Abstract
Background: Sexual minority women (SMW) face barriers to healthcare that may result in lower utilization of cervical cancer screening. Previous experiences with the healthcare system—specifically reproductive health-related encounters—have the potential to affect future use of screening services. This study aimed to examine the association between pregnancy history and cervical cancer screening in a diverse sample of SMW. Anderson's Behavioral Model of Health Services Use guided the selection of variables included in the study.
Methods: We performed a secondary analysis of cross-sectional data from the third wave of the Chicago Health and Life Experiences of Women (CHLEW) Study, a longitudinal study of SMW in the Midwestern United States. We performed multivariable logistic regression to address the study aims, restricting the sample to women ages 21–45 (n = 430).
Results: Reporting a previous pregnancy was consistently positively associated with past-year Pap testing. In the multivariable model, bisexual identity and disclosing one's sexual orientation to healthcare providers were also positively associated with past-year Pap test.
Conclusions: This analysis provides preliminary evidence that SMW who have been pregnant are more likely to receive Pap testing and that multiple sociodemographic factors are likely to impact screening in this population. Clinicians should screen all patients with a cervix for cervical cancer and should encourage screening for all SMW. Future studies should prioritize longitudinal analyses to examine the temporality of reproductive history and healthcare seeking, focus on where SMW seek care, and understand how intersecting components of identity may shape the healthcare utilization of this population.
Keywords: LGBT health, health disparities, cervical cancer screening, pregnancy
Introduction
Cervical cancer screening via Papanicolaou test (Pap test) is a vital public health service, which has dramatically reduced cervical cancer mortality in the United States (US).1 According to the most recent available data, 12,578 new cases of cervical cancer were diagnosed and 4,115 women died of cervical cancer in the US in 2014.2 However, disparities in access to and use of Pap testing persist by race and ethnicity, socioeconomic status, and sexual orientation, among other sociodemographic factors.3,4 Based on the United States Preventive Services Task Force (USPSTF) recommendations, all people with a cervix are at risk for cervical cancer and thus should be screened regardless of sexual history, sexual orientation, or gender identity.5 However, compared to what is known about predictors of screening among heterosexual women, relatively little research has examined the relationship between sexual orientation and screening, or how to increase screening among sexual minority women (SMW), or those who identify as lesbian, gay, bisexual, or other nonheterosexual identities.
SMW face various individual and structural barriers to healthcare that result in lower utilization of primary and preventive healthcare services.6–8 Some research suggests that both SMW and healthcare providers may assume that SMW are not at risk for human papilloma virus (HPV) or other sexually transmitted infections (STIs).6–9 However, most SMW, including lesbian women, have had sexual encounters with men,10,11 and HPV and other STIs are transmissible between female partners and via objects used during sexual activity.12,13 In fact, SMW may be at an increased risk for cervical cancer compared to their heterosexual peers, as risk factors such as early age at sexual debut, low rates of hormonal contraceptive use, and smoking tend to aggregate among SMW.14 Existing research is not consistent with regard to SMW's use of cervical cancer screening. However, some studies have found that at least some groups of SMW report lower rates of cervical cancer screening9,15–18 and STI testing19–21 than their heterosexual counterparts.
Health-related “cues to screening” that are common for heterosexual women may be absent in populations of SMW. These cues include a general awareness of being at risk for HPV or cervical cancer. Previous studies have found that although SMW overall tend to have lower risk perceptions for HPV infection, higher perceptions are associated with higher odds of receiving Pap tests in this population.6,9 Important cues to screening also include the use of other sexual and reproductive health services. Receiving hormonal contraception, HPV vaccination, and STI testing have all been shown to increase odds of cervical cancer screening, but again, SMW may be less likely to utilize these services than are heterosexual women.18,22–24 Pregnancy and related healthcare experiences may act similarly as a cue to screening for SMW. Most pregnancies necessitate healthcare utilization, including fertility services, prenatal care, termination services, and/or birth care, all of which may present opportunities for discussion of cervical cancer screening. Many SMW experience pregnancy in various circumstances, including through assistive reproductive technologies,25,26 consensual sexual intercourse with male partners, or as the result of sexual assault and rape, for which SMW are at increased risk.27
Some previous studies have examined other healthcare services as correlates of cervical cancer screening among SMW. Having a regular healthcare provider,8,22,28,29 provider recommendation for Pap testing,8,22,23,30 and effective communication with providers23,31,32 have been found to be positively associated with cervical cancer screening among SMW. Disclosing one's sexual minority identity, or “coming out” to healthcare providers, has also been positively associated with screening, although concerns about and experiences of discrimination are common.8,22,28,32 These studies provide further evidence that certain healthcare encounters do increase the odds of Pap testing among SMW. Pregnancy-related encounters may strongly influence the odds of Pap test utilization among some SMW.
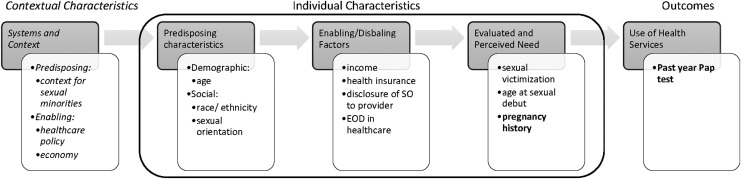
We used an adapted form of Andersen's Behavioral Model of Health Services Use33 to guide our investigation of potential relationships between pregnancy history and past-year Pap testing among SMW, adjusting for several covariates (Fig. 1). This model was originally developed to explain disparities in the use of health services and has been modified over the past several decades to account for new understandings of the sociopolitical influences on health services use.33,34 Other investigators have specifically used this model to examine health service use in SMW35 and other socially vulnerable populations.34
FIG. 1.
Theoretical model of factors influencing Pap test among SMW, adapted from Andersen's Behavioral Model of Health Services Use. Although we acknowledge that contextual characteristics (italicized) are important to understand patterns of health services use among SMW, the current analysis focuses on individual-level characteristics identified in this model. Pregnancy history and past-year Pap test (in bold) are the primary predictor of interest and outcome, respectively. EOD, experiences of discrimination; SMW, sexual minority women; SO, sexual orientation.
While Andersen's full model includes contextual characteristics that play important roles in predicting health service use in populations, in this analysis we focus on the individual-level factors that may predict Pap test use among SMW (Fig. 1). These individual-level factors include predisposing, enabling, and need-based factors. Predisposing factors include demographics such as age, as well as individual characteristics that reflect larger social structures, such as race, ethnicity, and sexual orientation. Enabling or disabling factors are those that affect an individual's ability to seek specific services and do so comfortably and safely, including income, health insurance status, sexual orientation disclosure to healthcare providers, and experiences of discrimination in healthcare settings. Factors related to need reflect both perceived and evaluated need for a particular healthcare service. Perceived need refers to the perceptions of both individuals and providers, where evaluated need most often refers to a set of relatively objective clinical criteria.33,36
Study aims
Drawing from extant literature and Anderson's Behavioral Model, we aimed to examine the association between pregnancy history and cervical cancer screening among a diverse community sample of SMW of reproductive age (21–45), accounting for potential covariates and confounders, including demographic factors, socioeconomic status, experiences related to sexual minority status, and sexual victimization history.
Methods
Sample and procedures
We conducted a secondary analysis using cross-sectional data from the third wave of the Chicago Health and Life Experiences of Women (CHLEW) Study, collected during 2010–2012. CHLEW is a three-wave, 18-year, longitudinal cohort study of adult SMW in the Chicago area. CHLEW participants were initially recruited in 2000–2001 using a broad range of community-based recruitment techniques. Recruitment targeted cisgender SMW (those whose gender identity aligns with the sex they were assigned at birth)27 who have typically been underrepresented in studies of SMW's health, such as older (>50 years) and younger (<25 years) women, racial and ethnic minorities, and those without a college education. Data were collected by trained interviewers using computer-assisted interview techniques.
Criteria for participation in the baseline (wave 1) survey were at least 18 years old, the ability to read and speak English, and lesbian identity. However, 11 women in the sample subsequently identified as bisexual during the actual interview. At the third wave of data collection (2010–2012), 354 participants (79%) from the baseline sample were reinterviewed. An additional sample of 336 women was also recruited using targeted sampling methods to increase the number of bisexual, racial/ethnic minority, and younger women.37,38 We analyzed data from the third wave of CHLEW as it provided the most recent cervical cancer screening data from the largest and most diverse sample. To focus on participants of potentially reproductive age, women ages 21–45 at the wave 3 interview were included in the current analysis, for a total sample size of 430.
Human subject considerations
The University of Illinois at Chicago's Institutional Review Board approved each wave of the CHLEW study. CHLEW study interviewers were all women who received 20 hours of training on general field-interviewing techniques and potentially sensitive topics such as sexual orientation, violence and victimization, and substance use. Following a review of the purpose and procedures of the study, participants provided informed consent. A distress protocol was in place for any participant who became upset or disturbed during the interview (none did), and every participant was given a referral list for local agencies and hotlines before beginning the interview. The University of Pennsylvania Institutional Review Board approved the current analysis. CHLEW researchers shared deidentified data through e-mail, and data files were subsequently stored in password-protected folders.
Measures
Outcomes
The primary outcome of interest, cervical cancer screening, was defined as a dichotomous measure (yes/no) of past-year Pap testing. We operationalized this variable as participant self-report of a Pap test within the previous year at the third wave of CHLEW data collection (2010–2012). Although annual Pap testing does not reflect current screening guidelines for most women, at the time of interview, American Cancer Society (ACS) consensus guidelines endorsed yearly Pap testing with conventional methods or every 2 years with “liquid-based Pap testing” for all women up to age 30, transitioning to Pap testing every 3 years only after three consecutive normal Pap tests.39
Primary independent variable
The primary predictor of interest was pregnancy history. We defined pregnancy history as participant self-report of ever having been pregnant before the time of interview (yes/no). Based on Andersen's model, we conceptualized pregnancy history as a factor related to perceived need for screening, since healthcare providers are likely to recommend regular screening to a woman who has been pregnant, and cervical cancer screening is a routine part of most prenatal care.
Covariates
Potential covariates included predisposing factors, enabling factors, and need-based factors as described by Andersen's Behavioral Model. Predisposing factors included categorical variables measuring specific sexual orientation (lesbian, bisexual, or other), race/ethnicity (white, Black/African American, Hispanic/Latina, or other), and a continuous age variable. Enabling factors related to economic status included a categorical income measure using income quartiles of the CHLEW sample and a binary measure of health insurance status (any insurance vs. none). We also conceptualized sexual orientation disclosure to providers (whether the participant disclosed to all providers vs. not disclosed to all providers) and participant report of experiencing any form of discrimination in a healthcare setting in the previous year (yes/no) as enabling or disabling factors. Both were measured using dichotomous variables based on participant self-report. Factors related to need for screening included a continuous measure of participants' age at sexual debut, as early sexual debut has been shown to increase sexual and reproductive health risks,40 and a dichotomous measure of history of any sexual victimization, as this would likely increase both perceived and evaluated need for future cancer screening.41 Participants were classified as having experienced sexual victimization if they reported experiencing sexual abuse during childhood or answered “yes” to either of the following questions: “Have you ever been raped, that is, someone had sexual intercourse with you, when you did not want to, by threatening you or using some degree of force?”; “Have you ever experienced any other kind of sexual assault?”
Statistical analyses
Descriptive statistics were generated to characterize the sample. Means and standard deviations (SDs) were used to describe continuous variables. Frequencies and percentages were used to describe dichotomous or categorical variables. Univariate logistic regression models were used to quantify the individual impact of each predictor of interest on the odds of having a Pap test in the past year. Next, a multivariable logistic regression model was generated, including pregnancy history (the primary independent variable), and the other predisposing, enabling, and disabling and need-based factors identified in the theoretical model. Model assumptions, including multicollinearity of independent variables and observation independence, were checked. Statistical significance (α) was set to the 0.05 level. Based on a sample size of 430 we had the ability to detect an odds ratio (OR) of ∼1.79 with 80% power and α set to 0.05. We also conducted post hoc chi-square analyses to test for race/ethnicity differences in health insurance status in the sample. All statistical analyses were accomplished using SAS statistical analysis software Version 9.4 (copyright© 2013; SAS Institute, Inc., Cary, NC).
Results
Table 1 displays the sample characteristics (n = 430). In this sample, approximately 61% of participants reported having no pregnancy history, and 60% of participants reported having a Pap test in the previous year. The mean age of the sample was 32.1 years old (SD = 7.3), and the sample was 33% white, 34% Black/African American, and 27% Hispanic/Latina. Approximately 61% of the sample identified as lesbian, where 30% identified as bisexual and 9% as some other nonheterosexual identity. Notably, only 10% of the sample reported that they had experienced recent discrimination in a healthcare setting.
Table 1.
Distributions of All Study Variables in the Sample (n = 430)
| Variable | n | Percent (%) |
|---|---|---|
| Predisposing factors | ||
| Age | 32.1 (Mean) | 7.3 (SD) |
| Sexual orientation | ||
| Lesbian | 263 | 61.2 |
| Bisexual | 127 | 29.5 |
| Other | 40 | 9.3 |
| Race/ethnicity | ||
| White | 143 | 33.3 |
| Black/African American | 148 | 34.4 |
| Hispanic/Latina | 118 | 27.4 |
| Other | 21 | 4.9 |
| Enabling/disabling factors | ||
| Health insurance status | ||
| No insurance | 144 | 33.5 |
| Any insurance | 286 | 66.5 |
| Income | ||
| $0–$14,999 | 115 | 28.1 |
| $15,000–$39,999 | 103 | 25.1 |
| $40,000–$74,999 | 103 | 25.1 |
| >$75,000 | 89 | 21.7 |
| Out to all healthcare providers | ||
| No | 147 | 34.2 |
| Yes | 283 | 65.8 |
| Discrimination in healthcare | ||
| No | 388 | 90.2 |
| Yes | 42 | 9.8 |
| Need-based factors | ||
| Primary predictor: ever pregnant | ||
| No | 262 | 60.9 |
| Yes | 168 | 39.1 |
| Age at sexual debut | 16.4 (Mean) | 3.5 (SD) |
| Sexual victimization | ||
| No | 191 | 44.4 |
| Yes | 239 | 55.6 |
| Outcome | ||
| Past-year Pap test | ||
| No | 173 | 40.2 |
| Yes | 257 | 59.8 |
SD, standard deviation.
Table 2 displays the odds ratios and 95% confidence intervals from unadjusted and adjusted multivariate regression models. Univariate logistic regression model results demonstrated that pregnancy history was significantly associated with past-year Pap testing (OR = 1.76, 95% confidence interval, CI = [1.17–2.63], p = 0.006). Among the other model-based predictors, only Black/African American identity (OR 1.63, 95% CI = [1.02–2.62], p = 0.042) and bisexual identity (OR 1.60, 95% CI = [1.03–2.49], p = 0.038) compared to white and lesbian identities, respectively, were significantly associated with past-year Pap testing at the p < 0.05 level.
Table 2.
Unadjusted and Adjusted Odds Ratios of Participants Reporting a Pap Test Within the Past Year (n = 430)
| Variable | Unadjusted | 95% CI | Adjusted | 95% CI |
|---|---|---|---|---|
| Predisposing factors | ||||
| Age | 0.975 | 0.949–1.001 | 0.951** | 0.918–0.985 |
| Race/ethnicity | ||||
| White (ref.) | 1.0 | 1.0 | ||
| Black/A.A. | 1.633* | 1.017–2.623 | 1.609 | 0.906–2.858 |
| Hispanic/Latina | 1.215 | 0.742–1.990 | 1.179 | 0.679–2.048 |
| Other | 0.917 | 0.366–2.294 | 0.688 | 0.257–1.841 |
| Sexual orientation | ||||
| Lesbian (ref.) | 1.0 | 1.0 | ||
| Bisexual | 1.597* | 1.026–2.486 | 1.770* | 1.041–3.009 |
| Other | 1.315 | 0.663–2.609 | 1.289 | 0.621–2.676 |
| Enabling/disabling factors | ||||
| Income | ||||
| $0–$14,999 | 1.0 | 1.0 | ||
| $15,000–$39,999 | 0.713 | 0.414–1.227 | 0.843 | 0.471–1.511 |
| $40,000–$74,999 | 0.944 | 0.545–1.637 | 1.160 | 0.610–2.207 |
| >$75,000 | 0.809 | 0.459–1.426 | 1.133 | 0.562–2.286 |
| Health insurance | 1.356 | 0.904–2.035 | 1.614 | 0.983–2.649 |
| Disclosure of SO | 1.231 | 0.821–1.845 | 1.622* | 1.011–2.602 |
| EOD in healthcare | 0.716 | 0.378–1.357 | 0.801 | 0.395–1.622 |
| Need-based factors | ||||
| Ever pregnant | 1.757** | 1.172–2.634 | 1.741* | 1.037–2.923 |
| Age at sexual debut | 0.967 | 0.915–1.022 | 0.986 | 0.928–1.047 |
| Sexual victimization | 1.131 | 0.768–1.667 | 1.030 | 0.662–1.602 |
*p < 0.05; **p < 0.01.
CI, confidence interval; EOD, experiences of discrimination; SO, sexual orientation.
In the multivariate model, the positive association between pregnancy history and past-year Pap testing remained statistically significant. Women who reported having a pregnancy history had a 74% increased odds of a past-year Pap test than women without any pregnancy history (OR 1.74, 95% CI = [1.04–2.92], p = 0.036). Age was negatively associated with past-year Pap testing, with each year of increase in age reflecting a 5% reduction in the odds of reporting a past-year Pap test (OR 0.95, 95% CI = [0.92–0.99], p = 0.005). Bisexual women also had a 77% higher odds of past-year Pap test compared to lesbian-identified women (OR 1.77, 95% CI = [1.04–3.01], p = 0.035). Among the four enabling/disabling factors examined in the model, only disclosure of sexual orientation to healthcare providers was significantly associated with past-year Pap testing. Those who had disclosed their sexual orientation to all their healthcare providers had a 62% higher odds of past-year Pap testing than those who had not (OR 1.62, 95% CI = [1.01–2.60], p = 0.045).
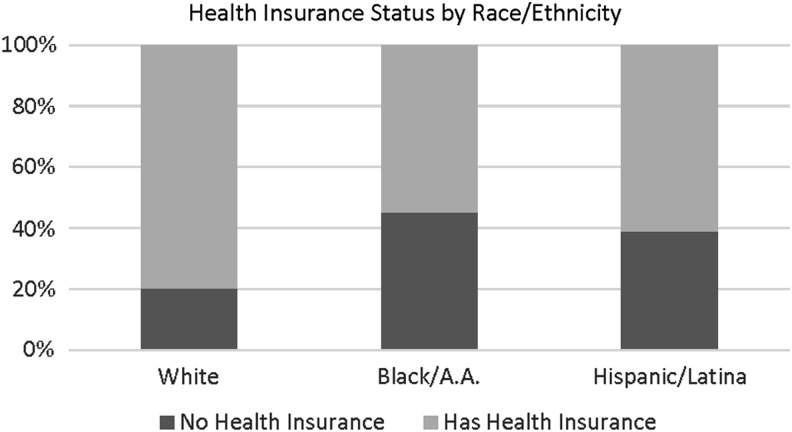
Although health insurance status was only marginally significant in the multivariable model (OR 1.61, 95% CI = [0.98–2.65], p = 0.058), estimated ORs suggest that being insured may also be positively associated with past-year Pap testing. Similarly, the race/ethnicity of participants was not statistically significant in the multivariable model, but OR estimates for past-year Pap testing among Black/African American women were increased compared to white women. Post hoc chi-square analyses of race/ethnicity and health insurance in the sample showed that comparatively more Black/African American participants were uninsured compared to white participants (Fig. 2) (45% vs. 20% uninsured, Wald χ2 21.37, p < 0.001).
FIG. 2.
Participants' health insurance status (any vs. none) by race/ethnicity group, excluding participants in the “other” race group (n = 419, Wald χ2 = 21.37, p < 0.001).
Discussion
Overall, our findings show that pregnancy history was positively associated with past-year Pap testing among SMW who are of reproductive age. Indeed, the magnitude of the OR estimate for pregnancy history remained stable even when controlling for many other factors likely to influence Pap testing uptake among SMW, including demographic factors, income and health insurance status, previous experiences of discrimination in healthcare, and history of victimization. These findings suggest preliminary evidence that SMW who have not been pregnant may be at higher risk of missing cervical cancer screening and that pregnancy-related experiences may be important “cues to screening” among SMW. SMW who have been pregnant may be more likely to think of themselves as at risk for HPV and cervical cancer. Pregnancy-related healthcare encounters may also serve as entry to the healthcare system for some SMW and thereby act as a cue to other types of preventive healthcare as well.
In addition, providers may be more likely to recommend and provide cervical cancer screening to SMW who report a previous pregnancy. Provider recommendations for Pap tests have been found to be important predictors of Pap test utilization.42 Congruent with other recent findings in studies of SMW's use of cervical cancer screening services,22,43 our findings also suggest an important relationship between disclosure of sexual orientation to providers and past-year Pap testing. This may similarly reflect the impact of communication on screening service utilization. It is unlikely that this reflects a causal relationship, where disclosure of minority sexual identity leads providers to recommend Pap testing. Instead, it likely reflects that SMW who perceive safety in disclosing sexual identity and sexual history to providers are more likely to receive evidence-based preventive care overall, including Pap testing. Of note, provider gender has been found to be associated with Pap testing among the general population of women (i.e., female healthcare providers report performing more Pap tests than male providers).4 Investigators explain this difference as a reflection of increased comfort and patient–provider communication among female patients, and this may particularly impact SMW. Healthcare providers should be aware that SMW are at risk for cervical cancer and need to be screened, regardless of pregnancy or other reproductive health history.
We did not find statistically significant differences across race/ethnicity groups in odds of cervical cancer screening. However, racial/ethnic minority SMW, specifically Black/African American SMW, were more likely to report past-year Pap testing than were white SMW in the unadjusted model. Previous studies of the general population have found that Black women are more likely than white women to report cervical cancer screening.4,44 This may be evidence of a “reverse disparity,” an instance in which an otherwise marginalized group seems to receive better care or have better health outcomes than the dominant group, but may still be subject to unconscious bias or discrimination. Similar reverse disparities have been documented among patients with end-stage renal disease, in which African American patients seem to have better survival rates, and among those with major depressive disorder, where racial and ethnic minorities seem to bear lower disease burden than whites.45–47 In this case, increased rates of sexual health screening among racial and ethnic minorities may reflect providers' assumptions about the sexual orientation or sexual behaviors of their patients based on their race or ethnicity. Various studies have demonstrated that unconscious racial bias influences providers' assumptions about the number of sex partners patients have, as well as the provider's willingness to prescribe preventive sexual health treatment.48,49 Providers' assumptions about sexual risk and therefore indications for cervical cancer screening may be different about African American SMW from those about white SMW. Alternatively, these differences may be a reflection of differences in health seeking behavior, driven by community-based norms around screening or other factors.6–9
Similarly, we did not find a statistically significant relationship between health insurance status and Pap testing among SMW in this sample. Federal Title X funding has made low- and no-cost cervical cancer screening available to many women. Increased funding for and awareness of these programs may increase screening rates among populations who are under- or uninsured.50 In addition, the presence of multiple clinics that target sexual and gender minority populations in the region where participants were recruited may increase the availability of free or low-cost Pap testing for uninsured women. These programs are funded, in part, by government initiatives and can mitigate the impact of racial and class disparities in health insurance status.51 However, much previous research has described how race, socioeconomic status, and gender all intersect and relate to insurance status in the United States, and there are likely to be multiple important interactions between these variables among SMW specifically.52,53 This is demonstrated by our post hoc analysis of the racial/ethnic identity and insurance status of the sample, which demonstrated significant differences in insurance rates among white, Black/African American, and Hispanic/Latina groups (Fig. 2). This finding illustrates that multiple intersecting relationships between predisposing, enabling, and need-based factors are likely to act in this population. Due to our sample size, we were not able to empirically test for these interactions.
Our findings confirm that SMW are not a homogenous group in terms of sexual and reproductive health and healthcare experiences. Mitigating misunderstandings about the risks of cervical cancer among SMW may be an important target of public health campaigns and healthcare provider education.
Study limitations
The findings of this study should be interpreted in light of the following limitations. First, our analysis tested for associations between pregnancy history and cervical cancer screening and was not able to determine causal relationships. Second, our analysis used cross-sectional data and therefore did not account for how the tested relationship may change over time. For example, we measured pregnancy history over the life span but only the most recent (past-year) potential Pap test. A woman receiving pregnancy-related care is likely to discuss Pap testing during prenatal care and may be more motivated to return for a certain number of repeat Pap tests, but that impact may not last over the entire age span reflected in the recommendations for Pap testing (21–65). We focused on participants' last Pap test although the benefit of Pap testing as preventive care is largely through regular, repeat testing over time. There may also be instances in which a reported pregnancy occurred within the past year after the reported Pap test. Some covariates included in this analysis such as experiences of discrimination also occur variably over the life span and we were therefore not able to capture a complete picture of their effect on SMW's use of Pap testing.
In addition, our measure of pregnancy history was binary and did not account for nuanced reproductive health history data such as gravida and parity or pregnancy outcomes. We were also unable to include other aspects of obstetric and gynecological history such as whether pregnancies were planned or desired, whether participants had received Gardasil®, the vaccine that prevents many types of HPV, or whether participants had been diagnosed with other gynecologic conditions. These aspects of women's obstetric and gynecological history are likely to impact their experiences with sexual and reproductive healthcare and therefore their likelihood of receiving cervical cancer screening.
Conclusions and Recommendations
Despite limitations, this analysis provides preliminary evidence that pregnancy history may be significantly associated with SMW's use of Pap testing. Recommendations for both clinicians and investigators can be drawn from these findings. First, health professional schools and clinical institutions should ensure that all healthcare providers are trained to recommend and provide comprehensive cancer screening for SMW. According to recent studies, medical and nursing schools currently place little emphasis on sexual or gender minority health.54,55 Therefore, practicing clinicians must learn best practices for caring for SMW and other sexual minority populations by independently seeking out relevant resources that confirm that all persons with a cervix should be screened for cervical cancer. In addition, findings from this study suggest that providers may only recommend cervical cancer screening at visits directly related to reproductive health (such as pregnancy-related visits). Since SMW may be less likely to need or use some reproductive health services, providers should also discuss and encourage cervical cancer screening at a wider variety of clinical encounters. Tools such as electronic health records have the potential to increase screening by generating automated reminders for clinicians and patients about their next recommended screening. This may be increasingly important under the most current screening guidelines, which lengthen the time between recommended Papanicolaou tests for most people.39
Future studies using longitudinal data are needed to understand the complex associations between obstetric history and cervical cancer screening in the context of SMW's lives. Importantly, more complete reproductive health history data such as pregnancy outcomes, plannedness of pregnancies, diagnosis of reproductive illnesses or conditions, and contraceptive use will be important to illuminate which specific aspects of health history support or limit screening uptake. In addition, the quality and experience of sexual and reproductive healthcare encounters also likely influence whether an individual will return for routine preventive care.
Future research should also investigate SMW's choices about where to seek healthcare. Some sexual minority communities have lower access to healthcare that is safe and affirming. Others, specifically those who reside in urban environments, may seek care at clinics that specifically cater to sexual and gender minority populations where providers may be more comfortable initiating discussions about sexual identity and behavior and more knowledgeable about SMW's risks and screening needs. Discussing sexual health and planning for disease prevention may be different experiences for SMW at these clinics than in other primary or reproductive healthcare settings.
Finally, future analyses should also test the moderating effect of age, race/ethnicity, and other demographic factors on the relationship between pregnancy history and cervical cancer screening. Investigators can use frameworks that explore the various ways multiple marginalized identities and overlapping systems of oppression can ultimately impact the health of SMW, such as Intersectionality Theory. To develop more nuanced understandings of the health and healthcare utilization of SMW, research must begin to conceptualize sexual orientation as one of many intersecting components of individuals' lives that may influence their use of preventive healthcare.
Acknowledgments
The authors acknowledge Kelly Martin at the University of Illinois at Chicago and Dr. Cindy Veldhuis at Columbia University for their expertise and assistance with the CHLEW data set and relevant variables. The first author was supported by a National Institute of Nursing Training Grant (T32 NR007100, PI: M.S.S.; Medoff-Cooper, B.) for Research on Vulnerable Women, Children and Families while conducting the review. This research was also supported by the National Institutes of Health under Ruth L. Kirschstein National Research Service Award (T32HD049302, PI: Ehrenthal, D.) from the National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. NIH. Cervical Cancer Fact Sheet. National Institutes of Health, 1996. Available at: https://report.nih.gov/nihfactsheets/Pdfs/CervicalCancer(NCI).pdf Updated October 2010. Accessed July7, 2018
- 2. United States Cancer Statistics Working Group. United States cancer statistics: 1999–2014 incidence and mortality web-based report. Atlanta, GA: Centers for Disease Control and Prevention and National Cancer Institute; Updated 2017. Available at: https://gis.cdc.gov/grasp/USCS/DataViz.html [Google Scholar]
- 3. Beavis AL, Gravitt PE, Rositch AF. Hysterectomy-corrected cervical cancer mortality rates reveal a larger racial disparity in the United States. Cancer 2017;123:1044–1050 [DOI] [PubMed] [Google Scholar]
- 4. Newmann SJ, Garner EO. Social inequities along the cervical cancer continuum: A structured review. Cancer Causes Control 2005;16:63–70 [DOI] [PubMed] [Google Scholar]
- 5. USPSTF. Final recommendation statement: Cervical cancer: Screening, March 2012. U.S. Preventative Services Task Force, 2012. Available at: www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening Accessed June1, 2018
- 6. Eaton L, Kalichman S, Cain D, et al. Perceived prevalence and risks for human papillomavirus (HPV) infection among women who have sex with women. J Womens Health 2008;17:75–83 [DOI] [PubMed] [Google Scholar]
- 7. Tracy JK, Lydecker AD, Ireland L. Barriers to cervical cancer screening among lesbians. J Womens Health 2010;19:229–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tracy JK, Schluterman NH, Greenberg DR. Understanding cervical cancer screening among lesbians: A national survey. BMC public health 2013;13:442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Charlton BM, Corliss HL, Missmer SA, et al. Influence of hormonal contraceptive use and health beliefs on sexual orientation disparities in Papanicolaou test use. Am J Public Health 2014;104:319–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Diamant AL, Schuster MA, McGuigan K, Lever J. Lesbians' sexual history with men: Implications for taking a sexual history. Arch Intern Med 1999;159:2730–2736 [DOI] [PubMed] [Google Scholar]
- 11. Mustanski B, Birkett M, Greene GJ, Rosario M, Bostwick W, Everett BG. The association between sexual orientation identity and behavior across race/ethnicity, sex, and age in a probability sample of high school students. Am J Public Health 2013;104:237–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Anderson TA, Schick V, Herbenick D, Dodge B, Fortenberry JD. A study of human papillomavirus on vaginally inserted sex toys, before and after cleaning, among women who have sex with women and men. Sex Transm Infect 2014;90:529–531 [DOI] [PubMed] [Google Scholar]
- 13. Moszynski P. Cervical cancer virus can be transmitted through same sex relationships, report warns. BMJ 2009;339:b5667. [DOI] [PubMed] [Google Scholar]
- 14. Brown JP, Tracy JK. Lesbians and cancer: An overlooked health disparity. Cancer Causes Control 2008;19:1009–1020 [DOI] [PubMed] [Google Scholar]
- 15. Agénor M, Krieger N, Austin SB, Haneuse S, Gottlieb BR. At the intersection of sexual orientation, race/ethnicity, and cervical cancer screening: Assessing Pap test use disparities by sex of sexual partners among black, Latina, and white US women. Soc Sci Med 2014;116:110–118 [DOI] [PubMed] [Google Scholar]
- 16. Charlton BM, Corliss HL, Missmer SA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and young adult females. J Adolesc Health 2011;49:505–510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. National Academy of Medicine. Health of lesbian, gay, bisexual, and transgender populations. Lancet 2011;377:1211. [DOI] [PubMed] [Google Scholar]
- 18. Agénor M, Krieger N, Austin SB, Haneuse S, Gottlieb BR. Sexual orientation disparities in Papanicolaou test use among US women: The role of sexual and reproductive health services. Am J Public Health 2014;104:e68–e73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bauer GR, Welles SL. Beyond assumptions of negligible risk: Sexually transmitted diseases and women who have sex with women. Am J Public Health 2001;91:1282–1286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McCauley HL, Silverman JG, Decker MR, et al. Sexual and reproductive health indicators and intimate partner violence victimization among female family planning clinic patients who have sex with women and men. J Womens Health 2015;24:621–628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mullinax M, Schick V, Rosenberg J, Herbenick D, Reece M. Screening for sexually transmitted infections (STIs) among a heterogeneous group of WSW(M). Int J Sex Health 2016;28:9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Reiter PL, McRee AL. Cervical cancer screening (Pap testing) behaviours and acceptability of human papillomavirus self-testing among lesbian and bisexual women aged 21–26 years in the USA. J Fam Plann Reprod Health Care 2015;41:259–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Johnson MJ, Mueller M, Eliason MJ, Stuart G, Nemeth LS. Quantitative and mixed analyses to identify factors that affect cervical cancer screening uptake among lesbian and bisexual women and transgender men. J Clin Nurs 2016;25:3628–3642 [DOI] [PubMed] [Google Scholar]
- 24. Agénor M, Austin SB, Kort D, Austin EL, Muzny CA. Sexual orientation and sexual and reproductive health among african american sexual minority women in the U.S. South. Womens Health Issues 2016;26:612–621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bos HM, van Balen F, van den Boom DC. Planned lesbian families: Their desire and motivation to have children. Hum Reprod 2003;18:2216–2224 [DOI] [PubMed] [Google Scholar]
- 26. Marina S, Marina D, Marina F, Fosas N, Galiana N, Jove I. Sharing motherhood: Biological lesbian co-mothers, a new IVF indication. Hum Reprod 2010;25:938–941 [DOI] [PubMed] [Google Scholar]
- 27. Fenway Health. Glossary of gender and transgender terms. Updated 2010. Available at: http://fenwayhealth.org/documents/the-fenway-institute/handouts/Handout_7-C_Glossary_of_Gender_and_Transgender_Terms__fi.pdf Accessed June1, 2018
- 28. Diamant AL, Schuster MA, Lever J. Receipt of preventive health care services by lesbians. Am J Prev Med 2000;19:141–148 [DOI] [PubMed] [Google Scholar]
- 29. Matthews AK, Brandenburg DL, Johnson TP, Hughes TL. Correlates of underutilization of gynecological cancer screening among lesbian and heterosexual women. Prev Med 2004;38:105–113 [DOI] [PubMed] [Google Scholar]
- 30. Marrazzo JM, Koutsky LA, Kiviat NB, Kuypers JM, Stine K. Papanicolaou test screening and prevalence of genital human papillomavirus among women who have sex with women. Am J Public Health 2001;91:947–952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Agénor M, Bailey Z, Krieger N, Austin SB, Gottlieb BR. Exploring the cervical cancer screening experiences of black lesbian, bisexual, and queer women: The role of patient-provider communication. Women Health 2015;55:717–736 [DOI] [PubMed] [Google Scholar]
- 32. Clark MA, Bonacore L, Wright SJ, Armstrong G, Rakowski W. The cancer screening project for women: Experiences of women who partner with women and women who partner with men. Women Health 2003;38:19–33 [DOI] [PubMed] [Google Scholar]
- 33. Andersen RM. National health surveys and the behavioral model of health services use. Med Care 2008;46:647–653 [DOI] [PubMed] [Google Scholar]
- 34. Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: Application to medical care use and outcomes for homeless people. Health Serv Res 2000;34:1273–1302 [PMC free article] [PubMed] [Google Scholar]
- 35. Baldwin AM, Dodge B, Schick V, Sanders SA, Fortenberry JD. Sexual minority women's satisfaction with health care providers and state-level structural support: investigating the impact of lesbian, gay, bisexual, and transgender nondiscrimination legislation. Womens Health Issues 2017;27:271–278 [DOI] [PubMed] [Google Scholar]
- 36. Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav 1995;36:1–10 [PubMed] [Google Scholar]
- 37. Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems 1997;44:174–199 [Google Scholar]
- 38. Heckathorn DD. Respondent-driven sampling II: Deriving valid population estimates from chain-referral samples of hidden populations. Social Problems 2002;49:11–34 [Google Scholar]
- 39. The American Cancer Society Medical and Editorial Content Team. History of ACS recommendations for the early detection of cancer in people without symptoms. American Cancer Society. Updated 2015. Available at: www.cancer.org/health-care-professionals/american-cancer-society-prevention-early-detection-guidelines/overview/chronological-history-of-acs-recommendations.html Accessed June1, 2018
- 40. Haydon AA, Herring AH, Halpern CT. Associations between patterns of emerging sexual behavior and young adult reproductive health. Perspect Sex Reprod Health 2012;44:218–227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hsieh H-F, Heinze JE, Lang I, Mistry R, Buu A, Zimmerman MA. Violence victimization, social support, and Papanicolaou smear outcomes: A longitudinal study from adolescence to young adulthood. J Womens Health 2017;26:1340–1349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Plourde N, Brown HK, Vigod S, Cobigo V. Contextual factors associated with uptake of breast and cervical cancer screening: A systematic review of the literature. Women Health 2016;56:906–925 [DOI] [PubMed] [Google Scholar]
- 43. Youatt EJ, Harris LH, Harper GW, Janz NK, Bauermeister JA. Sexual health care services among young adult sexual minority women. Sex Res Social Policy 2017:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Miles-Richardson S, Allen S, Claridy MD, Booker EA, Gerbi G. Factors associated with self-reported cervical cancer screening among women aged 18 years and older in the United States. J Community Health 2017;42:72–77 [DOI] [PubMed] [Google Scholar]
- 45. Gurmankin AD, Polsky D, Volpp KG. Accounting for apparent “reverse” racial disparities in Department of Veterans Affairs (VA)-based medical care: Influence of out-of-VA care. Am J Public Health 2004;94:2076–2078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Newsome BB, McClellan WM, Coffey CS, Allison JJ, Kiefe CI, Warnock DG. Survival advantage of black patients with kidney disease after acute myocardial infarction. Clin J Am Soc Nephrol 2006;1:993–999 [DOI] [PubMed] [Google Scholar]
- 47. Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch Gen Psychiatry 2007;64:305–315 [DOI] [PubMed] [Google Scholar]
- 48. Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): Assumptions about sexual risk compensation and implications for access. AIDS Behav 2014;18:226–240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Thorburn S, Bogart LM. African American women and family planning services: Perceptions of discrimination. Women Health 2005;42:23–39 [DOI] [PubMed] [Google Scholar]
- 50. U.S. Department of Health and Human Services. About Title X Grants. U.S. Department of Health and Human Services, Office of Population Affairs. Updated 2017. Available at: www.hhs.gov/opa/title-x-family-planning/about-title-x-grants/index.html Accessed June1, 2018
- 51. CDC. STD AAPPS FOA Fact Sheet. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Updated 2013. Available at: www.cdc.gov/std/foa/aapps/factsheet.htm Accessed June1, 2018
- 52. Gonzales G, Ortiz K. Health insurance disparities among racial/ethnic minorities in same-sex relationships: An intersectional approach. Am J Public Health 2015;105:1106–1113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gonzales G, Blewett LA. National and state-specific health insurance disparities for adults in same-sex relationships. Am J Public Health 2014;104:e95–e104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA 2011;306:971–977 [DOI] [PubMed] [Google Scholar]
- 55. Lim F, Johnson M, Eliason M. A National Survey of Faculty Knowledge, Experience, and Readiness for Teaching Lesbian, Gay, Bisexual, and Transgender Health in Baccalaureate Nursing Programs. Nurs Educ Perspect 2015;36:144–152 [Google Scholar]