10.11607/jomi.2014suppl.g1.2. [DOI] [PubMed] [Google Scholar]
- 40.Kumar L., Tanveer Q., Kumar V., Javaid M., Haleem A. Developing low cost 3 D printer. Int J Appl Sci Eng Res. 2016;5:433–447. [Google Scholar]
- 41.Chang S., Lo C., Jiang C., Juan D. The fit consideration of the denture manufactured by 3D printing and sintering. Int Pharm J Med Biol Sci. 2015;4:184–187. [Google Scholar]
- 42.Javaid M., Haleem A. Current status and challenges of Additive manufacturing in orthopaedics: an overview. J Clin Orthop Trauma. 2018;10(2):380–386. doi: 10.1016/j.jcot.2018.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen J., Zhang Z., Chen X., Zhang C., Zhang G., Xu Z. Design and manufacture of customized dental implants by using reverse engineering and selective laser melting technology. J Prosthet Dent. 2014;112:1088–1095. doi: 10.1016/j.prosdent.2014.04.026. [DOI] [PubMed] [Google Scholar]
- 44.Francisco V., Jessica S., Joao C. 3D virtual planning in orthognathic surgery and CAD/CAM surgical splints generation in one patient with craniofacial microsomia: a case report. Dent Press J Orthod. 2016;21(1):89–100. doi: 10.1590/2177-6709.21.1.089-100.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tunchel S., Blay A., Kolerman R., Mijiritsky E., Shibli J.A. 3D printing/additive manufacturing single titanium dental implants: a prospective multicenter study with 3 years of follow-up. Int J Dentistry. 2016;2016:1–9. doi: 10.1155/2016/8590971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Flügge T.V., Nelson K., Schmelzeisen R., Metzger M.C. Three-dimensional plotting and printing of an implant drilling guide: simplifying guided implant surgery. J Oral Maxillofac Surg. 2013;71:1340–1346. doi: 10.1016/j.joms.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 47.Klammert U., Gbureck U., Vorndran E., R€odiger J., Meyer-Marcotty P., K€ubler A.C. 3D powder printed calcium phosphate implants for reconstruction of cranial and maxillofacial defects. J Cranio-Maxillofacial Surg. 2010;38:565–570. doi: 10.1016/j.jcms.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 48.Chiang M.T., Li T., Yeh H.W. Evaluation of missing-tooth effect on articular eminence inclination of temporomandibular joint. J Dent Sci. 2015;10:383–387. [Google Scholar]
- 49.Javaid M., Haleem A., Kumar L. Current status and applications of 3D scanning in dentistry. Clin Epidemiol Global Health. 2018 [Google Scholar]
- 50.Moin D.A., Derksen W., Verweij J., van Merkesteijn R., Wismeijer D. A novel approach for computer-assisted template-guided auto transplantation of teeth with custom 3D designed/printed surgical tooling. An ex vivo proof of concept. J Oral Maxillofac Surg. 2016;74(5):895–902. doi: 10.1016/j.joms.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 51.Yamamoto S., Kanazawa M., Iwaki M., Jokanovic A., Minakuchi S. Effects of offset values for artificial teeth positions in CAD/CAM complete denture. Comput Biol Med. 2017;52:1–7. doi: 10.1016/j.compbiomed.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 52.Van Assche N., van Steenberghe D., Guerrero M.E. Accuracy of implant placement based on pre-surgical planning of three-dimensional cone-beam images: a pilot study. Clin Periodontol. 2007;34:816–821. doi: 10.1111/j.1600-051X.2007.01110.x. [DOI] [PubMed] [Google Scholar]
- 53.Xia J., Ip H.H., Samman N. Computer_assisted three-dimensional surgical planning and simulation: 3D virtual osteotomy. Int J Oral Maxillofac Surg. 2000;29(1):11–17. [PubMed] [Google Scholar]
- 54.Li H., Song L., Sun J., Ma J., Shen Z. Dental ceramic prostheses by stereolithography based additive manufacturing: potentials and challenges. Adv Appl Ceram. 2018 doi: 10.1080/17436753.2018.1447834. [DOI] [Google Scholar]
- 55.Bhargav A., Sanjairaj V., Rosa V., Feng L.W., Fuh Yh J. Applications of additive manufacturing in dentistry: a review. J Biomed Mater Res B Appl Biomater. 2017 doi: 10.1002/jbm.b.33961. [DOI] [PubMed] [Google Scholar]
- 56.Liu Q., Leu M., Schmitt S. Rapid prototyping in dentistry: technology and application. Int J Adv Manuf Technol. 2006;29:317–335. [Google Scholar]
- 57.Evans J.W., Desai P.S. Applications for three-dimensional printing in dentistry. J Multidiscip Care. 2016 http://decisionsindentistry.com/article/applications-three-dimensional-printing-dentistry/ [Google Scholar]
- 58.Soares P.V., de Almeida Milito G., Pereira F.A. Rapid prototyping and 3D-Virtual models for operative dentistry education in Brazil. J Dent Educ. 2013;77(3):358–363. [PubMed] [Google Scholar]
- 59.Chan D.C.N., Frazier K.B., Tse L., Rosen D. Application of rapid prototyping to operative dentistry curriculum. J Dent Educ. 2004;68(1):64–70. [PubMed] [Google Scholar]
- 60.Kurenov S.N., Ionita C., Sammons D., Demmy T.L. Three-dimensional printing to facilitate anatomic study, device development, simulation, and planning in thoracic surgery. J Thorac Cardiovasc Surg. 2015;149:973–979. doi: 10.1016/j.jtcvs.2014.12.059. [DOI] [PubMed] [Google Scholar]
- 61.Haleem A., Javaid M. Role of CT and MRI in the design and development of orthopaedic model using additive manufacturing. J Clin Orthop Trauma. 2018;9(3):213–217. doi: 10.1016/j.jcot.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Singh R.P., Kataria R., Singhal S. Performance evaluation of macor dental ceramic: an investigation with rotary ultrasonic machining. Adv Dent Oral Health. 2018;8(2):1–6. [Google Scholar]
- 63.Miyazaki T., Hotta Y. CAD/CAM systems available for the fabrication of crown and bridge restorations. Aust Dent J. 2011;56:97–106. doi: 10.1111/j.1834-7819.2010.01300.x. [DOI] [PubMed] [Google Scholar]
- 64.Kapos T., Evans C. CAD/CAM technology for implant abutments, crowns, superstructures. Int J Oral Maxillofac Implant. 2014;29:117–136. doi: 10.11607/jomi.2014suppl.g2.3. [DOI] [PubMed] [Google Scholar]
- 65.Bibb R., Eggbeer D., Williams R. Rapid manufacture of removable partial denture frameworks. Rapid Prototyp J. 2006;12(2):95–99. [Google Scholar]
- 66.Harris B.D., Nilsson S., Poole C.M. A feasibility study for using ABS plastic and a low-cost 3D printer for patient-specific brachytherapy mould design. Australas Phys Eng Sci Med. 2015;38:399–412. doi: 10.1007/s13246-015-0356-3. [DOI] [PubMed] [Google Scholar]
- 67.Dawood A., Patel S., Brown J. Cone beam CT in dental practice. Br Dent J. 2009;207:23–28. doi: 10.1038/sj.bdj.2009.560. [DOI] [PubMed] [Google Scholar]
- 68.Kaeppler G. Applications of cone beam computed tomography in dental and oral medicine. Int J Comput Dent. 2010;13:203–219. [PubMed] [Google Scholar]
- 69.Takemoto M., Fujibayashi S., Ota E. Additive-manufactured patient-specific titanium templates for thoracic pedicle screw placement: novel design with reduced contact area. Eur Spine J. 2015;25(6):1698–1705. doi: 10.1007/s00586-015-3908-z. [DOI] [PubMed] [Google Scholar]
- 70.Singh R.P., Singhal S. Rotary ultrasonic machining of macor ceramic: an experimental investigation and microstructure analysis. Mater Manuf Process. 2017;32(9):927–939. [Google Scholar]
- 71.Negi S., Dhiman S., Sharma R.K. Basics and applications of rapid prototyping medical models. Rapid Prototyp J. 2014;20:256–267. [Google Scholar]
- 72.Karageorgiou V., Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials. 2005;26(27):5474–5491. doi: 10.1016/j.biomaterials.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 73.Mehrotra D. Dentistry: changing paradigm with growth of basic sciences. J Oral Biol Craniofac Res. 2014;4(3):159. doi: 10.1016/j.jobcr.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mehrotra D. Oral sciences: history and future research. J Oral Biol Craniofac Res. 2014;4(2):69. doi: 10.1016/j.jobcr.2014.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moin D.A., Derksen W., Verweij J., van Merkesteijn R., Wismeijer D. A novel approach for computer-assisted template-guided auto transplantation of teeth with custom 3D designed/printed surgical tooling. An ex vivo proof of concept. J Oral Maxillofac Surg. 2016;74(5):895–902. doi: 10.1016/j.joms.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 76.Anadioti E., Kane B., Soulas E. Current and emerging applications of 3D printing in restorative dentistry. Curr Oral Health Rep. 2018;5(2):133–139. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.