Abstract
Acute kidney injury (AKI) is a clinical syndrome characterized by a rapid loss of renal function, which may further develop into chronic kidney damage (CKD) or even end-stage renal disease (ESRD). AKI is a global health problem associated with high morbidity and costly treatments, and there is no specific or effective strategy to treat AKI. In recent years, Traditional Chinese Medicine (TCM) has attracted more attention, with lines of evidence showing that application of TCM improved AKI, and the mechanisms of action for some TCMs have been well illustrated. However, reviews summarizing the progress in this field are still lacking. In this paper, we reviewed TCM preparations and TCM monomers in the treatment of AKI over the last 10 years, describing their renal protective effects and mechanisms of action, including alleviating inflammation, programmed cell death, necrosis, and reactive oxygen species. By focusing on the mechanisms of TCMs to improve renal function, we provide effective complementary evidence to promote the development of TCMs to treat AKI. Moreover, we also summarized TCMs with nephrotoxicity, which provides a more comprehensive understanding of TCMs in the treatment of AKI. This review may provide a theoretical basis for the clinical application of TCMs in the future.
Keywords: acute kidney injury (AKI), traditional Chinese medicine (TCM), inflammation, apoptosis, nephrotoxicity
Introduction
Acute kidney injury (AKI), characterized by an abrupt decline of renal function, can be induced by numerous causes including renal ischemia reperfusion injury (IRI), nephrotoxic insults and infection of sepsis (Waikar et al., 2008; Linkermann, 2016). Accumulating evidence shows that AKI is a global public health concern and a pivotal threat to human health, especially in hospitalized patients, as it impacts more than 13 million patients per year (Chertow et al., 2005; Lameire et al., 2013; Thomas et al., 2015; Yang et al., 2015; Allison, 2016). Excessive inflammatory responses, oxidative stress, and the imbalance of the damage and repair of renal tubules, are all highly involved in the pathological process of AKI, however, specific targets and effective therapies are still lacking (Sancho-Martinez et al., 2015; Yang et al., 2016; Zuk and Bonventre, 2016).
Traditional Chinese medicine (TCM) has been widely used for the treatment of AKI and its complications in China and neighboring countries, including Japan and Korea, for a long time. Some TCM-based therapies show good results and high efficacy in inhibiting inflammatory responses, programmed cell death and oxidative stress. In this regard, the therapeutic effects of TCMs have widely been tested in animal models of AKI and even in patients. For instance, the Xuebijing Injection is effective in improving clinical symptoms of sepsis-induced AKI patients after the Wenchuan Earthquake (Yuxi et al., 2017). Our recent study showed that wogonin not only protects cisplatin-induced AKI, but also preserves and even promotes the anti-tumor effect of cisplatin (Meng et al., 2018). However, it is noteworthy that some TCMs, such as aristolochic acids and other plant alkaloids, are nephrotoxic, (Yang et al., 2018). So, the application of TCM should be carefully evaluated.
In this paper, we reviewed the therapeutic effects of TCMs on AKI and the mechanism of action based on the assessment of evidence that supports hypotheses, additionally, TCMs with nephrotoxicity have also been discussed.
Applications of TCM in AKI
TCM Preparations in AKI
Until now, several TCM preparations have been tested in the treatment of AKI. There are shown in Table 1.
Table 1.
Application of TCM Preparations in the treatment of acute kidney injury.
| Names | Origins | Models | Function | Mechanisms |
|---|---|---|---|---|
| A&A | Astragalus membranaceus var. mongholicus and Angelica sinensis | I/R-induced kidney injury | Decreasing cell necrosis | By inducing JNK (Cai et al., 2001; Meng et al., 2007) |
| DFD | Radix et Rhizoma Rhei, Radix Aconiti Lateralis Praeparata, and Radix et Rhizoma Asari | Adenine-induced renal injury | Inhibiting apoptosis | By blocking TGF-β1-JNK (Tu et al., 2014) |
| Xuebijing injection | Radix paeoniae rubra, Chuan dome, Salvia miltiorrhiza, Safflower, and Chinese angelica | Serious scald-induced renal injury | Alleviating renal function | By suppressing HMGB1 (Wang et al., 2007) |
| HLJDD | Rhizoma coptidis (RC), Cortex phellodendri (CP), Radix scutellariae (RS), and Fructus gardenia | LPS-induced AKI | Attenuating apoptosis | Activating the Akt/HO-1 pathway and inhibiting NF-kB and MAPK activation (Li et al., 2017) |
| ZDW | Cornus officinalis Siebold & Zucc., Radix Rehmanniae preparata, Dioscorea oppositifolia L., Cortex Phellodendri, rhizome, Moutan Cortex, Rhizoma Alismatis, and Wolf | Gentamicin-induced renal injury | Attenuating apoptosis | By limiting caspase-3 activation (Hsu et al., 2014) |
Astragalus membranaceus var. mongholicus and Angelica sinensis (A&A)
Decoctions of roots from A&A can improve renal blood flow in a murine model of acute ischemic renal injury, possibly by increasing NO production by activating eNOS and scavenging ROS, therefore accelerating renal repair after ischemic injury (Meng et al., 2007). Moreover, the therapeutic effect of A&A may be JNK-dependent (Cai et al., 2001).
Dahuang Fuzi Decoction (DFD)
Dahuang Fuzi Decoction (DFD) consists of Radix et Rhizoma Rhei, Radix Aconiti Lateralis Praeparata, and Radix et Rhizoma Asari. Emerging evidence indicates that DFD attenuates adenine-triggered renal damage and tubular epithelial apoptosis, by blocking the activation of TGF-β1-JNK pathways (Tu et al., 2014).
Xuebijing Injection
It consists of chuan dome, radix paeoniae rubra, safflower, Salvia miltiorrhiza, and Chinese angelica. Administration of a Xuebijing injection can suppress the production and release of high mobility group box-1 protein (HMGB1) in the kidney, thereby alleviating serious scald injury-induced AKI (Wang et al., 2007). In addition, an intravenous injection of Xuebijing attenuates the inflammatory response in AKI rats with paraquat poisoning (Xu et al., 2017). Importantly, Xuebijing improved the clinical symptoms of patients with sepsis-induced AKI after the Wenchuan Earthquake (Yuxi et al., 2017).
Huang-Lian-Jie-Du-Decoction (HLJDD)
It is composed of Rhizoma coptidis (RC), Cortex phellodendri (CP), Radix scutellariae (RS), and Fructus gardenia by a weight ratio of 3:2:2:3. HLJDD effectively suppresses LPS-induced AKI by activating Akt/HO-1 pathway and inhibiting NF-κB and MAPK activation in mice (Li et al., 2017).
Zhibai Dihuang Wan (ZDW)
ZDW is a polyherbal formula mixed with Rehmannia glutinosa (Gaertn.) DC, baked (Radix Rehmanniae preparata), Cornus officinalis Siebold & Zucc., Dioscorea oppositifolia L., Paeonia suffruticosa Andrews, Alisma plantago-aquatica L., rhizome (Rhizoma Alismatis), and Poria cocos (Schw.) Wolf. ZDW has been used to treat chronic kidney diseases, like diabetic nephropathy, for many years. A recent study revealed that ZDW also protected against gentamicin-induced AKI both in vivo and in vitro, because it attenuated apoptosis of renal tubular epithelial cells by limiting caspase-3 activation (Hsu et al., 2014).
TCM Monomers in AKI
Compared with TCM preparations, TCM Monomers have recently attracted more attention in the treatment of diseases because they have certain molecular structures, clear mechanisms of action, predicted pharmacological effects and less drug-drug interactions. In the kidney, numerous TCM monomers have been applied in treating renal diseases including AKI caused by different stimuli. Therefore, we list TCMs that have comprehensively been studied to protect against AKI in recent years.
Astaxanthin (ATX)
Astaxanthin (ATX) is a natural carotenoid extracted from marine organisms which are widely applied because of their strong antioxidant effect. Current studies demonstrate the renoprotective effects of ATX in many AKI models. ATX (5 mg/kg for 14 days via oral gavage) can improve I/R-induced AKI by exerting antioxidant activity and inhibiting tubular apoptosis/necrosis via scavenging free radicals (Qiu et al., 2015). Moreover, ATX (40 mg/kg for 5 days by intraperitoneal injection) attenuated arsenic-induced AKI by fulfilling antioxidant functions and reducing As accumulation (Wang et al., 2014), and ATX (50 mg/kg for 12 h by gavage) ameliorated HgCl2-induecd AKI by exerting anti-oxidant activity and preventing lipid and protein oxidation (Augusti et al., 2008). ATX (20 mg/kg 12 h via tail intravenous injection) consistently improved early AKI, following a severe burn, by modulating antioxidant activity and Akt/Bad/Caspases-mediated mitochondrial-apoptotic pathway (Guo et al., 2015).
Baicalin
Baicalin is a Scutellaria baicalensis-derived flavonoid which has been tested in multiple types of AKI models. In clinical trials, Baicalin protects against AKI in pediatric sepsis by inhibiting renal cell apoptosis (Zhu et al., 2016). In ischemia-reperfusion injured kidney, Baicalin (10 μmol/L for 24 h) exerts protective effects by inhibiting TLR2/4-mediated inflammation and mitochondrial stress-induced apoptosis of tubular epithelial cells (Ji et al., 2014). Administration of Baicalin (100 μmol/L) in HK-2 cells consistently reduced H2O2-induced cytotoxicity by activating downstream Nrf2 signaling and attenuating ER stress (Lin et al., 2014). These findings are supported by recent findings that Baicalin (50 mg/kg, i.p. for 2 weeks) prevents Lead (Pb)-induced renal injury and pediatric sepsis-induced AKI by blocking oxidative stress and apoptosis (Zhang et al., 2016; Zhu et al., 2016). Moreover, it is of note that baicalin is a novel PPAR-γ activator which may suppress NF-κB-mediated inflammation effectively (Lim et al., 2012).
Cordyceps sinensis (CS)
Cordyceps sinensis (CS) is used as a tonic food which is derived from an entomogenous fungus (Zhu et al., 1998). CS (5 g/kg via intragastric for 2 days) improves the outcome of I/R-induced AKI via different mechanisms including modulating SDF-1/CXCR4-signaling axis (Wang et al., 2013), up-regulating expression of HIF-1α, down-regulating the expression of NGAL (Yu et al., 2012) and reducing the expression level of TLR-4 (Zhou and Hu, 2010). Moreover, treatment of CS (1.5 mg/200 μl) significantly alleviates stress responses and tissue damage by reducing autophagy and apoptosis in LPS-induced AKI (Wu et al., 2011). Additionally, CSP, as the mycelia glycoproteins of Cordyceps sobolifera, significantly suppresses cyclosporine A (CsA)-induced apoptosis and protects against nephron loss via increasing magnesium reabsorption (Chyau et al., 2014).
Epigallocatechin Gallate (EGCG)
As a major component of green tea, EGCG is famous for its anti-inflammatory and anti-apoptotic properties. EGCG, as a potent inducer of HO-1, can suppress renal injury by reducing oxidative stress and inflammation in several AKI models induced by contrast (EGCG 20 mg/kg intravenously) (Gao Z. et al., 2016), I/R (EGCG 50 mg/kg i.p. for 24 h) (Lv et al., 2015) and cisplatin (EGCG 100 mg/kg i.p. for 12 days) (Sahin et al., 2010), respectively. Furthermore, underlying mechanisms have extensively been explored in cisplatin nephropathy, EGCG (100 mg/kg i.p. for 2 days) prevented activation of ERK, the NF-κB pathway and caspase-12 while down-regulating the Fas-conducted extrinsic pathway and Bcl-2/Bax ratio, thereby reducing the apoptosis of tubular epithelial cells (Zou et al., 2014; Chen B. et al., 2015; Pan et al., 2015).
Ginsenoside Rd (GSRd)
Ginsenoside Rd (GSRd) is isolated from the root of Panax ginseng and applied to protect cells in various types of diseases especially ischemia diseases (Ye et al., 2011). It is noteworthy that GSRd has an impact on different cell types which are involved in AKI. For instance, previous studies identified that GSRd (50 mg/kg i.p. for 2 days) prevented M1 macrophage polarization in I/R-injured kidney (Ren et al., 2016). Additionally, GSRd (5 mg/kg i.p. for 30 days) protected proximal tubule cells against I/R model-induced hypoxia-reoxygenation by inhibiting oxygen free radicals from attacking cell membranes (Yokozawa et al., 1998). The renoprotective effect of GSRd (5 mg/kg i.p. for 30 days) was further determined in cisplatin and glycerol-induced AKI models, treatment of GSRd decreased apoptosis-triggered DNA fragmentation and oxidative stress (Yokozawa and Liu, 2000; Yokozawa and Dong, 2001; Zhou et al., 2014). Other Ginsenosides, such as Rb1, Rg1 (80 mg/L for 24 h) and Rg3 also proved to be effective in the treatment of AKI. It has been identified that administration of Ginsenoside Rb1 relieves apoptosis of HK-2 cells in response to serum from I/R AKI (Zhu et al., 2009). Ginsenoside Rg1 reduces aldosterone-induced oxidative stress and abnormal autophagy correlates with AMPK/mTOR pathway. Ginsenosides 20(S)-Rg3 exerts therapeutic effects in both cisplatin (GSRd 250 μg/mL for 24 h) and LPS (GSRd 10 mg/kg i.p. for 15 days)-induced AKI by targeting JNK-p53-caspase-3 axis and NF-κB signaling pathway (Kang et al., 2007; Wang et al., 2015; Han et al., 2016).
Resveratrol (RSV)
Resveratrol (RSV), a popular natural phenolic compound which is abundant in wines and grape skins, protects against multiple types of AKI due to its low toxicity, powerful antioxidants, and anti-inflammatory properties. Resveratrol (100 mg/kg for 20 h by oral gavage) can attenuate LPS-induced AKI by suppressing inflammation and apoptosis driven by macrophages (Chen L. et al., 2015). Resveratrol (10 mg/kg i.p. for 12 h) consistently protects against sepsis-induced tubular epithelium injury by restoring the renal microcirculation and scavenging reactive nitrogen species (Holthoff et al., 2012). In addition, resveratrol (3 mg/kg for 6 days via the forearm vein) ameliorates arsenic trioxide (As2O3)-induced nephrotoxicity by antagonizing oxidative stress and facilitating arsenic metabolism (Yu et al., 2013). Moreover, resveratrol is proven to be an anti-inflammatory agent in glycerol (RSV 25 mg/kg/day for 4 days via gastric intubation)- and cisplatin (RSV 25 mg/kg/day i.p. for 2/5 days)-induced AKI (de Jesus Soares et al., 2007; Do Amaral et al., 2008). Furthermore, previous studies demonstrated that resveratrol-mediated activation of SIRT1 improved cisplatin (RSV 10 mg/kg orally once a day for 7 days)-induced AKI by deacetylating p53 and reducing apoptosis (Kim et al., 2011), and RSV also inhibited sepsis (RSV 10 mg/kg i.p. for 3 days)-induced AKI and renal inflammation through NF-κB de-acetylation (Gan et al., 2017) or SIRT3-mediated deacetylation of SOD2 (Xu et al., 2016). Resveratrol (30 mg/kg i.p. for 12 h) protected against early sepsis-induced AKI by inhibiting the endoplasmic reticulum stress (IRE1)-activated NF-κB pathway (Wang et al., 2017). A previous study showed that RSVA405 (3 mg/kg i.p. for 24 h) and RSVA314 (3 mg/kg i.p. for 24 h), two biologically active resveratrol analogs (RSVAs), attenuated I/R-induced AKI by exerting anti-oxidative and anti-inflammatory effects, indicating that RSV and its derivatives may be promising agents to prevent and/or treat AKI with high efficiency (Khader et al., 2015).
Tetramethylpyrazine (TMP)
Tetramethylpyrazine (TMP) is a natural product isolated from the Chinese herb Ligusticum wallichii Franch., which is famous for its antioxidative and anti-inflammatory effects. Previous studies showed that treatment with TMP protects against arsenic (TMP 100 μM for 6 h)-induced nephrotoxicity by targeting HO-1 and ARS2, which was further evidenced by the findings that TMP (20 mg/kg/day i.p. for 7 days) relieves gentamicin-induced AKI by enhancing Hax-1 mitochondrial localization in HO-1-dependent mechanisms (Sue et al., 2009; Gong et al., 2016). Additionally, by suppressing ROS production and the consequential inflammatory response, TMP protected against cisplatin (80 mg/kg/day orally for 7 days) or arsenic (100 μM for 24 h)-induced AKI (Ali et al., 2008; Gong et al., 2015). Moreover, a recent study showed that TMP (80 mg/kg/day i.p. for 4 days) suppressed the apoptosis of renal cells by targeting FoxO1, a pro-apoptotic transcription factor, to prevent contrast-induced AKI (Gong et al., 2013). Interestingly, TMP exerted a renoprotective role by downregulating P-selectin, which has been accepted as a key modulator of neutrophil infiltration in I/R kidney injury (Chen et al., 2003).
Our group also tested the therapeutic potential of traditional Chinese medicine in the treatment of AKI. We screened 10 kinds of Chinese herbal medicine with anti-inflammatory effects and found that wogonin and protocatechuic aldehyde had significant therapeutic effects. Wogonin inhibits cisplatin-induced renal damage by inhibiting RIPK1-mediated necroptosis and attenuates inflammation (Meng et al., 2018), whereas protocatechuic aldehyde (PA) not only inhibits necroptosis, but also effectively reduces cisplatin-induced over-production of ROS (Gao L. et al., 2016). Interestingly, we all know that cisplatin is commonly used as an anti-cancer drugs in clinic, and these two TCMs could even promote anti-tumor effects of cisplatin, so wogonin and protocatechuic aldehyde may be renoprotective adjuvants for cisplatin-based anticancer therapy.
There are many other TCMs to treat AKI, and these are listed in Table 2.
Table 2.
Application of TCM monomers in the treatment of acute kidney injury.
| Names | Origins | Models | Functions | Mechanisms |
|---|---|---|---|---|
| Alpinetin | Alpinia katsumadai Hayata | LPS-induced AKI | Inhibiting inflammation. | By enhancing Nrf2 and HO-1 (Huang et al., 2015) |
| Astragaloside IV (AS-IV) | Astragaloside | Cisplatin-induced AKI | Inhibiting oxidative damage and inflammatory response. | By activation of Nrf2 and suppression of NF-κB activation (Yan et al., 2017) |
| Astaxanthin (ATX) | Carotenoid in marine organisms | I/R, As2O3, HgCl2-induced AKI | Antioxidant activity; Inhibiting apoptosis. | By Akt/Bad/caspases pathway (Augusti et al., 2008; Wang et al., 2014; Guo et al., 2015; Qiu et al., 2015) |
| Baicalin | Scutellaria baicalensis | H2O2, -induced AKI | Blocking oxidative stress, ER stress and apoptosis. | By activating Nrf2 signaling (Lin et al., 2014) |
| Pb, pediatric sepsis – induced AKI | Zhang Z. et al., 2017 | |||
| I/R-induced AKI | Inhibiting inflammation and apoptosis. | By inhibiting TLR2/4 and mitochondrial stress (Ji et al., 2014) | ||
| LPS-induced AKI | By activating PPARγ and inhibiting NF-κB (Lim et al., 2012) | |||
| Breviscapine | Erigeron breviscapus | Cisplatin-induced AKI | Inhibiting lipid peroxidation and ferroptosis. | By decreasing MDA, SOD, increasing glutathione peroxidase levels (Lou et al., 2015) |
| Chlorogenic Acid | Plant polyphenols | LPS-induced AKI | Suppressing inflammation. | By inhibiting TLR4/NF-κB signaling pathway (Ye et al., 2017) |
| Cordyceps sinensis (CS) | An entomogenous fungus | I/R-induced renal injury | Inhibiting inflammation and apoptosis. | By modulating SDF-1/CXCR4-signaling, reducing TLR-4,increasing HIF-1α (Zhou and Hu, 2010; Yu et al., 2012; Wang et al., 2013) |
| LPS-induced AKI | Reducing autophagy and apoptosis. | By reducing ED-1, GRP78 (Wu et al., 2011) | ||
| (CSP) | Cordyceps sobolifera | CsA – induced AKI | Suppressing apoptosis. | By enhancing TRMP6 and TRMP7 (Chyau et al., 2014) |
| Curcumin | Curcuma longa | Rhabdomyolysis (RM)-induced AKI | Reducing renal oxidative stress. | By inhibiting AMPK and Nrf2/HO-1 (Wu et al., 2017) |
| I/R-induced AKI | By NMDA receptor antagonism (Kaur et al., 2016) | |||
| Glycerol-induced AKI | Ameliorating cell apoptosis. | By activating the PI3K/Akt pathway (Wu et al., 2017) | ||
| Cisplatin-induced AKI | Preventing renal alterations. Inhibiting inflammatory. | By preventing mitochondrial bioenergetics and dynamic and SIRT3 levels (Ortega-Dominguez et al., 2017). By inhibiting Mincle-maintained M1 macrophage phenotype (Tan et al., 2019) | ||
| Emodin | Rheum palmatum | LPS-induced AKI | Inhibiting inflammatory. | By inhibiting TLR2 (Li et al., 2015) or TLR4 (Zhu et al., 2012) |
| Cisplatin-induced AKI | Inhibiting apoptosis and activating autophagy. | By modulating the AMPK/mTOR signaling (Liu et al., 2016) | ||
| Epigallocatechin gallate (EGCG) | Green tea | Contrast-induced AKI | Alleviating apoptosis, oxidative stress and inflammation. | By increasing HO-1 and Nrf2 (Gao Z. et al., 2016) |
| I/R, Cisplatin -induced AKI | Inhibiting inflammatory, Decreasing oxidative/nitrative stress. | By activating HO-1 (Sahin et al., 2010; Lv et al., 2015; Pan et al., 2015) | ||
| Inhibiting apoptosis. | By preventing ERK (Zou et al., 2014) | |||
| Ginsenoside Rd (GSRd) | Panax ginseng | I/R-induced AKI | Suppressing inflammatory. | By inhibiting oxygen free radicals (Ye et al., 2011) |
| Cisplatin-induced AKI | Decreasing apoptosis. | Yokozawa and Liu, 2000 | ||
| Glycerol-induced AKI | Reducing renal oxidative stress. | Zhou et al., 2014 | ||
| (Rb1, Rg1) | I/R-induced AKI | Reducing apoptosis. | Zhu et al., 2009 | |
| (Rg1) | Aldosterone- induced AKI | Reducing oxidative stress and autophagy. | By decreasing AMPK/mTOR pathway (Wang et al., 2015) | |
| (Ginsenoside Rg3) | Panax ginseng | Cisplatin-induced AKI | Decreasing apoptosis. | By blocking the JNK-p53-caspase-3 signaling (Han et al., 2016) |
| LPS-induced AKI | Decreasing inflammatory. | By inhibiting NF-κB (Kang et al., 2007) | ||
| Esculentoside A (EsA) | Phytolacca esculenta | LPS-induced AKI | Alleviating inflammation. | By activating PPAR-γ (Chen et al., 2017) |
| Puncture-induced AKI | By regulating the TLR4/MyD88/HMGB1 signaling pathway (Sun et al., 2017) | |||
| Galangin | Propolis and Alpinia officinarum | Cisplatin-induced AKI | Attenuating oxidative stress, inflammation, and cell death. | By inhibiting ERK, NF-κB and RIPK1-mediated necroptosis signaling pathways (Huang et al., 2017) |
| Ginkgetin aglycone (GA) | Ginkgo biloba extract | LPS-induced AKI | Decreasing inflammatory. | By activating SIRT1 via inhibiting the NF-κB signaling pathway (Zhang J. et al., 2017) |
| Glycyrrhizic acid (GA) | Ingredient in licorice | LPS-induced renal injury | Inhibiting cell apoptosis, oxidative stress. | By activating ERK and inhibiting NF-κB (Zhao et al., 2016) |
| I/R-induced renal injury | Reducing tubular necrosis. | By inhibiting HMGB1 and enhancing Nrf2 (Lau et al., 2014) | ||
| (GA, 18βGA) | Cisplatin-induced AKI | Inhibiting renal tubular epithelial cells apoptosis. | By enhancing BMP-7 epigenetically through targeting HDAC2 (Ma et al., 2016) | |
| Alleviating oxidative status and inflammatory. | Arjumand and Sultana, 2011; Wu et al., 2015 | |||
| Gypenoside (GP) | Gynostemma pentaphyllum | I/R-induced renal injury | Attenuating inflammatory and oxidative stress. | By inhibiting ERK signaling (Ye et al., 2016) |
| Hyperin | Ericaceae, Guttifera, and Celastraceae | Cisplatin-induced AKI | Attenuating inflammatory. | By inhibiting NF-κB and activating nuclear factor E2-related factor-2 signaling pathways (Chao et al., 2016) |
| Honokiol | Magnolia officinalis | LPS-induced AKI | Inhibition of oxidative stress and Inflammation. | By inhibiting TLR2/4/MyD88 signaling pathway (Xia et al., 2019) |
| Isoacteoside (ISO) | Monochasma savatieri | LPS-induced AKI | Attenuating inflammatory. | By inhibiting TLR4 dimerization to activate the MyD88-TAK1- NF-κB/MAPK signaling cascades and TRIF pathway (Gao et al., 2017) |
| Leonurine (LEO) | Leonurus cardiaca | LPS-induced renal injury | Inhibiting inflammatory and oxidative stress. | By down-regulating NF-κB (Xu et al., 2014) |
| Ligustrazine (LIG) | Ligusticum wallichii Franch. | Cisplatin/I/R-induced renal injury | Down-regulating oxidative stress and apoptosis, decreasing neutrophils infiltration. | Liu et al., 2008; Feng et al., 2011 |
| Pancreatitis-induced AKI | Improving renal function. | By improve microcirculatory disorder (MCD) (Zhang et al., 2006) | ||
| Loganetin | Loganin | Rhabdomyolysis-induced AKI | Improving renal function. | By inhibiting TLR4 activity and blocking the JNK/p38 pathway (Li et al., 2019) |
| Luteolin | Celery, Green pepper, and Chamomile | D-galactose-induced AKI | Attenuating inflammatory and oxidative stress. | By suppressing phosphorylation of p38 MAPK (Xu et al., 2015) |
| Cisplatin-induced AKI | Alleviating inflammation. | By inhibiting NF-κB (Domitrovic et al., 2013) | ||
| Decreasing apoptosis. | By decreasing p53 (Kang et al., 2011) | |||
| Nerolidol | Essential oils | LPS-induced AKI | Alleviating inflammation. | By inhibiting TLR4-NF-κB signal pathway (Zhang L. et al., 2017) |
| Osthole | Cnidium monnieri (L.) Cusson fruit | LPS-induced AKI | Inhibiting inflammation. | By down-regulating NF-κB pathway (Yu et al., 2017) |
| I/R-induced renal injury | Abrogating inflammation. | By suppressing JAK2/STAT3 signaling, NF-κB and activating PI3K/Akt signaling (Luo et al., 2016) | ||
| Pachymic acid (PA) | A lanostane-type triterpenoid from Poria cocos | Sepsis-induced AKI | Inhibiting inflammatory function and antioxidant effect via. | By activating Nrf2/HO-1 pathway (Cai et al., 2017) |
| Paeonol | Paeonia moutan Sims | Endotoxin-induced AKI | Alleviating inflammation. | By inhibiting TLR4-NF-κB signal pathway (Fan et al., 2016) |
| Panax quinquefolius (PQS) | Panax quinquefolius | Cisplatin-induced AKI | Suppressing oxidative stress, inflammation, and apoptosis. | By inhibiting Nox4-iNOS, NF-κB-COX-2, and caspase3/9 (Ma et al., 2017) |
| Paeoniflorin (PF) | Radix Paeoniae Rubra | Pancreatitis-induced AKI | Inhibiting inflammation and cell apoptosis. | By inhibiting NF-κB (Wang et al., 2016) |
| ConA-induced renal injury | Attenuating inflammatory response. | By inhibiting CXCR3/CXCL11 (Liu C. et al., 2015) | ||
| Panaxadiol Saponin (PDS) | Ginseng stem and leaves | LPS-induced AKI | Inhibiting inflammatory and oxidative stress. | By blocking NF-κB pathway (Chen Y. et al., 2015) |
| Panax notoginseng saponins (PNS) | Panax notoginseng | Cisplatin-induced AKI | Reducing renal tissue apoptosis. | By inhibiting the mitochondrial apoptosis (Liu et al., 2014) |
| Increasing mitochondrial autophagy. | By enhancing HIF-1α/BNIP3 (Liu X. et al., 2015) | |||
| Notoginsenoside R1 (NR1) | I/R-induced renal injury | Blocking apoptosis and inflammatory response. | By suppressing p38 and NF-κB (Liu et al., 2010) | |
| Polydatin (PD) | Polygonum cuspidatum Sieb. | I/R, Sepsis-induced AKI | Attenuating inflammatory response | By regulating TLR4/NF-κB and enhancing PI3K/Akt (Liu H. et al., 2015) |
| Protocatechuic Aldehyde (PA) | Salvia miltiorrhiza (Lamiaceae) | Cisplatin-induced AKI | Suppressing Nox-mediated oxidative stress and renal inflammation. | By suppressing Nox-mediated oxidative stress targeting RIPK1-mediated necroptosis (Gao L. et al., 2016) |
| Quercetin (QC) | Bioflavonoids in the plant kingdom | I/R-induced AKI | Activating autophagy | By increasing AMPK (Chen et al., 2014) |
| HgCl2-induced AKI | Limiting apoptosis. | Shin et al., 2015 | ||
| Cisplatin-induced AKI | Decreasing cell necrosis and inflammatory. | By inhibiting NF-κB (Francescato et al., 2004) | ||
| RA-X II | Rubia yunnanensis | LPS-induced AKI | Inhibiting oxidative stress and inflammatory. | By suppressing NF-κB and MAPKs regulated by HO-1/Nrf2 pathway (An and Shang, 2018) |
| Resveratrol (RSV) | Grapes and red wine | LPS-induced AKI | Attenuating inflammatory response. | By NF-B-P65 de-acetylation (Gan et al., 2017), SIRT3-mediated deacetylation of SOD2 (Xu et al., 2016), inhibiting endoplasmic reticulum stress (IRE1)-activated NF-κB pathway (Wang et al., 2017) and via the activation of Nrf2 signaling pathway (Wang et al., 2018) |
| Cisplatin-induced AKI | Suppressing inflammation and apoptosis. | By activating SIRT1 through deacetylating p53 (Kim et al., 2011) | ||
| Glycerol-induced AKI | Suppressing inflammatory and lipid peroxidation. | By decreasing NF-κB and HO-1 (de Jesus Soares et al., 2007) | ||
| (RSVA405 RSVA314) | As2O3, I/R -induced AKI | Antagonizing oxidative stress. | Holthoff et al., 2012; Yu et al., 2013 | |
| Tanshinone I | Salvia miltiorrhiza | AAI-induced renal injury | Inducing apoptosis and autophagy. | By inducing Atg5 (Feng et al., 2013) |
| Tanshinone IIA | Folic Acid-induced AKI | Inhibiting inflammatory response. | Jiang et al., 2016 | |
| Tenuigenin (TNG) | Polygala tenuifolia | LPS-induced AKI | Attenuating inflammatory response. | Inhibiting TLR4/NF-κB signaling pathway (Fu et al., 2016) |
| Tetramethylpyrazine (TMP) | Ligusticum wallichii Franch. | Arsenic, Cisplatin-induced AKI | Inhibiting inflammatory and oxidative stress. | By down-regulating HO-1 and ARS2 (Gong et al., 2016) |
| Gentamicin-induced AKI | Inhibiting inflammatory and apoptosis. | By enhancing Hax-1 and HO-1 (Sue et al., 2009) | ||
| Sodium arsenite-induced AKI | Suppressing ROS production, mitochondrial dysfunction and inflammatory. | By suppressing programmed cell death (Gong et al., 2015) | ||
| Contrast-induced AKI | Suppressing autophagy and apoptosis. | By suppressing p38 MAPK and targeting FoxO1 (Gong et al., 2013) | ||
| I/R-induced renal injury | Alleviating histopathological damage. | By down-regulating P-selectin (Chen et al., 2003) | ||
| Triptolide (PG490-88) | Tripterygium wilfordii Hook.F | Cisplatin-induced AKI | Decreasing cell necrosis. | By decreasing phosphorylation of ERK (Kim et al., 2014) |
| Wogonin | Scutellaria baicalensis Georgi | Cisplatin-induced AKI | Attenuating inflammatory response. | By targeting RIPK1-mediated necroptosis (Meng et al., 2018) |
Mechanisms Involved in the Therapeutic Effect of TCMs in AKI
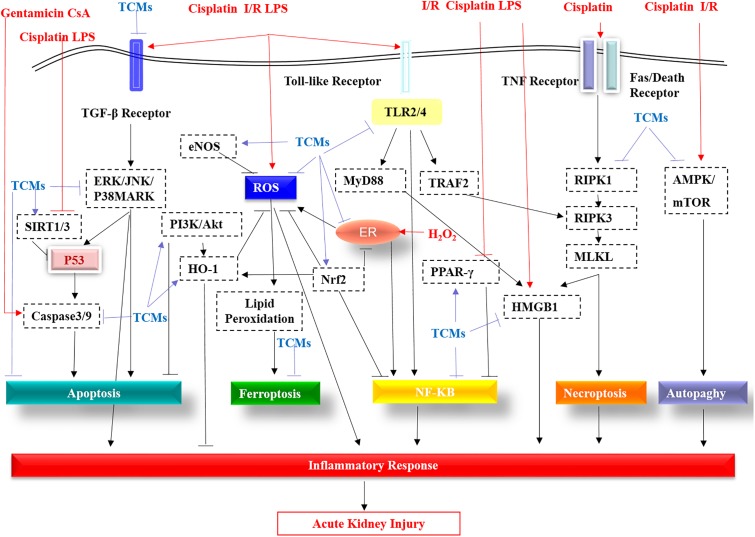
As shown in Figure 1, the TGF-β receptor, Toll-like receptors (TLRs), TNF receptor, and FASL/Death receptors are stimulated by LPS, cisplatin and I/R, etc., then these receptors activate downstream pathways, further triggering ROS production and inflammatory responses, eventually leading to kidney damage. TCMs suppress cisplatin/LPS/I/R-stimulated TLRs including TLR2/4, or by activating PPAR, further inhibiting the NF-κB pathway and reducing inflammation. Moreover, TCMs reduce apoptosis by inhibiting TGF-β, PI3K/AKT and ERK/JNK/P38MARK pathways. In addition, TCMs inhibit autophagy by targeting AMPK/mTOR. In recent years, new cell death mechanisms like programmed necrosis and ferroptosis have also attracted attention. Wogonin and protocatechuic aldehyde can effectively inhibit RIPK1/RIPK3-mediated necroptosis. Breviscapine can reduce ferroptosis by increasing glutathione peroxidase levels. Additionally, TCMs can inhibit H2O2-induced endoplasmic reticulum (ER) stress and further reduce ROS production. In the AKI model, ROS, HMGB1, P53, Nrf2, HO-1, and SIRT1/3 are regarded as potential therapeutic targets of TCMs.
FIGURE 1.
The molecular pathways targeted by the TCMs covered in this review are summarized. TGF-β receptor, Toll-like receptors (TLRs), TNF receptor, and FASL/Death receptors are stimulated by LPS, cisplatin, I/R, etc. These receptors are then activated by the downstream pathway, further triggering ROS production and an inflammatory response, eventually leading to kidney damage. TCMs suppress cisplatin/LPS/I/R-stimulated Toll-like receptors (TLR2/4), or by activating PPAR-γ, further inhibiting the NF-κB pathway and reducing inflammation. Additionally, apart from targeting caspase3/9, TCMs reduce apoptosis by inhibiting the TGF-β receptor, the ERK/JNK/P38MARK pathway and by promoting PI3K/AKT. In addition, TCMs inhibit autophagy by targeting inhibition of AMPK/mTOR. In addition to the traditional apoptosis, autophagy, programmed necrosis and ferroptosis are also caused during AKI. Wogonin and protocatechuic aldehyde can effectively inhibit RIPK1 in the RIPK1/RIPK3/MLKL of necroptosis. TLR2/4-mediated TRAF2 has a stimulant effect on RIPK3. Induction of HMGB2 by necroptosis and TLR2/4-regulated MyD88 aggravates the inflammatory response of acute kidney injury, while TCMs significantly improve this phenomenon via direct or indirect effects. Breviscapine can reduce ferroptosis by increasing glutathione peroxidase levels. In acute kidney injury, the production of ROS, the multiple roles of P53, the protective effects of eNOS, Nrf2, HO-1, and SIRT1/3 all become therapeutic targets of TCMs.
Nephrotoxicity of TCMs
It has been recorded that up to 25% of all cases of AKI may be correlated to nephrotoxic medications (Bentley et al., 2010). As shown in Table 3, previous studies indicate that some TCMs, including aristolochic acid, anthraquinones, flavonoids, and glycosides from herbs, non-steroidal anti-inflammatory drugs, aminoglycosides, cytostatic drugs, osmotic agents, radiocontrast, and phosphate salts, may lead to kidney damage and induce AKI (Liangos, 2012; Yang et al., 2018). Several reasons contributing to nephrotoxicity of TCMs include the intrinsic toxicity of herb medicines, incorrect dosing, interactions between herbs and medications, adulteration, incorrect processing and storage, and contamination by heavy metals (Yang et al., 2018).
Table 3.
Application of TCM monomers which can induce acute kidney injury.
| Names | Origins | Functions | Mechanisms |
|---|---|---|---|
| Aristolochia acids (AA) | Aristolochia species | Increasing oxidative stress and inflammatory | Increasing Nox2 and reducing NO bioavailability (Sato et al., 2004; Debelle et al., 2008) |
| Andrographide | A herbaceous plant in the family Acanthaceae | Promoting cell necrosis | Unclear (Zhang et al., 2014) |
| Sciadopitysin | Taxus celebica | Inducing acute tubular necrosis and acute interstitial nephritis | (Lin and Ho, 1994) |
| Triptolide | Tripterygium wilfordii Hook.f | Accelerating oxidative stress and inducing apoptosis | Inducing production of ROS (Yang et al., 2012) |
It was reported that two patients took sciadopitysin, a kind of flavonoid extracted from Taxus celebica to treat diabetes mellitus, and suffered acute tubular necrosis and acute interstitial nephritis (Lin and Ho, 1994). Andrographolide (Chuan Xin Lian) is widely used in China for the treatment of dysentery and respiratory tract infection. It is noteworthy that a systemic analysis, based on clinical cases reported in Chinese literature from January 1978 to August 2013, revealed 26 patients with AKI induced by andrographolide. The major pathologic features in these patients were acute tubular necrosis. The mechanism is still obscure (Zhang et al., 2014). Aristolochia acids (AA) is extracted from Aristolochia fangchi, within which aristolochic acid I (AAI) and aristolochic acid II (AAII) are well known. AA has widely been used as an anti-inflammatory agent. However, a series of studies demonstrated that AA could induce early and transient acute tubular necrosis and progressive tubulointerstitial injury, which finally lead to renal fibrosis (Sato et al., 2004; Debelle et al., 2008; Zhou et al., 2010; DeBroe, 2012). AA also caused nephropathy, by inducing DNA adduct formation (Allard et al., 2013). Some drugs related with AA are nephrotoxic due to the intrinsic toxicity of herbs and the misidentification of potentially toxic compounds. The root of asarum (also known as Xi Xin) contains low levels of AA and has widely been used as an analgesic for headache, toothache, and inflammatory diseases. But the whole asarum plant contains high levels of AA (Drew et al., 2002). Triptolide, isolated from Tripterygium wilfordii Hook.f (TWHf)-derived diterpenoid, has been commonly used for its immunosuppressive and anti-cancer properties (Carter et al., 2006). However, administration of triptolide may result in severe kidney injury by impairing the antioxidant system, promoting production of reactive oxygen species and inducing apoptosis of tubular epithelial cells, which may limit the application of triptolide in the clinic (Yang et al., 2011, 2012).
Prevention and Treatment of TCMs-Induced AKI
The first principle of effective therapy is to acknowledge and prevent or minimize nephrotoxicity of TCMs. In this regard, several strategies should be applied: (1) In view of the intrinsic toxicity of some herbs, researchers could modify molecular structure of TCMs to lower the toxic effects without affecting their therapeutic effects. It is essential to reveal the compound/phytochemicals present in the formulations which are correlated with the toxicity in AKI. (2) As for the incorrect identification, processing and storage, standardization of herbal products need to be emphasized. We should also ensure safe manufacturing processes to avoid contamination from heavy metals and other ingredients. (3) We should determine and limit the dosing and duration of drugs usage through adequate preclinical trials and dose conversions between animals and humans. Safe and effective dose ranges for humans as well as appropriate monitoring for adverse effects are also needed. (4) It is worth mentioning that pharmacists and doctors should clearly know the interactions between TCMs and other medications before prescribing these drugs to patients. (5) For patients with special conditions, like chronic kidney disease and liver disease, their medication needs to be carefully considered.
Conclusion and Perspectives
Collectively, previous studies showed that numerous types of TCMs protect against AKI via different mechanisms of action, including inhibiting inflammation, cell apoptosis, necroptosis, ferroptosis, and restraining oxidative stress etc. These data support the potential application of these TCMs as novel therapeutic agents in treating patients with AKI. Although some TCMs have entered preclinical trials, it is essential to initiate pre-clinical pharmacologic and toxicologic trials and clinical trials to evaluate the efficacy and safety of TCMs usage. Moreover, considering that some TCMs are deleterious to the kidney, they should be attracted more attention when utilized. In addition, it is believed that western medicines always relieve symptoms quickly while TCMs exert therapeutic effects gently and fundamentally. In this regard, the combination of TCMs and western medicines may become a promising treatment strategy for AKI by taking advantages of both and by limiting side effects. The interaction between medicines should also be considered. In conclusion, from a holistic point of view, TCM-based anti-AKI therapy should be emphasized and extensively explored, as this may help to minimize the morbidity and mortality of AKI and prolong the survival of patients.
Author Contributions
JL, XM, and CH designed the theme and direction of the manuscript. LZ and XL critically revised the manuscript. HL drafted the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
- AKI
acute kidney injury
- ER stress
endoplasmic reticulum stress
- ERK
extracellular signal-regulated kinase
- HMGB1
high mobility group box 1
- HO-1
heme oxygenase (HO)-1
- i.p.
intraperitoneal
- I/R
ischemic reperfusion
- JNK
C-jun N-terminal kinase
- LPS
lipopolysaccharide
- MLKL
mixed-lineage kinase like domain
- Nrf2
nuclear factor 2 correlation factor
- PI3K/AKT
phosphatidylinositol 3-hydroxy kinase/protein kinase
- PPAR-γ
peroxisome proliferators-activated receptor-γ
- RIPK
receptor interacting serine-threonine protein kinase
- ROS
reactive oxygen species
- SIRT
silent information regulator
- TCMs
traditional Chinese medicines
Footnotes
Funding. This study was supported by the National Natural Science Foundation of China (No. 81770609), Anhui University of Science and Technology (No. 1704a0802161), and Technological Fund of Anhui Province for Outstanding Youth of China (Grant No. 1608085J07).
References
- Ali B. H., Al-Moundhri M., Eldin M. T., Nemmar A., Al-Siyabi S., Annamalai K. (2008). Amelioration of cisplatin-induced nephrotoxicity in rats by tetramethylpyrazine, a major constituent of the Chinese herb Ligusticum wallichi. Exp. Biol. Med. 233 891–896. 10.3181/0711-RM-315 [DOI] [PubMed] [Google Scholar]
- Allard T., Wenner T., Greten H. J., Efferth T. (2013). Mechanisms of herb-induced nephrotoxicity. Curr. Med. Chem. 20 2812–2819. 10.2174/0929867311320220006 [DOI] [PubMed] [Google Scholar]
- Allison S. J. (2016). Acute kidney injury: AIMing to enhance debris clearance and improve outcomes in AKI. Nat. Rev. Nephrol. 12:123. 10.1038/nrneph.2016.3 [DOI] [PubMed] [Google Scholar]
- An X., Shang F. (2018). RA-XII exerts anti-oxidant and anti-inflammatory activities on lipopolysaccharide-induced acute renal injury by suppressing NF-kappaB and MAPKs regulated by HO-1/Nrf2 pathway. Biochem. Biophys. Res. Commun. 495 2317–2323. 10.1016/j.bbrc.2017.12.131 [DOI] [PubMed] [Google Scholar]
- Arjumand W., Sultana S. (2011). Glycyrrhizic acid: a phytochemical with a protective role against cisplatin-induced genotoxicity and nephrotoxicity. Life Sci. 89 422–429. 10.1016/j.lfs.2011.06.016 [DOI] [PubMed] [Google Scholar]
- Augusti P. R., Conterato G. M., Somacal S., Sobieski R., Spohr P. R., Torres J. V., et al. (2008). Effect of astaxanthin on kidney function impairment and oxidative stress induced by mercuric chloride in rats. Food Chem. Toxicol. 46 212–219. 10.1016/j.fct.2007.08.001 [DOI] [PubMed] [Google Scholar]
- Bentley M. L., Corwin H. L., Dasta J. (2010). Drug-induced acute kidney injury in the critically ill adult: recognition and prevention strategies. Crit. Care Med. 38 S169–S174. 10.1097/CCM.0b013e3181de0c60 [DOI] [PubMed] [Google Scholar]
- Cai Q., Li X., Wang H. (2001). Astragali and Angelica protect the kidney against ischemia and reperfusion injury and accelerate recovery. Chin. Med. J. 114 119–123. [PubMed] [Google Scholar]
- Cai Z. Y., Sheng Z. X., Yao H. (2017). Pachymic acid ameliorates sepsis-induced acute kidney injury by suppressing inflammation and activating the Nrf2/HO-1 pathway in rats. Eur. Rev. Med. Pharmacol. Sci. 21 1924–1931. [PubMed] [Google Scholar]
- Carter B. Z., Mak D. H., Schober W. D., McQueen T., Harris D., Estrov Z., et al. (2006). Triptolide induces caspase-dependent cell death mediated via the mitochondrial pathway in leukemic cells. Blood 108 630–637. 10.1182/blood-2005-09-3898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao C. S., Tsai C. S., Chang Y. P., Chen J. M., Chin H. K., Yang S. C. (2016). Hyperin inhibits nuclear factor kappa B and activates nuclear factor E2-related factor-2 signaling pathways in cisplatin-induced acute kidney injury in mice. Int. Immunopharmacol. 40 517–523. 10.1016/j.intimp.2016.09.020 [DOI] [PubMed] [Google Scholar]
- Chen B., Liu G., Zou P., Li X., Hao Q., Jiang B., et al. (2015). Epigallocatechin-3-gallate protects against cisplatin-induced nephrotoxicity by inhibiting endoplasmic reticulum stress-induced apoptosis. Exp. Biol. Med. 240 1513–1519. 10.1177/1535370215573394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B. L., Wang L. T., Huang K. H., Wang C. C., Chiang C. K., Liu S. H. (2014). Quercetin attenuates renal ischemia/reperfusion injury via an activation of AMP-activated protein kinase-regulated autophagy pathway. J. Nutr. Biochem. 25 1226–1234. 10.1016/j.jnutbio.2014.05.013 [DOI] [PubMed] [Google Scholar]
- Chen D. Z., Chen L. Q., Lin M. X., Gong Y. Q., Ying B. Y., Wei D. Z. (2017). Esculentoside A inhibits LPS-induced acute kidney injury by activating PPAR-gamma. Microb. Pathog. 110 208–213. 10.1016/j.micpath.2017.06.037 [DOI] [PubMed] [Google Scholar]
- Chen J. L., Zhou T., Chen W. X., Zhu J. S., Chen N. W., Zhang M. J., et al. (2003). Effect of tetramethylpyrazine on P-selectin and hepatic/renal ischemia and reperfusion injury in rats. World J. Gastroenterol. 9 1563–1566. 10.3748/wjg.v9.i7.1563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L., Yang S., Zumbrun E. E., Guan H., Nagarkatti P. S., Nagarkatti M. (2015). Resveratrol attenuates lipopolysaccharide-induced acute kidney injury by suppressing inflammation driven by macrophages. Mol. Nutr. Food Res. 59 853–864. 10.1002/mnfr.201400819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Du Y., Li Y., Wang X., Gao P., Yang G., et al. (2015). Panaxadiol saponin and dexamethasone improve renal function in lipopolysaccharide-induced mouse model of acute kidney injury. PLoS One 10:e0134653. 10.1371/journal.pone.0134653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chertow G. M., Burdick E., Honour M., Bonventre J. V., Bates D. W. (2005). Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J. Am. Soc. Nephrol. 16 3365–3370. 10.1681/ASN.2004090740 [DOI] [PubMed] [Google Scholar]
- Chyau C. C., Chen C. C., Chen J. C., Yang T. C., Shu K. H., Cheng C. H. (2014). Mycelia glycoproteins from Cordyceps sobolifera ameliorate cyclosporine-induced renal tubule dysfunction in rats. J. Ethnopharmacol. 153 650–658. 10.1016/j.jep.2014.03.020 [DOI] [PubMed] [Google Scholar]
- Debelle F. D., Vanherweghem J. L., Nortier J. L. (2008). Aristolochic acid nephropathy: a worldwide problem. Kidney Int. 74 158–169. 10.1038/ki.2008.129 [DOI] [PubMed] [Google Scholar]
- DeBroe M. E. (2012). Chinese herbs nephropathy and Balkan endemic nephropathy: toward a single entity, aristolochic acid nephropathy. Kidney Int. 81 513–515. 10.1038/ki.2011.428 [DOI] [PubMed] [Google Scholar]
- de Jesus Soares T., Volpini R. A., Francescato H. D., Costa R. S., da Silva C. G., Coimbra T. M. (2007). Effects of resveratrol on glycerol-induced renal injury. Life Sci. 81 647–656. 10.1016/j.lfs.2007.06.032 [DOI] [PubMed] [Google Scholar]
- Do Amaral C. L., Francescato H. D., Coimbra T. M., Costa R. S., Darin J. D., Antunes L. M., et al. (2008). Resveratrol attenuates cisplatin-induced nephrotoxicity in rats. Arch. Toxicol. 82 363–370. 10.1007/s00204-007-0262-x [DOI] [PubMed] [Google Scholar]
- Domitrovic R., Cvijanovic O., Pugel E. P., Zagorac G. B., Mahmutefendic H., Skoda M. (2013). Luteolin ameliorates cisplatin-induced nephrotoxicity in mice through inhibition of platinum accumulation, inflammation and apoptosis in the kidney. Toxicology 310 115–123. 10.1016/j.tox.2013.05.015 [DOI] [PubMed] [Google Scholar]
- Drew A. K., Whyte I. M., Bensoussan A., Dawson A. H., Zhu X., Myers S. P. (2002). Chinese herbal medicine toxicology database: monograph on Herba Asari, “xi xin”. J. Toxicol. Clin. Toxicol. 40 169–172. 10.1081/CLT-120004405 [DOI] [PubMed] [Google Scholar]
- Fan H. Y., Qi D., Yu C., Zhao F., Liu T., Zhang Z. K., et al. (2016). Paeonol protects endotoxin-induced acute kidney injury: potential mechanism of inhibiting TLR4-NF-kappaB signal pathway. Oncotarget 7 39497–39510. 10.18632/oncotarget.8347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng C., Xie X., Wu M., Li C., Gao M., Liu M., et al. (2013). Tanshinone I protects mice from aristolochic acid I-induced kidney injury by induction of CYP1A. Environ. Toxicol. Pharmacol. 36 850–857. 10.1016/j.etap.2013.07.017 [DOI] [PubMed] [Google Scholar]
- Feng L., Ke N., Cheng F., Guo Y., Li S., Li Q., et al. (2011). The protective mechanism of ligustrazine against renal ischemia/reperfusion injury. J. Surg. Res. 166 298–305. 10.1016/j.jss.2009.04.005 [DOI] [PubMed] [Google Scholar]
- Francescato H. D., Coimbra T. M., Costa R. S., Bianchi Mde L. (2004). Protective effect of quercetin on the evolution of cisplatin-induced acute tubular necrosis. Kidney Blood Press. Res. 27 148–158. 10.1159/000078309 [DOI] [PubMed] [Google Scholar]
- Fu H., Hu Z., Di X., Zhang Q., Zhou R., Du H. (2016). Tenuigenin exhibits protective effects against LPS-induced acute kidney injury via inhibiting TLR4/NF-kappaB signaling pathway. Eur. J. Pharmacol. 791 229–234. 10.1016/j.ejphar.2016.08.013 [DOI] [PubMed] [Google Scholar]
- Gan Y., Tao S., Cao D., Xie H., Zeng Q. (2017). Protection of resveratrol on acute kidney injury in septic rats. Hum. Exp. Toxicol. 36 1015–1022. 10.1177/0960327116678298 [DOI] [PubMed] [Google Scholar]
- Gao H., Cui Y., Kang N., Liu X., Liu Y., Zou Y., et al. (2017). Isoacteoside, a dihydroxyphenylethyl glycoside, exhibits anti-inflammatory effects through blocking toll-like receptor 4 dimerization. Br. J. Pharmacol. 174 2880–2896. 10.1111/bph.13912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao L., Wu W. F., Dong L., Ren G. L., Li H. D., Yang Q., et al. (2016). Protocatechuic aldehyde attenuates cisplatin-induced acute kidney injury by suppressing nox-mediated oxidative stress and renal inflammation. Front. Pharmacol. 7:479. 10.3389/fphar.2016.00479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Z., Han Y., Hu Y., Wu X., Wang Y., Zhang X., et al. (2016). Targeting HO-1 by epigallocatechin-3-gallate reduces contrast-induced renal injury via anti-oxidative stress and anti-inflammation pathways. PLoS One 11:e0149032. 10.1371/journal.pone.0149032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong X., Ivanov V. N., Davidson M. M., Hei T. K. (2015). Tetramethylpyrazine (TMP) protects against sodium arsenite-induced nephrotoxicity by suppressing ROS production, mitochondrial dysfunction, pro-inflammatory signaling pathways and programed cell death. Arch. Toxicol. 89 1057–1070. 10.1007/s00204-014-1302-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong X., Ivanov V. N., Hei T. K. (2016). 2,3,5,6-Tetramethylpyrazine (TMP) down-regulated arsenic-induced heme oxygenase-1 and ARS2 expression by inhibiting Nrf2, NF-kappaB, AP-1 and MAPK pathways in human proximal tubular cells. Arch. Toxicol. 90 2187–2200. 10.1007/s00204-015-1600-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong X., Wang Q., Tang X., Wang Y., Fu D., Lu H., et al. (2013). Tetramethylpyrazine prevents contrast-induced nephropathy by inhibiting p38 MAPK and FoxO1 signaling pathways. Am. J. Nephrol. 37 199–207. 10.1159/000347033 [DOI] [PubMed] [Google Scholar]
- Guo S. X., Zhou H. L., Huang C. L., You C. G., Fang Q., Wu P., et al. (2015). Astaxanthin attenuates early acute kidney injury following severe burns in rats by ameliorating oxidative stress and mitochondrial-related apoptosis. Mar. Drugs 13 2105–2123. 10.3390/md13042105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han M. S., Han I. H., Lee D., An J. M., Kim S. N., Shin M. S., et al. (2016). Beneficial effects of fermented black ginseng and its ginsenoside 20(S)-Rg3 against cisplatin-induced nephrotoxicity in LLC-PK1 cells. J. Ginseng Res. 40 135–140. 10.1016/j.jgr.2015.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holthoff J. H., Wang Z., Seely K. A., Gokden N., Mayeux P. R. (2012). Resveratrol improves renal microcirculation, protects the tubular epithelium, and prolongs survival in a mouse model of sepsis-induced acute kidney injury. Kidney Int. 81 370–378. 10.1038/ki.2011.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu Y. H., Chen T. H., Wu M. Y., Lin Y. F., Chen W. L., Cheng T. H., et al. (2014). Protective effects of Zhibai Dihuang Wan on renal tubular cells affected with gentamicin-induced apoptosis. J. Ethnopharmacol. 151 635–642. 10.1016/j.jep.2013.11.031 [DOI] [PubMed] [Google Scholar]
- Huang Y., Zhou L. S., Yan L., Ren J., Zhou D. X., Li S. S. (2015). Alpinetin inhibits lipopolysaccharide-induced acute kidney injury in mice. Int. Immunopharmacol. 28 1003–1008. 10.1016/j.intimp.2015.08.002 [DOI] [PubMed] [Google Scholar]
- Huang Y. C., Tsai M. S., Hsieh P. C., Shih J. H., Wang T. S., Wang Y. C., et al. (2017). Galangin ameliorates cisplatin-induced nephrotoxicity by attenuating oxidative stress, inflammation and cell death in mice through inhibition of ERK and NF-kappaB signaling. Toxicol. Appl. Pharmacol. 329 128–139. 10.1016/j.taap.2017.05.034 [DOI] [PubMed] [Google Scholar]
- Ji H. L., Tong L. G., Bai C. Z., Song M. Q., Chen N. H., Feng M. L. (2014). [Protective effect of baicalin against rotenone induced injury on PC12 cells]. Zhongguo Zhong Yao Za Zhi 39 2947–2951. [PubMed] [Google Scholar]
- Jiang C., Zhu W., Shao Q., Yan X., Jin B., Zhang M., et al. (2016). Tanshinone IIA protects against folic acid-induced acute kidney injury. Am. J. Chin. Med. 44 737–753. 10.1142/S0192415X16500403 [DOI] [PubMed] [Google Scholar]
- Kang K. P., Park S. K., Kim D. H., Sung M. J., Jung Y. J., Lee A. S., et al. (2011). Luteolin ameliorates cisplatin-induced acute kidney injury in mice by regulation of p53-dependent renal tubular apoptosis. Nephrol. Dial. Transplant. 26 814–822. 10.1093/ndt/gfq528 [DOI] [PubMed] [Google Scholar]
- Kang K. S., Kim H. Y., Yamabe N., Park J. H., Yokozawa T. (2007). Preventive effect of 20(S)-ginsenoside Rg3 against lipopolysaccharide-induced hepatic and renal injury in rats. Free Radic. Res. 41 1181–1188. 10.1080/10715760701581740 [DOI] [PubMed] [Google Scholar]
- Kaur A., Kaur T., Singh B., Pathak D., Singh H., Buttar, et al. (2016). Curcumin alleviates ischemia reperfusion-induced acute kidney injury through NMDA receptor antagonism in rats. Ren. Fail. 38 1462–1467. 10.1080/0886022X.2016.1214892 [DOI] [PubMed] [Google Scholar]
- Khader A., Yang W. L., Kuncewitch M., Prince J. M., Marambaud P., Nicastro J., et al. (2015). Novel resveratrol analogues attenuate renal ischemic injury in rats. J. Surg. Res. 193 807–815. 10.1016/j.jss.2014.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D. H., Jung Y. J., Lee J. E., Lee A. S., Kang K. P., Lee S., et al. (2011). SIRT1 activation by resveratrol ameliorates cisplatin-induced renal injury through deacetylation of p53. Am. J. Physiol. Renal Physiol. 301 F427–F435. 10.1152/ajprenal.00258.2010 [DOI] [PubMed] [Google Scholar]
- Kim H. J., Ravichandran K., Ozkok A., Wang Q., He Z., Jani A., et al. (2014). The water-soluble triptolide derivative PG490-88 protects against cisplatin-induced acute kidney injury. J. Pharmacol. Exp. Ther. 349 518–525. 10.1124/jpet.114.213769 [DOI] [PubMed] [Google Scholar]
- Lameire N. H., Bagga A., Cruz D., De Maeseneer J., Endre Z., Kellum J. A., et al. (2013). Acute kidney injury: an increasing global concern. Lancet 382 170–179. 10.1016/S0140-6736(13)60647-9 [DOI] [PubMed] [Google Scholar]
- Lau A., Wang S., Liu W., Haig A., Zhang Z. X., Jevnikar A. M. (2014). Glycyrrhizic acid ameliorates HMGB1-mediated cell death and inflammation after renal ischemia reperfusion injury. Am. J. Nephrol. 40 84–95. 10.1159/000364908 [DOI] [PubMed] [Google Scholar]
- Li J., Tan Y. J., Wang M. Z., Sun Y., Li G. Y., Wang Q. L., et al. (2019). Loganetin protects against rhabdomyolysis-induced acute kidney injury by modulating the Toll-like receptor 4 signalling pathway. Br. J. Pharmacol. 10.1111/bph.14595 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li P., Liao S. T., Wang J. S., Zhang Q., Xu D. Q., Lv Y., et al. (2017). Protection by Huang-Lian-Jie-Du decoction and its constituent herbs of lipopolysaccharide-induced acute kidney injury. FEBS Open Bio 7 221–236. 10.1002/2211-5463.12178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Xiong W., Yang J., Zhong J., Zhang L., Zheng J., et al. (2015). Attenuation of inflammation by emodin in lipopolysaccharide-induced acute kidney injury via inhibition of toll-like receptor 2 signal pathway. Iran. J. Kidney Dis. 9 202–208. [PubMed] [Google Scholar]
- Liangos O. (2012). Drugs and AKI. Minerva Urol. Nefrol. 64 51–62. [PubMed] [Google Scholar]
- Lim H. A., Lee E. K., Kim J. M., Park M. H., Kim D. H., Choi Y. J., et al. (2012). PPARgamma activation by baicalin suppresses NF-kappaB-mediated inflammation in aged rat kidney. Biogerontology 13 133–145. 10.1007/s10522-011-9361-4 [DOI] [PubMed] [Google Scholar]
- Lin J. L., Ho Y. S. (1994). Flavonoid-induced acute nephropathy. Am. J. Kidney Dis. 23 433–440. 10.1016/S0272-6386(12)81008-0 [DOI] [PubMed] [Google Scholar]
- Lin M., Li L., Zhang Y., Zheng L., Xu M., Rong R., et al. (2014). Baicalin ameliorates H2O2 induced cytotoxicity in HK-2 cells through the inhibition of ER stress and the activation of Nrf2 signaling. Int. J. Mol. Sci. 15 12507–12522. 10.3390/ijms150712507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linkermann A. (2016). Nonapoptotic cell death in acute kidney injury and transplantation. Kidney Int. 89 46–57. 10.1016/j.kint.2015.10.008 [DOI] [PubMed] [Google Scholar]
- Liu C., Cheng Z., Wang Y., Dai X., Zhang J., Xue D. (2015). Paeoniflorin exerts a nephroprotective effect on concanavalin A-induced damage through inhibition of macrophage infiltration. Diagn. Pathol. 10:120. 10.1186/s13000-015-0347-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Gu L. B., Tu Y., Hu H., Huang Y. R., Sun W. (2016). Emodin ameliorates cisplatin-induced apoptosis of rat renal tubular cells in vitro by activating autophagy. Acta Pharmacol. Sin. 37 235–245. 10.1038/aps.2015.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H. B., Meng Q. H., Huang C., Wang J. B., Liu X. W. (2015). Nephroprotective effects of polydatin against ischemia/reperfusion injury: a role for the PI3K/Akt signal pathway. Oxid. Med. Cell. Longev. 2015:362158. 10.1155/2015/362158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W. J., Tang H. T., Jia Y. T., Ma B., Fu J. F., Wang Y., et al. (2010). Notoginsenoside R1 attenuates renal ischemia-reperfusion injury in rats. Shock 34 314–320. 10.1097/SHK.0b013e3181ceede4 [DOI] [PubMed] [Google Scholar]
- Liu X., Huang Z., Zou X., Yang Y., Qiu Y., Wen Y. (2014). Panax notoginseng saponins attenuates cisplatin-induced nephrotoxicity via inhibiting the mitochondrial pathway of apoptosis. Int. J. Clin. Exp. Pathol. 7 8391–8400. [PMC free article] [PubMed] [Google Scholar]
- Liu X., Huang Z., Zou X., Yang Y., Qiu Y., Wen Y. (2015). Possible mechanism of PNS protection against cisplatin-induced nephrotoxicity in rat models. Toxicol. Mech. Methods 25 347–354. 10.3109/15376516.2015.1006492 [DOI] [PubMed] [Google Scholar]
- Liu X. H., Li J., Li Q. X., Ai Y. X., Zhang L. (2008). Protective effects of ligustrazine on cisplatin-induced oxidative stress, apoptosis and nephrotoxicity in rats. Environ. Toxicol. Pharmacol. 26 49–55. 10.1016/j.etap.2008.01.006 [DOI] [PubMed] [Google Scholar]
- Lou X. Y., Cheng J. L., Zhang B. (2015). Therapeutic effect and mechanism of breviscapine on cisplatin-induced nephrotoxicity in mice. Asian Pac. J. Trop. Med. 8 873–877. 10.1016/j.apjtm.2015.09.017 [DOI] [PubMed] [Google Scholar]
- Luo L. N., Xie Q., Zhang X. G., Jiang R. (2016). Osthole decreases renal ischemia-reperfusion injury by suppressing JAK2/STAT3 signaling activation. Exp. Ther. Med. 12 2009–2014. 10.3892/etm.2016.3603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv J., Feng M., Zhang L., Wan X., Zeng Y. C., Liang P. F., et al. (2015). Protective effect of epigallocatechin gallate, a major constituent of green tea, against renal ischemia-reperfusion injury in rats. Int. Urol. Nephrol. 47 1429–1435. 10.1007/s11255-015-1030-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma T., Huang C., Meng X., Li X., Zhang Y., Ji S., et al. (2016). A potential adjuvant chemotherapeutics, 18beta-glycyrrhetinic acid, inhibits renal tubular epithelial cells apoptosis via enhancing BMP-7 epigenetically through targeting HDAC2. Sci. Rep. 6:25396. 10.1038/srep25396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Z. N., Li Y. Z., Li W., Yan X. T., Yang G., Zhang J., et al. (2017). Nephroprotective effects of saponins from leaves of Panax quinquefolius against cisplatin-induced acute kidney injury. Int. J. Mol. Sci. 18:E1407. 10.3390/ijms18071407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng L., Qu L., Tang J., Cai S. Q., Wang H., Li X. (2007). A combination of Chinese herbs, Astragalus membranaceus var. mongholicus and Angelica sinensis, enhanced nitric oxide production in obstructed rat kidney. Vascul. Pharmacol. 47 174–183. 10.1016/j.vph.2007.06.002 [DOI] [PubMed] [Google Scholar]
- Meng X. M., Li H. D., Wu W. F., Ming-Kuen Tang P., Ren G. L., Gao L., et al. (2018). Wogonin protects against cisplatin-induced acute kidney injury by targeting RIPK1-mediated necroptosis. Lab. Invest. 98 79–94. 10.1038/labinvest.2017.115 [DOI] [PubMed] [Google Scholar]
- Ortega-Dominguez B., Aparicio-Trejo O. E., Garcia-Arroyo F. E., Leon-Contreras J. C., Tapia E., Molina-Jijon E., et al. (2017). Curcumin prevents cisplatin-induced renal alterations in mitochondrial bioenergetics and dynamic. Food Chem. Toxicol. 107 373–385. 10.1016/j.fct.2017.07.018 [DOI] [PubMed] [Google Scholar]
- Pan H., Chen J., Shen K., Wang X., Wang P., Fu G., et al. (2015). Mitochondrial modulation by Epigallocatechin 3-Gallate ameliorates cisplatin induced renal injury through decreasing oxidative/nitrative stress, inflammation and NF-kB in mice. PLoS One 10:e0124775. 10.1371/journal.pone.0124775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu X., Fu K., Zhao X., Zhang Y., Yuan Y., Zhang S., et al. (2015). Protective effects of astaxanthin against ischemia/reperfusion induced renal injury in mice. J. Transl. Med. 13:28. 10.1186/s12967-015-0388-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren K., Jin C., Ma P., Ren Q., Jia Z., Zhu D. (2016). Ginsenoside Rd alleviates mouse acute renal ischemia/reperfusion injury by modulating macrophage phenotype. J. Ginseng Res. 40 196–202. 10.1016/j.jgr.2015.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin K., Tuzcu M., Gencoglu H., Dogukan A., Timurkan M., Sahin N., et al. (2010). Epigallocatechin-3-gallate activates Nrf2/HO-1 signaling pathway in cisplatin-induced nephrotoxicity in rats. Life Sci. 87 240–245. 10.1016/j.lfs.2010.06.014 [DOI] [PubMed] [Google Scholar]
- Sancho-Martinez S. M., Lopez-Novoa J. M., Lopez-Hernandez F. J. (2015). Pathophysiological role of different tubular epithelial cell death modes in acute kidney injury. Clin. Kidney J. 8 548–559. 10.1093/ckj/sfv069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato N., Takahashi D., Chen S. M., Tsuchiya R., Mukoyama T., Yamagata S., et al. (2004). Acute nephrotoxicity of aristolochic acids in mice. J. Pharm. Pharmacol. 56 221–229. 10.1211/0022357023051 [DOI] [PubMed] [Google Scholar]
- Shin Y. J., Kim J. J., Kim Y. J., Kim W. H., Park E. Y., Kim I. Y., et al. (2015). Protective effects of quercetin against HgCl(2)-induced nephrotoxicity in sprague-dawley rats. J. Med. Food 18 524–534. 10.1089/jmf.2014.3242 [DOI] [PubMed] [Google Scholar]
- Sue Y. M., Cheng C. F., Chang C. C., Chou Y., Chen C. H., Juan S. H. (2009). Antioxidation and anti-inflammation by haem oxygenase-1 contribute to protection by tetramethylpyrazine against gentamicin-induced apoptosis in murine renal tubular cells. Nephrol. Dial. Transplant. 24 769–777. 10.1093/ndt/gfn545 [DOI] [PubMed] [Google Scholar]
- Sun G., Yang W., Zhang Y., Zhao M. (2017). Esculentoside A ameliorates cecal ligation and puncture-induced acute kidney injury in rats. Exp. Anim. 66 303–312. 10.1538/expanim.16-0102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan R. Z., Liu J., Zhang Y. Y., Wang H. L., Li J. C., Liu Y. H., et al. (2019). Curcumin relieved cisplatin-induced kidney inflammation through inhibiting Mincle-maintained M1 macrophage phenotype. Phytomedicine 52 284–294. 10.1016/j.phymed.2018.09.210 [DOI] [PubMed] [Google Scholar]
- Thomas M. E., Blaine C., Dawnay A., Devonald M. A., Ftouh S., Laing C., et al. (2015). The definition of acute kidney injury and its use in practice. Kidney Int. 87 62–73. 10.1038/ki.2014.328 [DOI] [PubMed] [Google Scholar]
- Tu Y., Sun W., Wan Y. G., Gao K., Liu H., Yu B. Y., et al. (2014). Dahuang Fuzi Decoction ameliorates tubular epithelial apoptosis and renal damage via inhibiting TGF-beta1-JNK signaling pathway activation in vivo. J. Ethnopharmacol. 156 115–124. 10.1016/j.jep.2014.08.035 [DOI] [PubMed] [Google Scholar]
- Waikar S. S., Liu K. D., Chertow G. M. (2008). Diagnosis, epidemiology and outcomes of acute kidney injury. Clin. J. Am. Soc. Nephrol. 3 844–861. 10.2215/CJN.05191107 [DOI] [PubMed] [Google Scholar]
- Wang H. P., Liu C. W., Chang H. W., Tsai J. W., Sung Y. Z., Chang L. C. (2013). Cordyceps sinensis protects against renal ischemia/reperfusion injury in rats. Mol. Biol. Rep. 40 2347–2355. 10.1007/s11033-012-2316-2 [DOI] [PubMed] [Google Scholar]
- Wang L., Mao N., Tan R. Z., Wang H. L., Wen J., Liu Y. H., et al. (2015). Ginsenoside Rg1 reduces aldosterone-induced autophagy via the AMPK/mTOR pathway in NRK-52E cells. Int. J. Mol. Med. 36 518–526. 10.3892/ijmm.2015.2242 [DOI] [PubMed] [Google Scholar]
- Wang N., Mao L., Yang L., Zou J., Liu K., Liu M., et al. (2017). Resveratrol protects against early polymicrobial sepsis-induced acute kidney injury through inhibiting endoplasmic reticulum stress-activated NF-kappaB pathway. Oncotarget 8 36449–36461. 10.18632/oncotarget.16860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P., Wang W., Shi Q., Zhao L., Mei F., Li C., et al. (2016). Paeoniflorin ameliorates acute necrotizing pancreatitis and pancreatitis induced acute renal injury. Mol. Med. Rep. 14 1123–1131. 10.3892/mmr.2016.5351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Yao Y. M., Wang W. J., Xian L. M., Dong N., Xu S., et al. (2007). [Effect of Xuebijing injection on renal high mobility group box-1 protein expression and acute kidney injury in rats after scald injury]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 29 478–483. [PubMed] [Google Scholar]
- Wang X., Zhao H., Shao Y., Wang P., Wei Y., Zhang W., et al. (2014). Nephroprotective effect of astaxanthin against trivalent inorganic arsenic-induced renal injury in wistar rats. Nutr. Res. Pract. 8 46–53. 10.4162/nrp.2014.8.1.46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Feng F., Liu M., Xue J., Huang H. (2018). Resveratrol ameliorates sepsis-induced acute kidney injury in a pediatric rat model via Nrf2 signaling pathway. Exp. Ther. Med. 16 3233–3240. 10.3892/etm.2018.6533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C. H., Chen A. Z., Yen G. C. (2015). Protective effects of glycyrrhizic acid and 18beta-glycyrrhetinic acid against cisplatin-induced nephrotoxicity in BALB/c mice. J. Agric. Food Chem. 63 1200–1209. 10.1021/jf505471a [DOI] [PubMed] [Google Scholar]
- Wu J., Pan X., Fu H., Zheng Y., Dai Y., Yin Y., et al. (2017). Effect of curcumin on glycerol-induced acute kidney injury in rats. Sci. Rep. 7:10114. 10.1038/s41598-017-10693-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu M. F., Li P. C., Chen C. C., Ye S. S., Chien C. T., Yu C. C. (2011). Cordyceps sobolifera extract ameliorates lipopolysaccharide-induced renal dysfunction in the rat. Am. J. Chin. Med. 39 523–535. 10.1142/S0192415X11009007 [DOI] [PubMed] [Google Scholar]
- Xia S., Lin H., Liu H., Lu Z., Wang H., Fan S., et al. (2019). Honokiol attenuates sepsis-associated acute kidney injury via the inhibition of oxidative stress and inflammation. Inflammation 10.1007/s10753-018-0937-x [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Xu D., Chen M., Ren X., Wu Y. (2014). Leonurine ameliorates LPS-induced acute kidney injury via suppressing ROS-mediated NF-kappaB signaling pathway. Fitoterapia 97 148–155. 10.1016/j.fitote.2014.06.005 [DOI] [PubMed] [Google Scholar]
- Xu J. J., Zhen J. T., Tang L., Lin Q. M. (2017). Intravenous injection of Xuebijing attenuates acute kidney injury in rats with paraquat intoxication. World J. Emerg. Med. 8 61–64. 10.5847/wjem.j.1920-8642.2017.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Y., Zhang J., Liu J., Li S., Li C., Wang W., et al. (2015). Luteolin attenuate the D-galactose-induced renal damage by attenuation of oxidative stress and inflammation. Nat. Prod. Res. 29 1078–1082. 10.1080/14786419.2014.981181 [DOI] [PubMed] [Google Scholar]
- Xu S., Gao Y., Zhang Q., Wei S., Chen Z., Dai X., et al. (2016). SIRT1/3 activation by resveratrol attenuates acute kidney injury in a septic rat model. Oxid. Med. Cell. Longev. 2016:7296092. 10.1155/2016/7296092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan W., Xu Y., Yuan Y., Tian L., Wang Q., Xie Y., et al. (2017). Renoprotective mechanisms of Astragaloside IV in cisplatin-induced acute kidney injury. Free Radic. Res. 51 669–683. 10.1080/10715762.2017.1361532 [DOI] [PubMed] [Google Scholar]
- Yang B., Xie Y., Guo M., Rosner M. H., Yang H., Ronco C. (2018). Nephrotoxicity and Chinese herbal medicine. Clin. J. Am. Soc. Nephrol. 13 1605–1611. 10.2215/CJN.11571017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F., Ren L., Zhuo L., Ananda S., Liu L. (2012). Involvement of oxidative stress in the mechanism of triptolide-induced acute nephrotoxicity in rats. Exp. Toxicol. Pathol. 64 905–911. 10.1016/j.etp.2011.03.013 [DOI] [PubMed] [Google Scholar]
- Yang F., Zhuo L., Ananda S., Sun T., Li S., Liu L. (2011). Role of reactive oxygen species in triptolide-induced apoptosis of renal tubular cells and renal injury in rats. J. Huazhong Univ. Sci. Technolog. Med. Sci. 31 335–341. 10.1007/s11596-011-0377-4 [DOI] [PubMed] [Google Scholar]
- Yang L., Xing G., Wang L., Wu Y., Li S., Xu G., et al. (2015). Acute kidney injury in China: a cross-sectional survey. Lancet 386 1465–1471. 10.1016/S0140-6736(15)00344-X [DOI] [PubMed] [Google Scholar]
- Yang Y., Song M., Liu Y., Liu H., Sun L., Peng Y., et al. (2016). Renoprotective approaches and strategies in acute kidney injury. Pharmacol. Ther. 163 58–73. 10.1016/j.pharmthera.2016.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye H. Y., Jin J., Jin L. W., Chen Y., Zhou Z. H., Li Z. Y. (2017). Chlorogenic acid attenuates lipopolysaccharide-induced acute kidney injury by inhibiting TLR4/NF-kappaB signal pathway. Inflammation 40 523–529. 10.1007/s10753-016-0498-9 [DOI] [PubMed] [Google Scholar]
- Ye Q., Zhu Y. I., Ye S., Liu H., She X., Niu Y., et al. (2016). Gypenoside attenuates renal ischemia/reperfusion injury in mice by inhibition of ERK signaling. Exp. Ther. Med. 11 1499–1505. 10.3892/etm.2016.3034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye R., Yang Q., Kong X., Han J., Zhang X., Zhang Y., et al. (2011). Ginsenoside Rd attenuates early oxidative damage and sequential inflammatory response after transient focal ischemia in rats. Neurochem. Int. 58 391–398. 10.1016/j.neuint.2010.12.015 [DOI] [PubMed] [Google Scholar]
- Yokozawa T., Dong E. (2001). Role of ginsenoside-Rd in cisplatin-induced renal injury: special reference to DNA fragmentation. Nephron 89 433–438. 10.1159/000046116 [DOI] [PubMed] [Google Scholar]
- Yokozawa T., Liu Z. W. (2000). The role of ginsenoside-Rd in cisplatin-induced acute renal failure. Ren. Fail. 22 115–127. 10.1081/JDI-100100858 [DOI] [PubMed] [Google Scholar]
- Yokozawa T., Liu Z. W., Dong E. (1998). A study of ginsenoside-Rd in a renal ischemia-reperfusion model. Nephron 78 201–206. 10.1159/000044911 [DOI] [PubMed] [Google Scholar]
- Yu C., Li P., Qi D., Wang L., Qu H. L., Zhang Y. J., et al. (2017). Osthole protects sepsis-induced acute kidney injury via down-regulating NF-kappaB signal pathway. Oncotarget 8 4796–4813. 10.18632/oncotarget.13592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu H., Zhou Q., Huang R., Yuan M., Ao X., Yang J. (2012). [Effect of Cordyceps sinensis on the expression of HIF-1alpha and NGAL in rats with renal ischemia-reperfusion injury]. Zhong Nan Da Xue Xue Bao Yi Xue Ban 37 57–66. 10.3969/j.issn.1672-7347.2012.01.011 [DOI] [PubMed] [Google Scholar]
- Yu M., Xue J., Li Y., Zhang W., Ma D., Liu L., et al. (2013). Resveratrol protects against arsenic trioxide-induced nephrotoxicity by facilitating arsenic metabolism and decreasing oxidative stress. Arch. Toxicol. 87 1025–1035. 10.1007/s00204-013-1026-4 [DOI] [PubMed] [Google Scholar]
- Yuxi Q., Zhang H., Baili Y., Shi S. (2017). Effects of xuebijing injection for patients with sepsis-induced acute kidney injury after Wenchuan earthquake. Altern. Ther. Health Med. 23 36–42. [PubMed] [Google Scholar]
- Zhang J., Yang S., Chen F., Li H., Chen B. (2017). Ginkgetin aglycone ameliorates LPS-induced acute kidney injury by activating SIRT1 via inhibiting the NF-kappaB signaling pathway. Cell Biosci. 7:44. 10.1186/s13578-017-0173-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J. X., Dang S. C., Qu J. G., Wang X. Q. (2006). Ligustrazine alleviates acute renal injury in a rat model of acute necrotizing pancreatitis. World J. Gastroenterol. 12 7705–7709. 10.3748/wjg.v12.i47.7705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Sun D., Bao Y., Shi Y., Cui Y., Guo M. (2017). Nerolidol protects against LPS-induced acute kidney injury via inhibiting TLR4/NF-kappaB signaling. Phytother. Res. 31 459–465. 10.1002/ptr.5770 [DOI] [PubMed] [Google Scholar]
- Zhang W. X., Zhang Z. M., Zhang Z. Q., Wang Y., Zhou W. (2014). Andrographolide induced acute kidney injury: analysis of 26 cases reported in Chinese Literature. Nephrology 19 21–26. 10.1111/nep.12172 [DOI] [PubMed] [Google Scholar]
- Zhang Z., Gao X., Guo M., Jiang H., Cao Y., Zhang N. (2016). The protective effect of baicalin against lead-induced renal oxidative damage in mice. Biol. Trace Elem. Res. 175 129–135. 10.1007/s12011-016-0731-2 [DOI] [PubMed] [Google Scholar]
- Zhang Z., Gao X., Guo M., Jiang H., Cao Y., Zhang N. (2017). The protective effect of baicalin against lead-induced renal oxidative damage in mice. Biol. Trace Elem. Res. 175 129–135. 10.1007/s12011-016-0731-2 [DOI] [PubMed] [Google Scholar]
- Zhao H., Liu Z., Shen H., Jin S., Zhang S. (2016). Glycyrrhizic acid pretreatment prevents sepsis-induced acute kidney injury via suppressing inflammation, apoptosis and oxidative stress. Eur. J. Pharmacol. 781 92–99. 10.1016/j.ejphar.2016.04.006 [DOI] [PubMed] [Google Scholar]
- Zhou J., Zhang H. A., Lin Y., Liu H. M., Cui Y. M., Xu Y., et al. (2014). Protective effect of ginsenoside against acute renal failure via reduction of renal oxidative stress and enhanced expression of ChAT in the proximal convoluted tubule and ERK1/2 in the paraventricular nuclei. Physiol. Res. 63 597–604. [DOI] [PubMed] [Google Scholar]
- Zhou L., Fu P., Huang X. R., Liu F., Lai K. N., Lan H. Y. (2010). Activation of p53 promotes renal injury in acute aristolochic acid nephropathy. J. Am. Soc. Nephrol. 21 31–41. 10.1681/ASN.2008111133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Q., Hu S. (2010). [Effect of Cordyceps Cinensis extractant on apoptosis and expression of Toll-like receptor 4 mRNA in the ischemia-reperfusion injured NRK-52E cells]. Zhong Nan Da Xue Xue Bao Yi Xue Ban 35 77–84. 10.3969/j.issn.1672-7347.2010.01.011 [DOI] [PubMed] [Google Scholar]
- Zhu J. S., Halpern G. M., Jones K. (1998). The scientific rediscovery of an ancient Chinese herbal medicine: Cordyceps sinensis: part I. J. Altern. Complement. Med. 4 289–303. 10.1089/acm.1998.4.3-289 [DOI] [PubMed] [Google Scholar]
- Zhu M. X., Ran B., Feng Z. Q., Pan Q. W. (2009). [Effects of Rb1 and Rg1 on the expression of Bcl-2, Bax in apoptosis of HK-2 cells induced by the serum of kidney ischemia/reperfusion]. Zhongguo Ying Yong Sheng Li Xue Za Zhi 25 496–499. [PubMed] [Google Scholar]
- Zhu X. L., Wang Y. J., Yang Y., Yang R. C., Zhu B., Zhang Y., et al. (2012). Suppression of lipopolysaccharide-induced upregulation of toll-like receptor 4 by emodin in mouse proximal tubular epithelial cells. Mol. Med. Rep. 6 493–500. 10.3892/mmr.2012.960 [DOI] [PubMed] [Google Scholar]
- Zhu Y., Fu Y., Lin H. (2016). Baicalin inhibits renal cell apoptosis and protects against acute kidney injury in pediatric sepsis. Med. Sci. Monit. 22 5109–5115. 10.12659/MSM.899061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou P., Song J., Jiang B., Pei F., Chen B., Yang X., et al. (2014). Epigallocatechin-3-gallate protects against cisplatin nephrotoxicity by inhibiting the apoptosis in mouse. Int. J. Clin. Exp. Pathol. 7 4607–4616. [PMC free article] [PubMed] [Google Scholar]
- Zuk A., Bonventre J. V. (2016). Acute kidney injury. Annu. Rev. Med. 67 293–307. 10.1146/annurev-med-050214-013407 [DOI] [PMC free article] [PubMed] [Google Scholar]