Abstract
Background:
Medial patellofemoral ligament (MPFL) reconstruction is the treatment of choice for recurrent patellar instability in the skeletally immature patient. Avoiding the open physes during anatomic MPFL reconstruction is a challenge in this population.
Purpose:
To describe a novel method using magnetic resonance imaging (MRI) to determine the distance from the Schöttle point to the medial distal femoral physis among skeletally immature individuals with patellar instability.
Study Design:
Descriptive laboratory study.
Methods:
Preoperative MRI scans were analyzed from 34 patients with open distal femoral physes and lateral patellar instability. With the multiplanar reconstruction mode on a picture archiving and communication system (PACS), the location of the Schöttle point was determined according to previously reported distances from the posterior femoral cortical line and the posterior origin of the medial femoral condyle. This location was then extrapolated to the most medial sagittal slice on MRI showing the medial distal femoral physis. The distance was measured from this point to the most distal aspect of the physis.
Results:
The mean age of the study cohort was 13.6 years (range, 10.6-15.7 years); there were 13 males and 21 females. The mean distance from the medial distal femoral physis to the Schöttle point was 7.27 ± 1.78 mm. The Schöttle point was distal to the medial distal femoral physis in all cases. There was no significant correlation between age and mean distance in either the overall study population (r = 0.046, P = .798) or when stratified by sex (females, P = .629; males, P = .089). The distance between the Schöttle point and the medial distal femoral physis was shorter for females than for males (6.51 vs 7.71 mm, P = .043). After adjustment for age, females on average were 1.31 mm closer to the Schöttle point than were males (B = –1.31, P = .041).
Conclusion:
This technique can be used to determine the distance between the medial distal femoral physis and the Schöttle point. The Schöttle point was distal to the physis in all patients, and it was closer to the physis in skeletally immature females compared with age-matched males.
Clinical Relevance:
The long-term repercussions of improperly placed MPFL reconstruction include recurrent patellar instability, increased patellofemoral contact pressures and overtensioning of the ligament, and possibly patellofemoral arthritis. The current technique can be used preoperatively to determine the appropriate safe distance for drilling a socket distal to the physis.
Keywords: patellar instability, Schöttle point, pediatric sports medicine, medial patellofemoral ligament (MPFL) reconstruction
Patellar instability is a common injury in the active youth population, with an estimated annual incidence of first-time dislocations of 5.8 per 100,0004 and incidence increasing to 43 per 100,000 in children younger than 16 years.15 Fithian et al4 found the highest risk to be among females aged 10 to 17 years. Skeletal immaturity is among other anatomic factors that have been associated with a higher risk of patellar dislocation.6,10,11
Medial patellofemoral ligament (MPFL) reconstruction is the treatment of choice for patients with recurrent patellar instability. Using cadaveric specimens confirmed by fluoroscopy, Schöttle et al19 and Redfern et al17 identified anatomic landmarks on the medial femoral condyle to reproducibly identify the femoral insertion of the MPFL, which included a point 1 mm anterior to the posterior cortex extension line, 2.5 mm distal to the posterior origin of the medial femoral condyle, and proximal to the level of the Blumensaat line on lateral radiograph. In MPFL reconstruction, anatomic reconstruction is recommended, as graft malpositioning has been shown to alter patellofemoral biomechanics and lead to increased force and contact pressure to the medial patellofemoral cartilage.2,18 Parikh et al16 showed that 47% of complications in MPFL reconstruction among young patients were due to preventable technical factors, with one-third of these complications associated with improper femoral tunnel placement.
In the skeletally immature patient, the relationship between the femoral insertion of the MPFL and the femoral physis is important. The challenge is achieving anatomic fixation on the femoral side while respecting the open physis.14 Physeal safety is critical to prevent leg length discrepancy and angular deformity. Additionally, anatomic reproduction of the femoral insertion site of the MPFL is important for re-creating an isometric MPFL reconstruction and for potentially long-term outcomes regarding cartilaginous wear of the patellofemoral compartment.2,12
Prior cadaveric and radiographic studies1,5,8,13,20–22 have shown anatomic variation in the distance between the femoral insertion of the MPFL and distal femoral physis, with the distance generally being within millimeters of the physis. Other factors, such as age and sex, have also been suggested to influence this distance in patients with open physes.1,5,21 Magnetic resonance imaging (MRI) is normally obtained preoperatively after a patellar instability event to evaluate for concomitant injuries, including osteochondral fractures and/or loose bodies. MRI is a preferred imaging modality in the skeletally immature population given its lack of ionizing radiation.
We present a novel method for determining the distance from the Schöttle point to the medial distal femoral physis on MRI that can be translated to a safe intraoperative location for femoral socket placement in MPFL reconstruction via an all-epiphyseal technique. We hypothesized that this method will be reproducible between measurers. We also hypothesized that the distance between the Schöttle point and the distal femoral physis will be anatomically close and will decrease from the MPFL origin, becoming more proximal with increasing age and being less for females than males after adjusting for age.
Methods
After institutional review board approval, we retrospectively reviewed MRI scans (1.5- or 3.0-T magnets; General Electric Healthcare) performed from 2011 to 2017 in 34 children and adolescents after acute lateral patellar dislocation. An electronic picture archiving and communication system (PACS; Sectra IDS7) was used to identify patients who underwent knee MRI at a single institution. Patients were eligible for inclusion if they were between 10 and 16 years old and skeletally immature and had recently sustained a patellar dislocation. Exclusion criteria included previous surgical treatment and significant congenital or syndromic structural abnormality.
The MRI scans were independently reviewed by a sports medicine fellowship–trained attending physician with a practice focus on patellar instability (B.S.S.; senior author) and a current sports medicine fellow (M.E.B.). Using the sagittal proton density series and multiplanar reconstruction mode on our PACS to create a perfect lateral image, we determined the location of the Schöttle point based on previously reported distances from the posterior femoral cortical line and posterior origin of the medial femoral condyle (Appendix and Figure 1). This location was then extrapolated to the most medial sagittal slice on MRI showing the medial distal femoral physis. The distance was measured from this point to the most distal aspect of the physis (Figure 2).
Figure 1.
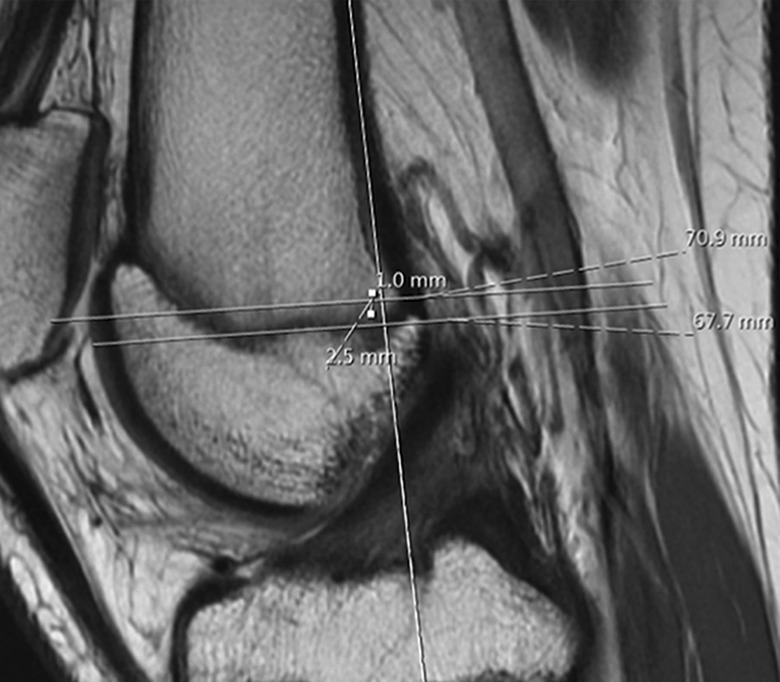
Using the sagittal series on magnetic resonance imaging, a line is made in line with the posterior femoral cortex on the image with the best view of the anterior cruciate ligament. A second line is drawn at the most posterior aspect of the Blumensaat line perpendicular to the posterior cortical line. A third line is drawn at the most proximal aspect of the posterior femoral condyle that is perpendicular to the posterior cortical line. A point is measured that is 1 mm anterior to the posterior cortical line and 2.5 mm distal to the medial femoral condyle line, designated as the Schöttle point.
Figure 2.
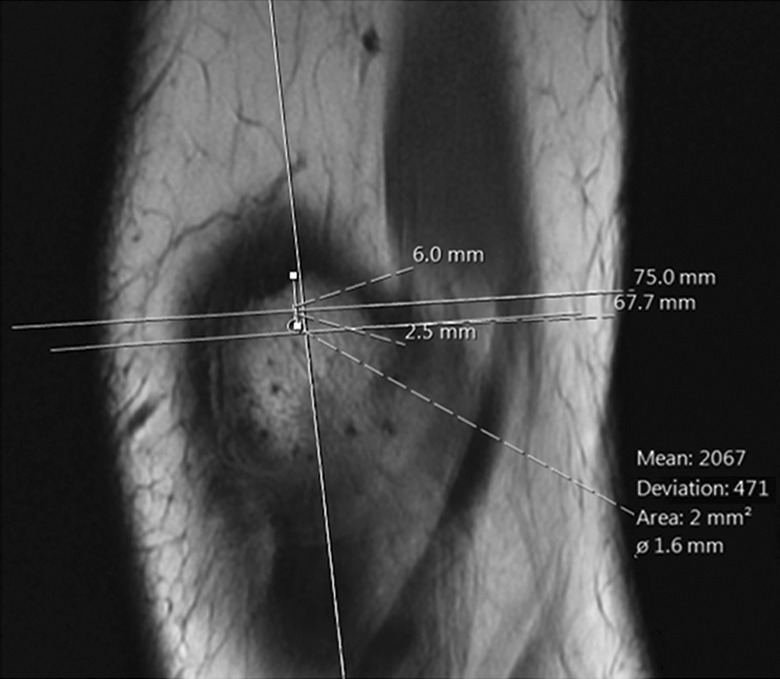
Scroll to the farthest sagittal image where the physis is still visible on the medial femoral condyle. Measure the proximal-distal distance from the physis to the Schöttle point in a line perpendicular to the posterior femoral cortex. Here the distance is 6 mm.
Statistical Methods
Shapiro-Wilks tests were performed to evaluate the assumption of normality for all continuous variables. The intraclass correlation coefficient (ICC) was used to determine interrater reliability of mean distance measures between the senior author and the fellow. The Pearson correlation coefficient was used to evaluate the relationship between the continuous variables of age and mean distance, for the overall population as well as stratified by sex. An independent samples t test was used to compare the mean distance measurements between males and females. Age and sex were included as variables of interest in a multivariable regression model for the dependent variable of mean distance between the Schöttle point and the distal femoral physis. All analyses were performed with SPSS (v 23.0; IBM Corp). Statistical significance was defined as P ≤ .05.
Results
Shapiro-Wilks tests confirmed the assumption of normality for age (P = .157) and mean distance (P = .383). The mean age of the cohort was 13.6 years (range, 10.6-15.7 years). There were 13 males and 21 females (N = 34). The mean ± SD distance from the medial distal femoral physis to the Schöttle point was 7.27 ± 1.78 mm (range, 3.3-10.5 mm). The Schöttle point was distal to the medial distal femoral physis in all cases. The interrater reliability of mean distance between raters was excellent by the standards described by Landis and Koch9 (ICC = 0.854; 95% CI, 0.708-0.927; P < .001). As reliability was so high between raters, the analysis of data reported is resultant from measurements from a single, randomly selected rater (B.S.S.).
Bivariate correlation between age and mean distance showed no significance for the overall population (r = 0.046, P = .798) (Table 1). When stratified by sex, neither males (P = .089) nor females (P = .629) showed any correlation between age and distance. Results from the independent samples t test showed that on average, females (6.51 mm; range, 3.3-10.5 mm) had a shorter distance to the Schöttle point when compared with males (7.71 mm; range, 4.2-10.2 mm; P = .043) (Table 2). Multivariable regression analysis determined that after adjustment for age, females on average were 1.31 mm closer to the Schöttle point compared with males (B = –1.31, P = .041) (Table 3).
TABLE 1.
Bivariate Correlation Between Mean Distance to Physis and Patient Agea
| r | P Value | |
|---|---|---|
| Overall (N = 34) | 0.046 | .798 |
| Males (n = 13) | 0.490 | .089 |
| Females (n = 21) | 0.112 | .629 |
aResults of Pearson correlation between the mean distance from the physis to the Schöttle point and patient age at the time of magnetic resonance imaging scan.
TABLE 2.
Comparison of Mean Distance With Physis and Patient Age Between the Sexesa
| Males | Females | P Value | |
|---|---|---|---|
| Distance from physis to the Schöttle point | 7.71 ± 1.36 | 6.51 ± 1.73 | .043 |
| Age at MRI, y | 14.26 ± 1.35 | 13.27 ± 1.22 | .033 |
aData are reported as mean ± SD. MRI, magnetic resonance imaging.
TABLE 3.
Multivariable Regression Model for Variables Associated With Mean Distance to Physis
| Clinical Characteristic | Beta Coefficient | SE | P Value |
|---|---|---|---|
| Female sex | –1.31 | 0.61 | .041 |
| Age | –0.12 | 0.23 | .602 |
Discussion
In this study, we demonstrated a reproducible method of measuring the distance between the Schöttle point and the medial distal femoral physis. This novel, reproducible technique can be utilized preoperatively to determine the appropriate safe distance from the physis for socket drilling and fixation entry point using preoperative MRI. Another valuable use for this technique is the ability to assess femoral MPFL location on postoperative MRI in patients with failed MPFL reconstruction. As there is anatomic variation among all patients, this method can offer individualized assessment of the MPFL to the medial distal femoral distance to best re-create anatomy while protecting the physis.
Ensuring physeal safety during MPFL reconstruction is critical in the skeletally immature population, as the standard adult surgical technique of using screw fixation in the distal femur has been shown to frequently disturb the medial distal femoral physis.5 An understanding of the close proximity of the MPFL origin to the medial distal femoral physis is important when considering screw placement and trajectory, as placement distal to the physis with a distal oblique trajectory has been shown to safely avoid physeal and joint penetration as compared with parallel screw placement.5 Determining a safe and anatomic starting point is critical during preoperative planning for MPFL reconstruction.
The distance between the femoral insertion of the MPFL and the distal femoral physis has shown anatomic variation in cadaveric21,22 and radiographic5,8,13,20 studies. While this has most commonly been measured on plain radiographs,13,19,20 our study used preoperative MRI scans to accurately determine the distance between the femoral insertion of the MPFL and the medial distal femoral physis with a novel, reproducible method with high interrater reliability (ICC = 0.854, P < .001). This is a consistent method that is based on the patient’s own anatomic landmarks. Our method allows for the creation of a more perfect lateral image, accounting for some of the rotational variability with lateral radiographs. Unlike plain radiographs and computed tomography scans, MRI does not use ionizing radiation, which is another important consideration in the pediatric population, particularly in the instability population, who may be subjected to multiple imaging studies during the clinical course of their condition.
Our study revealed the mean distance between the Schöttle point and the medial distal femoral physis to be 7.27 ± 1.78 mm distal to the physis. This location is similar to prior radiographic and cadaveric studies with different measurement methods. Using MRI, Greenrod et al5 reported that the femoral origin of the MPFL was distal to the distal femoral physis in all patients by a mean 10 mm (range, 2-16 mm), while Kepler et al8 cited this distance as 5 mm distal to the femoral growth plate (range, 7.5 mm proximal to 16 mm distal). Using the Schöttle method on lateral plain radiographs, Shea et al20 found the MPFL origin to be on average between 2 and 5 mm proximal to the physis depending on sex, while Nelitz et al13 cited the location as being 3.2 mm proximal to the physis. However, when considering the anteroposterior measurements, Nelitz et al13 indicated the median origin of the MPFL to be 6.4 mm (range, 2.9-8.5 mm) distal to the physis in all patients.
Our measurement of the Schöttle point being on average 7.27 mm (range, 3.3-10.5 mm) distal to the physis, as well as the distances from the MRI studies of Kepler et al8 and Greenrod et al,5 were slightly greater in distance from the physis and more frequently distal to the physis as compared with the studies using plain radiographs.13,20 The cadaveric study by Farrow et al3 revealed a mean distance similar to that of our study, with the MPFL attachment being a mean 8.5 mm distal to the medial aspect of the distal femoral physis. The similarity in findings between the MRI studies and the cadaveric study could be related to the increased accuracy of identification of anatomic landmarks on MRI over plain radiographs. Furthermore, Huston et al7 reported significant interobserver variance on both adult and pediatric lateral knee radiographs using the Schöttle technique, although it was greater for adult knees. This finding was potentially related to the perceived landmark variability on plain radiographs.
While our study demonstrated no association between age and the distance of the Schöttle point to the distal femoral physis, we did find that this distance was 1.31 mm closer/more proximal in females compared with males of the same age. While our numbers may have been too low to detect a significant difference, females generally reach skeletal maturity before males. Although a difference of 1.31 mm may not be clinically significant, the closer distance to the physis and MPFL origin for age-matched females could suggest that the distance between the MPFL origin and physis decreases or the MPFL origin becomes more proximal when approaching skeletal maturity. In a recent cadaveric study, Shea et al21 reported a more proximal femoral origin footprint of the MPFL in older specimens, with the majority ≥7 years old having an MPFL origin just proximal to the physis (0.8 mm proximal to physis ≥7 years old vs 4.7 mm distal <7 years old). Similarly, in an MRI review of skeletally immature knee anatomy, Edmonds et al1 indicated that the MPFL origin starts distal to the physis and moves proximally with age (ρ = 0.33, P < .001) such that, by age 7 years, it is found at or above the femoral physis. This, however, differs from the MRI findings of Greenrod et al,5 who found a statistically significant increase in the MPFL-to-physis distance (approximately 0.6 mm more distal per year; r = 0.51, P < .001) with advancing age. More research is necessary to better define the relationship among sex, age, and the distance of the MPFL origin to the distal femoral physis.
Limitations
There are several limitations to this study. This was an observational case series; thus, we were not able to monitor the changes in the distance of the Schöttle point to physis within specific individuals over time. We also included more females (n = 21) than males (n = 13), but this is representative of the young patellar instability population.4 Our measurements included the sagittal view only, which does not fully consider the distal femoral growth plate anatomy in all planes. However, as the lateral image is important for determining the start point to drill the femoral socket in preoperative planning and intraoperatively, we believe that this is the most important view to assess placement. This method will not replace the standard intraoperative method of using fluoroscopy to identify the Schöttle point, but it will provide individual approximation of the distance between the Schöttle point and the medial distal femoral physis with advanced imaging to aid in preoperative planning. Unique to this study, the use of the multiplanar reconstruction mode of the PACS to create a perfect lateral image of the knee was important for accurate and reproducible measurements, although not all imaging systems may have this feature.
Further limitations include our sample numbers, which may not have been high enough to detect clinically significant differences in comparison by age and sex. Additionally, we did not include patients younger than 10 years in this analysis, as our aim was to include the nonsyndromic traumatic sports-related dislocator population. In comparing our study with previous relevant studies, we found notable differences in study subjects, including cadaveric versus living patients, imaging modalities (radiograph, computed tomography, and MRI), and method of localization of MPFL insertion (anatomic dissection, radiological landmarks, and direct identification of ligament insertion on MRI), making direct comparison imperfect. However, we tried to call attention to and address these differences in the analysis of the current study with what is available in the literature. Finally, we note that while obtaining an anatomic radiographic starting point for graft insertion is important, graft isometry still must be assessed and fixation adjusted if the point is not found to be isometric.
Conclusion
For patients with open physes, the novel technique we describe can be utilized preoperatively to determine the appropriate safe distance to be drilling a socket. We found the Schöttle point to be distal to the physis in all patients, with skeletally immature females having a closer distance to the physis compared with age-matched males. As there is anatomic variation among all patients, this method can offer individualized assessment of the distance between the Schöttle point and the medial distal femoral physis to best re-create anatomy while protecting the physis.
Appendix
Directions for Determining the Schöttle Point on Magnetic Resonance Imaging With a Picture Archiving and Communication System
Open Sagittal Series on MRI.
- Right-click—select “MPR.”
- Image with 4 individual screens will open.
- Top left—axial (poor resolution)
- Bottom left—coronal (poor resolution)
- Top right—sagittal (good resolution)
- First: Scroll on the axial image (top left screen) until you see the posterior femoral condyles. Adjust the red line so that it touches the posterior aspect of both the medial and lateral femoral condyle.
- Drag the line proximal and distal by grabbing in the middle of the screen.
- Change the orientation/tilt of the line by grabbing the thicker portions of the line on the sides of the screen.
- Second: Adjust the yellow horizontal line on the coronal image (bottom left screen) so that it is touching the distal aspect of both the medial and the lateral femoral condyle.
- Drag the line proximal and distal by grabbing in the middle of the screen.
- Change the orientation/ tilt of the line by grabbing the thicker portions of the line on the sides of the screen.
- This should have changed the orientation of the sagittal image (top right) so that the condyles are “perfectly” superimposed as in a true lateral radiograph.
- You can scroll through the sagittal series to do a rough check of this.
Double-click the sagittal image to make it larger.
Scroll to the sagittal image with the best view of the ACL.
- Draw the line of the posterior cortex.
- Right-click and select the measurement tool.
- Click to make the start of the line, move the mouse to draw a line, scroll to another image and click the mouse again to end the line.
- This will ensure that the measurement shows up as you scroll through the series.
- Go back to the image with the best view of the ACL and adjust the line so that it is on the posterior cortex.
- Draw the line at the most posterior aspect of the Blumensaat line.
- Go to the image where you can see the ACL, and draw a line at the most posterior aspect of the Blumensaat line (top of ACL) so that it is perpendicular to the posterior cortical line.
- Use the technique in 8b to make the line stay in place.
- Draw the line at the most proximal aspect of the medial femoral condyle.
- Go to the image at the middle of the medial femoral condyle on the coronal image—draw a line at the proximal aspect of the medial femoral condyle so that it is perpendicular to the posterior cortical line.
- Use the technique in 8b to make the line stay in place.
- Measure the location that is
- 1 mm anterior to the posterior cortical line (8).
- 2.5 mm distal to the medial femoral condyle line.
- Mark the location
- Right-click—select the ROI circle tool.
- One click to start the circle, scroll to another image, and do the second click. This will place a small circle at the location of the Schöttle point. It should also stay in place.
- Scroll to the farthest sagittal image where you can still see the physis on the medial femoral condyle.
- Measure the proximal-distal distance from the physis to the Schöttle point in a line perpendicular to the posterior femoral cortex.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.E.B. has received educational support from Smith & Nephew; S.R.B. has received educational support from Arthrex; and B.S.S. has received speaking fees and educational support from Arthrex and hospitality payments from DePuy. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Hospital for Special Surgery Institutional Review Board (No. 2014-123).
References
- 1. Edmonds EW, Bathen M, Bastrom TP. Normal parameters of the skeletally immature knee: developmental changes on magnetic resonance imaging. J Pediatr Orthop. 2015;35(7):712–720. [DOI] [PubMed] [Google Scholar]
- 2. Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34(9):1478–1485. [DOI] [PubMed] [Google Scholar]
- 3. Farrow LD, Alentado VJ, Abdulnabi Z, Gilmore A, Liu RW. The relationship of the medial patellofemoral ligament attachment to the distal femoral physis. Am J Sports Med. 2014;42(9):2214–2218. [DOI] [PubMed] [Google Scholar]
- 4. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. [DOI] [PubMed] [Google Scholar]
- 5. Greenrod W, Cox J, Astori I, Baulch J, Williams J. A magnetic resonance imaging study of the significance of the distal femoral physis during medial patellofemoral ligament reconstruction. Orthop J Sports Med. 2013;1(4):23259 67113502638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations: the natural history. Am J Sports Med. 1986;14(2):117–120. [DOI] [PubMed] [Google Scholar]
- 7. Huston KL, Okoroafor UC, Kaar SG, Wentt CL, Saluan P, Farrow LD. Evaluation of the Schöttle technique in the pediatric knee. Orthop J Sports Med. 2017;5(11):23259 67117740078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kepler CK, Bogner EA, Hammoud S, Malcolmson G, Potter HG, Green DW. Zone of injury of the medial patellofemoral ligament after acute patellar dislocation in children and adolescents. Am J Sports Med. 2011;39(7):1444–1449. [DOI] [PubMed] [Google Scholar]
- 9. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 10. Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41(3):575–581. [DOI] [PubMed] [Google Scholar]
- 11. Maenpaa H, Lehto MU. Patellofemoral osteoarthritis after patellar dislocation. Clin Orthop Relat Res. 1997;339:156–162. [DOI] [PubMed] [Google Scholar]
- 12. Melegari TM, Parks BG, Matthews LS. Patellofemoral contact area and pressure after medial patellofemoral ligament reconstruction. Am J Sports Med. 2008;36(4):747–752. [DOI] [PubMed] [Google Scholar]
- 13. Nelitz M, Dornacher D, Dreyhaupt J, Reichel H, Lippacher S. The relation of the distal femoral physis and the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2067–2071. [DOI] [PubMed] [Google Scholar]
- 14. Nguyen CV, Farrow LD, Liu RW, Gilmore A. Safe drilling paths in the distal femoral epiphysis for pediatric medial patellofemoral ligament reconstruction. Am J Sports Med. 2017;45(5):1085–1089. [DOI] [PubMed] [Google Scholar]
- 15. Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14(4):513–515. [DOI] [PubMed] [Google Scholar]
- 16. Parikh SN, Nathan ST, Wall EJ, Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41(5):1030–1038. [DOI] [PubMed] [Google Scholar]
- 17. Redfern J, Kamath G, Burks R. Anatomical confirmation of the use of radiographic landmarks in medial patellofemoral ligament reconstruction. Am J Sports Med. 2010;38(2):293–297. [DOI] [PubMed] [Google Scholar]
- 18. Sanchis-Alfonso V, Montesinos-Berry E, Ramirez-Fuentes C, Leal-Blanquet J, Gelber PE, Monllau JC. Failed medial patellofemoral ligament reconstruction: causes and surgical strategies. World J Orthop. 2017;8(2):115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. [DOI] [PubMed] [Google Scholar]
- 20. Shea KG, Grimm NL, Belzer J, Burks RT, Pfeiffer R. The relation of the femoral physis and the medial patellofemoral ligament. Arthroscopy. 2010;26(8):1083–1087. [DOI] [PubMed] [Google Scholar]
- 21. Shea KG, Martinson WD, Cannamela PC, et al. Variation in the medial patellofemoral ligament origin in the skeletally immature knee: an anatomic study. Am J Sports Med. 2018;46(2):363–369. [DOI] [PubMed] [Google Scholar]
- 22. Shea KG, Styhl AC, Jacobs JC, et al. The relationship of the femoral physis and the medial patellofemoral ligament in children. Am J Sports Med. 2016;44(11):2833–2837. [DOI] [PubMed] [Google Scholar]


