Abstract
Context:
Menopause is associated with high risk of depression among women. Studies have shown that group cognitive behavioral theory (CBT) is safe and effective treatment for depression among menopausal women; however, only limited studies are conducted in India.
Aims:
To examine the efficacy of group CBT for depression among menopausal woman.
Settings and Design:
A randomized, controlled trial design was adopted with longitudinal measurement of outcomes for 6 months. The study was conducted from January 2017 to November 2017 at selected Primary Health Centre (PHC) area, urban Bengaluru.
Subject and Methods:
Participants were 80 women from selected PHC areas, Bengaluru, India. The participants were randomly assigned to either the experimental or control group by computer-generated random numbers. The experimental group received six weekly group CBT sessions. Depression was evaluated for both groups at the baseline and at two follow-up assessments in the 1st and 6th month. Treatment effects of the group CBT were analyzed by repeated-measures analysis of variance.
Statistical Analysis Used:
Data were analyzed using Statistical Package for the Social Sciences software package (Version 23).
Results:
The results showed that comparisons of depression scores between the two groups before initiating group CBT were not significant. Statistically significant reduction in depression scores were seen among experimental group compared to control group over the 6-month period.
Conclusion:
This study concluded that group CBT is effective for reducing depression among menopausal woman.
Keywords: Depression and menopause, group cognitive behavioral therapy, menopause
Introduction
Depression is an extremely common illness affecting people of all ages, genders, socioeconomic groups, and religions in India and all over the world. Globally, an estimated 322 million people were affected by depression in 2015.[1] Previous studies on prevalence of depression in India reported incidence ranging from 1.8% (severe) to 39.6% (mild to moderately severe) with higher rates among females.[2,3,4] The transition to menopause is a period of increased risk of depression among women.[5,6] The study conducted by Bromberger et al. showed that women were two to four times more likely to experience major depression episodes when they were perimenopausal or early postmenopausal;[7] another study conducted by Afshari et al. showed that 59.8% of the 1280 samples were depressed; in particular, 39.8% had mild depression, 16% moderate depression, and 4% severe depression among menopausal women.[8]
The prevalence of anxiety symptoms in menopausal women is substantial, with estimates of as high as 51% women reporting tension/nervousness or irritability in the past 2 weeks or at the time of reporting and 25% reporting frequent irritability or nervousness.[9] The study conducted by Yazdanpanhi et al. showed that there is a higher risk of stress, anxiety, and depression among women who are experiencing menopausal symptoms.[10] An Indian cross-sectional study reported level of syndromal depression and anxiety to be 86.7% and 88.9%, respectively, among women aged 40–60 years. Most patients had the moderate type of depression (49.5%) followed by mild (29.4%) and severe depression (7.8%).[11]
Depression adversely affects an individual's social relationship, capacity to work and learn, and is an indicator of the risk of self-harm and suicide.[12] Depression is also potentially harmful to physical health in addition to negatively impacting women's psychosocial wellbeing.[13] Considering physical and psychological problems that threaten women during this period, it seems that therapies that can help women cope with these problems, especially psychological ones, will be useful. One of the effective ways is cognitive behavioral therapy (CBT). The general physician or community mental health nurse is usually the first health professional whom women rely on to relieve their menopause symptoms. It is essential for the primary health care person to know how to properly approach women at this stage of their life and how to provide them the best and safe treatment.[14] Because only limited studies have been done among menopausal women in India, the present study focused on reducing depression of menopausal women by using group CBT delivered by nurses at primary health care center.
Aim
To examine the efficacy of group CBT for depression among menopausal woman.
Subjects and Methods
A randomized, controlled trial design was adopted with longitudinal measurement of outcomes for 6 months. This study was conducted from January 2017 to November 2017 at a selected PHC area, urban Bengaluru. Based on the findings of a pilot study, power analysis was carried out by using G*Power 3.1.9.2 software program by keeping the power of study at 80% (P < 0.05; two-tailed). The power analysis revealed that 30 participants in each group would be sufficient to achieve statistical significance, and hence, a total 80 participants were included in the study. The researcher initially screened menopausal women for depression symptoms using standardized tools, and those who meeting the inclusion criteria and agreeing to attend the study were selected after giving them further explanations about the study, assuring them about the confidentiality of their information, and obtaining a written consent from them. Subsequently, the participants were assigned to experimental and control groups through computer-generated random numbers. The experimental group received six weekly group CBT sessions lasting for 50–60 min; the sessions included psycho-education, relaxation exercises, and cognitive and behavioral strategies to overcome depression. In total, 316 women were approached, of whom 10 were not willing to participate. Out of 306 women, 102 scored positive for depression and met the inclusion criteria of being 40–60 years of age, menopausal, having ability to read and write Kannada or English; the study excluded women with chronic disorders and those undergoing any type of treatment [Figure 1].
Figure 1.
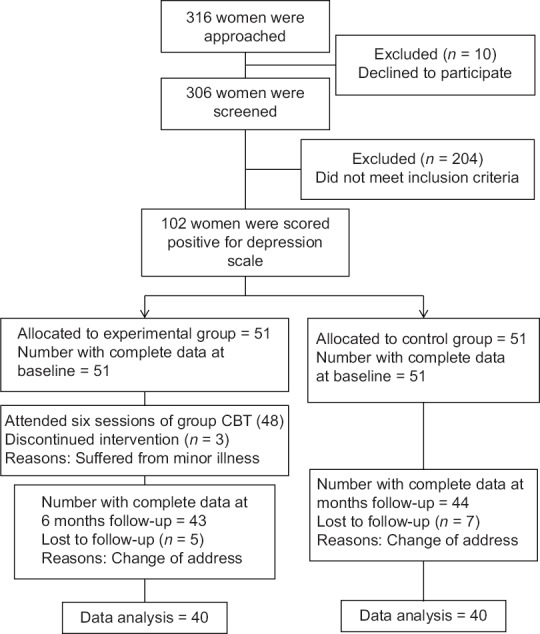
Flow chart showing distribution of women in experimental and control group
Data collection
After obtaining formal permission from the concerned authority, recruitment of participants took place at a selected PHC area. The author initially screened for depression. Each woman was contacted and a baseline assessment was done. They were informed that they would be randomly assigned to either the experimental or control group, as well as about the kind of participation required by them. Following the baseline assessment, all participants were randomly assigned by the author to either the experimental or control group. Six sessions of CBT were administered in the experimental group by one session per week for 6 weeks. Each session lasted for 50–60 min. Post assessment was carried out for both groups at 1 month and at 6 months.
Ethical consideration
The study protocol was approved by the institutional ethical committee. Formal permission was obtained from concerned area Medical Officer, and informed consent was taken from all participants. The purpose, nature, duration of the study, the researchers contact information, confidentiality, their right not to participate, or to withdraw at any time, and risks and benefits of the study were explained.
Assessment
Women who fulfilled the inclusion criteria were administered the Sociodemographic Performa and Center for Epidemiological Studies Depression Scale.
Sociodemographic Proforma: It includes questions on age, religion, marital status, educational qualification, occupation, monthly family income, type of family, number of children, and duration of menopause
Center for Epidemiological Studies Depression Scale (CES-D): This scale was developed initially by Laurie Radloff (1977) and is a 20-item self-report depression inventory with possible scores ranging from 0 to 60. Each response to an item is scored as follows: 0 = “Not At All;” 1 = “A Little;” 2 = “Some;” and 3 = “A Lot.” However, items 4, 8, 12, and 16 are phrased positively, and thus are scored in an opposite order: 3 = “Not At All;” 2 = “A Little;” 1 = “Some;” and 0 = “A Lot.” Higher CES-D scores indicate increasing levels of depression. A cut-off score of 16 or above was suggestive of depressive symptoms with good sensitivity and specificity and high internal consistency.[15]
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences software package (version 23, International Business Machines Corporation, US), and results were presented in a tabular form. Baseline characteristics of the experimental and control groups were compared using Chi-square or independent t-tests for categorical or continuous variables, respectively. The changes in the outcome variables from baseline to the 6-month follow-up were compared using repeated measures analysis of variance (ANOVA).
Results
Sample characteristics
Mean age of the sample was 48.89 years (SD 0.63); 65% were Hindu; 87.5% were married; and 47.5% of the reported no formal education whereas 60% of respondents were housewives. Median monthly family income of the sample was INR 7500 (Mean = 9383, SD = 3402). Sixty-eight percent were from joint family, 51.25% were having two children, and 80% of the respondents’ duration of menopause was less than 2 years. Both the groups (experimental and control) were comparable in terms of their baseline characteristics [Table 1].
Table 1.
Demographic characteristics of experimental and control group
| Demographic data | Items | Groups | χ2/t | P | |
|---|---|---|---|---|---|
| Experimental (n=40) | Control (n=40) | ||||
| Age in years (Mean SD) | 48.63 (0.55) | 49.16 (0.8) | 0.96 | 0.36 | |
| Religion | Hindu | 24 (60) | 28 (70) | 1.68 | 0.66 |
| Muslim | 06 (15) | 04 (10) | |||
| Christian | 10 (25) | 08 (20) | |||
| Marital status | Married | 34 (85) | 36 (90) | 0.46 | 0.27 |
| Widow | 06 (15) | 04 (10) | |||
| Educational qualification | No formal Education | 20 (50) | 18 (45) | 6.83 | 0.84 |
| Primary Education | 04 (10) | 10 (25) | |||
| Secondary Education | 06 (15) | 05 (12.5) | |||
| PUC | 07 (17.5) | 05 (12.5) | |||
| Degree and above | 03 (7.5) | 02 (5) | |||
| Occupation | Government Job | 04 (10) | 02 (5) | 4.48 | 0.25 |
| Private Job | 08 (20) | 06 (15) | |||
| Business | 05 (12.5) | 07 (17.5) | |||
| House wife | 23 (57.5) | 25 (62.5) | |||
| Monthly family income (Mean SD) | 8966 (3605) | 9800 (3199) | 0.82 | 0.68 | |
| Type of family | Nuclear | 10 (25) | 15 (37.5) | 1.32 | 0.56 |
| Joint | 30 (75) | 25 (62.5) | |||
| Number of children | 1 | 16 (40) | 13 (32.5) | 2.12 | 0.74 |
| 2 | 20 (50) | 21 (52.5) | |||
| More than 2 | 04 (10) | 06 (15) | |||
| Duration of menopause | 0-2 years | 34 (85) | 30 (75) | 3.25 | 0.59 |
| 3-5 years | 04 (10) | 06 (15) | |||
| Above 5 years | 02 (5) | 04 (10) | |||
There was no statistically significant difference between the two groups on depression score at baseline, however at 6 months, depression scores decreased among the experimental group compare to the control group.
Intervention effect
Repeated-measures ANOVA was conducted to determine the changes in the outcome variables from the baseline to 6-month follow-up. There were significant CBT intervention effects on depression among menopausal women. Compared with the control group, the CBT group showed statistically significant decrease in depression scores (F = 25.26, P = 0.000) over the 6-month period [Table 2].
Table 2.
Group comparison of depression scores across the time points (n=80)
| Time of assessment | Experimental group Mean (SD) | Control group Mean (SD) | Time effect F/P | Group effect F/P | Time × group effect F/P |
|---|---|---|---|---|---|
| Baseline (T0) | 19.03 (5.62) | 19.58 (4.89) | F=39.15, P=0.000 | F=4.34, P=0.034 | F=25.26, P=0.000 |
| 1 month (T1) | 16.40 (4.33) | 19.86 (5.03) | |||
| 6 month (T2) | 10.23 (3.12) | 20.92 (5.12) |
Discussion
The present study suggests that group CBT intervention was effective in reducing depression among menopausal women in the experimental group. The intervention included an explanation regarding the nature of problems, techniques for managing somatic reactions with relaxation training, and cognitive restructuring by identifying and challenging automatic thoughts; practicing problem-solving for coping with anticipated challenges; and to cope with hormonal changes. As depressed patients exaggerate the risk of danger, these techniques make these patients think logically in such situations. On the other hand, when these techniques are employed in group sessions, they help the patients understand that they are not alone and other patients have similar problem. This results in reducing the feelings of loneliness, blame, and shyness. This also enables them to exchange constructive communication regarding solutions or coping strategies. Our findings echo previous research which shows that CBT intervention combining behavioral, cognitive, and educational strategies such as identifying and restructuring any unhelpful thoughts, behavioral strategies and psychological techniques to cope with psychological distress was effective in improving insomnia problems and quality of life among depressed women.[16] The study conducted by Stefanopoulou et al. found that Telephone-guided Self-Help forms of CBT are effective for women with problematic menopausal hot flushes and night sweats.[17] Norton et al. found that group CBT was effective for problematic menopause.[18] The study conducted by Nowakowski et al. found that among midlife women experiencing insomnia and nocturnal hot flashes, a four-session CBT intervention targeting both insomnia and hot flashes led to clinically meaningful improvements in sleep and depressive symptoms;[19] Cheng et al. also found that depression severity symptoms has been decreased among women who underwent CBT compared to the control condition.[20]
We found that there is no statistically significant difference between the two groups on depression score at baseline, but at 6 months, depression scores decreased among the experimental group compared to the control group. Our findings echo previous research which shows that menopausal women who underwent CBT exhibited significantly lower rates of clinically significant depression at posttreatment (8.2%) compared to the control group (19%).[20]
The general physician or primary care providers are the first health professionals whom women rely on to relieve their menopausal symptoms. The study conducted by Al-Eassa et al. shows that there is a lack of primary care physicians’ knowledge and confidence in recognizing the signs and symptoms of menopause and prescribing appropriate management.[21] General physicians are in a strategic position for identifying women at risk and choosing the appropriate prevention and therapeutic strategies.[22] Physicians are prescribing nondrug options which is becoming increasingly popular for managing menopausal complications;[23] hence, our study enlightens the knowledge of primary care providers.
Limitations
There are a few limitations of the present study. First, due to a modest sample size, the study's generalization is limited. Second, we had follow-up assessment till 6 months and did not evaluate whether intervention effects were long lasting. Finally, the Center for Epidemiological Studies Depression Scale is used to measure depression. This scale cannot diagnose conditions as ICD or DSM can do. On the other hand, group CBT cannot address each condition in detail. Therefore, it is advised that in future studies where group therapies are done, individual problems be addressed as well.
Conclusion
The study showed the feasibility of group cognitive behavioral therapy delivered by nurses for reducing depression among menopausal women. There is a need to create nationwide public awareness campaign through media, newspapers, radio programs, involvement of nongovernmental organizations, schools and colleges, and integrating distribution of public education materials with multipurpose workers so that early detection of depression among menopausal women is possible at the grassroots level. Routine screening of all women visiting antenatal, postnatal, and geriatric clinics; primary health centers in addition to general outpatient psychiatric clinics for depression is recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Depression and other common mental disorders: Global health estimates. Geneva: World Health Organization; 2017. [Last accessed on 2018 Sep 19]. Available from: http://apps.who.int/iris/handle/10665/254610 . [Google Scholar]
- 2.Charlson FJ, Baxter AJ, Cheng HG, Shidhaye R, Whiteford HA. The burden of mental, neurological, and substance use disorders in China and India: A systematic analysis of community representative epidemiological studies. Lancet. 2016;388:376–89. doi: 10.1016/S0140-6736(16)30590-6. [DOI] [PubMed] [Google Scholar]
- 3.Behera P, Sharan P, Mishra AK, Nongkynrih B, Kant S, Gupta SK. Prevalence and determinants of depression among elderly persons in a rural community from northern India. Natl Med J India. 2016;29:129–35. [PubMed] [Google Scholar]
- 4.Sengupta P, Benjamin AI. Prevalence of depression and associated risk factors among the elderly in urban and rural field practice areas of a tertiary care institution in Ludhiana. Indian J Public Health. 2015;59:3–8. doi: 10.4103/0019-557X.152845. [DOI] [PubMed] [Google Scholar]
- 5.Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition: The Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63:385–90. doi: 10.1001/archpsyc.63.4.385. [DOI] [PubMed] [Google Scholar]
- 6.Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006;63:375–82. doi: 10.1001/archpsyc.63.4.375. [DOI] [PubMed] [Google Scholar]
- 7.Bromberger JT, Kravitz HM, Chang YF, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: Study of Women's Health Across the Nation (SWAN) Psychol Med. 2011;41:1879–88. doi: 10.1017/S003329171100016X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Afshari P, Manochehri S, Tadayon M, Kianfar M, Haghighizade M. Prevalence of depression in Postmenopausal women, Jundishapur. J Chronic Dis Care. 2015;4:e27521. [Google Scholar]
- 9.Bromberger JT, Kravitz HM, Chang Y. Does risk for anxiety increase during the menopausal transition.Study of women's health across the nation? Menopause. 2013;20:488–95. doi: 10.1097/GME.0b013e3182730599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yazdanpanahi Z, Nikkholgh M, Akbarzadeh M, Pourahmad S. Stress, anxiety, depression and sexual dysfunction among postmenopausal women in shiraz, Iran, 2015. J Fam Community Med. 2018;25:82–7. doi: 10.4103/jfcm.JFCM_117_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bansal P, Chaudhary A, Soni RK, Sharma S, Gupta VK, Kaushal P. Depression and anxiety among middle-aged women: A community-based study. J Family Med Prim Care. 2015;4:576–81. doi: 10.4103/2249-4863.174297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clayton A, Guico-Pabia C. Recognition of depression among women presenting with menopausal symptoms. Menopause. 2008;1:758–67. doi: 10.1097/gme.0b013e31815dba9c. [DOI] [PubMed] [Google Scholar]
- 13.Perez-Lopez FR, Chedraui P, Gilbert JJ, Perez-Roncero G. Cardiovascular risk in menopausal women and prevalent related co-morbid conditions: Facing the post-Women's Health Initiative era. Fertil Steril. 2009;9:1171–86. doi: 10.1016/j.fertnstert.2009.06.032. [DOI] [PubMed] [Google Scholar]
- 14.Cavadas LF, Nunes A, Pinheiro M, Silva PT. Management of menopause in primary health care. Acta Med Port. 2010;23:227–36. [PubMed] [Google Scholar]
- 15.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiological Studies-Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12:277–87. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- 16.Qiu H, Ren W, Yang Y, Zhu X, Mao G, Mao S, et al. Effects of cognitive behavioral therapy for depression on improving insomnia and quality of life in Chinese women with breast cancer: Results of a randomized, controlled, multicenter trial. Neuropsychiatr Dis Treat. 2018;14:2665–73. doi: 10.2147/NDT.S171297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stefanopoulou E, Hunter MS. Telephone-guided self-help cognitive behavioural therapy for menopausal symptoms. Maturitas. 2014;77:73–7. doi: 10.1016/j.maturitas.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 18.Norton S, Chilcot J, Hunter MS. Cognitive-behavior therapy for menopausal symptoms: Moderators and mediators of treatment effects. Menopause. 2014;21:574–8. doi: 10.1097/GME.0000000000000095. [DOI] [PubMed] [Google Scholar]
- 19.Nowakowski S, Thurston RC, Meers JM, Stout-Aguilar J, Sadruddin SM, Hayman JM, et al. Cognitive behavioral therapy for menopausal insomnia in midlife women with insomnia and nocturnal hot flashes. Sleep. 2017;40:A125. [Google Scholar]
- 20.Cheng P, Fellman-Couture C, Ahmedani B, Tallent G, Arnedt J, Roehrs T, et al. 1086 CBT-I for Menopause related insomnia also reduces depression severity. Sleep. 2017;40:A405. [Google Scholar]
- 21.Al-Eassa AA, Al-Fadel AM, Al-Ajmi MA, Al-Najjar AA, Makboul GM, Elshazly M. Knowledge and attitude of primary care doctors towards management of postmenopausal symptoms. Alexandria J Med. 2012;48:167–73. [Google Scholar]
- 22.Michieli R, Musto M. Bone health in menopausal women: A role for General Practitioners. Clin Cases Miner Bone Metab. 2017;14:71–3. doi: 10.11138/ccmbm/2017.14.1.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnston J. Managing the menopause: Practical choices faced in primary care. Climacteric. 2011;14:8–12. doi: 10.3109/13697137.2011.626616. [DOI] [PubMed] [Google Scholar]


