Abstract
Background:
Post 2015, the Millennium Development Goals (MDGs) will undergo a transition to Sustainable Development Goals (SDGs). Therefore, it becomes necessary to assess the determinants influencing the present status of MDGs. This study was conducted to assess the progress, short comings related to the transition from MDGs to SDGs in a metropolitan city. It provides practical insights for extrapolating need based strategies related to the SDGs.
Methods:
Study was conducted in a metropolitan city, Mumbai. Situational analysis of the city was done using monthly and annual performance reports and key informant's interviews at city level. Qualitative analysis was done using thematic analysis.
Results:
The current infant mortality rate of Mumbai is 26.72 and under-five mortality rate is 38.7/1000 live births. The current MMR of mumbai is 88. The responses from the key informants’ spanned three major themes: Concerns and challenges; Good practices and schemes in pipeline; and Opportunities envisioned. Eight major challenging areas were identified. Opportunities are sustainable models of public-private partnership; Involvement of NGOs and AYUSH practitioners; and IT sector involvement, HMIS, e- governance, and Corporate Social Responsibility (CSR).
Conclusions:
Significant progress has been made in the field of maternal and child health (MCH), and sustained efforts are required. Maternal mortality figures may be illusive because of the effect of migration and referral cases. Socio-demographic issues of development need to be addressed through governance. Mechanism for intersectoral coordination, IT support, surveillance, and tracking of pregnant mothers needs to be developed. The linkage of MCH services with developmental programs needed.
Keywords: Key informant interviews, maternal health, millennium development goals, sustainable development goals, qualitative
Introduction
India has experienced considerable improvement in maternal and child health care since the millennium declaration 2000. However, inequities in these services are still persistent across different states, and also in different districts within the state. Maharashtra, as a state has reported progress in all the outcome indicators of health, some of its achievements even better than the national average. It has made significant reduction in the infant mortality rate (IMR) (a drop of 20 points over last decade), a steady drop in the under-five mortality rate (U-5MR), and maternal mortality ratio (MMR). However, this progress has been uneven across the rural and urban districts.
Mumbai, capital city of Maharashtra is India's most populous city, with more than 16 million people spanning multiple ethnicities, cultures, and linguistic groups. More than half of Mumbai's population currently lives in slums.[1] The large influx of migrants invariably necessitates comparison of Millennium Development Goals (MDG) achievements with indigenous population. This will facilitate optimal planning of resources for the post 2015 agenda reflected in the Sustainable Development Goals (SDGs).[2]
The gaps in the expectations and achievements identified by a realistic situational analysis of pre and post MDG era are vital at this stage. The present study measures the indicators of maternal and child health (MCH) and provides practical insights for technical, managerial, and organizational interventions for an effective transition from MDGs to SDGs.
Subjects and Methods
This study was conducted in the metropolitan city, Mumbai, Maharashtra, India in collaboration with Municipal Corporation of Greater Mumbai (MCGM). Ethical approval was obtained from Institutional Ethics Committee. A mixed methods approach was used. For situational analysis, data pertaining to MCH indicators were obtained from the public health department of MCGM for the years 2011 to 2015 and analyzed for descriptive statistics using Microsoft Excel 2016 version. In addition, key informant interviews were done with a total of nine stakeholders (program managers) concerned with MCH activities using a pre-designed interview guide. Triangulation was done at the time of analysis. Thematic analysis[3,4] was done for the interview transcripts. An integrated approach (inductive as well as deductive) was used.[3,5] In vivo codes were used to develop themes and sub-themes.
Results
Situational analysis
The data which were obtained from public health department, MCGM yielded the following results. It is observed that there is a steady decline in the child mortality indicators [Figure 1]. The current IMR of Mumbai is 26.72 and U- MR is 38.7/1000 live births, which is well below the MDG target set for India i.e. 27 and 42/1000 live births, respectively. Other child mortality indicators such as neonatal mortality rate and still birth rate have also shown declining trend.
Figure 1.
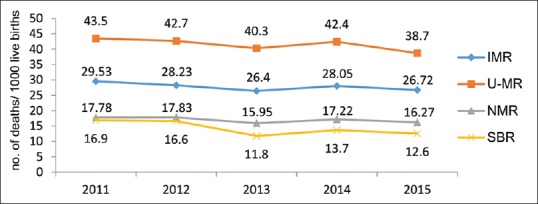
Trends in child mortality indicators in Mumbai city.
*IMR: Infant mortality rate, U- MR: Under -5 mortality ratio, NMR: Neonatal mortality rate, SBR: Still birth rate
Figure 2 shows the trend in MMR in the past 5 years. The MMR shows a slight increasing trend.
Figure 2.
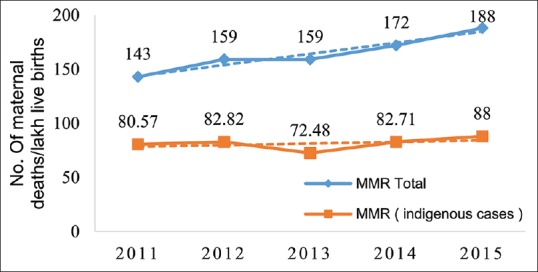
Trends in maternal mortality ratio in Mumbai city. *MMR total: Includes all cases which delivered in Mumbai i.e. referral cases also included for calculation purpose. †MMR (Indigenous cases): Does not include any referral case, only indigenous population included for calculation purpose
Comparing rates of all patients seeking treatment in Mumbai (i.e. referrals) to only indigenous cases of Mumbai, the MMR changes significantly [Table 1]. The current MMR of mumbai is 88. Major public hospitals i.e. Sir JJ group of Hospitals, BYL Nair Hospital, King Edward Memorial Hospital, Sion Hospital, and R N Cooper Municipal General Hospital consists of 16% of the total deliveries. The Peripheral Municipal Hospitals and Major hospitals together consist of 32% deliveries in the city. Figure 3 shows the hospital wise maternal deaths in the Major hospitals in 2015, and Figure 4 shows their classification according to the residence. It is observed that the majority of the maternal deaths in Sir JJ group of Hospitals, BYL Nair Hospital, and King Edward Memorial Hospital are referral cases from outside Mumbai.
Table 1.
Concerns and challenges faced to achieve maternal and child health related MDG targets
| Concerns/Challenges | Grading | Verbal responses | Inference |
|---|---|---|---|
| Infrastructure | ++ | “We have only one [NRC] at Sion now, considering the population of Mumbai at least 2-3 more are needed.” | There is a shortage of intensive care units for both mother and child; more Nutritional rehabilitation centers should come up. In addition, the existing infrastructure should be converted to more 24×7 services to handle emergencies. |
| Manpower | +++ | “…there should be separate MOH for health and non-health activities, or else they are busy with administrative work only and this compromises the health activities.” | There is a shortage of outreach workers and intensivists for maternal and child care. In addition, there is lack of qualified public health professionals in management cadre. As per population norms with creation of new health posts, new staff needs to be recruited to decrease burden on the existing staff and improve efficiency. |
| Logistics | + | “These 108 people [ambulance staff] they don’t want to transfer any patient from one hospital to another if the patient wants. sometimes it becomes a problem, only if there is a referral then they go, sometimes they are busy with one case then, we have to see how to shift them…” | The key informants were of the opinion that laboratories though well-equipped lack newer technology, blood in the blood banks are inadequate, the ambulance services mostly take only transfer calls and not regular referrals/investigations/pick up drop of patient. No alternate source of transport is available. Many of these ambulances are mere vehicles and not equipped as ambulances should be. |
| “… various schemes are in place but, still patient pick up drop facility is not available. ” | |||
| Funds | + | “ funds is not an issue… no dedicated funds for MDGs as such but it is included in other program funds itself……. “ | Funds are more or less adequate, but red tapism can be seen in procurement and expenditure |
| “… we don’t need separate funds… Paper work is tedious…” | |||
| Health services | ++ | “People have disease oriented mind-set, in slums we are able to each 90% and we provide preventive and promotive services. But, in cities, people who go to private don’t get it.” | There is a dearth in providing preventive and promotive care as more than 60% of the population use private sector, which does not provide these services. Early Antenatal registration which is a concern can be significantly reduced if this is done. Public Private Partnerships and NGO involvement needs more improvement. Tracking of antenatal women is also not up to the mark. |
| “People in Mumbai do not have time, they don’t prefer 9×4 services as it is crowded. And we don’t have enough emergency services.” | |||
| Training | + | “ at senior level we have no training ” | Training activities take place regularly, but there is lack of training at managerial level. Induction training does not always happen at the right time. |
| “ Sometimes induction training may be delayed by 2-3 months ” | |||
| Vulnerable population | +++ | “We have to reach out to the slums, the Adivasi Padas beyond national park …. do not accept immunization …. “ | Mumbai has a high density of population residing in thick slums (both identified and unidentified slums), Migrant population which have unregistered pregnancies, home deliveries, and unwillingness for immunization. |
| “Migrant population … they have no card, no details… the pregnancy is unregistered …” | |||
| Support | +++ | “Not that there is no political will… people do not demand it. Lack of awareness among masses…. ” | Political will is yet to develop for MCH services. It is limited to arrange camps and provide refreshments during the same. |
| “they are helping so much for outbreaks and all… maternal health not much is being done.” | There is no intrinsic motivation for intersectoral coordination; tendency to respond to only orders issued by higher authorities. Engineering, repair and maintenance, and solid waste management department are some important non-health department whose cooperation is necessary. | ||
| Structured plan to improve community participation is not in place. There is no direct support from international agencies. Whatever support whether financial or non-financial, also comes in project mode and not an ongoing process. | |||
| “Make health more than just responsibility of doctors.” | |||
| “ see it has [Community participation] improved, but we don’t have a plan. We have set up Mahila Arogya Samitis, our CHVs are going for house visits but …. We don’t have a structure …” “WHO, UNICEF are associated with pulse polio immunization sometimes, Bill and Melinda Gates foundation work for HIV/AIDS … But, nothing is constant, it’s all in project mode… we are not directly associated with them.” |
*Key for grading : + Minimally challenging/minimal concerns, ++ Moderately challenging/moderate concerns, +++ Very challenging/severe concern. †NRC-Nutritional Rehabilitation Centre
Figure 3.
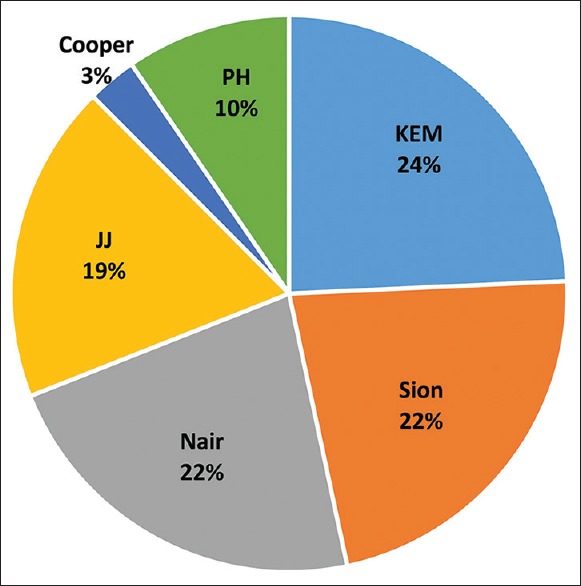
Maternal deaths in major public hospitals in Mumbai in 2015 (n = 305)
Figure 4.
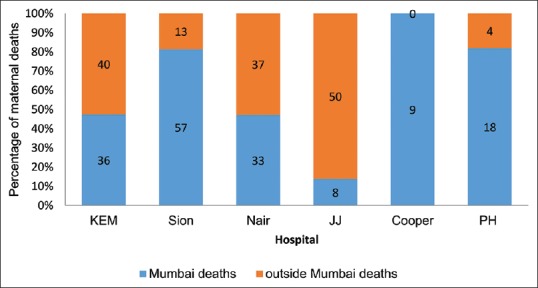
Maternal deaths based on residence in major public hospitals in Mumbai in 2015 (n = 305). *Mumbai deaths include indigenous cases of Mumbai †Outside Mumbai deaths include referral cases from nearby districts
In 2015, 97.93% of deliveries in Mumbai were institutinal deliveries. The contraception prevalence rate has gone up from 46% at the time of formulation of MDGs to 62% in 2015. The condom use rate in 2015 is 117%.
Response analysis
Nine key informants were interviewed using a pre-designed interview guide. All the interviews were conducted by the first author. All of them had an experience of more than 20 years in the field of public health, family welfare, and MCH.
Attitude of the stakeholders on performance of the city
The key informants are of the opinion that there has been good achievement in the field of MDGs. There is good achievement in the field of child health. Maternal mortality is a lagging area. Although the trend looks like it is not decreasing but constant since 2 to 3 years, in reality it is because of better reporting. A strong sense of commitment was observed among all the stakeholders toward improvement of the MCH scenario in Mumbai:
“There is good achievement in the field of child health and we have to sustain it.”
“Maternal health is our top most priority now….”
The responses from the key informants’ spanned three major themes: Concerns and challenges; Good practices and schemes in pipeline; and Opportunities envisioned.
Concerns and challenges
This theme represents hindrances to achieve the MCH related targets. This has been further divided into eight sub-themes. The sub-themes and inferences drawn are given in Table 1.
“Public health never works in ideal condition. Stop complaining… In public health service delivery is most important thing. More than anything …”
“…because it is [public health services] free no one cares, this attitude must change.”
All the respondents were unanimously of the opinion that the challenges are not easy to achieve even if identified. Hence, innovative ways to work in these conditions have to be devised.
Good practices and schemes in pipeline
This is the second theme that emerged from the key informant interviews. They have discussed a few good practices and some schemes in pipeline [Table 2]
Table 2.
Description of good practices/schemes in pipeline
| Good practices/schemes in pipeline | Description | Grading |
|---|---|---|
| Awards | Awards are being given regularly in MCGM for good performance especially in the field of contraception at all levels. Recognition is also given to the best dedicated staff in each ward | ++ |
| Slum adoption scheme (Dattak Vasti Yojana) | MCGM had initiated this community led sanitation program. Plan is to incorporate similar plan in favor of maternal and child health. | ++ |
| Public private initiatives | These initiatives are being taken up for items which are not budgeted. “Aapli Chikitsa” is one such scheme, which is a plan for outsourcing of laboratory investigations and drugs when facility is not available. | ++ |
| Infrastructure up gradation | Laboratory facilities are present at all dispensaries, maternity hospitals, and higher centers. Under NUHM, laboratory facilities are being started at health posts too. Proposal for setting up two more NRCs are in pipeline. Evening OPDs are being started in the new U-PHCs and enrollment of private ambulances at subsidized rate. | +++ |
| Soft skills training | The key informants recognize that there is a need to improve skill based training compared to knowledge based training. The training cell of MCGM is looking into this matter. Outsourcing of consultants can be done for the same. | ++ |
| Mahila Arogya Samiti | Formation is already in process. | +++ |
| Ambulance services | Ambulance services are being provided by private agencies (The Lion’s Club), political parties (Shivsena, Nationalist Congress Party), and Fire Brigade for MCH services. There is a proposal to introduce Two-Wheeler ambulance services for slum areas as these are not accessible by Four-Wheelers. These ambulances will provide first aid at site. | ++ |
*Key: + somewhat beneficial/effective, ++ Beneficial/effective, +++ Very beneficial/effective
Opportunities envisioned
The key informants’ narratives highlight certain areas that has scope in the future and will certainly help in achievement of SGDs by 2030. In order of priority these are sustainable models of public-private partnership (PPP); NGOs which should work in line with government programs and hard to reach areas like slums; Involvement of AYUSH practitioners in preventive and promotive care; and IT sector involvement, HMIS, e-governance, and CSR. Some narratives highlighting their views are given in Table 3.
Table 3.
Opportunities envisioned for achievement of SDGs
| Opportunities | Verbal responses | Grading |
|---|---|---|
| Public-private partnership | “we need sustainable models for PPP, we are exploring and other medical colleges or department can also come up with plans. It has to be attractive for private also otherwise they [private sector] will leave” | +++ |
| NGO involvement | “Our programs do not fully reach these slum people. No health worker is willing to work there. the NGOs should work in these areas not where already we are giving services….” | +++ |
| HMIS and E- Governance | “e-Governance is a far sighted thing as of now… if we have to achieve the SDGs we need to move towards it… we need more computers, internet facility … HMIS was thought to be difficult but it has come now… our staff is open to new things” | ++ |
| Information technology | “Everything these days is IT only, software apps. MCGM has many apps related to health, record keeping, analysis, registration, all systems… more transparency and less corruption because of this.” | ++ |
| CSR | CSR activities can focus on training, provision of newer technology, and working in slums. | + |
| Integration of AYUSH | “… When AYUSH is a proven pathy then why not involve them in primary care ” | ++ |
*Key: + Somewhat important for achieving SDGs, ++ Important for achieving SDGs, +++ Very important for achieving SDGs
Discussion
There has been considerable progress in the health indicators since the formulation of MDGs, which is evident from the various reports released by the United Nations, United Nations Development Program (UNDP) in particular.[2,6] In 2010, universal appeal was made by United Nations to all member countries to focus on accelerating favorable child health indicators on a priority.[7] At local governance level, especially in this metropolitan city, appropriate actions were taken in this regard. In 2013, the Municipal Corporation took a resolution to implement the National Urban Health Mission in Mumbai. The National Health Programs have been instrumental for achievement of the MDGs.
The pre-MDG status in the years 2011, 2012, 2013, and 2014 have been compared with the achievements in 2015 [Figures 1 and 2]. The Maternal and Child Health (MCH) indicators show a consistent declining trend. The MDG target indicators of Goal 4 have been achieved. The total MMR is showing an increasing trend. This can be attributed especially to the focus on 100% antenatal care coverage and institutional delivery. This has resulted in enhanced reporting of maternal deaths in the city. Further, the rates include maternal deaths among those who are referral cases from outside Mumbai. If the rates are compared with indigenous cases only then, the rates are below the national average stabilizing around 88. This would then also mean that the MDG 5 target of MMR has been achieved. If all referral cases are included, the situation seems alarming as it is above the national average of 167 too. Overall, in the area of maternal mortality, the situation in India is not very promising and requires more concerted efforts.[8,9,10,11,12,13]
During this study, it was found that in Mumbai around 32% of the deliveries occur in public sector and rest 67% occur in private sector. In 2015, 97.93% of deliveries in Mumbai were institutinal deliveries. Approximately, 0.82% deliveries occured at home. Although this may seem a good percentage, in absolute numbers it means around 3,476 deliveries in 2015 did not occur in a hospital. In a study by Griffiths and Stephenson about user perspective of care services Mumbai and Pune, it was found that women thought better services were provided by private sector, and poor quality of government services were motivating factors for home deliveries.[14] Similar finding is also found in another study by Alcock G et al.[7] Effective task shifting and engagement of AYUSH practitioners has shown good results in rural parts of Maharashtra.[13] Similar model can be implemented in difficult to reach slum areas to tackle the home deliveries effectively.
The attitude among the top-level managers of the MCH program indicated the highest priority for maternal health within the department. They were enthusiastic about mainstreaming the MCH action plan in the various cadres of health personnel related to the Family Welfare (FW) MCH department. In a study by Marta Lomazzi et al., they also found that highest importance was placed on MDGs dealing with women, poverty sear hunger reduction, and disease prevention and management (percentage agreement: 34%, 20%, and 19%, respectively). They recognized that improvements in women's living conditions, better maternal (and child) health, and women's empowerment represented the most cost-effective achievement for health systems.[15]
It is also necessary to focus on improving the primary health care from prenatal to postnatal period.[10,12] Since the advent of National Rural health Mission, the situation of primary health care in rural parts of India has seen lot of improvement. It is now necessary to focus the attention on urban areas especially the urban slums and devise primary health care strategies which foster community engagement. Robert Black et al. in a review have compiled various effective interventions for mother and newborn, which can be provided easily by the community health workers. They are birth and newborn care planning, nutrition supplementation, HIV testing, effective referral management, and promotion of breastfeeding among many others.[12]
On provoking the responses of key informants to their contribution in MDGs, it was communicated that new need based strategies and schemes were devised for promotion of MCH activities. These included awards and recognition for good work, PPI initiatives such as “Aapli Chikitsa” and tie-up of private blood banks with maternity homes for blood and blood products and formation of Mahila Arogya Samiti, which is already in process. The importance of Mahila Arogya Samiti and community health workers in general has been also proposed by Rajesh Rai in his study for maintaining continuum of care in maternal health services. He also proposes the importance of computerization in record maintenance.[16] There is a proposal to introduce “Two-Wheeler” ambulance services for slum areas as these are not accessible by “Four-Wheelers.” These ambulances will provide first aid at site. There is documented evidence that accessibility and round the clock services improve the health seeking behavior and promote more institutional deliveries too.[8,12,17,18,19] The training cell of Municipal Corporation of Greater Mumbai (MCGM) is looking into outsourcing of consultants to improve skill based training. The need for context specific strategies and investments across multiple sector has been highlighted in the study on success factors for reducing maternal and child mortality in the fast track countries by Kuruvilla et al.[20]
In addition to the above measures, in our study area, regular supervision, review meetings, instructional circulars were implemented diligently. These were verified from the available records. However, there is lack of any standard protocol by which they can effectively measure the progress. This pertinent issue needs to be addressed soon.[11] The managers express their concern over the need for infrastructure support, especially for Nutritional Rehabilitation Centres and ICUs for neonatal care. Under National Urban Health Mission (NUHM), laboratory facilities are being started at Health posts too. Proposal for setting up two more Nutrition Rehabilitation Centre (NRC) s are in pipeline. Evening OPDs are being started in the new urban- primary health centres (U –PHCs). Under NUHM, on ad hoc basis, although there is provision for man power, their utility is inadequate as the recruitment is volatile and depletion rate is higher. Further need for repeated training program is equally exhaustive. Hence, their should be permanent recruitment in sectoral organization, especially in MCH. From the observation of key informants, the priority areas which needs to be addressed are manpower shortages in NICUs and Sick Newborn Care Unit (SNCUs). Thrust areas for PPP such as laboratory services, bloodbanks, and network need to be established. A review article by Chatterjee and Paily lists infrastructural problems and organisational failures among many others as non-medical problems, which contribute to maternal and child deaths. They suggest holistic approaches to deal with the barriers such as upgradation of infrastructure, skilled manpower, promotion of institutional deliveries, and recent strategies such as PPPs. The challenges of inadequate ambulance service is also highlighted by them.[21]
Conclusion
Thus, we can conclude by saying significant progress has been made in the field of child health, and sustained efforts are required. Maternal mortality figures may be illusive because of the effect of migration and referral cases. The migrant population adds additional burden on the existing health care system. A spirit of enthusiasm and commitment toward health is observed among stake holders. Socio-demographic issues of development need to be addressed through governance. Mechanism for intersectoral coordination, PPP, IT support for logistics and management, surveillance, and tracking of pregnant mothers needs to be developed. Innovative programs for involvement of private sector in MCH services required, which can vary from place to place depending on local needs. The linkage of MCH services with developmental programs like slum adoption scheme needs to be done. The existing referral system needs to be strengthened. Dedicated vehicles/ambulances exclusively for MCH services in all wards needs to be ensured. Soft skills training should be provided among all cadre of health staff in communication, rapport building, and team work. Awards and incentives for well performing health workers can be arranged.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Skordis-Worrall J, Pace N, Bapat U, Das S, More NS, Joshi W, et al. Maternal and neonatal health expenditure in mumbai slums (India): A cross sectional study. BMC Public Health. 2011;11:150. doi: 10.1186/1471-2458-11-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.India and the MDGs Towards a sustainable future for all. 2015. [Last accessed on 2018 Nov 16]. Available from : https://www.unescap.org/sites/default/files/India_and_the_MDGs_0.pdf .
- 3.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. doi: 10.1186/1471-2288-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 5.Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Serv Res. 2007;42:1758–72. doi: 10.1111/j.1475-6773.2006.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh S, Maitra S, Bhaskar S, Pal RP, Hansraj . Millennium Development Goals India Country Report 2015. New Delhi: 2015. [Google Scholar]
- 7.Alcock G, Das S, More NS, Hate K, More S, Pantvaidya S, et al. Examining inequalities in uptake of maternal health care and choice of provider in underserved urban areas of Mumbai, India: A mixed methods study. BMC Pregnancy Childbirth. 2015;15:231. doi: 10.1186/s12884-015-0661-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar S, Dansereau E. Supply-side barriers to maternity-care in India: A facility-based analysis. PLoS One. 2014;9:e103927. doi: 10.1371/journal.pone.0103927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar PR, Ranjan D, Pejaver K. Millennium development goals: Regional perspectives-India. Arch Dis Child. 2015;100:s59–60. doi: 10.1136/archdischild-2013-305537. [DOI] [PubMed] [Google Scholar]
- 10.Rai RK, Tulchinsky TH. Addressing the sluggish progress in reducing maternal mortality in India. Asia Pacific J Public Heal. 2012;27 doi: 10.1177/1010539512436883. doi: 10.1177/1010539512436883. [DOI] [PubMed] [Google Scholar]
- 11.Srivastava A. Standardizing evaluation process: Necessary for achieving SDGs -A case study of India. Eval Program Plann. 2018;69:118–24. doi: 10.1016/j.evalprogplan.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Black RE, Taylor CE, Arole S, Bang A, Bhutta ZA, Mushtaque A, et al. Comprehensive review of the evidence regarding the effectiveness of community–based primary health care in improving maternal, neonatal and child health: 8.summary and recommendations of the Expert Panel. J Glob Health. 2017;7:010908. doi: 10.7189/jogh.07.010908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chandhiok N, Joglekar N, Shrotri A, Choudhury P, Chaudhury N, Singh S. Task-shifting challenges for provision of skilled birth attendance: A qualitative exploration. Int Health. 2015;7:195–203. doi: 10.1093/inthealth/ihu048. [DOI] [PubMed] [Google Scholar]
- 14.Griffiths P, Stephenson R. Understanding users’ perspectives of barriers to maternal health care use in Maharashtra, India. J Biosoc Sci. 2001;33:339–59. doi: 10.1017/s002193200100339x. [DOI] [PubMed] [Google Scholar]
- 15.Lomazzi M, Laaser U, Theisling M, Tapia L, Borisch B. Millennium development goals: How public health professionals perceive the achievement of MDGs. Glob Health Action. 2014;7:24352. doi: 10.3402/gha.v7.24352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rai RK. Tracking women and children in a continuum of reproductive, maternal, newborn, and child healthcare (RMNCH) in India. J Epidemiol Glob Health. 2014;4:239–43. doi: 10.1016/j.jegh.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sahoo J, Vir Singh S, Kishore Gupta V, Garg S, Kishore J. Do socio-demographic factors still predict the choice of place of delivery: A cross-sectional study in rural North India. J Epidemiol Glob Health. 2015;5:s27–34. doi: 10.1016/j.jegh.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mishra N, Panda M, Pyne S, Srinivas N, Pati S, Pati S. Barriers and enablers to adoption of intrauterine device as a contraceptive method: A multi-stakeholder perspective. J Fam Med Prim Care. 2017;6:616–21. doi: 10.4103/2249-4863.222028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fadel SA, Ram U, Morris SK, Begum R, Shet A, Jotkar R, et al. Facility delivery, postnatal care and neonatal deaths in India: Nationally-representative case-control studies. PLoS One. 2015;10:e0140448. doi: 10.1371/journal.pone.0140448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuruvilla S, Schweitzer J, Bishai D, Chowdhury S, Caramani D, Frost L, et al. Success factors for reducing maternal and child mortality. Bull World Heal Organ World Heal Organ. 2014;92:533–44. doi: 10.2471/BLT.14.138131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chatterjee A, Paily VP. Achieving millennium development goals 4 and 5 in India. BJOG An Int J Obstet Gynaecol. 2011;118:47–59. doi: 10.1111/j.1471-0528.2011.03112.x. [DOI] [PubMed] [Google Scholar]


