Abstract
Introduction: Little is known about how exposure to adverse childhood experiences (ACEs) and protective factors, such as resilience, influence prenatal mental and behavioral health. This study examined associations between exposure to ACEs and mental and behavioral health during pregnancy overall and among women with high versus low levels of resilience.
Materials and Methods: Women in two Kaiser Permanente Northern California medical centers were screened for ACEs and resilience during prenatal care (∼14–23 weeks of gestation; N = 355). Multivariable logistic regression analyses examined associations between ACEs and prenatal mental and behavioral health conditions overall and for women with low (≤32) versus high (>32) resilience on the 10-item Connor-Davidson Resilience Scale.
Results: Overall, 54% of women reported 0 ACEs, 28% 1–2 ACEs, and 18% 3+ ACEs. Relative to women with 0 ACEs, those with 1–2 ACEs had higher odds of an anxiety or depressive disorder and intimate partner violence (IPV) (odds ratios [ORs] 2.42–3.12, p < 0.05), and those with 3+ ACEs had higher odds of an anxiety or depressive disorder, depression symptoms, and IPV (ORs 3.08–4.71, p < 0.05). In stratified analyses by high (56%) and low (44%) resilience, having one or more ACEs (vs. 0 ACEs) was only associated with worse mental and behavioral health in women with low resilience.
Conclusions: ACEs predicted mental and behavioral health conditions among pregnant women, and associations were the strongest among women with low levels of current resilience. Longitudinal research is needed to understand the causal mechanisms underlying these associations.
Keywords: adverse childhood experiences, mental health, pregnancy, intimate partner violence, resilience
Introduction
Adverse childhood experiences (ACEs), defined as physical, sexual, or emotional abuse, neglect, parental loss, or family dysfunction before the age of 18, are common,1 with approximately two-thirds of adults in the United States experiencing at least one form of ACE.2 There is a strong dose–response relationship between exposure to ACEs and poor health outcomes, including depression, anxiety, substance use, sexually transmitted diseases, suicide attempts, and a range of chronic diseases.2–10 These health risks are compounded by continued stressful experiences such as intimate partner violence (IPV) in adulthood.11–17
Less studied but of great interest is the potential impact of ACEs on maternal health outcomes during pregnancy. A small but growing body of literature suggests that ACEs are associated with increased mental health risks during pregnancy, including higher depressive symptoms,18–21 anxiety,22,23 suicidality,24,25 and substance use.20,26–28 In addition, a history of ACE exposure is associated with higher rates of psychosocial difficulties29 and IPV in pregnancy,20,30–32 which contribute to poor mental health outcomes. ACE-related mental and behavioral health conditions are associated with both adverse pregnancy outcomes and poorer child health,33–44 making it critically important to understand and reduce the risk of developing these conditions.
Although the literature on the health impacts of ACEs is robust, studies have generally omitted protective and positive factors, such as resilience, even though evidence suggests that they can influence the impact of ACEs on an individual.45 Resilience reflects one's adaptive ability to cope with adversity, bounce back after hardship, handle unpleasant feelings, and adapt to change,46,47 Resilience may modify the impact of ACE exposure by encouraging the use of healthy, rather than maladaptive, coping strategies, promoting self-esteem, and from internal capabilities or environmental resources.48,49 Researchers have recently called for the inclusion of strength-based questions in studies of ACEs to better understand whether and how protective factors reduce the negative impact of ACEs on health and functioning.45 To address this gap in knowledge, several recent studies have investigated the potential protective role of resilience in adulthood on mental and behavioral health outcomes.50–53 The majority of these studies have found evidence consistent with a buffering effect of resilience on the association between ACEs and psychological distress,54,55 depression,50,51,56 emotion dysregulation,52 and substance use.57 However, one study found that although resilience moderated the association between adult trauma exposure and depression, it did not moderate the association between ACEs and depression.53
To our knowledge, only one study to date has examined whether the relationship between ACEs and mental and behavioral health during pregnancy or the postpartum period varies with resilience. Sexton et al. found that resilience moderated associations between ACEs and postpartum major depressive disorder and posttraumatic stress disorder in a sample of 214 mothers, such that risk for these conditions was the highest among women who had a combination of both ACEs and low resilience.58 Given the deleterious consequences of mental and behavioral health conditions during pregnancy on mothers and their babies, it is critical to examine whether resilience buffers the negative impacts of ACEs on prenatal mental and behavioral health.
In this study, we examined the hypothesis that ACEs would be associated with mental and behavioral health conditions during pregnancy, including anxiety, depression, substance use, and exposure to IPV. In addition, we conducted stratified analyses for pregnant women with high versus low levels of resilience to test the hypothesis that associations between ACEs and mental and behavioral health conditions would be stronger for women with low versus high levels of resilience. To our knowledge, this is the first study to examine how ACEs and resilience combine to influence a range of mental and behavioral health outcomes during pregnancy.
Materials and Methods
Study site
Kaiser Permanente Northern California (KPNC) is a nonprofit, integrated healthcare delivery system that insures >40% of the Northern California region's commercially insured population and provides health services to >4 million members.59 KPNC has >40,000 pregnancies each year across 15 medical centers. KPNC patients are diverse and generally representative of the northern California population.60
From March 1, 2016 to June 30, 2016, KPNC implemented a pilot program to screen English-speaking women aged ≥18 for ACEs and resilience at their second or third prenatal visit (between 16 and 23 weeks gestation) as part of standard prenatal care in two KPNC medical centers. All patients who met the criteria described earlier were included in the study. Patients completed the ACEs and resilience questionnaires in the exam room. Clinicians reviewed the questionnaires with patients and provided resources, including an educational handout with relevant classes, support groups, books, videos and community resources, and referrals as needed. Additional details on study materials and methods have been previously published.61
Participants
Three-hundred fifty-five English-speaking women completed the ACEs and resilience questionnaires during the 4-month study period. As previously reported, 50 women (12%) who were offered but did not complete the ACE/resilience questionnaire were not significantly different from those who did complete the questionnaire on demographics, with the exception that they were more likely to be of “Other” or “Unknown” race/ethnicity.61 This study was approved by the KPNC Institutional Review Board.
Measures
We used a modified version of the 11-item Behavioral Risk Factor Surveillance System Questionnaire62 to assess eight ACE exposures before age 18. The modified version was developed for easier self-administration in a healthcare setting and to be appropriate for prenatal patients. Questions are presented in Table 1. Response options were yes or no; possible ACE scores ranged from 0 to 8. Given that ACEs are highly interrelated,63 and the cumulative impact may be stronger than the impact of individual ACEs, we categorized ACEs into three categories for this study (0, 1–2, 3+) as done in our prior work with prenatal patients.61 For stratified analyses by resilience, we combined 1–2 and 3+ ACEs and examined 0 versus 1+ ACEs to increase power for analyses among the smaller stratified populations. Studies suggest that exposure to one or more ACEs increases health risk, suggesting this stratification is clinically relevant.64,65 We also ran stratified analyses by resilience with 0–1 ACEs versus 2+ ACEs and the pattern of results was similar (not shown).
Table 1.
Prevalence of Adverse Childhood Experiences Among Pregnant Women (N = 355)
| Individual ACEs | |
|---|---|
| Before your 18th birthday: | % |
| Did you lose a parent through divorce, abandonment, death, or other reason? | 27 |
| Did a parent or adult in your home ever swear at you, insult you, or put you down? | 19 |
| Did you live with anyone who was a problem drinker, alcoholic or who used street drugs? | 19 |
| Did you have someone in your household who was depressed, mentally ill or attempted suicide? | 16 |
| Not including spanking, did a parent or adult in your home ever hit, beat, kick, or physically hurt you in any way? | 9 |
| Did you have a member of your household who went to prison? | 9 |
| Did your parents or adults in your home ever hit, punch, or beat each other up? | 8 |
| Did you experience sexual abuse by an adult or person at least 5 years older? | 8 |
| Number of ACEs | |
| 0 | 54 |
| 1 | 18 |
| 2 | 10 |
| 3+ | 18 |
ACE, adverse childhood experience.
The 10-item Connor-Davidson Resilience Scale (CD-RISC 10) is a widely used, validated, self-reported measure of core aspects of past-month psychological resilience (e.g., ability to bounce back after hardship, handle unpleasant or painful feelings, ability to adapt to change, see the humorous side of problems) that has been used in prior research with prenatal and postpartum patients.61,66 Answer options range from “not at all true” (0) to “true nearly all the time” (4), with higher scores indicating higher resilience, and total scores ranging from 0 to 40.58,67 We utilized the CD-RISC 10 in this study and dichotomized resilience based on the national average (low ≤32 and high >32).66
Diagnoses of anxiety and depressive disorders diagnosed during pregnancy were extracted from the electronic health record (EHR) by using International Classification of Diseases (ICD)-9 or ICD-10 codes (Supplementary Table S1).
Depression symptoms were based on the Patient Health Questionnaire (PHQ-9),68 which is given during pregnancy as part of standard prenatal care (<5 none, 5–9 mild depression, 10+ moderate/severe depression). Scores range from 0 to 27 and were dichotomized into no depression (<5) versus mild, moderate, or severe depression (≥5) to include subclinical levels of depression symptoms and supplement data on depressive disorder diagnoses. Of the 355 women in this study, 63 women (17.7%) were missing a PHQ-9 score. Missing a PHQ-9 score was not significantly associated with ACEs or any demographic characteristics.
Exposure to IPV was based on either (i) an ICD-9 or ICD-10 diagnosis of IPV within 1 year of the ACEs screening (Supplementary Table S1) or (ii) self-reported exposure to IPV as part of routine prenatal screening. Women with an IPV diagnosis during pregnancy (which could include a history of IPV) or endorsement of IPV during routine screening in prenatal care were coded as positive for IPV.
KPNC pregnant women are routinely screened for prenatal alcohol and marijuana use as standard part of entry to prenatal care, via both self-report on a prenatal substance use screening questionnaire and toxicology testing (typically between 6 and 13 weeks gestation). Prenatal alcohol and marijuana use were defined as self-reported use of any amount alcohol or marijuana since pregnancy or a positive toxicology test for alcohol or cannabis as part of standard prenatal substance use screening.
Smoking status is routinely asked about and documented in the EHR for all pregnant patients. We obtained patient-reported smoking status (i.e., current, former, or never-smoker) from the EHR at the time of the ACEs screening.69 Prior studies support the validity of EHR-based smoking status data.70–72
Demographic characteristics for each patient were collected from the EHR and include patient age at screening, race/ethnicity (non-Hispanic white, Asian/Pacific Islander, Black, Hispanic, Other/unknown), and neighborhood median income.
Analyses
All statistical analyses were performed in SAS 9.3. Data were assessed for normality, and non-parametric tests were used for non-normally distributed variables. Descriptive statistics were used to describe the prevalence of each ACE category (0, 1–2, 3+) and the mean number of ACEs. Demographic and mental and behavioral health conditions were calculated for the sample overall and by ACE category. Chi-square tests were used to examine whether demographic and mental and behavioral health variables differed by ACE category. A non-parametric Kruskal–Wallis test was used to test whether age differed by ACE category. Multivariable logistic regression models were run to calculate the odds of mental and behavioral health conditions during pregnancy by ACE category, adjusting for age, race, and median neighborhood income. For multivariable analyses, we combined individual types of prenatal substance use into an overall substance use variable.
Next, we calculated the prevalence of mental and behavioral health conditions by ACE category separately for women with low and high levels of resilience. Stratified multivariable logistic regression analysis was used to calculate the odds of mental and behavioral health conditions during pregnancy by ACE category, adjusting for age, race, and median neighborhood income, separately for women with high and low resilience. All stratified analyses used a dichotomous measure of ACEs (0 vs. 1+) to increase power for analyses among the smaller stratified populations.
Results
The sample of 355 women was 41.4% White, 25.9% Hispanic, 16.3% Black, 13.5% Asian/Pacific Islander, and 2.8% Other; 8.2% had a neighborhood median income <$40,000, 34.8% had a neighborhood median income of $40,000–$79,999, 44.5% had a neighborhood median income of $80,000–109,000, and 12.5% had a neighborhood median income >$110,000. The median age was 30 (Interquartile range [IQR]: 22–38).
The prevalence of each ACE is presented in Table 1. The most common ACEs reported were “losing a parent through divorce, abandonment, death or other reason” (27%), “being verbally put down by a parent or adult” (19%), and “living with someone with a drinking or drug problem” (19%). A total of 193 (54%) women reported 0 ACEs, 99 (28%) women reported 1 or 2 ACEs, and 63 (18%) women reported 3+ ACEs. Women with 0, 1–2, and 3+ ACEs were not significantly different on race/ethnicity, neighborhood median income, or age. The median and mean ACEs scores were 0 (IQR: 0–1) and 1 (standard deviation = 1.6), respectively.
The median resilience score was 34 (IQR: 29–37), and 44% had low resilience based on a score at or below the national average of 32. Women with low resilience (≤32) and high resilience (>32) did not differ significantly on mean number of ACEs, race/ethnicity, neighborhood median income, or age.
Overall, 11.6% of the sample had an anxiety disorder, 9.9% had a depressive disorder, 27.4% had any self-reported current depression symptoms, and 7.6% had an IPV diagnosis during this pregnancy or in the previous 12 months. In terms of prenatal substance use, 7.6% screened positive for any alcohol use, 9.8% screened positive for any marijuana use, 1.4% were current smokers, and 17% screened positive for any of the three substances.
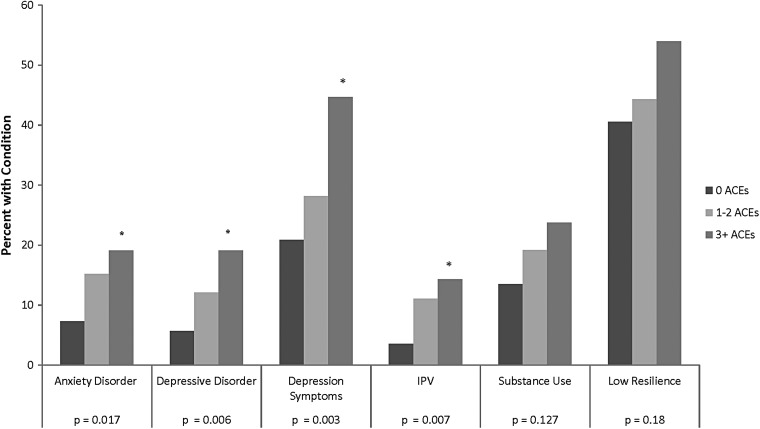
Chi-square analyses indicated that ACEs were associated with an increased likelihood of having an anxiety disorder (p = 0.017), depressive disorder (p = 0.006), any depression symptoms (p = 0.003), experiencing IPV (p = 0.007), and cigarette smoking (p = 0.043) (Fig. 1). Use of alcohol, marijuana, overall substance use, and low resilience did not differ significantly by ACEs, but did follow the same trend as the other mental and behavioral health conditions.
FIG. 1.
Prevalence of mental and behavioral health conditions among pregnant women by ACEs. Depressive symptoms are based on the Patient Health Questionnaire-9 survey routinely given during the first trimester of prenatal care. IPV includes a diagnosis of IPV in the EHR in the year before or during pregnancy or endorsing any of the three questions related to IPV at the beginning of prenatal care. Low resilience is based on a score below the national average (≤32) on the Connor-Davidson RISC-10 Resilience questionnaire given at the time of ACE screening. *Significant at p < 0.05. ACE, adverse childhood experience; EHR, electronic health record; IPV, intimate partner violence.
Results from multivariable models examining associations between ACEs and prenatal mental and behavioral health adjusting for age, race/ethnicity, and median neighborhood income found a graded relationship between ACEs and several mental and behavioral health outcomes (Table 2). Women with 1–2 ACEs had significantly increased odds of an anxiety disorder (OR = 2.42, 95% confidence interval [CI] = 1.09–5.41), depressive disorder (OR = 2.49, 95% CI = 1.03–6.00), and IPV (OR = 3.12, 95% CI = 1.13–8.61) relative to those with 0 ACEs. Women with 3+ ACEs had significantly increased odds of an anxiety disorder (OR = 3.08, 95% CI = 1.28–7.39), depressive disorder (OR = 3.98, 95% CI = 1.60–9.90), depressive symptoms (OR = 3.13, 95% CI = 1.58–6.17), and IPV (OR = 4.71, 95% CI = 1.59–13.95) relative to those with 0 ACEs. Increased odds for all outcomes were larger for the 3+ versus 0 ACEs comparison relative to the 1–2 ACEs versus 0 ACEs comparison, indicative of a cumulative effect of ACEs. The ACEs were not significantly associated with prenatal substance use or low resilience.
Table 2.
Multivariable Models of Odds of Mental and Behavioral Health Conditions by Adverse Childhood Experiences Among Pregnant Women (N = 355)
| 0 ACEs% | 1–2 ACEs% | 3+ ACEs% | 1–2 ACEs vs. 0 | 3+ ACEs vs. 0 | |||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||||
| Condition | |||||||
| Anxiety disorder | 7.3 | 15.2 | 19.1 | 2.42 (1.09–5.41) | 0.031 | 3.08 (1.28–7.39) | 0.012 |
| Depressive disorder | 5.7 | 12.1 | 19.1 | 2.49 (1.03–6.00) | 0.043 | 3.98 (1.60–9.90) | 0.003 |
| Any depression symptoms | 20.9 | 28.2 | 44.6 | 1.46 (0.77–2.77) | 0.251 | 3.13 (1.58–6.17) | 0.001 |
| Intimate partner violence | 3.6 | 11.1 | 14.3 | 3.12 (1.13–8.61) | 0.028 | 4.71 (1.59–13.95) | 0.005 |
| Prenatal substance use | 13.7 | 19.6 | 25.0 | 1.53 (0.77–3.04) | 0.222 | 1.93 (0.91–4.12) | 0.088 |
| Low resilience | 40.6 | 44.4 | 54.0 | 1.16 (0.70–1.92) | 0.569 | 1.69 (0.79–3.13) | 0.078 |
Bold values are significant at p < .05.
All analyses adjusted for age, age squared, race, and median neighborhood income. Depressive symptoms are based on the PHQ-9 survey routinely given during the first trimester of prenatal care. IPV includes a diagnosis of IPV in the EHR in the year before or during pregnancy or endorsing any of the three questions related to IPV at the beginning of prenatal care. Low resilience is based on a score below the national average (≤32) on the Connor-Davidson RISC-10 Resilience questionnaire given at the time of ACEs screening.
IPV, intimate partner violence; PHQ, Patient Health Questionnaire; OR, odds ratio; CI, confidence interval.
Stratified analyses by high and low resilience
The prevalence of each mental and behavioral health condition by dichotomous ACE category (0 vs. 1+) and resilience status is presented in Figure 2. Among the 192 women with 0 ACEs, 78 had low resilience (41%) and 114 had high resilience (59%). Among the 160 women with 1+ ACEs, 77 had low resilience (48%) and 83 had high resilience (52%). Among those with low resilience, those with 1+ versus 0 ACEs had a higher prevalence of anxiety disorders (26% vs. 9%; p = 0.01), depressive disorders (22% vs. 9%; p = 0.02), depression symptoms (46% vs. 27%; p = 0.05), and IPV (17% vs. 4%; p = 0.01), but not substance use (21% vs. 18%; p = 0.66). In contrast, among those with high resilience, having 1+ versus 0 ACEs was not significantly associated with anxiety disorders (8% vs. 6%; p = 0.54), depressive disorders (7% vs. 4%; p = 0.33), depression symptoms (23% vs. 15%; p = 0.20), or IPV (8% vs. 4%; p = 0.21), but it was associated with a higher prevalence of substance use (20% vs. 11%; p = 0.05).
FIG. 2.
Prevalence of mental and behavioral health conditions among pregnant women by ACEs and resilience. Resilience was measured by using the Connor-Davidson Resilience Scale (CD-RISC 10), which defines low resilience as ≤32 and high resilience as >32. *Significant at p < 0.05.
Results from stratified multivariable models examining resilience-specific associations between ACEs and prenatal mental and behavioral health adjusting for age, race/ethnicity, and median neighborhood income are presented in Table 3. Among women with low resilience, those with 1+ ACEs had significantly increased odds of an anxiety disorder (OR = 4.21, 95% CI = 1.54–11.50), depressive disorder (OR = 3.09, 95% CI = 1.13–8.45), and IPV (OR = 6.50, 95% CI = 1.47–28.71) relative to those with 0 ACEs. Conversely, ACEs were not significantly associated with mental and behavioral health conditions among women with high resilience.
Table 3.
Multivariable Models of Odds of Mental and Behavioral Health Conditions by Adverse Childhood Experiences and Resilience Among Pregnant Women (N = 355)
| Low resilience 1+ ACEs vs. 0 ACEs | High resilience 1+ ACEs vs. 0 ACEs | |||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Condition | ||||
| Anxiety disorder | 4.21 (1.54–11.50) | 0.005 | 1.44 (0.44–4.72) | 0.545 |
| Depressive disorder | 3.09 (1.13–8.45) | 0.027 | 2.95 (0.73–11.90) | 0.129 |
| Depression symptoms | 2.05 (0.96–4.38) | 0.086 | 1.70 (0.71–4.07) | 0.235 |
| Intimate partner violence | 6.50 (1.47–28.71) | 0.014 | 2.41 (0.66–8.84) | 0.184 |
| Prenatal substance use | 1.29 (0.54–3.10) | 0.572 | 1.99 (0.85–4.65) | 0.113 |
Bold values are significant at p < .05.
Depressive symptoms are based on the PHQ-9 survey routinely given during the first trimester of prenatal care. IPV includes a diagnosis of IPV in the EHR in the year before or during pregnancy or endorsing any of the three questions related to IPV at the beginning of prenatal care. Low resilience is based on a score below the national average (≤32), and high resilience is based on a score greater than or equal to the national average (>32) on the Connor-Davidson RISC-10 Resilience questionnaire given at the time of ACEs screening.
Discussion
This study of the association between ACEs, resilience, and mental and behavioral health conditions in pregnancy has three key findings. First, there was a dose–response relationship between ACEs and prevalence of prenatal anxiety, depression, and exposure to IPV, consistent with previous studies.18,19,32 Second, the associations between having any ACEs and mental and behavioral health conditions were stronger and significant only for women who reported low levels of resilience during pregnancy. Third, ACEs were not associated with use of cigarettes, alcohol, or marijuana during pregnancy in multivariable models, regardless of resilience.
Results from this study lend support to a small but growing body of literature suggesting that ACEs are associated with greater mental and behavioral health problems during pregnancy, including psychosocial difficulties,29 depressive symptoms,18–21 anxiety,22,23 and risk for IPV.20,30,31 Findings indicate that relative to women with 0 ACEs, women with 1–2 ACEs had between 2.4- and 3.1-fold increased odds of having an anxiety disorder, depressive disorder, or IPV during pregnancy; whereas women with 3+ ACEs had between 3.1- and 4.7-fold greater odds of having an anxiety disorder, depressive disorder, depressive symptoms, or IPV during pregnancy. Interestingly, the strongest association was between ACEs and adult IPV. This novel finding in this prenatal population is consistent with the literature suggesting that victimization in childhood increases risk for experiencing IPV in adulthood.12,15,16 The exact mediating and moderating relationships between ACEs, IPV, and mental health remain to be established.11
These results fit well with a larger body of literature surrounding the biological mechanisms underlying the connection between ACE exposure and mental and behavioral health outcomes.73 Prolonged stress exposure, particularly during the neurodevelopmentally vulnerable period of infancy through early childhood, can reprogram the physiological stress response system through epigenetic reprogramming74 and is associated with volumetric differences in stress-sensitive brain regions.75 ACE exposure is associated with molecular markers of aging and disease risk, such as telomere shortening and mitochondrial DNA copy number increases.73,76,77 These results suggest that such molecular mechanisms may impact women in the prenatal period as well, which is particularly important given the potential for intergenerational transmission of ACEs through these biological mechanisms.78
A particularly important contribution of this article is the finding that during pregnancy, resilience, or the adaptive ability to cope with adversity,46 may mitigate the negative impact of ACEs on mental and behavioral health. For example, among women with high resilience, the prevalence of an anxiety disorder was similar among those with 0 (6%) and 1+ ACE (8%). However, anxiety disorders were about three times more prevalent in women with 1+ ACEs compared with women with 0 ACEs in the low resilience group (26% vs. 9%). Similar increased prevalence was found for depressive disorders, depression symptoms, and IPV for women with 1+ ACEs compared with women with 0 ACEs in the low resilience group. Although these findings are consistent with the hypothesis that resilience may moderate the impact of childhood adversity exposure, underscoring the importance of taking resilience into account when screening for adversity, we are unable to determine the direction of these associations due to the cross-sectional nature of the study. It is also possible, for example, that mental and behavioral health problems during the prenatal period contribute to lower levels of resilience.
In contrast to prior studies that have found greater risk of prenatal substance use among women with ACEs,20,26–28 ACEs were not significantly associated with substance use upon entry to prenatal care in multivariable models regardless of resilience. Our measures of prenatal marijuana and alcohol use were based on screening at ∼8 weeks gestation, and due to the nature of our screening, we are unable to distinguish prenatal substance use before versus after women knew they were pregnant and we could not tell whether women continued to use substances throughout pregnancy. We were also not able to determine the heaviness of substance use in pregnancy, and the lack of significant association may be due to these factors. Future studies with larger samples that include more refined measures of substance use in pregnancy (e.g., quantity, frequency, trimester of use) are needed to better understand the association of ACEs with prenatal substance use.
Mitigating the effects of ACEs on mental and behavioral health will require developing and testing interventions that foster resilience in pregnancy. Interventions such as resilience training, which includes emotional regulation training, cognitive and behavioral approaches to reframe thoughts and refocus on positive emotion, improving physical health through sleep, exercise, nutrition and relaxation, social support, and mindfulness, hold promise toward building resilience.79–81 Researchers have highlighted the need for services matched to key moderators, such as resilience,82 that are responsive to intervention.83–85 Trauma-informed treatment approaches exist and data on their efficacy are growing.86 For example, psychoeducational programs designed to meet pregnancy-specific needs of women with ACEs exposure may help to improve mental and behavioral health.87 Further research is needed regarding the optimal content and timing of such programs.
Healthcare organizations have the opportunity to empower prenatal patients to cultivate their strengths and build on existing resources. This study demonstrates that ACEs and resilience screening during standard prenatal care can help clinicians identify women at risk of mental and behavioral health problems, including IPV, who may need extra support or services during pregnancy and the postpartum period. Women's health clinicians and prenatal patients should be educated about the relevance of ACEs and resilience to patients' health in pregnancy. Models integrating substance use treatment, mental health services, parenting education, family support, and other services can address these needs.88 Incorporating ACEs and resilience screening as part of standard prenatal care is feasible and generally acceptable to patients and clinicians, provided that appropriate training and adequate mental and behavioral health referral resources are available.61 Comprehensive and routine screening for ACEs, resilience, and mental and behavioral health conditions, in conjunction with interventions, resources, and treatment, is likely to have a strong return on investment when the health of both the mother and child is considered.
Additional longitudinal research is needed to investigate how obstetric and pediatric clinicians can promote perinatal resilience through screening, brief intervention, and broader systems-level changes, and to determine whether prenatal ACEs and resilience screening and intervention is associated with improved maternal or pediatric outcomes and reduced healthcare costs.
Strengths and limitations
To our knowledge, this is the first study to examine associations between ACEs and multiple mental and behavioral health conditions during pregnancy separately for women with high and low levels of resilience. KPNC's integrated healthcare delivery system and robust EHR allowed us to examine associations between self-reported exposure to ACEs and resilience assessed as part of standard prenatal care and mental and behavioral health conditions and IPV in an ethnically diverse population of pregnant women. However, several limitations should be noted. This study took place in two KPNC medical centers and was limited to English-speaking adult patients screened for ACEs at their second or third prenatal visit (at ∼14–23 weeks gestation), and results may not generalize to non-English-speaking patients, those without healthcare, and those who enter prenatal care late. Future research is needed to examine associations between ACEs, resilience, and mental and behavioral health conditions in non-English-speaking women and adolescent patients. Twelve percent of women chose not to complete the ACEs questionnaire and, although those women were similar on demographic characteristics to women who completed the screening, our study did not assess reasons for non-completion. Our measures of ACEs, resilience, and certain mental and behavioral health outcomes were based on self-report and are subject to self-report biases; however, it is noteworthy that past research indicates good test–retest reliability for ACEs.9 In addition, our ACEs questions did not assess ACEs severity, frequency, age or duration of exposure, or neglect, and all ACEs were considered equal (e.g., physical abuse was equivalent to losing a parent through divorce). We used the term “sexual abuse” in our ACEs screening, but future research should avoid emotion-laden terms such as “abuse,” which may lead to underreporting,89 and should instead use descriptive questions. In addition, due to sample size limitations, we dichotomized ACEs (0 vs. 1+) and resilience (high vs. low) in stratified analyses, which may have muted our findings. Additional studies with larger sample sizes that include more detailed information about a broader range of ACEs and more nuanced categorization of resilience are needed to better understand how childhood experiences and resilience impact mental and behavioral health. Finally, due to the cross-sectional nature of the study design, we are unable to determine causality between resilience and maternal mental and behavioral health.
Conclusions
The prenatal period has been identified as a unique window of opportunity for clinicians to impact a family's long-term health by identifying women with ACEs and providing appropriate resources.25,61 Pregnant women have increased contact with the healthcare system and are often motivated to live healthier lifestyles to improve the health of their developing child. This study adds novel data to the literature on protective factors related to maternal mental and behavioral health during pregnancy, indicating that although ACEs are important risk factors for poorer maternal mental and behavioral health in pregnancy, resilience may help mitigate this risk. Longitudinal cohort studies with larger samples will allow for greater understanding of the causal mechanisms through which ACEs and resilience combine to influence maternal behavioral health. In addition, future studies are needed to develop strategies and interventions to increase women's sense of resilience in the prenatal period and to directly test whether improvements in resilience during pregnancy reduce the adverse impact of ACEs on prenatal mental and behavioral health.
Supplementary Material
Acknowledgments
This study was supported by a Grant from the Kaiser Permanente Community Benefits Program and an NIH NIDA K01 Award (DA043604). The authors thank Carla Wicks, Fiona Sinclair, Krista Kotz, Diane Lott-Garcia, Dorothy Ferguson, and Gina Smith-Anderson for their assistance with the pilot study implementation.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Centers for Disease Control and Prevention. Adverse childhood experiences reported by adults—five states, 2009. MMWR Morb Mortal Wkly Rep 2010;59:1609–1613 [PubMed] [Google Scholar]
- 2. Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. JAMA 2001;286:3089–3096 [DOI] [PubMed] [Google Scholar]
- 3. Anda RF, Brown DW, Felitti VJ, Dube SR, Giles WH. Adverse childhood experiences and prescription drug use in a cohort study of adult HMO patients. BMC Public Health 2008;8:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci 2006;256:174–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown DW, Anda RF, Tiemeier H, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med 2009;37:389–396 [DOI] [PubMed] [Google Scholar]
- 6. Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord 2004;82:217–225 [DOI] [PubMed] [Google Scholar]
- 7. Cuijpers P, Smit F, Unger F, Stikkelbroek Y, Ten Have M, de Graaf R. The disease burden of childhood adversities in adults: A population-based study. Child Abuse Negl 2011;35:937–945 [DOI] [PubMed] [Google Scholar]
- 8. Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav 2002;27:713–725 [DOI] [PubMed] [Google Scholar]
- 9. Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: The adverse childhood experiences study. Pediatrics 2003;111:564–572 [DOI] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention. Adverse childhood experiences (ACEs). Ace Study, 2016. Available at: https://cdc.gov/violenceprevention/acestudy Accessed March3, 2018
- 11. Afifi TO, MacMillan H, Cox BJ, Asmundson GJ, Stein MB, Sareen J. Mental health correlates of intimate partner violence in marital relationships in a nationally representative sample of males and females. J Interpers Violence 2009;24:1398–1417 [DOI] [PubMed] [Google Scholar]
- 12. Bensley L, Van Eenwyk J, Wynkoop Simmons K. Childhood family violence history and women's risk for intimate partner violence and poor health. Am J Prev Med 2003;25:38–44 [DOI] [PubMed] [Google Scholar]
- 13. Fergusson DM, Boden JM, Horwood J. Developmental antecedents of interpartner violence in a New Zealand birth cohort. J Fam Violence 2008;23:737–753 [Google Scholar]
- 14. McKinney CM, Caetano R, Ramisetty-Mikler S, Nelson S. Childhood family violence and perpetration and victimization of intimate partner violence: Findings from a national population-based study of couples. Ann Epidemiol 2009;19:25–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roberts AL, McLaughlin KA, Conron KJ, Koenen KC. Adulthood stressors, history of childhood adversity, and risk of perpetration of intimate partner violence. Am J Prev Med 2011;40:128–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stith SM, Rosen KH, Middleton KA, Busch AL, Lundeberg K, Carlton RP. The intergenerational transmission of spouse abuse: A meta-analysis. J Marriage Fam 2000;62:640–654 [Google Scholar]
- 17. White HR, Widom CS. Intimate partner violence among abused and neglected children in young adulthood: The mediating effects of early aggression, antisocial personality, hostility and alcohol problems. Aggress Behav 2003;29:332–345 [Google Scholar]
- 18. Angerud K, Annerback EM, Tyden T, Boddeti S, Kristiansson P. Adverse childhood experiences and depressive symptomatology among pregnant women. Acta Obstet Gynecol Scand 2018;97:701–708 [DOI] [PubMed] [Google Scholar]
- 19. Chung EK, Mathew L, Elo IT, Coyne JC, Culhane JF. Depressive symptoms in disadvantaged women receiving prenatal care: The influence of adverse and positive childhood experiences. Ambul Pediatr 2008;8:109–116 [DOI] [PubMed] [Google Scholar]
- 20. Leeners B, Rath W, Block E, Gorres G, Tschudin S. Risk factors for unfavorable pregnancy outcome in women with adverse childhood experiences. J Perinat Med 2014;42:171–178 [DOI] [PubMed] [Google Scholar]
- 21. McDonnell CG, Valentino K. Intergenerational effects of childhood trauma: Evaluating pathways among maternal ACEs, perinatal depressive symptoms, and infant outcomes. Child Maltreat 2016;21: pii: [DOI] [PubMed] [Google Scholar]
- 22. Buist A, Gotman N, Yonkers KA. Generalized anxiety disorder: Course and risk factors in pregnancy. J Affect Disord 2011;131:277–283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Agrati D, Browne D, Jonas W, et al. Maternal anxiety from pregnancy to 2 years postpartum: Transactional patterns of maternal early adversity and child temperament. Arch Womens Ment Health 2015;18:693–705 [DOI] [PubMed] [Google Scholar]
- 24. Farber EW, Herbert SE, Reviere SL. Childhood abuse and suicidality in obstetrics patients in a hospital-based urban prenatal clinic. Gen Hosp Psychiatry 1996;18:56–60 [DOI] [PubMed] [Google Scholar]
- 25. Madigan S, Wade M, Plamondon A, Maguire JL, Jenkins JM. Maternal adverse childhood experience and infant health: Biomedical and psychosocial risks as intermediary mechanisms. J Pediatr 2017;187:282–289.e1. [DOI] [PubMed] [Google Scholar]
- 26. Frankenberger DJ, Clements-Nolle K, Yang W. The association between adverse childhood experiences and alcohol use during pregnancy in a representative sample of adult women. Womens Health Issues 2015;25:688–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chung EK, Nurmohamed L, Mathew L, Elo IT, Coyne JC, Culhane JF. Risky health behaviors among mothers-to-be: The impact of adverse childhood experiences. Acad Pediatr 2010;10:245–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nelson DB, Uscher-Pines L, Staples SR, Grisso JA. Childhood violence and behavioral effects among urban pregnant women. J Womens Health (Larchmt) 2010;19:1177–1183 [DOI] [PubMed] [Google Scholar]
- 29. Racine NM, Madigan SL, Plamondon AR, McDonald SW, Tough SC. Differential associations of adverse childhood experience on maternal health. Am J Prev Med 2018;54:368–375 [DOI] [PubMed] [Google Scholar]
- 30. Castro R, Peek-Asa C, Garcia L, Ruiz A, Kraus JF. Risks for abuse against pregnant Hispanic women: Morelos, Mexico and Los Angeles County, California. Am J Prev Med 2003;25:325–332 [DOI] [PubMed] [Google Scholar]
- 31. Huth-Bocks AC, Krause K, Ahlfs-Dunn S, Gallagher E, Scott S. Relational trauma and posttraumatic stress symptoms among pregnant women. Psychodyn Psychiatry 2013;41:277–301 [DOI] [PubMed] [Google Scholar]
- 32. Barrios YV, Gelaye B, Zhong Q, et al. Association of childhood physical and sexual abuse with intimate partner violence, poor general health and depressive symptoms among pregnant women. PLoS One 2015;10:e0116609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Maina G, Saracco P, Giolito MR, Danelon D, Bogetto F, Todros T. Impact of maternal psychological distress on fetal weight, prematurity and intrauterine growth retardation. J Affect Disord 2008;111:214–220 [DOI] [PubMed] [Google Scholar]
- 34. Field T. Prenatal depression effects on early development: A review. Infant Behav Dev 2011;34:1–14 [DOI] [PubMed] [Google Scholar]
- 35. Dieter JNI, Emory EK, Johnson KC, Raynor BD. Maternal depression and anxiety effects on the human fetus: Preliminary findings and clinical implications. Infant Ment Health J 2008;29:420–441 [DOI] [PubMed] [Google Scholar]
- 36. O'Connor TG, Heron J, Golding J, Beveridge M, Glover V. Maternal antenatal anxiety and children's behavioural/emotional problems at 4 years. Report from the Avon Longitudinal Study of Parents and Children. Br J Psychiatry 2002;180:502–508 [DOI] [PubMed] [Google Scholar]
- 37. Van den Bergh BR, Mennes M, Oosterlaan J, et al. High antenatal maternal anxiety is related to impulsivity during performance on cognitive tasks in 14- and 15-year-olds. Neurosci Biobehav Rev 2005;29:259–269 [DOI] [PubMed] [Google Scholar]
- 38. Boy A, Salihu HM. Intimate partner violence and birth outcomes: A systematic review. Int J Fertil Womens Med 2004;49:159–164 [PubMed] [Google Scholar]
- 39. Murphy CC, Schei B, Myhr TL, Du Mont J. Abuse: A risk factor for low birth weight? A systematic review and meta-analysis. CMAJ 2001;164:1567–1572 [PMC free article] [PubMed] [Google Scholar]
- 40. Rosen D, Seng JS, Tolman RM, Mallinger G. Intimate partner violence, depression, and posttraumatic stress disorder as additional predictors of low birth weight infants among low-income mothers. J Interpers Violence 2007;22:1305–1314 [DOI] [PubMed] [Google Scholar]
- 41. Silverman JG, Decker MR, Reed E, Raj A. Intimate partner violence victimization prior to and during pregnancy among women residing in 26 U.S. states: Associations with maternal and neonatal health. Am J Obstet Gynecol 2006;195:140–148 [DOI] [PubMed] [Google Scholar]
- 42. Bandstra ES, Morrow CE, Mansoor E, Accornero VH. Prenatal drug exposure: Infant and toddler outcomes. J Affect Disord 2010;29:245–258 [DOI] [PubMed] [Google Scholar]
- 43. Forray A, Foster D. Substance use in the perinatal period. Curr Psychiatry Rep 2015;17:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pollack H, Lantz PM, Frohna JG. Maternal smoking and adverse birth outcomes among singletons and twins. Am J Public Health 2000;90:395–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Leitch L. Action steps using ACEs and trauma-informed care: A resilience model. Health Justice 2017;5:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bonanno GA. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol 2004;59:20–28 [DOI] [PubMed] [Google Scholar]
- 47. Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003;18:76–82 [DOI] [PubMed] [Google Scholar]
- 48. Bolger KE, Patterson CJ. Sequelae of child maltreatment: Vulnerability and resilience. In: Luthar SS, ed. Resilience and vulnerability: Adaption in the context of childhood adversity. New York: Cambridge University Press, 2003:156–181 [Google Scholar]
- 49. Lutha SS, Cicchetti D. The construct of resilience: Implications for interventions and social policies. Dev Psychopathol 2000;12:857–885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Poole JC, Dobson KS, Pusch D. Childhood adversity and adult depression: The protective role of psychological resilience. Child Abuse Negl 2017;64:89–100 [DOI] [PubMed] [Google Scholar]
- 51. Youssef NA, Belew D, Hao G, et al. Racial/ethnic differences in the association of childhood adversities with depression and the role of resilience. J Affect Disord 2017;208:577–581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Poole JC, Dobson KS, Pusch D. Anxiety among adults with a history of childhood adversity: Psychological resilience moderates the indirect effect of emotion dysregulation. J Affect Disord 2017;217:144–152 [DOI] [PubMed] [Google Scholar]
- 53. Wingo AP, Wrenn G, Pelletier T, Gutman AR, Bradley B, Ressler KJ. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. J Affect Disord 2010;126:411–414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Beutel ME, Tibubos AN, Klein EM, et al. Childhood adversities and distress—the role of resilience in a representative sample. PLoS One 2017;12:e0173826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behav Res Ther 2006;44:585–599 [DOI] [PubMed] [Google Scholar]
- 56. Schulz A, Becker M, Van der Auwera S, et al. The impact of childhood trauma on depression: Does resilience matter? Population-based results from the Study of Health in Pomerania. J Psychosom Res 2014;77:97–103 [DOI] [PubMed] [Google Scholar]
- 57. Wingo AP, Ressler KJ, Bradley B. Resilience characteristics mitigate tendency for harmful alcohol and illicit drug use in adults with a history of childhood abuse: A cross-sectional study of 2024 inner-city men and women. J Psychiatr Res 2014;51:93–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Sexton MB, Hamilton L, McGinnis EW, Rosenblum KL, Muzik M. The roles of resilience and childhood trauma history: Main and moderating effects on postpartum maternal mental health and functioning. J Affect Disord 2015;174:562–568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Terhune C. Report: Kaiser tops state health insurance market with 40% share. Los Angeles Times; January 29, 2013. Available at: http://articles.latimes.com/2013/jan/29/business/la-fi-mo-health-insure-market-20130129 Accessed February16, 2018
- 60. Selby JV, Smith DH, Johnson ES, Raebel MA, Friedman GD, McFarland BH. Kaiser permanente medical care program. In: Strom BL, ed. Pharmacoepidemiology, 4th ed. New York: Wiley, 2005:241–259 [Google Scholar]
- 61. Flanagan T, Alabaster A, McCaw B, Stoller N, Watson C, Young-Wolff KC. Feasibility and acceptability of screening for adverse childhood experiences in prenatal care. J Womens Health (Larchmt) 2018;27:903–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Centers for Disease Control and Prevention (CDC). Behavioral risk factor surveillance system survey ACE data, 2009–2014. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2016. [Google Scholar]
- 63. Dong M, Anda RF, Felitti VJ, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl 2004;28:771–784 [DOI] [PubMed] [Google Scholar]
- 64. Bethell CD, Carle A, Hudziak J, et al. Methods to assess adverse childhood experiences of children and families: Toward approaches to promote child well-being in policy and practice. Acad Pediatr 2017;17(7S):S51–S69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017;2:e356–e366 [DOI] [PubMed] [Google Scholar]
- 66. Connor KM, Davidson JR. The Connor-Davidson Resilience Scale (CD-RISC). 2017. Available at: http://cd-risc.com/index.php Accessed March3, 2018 [DOI] [PubMed]
- 67. Li G, Kong L, Zhou H, Kang X, Fang Y, Li P. Relationship between prenatal maternal stress and sleep quality in Chinese pregnant women: The mediation effect of resilience. Sleep Med 2016;25:8–12 [DOI] [PubMed] [Google Scholar]
- 68. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Goldstein A, Gee S, Mirkin R. Tobacco dependence program: A multifaceted systems approach to reducing tobacco use among Kaiser permanente members in Northern California. Perm J 2005;9:9–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. McGinnis KA, Brandt CA, Skanderson M, et al. Validating smoking data from the Veteran's Affairs Health Factors dataset, an electronic data source. Nicotine Tob Res 2011;13:1233–1239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. McVeigh KH, Newton-Dame R, Chan PY, et al. Can electronic health records be used for population health surveillance? Validating population health metrics against established survey data. EGEMS (Wash DC) 2016;4:1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Marston L, Carpenter JR, Walters KR, et al. Smoker, ex-smoker or non-smoker? The validity of routinely recorded smoking status in UK primary care: A cross-sectional study. BMJ Open 2014;4:e004958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Ridout SJ, Ridout KK, Kao HT, et al. Telomeres, early-life stress and mental illness. Adv Psychosom Med 2015;34:92–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Tyrka AR, Ridout KK, Parade SH. Childhood adversity and epigenetic regulation of glucocorticoid signaling genes: Associations in children and adults. Dev Psychopathol 2016;28(4pt2):1319–1331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat Rev Neurosci 2016;17:652–666 [DOI] [PubMed] [Google Scholar]
- 76. Ridout KK, Carpenter LL, Tyrka AR. The cellular sequelae of early stress: Focus on aging and mitochondria. Neuropsychopharmacology 2016;41:388–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Ridout KK, Levandowski M, Ridout SJ, et al. Early life adversity and telomere length: A meta-analysis. Mol Psychiatry 2018;23:858–871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Bowers ME, Yehuda R. Intergenerational transmission of stress in humans. Neuropsychopharmacology 2016;41:232–244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Chandler GE, Roberts SJ, Chiodo L. Resilience intervention for young adults with adverse childhood experiences. J Am Psychiatr Nurses Assoc 2015;21:406–416 [DOI] [PubMed] [Google Scholar]
- 80. Bellis MA, Hardcastle K, Ford K, et al. Does continuous trusted adult support in childhood impart life-course resilience against adverse childhood experiences—a retrospective study on adult health-harming behaviours and mental well-being. BMC Psychiatry 2017;17:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Adler AB, Williams J, McGurk D, Moss A, Bliese PD. Resilience training with soldiers during basic combat training: Randomisation by platoon. Appl Psychol Health Well Being 2015;7:85–107 [DOI] [PubMed] [Google Scholar]
- 82. Meredith LS, Sherbourne CD, Gaillot SJ, et al. Promoting psychological resilience in the U.S. Military. Rand Health Q 2011;1:2. [PMC free article] [PubMed] [Google Scholar]
- 83. Shonkoff JP. Capitalizing on advances in science to reduce the health consequences of early childhood adversity. JAMA Pediatr 2016;170:1003–1007 [DOI] [PubMed] [Google Scholar]
- 84. Steinhardt M, Dolbier C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J Am Coll Health 2008;56:445–453 [DOI] [PubMed] [Google Scholar]
- 85. Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program's effect on depressive symptoms. J Consult Clin Psychol 2009;77:1042–1054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Davis R, Maul A. Trauma-informed care: Opportunities for high-need, high-cost Medicaid populations. Center for Health Care Strategies, Inc., 2015. Available at: http://chcs.org/media/TIC-Brief-031915_final.pdf Accessed March3, 2018
- 87. Rowe H, Sperlich M, Cameron H, Seng J. A quasi-experimental outcomes analysis of a psychoeducation intervention for pregnant women with abuse-related posttraumatic stress. J Obstet Gynecol Neonatal Nurs 2014;43:282–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Paull S. ACEs histories for mothers recovering from substance abuse. ACES too high, 2015. Available at: https://acestoohigh.com/2015/12/27/aces-histories-for-mothers-recovering-from-substance-abuse Accessed March27, 2018
- 89. Thombs BD, Bernstein DP, Ziegelstein RC, et al. An evaluation of screening questions for childhood abuse in 2 community samples: Implications for clinical practice. Arch Intern Med 2006;166:2020–2026 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.