Abstract
Context:
The burden of non-communicable diseases will sooner overwhelm the health system of the country and could curtail future economic development. Hypertension causes highest cardiovascular morbidities. To attain target Blood Pressure (BP), different strategies are required, which are area specific. The validity of rule of halves of hypertension in various settings needs to be studied for developing strategies for that particular geographical area. To utilize the resources in more efficient way, strategies need to differ in rural-urban and underserved- well-served areas.
Aims:
The present study aims at exploring whether the rule of halves holds good in the city of Mumbai as the findings of such research may have implications on strategies to control hypertension in communities. Hence, the objectives of this study are to ascertain the proportion of persons with hypertension with respect to the status of diagnosis, treatment, adequate treatment, and validate it with existing rule of halves.
Setting and Design:
Study was conducted in the urban field practice area of a teaching hospital and medical college of Mumbai that comprises 42 chawl (housing structures); study design- cross-sectional observational study.
Materials and Methods:
This observational cross-sectional study was conducted over a period of 18 months in the field practice area of a teaching hospital and medical college of Mumbai with a total population of 43,069. Sample size was 667. After ethical clearance, participants were interviewed using pretested semi-structured interview schedule that included socio-demographic factors, risk factor evaluation, clinical examination, and anthropometry. Subjects with diagnosed hypertension were questioned thoroughly about hypertension adherence.
Statistical Analysis:
Descriptive statistics was applied on quantitative data.
Results:
A total of 667 people from five chawls of age more than 35 years were included into the study. The mean age of study subjects was 50.84 ± 11.47 years. Out of total 667 respondents, 20.3% respondents were normotensive, 50.3% respondents were pre-hypertensive, 25.3% respondents were in stage 1 hypertension, and 4% respondents were in stage 2 hypertension. In contrary to the classical rule of halves, the present study shows only 31% of the diagnosed hypertensives are adequately treated.
Conclusions:
The strategies in the national programs are from the traditional understanding of rule of halves and emphasize increasing awareness and treatment. Family physician should actively involve in regular screening, treatment, and adherence of hypertension treatment. As a part of primary care, community participation is required for effectively achieving the target BP goal of the population.
Keywords: Hypertension, policy making, prevalence, rule of halves
Introduction
Non-communicable diseases (NCDs) are not only a concern for health but also a threat for productivity and economic growth of the country. The burden of NCD will sooner overwhelm the health system of the country and could curtail future economic development. India is expected to lose $4.58 trillion before 2030 because of NCDs.[1] United Nations Population Division (2011) shows that India's old population will be more than double by 2050 as compared to 2010. The survey conducted by India Human Development Survey 2015 found out that the prevalence of hypertension among elderly is doubled during the time period 2005–12 in India. The number of people with hypertension is expected to increase from 118.2 million in 2000 to 213·5 million in 2025, with nearly equal number of men and women.[2]
Cardiovascular complications are the most dreadful complication of NCD’s. Hypertension is the most common cardiovascular disorder that may be asymptomatic many a times. In developed countries, decrease in the population mean of blood pressure (BP) is attributable to increased awareness, diagnosis, control, and adherence to treatment. Despite the stable prevalence in western countries, control rates have improved more than double. Conversely, Asian studies have reported increasing prevalence and lower levels of treatment and control. Because of its silent and asymptomatic nature, it was supposed to follow “rule of halves.” This terminology was coined in 1970 in America, reported in Scotland, and from parts of India.[3]
The rule of halves states that “half of hypertensive patients are not known to health services (i.e., remain undiagnosed), half of those with known hypertension do not receive any treatment, and half of those who are treated, do not achieve adequate control.” Studies have confirmed that the rule of halves holds good in Indian setting.[3,4] However, there is a reason to believe that the rule of halves might have changed given the fact that the awareness on the issue seems to be improved in urban India, especially in the metropolis.
The present study aims at exploring whether the rule of halves holds good in the city of Mumbai as the findings of such research may have implications on strategies to control hypertension in communities. It will guide the policy makers and program managers to concentrate their efforts on effectively controlling hypertension with optimal resources.
Data at sub-national level are needed for scrutinizing the situation regarding the existence of rule of halves. There is a definite knowledge gap of level of awareness, control, and treatment that can be resolved by doing a systematic analysis of regional epidemiological studies. Hence, the objectives of this study are to estimate the prevalence of hypertension among persons above 35 years of age; to ascertain the proportion of persons with hypertension with respect to the status of diagnosis, treatment, and adequate treatment.
Materials and Methods
Study design and settings
This observational cross-sectional study was conducted over a period of 18 months from December 2011 to May 2013 in the field practice area of a teaching hospital and medical college of Mumbai that comprises of 42 Bombay Development Directorate (BDD) chawls. A chawl is a typical structure, with four floors containing 80 houses each usually inhabited by lower middle class population in the city. Sample size was calculated from expected prevalence 48% in >35 age group in similar setting in Mumbai[5] with alpha error 0.01, acceptable margin of error taken as 0.05 and was found to be 663. To achieve this sample size, five out of these 42 chawls were randomly selected, and all the persons above 35 years of age were enrolled. The number of participants turned out to be 667.
Participants
Subjects with severe chronic comorbidities were excluded from the study. Informed consent documents were obtained prior to which each subject was described about the study and its purpose. Participants were interviewed using pretested semi-structured interview schedule which was about socio-demographic factors, risk factor evaluation, clinical examination, and anthropometry.
Measures
BP was measured in sitting position in all respondents on left upper arm using mercury sphygmomanometer with arm positioned at heart level. Repeated BP measurement was taken after 30 min for those with elevated BP. Out of all the respondents, 39% were male and rest female.
Ethics approval
Ethical clearance was obtained from Institutional Ethics Committee of SETH GSMC and KEM hospital, which are guided by the ICH GCP guidelines, Ethical principles set forth in Declaration of Helsinki, and the ethical guidelines on biomedical research on human participants laid down by Indian Council of Medical Research.
Data analysis
Data were entered in Microsoft excel 2016 spread sheet to organize and tabulate data for statistical analysis.
Outcomes
According to Joint National Committee (JNC) 7 criteria, prevalence of hypertension was calculated by counting respondents whose BP was greater than or equal to 140/90 mm Hg[6] and respondents who were already on anti-hypertensive medication. All participants were inquired whether they had been diagnosed with hypertension (awareness) or were receiving anti-hypertensive medications if any. Out of those hypertensives, who had normal BP below 140/90 mm Hg as per JNC 7 criteria were considered as controlled. Height was measured using a stadiometer with bare foot nearest to 0.1 cm. Weight was measured using digital weighing scale. Body mass index (BMI) is defined as the individual's body weight in kilograms divided by the square of his or her height in meters. According to WHO classification,[7] BMI less than 18.50 is underweight, 18.50 to 24.99 is normal, 25.00 to 29.99 is overweight, and more than 30.00 is obese.
Data entry was done using excel software. Analysis was performed using SPSS software. Prevalence rates were reported as percentage. Multivariate logistic regression analysis was performed to determine the predictors of hypertension, awareness, and control of hypertension.
Results
A total of 667 persons from five chawls of age more than 35 years were included into the study. The mean age of study subjects was 50.84 years, and standard deviation was 11.47 years. Table 1 shows percentage distribution of study subjects according to BP measurements.
Table 1.
Percentage distribution of BP among the study subjects according to the BP recording at the time of study
| Male (%) | Female (%) | n (%) | |
|---|---|---|---|
| Normal | 46 (34) | 90 (66) | 136 (20.3) |
| Pre hypertension | 141 (42) | 195 (58) | 336 (50.3) |
| HTN Stage 1 | 66 (39) | 103 (61) | 169 (25.4) |
| HTN Stage 2 | 10 (38) | 16 (62) | 26 (4) |
| Grand total | 163 (24) | 404 (76) | 667 (100) |
Out of the all respondents, 250 (37.48%) were found to be hypertensives, 282 (42.2%) prehypertensives, and 136 (20.3%) subjects were normotensive as per JNC 7. Thus, total 417 were labeled as normotensives, and the prevalence of hypertension was 37.48%. There was no significant difference between prevalence among males (37.26%) and females (37.62%). The prevalence was 27% in 35–44 years of age group and 31% in 45–54 years of age group. It increased steeply after the age of 55 years giving a prevalence of 55% in 55–64 years’ age group and 54% in 65–74 years’ age group. Above 75 years of age, the prevalence was 62%.
Out of the 250 hypertensives, 64 (25.6%) were newly diagnosed during the survey, and 186 (74.4%) were already diagnosed cases. In total, 177 (95.2%) of those diagnosed cases were already on treatment. Out of 55 (31.1%), those who were on treatment had their BP adequately controlled, and rest 122 (68.9%) were having poorly controlled BP.
At the time of survey, 136 (20.3%) of the population had BP in the normal range (Systolic <120, Diastolic <80), 336 (50.3%) of the population were pre-hypertensive (Systolic/Diastolic = 120–139/80–89), 169 (25.4%) respondents had hypertension stage 1(Systolic/Diastolic = 140–159/90–99), and 26 (4%) respondent had BP in the range of stage 2 (Systolic≥=160, Diastolic≥=100) hypertension.
Hence, in summary, 37.48% of total population is hypertensive, 74.4% of those were diagnosed appropriately, and 95.2% of the diagnosed were taking treatment. However, the most striking result to emerge from the data is that only 31.1% of those taking treatment were adequately controlled.
Discussion
In statistical etymology, rule of halves is a restatement of “median concept.” It was established that hypertension follows rule of halves according to the researches in various parts of the world. However, evidences from developed countries prove that this concept is changing as the improvement in diagnosis and treatment, decreases the percentage in rule of halves.[8] Rule of halve signifies weaker health system and awareness about the control. Current prevalence of hypertension as per the study is 37.48% that is similar to other studies in similar urban settings across the globe i.e., 30 to 37%.[9] In contrary to the classical rule of halves, the present study shows that nearly 95.2% of diagnosed cases are seeking treatment. Figure 1 shows the elements of rule of halves scaled to the study findings, whereas Figure 2 shows the originally depicted rule of halves. The matter of apprehension is despite accessing health care their BP is not adequately controlled i.e., 68.9% of those are inadequately treated.
Figure 1.
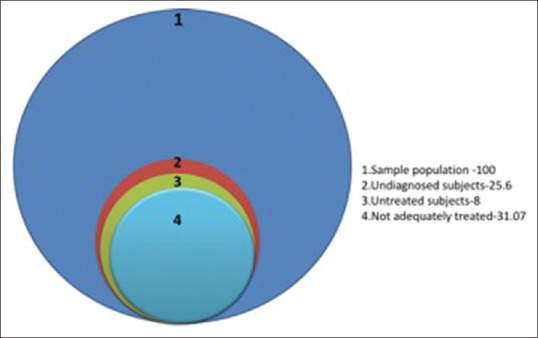
Showing the elements of rule of halves as per the study population
Figure 2.

Showing the originally depicted rule of halves
The strategies in the national programs are from the traditional understanding of rule of halves and emphasize increasing awareness and treatment. However, in metropolis, the awareness seems to be improved and the proportion of people seeking treatment has substantially increased. Hence, specific strategies need to be emphasized in various regions depending on the level of awareness of percentage getting diagnosed, percentage getting treated, and those with adequate control. The existing strategy works best in rural and peri-urban areas where rule of halves still holds good. In the scenario similar to our research setting, the capacity building of service providers and behavior change strategies to improve compliance to treatment need more emphasize while enhancing the level of awareness.
In India, the characteristic of population varies across state borders. The awareness of being hypertensive varies from 21% in Himachal[10] to nearly 50% in Kerala.[11] A study conducted in Aligarh in a rural adopted village asserts the existence of rule of halves in rural northern India.[3] Chennai urban population study also affirms the existence of rule of halves there.[4] Despite the launch of National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS), the awareness level of people has not improved much. This program has proposed the control measures, diagnosis, and treatment of hypertension according to WHO standards. The goal is to reduce BP to 130/85 mm of Hg and more ideally to 120/80 mm of Hg. The known risk factors are physical activity, obesity, daily sodium intake, and alcohol consumption.[12]
Management comprises of assessing the medical history, physical examination, laboratory investigations, and drug therapy. Behavioral changes through counseling of patients for regular physical activity, salt restricted diet, and managing stress should be done. There are certain contra indications for using each drug, and certain drugs are more preferred for co-morbid conditions. Certain western studies in urban scenario show excellent prescription compliance,[13] but similar studies are lacking in India. To maintain the competency of prescribing appropriate drug to the patients, family physician or general practitioner (GP) being the first contact of care should be regularly updated about recent changes in the management guidelines. Luders et al.[14] in their study found out that regular physician training sessions and feedback programs help to reduce BP goals in primary health care. Poor counseling of patients regarding adherence, complications, and life style activities can be a major concern in adherence.[12] Here, the role of family physician is very vital as they are in regular contact with the patient and have attained their trust over years. The scope of counseling is somewhat limited in private hospitals because of patient load, whereas family physicians have an extra edge for counseling as the regular doctor-patient barrier is less between them.
An interventional study conducted in Kerala has found out the importance of community participation in BP control. Volunteers selected from the community were trained by local Primary Health Centre (PHC) for regularly monitoring BP and recording anthropometry of the subjects. Besides proper counseling sessions, they used to project short films related to cardiovascular health and distributed booklets for describing the importance of adherence and preventing complications in hypertensives in local language. This intervention has shown considerable decrease in mean BP among study population over a period of time.[15] Similar suggestions were put forward by a study conducted in USA among physicians that task shifting from physicians to well-trained non-physician health workers can surmount the burden of patient number on physicians and GP’s. Patient centered model or patient participation in decision making regarding treatment has also found to be effective in primary care for decreasing mean BP.[14] Pharmacist entered data for treatment compliance has also shown to be effective in BP control.[16] More attention of policy makers is needed in making PHC functional and use of accurate BP machine.
From the results, following recommendations are put forward by our study. From 30 years of age, annual hypertension screening should be done by family physician. Those found to be hypertensive should be registered and properly counseled about complications and importance of adherence. Family screening and other comorbidities will be sought. In addition, short regular surveys to be conducted on degree of prescription compliance in family clinics. As a part of improved primary care, community participation or task shifting through non physicians are required for effective BP control.
A population based approach is essential for long-term prevention of the disease condition. In addition, there is a national wide scope of the study for knowing the awareness level of patients and level of control in different parts of the country and thereby helping in deriving essential strategies to solve the problem. In India, data on awareness and treatment are not available till now, on national basis except a few studies at different geographical zones of the country.[17]
Limitations
The results can be generalized only to a similar population. Adherence to treatment was weighed from previous 1 week recall of medication intake. BP were recorded only twice that might have altered the actual prevalence of BP. Better diagnosis and treatment figures may be because of the improved medical facility in the study area Although white coat hypertension can contribute to fluctuation in BP recording, we tried to create good rapport with the patient to reduce it.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bloom DE, Cafiero-Fonseca ET, Candeias V, Adashi E, Bloom L, Gurfein L, et al. Economics of Non-Communicable Diseases in India: The Costs and Returns on Investment of Interventions to Promote Healthy Living and Prevent, Treat, and Manage NCDs. World Economic Forum, Harvard School of Public Health. 2014 [Google Scholar]
- 2.KearneyPM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension-analysis of worldwide data. Lancet. 2005;365:217–23. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 3.Faizi N, Ahmad A, Khalique N, Shah M, Khan M, Maroof M. Existence of rule of halves in hypertension: An exploratory analysis in an Indian village. Mater Socio Medica. 2016;28:95–8. doi: 10.5455/msm.2016.28.95-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shanthirani CS, Pradeepa R, Deepa R, Premalatha G, Saroja R, Mohan V. Prevalence and risk factors of hypertension in a selected South Indian population-the Chennai urban population study. J Assoc Physicians India. 2003;51:20–7. [PubMed] [Google Scholar]
- 5.Gupta R, Pandey RM, Misra A, Agrawal A, Misra P, Dey S, et al. High prevalence and low awareness, treatment and control of hypertension in Asian Indian women. J Hum Hypertens. 2012;26:585–93. doi: 10.1038/jhh.2011.79. [DOI] [PubMed] [Google Scholar]
- 6.National Institutes of National Heart, Lung and BIP, Education NHBP. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Vol. 7. NIH Public. n.d; 2016. [PubMed] [Google Scholar]
- 7.World Health Organization. Obesity:preventing and managing the global epidemic. World Heal Organ - Tech Rep Ser. 2000:1–268. doi:10.1016/S0140-6736(03)15268-3. [PubMed] [Google Scholar]
- 8.Hooker RC, Cowap N, Newson R, Freeman GK. Better by half: hypertension in the elderly and the ‘rule of halves’: A primary care audit of the clinical computer record as a springboard to improving care. Fam Pract. 1999;16:123–8. doi: 10.1093/fampra/16.2.123. [DOI] [PubMed] [Google Scholar]
- 9.Bushara SO, Noor SK, Ibraheem AAH, Elmadhoun WM, Ahmed MH. Prevalence of and risk factors for hypertension among urban communities of North Sudan: Detecting a silent killer. J Fam Med Prim Care. 2016;5:605–10. doi: 10.4103/2249-4863.197317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhardwaj R, Kandori A, Marwah R, Vaidya P, Singh B, Dhiman P, et al. Prevalence, awareness and control of hypertension in rural communities of Himachal Pradesh. J Assoc Physicians India. 2010;58:423–4. 429. [PubMed] [Google Scholar]
- 11.Zachariah MG, Thankappan KR, Alex SC, Sarma PS, Vasan RS. Prevalence, correlates, awareness, treatment, and control of hypertension in a middle-aged urban population in Kerala. Indian Heart J. 2003;55:245–51. [PubMed] [Google Scholar]
- 12.Fang Y, Wang HHX, Liang M, Yeung MS, Leung C, Chan CH, et al. The adoption of hypertension reference framework: An investigation among primary care physicians of Hong Kong. PLoS One. 2018;13:e0205529. doi: 10.1371/journal.pone.0205529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Novello MF, Luiza M, Rosa G, Ferreira RT, Nunes IG, José A, et al. Compliance with the prescription of antihypertensive medications and blood pressure control in primary care. Arq Bras Cardiol. 2017;108:135–42. doi: 10.5935/abc.20170009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luders S, Schrader J, Schmieder RE, Smolka W, Wegscheider K, Bestehorn K. Improvement of hypertension management by structured physician education and feedback system: Cluster randomized trial. Eur J Cardiovasc Prev Rehabil. 2010;17:271–9. doi: 10.1097/HJR.0b013e328330be62. [DOI] [PubMed] [Google Scholar]
- 15.Thankappan KR, Sivasankaran S, Mini GK, Daivadanam M. Impact of a community based intervention program on awareness, treatment and control of hypertension in a rural Panchayat, Kerala, India. Indian Heart J. 2013;65:504–9. doi: 10.1016/j.ihj.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castelli G, Bacci JL, Dombrowski SK, Osborne M, Difilippo A, Klatt PM, et al. Pharmacist-delivered comprehensive medication management within family medicine practices an evaluation of the SCRIPT project. Fam Med. 2018;50:605–12. doi: 10.22454/FamMed.2018.391124. [DOI] [PubMed] [Google Scholar]
- 17.Mohan S, Campbell N, Chockalingam A. Time to effectively address hypertension in India. Indian J Med Res. 2013;137:627–31. [PMC free article] [PubMed] [Google Scholar]


