Abstract
Background:
Enough evidence exists to attribute the occurrence of diarrheal disease outbreaks due to open defecation practice and unsafe sanitation methods. Open defecation enables pathogens such as virus, bacteria, and protozoa to infect humans by means of fecal–oral transmission methods through contaminated fluids, water, and fomites. To curb the malefic effects of open defecation, the Indian government had initiated pro sanitation program namely Swachh Bharat Mission (SBM) in 2014. SBM became the world's largest toilet-building initiative. More than 95 million toilets have been built across rural and urban India since the launch of this mission. This articulation summarizes the trend analysis of acute diarrheal disease (ADD) outbreaks over a 9-year period with emphasis on changes due to the building of toilets under the clean India campaign.
Methods:
Weekly ADD outbreaks data from national-level Integrated Disease Surveillance Program between 2010 and 2018 were used for trend analysis along with the number of toilets constructed in rural areas under SBM from the year 2014.
Results:
ADD outbreaks were analyzed from 2010 to 2018. The number of ADD outbreaks per year during the past 2 years (i.e., 2017 and 2018) of SBM regime was lesser than in any year during the investigation period. Seasonal variations during the months of May, June, July, and August account for 55%–60% of ADD outbreaks in any of the years; but for 2018, the total outbreaks were 46%, which is significantly lower than that of regular range of outbreaks in the peak season.
Conclusion:
The recent pattern of ADD outbreaks exhibits a declining rate.
Keywords: Acute diarrheal disease outbreaks, open defecation, sustainable development, Swachh Bharat Mission, toilet
Introduction
The interaction between diarrheal diseases and the environment we live is highly reciprocal. The more we defecate in open, the more probability for fecal–oral transmissions, and thus more diarrheal cases. During diarrhea, a patient usually has abnormally loose or fluid stools which are passed more frequent than in normal and this causes depleting body fluids resulting in profound dehydration. Acute diarrhea refers to many episodes of infectious diarrhea which have a rapid onset and short life (less than 14 days). Diarrhea is categorized as a common illness but acts as a global killer. Liu et al. reported that diarrhea kills approximately 2195 children every day which is more than AIDS, malaria, and measles combined.[1] Global Diarrhea Burden from WASH mentioned that diarrheal diseases account for one in nine child deaths worldwide, making diarrhea the second leading cause of death among children under the age of 5 years.[2]
Most diarrheal germs are spread from the stools of one person to the mouth of another and transmitted through contaminated water, food, or fomites. The contamination with stools will happen if people practice open defecation near water sources, open spaces, and fields. The causative infectious agents due to open defecation include bacteria (Vibrio cholerae, Shigella species), viruses (Rotavirus, Entamoeba histolytica, Giardia lamblia), and helminths (Ascaris lumbricoides, Necator americanus, Taenia saginata). Brown et al. explained that excreta-related pathogens will find a new host from feces to food through fluids, fields, flies, fomites, and fingers.[3] Children are more vulnerable to this fecal–oral transmission process. De Graaf et al. elaborated the transmission amplifiers of enteric pathogens between humans through the fecal–oral route.[4] The practice of open defecation acts a basis for all infections and morbidity.[5]
Colombara et al. mentioned that the chronic health consequences of acute enteric infections are very much higher in India.[6] Ahs et al. mentioned that diarrheal diseases are associated with poor socioeconomic conditions, such as lack of access to safe water and sanitation, poor hygienic practices, and unsafe human waste disposal.[7] Literature study shows strong evidence that both sanitation and hygienic interventions are highly effective in reducing risks of diarrhea.[8] Studies done by Coffey et al. reported that open defecation constitutes a health and human capital crisis in India due to the stubborn practice of open defecation.[9]
As per the 2011 Census of India, 68.84% of India's population lived in villages; among those, only 32.70% of the households had access to toilets.[10] United Nations Sustainable Development Goal 6 (SDG6) aims to “achieve access to adequate and equitable sanitation and hygiene for all and end open defecation, paying special attention to the needs of women and girls and those in vulnerable situations.”[11] To adhere to the SDG6 targets and also to amplify the public health needs, the Indian government has committed to ending open defecation and unsafe sanitation method by 2019, the 150th anniversary of Mahatma Gandhi's birth. In October 2014, it had launched a fully funded national hygiene, sanitation, and waste management campaign called Swachh Bharat Mission (SBM).[12] The extent of the mission will cover both rural and urban areas of the country. The urban component of the mission will be implemented by the Ministry of Urban Development, and the rural component by the Ministry of Drinking Water and Sanitation. The overall objectives of SBM are categorized as follows:[13,14]
Bring about an improvement in the general quality of life in the rural and urban areas, by promoting cleanliness, hygiene, and eliminating open defecation
Accelerate sanitation coverage to achieve the vision of SBM by 2nd October 2019 through construction of individual household toilets, public toilets, and community toilets along with provisions of water storage and hand wash
Motivate the communities and village development institutions to adopt sustainable sanitation practices and facilities through awareness creation and health education. The mission should bring positive behavioral change regarding healthy sanitation practices in both rural and urban areas. Generating awareness about sanitation and its linkage with public health is also one of the top priorities in SBM
Encourage cost-effective and appropriate technologies for ecologically safe and sustainable sanitation. Augmentation of the modern and scientific municipal solid and liquid waste management is one more area where SBM is been capitalized
Create a significant positive impact on gender and promote social inclusion by improving sanitation especially in marginalized communities
Capacity augmentation to create an enabling environment for private sector participation in Capex (capital expenditure) and Open (operation and maintenance).
The strategy is to move toward a “Swachh Bharat” aka Cleaner India by making it a massive mass movement that seeks to engage everyone in the task of cleaning homes, workplaces, villages, cities, and surroundings, in a collective quest. As on date, the progress reported for rural sanitation coverage is 98.8%; 92 millions of toilets were constructed, and 604 districts were declared with open defecation free (ODF) status. With respect to urban sanitation, 5.9 million of individual household toilets, community, and public toilets were constructed. Approximately 3461 cities/town were declared with ODF status.
An outbreak can be understood as an incident in which two or more people in a community, thought to have a common exposure, experience a similar illness or proven infection. This article investigates the trend of acute diarrheal disease (ADD) outbreaks occurred over a span of 9 years and correlates with that of SBM's objectives.
Methods
National-level disease surveillance programs are highly useful to ensure global health security through a means to monitor the disease spread and at the same time to provide a public health response.[15]
Controllability of communicable disease relies on the effectiveness of the response systems. An effective response system depends on effective disease surveillance, where surveillance is the first step toward prevention.[16] In India, National Centre for Diseases Control under the Directorate General of Health Services, Ministry of Health and Family Welfare, is the focal point for Integrated Disease Surveillance Program (IDSP).[17] IDSP consists of state-of-art cyber-infrastructure connecting all states and district headquarters to collect, compile, analyze, and disseminate the data to the public. In this article, ADD outbreaks for 9 years (2010–2018) were retrieved from IDSP weekly reports. The trend has been analyzed and inference has been compiled.
Earlier IDSP weekly reports were used by medical researches for investigating outbreaks related to hepatitis E, Zika virus, Kyasanur forest disease, dengue, and chikungunya.[18,19,20,21,22] Debnath and Ponnaiah in their findings mentioned that timeliness of reporting is acceptable with respect to ADD outbreaks in IDSP database.[23]
The weekly reports of IDSP data are organized at the district level with information pertaining to disease, number of humans effected, date stamp of the outbreak, and case details. All the ADD outbreaks from 2010 to 2018 were retrieved from IDSP weekly outbreaks database.[17]
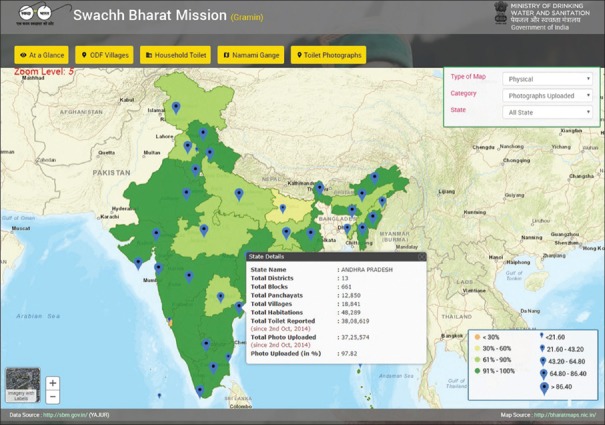
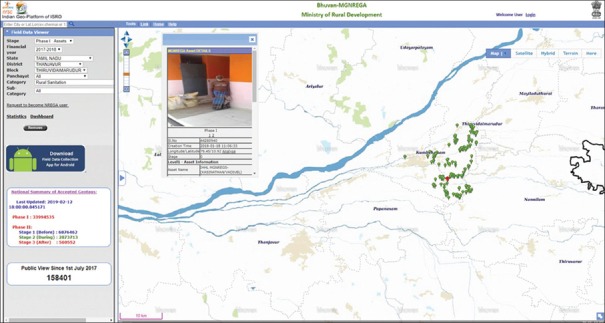
Monthly toilets construed and completed in all forms were taken from SBM web portal (https://sbm.gov.in) which is maintained by the Ministry of Drinking Water and Sanitation. The SBM web portal contains all the results from various management information systems (MIS) and disseminated through the online dashboards for the purpose of transparency and accountability. The progress of SBM is shown for social reporting using web-based geographic information system (GIS) along with the information about the total number of photographs that are uploaded. Figure 1 depicts the dashboard of SBM. On regular intervals and during milestone achievements, Indian government issues press information about the highlights of the mission.[24] Geospatial platforms like Bhuvan web portal (http://bhuvan.nrsc.gov.in) were used to disseminate geotagged photographs as a part of the evidence as shown in Figure 2.
Figure 1.
Dashboard of Swachh Bharat Mission for social reporting which gives progress of the mission along with open defecation free (ODF) status of the villages
Figure 2.
Bhuvan web portal depicting location based photographic evidence of toilets build under convergence programs
Results
Table 1 represents the year-wise count of ADD outbreaks, summer and July season peaks, the total number of toilets constructed under SBM, and total villages that gained the status of ODF. The following remarks are derived from the statistical observations done on the trend from 2010 to 2018.
Table 1.
Total number of acute diarrheal diseases, peak outbreaks, and number of toilets constructed under SBM
| Year | No. of total ADD outbreaks in a year | Total ADD outbreaks during summer peak | Total ADD outbreaks during July peak | Total no. of ADD outbreaks during May, June, July, and August and their % with respect to total yearly ADD outbreaks | No. of toilets constructed under SBM (in millions)* | Total no. of villages declared as ODF and % |
|---|---|---|---|---|---|---|
| 2010 | 415 | 62 | 51 | 226 (54.46) | ||
| 2011 | 536 | 65 | 96 | 284 (52.98) | ||
| 2012 | 470 | 76 | 97 | 295 (62.76) | ||
| 2013 | 613 | 62 | 133 | 353 (57.58) | ||
| 2014 | 344 | 37 | 70 | 200 (58.13) | 1.5 | |
| 2015 | 437 | 48 | 88 | 256 (58.58) | 12.5 | 47,021 (7.9) |
| 2016 | 631 | 93 | 152 | 393 (62.28) | 30.5 | 182,621 (30.5) |
| 2017 | 318 | 46 | 64 | 178 (55.97) | 57.1 | 349,319 (58.2) |
| 2018 | 324 | 38 | 51 | 151 (46.60) | 90.5 | 550,485 (85.9) |
SBM: Swachh Bharat Mission; ADD: Acute diarrheal disease; ODF: Open defecation free, *SBM initiated in October, 2014
2017 and 2018 recorded the lowest number of total ADD outbreaks
Summer peak of 2018 showed the lowest number of ADD outbreaks in comparison to the remaining years’ summer peaks. Remarkably, the total outbreaks that recorded during this year were much lower than the total outbreaks that were recorded during 2010
It is worth mentioning that the outbreaks were directly proportional to the population as the risk of spreading the disease to others will increase with an increase in the population.[25] The population of India as per the census for the year 2011 was 1.21 billion, and the model-derived population at the end of the year 2018 was 1.37 billion.[26] The trend of total ADD outbreaks showed 50% lower for 2017 and 2018 in comparison to the total ADD outbreaks that occurred during 2016
The impact of seasonality is highly correlated with ADD outbreaks.[27] Evidentially, 52%–60% of ADD outbreaks were recorded in India during the months of May, June, July, and August from 2010 till 2017. In 2018, certain environmental correction seemed to have happened as these four months have recorded a lesser number of outbreaks in comparison to previous years (46.60% only).
Figures 3 and 4 depict the trend line of monthly total and a yearly total of ADD outbreaks, respectively, from 2010 to 2018. The trend line shows that in 2017 and 2018, the ADD outbreaks are minimum for the months of May, July, August, September, November, and December. Figure 5 represents the bubble chart for the ADD outbreaks for the hotspot districts in the states of Gujarat, Andhra Pradesh, Telangana, West Bengal, Karnataka, and Assam. Interpretation from this bubble chart clearly shows that for 2017 and 2018, there is a recognizable change in ADD outbreaks’ pattern.
Figure 3.
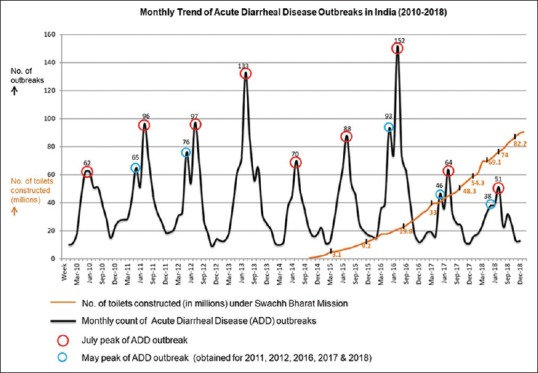
Graph plotted for monthly Acute Diarrheal Disease (ADD) outbreaks from the year 2010 till 2018. Minimum July peak obtained was in the year 2018 (during Swachh Bharat Mission regime) and gradual reduction of ADD outbreaks is seen in the year 2017 and 2018
Figure 4.
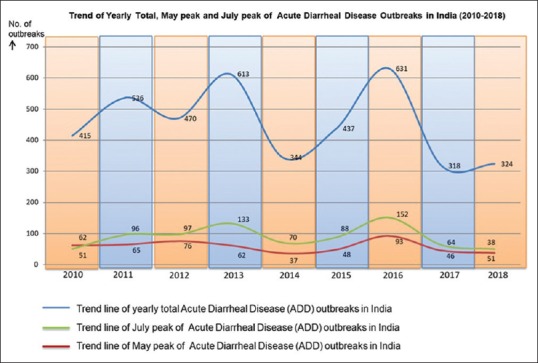
Trend of yearly total Acute Diarrheal Disease outbreaks from the year 2010 till 2018 along with trend of summer and July peaks. Evidence of lowest total ADD outbreaks were seen during the years 2017 and 2018
Figure 5.
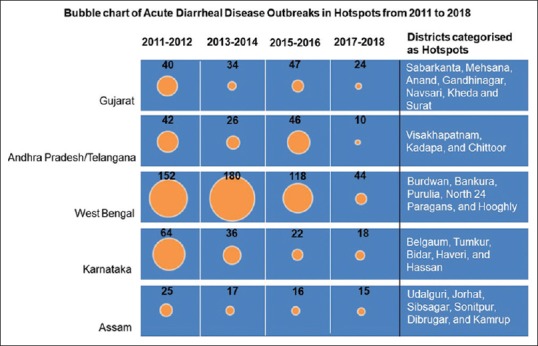
Bubble chart representing total acute diarrheal disease outbreaks for the districts categorised as hotspots in five states
Discussion
Hutton et al. while reporting their work on global cost–benefit analysis of water supply and sanitation interventions for developing regions explained that the accrued returns will be on higher side.[28] Earlier, the Government of India had initiated programs such as Central Rural Sanitation Program in 1986 which failed because the reality on the ground did not match the requirements for success.[29] Total Sanitation Campaign (TSC) was launched in the year 1999 including the key lessons that were learned from previous ones and consisted of forward looking policies, combined resources, strong institute setting, and decentralized delivery.[30] TSC resulted in semi-success as the progress observed was uneven but high citizen participation, strong monitoring, and political determination were intensified. TSC was restructured and renamed as Nirmal Bharat Abhiyan (NBA) in 2012. In 2014, the sanitation flagship program was redesigned once again and rechristened to SBM, which aimed at providing access to sanitation facilities and eradicating the practice of open defecation by 2019.
Prüss-Üstün and Corvalán specified that human behavior is also a major factor that can be attributed to ADD outbreaks along with poor sanitation methods.[31] Iyer in his report mentioned that “Unlike earlier era sanitation programmes, the SBM is not only a toilet construction programme but also a mass level behaviour change movement.”[32] While mass media campaigns act as motivators, the real key for bringing the behavior change on the ground is to have grassroots-level trained and incentivized motivators who can bring about interpersonal communication with the villagers and households to trigger the demand for using toilets and sensitivity toward sanitation. Table 2 depicts the budget allocations by the Government of India for SBM.[33,34] These large-scale budget allocations clearly indicate that the Indian government has a keen interest in this large-scale sanitation intervention.
Table 2.
| Category of SBM | Budget allocations (in INR billion) | ||||
|---|---|---|---|---|---|
| FY 2014-15 | FY 2015-16 | FY 2016-17 | FY 2017-18 | FY 2017-18 | |
| SBM - G | 28.50 | 65.25 | 105 | 169.48 | 153.43 |
| SBM - U | 16.91 | 10.00 | 23.00 | 23.00 | 25.00 |
SBM: Swachh Bharat Mission
Data journalists termed SBM as “India's sanitation revolution” based on the progress of the project.[35] Surveys done by Coffey et al. (before the launch of SBM) and recently by Gupta et al. hinted heterogeneous results from their study areas, but mentioned that more people are switching to latrine use.[9,36] Roy and Pramanick while assessing the progress of sanitation in India have analyzed the interrelationships between SDG 6, SDG 3, and SDG 1.[37] Their study concluded with a positive impact of increasing per capita gross domestic product (GDP) on improving sanitation-related indicators, which in turn positively influence to reduce water and sanitation-related diseases, especially in children and aged population.
In the global perspective, the sanitation revolution of the Victorian era was the most important medical milestone since 1840 as there was a dramatic reduction in morbidity and mortality associated with fecal–oral infections in Britain and the surroundings.[3] During 1960, open defecation was rampant in Singapore due to which public health was worst affected due to frequent outbreaks of diarrhea.[38] Government's intervention in environmental-driven efforts between 1977 and 1987 and resolution like “Sanitation for All” made Singapore to gain a reputation as place of orderliness. Zambia has made great progress in the area of public health after adopting community led total sanitation (CLED) program which ensured safe disposal of fecal matter.[39]
Zwane and Kremer in their report mentioned that the elimination of open defecation is an important key for fighting diarrheal disease in developing countries.[40] Ashbolt has explained the interlinking nature of poor sanitation with enteric pathogen exposure and the main disease outcome as diarrhea.[41] Researchers and practitioners like Allam et al., Koria et al., Alexander and Blackburn, and Patil et al. have earlier concluded that there is a strong correlation of ADD outbreaks and open defecation practice.[42,43,44,45] The success phenomenon that was observed from this investigation is the sudden decrease in the trend line of ADD outbreaks during recent years. This sudden decrease in the ADD outbreaks can be attributed to toilet usage (if not 100%, but to a certain proportion). Toilet usage may have reduced pathogen exposure to a considerable extent. Toilet construction spree has been evaluated by many researchers, but usage is yet to be evaluated. Currently, the number of toilets that have been constructed and ODF status that was given to villages clearly give the signs of achieving the targets of SBM much before 2nd October 2019. The contributions in the form of political push, public financing, partnerships, and people participation have revolutionized the world's largest sanitation program in India. Full-fledged evaluation of SBM has to be made using the indicators of SDG 6.2. Economic significance is one more area where the decrease in ADD outbreaks can significantly strengthen the GDP. However, the results from our investigation suggest that the anticipated change has started as per the ambitions of SBM.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Deep gratitude is expressed by the authors to Dr. Kuldeep Singh, Dean (Academics), AIIMS, Jodhpur, India and Shri. Santanu Chowdhury, Director, National Remote Sensing Centre, Hyderabad, India for their valuable guidance and also for providing facilities to carry out research and developmental projects in the area of heterogeneity with Geospatial Technology and Public Health. The authors are also thankful to Prof. Gollapalli Nageswara Rao, Vice Chancellor, Andhra University, Visakhapatnam, India for his motivation and encouragement.
References
- 1.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–61. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 2.WASH. Global Diarrhea Burden. [Last accessed on 2019 Feb 09]. Available from: https://www.cdc.gov/healthywater/global/diarrhea-burden.html#one .
- 3.Brown J, Cairncross S, Ensink JH. Water, sanitation, hygiene and enteric infections in children. Arch Dis Child. 2013;98:629–34. doi: 10.1136/archdischild-2011-301528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Graaf M, Beck R, Caccio SM, Duim B, Fraaij PL, Le Guyader FS, et al. Sustained fecal-oral human-to-human transmission following a zoonotic event. Curr Opin Virol. 2017;22:1–6. doi: 10.1016/j.coviro.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ambesh P, Ambesh SP. Open defecation in India: A major health hazard and hurdle in infection control. J Clin Diagn Res. 2016;10:IL01. doi: 10.7860/JCDR/2016/20723.8098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colombara DV, Khalil IA, Rao PC, Troeger C, Forouzanfar MH, Riddle MS, et al. Chronic health consequences of acute enteric infections in the developing world. Am J Gastroenterol. 2016;3:4. [Google Scholar]
- 7.Ahs JW, Tao W, Löfgren J, Forsberg BC. Diarrheal diseases in low-and middle-income countries: Incidence, prevention and management. Open Infect Dis J. 2010;4:113–24. [Google Scholar]
- 8.3ie. Running Water, working toilets and safe hygiene practices: Essentials services to save lives. [Last accessed on 2019 Feb 09]. Available from: http://www. 3ieimpact.org/evidence-hub/publications/impact.evaluation/running.water-working-toilets-and-safe-hygiene .
- 9.Coffey D, Gupta A, Hathi P, Khurana N, Spears D, Srivastav N, et al. Revealed preference for open defecation. Econ Political Wkly. 2014;49:43. [Google Scholar]
- 10.Ghosh SK, editor. Waste Management and Resource Efficiency: Proceedings of 6th IconSWM 2016. Springer; 2018. [Google Scholar]
- 11.SDG. Sustainable Development Goals. Knowledge Platform. [Last accessed on 2019 Feb 09]. Available from: https://sustainabledevelopment.un.org/
- 12.SBM. Swachh Bharat Mission – Gramin. [Last accessed on 2019 Feb 09]. Available from: http://swachhbharatmission.gov.in/sbmcms/index.htm .
- 13.SBM-G. Guidelines for Swachh Bharat Mission – Gramin. [Last accessed on 2019 Feb 19]. Available from: https://mdws.gov.in/sites/default/files/Complete%20set%20guidelines_1.pdf .
- 14.SBM-U. Guidelines for Swachh Bharat Mission – Urban. [Last accessed on 2019 Feb 19]. Available from: http://164.100.228.143:8080/sbm/content/writereaddata/SBM_Guideline.pdf .
- 15.World Health Assembly. International Health Regulations (2005) Geneva: World Health Organization; 2006. [Google Scholar]
- 16.Sharma R, Ratnesh L, Karad AB, Kandpal H, Dhariwal AC, Ichhupujani RL. Communicable disease outbreak detection by using supplementary tools to conventional surveillance methods under Integrated Disease Surveillance Project (IDSP), India. J Commun Dis. 2009;41:149–59. [PubMed] [Google Scholar]
- 17.IDSP. Integrated Disease Surveillance Program – National Centre for Diseases Control. [Last accessed on 2019 Feb 19]. Available from: https://idsp.nic.in .
- 18.Raval DA, Chauhan NT, Katara RS, Mishra PP, Zankar DV. Outbreak of hepatitis E with bimodal peak in rural area of Bhavnagar, India, 2010. Ann Trop Med Public Health. 2012;5:190. [Google Scholar]
- 19.Yadav PD, Malhotra B, Sapkal G, Nyayanit DA, Deshpande G, Gupta N, et al. Zika virus outbreak in Rajasthan, India in 2018 was caused by a virus endemic to Asia. Infect Genet Evol 2019; Online First. doi: 10.1016/j.meegid.2019.01.026. [DOI] [PubMed] [Google Scholar]
- 20.Chakraborty S, Andrade FC, Ghosh S, Uelmen J, O. Ruiz M. Historical expansion of Kyasanur forest disease in India from 1957 to 2017: A retrospective analysis. GeoHealth. 2019:3. doi: 10.1029/2018GH000164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chandran R, Azeez PA. Outbreak of dengue in Tamil Nadu, India. Curr Sci. 2015;10:171–6. [Google Scholar]
- 22.Shil P, Kothawale DR, Sudeep AB. Rainfall and Chikungunya incidences in India during 2010–2014. Virus Dis. 2018;29:46–53. doi: 10.1007/s13337-018-0428-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Debnath F, Ponnaiah M. Improved timeliness for reporting of acute diarrhoeal disease under surveillance overtime: Evaluation of integrated disease surveillance programme in North 24 Parganas, West Bengal, India, 2015. Clin Epidemiol Glob Health. 2018;6:163–7. [Google Scholar]
- 24.PIB. Ministry of Drinking Water & Sanitation. [Last accessed on 2019 Feb 09]. Available from: http://www.pib.nic.in/PressReleaseIframePage.aspx?PRID=1517640 .
- 25.Riddle MS, DuPont HL, Connor BA. ACG clinical guideline: Diagnosis, treatment, and prevention of acute diarrheal infections in adults. Am J Gastroenterol. 2016;111:602. doi: 10.1038/ajg.2016.126. [DOI] [PubMed] [Google Scholar]
- 26.Population. Our growing population. [Last accessed on 2019 Feb 09]. Available from: http://www.un.org/en/sections/issues-depth/population/
- 27.Pinfold JV, Horan NJ, Mara DD. Seasonal effects on the reported incidence of acute diarrhoeal disease in northeast Thailand. Int J Epidemiol. 1991;20:777–86. doi: 10.1093/ije/20.3.777. [DOI] [PubMed] [Google Scholar]
- 28.Hutton G, Haller L, Bartram J. Global cost-benefit analysis of water supply and sanitation interventions. J Water Health. 2007;5:481–502. doi: 10.2166/wh.2007.009. [DOI] [PubMed] [Google Scholar]
- 29.Ramani SV, Sadre Ghazi S, Duysters G. On the diffusion of toilets as bottom of the pyramid innovation: Lessons from sanitation entrepreneurs. Technol Forecast Soc Change. 2012;79:676–87. [Google Scholar]
- 30.Wicken J, Verhagen J, Sijbesma C, Da Silva C, Ryan P. Beyond construction; use by all. A collection of case studies from sanitation and hygiene promotion practitioners in South Asia. London and Delft: WaterAid, IRC International Water and Sanitation Centre. 2008 [Google Scholar]
- 31.Prüss-Üstün A, Corvalán C. Preventing Disease through Healthy Environments. towards an Estimate of the Environmental Burden of Disease. Geneva: World Health Organization; 2006. [Google Scholar]
- 32.Iyer The Swachh Bharat Mission: Everyone's Business. [Last accessed on 2019 Feb 09]. Available from: http://pibarchive.nic.in/ndagov/pstory/pStory47.pdf .
- 33.Budget Briefs. Swachh Bharat Mission – Gramin (SBM-G). GoI 2018-19. [Last accessed on 2019 Feb 19]. Available from: https://accountabilityindia.in/sites/default/files/pdf_files/Swachh%20Bharat%20Mission (Gramin)_0.pdf .
- 34.Budget Briefs. Swachh Bharat Mission – Urban (SBM-U). GoI 2018-19. [Last accessed on 2019 Feb 19]. Available from: https://accountabilityindia.in/sites/default/files/pdf_files/Swachh%20Bharat%20Mission%20Urban_0.pdf .
- 35.Statista. India's Toilet Building Revolution by Niall McCarthy. 2018. [Last accessed on 2019 Feb 09]. Available from: https://www.statista.com/chart/14924/indias-toilet-building-revolution/
- 36.Gupta A, Khalid N, Desphande D, Hathi P, Kapur A, Srivastav N, et al. Changes in Open Defecation in Rural North India: 2014-2018. IZA Discussion Papers 12065, Institute for the Study of Labor (IZA) 2018 [Google Scholar]
- 37.Roy A, Pramanick K. Analysing progress of sustainable development goal 6 in India: Past, present, and future. J Environ Manage. 2019;232:1049–65. doi: 10.1016/j.jenvman.2018.11.060. [DOI] [PubMed] [Google Scholar]
- 38.World Toilet. 50 years of sanitation in Singapore. [Last accessed on 2019 Feb 09]. Available from: http://worldtoilet.org/50.years-of-sanitationin.singapore/
- 39.Zulu G, Harvey P, Mukosha L. Revolutionising sanitation in Zambia: Scaling up CLTS. PLA. 2010;61:131–40. [Google Scholar]
- 40.Zwane AP, Kremer M. What works in fighting diarrheal diseases in developing countries. A critical review? World Bank Res Obser. 2007;22:1–24. [Google Scholar]
- 41.Ashbolt NJ. Microbial contamination of drinking water and disease outcomes in developing regions. Toxicology. 2004;198:229–38. doi: 10.1016/j.tox.2004.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Allam RR, Uthappa CK, Nalini C, Udaragudi PR, Tadi GP, Murhekar MV. An outbreak of cholera due to contaminated water, Medak District, Andhra Pradesh, India, 2013. Indian J Community Med. 2015;40:283. doi: 10.4103/0970-0218.164408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Koria B, Boricha BP, Munsi H, Sarvaiya J. Outbreak investigation of acute diarrheal disease in Palitana urban, Gujarat. Int J Community Med Public Health. 2017;4:2294–6. [Google Scholar]
- 44.Alexander KA, Blackburn JK. Overcoming barriers in evaluating outbreaks of diarrheal disease in resource poor settings: assessment of recurrent outbreaks in Chobe District, Botswana. BMC Public Health. 2013;13:775. doi: 10.1186/1471-2458-13-775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patil SB, Deshmukh D, Dixit JV, Damle AS. Epidemiological investigation of an outbreak of acute diarrheal disease: A shoe leather epidemiology. J Glob Infect Dis. 2011;3:361. doi: 10.4103/0974-777X.91060. [DOI] [PMC free article] [PubMed] [Google Scholar]