Abstract
Background:
Migraine is a common disease with neurovascular nature, which is commonly prevalent in the general population. Due to the significant prevalence of migraine and its long-term complications, it is necessary to pay attention to its exacerbating factors. Therefore, the aim of this study was to evaluate the frequency distribution of dyslipidemia in patients with migraine compared with control group.
Materials and Methods:
This is a case–control study, in which 50 patients with migraine (with aura and without aura) were confirmed by the criteria of International Headache Society. Migraineurs and control group (n = 50) were selected from among patients who referred to the Neurology Clinic of Imam Hossein Hospital. The levels of total cholesterol, triglyceride, low-density lipoprotein (LDL), and high-density lipoprotein (HDL) cholesterol were measured in both the groups. SPSS software (version 21) was used to analyze the data.
Results:
The findings showed that among migraineurs, 21 patients (42%) revealed high levels of cholesterol and 22 revealed high levels of LDL (44%); whereas among subjects without migraine, 12 subjects (24%) exhibited high levels of cholesterol and 12 (24%) high levels of LDL, where a significant correlation between the two groups was achieved.
Conclusion:
The present results showed that migraine is associated with higher level of cholesterol and LDL when compared with the control group, where a significant relationship was found.
Keywords: Cholesterol, HDL, headache, LDL, migraine, triglycerides
Introduction
Headache is recognized as the third most common cause of disability worldwide, causing severe disability in a person with headache (especially in migraine headaches) and causing many social and economic losses. The overall prevalence of migraine in the Western countries is between 5% and 9% in men and 12% and 25% in women.[1,2,3] Migraine is a common disease characterized by neurovascular disease, which has a significant prevalence in the general population, and this highlights the disease from other causes of headache. It usually begins in the first three decades of life and is most prevalent in puberty, although migraine attacks may occur at any age. Many patients with migraine are over 60 years of age.[4,5] This necessitates the double attention to this disease. Regarding the significant prevalence of migraine and its long-term complications, it is necessary to pay attention to its exacerbating factors. One of the factors is the role of dyslipidemia in the development and intensification of migraine attacks. A number of studies have shown that high levels of cholesterol may occur even in more than 50% of patients with migraine.[6,7,8] The fundamental problem in the proper diagnosis of dyslipidemia is related to its intrinsic and silent nature, which can lead to major and destructive complications such as stroke, heart attacks, and even death.[9,10] Some studies have suggested that the frequency and severity of migraine attacks may be related to the level of blood lipids. Based on these studies, higher levels of serum lipids are associated with the frequency and severity of migraine attacks.[11,12,13] Other studies in this area have pointed to an increased risk of cardiovascular diseases such as stroke, atherosclerosis, and even coronary heart disease in patients with migraine; one of the possible risk factors for this can be the presence of dyslipidemia in patients with migraine.[14,15,16] Due to the high prevalence of migraine in Iran, studies should be performed to turn attention to this issue, which has been neglected so far.
Regarding the high prevalence of migraine, the significant disability caused by this disease, and its many social and economic disadvantages, special attention should be paid to exacerbating factors such as dyslipidemia and long-term complications of the disease. Considering the known role of dyslipidemia as a cardiovascular risk factor and its possible role in the frequency and severity of migraine attacks, it is necessary to pay more attention to early detection and effective treatment of this disorder. Therefore, this study was aimed to investigate serum lipid levels including total triglycerides, total cholesterol, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) in two groups of migraine and control.
Materials and Methods
Patients
In this case–control study, 50 patients with migraine (with aura and without aura) were randomly assigned to the study, and their disease was confirmed based on the criteria of International Headache Society.[17,18] Patients with migraine and control group were selected from among the patients referring to the Neurology Clinic of Imam Hossein Hospital with nonheadache causes.
Inclusion criteria included patients with migraine (with aura and without aura) whose disease was confirmed on the basis of the International Association of Headache.
Exclusion criteria included (1) patients with diabetes, (2) cardiovascular disease, and (3) patients treated with cholesterol- and triglycerides-lowering drugs. Hospital selection was performed to facilitate comparison of the control group to patients with migraine. Cholesterol levels <200 mg/dL, triglyceride levels <200 mg/dL, HDL >50 mg/dL, and LDL <150 mg/dL were considered to be dyslipidemia as previously described.[8]
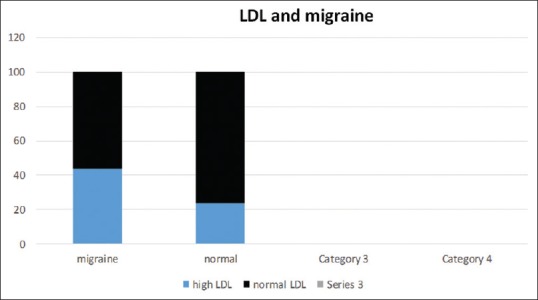
Sample size
The sample size was determined based on the ratio of hyperlipidemia in the case and control groups using the following formula. In addition, the proportion of hyperlipidemia was calculated according to Venkatesan et al.[19]
where α = type 1 error = 5%; 1- β = exponent = 80%; P1 = ratio of hyperlipidemia in the control group = 17%; P2 = ratio of hyperlipidemia in case group = 44.5%.
The minimum sample size in each group was 45. Sampling was done by convenience sampling in each case and control group.
Ethical considerations
Participants were entered into the study after giving full explanations and informed consent in a special form. This study did not impose any additional cost on the patient's treatment process, and the cost of these studies was borne by the researchers of this study. Regarding numerous studies and studies carried out in this field, this study does not impose unwanted side effects on patients.
Data analysis
SPSS v. 21 software was applied to analyze the data. For data analysis, independent t-test, one-way analysis of variance, Chi-square test, and Pearson's correlation coefficient were used. Furthermore, logistic regression was used to control confused variables. To describe the data, the mean (standard deviation) or median (interquartile range), number (percentage), and odds ratios were also used. All tests were performed at a significant level of 5%.
Results
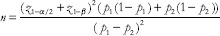
The prevalence of dyslipidemia was compared in two groups of migraine and migraine-free patients. High levels of triglyceride were seen in 9 subjects (18%) in the migraine group, whereas they were observed in 8 subjects (16%) in the migraine-free group (16%). Chi-square did not show a significant statistical difference between the two groups [P > 0.05; Figure 1].
Figure 1.
Relative frequency of hypertriglyceridemia in both groups of migraineurs and non-migraineurs
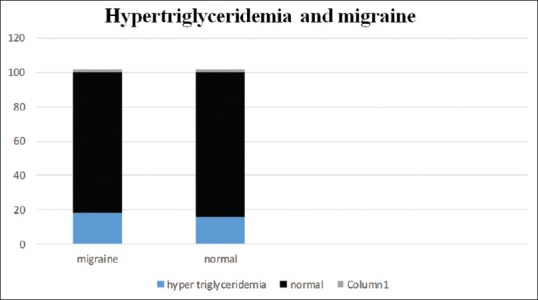
Among patients with migraine, high cholesterol was diagnosed in 21 subjects (42%), whereas 12 (24%) patients exhibited high levels of cholesterol in subjects without migraine, where a statistically significant difference was found between the two groups [P = 0.044; Figure 2].
Figure 2.
Relative frequency of hypercholesterolemia in both groups of migraineurs and non-migraineurs
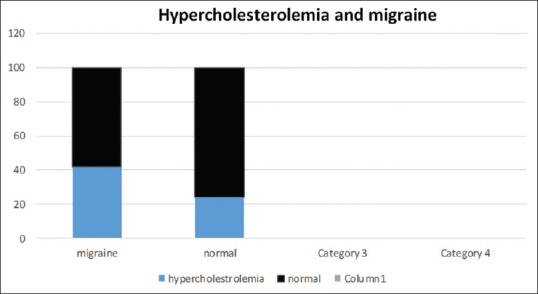
High levels of LDL were also found in 22 patients (44%) among the patients in migraine group, whereas high levels of LDL were measurable in 12 subjects (24%) in individuals without migraine. Chi-square test revealed a significant statistical difference between the two groups (P = 0.028). In the migraine group, abnormal HDL levels were detected in 10 patients (20%). Among the control group, 9 subjects (18%) exhibited abnormal HDL levels, which did not show significant statistical significance [P = 0.5; Figures 3 and 4].
Figure 3.
Relative frequency of dyslipidemia (LDL abnormalities) in both groups of migraineurs and non-migraineurs
Figure 4.
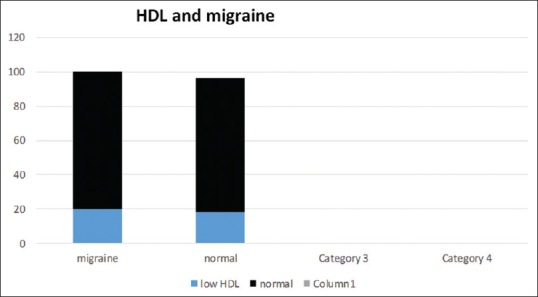
Relative frequency of dyslipidemia (HDL abnormalities) in both groups of migraineurs and non-migraineurs
Discussion
Migraine is a common disabling disorder, which affects 12% of the world's population. Approximately 13% of US citizens are said to have migraine attacks every year. According to the World Health Organization, migraine is ranked 20th in the world's debilitating disorder, and the resulting burden (health and cost) from migraine alone exceeds the burden of epilepsy, stroke, Parkinson's disease, multiple sclerosis, and Alzheimer's disease.[2] The overall prevalence of migraine in the Western countries is between 5% and 9% in men and 12% and 25% in women.[20] Similar studies have been performed in various studies on different age, sex, and occupation levels in Iran, which indicate a high prevalence of migraines.[21,22]
Given the significant prevalence of migraine in the world and in Iran, more attention should be paid to clarifying the causes, severity, consequences, and complications of the disease. One of the factors that has been studied in several studies is the significant association of dyslipidemia with other metabolic disorders, including insulin resistance in migraine sufferers especially migraine aura.
Some recent studies have suggested that the intensity and frequency of migraine attacks may be related to the level of blood lipids.[23,24,25] The mentioned issues emphasize the importance of further studying the association of these metabolic disorders as controllable risk factors for cardiovascular disorders.
Regarding the lack of study on the prevalence of dyslipidemia in patients with migraine in Iran, we investigated the distribution of triglycerides, cholesterol, LDL, and HDL in patients with migraine compared with the control group.
Our results revealed that in the migraine group, 9 patients (18%) showed high levels of triglyceride and 10 (20%) had abnormal HDL levels; whereas in the control group, 8 subjects (16%) had high levels of triglyceride and abnormal HDL levels were seen in 9 (18%) patients. The results of the statistical test did not show a significant relationship between the two groups.
On the other hand, in the migraine group, 21 patients (42%) exhibited high levels of cholesterol and 22 (44%) had high levels of LDL; whereas in people without migraine, 12 subjects (24%) showed high levels of cholesterol and high levels of LDL were seen in 12 subjects (24%), which showed a significant correlation between the two groups.
In line with our study, some recent studies have shown that the prevalence of dyslipidemia in migraine sufferers is higher than the normal population, and the frequency and severity of migraine attacks are related to serum lipid levels. For instance, Gruber et al. reported a clear increase in cholesterol, LDL-C, and oxidized LDL-C in normal-weight migraineurs, and an increase in oxidized LDL-C has been associated with a 7.93-fold increased risk of migraine.[11] Scher et al. indicated that migraineurs with aura were more likely to show an unsatisfactory level of cholesterol profile, where the mean total cholesterol was higher in migraineurs with aura when compared with normal population. The ratio of HDL cholesterol to total cholesterol was found to be greater than 5.
Migraine, especially with aura, is associated with a higher risk of cardiovascular disease compared with individuals without migraine.[5] Another study evaluated lipid profile parameters among episodic migraineurs and healthy participants, where the values of total cholesterol and very-low-density lipoprotein levels were significantly associated with migraine.[19] A study by Kurth et al. in 2008 reported that migraines are closely linked to the unfavorable factors of cardiovascular diseases and the increased risk of cardiovascular diseases. In this cohort analysis of 5087 women, there was a significant increase in total cholesterol, non-HDL cholesterol, apo protein B100, and C-reactive protein in the migraine group compared with the nonmigraine control group, where all these increases were statistically significant[26]; the results of all these studies are consistent with the results of our study. One of the important factors in all these studies is the disturbance in serum lipid levels as an etiologic factor, which was confirmed in our study.
Conclusion
Comparison of differences in triglyceride, cholesterol, LDL, and HDL levels between migraine and control group showed that there was a higher level of cholesterol and LDL in the migraineurs when compared with the control group, which shows a significant relationship. However, triglyceride and HDL levels in patients with migraine did not differ significantly with the control group.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Steiner TJ, Birbeck GL, Jensen RH, Katsarava Z, Stovner LJ, Martelletti P. Headache disorders are third cause of disability worldwide. J Headache Pain. 2015;16:58. doi: 10.1186/s10194-015-0544-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO, Lifting the burden. Atlas of headache disorders and resourcesin the world 2011. ISBN: 9789241564212. https://www.who.int/mental_health/management/atlas_headache_disorders/en/
- 3.Manzoni GC, Stovner LJ. Epidemiology of headache. In: Nappi G, Moskowitz MA, editors. Headache Handbook of Clinical Neurology. 3rd series. Vol. 97. Edinburgh: Elsevier; 2011. pp. 3–22. [DOI] [PubMed] [Google Scholar]
- 4.Haan J, Hollander J, Ferrari MD. Migraine in the elderly: A review. Cephalalgia. 2007;27:97–106. doi: 10.1111/j.1468-2982.2006.01250.x. [DOI] [PubMed] [Google Scholar]
- 5.Scher AI, Terwindt GM, Picavet HS, Verschuren WM, Ferrari MD, Launer LJ. Cardiovascular risk factors and migraine: The GEM population-based study. Neurology. 2005;64:614–20. doi: 10.1212/01.WNL.0000151857.43225.49. [DOI] [PubMed] [Google Scholar]
- 6.Hadj-Taieb S, Elasmi M, Hammami MB, Marrakchi R, Amani K, Omar S, et al. Dyslipidemia in the Greater Tunis population: prevalence and determinants. Clin Lab. 2012;58:763–70. [PubMed] [Google Scholar]
- 7.Ford ES, Li C, Pearson WS, Zhao G, Mokdad AH. Trends in hypercholesterolemia, treatment and control among United States adults. Int J Cardiol. 2010;140:226–35. doi: 10.1016/j.ijcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 8.Poorolajal J, Zamani R, Mir-Moeini R, Amiri B, Majzoobi MM, Erfani H, et al. Five-year evaluation of chronic diseases in Hamadan, Iran: 2005–2009. Iran J Public Health. 2012;41:71–81. [PMC free article] [PubMed] [Google Scholar]
- 9.Ko M, Kim MT, Nam JJ. Assessing risk factors of coronary heart disease and its risk prediction among Korean adults: The 2001 Korea National Health and Nutrition Examination Survey. Int J Cardiol. 2006;110:184–90. doi: 10.1016/j.ijcard.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 10.Alexander CM, Landsman PB, Teutsch SM. Diabetes mellitus, impaired fasting glucose, atherosclerotic risk factors, and prevalence of coronary heart disease. Am J Cardiol. 2000;86:897–902. doi: 10.1016/s0002-9149(00)01118-8. [DOI] [PubMed] [Google Scholar]
- 11.Gruber HJ, Bernecker C, Pailer S, Lechner A, Horejsi R, Möller R, et al. Lipid profile in normal weight migraineurs – Evidence for cardiovascular risk. Eur J Neurol. 2010;17:419–25. doi: 10.1111/j.1468-1331.2009.02861.x. [DOI] [PubMed] [Google Scholar]
- 12.Tana C, Santilli F, Martelletti P, di Vincenzo A, Cipollone F, Davì G, et al. Correlation between migraine severity and cholesterol levels. Pain Pract. 2015;15:662–70. doi: 10.1111/papr.12229. [DOI] [PubMed] [Google Scholar]
- 13.Rist PM, Tzourio C, Kurth T. Associations between lipid levels and migraine: cross-sectional analysis in the epidemiology of vascular ageing study. Cephalalgia. 2011;31:1459–65. doi: 10.1177/0333102411421682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bigal ME, Kurth T, Hu H, Santanello N, Lipton RB. Migraine and cardiovascular disease in the population.The American Migraine Prevalence and Prevention Study. Neurology. 2009;72:1864–71. doi: 10.1212/WNL.0b013e3181a71220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elliott D. Migraine and stroke: current perspectives. Neurol Res. 2008;30:801–12. doi: 10.1179/174313208X341049. [DOI] [PubMed] [Google Scholar]
- 16.Rose KM, Wong TY, Carson AP, Couper DJ, Klein R, Sharrett AR. Migraine and retinal microvascular abnormalities: the Atherosclerosis Risk in Communities Study. Neurology. 2007;68:1694–700. doi: 10.1212/01.wnl.0000261916.42871.05. [DOI] [PubMed] [Google Scholar]
- 17.The International Classification of Headache Disorders. Cephalalgia. 2004;24:24–33. [Google Scholar]
- 18.The International Classification of Headache Disorders, 3rd edition (beta version) Cephalalgia. 2013;33:644–58. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 19.Rangan V, Thangavel D, Bedi M, Varshney VP, Jayabal M, Subramaniam V. Comparative study of lipid profile between episodic migraineurs and healthy volunteers. Int J Med Sci Public Health. 2015;4:327–330. [Google Scholar]
- 20.Lipton RB. Chronic migraine, classification, differential diagnosis, and epidemiology. Headache. 2011;51(Suppl 2):77–83. doi: 10.1111/j.1526-4610.2011.01954.x. [DOI] [PubMed] [Google Scholar]
- 21.Jamshidifar F, Sadeghi O, Nasiri M, Askari GH, Maghsoudi Z, Khorvash F. The relationship between migraine and cardiovascular diseases: Review on evidence. J Clin Exc. 2014;3:1–11. [Google Scholar]
- 22.Sadeghi O, Askari GhR, Maghsoudi Z, Nasiri M, Khorvash F. Migraine and risk of stroke: Review of current evidence. Jundishapur J Chronic Dis Care. 2014;3:e21707. [Google Scholar]
- 23.Saadatnia M, Haghjooy Javanmard SH, Amini L, Salmasi M. Comparison of the severity, duration and frequency of headaches between migraine patients with and without metabolic syndrome. J Isfahan Med Sch. 2012;30:1687–95. [Google Scholar]
- 24.Janoska M, Chorążka K, Domitrz I. Migraine frequency and its association with dyslipidemia in women. Neurol Neurochir Pol. 2015;49:95–8. doi: 10.1016/j.pjnns.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Ferrara LA, Pacioni D, Di Fronzo V, Russo BF, Speranza E, Carlino V, et al. Low-lipid diet reduces frequency and severity of acute migraine attacks. Nutr Metab Cardiovasc Dis. 2015;25:370–5. doi: 10.1016/j.numecd.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 26.Kurth T, Ridker PM, Buring JE. Migraine and biomarkers of cardiovascular disease in women. Cephalalgia. 2008;28:49–56. doi: 10.1111/j.1468-2982.2007.01467.x. [DOI] [PubMed] [Google Scholar]


